Décentralisation du traitement anti‐VIH dans les pays à revenu faible et intermédiaire
Information
- DOI:
- https://doi.org/10.1002/14651858.CD009987.pub2Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 27 June 2013see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane HIV/AIDS Group
- Copyright:
-
- Copyright © 2013 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
TK and FBA conducted eligibility of the searches, and together with NF did data extraction, and quality assessment. PG resolved differences when needed. TK entered the data and conducted the analyses and wrote the first draft of the review. NF, FBA and PG provided regular feedback into the overall results and their interpretation. PG developed the framework for the nomenclature and models of health care delivery which were initially described in the protocol.
Sources of support
Internal sources
-
South African Cochrane Centre, South Africa.
External sources
-
World Health Organization, Department of HIV/AIDS, Switzerland.
Provided some funding support towards completing this review, as a subcontract through the University of California, San Francisco (UCSF)
-
UKaid from the UK Government for the benefit of developing countries (DFiD), UK.
Funding received through a grant from DFiD to the Effective Health Care Research Consortium
Declarations of interest
None declared.
Acknowledgements
The Effective Health Care Research Consortium, including Paul Garner, are funded by UKaid from the UK Government for the benefit of developing countries. We would also like to acknowledge the assistance of the South African Cochrane Centre. Thanks for the support from the Cochrane HIV/AIDS Review Group, University of California, San Francisco.
Version history
| Published | Title | Stage | Authors | Version |
| 2013 Jun 27 | Decentralising HIV treatment in lower‐ and middle‐income countries | Review | Tamara Kredo, Nathan Ford, Folasade B Adeniyi, Paul Garner | |
| 2012 Jul 11 | Decentralising HIV treatment delivery in middle‐ and low‐income countries | Protocol | Tamara Kredo, Nathan Ford, Folasade B Adeniyi, Paul Garner | |
Differences between protocol and review
Newcastle‐Ottawa tool for assessing quality of cohort studies was not used in the review as it did not adequately address the relevant items of quality included studies.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- *Developing Countries;
- Anti‐HIV Agents [*supply & distribution];
- Cohort Studies;
- Community Health Centers [statistics & numerical data];
- HIV Infections [*drug therapy];
- Health Services Accessibility [*organization & administration, standards];
- Medication Adherence [*statistics & numerical data];
- Patient Dropouts [statistics & numerical data];
- Randomized Controlled Trials as Topic;
Medical Subject Headings Check Words
Humans;

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Partial decentralisation ‐ initiation in hospital, maintenance at health centre, outcome: 1.1 Death or lost to care (12 months).

Forest plot of comparison: 1 Partial decentralisation ‐ initiation in hospital, maintenance at health centre, outcome: 1.2 Lost to care.

Forest plot of comparison: 1 Partial decentralisation ‐ initiation in hospital, maintenance at health centre, outcome: 1.3 Death.

Forest plot of comparison: 2 Full decentralisation ‐ initiation and maintenance in health centre, outcome: 2.1 Death or lost to care (12 months).

Forest plot of comparison: 2 Full decentralisation ‐ initiation and maintenance in health centre, outcome: 2.2 Lost to care.

Forest plot of comparison: 2 Full decentralisation ‐ initiation and maintenance in health centre, outcome: 2.3 Death.

Forest plot of comparison: 3 Decentralisation ‐ from the facility to the community for antiretroviral maintenance therapy, outcome: 3.1 Death or lost to care (12 months).

Forest plot of comparison: 3 Decentralisation ‐ to community from facility, outcome: 3.2 lost to care.
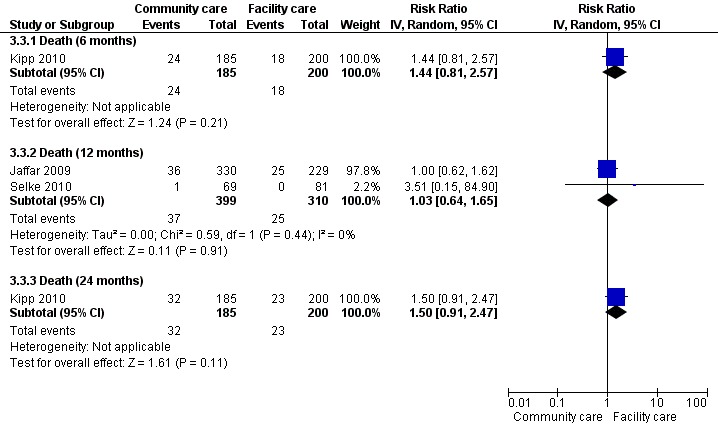
Forest plot of comparison: 3 Decentralisation ‐ to community from facility, outcome: 3.1 Death.

Comparison 1 Partial decentralisation ‐ initiation in hospital, maintenance at health centre, Outcome 1 Death or lost to care (12 months).

Comparison 1 Partial decentralisation ‐ initiation in hospital, maintenance at health centre, Outcome 2 Lost to care.

Comparison 1 Partial decentralisation ‐ initiation in hospital, maintenance at health centre, Outcome 3 Death.
| Study | Down referred patient | Hospital care patient | P‐value |
| cost of travel | |||
| Humphreys 2010 | Average cost for follow up care USD 0.74 | Average cost for follow up care USD 1.5 | P = 0.001 |
Comparison 1 Partial decentralisation ‐ initiation in hospital, maintenance at health centre, Outcome 4 Cost of travel.

Comparison 2 Full decentralisation ‐ initiation and maintenance in health centre, Outcome 1 Death or lost to care (12 months).
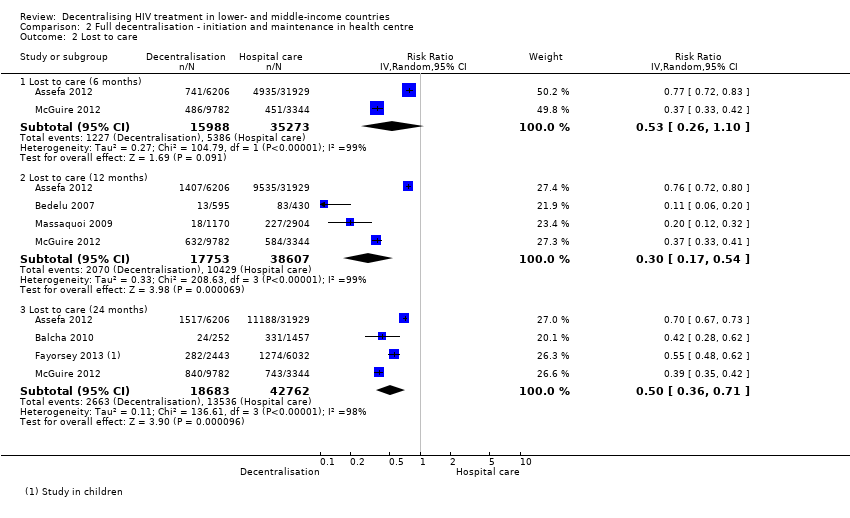
Comparison 2 Full decentralisation ‐ initiation and maintenance in health centre, Outcome 2 Lost to care.

Comparison 2 Full decentralisation ‐ initiation and maintenance in health centre, Outcome 3 Death.
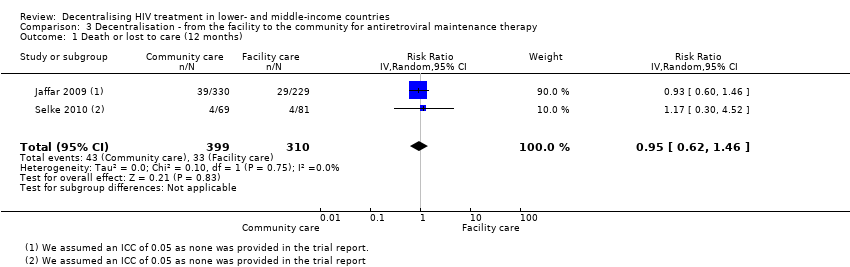
Comparison 3 Decentralisation ‐ from the facility to the community for antiretroviral maintenance therapy, Outcome 1 Death or lost to care (12 months).

Comparison 3 Decentralisation ‐ from the facility to the community for antiretroviral maintenance therapy, Outcome 2 Lost to care.

Comparison 3 Decentralisation ‐ from the facility to the community for antiretroviral maintenance therapy, Outcome 3 Death.
| Study | Home based care | Hospital based care |
| Jaffar 2009 | total cost per year for transport, lunch, childcare costs, lost work time: $18/year (after first year) | total cost per year for transport, lunch, childcare costs, lost work time: $54/ year (after the first year) |
| Kipp 2010 | Transport cost $0.74/ visit for home based care | Transport cost $1.5/ visit for facility based care |
Comparison 3 Decentralisation ‐ from the facility to the community for antiretroviral maintenance therapy, Outcome 4 Cost to patient.
| Antiretroviral therapy initiated in a hospital, maintained at a health centre for HIV infected patients | ||||||
| Patient or population: HIV infected patients | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Antiretroviral therapy initiated in a hospital, maintained at a health centre | |||||
| Death or lost to care | 218 per 1000 | 100 per 1000 | RR 0.46 | 39090 | ⊕⊕⊕⊝ | |
| Lost to care | 134 per 1000 | 74 per 1000 | RR 0.55 | 39090 | ⊕⊕⊝⊝ | |
| Death | 84 per 1000 | 28 per 1000 | RR 0.34 | 39090 | ⊕⊕⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 No serious inconsistency. All four studies report a decrease in attrition at 12 months. | ||||||
| Antiretroviral therapy be started and maintained in health centre for HIV infected patients | ||||||
| Patient or population: HIV infected patients | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Antiretroviral therapy be started and maintained in health centre | |||||
| Death or lost to care | 365 per 1000 | 256 per 1000 | RR 0.7 | 56360 | ⊕⊝⊝⊝ | |
| Lost to care | 270 per 1000 | 81 per 1000 | RR 0.3 | 56360 | ⊕⊕⊕⊝ | |
| Death | 97 per 1000 | 106 per 1000 | RR 1.1 | 55099 | ⊕⊝⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded by 1 for methodological limitations. Bedelu 2008, McGuire 2013 and Massaquoi 2009 included sicker patients at the hospital setting, Assefa has unknown baseline risk as other baseline characteristics were not reported. This bias would tend to favour therapy provided at the health centre. | ||||||
| Decentralisation from the facility to the community for antiretroviral maintenance therapy for HIV‐infected patients | ||||||
| Patient or population: HIV‐infected patients | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Decentralisation from the facility to the community for antiretroviral maintenance therapy | |||||
| Death or lost to care | 106 per 1000 | 101 per 1000 | RR 0.95 | 709 | ⊕⊕⊕⊝ | |
| Lost to care | 26 per 1000 | 21 per 1000 | RR 0.81 | 709 | ⊕⊕⊕⊝ | |
| Death | Moderate | RR 1.03 | 709 | ⊕⊕⊕⊝ | ||
| 55 per 1000 | 57 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Not downgraded for indirectness. Note that the trials were conducted in Kenya and Uganda in adult populations. | ||||||
| Tier | Highest cadre | Terms often used | Facility and staff | Equipment facilities |
| Community | Individual with maximum of few months training; paid or unpaid | 1a. Family led care | Family member |
|
|
| 1b. Village volunteer | Trained volunteer; health assistants | HIV tests, counselling, replenish drugs | |
|
| 1c. Primary care clinic | Nurse aide or community health worker with a few months training |
| |
| Health centre | clinical officer or nurse (2+ years training) | Health centres; district hospitals | Purpose built with at least one paramedic or nurse with some health assistants | HIV tests; antiretrovirals; opportunistic infections medicines; point of care laboratories |
| Health centre (enhanced) | Clinical officer or nurse (2 + years training) | Health centres, primary healthcare clinics, district hospitals | Purpose built with at least one paramedic or nurse with some health assistants, with input from a doctor (may be via mobile support service) | HIV tests; antiretrovirals; opportunistic infections medicines; point of care laboratories |
| Hospital | Doctor | Health centres; district hospitals | Purpose built with at least one medical doctor with nurses / paramedics and assistants | CD4 count Medicines Not viral load |
| Hospital (advanced) | Specialist doctor | District hospital; referral hospital | Purpose built with at least 2 specialist doctors with nurses / paramedics and assistants | Viral load and full investigations |
| Our term | Initiation | Follow‐up |
| Standard hospital model | Hospital | Hospital |
| Partial decentralisation | Hospital | Health centre |
| Full decentralisation | Health centre | Health centre |
| Full decentralisation with regular hospital support | Health centre (weekly clinics with hospital staff) | Health centre (weekly clinics with hospital staff) |
| Community | Primary (tier 1c) Health centre
| Primary (tier 1c) (monitor six monthly by health centre) |
| Models of care | Provider details | Laboratory facilities | Community support | Training in ART initiation and maintenance | Supervision or mentoring | Referral | |
| Partial decentralisation | |||||||
| Bock 2008 | Health centres (enhanced) | Doctors | yes | not stated | not stated | specialists available | yes |
| Hospital (advanced) | Doctors | yes | not stated | yes | specialists available | not applicable | |
| Brennan 2011 | Health centres | Primary health care nurses | not stated | not stated | yes | yes ‐ telephonic | yes ‐ to hospital |
|
| Hospitals | Doctors | not stated | not stated | not applicable | not applicable | not applicable |
| Chan 2010 | Health centres | Nurses and health surveillance assistants | no | Expert patients | yes | yes ‐ from hospital | not stated |
|
| Hospitals | Clinical officers, nurses and doctors | yes | Home‐based care volunteers | not applicable | not applicable | not stated |
| Fatti 2010 | Health centres | Doctors | yes | Community‐based adherence counsellors | not stated | not stated | not stated |
|
| Hospitals | Doctors | yes | not stated | not stated | not stated | not stated |
| Hansudewechakul 2012 | health centres | Nurses | yes | yes | yes | yes | not stated |
| Hospital | Doctors | yes | yes | yes | not applicable | not stated | |
| Humphreys 2010 | Health centres | Nurses | no | not stated | yes | yes ‐ monthly visit from nurse and counsellor | yes |
| Hospital | Doctors | yes | not stated | not applicable | not applicable | not applicable | |
| Full decentralisation | |||||||
| Assefa 2012 | Health centres | Health officers, nurse | not stated | Community health workers, adherence counselling, defaulter tracing, referral and linkage between facilities | not stated | not stated | yes ‐ to hospital |
|
| Hospitals | Doctors | not stated | none | not stated | not stated | not applicable |
| Balcha 2010 | Health centres | Health officers, nurses, data clerk, pharmacy technicians | not stated | not stated | not stated | not stated | yes ‐ to hospital |
|
| Hospitals | Nurses, data clerks, pharmacists | not stated | not stated | not stated | not stated | not applicable |
| Bedelu 2007 | Health centres | Nurses | no | Community health workers, adherence support, defaulter tracing | yes | yes ‐ mobile team | yes ‐ to hospital |
|
| Hospitals | Doctors | yes | no | not stated | not applicable | not applicable |
| Fayorsey 2013 | health centres | doctors and nurses | 8/182 sites CD4 machines | variable by site | not stated | not stated | yes |
| Hospitals | doctors and nurses | 54/92 sites Cd4 machines | variable by site | not stated | not stated | not applicable | |
| Massaquoi 2009 | Health centres | Medical assistants and nurse | yes | yes | yes | yes | yes ‐ to hospital |
|
| Hospitals | Doctors | yes | not stated | yes | not applicable | not applicable |
| McGuire 2012 | Health centres | Clinical officers, nurses and medical assistants | yes | yes | yes | not stated | yes |
| Hospitals | Clinical officers and nurses | yes | yes | not stated | not stated | not applicable | |
| Odafe 2012 | Hospitals | Medical doctors | yes | yes | not stated | not stated | not stated |
| Hospitals (advanced) | Medical specialists | yes | not stated | not stated | not applicable | not applicable | |
| Decentralisation from facility to community | |||||||
| Jaffar | Community | Field officers | no | not stated | yes | yes | yes |
|
| Health centres | Clinical staff | yes | not stated | yes | yes | not applicable |
| Kipp | Community | Unpaid volunteers, >18 years old and literate | no | Treatment supporter to assist with adherence | yes | yes | yes |
|
| Health centres | Doctors | yes | no | not applicable | not stated | not applicable |
| Selke | Community | Community care co‐ordinators | no | Computer aided devices | yes | yes | yes |
|
| Health centres | Clinical officers, doctor (1 day/ week) | yes | no | not applicable | not applicable | not applicable |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death or lost to care (12 months) Show forest plot | 4 | 39090 | Risk Ratio (IV, Random, 95% CI) | 0.46 [0.29, 0.71] |
| 1.1 Adults | 2 | 29492 | Risk Ratio (IV, Random, 95% CI) | 0.49 [0.21, 1.12] |
| 1.2 Children | 1 | 1505 | Risk Ratio (IV, Random, 95% CI) | 0.45 [0.27, 0.74] |
| 1.3 Adults and children | 1 | 8093 | Risk Ratio (IV, Random, 95% CI) | 0.39 [0.35, 0.43] |
| 2 Lost to care Show forest plot | 6 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Lost to care (6 months) | 3 | 28699 | Risk Ratio (IV, Random, 95% CI) | 0.99 [0.56, 1.76] |
| 2.2 Lost to care (12 months) | 4 | 39090 | Risk Ratio (IV, Random, 95% CI) | 0.55 [0.45, 0.69] |
| 2.3 Lost to care (24 months) | 1 | 543 | Risk Ratio (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Death Show forest plot | 6 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Death (6 months) | 3 | 28699 | Risk Ratio (IV, Random, 95% CI) | 0.52 [0.19, 1.41] |
| 3.2 Death (12 months) | 4 | 39090 | Risk Ratio (IV, Random, 95% CI) | 0.34 [0.13, 0.87] |
| 3.3 Death (24 months) | 1 | 543 | Risk Ratio (IV, Random, 95% CI) | 0.04 [0.00, 0.58] |
| 4 Cost of travel Show forest plot | Other data | No numeric data | ||
| 4.1 cost of travel | Other data | No numeric data | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death or lost to care (12 months) Show forest plot | 4 | 56360 | Risk Ratio (IV, Random, 95% CI) | 0.70 [0.47, 1.02] |
| 1.1 Adults | 3 | 52286 | Risk Ratio (IV, Random, 95% CI) | 0.62 [0.39, 0.99] |
| 1.2 Adults and children | 1 | 4074 | Risk Ratio (IV, Random, 95% CI) | 0.97 [0.82, 1.15] |
| 2 Lost to care Show forest plot | 6 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Lost to care (6 months) | 2 | 51261 | Risk Ratio (IV, Random, 95% CI) | 0.53 [0.26, 1.10] |
| 2.2 Lost to care (12 months) | 4 | 56360 | Risk Ratio (IV, Random, 95% CI) | 0.30 [0.17, 0.54] |
| 2.3 Lost to care (24 months) | 4 | 61445 | Risk Ratio (IV, Random, 95% CI) | 0.50 [0.36, 0.71] |
| 3 Death Show forest plot | 6 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Death (6 months) | 2 | 50000 | Risk Ratio (IV, Random, 95% CI) | 0.84 [0.35, 2.00] |
| 3.2 Death (12 Months) | 4 | 55099 | Risk Ratio (IV, Random, 95% CI) | 1.10 [0.63, 1.92] |
| 3.3 Death (24 months) | 4 | 60184 | Risk Ratio (IV, Random, 95% CI) | 0.64 [0.39, 1.06] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death or lost to care (12 months) Show forest plot | 2 | 709 | Risk Ratio (IV, Random, 95% CI) | 0.95 [0.62, 1.46] |
| 2 Lost to care Show forest plot | 3 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Lost to care (6 months) | 1 | 385 | Risk Ratio (IV, Random, 95% CI) | 1.49 [0.81, 2.74] |
| 2.2 Lost to care (12 months) | 2 | 709 | Risk Ratio (IV, Random, 95% CI) | 0.81 [0.30, 2.21] |
| 2.3 Lost to care (24 months) | 1 | 385 | Risk Ratio (IV, Random, 95% CI) | 0.74 [0.46, 1.20] |
| 3 Death Show forest plot | 3 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Death (6 months) | 1 | 385 | Risk Ratio (IV, Random, 95% CI) | 1.44 [0.81, 2.57] |
| 3.2 Death (12 months) | 2 | 709 | Risk Ratio (IV, Random, 95% CI) | 1.03 [0.64, 1.65] |
| 3.3 Death (24 months) | 1 | 385 | Risk Ratio (IV, Random, 95% CI) | 1.50 [0.91, 2.47] |
| 4 Cost to patient Show forest plot | Other data | No numeric data | ||


