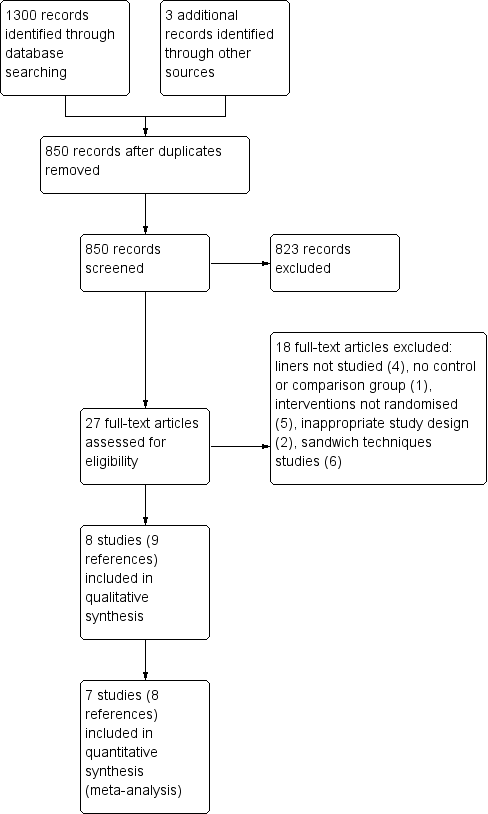
Recubrimiento para las caries dentales en las restauraciones de clase I y clase II con composite basado en resina
References
References to studies included in this review
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Jump to:
| Methods | Trial design: Split‐mouth Location: Dental school, Saudi Arabia Funding source: None mentioned | |
| Participants | Inclusion criteria: Occlusal caries on contralateral posterior teeth with small or moderately large carious lesions ‐ the bucco‐lingual dimensions of each cavity were less than half the intercuspal width Age: Males 16‐52 years Exclusion criteria: Orofacial pain, including toothache, percussion tenderness, periapical radiolucency Number of randomised individuals: n/a Number of randomised teeth: 88 Number of individuals evaluated: 44 Dropouts: None | |
| Interventions | RMGI liner under RBC restoration (no bonding agent used) compared to no liner (bonding agent only) under RBC restoration | |
| Outcomes | Postoperative hypersensitivity as measured by CRM in time (seconds) and patient reporting | |
| Notes | Based on these data the study authors concluded that the liner group had less sensitivity but it seems that both groups had no clinically significant sensitivity after 30 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "There was randomization in the selection of the right and left teeth for the adhesive or glass‐ionomer lining" Comment: No other additional information was provided ‐ it is unclear how the randomization was performed and how easy it would have been for the operators to deviate from the randomization prescribed |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants may or may not have been blinded – no information provided. Operator was not blinded – knew which tooth received liner |
| Blinding of outcome assessment (detection bias) | Low risk | "The measurement of CRM at the recall visits was by another dentist who was unaware of the lining that the experimental teeth had received" |
| Incomplete outcome data (attrition bias) | Low risk | No participants dropped out |
| Selective reporting (reporting bias) | Low risk | All data reported |
| Other bias | High risk | A validated instrument to measure patient‐reported sensitivity was not used |
| Methods | Trial design: Parallel‐group Location: Dental school postgraduate clinic Bangkok, Thailand Funding source: None mentioned | |
| Participants | Inclusion criteria: At least 1 deep primary occlusal caries without other defects in a first or second permanent molar, at least 1 opposing tooth, periodontal tissues healthy or only mildly inflamed, no previous signs and symptoms of pulpal and periapical disease, preoperative sensitivity relieved immediately after removal of stimulus, and no spontaneous pain Age: 18‐30 years Exclusion criteria: Medical problems (unspecified), orofacial pain, other defects or restorations on the tooth, cavity depth less than 3 mm, pulpal exposure, no opposing tooth, periodontal disease, signs or symptoms of periapical or pulpal disease Number of randomised individuals: n/a Number of randomised teeth: 62 Number of individuals evaluated: 34 Dropouts: 19 | |
| Interventions | RMGI liner under RBC restoration compared to no liner under RBC restoration | |
| Outcomes | Postoperative hypersensitivity as measured by patient reporting Restoration longevity | |
| Notes | 2 different bonding agents were used, with no explanation of how the distribution was determined. A further study was identified (Banomyong 2011); authors confirmed overlap in participants between the 2013 and 2011 papers | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "One of the two restorative procedures was randomly allocated. Each participant was unaware of the restoration" Comment: No other additional information provided ‐ it is unclear how the randomization was performed and how easy it was for the operators to deviate from the randomization prescribed |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants were unaware of the intervention, however, the operator and evaluator were the same person, "the operator (DB)" "all restorations were examined by one evaluator (DB)" |
| Blinding of outcome assessment (detection bias) | High risk | Operator and evaluator were the same person, "the operator (DB)" (page 3) "all restorations were examined by one evaluator (DB)" |
| Incomplete outcome data (attrition bias) | High risk | 13/31 teeth from experimental group and 6/31 teeth from control group were not included in evaluation |
| Selective reporting (reporting bias) | Low risk | All data reported |
| Other bias | Low risk | None detected |
| Methods | Trial design: Split‐mouth Location: Department of Operative Dentistry and Periodontolgy, Germany Funding source: Ivoclar Vivadent | |
| Participants | Inclusion criteria: Adults with 2 comparable Class I or II cavities to be restored with a dental composite; positive sensitivity and existing antagonist and neighboring teeth Age: Not specified Exclusion criteria: Underage, systemic diseases, allergies to 1 of the substances of content, gravidity, lactation, teeth that needed direct pulp capping, and endodontically treated teeth Number of randomised individuals: 50 Number of randomised teeth: 100 Number of individuals evaluated: 44 (87 teeth) Dropouts: 6 | |
| Interventions | Flowable composite Tetric EvoFlow under Tetric EvoCeram compared to Tetric EvoCeram only (both groups used adhesive system AdheSE One) | |
| Outcomes | Postoperative hypersensitivity as measured by CRM using subjective descriptive patient‐response criteria Modified Ryge criteria categories evaluated (color match, marginal discoloration, filing integrity, marginal adaptation, surface, secondary caries, proximal contact, and hypersensitivity) Restoration longevity | |
| Notes | "The sample size was determined by a statistician ....for 5% level of significance and a power of 90%" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...computer generated randomization list" |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants may or may not have been blinded – no information provided. Operator was not blinded – knew which tooth received liner |
| Blinding of outcome assessment (detection bias) | Low risk | "Two blinded, calibrated clinicians not involved with the treatment procedures evaluated each restoration" |
| Incomplete outcome data (attrition bias) | Low risk | All participants evaluated at 6 and 12 months. 6 participants were lost for the 2‐year evaluation due to address changes; unlikely to influence results |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported |
| Other bias | Low risk | None detected |
| Methods | Trial design: Parallel‐group Location: Dental school, USA Funding source: None mentioned | |
| Participants | Inclusion criteria: Adults in need of only 1 moderate to large Class II or complex Class I restoration on a molar; occlusally the final margin had to extend more than halfway from the central groove to the cusp tip; interproximally, the final facial and/or lingual margin of the proximal box had to extend at least halfway between minimal clearance and the line angle; no contraindications to routine dental treatment; participant had to be likely to remain in the area for the length of the study Age: Adults (specific age not reported) Exclusion criteria: Removal of caries resulting in exposure of dental pulp Number of randomised individuals: 50 Number of randomised teeth: 25 teeth in each group Number of individuals evaluated: 44 Dropouts: 6 total ‐ 3 from each group | |
| Interventions | Flowable liner under 1 brand RBC restoration compared to no flowable liner under another brand of RBC restoration | |
| Outcomes | Restoration longevity | |
| Notes | Results for marginal staining reported in Table 1 for only 43 of the 44 restorations evaluated. (1) "restoration experienced a bulk fracture and loss of restorative material substantial enough to expose the dentin. The loss of restorative material created a situation where it was not possible to rate this restoration for any of the other categories" (page 365). Additionally, half of the restorations in each group also received surface sealer postplacement and two subjects were not treated due to depth of caries (pulp exposures anticipated). It should also be noted that although the authors listed postoperative sensitivity among the criteria to be evaluated they did not mention how this would be measured and they did not include any data for this criteria or provide any information in the results nor discussion regarding postoperative sensitivity. Therefore, we included this study only in the longevity portion of this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "At the operative appointment, eligible participants were randomly assigned to 1 of 4 groups. While the operators were aware of this assignment, the evaluators and the participants were not. Thus the study design was a randomized, double‐blind clinical trial" |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | Low risk | Participants were blinded but operators were not |
| Blinding of outcome assessment (detection bias) | Low risk | "..the evaluators and the participants were not aware of the assignment" |
| Incomplete outcome data (attrition bias) | High risk | There is no mention of how missing data due to dropouts were treated |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported |
| Other bias | Low risk | None detected |
| Methods | Trial design: Parallel‐group Location: Dental school postgraduate clinic Bangkok, Thailand Funding source: None mentioned | |
| Participants | Inclusion criteria: At least 1 moderate to deep primary occlusal caries (at least 2 mm deep after caries removal) in a first or second permanent molar without caries on other surfaces; at least 1 opposing tooth; periodontal tissues healthy or mildly inflamed without gingival recession/alveolar bone loss; no previous signs and symptoms of pulpal and periapical disease, preoperative sensitivy relieved immediately after removal of stimulus, and no spontaneous pain; at least 1 antagonist tooth with occlusal contact more than 50% of the occlusal surface Age: 18‐40 years Exclusion criteria: Either the cavity depth after caries removal was less than 2 mm or a pulp exposure or near pulp exposure, in which a calcium hydroxide agent was placed; psychological disorders; neurological diseases; TMD; pregnancy or lactation; patients taking any analgesic or anti‐inflammatory drugs regularly; allergies to materials used in the trial; teeth with previous restoration(s), tooth surface loss (attrition, erosion, abrasion or abfraction); teeth diagnosed with cracked tooth syndrome; teeth that had received orthodontic treatment in past 3 months Number of randomised individuals: 72 Number of randomised teeth: 106 Number of individuals evaluated: 70 Dropouts: 2 | |
| Interventions | RMGI liner under RBC restoration using 2 different bonding agents compared to no liner under RBC restoration using 2 different bonding agents | |
| Outcomes | Postoperative hypersensitivity as measured CRM on a VAS, yes/no criteria, and also by patient reporting | |
| Notes | Some participants had multiple restorations in different quadrants | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...blocking randomization list" |
| Allocation concealment (selection bias) | Low risk | "...sealed envelope" |
| Blinding of participants and personnel (performance bias) | Low risk | Participants were blinded but operators were not |
| Blinding of outcome assessment (detection bias) | High risk | "One to four restorations were randomly allocated in each patient by a single operator (DB) according to a blocking randomization list." "At recall, the evaluator (DB) was blinded to the restoration that was being evaluated" |
| Incomplete outcome data (attrition bias) | Low risk | "Two patients (three restorations) were lost during recall and were excluded before data analysis (from telephone interviewing, these patients reported no postoperative tooth sensitivity in daily function)" |
| Selective reporting (reporting bias) | Low risk | "…five patients (five restorations) missed the one‐week recall; however, these patients were still included in the data analysis. All patients attended the one‐month recall" |
| Other bias | Low risk | None detected |
| Methods | Trial design: Split‐mouth Location: Dental school faculty practice Istanbul, Turkey Funding source: None mentioned | |
| Participants | Inclusion criteria: Patients with 2 primary occlusal caries in molars in occlusion that were not mobile. Lesions diagnosed by visual inspection and radiographically Age: 18 to 48 years Exclusion criteria: Poor oral hygiene Number of randomised individuals: 54 Number of randomised teeth: 27 in each group Number of individuals evaluated: 50 Dropouts: 4 | |
| Interventions | Flowable liner under 2 brands RBC restoration compared to no liner under same 2 brands RBC restoration | |
| Outcomes | Postoperative hypersensitivity as measured by patient reporting Restoration longevity | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "…materials were allocated randomly" |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | Low risk | "The examiners were not involved in the filling placements" |
| Incomplete outcome data (attrition bias) | Low risk | All data reported |
| Selective reporting (reporting bias) | Low risk | All data reported |
| Other bias | Low risk | None detected |
| Methods | Trial design: Parallel‐group Location: Private dental offices, USA Funding source: NIDCR | |
| Participants | Inclusion criteria: Moderate to deep primary occlusal caries (at least 2 mm deep after caries removal) in a first or second permanent molar without caries on other surfaces; at least 1 opposing tooth; periodontal tissues healthy or mildly inflamed without gingival recession/alveolar bone loss; no previous signs and symptoms of pulpal and periapical disease, preoperative sensitivity relieved immediately after removal of stimulus, and no spontaneous pain; at least 1 antagonist tooth with occlusal contact more than 50% of the occlusal surface Age: 15‐60 years Exclusion criteria: Either the cavity depth after caries removal was less than 2 mm or a pulp exposure or near pulp exposure, in which a calcium hydroxide agent was placed; psychological disorders; neurological diseases; TMD; pregnancy or lactation; patients taking any analgesic or anti‐inflammatory drugs regularly; allergies to materials used in the trial; teeth with previous restoration(s), tooth surface loss (attrition, erosion, abrasion or abfraction); teeth diagnosed with cracked tooth syndrome; teeth that had received orthodontic treatment in past 3 months Number of randomised individuals: 341 Number of randomised teeth: 347 Number of individuals evaluated: 333 Dropouts: 8 | |
| Interventions | RMGI liner under RBC restoration compared to no liner under RBC restoration | |
| Outcomes | Postoperative hypersensitivity as measured by CRM on a VAS | |
| Notes | Caries classification and dentin caries activity for each lesion, sleep bruxism and caries risk for each patient were also assessed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "On enrolment, eligible participants were randomly assigned one to one (blocking within practice, using random block sizes) between the following treatment arms..." |
| Allocation concealment (selection bias) | Low risk | Randomization done centrally ‐ not in each practice |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants may or may not have been blinded – no information provided |
| Blinding of outcome assessment (detection bias) | High risk | Operator and evaluator were the same person "P‐Is completed restorations according to the treatment arm assigned and liner (if used)" and "P‐Is saw participants for evaluation at one and four weeks after treatment" |
| Incomplete outcome data (attrition bias) | Low risk | All data reported |
| Selective reporting (reporting bias) | Low risk | All data reported |
| Other bias | Low risk | None detected |
| Methods | Trial design: Parallel‐group Location: Göttingen, Germany Funding source: University of Göttingen | |
| Participants | Inclusion criteria: Caries media or caries profunda (according to bitewing radiographs), insufficient fillings, positive reaction to a vitality test (cold test), no signs of pulp inflammation, no spontaneous pain attacks before treatment, only premolars and molars, only 1 filling per tooth, and a minimum extension of the cavity of 1 mm in width Age: 18 years or older Exclusion criteria: Patients under 18 years, pregnancy, breastfeeding, immunosuppressed or addicted patients Number of randomised individuals: 123 Number of randomised teeth: 123 Number of individuals evaluated: 123 Dropouts: None | |
| Interventions | Calcium hydroxide (CaOH) liner under 2 brands RBC restoration compared to no liner under 2 brands RBC restoration | |
| Outcomes | Postoperative hypersensitivity as measured by patient reporting | |
| Notes | Maximum age of participants not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The decision to use a calcium hydroxide liner or not was made by tossing a coin" |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | Low risk | Participants were blinded. "The patients were not told to which cavity‐depth group their tooth was allocated and if calcium hydroxide was used or not." Operators were not blinded but risk of bias still low even though operator not blinded as it is not possible to blind the operator |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | Low risk | All data reported |
| Selective reporting (reporting bias) | Low risk | All data reported |
| Other bias | Low risk | None detected |
CRM: cold response measurement; RBC: resin‐based composite; RMGI: resin‐modified glass ionomer; TMD: temporomandibular disorder; VAS: visual analog scale.
Characteristics of excluded studies [ordered by study ID]
Jump to:
| Study | Reason for exclusion |
| Liners not studied | |
| Sandwich technique study | |
| Sandwich technique study | |
| Interventions not randomized | |
| Interventions not randomized | |
| Liners not studied | |
| Sandwich technique study | |
| No control or comparison group | |
| Interventions not randomized | |
| Sandwich technique study | |
| Liners not studied | |
| Interventions not randomized, restorative material no longer available (UV light‐cured RBC) | |
| Inappropriate study design ‐ the study compared 1 brand of RBC placed without a liner to a second brand of RBC placed with a flowable composite as a liner | |
| Liners not studied | |
| Interventions not randomized | |
| Sandwich technique study | |
| Sandwich technique study | |
| Inappropriate study design ‐ the decision of which restoration to place (composite or amalgam) was left to the discretion of the operator and information regarding the decisions was not provided |
RBC: resin‐based composite; UV: ultra violet.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Postoperative hypersensitivity (POH) by patient report (Y/N) Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.1 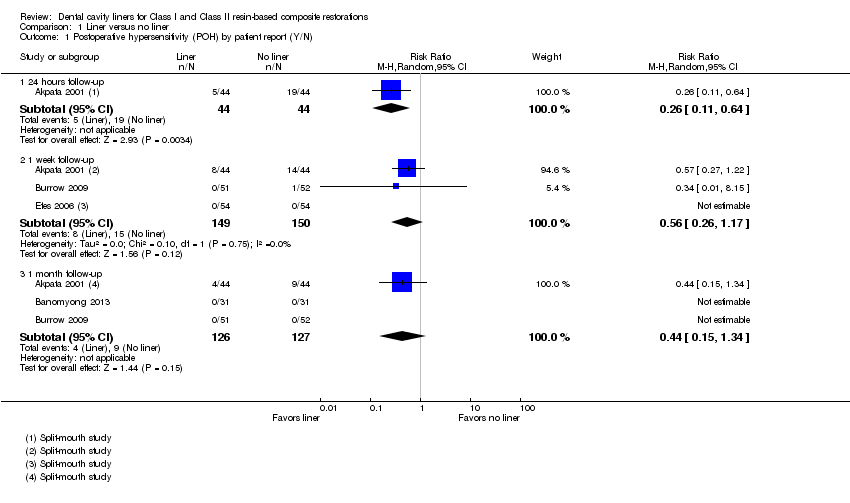 Comparison 1 Liner versus no liner, Outcome 1 Postoperative hypersensitivity (POH) by patient report (Y/N). | ||||
| 1.1 24 hours follow‐up | 1 | 88 | Risk Ratio (M‐H, Random, 95% CI) | 0.26 [0.11, 0.64] |
| 1.2 1 week follow‐up | 3 | 299 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.26, 1.17] |
| 1.3 1 month follow‐up | 3 | 253 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.15, 1.34] |
| 2 Postoperative hypersensitivity (POH) by patient report (VAS) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1 Liner versus no liner, Outcome 2 Postoperative hypersensitivity (POH) by patient report (VAS). | ||||
| 2.1 1 week follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 1 month follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Cold response measurement (CRM) (time it took in seconds for patient to feel cold sensation) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.3  Comparison 1 Liner versus no liner, Outcome 3 Cold response measurement (CRM) (time it took in seconds for patient to feel cold sensation). | ||||
| 3.1 24 hours follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 1 week follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 1 month follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Cold response measurement (CRM) (VAS) Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.4  Comparison 1 Liner versus no liner, Outcome 4 Cold response measurement (CRM) (VAS). | ||||
| 4.1 1 week follow‐up | 2 | 447 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.67, 0.26] |
| 4.2 1 month follow‐up | 2 | 444 | Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.76, 0.11] |
| 5 Cold response measurement (CRM) (Y/N) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 1.5  Comparison 1 Liner versus no liner, Outcome 5 Cold response measurement (CRM) (Y/N). | ||||
| 5.1 1 week follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 1 month follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Restoration failure at 1 year follow‐up Show forest plot | 4 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.07, 15.00] |
| Analysis 1.6  Comparison 1 Liner versus no liner, Outcome 6 Restoration failure at 1 year follow‐up. | ||||

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
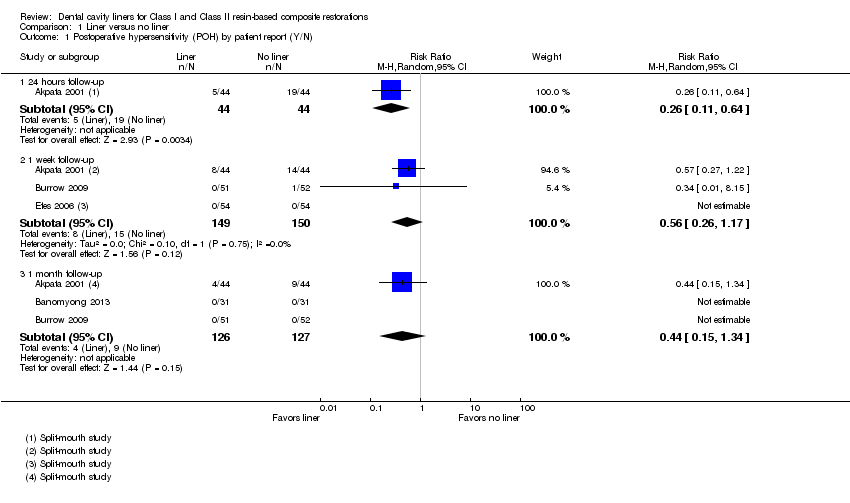
Comparison 1 Liner versus no liner, Outcome 1 Postoperative hypersensitivity (POH) by patient report (Y/N).

Comparison 1 Liner versus no liner, Outcome 2 Postoperative hypersensitivity (POH) by patient report (VAS).

Comparison 1 Liner versus no liner, Outcome 3 Cold response measurement (CRM) (time it took in seconds for patient to feel cold sensation).

Comparison 1 Liner versus no liner, Outcome 4 Cold response measurement (CRM) (VAS).

Comparison 1 Liner versus no liner, Outcome 5 Cold response measurement (CRM) (Y/N).

Comparison 1 Liner versus no liner, Outcome 6 Restoration failure at 1 year follow‐up.
| Liner versus no liner for Class I and Class II resin‐based composite restorations | ||||||
| Patient or population: Patients requiring Class I or Class II resin‐based composite restorations Settings: General practice Intervention: Liner Comparison: No liner | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of restorations | Quality of the evidence | Comments | |
| Assumed risk* | Corresponding risk | |||||
| No liner | Liner | |||||
| Postoperative hypersensitivity (POH) (Patient‐reported Y/N) Follow‐up: 1 week | 100 per 1000 | 56 per 1000 | RR 0.56 | 299 | ⊕⊕⊝⊝1 | POH was also measured at 24 hours (1 trial at high risk of bias) and 1 month (3 trials at high/unclear risk of bias). A benefit in favour of liners was shown at 24 hours; this difference was not maintained at any other time point 1 additional high risk of bias study measured patient‐reported POH using VAS. A benefit was shown in favour of liners at 1 week and 1 month follow‐up |
| Postoperative cold response measurement (CRM) (time it took in seconds for patient to feel cold sensation) Follow‐up: 1 week | The mean postoperative CRM at 1 week (time it took in seconds for patient to feel cold sensation) was 16 seconds | MD 6 seconds more | 88 | ⊕⊕⊝⊝2 | CRM was also measured at 24 hours (1 trial at high risk of bias) and 1 month (1 trial at high risk of bias). No difference was shown between the use of liners and no liners at either time point Other methods of measuring CRM (using VAS or Y/N response) showed no difference between liners and no liners at any time point | |
| Restoration failure Follow‐up: 1 year | 7 per 1000 | 7 per 1000 | RR 1.00 | 281 | ⊕⊕⊝⊝1 | Restoration failure at 2‐year follow‐up also showed no difference between the use of liners or not |
| Adverse events | None reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| *Assumed risk based on control group risk. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Postoperative hypersensitivity (POH) by patient report (Y/N) Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 24 hours follow‐up | 1 | 88 | Risk Ratio (M‐H, Random, 95% CI) | 0.26 [0.11, 0.64] |
| 1.2 1 week follow‐up | 3 | 299 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.26, 1.17] |
| 1.3 1 month follow‐up | 3 | 253 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.15, 1.34] |
| 2 Postoperative hypersensitivity (POH) by patient report (VAS) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 1 week follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 1 month follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Cold response measurement (CRM) (time it took in seconds for patient to feel cold sensation) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 24 hours follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 1 week follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 1 month follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Cold response measurement (CRM) (VAS) Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 1 week follow‐up | 2 | 447 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.67, 0.26] |
| 4.2 1 month follow‐up | 2 | 444 | Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.76, 0.11] |
| 5 Cold response measurement (CRM) (Y/N) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.1 1 week follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 1 month follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Restoration failure at 1 year follow‐up Show forest plot | 4 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.07, 15.00] |