Técnicas de relajación para el tratamiento del dolor durante el trabajo de parto
References
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Parallel RCT of breathing techniques and relaxation compared with usual care (nursing) | |
| Participants | 65 women were recruited from the antenatal ward, obstetric ward and postnatal ward of a public hospital, located in Goias, Brazil. Inclusion criteria: primiparas with normal labour and at low risk, in latent phase (≦ 4 cm dilation) of labour on admission, no obstetric disease or complications, not having previously participated in psychoprophylactic preparation courses for childbirth Exclusion criteria: dystocia, fetal distress, obstetrical disease or indication for caesarean, requirement for forceps delivery or use of analgesia | |
| Interventions | Intervention: Individualised nursing care with advice and encouraging the use of breathing techniques and relaxation. Adopted from Grantly Dick Read and Fernand Lamaze from admission of mother until delivery. Breathing techniques used during contractions at different stages of labour and during delivery. Latent phase total respiration (thoracic abdominal breathing slowly, with deep inspiration and expiration, in a natural rhythm. Active phase: thoracic breathing slowly (slow breathing with deep inspiration and expiration, a natural rhythm, directing the breath to the chest. Transition phase: pressure breathing without performing abdominal pressure force (breath slow, deep breathing with sustained for periods during contractile pull in order to maintain the diaphragm force acting on the uterus, followed by long expiration. Explusion period; pressure breathing with the exertion of the abdominal force (contraction of skeletal muscle) at the time of the tugs. Relaxation techniques: release all body muscles associated with the total respiration, in intervals of uterine contractions Control: routine nursing care | |
| Outcomes | Self‐assessment scales: STAI and VAS to evaluate the intensity of pain VAS evaluated in early stages of latent, active and transition, at the time of contraction STAI administered in latent phase of labour and state of anxiety and active phases of transition and in the immediate postpartum period Length of labour | |
| Notes | Study duration May 2000‐March 2001 Funding: not reported Conflicts of interest: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss with randomisation in a 1:1 ratio (17 control group, 19 experimental group) |
| Allocation concealment (selection bias) | Low risk | Allocation unknown until the moment of coin toss |
| Blinding of participants and personnel (performance bias) | High risk | Interventions were substantially different and obvious to an observer. Allocation was known to participants and clinicians |
| Blinding of outcome assessment (detection bias) | High risk | Outcomes would be recorded by staff providing care, who would be aware of the intervention |
| Incomplete outcome data (attrition bias) | High risk | Postrandomisation exclusions: 29 (44.62%) were excluded, 12 for use of exogenous oxytocin, 2 for forceps delivery and 15 caesarean delivery. Data not presented by group |
| Selective reporting (reporting bias) | Unclear risk | The study protocol is not available but the study excluded clinical outcomes |
| Other bias | Unclear risk | Data were not presented on the baselines characteristics of those excluded after randomisation |
| Methods | Parallel RCT of relaxation compared with usual care | |
| Participants | 62 women aged 20‐30 years recruited from the Fatemieh Hospital, Hamadan, Iran Inclusion criteria: primiparous with no obstetric complications Exclusion criteria: no exclusion criteria were specified | |
| Interventions | No women in either group received analgesics before or during labour. Intervention: followed instructions under the supervision of 1 of the researchers. The relaxation intervention followed a standard method involving the participants to be positioned in a comfortable state, in a quiet environment and tensing and relaxing muscles in the toes, feet, ankles, calves, knees, thighs, lower abdomen, upper abdomen, shoulders, arms, hands, fingers, neck, face and heads. Control: standard care | |
| Outcomes | Pain was assessed along a NRS. Pain intensity was measured during the first phase of labour, active phase (dilatation < 7 cm), second phase of labour (dilatation 10 cm), and pain intensity was expressed as low (1‐4), mild (5‐6), severe (7‐8), very severe (9‐10). Behavioural indicators of pain were also recorded | |
| Notes | Dates of study: 2002 Funding: not reported Conflicts of interest: none | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details could be obtained from the study author |
| Allocation concealment (selection bias) | Unclear risk | No details could be obtained from the study author |
| Blinding of participants and personnel (performance bias) | High risk | Women and clinicians were not blind to group allocation |
| Blinding of outcome assessment (detection bias) | High risk | Outcomes would be recorded by staff providing care, who would be aware of the intervention |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Protocol not reported |
| Other bias | Unclear risk | Insufficient reporting |
| Methods | Parallel RCT of labour preparation (relaxation and breathing techniques) versus usual care | |
| Participants | Inclusion criteria: 120 women from 20 weeks’ gestation planning vaginal delivery without pregnancy complications and without abnormal stress in the previous year. Exclusion criteria: dissatisfaction to continue with the study, incidence of stressful events, abnormalities and fetal and neonatal death. Women recruited from a public health centre, Iran | |
| Interventions | Intervention: labour preparation classes: classes were conducted in groups of 10, twice per week for 8 sessions, each lasting 1.5 h, between weeks 20 and 37. The topics included stretching exercises, relaxation, massage and breathing patterns during labour and in postpartum Control: routine pregnancy care | |
| Outcomes | Vitality scores | |
| Notes | Dates of study: 2010 Funding: not reported Conflicts of interest: none | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Not described but staff and participants likely to be aware of this intervention |
| Blinding of outcome assessment (detection bias) | High risk | Not reported but likely to be high as outcomes were assessed in labour and staff were aware of treatment allocation |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient reporting |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting |
| Other bias | Unclear risk | Insufficient reporting |
| Methods | Multicentre RCT of natural childbirth preparation with psychoprophylactic training versus usual antenatal care. Pregnant women and their partners were randomised into groups of approximately 12 people (median 6 couples). 106 natural groups: 101 standard care groups. Educators were randomised individually to lead groups according to either model during the entire study period | |
| Participants | 1087 nulliparous women and 1064 partners. Recruitment was from 15 antenatal clinics in Sweden Inclusion criteria: nulliparous, Swedish‐speaking and attending any of the participating clinics Exclusion criteria: multiparous, non Swedish‐speaking, attendance at other clinic | |
| Interventions | Intervention: natural model for antenatal education focusing on preparation for childbirth only, including training in psychoprophylaxis. Information was given about nonpharmacological methods for pain relief and the partner’s role as a coach during labour. In each session, 30 min were spent on practical training in breathing, relaxation and massage techniques. Psychoprophylactic training between sessions was encouraged and a booklet to facilitate homework was distributed. The attitude of the educator was encouraged to be in favour of natural birth. No parenthood preparation was included. Control: the standard care model, equal time was allocated to information and discussion about childbirth and parenthood issues to reflect the content of antenatal education as provided by antenatal clinics in Sweden. Within these limits the teaching methods of the standard care groups could vary. The educators in this model were free to present films, arrange visits to the delivery ward. No information about breathing, relaxation or other specific techniques for coping with labour pain was included. | |
| Outcomes | Epidural analgesia during labour, labour pain, mode of delivery, experience of childbirth as measured by Wijma Delivery Experience Questionnairere at baseline and 3 months postnatal, parental stress measured by the Swedish Parenthood Stress Questionnaire at baseline and 3 months postnatal | |
| Notes | Duration of study: January 2006‐May 2007 Funding: this work was funded by the Swedish Research Council and Karolinska Institute. All study authors state their independence Conflicts of interest: none | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified computer‐generated group randomisation Randomisation stratified per clinic and within clinic |
| Allocation concealment (selection bias) | Low risk | Central randomisation |
| Blinding of participants and personnel (performance bias) | High risk | There was no blinding |
| Blinding of outcome assessment (detection bias) | High risk | Data entry was blind to group allocation but analysis was not undertaken blinded |
| Incomplete outcome data (attrition bias) | Low risk | 11% of women, and 19% men did not receive the active intervention, 10% women, and 17% men did not receive standard care. The reasons were the same: inconvenient timing of classes, preterm labour, medical complications. Loss at 3‐month follow‐up was similar between groups |
| Selective reporting (reporting bias) | Low risk | Study protocol not available but manuscript includes all expected outcomes. |
| Other bias | Low risk | The trialists noted that while individual women were randomised to intervention and control groups, the intervention was delivered at the level of groups and there may have been a group effect. They report that there was minimal differences between groups and there was no adjustment needed for possible group effects. |
| Methods | Parallel RCT of a deep breathing relaxation techniques compared with usual care | |
| Participants | Recruitment from Professor Bandeira Filho Maternity Hospital, in Recife, Brazil Inclusion criteria: low‐risk primigravid women, 16‐35 years old, 37‐41 weeks of gestation in active labour Exclusion criteria: women with multiple pregnancies, pregnancy with a dead fetus, analgesic use, clinical instability and psychiatric disorders | |
| Interventions | Intervention: breathing patterns during contraction – deep inspiration and prolonged or fractional exhalation. Respiratory patterns, used in accordance with dilation period, were interrupted at signs of breathing discomfort or when respiratory rate increased > 20 breaths/min Women were instructed to inhale slowly, count from 1‐5 and breathe out gradually, counting from 5‐1. The inspiratory phase was not stimulated to full lung capacity; thus, there was an inspiratory reserve volume. For the breathing pattern with postexhalation pause, they were instructed to take a deep breath and increase the postexhalation pause (1e2 s). With respect to expiratory deceleration, the participant was instructed to take an extended exhalation, propelling the lips forward (pursed lip breathing). This pattern was used mainly when contractions were strong The physiotherapist demonstrated these patterns so the women would be able to execute them properly. Total number randomised: n = 67 Control: usual care 73 women randomised; “treated in‐line with standard procedures” – usual care not described | |
| Outcomes | Primary outcome: maternal anxiety ‐ STAI Secondary outcome: pain (VAS), satisfaction, fatigue, mode of delivery and duration of labour Neonatal: the 5‐minute Apgar score | |
| Notes | Dates of study: not reported Funding: scholarship from Foundation for Science and Technology of the State of Pernambuco (FACEPE) Conflicts of interest: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random Allocation Software 1.0 |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes sequentially numbered from 1‐140 were prepared. Each number indicated the participant's group, according to a randomisation chart. In order to ensure confidentiality, a physiotherapist not involved in this research prepared both the randomisation and the envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Not feasible and no separate delivery suites |
| Blinding of outcome assessment (detection bias) | High risk | Not reported although staff recording outcomes in labour were likely to be aware of treatment group |
| Incomplete outcome data (attrition bias) | Low risk | Total missing data n = 19 (n = 7 intervention and n = 12 control). Multiple imputation methods were used to address missing values which could be included in the analysis |
| Selective reporting (reporting bias) | Unclear risk | ClinicalTrials.gov Identifier: NCT02164227 ‐ only primary outcome listed on register ‐ protocol not available |
| Other bias | Unclear risk | Insufficient reporting |
| Methods | Parallel RCT of yoga compared with usual care | |
| Participants | 74 women were recruited from 2 public hospitals in Southern Thailand. Inclusion criteria: primiparous women without serious illness or high‐risk complications during pregnancy; receiving antenatal care from the start, or at least 2nd trimester of pregnancy; and, without prior experience of practising yoga; > 18 years old; able to communicate and write in Thai Exclusion criteria: not specified | |
| Interventions | Intervention: participants in the experimental group received a series of six 60‐min yoga practice sessions at the 26th, 28th, 30th, 32nd, 34th, 36th, and 37th week of gestation. The yoga programme was a combination of: (a) educational activities, giving a brief description of basic anatomical structures related to pregnancy and birth and (b) yoga, explaining the concepts related to each session. Yoga asanas, chanting om, breathing awareness, yoga nidra, and dhyana were practiced harmoniously and in an orderly manner. The women were provided a booklet and tape cassette, for self‐study, that explained the principles and benefits of each yoga practice. All were asked to practise at home at least 3 times a week, starting after the first yoga practice session and continuing for a period of 10‐12 weeks. The number of weeks of practice (10, 11 or 12) depended upon whether the women started their first yoga practice session at the 26th, 27th or 28th week of gestation. Participants were informed they could practice, at home, > 3 times a week. So investigators could monitor participants’ involvement in each yoga session they performed at home, they were asked to maintain a record, in diary format. In addition, to ensure compliance with the research protocol, weekly telephone calls were made by investigators to each participant. Control: usual care. Control group participants were seen by researchers at each of their hospital visits. They engaged in casual conversation for 20‐30 min. To ensure compliance with research protocol, weekly phone calls were made by investigators to each participant. | |
| Outcomes | VAS Total Comfort Maternal comfort questionnaire (MCQ) Labour pain using visual analogue sensation of pain scale (VASPS) to assess labour pain Pain behavioural observation scale (PBOS) to assess investigator‐observed labour pain Birth outcomes by Apgar scores Length of labour Augmentation Pethidine usage for pain relief | |
| Notes | Study duration: January 2005‐February 2006 Funding: partially funded by the Faculty of Graduate Studies, Prince of Songkla University, Hat Yai, Songkhla, Thailand Conflicts of interest: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence. Stratified randomisation according to maternal age, marital status, education, income and trait‐anxiety. Randomisation in ratio of 1:1 |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Participants and the clinician were not blind and it is possible the outcome measurement may have been influenced by a lack of blinding |
| Blinding of outcome assessment (detection bias) | High risk | Not reported but outcome measurement may have been influenced by lack of blinding |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient reporting |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Other bias | Low risk | No imbalance in baseline characteristics or differential diagnosis |
| Methods | Reported to be RCT but no information on methods in the brief abstract | |
| Participants | 95 women expecting a normal spontaneous birth. Iran | |
| Interventions | Intervention: routine care and music therapy for 45 min Total number randomised: n = 45 Control: routine care only Total number randomised: n = 50 | |
| Outcomes | Labour pain reported on a VAS | |
| Notes | Although this study is eligible for inclusion in the review no usable outcome data were reported and so no data from this study are included in our analyses. We have attempted to find contact information for the study author, but have been unsuccessful. Dates of study: not reported Funding: not reported Conflicts of interest: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described in brief abstract |
| Allocation concealment (selection bias) | Unclear risk | Not described in brief abstract |
| Blinding of participants and personnel (performance bias) | High risk | Not described but likely to be high as it is difficult to blind this type of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Not described but likely to be high as it is difficult to blind this type of intervention |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described |
| Selective reporting (reporting bias) | Unclear risk | Very little information |
| Other bias | Unclear risk | Too little information to assess |
| Methods | Parallel controlled partial double‐blind trial of RAT versus traditional psychoprophylaxis method | |
| Participants | 53 women were randomly assigned to their study group. Women were aged 20‐35 years, participated in no fewer than 5 sessions Inclusion criteria: no physical abnormalities, obstetric score < 30 The study was undertaken at a University Clinic in Verona, Italy | |
| Interventions | Intervention: RAT consists of the woman learning to auto‐induce an autogenous state and to reduce her muscle tone by deep relaxation. Control: no details provided | |
| Outcomes | Emotional state during labour and after childbirth, pain, pain experience, Apgar score, length of labour | |
| Notes | There was no power analysis Dates of study: not reported Funding: not reported Conflicts of interest: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation was used but no details provided |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of participants and personnel (performance bias) | High risk | Partcipants were not blind to their group allocation |
| Blinding of outcome assessment (detection bias) | Unclear risk | The outcome analyst was reported to be blind to group allocation |
| Incomplete outcome data (attrition bias) | Unclear risk | Data available on 34 women |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Other bias | Low risk | No imbalance at baseline. No other biases apparent |
| Methods | Parallel RCT comparing mindfulness in labour versus education alone | |
| Participants | 30 first time mothers in their third trimester of pregnancy were randomly assigned to 1 of 2 study groups. Inclusion criteria: English‐speaking nulliparous women with low‐risk, healthy, singleton pregnancies in their third trimester who were planning a hospital birth and willing to be randomised. Exclusion criteria: high‐risk pregnancy, extensive prior experience with meditation or yoga practice (brief prenatal yoga did not lead to exclusion), participation in other mind/body childbirth preparation courses (e.g. Hypnobirthing, Bradley Method), or planned caesarean birth. Classes were delivered in a community setting in the USA | |
| Interventions | Intervention: Mindfullness in Labor (MIL) is a brief intervention for pregnant women and their partners specifically designed to target labour‐related fear and pain by teaching tailored mindfulness‐based coping strategies. It is a childbirth‐specific, short form of the 9‐week Mindfulness‐Based Childbirth and Parenting program (MBCP). The MIL course is delivered by professionally certified MBCP instructors and it is held over 1 weekend (Friday evening and all day Saturday and Sunday) for a total of 18h of mindfulness training. Mindfulness strategies for coping with labour‐related pain and fear are taught through interactive, experiential activities, with periods of didactic instruction. To meet these objectives, instruction in formal mindfulness meditation are given during the workshop, including body scan, mindful movement/yoga, sitting and walking meditation, and mindful eating, as well as activities of daily living and pain coping strategies, such as mindfulness of breath, partner touch, body movement, and “sounding” (using low and/or loud vocal tones during periods of intense physical sensation). Control: participants assigned to the TAU control condition were provided with a list of study‐approved childbirth courses of comparable length and quality to the MIL intervention, but without any mindfulness meditation, mindful movement/yoga, or other core mind/body component (e.g. hypnosis) | |
| Outcomes | Childbirth Self‐Efficacy Inventory Pain Catastrophizing Scale Perceived labour pain (VAS) Use of pain medication in labour was ascertained from medical record review Birth satisfaction (Wijma Delivery Expectancy/Experience Questionnaire) | |
| Notes | Dates of study: not reported. Funding: funding for this study was provided by a grant from the Mount Zion Health Fund, San Francisco, CA, administered by the University of California, San Francisco (UCSF) School of Medicine. 2 study authors were supported by the US National Institutes of Health/National Center for Complementary and Integrative Health (NIH/NCCIH) through career development awards (LGD: K01 AT005270; MTC: K01 AT006545) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was stratified by pre‐course intention to use epidural anaesthesia and was performed with randomly varying blocks of 2 and 5 using a pre‐programmed computer database. A UCSF senior biostatistician not affiliated with the study generated the randomisation scheme. |
| Allocation concealment (selection bias) | Low risk | The study project manager (JGC) enrolled and consented study participants; group assignment and subsequent debriefing regarding intervention attendance was conducted by opening a sealed envelope provided by the biostatistician. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding attempted |
| Blinding of outcome assessment (detection bias) | Low risk | Data collection was completed online and through medical record review. The remaining study authors (including data analysts) were blinded to participant study condition |
| Incomplete outcome data (attrition bias) | Low risk | Dropouts balanced between groups and unlikely to be related to intervention. Loss to follow‐up low |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol available |
| Other bias | Unclear risk | Insufficient information to assess |
| Methods | RCT of music plus Lamaze breathing techniques versus Lamaze breathing techniques alone | |
| Participants | 30 primiparous couples recruited from the Kansas medical centre, USA. Inclusion criteria: not specified Exclusion criteria: not specified | |
| Interventions | All groups received instruction on Lamaze breathing techniques. During stage I, phase I (latent) labour, slow chest breathing was used. With phase 2 labour, shallow chest breathing was used to assist the woman cope with the increasing strength of the contractions Intervention: during phase 1 music was slow 4/4 tempo with a distinct drum beat. During phase 2, the tempo of the music increased as well as the volume of music. During transition the volume was regulated to meet the individuals' needs, a moderate‐fast tempo was used. During stage II expulsion, a driving melody was used with strong percussions, strong rhythm and increased volume to encourage pushing. The music was tape recorded and couples had the option of using headphones. Control: as above, no intervention | |
| Outcomes | Use of pain relief | |
| Notes | Dates of study: not reported Funding: not reported Conflicts of interest: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Participants and therapist were not blind to group allocation |
| Blinding of outcome assessment (detection bias) | Unclear risk | Outcome assessor were not blind to group allocation |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear on whether data collection was complete |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting |
| Other bias | Unclear risk | Insufficient reporting |
| Methods | RCT initially with 3 arms with a 4th added later | |
| Participants | 78 primipara women were recruited from the obstetrics department at the Mirano Hospital, Italy Inclusion criteria: no obstetric complication, anxiety score of ≥ 7 at 26 weeks of pregnancy. Exclusion criteria: not stated | |
| Interventions | Intervention commenced at 32 weeks Intervention group 1: 26 women allocated to the intervention group, they received obstetric psychoprophylaxis and 4‐weekly guided relaxation sessions on an individual level guided by 2 teachers with biofeedback. Interventon group 2: a second intervention group of 26 women received the psychoprophylaxis, and counselling. Control 1: 26 women received obstetric psychoprophylaxis only, and saw the psychologist for analysis of test results only. Control 2: a second comparison group was added of 12 women who came to the hospital for antenatal checks and birthing only. | |
| Outcomes | Duration of labour, mode of birth, anxiety scores | |
| Notes | Dates of study: not reported Funding: not reported Conflicts of interest: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Not described and does not appear as if there was any attempt to introduce blinding |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | High risk | Large number of dropouts from initial randomisation: 26: 26:26:12 to 6:7:23:12. Reason for losses not reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting |
| Other bias | Unclear risk | Insufficient reporting |
| Methods | RCT with individual randomisation | |
| Participants | Stavanger University Hospital, Norway. Dates of recruitment not stated. 58 women randomised Inclusion criteria: healthy pregnant women at the beginning of the 3rd trimester expected to have a vaginal birth attending for regular pregnancy healthcare at the study hospital Exclusion criteria: not described | |
| Interventions | Intervention: usual care plus a CD and booklet. The CD included instructions and 3 relaxation tracks, 1 with relaxing music and guided imagery of the birth process, 1 with music and positive affirmation, and 1 with music only. Women were advised to practise 15 min with the CD daily and to record when they did it. They were not told to use the CDs during the birth but could if they wanted to. Total number randomised: n = 29 women Control: usual care with no CD Total number randomised: n = 29 | |
| Outcomes | Primary outcome was well‐being (measured on the Edmonton scale or ESAS) 1 day after delivery; pain (NRS 0‐10, 10 worst) during labour and delivery (3 times) and 1 day after delivery, anxiety (VAS 0‐100, 100 worst) during delivery (not clear) and 1 day after delivery. Apgar score (reported as mean at 1 minute) | |
| Notes | Dates of study: not reported Funding: funding reported to be provided by the investigators' employing institutions (university hospitals in Norway) Conflicts of interest: reported that the authors had no conflicts of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Reported as “randomised ahead by pulling numbers” |
| Allocation concealment (selection bias) | Low risk | Probably low risk. “participants were given a sealed unmarked envelope.” |
| Blinding of participants and personnel (performance bias) | High risk | Probably high risk. It was stated that investigators were blind, but it was not clear whether the CDs were distributed by staff providing care and women would be aware of the intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | Staff providing care may have been aware of the intervention and they would be recording outcomes during delivery. It is not clear whether staff or researchers collected pre‐ and postintervention scores (e.g. for day after delivery measures) |
| Incomplete outcome data (attrition bias) | High risk | It was not clear when outcome data were collected. There was reference to “early and late responders”; some women did not complete post‐test questionnaires until more than a week after the birth (15/27 respondents for control group and 18/27 in the intervention group). While data on well‐being were collected 50/58 of those randomised this applied to only 25/58 for pain scores in labour and 29/58 for anxiety |
| Selective reporting (reporting bias) | High risk | Much data were not collected at the appropriate time. Further results were not fully reported. It was suggested that pain and anxiety were measured several times during labour but there was a single pain and anxiety score reported (it was not clear whether this represented some sort of average of all time points or if not, at what point during labour outcomes were reported) |
| Other bias | Unclear risk | There was some baseline imbalance between groups for anxiety |
| Methods | A clinical trial comparing music to no music on labour pain and labour progress | |
| Participants | 30 primiparous women from Bentolhoda hospital of Bushehr city of Iran in the active stage of labour. Inclusion criteria: primipara, aged 20‐30, lived in urban dwellings, been in a complete physical and mental health status | |
| Interventions | Intervention: directed imagination with music was taught to the experimental group (when there was no uterine contraction) and then the light music of “Barane Eshgh” (Love Rain) composed by Manouchehr Cheshmazar was played by headphone for 30 min for women of the experimental group, and after removing the headphones and in case there was no uterine contraction, the parturients were asked to explain the severity of their pain based on the 3 numerical, visual and verbal scales while listening to the music and their statements were recorded. Then, the music was played again to the parturient after half an hour and it was continued for 2 h after hospitalisation. At the end of the second h, labour progress and severity of pain were again measured and recorded. Control: no music | |
| Outcomes | Pain level (visual pain level, verbal pain level and numeric pain level) and delivery progress (uterine contractions and dilation) | |
| Notes | Unclear if randomised or quasi‐randomised ‐ study authors contacted to confirm Attempted to contact study authors on the 19 June 2017 Dates of study: not reported Funding: not reported Conflicts of interest: none | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details were reported |
| Allocation concealment (selection bias) | Unclear risk | No details were reported |
| Blinding of participants and personnel (performance bias) | High risk | Probably high risk, women and clinicians were not blind to group allocation |
| Blinding of outcome assessment (detection bias) | Unclear risk | Staff providing care may have been aware of the intervention and they would be recording outcomes during delivery, no reporting was made |
| Incomplete outcome data (attrition bias) | Low risk | No attrition reported |
| Selective reporting (reporting bias) | Unclear risk | No protocol was available |
| Other bias | Unclear risk | Unclear due to insufficient reporting |
| Methods | 3‐armed, parallel RCT comparing massage + relaxation, music therapy + relaxation versus treatment as usual | |
| Participants | 90 pregnant women took classes at 35‐37 weeks' gestation. Inclusion criteria: from 20 weeks' gestation Exclusion criteria: planned elective caesarean section, multiple pregnancy, existing medical problems that precluded the use of massage, previous use of the massage programme or a strong preference for a particular form of pain relief; not fluent English speaker; not intending to have a birth companion Recruitment was undertaken through Horton Maternity Unit, Banbury, United Kingdom (2004‐2006) | |
| Interventions | Intervention: women attended a 2.5 h class between 35‐37 weeks' gestation with their chosen birth companion. Participants were asked to practise the programme at least 3 evenings a week, for about 30–45 min, until 39 weeks and then a combination of techniques every evening, until hospital admission for labour/induction. The class taught breathing and visualisation techniques, and music. The woman and her birth partner were encouraged to practise a slow breathing rhythm and visualisation techniques were taken from readings in a well known book (Broncher 1992). The woman and her birth partner chose their favourite music. Women were also able to attend usual antenatal classes. Control group 1: usual care. Women allocated to the control group were given the option and encouraged to attend the usual antenatal preparation classes currently available at the trial site. For the duration of the trial there were three, 2.5 hour classes, which included an antenatal and labour session incorporating information about labour, methods of pain relief and types of delivery. Control group 2: massage + relaxation Women attended a 2.5 h class between 35‐37 weeks' gestation with their chosen birth companion. Massage techniques were taught by the midwife/therapist. The birth partner learnt to perform slow rhythmic long stroke massage movements using the flats of the hands. These strokes were combined with slow rhythmic breathing and performed primarily on the lower back and also the upper and lower limbs. The massaging hands move upwards during inspiration and downwards during expiration. The woman and her birth partner were taught to synchronise massage strokes with controlled breathing. The visualisation/mind mapping component was taught, by asking the woman to visualise/focus on the massaging hands. Participants were asked to practise the programme at least 3 evenings a week, for about 30–45 min, until 39 weeks and then a combination of techniques every evening, until hospital admission for labour/induction | |
| Outcomes | The primary outcome measure was self‐reported labour pain, using the VAS. The secondary outcomes were the use of pharmacological analgesia, obstetric interventions, birth outcomes and women’s birth‐related worries based on the Cambridge Birth Worry Scale, maternal satisfaction and sense of control (Labour Agentry Scale) | |
| Notes | Dates of study: 2004‐2006 Funding: complementary medicine grant from Oxfordshire Health Services Research Committee (OHSRC) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women were randomised to study groups by a computer‐based randomisation program supplied by the National Perinatal Epidemiology Unit (NPEU), University of Oxford |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | No blinding possible due to nature of intervention groups |
| Blinding of outcome assessment (detection bias) | High risk | Pain self‐reported outcomes, may be affected by lack of blinding. No blinding of research midwife collecting other outcome data |
| Incomplete outcome data (attrition bias) | Low risk | Dropouts not significantly different between groups and unlikely to be due to intervention. Dropout rate 10% or less across all groups |
| Selective reporting (reporting bias) | Low risk | All outcomes reported from protocol |
| Other bias | Unclear risk | No baseline imbalances |
| Methods | Parallel RCT of music plus standard care compared with usual care | |
| Participants | 103 participants were recruited from 2 hospitals in southern Taiwan Inclusion criteria: normal pregnancy; primiparous, at term; planned vaginal delivery; singleton; no intention to use pharmacological analgesic during labour Exclusion criteria: not stated | |
| Interventions | Intervention: participants could choose 1 of the following types of relaxing, anxiety reducing music: classical (e.g. Beethoven: For Elise, Debussy: Preludes I Livre VIII, La fille aux cheveux de lin and Kreisler: Liebesfreud), light (e.g. Liszt: Liebestraum, Rachmaninoff: Piano Concerto No. 2 in C Minor and Williams: Dream of Olwen), popular (e.g. The sound of silence, Somewhere in time and The way we are), crystal children’s (e.g. Doll country, Little honey‐bee, Jasmine) or Chinese religious music (Buddhist music, Sutra). In addition to receiving standard nursing care, the experimental participants listened to 1 of these for at least 30 min during the latent phase (2‐4 cm cervical dilation) and active phase (5‐7 cm cervical dilation) of labour. To account for the wide variety of music‐listening habits, participants were allowed to choose whether or not to use headphones. Control: participants in the control group were not aware that they had not had the opportunity to listen to music, but they received routine care after admission | |
| Outcomes | VAS for pain and present behavioural intensity (PBI), 2 anxiety measures: VAS for anxiety (VASA) and FT and 1 open‐ended questionnaire 24 h after childbirth, women in the experimental group were asked to complete an open‐ended questionnaire to indicate their perceptions of the effectiveness of music therapy on pain and anxiety and a 5‐point scale to evaluate the helpfulness of music | |
| Notes | Dates of study: not reported Funding: this study was funded by the National Science Council, Taipei, Taiwan, NSC 90‐2314‐B‐037‐072 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Lot drawing |
| Allocation concealment (selection bias) | Low risk | Coded balls |
| Blinding of participants and personnel (performance bias) | High risk | Blinding not attempted although the control group was unaware of the intervention group |
| Blinding of outcome assessment (detection bias) | High risk | Not described but likely to be high as it is difficult to blind this type of intervention |
| Incomplete outcome data (attrition bias) | High risk | 51 initially allocated to each group. 40% loss of data although no difference between groups. Postrandomisation exclusions: intervention group: prolonged labour and caesarean delivery n = 5, use of epidural n = 15 Control group: prolonged labour and caesarean delivery n = 4, use of epidural n = 18 |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Other bias | Unclear risk | No imbalance at randomisation |
| Methods | Parallel, single‐blind, RCT of audio‐analgesia | |
| Participants | 25 women randomised to the trial Inclusion criteria: singleton pregnancy in the 1st stage of labour Exclusion criteria: history of ear disease or vestibular disturbance The trial was undertaken in England | |
| Interventions | Intervention: women in the experimental arm listened to white sound set at 120 decibels. Control: listened to white sound at a maximum 90 decibels (it was presumed at this level there is no physiological effect). The intervention started when the woman was in established labour. If the women became tired the audio‐analgesia was stopped and resumed later. If the midwife considered the pain relief inadequate, the audio analgesia was stopped and inhalation analgesia started | |
| Outcomes | Midwife's opinion of pain relief from audio‐analgesia, woman's satisfaction with 'sea noise' | |
| Notes | There was no sample‐size calculation. No details were provided on baseline characteristics. Dates of study: not reported Funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient details to determine if blinding was undertaken |
| Blinding of outcome assessment (detection bias) | Unclear risk | It was unclear whether the outcome assessor and analyst were blind |
| Incomplete outcome data (attrition bias) | Low risk | 1 (4%) woman withdrew from the trial |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Other bias | Unclear risk | Insufficient reporting |
| Methods | Randomised factorial design of yoga position + music compared with postural management (5 groups) | |
| Participants | 207 women were recruited to the trial from a regional hospital in Southern Thailand. Inclusion criteria: primiparous women, aged 18‐35 years, in latent phase for no more than 10 h, single fetus Exclusion criteria: received analgesics before the starting the study, induced labour, SROM > than 20 h previously, history of psychiatric problems, hearing difficulty, asthma, infection, negative reactions whilst listening to music, cephalic presentation, 38‐42 weeks' gestation, estimated fetal weight 2.5 kg‐4 kg | |
| Interventions | Intervention: yoga + music The PSU Cat is the position whereby women lean on the inclined (30°‐45°) head of the bed and the knee is bent on the bed. The head of the woman is placed on the raised head of the bed. Mechanism of the PSU Cat position: when the mother in a prone position is allowed to lean her body forward on the bed, then the weight of the infant will be put onto the abdomen and this position will relieve back pain. Leaning forward stops the abdominal muscle suppressing the uterus, thus making the uterus extend over a longer area which facilitates fetal axis pressure leading to an increase of oxytocin. Being in the PSU Cat position means the uterus does not compress the blood vessel in the pelvic area so that the blood can be sent to the uterus without the obstruction of the blood vessel supplying the uterus. When the fetal axis pressure makes flexion of the fetus rapid this leads to easier internal rotation. Gravity then helps the fetus to descend faster. This helps to fix the unstable ilium and sacrum bones in the changing of the sacroiliac ligament, thus reducing labour pain. When the muscles relax for longer periods of time this helps to reduce the labour pains. Intervention for the 5 experimental groups from cervical dilation of 3‐4 cm until cervical dilation of 10 cm or at least 4 h were as follows.
| |
| Outcomes |
NOTE not all raw data were reported, results presented graphically | |
| Notes | Dates of study: not reported Funding: Prince of Songkla University Grant | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Unable to obtain details from study author |
| Blinding of participants and personnel (performance bias) | High risk | The participants and clinicians were not blind |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient reporting |
| Incomplete outcome data (attrition bias) | Low risk | Data were complete |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Other bias | Low risk | There were no differences in baseline characteristics |
| Methods | RCT comparing music to usual care on labour pain | |
| Participants | 161 women attending for antenatal care at the study hospital in Turkey between September 2011 and September 2012. Inclusion criteria: primiparous, aged 18‐35 years, 37‐41 weeks’ gestation, singleton pregnancy with cephalic presentation, expected to have normal birthweight baby and vaginal birth. Exclusion criteria: hypertensive disorders, diabetes, IUGR, PROM, treatment with analgesics or antipsychotic medication, hearing difficulties, chronic pain, severe dysmenorrhoea, fetal death, cardiovascular or other fetal anomaly, inability to understand VAS | |
| Interventions | Intervention: music therapy. 1 of 5 types of music (by choice via headphones) classical music, Turkish art or folk music or Turkish classical music or popular music. The intervention started at 2 cm cervical dilatation, later in labour more rhythmic music was introduced by the midwife, music continued until the end of the third stage Control: used a blank CD | |
| Outcomes | Primary outcome VAS pain score (0‐10 cm); anxiety (VAS), maternal blood pressure, and fetal movements and heart rate | |
| Notes | Waiting on confirmation of study parameters from study authors (contacted 5 June 2017) Dates of study: 2011‐2012 Funding: none | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation sequence |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Women would have known of their group status |
| Blinding of outcome assessment (detection bias) | High risk | Not reported although measurement was by staff providing care |
| Incomplete outcome data (attrition bias) | High risk | 24 women were postrandomisation exclusions. Reasons for exclusion included caesarean section, cervical dilatation > 3 and forgetting their group allocation |
| Selective reporting (reporting bias) | High risk | Discrepency in 2 similar papers describing the power calculation, denominators and outcomes collected |
| Other bias | Unclear risk | Baseline characteristics between groups are similar |
| Methods | Parallel RCT of breathing compared with usual care | |
| Participants | 40 women were recruited from SKK Bakirkoy Hospital, Istanbul, Turkey Inclusion criteria: primiparous, 38‐42 weeks pregnant, at low risk, expecting normal vaginal delivery Exclusion criteria: not stated | |
| Interventions | Intervention: investigators provided information about labour, breathing techniques and massage in the latent phase of labour, and accompanied these women during labour. The women received nurse‐administered massage and were encouraged to perform breathing exercises and self‐administered massage. They were also instructed to change their positions and to relax. Slow, deep inhalations were encouraged in the latent phase and rapid, shallow breathing was encouraged in the active phase. The pant‐blow abdominal breathing technique was applied in the 2nd stage of labour. Plus lower and upper back massages were administered by a nurse. Women were also instructed to give themselves a soft massage in the abdominal area using their fingers. Control: women were monitored routinely in the labour room and did not receive education or supportive nursing care | |
| Outcomes | Pain assessment conducted at 2 cm, 4 cm, 6 cm, 8 cm and 10 cm along a VAS. Behaviour was observed and classified by the study investigator. Postnatal interview 2 h after delivery. | |
| Notes | Dates of study: Recruitment 1 January 2000‐1 September 2000 Funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported and no additional details could be obtained from the study author |
| Allocation concealment (selection bias) | Unclear risk | Not reported and no additional details could be obtained from the study author |
| Blinding of participants and personnel (performance bias) | High risk | Women and care providers were not blind to the intervention |
| Blinding of outcome assessment (detection bias) | High risk | Not described but likely to be high as it is difficult to blind this type of intervention |
| Incomplete outcome data (attrition bias) | Low risk | Not explicitly discussed although data appear complete from all study participants randomised to the trial |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Other bias | Low risk | Slight imbalance in randomisation of gravida at baseline, higher gravida in the control group |
IUGR: intrauterine growth restriction
NRS: numerical rating scale
PROM: premature rupture of membranes
RCT: randomised controlled trial
RAT: respiratory autogenic training
SROM: spontaneous rupture of membranes
STAI: State‐Trait Anxiety Inventory
VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| This study delivered a breathing techniques intervention, with the control group Valsalva maneuver. This is not a relevant comparison for this review. | |
| This study evaluated the role of antenatal education on anxiety and women's emotions during labour and birthing. Publication was by abstract from conference proceedings only and we have not been able to obtain further study details from the authors. | |
| The intervention was a birth ball. This intervention does not meet the criteria for a relaxation technique. | |
| This trial delivered a relaxation intervention for women with anxiety, it was not designed to reduce pain in labour. | |
| In this qualitative study, 11 women attending childbirth education classes volunteered to participate in a study examining the effect of music during labour. The participants were randomly assigned to receive music use and labour support or labour support alone (control group) during labour. The participants selected the music; they were instructed to listen to some music daily during their pregnancy and to play the music during labour. The paper reports on a qualitative analysis of interviews conducted with the participants within 72 hours of delivery. | |
| This trial examined the effect of maternal respiration in labour, and was not relevant to this review. | |
| This relaxation intervention was not designed to reduce pain in labour. | |
| The methods used in this study were not clear. Author correspondence reports that allocation to groups was matched. | |
| Intervention was birth ball; this intervention is not a relaxation technique and does not fit the review’s inclusion criteria. | |
| The music intervention was delivered only at the time of the placement of the epidural. | |
| Intervention in this study was not a relaxation technique. | |
| The comparison group in this study received massage; this comparison does not meet the eligibility criteria. | |
| Not a RCT | |
| Intervention was birth ball; this is not a relaxation technique and does not fit the review’s inclusion criteria. | |
| This paper reported on 2 studies that examined the effects of music on analogued labour pain; the first involving music, the second using a combination of imagery and music. 20 women were included in this study which was undertaken in the USA. This study was not conducted on women during labour and therefore did not meet the inclusion criteria for this review. | |
| The trial evaluates a psychological suggestion therapy intervention rather than a relaxation therapy. | |
| Relaxation was 1 component of an intervention to reduce anxiety and depression and reduce the rate of caesarean section. | |
| The intervention was antenatal exercises. this does not fit review’s inclusion criteria. | |
| Relaxation intervention designed to prolong duration of pregnancy for women in preterm labour. | |
| Massage was used as the control and this comparison does not meet the eligibility criteria. | |
| This intervention not designed to reduce pain and does not meet the inclusion criteria of the review. | |
| This complex intervention was not primarily relaxation focused and will be included in a related review examining massage for pain relief in labour. | |
| Ambulation and birthing ball therapy in first stage of labour do not meet our criteria for the intervention. | |
| The intervention was not designed to reduce pain in labour. The study addressed reducing back pain in pregnancy, preventing urinary incontinence and reducing anxiety. | |
| Intervention was birth ball, this intervention does not fit the review’s inclusion criteria. | |
| In this study the intervention was exercise; this intervention did not meet our inclusion criteria. | |
| This was not a RCT | |
| Not a relaxation intervention | |
| The intervention in this study was not a relaxation technique. | |
| Intervention was birth ball; this intervention is not a relaxation technique and does not fit the review’s inclusion criteria. | |
| Information on methods and outcomes were not clear and clarification could not be obtained from the study author. | |
| Intervention was position in labour and not a relaxation intervention. | |
| There was limited information on methods and we were unable to ascertain from the author details of randomisation and to obtain raw data. | |
| The trial evaluates a psychological suggestion therapy intervention rather than a relaxation therapy. | |
| Intervention was a peanut ball and not a relevant intervention for this review. | |
| This trial randomised 30 women to a non‐music control group and 24 to a music group; it was not clear that the intervention was to reduce pain in labour. | |
| This trial evaluated the role of guided imagery on blood loss during labour and was not designed to reduce pain. | |
| Not a RCT | |
| Not a RCT | |
| Birth ball and not a relevant intervention for this review. | |
| This study evaluated an antenatal education to perform respiration and relaxation techniques during labour. Publication is by abstract from conference proceedings only and we have not been able to obtain further study details from the study authors. | |
| In this study the control group received a massage intervention which is not a relevant comparison for this review. | |
| Stress management course and intervention not used in labour. | |
| Birth ball and not a relevant intervention for this review. | |
| The study was not designed to reduce pain in labour. |
RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Clinical trial comparing antenatal yoga vs usual care on labour pain and delivery outcomes |
| Participants | 60 primiparous women, aged 18‐35 years old presenting to Mirza Koochak Khan hospital in Tehran, Iran from March 2013 to Jun 2014. Inclusion criteria: no serious illness or high‐risk complications during pregnancy and delivery, BMI between 19.8 or 26 respectively, non‐elective caesarean, never having a previous experience with yoga and other exercise such as Pilates or Tai Chi, absence of fetal abnormalities or fetal growth retardation (IUGR) which was confirmed by ultrasonography |
| Interventions | Intervention: yoga. 5 components of yoga practice including yoga asanas, chanting om, breathing awareness, yoga Nidra, Dhyana were taught to women who had not practiced yoga or other exercise such as Pilates or Tai Chi. Participants in the intervention group were asked to perform yoga exercises daily starting at the 26th and continuing until the end of their 37th week of gestation. This consisted of a 60‐min yoga work out a 3 times a week. All experimental participants joined supervised yoga classes provided by a yoga expert to ensure correct form and safety. A booklet and yoga training DVD were provided for each woman containing principles and benefits of each yoga posture, as well as demonstrating the proper technique. Control: routine midwifery care through scheduled hospital visits |
| Outcomes | Labour pain was assessed by the VAS (0 = no pain and 10 = most severe pain woman had experienced). Pain scores were measured in both groups when cervical dilatation researched 3‐4 cm and then 2 h after the first and 2 h after second measurements. Labour outcomes included duration of first, second and third stage, induction, birth mode, analgesia consumption, newborn baby, birth and Apgar scores |
| Notes | Randomisation method unclear ‐ contacted study authors 19 June 2017 to clarify |
| Methods | We have been unable to obtain the thesis. No details available |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes |
| Methods | Reported to be a randomised trial |
| Participants | Nulliparous women in labour |
| Interventions | Physiological delivery versus a complex intervention including aromatherapy, pelvic exercises with ball, back and stomach massage during contraction using Lavandula oil, and an accompanying person in active phase |
| Outcomes | Unclear |
| Notes | Assessment from brief abstract. Attempting to obtain a translation of the study report |
| Methods | Unclear ‐ clinical trial comparing relaxation and meditation versus an unknown control |
| Participants | 90 primiparous women presenting to Fatemah hospital clinic |
| Interventions | Intervention: relaxation and meditation techniques were taught during the third trimester (28‐30 weeks) Control: unclear |
| Outcomes | Pain scores during labour |
| Notes | Awaiting translation ‐ data from English abstract only |
BMI; body mass index
VAS: visual analogue scale
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Effects of relaxation and guided imagery training on pain at childbirth |
| Methods | RCT |
| Participants | Inclusion criteria: 110 primiparous women, who speak Hebrew Exclusion criteria: obstetric complications, planning an elective caesarean section, medical complications (high blood pressure, diabetes), history of mental illness |
| Interventions | Intervention: relaxation using breathing and muscle relaxation and guided imagery (safe place) Control: supportive care |
| Outcomes | Pain intensity, use of epidurals |
| Starting date | August 2009 |
| Contact information | Efrat Esterkin, MA, [email protected] |
| Notes |
| Trial name or title | Breathing exercises for labour pain and duration |
| Methods | RCT |
| Participants | Inclusion criteria: 250 nulliparous women between 37‐42 weeks of gestation Exclusion criteria: analgesic use, clinical instability and psychiatric disorders |
| Interventions | Intervention: breathing exercises at the first stage of labour Control: routine care services |
| Outcomes | VAS to identify perception of pain during the second stage of labour. Duration of the second stage of labour and Apgar scores for newborns |
| Starting date | May 2016 |
| Contact information | Yasemin Cayir, Ataturk University |
| Notes | Study was conducted at Nenehatun Obstetric and Gynecology Hospital between May‐June 2016, in Erzurum, Turkey. Currently not recruiting |
RCT: randomised controlled trial
VAS: visual analogue scale
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.1 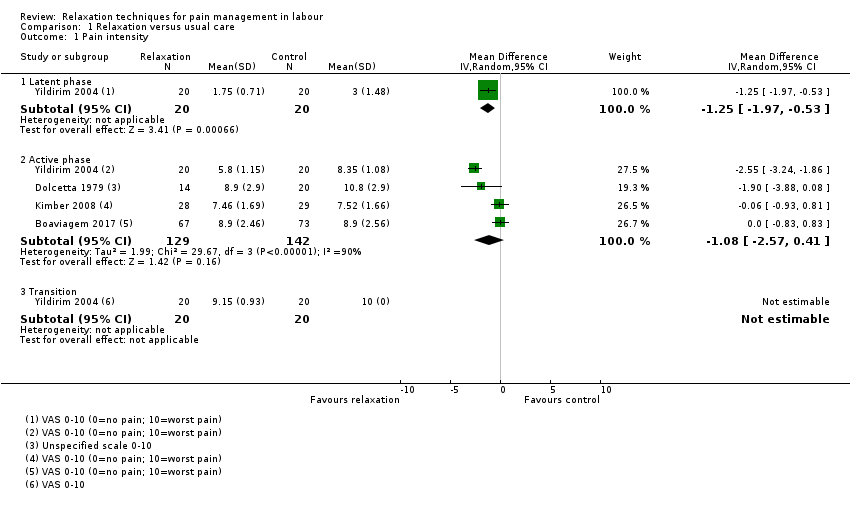 Comparison 1 Relaxation versus usual care, Outcome 1 Pain intensity. | ||||
| 1.1 Latent phase | 1 | 40 | Mean Difference (IV, Random, 95% CI) | ‐1.25 [‐1.97, ‐0.53] |
| 1.2 Active phase | 4 | 271 | Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐2.57, 0.41] |
| 1.3 Transition | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Pain intensity Show forest plot | 1 | 977 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.23, 0.23] |
| Analysis 1.2  Comparison 1 Relaxation versus usual care, Outcome 2 Pain intensity. | ||||
| 3 Satisfaction with pain relief Show forest plot | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.0 [1.10, 58.19] |
| Analysis 1.3 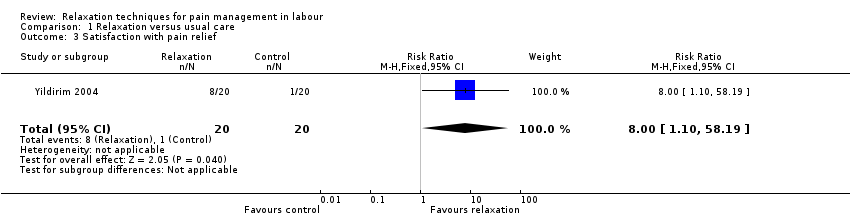 Comparison 1 Relaxation versus usual care, Outcome 3 Satisfaction with pain relief. | ||||
| 4 Satisfaction with childbirth experience Show forest plot | 3 | 1176 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.37, 0.31] |
| Analysis 1.4  Comparison 1 Relaxation versus usual care, Outcome 4 Satisfaction with childbirth experience. | ||||
| 5 Assisted vaginal birth Show forest plot | 4 | 1122 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.20, 1.84] |
| Analysis 1.5  Comparison 1 Relaxation versus usual care, Outcome 5 Assisted vaginal birth. | ||||
| 6 Caesarean section Show forest plot | 4 | 1122 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.26, 2.01] |
| Analysis 1.6 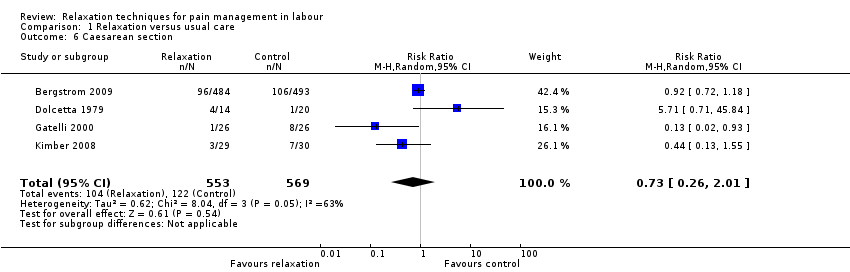 Comparison 1 Relaxation versus usual care, Outcome 6 Caesarean section. | ||||
| 7 Admission to special care nursery Show forest plot | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.07, 15.77] |
| Analysis 1.7  Comparison 1 Relaxation versus usual care, Outcome 7 Admission to special care nursery. | ||||
| 8 Low Apgar score < 7 at 5 minutes Show forest plot | 1 | 34 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.02, 10.69] |
| Analysis 1.8  Comparison 1 Relaxation versus usual care, Outcome 8 Low Apgar score < 7 at 5 minutes. | ||||
| 9 Use of pharmacological pain relief Show forest plot | 2 | 1036 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.88, 1.11] |
| Analysis 1.9  Comparison 1 Relaxation versus usual care, Outcome 9 Use of pharmacological pain relief. | ||||
| 9.1 Epidural | 1 | 977 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.88, 1.13] |
| 9.2 Any additional pharmacological intervention | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.61, 1.28] |
| 10 Length of labour Show forest plot | 3 | 224 | Mean Difference (IV, Random, 95% CI) | 39.30 [‐41.34, 119.93] |
| Analysis 1.10 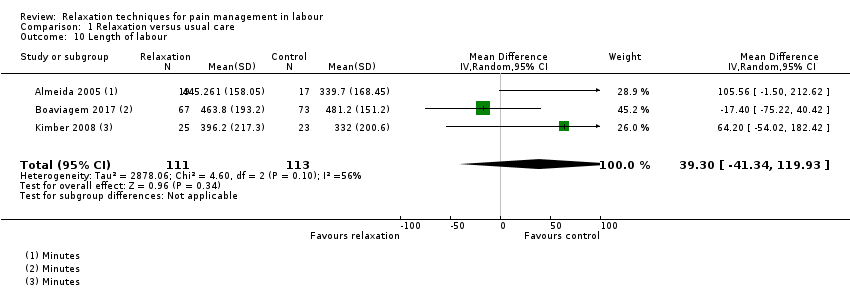 Comparison 1 Relaxation versus usual care, Outcome 10 Length of labour. | ||||
| 11 Need for augmentation with oxytocin Show forest plot | 1 | 34 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.82, 1.59] |
| Analysis 1.11 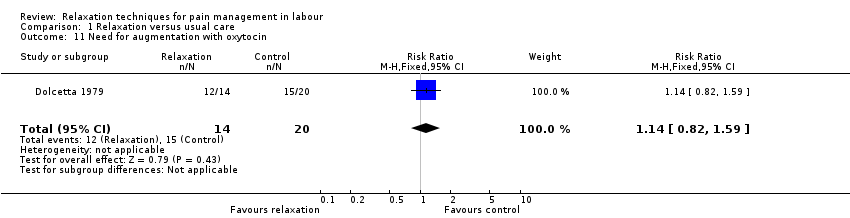 Comparison 1 Relaxation versus usual care, Outcome 11 Need for augmentation with oxytocin. | ||||
| 12 Anxiety Show forest plot | 1 | 140 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐4.15, 4.75] |
| Analysis 1.12  Comparison 1 Relaxation versus usual care, Outcome 12 Anxiety. | ||||
| 13 Non‐prespecified: vitality Show forest plot | 1 | 117 | Mean Difference (IV, Fixed, 95% CI) | 13.10 [10.58, 15.62] |
| Analysis 1.13 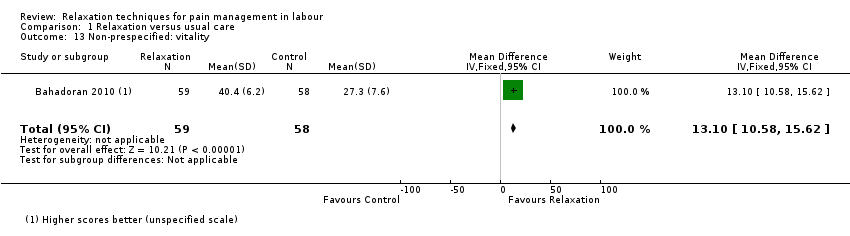 Comparison 1 Relaxation versus usual care, Outcome 13 Non‐prespecified: vitality. | ||||
| 14 Non‐prespecified: fatigue in labour Show forest plot | 1 | 140 | Mean Difference (IV, Fixed, 95% CI) | 0.5 [‐1.44, 2.44] |
| Analysis 1.14  Comparison 1 Relaxation versus usual care, Outcome 14 Non‐prespecified: fatigue in labour. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐6.12 [‐11.77, ‐0.47] |
| Analysis 2.1 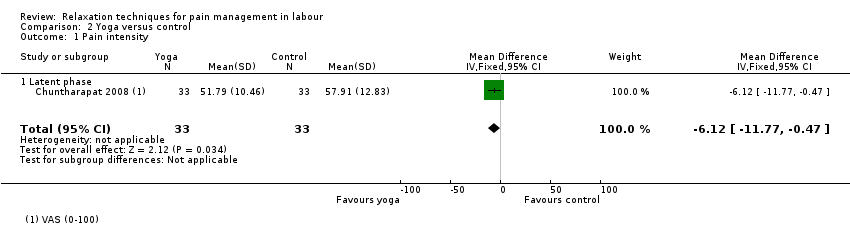 Comparison 2 Yoga versus control, Outcome 1 Pain intensity. | ||||
| 1.1 Latent phase | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐6.12 [‐11.77, ‐0.47] |
| 2 Satisfaction with pain relief Show forest plot | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | 7.88 [1.51, 14.25] |
| Analysis 2.2 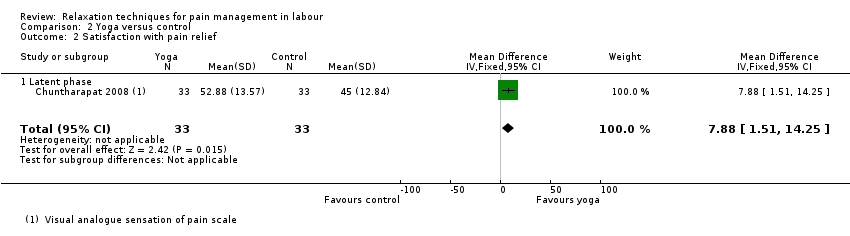 Comparison 2 Yoga versus control, Outcome 2 Satisfaction with pain relief. | ||||
| 2.1 Latent phase | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | 7.88 [1.51, 14.25] |
| 3 Satisfaction with childbirth experience Show forest plot | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | 6.34 [0.26, 12.42] |
| Analysis 2.3  Comparison 2 Yoga versus control, Outcome 3 Satisfaction with childbirth experience. | ||||
| 4 Low Apgar score < 7 at 5 minutes Show forest plot | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 2.4  Comparison 2 Yoga versus control, Outcome 4 Low Apgar score < 7 at 5 minutes. | ||||
| 5 Use of pharmacological pain relief Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.5  Comparison 2 Yoga versus control, Outcome 5 Use of pharmacological pain relief. | ||||
| 5.1 Usual care | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.49, 1.38] |
| 5.2 Supine position | 1 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.01, 0.35] |
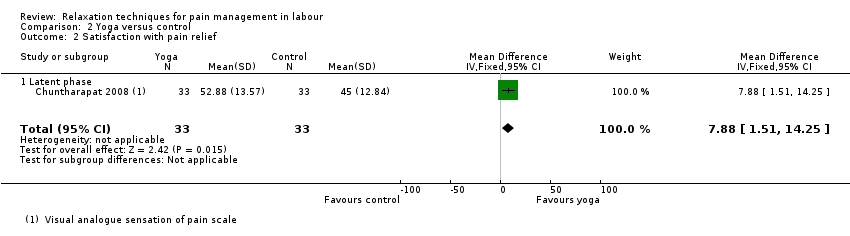
| 6 Length of labour Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.6 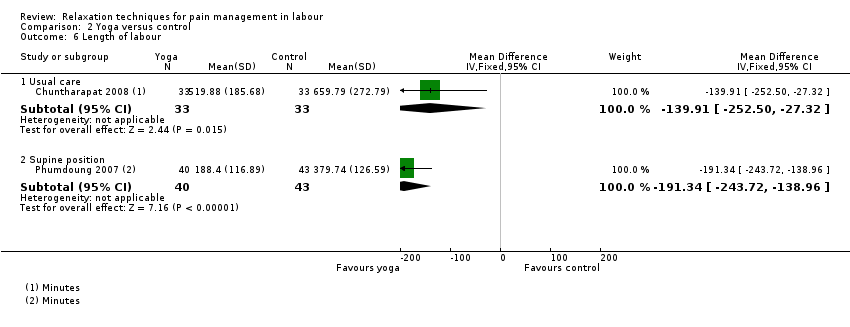 Comparison 2 Yoga versus control, Outcome 6 Length of labour. | ||||
| 6.1 Usual care | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐139.91 [‐252.50, ‐27.32] |
| 6.2 Supine position | 1 | 83 | Mean Difference (IV, Fixed, 95% CI) | ‐191.34 [‐243.72, ‐138.96] |
| 7 Need for augmentation with oxytocin Show forest plot | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.45, 1.31] |
| Analysis 2.7  Comparison 2 Yoga versus control, Outcome 7 Need for augmentation with oxytocin. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
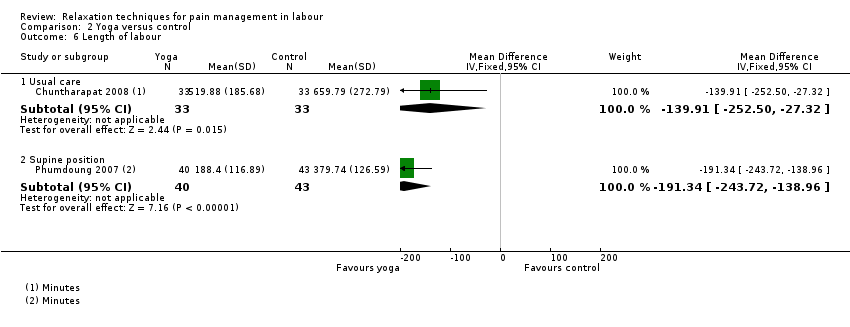
| 1 Pain intensity Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 3.1 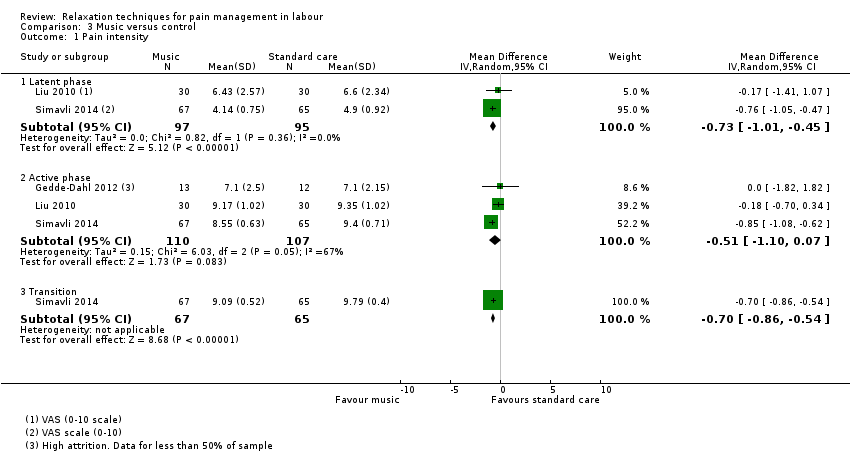 Comparison 3 Music versus control, Outcome 1 Pain intensity. | ||||
| 1.1 Latent phase | 2 | 192 | Mean Difference (IV, Random, 95% CI) | ‐0.73 [‐1.01, ‐0.45] |
| 1.2 Active phase | 3 | 217 | Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐1.10, 0.07] |
| 1.3 Transition | 1 | 132 | Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐0.86, ‐0.54] |
| 2 Assisted vaginal birth Show forest plot | 1 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.08, 2.05] |
| Analysis 3.2  Comparison 3 Music versus control, Outcome 2 Assisted vaginal birth. | ||||
| 3 Caesarean section Show forest plot | 2 | 216 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.36, 1.70] |
| Analysis 3.3  Comparison 3 Music versus control, Outcome 3 Caesarean section. | ||||
| 4 Admission to special care nursery Show forest plot | 1 | 155 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.05, 1.01] |
| Analysis 3.4 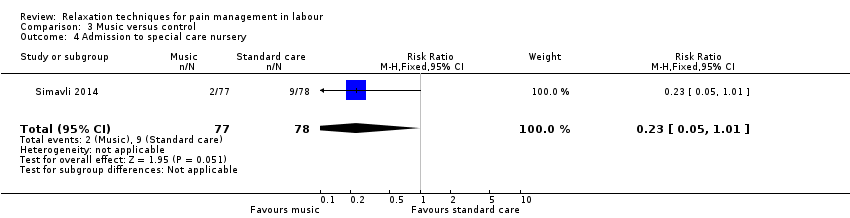 Comparison 3 Music versus control, Outcome 4 Admission to special care nursery. | ||||
| 5 Use of pharmacological pain relief Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.53, 1.32] |
| Analysis 3.5  Comparison 3 Music versus control, Outcome 5 Use of pharmacological pain relief. | ||||
| 6 Length of labour Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐2.60 [‐11.58, 6.38] |
| Analysis 3.6 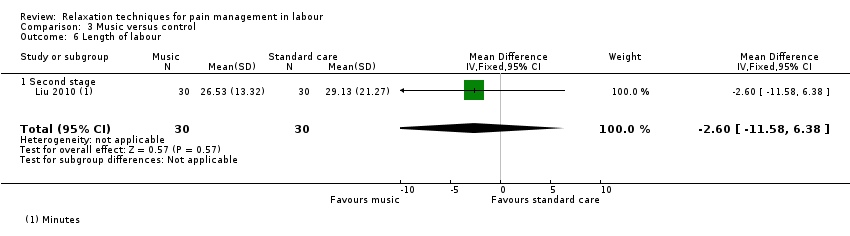 Comparison 3 Music versus control, Outcome 6 Length of labour. | ||||
| 6.1 Second stage | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐2.60 [‐11.58, 6.38] |
| 7 Anxiety Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 3.7  Comparison 3 Music versus control, Outcome 7 Anxiety. | ||||
| 7.1 Latent phase | 2 | 192 | Mean Difference (IV, Random, 95% CI) | 0.08 [‐1.86, 2.02] |
| 7.2 Active phase | 2 | 192 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐1.74, 1.13] |
| 7.3 Transition | 1 | 132 | Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐0.82, ‐0.50] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Satisfaction with pain relief Show forest plot | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.82, 4.89] |
| Analysis 4.1  Comparison 4 Audio‐analgesia versus control, Outcome 1 Satisfaction with pain relief. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Sense of control in labour Show forest plot | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | 31.30 [1.61, 60.99] |
| Analysis 5.1  Comparison 5 Mindfulness training versus usual care, Outcome 1 Sense of control in labour. | ||||
| 2 Satisfaction with childbirth Show forest plot | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | ‐4.5 [‐17.61, 8.61] |
| Analysis 5.2  Comparison 5 Mindfulness training versus usual care, Outcome 2 Satisfaction with childbirth. | ||||
| 3 Assisted vaginal birth Show forest plot | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.01, 7.09] |
| Analysis 5.3  Comparison 5 Mindfulness training versus usual care, Outcome 3 Assisted vaginal birth. | ||||
| 4 Caesarean section Show forest plot | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.15, 5.76] |
| Analysis 5.4  Comparison 5 Mindfulness training versus usual care, Outcome 4 Caesarean section. | ||||
| 5 Need for pharmacological pain relief Show forest plot | 1 | 26 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.20, 1.26] |
| Analysis 5.5 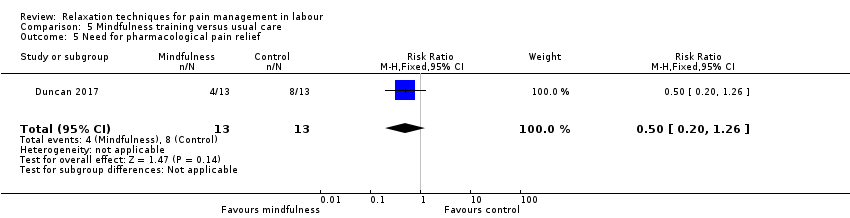 Comparison 5 Mindfulness training versus usual care, Outcome 5 Need for pharmacological pain relief. | ||||

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
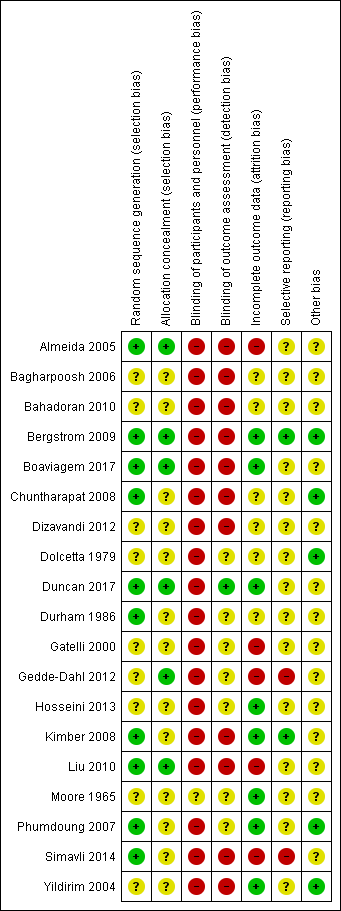
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
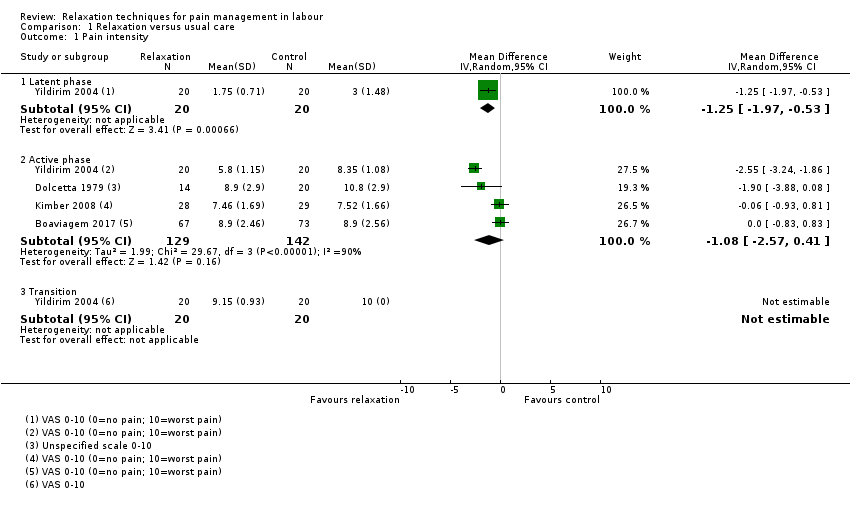
Comparison 1 Relaxation versus usual care, Outcome 1 Pain intensity.

Comparison 1 Relaxation versus usual care, Outcome 2 Pain intensity.
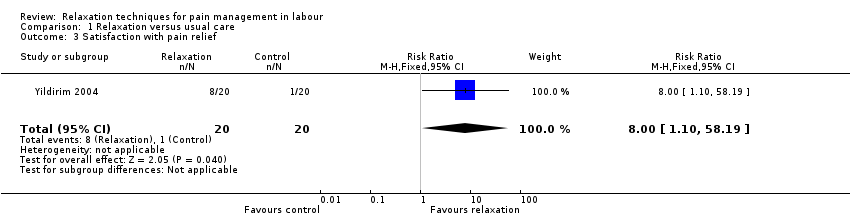
Comparison 1 Relaxation versus usual care, Outcome 3 Satisfaction with pain relief.

Comparison 1 Relaxation versus usual care, Outcome 4 Satisfaction with childbirth experience.

Comparison 1 Relaxation versus usual care, Outcome 5 Assisted vaginal birth.
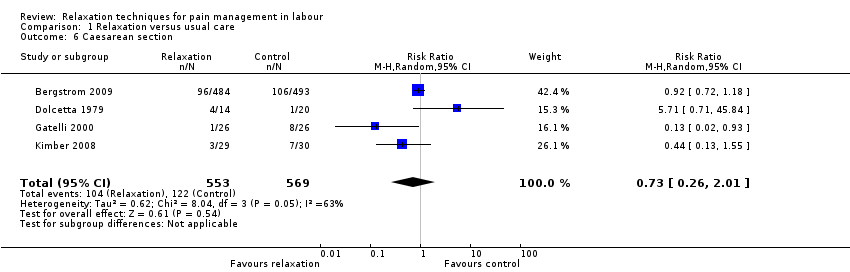
Comparison 1 Relaxation versus usual care, Outcome 6 Caesarean section.

Comparison 1 Relaxation versus usual care, Outcome 7 Admission to special care nursery.

Comparison 1 Relaxation versus usual care, Outcome 8 Low Apgar score < 7 at 5 minutes.

Comparison 1 Relaxation versus usual care, Outcome 9 Use of pharmacological pain relief.
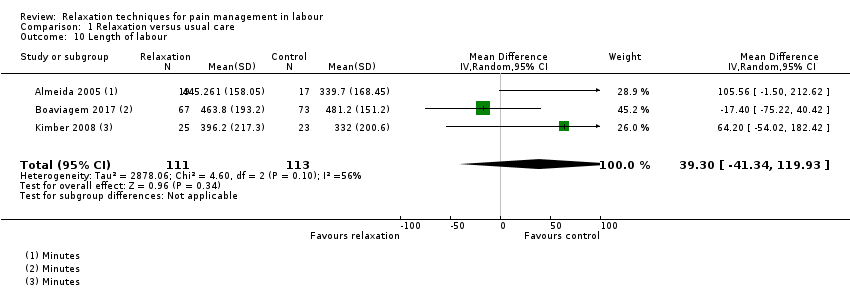
Comparison 1 Relaxation versus usual care, Outcome 10 Length of labour.
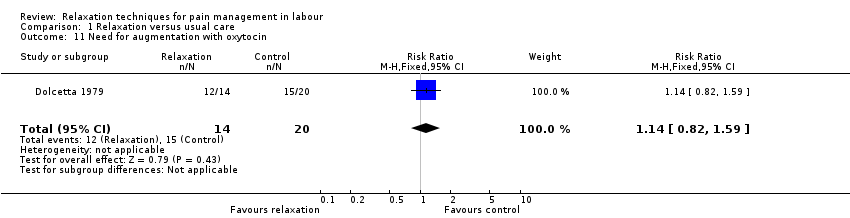
Comparison 1 Relaxation versus usual care, Outcome 11 Need for augmentation with oxytocin.

Comparison 1 Relaxation versus usual care, Outcome 12 Anxiety.
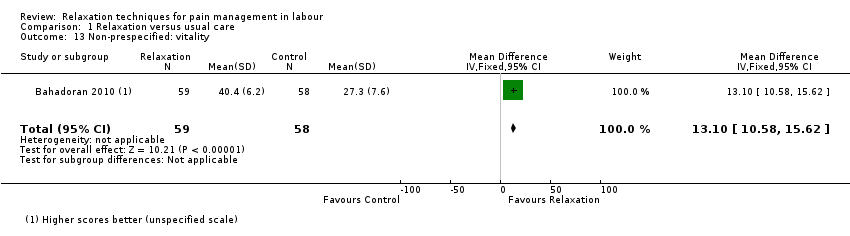
Comparison 1 Relaxation versus usual care, Outcome 13 Non‐prespecified: vitality.

Comparison 1 Relaxation versus usual care, Outcome 14 Non‐prespecified: fatigue in labour.
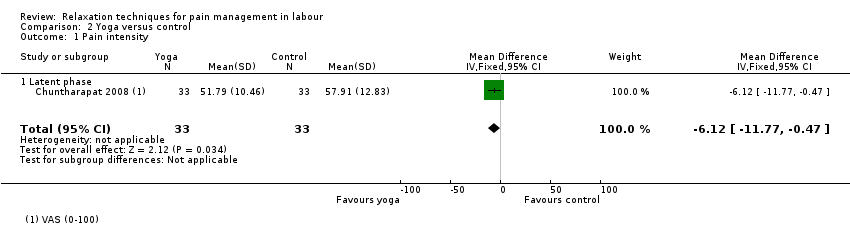
Comparison 2 Yoga versus control, Outcome 1 Pain intensity.
Comparison 2 Yoga versus control, Outcome 2 Satisfaction with pain relief.

Comparison 2 Yoga versus control, Outcome 3 Satisfaction with childbirth experience.

Comparison 2 Yoga versus control, Outcome 4 Low Apgar score < 7 at 5 minutes.

Comparison 2 Yoga versus control, Outcome 5 Use of pharmacological pain relief.
Comparison 2 Yoga versus control, Outcome 6 Length of labour.

Comparison 2 Yoga versus control, Outcome 7 Need for augmentation with oxytocin.
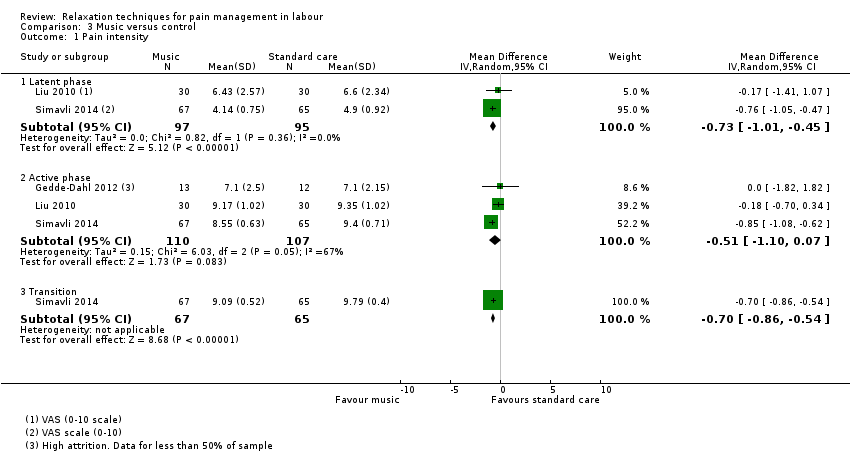
Comparison 3 Music versus control, Outcome 1 Pain intensity.

Comparison 3 Music versus control, Outcome 2 Assisted vaginal birth.

Comparison 3 Music versus control, Outcome 3 Caesarean section.
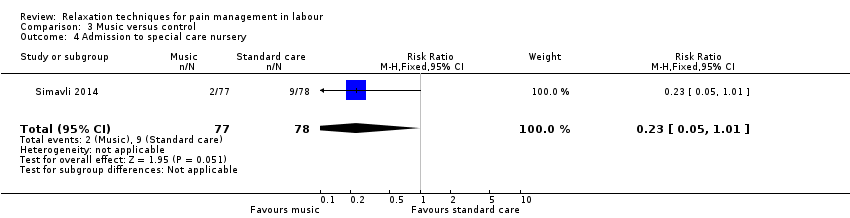
Comparison 3 Music versus control, Outcome 4 Admission to special care nursery.

Comparison 3 Music versus control, Outcome 5 Use of pharmacological pain relief.
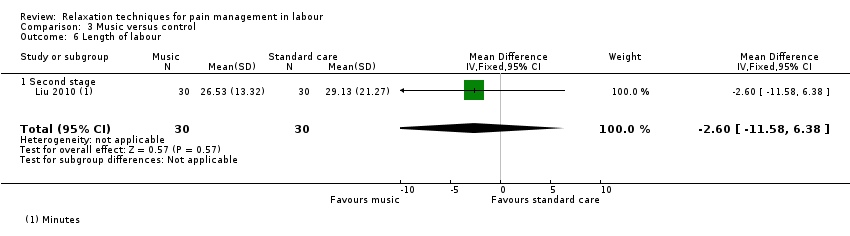
Comparison 3 Music versus control, Outcome 6 Length of labour.

Comparison 3 Music versus control, Outcome 7 Anxiety.

Comparison 4 Audio‐analgesia versus control, Outcome 1 Satisfaction with pain relief.

Comparison 5 Mindfulness training versus usual care, Outcome 1 Sense of control in labour.

Comparison 5 Mindfulness training versus usual care, Outcome 2 Satisfaction with childbirth.

Comparison 5 Mindfulness training versus usual care, Outcome 3 Assisted vaginal birth.

Comparison 5 Mindfulness training versus usual care, Outcome 4 Caesarean section.
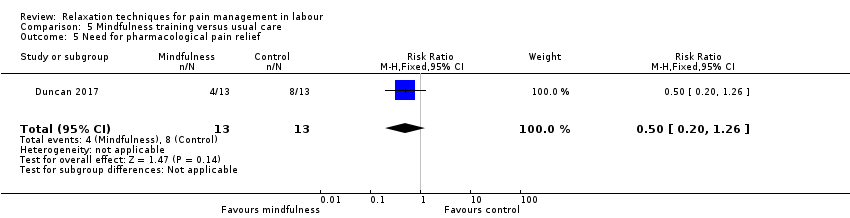
Comparison 5 Mindfulness training versus usual care, Outcome 5 Need for pharmacological pain relief.
| Relaxation compared to usual care for pain management in labour | ||||||
| Patient or population: women in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with usual care | Risk with relaxation | |||||
| Pain intensity: active phase (lower scores indicate less intense pain) | The mean pain intensity ‐ active phase was 7.8 | MD 1.08 lower | ‐ | 271 | ⊕⊝⊝⊝ | |
| Satisfaction with pain relief (higher proportion high satisfaction) | Study population | RR 8.00 | 40 | ⊕⊝⊝⊝ | ||
| 50 per 1000 | 400 per 1000 | |||||
| Sense of control in labour | ‐ | ‐ | ‐ | ‐ | ‐ | No trial reported this outcome |
| Satisfaction with childbirth experience (higher scores indicate more satisfaction) | The mean satisfaction with childbirth experience using a variety of outcome measures was 27.1 | SMD 0.03 lower | ‐ | 1176 | ⊕⊝⊝⊝ | |
| Breastfeeding | ‐ | ‐ | ‐ | ‐ | ‐ | No trial reported this outcome |
| Assisted vaginal birth | Study population | Average RR 0.61 | 1122 | ⊕⊝⊝⊝ | ||
| 149 per 1000 | 91 per 1000 | |||||
| Caesarean section | Study population | Average RR 0.73 | 1122 | ⊕⊝⊝⊝ | ||
| 214 per 1000 | 157 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level: most of the pooled effect provided by studies with high risk of bias in allocation concealment and/or blinding. | ||||||
| Yoga compared to control for pain management in labour | ||||||
| Patient or population: women in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with control | Risk with yoga | |||||
| Pain intensity (lower scores indicate less intense pain) | The mean pain intensity was 57.91 | MD 6.12 lower | ‐ | 66 | ⊕⊕⊝⊝ | |
| Satisfaction with pain relief Higher scores indicate greater satisfaction with pain relief | The mean satisfaction with pain relief was 45 | MD 7.88 higher | ‐ | 66 | ⊕⊕⊝⊝ | |
| Sense of control in labour | ‐ | ‐ | ‐ | ‐ | ‐ | No trial reported this outcome |
| Satisfaction with childbirth experience (higher scores indicate greater satisfaction) | The mean satisfaction with childbirth experience was 150.36 | MD 6.34 higher | ‐ | 66 | ⊕⊕⊝⊝ | |
| Breastfeeding | ‐ | ‐ | ‐ | ‐ | ‐ | No trial reported this outcome |
| Assisted vaginal birth | ‐ | ‐ | ‐ | ‐ | ‐ | No trial reported this outcome |
| Caesarean section | ‐ | ‐ | ‐ | ‐ | ‐ | No trial reported this outcome |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level: high risk of bias in blinding domains. | ||||||
| Music compared to control for pain management in labour | ||||||
| Patient or population: women in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with control | Risk with music | |||||
| Pain intensity ‐ active phase (lower scores indicate less intense pain) | The mean pain intensity ‐ active phase was 8.61 | MD 0.51 lower | ‐ | 217 | ⊕⊝⊝⊝ | |
| Satisfaction with pain relief | ‐ | ‐ | ‐ | ‐ | ‐ | No trial reported this outcome |
| Sense of control in labour | ‐ | ‐ | ‐ | ‐ | ‐ | No trial reported this outcome |
| Satisfaction with childbirth experience | ‐ | ‐ | ‐ | ‐ | ‐ | No trial reported this outcome |
| Breastfeeding | ‐ | ‐ | ‐ | ‐ | ‐ | No trial reported this outcome |
| Assisted vaginal birth | Study population | RR 0.41 | 156 | ⊕⊝⊝⊝ | ||
| 63 per 1000 | 26 per 1000 | |||||
| Caesarean section | Study population | RR 0.78 | 216 | ⊕⊝⊝⊝ | ||
| 119 per 1000 | 93 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded two levels: all included studies had at least two domains with high risk of bias | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Latent phase | 1 | 40 | Mean Difference (IV, Random, 95% CI) | ‐1.25 [‐1.97, ‐0.53] |
| 1.2 Active phase | 4 | 271 | Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐2.57, 0.41] |
| 1.3 Transition | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Pain intensity Show forest plot | 1 | 977 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.23, 0.23] |
| 3 Satisfaction with pain relief Show forest plot | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.0 [1.10, 58.19] |
| 4 Satisfaction with childbirth experience Show forest plot | 3 | 1176 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.37, 0.31] |
| 5 Assisted vaginal birth Show forest plot | 4 | 1122 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.20, 1.84] |
| 6 Caesarean section Show forest plot | 4 | 1122 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.26, 2.01] |
| 7 Admission to special care nursery Show forest plot | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.07, 15.77] |
| 8 Low Apgar score < 7 at 5 minutes Show forest plot | 1 | 34 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.02, 10.69] |
| 9 Use of pharmacological pain relief Show forest plot | 2 | 1036 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.88, 1.11] |
| 9.1 Epidural | 1 | 977 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.88, 1.13] |
| 9.2 Any additional pharmacological intervention | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.61, 1.28] |
| 10 Length of labour Show forest plot | 3 | 224 | Mean Difference (IV, Random, 95% CI) | 39.30 [‐41.34, 119.93] |
| 11 Need for augmentation with oxytocin Show forest plot | 1 | 34 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.82, 1.59] |
| 12 Anxiety Show forest plot | 1 | 140 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐4.15, 4.75] |
| 13 Non‐prespecified: vitality Show forest plot | 1 | 117 | Mean Difference (IV, Fixed, 95% CI) | 13.10 [10.58, 15.62] |
| 14 Non‐prespecified: fatigue in labour Show forest plot | 1 | 140 | Mean Difference (IV, Fixed, 95% CI) | 0.5 [‐1.44, 2.44] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐6.12 [‐11.77, ‐0.47] |
| 1.1 Latent phase | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐6.12 [‐11.77, ‐0.47] |
| 2 Satisfaction with pain relief Show forest plot | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | 7.88 [1.51, 14.25] |
| 2.1 Latent phase | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | 7.88 [1.51, 14.25] |
| 3 Satisfaction with childbirth experience Show forest plot | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | 6.34 [0.26, 12.42] |
| 4 Low Apgar score < 7 at 5 minutes Show forest plot | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Use of pharmacological pain relief Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Usual care | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.49, 1.38] |
| 5.2 Supine position | 1 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.01, 0.35] |
| 6 Length of labour Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Usual care | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐139.91 [‐252.50, ‐27.32] |
| 6.2 Supine position | 1 | 83 | Mean Difference (IV, Fixed, 95% CI) | ‐191.34 [‐243.72, ‐138.96] |
| 7 Need for augmentation with oxytocin Show forest plot | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.45, 1.31] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Latent phase | 2 | 192 | Mean Difference (IV, Random, 95% CI) | ‐0.73 [‐1.01, ‐0.45] |
| 1.2 Active phase | 3 | 217 | Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐1.10, 0.07] |
| 1.3 Transition | 1 | 132 | Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐0.86, ‐0.54] |
| 2 Assisted vaginal birth Show forest plot | 1 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.08, 2.05] |
| 3 Caesarean section Show forest plot | 2 | 216 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.36, 1.70] |
| 4 Admission to special care nursery Show forest plot | 1 | 155 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.05, 1.01] |
| 5 Use of pharmacological pain relief Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.53, 1.32] |
| 6 Length of labour Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐2.60 [‐11.58, 6.38] |
| 6.1 Second stage | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐2.60 [‐11.58, 6.38] |
| 7 Anxiety Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Latent phase | 2 | 192 | Mean Difference (IV, Random, 95% CI) | 0.08 [‐1.86, 2.02] |
| 7.2 Active phase | 2 | 192 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐1.74, 1.13] |
| 7.3 Transition | 1 | 132 | Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐0.82, ‐0.50] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Satisfaction with pain relief Show forest plot | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.82, 4.89] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Sense of control in labour Show forest plot | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | 31.30 [1.61, 60.99] |
| 2 Satisfaction with childbirth Show forest plot | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | ‐4.5 [‐17.61, 8.61] |
| 3 Assisted vaginal birth Show forest plot | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.01, 7.09] |
| 4 Caesarean section Show forest plot | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.15, 5.76] |
| 5 Need for pharmacological pain relief Show forest plot | 1 | 26 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.20, 1.26] |


