Herramientas creadas y distribuidas por los realizadores de guías para promover la adopción de las mismas
Information
- DOI:
- https://doi.org/10.1002/14651858.CD010669.pub2Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 22 August 2016see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Effective Practice and Organisation of Care Group
- Copyright:
-
- Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
GF contributed to the writing of the protocol, led the screening of the studies for inclusion and data extraction, and drafted the review.
AH assisted with screening studies for inclusion and data extraction, and commented on drafts of the review.
LG assisted with screening studies for inclusion and data extraction, and commented on drafts of the review.
ME contributed to the writing of the protocol.
JG commented on the final version of the review prior to peer review.
GL suggested the topic of the review, and commented on drafts of the review.
SS contributed to the writing of the protocol, assisted with screening studies for inclusion, and commented on drafts of the review.
Sources of support
Internal sources
-
Nuffield Department of Population Health, University of Oxford., UK.
External sources
-
NIHR Cochrane EPOC programme grant, UK.
Declarations of interest
GF None known.
AH None known.
LG None known.
ME None known.
JG holds the Canada Research Chair in Health Knowledge Transfer and Uptake.
GL is Deputy Chief Executive and Director of Health and Social Care at the National Institute for Health and Care Excellence (NICE), and has responsibility for the implementation programme that includes the development of implementation tools.
SS None known.
Acknowledgements
We wish to thank senior information scientist Nia Roberts at the Bodleian library (Oxford, UK), for developing the search strategy and for running the electronic searches. We would also like to acknowledge Hannah Parke (from King's improvement Science) for assistance with the sifting.
Lucy Goulding and Hannah Parke are staff members at King's Improvement Science, and they wish to acknowledge their funders: King’s Improvement Science is part of the NIHR CLAHRC South London and comprises a specialist team of improvement scientists and senior researchers based at King’s College London. Its work is funded by King’s Health Partners (Guy’s and St Thomas’ NHS Foundation Trust, King’s College Hospital NHS Foundation Trust, King’s College London and South London and Maudsley NHS Foundation Trust), Guy’s and St Thomas’ Charity, the Maudsley Charity and the Health Foundation.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding and a Cochrane programme grant to the EPOC Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Version history
| Published | Title | Stage | Authors | Version |
| 2016 Aug 22 | Tools developed and disseminated by guideline producers to promote the uptake of their guidelines | Review | Gerd Flodgren, Amanda M Hall, Lucy Goulding, Martin P Eccles, Jeremy M Grimshaw, Gillian C Leng, Sasha Shepperd | |
| 2013 Aug 09 | Tools developed and disseminated by guideline producers to promote the uptake of their guidelines | Protocol | Gerd Flodgren, Martin P Eccles, Jeremy Grimshaw, Gillian C Leng, Sasha Shepperd | |
Differences between protocol and review
Two new review authors (AH and LG), who were not involved at the protocol stage, are included in the review team.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- *Practice Guidelines as Topic;
- Delivery of Health Care [economics, *standards];
- Family Practice;
- Guideline Adherence [*statistics & numerical data];
- Health Resources [statistics & numerical data];
- Medical Staff, Hospital;
- Physical Therapy Specialty [education];
- Randomized Controlled Trials as Topic;
- Reminder Systems;
- Teaching Materials;
PICOs

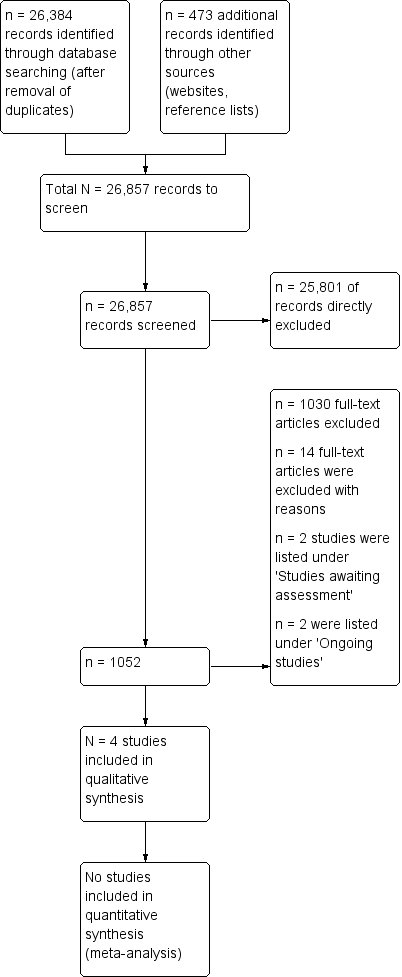
Risk of bias summary: review authors' judgements about each risk of bias item for each included study. White space indicate studies not reporting non‐objective outcomes and for which risk of bias could not be assessed.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies. White spcace indicate studies not reporting non‐objective outcomes and for which risk of bias could not be assessed.
| Clinical practice guideline (CPG) + implementation tool compared with CPG only for adherence to guidelines | ||||
| Patient or population: Healthcare professionals (physiotherapists, hospital physicians) providing care for people with different clinical conditions (patients with non specific low back pain, patients with symptoms indicating a need for a thyroid function test) Setting: Private physiotherapy clinics in the Netherlands, general hospitals in France Intervention: CPG + guideline implementation tool (e.g. training workshops, paper‐based materials and order forms, reminders, web‐based tools) | ||||
| Outcomes | Median ARD (Absolute risk difference) | No of Participants | Certainty of the evidence | Comments |
| Adherence to guidelines | Guideline tools provided to healthcare professionals as an aid to improve the use of a CPG probably lead to improved adherence with the CPG, as compared to guidelines only. Median ARD: 0.135 (0.115 to 0.15.9) at mean 4 weeks follow‐up | 68 physio‐ therapy practices; and 6 hospitals (2 C‐RCTs) | ⊕⊕⊕⊝ | 2 of the 4 included studies reported a proxy measure for adherence to guidelines, and results from these studies could therefore not be included in the ARD calculation |
| Costs | Guideline tools aimed at improving the use of guidelines may lead to little or no difference in healthcare costs | 68 physio‐ therapy clinics (1 C‐RCT) | ⊕⊕⊝⊝ low2 | 1 trial reported no difference in mean direct annual cost* per patient between intervention and control groups. 1 French paper belonging to 1 of the included trials (6 hospitals) and reporting on costs awaits translation |
| * Direct costs included costs of the dissemination of the guideline and healthcare resource use by the patient GRADE Working Group grades of evidence | ||||
| 1We downgraded the certainty of the evidence one step due to high risk of bias. 2We downgraded the certainty of the evidence two steps due to imprecision. | ||||
| Author Year Targeted behaviour | Guideline developers | Literature review | Critical appraisal | Consensus processes | Key stakeholder involvement | Barriers/facilitator assessment |
| Targeted behaviour: management of non‐specific low back pain Number of recommendations: 4 main recommendations | The Royal Dutch Physiotherapy Association. | CPGs2 were constructed on the basis of the phases of the physiotherapy process, using the Dutch method of developing physiotherapy guidelines, and evidence from systematic reviews were identified through searching electronic databases | Not mentioned but probably included in the Dutch method of developing CPGs | Based on scientific evidence. If no evidence was available, consensus between experts was obtained | The CPGs were pilot‐tested among 100 physiotherapists and reviewed by an external multidisciplinary panel | Barriers to change were assessed through a survey as part of the CPG development process |
| Targeted behaviour: appropriate thyroid function testing Number of recommendations: not reported | The Committee for Co‐ordinating Clinical Evaluation and Quality in | The CPG developers conducted a comprehensive review of the literature | ‐ | CPG3 development involved an expert consensus process. | ‐ | ‐ |
| Targeted behaviour: appropriate duration of intravenous antibiotic therapy for treatment of pneumonia Number of recommendations: a 2‐step recommendation | Researchers who were part of the Pneumonia Patient Outcomes Research Team (PORT) | The CPG was based on a review of the medical literature, and empiric evidence on time to reach clinical stability | ‐ | The CPG development process involved the consensus of an 8‐member national guideline panel | The guideline was reviewed by clinical opinion leaders at each study site, and was approved for local use by the relevant utilisation management department. | ‐ |
| Targeted behaviour: management of cardiovascular risk Number of recommendations: no information | Canadian Diabetes Association (and Expert Committee members) | Expert Committee members evaluated the relevant literature, and guidelines were developed and initially reviewed | After formulating new recommendations or modifying existing | Based on scientific evidence/review of the literature | A draft document was circulated nationally and | ‐ |
| 1Khunti 1998. Development of evidence‐based review criteria for the management of patients with depression in general practice. No published version of the guideline found. | ||||||
| Author Year | Delivery of the intervention | Theoretical models/ frameworks used | Evidence base | Targeted to barriers | Key stakeholder involvement |
| Type of intervention: simple, but multicomponent; active only Intervention target: the healthcare professional Targeted behaviour: management of nonspecific low back pain | Mode: face‐to‐face Provider: The primary investigator and 1 of 2 additional trainers with adequate clinical experience in the management of low back pain supervised the training sessions | ‐ | "The sessions were based on interventions that have all been shown to be effective, such as interactive education and discussion, feedback, and reminders".1,2,3,4,5 | The content of the strategy was determined on the basis of information about the expected barriers for implementation gathered during the development of the CPGs | 2 experts gave advice on the content of the strategy |
| Type of intervention: multicomponent; passive only Intervention target: the healthcare professional Targeted behaviour: appropriate thyroid function testing | Mode: Paper‐based materials Provider: none | ‐ | "Among the clinical guideline diffusion strategies, the most effective are feedback, reminders, academic detailing and financial incentives1,2,4,5 Administrative procedures such as the implementation of test request forms have also proved effective." | ‐ | ‐ |
| Type of intervention: single; active + passive Intervention target: the healthcare professional Targeted behaviour: appropriate duration of intravenous antibiotic therapy for treatment of pneumonia | Mode: Paper‐based material (detail sheets/treatment recommendations in patient records) and telephone reminder Provider: nurse delivered telephone reminder | ‐ | "The multifaceted guideline dissemination strategy consisted of interventions of proven benefit, including real‐time physician reminders" 1,6,7,8 | ‐ | ‐ |
| Type of intervention: passive Intervention target: family physicians (and diabetes patients at high risk of cardiovascular disease) Targeted behaviour: management of cardiovascular risk factors and outcomes of cardiovascular disease in people with diabetes | Mode: printed educational materials Targeting the family physician: The cardiovascular disease toolkit was a collection of printed educational materials, packaged in a brightly‐coloured box with CDA branding, sent to Canadian family physicians. The contents included an introductory letter from the Chair of the practice Provider: NA13 | The implicit theory behind its | "The literature has demonstrated that the benefits of printed educational interventions are, at best, modest. A systematic review of methods to improve practice guideline adherence demonstrated an absolute improvement of 8% for educational materials. A more recent Cochrane review found that printed educational materials led to a median absolute improvement in performance of only 2% (25). Studies of printed materials specifically tied to clinical practice guidelines also showed modest benefits. A small English study randomised 42 family physicians to receive an algorithm for monitoring and treatment of hypertension of diabetic patients based on practice guidelines, but found no difference in blood pressure control between the intervention and control groups. However, some processes of care were slightly improved: patients in the intervention group were prescribed higher doses of antihypertensive medications, and had more physician visits to monitor blood pressure. In a larger Canadian study, family physicians were randomised to receive a 1‐page summary of a 3‐year‐old practice guideline on anti‐anginal therapy from the local medical governing body. No differences were noted in prescription of β‐blockers, antiplatelet agents, or lipid‐lowering drugs between groups in the 7000 patients reviewed" 9,10,11,12 | ‐ | The toolkit was |
| 1Bero 1998 Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. | |||||
| Author Year | Tailoring | Feedback | Educational outreach/ Academic detailing/ Small group discussions | Reminders (paper, electronic, telephone) | Decision support tools | Other (test order forms, supportive materials etc.) |
| The content of the strategy was determined on the basis of information about the expected barriers for implementation gathered during the development of the clinical guidelines. | ‐ | 2 interactive training sessions, each lasting 2½ hours, for groups of 8 – 12 physiotherapists (including feedback on current management and reminders). For each session a preparation time of 2 hours was recommended. | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | Pocket memorandum card. | ‐ | Test request form. | |
| ‐ | ‐ | ‐ | Paper‐based detail sheet/ treatment recommendations put into the patient's record + real‐time nurse telephone reminder | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | Printed educational materials |
| Author Year | Clinical outcomes; Medical complications | Quality of life Satisfaction with care | Mortality | Healthcare resource use (including medications prescribed) | Costs |
| ‐ | Quality of Life (assessed with the EQ‐5D1), mean (SD): BL: Intervention: 0.6730 (0.2042); Control: 0.6134 (0.2661), P = 0.006. At 6 weeks: Intervention: 0.7778 (0.1978); Control: 0.7497 (0.2316) At 12 weeks: Intervention: 0.8141 (0.1988); Control: 0.7873 (0.2210) Note: results for 26 and 52 weeks reported graphically | ‐ | ‐ | Mean annual cost (Euros) per patient (SD): Direct cost2: Intervention: 374 (437). Control: 449 (572). The costs (Euro) of releasing a new guideline for low back pain to 18,000 physiotherapists: Intervention (active strategy): 87,416 Control (passive strategy): 63,101 | |
| ‐ | ‐ | ‐ | ‐ | Cost paper awaits translation | |
| In‐hospital medical complications, number (%): Intervention:157 (55); Control: 206 (63), P = 0.04 Functional status3 SF‐12 physical health composite score: Intervention:45 ± 7, n = 181; SF‐12 mental health composite score: Intervention: 45 ± 6; Control: 45 ± 7, P = 0.71 | Patient satisfaction with care4 , number (%): Not satisfied with overall care: Intervention: 12 (5.3), n = 228; Control: 11 (4.0), n = 273, P = 0.67 Believed length of stay was too short: Intervention: 59 (26.1); Control: 54 (20.2), P = 0.16 Return to usual activities5,Hazard ratio (95% CI): Nonworkers: 1.09 (0.83 to 1.43), P = 0.55 Workers: 0.85 (0.54 to 1.35); P = 0.49 Return to work (workers) 0.99 (0.63 to 1.58), P = 0.98 | Mortality6 all‐cause, number (%): Intervention: 22 (8), n = 283; Control: 29 (9), n = 325, P = 0.70 Pneumonia‐related mortality, number (%): Intervention: 15 (5); Control: 23 (7), P = 0.44 | Length of index hospital (days) stay, median (IQR): Intervention: 5.0 (3.0 to 7.0); Control: 5.0 (3.0 to 8.0); Hazard ratio (95% CI): 1.16 (0.97 to 1.38), P = 0.11 Rehospitalisation7 number (%): Intervention:37 (14); Control:33 (11), P = 0.42 Duration (days) of intravenous antibiotic therapy, median (IQR): Intervention: 3.0 (2.0 to 5.0),n = 283; Control: 4.0 (2.6 to 6.0), n = 325; Hazard ratio (95% CI): 1.23 (1.00 to 1.52), P = 0.06 | ‐ | |
| Clinical data study: Intervention: n = 40 practices/795 patients; Control: n = 40 practices/797 patients Cardiovascular risk reduction (secondary outcomes): Proportion of participants reaching glycaemic control targets (HbA1c < 7.0%): Intervention: 58.5%; Control: 58.8%; OR 0.93 (0.71 to 1.21), P = 0.58 Proportion of participants reaching blood pressure control targets (< 130/80): Intervention: 52.8%; Control: 63.5%, OR 0.72 (0.53 to 0.98), P = 0.04 Proportion of participants reaching LDL‐cholesterol control targets (< 2.0 mmol/L): Intervention: 59.2%; Control: 61.7% , OR 0.90 (0.68 to 1.18), P = 0.43 Proportion of participants reaching Total to HDL‐cholesterol ratio (< 4.0): Intervention: 74.2%; Control: 76.8%, OR 0.85 (0.63 to1.14), P = 0.27 Clinical (secondary outcomes): When HbA1c > 8.0%: Intervention: 11.8%; Control: 13.0%, OR 0.98 (0.48 to 1.98), P = 0.95 When blood pressure > 140/90: Intervention: 5.6%; Control: 7.2%, OR 0.67 (0.25 to 1.82), P = 0.43 When LDL cholesterol > 3.0 mmol/L: Intervention: 43.5%; Control: 45.2%, OR 0.94 (0.53 to 1.67), P = 0.83 Administrative data study : Intervention: 2008 practices (467,713 participants); Control: 1999 practices (466, 076 participants) Secondary outcomes: | ‐ | Administrative data study : Intervention: 2008 practices (467,713 participants); Control: 1999 practices (466,076 participants) Primary outcome: Death or non‐fatal myocardial infarction: Intervention: 2.5%; Control: 2.5%; OR 1.00 (0.96 to 1.03), P = 0.77 Secondary outcomes: Medication initiation (ACEI/ARB > 1 antihypertensive class, or > 2, or > 3, statin, glucose‐lowering drugs, insulin, nitrate): OR, range: from 0.96 to 1.02, P values from 0.03 to 0.94 | Clinical data study: Primary outcome: Proportion of participants prescribed statins (new or renewed prescription): Intervention: 700 (88.1%); Control: 725 (90.1%); OR 0.73, 95% CI 0.42 to 1.26, P = 0.26 Proportion of participants prescribed an ACEI/ARB: Intervention: Control: Secondary outcome. Administrative data study : Secondary outcomes: CAD assessment (electrocardiogram, cardiac stress test, nuclear imaging, coronary angiography, coronary revascularisation, cardiology or internal medicine visit): OR, range: from 0.96 to 1.00, P values from 0.02 to 0.83 | ‐ | |
| 1EQ‐5D: a standardised instrument for use as a measure of health outcome.The EQ‐5D has five dimensions: mobility, self‐care, usual activity,pain/discomfort and anxiety/depression. Each dimension has three levels, no problems, some problems and serious problems. Hence, EQ‐5D has 243 possible health states. Utility values of the general public for these health states as measured with the time tradeoff technique on a random sample of the adult population of the United Kingdom, the MVH‐A1 tariff, were applied in this study. The scores range from −0.594 (worst situation) to 1.0 (perfect health). | |||||
| Author Year | Adherence Outcomes | Participants (Settings) | Control Adherence | Intervention Adherence | Median ARD |
| (Hoijenboos 2005) Targeted behaviour: management of non specific low back pain GL tool used: interactive training workshop X2 | Adherence to 4 guideline recommendations: i) Limit number of sessions in normal course back pain ii) Set functional treatment goals iii) Use mainly active interventions iv) Give adequate information Note: an increase was desirable for all outcomes | 113 physiotherapists (68 private physiotherapy practices) | i) Post: 14 (13), n = 253 ii) Post: 180 (71) iii) Post: 154 (60) iv) Post: 221 (87) | i) Post: 32 (27), n = 247 ii) Post: 188 (79) iii) Post: 183 (77) iv) Post: 229 (96) | +0.115 11.5% higher adherence in the intervention group i) 0.14% ii) 0.08% iii) 0.17% iv) 0.09% |
| Targeted behaviour: appropriate thyroid function testing Guideline tool used: | Global Guideline Conformity Rate | 1412 physicians (6 general hospitals) | Pre: 62.0% (95% CI 47.7 to 76.4) | Dual intervention group: Post: 77.9% (95% CI 68.9 to 87.0) Note: only results for the dual intervention presented here | +0.159% |
| Targeted behaviour: appropriate duration of intravenous antibiotic therapy for treatment of pneumonia GL tool used: detail sheet/ treatment recommendations+ telephone reminder | No adherence outcomes reported, only proxies | 545 physicians (7 not‐for‐profit hospitals) | ‐ | ‐ | ‐ |
| Targeted behaviour: improved cardiovascular risk factor management in people with diabetes Guideline tool used: printed educational material | No adherence outcomes reported, only proxies | 2 separate studies: Administrative data study: n = 4007 practices: Intervention: 2008; Control: 1999 Clinical data study. n = 80 practices (1592 patients); Intervention: 40 practices (8795 patients); Control: 40 practices (8797 patients) | ‐ | ‐ | ‐ |