Fármacos perioperatorios para la prevención del aumento temporal de la presión intraocular después de la trabeculoplastia con láser
Information
- DOI:
- https://doi.org/10.1002/14651858.CD010746.pub2Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 23 February 2017see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Eyes and Vision Group
- Copyright:
-
- Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
The protocol for this review was written by LZ with significant contributions from JW and DM.
Screening and data extraction: LZ and JW with assistance from CEV staff Elizabeth Clearfield (EC), Sueko Ng, and Nan Zhang.
Data checking and entering: EC.
Data reviewed: LZ.
Writing: LZ and EC with contributions from JW and DM.
Sources of support
Internal sources
-
No sources of support supplied
External sources
-
Grant 1 U01 EY020522, National Eye Institute, National Institutes of Health, USA.
Funding for methodological support from the Cochrane Eyes and Vision US Project
-
National Institute for Health Research (NIHR), UK.
-
Richard Wormald, Co‐ordinating Editor for Cochrane Eyes and Vision (CEV) acknowledges financial support for his CEV research sessions from the Department of Health through the award made by the National Institute for Health Research to Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology for a Specialist Biomedical Research Centre for Ophthalmology.
-
The NIHR also funds the CEV Editorial Base in London.
The views expressed in this publication are those of the authors and not necessarily those of the NIHR, NHS, or the Department of Health.
-
Declarations of interest
LZ none known.
JW none known.
DM none known.
Acknowledgements
We acknowledge the Cochrane Eyes and Vision (CEV) US Project for providing methodological support and for developing and conducting the search strategies. We also thank Barbara Hawkins, Stefano Miglior, and Augusto Azuara‐Blanco for comments to the review drafts.
Version history
| Published | Title | Stage | Authors | Version |
| 2017 Feb 23 | Perioperative medications for preventing temporarily increased intraocular pressure after laser trabeculoplasty | Review | Linda Zhang, Jennifer S Weizer, David C Musch | |
| 2013 Sep 11 | Perioperative medications for preventing temporarily increased intraocular pressure after laser trabeculoplasty | Protocol | Linda Zhang, Jennifer S Weizer, David C Musch | |
Differences between protocol and review
We added the methods for the 'Summary of findings' tables and GRADE assessment that were not included in the original protocol. We were unable to use some methods and perform some analyses we had outlined in the protocol (Zhang 2013). For example, we had planned to conduct sensitivity analyses to assess the influence of industry‐funded studies, studies with missing data, and studies assessed as having a high risk of selection or attrition bias, but selection and attrition bias were not major concerns among our included studies. We had also planned a sensitivity analysis to remove industry‐funded studies, but the majority of the studies contributing data to our analyses were industry‐funded, and removing them would leave too few data to draw any conclusions.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Adrenergic alpha‐2 Receptor Agonists [therapeutic use];
- Antihypertensive Agents [adverse effects, *therapeutic use];
- Brimonidine Tartrate [therapeutic use];
- Clonidine [analogs & derivatives, therapeutic use];
- Conjunctiva [drug effects];
- Glaucoma, Open‐Angle [*surgery];
- Intraocular Pressure [*drug effects];
- Ocular Hypertension [*prevention & control];
- Pilocarpine [therapeutic use];
- Postoperative Complications [*prevention & control];
- Randomized Controlled Trials as Topic;
- Trabeculectomy [*adverse effects];
Medical Subject Headings Check Words
Humans;
PICOs

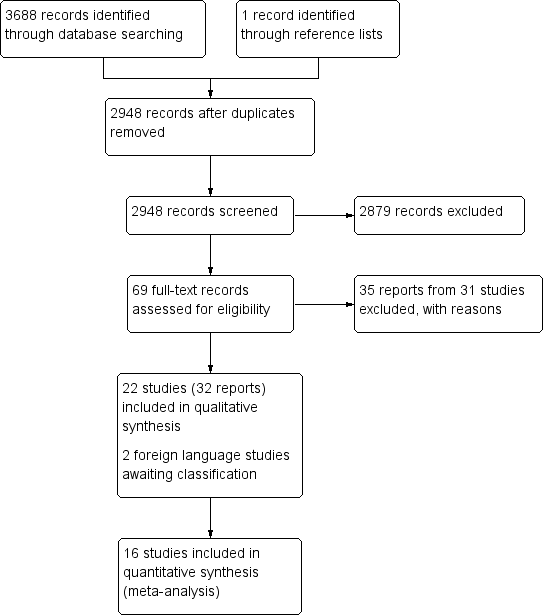
Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.
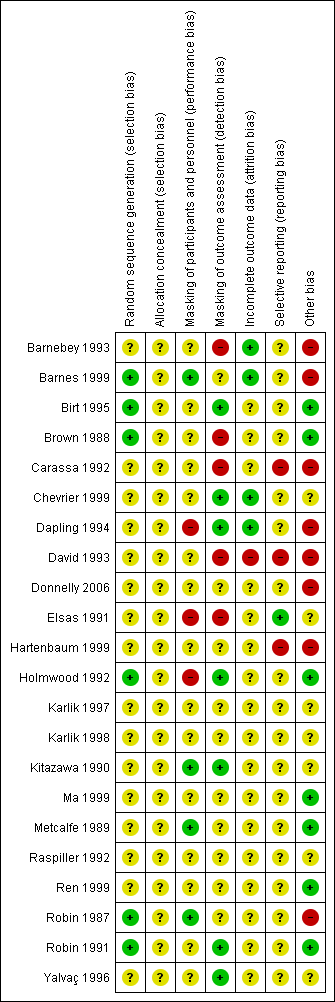
Risk of bias summary: review authors' judgments about each risk of bias item for each included study.

Forest plot of comparison: 1 Medication versus placebo (regardless of timing), outcome: 1.4 Intraocular pressure (IOP) increase ≥ 5 mmHg two to 24 hours after laser trabeculoplasty (LTP).

Forest plot of comparison: 3 Medication versus medication: apraclonidine versus pilocarpine (regardless of timing), outcome: 3.2 Intraocular pressure (IOP) increase of ≥ 5 mmHg two to 24 after laser trabeculoplasty (LTP).
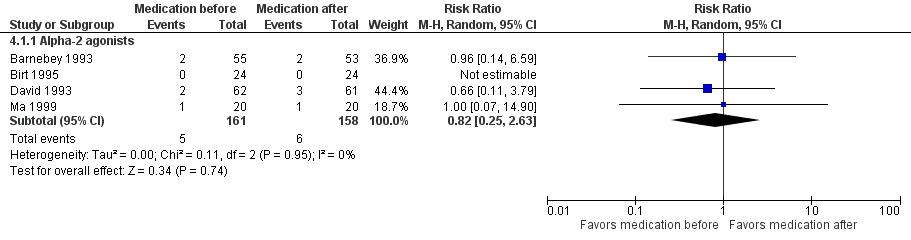
Forest plot of comparison: 4 Timing comparison: medication before versus medication after, outcome: 4.1 Intraocular pressure (IOP) increase of ≥ 5 mmHg two to 24 hours after laser trabeculoplasty (LTP).
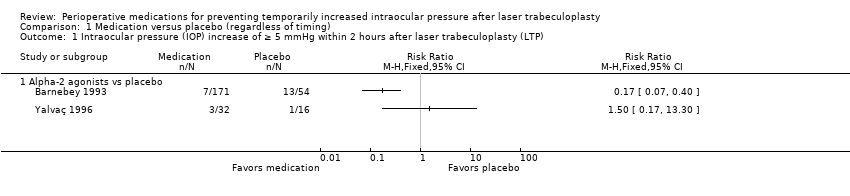
Comparison 1 Medication versus placebo (regardless of timing), Outcome 1 Intraocular pressure (IOP) increase of ≥ 5 mmHg within 2 hours after laser trabeculoplasty (LTP).

Comparison 1 Medication versus placebo (regardless of timing), Outcome 2 IOP increase of ≥ 10 mmHg within 2 hours after LTP.

Comparison 1 Medication versus placebo (regardless of timing), Outcome 3 Mean change in IOP from pre‐LTP to measurements taken within 2 hours after LTP.
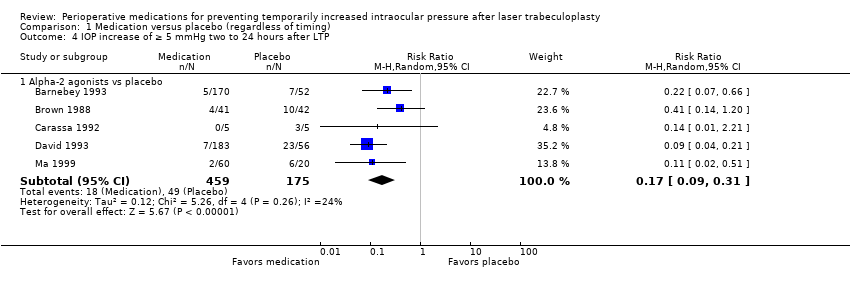
Comparison 1 Medication versus placebo (regardless of timing), Outcome 4 IOP increase of ≥ 5 mmHg two to 24 hours after LTP.
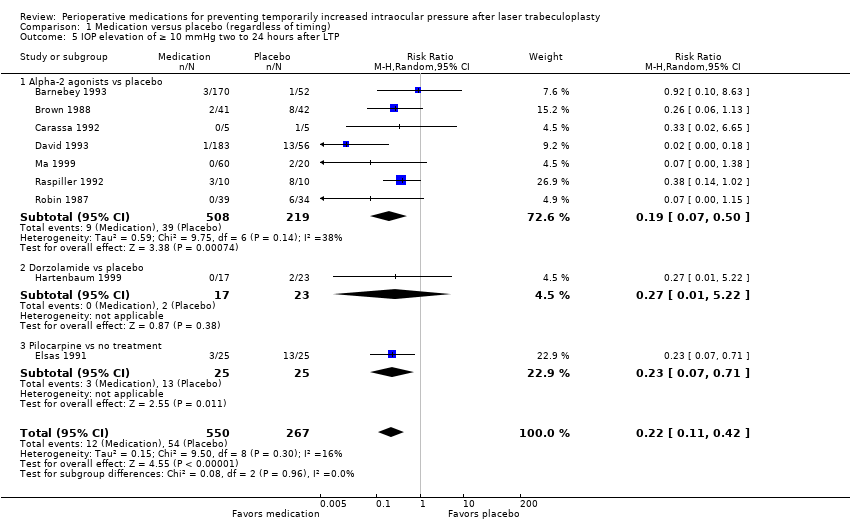
Comparison 1 Medication versus placebo (regardless of timing), Outcome 5 IOP elevation of ≥ 10 mmHg two to 24 hours after LTP.

Comparison 1 Medication versus placebo (regardless of timing), Outcome 6 Mean change in IOP from pre‐LTP to measurements two to 24 hours after LTP.
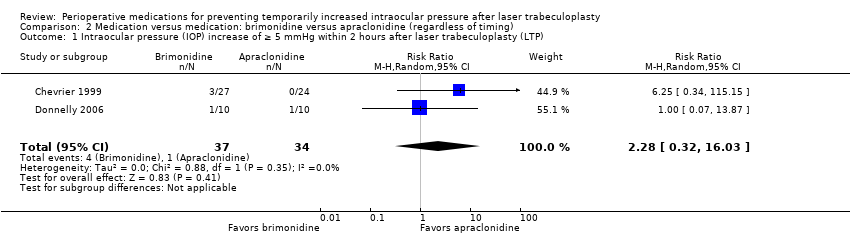
Comparison 2 Medication versus medication: brimonidine versus apraclonidine (regardless of timing), Outcome 1 Intraocular pressure (IOP) increase of ≥ 5 mmHg within 2 hours after laser trabeculoplasty (LTP).

Comparison 2 Medication versus medication: brimonidine versus apraclonidine (regardless of timing), Outcome 2 Mean change in IOP from pre‐LTP to measurements taken within 2 hours after LTP (mmHg).

Comparison 3 Medication versus medication: apraclonidine versus pilocarpine (regardless of timing), Outcome 1 Mean change in intraocular pressure (IOP) from pre‐laser trabeculoplasty (LTP) to measurements taken within 2 hours after LTP (mmHg).

Comparison 3 Medication versus medication: apraclonidine versus pilocarpine (regardless of timing), Outcome 2 IOP increase of ≥ 5 mmHg two to 24 hours after LTP.

Comparison 3 Medication versus medication: apraclonidine versus pilocarpine (regardless of timing), Outcome 3 IOP increase of ≥ 10 mmHg two to 24 hours after LTP.
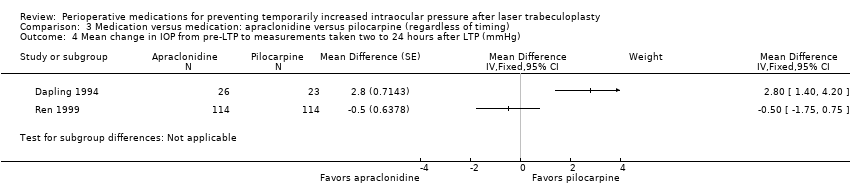
Comparison 3 Medication versus medication: apraclonidine versus pilocarpine (regardless of timing), Outcome 4 Mean change in IOP from pre‐LTP to measurements taken two to 24 hours after LTP (mmHg).

Comparison 4 Timing comparison: medication before versus medication after, Outcome 1 Intraocular pressure (IOP) increase of ≥ 5 mmHg two to 24 hours after laser trabeculoplasty (LTP).
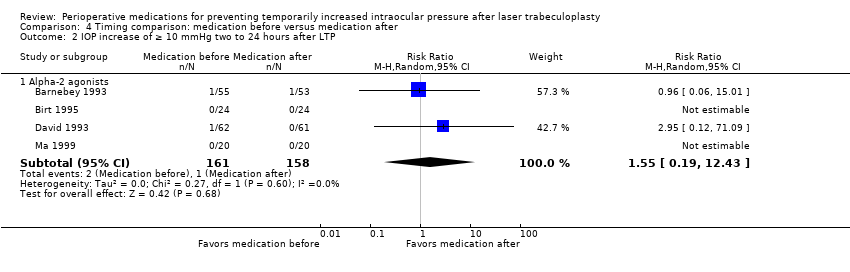
Comparison 4 Timing comparison: medication before versus medication after, Outcome 2 IOP increase of ≥ 10 mmHg two to 24 hours after LTP.

Comparison 4 Timing comparison: medication before versus medication after, Outcome 3 Mean change in IOP from pre‐LTP to measurements taken more than 2 hours but within 24 hours after LTP (mmHg).

Comparison 5 Adverse events, Outcome 1 Conjunctival blanching (brimonidine vs placebo).
| Medication compared with placebo for preventing temporarily increased IOP after LTP | ||||||
| Participant or population: people with glaucoma receiving LTP Intervention: IOP‐lowering medication (apraclonidine, acetazolamide, brimonidine, pilocarpine) Comparison: placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo | Medication | |||||
| IOP increase of ≥ 5 mmHg within 2 hours | See comment | ‐ | 273 | ⊕⊕⊝⊝1,2 | Medications in this comparison were apraclonidine and brimonidine. 2 studies reported on this outcome and 1 favored the alpha‐2 agonists while the other favored placebo. Due to significant statistical heterogeneity (I2 = 70%), we did not perform a meta‐analysis. | |
| IOP increase of ≥ 10 mmHg within 2 hours | 195 per 1000 | 10 per 1000 | RR 0.05 (0.01 to 0.20) | 446 | ⊕⊕⊕⊝1 | Medications in this comparison were acetazolamide, apraclonidine, and brimonidine. |
| Mean change in IOP from pre‐LTP within 2 hours | The mean change in IOP ranged across control groups from0.4 mmHg to 4.40 mmHg, for 3 included studies | The mean change in IOP in the intervention groups was 7.43 mmHg lower | ‐ | 151 | ⊕⊕⊕⊝1 | Each of the studies included in this outcome compared apraclonidine vs placebo. |
| IOP increase of ≥ 5 mmHg between 2 and 24 hours | 280 per 1000 | 48 per 1000 | RR 0.17 (0.09 to 0.31) | 634 | ⊕⊕⊝⊝3 Low | Medications in this comparison were apraclonidine and brimonidine. |
| IOP increase of ≥ 10 mmHg between 2 and 24 hours | 202 per 1000 | 44 per 1000 | RR 0.22 (0.11 to 0.42) | 817 | ⊕⊝⊝⊝3,4 | Medications in this comparison were apraclonidine, brimonidine, dorozolamide, and pilocarpine. |
| Mean change in IOP from pre‐LTP between 2 and 24 hours | The mean change in IOP ranged across control groups from‐2.0 mmHg to 0.63 mmHg, for 3 included studies | The mean change in IOP in the intervention groups was 5.32 mmHg lower | ‐ | 151 | ⊕⊕⊕⊝1 | Each of the studies included in this outcome compared apraclonidine vs placebo. |
| Adverse events ‐ conjunctival blanching during study period | See comment | ‐ | 319 (2 studies) | ⊕⊕⊕⊝1 | 2 studies reported on conjunctival blanching; however, due to significant statistical heterogeneity (I2 = 95%), we did not perform a meta‐analysis. In both studies, conjunctival blanching was reported in more participants in the group that received an alpha‐2 agonist compared with participants who received placebo. 1 other study that reported only the range of participants who had conjunctival blanching also reported that this adverse event was more frequent in the groups receiving brimonidine vs placebo. Other adverse events reported for the comparison of medication vs placebo were lid retraction and conjunctival hyperemia, reported in 1 study each. | |
| *The basis for the assumed risk is the control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 The certainty of the evidence was downgraded due to concerns of risk of bias: masking of outcomes assessors was difficult and in one study, the authors of some studies worked with the company making the study drug. 2 The certainty of the evidence was downgraded due to inconsistency of the outcome measurements in the individual studies: one favored medication and one favored placebo. 3 The certainty of the evidence was downgraded two levels due to concerns of very serious plausible bias: some studies in these analyses had issues with masking of outcomes assessors, high risk of selective reporting, and authors associated with the manufacturer of the study drug. 4 The certainty of the evidence was downgraded due to imprecision: there is a small number of events in the medication groups. | ||||||
| Brimonidine compared with apraclonidine for preventing temporarily increased IOP after LTP | ||||||
| Participant or population: people with glaucoma receiving LTP Intervention: brimonidine Comparison: apraclonidine | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Apraclonidine | Brimonidine | |||||
| IOP increase of ≥ 5 mmHg within 2 hours | 29 per 1000 | 67 per 1000 | RR 2.28 (0.32 to 16.03) | 71 | ⊕⊝⊝⊝1,2,3 | 1 other study reported this outcome but found that no participants in either study group had an IOP increase of ≥ 5 mmHg. This study was not included in the meta‐analysis. |
| IOP increase of ≥ 10 mmHg within 2 hours | See comment | ‐ | ‐ | ‐ | 1 study reported that no participants given either medication had an IOP increase of ≥ 10 mmHg. Another study reported that only 1 eye that had received apraclonidine had an IOP spike > 10 mmHg, but this was not statistically significant given the size of the study (RR 0.33, 95% CI 0.02 to 7.32). | |
| Mean change in IOP from pre‐LTP within 2 hours | The mean change in IOP ranged across control groups from‐4.29 to ‐5.00 mmHg | The mean change in IOP in the intervention groups was 0.69 mmHg lower (2.56 lower to 1.17 higher) | ‐ | 71 | ⊕⊕⊕⊝3 | ‐ |
| IOP increase of ≥ 5 mmHg between 2 and 24 hours | This outcome was not reported for this comparison. | |||||
| IOP increase of ≥ 10 mmHg between 2 and 24 hours | This outcome was not reported for this comparison. | |||||
| Mean change in IOP from pre‐LTP between 2 and 24 hours | See comment | ‐ | ‐ | ‐ | 1 study reported that participants randomized to receive brimonidine had a mean (± SD) IOP reduction of 2.6 ± 3.6 mmHg, while participants randomized to receive apraclonidine had a mean IOP reduction of 2.3 ± 3.7 mmHg (MD ‐0.30 mmHg, 95% CI ‐2.41 to 1.81). | |
| Adverse events ‐ during study period | This outcome was not reported for this comparison. | |||||
| *The basis for the assumed risk is the control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 The certainty of the evidence was downgraded two levels due to imprecision: our effect measurement had a very wide confidence interval. 2 The certainty of the evidence was downgraded due to inconsistency: the RRs of the individual trials were very different. 3 The certainty of the evidence was downgraded due to concerns of risk of bias: masking of participants and personnel was unclear, and in one study, both eyes of the participants were included in the study and received different medications but the authors did not report if and how they took into account the interdependability of eyes. | ||||||
| Apraclonidine compared with pilocarpine for temporarily increased IOP after LTP | ||||||
| Participant or population: people with glaucoma receiving LTP Intervention: apraclonidine Comparison: pilocarpine | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Pilocarpine | Apraclonidine | |||||
| IOP increase of ≥ 5 mmHg within 2 hours | See comment | ‐ | ‐ | ‐ | 1 study reported that 8.8% of the apraclonidine group had an increase of ≥ 5 mmHg vs 4.4% of the pilocarpine group. These were not statistically different (RR 2.00, 95% CI 0.71 to 5.67). | |
| IOP increase of ≥ 10 mmHg within 2 hours | This outcome was not reported for this comparison. | |||||
| Mean change in IOP from pre‐LTP within 2 hours | The mean change in IOP was only reported in 1 study: ‐3.6 mmHg. The second study reported only the mean IOP at a time point rather than the mean change | The mean change in IOP in the intervention groups was 0.61 mmHg higher (0.44 lower to 1.66 higher) | ‐ | 277 | ⊕⊕⊕⊝1 | ‐ |
| IOP increase of ≥ 5 mmHg between 2 and 24 hours | See comment. | ⊕⊕⊝⊝1, 2 | 2 studies reported on this outcome and 1 favored apraclonidine while the other favored pilocarpine. Due to significant statistical heterogeneity (I2 = 91%), we did not perform a meta‐analysis. | |||
| IOP increase of ≥ 10 mmHg between 2 and 24 hours | 13 per 1000 | 12 per 1000 | RR 0.87 (0.14 to 5.63) | 390 | ⊕⊕⊝⊝2,3 | 1 additional study reported on this outcome but found that no participants in either study group had an IOP increase of ≥ 10 mmHg. This study was not included in the meta‐analysis. |
| Mean change in IOP from pre‐LTP between 2 and 24 hours | See comment. | ‐ | 277 | ⊕⊕⊝⊝1, 2 | 2 studies reported on this outcome and 1 favored apraclonidine while the other favored pilocarpine. Due to significant statistical heterogeneity (I2 = 92%), we did not perform a meta‐analysis. | |
| Adverse events ‐ during study period | This outcome was not reported for this comparison. | |||||
| *The basis for the assumed risk is the control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 The certainty of the evidence was downgraded due to concerns of plausible bias: one study included in the analyses had issues with masking of their participants due to the nature of the study design, and additionally the authors were employees of the company that manufactured the study drug. 2 The certainty of the evidence was downgraded due to inconsistency: in each outcome analysis, one study favored pilocarpine while the other favored apraclonidine. 3 The certainty of the evidence was downgraded due to imprecision: our effect measurement had a very wide confidence interval. | ||||||
| Medication given before LTP compared with the same medication given after LTP for temporarily increased IOP after LTP | ||||||
| Participant or population: people with glaucoma receiving LTP Intervention: medication before LTP Comparison: medication after LTP | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Medication after LTP | Medication before LTP | |||||
| IOP increase of ≥ 5 mmHg within 2 hours | See comment | ‐ | ‐ | ‐ | 1 study comparing apraclonidine given before and after surgery reported no participants had an increase of ≥ 5 mmHg. Another study reported that 5.3% of participants given brimonidine before surgery had an IOP increase of ≥ 5 mmHg, compared with 7.5% of participants given brimonidine after surgery (RR 0.70, 95% CI 0.16 to 2.97). | |
| IOP increase of ≥ 10 mmHg within 2 hours | See comment | ‐ | ‐ | ‐ | 1 study comparing apraclonidine given before and after surgery reported no participants had an increase of ≥ 10 mmHg. Another study reported that only 1 study participant had this high of an increase, and they had been randomized to brimonidine before surgery. | |
| Mean change in IOP from pre‐LTP within 2 hours | See comment | ‐ | ‐ | ‐ | Mean change in IOP from pre‐LTP to measurements taken within 2 hours after LTP was not reported in any study, but 1 study did report the mean IOP for the 2 study arms within 2 hours and it was not statistically different between the 2 groups. | |
| IOP increase of ≥ 5 mmHg between 2 and 24 hours | 38 per 1000 | 31 per 1000 | RR 0.82 (0.25 to 2.63) | 319 | ⊕⊕⊕⊝1 | ‐ |
| IOP increase of ≥ 10 mmHg between 2 and 24 hours | 6 per 1000 | 10 per 1000 | RR 1.55 (0.19 to 12.43) | 319 | ⊕⊝⊝⊝1,2 | ‐ |
| Mean change in IOP from pre‐LTP between 2 and 24 hours | The mean change in IOP was only reported in 1 study: ‐3.4 mmHg. The other 2 studies reported only the mean IOP at a time point rather than the mean change: range was13.0 mmHg to 18.6 mmHg | The mean change in IOP in the intervention groups was 1.07 mmHg lower (2.51 lower to 0.37 higher) | ‐ | 198 | ⊕⊕⊕⊝3 | ‐ |
| Adverse events ‐ during study period | This outcome was not reported for this comparison. | |||||
| *The basis for the assumed risk is the control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 The certainty of the evidence was downgraded due to concerns of plausible bias: masking of outcomes assessors was difficult and the authors of two studies work with the company making the study drug; one study had a high risk of selective reporting bias. 2 The certainty of the evidence was downgraded two levels due to imprecision: the included studies for which data were available had very wide confidence intervals. 3 The certainty of the evidence was downgraded due to inconsistency: of the three included studies, two favored medication given before surgery, and the other favored medication given after surgery. | ||||||
| Study ID | Types of participants | Number of treatment groups | Type of trabeculoplasty | Degree of laser | Comparison (baseline IOP in mmHg) |
| Uncontrolled glaucoma | 4 | ALT | 360 | Brimonidine before and after vs brimonidine before and vehicle after vs vehicle before and brimonidine after vs vehicle before and after (individual baseline IOPs not reported; range 23.4 ± 0.6 to 24.3 ± 0.7) | |
| POAG, pigmentary glaucoma, pseudoexfoliation syndrome, or ocular hypertension | 2 | ALT | 360 | Brimonidine (19.6 ± 4.5) vs apraclonidine (20.5 ± 4.6) | |
| POAG | 3 | ALT | 180 | Apraclonidine before and after (22.2 ± 3.6) vs apraclonidine before (23.9 ± 5.3) vs apraclonidine after (22.1 ± 3.2) | |
| Inadequately controlled IOP despite maximum‐tolerated medical therapy | 2 | ALT | 360 | Apraclonidine before and after vs placebo before and after (IOPs not available) | |
| Advanced glaucoma on maximal tolerated medical therapy with inadequate IOP control | 2 | ALT | 360 | Apraclonidine before and after (19.20 ± 5.95) vs placebo before and after (19.80 ± 5.23) | |
| Candidates for ALT, peripheral iridectomy, or posterior capsulotomy | 2 | ALT | 180 | Brimonidine before (20.3 ± 6) vs apraclonidine before (20.0 ± 5.1) *the reported IOPs included participants who received other types of glaucoma surgery besides ALT | |
| OAG | 3 (1 combination group not of interest in this study) | ALT | 180 | Apraclonidine before and after vs pilocarpine after ("all eyes had...an IOP greater than 21mmHg") | |
| Participants undergoing ALT | 4 | ALT | 360 | Brimonidine before and after (23.3) vs brimonidine before, placebo after (23.9) vs placebo before, brimonidine after (24.1) vs placebo before and after (24.0) | |
| POAG | 2 (opposite eyes) | SLT | 360 | Brimonidine before vs apraclonidine after (right eyes: 18, left eyes: 18.4) | |
| Exfoliative glaucoma and simple glaucoma | 2 | ALT | 360 | Pilocarpine before (34.9 ± 8.1) vs no treatment (33.3 ± 5.6) | |
| OAG requiring ALT | 2 | ALT | 180 | Dorzolamide before and after (18.3 ± 0.57) vs placebo before and after (19.6 ± 0.72) | |
| OAG | 2 | ALT | 360 | Apraclonidine before and after (22.6 ± 0.9) vs apraclonidine after (22.6 ± 0.6) | |
| Glaucoma | 2 | ALT | 180 | Latanoprost before (24.1) vs apraclonidine before (23.2) | |
| Glaucoma | 2 | ALT | 180 | Latanoprost before vs apraclonidine before | |
| POAG | 2 | ALT | 180 | Apraclonidine before and after (24.2 ± 9.0) vs placebo before and after (23.2 ± 6.8) | |
| Glaucoma | 4 | ALT | 180 | Brimonidine before and after (24.9) vs brimonidine before, placebo after (24.8) vs placebo before, brimonidine after (24.1) vs placebo before and after (24.6) | |
| Uncontrolled OAG | 2 | ALT | 180 | Acetazolamide before (23.6 ± 6.1) vs placebo before (23.7 ± 6.5) | |
| POAG | 2 | ALT | 360 | ALO 2145 (apraclonidine) before and after (20.1 ± 4.07) vs placebo before and after (25.0 ± 5.47) | |
| POAG | 2 | ALT | 180 | Apraclonidine before (23.2 ± 4.5) vs pilocarpine before (21.7 ± 3.5) | |
| OAG | 2 | ALT | 360 | ALO 2145 (apraclonidine) before and after (26.4 ± 3.0) vs placebo before and after (27.9 ± 6.9) | |
| OAG with disc and visual field damage | 5 | ALT | 360 | Apraclonidine before and after (27.2 ± 5.1) vs timolol before and after (27.6 ± 4.1) vs pilocarpine before and after (27.1 ± 5.1) vs dipivefrin before and after (25.9 ± 3.0) vs acetazolamide before and after (25.7 ± 3.9) | |
| POAG | 3 | ALT | 360 and 180 | Apraclonidine before and after, 180° ALT (26.1 ± 5.1) vs placebo before and after, 180° ALT (25.6 ± 3.4) vs apraclonidine before and after, 360° ALT (26.4 ± 3.1) | |
| ALT: argon laser trabeculoplasty; IOP: intraocular pressure; OAG: open‐angle glaucoma; POAG: primary open‐angle glaucoma; SLT: selective laser trabeculoplasty. | |||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intraocular pressure (IOP) increase of ≥ 5 mmHg within 2 hours after laser trabeculoplasty (LTP) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Alpha‐2 agonists vs placebo | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 IOP increase of ≥ 10 mmHg within 2 hours after LTP Show forest plot | 4 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 0.05 [0.01, 0.20] |
| 2.1 Acetazolamide vs placebo | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.03 [0.00, 0.52] |
| 2.2 Alpha‐2 agonists vs placebo | 3 | 346 | Risk Ratio (M‐H, Random, 95% CI) | 0.06 [0.01, 0.27] |
| 3 Mean change in IOP from pre‐LTP to measurements taken within 2 hours after LTP Show forest plot | 4 | Mean Difference (Random, 95% CI) | Subtotals only | |
| 3.1 Apraclonidine vs placebo (mmHg) | 4 | 151 | Mean Difference (Random, 95% CI) | ‐7.43 [‐10.60, ‐4.27] |
| 4 IOP increase of ≥ 5 mmHg two to 24 hours after LTP Show forest plot | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Alpha‐2 agonists vs placebo | 5 | 634 | Risk Ratio (M‐H, Random, 95% CI) | 0.17 [0.09, 0.31] |
| 5 IOP elevation of ≥ 10 mmHg two to 24 hours after LTP Show forest plot | 9 | 817 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.11, 0.42] |
| 5.1 Alpha‐2 agonists vs placebo | 7 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 0.19 [0.07, 0.50] |
| 5.2 Dorzolamide vs placebo | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.01, 5.22] |
| 5.3 Pilocarpine vs no treatment | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 0.23 [0.07, 0.71] |
| 6 Mean change in IOP from pre‐LTP to measurements two to 24 hours after LTP Show forest plot | 4 | Mean Difference (Random, 95% CI) | Subtotals only | |
| 6.1 Apraclonidine vs placebo (mmHg) | 4 | 151 | Mean Difference (Random, 95% CI) | ‐5.32 [‐7.37, ‐3.28] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intraocular pressure (IOP) increase of ≥ 5 mmHg within 2 hours after laser trabeculoplasty (LTP) Show forest plot | 2 | 71 | Risk Ratio (M‐H, Random, 95% CI) | 2.28 [0.32, 16.03] |
| 2 Mean change in IOP from pre‐LTP to measurements taken within 2 hours after LTP (mmHg) Show forest plot | 2 | 71 | Mean Difference (IV, Random, 95% CI) | ‐0.69 [‐2.56, 1.17] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mean change in intraocular pressure (IOP) from pre‐laser trabeculoplasty (LTP) to measurements taken within 2 hours after LTP (mmHg) Show forest plot | 2 | 277 | Mean Difference (Random, 95% CI) | 0.61 [‐0.44, 1.66] |
| 2 IOP increase of ≥ 5 mmHg two to 24 hours after LTP Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3 IOP increase of ≥ 10 mmHg two to 24 hours after LTP Show forest plot | 2 | 390 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.14, 5.63] |
| 4 Mean change in IOP from pre‐LTP to measurements taken two to 24 hours after LTP (mmHg) Show forest plot | 2 | Mean Difference (Fixed, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intraocular pressure (IOP) increase of ≥ 5 mmHg two to 24 hours after laser trabeculoplasty (LTP) Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Alpha‐2 agonists | 4 | 319 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.25, 2.63] |
| 2 IOP increase of ≥ 10 mmHg two to 24 hours after LTP Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Alpha‐2 agonists | 4 | 319 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.19, 12.43] |
| 3 Mean change in IOP from pre‐LTP to measurements taken more than 2 hours but within 24 hours after LTP (mmHg) Show forest plot | 3 | Mean Difference (Random, 95% CI) | Subtotals only | |
| 3.1 Alpha‐2 agonists (mmHg) | 3 | 198 | Mean Difference (Random, 95% CI) | ‐1.07 [‐2.51, 0.37] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Conjunctival blanching (brimonidine vs placebo) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |