Ejercicio para la reducción del temor a las caídas en pacientes mayores que residen en la comunidad
References
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT | |
| Participants | Country: Australia n = 163 67% female Mean age in years (SD) = 75 (5.5) Study population: recruited from general practice clinics or 2 acute physiotherapy departments Inclusion criteria: participants were aged 65 years and older recruited from general practice clinics with 1 or more physical performance impairments known to be important risk factors for falls (i.e. lower limb weakness, poor balance and slow reaction time) Exclusion criteria: cognitive impairments, degenerative conditions or medical condition involving neuromuscular, skeletal or cardiovascular system which could prevent them from taking part in an exercise programme | |
| Interventions | 1. Exercise group (n = 83). Weekly structured exercise group in a community setting, combined with a home exercise programme and written information on practical strategies for avoiding falls. Classes ran for 1 hour, over 4 terms for 1 year (37 classes) and steadily increased in speed and complexity. Class content was designed by a physiotherapist to specifically address physical falls risk factors and was delivered in groups of 6 to 18. Content included stretching, balance, co‐ordination, aerobic capacity and muscle strengthening exercises. The home exercise programme was based on the class content with diaries to record participation. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control group (n = 80). Provided with the same information about falls prevention, but no alternative 'non‐exercise' activity | |
| Outcomes | Number of falls (recorded by retrospective monthly fall calendars); fear of falling (single‐item measure ‐ recorded as % of participants who are afraid of falling); physical activity (Physical Activity Scale for the Elderly (PASE)). Outcomes were measured at baseline and 6 months post baseline. Falls were measured over the 12‐month intervention period | |
| Notes | The outcomes for the study were measured at 6 months into the 12‐month trial as this was deemed a sufficient period to achieve the beneficial results of the exercise programme. Adherence: 91% were still attending exercise classes at the end of the trial and performing home exercises at least once a week | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No further information provided on sequence generation |
| Allocation concealment (selection bias) | Unclear risk | "Subjects were randomised in matched blocks (n = 6) after the baseline assessment using consecutively numbered opaque envelopes". Paper does not say if envelopes were sealed |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Fear of falling, number of falls and PASE were self reported by unblinded participants |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Falls data collected retrospectively by postal survey at the end of each month |
| Methods | RCT | |
| Participants | Country: New Zealand n = 233 100% female Mean age in years (SD) = 84 (3.3) Study population: recruited from general practice registers Inclusion criteria: women aged 80 and over who lived in the community recruited from general practice, able to move around within their own home and not receiving physiotherapy Exclusion criteria: score < 7 from 10 on the Mental Status Questionnaire (MSQ) | |
| Interventions | 1. Exercise group (n = 116). 1‐year home‐based exercise programme prescribed by a physiotherapist. Exercises took approximately 30 minutes to complete and participants were to complete them at least 3 times a week, and walk outside the home at least 3 times per week. The programme included moderate intensity strengthening exercises with ankle cuff weights (0.5 kg and 1 kg), strength, balance and "active range of movement" exercises. The physiotherapist visited participants 4 times over 2 months prescribing a selection of exercise at appropriate and increasing levels of difficulty, and a walking plan. Participants were telephoned regularly to maintain motivation. ProFaNE taxonomy classification: strength/resistance 2. Control group (n = 117). Participants received a social visit from the research nurse 4 times during the first 2 months and telephoned them regularly during the year of follow‐up | |
| Outcomes | Number of falls (recorded by monthly fall calendars); falls efficacy (Falls Efficacy Scale (FES)); physical activity (PASE). Outcomes were measured at baseline and post intervention. FES and PASE only presented as % change from baseline | |
| Notes | Adherence: after 1 year 42% were still completing the exercise programme 3 or more times a week | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The group allocation schedule was developed by a statistician using computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | Central allocation (telephone) after all baseline questionnaires and assessments were completed. List held off site by an independent person |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Number of falls, FES and PASE were self reported by unblinded participants |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Low risk | Appears to be free of other sources of bias |
| Methods | RCT | |
| Participants | Country: Australia n = 34 47% female Mean age in years (SD) = 82 (6.0) Study population: recruited from the Department of Veterans Affairs Home Front Database and a list from a general medical practice Inclusion criteria: community‐dwelling older adults aged 70 years and above who had 2 or more falls or an injurious fall in the past year Exclusion criteria: moderate to severe cognitive problems (> 2 errors on the Short Portable Mental Status Questionnaire); non‐conversational English; unable to walk around independently; resident in nursing home or hostel; unstable or terminal medical illness that would preclude planned exercises; neurological conditions that would result in motor performance difficulties (e.g. Parkinson's disease) | |
| Interventions | 1. Lifestyle approach to reducing Falls through Exercise (LiFE) (n = 18). Home‐based lifestyle‐integrated balance and strengthening exercise programme specifically developed for fall prevention. LiFE was taught in 5 home visits with 2 booster visits over a 3‐month period and 2 follow‐up phone calls. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control (n = 16). No intervention | |
| Outcomes | Number of falls (recorded by monthly fall calendars); falls efficacy (Modified Falls‐Efficacy Scale (MFES)); balance confidence (Activities Specific Balance Confidence Scale (ABC)). Measured at baseline, post intervention and 3 months follow‐up | |
| Notes | Adherence rates not reported MFES and ABC means and SDs obtained through personal communication with author | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation using a random numbers table and stratifying by age and fall history (1 to 2 falls; ≥ 3 falls), but no further information provided |
| Allocation concealment (selection bias) | High risk | Open random allocation schedule. Participants were allocated in order of completion from random number list by an investigator not involved in assessment or intervention |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Number of falls, MFES and ABC were self reported by unblinded participants |
| Incomplete outcome data (attrition bias) | High risk | Outcome data are based on > 80% of participants in intervention group, but < 80% for the control group |
| Selective reporting (reporting bias) | High risk | Stated that adherence was monitored for the exercise group but data are not presented. Protocol not available |
| Other bias | Unclear risk | The intervention group were able to stand for longer on the tandem stand eyes open test (median 15 seconds) than the control group (median 1.65 seconds) at baseline. This baseline difference was adjusted for in the falls analysis and the results remained significant. The LiFE intervention was developed collaboratively by 4 of the authors |
| Methods | RCT | |
| Participants | Country: Germany n = 144 (groups 2 and 4 below) 47% female Mean age in years (SD) = 76 (4.1) Study population: recruited from a health insurance database Inclusion criteria: community‐dwelling older adults aged 70 to 90 who had fallen in the past 6 months or reported a fear of falling Exclusion criteria: those who were unable to walk around independently or had cognitive impairment (as noted by a score < 25 on the Digit Symbol Substitution Test (DSST)) | |
| Interventions | 1. Strength and Balance Group (SBG) (n = 63). Weight‐bearing exercises with dumbbells and balance challenging exercises, stretching, plus sensory training including standing and walking with eyes closed or on unstable surfaces and training in the perception of centre of gravity in relation to the base of support 2. Fitness Group (FG) (n = 64). Strength and balance exercise with endurance training (walking with change of pace and direction and Nordic walking). ProFaNE taxonomy classification: strength/resistance 3. Multifaceted Group (MG) (n = 73). Strength and balance training with fall risk education to address fall‐related psychological aspects and cognitive training 4. Control Group (n = 80). No intervention All active interventions included progressive exercises for upper and lower body strength, standing weight‐bearing exercises with dumbbells and balance exercises. Interventions were provided by 2 fall prevention instructors for a period of 16 weeks with 2 1‐hour group sessions per week The intervention group used in the meta‐analysis comprised only the FG | |
| Outcomes | Number of falls (recorded by monthly fall calendars); balance confidence (ABC); measured at post intervention, 6 months and 18 months follow‐up. ABC score at 6 months follow‐up used in the analysis of fear of falling at 6 months or more post intervention | |
| Notes | Adherence rates: majority of participants (> 80%) attended at least 24 of the 32 sessions | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A third party not involved in the study applied a computerised random‐number generator |
| Allocation concealment (selection bias) | Unclear risk | A third party not involved in the study applied a computerised random number generator |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Number of falls and ABC were self reported by unblinded participants |
| Incomplete outcome data (attrition bias) | High risk | Outcome data are based on < 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | No baseline scores for ABC presented. The control group had a greater proportion reporting fear of falling and higher education levels than the intervention group (fitness group) at baseline. Analyses were adjusted for these variables. The majority of falls occurred during sports activities (including cycling and skiing) |
| Methods | RCT | |
| Participants | Country: Australia n = 53 60% female Mean age in years (SD) = 81 (7.7) Study population: patients of a publicly funded, metropolitan, tertiary hospital Inclusion criteria: aged 65 years and over, treated on the geriatric rehabilitation medical or surgical units of a local hospital being planned for discharge to the community, gait instability as determined by physiotherapists or walked with a mobility aid Exclusion criteria: severe cardiac disease, cognitive impairment (determined by Abbreviated Mental Test Score less than 6 out of 10), aggressive behaviour, restricted lower limb weight‐bearing status or had been referred for post discharge community rehabilitation services | |
| Interventions | 1. Exercise Group (n = 19). A DVD and workbook describing a progressive 2‐month home exercise programme based on the Kitchen Table exercise programme containing lower limb strength and balance exercises with 6 types of exercises each with 6 different levels of difficulty. A physiotherapist visited participants at home to help engagement with the DVD and workbook, ensure a safe environment and set appropriate starting level.The physiotherapist also made weekly phone calls for 8 weeks after the first home visit to measure participation in the exercise programme and to give advice on any problems the participants had encountered in attempting the exercise programme. Participants were encouraged to continue the exercise after the 8 weeks. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control (n = 34). No intervention | |
| Outcomes | Number of falls (recorded by monthly fall calendars); balance confidence (ABC). Measured at baseline and post intervention | |
| Notes | Adherence: less than 50% were still completing the exercise programme at the end of the trial | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random number generator |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, sealed, opaque envelopes (with participant numbers) |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Number of falls and ABC scales were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Control group had longer length of hospital stay and higher median number of falls than intervention group at baseline |
| Methods | RCT | |
| Participants | Country: Sweden n = 59 71% female Mean age in years (range) = 77 (67 to 93) Study population: recruited from advertisements in local newspapers Inclusion criteria: community‐dwelling older people aged 65 years or older, with a fear of falling and/or an experience of a fall during the previous 12 months. An ability to walk unaided indoors and a mini mental state examination score equal or greater than 24. Recruited by advertisements in local newspapers Exclusion criteria: severely impaired vision or hearing, severe cancer, severe pain, neurological disease or damage with symptoms, dizziness requiring medical care, or heart and respiratory symptoms that might affect participation | |
| Interventions | 1. Balance group training (n = 38). Individually adjusted progressive and specific balance training, provided by physiotherapists for 45 minutes 3 times per week for 3 months. The programme was performed at 5 levels, each reflecting different demands on the postural control system. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control (n = 21). No intervention | |
| Outcomes | Concern about falling (FES‐International (FES‐I); depressive symptoms (Geriatric Depression Scale‐20 (GDS‐20)). Measured at baseline and post intervention | |
| Notes | Adherence rates not reported FES‐I and GDS‐20 means and SDs obtained through personal communication with author | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Subjects drew an allocation slip from an envelope filled with 20 slips in a 2:1 ratio. No further information given on sequence generation |
| Allocation concealment (selection bias) | High risk | Participants could possibly see their allocation as they drew the allocation slip themselves from the envelope. No further information provided |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | FES‐I and GDS‐20 were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | High risk | GDS scores not presented. Protocol not available |
| Other bias | Low risk | Appears to be free of other sources of bias |
| Methods | RCT | |
| Participants | Country: USA n = 97 63% female Mean age in years (range) = 72 (63 to 87) Study population: recruited from local community. No further details given Inclusion criteria: able to walk around independently (unassisted or with a walking aid) and be able to follow a structured exercise programme Exclusion criteria: acute neurological or orthopaedic conditions, history of dementia | |
| Interventions | 1. Home Exercise (HE) Programme (n = 32). Participants expected to perform a set of 20‐minute balance exercises and activities on an independent basis 3 times a week for 4 weeks. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Computer Balance (CB) Training (n = 34). Biodex balance system which provides an unstable platform that moves in response to changes in the user's centre of mass and tilts up to 20 degrees in every direction. 4‐week programme with 8 stability levels, supervised by a research assistant. First 2 weeks consisted of a 10‐minute warm‐up and then 10 minutes training. Final 2 weeks consisted of a 15 minute warm‐up and then 15 minutes training. In the final week, participants were given goggles to obscure their vision during the warm‐up exercises. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 3. Control group (n = 31). No training programme for 4 weeks and advised not to engage in any new exercise or training programmes for the duration of the trial The intervention group used in the analysis comprised the combined HE and CB groups | |
| Outcomes | Falls efficacy (MFES). Measured at baseline and post intervention | |
| Notes | Adherence: over 90% adhered to the exercise programme. Cash incentive offered | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned but no further information provided |
| Allocation concealment (selection bias) | Unclear risk | No information on allocation concealment provided |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | MFES was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Participants received a monetary compensation for their participation in the study, with intervention groups compensated at a higher rate than the control group |
| Methods | RCT | |
| Participants | Country: Finland n = 149 100% female Mean age in years = 73 (2.3) Study population: random population sample invited to express interest in study by post Inclusion criteria: 70 to 79‐year old women living in the city of Tampere, Finland; willingness to participate, full understanding of the study procedures, no history of any illness contraindicating exercise or limiting participation in the exercise programme or of illness affecting balance or bone, no uncorrected vision problems, and taking no medications known to affect balance or bone metabolism (within 12 months before the enrolment) Exclusion criteria: participants were excluded if they did high‐intensity exercises more than twice a week or if there femoral‐neck T score was lower than –2.5 (i.e. indicating osteoporosis and requiring medical attention) | |
| Interventions | 1. A resistance‐training (RT) group (n = 37). The resistance training consisted of exercises for large muscle groups with increasing intensity from 50% to 60% of 1‐repetition maximum (1RM) to 75% to 80% of 1RM. ProFaNE taxonomy classification: strength/resistance 2. A balance‐jumping (BJ) group (n = 37). The balance‐jumping training comprised modified aerobics and step aerobics including a variety of balance, agility and impact exercises The degree of difficulty of movements, steps, impacts, and jumps was gradually increased. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 3. A combination (CG) group doing resistance and balance‐jumping training (n = 38). The combination training programme consisted of resistance and balance‐jumping training in alternating weeks. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 4. No intervention (n = 37). Participants in the control group were asked to maintain their pre‐study level of physical activity during the 12‐month trial The intervention lasted for 3 weekly sessions of 45 minutes for 12 months The intervention group used in the analysis comprised the combined RT, BJ and CG groups | |
| Outcomes | Fear of falling (visual analogue scale ‐ no fear at all (0) to very great fear (100)). Measured at baseline, post intervention and 12 months | |
| Notes | Adherence: 67% adhered to the exercise programmes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation list |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | VAS was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Self rated general health slightly better in the intervention group than control group at baseline |
| Methods | RCT ‐ cross‐over design | |
| Participants | Country: Taiwan n = 30 57% female Mean age in years (SD) = 72 (4.6) Study population: recruitment not described Inclusion criteria: community‐dwelling older adults aged 65 years and above Exclusion criteria: participants were excluded if they had a neurological condition such as Parkinson's disease, dementia and stroke, or if they had arthritis, vision impairment and cardiovascular disease that impaired walking, or if they were unable to walk without assistance | |
| Interventions | 1. Xavix Measured Step System (XMSS) (n = 15) console with 1 step mat and connectors to TV. The XMSS exercise was conducted for 30 minutes, 3 times a week for 6 weeks. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control group (n = 15). No intervention for the first 6 weeks, then given XMSS exercises for 6 weeks. The first 6 weeks served as the control | |
| Outcomes | Falls efficacy (MFES). Measured at baseline and post intervention, and 6 weeks post intervention (after cross‐over) | |
| Notes | Adherence rates not reported Data were used from the first period prior to cross‐over | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned but no further information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | MFES was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Intervention group had higher MFES and Berg Balance Scale scores and lower Timed Up and Go times at baseline than control group |
| Methods | Quasi‐randomised trial | |
| Participants | Country: Canada n = 24 83% female Mean age in years (SD) = 71 (not reported) Study population: recruited from the community and from residential care facilities Inclusion criteria: aged 65 or older, able to stand and walk without an aid Exclusion criteria: participants with diabetes, neurological or sensory disorders, recurrent dizziness or unsteadiness, use of medications that may affect balance, joint replacement and medical conditions interfering with daily activities | |
| Interventions | 1. Computerised balance training group (n = 12). 1‐hour computerised balance training sessions completed twice per week over an 8‐week period. Participants stood on a Kistler force platform and were asked to complete 15 computerised balance tests lasting 1 minute each, with resting periods given after each trial. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control group (n = 12). No intervention | |
| Outcomes | Balance confidence (ABC). Measured at baseline and post intervention | |
| Notes | Adherence rates not reported ABC means and SDs obtained through personal communication with author | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Sequence generated by alternation. The author stated in a personal communication that this was achieved by "First subject was in group 1, second in group 2, third in group 1 etc." |
| Allocation concealment (selection bias) | High risk | Allocation not concealed. Quasi‐randomised study |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | ABC was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Paper describes only minimal baseline characteristics, so unclear if groups well balanced at baseline |
| Methods | RCT | |
| Participants | Country: Taiwan n = 100 (groups 1 and 2 only) 51% female Mean age in years (SD) = 77 (not reported) Study population: recruited from clinics and hospitals in rural agricultural area Inclusion criteria: community‐dwelling older adults aged 65 and older who had required medical attention due to sustaining a fall in the previous 4 weeks Exclusion criteria: none specified | |
| Interventions | Intervention details: 1. Home‐based exercise group (n = 50). The intervention consisted of stretching, muscle strengthening and balance training. Participants exercised at home once every 2 weeks under supervision and were instructed to practice these exercises at least 3 times a week during the 4‐month intervention period. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Home safety assessment and modification group (n = 50). Participants were visited by a public health worker to perform a safety assessment on their home environment and given a list of specifically recommended modifications 3. Education group (n = 50). Participants received 1 social visit of 30 to 40 minutes every 2 weeks over the study period, plus pamphlets on falls prevention, including stretching and strengthening exercises to encourage initiation and persistence in activities The intervention group used for this review comprised the home‐based exercise group and the control group comprised the home safety assessment and modification group | |
| Outcomes | Fear of falling (visual analogue scale); 15‐item Geriatric Depression Scale (GDS); number of falls (self reported). Measured at baseline, and 2 and 4 months post intervention | |
| Notes | Fear of falling was assessed using a 10 cm visual analogue scale, marked with the labels "No fear" and "Extremely fearful" where participants were asked to place a mark on the line at the point representing the extent of their fear Adherence rates not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Block randomised, but no information provided about randomisation sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | VAS and GDS‐15 self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | High risk | Outcome data are based on ≥ 80% of participants in control group, but < 80% in intervention group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all prespecified outcomes have been reported |
| Other bias | Unclear risk | Most baseline characteristics not presented by treatment group so unclear if groups well balanced at baseline |
| Methods | RCT | |
| Participants | Country: Netherlands n = 269 71% female Mean age in years (SD) = 77 (4.7) Study population: recruited from general practices Inclusion criteria: aged 70 years and older living at home and having a high falls risk (defined as 1 or more self reported fall incidents in the year preceding the study or at least 2 self reported risk factors for falling (disturbed balance, mobility problems, dizziness, and the use of benzodiazepines or diuretics)) Exclusion criteria: none specified | |
| Interventions | 1. Tai Chi Chuan group (n = 138). Participants received 1 hour of Tai Chi Chuan training twice a week for 13 weeks. Classes were provided by 4 professional Tai Chi Chuan instructors using a predefined protocol. Participants were encouraged to practice at home at least twice a week for 15 minutes. Also received a brochure explaining how to prevent fall incidents in and around the house. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 2. Control group (n = 131). No intervention | |
| Outcomes | Number of falls (recorded by monthly fall calendars); falls efficacy (FES); physical activity (PASE). Measured at baseline, post intervention and 9 months follow‐up | |
| Notes | Adherence: 47% attended at least 80% of the Tai Chi lessons | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation list |
| Allocation concealment (selection bias) | Unclear risk | No information provided on allocation concealment. An independent research assistant performed a pre‐stratified block randomisation |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Number of falls, FES and PASE were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | High risk | Outcome data are based on < 80% of participants in each group at all follow‐up time points |
| Selective reporting (reporting bias) | Low risk | Protocol available. All pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Inconsistency between the number of participants with missing data in flow chart and the denominators reported in the text for falls outcomes |
| Methods | RCT | |
| Participants | Country: Australia n = 43 70% female Mean age in years (SD) = 79 (5.9) Study population: recruited from the community by postal invitation Inclusion criteria: community‐dwelling older adults aged 65 years and over Exclusion criteria: participants were excluded if they reported uncontrolled hypertension, heart attack in the previous year, irregular heart beat and if they already belonged to a formal exercise class | |
| Interventions | 1. Conventional Exercise (CE) group (n = 17). Low intensity stretching and conditioning exercises using body weight and light dumbbells as resistance. Performed 2 days per week for 10 weeks with each session approximately lasting 30 to 45 minutes. ProFaNE taxonomy classification: strength/resistance 2. Holistic exercise (HE) group (n = 18). Participants used a Range of Motion (RoM) dance method using the principles of Tai Chi. Performed 2 days per week for 10 weeks with each session approximately lasting 30 to 45 minutes. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 3. Control group (n = 8). No intervention The intervention group used in the analysis comprised the combined CE and HE groups | |
| Outcomes | Falls efficacy (MFES). Measured at baseline and post intervention | |
| Notes | Adherence: adherence did not differ between groups. Combined adherence over 80% in each group Data on the number of females obtained from personal communication with author | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided about sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | MFES was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | High risk | Outcome data are based on < 80% of participants in Holistic and Conventional exercise groups, and > 80% of participants in the control group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Very minimal baseline data presented so unclear if groups well balanced at baseline |
| Methods | RCT | |
| Participants | Country: Vietnam n = 96 50% female Mean age in years (SD) = 69 (5.1) Study population: recruitment not described Inclusion criteria: community‐dwelling older adults aged 60 to 79 years old. Being able to finish the Mini Mental State Examination (MMSE) with a score greater than 25 and having no experience in Tai Chi Exclusion criteria: serious diseases, such as symptomatic coronary insufficiency, angina, arrhythmia, orthostatic hypotension, and dementia | |
| Interventions | 1. Tai Chi (n =48). Participants in the Tai Chi group attended a 60‐minute Tai Chi practice session twice a week for 6 months. The session consisted of a 15‐minute warm‐up and a 15‐minute cool‐down period. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 2. No intervention (n = 48) | |
| Outcomes | Falls efficacy (FES). Measured at baseline, interim and post intervention | |
| Notes | Adherence rates not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned but no further information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | FES was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | High risk | Outcome data are based on > 80% of participants in intervention group but < 80% of participants in the control group |
| Selective reporting (reporting bias) | Unclear risk | Time periods for interim data not reported. Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | FES slightly higher in control group than intervention group at baseline |
| Methods | Cluster‐RCT with randomisation by senior centre | |
| Participants | Country: USA n = 107 (groups 1 and 4 only) and 8 senior centres 89% female Mean age in years (SD) = 75 (7.5) Study population: recruited from 16 senior centres located in low socioeconomic areas Inclusion criteria: aged over 60 living in a senior centre Exclusion criteria: none given | |
| Interventions | Intervention details: 1. Exercise intervention (n = 57). Participants performed the low intensity "stand‐up/step‐up" exercises, designed to improve strength and balance for 1 hour 3 times per week for 1 year. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Cognitive‐behavioural intervention (n = 51). Participants received health and safety advice to prevent falls, relaxation training and video game playing to improve reaction time 1 hour per week for 1 year 3. Exercise‐cognitive intervention (n = 72). 1 meeting per week as per cognitive behavioural intervention group and 2 meetings per week focusing on exercise, relaxation training and discussion of safety topics for 1 year 4. Discussion control group (n = 50). Participants discussed health and discussion topics of interest to older people 1 hour per week for 1 year The intervention group used for this review comprised the exercise group and the control group comprised the discussion group | |
| Outcomes | Fear of falling (measured by 5‐point scale (1 = not at all worried to 5 = extremely worried)) | |
| Notes | Adherence: 77% of the exercise group attended at least 67% of the exercise classes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned but no further information provided |
| Allocation concealment (selection bias) | Unclear risk | Senior centres were randomised but no information given on concealment of allocation |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Fear of falling and number of falls self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | High risk | Outcome data are based on < 80% of participants in the intervention group but > 80% of participants in the control group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Analyses do not appear to be adjusted for clustering |
| Methods | RCT | |
| Participants | Country: USA n = 40 65% female Mean age in years (SD) = 85 (5.4) Study population: recruited from retirement communities Inclusion criteria: community‐dwelling adults between 60 and 95 years of age, able to participate in physical activity for 45 to 60 minutes and who verbally reported having normal vision Exclusion criteria: participants with known orthopaedic, neurological or circulatory disorders that would prevent them from participating in the study | |
| Interventions | 1. Virtual reality group (n = 20). Participants used 3 different balance games from the Nintendo® Wii Fit Software package. Participants alternated the exercise game sequence week‐to‐week during the 18‐session intervention (3 times a week for 6 weeks). Each session lasted approximately 35 to 45 minutes. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. No intervention (n = 20) | |
| Outcomes | Balance confidence (ABC); depressive symptoms (Geriatric Depression Scale). Measured at baseline and post intervention | |
| Notes | Adherence: 80% met the 15 sessions minimum | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned but no further information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided on allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | ABC and GDS were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Little baseline data presented. ABC score was higher at baseline in the control group than the intervention group. GDS score was higher at baseline in the intervention group than the control group |
| Methods | Cluster‐RCT with randomisation by senior centre | |
| Participants | Country: USA n = 166 participants and 13 senior centres 81% female Mean age in years (SD) = 73 (8.2) Study population: recruited from senior centres Inclusion criteria: community‐dwelling urban minority older adults aged 60 years and older, having a blood pressure recording less than 200/100, heart rate between 60 to 120, no known recent (within past 6 months) history of heart attack, stroke or new irregular heartbeat Exclusion criteria: not obtaining consent from their primary health care provider | |
| Interventions | 1. Senior Exercise Self‐efficacy Project (SESEP) group (n = 100). 12 weeks of twice weekly exercise sessions, each lasting between 60 and 90 minutes, and including stretching, resistance and aerobic activities; plus 30 minutes per week of group efficacy‐enhancing programme. ProFaNE taxonomy classification: strength/resistance 2. Control (n = 66). Participants provided with twice weekly 60 to 90‐minute sessions of nutrition education for 12 weeks | |
| Outcomes | Fear of falling (self rated on a scale of 0 to 4); depressive symptoms (GDS); overall activity (Yale Physical Activity Survey (YPAS)). Measured at baseline and post intervention | |
| Notes | Adherence: mean adherence rate was 77% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generated by coin toss |
| Allocation concealment (selection bias) | Unclear risk | Senior centres were randomised by geographic area using coin toss. No information given on concealment of allocation |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Fear of falling, GDS and YPAS self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | High risk | Outcome data are based on < 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Analyses do not appear to be adjusted for clustering |
| Methods | RCT | |
| Participants | Country: Finland n = 28 100% female Mean age in years (SD) = 82 (5.2) Study population: recruited from residential care homes Inclusion criteria: female, aged 70 years or over, living in residential care Exclusion criteria: unable to stand without a walking aid, unable to see visual feedback from a computer screen and unable to follow instructions | |
| Interventions | 1. Exercise (n = 20) group. Participants attended 20‐ to 30‐minute long individualised specific balance exercise sessions using a computerised force platform with visual feedback 3 times a week for 4 weeks. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control (n = 8) group. No intervention | |
| Outcomes | Number of falls (self reported monthly fall calendar); Fear of falling (single‐item measure ("No", "Yes, some", "Yes, a lot"); physical activity (the Senior Fitness Test). Measured at baseline, post intervention and 12‐month follow‐up | |
| Notes | Adherence: over 90% adhered to the exercise programme | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done in blocks by drawing lots |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Number of falls and fear of falling were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Intervention group undertook more physical activity and more reported high fear of falling at baseline than control group |
| Methods | RCT | |
| Participants | Country: Australia n = 54 80% female Mean age in years (SD) = 68 (7.1) Study population: recruited from advertisements in local newspapers, newsletters and websites Inclusion criteria: participants were eligible if they were community‐dwelling, aged 59 years or older, were cognitively intact (defined as a score of ≥ 7 on the Short Portable Mental Status Questionnaire) and were willing and able to attend 12 weeks of group‐based yoga classes Exclusion criteria: having a medical condition that precludes exercise (e.g. unstable cardiac disease, uncontrolled hypertension, uncontrolled metabolic diseases, and large abdominal aortic aneurysm), minimal English language skills, hostel or nursing home resident, and/or current participation in yoga or Tai Chi | |
| Interventions | 1. Yoga (n = 27). Participants attended a 1‐hour, twice‐weekly, group‐based yoga class for 12 weeks. Participants were also instructed to practise the poses at home for 10 to 20 minutes on at least 2 days per week. The balance challenge increased over time by gradually increasing the difficulty of the postures performed. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 2. Control (n = 27) group. Provided with information about falls prevention | |
| Outcomes | Concern about falling (FES‐I). Measured at baseline and post intervention | |
| Notes | Adherence: 70% attended at least 20 out of 24 classes, 30% attended all classes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number schedule |
| Allocation concealment (selection bias) | Unclear risk | An investigator not involved in recruitment performed a pre‐stratified block randomisation using a computer‐generated random number schedule. No further information provided on allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | FES‐I was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Higher proportion of control group reported balance as fair or poor than the intervention group at baseline |
| Methods | RCT | |
| Participants | Country: USA n = 47 70% female Mean age in years (SD) = 76 (7.3) Study population: recruited from senior centres, churches and retirement communities Inclusion criteria: older adults aged 65 years or older Exclusion criteria: participants were screened on the Mini‐Mental State Examination and their performance on the Timed Up and Go (TUG). No further information provided | |
| Interventions | 1. Feldenkrais intervention (FG) (n = 25). 1‐hour Feldenkrais sessions were held 3 times per week for 5 weeks. Feldenkrais is a mind‐body exercise that involves gentle movements carried out in a quiet, non‐competitive environment focused on improving balance and mobility. Classes were taught by a certified Feldenkrais teacher. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 2. Control group (n = 22). Waiting list control | |
| Outcomes | Falls efficacy (FES); balance confidence (ABC). Measured at baseline and post intervention | |
| Notes | Adherence: over 90% adhered to the exercise programme. 6 of the control group crossed over to the FG at the end of the intervention period. Their data are only included prior to cross‐over FES and ABC means and SDs obtained through personal communication with author | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The screening TUG score and age were used to complete the stratified randomisation of participants. No further information provided |
| Allocation concealment (selection bias) | Unclear risk | No information given on allocation concealment. Persons who expressed a desire to attend the same class (couples, friends and carpool) were allowed to do so in order to facilitate participation. Members of these units were assigned to the same treatment |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | FES and ABC were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | The control group had a lower BMI and had experienced a higher number of falls in the 3 months prior to randomisation than the intervention group |
| Methods | RCT | |
| Participants | Country: Australia n = 180 79% female Mean age in years (SD) = 80 (7.0) Study population: inpatients from aged care and rehabilitation services were approached to participate after leaving hospital Inclusion criteria: older people aged 65 years or older recently discharged from an Aged Care and Rehabilitation hospital, who were medically fit to exercise and had completed hospital‐related rehabilitation Exclusion criteria: participants were excluded if they had medical contraindications to exercise, if they were cognitively impaired (Mini‐Mental State Examination score < 24 out of 30), or if they were discharged to a high‐care residential facility | |
| Interventions | 1. Seated exercises (SE) (n = 60). Prescribed exercises to be performed while sitting on a standard dining chair with cuff weights and exercise bands. Exercises were to be done 3 times a week for 12 weeks, with the physiotherapist visiting 8 times in the 12 weeks to ensure the exercises were being performed correctly and to progress exercise intensity. ProFaNE taxonomy classification: strength/resistance 2. Weight‐bearing exercises (WBE) (n = 60). Prescribed strengthening and resistance exercises to be performed while standing with a chair or bench for support if required. Resistance was provided with weight‐loaded waist belts. Exercises were to be done 3 times a week for 12 weeks, with the physiotherapist visiting 8 times in the 12 weeks to ensure the exercises were being performed correctly and to progress exercise intensity. ProFaNE taxonomy classification: strength/resistance 3. Control group (n = 60). Received a 1‐hour social visit by a research assistant each week for 12 weeks The intervention group used in the analysis comprised the combined SE and WBE groups | |
| Outcomes | Number of falls (self reported weekly fall calendar); falls efficacy (MFES); depressive symptoms (GDS). Measured at baseline, post intervention and 3 months follow‐up | |
| Notes | Adherence: mean adherence rate was 70% in the seated exercise group, and 62% in the weight‐bearing group MFES means and SDs obtained through personal communication with author | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was performed in blocks of 15 participants by computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Allocations for each participant were concealed in opaque envelopes. Unclear if envelopes were sealed or not |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Number of falls, MFES and GDS were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Methods | RCT | |
| Participants | Country: Australia n = 62 76% female Mean age in years (SD) = 75 (8.2) Study population: recruited from advertisements in newspapers, promotion at local community groups and retirement villages and from volunteers in a research database Inclusion criteria: adults aged 55 years or over living at home, in a retirement village or a low‐care residential aged‐care facility, and who have at least 1 functional impairment (based on the Frenchay Activity Index) or have a history of 1 or more falls in the previous 6 months Exclusion criteria: cognitive impairment (< 7 on the Abbreviated Mental Test Score), inability to understand English, and unable to stand unsupported for at least 1 minute or walk a short distance indoors (minimum 5 metres) without a walking aid | |
| Interventions | 1. Exercise group (n = 29). Participants participated in the Getting Grounded Gracefully programme based on the Feldenkrais method to specifically target dynamic balance, postural and turning stability, and weight‐shift transfers, which involved 2 40‐ to 60‐minute sessions per week over an 8‐week period. Classes were conducted at a community‐library meeting group and provided by the programme designer, an experienced Feldenkrais practitioner. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 2. Control group (n = 33). No intervention | |
| Outcomes | Falls efficacy (MFES). Measured at baseline and post intervention | |
| Notes | Participants included those living in low‐care residential homes where they were provided with help with dressing, eating, bathing and other support services such as cleaning, laundry and meals. No nursing care provided Adherence: mean adherence rate was 88% Personal communication with author to confirm participants were not receiving nursing care at the low‐care residential facility | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly ordered opaque envelopes used, but no information provided on how random sequence generated |
| Allocation concealment (selection bias) | Unclear risk | Participants were randomised to the intervention group or control group by the use of randomly ordered opaque envelopes by a research officer not involved in the assessments. Unclear if envelopes were sealed |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | FES was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | A conflict of interest might have been present in that the designer (and supplier) of the Getting Grounded Gracefully programme was the Feldenkrais practitioner in this study and that CDs of the programme were purchased by interested participants at the end of the study |
| Methods | RCT ‐ cross‐over design | |
| Participants | Country: USA n = 77 74% female Mean age in years (range) = 81 (61 to 92) Study population: recruited from posted flyers and flyers on bulletin boards in residential facilities Inclusion criteria: older adults (age range 61 to 92 years) living independently in a continuing care retirement community Exclusion criteria: history of hip fracture or replacement, currently enrolled in a balance study, knee replacement, Parkinson's disease, neurological condition which interfered with balance or walking, leukaemia or cancer, using an assistive device to walk 25 feet or further, Mini‐Mental State Exam score < 24 | |
| Interventions | 1. Tai Chi Chuan (TC) group (n = 41). 1‐hour twice weekly Tai Chi classes conducted for 20 weeks focusing on gait, balance and strength. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 2. Control group (n = 36). No intervention for the first 20 weeks, then given Tai Chi classes for 20 weeks. The first 20 weeks served as the control | |
| Outcomes | Balance confidence (ABC). Measured at baseline, 10 weeks post baseline, post intervention and 5 months follow‐up | |
| Notes | Adherence rates not reported Data were used from the first period prior to cross‐over ABC means and SDs obtained through personal communication with author | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Patients were "randomised" to a group, but no information provided on how randomisation sequence generated |
| Allocation concealment (selection bias) | Unclear risk | "After all eligible patients completed the baseline assessments, they were randomised to the early or late groups." No information provided on allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | ABC was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | High risk | Outcome data are based on < 80% of participants in each group. Only 46% of participants remained in trial at 40 weeks. Those remaining had significantly higher baseline functional assessment scores than those lost to follow‐up |
| Selective reporting (reporting bias) | High risk | No baseline or follow‐up data reported for ABC. Protocol not available |
| Other bias | Unclear risk | Most baseline data only presented for those with outcome data at specific time points. Unclear if groups well balanced at baseline |
| Methods | Randomised trial with additional non‐randomised group | |
| Participants | Country: The Netherlands n = 58 (groups 1 and 2 only) 72% female Mean age in years (SD) = 74 (5.7) Study population: recruited from advertisements in newspapers Inclusion criteria: community‐dwelling older adults aged 65 and over, with at least 1 fall prior to participation and able to walk 15 minutes without the use of a walking aid Exclusion criteria: severe cardiac, pulmonary or musculoskeletal disorders, pathologies associated with increased fall risk (i.e. stroke or Parkinson's disease), osteoporosis and the use of psychotropic drugs | |
| Interventions | 1. Exercise group (n = 30). Twice weekly 1.5‐hour exercise sessions for 5 weeks comprised of balance, gait and co‐ordination training in an obstacle course, walking exercises that stimulated walking in a crowded environment with changes in speed and direction, the practice of fall techniques derived from marital arts. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control group (n = 28). No intervention 3. Non‐randomised group (n = 49). Assigned same exercise as Exercise group above. Non‐randomised group participants have been excluded from analyses in this review | |
| Outcomes | Number of falls (recorded by monthly fall calendars) measured at baseline, 6 months and 7 months follow‐up after intervention. Balance confidence (ABC). Measured at baseline and post intervention | |
| Notes | Adherence: mean attendance rate was 87% for the combined exercise group and non‐randomised group ABC means and SDs (excluding non‐randomised group) obtained through personal communication with author | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The following information was obtained from Gillespie 2012. Quote: "Block randomisation (3 blocks of 20) with gender stratification with equal probability for either exercise or control group assignment." |
| Allocation concealment (selection bias) | Unclear risk | The following information was obtained from Gillespie 2012. Quote:"The group allocation sequence was concealed (to both researchers and participants) until assignment of interventions. We had participants draw a sealed envelope with group allocation ticket from a box containing all remaining envelopes in the block" |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Falls incidence and ABC were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | The intervention group had a significantly higher proportion of fallers at baseline than the control group |
| Methods | RCT | |
| Participants | Country: Canada n = 36 % female not reported Mean age in years (SD) = not reported Study population: recruited from advertisements in newspapers and flyers Inclusion criteria: community‐dwelling older adults aged 65 years and older Exclusion criteria: pre‐existing major lower extremity pathology neurological disorders or balance difficulties, and health conditions that would prevent participation in the exercise programme | |
| Interventions | 1. Exercise group (n = 17). 1‐hour sensory specific balance classes were held 3 times per week over an 8‐week period, following the FallProof programme which focuses on static and dynamic balance exercises with transitions between different sensory conditions. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control group (n = 19). 1‐hour falls prevention education group, held once a week for 8 weeks. The education group received information about 'non‐exercise' related potential fall risk factors, such as nutrition, environmental hazards and the importance of sleep | |
| Outcomes | Balance confidence (ABC); physical activity (PASE). Measured at baseline and post intervention. Additionally the exercise group were re‐assessed at 2 months follow‐up | |
| Notes | Adherence: mean adherence rate was 66% Personal communication with author confirmed no exercise information was provided to the control group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomised into the exercise or education group. No information given on generation of randomisation schedule |
| Allocation concealment (selection bias) | Unclear risk | No information provided on allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | ABC and PASE were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | Unclear risk | 44 participants randomised into the exercise or control group. The number per group at baseline is not reported. Outcomes assessed on 17 exercise group and 19 control group participants |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Limited baseline data reported so unable to assess if groups were well balanced at baseline |
| Methods | RCT | |
| Participants | Country: USA n = 200 81% female Mean age in years (SD) = 76 (4.7) Study population: recruited by advertisements in newspapers and from an independent living facility Inclusion criteria: aged 70 years and older, living in unsupervised environments, ambulatory and agreeing to participate weekly for 15 weeks with 4‐month follow‐up Exclusion criteria: the presence of debilitating conditions such as cognitive impairments, metastatic cancer, crippling arthritis, Parkinson's disease or major stroke, or profound visual defects that could compromise balance or ambulation | |
| Interventions | 1. Computerised Balance Training (BT) group (n = 64). Individual balance training on a computerised force platform. Participants had 1 hour of instruction per week (with approximately 45 minutes individual contact time with an instructor) for 15 weeks. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Tai Chi Quan (TC) group (n = 72). Classes of Tai Chi Quan focusing on all components of movement that typically becomes limited with ageing. Participants had 2 hours of instruction per week (2 separate sessions) with a total of approximately 45 minutes contact time with an instructor. Participants were encouraged to practice at least 15 minutes twice a day at home. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 3. Education group (n = 64). Weekly 1‐hour meetings for 15 weeks were held with a gerontological nurse/researcher to discuss a variety of topics such as pharmacological management, sleep disorders, cognitive deficits, coping with bereavement and other issues important to each group The intervention group used in the analysis comprised the combined BT and TC groups | |
| Outcomes | Number of falls (recorded by weekly fall calendars); falls efficacy (FES) and Center for Epidemiologic Studies ‐ Depression (CES‐D) scale. Falls were defined using the FICSIT definition ("unintentionally coming to rest on the ground, floor or lower level") and the Atlanta site definition ("falls resulting in fractures, dislocation, sprains, bruises, lacerations, scrapes and other medical problems"). Mean and SD for FES presented at baseline and categories of fear of falling (not at all afraid, somewhat afraid, fairly afraid, very afraid of falling) presented at follow‐up. Measured at baseline, post intervention and at 4‐month follow‐up | |
| Notes | We used falls defined using the FICSIT definition in the meta‐analysis. A subset of participants (n = 72) who "tended to be reclusive" were reported on in Wolf 1997. Adherence: over 90% adhered to the exercise programme | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Individuals were assigned to an intervention using a computer‐generated, fixed randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | No information provided on allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Number of falls and fear of falling were self reported by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data are based on ≥ 80% of participants in each group |
| Selective reporting (reporting bias) | High risk | Protocol not available. Data only presented for outcomes that differed significantly between groups post intervention or at follow‐up |
| Other bias | Unclear risk | The Tai Chi group had a higher proportion of participants in paid work than the balance training or control group, a higher proportion volunteering than the balance training group and a higher proportion with cataracts than the control group at baseline. The Tai Chi group had a lower mean BMI than the balance training or control group at baseline |
| Methods | RCT | |
| Participants | Country: The Netherlands n = 94 73% female Mean age in years (SD) = 84 (5.6) Study population: recruited from 3 residential care facilities and by advertisements in newspapers Inclusion criteria: older adults aged 75 years and older, living independently or in a residential care facility Exclusion criteria: recovering from an acute illness, received physical therapy during the previous month, a Mini‐Mental State Examination score < 17, Berg Balance Scale (BBS) score < 52 and impaired balance during functional activities (as determined by a physiotherapist) | |
| Interventions | 1. Balance training group (n = 47). Participants received 12 sessions of 30‐minute balance training provided by physical and recreational therapists 2 to 3 times per week during a 4‐ to 6‐week period at home or at a physical therapy department. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control group (n = 47). Offered individual‐orientated activities including handicraft, music, media, board games, discussion groups, memory training and car tours | |
| Outcomes | Fear of falling (visual analogue scale (VAS)); anxiety and depression (Hospital Anxiety and Depression Scale (HADS)). Measured at baseline, post intervention and 1 month follow‐up | |
| Notes | Adherence rates not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Subjects were randomly assigned to the 2 treatments using sealed envelopes selected by a blindfolded person. No information provided on how randomisation sequence generated |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes selected by a blindfolded person. Unclear if envelopes were sequentially numbered |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | VAS and HADS were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | High risk | Outcome data are based on > 80% of participants in the control group, but < 80% in the intervention group |
| Selective reporting (reporting bias) | High risk | Means and SDs not presented for HADS. Protocol not available |
| Other bias | Unclear risk | Control group had slightly higher HADS depression scores at baseline than the intervention group |
| Methods | RCT | |
| Participants | Country: Australia n = 165 44% female Mean age in years (SD) = 81 (6.2) Study population: recruited from advertisements in newspapers, newsletters and presentations to community groups Inclusion criteria: community‐dwelling older adults aged 65 years and older, community ambulant, requiring no walking aid, no more than 1 fall in the previous 12 months, having concerns about balance and a mild balance dysfunction Exclusion criteria: participants were excluded if balance performance was within normal limits | |
| Interventions | 1. Home‐based exercise programme (n = 82). Participants received a 6‐month physical therapist prescribed balance and strength home exercise programme based on the Otago Exercise Program and the Visual Health Information Balance and Vestibular Exercise Kit. The programme consisted of a warm‐up, balance and strength exercises with a tailored walking programme. All exercises were performed without upper limb support and with ankle weights if able. Participants were instructed to perform exercises taking approximately 20 minutes 5 times per week and a graduated walking programme aiming for at least 30 minutes per day. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control (n = 83). No intervention | |
| Outcomes | Number of falls (self reported); falls efficacy (MFES); Human Activity Profile ‐ Adjusted Activity Score (HAP‐AAS). Measured at baseline and post intervention | |
| Notes | Adherence: 44.1% reported full adherence | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Group allocation schedule was developed by computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Group allocation was performed by a researcher who was not involved in recruiting or assessing participants. No further information on allocation concealment provided |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Number of falls, MFES and HAP‐AAS were self reported by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | High risk | Outcome data are based on < 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Groups appeared well balanced at baseline. Those who withdrew from the trial had significantly worse scores on the step test and limit of stability maximum excursion test than those who completed the trial |
| Methods | RCT | |
| Participants | Country: South Korea n = 21 100% female Mean age in years (SD) = 71 (2.7) Study population: community volunteers. No further information provided Inclusion criteria: community‐dwelling older women aged 65 years and older capable of participating in moderate intensity aerobic and resistance exercises, with no more than 1 risk factor for cardiovascular disease Exclusion criteria: difficulty with activities of daily living (ADL), uncontrolled hypertension, a history of metabolic disorders, irregular menstrual cycles or amenorrhoea, hip or vertebral fracture and currently taking hormones or hormonal medication | |
| Interventions | 1. Exercise group (n = 11). Participants were involved in a 12‐week supervised walking exercise programme 3 times a week wearing ankle weights (1 kg each) in an outdoor field in a local elementary school. The programme included a 10‐minute warm‐up without ankle weights, 45 minutes of walking with ankle weights, and a 5‐minute cool down without ankle weights. Exercise intensity was maintained at 60% of heart rate reserve (HRR) determined by a heart rate monitor. ProFaNE taxonomy classification: strength/resistance 2. Control group (n = 10). No intervention | |
| Outcomes | Falls efficacy (K‐FES), Tideiksaar (1997) Fear of Falling questionnaire Yale Physical Activity score (YPAS). Measured at baseline and post intervention | |
| Notes | Adherence rates not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned, but no information provided about randomisation sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Tideiksaar Fear of Falling questionnaire and K‐FES were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | High risk | Outcome data are based on < 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Low risk | Appears to be free of other sources of bias |
| Methods | RCT | |
| Participants | Country: China n = 49 47% female Mean age in years (SD) = 70 (4.3) Study population: selected from a previous study investigating falls among community‐dwelling older adults Inclusion criteria: community‐dwelling older adults aged 60 and older who had a lower ability for maintaining balance (defined as a 1‐leg stand time between 5 and 20 seconds) and able to walk around independently Exclusion criteria: participants were excluded if they had a 1‐leg stance time of less than 5 seconds and were considered at risk to practice Tai Chi Chuan | |
| Interventions | 1. Tai Chi Chuan (TC) group (n = 25). Participants attended 1‐hour group classes 7 times a week for 8 weeks and were instructed to perform 24 simplified forms of TC. Exercises were performed in a park and taught by experienced TC instructors. If participants could not attend the class, they were asked to complete a home TC programme consisting of 11 easy forms of TC taking approximately 30 minutes to complete. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 2. Control group (n = 24). No intervention | |
| Outcomes | Falls efficacy (FES ‐ translated into Chinese). Measured at baseline and post intervention | |
| Notes | Adherence: over 90% adhered to the exercise programme | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Prior to randomisation, the 49 participants were divided into 25 pairs according to sex, experience of falling and exercise habits. Not all pairs were matched for sex or exercise habits. Pairs were then randomly assigned to either the intervention or control group by a coin toss |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | FES was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Participants were selected from a previous study by the authors (Zhang et al 2003) |
ABC: Activities‐specific Balance Confidence scale
BBS: Berg Balance Scale
BMI: body mass index
FES: Falls Efficacy Scale
FES‐I: FES‐International
FICSIT: 'Frailty and Injuries: Cooperative Studies of Intervention Techniques' study
GDS: Geriatric Depression Scale
GDS‐20: Geriatric Depression Scale‐20
HADS: Hospital Anxiety and Depression Scale
HAP‐AAS: Human Activity Profile ‐ Adjusted Activity Score
K‐FES: Korean version of the FES
LiFE: Lifestyle approach to reducing Falls through Exercise
MFES: Modified Falls‐Efficacy Scale
PASE: Physical Activity Scale for the Elderly
RCT: randomised controlled trial
SD: standard deviation
TUG: Timed Up and Go
VAS: visual analogue scale
XMSS: Xavix Measured Step System
YPAS: Yale Physical Activity Survey
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not a RCT or quasi‐RCT | |
| Multi‐component intervention. Participants received strength and balance exercises plus 6 home safety education sessions. Comparator group invited to attend exercise programme for 6 classes | |
| Not a RCT or quasi‐RCT | |
| Multi‐component intervention. Participants received exercise and mental practice of motor imagery. Comparator group were provided with exercise | |
| Comparator group were assigned to a walking programme | |
| Multi‐component intervention. Participants were allocated to a multidimensional training programme and behaviour counselling | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Fear of falling not measured | |
| Community‐dwelling people and nursing home residents. Data not presented separately for community participants | |
| Multi‐component intervention. Participants invited to attend a falls prevention programme involving a medical review, physiotherapy and occupational therapy treatments | |
| Not a RCT or quasi‐RCT | |
| Multi‐component intervention. The intervention group received medical assessment, physiotherapy and occupational therapy | |
| Not a RCT or quasi‐RCT | |
| Study population restricted to participants with osteopenia or osteoporosis | |
| Multi‐component intervention. Participants received training on a virtual reality system, an invitation to join an exercise programme, medication review, home visit by an occupational therapist, hearing and visual assessment, nutritional supplements and educational materials on falls prevention. Comparator group participants received the same intervention but with no training on the virtual reality system | |
| Majority of participants under 65 years old | |
| Multi‐component intervention. Exercise group referred to optometrist, podiatrist, physical therapist and occupational therapist | |
| Participants recruited from low and high‐level care nursing centres | |
| Multi‐component intervention. Physical and psychological interventions provided | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Multi‐component intervention. Participants provided with physical and occupational therapy | |
| Study population restricted to participants with adult‐onset hyperkyphosis | |
| Comparator group received resistance, balance and physical fitness training | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Multi‐component intervention. Tai Chi with cognitive behavioural strategies | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Comparator group received strength and balance exercises | |
| Comparator group received strength and balance exercises | |
| Nursing home residents | |
| Multi‐component intervention. Intervention group received general guidance for physical activity, guidance for adequate nutrition, individually tailored or group training of strength and balance, treatment of illnesses increasing the risk of falling, review of medications, home hazard assessment and modification | |
| Multi‐component intervention. Intervention group received strength and balance training, community falls prevention rehabilitation and medical and social care | |
| Multi‐component intervention. Intervention group received exercise training in combination with cognitive training. Comparator group received exercise training | |
| No exercise intervention reported. Health coaching programme using face to face and telephone coaching sessions | |
| Fear of falling not measured | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Comparator group received a wellness programme of low‐intensity walking and strength and balance exercises. Fear of falling not measured | |
| Multi‐component intervention. Intervention group received exercises on a Green Prescription and motivational interviewing techniques from exercise specialists. Fear of falling not measured | |
| Intervention did not include exercise | |
| Study population restricted to community‐dwelling women aged 70 or older with multiple symptoms of geriatric syndrome (MSGS) including functional decline, urinary incontinence and fear of falling | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Multi‐component intervention. All participants given home safety and modification advice in addition to their exercise. Comparator group provided with a gym‐based rehabilitation programme and home exercise | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Comparator group were provided with 4 1‐hour presentations on osteoporosis and exercise in older adults, including discussion and handouts over a 10‐week period | |
| Comparator group were provided with a stretching exercise programme for 1 hour, 3 times a week, for 26 weeks | |
| Intervention did not include exercise | |
| Not a RCT or quasi‐RCT | |
| Comparator group provided with seated exercises | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Fear of falling not measured | |
| Multi‐component interventions. The extensive intervention group received group exercises and strategies for maximising vision and sensation. The minimal intervention group received home exercise sheets and written advice about how to maximise their vision and take precautions for loss of peripheral sensation | |
| Study population restricted to participants with ≥ 1 risk factor for falling (≥ 2 falls in previous year, loneliness, poor self rated health, poor visual acuity, poor hearing, depression, poor cognition, impaired balance, impaired chair rise and slow walking speed) | |
| Not a RCT or quasi‐RCT | |
| Multi‐component intervention. Intervention group provided with exercise, falls risk assessment and medication review | |
| Not a RCT or quasi‐RCT | |
| Fear of falling not measured | |
| Comparator group provided with walking exercises for 2 hours, 2 times per week, for 10 weeks | |
| Multi‐component intervention. Intervention group exercised and took calcium supplements | |
| Comparator group provided with strength training exercises 3 times a week for 18 months | |
| Not a RCT or quasi‐RCT | |
| Fear of falling not measured | |
| Not a RCT or quasi‐RCT | |
| Fear of falling not measured | |
| Multi‐component intervention. Intervention group received a comprehensive health assessment combined with tailored risk reduction strategies such as strength and balance exercises | |
| Multi‐component intervention. Intervention participants received a "customised multifactorial falls prevention program" | |
| Multi‐component intervention. Strength and balance training, plus falls risk factor assessment followed by a comprehensive geriatric assessment and treatment | |
| Multi‐component intervention. Intervention included fall prevention programme with alfacalcidol and calcium, patient education and a mobility programme | |
| Comparator group participated in a walking programme | |
| Multi‐component intervention. Participants received exercise and vitamin D supplementation | |
| Comparator group received a standard programme of physical therapy for gait and balance | |
| Comparator group performed strength and balance exercises 3 times a week for 12 weeks | |
| Comparator group received wellness education, which consisted of supervised group training done once a week with the focus on stretching and flexibility exercises | |
| Comparator group received balance training strategies | |
| Comparator group provided with treadmill exercises. Fear of falling not measured | |
| Multi‐component intervention. Before randomisation, all participants attended 3 educational classes that discussed falling, osteoporosis and bone fracture. Comparator group were provided with daily stretch exercises | |
| Fear of falling not measured | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Multi‐component intervention. Participants provided with exercise and protein‐enriched energy supplement | |
| Comparator group performed low‐intensity knee extension exercises daily for 6 weeks | |
| Fear of falling not measured | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Multi‐component intervention. Participants provided with home exercises and a 32‐page booklet about fall prevention. The booklet contained information about risk factors for falls, environmental modification for falls risk reduction and what to do after a fall | |
| Comparator group provided with strength and balance training | |
| Not a RCT or quasi‐RCT | |
| Comparator group provided with balance training exercises | |
| Fear of falling not measured | |
| Majority of participants under 65 years old | |
| Comparator group provided with resistance exercises 3 days a week for 12 weeks | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Multi‐component intervention. Intervention group received balance retraining exercises and efficacy training (including discussion of group fears, introduction to home safety and an opportunity to practise any skill that is difficult or avoided secondary to fear). Comparator group provided with balance retraining exercises | |
| Not a RCT or quasi‐RCT | |
| Fear of falling not measured | |
| Not a RCT or quasi‐RCT | |
| Comparator group provided with strength and balance exercises, assessment of walking aids, a gait re‐education programme and an unsupervised walking programme | |
| Not a RCT or quasi‐RCT | |
| Nursing home residents | |
| Not a RCT or quasi‐RCT | |
| Multi‐component intervention. Participants received group discussions focused on self efficacy, cognitive restructuring and exercise | |
| Comparator group provided with strength and walking exercises | |
| Multi‐component intervention. Care home staff received depression awareness and physical activity training. Intervention participants received a twice weekly exercise group | |
| Not a RCT or quasi‐RCT | |
| Multi‐component intervention. Participants received personalised exercises and medical treatment | |
| Fear of falling not measured | |
| Multi‐component intervention. Intervention participants received a 16‐week balance and mobility exercise group with a self efficacy intervention. Comparator group provided with balance and mobility exercises | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Fear of falling not measured | |
| Majority of participants under 65 years old | |
| Comparator group provided with Tai Chi exercises | |
| Not a RCT or quasi‐RCT | |
| Comparator group provided with strength and balance training exercises each week | |
| Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT |
RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | RCT |
| Participants | Country: Japan n = 171 % female not reported Mean age in years (SD) = 74.1 (not reported) Study population: recruited via advertisements in publications and clubs for the elderly Inclusion criteria: community‐dwelling, aged ≥ 65, ambulatory with or without assisting devices Exclusion criteria: cerebrovascular or cardiovascular accidents reported within the past 6 months, acute liver problems or the active phase of chronic hepatitis, diabetes mellitus with a history of hypoglycaemic attack, or with fasting levels of plasma glucose concentrations of 200 mg/dl or higher, or with complications such as retinopathy or nephropathy, systolic blood pressure above 180 mm Hg or diastolic blood pressure above 110 mm Hg at rest, diagnosis of severe heart disease or an acute orthopaedic problem, diagnosis of dementia or depression made by a medical doctor, or an inability to understand and follow the instructions of the research staff; restriction of physical activities by a medical doctor |
| Interventions | 1. Exercise group (n = 86). Group‐based resistance and balance training for 1.5 hours, twice weekly, for 3 months 2. Control group (n = 85). Health education group for 1.5 hours, twice a month, for 3 months. Lectures included "Knowledge of Resistance Training" |
| Outcomes | Falls efficacy (FES ‐ translated into Japanese, with the degree of confidence in accomplishing tasks based on a scale of 1 to 4 rather than 1 to 10). Measured at baseline and post intervention |
| Notes | — |
| Methods | RCT |
| Participants | Country: Canada n = 38 74% female Mean age in years (SD) = 77.1 (5.1) for exercise group, 78.0 (5.5) for control Study population: recruited through newspaper and radio advertisements seeking individuals fearful of falling Inclusion criteria: seniors living independently with a lasting concern about falling causing them to avoid or curtail activities they felt they were capable of doing Exclusion criteria: coexisting conditions affecting balance (e.g. neuropathy, vestibular deficits, mobility limiting arthritis, pre‐existing neurological conditions), not being able to commit to an 8‐week intervention |
| Interventions | 1. Exercise group (n = 17). Group‐based low‐resistance exercises and weight shifting activities, and a 40‐minute, twice weekly home programme of exercises and stretches 2. Control group (n = 17). Group‐based education programme focused on identifying and reducing risk factors for falls. Topics included "the importance of good nutrition and activity" Both groups were delivered by a physiotherapist for 1 hour, weekly, for 8 weeks |
| Outcomes | Balance confidence (ABC). Measured at baseline, post intervention and 6 weeks follow‐up. Adherence to exercise intervention measured by class attendance and participant log books |
| Notes | 38 participants randomised but 4 withdrew during study. Number of participants randomised to each group before the withdrawals not reported |
| Methods | RCT |
| Participants | Country: Australia n = 67 54% female Mean age in years (SD) = 71.2 (1.3) for high‐velocity training group, 69.6 (1.1) for strength training group, 69.3 (1.0) for control Study population: recruited by newspaper advertisement Inclusion criteria: independently living, community‐dwelling, aged 65 to 84 Exclusion criteria: acute or terminal illness, unstable or ongoing cardiovascular and/or respiratory disorder, neurological or musculoskeletal disease or impairment, resistance training experience within the previous 12 months, the inability to commit to a period of time equivalent to the duration of the study |
| Interventions | 1. High‐velocity training group (n = 23). High‐velocity varied resistance exercises 2. Strength training group (n = 22). Constant resistance exercises 3. Control group (n = 22). Non‐training group Participants in the exercise interventions trained twice weekly for 24 weeks |
| Outcomes | Balance confidence (ABC); physical activity (PASE). Measured at baseline and post intervention |
| Notes | All participants were invited to attend 2 familiarisation sessions, during which exercise techniques were demonstrated and practised, before baseline assessments and randomisation |
| Methods | RCT |
| Participants | Country: Denmark n = 58 69% female Mean age in years (SD) = 75 (6) Study population: recruited through advertisements in local newspapers, senior citizens' clubs, and senior society organisations Inclusion criteria: ≥ 65, self reported balance poor to average (on a discrete scale: good, average, poor), capability of understanding verbal instructions Exclusion criteria: orthopaedic surgery within the previous 6 months, acute illness within the previous 3 weeks, physiotherapy within the previous month, poor visual acuity (not capable of seeing the visual features on the TV screen) |
| Interventions | 1. Exercise group (n = 28). Biofeedback‐based Nintendo Wii training for 35 (SD 5) minutes, twice weekly, for 10 weeks 2. Control group (n = 30). Daily use of ethylene vinyl acetate copolymer shoe insoles for 10 weeks. Participants were explicitly informed that the use of insoles was expected to increase sensory inputs from the feet to the central nervous system, resulting in an improved postural balance |
| Outcomes | Concern about falling (short FES‐I). Measured at baseline and post intervention |
| Notes | Study record reported at ‐ NCT01371253. 10 weeks of Nintendo Wii Fit balance training improved postural balance and muscle strength in elderly individuals. http://clinicaltrials.gov/show/NCT01371253 (accessed 1 August 2013) |
| Methods | RCT |
| Participants | Country: USA n = 24 92% female Mean age in years (SD) = 72.5 (6.8) in balance training group, 72.0 (5.5) in weight training group, 76.5 (8.3) in control Study population: recruited from the local community via advertisements Inclusion criteria: older adults, no history of the formal weight and balance exercises in the past 6 months, current exercises (such as walking, running, swimming, dancing, gardening, tennis and golf) do not particularly target weight lifting and balance control, current exercises that target improved muscle strength and balance do not exceed more than 30 minutes a week in total Exclusion criteria: physical problems (i.e. hip, knee, ankle problems) |
| Interventions | 1. Balance training group (n = 6) 2. Weight training group (n = 6) 3. Control group (n = 6). Social activities (picnics, bingo, shopping and park visits). Activities that required physical performance were not included in the control group activities, except for walking The groups met for 50 to 60 minutes, 3 times weekly, for 8 weeks |
| Outcomes | Fear of falling (on a scale from 1 to 10 (10 being high)). Measured at baseline and post intervention |
| Notes | 24 participants randomised, but 5 withdrew and 1 participant's data were eliminated because his physical abilities were exceptionally superior to the other participants' physical abilities. Number of participants randomised to each group before the withdrawals and data elimination not reported |
| Methods | RCT |
| Participants | Country: USA n = 26 100% female Mean age in years (SD) = 76.1 (6.4) Study population: recruited from among the current users of any of the activities sponsored by a hospital supported senior wellness programme Inclusion criteria: willingness to participate after full understanding of the elements and risks involved, completion of a health history form and a signed informed consent form Exclusion criteria: advanced osteoporosis, hip replacement, glaucoma, Parkinson's disease, common occurrences of dizziness, any surgery within the past year |
| Interventions | 1. Group‐based yoga exercises (n = 10) 2. Group‐based balance training exercises (n = 10) 3. Control group (n = 6). Fall risk awareness group. Topics included "exercise" and "walking/healthy feet" All groups met for 1 hour, twice weekly, for 8 weeks |
| Outcomes | Falls efficacy (FES); balance confidence (ABC). Measured at baseline, every other week, post intervention and at 1 month follow‐up. Adherence to exercise interventions measured by class attendance |
| Notes | — |
| Methods | RCT |
| Participants | Country: USA n = 311 94% female Mean age in years (SD) = 80.9 (6.6) for Tai Chi group, 80.8 (5.8) for wellness education group Study population: recruited from congregate living facilities Inclusion criteria: ≥ 70, transitioning to frailty, fallen at least once in the past year Exclusion criteria: major unstable cardiopulmonary diseases (ischaemic chest pain, unaccustomed shortness of breath, shortness of breath with mild exertion, recurrent syncopal episodes, orthopnoea, paroxysmal nocturnal dyspnoea, palpitations, tachycardia, claudication or severe pitting ankle oedema), cognitive impairment defined as a Mini‐Mental State Examination (MMSE) score of less than 24, contraindications to physical exercise, such as major orthopaedic conditions (e.g. severe lumbar spine, hip, knee, or ankle arthritis that limits exercise capability), restricted to a wheelchair; terminal cancer; or evidence of any other progressive or unstable neurological or medical condition |
| Interventions | 1. Exercise group (n = 158). Group‐based Tai Chi, for 60 to 90 minutes, twice weekly, for 48 weeks 2. Control group (n = 153). Wellness education programme for 1 hour, weekly, for 48 weeks. Topics included "exercise and balance" |
| Outcomes | Falls efficacy (FES); balance confidence (ABC); depression (CES‐D). Measured at baseline and every 4 months for 12 months during a 48‐week intervention. Number of falls (recorded by weekly forms). Adherence to exercise intervention measured by class attendance |
| Notes | Fear of falling sub‐study reported at ‐ Sattin R, Easley K, Wolf S, Chen Y, Kutner M. Reduction in fear of falling through intense tai chi exercise training in older, transitionally frail adults. Journal of American Geriatrics Society 2005;53:1168‐78 |
ABC: Activities‐specific Balance Confidence scale
CES‐D: Center for Epidemiologic Studies ‐ Depression scale
FES: Falls Efficacy Scale
FES‐I: FES‐International
RCT: randomised controlled trial
SD: standard deviation
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Multicentre cluster‐randomised trial comparing a community group exercise programme with home based exercise with usual care for over 65s in primary care |
| Methods | Cluster‐RCT |
| Participants | N = 1200 Setting: UK Inclusion criteria: community‐dwelling older adults aged 65 and over, able to walk around independently indoors and outdoors (with or without a walking aid) and not undergoing long term physiotherapy Exclusion criteria: 3 or more falls in the previous year ("frequent fallers"), resting BP > 180/100 mm Hg, uncontrolled arrhythmia, critical aortic stenosis, very severe vestibular disturbances, psychiatric conditions, significant cognitive impairment (unable to follow simple instructions), acute medical problems such as pneumonia or acute rheumatoid arthritis, hip/knee replacement in past 3 months, stroke/transient ischaemic attacks in the last 6 months or not living independently (e.g. residential or nursing care) |
| Interventions | 1. Home‐based exercise programme (n = 400). Otago Exercise Programme (OEP) consists of 30‐minute leg muscle strengthening and balance retraining exercises progressing in difficulty performed at least 3 times per week, for 24 weeks. Participants also advised to walk at least twice per week for up to 30 minutes at a moderate pace 2. Community‐based exercise programme (FaME) (n = 400). 1‐hour group exercise class in a local community centre, and 2 30‐minute home exercise sessions (based on the OEP) per week, for 24 weeks. Participants also advised to walk at least twice per week for up to 30 minutes at a moderate pace 3. Treatment as usual (TAU). No intervention |
| Outcomes | Number and type of falls (fall diary); fear of falling (FES‐I); balance confidence (ConfBal); quality of life (Older People's QOL Questionnaire (OPQOL); SF‐12); economic analysis |
| Starting date | June 2008 |
| Contact information | Prof Steve Iliffe Department of Primary Care & Population Health University College London Rowland Hill Street London NW3 2PF United Kingdom |
| Notes | Recruitment completed. Study end date May 2013 |
| Trial name or title | Prevention of falls in community‐dwelling older adults by a standardized assessment of fall risks in the general practitioner setting and through implementation of a network for effective individual reduction on fall risks |
| Methods | RCT |
| Participants | N = 378 Setting: Germany Inclusion criteria: community‐dwelling adults aged 65 years and older with an increased risk of falling, as seen by history of falls, fear of falling, chair rise > 10 seconds, TUG > 10 seconds and subjective and objective balance deficits Exclusion criteria: older people not living independently, or suffering from physical or mental restrictions that do not allow the participation in an exercise programme or the assessment of risk of falling |
| Interventions | 1. Exercise group. 16‐week exercise programme performed once a week for 60 minutes. Exercises include strength/power training, balance/gait training, behavioural aspects, perceptual and functional training 2. Control group. No intervention |
| Outcomes | Number of falls and falls rates (fall diary); fear of falling (FES‐I); quality of life (EuroQol) |
| Starting date | April 2009 |
| Contact information | Dr Monika Siegrist Department of Medicine Division of Prevention and Sports Medicine Technische Universität Munich 80809 Germany |
| Notes | Study has been completed March 2012. Data expected to be published spring or summer 2013 (as per email from Chief Investigator received January 2013) |
BP: blood pressure
RCT: randomised controlled trial
TUG: Timed Up and Go
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Fear of falling as measured by single‐item question, falls efficacy, balance confidence and concern about falling, post intervention Show forest plot | 24 | 1692 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| Analysis 1.1  Comparison 1 Exercise versus control: primary outcome ‐ fear of falling, post intervention, Outcome 1 Fear of falling as measured by single‐item question, falls efficacy, balance confidence and concern about falling, post intervention. | ||||
| 1.1 Fear of falling as measured by single‐item question | 4 | 380 | Std. Mean Difference (Random, 95% CI) | 0.17 [‐0.06, 0.39] |
| 1.2 Falls efficacy measured using the FES, MFES or K‐FES | 12 | 872 | Std. Mean Difference (Random, 95% CI) | 0.56 [0.21, 0.90] |
| 1.3 Balance confidence measured using ABC | 6 | 333 | Std. Mean Difference (Random, 95% CI) | 0.13 [‐0.10, 0.37] |
| 1.4 Concern about falling measured using the FES‐I and Short FES‐I | 2 | 107 | Std. Mean Difference (Random, 95% CI) | 0.52 [‐0.09, 1.12] |
| 2 Fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, short term follow‐up (< 6 months) Show forest plot | 4 | 356 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.17 [‐0.05, 0.38] |
| Analysis 1.2  Comparison 1 Exercise versus control: primary outcome ‐ fear of falling, post intervention, Outcome 2 Fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, short term follow‐up (< 6 months). | ||||
| 3 Fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, long term follow‐up (6 months and more) Show forest plot | 3 | 386 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.01, 0.41] |
| Analysis 1.3 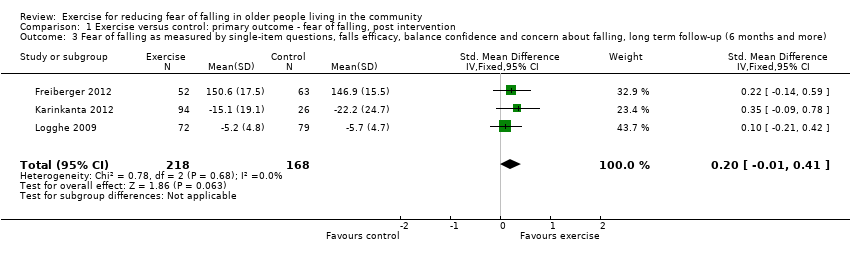 Comparison 1 Exercise versus control: primary outcome ‐ fear of falling, post intervention, Outcome 3 Fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, long term follow‐up (6 months and more). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Type of exercise (as classified using ProFaNE taxonomy) Show forest plot | 22 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| Analysis 2.1  Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 1 Type of exercise (as classified using ProFaNE taxonomy). | ||||
| 1.1 3D (Tai Chi) | 7 | 483 | Std. Mean Difference (Random, 95% CI) | 0.60 [0.09, 1.12] |
| 1.2 Strength/resistance | 4 | 416 | Std. Mean Difference (Random, 95% CI) | 0.08 [‐0.18, 0.34] |
| 1.3 Gait, balance, co‐ordination, functional tasks | 11 | 619 | Std. Mean Difference (Random, 95% CI) | 0.27 [0.05, 0.50] |
| 2 Type of control group Show forest plot | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| Analysis 2.2  Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 2 Type of control group. | ||||
| 2.1 Alternative intervention (e.g. social group, education, etc) | 6 | 499 | Std. Mean Difference (Random, 95% CI) | 0.11 [‐0.08, 0.29] |
| 2.2 No intervention | 18 | 1199 | Std. Mean Difference (Random, 95% CI) | 0.48 [0.22, 0.73] |
| 3 Recruited participants at increased risk of falls Show forest plot | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| Analysis 2.3  Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 3 Recruited participants at increased risk of falls. | ||||
| 3.1 Studies not recruiting participants on the basis of increased risk of falls | 14 | 926 | Std. Mean Difference (Random, 95% CI) | 0.44 [0.14, 0.74] |
| 3.2 Studies recruiting participants at increased risk of falls | 10 | 772 | Std. Mean Difference (Random, 95% CI) | 0.24 [0.04, 0.45] |
| 4 Type of exercise (individual versus group) Show forest plot | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| Analysis 2.4 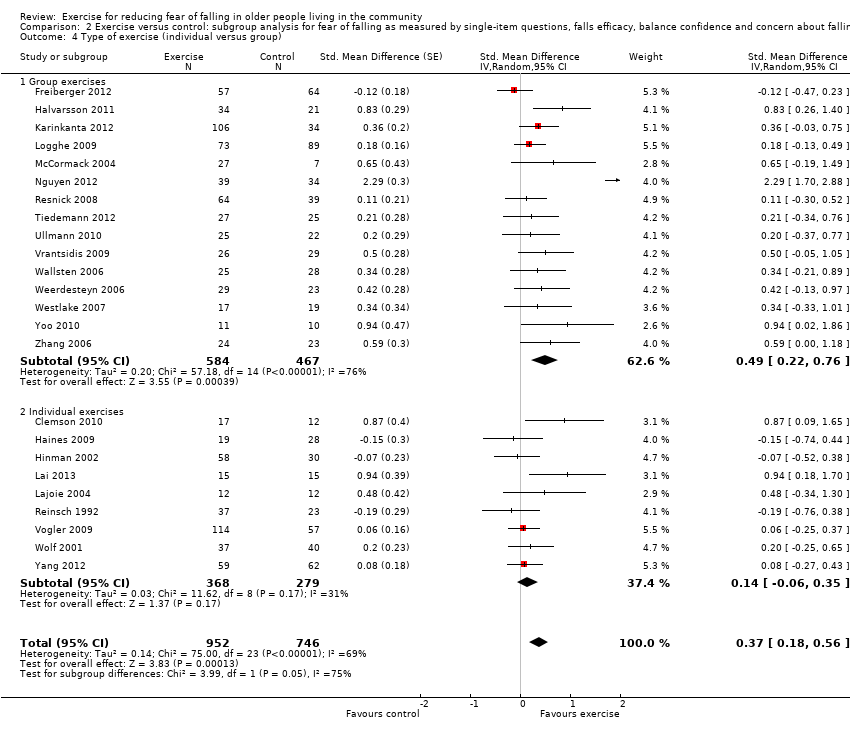 Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 4 Type of exercise (individual versus group). | ||||
| 4.1 Group exercises | 15 | 1051 | Std. Mean Difference (Random, 95% CI) | 0.49 [0.22, 0.76] |
| 4.2 Individual exercises | 9 | 647 | Std. Mean Difference (Random, 95% CI) | 0.14 [‐0.06, 0.35] |
| 5 Frequency of exercise Show forest plot | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| Analysis 2.5  Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 5 Frequency of exercise. | ||||
| 5.1 1 to 3 times per week | 20 | 1339 | Std. Mean Difference (Random, 95% CI) | 0.38 [0.15, 0.61] |
| 5.2 4 or more times per week | 4 | 359 | Std. Mean Difference (Random, 95% CI) | 0.30 [0.01, 0.58] |
| 6 Duration of exercise Show forest plot | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| Analysis 2.6  Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 6 Duration of exercise. | ||||
| 6.1 Up to 12 weeks | 17 | 968 | Std. Mean Difference (Random, 95% CI) | 0.32 [0.16, 0.48] |
| 6.2 13 to 26 weeks | 5 | 530 | Std. Mean Difference (Random, 95% CI) | 0.52 [‐0.13, 1.17] |
| 6.3 More than 26 weeks | 2 | 200 | Std. Mean Difference (Random, 95% CI) | 0.13 [‐0.41, 0.66] |
| 7 Primary aim of the study Show forest plot | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| Analysis 2.7  Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 7 Primary aim of the study. | ||||
| 7.1 To reduce fear of falling | 7 | 471 | Std. Mean Difference (Random, 95% CI) | 0.42 [0.13, 0.72] |
| 7.2 Other primary aim (e.g. balance improvement, fall prevention, etc) | 17 | 1227 | Std. Mean Difference (Random, 95% CI) | 0.34 [0.10, 0.59] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Occurrence of at least one fall Show forest plot | 9 | 1113 | Risk Ratio (IV, Fixed, 95% CI) | 0.85 [0.74, 0.98] |
| Analysis 3.1 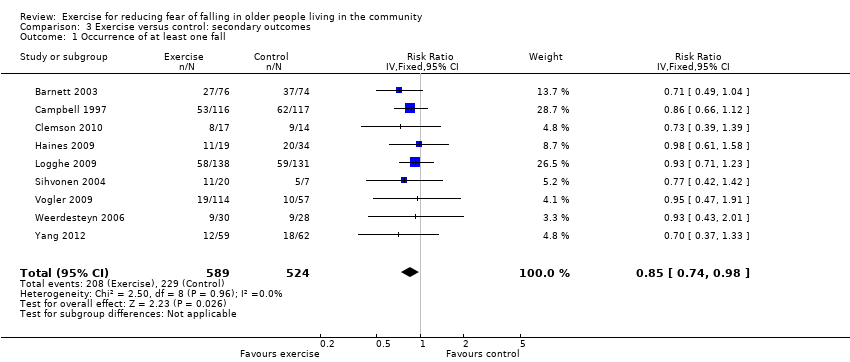 Comparison 3 Exercise versus control: secondary outcomes, Outcome 1 Occurrence of at least one fall. | ||||
| 2 Falls rate Show forest plot | 9 | 1121 | Rate Ratio (Random, 95% CI) | 0.68 [0.53, 0.87] |
| Analysis 3.2  Comparison 3 Exercise versus control: secondary outcomes, Outcome 2 Falls rate. | ||||
| 3 Depression score, post intervention Show forest plot | 4 | 406 | Std. Mean Difference (Fixed, 95% CI) | ‐0.08 [‐0.28, 0.13] |
| Analysis 3.3  Comparison 3 Exercise versus control: secondary outcomes, Outcome 3 Depression score, post intervention. | ||||
| 4 Depression score, short‐term follow‐up (< 6 months) Show forest plot | 3 | 327 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.02, 0.43] |
| Analysis 3.4  Comparison 3 Exercise versus control: secondary outcomes, Outcome 4 Depression score, short‐term follow‐up (< 6 months). | ||||
| 5 Physical activity as measured using PASE (Physical Activity Scale for the Elderly) Show forest plot | 4 | 547 | Mean Difference (IV, Fixed, 95% CI) | 3.44 [‐1.65, 8.54] |
| Analysis 3.5  Comparison 3 Exercise versus control: secondary outcomes, Outcome 5 Physical activity as measured using PASE (Physical Activity Scale for the Elderly). | ||||

'Risk of bias' summary: authors' judgements about each risk of bias item for each included study

'Risk of bias' graph: authors' judgements about each risk of bias item presented as percentages across all included studies

Forest plot: Exercise versus control: primary outcome ‐ fear of falling, post intervention

Exercise versus control: primary outcome ‐ fear of falling, post intervention (see Figure 4 for forest plot)

Comparison 1 Exercise versus control: primary outcome ‐ fear of falling, post intervention, Outcome 1 Fear of falling as measured by single‐item question, falls efficacy, balance confidence and concern about falling, post intervention.

Comparison 1 Exercise versus control: primary outcome ‐ fear of falling, post intervention, Outcome 2 Fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, short term follow‐up (< 6 months).
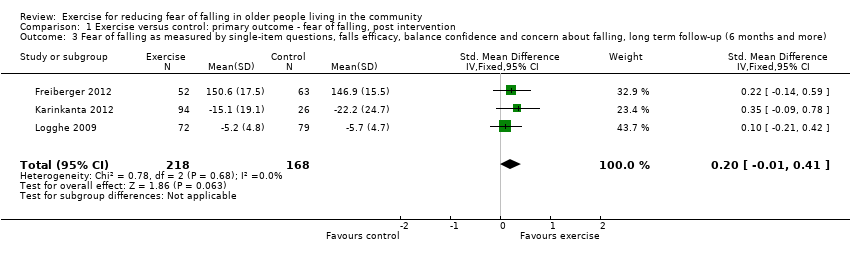
Comparison 1 Exercise versus control: primary outcome ‐ fear of falling, post intervention, Outcome 3 Fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, long term follow‐up (6 months and more).

Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 1 Type of exercise (as classified using ProFaNE taxonomy).

Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 2 Type of control group.

Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 3 Recruited participants at increased risk of falls.
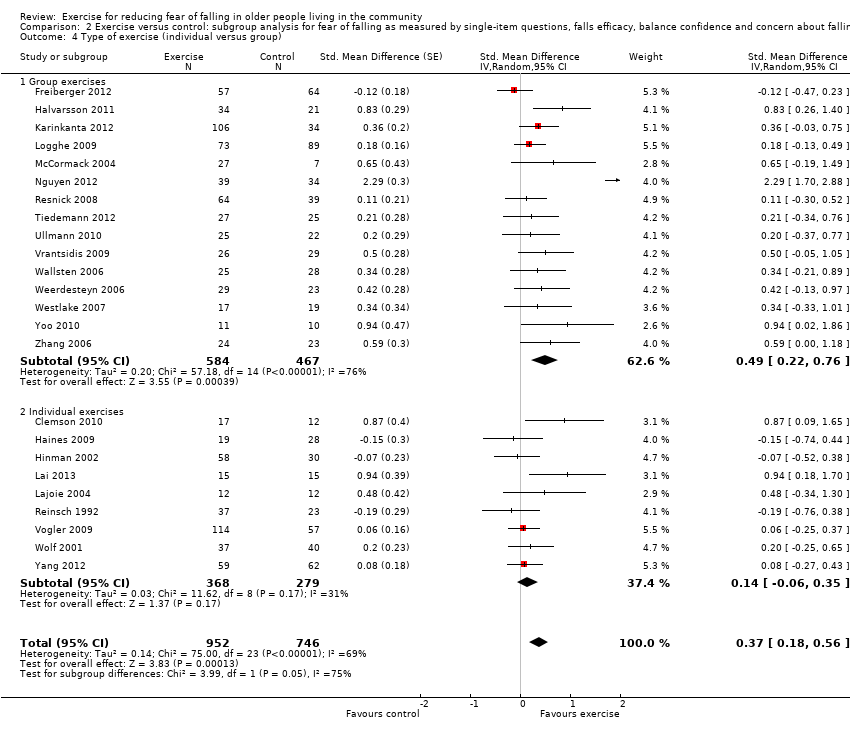
Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 4 Type of exercise (individual versus group).

Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 5 Frequency of exercise.

Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 6 Duration of exercise.

Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 7 Primary aim of the study.
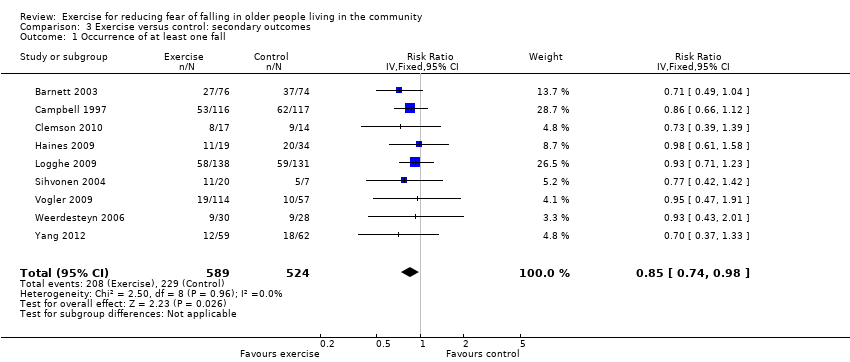
Comparison 3 Exercise versus control: secondary outcomes, Outcome 1 Occurrence of at least one fall.

Comparison 3 Exercise versus control: secondary outcomes, Outcome 2 Falls rate.

Comparison 3 Exercise versus control: secondary outcomes, Outcome 3 Depression score, post intervention.

Comparison 3 Exercise versus control: secondary outcomes, Outcome 4 Depression score, short‐term follow‐up (< 6 months).

Comparison 3 Exercise versus control: secondary outcomes, Outcome 5 Physical activity as measured using PASE (Physical Activity Scale for the Elderly).
| Exercise for reducing fear of falling in older people living in the community | ||||||
| Population: older people living in the community Control: no intervention or alternative non‐exercise intervention2 | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Exercise | |||||
| Fear of falling3 Immediately post intervention | The mean fear of falling score4 in the intervention | SMD 0.37 (0.18 to 0.56) | 1692 (24 studies) | ⊕⊕⊝⊝ | 0.2 SD represents a small difference, 0.5 SD a moderate difference and 0.8 SD a large difference We are unaware of any definitions of minimal clinically important difference for any fear of falling measure1 There was significant heterogeneity of effect sizes, which was attributable mainly to 1 study, Nguyen 2012, having a much larger effect size than other studies. Upon removal of this study, the effect size reduced to SMD 0.24, 95% CI 0.12 to 0.36; 23 studies; 1619 participants None of the subgroup analyses6 provided robust evidence of a difference in effect between different subgroups. The possible exception was evidence of a smaller effect, which included no reduction, of exercise when compared with an alternative control2 | |
| Fear of falling < 6 months follow‐up | The mean fear of falling score in the intervention | SMD 0.17 (‐0.05 to 0.38) | 356 (4 studies) | ⊕⊝⊝⊝ | Very low quality evidence7 was also available from 3 studies (386 participants) at long‐term follow‐up (6 or more months post end of the intervention period): SMD 0.20, 95% CI ‐0.01 to 0.41 | |
| Occurrence of at least 1 fall Follow‐up: 2 to 12 months | 500/10008 | 425/1000 (370 to 490) | RR 0.85 | 1113 | ⊕⊝⊝⊝ | Some studies measured falls using prospective falls diaries, some measured falls retrospectively and in some studies it was unclear whether falls were measured prospectively or retrospectively Note: Studies included in the analysis represent only a subset of studies evaluating the effect of exercise interventions on falls risk Very low quality evidence9 suggests exercise interventions were associated with a significant reduction in the rate of falls (rate ratio 0.68, 95% CI 0.53 to 0.87; 9 studies; 1121 participants) |
| Depressive symptoms10 | The mean depression score in the intervention | SMD ‐0.08 (‐0.28 to 0.13) | 406 | ⊕⊝⊝⊝ | 0.2 SD represents a small difference, 0.5 a moderate difference and 0.8 a large difference Note: Studies included in the analysis represent only a very small subset of studies evaluating the effect of exercise interventions on symptoms of depression | |
| Anxiety | Mean HADS11 anxiety score = 4.3 (SD 3.4) | Mean HADS anxiety score = 4.3 (SD 3.9) | Difference between means = 0. No 95% CI reported | 77 participants (1 study) | ⊕⊝⊝⊝ | Anxiety was reported by the subscale of HADS, which ranged from 0 to 21 with a higher score indicating higher symptoms of anxiety Note: This study represents only a subset of studies evaluating the effect of exercise interventions on anxiety |
| Physical activity | The mean physical activity score in the intervention | MD 3.44 | 547 | ⊕⊝⊝⊝ | All studies used the Physical Activity Scale for the Elderly (PASE) scale, which ranged from 0 to 400, with a higher score indicating greater physical activity Note: Studies included in the analysis represent only a subset of studies evaluating the effect of exercise interventions on physical activity | |
| Activity avoidance or restriction | See comment | See comment | No studies reported this outcome | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1The exercises interventions in the included trials fell into three categories: 3D (Tai Chi, Yoga); gait, balance, co‐ordination, functional tasks; and strength and resistance based interventions. They were either supervised or unsupervised activities, delivered in group settings or individually; and varied in duration from up to 12 weeks to over 26 weeks. The majority of exercise interventions were to be performed between one to three times per week. FES: 10 questions rated 1 (very confident) to 10 (not confident at all). A higher score indicates a lower perceived self efficacy at avoiding falls. Single item questions: 4Pooled effect sizes did not differ significantly between the different scales used to measure fear of falling (test for subgroup differences: Chi² = 5.21, df = 3, P value = 0.16). GDS Scale: 30 questions, range 0 to 30 with higher scores indicating greater symptoms of depression. 11HADS = Hospital Anxiety and Depression Scale. | ||||||
| Study | Time point | Scale | Scale direction | Intervention group mean | Intervention group SD | Intervention group number of participants | Control group mean | Control group SD | Control group number of participants |
| Post intervention | MFES | High score = low FOF | 49.4 | 6.1 | 17 | 42.6 | 9.4 | 12 | |
| Post intervention | ABC | High score = low FOF | 995.3 | 377.9 | 17 | 805.0 | 297.1 | 12 | |
| Post intervention | ABC | High score = low FOF | 148.6 | 16.8 | 57 | 150.3 | 12.4 | 64 | |
| Post intervention | ABC | High score = low FOF | 5.3 | 2.0 | 19 | 5.6 | 2.0 | 28 | |
| Post intervention | FES‐I | High score = high FOF | ‐22.6 | 6.1 | 34 | ‐28.9 | 9.3 | 21 | |
| Post intervention | MFES | High score = low FOF | 134.6 | 10.9 | 58 | 135.4 | 14.1 | 30 | |
| Post intervention | 100 mm VAS | High score = high FOF | ‐10.7 | 15.7 | 106 | ‐16.9 | 21.2 | 34 | |
| Post intervention | MFES | High score = low FOF | 136.0 | 6.1 | 15 | 116.4 | 27.9 | 15 | |
| Post intervention | ABC | High score = low FOF | 92.0 | 8.0 | 12 | 82.5 | 26.0 | 12 | |
| Post intervention | FES | High score = high FOF | ‐4.9 | 4.4 | 73 | ‐5.8 | 5.3 | 89 | |
| Post intervention | MFES | High score = low FOF | 9.1 | 1.5 | 27 | 8.1 | 2.4 | 7 | |
| Post intervention | FES | High score = high FOF | ‐35.2 | 5.9 | 39 | ‐51.4 | 8.1 | 34 | |
| Post intervention | Participants asked to rate fear of falling on a scale of 0 to 4 (0 = low, 4 = high) | High score = high FOF | ‐1.6 | 1.8 | 64 | ‐1.8 | 1.8 | 39 | |
| Post intervention | Participants asked to rate worry about falling on a scale of 1 to 5 (1 = not at all worried, 5 = extremely worried) | High score = high FOF | ‐1.5 | 0.8 | 44 | ‐1.7 | 1.3 | 42 | |
| Post intervention | FES‐I | High score = high FOF | ‐9.8 | 4.5 | 27 | ‐10.6 | 3.2 | 25 | |
| Post intervention | FES | High score = low FOF | 9.3 | 1.4 | 19 | 9.0 | 1.7 | 22 | |
| Post intervention | ABC | High score = low FOF | 83.5 | 13.5 | 19 | 86.4 | 10.6 | 22 | |
| Post intervention | MFES | High score = low FOF | 8.6 | 1.8 | 114 | 8.5 | 1.8 | 57 | |
| Post intervention | MFES | High score = low FOF | 8.6 | 1.6 | 26 | 7.7 | 1.9 | 29 | |
| Post intervention | ABC | High score = low FOF | 76.2 | 20.3 | 25 | 70.5 | 12.3 | 28 | |
| Post intervention | ABC | High score = low FOF | 76.3 | 13.4 | 29 | 69.7 | 17.8 | 23 | |
| Post intervention | ABC | High score = low FOF | 85.7 | 9.5 | 17 | 79.1 | 24.2 | 19 | |
| Post intervention | 100 mm VAS | High score = high FOF | ‐38.6 | 29.7 | 37 | ‐44.7 | 29.9 | 40 | |
| Post intervention | MFES | High score = low FOF | 9.2 | 1.2 | 59 | 9.1 | 1.4 | 62 | |
| Post intervention | K‐FES | High score = low FOF | 100.0 | 0.0 | 11 | 95.4 | 6.8 | 10 | |
| Post intervention | FES | High score = low FOF | 78.3 | 4.0 | 24 | 75.3 | 5.9 | 23 | |
| ABC: Activities‐specific Balance Confidence scale | |||||||||
| Study | Time point | Scale | Scale direction | Intervention group mean | Intervention group SD | Intervention group number of participants | Control group mean | Control group SD | Control group number of participants |
| Post intervention | GDS‐20 | Higher score = greater symptoms of depression | 2.7 | 2.4 | 34 | 3 | 2 | 21 | |
| Post intervention | GDS 5‐item | Higher score = greater symptoms of depression | 0.41 | 0.79 | 64 | 0.79 | 1.1 | 39 | |
| Post intervention | GDS | Higher score = greater symptoms of depression | 7.2 | 4.49 | 114 | 6.4 | 4.3 | 57 | |
| Post intervention | HADS‐Depression | Higher score = greater symptoms of depression | 4.8 | 3.85 | 37 | 5.6 | 4.01 | 40 | |
| GDS: Geriatric Depression Scale | |||||||||
| Study | Exercise type classified using the ProFaNE taxonomy of interventions (ProFaNE 2011) | Control Type | Supervised activity? | Group setting? |
| Gait, balance, co‐ordination, functional tasks | Education (falls prevention) | Supervised | Group | |
| Strength/resistance | Social visits | Unsupervised | Individual | |
| Gait, balance, co‐ordination, functional tasks | No intervention | Unsupervised | Individual | |
| Strength/resistance | No intervention | Supervised | Group | |
| Gait, balance, co‐ordination, functional tasks | No intervention | Unsupervised | Individual | |
| Gait, balance, co‐ordination, functional tasks | No intervention | Supervised | Group | |
| Home exercise programme: gait, balance, co‐ordination, functional tasks | No intervention | Supervised | Individual | |
| Computerised balance training: gait, balance, co‐ordination, functional tasks | No intervention | Unsupervised | Individual | |
| Resistance training: strength/resistance | No intervention | Supervised | Group | |
| Balance jumping: gait, balance, co‐ordination, functional tasks | No intervention | Supervised | Group | |
| Combined resistance and balance jumping: gait, balance, co‐ordination, functional tasks | No intervention | Supervised | Group | |
| Gait, balance, co‐ordination, functional tasks | No intervention | Supervised | Individual | |
| Gait, balance, co‐ordination, functional tasks | No intervention | Supervised | Individual | |
| Gait, balance, co‐ordination, functional tasks | Home safety assessment | Supervised | Individual | |
| 3D (Tai Chi, Qi Gong, dance, yoga) | No intervention | Supervised | Group | |
| Holistic exercise: 3D (Tai Chi, Qi Gong, dance, yoga) | No intervention | Supervised | Group | |
| Conventional exercise: strength/resistance | No intervention | Supervised | Group | |
| 3D (Tai Chi, Qi Gong, dance, yoga) | No intervention | Supervised | Group | |
| Gait, balance, co‐ordination, functional tasks | Discussion group | Unsupervised | Individual | |
| Gait, balance, co‐ordination, functional tasks | No intervention | Supervised | Individual | |
| Strength/resistance | Education (nutrition) | Supervised | Group | |
| Gait, balance, co‐ordination, functional tasks | No intervention | Unsupervised | Individual | |
| 3D (Tai Chi, Qi Gong, dance, yoga) | Education (falls prevention) | Supervised | Group | |
| 3D (Tai Chi, Qi Gong, dance, yoga) | No intervention | Supervised | Group | |
| Seated exercise: strength/resistance | Social visits | Unsupervised | Individual | |
| Weight‐bearing exercise: strength/resistance | Social visits | Unsupervised | Individual | |
| 3D (Tai Chi, Qi Gong, dance, yoga) | No intervention | Supervised | Group | |
| 3D (Tai Chi, Qi Gong, dance, yoga) | No intervention | Supervised | Group | |
| Gait, balance, co‐ordination, functional tasks | No intervention | Supervised | Group | |
| Gait, balance, co‐ordination, functional tasks | Education (falls prevention) | Supervised | Group | |
| Tai chi: 3D (Tai Chi, Qi Gong, dance, yoga) | Education (gerontology) | Supervised | Group | |
| Computerised balance training: gait, balance, co‐ordination, functional tasks | Education (gerontology) | Supervised | Individual | |
| Gait, balance, co‐ordination, functional tasks | Crafts/games | Supervised | Individual | |
| Gait, balance, co‐ordination, functional tasks | No intervention | Unsupervised | Individual | |
| Strength/resistance | No intervention | Supervised | Group | |
| 3D (Tai Chi, Qi Gong, dance, yoga) | No intervention | Supervised | Group | |
| Five studies had two or more arms with exercise interventions. Each intervention arm is described separately in the table. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Fear of falling as measured by single‐item question, falls efficacy, balance confidence and concern about falling, post intervention Show forest plot | 24 | 1692 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| 1.1 Fear of falling as measured by single‐item question | 4 | 380 | Std. Mean Difference (Random, 95% CI) | 0.17 [‐0.06, 0.39] |
| 1.2 Falls efficacy measured using the FES, MFES or K‐FES | 12 | 872 | Std. Mean Difference (Random, 95% CI) | 0.56 [0.21, 0.90] |
| 1.3 Balance confidence measured using ABC | 6 | 333 | Std. Mean Difference (Random, 95% CI) | 0.13 [‐0.10, 0.37] |
| 1.4 Concern about falling measured using the FES‐I and Short FES‐I | 2 | 107 | Std. Mean Difference (Random, 95% CI) | 0.52 [‐0.09, 1.12] |
| 2 Fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, short term follow‐up (< 6 months) Show forest plot | 4 | 356 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.17 [‐0.05, 0.38] |
| 3 Fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, long term follow‐up (6 months and more) Show forest plot | 3 | 386 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.01, 0.41] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Type of exercise (as classified using ProFaNE taxonomy) Show forest plot | 22 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 1.1 3D (Tai Chi) | 7 | 483 | Std. Mean Difference (Random, 95% CI) | 0.60 [0.09, 1.12] |
| 1.2 Strength/resistance | 4 | 416 | Std. Mean Difference (Random, 95% CI) | 0.08 [‐0.18, 0.34] |
| 1.3 Gait, balance, co‐ordination, functional tasks | 11 | 619 | Std. Mean Difference (Random, 95% CI) | 0.27 [0.05, 0.50] |
| 2 Type of control group Show forest plot | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| 2.1 Alternative intervention (e.g. social group, education, etc) | 6 | 499 | Std. Mean Difference (Random, 95% CI) | 0.11 [‐0.08, 0.29] |
| 2.2 No intervention | 18 | 1199 | Std. Mean Difference (Random, 95% CI) | 0.48 [0.22, 0.73] |
| 3 Recruited participants at increased risk of falls Show forest plot | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| 3.1 Studies not recruiting participants on the basis of increased risk of falls | 14 | 926 | Std. Mean Difference (Random, 95% CI) | 0.44 [0.14, 0.74] |
| 3.2 Studies recruiting participants at increased risk of falls | 10 | 772 | Std. Mean Difference (Random, 95% CI) | 0.24 [0.04, 0.45] |
| 4 Type of exercise (individual versus group) Show forest plot | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| 4.1 Group exercises | 15 | 1051 | Std. Mean Difference (Random, 95% CI) | 0.49 [0.22, 0.76] |
| 4.2 Individual exercises | 9 | 647 | Std. Mean Difference (Random, 95% CI) | 0.14 [‐0.06, 0.35] |
| 5 Frequency of exercise Show forest plot | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| 5.1 1 to 3 times per week | 20 | 1339 | Std. Mean Difference (Random, 95% CI) | 0.38 [0.15, 0.61] |
| 5.2 4 or more times per week | 4 | 359 | Std. Mean Difference (Random, 95% CI) | 0.30 [0.01, 0.58] |
| 6 Duration of exercise Show forest plot | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| 6.1 Up to 12 weeks | 17 | 968 | Std. Mean Difference (Random, 95% CI) | 0.32 [0.16, 0.48] |
| 6.2 13 to 26 weeks | 5 | 530 | Std. Mean Difference (Random, 95% CI) | 0.52 [‐0.13, 1.17] |
| 6.3 More than 26 weeks | 2 | 200 | Std. Mean Difference (Random, 95% CI) | 0.13 [‐0.41, 0.66] |
| 7 Primary aim of the study Show forest plot | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| 7.1 To reduce fear of falling | 7 | 471 | Std. Mean Difference (Random, 95% CI) | 0.42 [0.13, 0.72] |
| 7.2 Other primary aim (e.g. balance improvement, fall prevention, etc) | 17 | 1227 | Std. Mean Difference (Random, 95% CI) | 0.34 [0.10, 0.59] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Occurrence of at least one fall Show forest plot | 9 | 1113 | Risk Ratio (IV, Fixed, 95% CI) | 0.85 [0.74, 0.98] |
| 2 Falls rate Show forest plot | 9 | 1121 | Rate Ratio (Random, 95% CI) | 0.68 [0.53, 0.87] |
| 3 Depression score, post intervention Show forest plot | 4 | 406 | Std. Mean Difference (Fixed, 95% CI) | ‐0.08 [‐0.28, 0.13] |
| 4 Depression score, short‐term follow‐up (< 6 months) Show forest plot | 3 | 327 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.02, 0.43] |
| 5 Physical activity as measured using PASE (Physical Activity Scale for the Elderly) Show forest plot | 4 | 547 | Mean Difference (IV, Fixed, 95% CI) | 3.44 [‐1.65, 8.54] |


