Anti‐vascular endothelial growth factor for macular oedema secondary to branch retinal vein occlusion
Information
- DOI:
- https://doi.org/10.1002/14651858.CD009510.pub3Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 07 July 2020see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Eyes and Vision Group
- Copyright:
-
- Copyright © 2020 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
2020 update
Conceiving the review: Cochrane Eyes and Vision
Designing the review: DM, ZS
Co‐ordinating the review: DM, ZS
Data collection for the review:
-
Designing electronic search strategies: Cochrane Eyes and Vision Group editorial base
-
Undertaking manual searches: DM, ZS
-
Screening search results: DM, ZS, OM
-
Organising retrieval of papers: DM, ZS
-
Screening retrieved papers against inclusion criteria: DM, ZS
-
Appraising quality of papers: DM, ZS
-
Extracting data from papers: DM, ZS
-
Writing to authors of papers for additional information: DM, ZS
-
Providing additional data about papers: DM, ZS
-
Obtaining and screening data on unpublished studies: DM, ZS
Data management for the review
-
Entering data into RevMan 5: DM, ZS
-
Checking that data entered into RevMan 5 is correct: DM, ZS
Analysis of data: CB, DM, ZS
-
Interpretation of data
-
-
Providing a methodological perspective: CB, DM
-
Providing a clinical perspective: DM, ZS, OM
-
Providing a policy perspective: CB
-
Writing the review: DM, ZS
Providing general advice on the review: CB, DM, ZS, OM
Sources of support
Internal sources
-
National Institute for Health Research (NIHR), UK
Catey Bunce acknowledges financial support from the Department of Health through the award made by the National Institute for Health Research to Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology for a Specialist Biomedical Research Centre for Ophthalmology. The views expressed in this publication are those of the authors and not necessarily those of the Department of Health.
External sources
-
No sources of support supplied
Declarations of interest
No authors have any financial or proprietary interest in any product mentioned.
Acknowledgements
Cochrane Eyes and Vision (CEV) created and executed the electronic searches. We thank David Charteris and Robin Hamilton for their contributions to a first publication of this review (Mitry 2011). We would like to acknowledge and thank Anupa Shah and Jennifer Evans for their help and assistance throughout the review process. We thank Tasanee Braithwaite, Gianni Virgili and Kristina Lindsley for their comments on the review.
Version history
| Published | Title | Stage | Authors | Version |
| 2020 Jul 07 | Anti‐vascular endothelial growth factor for macular oedema secondary to branch retinal vein occlusion | Review | Zaid Shalchi, Omar Mahroo, Catey Bunce, Danny Mitry | |
| 2013 Jan 31 | Anti‐vascular endothelial growth factor for macular oedema secondary to branch retinal vein occlusion | Review | Danny Mitry, Catey Bunce, David Charteris | |
| 2011 Dec 07 | Anti‐vascular endothelial growth factor for macular oedema secondary to branch retinal vein occlusion | Protocol | Danny Mitry, Catey Bunce, David Charteris | |
Differences between protocol and review
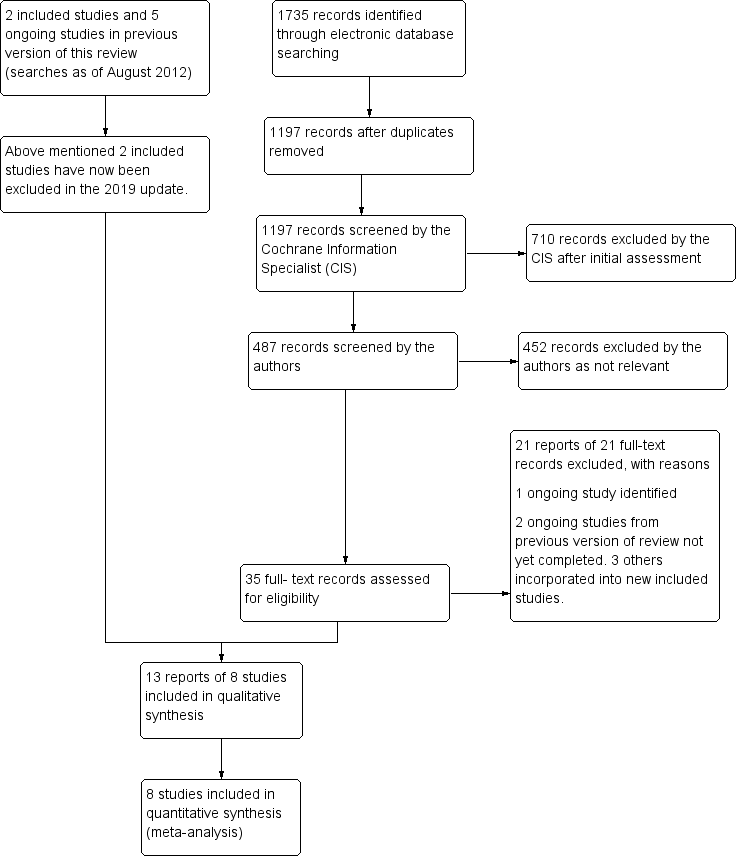
There were no differences between the protocol and this updated 2020 version of the review. In the first version of this review, a paucity of RCTs meant two studies were included that this subsequent update has excluded. Russo 2009, a quasi‐RCT has been excluded as new RCT data from other studies has became available. BRAVO 2010 has now been excluded due to the ability for both the sham and anti‐VEGF arms to receive rescue laser, and this combination therapy is specifically excluded by the protocol.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Angiogenesis Inhibitors [*administration & dosage, adverse effects];
- Antibodies, Monoclonal, Humanized [*administration & dosage, adverse effects];
- Bevacizumab [administration & dosage];
- Intravitreal Injections;
- Laser Coagulation;
- Laser Therapy;
- Macular Edema [*drug therapy, etiology, surgery];
- Randomized Controlled Trials as Topic;
- Ranibizumab [administration & dosage];
- Receptors, Vascular Endothelial Growth Factor [administration & dosage];
- Recombinant Fusion Proteins [administration & dosage];
- Retinal Vein Occlusion [*complications];
- Salvage Therapy [methods];
- Steroids [administration & dosage];
- Vascular Endothelial Growth Factor A [*antagonists & inhibitors];
- Visual Acuity [drug effects];
Medical Subject Headings Check Words
Humans;
PICOs

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
![Forest plot of comparison: 2 Anti‐VEGF v laser, outcome: 2.2 Mean VA change at 6 months [letters].](/cdsr/doi/10.1002/14651858.CD009510.pub3/media/CDSR/CD009510/image_n/nCD009510-FIG-03.svg)
Forest plot of comparison: 2 Anti‐VEGF v laser, outcome: 2.2 Mean VA change at 6 months [letters].

Forest plot of comparison: 2 Anti‐VEGF v laser, outcome: 2.5 APTC events.

Forest plot of comparison: 3 Anti‐VEGF v steroid, outcome: 3.1 Gain of 15 letters or more at 6 months.

Forest plot of comparison: 3 Anti‐VEGF v steroid, outcome: 3.9 Raised IOP.

Comparison 1: Anti‐VEGF v sham, Outcome 1: Gain of 15 letters or more at 6 months

Comparison 1: Anti‐VEGF v sham, Outcome 2: Mean VA change at 6 months

Comparison 1: Anti‐VEGF v sham, Outcome 3: Loss of 15 letters or more at 6 months

Comparison 1: Anti‐VEGF v sham, Outcome 4: Mean CRT change at 6 months

Comparison 1: Anti‐VEGF v sham, Outcome 5: Cataract

Comparison 1: Anti‐VEGF v sham, Outcome 6: Raised IOP

Comparison 1: Anti‐VEGF v sham, Outcome 7: APTC events

Comparison 1: Anti‐VEGF v sham, Outcome 8: Quality of life change

Comparison 2: Anti‐VEGF v laser, Outcome 1: Gain of 15 letters or more at 6 months

Comparison 2: Anti‐VEGF v laser, Outcome 2: Mean VA change at 6 months

Comparison 2: Anti‐VEGF v laser, Outcome 3: Mean CRT change at 6 months

Comparison 2: Anti‐VEGF v laser, Outcome 4: Cataract

Comparison 2: Anti‐VEGF v laser, Outcome 5: APTC events

Comparison 3: Anti‐VEGF v steroid, Outcome 1: Gain of 15 letters or more at 6 months

Comparison 3: Anti‐VEGF v steroid, Outcome 2: Gain of 15 letters or more at 12 months

Comparison 3: Anti‐VEGF v steroid, Outcome 3: Mean VA change at 6 months

Comparison 3: Anti‐VEGF v steroid, Outcome 4: Mean VA change at 12 months

Comparison 3: Anti‐VEGF v steroid, Outcome 5: Mean CRT change at 6 months

Comparison 3: Anti‐VEGF v steroid, Outcome 6: Mean CRT change at 12 months

Comparison 3: Anti‐VEGF v steroid, Outcome 7: Quality of life change at 12 months

Comparison 3: Anti‐VEGF v steroid, Outcome 8: Cataract

Comparison 3: Anti‐VEGF v steroid, Outcome 9: Raised IOP

Comparison 3: Anti‐VEGF v steroid, Outcome 10: APTC events

Comparison 3: Anti‐VEGF v steroid, Outcome 11: Endophthalmitis
| Anti‐VEGF v sham for macular oedema secondary to branch retinal vein occlusion | |||||||
| Patient or population: macular oedema secondary to branch retinal vein occlusion | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | ||
|---|---|---|---|---|---|---|---|
| Risk with sham | Risk with anti‐VEGF | ||||||
| Gain of 15 letters or more of visual acuity at 6 months | 6 months | 269 per 1000 | 462 per 1000 | RR 1.72 | 283 | ⊕⊕⊕ | |
| 12 months | Data not available because participants in sham group received anti‐VEGF after 6 months | ||||||
| Mean change in visual acuity letters at 6 months measured with a logMAR chart (higher letter score is better visual acuity) | 6 months | The mean VA change with sham was 5 letters | The mean number of letters read with anti‐VEGF was 7.50 letters more (5.29 more to 9.71 more) | ‐ | 282 | ⊕⊕⊕ | |
| 12 months | Data not available because participants in sham group received anti‐VEGF after 6 months | ||||||
| Mean central retinal thickness (CRT) change at 6 months in microns (lower value is better) | The mean CRT change with sham was −207 microns | The mean CRT with anti‐VEGF was 57.5 microns less | ‐ | 281 | ⊕⊕⊕ | ||
| Adverse outcomes at any time point | Cataract | 11 per 1000 | 11 per 1000 (1 to 106) | RR 0.98 (0.09 to 10.66) | 283 (1 RCT) | ⊕ | 12 month results. Patients in the sham arm were able to receive rescue anti‐VEGF after 6 months. |
| Raised IOP* | 1 per 1000 | 6 per 1000 (0 to 101) | RR 5.41 (0.30 to 96.88) | 283 (1 RCT) | ⊕ | ||
| APTC events | 22 per 1000 | 32 per 1000 (6 to 142) | RR 1.47 (0.30 to 7.14) | 283 (1 RCT) | ⊕ | ||
| Endophthalmitis | No endophthalmitis was reported in either anti‐VEGF (n = 190) or sham (n = 91) arms | ||||||
| Mean change in quality of life (QoL) at 12 months on the National Eye Institute Visual Functioning Questionnaire‐25 (VFQ‐25) (scored 0 to 100) (higher score is better quality of life) | The mean QoL change with sham was 0 | The mean QoL score with anti‐VEGF was 7.60 higher (4.30 to 10.90) | ‐ | 281 (1 RCT) | ⊕⊕⊕ | Data collected at 6 months because participants in sham group received anti‐VEGF after 6 months | |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). Where no events observed in control group, we have used an estimate of 1 per 1000 for illustrative purposes. | |||||||
| GRADE Working Group grades of evidence | |||||||
| 1Downgraded 1 level for risk of bias 2Downgraded 2 levels for imprecision and 1 level for risk of bias | |||||||
| Anti‐VEGF compared to laser for branch retinal vein occlusion (BRVO) | |||||||
| Patient or population: people with BRVO | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | ||
|---|---|---|---|---|---|---|---|
| Risk with laser | Risk with anti‐VEGF | ||||||
| Gain of 15 letters or more of visual acuity | 6 months | 260 per 1000 | 543 per 1000 | RR 2.09 | 201 | ⊕⊕⊕ | |
| 12 months | Data not available because participants in sham group received anti‐VEGF after 6 months | ||||||
| Mean change in visual acuity letters measured with a logMAR chart (higher letter score is better visual acuity) | 6 months | The mean visual acuity change with laser ranged from 2 to 7 letters | The mean number of letters read with anti‐VEGF was 9.63 letters more | ‐ | 473 | ⊕⊕⊕ | |
| 12 months | Data not available because participants in sham group received anti‐VEGF after 6 months | ||||||
| Mean central retinal thickness (CRT) change at 6 months in microns (lower value is better) | The mean CRT change with laser was −128 microns | The mean CRT change with anti‐VEGF was 147.47 microns less | ‐ | 201 | ⊕⊕⊕ | ||
| Adverse outcomes at any time point | Cataract* | 1 per 1000 | 3 per 1000 (0 to 75) | RR 2.97 (0.12 to 71.89) | 456 (2 RCTs) | ⊕ | |
| Raised IOP* | No raised IOP was reported in either anti‐VEGF (n = 182) or laser (n = 93) groups | ⊕ | |||||
| APTC events | 5 per 1000 | 4 per 1000 (1 to 37) | RR 0.99 (0.15 to 6.78) | 476 (3 RCTs) | ⊕ | ||
| Endophthalmitis | No endophthalmitis was reported in either anti‐VEGF (n = 284) or laser (n = 192) arms | ⊕ | |||||
| Mean change in quality of life at 12 months on the National Eye Institute Visual Functioning Questionnaire‐25 (VFQ‐25) (scored 0 to 100) (higher score is better quality of life) | Not reported | ||||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). Where no events observed in control group, we have used an estimate of 1 per 1000 for illustrative purposes. | |||||||
| GRADE Working Group grades of evidence | |||||||
| 1Downgraded 1 level for risk of bias 2Downgraded 1 level for risk of bias and 2 levels for imprecision | |||||||
| Anti‐VEGF compared to steroid for BRVO | |||||||
| Patient or population: people with BRVO | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | ||
|---|---|---|---|---|---|---|---|
| Risk with steroid | Risk with anti‐VEGF | ||||||
| Gain of 15 letters or more of visual acuity | 6 months | 379 per 1000 | 633 per 1000 | RR 1.67 | 330 | ⊕⊕⊕⊕ | |
| 12 months | 338 per 1000 | 595 per 1000 (460 to 771) | RR 1.76 | 307 | ⊕⊕⊕⊕ | ||
| Mean change in visual acuity letters measured with a logMAR chart (higher letter score is better visual acuity) | 6 months | The mean visual acuity change with steroid ranged from 9 to 11 letters | The mean number of letters read with anti‐VEGF was 8.22 more | ‐ | 330 | ⊕⊕⊕⊕ | |
| 12 months | The mean visual acuity change with steroid ranged from 6 to 8 letters | The mean number of letters read with anti‐VEGF was on average 9.15 letters more (6.32 more to 11.97 more) | ‐ | 343 (2 RCTs) | ⊕⊕⊕⊕ | ||
| Mean central retinal thickness (CRT) change at 12 months in microns (lower value is better) | The mean CRT change with steroid ranged from −249 to −306 microns | The mean CRT change with anti‐VEGF was 26.92 microns less | ‐ | 343 | ⊕⊕⊕ | ||
| Adverse outcomes at any time point | Cataract | 125 per 1000 | 22 per 1000 (7 to 75) | RR 0.12 (0.04 to 0.32) | 551 (3 RCTs) | ⊕⊕⊕ | |
| Raised IOP | 240 per 1000 | 57 per 1000 (34 to 94) | RR 0.25 (0.16 to 0.40) | 673 (4 RCTs) | ⊕⊕⊕ | ||
| APTC events | 1 per 1000 | 3 per 1000 (0 to 74) | RR 3.02 (0.12 to 73.55) | 587 (3 RCTs) | ⊕ | ||
| Endophthalmitis | No endophthalmitis was reported in either anti‐VEGF (n = 187) or steroid (n = 179) arms. | ||||||
| Mean change in quality of life at 12 months on the National Eye Institute Visual Functioning Questionnaire‐25 (VFQ‐25) (scored 0 to 100) (higher score is better quality of life) | The mean change in quality of life score with steroid was 3.5 | The mean change in quality of life score with anti‐VEGF was 3.10 higher | ‐ | 307 | ⊕⊕⊕ | ||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
| 1 One study was judged to be at high risk of attrition bias because participants in the steroid group dropped out of the study due to adverse effects and poor response. We did not downgrade for risk of bias as the direction of the risk of bias is likely to be favouring the steroid group and so the estimate of effect reported here may well be an under‐estimate. 2Downgraded 1 level for risk of bias (studies were at high risk of attrition bias) 3Downgraded 2 levels for imprecision and 1 level for risk of bias | |||||||
| Study name | Number of eyes included | Prospective recruitment | Drug and dose | Mean IVI | Mean f‐up | Outcome |
| 32 eyes | No | Bevacizumab 1.25 mg
| 1.7 | 4 m (median) | Mean BCVA (logMAR) improved from 0.7 to 0.5 and mean CMT improved from 454 µm to 305 µm | |
| 42 eyes (All non‐ischaemic) | No | Bevacizumab 1.25 mg |
| 12 m | Improvement in mean Snellen BCVA from 20/280 to 20/170 at final follow‐up. Mean CMT reduction from 451 µm to 400 µm at 6 mths. | |
| 39 eyes (14 with MO and BRVO) | No | Bevacizumab 1.25 mg | 1.4 | 5.4 m | 50% of patients had previous laser treatment. The mean log‐MAR of the BRVO group was 0.71, and this improved 1 month after the second injection to 0.34. The mean CMT was 468.6 µm which decreased to 186.4 µm at final follow‐up. No significant ocular or systemic SE. | |
| 191 eyes Comparative study: IVB (n = 73) versus IVTA (n = 118) (non‐ischaemic = 90%) | No | Bevacizumab 1.25 mg
| 1.9 | 11.1 m | Mean BCVA (logMAR) improved from 0.91 to 0.45 in the IVB group and mean CMT decreased from 477 µm to 218 µm. | |
| 52 eyes Comparative study: IVTA (n = 17), IVB (n = 14), combined (n = 21) (All non‐ischaemic) | Yes | Bevacizumab 1.25 mg
| 1.6 | 6 m | Mean BCVA (logMAR) improved from 0.92 to 0.45 in the IVB group. No significant ocular or systemic SE. | |
| 83 eyes Comparative study: IVTA (n = 25), IVB (n = 24), no treatment (n = 34) (56% ischaemic) | Yes | Bevacizumab 2.5 mg
| 1 | 41.4 wks | BCVA (logMAR) improved from 0.95 to 0.79 at 12 weeks Mean CMT decreased from 457 µm to 323 µm 24 weeks after treatment | |
| 29 eyes Comparative study: IVTA (n = 16), IVB (n = 13) | No | Bevacizumab 1.25 mg
| 1.6 | 7.4 m | 61.5% of IVB group received previous laser treatment. Improvement in mean BCVA (logMAR) from 0.99 to 0.35 at final follow‐up. Reduction in mean CMT from 538 µm to 222 µm microns. No significant ocular or systemic side effects. | |
| 50 eyes | No | Bevacizumab 1.25 mg
| 1.94 | 7.9 m | 56% gained 5 or more ETDRS letters; 44% had less than 5 ETDRS letter gain or worse final BCVA. No significant ocular or systemic side effects. | |
| 28 eyes | Yes | Bevacizumab 1.25 mg
| 3.7 | 6 m | Improvement in mean BCVA (logMAR) from 0.8 to 0.44 at final follow‐up. Reduction in mean CMT from 486 µm to 268 µm. | |
| 52 eyes (23% ischaemic) | No | Bevacizumab 1.25 mg
| 3.3 | 12 m | Only 17 eyes (26%) returned for follow‐up. The median Snellen BCVA improved from 20/100 at baseline to 20/50 at 12 months. The mean CMT decreased by 205 µm compared with baseline. | |
| 12 eyes (40% ischaemic) | No | Bevacizumab 1.25 mg
| 4 | 9.8 m | Improvement in mean BCVA (logMAR) from 0.91 to 0.48 at final follow‐up. Reduction in mean CMT from 506 µm to 267.5 µm. | |
| 91 eyes | No | Bevacizumab 1.25 mg
| 1.3 | Up to 3 m | Mean reduction in CMT from 610 µm to 368 µm after 1 injection | |
| 61 eyes (34 with BRVO) | Yes | Bevacizumab 2.5 mg | 4.9 | 3 m | Mean BCVA (logMAR) improved from 0.50 to 0.32. Mean CMT decreased from 602 µm to 386 µm. | |
| 34 eyes Comparative study: IVTA (n = 34), IVB (n = 34) | No | Bevacizumab 1.25 mg
| 3.83 | 4.9 m | Mean BCVA improved by 0.14 logMAR units. Mean CMT decreased from 506 µm to 228 µm. | |
| 23 (All non‐ischaemic) | Yes | Bevacizumab 1.25 mg
| 1.6 in first 6 months and 0.8 in second 6 months | 12 m | The median VA gained 3.0 lines from baseline at 48 weeks and there was a decrease of 39% of the median CMT. | |
| 205 eyes | No | Bevacizumab 1.25 mg
|
| 36.8 wks
| The median BCVA (logMAR) was 0.6 at baseline improving to 0.4. Reduction in CMT, from a baseline of 454 µm to 248 µm. | |
| 50 eyes | Yes | Bevacizumab 1.25 mg
| 2 | 12 m | The mean BCVA (logMAR) improved from 0.53 to 0.26. Mean CMT decreased from 523 µm to 305 µm. | |
| 34 eyes | Yes | Bevacizumab 1.25 mg
| 2.9 | 6 m | The mean BCVA (logMAR) improved from 0.79 to 0.51 at 6 months. Mean CMT decreased from 474 µm to 316 µm. | |
| 29 eyes (21 with BRVO) | Yes | Bevacizumab 1.0 mg
| 2.3 | 6 m | Baseline mean BCVA was 50 ETDRS letters, by month 6, BCVA improved to 65 letters. CMT decreased from 558 µm to 382 µm. | |
| 18 eyes with BRVO (All non‐ischaemic) | No | Bevacizumab 1.25 mg
| 2.7 | 12 m | Baseline BCVA was 20/240 (logMAR 1.08) improving to 20/60 (logMAR 0.48) at the end of follow‐up (approx 12 months). The mean CMT decreased to 250 ± 48 µm. | |
| 12 eyes | No | Bevacizumab 1.25 mg
| 1 | 12 wks | Mean BCVA (logMAR) was 1.22 improving to 0.61. The mean CMT was 672.8 µm at baseline. There was a 44.6% decrease in CMT from baseline. | |
| 8 eyes | Yes | Ranibizumab 0.5 mg | 3.6 | 12 m | Mean improvement in BCVA (logMAR) from 0.80 0.41. Mean reduction of 275 µm in CMT from baseline. Contrast sensitivity, time and reading fluency improved significantly in the treated eyes. | |
| 21 eyes (BRVO only) | Yes | Bevacizumab 1 mg
| 8 | 12 m | In the BRVO group (n = 18), visual acuity increased from 55 letters (20/80) at baseline to 73 letters (20/32) at month 12. CMT decreased significantly by 241 μm after 12 months of follow‐up. | |
| 27 eyes | No | Bevacizumab 1.25 mg
| 2 | 5.3 m | Mean BCVA improved from 20/200 to 20/100 at final follow‐up. Mean CMT decreased from 487 µm to 332 µm at final follow‐up. No adverse side effects were observed following injections. | |
| 21 eyes | Yes | Bevacizumab 1.5 mg | 3 | 6.2 m | Mean BCVA (logMAR) improved from 0.81 to 0.55 at 6 months. Mean CMT decreased from 492 µm to 316 µm. | |
| 28 eyes | Yes | Ranibizumab 0.5 mg | 6 | 9 m | Mean BCVA (logMAR) improved from 0.74 to 0.49. Mean CMT decreased from 349 µm at baseline to 229 µm. | |
| 22 eyes (BRVO only) | No | Bevacizumab 2.5 mg | 2.6 | 23 wks | 76.5% of those with BRVO had a significant improved visual acuity (by at least 3 lines). Mean CMT decreased from 678 µm to 236 µm. | |
| 9 eyes | Yes | Bevacizumab 1.25 mg | 1 | 9 wks | Mean BCVA (logMAR) improved from 0.5 to 0.31 at 9 weeks. Mean CMT reduced from 408 µm to 309 µm. | |
| 25 eyes (12 with BRVO only) | Yes | Bevacizumab 2.5 mg | 2 | 6.5 m | 50% (6/12) had received previous treatment. Mean BCVA (logMAR) improved from 0.94 to 0.54 at final follow‐up. Mean CMT reduced from 392 µm to 234 µm. | |
| m: months; wks: weeks; BCVA: best‐corrected visual acuity; CMT: central macular thickness; IVTA: intravitreal triamcinolone; IVB: intravitreal bevacizumab; IVI: intravitreal injections; f‐up: follow‐up; VA: visual acuity | ||||||
| Study | Study details | Conclusion |
| Dose‐finding study: patients with CRVO (n = 14) and BRVO (n = 17) were randomised to receive either 0.3 mg ranibizumab or 0.5 mg ranibizumab and followed for 2 years | The 0.3 mg and 0.5 mg doses had similar results and when combined showed that 20 patients with BRVO had mean and median improvements in BCVA of 16.1 and 15 letters. After 2 years of follow‐up, only 5 of 17 patients with BRVO and 3 of 14 patients with CRVO were oedema‐free with no injections for at least 1 year. | |
| Dose‐finding study: patients with CRVO (n = 20) and BRVO (n = 20) were randomised to receive 3 monthly injections either 0.3 mg ranibizumab or 0.5 mg ranibizumab. | Primary end point at 3 months: improvement of 10 and 18 letters in the BRVO group for the lower and higher doses respectively. OCT showed that compared to lower dose injections, 0.5 mg of ranibizumab tended to cause more rapid reductions of central retinal thickening that lasted longer between injections. | |
| Retrospective study in eyes with CRVO and BRVO, 102 patients (64 in the anti‐VEGF (bevacizumab or ranibizumab) group, 38 in the DEX group) without previous treatment were included in this multi‐centre retrospective study and evaluated at baseline and 1, 3, 6, and 12 months after the onset of treatment. | Both the DEX and anti‐VEGF groups showed similar improvements in visual acuity and central retinal thickness. However, at 3 months, 5 patients (13%) in the DEX group and 20 (31%) in the anti‐VEGF group (P < 0.001) changed treatment due to poor response. | |
| Combination therapy retrospective study in CRVO and BRVO. 48 patients – 40 in the anti‐VEGF DEX sequence (AD group), 8 in the DEX anti‐VEGF sequence (DA group) – were included in this multicentre retrospective study and evaluated at baseline, 1, 3, 6 and 12 months after the switch. | VA significantly improved at 1 month in the AD group (P = 0.03) but not in the DA group (P = 0.40). CMT decreased significantly in the AD group at 1, 6 and 12 months (P = 0.002, P = 0.005 and P = 0.002, respectively). In the DA group, VA did not change from baseline at any time point, and CMT decreased at 1 month (P = 0.02) but not later on. | |
| Participants were randomised 1:1 to receive monthly treatment with bevacizumab or ranibizumab. The primary outcome was change in central foveal thickness at 6 months compared to baseline. | The trial randomised 98 patients to treatment with bevacizumab or ranibizumab. At 6 months, there were no differences in change in central foveal thickness between groups (bevacizumab: mean reduction of 212.6 microns, 95% CI (confidence interval) −288.3 to −137.0; ranibizumab: mean reduction of 243.8 microns, 95% CI, −309.6 to −178.0; P = 0.72, analysis of variance (ANOVA)). Both groups showed similar functional outcomes (bevacizumab: 0.33 logMAR gain, 95% CI, −0.47 to −0.18; ranibizumab: 0.34 log‐ MAR gain, 95% CI, −0.45 to −0.23; P = 0.38, ANOVA). | |
| The COMRADE‐B study was a 6‐month RCT comparing ranibizumab with dexamethasone implant. The extension study followed up a subset of the original study group for a further 6 months. | Patients enrolled in the extension study were limited only to German centres, and in general had better visual acuity outcomes at 6 months than those not enrolled. In the extension 6 months, eyes in the ranibizumab arm could receive ranibizumab as required. Eyes in the dexamethasone arm could receive 1 further dexamethasone implant in the extension 6 month period. 'Mean average change in best‐corrected visual acuity (BCVA) was significantly better for ranibizumab than dexamethasone (P = 0.0249).' Also, "elevated intraocular pressure (IOP) was more frequent with dexamethasone than ranibizumab treatment." | |
| 18 eyes with MO secondary to BRVO (of at least 3 months duration) were randomised to receive either IVB (n = 9) at baseline, month 1 and month 2 or (n = 9) IVB at baseline, month 1 and month 2 with grid laser photocoagulation after the second injection. | Both groups demonstrated a mean improvement in BCVA and CMT at 12 months, however the combination groups required fewer IVB injections; (median of 4 ± 1.1 for IVB alone versus 3 ± 0.4 in the combination group) (P = 0.03). | |
| Non‐randomised case series in CRVO and BRVO. 32 ME cases treated with Ozurdex and 32 ME cases treated with ranibizumab were enrolled, with 26 central (C)RVO and 6 branch (B)RVO participants in each group. The authors compared the results of best‐corrected visual acuity (BCVA), central retinal thickness, number of injections, and intraocular pressure (IOP) at 1, 2, 3, and 6 months after injection. | BCVA in both groups at each follow‐up were significantly increased compared to baseline with no statistical difference between the groups. Ozurdex and ranibizumab successfully reduced CMT at each follow‐up. Both CRVO and BRVO patients had significant between‐group differences in the mean number of injections. Among the CRVO patients, IOP in the Ozurdex group was significantly increased compared to baseline and the ranibizumab group at 1, 2, and 3 months postinjection. | |
| Non‐randomised case series in BRVO. A total of 19 patients (19 eyes) were included in this prospective pilot study. Initially, 8 eyes received three IV bevacizumab (group 1) and 11 received one IV Ozurdex (group 2). All the patients underwent a 1‐, 3‐, 4‐ and 6‐month follow‐up visit. A repeated IV bevacizumab (group 1) or IV Ozurdex (group 2) was proposed at 4 months when necessary. | The mean visual acuity was significantly better 1 month after treatment in group 2, while the mean central macular thickness was also significantly lower in group 2. However, there was no longer any difference between the 2 groups at 3, 4 and 6 months, neither in terms of visual | |
| Non‐randomised combination comparative study in CRVO and BRVO. Fifteen eyes were switched to ranibizumab, 12 to aflibercept, and 10 to dexamethasone. At 3, 6, 9, and 12 months, the outcome measures were visual acuity (VA) and central macular thickness (CMT). | 1 year after the switch, CMT decreased from 430.11 ± 91.21 to 291.86 ± 43.87 μm ( P < 0.001). VA increased in 59.5% of the eyes. No difference between the groups was found in those outcomes at 1 year, but the number of injections varied: 3.30 ± 0.95 for dexamethasone, 6.50 ± 2.11 for aflibercept, and 8.27 ± 2.37 for ranibizumab ( P < 0.001). | |
| Non‐randomised comparative study in BRVO of laser alone or laser with bevacizumab. 19 patients with macular oedema secondary to BRVO were assigned to either the group of 9 patients in combination therapy of laser photocoagulation with intravitreal bevacizumab or the group of 10 patients in the laser photocoagulation therapy. Complete ophthalmologic examinations were performed just before the therapy and at 1 month following the therapy. | Combination therapy of laser photocoagulation and single intravitreal bevacizumab injection resulted in a significantly better visual acuity compared to laser photocoagulation therapy (0.35 versus 0.13 logMAR; P = 0.041) and reduced macular thickness by 120.33 µm versus 71.50 µm (P = 0.277), although this difference was not significant. | |
| In this prospective interventional consecutive case series, previously untreated eyes with perfused MO were enclosed over a period of 16 months for bevacizumab (BEV) and for 29 months for grid laser photocoagulation (GLP). The follow‐up period was 1 year. Patients with persistent MO after 12 months of BEV were offered GLP and vice versa, and were followed up for another 12 months. | Both BEV (23 eyes) and GLP (21 eyes) caused a significant ( P < 0.05) reduction in central retinal thickness (CRT) at 12 months although this was delayed with GLP. However, BEV revealed a significantly better 'best‐corrected visual acuity' (BCVA) compared with GLP (0.2 vs 0.5 logMAR; P < 0.04). Switching therapy for non‐responders revealed a reduced CRT at another 12 months, although this was not significant. | |
| 42 confirmed cases (42 eyes) with macular oedema secondary to BRVO were randomised into 3 groups, each group contained 14 eyes. The ranibizumab group received intravitreal injection of ranibizumab (0.05 mL), the laser group received grid laser photocoagulation, and the combined group received a second therapy of grid laser photocoagulation after 1 wk of the intravitreal injection of ranibizumab. Best‐corrected visual acuity (BCVA) and the central macular thickness (CMT) preoperative and at 1, 3, 6 months after therapy was recorded. | The BCVA and the CMT had no differences among 3 groups pretherapy (P > 0.05). While BCVA was much better and CMT was reduced significantly post‐therapy than pre‐therapy in all 3 groups (P < 0.05). The BCVA and CMT in the ranibizumab group were significantly different in every time point (1, 3, 6 months) (P < 0.05). The BCVA declined and the CMT was thicker as time went on. In the laser group and the combined group, BCVA and CMT had little differences at different time points (P > 0.05); while the BCVA was better and the CMT was thinner in the combined group than ranibizumab group and laser group at every time point (P < 0.05). At 3 and 6 months, the BCVA was better and the CMT was thinner in laser group than ranibizumab group (P < 0.05). | |
| A 25‐health‐state Markov model considering ranges of visual acuity in both eyes was developed. Patients had a confirmed diagnosis of macular oedema secondary to BRVO and had best‐corrected visual acuity (BCVA) at baseline between 25 and 73 letters. The evaluation compared IVT‐AFL 2 mg with ranibizumab 0.5 mg: the frequency of injections and monitoring were identical for both treatments, taken from randomised trials and a physician survey. A systematic review and indirect comparison were conducted to determine the probabilities of gaining at least 15 BCVA letters from baseline to 6 months; BCVA was then extrapolated over time to determine costs and outcomes. Utilities were taken from published literature and costs were estimated from a UK payer perspective. Published drug prices were discounted to reflect patient access schemes. Costs and benefits were discounted at 3.5%. | The indirect comparison found that IVT‐AFL was associated with a small numerical advantage in the likelihood of gaining 15 BCVA letters, compared with ranibizumab (median odds ratio = 1.08, 95% Cl 0.43 to 2.56). IVT‐AFL was associated with a higher number of QALYs (0.045) per patient than ranibizumab. Both treatments are available to the National Health Service under confidential patient access schemes. Cost effectiveness was estimated for a range of possible discounts for each treatment. At price parity, IVT‐AFL reduces cost by GBP 4 per patient and was a dominant therapy. Results were sensitive to the unit cost of the drugs used, to comparative efficacy and number of injections for both treatments. | |
| In this prospective, randomised, non‐inferiority trial, 75 participants with macular oedema due to BRVO received intravitreal injections of ranibizumab (IVR) or bevacizumab (IVB) after 1:1 block randomisation. The primary outcome measure was the difference in mean changes in best‐corrected visual acuity (BCVA) at 6 months. Secondary outcome measures included mean change in central retinal thickness (CRT), the proportion of patients improving by > 15 letters and the proportion of patients developing neovascularisation. | Participants received either IVR (n = 37) or IVB (n = 38). The mean BCVA at baseline was 52.8 ± 14.4 letters (20/80) and 56.1 ± 10.0 letters (20/80) (P = 0.24) in the ranibizumab and bevacizumab groups, respectively. At 6 months, the mean gains in BCVA were +18.1 letters (95% CI +12.8 to +22.6; P < 0.0001) in the ranibizumab group and +15.6 letters (95% CI +12.0 to +20.5; P < 0.0001) in the bevacizumab group. The difference between the mean visual gains of the treated groups (bevacizumab–ranibizumab) was −2.5 letters (95% CI −8.0 to +5.0; P = 0.74). Mean reductions in CRT at 6 months were 177.1 ± 122.3 mm in the ranibizumab group (P < 0.0001) and 201.7 ± 166.2 mm in the bevacizumab group ( P < 0.0001), with no significant difference between the 2 groups (P = 0.48). The mean numbers of ranibizumab and bevacizumab injections were 3.2 ± 1.5 and 3.0 ± 1.4, respectively (P = 0.55). 2 serious adverse events occurred in the ranibizumab group and 1 in the bevacizumab group but both were unrelated to intravitreal injections. | |
| This was a prospective, randomised, interventional comparative study conducted in 45 eyes with ME secondary to BRVO who were treated primarily with IVB 1.25 mg (23 eyes, IVB group) or combination therapy of IVB 1.25 mg with a single simultaneous STA 40 mg (18 eyes, IVB/STA group). Re‐injections were performed with IVB if optical coherence tomography (OCT) showed recurrent ME associated with decreased visual acuity. The main outcome measurement was the number of additional IVB injections, and changes of best‐corrected visual acuity (BCVA) and central macular thickness (CMT) during a 6‐month follow‐up period were compared. | BCVA showed significant improvement in 2 groups at 6 months. In addition, CMT showed significant decrease in 2 groups at 6 months. No significant differences in the change of BCVA and CMT at 6 months after injection (P = 0.973, P = 0.639) were observed between the 2 groups. A statistically significant difference was found regarding the number of additional IVB injections (IVB group 0.96 ± 0.83; IVB/STA group 0.44 ± 0.70, P = 0.034). | |
| 81 eyes with acute (< 3 months) BRVO were randomly assigned to receive either 2 injections of 1.25 mg bevacizumab 6 weeks apart or sham injections. Follow‐up results were reported at 6 weeks and 12 weeks. | After week 6, visual improvements in the bevacizumab treated group were significantly better than the sham group. At 12 weeks there was no significant difference. There was a significant reduction in CMT both at 6 and at 12 weeks. | |
| In this randomised clinical trial, 86 eyes with recent onset (< 12 weeks) CRVO were assigned to 2 groups: bevacizumab (IVB) group (43 eyes) that received 3 monthly injections of 1.25 mg of IVB, and triamcinolone (IVT) group (43 eyes) that received 2 injections of 2 mg IVT 2 months apart. Outcomes were best‐corrected visual acuity (BCVA), central macular thickness (CMT), and intraocular pressure (IOP) changes. | Mean BCVA improved significantly at 6 months in both groups; from 0.87 ± 0.49 to 0.41 ± 0.35 logMAR in IVB group, and from 0.81 ± 0.45 to 0.62 ± 0.48 logMAR in IVT group (P < 0.001). However, between‐group differences reach a significant level at months 4 (P = 0.003) and 6 (P < 0.001) in favour of the IVB group. In terms of CMT reduction, the difference between the groups was statistically significant (P = 0.002) at month 6. Significant differences were noted more in the ischaemic cases in favour of the IVB group. Mean IOP rise was significantly higher in the IVT group at all visits. | |
| A Bayesian network meta‐analysis of RCTs of treatments for macular oedema secondary to BRVO. Interventions: ranibizumab 0.5 mg when necessary, aflibercept 2 mg monthly, dexamethasone 0.7 mg implant, laser photocoagulation, ranibizumab + laser, or sham intervention. Bevacizumab and triamcinolone were excluded. | 8 RCTs were identified for inclusion with 1743 adult patients. The probability of being the most efficacious treatment at month 6 or 12 based on letters gained was 54% for ranibizumab monotherapy, 30% for aflibercept, 16% for ranibizumab plus laser (adjunctive or prompt), and 0% for dexamethasone implant, laser or sham. The probability of being the most efficacious treatment for patients gaining ≥15 letters was 39% for aflibercept, 35% for ranibizumab monotherapy, 24% for ranibizumab plus laser, 2% for dexamethasone implant, and less than 1% for laser or sham. There was no statistical difference between ranibizumab monotherapy and aflibercept for letters gained (+1.4 letters for ranibizumab vs aflibercept with 95% credible interval (CrI) of −5.2 to +8.5 letters) or the OR for gaining ≥15 letters: 1.06 (95% CrI 0.16 to 8.94)). Dexamethasone implant was associated with significantly higher IOP/OH than antivascular endothelial growth factor agents (OR 13.1 (95% CrI 1.7 to 116.9)). | |
| A quasi‐RCT of 30 eyes in 30 patients in a single centre in Italy. 15 eyes received bevacizumab whilst 15 eyes received laser treatment. Follow‐up was for 12 months. | The laser arm showed improvement in VA of 0.21 and 0.20 logMAR at 6 and 12 months, respectively. The bevacizumab arm showed mean VA improvement at 6 and 12 months of 0.30 and 0.31, respectively (P < 0.05). CRT decreased by 42% in the laser arm and 60.3% in the bevacizumab arm at 12 months (P < 0.05). | |
| Participants received monthly injections of 0.5 mg ranibizumab for 7 months and those meeting | There was no significant difference in the slope of change in BCVA between months 7 and 15 in patients treated 'as needed' versus those treated with monthly injections (P = 0.509). Mean (standard deviation) change from baseline BCVA in Early Treatment Diabetic Retinopathy Study letter score at month 15 was 21.0 ± 14.1 in the PRN group (n = 82) versus 18.7 ± 14.1 in the monthly group (n = 80) and 14.5 ± 14.7 in NR participants (n = 13). The percentage of participants who achieved BCVA 20/40 at month 15 was 76.8% in the PRN group, 71.3% in the monthly group, and 46.2% in NR participants. The mean (standard deviation) change from baseline central subfield thickness was 247.8 ± 207.5 mm in the PRN group, 289.9 ± 177.2 mm in the monthly group, and 93.2 ± 225.2 mm in NR participants. There were no significant differences in mean BCVA gains or central subfield thickness reductions at month 15 between the PRN and monthly injection groups (all > 0.05). | |
| A study to investigate whether targeted retinal photocoagulation (TRP) of peripheral non‐perfused areas (NPAs) could prevent the recurrence of macular oedema (ME) due to branch retinal vein occlusion (BRVO) after intravitreal bevacizumab injection (IVB). Eyes received 1.25 mg IVB only (IVB group) or combined with TRP (IVB + TRP group) of NPAs, more than 5 disc areas identified by fluorescein angiography in the patients with ME secondary to BRVO. Best‐corrected visual acuity (BCVA) and central retinal thickness (CRT) determined by optical coherence tomography were measured every month for 6 months. | 38 patients were enrolled and randomised to IVB group (n = 19) and IVB + TRP group (n = 19). Both groups showed similar thinning in CRT at 1 week after IVB. The IVB + TRP group maintained thinner CRT at 2 (P = 0.0072) and 3 (P = 0.0086) months compared with IVB group. However, the difference in CRT became insignificant at 4, 5 and 6 months. The number of reinjections (± standard deviation) in IVB group (1.58 ±0.69) was significantly greater (P = 0.0025) than that in IVB + TRP group (0.83±0.62). BCVA significantly improved at 6 month in IVB + TRP group (P = 0.015), but not in IVB group. | |
| 20 eyes were randomised 3:1 to intravitreous injections of pegaptanib 0.3 or 1 mg at baseline and at weeks 6 and 12 with subsequent injections at 6‐week intervals at investigator discretion until week 48. Principal efficacy outcomes were change from baseline to week 54. | Results were similar in both dosage groups. Mean BCVA improved 14 letters and mean CMT decreased by 205 microns. | |
| 30 eyes of 30 patients with BRVO were randomised into 3 groups: group 1 (10 eyes) received grid laser treatment alone, group 2 received a single dose of intravitreal injection of ranibizumab (0.05 mL/0.5 mg) followed by grid laser treatment 7 days following injection. Group 3 (10 eyes) received 3 loading doses of intravitreal ranibizumab with grid laser treatment 7 days after the first injection. After 6 months follow‐up, the best‐corrected visual acuity and optical coherence tomography (OCT) and central macular thickness were observed. | After 6 months, the visual acuity of patients was improved significantly. There was an average increase of 11 letters, 17 letters and 18 letters in group 1, 2, and 3 respectively, with the average decrease in OCT being 208.7 mum, 312.9 mum and 326.8 mum, respectively, in these groups. Gain in visual acuity more than 3 lines was 1 case (10%) in group 1. There were 3 cases (30%) in group 2 and 4 cases (40%) in group 3. | |
| BCVA: best‐corrected visual acuity; BRVO: branch retinal vein occlusion; CMT: central macular thickness; CRVO: central retinal vein occlusion; IVB: intravitreal bevacizumab; MO: macular oedema; OCT: optical coherence tomography | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Gain of 15 letters or more at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.2 Mean VA change at 6 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.3 Loss of 15 letters or more at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.4 Mean CRT change at 6 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.5 Cataract Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.6 Raised IOP Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.7 APTC events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.8 Quality of life change Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.8.1 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.8.2 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Gain of 15 letters or more at 6 months Show forest plot | 2 | 201 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.09 [1.44, 3.05] |
| 2.2 Mean VA change at 6 months Show forest plot | 3 | 473 | Mean Difference (IV, Fixed, 95% CI) | 9.63 [7.23, 12.03] |
| 2.3 Mean CRT change at 6 months Show forest plot | 2 | 201 | Mean Difference (IV, Fixed, 95% CI) | ‐147.47 [‐200.19, ‐94.75] |
| 2.4 Cataract Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.5 APTC events Show forest plot | 3 | 476 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.15, 6.78] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Gain of 15 letters or more at 6 months Show forest plot | 2 | 330 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [1.33, 2.10] |
| 3.2 Gain of 15 letters or more at 12 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.3 Mean VA change at 6 months Show forest plot | 2 | 330 | Mean Difference (IV, Fixed, 95% CI) | 8.22 [5.69, 10.76] |
| 3.4 Mean VA change at 12 months Show forest plot | 2 | 343 | Mean Difference (IV, Fixed, 95% CI) | 9.15 [6.32, 11.97] |
| 3.5 Mean CRT change at 6 months Show forest plot | 2 | 330 | Mean Difference (IV, Fixed, 95% CI) | ‐66.79 [‐94.69, ‐38.90] |
| 3.6 Mean CRT change at 12 months Show forest plot | 2 | 343 | Mean Difference (IV, Fixed, 95% CI) | ‐26.92 [‐65.88, 12.04] |
| 3.7 Quality of life change at 12 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.8 Cataract Show forest plot | 3 | 637 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.04, 0.32] |
| 3.9 Raised IOP Show forest plot | 4 | 673 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.16, 0.40] |
| 3.10 APTC events Show forest plot | 3 | 587 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.02 [0.12, 73.55] |
| 3.11 Endophthalmitis Show forest plot | 3 | 366 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |