Laserska fotokoagulacija za proliferativnu dijabetičku retinopatiju
References
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Jump to:
| Methods | Within‐person RCT; both eyes included in study, eyes received different treatments | |
| Participants | Country: USA Number of participants (eyes): 867 (1734) % women: 44% Average age (range): 43 years (15‐69) Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Intervention (n= 867 eyes)
Comparator (n= 867 eyes)
This trial also considered xenon arc laser but this has not been considered in this review | |
| Outcomes | Primary outcome:
Secondary outcomes:
Follow‐up: every 4 months for 5 years | |
| Notes | Date conducted: April 1972‐September 1975 Sources of funding: NIH Declaration of interest: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "One eye of each patient was randomly assigned to immediate photocoagulation and the other to follow‐up without treatment . . ." Page 583, report number 8 Further details of sequence generation are on page 158 of report number 6 |
| Allocation concealment (selection bias) | Low risk | "The sealed envelope containing the assigned treatment was not to be opened in the clinic until a final determination had been made of the patient's eligibility and the patient had signed the consent form at the second initial visit" Page 158, report number 6 |
| Blinding of participants and personnel (performance bias) | High risk | Patients and personnel will have known which eye was treated |
| Blinding of participants and personnel (performance bias) | Low risk | We judged it unlikely that patient or carer knowledge of treatment assignment would impact on the progression of diabetic retinopathy |
| Blinding of outcome assessment (detection bias) | Low risk | " . . . measurement of best corrected visual acuity by examiners who did not know the identify of the treated eye and who attempted to reduce patient bias by urging the patient to read as far down the chart as possible with each eye, guessing at letters until more than one line was missed". Page 584, report number 8 |
| Blinding of outcome assessment (detection bias) | Unclear risk | ‐ |
| Incomplete outcome data (attrition bias) | Low risk | Attrition in patients but not in unit of analysis (eyes) |
| Selective reporting (reporting bias) | Unclear risk | No access to protocol |
| Other bias | Unclear risk | ‐ |
| Methods | Within‐person RCT; both eyes included in study, eyes received different treatments | |
| Participants | Country:USA Number of participants (eyes): 3711 (7422) % women: 44% Average age 48 years (estimated; range 18‐70) Inclusion criteria:
Exclusion criteria: | |
| Interventions | Intervention (n = 3711 eyes)
Comparator (n = 3711 eyes)
For the intervention group, eyes were also randomly allocated to 'full' or 'mild' PRP. For the comparator group, argon laser was applied if high risk PDR was detected | |
| Outcomes | Primary outcome:
Secondary outcomes:
Follow‐up: every 4 months for an unknown number of years | |
| Notes | Date conducted: April 1980 to June 1985 Sources of funding: NEI Declaration of interest: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The randomization schedules were designed to provide balance in: . . . the number of right and left eyes assigned to early photocoagulation". Page 746, report number 7 |
| Allocation concealment (selection bias) | Low risk | "At the randomization visit, the Clinical Center ophthalmologist and staff reviewed the patient's . . . eligibility. . . The sealed mailer from the Coordinating Center containing the description of the photocoagulation strategy . . . was then opened." Page 746, report number 7 |
| Blinding of participants and personnel (performance bias) | High risk | Treatments were quite different and patients' perception of treatment may well have affected assessment of visual acuity |
| Blinding of participants and personnel (performance bias) | Low risk | We judged it unlikely that patient or carer knowledge of treatment assignment would impact on the progression of diabetic retinopathy |
| Blinding of outcome assessment (detection bias) | Unclear risk | "The protocol specified that visual acuity examiners be trained and certified, that they be masked from treatment assignment; that they follow standard procedures for encouraging patients to make the maximum effort to read as many letters as possible with each eye". Page 747, report number 7 |
| Blinding of outcome assessment (detection bias) | Unclear risk | "Fundus Photograph Reading Center staff, without knowledge of treatment assignments and clinical data, followed a standardized procedure to grade fundus photographs and fluorescein angiograms for individual lesions of diabetic retinopathy" Page 748, report number 7 |
| Incomplete outcome data (attrition bias) | Low risk | Attrition in patients but not in unit of analysis (eyes) |
| Selective reporting (reporting bias) | Unclear risk | No access to protocol |
| Other bias | Unclear risk | ‐ |
| Methods | Within‐person RCT; botheyes included in study, eyes received different treatments | |
| Participants | Country: UK Number of participants (eyes): 94 (188 eyes) % women: 40% Average age (range): 41 years (18‐65) Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Intervention (n = 94)
Comparator (n = 94)
| |
| Outcomes | Outcomes:
Follow‐up: 6 months | |
| Notes | Date conducted: not reported but trial 'initiated' in 1973 Sources of funding: not reported Declaration of interest: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Low risk | Not mentioned, but unlikely to be a problem in a within‐person study |
| Blinding of participants and personnel (performance bias) | High risk | Treatments are quite different and patients' perception of treatment may well affect assessment of visual acuity |
| Blinding of participants and personnel (performance bias) | Unclear risk | ‐ |
| Blinding of outcome assessment (detection bias) | Low risk | " . . . best corrected visual acuities were obtained at each visit, on subjective |
| Blinding of outcome assessment (detection bias) | Unclear risk | ‐ |
| Incomplete outcome data (attrition bias) | High risk | "Eight patients subsequently receiving treatment to the 'control' eye were removed from the study at that point." Page 556 |
| Selective reporting (reporting bias) | Unclear risk | No access to protocol |
| Other bias | Unclear risk | ‐ |
| Methods | Parallel group RCT. One eye per person enrolled; unclear how eye selected | |
| Participants | Country: Japan Number of participants (eyes): 69 (69) % women: 25% Average age: 60 years Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Intervention (n = 32)
Comparator (n = 37)
For the comparator group: "Whenever PDR developed, PRP was performed. The development of PDR was defined as the detection of any of the following: neovascularization detected by ophthalmoscope or FA and preretinal hemorrhage or vitreous hemorrhage. Therefore, in this study, PDR includes not only high‐risk PDR but also early PDR as described by the Early Treatment Diabetic Retinopathy Study Research Group (ETDRS)" Page 53 In both intervention and comparator groups: " . . . photocoagulation for macular edema was permitted when the ophthalmologist in charge of this study considered it necessary". Page 53/54 | |
| Outcomes | Primary outcome:
Secondary outcomes:
Follow‐up: 3 years | |
| Notes | Date conducted: February 2004‐December 2008 Sources of funding: "This study was supported by a Grant‐in‐Aid for Scientific Research C (no. 17591856), 2005, from the Japan Society for the Promotion of Science. The following authors have indicated that they have received grants from the Japanese Government: Sadao Hori and Naohito Yamaguchi." Page 59 Declaration of interest: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patient data and FA images in those patients considered to be appropriate subjects by the ophthalmologists in charge of this study at each institution were sent to the Data Center in the Department of Public Health, Tokyo Women’s Medical University. At the Data Center, a designated ophthalmologist confirmed whether each patient’s data and FA images were appropriate. After confirmation, the patients were randomly assigned to either the nonphotocoagulation group (non‐PC group) or to the photocoagulation group (PC group) using random number tables, and the ophthalmologists in charge of this study were informed of the groups into which their patients had been randomized." Page 53 |
| Allocation concealment (selection bias) | Low risk | "Patient data and FA images in those patients considered to be appropriate subjects by the ophthalmologists in charge of this study at each institution were sent to the Data Center in the Department of Public Health, Tokyo Women’s Medical University. At the Data Center, a designated ophthalmologist confirmed whether each patient’s data and FA images were appropriate. After confirmation, the patients were randomly assigned to either the nonphotocoagulation group (non‐PC group) or to the photocoagulation group (PC group) using random number tables, and the ophthalmologists in charge of this study were informed of the groups into which their patients had been randomized." Page 53 |
| Blinding of participants and personnel (performance bias) | High risk | Not reported and treatments different |
| Blinding of participants and personnel (performance bias) | Low risk | We judged it unlikely that patient or carer knowledge of treatment assignment would impact on the progression of diabetic retinopathy |
| Blinding of outcome assessment (detection bias) | High risk | Not reported and treatments different |
| Blinding of outcome assessment (detection bias) | High risk | Not reported and treatments different |
| Incomplete outcome data (attrition bias) | High risk | "When we discontinued the study in December 2009, the courses of 17 patients (8 in the non‐PC group and 9 in the PC group) had not yet been observed for the whole 36 months, although these patients could potentially continue to be observed for the 36 months. Of the 69 patients, 36 (23 in the non‐PC group and 13 in the PC group) completed the 36‐month follow‐up in December 2009. Another 16 patients (6 in the non‐PC group and 10 in the PC group) had dropped out of the study for the following reasons: 10 stopped coming to the hospital, 3 switched hospitals, 1 developed severe visual loss due to central retinal artery occlusion, 1 died, and 1 developed an allergy to fluorescein. As the number of patients who dropped out of the study was somewhat larger in the PC than in the non‐PC group, we conducted the analysis using the intent‐to‐treat method in all 69 patients, as well as the treatment method in 36 patients". Page 54 Outcomes of relevance to this review were largely reported on the 36 patients followed‐up to three years. Development of PDR was reported in all 69 patients as well. |
| Selective reporting (reporting bias) | Unclear risk | No access to protocol |
| Other bias | High risk | "The study was discontinued in December 2009. An analysis performed in October 2009 revealed a significantly higher incidence of PDR in the non‐PC group. Thus, the Data Monitoring Committee suggested that continuing the study without providing the results to the public would be a major disadvantage to the patients randomized to the non‐PC group." Page 54 |
| Methods | Within‐person RCT; both eyes included in study, eyes received different treatments | |
| Participants | Country: USA Number of participants (eyes): 45 (90) % women: 48% Average age (range): not reported (16‐72) Inclusion criteria: not reported but participants had "neovascularisation of the disc" i.e. PDR Exclusion criteria: not reported | |
| Interventions | Intervention (n = 45)
Comparator (n = 45)
| |
| Outcomes | Primary outcome:
Follow‐up: 4 years | |
| Notes | Date conducted: 1973‐1974 Sources of funding: not reported Declaration of interest: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | " . . . only one eye was randomly assigned to treatment" Page 78 |
| Allocation concealment (selection bias) | Low risk | Not mentioned, but unlikely to be a problem in a within‐person study |
| Blinding of participants and personnel (performance bias) | Unclear risk | ‐ |
| Blinding of participants and personnel (performance bias) | Low risk | We judged it unlikely that patient or carer knowledge of treatment assignment would impact on the progression of diabetic retinopathy |
| Blinding of outcome assessment (detection bias) | Unclear risk | ‐ |
| Blinding of outcome assessment (detection bias) | High risk | Masking not mentioned and treatments quite different |
| Incomplete outcome data (attrition bias) | High risk | "Initially we reviewed the records of 83 consecutive patients assigned for a 4‐year follow‐up, but 16 patients dropped out at various stages because of death, inadequate follow‐up, or because the 'control' eye was also treated." Page 78 |
| Selective reporting (reporting bias) | Unclear risk | No access to protocol |
| Other bias | Unclear risk | ‐ |
Abbreviations
BCVA: best corrected visual acuity
DR: diabetic retinopathy
ETDRS: Early Treatment Diabetic Retinopathy Study Research Group
FA: fluorescein angiography
NEI: National Eye Institute
NIH: National institutes for Healh
PDR: proliferative diabetic retinopathy
PRP: panretinal photocoagulation
RCT: randomised controlled trial
Characteristics of excluded studies [ordered by study ID]
Jump to:
| Study | Reason for exclusion |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| Not an RCT | |
| Laser no longer in use | |
| Not RCT | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| Laser no longer in use | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| Not an RCT | |
| No untreated or deferred laser control group | |
| Not an RCT | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| Not an RCT | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| Unable to locate reference | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| Not an RCT | |
| No untreated or deferred laser control group | |
| Not an RCT | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| Not an RCT | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| Not an RCT | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| Not an RCT | |
| Not an RCT | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| Not an RCT | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| Laser no longer in use | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| Not an RCT | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group | |
| No untreated or deferred laser control group |
Abbreviation
RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
Jump to:
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Currently unable to source a copy of the article |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Currently unable to source a copy of the article |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Awaiting a translation of the report of the study |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Awaiting a translation of the report of the study |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Currently unable to source a copy of the article |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Currently unable to source a copy of the article |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Awaiting a translation of the report of the study |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Awaiting a translation of the report of the study |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Awaiting a translation of the report of the study |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Awaiting a translation of the report of the study |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Currently unable to source a copy of the article |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Awaiting a translation of the report of the study |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Awaiting a translation of the report of the study |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Loss of 15 or more letters BCVA at 12 months Show forest plot | 2 | 8926 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.89, 1.11] |
| Analysis 1.1  Comparison 1 Laser photocoagulation versus control, Outcome 1 Loss of 15 or more letters BCVA at 12 months. | ||||
| 2 Loss of 15 or more letters BCVA at 2 years Show forest plot | 2 | 8306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.80, 0.97] |
| Analysis 1.2  Comparison 1 Laser photocoagulation versus control, Outcome 2 Loss of 15 or more letters BCVA at 2 years. | ||||
| 3 Loss of 15 or more letters BCVA at 3 years Show forest plot | 2 | 7458 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.93, 1.23] |
| Analysis 1.3  Comparison 1 Laser photocoagulation versus control, Outcome 3 Loss of 15 or more letters BCVA at 3 years. | ||||
| 4 Severe visual loss (BCVA < 6/60) Show forest plot | 4 | 9276 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.24, 0.86] |
| Analysis 1.4  Comparison 1 Laser photocoagulation versus control, Outcome 4 Severe visual loss (BCVA < 6/60). | ||||
| 5 Progression of diabetic retinopathy Show forest plot | 4 | 8331 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.37, 0.64] |
| Analysis 1.5  Comparison 1 Laser photocoagulation versus control, Outcome 5 Progression of diabetic retinopathy. | ||||
| 6 Vitreous haemorrhage Show forest plot | 2 | 224 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.37, 0.85] |
| Analysis 1.6  Comparison 1 Laser photocoagulation versus control, Outcome 6 Vitreous haemorrhage. | ||||

Results from searching for studies for inclusion in the review

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Laser photocoagulation versus control, outcome: 1.1 Loss of 15 or more letters BCVA at 12 months

Forest plot of comparison: 1 Laser photocoagulation versus control, outcome: 1.4 Severe visual loss (BCVA < 6/60)
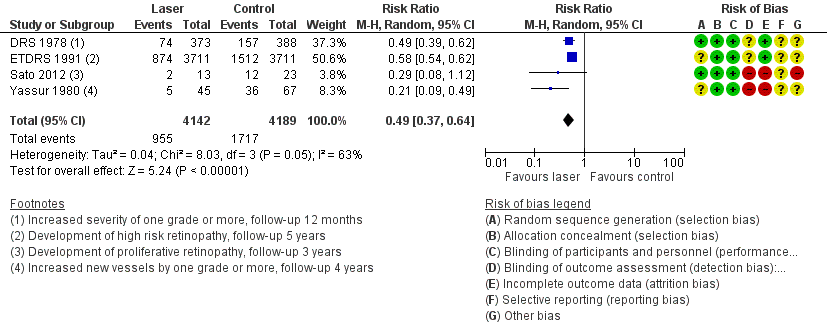
Forest plot of comparison: 1 Laser photocoagulation versus control, outcome: 1.5 Progression of diabetic retinopathy

Comparison 1 Laser photocoagulation versus control, Outcome 1 Loss of 15 or more letters BCVA at 12 months.

Comparison 1 Laser photocoagulation versus control, Outcome 2 Loss of 15 or more letters BCVA at 2 years.

Comparison 1 Laser photocoagulation versus control, Outcome 3 Loss of 15 or more letters BCVA at 3 years.

Comparison 1 Laser photocoagulation versus control, Outcome 4 Severe visual loss (BCVA < 6/60).

Comparison 1 Laser photocoagulation versus control, Outcome 5 Progression of diabetic retinopathy.

Comparison 1 Laser photocoagulation versus control, Outcome 6 Vitreous haemorrhage.
| Laser photocoagulation compared to no treatment (or deferred treatment) for diabetic retinopathy | ||||||
| Patient or population: people with diabetic retinopathy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk* | Corresponding risk | |||||
| No treatment or deferred treatment | Laser photocoagulation | |||||
| Loss of 15 or more letters BCVA Follow‐up: 12 months | Low risk (non‐proliferative DR) | RR 0.99 | 8926 | ⊕⊕⊝⊝ | The pooled RR 0.99 (0.89 to 1.11) is derived from one study with mainly low risk population RR 1.07 (0.92 to 1.23) and one study with mainly high risk population 0.86 (0.71 to 1.04) | |
| 100 per 1000 | 99 per 1000 | |||||
| High risk (proliferative DR) | ||||||
| 250 per 1000 | 248 per 1000 | |||||
| BCVA measured using logMAR acuity (0 = 6/6 visual acuity, higher score is worse visual acuity) Follow‐up: 12 months | The mean BCVA at 12 months in the control group was 0.12 logMAR | The mean BCVA at 12 months in the intervention group was 0.02 logMAR units higher (worse; 0.23 lower to 0.27 higher) | 36 | ⊕⊕⊝⊝ | ||
| Severe visual loss (BCVA < 6/60) Follow‐up: 12 months | Low risk (non‐proliferative DR) | RR 0.46 | 9276 | ⊕⊕⊕⊝ | ||
| 10 per 1000 | 5 per 1000 | |||||
| High risk (proliferative DR) | ||||||
| 50 per 1000 | 23 per 1000 | |||||
| Progression of diabetic retinopathy Follow‐up: 12 months | Low risk (non‐proliferative DR) | RR 0.49 | 8331 | ⊕⊕⊝⊝ | ||
| 100 per 1000 | 49 per 1000 | |||||
| High risk (proliferative DR) | ||||||
| 400 per 1000 | 196 per 1000 (148 to 256) | |||||
| Quality of life Follow‐up: 12 months | See comment | See comment | No studies reported this outcome | |||
| Pain Follow‐up: at time of treatment | See comment | See comment | No studies reported this outcome | |||
| Loss of driving licence Follow‐up: within three months of treatment | See comment | See comment | No studies reported this outcome | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| *Estimates of assumed risk are indicative only, as estimates at 12 months were not available in all studies. For the low risk populations they were estimated from ETDRS (but acknowledging that the control group received deferred laser) and for the high risk populations they were estimated from DRS and Hercules 1977. 1Downgraded for risk of bias (‐1): studies were not masked and treatment groups different 2Downgraded for inconsistency (‐1): I2 = 69% and effect estimates were in different directions. See comments for details 3Downgraded for imprecision (‐1): wide confidence intervals 4 There was heterogeneity (I2 = 70%) but all effect estimates favoured laser photocoagulation so we did not downgrade for inconsistency 5Downgraded for indirectness (‐1): study results were reported at 1, 3, 4 and 5 years | ||||||
| Study | Type of laser | Type of photocoagulation | Number (size) of burns | Intensity | Exposure time (seconds) | Number of sessions |
| Argon | Panretinal Focal treatment of new vessels | 800‐1600 (500 µm) or 500‐1000 (1000 µm) | Not reported | 0.1 | 1 (usually) | |
| Argon | Panretinal | Full: 1200‐1600 (500 µm) Mild: 400‐650 (500 µm) | Moderate | 0.1 | Full: 2 or more Mild: 1 | |
| Argon | Panretinal | 800 to 3000 (200 µm and 500 µm) | Minimal retinal blanching | Not reported | Up to 6 | |
| Not reported | Selective photocoagulation of non‐perfusion areas | (400 µm‐500 µm) | Not reported | Not reported | ||
| Argon | Panretinal | As for DRS 1978 | As for DRS 1978 | As for DRS 1978 | As for DRS 1978 |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Loss of 15 or more letters BCVA at 12 months Show forest plot | 2 | 8926 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.89, 1.11] |
| 2 Loss of 15 or more letters BCVA at 2 years Show forest plot | 2 | 8306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.80, 0.97] |
| 3 Loss of 15 or more letters BCVA at 3 years Show forest plot | 2 | 7458 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.93, 1.23] |
| 4 Severe visual loss (BCVA < 6/60) Show forest plot | 4 | 9276 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.24, 0.86] |
| 5 Progression of diabetic retinopathy Show forest plot | 4 | 8331 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.37, 0.64] |
| 6 Vitreous haemorrhage Show forest plot | 2 | 224 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.37, 0.85] |

