Movimientos pasivos para el tratamiento y la prevención de contracturas
References
References to studies included in this review
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Jump to:
| Methods | Design: within‐subject randomised controlled trial | |
| Participants | Health condition: adults with spinal cord injury Sample size: experimental group: 20 ankles; control group: 20 anklesa Setting: community, Australia Joint of interest: ankle Inclusion criteria: Participants were included if they:
Exclusion criteria: not reported Median age (IQR)
Gender
Study dates: not reported Other: Funding through the University of Sydney's Research and Development Grants Scheme. Conflict of interest not reported | |
| Interventions | Groups included in this review: Experimental group: PMs to one randomly allocated ankle of each participant
Control group: no PMs to the second ankle of the participant
| |
| Outcomes | Outcomes included in this review
Other outcomes
Outcomes testing period
| |
| Notes | aBoth ankles of 20 participants were included (a total of 40 ankles). No dropouts from the study were reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...a computer‐generated random number sequence was created by a person not involved in recruitment to determine allocation schedule" Comment: Authors have explained the procedure |
| Allocation concealment (selection bias) | Low risk | Quote: "...each participant's allocation was placed in a sealed, opaque, sequentially numbered envelope to ensure allocation" Comment: Authors have explained the procedure |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no dropouts |
| Selective reporting (reporting bias) | Low risk | Comment: all prestated outcomes reported |
| Other bias | Low risk | Comment: appears free of other bias |
| Blinding of participants and personnel (performance bias) | Low risk | Comment: not possible to blind participants and personnel; however, this was unlikely to bias the results because participants had paralysis and limited ability to influence outcomes |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "...all assessors were blinded to group allocation" |
| Methods | Design: multi‐centre single‐blinded randomised controlled trial | |
| Participants | Health condition: adults with dementia. Sample size: experimental group: 48a; control group: 54 Setting: nursing home residents, Netherlands Inclusion criteria: Participants were included if they:
Exclusion criteria: Participants were excluded if they:
Median age (range)
Gender
Study dates: Data collection occurred between April 2007 and April 2009 Other: Funding through the Vitalis WoonZorg Groep Eindhoven, the Netherlands. The first author was a part‐time employee at the Vitalis WoonZorg Groep | |
| Interventions | Groups included in this review: Experimental group: PMs to all limbs
Control group: no PMs to limbs
| |
| Outcomes | Outcomes included in this review
Other outcomes
Outcomes testing period Tested at baseline (one day before commencement of treatment), after two weeks and after four weeks (one day after treatment 12) | |
| Notes | a102 participants were randomly assigned, but one dropout was reported. Therefore, data from only 101 participants were included in the analyses (Analysis 2.1 and Analysis 3.1) bIt is not clear how a health condition occurring "during the trial" (so after randomisation) could be part of the exclusion criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...computerized and concealed block randomisation (block size four)" Comment: Authors have explained the procedure |
| Allocation concealment (selection bias) | Low risk | Quote: "The randomisation code was only available to the assigned therapists and was kept secret from all other personnel involved, including the primary investigator" Comment: Authors have explained the procedure, although the fixed block size of four may have enabled those recruiting to guess some participants' allocation if they were aware of this |
| Incomplete outcome data (attrition bias) | Low risk | Comment: one of 48 in the experimental group |
| Selective reporting (reporting bias) | Low risk | Comment: all prestated outcomes reported |
| Other bias | Low risk | Comment: appears free of other bias |
| Blinding of participants and personnel (performance bias) | Low risk | Comment: not possible to blind participants and personnel; however, this was unlikely to bias the results because participants were in the advanced stages of dementia with limited ability to influence outcomes |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "...all assessors were blinded to group allocation" |
Characteristics of excluded studies [ordered by study ID]
Jump to:
| Study | Reason for exclusion |
| Not clear whether PMs were administered to experimental participants | |
| Not a randomised controlled trial | |
| PMs administered through device | |
| PMs administered through device | |
| Systematic review of active interventions | |
| Animal study | |
| Compared active, passive range of motion exercises versus control group; therefore cannot isolate the effects of PMs | |
| No PMs administered | |
| No PMs administered | |
| PMs administered through device | |
| PMs not administered for treatment and prevention of contractures | |
| Compared a neural tension technique versus PMs (PMs were "within a small range of motion" and were administered to have an effect similar to that of placebo) | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Spinal cord injury Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.1  Comparison 1 Joint mobility—short‐term effects, Outcome 1 Spinal cord injury. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Paratonia Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2 Spasticity—short‐term effects, Outcome 1 Paratonia. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Paratonia Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.1  Comparison 3 Pain—short‐term effects, Outcome 1 Paratonia. | ||||
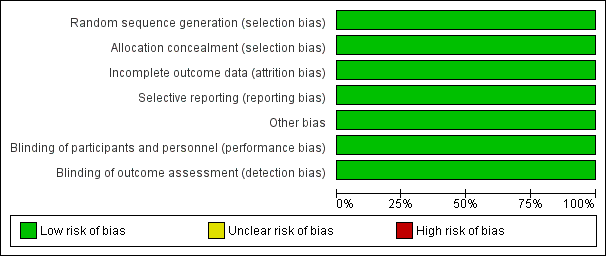
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies. Two studies are included in this review.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Joint mobility—short‐term effects, Outcome 1 Spinal cord injury.

Comparison 2 Spasticity—short‐term effects, Outcome 1 Paratonia.

Comparison 3 Pain—short‐term effects, Outcome 1 Paratonia.
| Short‐term effects on spasticity, pain and joint mobility | ||||||
| Patient or population: patients with or at risk of contractures | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | PMs versus no PMs | |||||
| Spasticity | Data were not pooled | Data were not pooled | Not estimable | 121 | ⊕⊝⊝⊝ | |
| Pain | Mean pain in control groups was | Mean pain in intervention groups was | Not estimable | 101 | ⊕⊝⊝⊝ | |
| Joint mobility | Mean joint mobility in control groups was | Mean joint mobility in intervention groups was | Not estimable | 40 | ⊕⊝⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| 1Consistency had been downgraded by one point because only one trial is included, and therefore the results cannot be consistent across different trials. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Spinal cord injury Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Paratonia Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Paratonia Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |


