Mass drug administration for malaria
Information
- DOI:
- https://doi.org/10.1002/14651858.CD008846.pub3Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 29 September 2021see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Infectious Diseases Group
- Copyright:
-
- Copyright © 2021 The Authors. Cochrane Database of Systematic Reviews published by John Wiley & Sons, Ltd. on behalf of The Cochrane Collaboration.
- This is an open access article under the terms of the Creative Commons Attribution-Non-Commercial Licence , which permits use, distribution and reproduction in any medium, provided the original work is properly cited and is not used for commercial purposes.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
MD, JH, SPK, and KAL conceived of and designed the protocol. MPS and MD reviewed the literature and extracted the data. KAL and LC helped to resolve discrepancies. MPS, LC, and MD conducted the analyses. MPS, LC, and MD drafted the manuscript. All authors reviewed and provided final approval of the manuscript prior to publication.
Sources of support
Internal sources
-
Centers for Disease Control and Prevention, USA
-
US President's Malaria Initiative, USA
JH received salary support
-
Liverpool School of Tropical Medicine, UK
External sources
-
Foreign, Commonwealth and Development Office (FCDO), UK
Project number 300342‐104
Declarations of interest
MPS has no known conflicts of interest.
JH has no known conflicts of interest.
LC has no known conflicts of interest.
KAL has no known conflicts of interest.
SPK has no known conflicts of interest.
MD has no known conflicts of interest.
Acknowledgements
The Academic Editor is Dr Joseph Okebe.
The editorial base of the Cochrane Infectious Diseases Group is funded by UK aid from the UK government for the benefit of low‐ and middle‐income countries (project number 300342‐104). The views expressed do not necessarily reflect the UK government’s official policies.
We thank Marty Chaplin, Statistical Editor with the Cochrane Infectious Diseases Group (CIDG), for the statistical advice provided in this review. We also appreciate the assistance of Vittoria Lutje, CIDG Information Specialist, for running the literature search strategy.
Leslie Choi is supported by the Research, Evidence and Development Initiative (READ‐It) project. READ‐It (project number 300342‐104) is funded by UK aid from the UK government; however, the views expressed in this review do not necessarily reflect the UK government’s official policies.
Jimee Hwang receives salary support from the US President's Malaria Initiative.
We acknowledge Dr Thom Eisele, Dr Alistair McLean, and Dr Ulrika Morris for sharing unpublished data from their trials and also for their permission to include these data in the review in preparation for the WHO Evidence Review Group meeting on MDA for malaria in September 2018. We also received assistance from Dr Lorenz von Seidlein regarding study clarifications.
Version history
| Published | Title | Stage | Authors | Version |
| 2021 Sep 29 | Mass drug administration for malaria | Review | Monica P Shah, Jimee Hwang, Leslie Choi, Kim A Lindblade, S Patrick Kachur, Meghna Desai | |
| 2013 Dec 09 | Mass drug administration for malaria | Review | Eugenie Poirot, Jacek Skarbinski, David Sinclair, S Patrick Kachur, Laurence Slutsker, Jimee Hwang | |
| 2010 Nov 10 | Mass drug administration for malaria | Protocol | Eugenie Poirot, Jimee Hwang, S Patrick Kachur, Laurence Slutsker, Jacek Skarbinski | |
Differences between protocol and review
Differences between review and review update
A new author team was formed for this 2021 review update, with several authors from the previous review version (JH, SPK). Dr Monica Shah is the contact author for this 2021 review update.
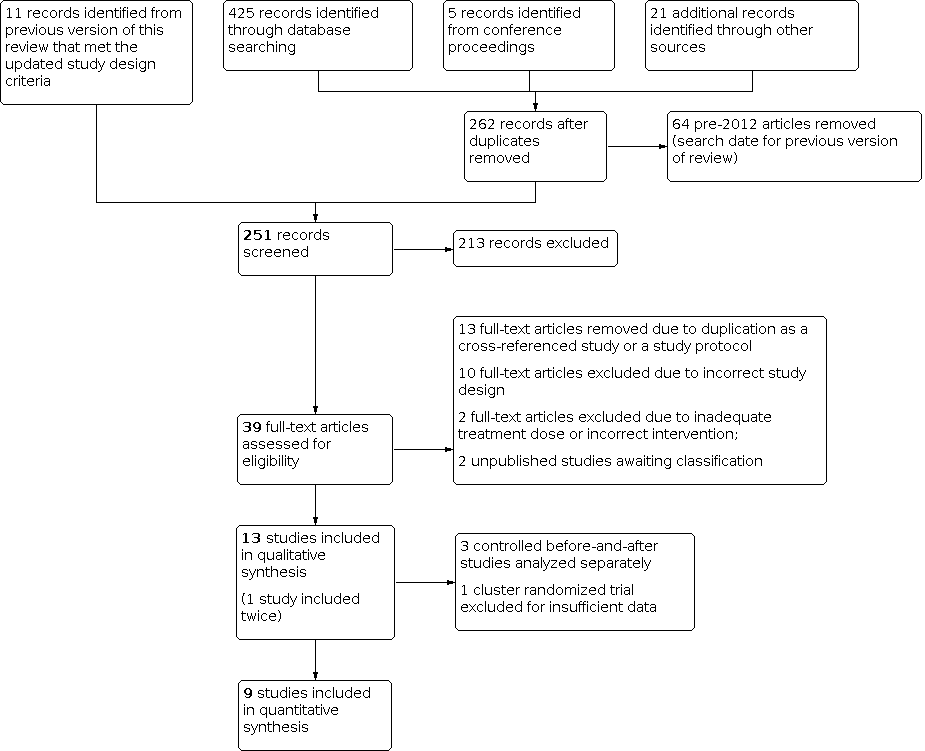
Pre‐specified revisions made to the background, inclusion criteria, and methods sections are detailed in Appendix 2. In addition, we analysed non‐randomized studies using a difference‐in‐difference analysis, as detailed in the methods section of this review update. We also conducted a post‐hoc analysis to explore differences in malaria epidemiology by continent as a reason for heterogeneity in effect of MDA on P falciparum parasitaemia prevalence at one to three months after MDA in very low‐ to low‐endemicity settings. The post‐hoc analysis by subgroup (studies conducted in Africa and Asia) is presented in Analysis 4.1.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Humans;
PICOs

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Comparison 1: MDA versus no MDA in moderate to high endemicity (cRCTs) on P falciparum outcomes, Outcome 1: Parasitaemia prevalence (P falciparum)

Comparison 1: MDA versus no MDA in moderate to high endemicity (cRCTs) on P falciparum outcomes, Outcome 2: Parasitaemia incidence (P falciparum)

Comparison 1: MDA versus no MDA in moderate to high endemicity (cRCTs) on P falciparum outcomes, Outcome 3: Confirmed malaria illness incidence (P falciparum)

Comparison 1: MDA versus no MDA in moderate to high endemicity (cRCTs) on P falciparum outcomes, Outcome 4: Gametocytaemia prevalence (P falciparum)

Comparison 1: MDA versus no MDA in moderate to high endemicity (cRCTs) on P falciparum outcomes, Outcome 5: Malaria‐specific mortality

Comparison 2: MDA versus no MDA in very low to low endemicity (cRCTs) on P falciparum outcomes, Outcome 1: Parasitaemia prevalence (P falciparum)

Comparison 2: MDA versus no MDA in very low to low endemicity (cRCTs) on P falciparum outcomes, Outcome 2: Parasitaemia incidence (P falciparum)

Comparison 2: MDA versus no MDA in very low to low endemicity (cRCTs) on P falciparum outcomes, Outcome 3: Confirmed malaria illness incidence (P falciparum)

Comparison 3: MDA versus no MDA in very low to low endemicity (cRCTs) on P vivax outcomes, Outcome 1: Parasitaemia prevalence (P vivax)

Comparison 3: MDA versus no MDA in very low to low endemicity (cRCTs) on P vivax outcomes, Outcome 2: Confirmed malaria illness incidence (P vivax)

Comparison 4: Supplemental analysis: post‐hoc subgroup analysis by continent, Outcome 1: Plasmodium falciparum parasitaemia prevalence post‐MDA 1‐3 months
| Patient or population: People of all ages living in an area with moderate to high endemicity of P falciparum malaria (≥ 10% prevalence) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with no MDA | Risk with MDA | |||||
| Follow‐up: 1 to 3 months | ||||||
| Parasitaemia prevalence | 5 per 100 | 9 per 100 | RR 1.76 | 786 | ⊕⊕⊝⊝ Due to imprecision | At 1‐3 months post‐MDA, parasite prevalence may increase in MDA compared no MDA. However, the effects vary and it is possible that MDA makes little or no difference on parasitaemia prevalence. |
| Parasitaemia incidence | 68 events per 100 person‐years | 42 events per 100 person‐years | Rate ratio 0.61 | 739 | ⊕⊕⊕⊝ Due to imprecision | At 1‐3 months post‐MDA, there is probably a reduction in parasitaemia incidence in MDA compared to no MDA. |
| Confirmed malaria illness incidence | 28 per 1000 population | 11 per 1000 population | Rate ratio 0.41 | 144,422 | ⊕⊕⊝⊝ Due to imprecision | At 1‐3 months post‐MDA, there may be a reduction in confirmed malaria illness incidence in MDA compared to no MDA. |
| Follow‐up: 4 to 6 months | ||||||
| Parasitaemia prevalence | 55 per 100 | 65 per 100 | RR 1.18 | 1414 | ⊕⊕⊕⊝ Due to imprecision | At 4‐6 months post‐MDA, there is probably little or no effect on parasitaemia prevalence in MDA compared to no MDA |
| Parasitaemia incidence | 129 events per 100 person‐years | 118 events per 100 person‐years | Rate ratio 0.91 | 1376 | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA has an effect on parasitaemia incidence at 4‐6 months post‐MDA |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aNot downgraded for inconsistency; the comparison presented is reported from a single study. | ||||||
| Patient or population: People of all ages living in an area with very low to low endemicity of P falciparum malaria (< 10% prevalence) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with Control | Risk with MDA | |||||
| Follow‐up: < 1 month | ||||||
| Parasitaemia prevalence | 12 per 100 | 1 per 100 | RR 0.12 | 1232 | ⊕⊕⊝⊝ Due to risk of bias and imprecision | At < 1 month post‐MDA, there may a reduction in parasitaemia prevalence in MDA compared to no MDA. |
| Follow‐up: 1 to 3 months | ||||||
| Parasitaemia prevalence | 3 per 100 | 1 per 100 (0 to 1) | RR: 0.25 (0.15 to 0.41) | 17,454 | ⊕⊕⊝⊝ Due to risk of bias | At 1‐3 months post‐MDA, there may a reduction in parasitaemia prevalence in MDA compared to no MDA. |
| Parasitaemia incidence | 15 events per 100 person‐years | 5 events per 100 person‐years | Rate ratio 0.37 | 736 | ⊕⊕⊕⊝ Due to imprecision | At 1‐3 months post‐MDA, there is probably a reduction in parasitaemia incidence in MDA compared to no MDA. |
| Confirmed malaria illness incidence | 6 per 1000 population | 4 per 1000 population | Rate ratio: 0.58 (0.12 to 2.73) | 130,651 | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA has an effect on confirmed malaria illness incidence at 1‐3 months post‐MDA compared to no MDA. |
| Follow‐up: 4 to 6 months | ||||||
| Parasitaemia prevalence | 5 per 100 | 3 per 100 (2 to 6) | RR: 0.63 (0.36 to 1.12) | 5670 (4 RCTs) | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA has an effect on parasitaemia prevalence at 4‐6 months post‐MDA compared to no MDA.
|
| Confirmed malaria illness incidence | 4 per 1000 population | 4 per 1000 population | Rate ratio 0.93 | 23,251 | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA has an effect on confirmed malaria illness incidence at 4‐6 months post‐MDA compared to no MDA. |
| Follow‐up: 7 to 12 months | ||||||
| Parasitaemia prevalence | 5 per 100 | 4 per 100 (3 to 6) | RR: 0.86 (0.55 to 1.36) | 7760 (5 RCTs) | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA has an effect on parasitaemia prevalence at 7‐12 months post‐MDA compared to no MDA. |
| Confirmed malaria illness incidence | 11 per 1000 population | 5 per 1000 population (2 to 12) | Rate ratio 0.47 (0.21 to 1.03) | 26,576 | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA has an effect on confirmed malaria illness incidence at 7‐12 months post‐MDA compared to no MDA. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded 1 level for risk of bias due to several criteria scored as high or unclear risk of bias. | ||||||
| Patient or population: People of all ages living in an area with very low to low endemicity of P falciparum malaria ( < 10% prevalence) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with Control | Risk with MDA | |||||
| Follow‐up: 13 to 18 months | ||||||
| Parasitaemia prevalence | 4 per 100 | 4 per 100 | RR 0.82 | 1537 | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA has an effect on parasitaemia prevalence at 13‐18 months post‐MDA compared to no MDA. |
| Confirmed malaria illness incidence | 17 per 1000 population | 13 per 1000 population | Rate ratio 0.77 | 23,251 | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA has an effect on confirmed malaria illness incidence at 13‐18 months post‐MDA compared to no MDA. |
| Follow‐up: 19 to 24 months | ||||||
| Parasitaemia prevalence | 3 per 100 | 1 per 100 | RR 0.34 | 1393 | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA has an effect on parasitaemia prevalence at 19‐24 months post‐MDA compared to no MDA. |
| Follow‐up: 25 months and above | ||||||
| Parasitaemia prevalence | 3 per 100 | 3 per 100 | RR 0.89 | 1521 | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA has an effect on parasitaemia prevalence at 25‐30 months post‐MDA compared to no MDA. |
| Parasitaemia prevalence | 3 per 100 | 4 per 100 | RR 1.25 | 1679 | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA has an effect on parasitaemia prevalence at 31‐36 months post‐MDA compared to no MDA. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded 2 levels for risk of bias due to several criteria scored as high or unclear risk of bias, including baseline imbalance, high risk of contamination, and a large unexplained increase in sampled population in the MDA group at this time point. | ||||||
| Patient or population: People of all ages living in an area with very low to low endemicity of P vivax malaria (< 10% prevalence) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with Control | Risk with MDA | |||||
| Follow‐up: < 1 month | ||||||
| Parasitaemia prevalence | 27 per 100 | 5 per 100 | RR 0.18 | 1232 | ⊕⊕⊝⊝ Due to risk of bias and imprecision | At < 1 month post‐MDA, there may a reduction in parasitaemia prevalence in MDA compared to no MDA. |
| Follow‐up: 1 to 3 months | ||||||
| Parasitaemia prevalence | 12 per 100 | 2 per 100 (1 to 3) | RR: 0.15 (0.10 to 0.24) | 6896 (5 RCTs) | ⊕⊕⊝⊝ Due to risk of bias | At 1‐3 months post‐MDA, there may a reduction in parasitaemia prevalence in MDA compared to no MDA. |
| Follow‐up: 4 to 6 months | ||||||
| Parasitaemia prevalence | 11 per 100 | 9 per 100 (7 to 10) | RR: 0.78 (0.63 to 0.95)
| 5670 (4 RCTs) | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA reduces parasitaemia prevalence at 4‐6 months post‐MDA compared to no MDA. |
| Follow‐up: 7 to 12 months | ||||||
| Parasitaemia prevalence | 9 per 100 | 11 per 100 (9 to 13) | RR: 1.12 (0.94 to 1.34) | 7760 (5 RCTs) | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA has an effect on parasitaemia prevalence at 7‐12 months post‐MDA compared to no MDA. |
| Confirmed malaria illness incidence | 41 per 1000 population | 57 per 1000 population (40 to 80) | Rate ratio: 1.38 (0.97 to 1.95) | 3325 (2 RCTs) | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA has an effect on confirmed malaria illness incidence at 7‐12 months post‐MDA compared to no MDA. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded 1 level for risk of bias due to several criteria scored as high or unclear risk of bias. | ||||||
| Patient or population: People of all ages living in an area with very low to low endemicity of P vivax malaria (< 10% prevalence) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with Control | Risk with MDA | |||||
| Follow‐up: 13 to 18 months | ||||||
| Parasitaemia prevalence | 17 per 100 | 14 per 100 | RR 0.81 | 1537 | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA reduces parasitaemia prevalence at 13‐18 months post‐MDA compared to no MDA. |
| Follow‐up: 19 to 24 months | ||||||
| Parasitaemia prevalence | 11 per 100 | 9 per 100 | RR 0.84 | 1393 | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA reduces parasitaemia prevalence at 19‐24 months post‐MDA compared to no MDA. |
| Follow‐up: 25 months and above | ||||||
| Parasitaemia prevalence | 11 per 100 | 9 per 100 | RR 0.89 | 1521 | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA reduces parasitaemia prevalence at 25‐30 months post‐MDA compared to no MDA. |
| Parasitaemia prevalence | 6 per 100 | 7 per 100 | RR 1.20 | 1679 | ⊕⊝⊝⊝ Due to risk of bias and imprecision | We do not know if MDA reduces parasitaemia prevalence at 31‐36 months post‐MDA compared to no MDA. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded 2 levels for risk of bias due to several criteria scored as high or unclear risk of bias, including a large unexplained increase in sampled population in the MDA group at this time point. | ||||||
| Study ID (Design) | Year(s) of study | Malaria endemicitya | Plasmodium species | Antimalarial drug resistance | MDA group | Control group | Co‐intervention(s)b | Outcomes reported (months of follow‐up post‐MDAc) | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Drug | Rounds, interval, and duration implemented | Population targeted (coverage) | ||||||||
| Eisele 2020 ZMBa (cRCT) | 2014‐2017 | Low | P falciparum | Widespread resistance to CQ and SP, but no evidence of resistance to artemisinin | DHAp | 4 rounds administered at start of rainy season, during rainy season, during dry season, and at start of rainy season over 15 months | 37,694 (79% in round 1; 63% in round 2; 76% in round 3; 66% in round 4) | No drug and no placebo | IRS, ITNs, and enhanced standard of care |
|
| Eisele 2020 ZMBb (cRCT) | 2014‐2017 | High | P falciparum | Widespread resistance to CQ and SP, but no evidence of resistance to artemisinin | DHAp | 4 rounds administered at start of rainy season, during rainy season, during dry season, and at start of rainy season over 15 months | 45,442 (79% in round 1; 63% in round 2; 76% in round 3; 66% in round 4) | No drug and no placebo | IRS, ITNs, and enhanced standard of care |
|
| Escudie 1962 BFA (CBA) | 1960‐1961 | High | P falciparum, P ovale, P malariae | ND | AQ‐PQ or CQ‐PQ | (Low frequency MDA) 7 rounds administered 28 days apart over 7 months | 1890 (75% to 91% per round) | No drug and no placebo | None (IRS arms excluded) |
|
| (High frequency MDA) 15 rounds administered 14 days apart over 7 months | 2560 (84% to 97% per round) |
| ||||||||
| Landier 2017 MMRa (cRCT) | 2013‐2015 | Low | P falciparum, P vivax | Artemisinin resistance firmly established | DHAp with PQ | 3 rounds administered 1 month apart over 3 months | 1434 (66% in round 1, 56% in round 2, and 65% in round 3) | Delayed MDA | ITNs, uninterrupted access to case management |
|
| McLean 2021 MMR (cRCT) | 2014‐2017 | Very low | P falciparum, P vivax | Artemisinin resistance: Kelch 13 mutation in 57% of samples at baseline | DHAp with PQ | 3 rounds administered 1 month apart over 3 months | 4622 (86% in round 1, 86% in round 2, 88% in round 3) | No drug and no placebo | ITNs, routine malaria control by village health workers |
|
| Molineaux 1980 NGA (CBA) | 1970‐1975 | High | P falciparum, P malariae, P ovale | ND | SP | (Low frequency MDA) 9 rounds administered 10 weeks apart over 18 months | 14,129 (73% to 92% per round) | No drug and no placebo | IRS |
|
| (High frequency MDA) 23 rounds administered 2 weeks apart during the wet seasons and 10 weeks apart during the dry seasons over 18 months | 1810 (72% to 91% per round) | |||||||||
| Morris 2018 TZA (cRCT) | 2016‐2017 | Very low | P falciparum, P malariae, P ovale, and P vivax | No evidence of resistance to first line treatment AS‐AQ | DHAp with PQ | 2 rounds administered 4 weeks apart over 6 weeks | 10,944 (91% in round 1, 88% in round 2) | No drug and no placebo | IRS and ITNs |
|
| Pongvongsa 2018 LAO (cRCT) | 2016‐2017 | Low | P falciparum, P vivax | ND | DHAp with PQ | 3 rounds administered 1 month apart over 3 months | 1006 (81% in round 1, 80% in round 2, and 82% in round 3) | Delayed MDA | ITNs, uninterrupted access to case management |
|
| Roberts 1964 KEN (CBA) | 1953‐1954 | Moderate | P falciparum | ND | Pyrimethamine | 2 rounds administered 1 year apart over 13 months | 101,000 (95% in round 1, 93% in round 2) | No drug and no placebo | None |
|
| Shekalaghe 2011 TZA (cRCT) | 2008 | Very low | P falciparum | ND | SP+AS with PQ | 1 round over 16 days | 1110 (95%) | Placebo | ITNs, single treatment campaign for trachoma with azithromycin |
|
| Tripura 2018 KHM (cRCT) | 2014‐2016 | Very low | P falciparum, P vivax | Reduced susceptibility to artemisinins and ACT partner drug resistance | DHAp | 3 rounds administered 1 month apart over 3 months | 858 (74% in round 1, 60% in round 2, and 71% in round 3) | Delayed MDA | ITNs, uninterrupted access to case management |
|
| von Seidlein 2003 GMB (cRCT) | 1999 | High | P falciparum | ND | SP+AS | 1 round over 1 month | 12,331 (89%) | Placebo | None |
|
| von Seidlein 2019 VNM (cRCT) | 2013‐2015 | Very low | P falciparum, P vivax | No evidence of resistance to DHAp at the start of study, but treatment failure to DHAp has increased following study | DHAp with PQ | 3 rounds administered 1 month apart over 3 months | 1439 (83% in round 1, 98% in round 2, and 99% in round 3) | Delayed MDA | ITNs, uninterrupted access to case management |
|
| ACT = artemisinin‐based combination therapy, AQ = amodiaquine, AS = artesunate, CBA = controlled before‐and‐after study, CQ = chloroquine, cRCT = cluster‐randomized controlled trial, DHAp = dihydroartemisinin piperaquine, ITNs = insecticide‐treated bed nets, IRS = indoor residual spraying, MDA = mass drug administration, PQ = primaquine, SP = sulfadoxine‐ (or sulfalene‐) pyrimethamine, NA = not applicable, ND = not described. aMalaria endemicity classified as very low (> 0% to < 1%), low (1% to < 10%), moderate (10% to < 35%) or high (≥ 35%) (WHO 2017). | ||||||||||
| Study ID (design) | Parasitaemia prevalence | Parasitaemia incidence | Confirmed malaria illness incidence | All‐cause or malaria‐specific mortality | Gametocytaemia prevalence | Adverse effects |
|---|---|---|---|---|---|---|
| Eisele 2020 ZMBa (cRCT) | Yes | Yes | Yes | No | No | Yes |
| Eisele 2020 ZMBb (cRCT) | Yes | Yes | Yes | No | No | Yes |
| Escudie 1962 BFA (CBA) | Yes | No | No | No | Yes | No |
| Landier 2017 MMRa (cRCT) | Yes | No | Yes | No | No | Yes |
| McLean 2021 MMR (cRCT) | Yes | No | No | No | No | Yes |
| Molineaux 1980 NGA (CBA) | Yes | No | No | No | Yes | No |
| Morris 2018 TZA (cRCT) | Yes | No | Yes | No | No | Yes |
| Pongvongsa 2018 LAO (cRCT) | Yes | No | No | No | No | Yes |
| Roberts 1964 KEN (CBA) | Yes | No | No | No | No | No |
| Shekalaghe 2011 TZA (cRCT) | Yes | No | Yes | No | Yes | Yes |
| Tripura 2018 KHM (cRCT) | Yes | No | Yes | No | No | Yes |
| von Seidlein 2003 GMB (cRCT) | Yes | Yes | Yes | Yes | Yes | Yes |
| von Seidlein 2019 VNM (cRCT) | Yes | No | No | No | No | Yes |
| CBA = controlled before‐and‐after study, cRCT = cluster‐randomized controlled trial | ||||||
| Study | Intervention, % (n) | Control % (n) | Difference‐in‐differences, percentage pointsa | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre‐MDA | During MDA | Post‐MDA | Pre‐MDA | During MDA | Post‐MDA | During MDA | Post‐MDA | |||||||
| 1 to 3 months | 4 to 6 months | 7 to 12 months | 1 to 3 months | 4 to 6 months | 7 to 12 months | 1 to 3 months | 4 to 6 months | 7 to 12 months | ||||||
| Low frequency MDA with AQ‐PQ or CQ‐PQ | 67.6 (190) | 21.6 (75) | 38.3 (105) | ND | ND | 59.4 (129) | 74.8 (517) | 386 (72.3) | ND | ND | ‐61.4 | ‐42.1 | ND | ND |
| High frequency MDA with AQ‐PQ or CQ‐PQ | 33.6 (131) | 12.6 (59) | 61.4 (286) | ND | ND | 59.4 (129) | 74.8 (517) | 386 (72.3) | ND | ND | ‐36.3 | 14.9 | ND | ND |
| Low frequency MDA with SP | 41.8 (525) | 1.9 (40) | ND | ND | ND | 49.1 (493) | 32.5 (380) | ND | ND | ND | ‐23.2 | ND | ND | ND |
| High frequency MDA with SP | 44.9 (754) | 7.3 (109) | ND | ND | ND | 49.1 (493) | 32.5 (380) | ND | ND | ND | ‐20.9 | ND | ND | ND |
| MDA with pyrimethamine | 8.3 (25) | 9 (188) | 2.9 (26) | (27) (4.5) | (15) (5) | 18 (154) | 34.4 (723) | 40.7 (366) | 37 (222) | 26 (78) | ‐15.8 | ‐28.1 | ‐22.8 | ‐11.3 |
| AQ = amodiaquine, CQ = chloroquine, MDA = mass drug administration, ND = no data, PQ = primaquine, SP = sulfalene‐pyrimethamine aCalculated as difference in proportion at the time period of during MDA or post‐MDA minus the proportion at pre‐MDA in the intervention and control separately and the difference in these two proportion differences between the intervention and control groups. | ||||||||||||||
| Study | Intervention, % (n) | Control, % (n) | Difference‐in‐differences percentage pointa | |||||
|---|---|---|---|---|---|---|---|---|
| Pre‐MDA | During MDA | Post‐MDA 1 to 3 months | Pre‐MDA | During MDA | Post‐MDA 1 to 3 months | During MDA | Post‐MDA 1 to 3 months | |
| Low frequency MDA with AQ‐PQ or CQ‐PQ | 20.3 (57) | 0.9 (3) | 38.3 (35) | 19.4 (42) | 14 (97) | 19.1 (102) | ‐14.1 | 18.3 |
| High frequency MDA with AQ‐PQ or CQ‐PQ | 8.2 (32) | 1.9 (9) | 61.4 (107) | 19.4 (42) | 14 (97) | 19.1 (102) | ‐1.0 | 53.4 |
| Low frequency MDA with SP | 10.1 (127) | 0.6 (12) | ND | 12.4 (124) | 7.9 (92) | ND | ‐5.0 | ND |
| High frequency MDA with SP | 12.4 (208) | 3.2 (48) | ND | 12.4 (124) | 7.9 (92) | ND | ‐4.7 | ND |
| AQ = amodiaquine, CQ = chloroquine, MDA = mass drug administration, ND = no data, SP = sulfalene‐pyrimethamine aCalculated as difference in proportion at the time period of during MDA or post‐MDA minus the proportion at pre‐MDA in the intervention and control separately and the difference in these two proportion differences between the intervention and control groups. | ||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Parasitaemia prevalence (P falciparum) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1.1 Baseline before MDA | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1.2 During MDA | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1.3 Post‐MDA 1‐3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1.4 Post‐MDA 4‐6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.2 Parasitaemia incidence (P falciparum) Show forest plot | 2 | Rate Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 1.2.1 Post‐MDA 1‐3 months | 1 | Rate Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 1.2.2 Post‐MDA 4‐6 months | 1 | Rate Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 1.3 Confirmed malaria illness incidence (P falciparum) Show forest plot | 1 | Rate Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 1.3.1 Baseline before MDA | 1 | Rate Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 1.3.2 Post‐MDA 1‐3 months | 1 | Rate Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 1.4 Gametocytaemia prevalence (P falciparum) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.4.1 Baseline before MDA | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.4.2 Post‐MDA 4‐6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.5 Malaria‐specific mortality Show forest plot | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 1.5.1 Post‐MDA 4‐6 months | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Parasitaemia prevalence (P falciparum) Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1.1 Baseline before MDA | 6 | 2093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.62, 1.26] |
| 2.1.2 During‐MDA | 2 | 991 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.07, 0.94] |
| 2.1.3 Post‐MDA <1 month | 1 | 234 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.03, 0.52] |
| 2.1.4 Post‐MDA 1‐3 months | 7 | 5718 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.15, 0.41] |
| 2.1.5 Post‐MDA 4‐6 months | 4 | 3129 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.36, 1.12] |
| 2.1.6 Post‐MDA 7‐12 months | 5 | 3704 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.55, 1.36] |
| 2.1.7 Post‐MDA 13‐18 months | 1 | 243 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.20, 3.34] |
| 2.1.8 Post‐MDA 19‐24 months | 1 | 239 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.06, 1.97] |
| 2.1.9 Post‐MDA 25‐30 months | 1 | 242 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.22, 3.62] |
| 2.1.10 Post‐MDA 31‐36 months | 1 | 246 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.25, 6.31] |
| 2.2 Parasitaemia incidence (P falciparum) Show forest plot | 1 | Rate Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2.2.1 Post‐MDA 1‐3 months | 1 | Rate Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2.3 Confirmed malaria illness incidence (P falciparum) Show forest plot | 4 | Rate Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 2.3.1 Baseline before MDA | 3 | Rate Ratio (IV, Fixed, 95% CI) | 0.87 [0.45, 1.69] | |
| 2.3.2 Post‐MDA 1‐3 months | 2 | Rate Ratio (IV, Fixed, 95% CI) | 0.58 [0.12, 2.73] | |
| 2.3.3 Post‐MDA 4‐6 months | 1 | Rate Ratio (IV, Fixed, 95% CI) | 0.93 [0.07, 12.43] | |
| 2.3.4 Post‐MDA 7‐12 months | 3 | Rate Ratio (IV, Fixed, 95% CI) | 0.47 [0.21, 1.03] | |
| 2.3.5 Post‐MDA 13‐18 months | 1 | Rate Ratio (IV, Fixed, 95% CI) | 0.77 [0.20, 3.03] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Parasitaemia prevalence (P vivax) Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1.1 Baseline before MDA | 5 | 3187 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.86, 1.21] |
| 3.1.2 Post‐MDA <1 month | 1 | 234 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.08, 0.40] |
| 3.1.3 Post‐MDA 1‐3 months | 5 | 2673 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.10, 0.24] |
| 3.1.4 Post‐MDA 4‐6 months | 4 | 3299 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.63, 0.95] |
| 3.1.5 Post‐MDA 7‐12 months | 5 | 4406 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.94, 1.34] |
| 3.1.6 Post‐MDA 13‐18 months | 1 | 243 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.44, 1.48] |
| 3.1.7 Post‐MDA 19‐24 months | 1 | 239 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.38, 1.83] |
| 3.1.8 Post‐MDA 25‐30 months | 1 | 242 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.41, 1.94] |
| 3.1.9 Post‐MDA 31‐36 months | 1 | 246 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.44, 3.29] |
| 3.2 Confirmed malaria illness incidence (P vivax) Show forest plot | 2 | Rate Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.2.1 Baseline before MDA | 1 | Rate Ratio (IV, Fixed, 95% CI) | 1.74 [0.67, 4.53] | |
| 3.2.2 Post‐MDA 7‐12 months | 2 | Rate Ratio (IV, Fixed, 95% CI) | 1.38 [0.97, 1.95] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 4.1 Plasmodium falciparum parasitaemia prevalence post‐MDA 1‐3 months Show forest plot | 7 | 5718 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.15, 0.41] |
| 4.1.1 Africa | 2 | 1033 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.32, 2.98] |
| 4.1.2 Asia | 5 | 4685 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.11, 0.33] |