Intervenciones para optimizar la prescripción para personas de edad avanzada en residencias geriátricas
References
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Jump to:
| Methods | Cluster‐RCT (randomised by nursing home) Total study duration: 14 months | |
| Participants | 1854 residents 33 nursing homes Setting: nursing homes Age: Average 83 years Gender: Intervention 70% female; control 67% female Country: Sweden Date of study: 1994/95 | |
| Interventions | The aim of the regular multidisciplinary meetings was to discuss and improve the use of drugs in nursing homes, and to decrease the use of drugs which, according to the advice of the workshop arranged by the Swedish Medical Products Agency, could cause confusion and impaired memory. In group discussions, the physician, pharmacist, one or more of the nursing home nurses, and in many cases, one or more of the assistant nurses and nurse aides reviewed the drug use of all residents on a monthly basis over a period of one year. The length and frequency of the meetings were adjusted by the participants to local conditions. The therapy changes that were discussed were thus based on the physician’s medical knowledge, the pharmacist’s pharmaceutical knowledge, and the nurses’ and other staff’s knowledge about the patients’ social and functional status.The selected pharmacists were educated prior to and during the intervention period. This education took the form of lectures and workshops, which took place on five occasions, twice before the intervention started and three times during the intervention period, for a total of 65.5 hours. The lectures were given by recognised experts, including clinical pharmacists, geriatricians, gerontologists, nurses and two community pharmacists with experience in nursing home consulting. Topics covered were gerontology/geriatrics (12.5 hours), drug use in the elderly (23.5 hours) and basic training in collaborative methods (18.5 hours). In addition, the pharmacists worked with patient cases in small groups, covering all the areas mentioned above (11 hours). In addition to the formal education, the pharmacists formed regional networks. The networking took place locally, whenever the pharmacist felt a need to have it. In order to make the networks constructive, the whole group was instructed by an educational specialist on one occasion. | |
| Outcomes | Medication‐related problems Not used for this review: Drug use | |
| Notes | Supported by the National Corporation of Swedish Pharmacies and the Swedish Pharmaceutical Society | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Homes were matched in pairs then each randomised to control or intervention. [Attempted to contact author for further information but unsuccessful] |
| Allocation concealment (selection bias) | Low risk | Cluster design |
| Blinding of participants and personnel (performance bias) | High risk | Blinding not conducted |
| Blinding of outcome assessment (detection bias) | High risk | Blinding not conducted |
| Blinding of outcome assessment (detection bias) | Unclear risk | No objective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | Not measured in this study |
| Incomplete outcome data (attrition bias) | Low risk | Medication‐related problems described for residents receiving intervention |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Similar baseline outcome measurements | Unclear risk | Medication‐related problems not measured at baseline |
| Similar baseline characteristics | Low risk | Similar baseline characteristics reported |
| Reliable primary outcome measure | Low risk | Drug use |
| Adequate protection against contamination | Unclear risk | Cluster design. [Attempted to contact author for further information but unsuccessful] |
| Other bias | Low risk | Appears to be free of other sources of bias |
| Methods | Cluster‐RCT (randomised by care facility) Total study duration: 14 months | |
| Participants | 36 facilities (18 intervention, 18 control). 1998 residents (1123 intervention, 875 control) Setting: Residential aged‐care (RAC) facilities Age: mean age not provided. Intervention: < 65, 6.4%; 65 to 74, 11.7%; 75 to 84, 29.5%; 85 to 94, 46.6%; 95 + 5.9%; control < 65, 7.5%; 65 to 74, 11.2%; 75 to 84, 29.1%; 85 to 94, 43.3%; 95 + 8.8% Gender: Intervention male 348 (31.0%), control male 242 (27.7%) Country: New Zealand Date of Study: 2010‐2012 | |
| Interventions | 1. Baseline facility assessment to identify areas of need and facility care plan developed in collaboration with the gerontology nurse specialist (GNS), and RAC facility clinical leadership (anonymised example available from authors on request) 2. Monitoring and benchmarking of resident indicators linked to quality of care provided (falls, nutrition, restraint use, weight loss, urinary tract infections, residents on nine medications); benchmarking was provided on three occasions during the intervention 3. Three 1‐hour multidisciplinary team (MDT) meetings, monthly for the first three months at each facility, including medication review by study geriatrician, GNS, general practitioner (GP), pharmacist, and nurse manager. Typically, six residents were 4. Gerontology education and clinical coaching for RAC nurses and caregivers, including advanced (end‐of‐life) care planning, nutrition/hydration, early detection of illness, falls prevention, end‐stage dementia care, communication with families, and practical aspects of care | |
| Outcomes | Hospital admissions (ambulatory sensitive hospitalisations, total acute admissions) Mortality | |
| Notes | Funded by the Health Research Council of New Zealand | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomised numbers |
| Allocation concealment (selection bias) | Low risk | Cluster design |
| Blinding of participants and personnel (performance bias) | High risk | Blinding not conducted |
| Blinding of outcome assessment (detection bias) | Unclear risk | No subjective outcomes measured |
| Blinding of outcome assessment (detection bias) | Low risk | Authors state that "'care was taken to blind investigators to facility identification wherever possible". However outcomes not likely to be influenced by lack of blinding |
| Incomplete outcome data (attrition bias) | Low risk | Reasons for attrition reported. Described as intention‐to‐treat by authors |
| Incomplete outcome data (attrition bias) | Low risk | Reasons for attrition reported. Described as intention‐to‐treat by authors |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported in the pre‐specified way in the protocol |
| Similar baseline outcome measurements | Low risk | Similar baseline outcome measurements (no baseline measurement of hospital admissions) |
| Similar baseline characteristics | Low risk | Similar baseline characteristics reported |
| Reliable primary outcome measure | Low risk | Hospital admissions |
| Adequate protection against contamination | Unclear risk | Cluster design. However, it was theoretically possible that some healthcare professionals may have moved between intervention and control nursing homes [author contacted] |
| Other bias | High risk | Medication reviews were undertaken for a non‐random subsample of 23% of intervention residents selected by multidisciplinary team |
| Methods | Cluster‐RCT (randomised by care facility) Total study duration: 3 months | |
| Participants | 10 facilities (5 intervention, 5 control). 154 residents (50 intervention, 54 control, 50 within‐facility control) Setting: High‐level residential aged‐care facilities (nursing homes) Age: Intervention mean 85.3, control mean 83.6, within‐facility control mean 84.6 Gender: Intervention male 22 (44%), control male 23 (43%), within‐facility control male 17 (34%) Country: Australia Date of Study: 1999 [Author contacted] | |
| Interventions | Outreach geriatric medication advisory service, case conferencing and medication review. GPs were invited to attend two multidisciplinary case conferences conducted 6 to 12 weeks apart. The resident’s GP, a geriatrician, a pharmacist, residential care staff and a representative of the Alzheimer’s Association of South Australia attended the case conferences, which were held at the facility. Residential care staff expanded on any issues in the case notes that required discussion and the Alzheimer’s Association of South Australia representative discussed non‐pharmacological management of dementia‐related behaviour. Each case conference was chaired by the GP, who used their medical records in addition to case notes from the facility. A problem list was developed by the GP in conjunction with the care staff and a medication review was conducted prior to each case conference. All facilities in the study, including those in the control group, received a half‐day workshop provided by the Alzheimer’s Association of South Australia, which examined the use of a toolkit in the management of challenging behaviours | |
| Outcomes | Measured at baseline and three months post‐intervention: Medication appropriateness (MAI) Drug costs (based on Australian Government Pharmaceutical Benefits Scheme) Not used in this review: Nursing Home Behaviour Problem Scale (NHBPS) Number of drugs | |
| Notes | Funded by The Quality Use of Medicines Evaluation Programme 2000‐2001, Health and Aged Care, General Practice National Innovations Funding Pool 1999‐2000, Health and Aged Care. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers used |
| Allocation concealment (selection bias) | Low risk | A researcher independent to the investigators generated the random sequence and cluster design. Staff were asked to “nominate” 20 residents from intervention sites and 10 residents from control sites. From the 20 intervention,10 were randomised to intervention and ten to within‐facility control using sequential sealed opaque envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding conducted |
| Blinding of outcome assessment (detection bias) | Low risk | Assessed by independent pharmacist blinded to allocation [author contacted] |
| Blinding of outcome assessment (detection bias) | Low risk | No blinding conducted, however outcomes not likely to be influenced by lack of blinding |
| Incomplete outcome data (attrition bias) | Unclear risk | Not measured in this study |
| Incomplete outcome data (attrition bias) | Low risk | Reasons for attrition reported (all due to deaths) and no statistically significant difference found in the proportion of residents lost between groups Described as intention‐to‐treat analysis by authors |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Similar baseline outcome measurements | High risk | There were differences in the Medication Appropriateness Index between groups at baseline: Control 4.1 (95% CI 2.4‐5.7); Within‐facility control 6.0 (95% CI 3.1‐9.0); Intervention 7.4 (95% CI 4.5‐10.3) |
| Similar baseline characteristics | Low risk | Similar baseline characteristics reported |
| Reliable primary outcome measure | Low risk | Medication Appropriateness Index |
| Adequate protection against contamination | Low risk | Cluster design. Randomised by care facility. GPs were checked to avoid contamination between intervention and control residents [author contacted]. No significant differences found between the within‐facility control and the control groups, therefore no evidence of a carry‐over effect of the intervention |
| Other bias | Low risk | Appears to be free of other sources of bias |
| Methods | RCT (randomised by patient) Total study duration: 8 weeks | |
| Participants | 110 patients (56 intervention, 54 control) from three hospitals discharged to 85 long‐term facilities Setting: Long‐term care facilities Age: Mean 82.7, .SD 6.4 Gender: 67 women (60.9%), 43 men (39.1%) Country: Australia Date of study: October 2002 to July 2003 | |
| Interventions | Pharmacist transition co‐ordinator The intervention focused on transferring information on medications to care providers in the long‐term care facilities, including the nursing staff, the family physician and the accredited community pharmacist. On the patient’s discharge from the hospital to the long‐term care facility both the family physician and the community pharmacist were faxed a medication transfer summary compiled by the transition pharmacist and signed by the hospital medical officer. This communication supplemented the usual hospital discharge summary and included specific information on changes to medications that had been made in the hospital and aspects of medication management that required monitoring. After transfer of the patient to the long‐term care facility, the transition pharmacist co‐ordinated an evidence‐based medication review that was to be performed by the community pharmacist contracted to the facility within 10 to 14 days of the transfer. The transition pharmacist also co‐ordinated a case conference involving him or herself, the family physician, the community pharmacist and a registered nurse at the facility within 14 to 28 days of the transfer. At this case conference, the transition pharmacist provided information concerning medication use and appropriateness The usual hospital discharge process received by the control group included a standard hospital discharge summary | |
| Outcomes | Measured at baseline and eight weeks post‐discharge: Adverse drug events (not defined) Hospital admissions (emergency department visits and hospital readmissions) Medication‐related problems Medication appropriateness (MAI) Not used for this review: Falls Worsening mobility Worsening behaviours Increased confusion Worsening pain | |
| Notes | Funded by the Australian Commonwealth Department Of Health and Ageing National Demonstration Hospitals Program. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Study biostatistician provided a computer‐generated allocation sequence using block randomisation |
| Allocation concealment (selection bias) | Low risk | Randomisation was co‐ordinated by a centralised hospital pharmacy service
|
| Blinding of participants and personnel (performance bias) | High risk | No blinding conducted |
| Blinding of outcome assessment (detection bias) | Low risk | Independent pharmacists blinded to allocation assessed Medication Appropriateness Index (MAI) |
| Blinding of outcome assessment (detection bias) | Low risk | No blinding conducted, however outcomes not likely to be influenced by lack of blinding |
| Incomplete outcome data (attrition bias) | Low risk | Similar attrition in both groups with similar reasons for dropouts. Described as intention‐to‐treat by authors |
| Incomplete outcome data (attrition bias) | Low risk | Similar attrition in both groups with similar reasons for dropouts. Described as intention‐to‐treat by authors |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Similar baseline outcome measurements | Low risk | Similar Medication Appropriateness Index scores at baseline. Other outcomes not measured at baseline |
| Similar baseline characteristics | Low risk | Similar baseline characteristics reported except more pre‐admission medications discontinued during hospitalisation in the control group |
| Reliable primary outcome measure | Low risk | Medication Appropriateness Index |
| Adequate protection against contamination | High risk | Randomised by patient therefore contamination possible |
| Other bias | Low risk | Appears to be free of other sources of bias |
| Methods | RCT (randomised by patient) Total study duration: 1 year | |
| Participants | 359 residents (176 control, 183 intervention) Setting: Chronic care geriatric facility Age: Mean 82.7 Gender: Intervention male 29.5%, control male 37.5% Country: Israel Date of Study: Not Stated | |
| Interventions | The intervention consisted of a medication review by the study pharmacist for all residents at study opening and six and 12 months later. The STOPP/START criteria were applied to identify potentially inappropriate prescriptions (PIPs) and potential prescription omissions (PPOs). Interventional recommendations that the study pharmacist made for residents in the intervention group but not in the control group were discussed with the chief physician at study opening and after six months. The chief physician decided whether to accept these recommendations and implement prescribing changes | |
| Outcomes | Measured at baseline and at 12 months: Hospital admissions (not defined) Mortality Quality of life (Medical Outcomes Study 12‐item Short‐Form Health Survey [SF‐12]) Medication‐related problems (number of pharmacist recommendations, acceptance of recommendations by the physician, number of treatment changes) Medication appropriateness (STOPP‐START) Medication costs (Average monthly medication costs in Israeli Shekels) Not used for this review: Falls Functioning (Functional Indepence Measure) | |
| Notes | Study was supported partly by a research grant from Keshet Association for the Elderly in Tel‐Aviv‐Yaffo | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | High risk | Blinding not conducted |
| Blinding of outcome assessment (detection bias) | High risk | Nurses who were unaware of group assignments assessed outcome measures. However, the study pharmacist collected data on outcome measures at follow‐up. |
| Blinding of outcome assessment (detection bias) | Low risk | Nurses who were unaware of group assignments assessed outcome measures. However, the study pharmacist collected data on outcome measures at follow‐up. Outcomes not likely to be influenced by lack of blinding |
| Incomplete outcome data (attrition bias) | Low risk | Reasons and proportions for attrition documented and similar in intervention and control. |
| Incomplete outcome data (attrition bias) | Low risk | Reasons and proportions for attrition documented and similar in intervention and control. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Similar baseline outcome measurements | Low risk | Similar baseline outcomes for falls, hospitalisations and medicine costs |
| Similar baseline characteristics | Low risk | Similar baseline characteristics reported |
| Reliable primary outcome measure | Low risk | Falls and hospitalisations |
| Adequate protection against contamination | High risk | Randomised by patient therefore contamination possible |
| Other bias | Low risk | Appears to be free from other sources of bias |
| Methods | Cluster‐RCT (randomised by care home) Total study duration: 8 months | |
| Participants | 330 residents (172 control, 158 intervention); 14 homes (7 matched pairs) Setting: Nursing homes Age: Control mean 78.9 SD 13.7; intervention mean 83.5 SD 9.2 Gender: Control 115 (67%) females; intervention 125 (79%) females Country: UK Date of study: Not stated | |
| Interventions | Medication review by pharmacist Medication review by the study pharmacist in the GP’s surgery, at the nursing home or (in exceptional circumstances) over the telephone. The pharmacist collected details of current medication for each resident from the medicines administration record chart in the home, together with a brief medical history and any current problems identified by the home staff. Three weeks after the medication review, the homes were revisited, to ascertain whether there had been any immediate problems with the changes in medication and to see if the suggested changes had been implemented | |
| Outcomes | Measured at time 0 (beginning of study), time 1 at four months (beginning of intervention) and at time 2 at eight months (end of intervention): Hospital admissions ("inpatient days") Mortality Medication‐related problems (number of pharmacist recommendations, acceptance of recommendations by the GP, number of treatment changes) Medication costs (not defined, £ sterling) Not used for this review: Mini‐Mental State Examination (MMSE) Geriatric Depression Scale (GDS) Brief Assessment Schedule Depression Cards (BASDEC) Crichton‐Royal Behaviour Rating Scale (CRBRS) Number of drugs per resident Type of drugs Reason for neuroleptic use Use of primary and secondary care resources Number of accidents Falls | |
| Notes | Funded by the North West NHS Executive | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated pseudo random numbers used |
| Allocation concealment (selection bias) | Low risk | Homes were randomised at the start of the start of a four‐month observation phase. Cluster design
|
| Blinding of participants and personnel (performance bias) | High risk | No blinding described |
| Blinding of outcome assessment (detection bias) | High risk | No blinding conducted |
| Blinding of outcome assessment (detection bias) | Low risk | No blinding conducted, however outcomes not likely to be influenced by lack of blinding |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Similar baseline outcome measurements | High risk | 14 (8.1%) deaths in control group versus 22 (13.9%) deaths in intervention group at baseline. No baseline measurements of other primary outcomes of this review |
| Similar baseline characteristics | High risk | Slightly fewer residents in the intervention group (158) versus control (172). In the control group, residents were younger (mean 78.9 SD 13.7 versus mean 83.5 SD 9.2) and there were fewer females (67% versus 79%) |
| Reliable primary outcome measure | Low risk | Crichton‐Royal Behaviour Rating Scale |
| Adequate protection against contamination | Low risk | Randomised by care home (which were in different geographical areas) |
| Other bias | Low risk | Appears to be free of other sources of bias |
| Methods | Cluster‐RCT (randomised by nursing home) Total study duration: 6 months | |
| Participants | Control group: 17 nursing homes and 29 doctors (372 participants). Intervention Group: 19 nursing homes and 30 doctors (344 participants) Setting: Nursing homes Age: Control mean 84.5 SD 10.4 ; intervention 84.24 mean SD 14.6 Gender: Control 72.1% female; intervention 74.0% female Country: Spain Date of study: February 2010 to February 2013 | |
| Interventions | Educational intervention delivered to 30 doctors Nursing home physician expert in drug use in older people delivered a structured educational intervention. The educational intervention included information on general aspects of prescription and drug use in geriatric patients, how to reduce the number of drugs and to perform regular reviews of medications, to avoid inappropriate drug use, to discontinue drugs that do not show benefit and to avoid under‐treatment with drugs that have shown benefit. Information also provided on adverse drug reactions in older people Educational material and references also provided to participants Educator also provided on‐demand prescription advice (via phone) for a six‐month period | |
| Outcomes | Measured at baseline and at nine months. Hospital admissions (total number of days spent in hospital) Medication appropriateness (STOPP‐START) Not used in this review: Falls Delirium Physician and nurse visit Emergency room visits Use of antipsychotics Use of delirium drugs | |
| Notes | Funded by the Ballesol group [author contacted] | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables |
| Allocation concealment (selection bias) | Low risk | Cluster design |
| Blinding of participants and personnel (performance bias) | High risk | Blinding not conducted |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Outcomes not likely to be influenced by lack of blinding |
| Incomplete outcome data (attrition bias) | Unclear risk | Per protocol analysis used. Dropouts were not identified by group |
| Incomplete outcome data (attrition bias) | Unclear risk | Per protocol analysis used. Dropouts were not identified by group |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Similar baseline outcome measurements | Low risk | Similar baseline outcome measurements for days in hospital and medication appropriateness |
| Similar baseline characteristics | Low risk | Similar baseline characteristics reported except worse functional status in intervention group; however, adjusting for this did not significantly change the results |
| Reliable primary outcome measure | Low risk | Objective measures of healthcare utilisation |
| Adequate protection against contamination | Unclear risk | Cluster design. However, it was theoretically possible that some physicians may have moved between intervention and control nursing homes [author contacted] |
| Other bias | Unclear risk | For prescribing appropriateness, a random sample of 311 from 1018 residents was used |
| Methods | Cluster‐RCT (randomised by care unit within two long‐term care facilities) Total study duration: 12 months | |
| Participants | 1,118 resident in 29 units in two long‐term care facilities Setting: Long‐term care facilities Age: Average 87.2 years Gender: 71.3% female Country: US and Canada Date of study: 2006‐7 [Author contacted] | |
| Interventions | Computerised provider order entry with clinical decision support. A team of geriatricians, pharmacists, health services researchers and information system specialists designed the clinical decision support system. The team reviewed the types of preventable adverse drug events based on previous research and widely accepted published criteria for suboptimal prescribing in elderly people available at the time of this study. All serious drug–drug interactions from a standard pharmaceutical drug interaction database were also reviewed and alerts were included for a limited number of more than 600 potentially serious interactions that were reviewed. For residents on the intervention units, the alerts were displayed in a pop‐up box to prescribers in real time when a drug order was entered. The pop‐up boxes were informational; they did not require specific actions from the prescriber and did not produce or revise orders automatically. On the control units, the alerts were not displayed to the prescribers | |
| Outcomes | Measured throughout study period (resident‐months): Adverse drug event (“an injury resulting from the use of a drug” includes medication error and adverse drug reaction) Severity of adverse drug event Preventability of adverse drug event | |
| Notes | Supported by the Agency for Healthcare Research and Quality. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation used. Within each block, units were randomly assigned using the random function in Microsoft Excel®. [Author contacted] |
| Allocation concealment (selection bias) | Low risk | Cluster design |
| Blinding of participants and personnel (performance bias) | High risk | Not conducted |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors were blind to allocation
|
| Blinding of outcome assessment (detection bias) | Unclear risk | No objective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Not measured in this study |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Similar baseline outcome measurements | Unclear risk | No baseline measurements of adverse drug effects |
| Similar baseline characteristics | Unclear risk | Baseline characteristics not reported, however, units were matched for bed size and general characteristics of residents and the unit |
| Reliable primary outcome measure | Low risk | Number of adverse drug events |
| Adequate protection against contamination | High risk | Cluster design. Efforts were made to limit crossover of prescribers between intervention and control units, however, some prescribers worked simultaneously on both intervention and control units. In an effort to assess the possibility that this may have led to changes in behaviour in the control group, the rate of responses to "unseen" alerts in the control units during the first versus the last quarter of the study was assessed at one of the study sites. The rate of response was lower in the last quarter, suggesting that prescribers did not adopt new habits due to seeing alerts on intervention units |
| Other bias | Low risk | Appears to be free of other sources of bias |
| Methods | Cluster‐RCT (randomised by ward) Total duration of study: 12 months | |
| Participants | 227 residents in 20 facilities (10 control, 10 intervention) Setting: Assisted living facilities Age: Control mean 83.5 SD 6.9; intervention mean 82.9 years SD 7.5 Gender: Control 77.1% female; intervention 65.3% female Country: Finland Date of Study: Not stated | |
| Interventions | Educational intervention: Two 4‐hour training sessions for nursing staff. Aim of session was to enable nurses to recognise harmful medications and corresponding adverse drug events. First 4‐hour session: lecture‐based, allowed participants to discuss medication‐related problems experienced by their own residents, introduced lists of harmful medications and suitable treatments. Also involved discussion about medication use for residents with real impairment and drug‐drug interactions Second 4‐hour session: case‐study‐based, demonstrate relevance and importance of topic to nurses During both training sessions nurses were encouraged to reflect on their own procedure and opportunities for improvement Those nurses that received this intervention were asked to identify potential medication‐related problem and highlight these to the consulting physician | |
| Outcomes | Assessed at 0, 6, 12 months Hospital admissions (hospital days) Mortality Health‐related Quality of Life (15D) Medication appropriateness (composite of Beers criteria, Anticholinergic Risk Scale, > 2 psychotropic medications, NSAIDs and proton pump inhibitors) Not used in this review: Cognitive assessment (MMSE) Nutritional assessment (Mini‐nutritional assessment) | |
| Notes | [author contacted] | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random number generator |
| Allocation concealment (selection bias) | Low risk | Cluster design |
| Blinding of participants and personnel (performance bias) | High risk | Blinding not conducted |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Low risk | Outcomes not likely to be influenced by lack of blinding |
| Incomplete outcome data (attrition bias) | Unclear risk | Reasons and proportions for attrition documented and similar in intervention and control. Described as intention‐to‐treat analysis by authors Overall attrition rate relatively high (27.8%) |
| Incomplete outcome data (attrition bias) | Unclear risk | Reasons and proportions for attrition documented and similar in intervention and control. Described as modified intention‐to‐treat analysis by authors Overall attrition rate relatively high (27.8%) |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Similar baseline outcome measurements | Unclear risk | Lower HRQoL in intervention group (15D score mean 0.61 [SD 0.12] vs 0.66 [0.11]) and higher mean number of harmful medications (2.9 [SD 1.8] vs 2.5 [SD 1.7]). Analyses were adjusted for these differences |
| Similar baseline characteristics | Unclear risk | More males (34.7% vs 22.9%), higher prevalence of ‘as‐needed’ medication (mean 3.6 [SD 2.3] vs 2.9 [SD2.0]), and higher number of comorbidities (Mean Charlson’s index 3.2 [2.0] vs 2.5 [1.8]) in intervention group. Analyses were adjusted for these differences |
| Reliable primary outcome measure | Low risk | Well‐defined potentially harmful medication use |
| Adequate protection against contamination | Unclear risk | Cluster design. However, it was theoretically possible that some nurses may have moved between intervention and control nursing homes, although this was deemed unlikely by the author [author contacted] |
| Other bias | Low risk | Appears to be free from other sources of bias |
| Methods | Cluster‐RCT (randomised by care home) Total study duration: Two years | |
| Participants | 3230 residents (905 intervention, 13 homes); 2325 control, 39 homes) Setting: Nursing homes Age: Intervention < 60 2.0%, 60‐69 6.6%, 70‐79 21.9%, 80‐89 47.4%, 90‐99 20.7%, ≥ 100 1.7% Control < 60 2.6%, 60‐69 5.4%, 70‐79 22.3%, 80‐89 46.7%, 90‐99 21.1%, ≥ 100 1.6% Gender: Not reported Country: Australia Date of Study: Not reported | |
| Interventions | Three‐phase intervention: introducing a new professional role to stakeholders with relationship‐building; nurse education; and medication review by pharmacists The clinical pharmacy service model introduced to each nursing home was supported with activities such as focus groups facilitated by a research nurse, written and telephone communication, and face‐to‐face professional contact between nursing home staff and clinical pharmacists on issues such as drug policy and specific resident problems, together with education and medication review by pharmacists holding a postgraduate diploma in clinical pharmacy. This was a multifaceted intervention directly targeting nursing homes. Most of the contact with GPs was indirect, using the existing relationships between nursing homes and visiting GPs. A number of focus groups and personal interviews about the project were conducted with GPs. In intervention homes, problem‐based education sessions (6 ± 9 seminars totaling approximately 11 h per home) were provided to nurses. Sessions addressed basic geriatric pharmacology and some common problems in long‐term care (depression, delirium and dementia, incontinence, falls, sleep disorders, constipation and pain). Sessions were supported by wall charts, bulletins, telephone calls and clinical pharmacy visits, averaging 26 h contact per home over the study. Written, referenced drug regimen reviews were prepared by the clinical pharmacists for 500 individual residents selected by the nursing home staff. The reviews highlighted the potential for: (1) adverse drug effects, (2) ceasing one or more drugs, (3) adding drugs, (4) better use of specific drug therapy, particularly psychoactive drugs, (5) non drug interventions, and (6) adverse effect and drug response monitoring. Initial reports (61% of total) were audited by a geriatrician before dissemination. Reports were placed in each resident's nursing home records, made available to the resident's GP and discussed with nursing staff. Drugs commonly targeted in reviews and education sessions included laxatives, histamine H2‐receptor antagonists, allopurinol, quinine, antibacterials, paracetamol, nonsteroidal anti‐inflammatory drugs (NSAIDs) and psychoactive drugs | |
| Outcomes | Measured at baseline and 12 months post‐intervention: Hospital admissions (not defined) Mortality (survival also assessed at 22 months) Medication‐related problems Medication costs (per resident per year based on prescription claims data) Not used for this review: Adverse events (from incident reports) Resident Classification Instrument (RCI) Drug use | |
| Notes | Supported by the Commonwealth Government of Australia under the Pharmaceutical Education Program | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Homes were assigned to intervention or control by being “drawn from a hat” |
| Allocation concealment (selection bias) | Low risk | Cluster design |
| Blinding of participants and personnel (performance bias) | High risk | No blinding conducted |
| Blinding of outcome assessment (detection bias) | High risk | No blinding reported |
| Blinding of outcome assessment (detection bias) | Low risk | No blinding reported, however outcomes not likely to be influenced by lack of blinding |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Similar baseline outcome measurements | Low risk | Slight imbalance in mortality and hospitalisations at baseline; however this was accounted for in the analysis |
| Similar baseline characteristics | Low risk | Similar baseline characteristics reported |
| Reliable primary outcome measure | Low risk | Mortality and Resident Classification Instrument (RCI) |
| Adequate protection against contamination | Unclear risk | Cluster design. [Attempted to contact author for further information but no response] |
| Other bias | High risk | Medication reviews were undertaken for a non‐random subsample of 500 residents (total intervention residents 905) selected by nursing staff |
| Methods | RCT (randomised by GP) Total study duration: 6 weeks | |
| Participants | 196 residents One nursing home Age: mean 84.5 years (59‐100) Gender: 25% male Country: Netherlands Date of study: 1993 | |
| Interventions | Feedback on GP prescribing from community pharmacist Group A received usual care, group B GPs issued with a medication list used by their patients, group C GPs received a medication list plus feedback from community pharmacist | |
| Outcomes | Medication‐related problems Not used for this review: drug use | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Low risk | Cluster design |
| Blinding of participants and personnel (performance bias) | High risk | No blinding conducted |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not measured in this study |
| Incomplete outcome data (attrition bias) | Unclear risk | Not measured in this study |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Similar baseline outcome measurements | Unclear risk | No baseline measurements of medication‐related problems |
| Similar baseline characteristics | High risk | Most baseline characteristics similar, however fewer males in group A and fewer medicines per resident in group B |
| Reliable primary outcome measure | Low risk | Drug use |
| Adequate protection against contamination | High risk | Randomised by GP, however control and intervention residents resided in the same nursing home |
| Other bias | Low risk | Appears to be free of other sources of bias |
| Methods | RCT (randomised by patient) Total study duration: 6 months | |
| Participants | 661 (331 intervention, 330 control) care home residents, 65 care homes Setting: Nursing and residential homes for older people Age: Intervention mean 85.3 (IQR 81‐90); control mean 84.9 (IQR 80‐90) Gender: Intervention 75 (22.7%) male; control 79 (23.9%) male Country: UK Date of study: 2002 | |
| Interventions | Medication review by a single pharmacist A clinical medication review was conducted by the study pharmacist who held a postgraduate qualification in clinical pharmacy, within 28 days of randomisation. It comprised a review of the GP clinical record and a consultation with the resident and carer. The pharmacist formulated recommendations with the resident and carer and passed them on a written proforma to the GP for acceptance and implementation. GP acceptance was signified by ticking a box on the proforma. Control patients received usual GP care | |
| Outcomes | Measured at baseline and six months ± three weeks post‐randomisation: Hospital admissions (non‐elective) Mortality Medication‐related problems Medicine costs (cost of 28 days of repeat medicines per participant) Not used for this review: Number of changes in medicines per participant Number of medicines per participant Recorded medication reviews Falls SMMSE Barthel index Number of GP consultations | |
| Notes | Funded by The Health Foundation, 90 Long Acre, London WC2 9RA (Registered Charity Number 286967) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients were randomised in randomly sized blocks of 2 to 8 patients using an algorithm written in Visual Basic in Microsoft Access |
| Allocation concealment (selection bias) | Low risk | Not reported in paper. Allocation was concealed to the research pharmacist and nurse data collector by statistician [Author contacted] |
| Blinding of participants and personnel (performance bias) | High risk | Open design, no blinding attempted |
| Blinding of outcome assessment (detection bias) | High risk | No blinding conducted |
| Blinding of outcome assessment (detection bias) | Low risk | No blinding conducted, however outcomes not likely to be influenced by lack of blinding |
| Incomplete outcome data (attrition bias) | Low risk | Similar attrition in both groups with similar reasons for dropouts. Described as intention‐to‐treat by authors |
| Incomplete outcome data (attrition bias) | Low risk | Similar attrition in both groups with similar reasons for dropouts. Described as intention‐to‐treat by authors |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Similar baseline outcome measurements | Low risk | Similar baseline measurements for hospital admissions and medicine costs |
| Similar baseline characteristics | Low risk | Similar baseline characteristics reported |
| Reliable primary outcome measure | Low risk | Number of changes in medication |
| Adequate protection against contamination | High risk | Randomised by patient therefore contamination possible |
| Other bias | Unclear risk | Sample size calculation indicated that 1600 residents were required, however, only 661 residents were recruited |
IQR: Interquartile Range
MMSE: Mini‐Mental State Examination
SD: Standard Deviation
I5D: 15 Dimensional Instrument of Health‐related Quality of Life
Characteristics of excluded studies [ordered by study ID]
Jump to:
| Study | Reason for exclusion |
| Whole medication regime not considered (psychoactive medicines only) | |
| Whole medication regime not considered (psychotropic and stroke medicines only) | |
| Focus was on delirium and falls | |
| Included community‐dwelling patients in addition to nursing home residents |
Characteristics of ongoing studies [ordered by study ID]
Jump to:
| Trial name or title | Multi‐professional clinical medication reviews in care homes for the elderly: study protocol for a randomised controlled trial with cost effectiveness analysis |
| Methods | Cluster RCT (randomised by care home) Total Study Duration: 12 months |
| Participants | Residents of 30 care homes for older people (average age > 65) |
| Interventions | Intervention homes will receive a multi‐professional medication review at baseline and at 6 months, with follow‐up at 12 months. Control homes will receive usual care (support they currently receive from the National Health Service), with data collection at baseline and 12 months. |
| Outcomes | Emergency hospital admissions and Accident and Emergency (A&E) visits (number of admissions in six months per patient) Medication costs (mean drug costs per patient ‐ net ingredient costs for 28 days) Not used for this review: Number of falls (mean per patient per month) |
| Starting date | 2011 |
| Contact information | |
| Notes |
| Trial name or title | Improving quality of life in nursing home residents: a cluster randomized clinical trial of efficacy (KOSMOS) |
| Methods | Cluster RCT (randomised by care home) Total Study Duration: ˜ 16 months |
| Participants | Residents of 38 care homes (˜ 310 participants, average age > 65) |
| Interventions | Staff training, study guidelines and manuals |
| Outcomes | Potentially inappropriate prescribing (number of drugs which match the STOPP criteria at each collection point) Medications which should be introduced (assessed using the START criteria) Hospital admissions Mortality Quality of life in late‐stage dementia Neuropsychiatric inventory Activities of daily living |
| Starting date | 2014 |
| Contact information | |
| Notes |
| Trial name or title | Discontinuing inappropriate medication in nursing home residents (DIM‐NHR Study): protocol of a cluster randomised controlled trial |
| Methods | Cluster RCT (elderly care physicians and wards randomised) |
| Participants | Residents of care home (˜ 600 residents) |
| Interventions | Multidisciplinary Multistep Medication Review (3MR) will be carried out by elderly care physicians in collaboration with a pharmacist. Data will be collected at baseline and 4 months after the 3MR has taken place. |
| Outcomes | Discontinuation of inappropriate medication (according to the STOPP criteria) Starting new medication (according to the START criteria) Harm (including mortality, falls, gastrointestinal bleeding, A&E and outpatient visits, physician consultations) Quality of life (measured with Dementia Quality of Life Instrument (DQI) and EQ‐5D‐3L Cognitive function measured using the Severe Impairment Battery (SIB) and the Mini‐Mental State Examination (MMSE) Expenditure on healthcare taking into account salary costs, medication costs, laboratory examinations,additional costs |
| Starting date | 2014 |
| Contact information | |
| Notes |
EQ‐5D‐3L: EuroQol 5 Dimension Health‐related Quality of Life

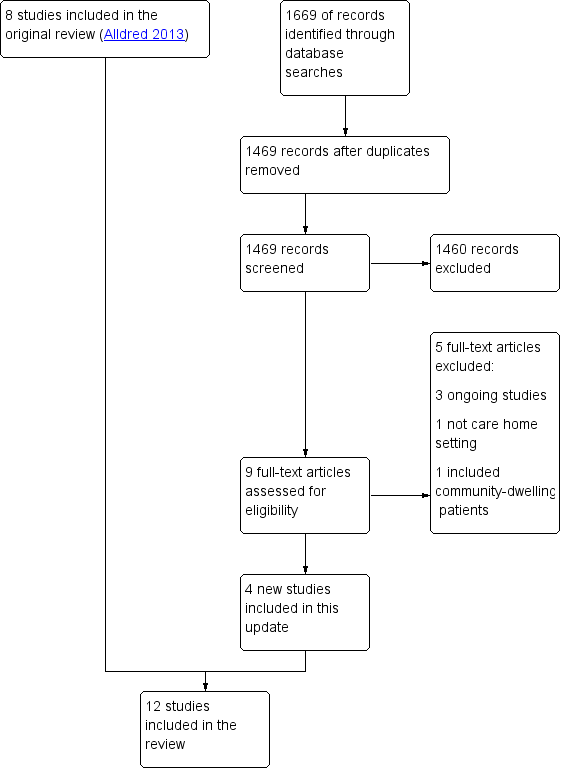
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
| Interventions to optimise prescribing compared with usual GP care for care home residents | |||
| Patient or population: older people (aged 65 years or older) living in care homes Settings: Institutionalised care facilities in Australia, Finland, Israel, Netherlands, New Zealand, Spain, Sweden, United Kingdom, and USA and Canada Intervention: Intervention to optimise prescribing (single or multicomponent intervention) Comparison: Usual care by general practitioner | |||
| Outcomes | Impact | No of Participants | Quality of the evidence |
| Adverse drug events | There was no evidence of an effect on adverse drug events | 1228 in 87 care homes (2 studies) | ⊕⊕⊝⊝ |
| Hospital admissions | It is uncertain whether medication review reduces hospital admissions | 7606 in 309 care homes (8 studies) | ⊕⊕⊝⊝ |
| Mortality | There was no evidence of an effect on mortality | 6805 in 188 care homes (6 studies) | ⊕⊕⊝⊝ |
| Quality of life | It is uncertain whether medication review improves quality of life | 586 in 21 care homes (2 studies) | ⊕⊕⊝⊝ |
| Medication‐related problems | Medication review may lead to the identification and resolution of medication‐related problems | 6640 in 251 care homes (7 studies) | ⊕⊕⊝⊝ |
| Medication appropriateness | Medication review may lead to an improvement in medication appropriateness | 1566 in 152 care homes (5 studies) | ⊕⊕⊝⊝ |
| Medicine costs | It is uncertain whether medication review decreases medication costs | 4734 in 142 care homes (5 studies) | ⊕⊝⊝⊝ |
| GRADE Working Group grades of evidence | |||
| Quality assessment of evidence for each outcome was based on study design, risk of bias, inconsistency, indirectness and imprecision. The evidence was downgraded from high to low for adverse drug events (Crotty 2004b; Gurwitz 2008) due to a serious risk of bias and imprecision. The evidence was downgraded from high to low for hospital admissions (Furniss 2000; Roberts 2001; Crotty 2004b; Zermansky 2006; Frankenthal 2014; Garcia‐Gollarte 2014; Pitkala 2014; Connolly 2015), mortality (Furniss 2000; Roberts 2001; Zermansky 2006; Frankenthal 2014; Pitkala 2014; Connolly 2015), quality of life (Frankenthal 2014; Pitkala 2014) and medication appropriateness (Crotty 2004a; Crotty 2004b; Frankenthal 2014; Garcia‐Gollarte 2014; Pitkala 2014) due to a serious risk of bias and inconsistency. The evidence for medicines costs (Furniss 2000; Roberts 2001; Crotty 2004a; Zermansky 2006; Frankenthal 2014 was downgraded from high to very low due to a serious risk of bias, inconsistency and imprecision. The evidence for medicine‐related problems (Strikwerda 1994; Claesson 1998; Furniss 2000; Roberts 2001; Crotty 2004b; Zermansky 2006; Frankenthal 2014 was reduced from high to low due to design, risk of bias and imprecision. | |||
| Study,Country, Design | Participants | Intervention | Outcome measures | Duration |
| Sweden Cluster‐RCT | 1854 residents in 33 nursing homes | Multidisciplinary meetings with physician, pharmacist and nurse(s) | Medication‐related problems | 14 months |
| Australia Cluster‐RCT | 1998 residents in 36 nursing homes | Multidisciplinary meetings with study geriatrician, a GP, a pharmacist and a nurse manager. Education of nurses and care‐givers | Hospital admissions Mortality | 14 months |
| Australia Cluster‐RCT | 154 residents in 10 nursing homes | Multidisciplinary case conferencing with GP, a geriatrician, a pharmacist, residential care staff and an Alzheimer's Association representative | Medication Appropriateness Index | 3 months |
| Australia Patient‐RCT | 110 patients discharged to 85 long‐term care facilities | Pharmacist transition co‐ordinator. Transfer of medicines information to nursing staff, family physician and community pharmacist plus medication review and case conferencing | Adverse drug events Hospital admissions Medication‐related problems Medication Appropriateness Index | 8 weeks |
| Israel Patient‐RCT | 359 residents in 1 chronic care geriatric facility | Medication review by the study pharmacist | Hospital admissions Mortality Quality of life Medication appropriateness (STOPP‐START) Medication‐related problems Medicine costs | 12 months |
| UK Cluster‐RCT | 330 residents in 14 nursing homes | Medication review by a single pharmacist | Hospital admissions Mortality Medication‐related problems Medicine costs | 8 months |
| Spain Cluster‐RCT | 716 residents in 36 nursing homes | Physician educational programme followed by on‐demand support (prescription advice) by phone | Hospital admissions (total number of days spent in hospital) Medication appropriateness (STOPP‐START) | 6 months |
| USA/Canada Cluster‐RCT | 1118 residents in 29 units in 2 long‐term care facilities | Computerised provider order entry with clinical decision support | Adverse drug events | 12 months |
| Finland Cluster‐RCT | 227 residents in 20 assisted living facilities | Nurse training and education | Hospital admissions Mortality Health‐related Quality of Life Medication appropriateness (Beer's criteria plus others) | 12 months |
| Australia Cluster‐RCT | 3230 residents in 52 nursing homes | Introduction of new professional role, nurse education and medication review by pharmacists | Hospital admissions Mortality Medication‐related problems Medicine costs | 24 months |
| Netherlands Cluster‐RCT | 196 residents in 1 nursing home | Feedback on GP prescribing from community pharmacist | Medication‐related problems | 6 weeks |
| UK Patient‐RCT | 661 residents in 65 care homes | Medication review by a single pharmacist | Hospital admissions Mortality Medication‐related problems Medicine costs | 6 months |