Rotación manual profiláctica de la malposición fetal para la reducción del parto quirúrgico
Information
- DOI:
- https://doi.org/10.1002/14651858.CD009298.pub2Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 22 December 2014see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Pregnancy and Childbirth Group
- Copyright:
-
- Copyright © 2014 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
Hala Phipps, Bradley de Vries, Jon Hyett and David Osborn wrote the protocol and review.
Hala Phipps, Bradley de Vries and Professor David Osborn assessed eligibility, study quality and extracted data.
Hala Phips is the guarantor for the review.
Sources of support
Internal sources
-
No sources of support supplied
External sources
-
Australasian Satellite of the Cochrane Neonatal Review Group, Australia.
-
Australasian Cochrane Centre, Australia.
Declarations of interest
David A Osborn: none known.
Dr Bradley de Vries, Hala Phipps and Clinical Professor Jon Hyett were involved in the designing and conducting of the one study (pilot randomised controlled trial) included in this review (Graham 2014). Brad de Vries, Hala Phipps and Jon Hyett have an NHMRC (National Health and Medical Research Council) grant and are currently performing a randomised controlled trial to assess the efficacy of manual rotation for malposition in the second stage of labour for reducing operative delivery. This randomised controlled trial is potentially eligible for inclusion in this review. All decisions relating to the inclusion of this trial, as well as assessment of risk of bias and data extraction, will include a member of the review team (David Osborn) who is not directly involved in the trials.
Acknowledgements
Frances Kellie and Denise Atherton for administrative assistance.
As part of the pre‐publication editorial process, this review was commented on by two peers (an editor and referee who was external to the editorial team), a member of the Pregnancy and Childbirth Group's international panel of consumers and the Group's statistical adviser.
Version history
| Published | Title | Stage | Authors | Version |
| 2014 Dec 22 | Prophylactic manual rotation for fetal malposition to reduce operative delivery | Review | Hala Phipps, Bradley de Vries, Jon Hyett, David A Osborn | |
| 2011 Oct 05 | Prophylactic manual rotation for fetal malposition to reduce operative delivery | Protocol | Hala Phipps, Bradley de Vries, Jon Hyett, David A Osborn | |
Differences between protocol and review
We have updated the methods text for the following sections in accordance with the Cochrane Pregnancy and Childbirth Group's standard methods text.
-
Assessment of reporting biases.
-
Subgroup analysis and investigation of heterogeneity.
We have added the following secondary outcomes that were not prespecified on our published protocol (Phipps 2011).
-
Maternal: Other adverse events.
-
Neonatal and infant: Non‐reassuring or pathological cardiotocograph during procedure.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Adult; Female; Humans; Pregnancy;
PICOs

Comparison 1 Manual rotation versus no manual rotation, Outcome 1 Operative delivery.

Comparison 1 Manual rotation versus no manual rotation, Outcome 2 Maternal mortality.

Comparison 1 Manual rotation versus no manual rotation, Outcome 3 Perinatal mortality.

Comparison 1 Manual rotation versus no manual rotation, Outcome 4 Caesarean section.

Comparison 1 Manual rotation versus no manual rotation, Outcome 5 Forceps delivery.
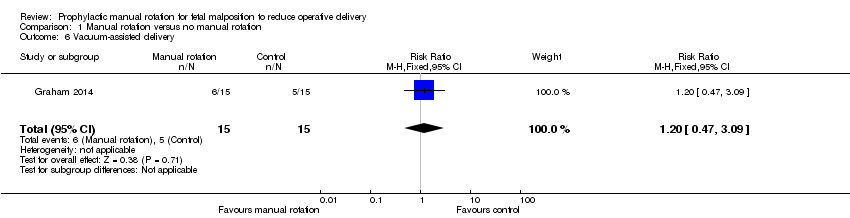
Comparison 1 Manual rotation versus no manual rotation, Outcome 6 Vacuum‐assisted delivery.

Comparison 1 Manual rotation versus no manual rotation, Outcome 7 Third‐ or fourth‐degree perineal trauma.
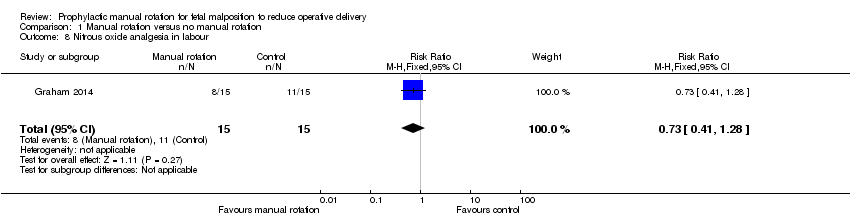
Comparison 1 Manual rotation versus no manual rotation, Outcome 8 Nitrous oxide analgesia in labour.

Comparison 1 Manual rotation versus no manual rotation, Outcome 9 Opiate analgesia in labour.

Comparison 1 Manual rotation versus no manual rotation, Outcome 10 Epidural analgesia in labour.

Comparison 1 Manual rotation versus no manual rotation, Outcome 11 Duration of second stage of labour.

Comparison 1 Manual rotation versus no manual rotation, Outcome 12 Blood loss (mL).

Comparison 1 Manual rotation versus no manual rotation, Outcome 13 Primary postpartum haemorrhage ≥ 500 mL.

Comparison 1 Manual rotation versus no manual rotation, Outcome 14 Maternal blood transfusion.

Comparison 1 Manual rotation versus no manual rotation, Outcome 15 Maternal postnatal infection.

Comparison 1 Manual rotation versus no manual rotation, Outcome 16 Length of maternal hospital stay (days).

Comparison 1 Manual rotation versus no manual rotation, Outcome 17 Non‐reassuring or pathological cardiotocograph during procedure.

Comparison 1 Manual rotation versus no manual rotation, Outcome 18 Non‐reassuring or pathological cardiotocograph at any time after allocation.

Comparison 1 Manual rotation versus no manual rotation, Outcome 19 Cord blood gas acidosis.

Comparison 1 Manual rotation versus no manual rotation, Outcome 20 Admission to neonatal intensive care unit.

Comparison 1 Manual rotation versus no manual rotation, Outcome 21 Neonatal resuscitation (positive pressure ventilation, cardiac compression or drug therapy).

Comparison 1 Manual rotation versus no manual rotation, Outcome 22 Mechanical ventilation (intermittent positive‐pressure ventilation/continuous positive airways pressure after resuscitation).

Comparison 1 Manual rotation versus no manual rotation, Outcome 23 Neonatal jaundice treated with phototherapy.

Comparison 1 Manual rotation versus no manual rotation, Outcome 24 Neonatal exchange transfusion.

Comparison 1 Manual rotation versus no manual rotation, Outcome 25 Polycythaemia treated with partial volume exchange transfusion.
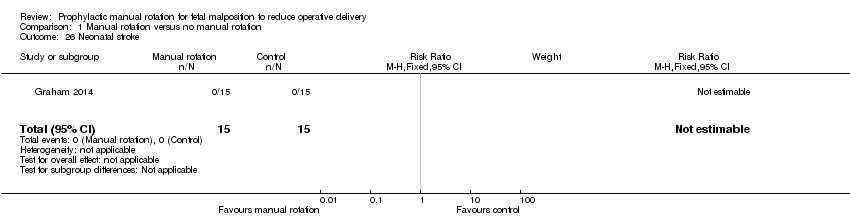
Comparison 1 Manual rotation versus no manual rotation, Outcome 26 Neonatal stroke.

Comparison 1 Manual rotation versus no manual rotation, Outcome 27 Neonatal intracranial bleed.

Comparison 1 Manual rotation versus no manual rotation, Outcome 28 Neonatal fracture.

Comparison 1 Manual rotation versus no manual rotation, Outcome 29 Scalp haematoma (e.g. cephalohaematoma or subgaleal haemorrhage).
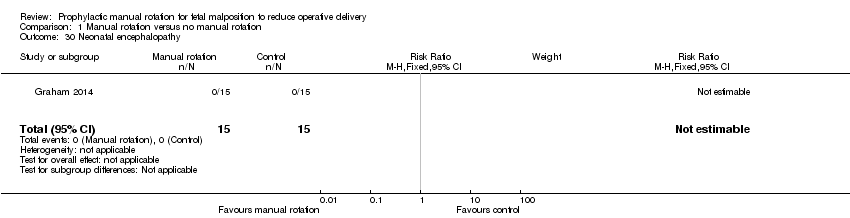
Comparison 1 Manual rotation versus no manual rotation, Outcome 30 Neonatal encephalopathy.

Comparison 1 Manual rotation versus no manual rotation, Outcome 31 Neonatal neuropraxia.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Operative delivery Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.79, 1.49] |
| 2 Maternal mortality Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Perinatal mortality Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Caesarean section Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.36, 4.97] |
| 5 Forceps delivery Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.20, 2.79] |
| 6 Vacuum‐assisted delivery Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.2 [0.47, 3.09] |
| 7 Third‐ or fourth‐degree perineal trauma Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.85] |
| 8 Nitrous oxide analgesia in labour Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.41, 1.28] |
| 9 Opiate analgesia in labour Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.24, 4.18] |
| 10 Epidural analgesia in labour Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.88, 1.55] |
| 11 Duration of second stage of labour Show forest plot | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐5.70 [‐58.34, 46.94] |
| 12 Blood loss (mL) Show forest plot | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 109.30 [‐78.51, 297.11] |
| 13 Primary postpartum haemorrhage ≥ 500 mL Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.24, 4.18] |
| 14 Maternal blood transfusion Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Maternal postnatal infection Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Length of maternal hospital stay (days) Show forest plot | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 0.84 [‐0.04, 1.72] |
| 17 Non‐reassuring or pathological cardiotocograph during procedure Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 68.26] |
| 18 Non‐reassuring or pathological cardiotocograph at any time after allocation Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.21, 1.55] |
| 19 Cord blood gas acidosis Show forest plot | 1 | 23 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.83 [0.19, 17.51] |
| 20 Admission to neonatal intensive care unit Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.61, 6.55] |
| 21 Neonatal resuscitation (positive pressure ventilation, cardiac compression or drug therapy) Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.31, 3.28] |
| 22 Mechanical ventilation (intermittent positive‐pressure ventilation/continuous positive airways pressure after resuscitation) Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.35, 25.68] |
| 23 Neonatal jaundice treated with phototherapy Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.05, 4.94] |
| 24 Neonatal exchange transfusion Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Polycythaemia treated with partial volume exchange transfusion Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 26 Neonatal stroke Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 27 Neonatal intracranial bleed Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 28 Neonatal fracture Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 29 Scalp haematoma (e.g. cephalohaematoma or subgaleal haemorrhage) Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 68.26] |
| 30 Neonatal encephalopathy Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 31 Neonatal neuropraxia Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |


