Cabestrillo con incisión simple para la incontinencia urinaria en mujeres
References
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Prospective RCT of TVT versus TVT‐Secur in the treatment of female SUI | |
| Participants | 60 female patients with SUI Exclusion criteria: detrusor overactivity, bladder capacity < 200 mL, grade III or IV cystocoele, type 0 SUI (Blaivas and Olsson classification 1988), recurrent SUI | |
| Interventions | TVT (bottom‐to‐top) (30) TVT‐Secur (U‐type) (30) | |
| Outcomes | Main outcome measures: operative time, bleeding, duration of catheterisation, intraoperative and postoperative complications, Impact of incontinence on quality‐of‐life questionnaire (IQoL), length of hospital stay, urodynamic assessment 9 months' follow‐up Well matched for baseline characteristics | |
| Notes | Quote: "cure means completely dry, while improvement means wetting but less than before surgery. Success rate includes cure and improvement" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "patients were randomly divided into two equal groups" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | All enrolled participants were included in the analysis |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Quasi‐randomised prospective study comparing Contasure Needleless (C‐NDL) versus TVT‐O in a non‐inferiority design | |
| Participants | 158 women with SUI with or without associated prolapse | |
| Interventions | TVT‐O (60) (21 had SUI surgery alone) Contasure Needleless (C‐NDL) (72) (34 had SUI surgery alone) | |
| Outcomes | Objective cure (stress test); subjective cure (Sandvik severity test, clinical history); Q‐tip test, ICIQ‐SF, urodynamics, complications, blood loss, postoperative pain | |
| Notes | Cure defined as negative stress test postoperatively, or score 0 on Sandvik questionnaire. Surgical procedure for stress incontinence only (with no prolapse surgery) done on 55 participants (34 in C‐NDL and 21 in TVT‐O) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "patients were assigned to one or other group of treatment depending on the last figure of their medical history number; last even figure was allocated for technical TVT‐O and last odd figure for C‐NDL" Comment: inadequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | High risk | 26 participants did not complete follow‐up schedule but were excluded from analysis. Statistical analysis performed on 60 participants in the TVT‐O group and on 72 in the C‐NDL group; these numbers are reported as adequate for analysis as per power calculation |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of surgeon not possible because of difference in technique. Blinding of participants not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Prospective randomised multi‐centre study comparing TVT versus TVT‐Secur | |
| Participants | 123 women with primary SUI or MUI with predominant SUI Inclusion criteria: age > 18 years; desires surgical treatment; does not desire future pregnancy; >= 3 mL leakage on standardised pad test; cough‐synchronous leakage on cough stress test Exclusion criteria: need for concomitant surgery for pelvic organ prolapse; regular PFMT for less than 3 months; planned or current pregnancy; previous surgery for urinary incontinence, bladder capacity < 300 mL; residual urinary volume > 100 mL; known detrusor instability; cystitis more than 4 times in the past 12 months | |
| Interventions | TVT (62) TVT‐Secur (61) | |
| Outcomes | Pad test, stress test, KHQ, voiding diary, visual analogue scale | |
| Notes | 2011 paper follow‐up at 2 months, but this is a full article. The 2012 paper is an abstract but reports 1‐year outcomes Subjective cure rate assessed but method of interpretation not defined. Study stopped at interim analysis because of poor outcomes and high rate of serious complications with TVT‐S 133 participants randomly assigned. Loss to follow‐up in 2 patients. 4 women were excluded because of protocol violations, and 4 declined surgery for personal reasons after they had been randomly assigned. Intention‐to‐treat analysis not done or reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Consenting women who fulfilled all inclusion criteria were randomised in a proportion of 1:1" |
| Allocation concealment (selection bias) | Low risk | Quote: "an equal proportion of assignments were mixed and placed in opaque envelopes which were then sealed, mixed again and numbered and kept at a central study secretariat" |
| Incomplete outcome data (attrition bias) | High risk | 133 participants randomly assigned. Loss to follow‐up in 2 patients. 4 women were excluded because of protocol violations, and 4 declined the surgery for personal reasons after they had been randomly assigned. Intention‐to‐treat analysis not done or reported |
| Blinding of participants and personnel (performance bias) | High risk | Surgeon and participant blinding not possible because of the nature of the procedure |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "the follow up was performed by an independent evaluator, usually a urotherapist" |
| Methods | Multi‐centre RCT of TVT‐Secur versus retropubic TVT for treatment of SUI. Non‐inferiority design. 24‐month follow‐up | |
| Participants | 263 women with urodynamic SUI, with or without genital prolapse Eligibility criteria: at least 21 years of age, demonstrated urodynamic SUI, desiring surgical treatment for incontinence Exclusion criteria: DO on urodynamics; PVR greater than 100 mL; history of previous synthetic, biological or fascial sub‐urethral sling; desire for future pregnancy; currently using anticoagulation or known bleeding diathesis; urethral diverticulum or fistula Patients who received TVT were more likely to undergo concurrent hysterectomy (26% vs 9% in TVT‐Secur arm) | |
| Interventions | TVT‐Secur (U‐type) (127) TVT (bottom‐up approach) (129) | |
| Outcomes | Primary outcome: subjective cure (absence of any urinary incontinence or retreatment) at 1 year Secondary outcome measures: bladder diary, postoperative pain, short‐ and long‐term complications, quality of life scores (Incontinence Severity Index, Pelvic Floor Distress Inventory‐20, Pelvic Floor Impact Questionnaire‐7, Patient Global Index of Improvement), change in sexual function | |
| Notes | Surgeons instructed to set tension of TVT so as to be 'tension‐free' (a spacer can be introduced between urethra and sling), whereas with TVT‐Secur, tension was set tightly, so that sling was directly opposed to the urethra and spacer could not be introduced | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random allocation with randomly permuted blocks used; stratified by site and presence or absence of prolapse beyond the hymen |
| Allocation concealment (selection bias) | Low risk | Consecutively numbered, sealed, opaque envelopes used |
| Incomplete outcome data (attrition bias) | High risk | 12 individuals randomly assigned to the mini‐sling arm had technical difficulties during insertion; 7 ended up receiving a TVT (6) or other retropubic sling (1) |
| Blinding of participants and personnel (performance bias) | Low risk | Sham incisions used in mini‐sling arm to facilitate blinding |
| Blinding of outcome assessment (detection bias) | Low risk | Research staff not involved in operation performed postoperative assessments |
| Methods | Prospective, single‐centre RCT | |
| Participants | 71 women with SUI Inclusion criteria: SUI symptoms together with objective evidence of USI, which had failed to resolve with conservative measures Exclusion criteria: previous continence surgery, evidence of voiding dysfunction, known bladder pathology, pelvic organ prolapse (POP‐Q stage 2 or above), recurrent UTI, plan to conceive in the future | |
| Interventions | Retropubic TVT (Advantage TVT) (33) Mini‐sling (MiniArc) (38) | |
| Outcomes | Primary outcome was presence of SUI at 6 weeks and 6 months postoperatively (KHQ and PGI‐I). Secondary outcomes were SUI and urodynamics at 6 months and complications | |
| Notes | 6‐Month follow‐up data from 2010 paper used for cure and operative outcomes In 2012 paper of MiniArc, 35/38 returned 3‐year questionnaires; Retropubic TVT, 26/33 returned 3‐year questionnaires. Data were used for redo surgery outcome | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Subjects were randomised using computer‐generated block randomisation sequence" |
| Allocation concealment (selection bias) | Low risk | Quote: "allocation to each group being performed via a series of opaque envelopes, by a member of the research team" |
| Incomplete outcome data (attrition bias) | Low risk | Subjective data available on all participants. Three participants declined urodynamics at 6 months (all in TVT arm) |
| Blinding of participants and personnel (performance bias) | Low risk | Participants blinded but researchers could not be blinded because of differences in devices |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not mentioned |
| Methods | Prospective single‐centre RCT comparing TVT‐O versus TVT‐Secur | |
| Participants | 122 women with SUI Exclusion criteria: DO, concomitant prolapse > stage 2 | |
| Interventions | TVT‐0 (56) TVT‐Secur (66) | |
| Outcomes | Clinical evaluation, pad test, KHQ, urodynamics. Mean follow‐up 24 months | |
| Notes | Abstract only. Ongoing study with additional data from Bianchi 2010; therefore 2012 abstract used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | Data available on all randomly assigned participants |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Prospective RCT comparing Ophira mini‐sling versus transobturator tape (Unitape, outside‐in) | |
| Participants | 73 women with SUI and no prolapse > stage 1 Exclusion criteria: PVR > 100 mL; coagulation disorders; current UTI; sequelae of previous radiation therapy of pelvis; anticoagulant therapy; vulvovaginitis; anaesthesia contraindication | |
| Interventions | Ophira mini‐sling performed under LA (45) Unitape TOT performed under regional anaesthesia (28) | |
| Outcomes | Primary outcome was objective cure at 6 months (defined as a 1‐hour pad weighing < 2 g and a negative stress test) Secondary outcome measures included quality of life and symptom severity scores ( I‐QOL, UDI‐6, respectively) and rate of complications | |
| Notes | Conference abstract only. 6‐Month follow‐up data available for only 29 Ophira and 15 Unitape participants reported here. Operative complications are reported for the full cohort | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation method not described. Unequal ratio of randomisation with no reason stated |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | All outcome data described for all participants |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Prospective RCT of MinArc versus Monarc | |
| Participants | 90 women with SUI undergoing primary anti‐incontinence surgery | |
| Interventions | Mini‐Arc (45) Monarc (TVTO) (45) | |
| Outcomes | Clinical and urodynamic evaluation at 24 months | |
| Notes | German paper, only abstract in English | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "women were randomly allocated" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | All outcome data reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Prospective, single‐centre RCT of TVT‐Secur versus TVT‐O | |
| Participants | 84 women with SUI Patients may have undergone concomitant prolapse surgery Groups well matched for baseline characteristics. | |
| Interventions | TVT‐Secur (Hammock type) (42) TVT‐O (42) | |
| Outcomes | Primary outcomes were intra‐operative complications, peri‐operative morbidity and post‐operative efficacy (at 1 year) | |
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Incomplete outcome data (attrition bias) | Low risk | All participant data included in analysis |
| Blinding of participants and personnel (performance bias) | Unclear risk | No description |
| Blinding of outcome assessment (detection bias) | Unclear risk | No description |
| Methods | Prospective, multi‐centre, unblinded RCT comparing TVT‐Secur versus TVT‐O | |
| Participants | 194 women with SUI, demonstrable during clinical and/or urodynamic evaluation. Exclusion criteria: recurrent SUI; concomitant surgery; stage 2 or greater genital prolapse | |
| Interventions | TVT SECUR (97) TVT‐O (98) | |
| Outcomes | Primary outcome was objective cure of SUI at 1 year, measured by standing cough stress test measured at 300 mL bladder volume or 70% of maximum bladder capacity, according to the participant voiding diary. Secondary outcome measures were perioperative morbidity, general quality of life scores using SF‐36 and disease‐specific QoL using UDI (Dutch version), pain VAS scores, subjective SUI reporting, urgency and or urgency urinary incontinence | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were assigned to surgical treatment by balanced non‐restricted randomisation. Block randomisation was done at each participating centre using a computerised random number generator" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | High risk | Relatively high dropout rate, but statistical analysis revealed no significant or clinically relevant difference between respondents and non‐respondents |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "Blinding of investigators and patients to group allocation was not possible since one procedure resulted in skin wound whilst the other was exit free" |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Single‐centre non‐blinded RCT of TVT‐Secur versus TVTO | |
| Participants | 43 women with SUI Inclusion criteria: SUI with demonstrable impact of SUI on quality‐of‐life questionnaires and positive cough stress test in urodynamics Exclusion criteria: intrinsic sphincter deficiency (MUCP < 20 cm H2O), previous sub‐urethral sling, predominant OAB symptoms, women planning future pregnancy, bleeding diathesis or anticoagulant therapy, immunosuppression, progressive neurological disease, evidence of systemic infection Patients with concomitant prolapse were also included, and some underwent concomitant repair Participants well matched for baseline characteristics | |
| Interventions | TVT‐Secur (42) TVTO (44) | |
| Outcomes | Reported at 12 weeks and 1 year Primary outcomes: objective failure (SUI demonstrated on cough test) Secondary outcomes: quality of life symptom questionnaires (PFDI‐20, PFIQ‐7), postoperative pain, mesh erosion or exposure, intraoperative estimated blood loss, length of procedure, postoperative pain (verbal analogue scale), need for sling revision, length of catheterisation postoperatively, need for second anti‐incontinence procedure | |
| Notes | Power analysis recommended 67 participants in each arm, but study was stopped early because of "several investigators voicing concerns about an increasing number of positive post‐operative CST in women undergoing TVT‐S." The study is therefore underpowered, and this unplanned interim analysis represents a high risk of bias | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Women were randomized in a 1:1 allocation" |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque, sealed envelopes used |
| Incomplete outcome data (attrition bias) | High risk | Study terminated early, therefore underrecruited |
| Blinding of participants and personnel (performance bias) | High risk | Neither surgeon nor participants blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Prospective RCT of TVT‐Secur versus TOT | |
| Participants | 40 women with SUI | |
| Interventions | TVT‐Secur (20) TOT (20) | |
| Outcomes | Urodynamics, KHQ, subjective cure, operative complications | |
| Notes | Abstract only. Minimal details on randomisation and methodology to allow judgement of the reliability of outcomes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Prospective single‐centre RCT | |
| Participants | 60 women with SUI | |
| Interventions | TVT‐Secur (38) CureMesh (22) | |
| Outcomes | Primary outcome: objective cure (no leakage on cough test with full bladder at 1 year) Secondary outcomes: participant perception of urgency severity, IQoL, BFLUTS, VAS | |
| Notes | Conference abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "women with SUI were randomly assigned" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described. Given the unequal allocation, this could be a significant risk |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Prospective, multi‐centre RCT of U‐ and H‐type methods of TVT‐Secur | |
| Participants | 285 women with urodynamic SUI, or MUI with predominant SUI Exclusion criteria: pelvic organ prolapse > stage 2; intention to have more children; neurological disease Age, menopausal status percentage of women with DO and number of urgency episodes were not balanced between groups | |
| Interventions | U‐type TVT Secur (165) H‐type TVT Secur (165) | |
| Outcomes | Primary outcome: objective cure (no leakage on stress test), subjective cure (response to Sandvik questionnaire) Secondary outcomes: Sandvik questionnaire, I‐QOL, ICIQ‐FLUTS, I‐VAS, 3‐day voiding diary | |
| Notes | 330 women recruited, 45 not in final analysis (including 28 lost to follow‐up at 1 year) from 41375 ICS abstract with 2‐year data on the same participants in Kim 2010. Five papers refer to the same study; Kim 2010 is a single‐centre report from the multi‐centre study, whereas Lee 2010 and 2011 are reports of the multi‐centre study. Data from the mutli‐centre study have been used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "the centre applied a stratified and permuted block randomisation method" |
| Allocation concealment (selection bias) | High risk | Quote: "consenting patients were randomly allocated in the operating room" |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data adequately analysed |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unclear whether participants were blinded; surgeons could not be blinded because of a difference in technique |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Prospective, single‐centre RCT of MiniArc versus Monarc | |
| Participants | 224 women with SUI or urodynamic stress incontinence Exclusion criteria: intrinsic sphincter deficiency; previous MUS; untreated DO; significant voiding dysfunction Patients who had previous SUI surgery were included Groups well matched at baseline | |
| Interventions | MiniArc (112) Monarc (112) | |
| Outcomes | Primary outcomes: objective cure (negative urodynamic stress or cough stress test), subjective cure (absence of participant‐reported SUI) Secondary outcomes: ICIQ‐SF, ICIQ OAB, PISQ12, IIQ‐7, PGII questionnaires, 24‐hr pad weight gain | |
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Computer‐generated random allocation was concealed and stratified to centre" |
| Allocation concealment (selection bias) | Unclear risk | As above, method not described |
| Incomplete outcome data (attrition bias) | Low risk | All randomly assigned participants completed follow‐up |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "Surgeons or patients were not blinded once allocation was revealed" |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Quasi‐randomised, single‐centre RCT of H‐type versus U‐type TVT‐Secur | |
| Participants | 87 women with SUI | |
| Interventions | H‐type TVT‐Secur (45) U‐type TVT‐Secur (42) | |
| Outcomes | Objective cure (absence of urine leakage on cough test), subjective cure (simple questionnaire), urodynamics. | |
| Notes | Prospective study but not adequately randomly assigned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Patients were allocated alternatively" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | High risk | 5 participants did not attend follow‐up and were excluded |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Prospective, pilot RCT comparing Ajust and TVT‐O | |
| Participants | 29 women with SUI Inclusion criteria: SUI or MUI with predominant SUI; women undergoing primary incontinence surgery; BMI < 35; previously failed or declined PFMT Exclusion criteria: predominant OAB; unwilling for randomisation; inability to understand English; concomitant surgery; patients requiring postoperative hospital stay for medical/social reasons Well matched for baseline characteristics | |
| Interventions | TVT‐O (15) Ajust (14) | |
| Outcomes | Primary outcomes: feasibility of recruitment and randomisation, acceptability and feasibility of the use of local anaesthetic in the mini‐sling arm Secondary outcomes: complications and short‐term success rate | |
| Notes | This report was submitted as a thesis for fulfilment of a bachelor of medicine degree and was primarily a feasibility study, but it reported on efficacy and complication rates as secondary outcome measures and is therefore included | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence used |
| Allocation concealment (selection bias) | Low risk | Allocation sequence kept electronically and concealed in opaque envelopes |
| Incomplete outcome data (attrition bias) | Low risk | Data available for all participants at 4‐week follow‐up. 2 participants unavailable for 3‐month follow‐up in TVT‐O arm |
| Blinding of participants and personnel (performance bias) | High risk | Neither participants nor surgeons blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Reported as beyond available resources for this small study, but assessments done by individuals not involved directly with index procedure |
| Methods | Prospective multi‐centre RCT comparing MiniArc versus Ajust system | |
| Participants | 66 women with previously untreated SUI | |
| Interventions | MiniArc (33) Ajust (33) | |
| Outcomes | Subjective cure assessed by 5‐point Likert scale, objective cure assessed by cough test | |
| Notes | Abstract only. English summary of results from Martan 2011 study. 43009 Non‐English abstract. Study results presented in Martan 2012 abstract (English), which has been included | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Women were randomly allocated by the envelope method" |
| Allocation concealment (selection bias) | Low risk | "Women were randomly allocated by the envelope method" |
| Incomplete outcome data (attrition bias) | Unclear risk | 3 participants did not complete 24‐month follow‐up. ITT analysis not done |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Prospective, single‐centre RCT comparing TVT‐S U and H‐types versus TVT‐O | |
| Participants | 197 women with proven urodynamic stress incontinence who had failed conservative therapy Exclusion criteria: predominant UUI, urodynamic detrusor instability, previous failed anti‐incontinence surgery, previous radiotherapy, PVR > 100 mL, bladder capacity < 300 mL, >= stage 2 pelvic organ prolapse, planned concomitant surgery, immobile urethra Well‐matched groups at baseline | |
| Interventions | TVT‐O (68) TVT‐S (H‐type) (64) TVT‐S (U‐type) (65) | |
| Outcomes | Primary outcomes: objective cure (stress test), subjective cure (ICIQ‐SF) Secondary outcomes: IQoL questionnaires, ultrasound examination, intraoperative and postoperative complications | |
| Notes | Unplanned interim analysis performed at two years; high failure rate in TVT‐S group, which calls into question the risk of bias due to unblinding of outcome assessors. After this interim analysis at two years, the study was only stopped at 3 years once "the minimum number of patients needed for final statistical analysis was achieved" Multiple papers included under this study heading, all referring to the same trial | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “We implemented randomization by placing pieces of paper containing the randomization allocation in sealed envelopes which were arranged for sequential opening” |
| Allocation concealment (selection bias) | Low risk | “We implemented randomization by placing pieces of paper containing the randomization allocation in sealed envelopes which were arranged for sequential opening” |
| Incomplete outcome data (attrition bias) | Unclear risk | Unplanned interim analysis, but adequate numbers recruited as per power calculation |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "The patients were not blinded" |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Multi‐centre prospective randomised study comparing Ajust versus TVT‐O | |
| Participants | 137 women with SUI who have failed or declined PFMT, undergoing primary anti‐incontinence procedure with the ability to understand the information leaflet Exclusion criteria: mixed incontinence with uncontrolled OAB symptoms or neurological symptoms such as MS | |
| Interventions | SIMS‐Ajust (69) performed under LA as an opt‐out policy TVT‐O (68) under GA | |
| Outcomes | Primary outcome: postoperative pain profile up to 4 weeks postoperatively Secondary outcomes: participant‐reported and objective success rates (cough stress test), reoperation rates, ICIQ‐FLUTS, KHQ, PISQ‐12, UPS, PGI‐I questionnaires | |
| Notes | Multiple reports of same trial. Full report from European Journal of Obstetrics & Gynaecology 2012 used as primary source of data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Block randomisation was done for each centre using number allocation software" |
| Allocation concealment (selection bias) | Low risk | Quote: "allocation to each group was performed via a telephone randomisation" |
| Incomplete outcome data (attrition bias) | Unclear risk | 8 lost to follow‐up in TVT‐O arm; sensitivity analysis performed but not reported in abstract |
| Blinding of participants and personnel (performance bias) | High risk | Participants could not be blinded, as only Ajust was done under LA |
| Blinding of outcome assessment (detection bias) | Low risk | Follow‐up conducted by an independent researcher who was blinded to type of procedure |
| Methods | Exploratory randomised phase 2 trial | |
| Participants | 90 women with clinically and urodynamically proven SUI and urethral hypermobility Exclusion criteria: previous surgery for SUI; genital prolapse >= stage 2 (by POP‐Q score); complaints of urgency, frequency, nocturia or demonstrable detrusor overactivity | |
| Interventions | TVT‐O (30), TVT‐SECUR (30) or MiniArc (30) | |
| Outcomes | Primary outcome: cure rate (considered cured if participants did not report any episodes of urine leakage, ceased to wear incontinence protection and had a negative cough test) Secondary outcomes: KHQ | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | All participant outcome data assessed adequately |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Multi‐centre, prospective RCT comparing three vaginal kits of single‐incision mini‐slings (Ajust, MiniArc and TVT‐Secur) | |
| Participants | 120 women with SUI who remained incontinent after at least three months of PFMT, or patients with MUI who had clinically demonstrable SUI while on oral antimuscarinic therapy Participants well matched for baseline characteristics. None had significant pelvic organ prolapse | |
| Interventions | Ajust (40), MiniArc (40) and TVT‐Secur (40) | |
| Outcomes | Operative time, blood loss, intraoperative and postoperative complications, feasibility (number of surgeries completed under local anaesthesia/total number of surgeries), degree of surgical difficulty, number of analgesic vials, participant satisfaction (using a visual analogue scale (VAS) ranging from 0 (absolutely unsatisfied) to 10 (completely satisfied) administered at hospital discharge) and postoperative pain | |
| Notes | Only surgical data reported in this paper. Data analysed by ITT | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The random allocation sequence was made in single blocks, using a single sequence of random assignment, obtained with the use of a computer‐generated randomization list" |
| Allocation concealment (selection bias) | Low risk | Quote: "The sequence was concealed from all investigators until the interventions were assigned using sequentially numbered opaque sealed envelopes, prepared distant from the study site, until surgeries were assigned (before entering the operating room)" |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data given for all enrolled participants |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "The study protocol was double‐blind, i.e. patients and data assessors were masked to the SIMS assigned" |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The study protocol was double blind, i.e., patients and data assessors were masked to the SIMS assigned" |
| Methods | Prospective RCT of TVT‐Secur versus MiniArc | |
| Participants | 110 women with at least one‐year symptomatic SUI | |
| Interventions | TVT‐SECUR (60) versus Mini‐Arc (50) | |
| Outcomes | Primary outcome: cure rate (absence of incontinence) | |
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "The randomisation was: each physician explained the pathology and the technique to use, offering only one" Comment: inadequate randomisation methods |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data available for all participants |
| Blinding of participants and personnel (performance bias) | High risk | Unblinded (from the description of randomisation) |
| Blinding of outcome assessment (detection bias) | High risk | As above |
| Methods | Single‐blind RCT comparing TVT‐O with Ajust in 2:1 design | |
| Participants | 156 women with clinically proven SUI (stress test) | |
| Interventions | Ajust (92) versus TVT‐O (51) | |
| Outcomes | Main outcomes were surgery‐related pain, efficacy and complications. Physical exam including cough stress test, UDI, IIQ, PGIS, PGII questionnaires. | |
| Notes | Abstract only. Reported before end of recruitment and some outcome measures reported at 6 weeks, others at 6 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | High risk | 7 women withdrew after randomisation, 3 received the wrong type of sling after allocation and were excluded, and 3 were yet to receive intervention at the time of writing. No ITT analysis |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "Women were blinded to the type of procedure by using a sham skin incision in the Ajust group" |
| Blinding of outcome assessment (detection bias) | High risk | Surgeon not blinded. Single‐blind trial |
| Methods | Prospective, single‐centre RCT comparing TVT‐O versus TVT‐Secur | |
| Participants | 80 women with SUI, reportedly well matched for baseline characteristics | |
| Interventions | TVT‐O (39) vs TVT‐S (41) | |
| Outcomes | Outcomes assessed at 3 and 12 months: physical exam, voiding diary, urodynamics, Stamey symptom severity scale, VAS (pain). Sandvik questionnaire for surgical outcomes assessed at 6 hours postoperatively. Unclear which was the primary outcome | |
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly assigned" Comment: limited information from abstract |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Unclear risk | Limited information available from abstract |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | 5‐Year results of prospective RCT of TOT versus TFS (tissue fixation system) | |
| Participants | 80 female patients with only urodynamically proven SUI. Exclusions: patients with overflow incontinence, those with OAB and those who underwent previous anti‐incontinence surgery Groups well matched for baseline characteristics | |
| Interventions | Group 1: TOT (40) Group 2: TFS (40) | |
| Outcomes | Simplified QoL score (grade 1‐5 to describe the limitation of normal activities by incontinence), CSPT (preweighed pad placed on vulva and participant with full bladder, asked to cough ten times. Pad weight increase greater than 1 gm assessed as positive, less than 1 gm assessed as negative) At 5 years: If supine, CSPT negative after the operation and participant reported restoration of continence, it was regarded as an objective cure. If participant reported restoration of continence but the supine CSPT was positive, it was regarded as subjective cure. If there was no change in incontinence after the operation, it was regarded as failure. Primary outcome measures: objective cure, subjective cure and failure at 5 years Secondary outcome measures: procedure duration, postoperative groin pain, postoperative urinary retention and mesh extrusion | |
| Notes | 4 participants from each group lost to follow‐up at 5 years. Not powered, as there were no published long‐term data on TOT/TFS at the time of starting the trial to perform a power analysis. Sample size chosen based on "expectations and practical considerations" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "participants were randomly allocated according to a computer program" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | 4 patients in each group lost to follow‐up because of moving away from the area |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Post‐operative assessment conducted by a senior surgeon at the urogynaecology clinic who did not participate in the operations" |
| Methods | Interim analysis of a prospective, randomised, non‐blinded study at a single institution | |
| Participants | Patients with urodynamically proven SUI, excluding those who had previous anti‐incontinence surgery, urodynamically diagnosed ISD (VLPP < 60 and/or MUCP < 40) or mixed incontinence with predominant detrusor overactivity. Groups well matched for baseline characteristics | |
| Interventions | Transobturator (Monarc) (38) or single incision (MiniArc) (43) | |
| Outcomes | Primary outcome: presence or absence of urine leakage on standard cough stress test Secondary outcomes: intraoperative data, UDI‐6, IIQ‐7, ICIQ and 3‐day voiding diary | |
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Allocation to treatment group was performed by a computer generated randomsation scheme and both surgeon and patient were blinded to allocation until onset of anaesthesia" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | High risk | Interim analysis. Aim to randomly assign 80 participants, 40 in each group. Only follow‐up of 24 in each arm included |
| Blinding of participants and personnel (performance bias) | High risk | Surgeons not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Described as a non‐blinded study but no further details given |
| Methods | Prospective randomised study of TVT‐O versus MiniArc versus Ajust | |
| Participants | 43 institutionalised elderly patients (nursing home residents) with predominant SUI | |
| Interventions | TVT‐O versus MiniArc versus Ajust | |
| Outcomes | ICIQ, intraoperative complications, de novo urgency, success rate | |
| Notes | Czech article with abstract in English but no usable data in abstract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Prospective, single‐centre RCT of TVT‐O versus TVT‐Secur | |
| Participants | 84 women with urodynamically proven SUI and symptomatic for at least 2 years Exclusion criteria: previous surgical/pharmacological treatment of SUI, predominant urge incontinence, genital prolapse >= stage 2, serious contraindication to surgery Groups were well matched for baseline characteristics | |
| Interventions | TVT‐Secur (37) versus TVT‐O (38) | |
| Outcomes | Primary outcome: objective sure of SUI (during cough test and exertion required in urodynamic evaluation) Secondary outcomes: duration of procedure, complications, PVR, ICIQ‐SF, KHQ, urinary diary | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomization list generated by a computer" |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Incomplete outcome data (attrition bias) | High risk | Outcome data provided for only 75 participants, others excluded as they did not complete follow‐up |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "patients were left blinded to the devices used until the end of the procedure" Comment: unclear as to whether this means participant blind was broken after the procedure Quote: "surgeon was obviously not blinded to the technique being used" |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Prospective RCT comparing TVT, TVT‐O and TVT‐Secur | |
| Participants | 102 women with SUI Exclusion criteria: previous surgery for SUI | |
| Interventions | TVT (32), TVT‐O (36) and TVT‐Secur (34) | |
| Outcomes | Primary outcome: cure (defined as negative cough stress test and absence of urine leak by subjective sense) Secondary outcomes: surgical time, blood loss, complications | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "patients were assigned by random allocation (computer generated)" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote: "allocation was concealed using opaque sealed envelopes" Comment: probably done |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data available for all 102 participants |
| Blinding of participants and personnel (performance bias) | High risk | Surgeon blinding not possible because of the nature of the techniques |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Methods | Prospective RCT of Contasure Needleless versus TOT | |
| Participants | 103 women with SUI | |
| Interventions | Contasure Needleless (52) versus TOT (51) | |
| Outcomes | 3‐Day frequency‐volume chart, PVR, symptom questionnaire, complications, operative time, symptoms | |
| Notes | Abstract only; 4‐week follow‐up period | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "(patients) were randomly divided into two groups according to their procedure" Comment: methods unclear |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Unclear risk | Limited information available from abstract |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
Abbreviations:
BMI: Body Mass Index
CST: Cough Stress Test
GA: General Anaesthetic
ICIQ‐SF: International Consultation on Incontinence Questionnaire – Short Form
ITT: Intention To Treat
KHQ: Kings Health Questionnaire
LA: Local Anaesthetic
MUCP: Mean Urethral Closure pressure
MUI: Mixed Urinary Incontinence
PFMT: Pelvic Floor Muscle Training
POP‐Q: Pelvic Organ Prolapse Quotient
PVR: Post‐Void Residual
QoL: Quality of Life
RCT: Randomised Controlled Trial
SUI: Stress Urinary Incontinence
TVT: Tension‐free Vaginal Tape
UDI: Urogenital Distress Inventory
USI: Urodynamic Stress Incontinence
UTI: Urinary Tract Infection
VAS: Visual Analogue Scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Randomised trial of local versus general anaesthesia, all had TVT procedure | |
| This is an ongoing prospective, multi‐centre registry. Not an RCT | |
| Comparator is not a single‐incision sling | |
| No mini‐sling comparator arm (TVT‐O vs another) | |
| Non‐randomised study correlating ultrasound findings with clinical signs of cure or failure in a subset of participants who had undergone TVT‐Secur (mini‐sling) from an RCT | |
| Experimental interventions do not conform to the definition of single‐incision slings | |
| This study compares pelvic organ prolapse (POP) repair plus mini‐sling versus POP repair alone |
Abbreviations:
TVT: Tension‐free Vaginal Tape
RCT: Randomised Controlled Trial
POP: Pelvic Organ Prolapse
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | This paper is in Russian; we were unable to obtain a copy and an English translation. We hope to include this in future updates |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | A randomised trial comparing two vaginal prolene sling surgeries for female urinary incontinence |
| Methods | RCT |
| Participants | Women with USI and no need for concomitant surgery |
| Interventions | Monarc versus MiniArc |
| Outcomes | Postoperative pain score assessed by visual analogue scale, continence rates (2‐day bladder diary), blood loss |
| Starting date | January 2012, target enrolment 50 |
| Contact information | Dr Andrew Foote |
| Notes | Identified from ANZCTR |
| Trial name or title | Trial comparing TVT‐Secur system and transvaginal obturator tape for surgical management of stress urinary incontinence |
| Methods | RCT |
| Participants | Women with clinically demonstrable SUI (cough test) but no POP > stage 1, predominant UUI or DO |
| Interventions | TVT‐Secur versus TVT‐O |
| Outcomes | Objective cure (cough test) |
| Starting date | May 2008, target enrolment 106 |
| Contact information | Ken D Maslow, St Boniface Hospital, Canada |
| Notes | Identified from clinicaltrials.gov |
| Trial name or title | Transvaginal tape (TVT)‐Secur versus TVT: a randomised controlled trial |
| Methods | RCT |
| Participants | Women with SUI not requiring prolapse surgery |
| Interventions | TVT‐Secur versus TVT |
| Outcomes | Objective cure (pad test, < 1 g increase in pad weight), subjective cure, UDI‐6, IIQ‐7, voiding dysfunction, sexual function, surgical complications, |
| Starting date | May 2008, target enrolment 74 |
| Contact information | Magaly Robert, University of Calgary |
| Notes | Identified from clinicaltrials.gov |
| Trial name or title | Tension‐free vaginal tape (TVT) Abbrevo and MiniArc sub‐urethral sling in women with stress urinary incontinence—a randomised controlled trial |
| Methods | RCT |
| Participants | Women 18 to 80 years of age with USI but not ISD enrolled from the urodynamic clinic |
| Interventions | TVT Abbrevo and MiniArc |
| Outcomes | Objective cure (cough test), subjective cure (ICIQ‐SF), IIQ‐7, PGI‐I, sexual function (PISQ‐12) |
| Starting date | December 2011, target sample 230 |
| Contact information | |
| Notes | Identified from ANZCTR |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women with urinary incontinence Show forest plot | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 6.1  Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 1 Number of women with urinary incontinence. | ||||
| 1.1 Bottom‐up approach | 5 | 573 | Risk Ratio (M‐H, Random, 95% CI) | 2.08 [1.04, 4.14] |
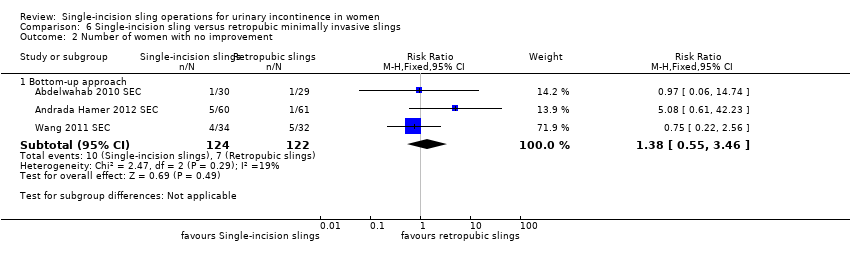
| 2 Number of women with no improvement Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.2 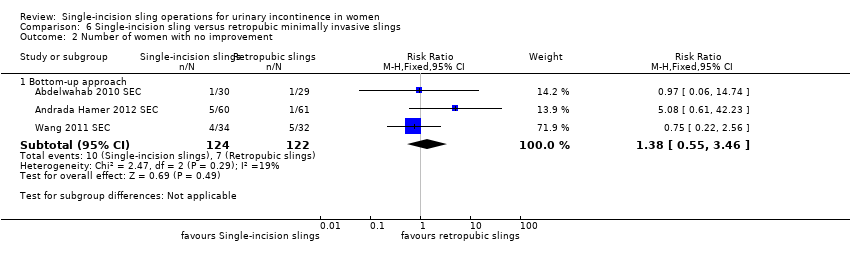 Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 2 Number of women with no improvement. | ||||
| 2.1 Bottom‐up approach | 3 | 246 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.38 [0.55, 3.46] |
| 3 Objectve measurement of incontinence Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.3  Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 3 Objectve measurement of incontinence. | ||||
| 3.1 Bottom‐up approach | 2 | 188 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.44 [2.06, 9.56] |
| 4 Condition‐specific health measures Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.4  Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 4 Condition‐specific health measures. | ||||
| 4.1 Bottom‐up approach | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Duration of operation (in minutes) Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 6.5  Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 5 Duration of operation (in minutes). | ||||
| 5.1 Bottom‐up approach | 3 | 386 | Mean Difference (IV, Random, 95% CI) | ‐17.33 [‐32.09, ‐2.57] |
| 6 Operative blood loss Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.6 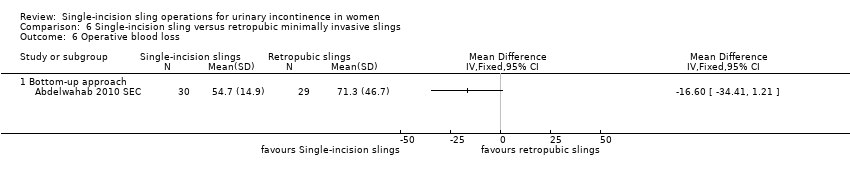 Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 6 Operative blood loss. | ||||
| 6.1 Bottom‐up approach | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Length of in‐patient stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.7 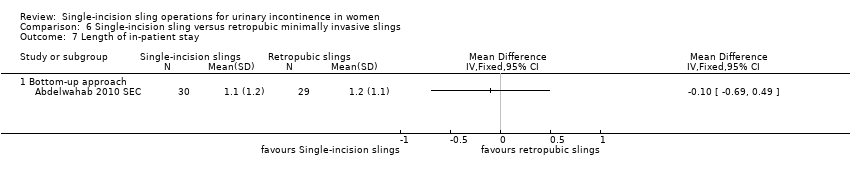 Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 7 Length of in‐patient stay. | ||||
| 7.1 Bottom‐up approach | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Major vascular or visceral injury Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.8 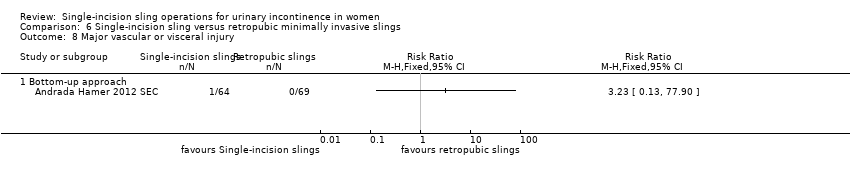 Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 8 Major vascular or visceral injury. | ||||
| 8.1 Bottom‐up approach | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Vaginal wall perforation Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.9  Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 9 Vaginal wall perforation. | ||||
| 9.1 Bottom‐up approach | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Bladder or urethral perforation Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.10 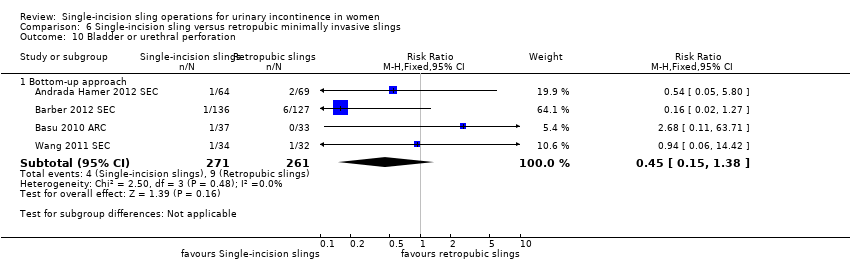 Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 10 Bladder or urethral perforation. | ||||
| 10.1 Bottom‐up approach | 4 | 532 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.15, 1.38] |
| 11 Urinary retention and need for catheterisation Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.11  Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 11 Urinary retention and need for catheterisation. | ||||
| 11.1 Bottom‐up approach | 5 | 578 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.38, 1.99] |
| 12 Infection related to use of synthetic mesh Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.12  Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 12 Infection related to use of synthetic mesh. | ||||
| 12.1 Bottom‐up approach | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.22, 17.89] |
| 13 Vaginal mesh exposure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.13  Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 13 Vaginal mesh exposure. | ||||
| 13.1 Bottom‐up approach | 2 | 333 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.23, 8.16] |
| 14 Mesh extrusion into the bladder or urethra Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.14  Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 14 Mesh extrusion into the bladder or urethra. | ||||
| 14.1 Bottom‐up approach | 3 | 445 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.19, 3.01] |
| 15 Long‐term pain or discomfort Show forest plot | 2 | 329 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 6.15  Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 15 Long‐term pain or discomfort. | ||||
| 15.1 Bottom‐up approach | 2 | 329 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
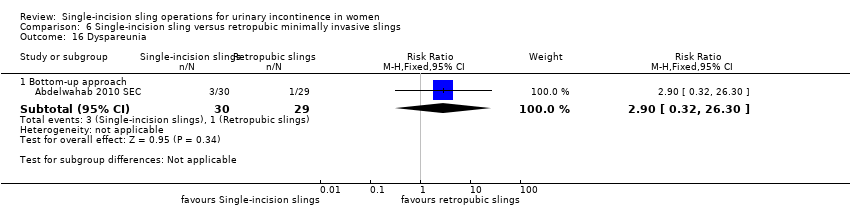
| 16 Dyspareunia Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.16 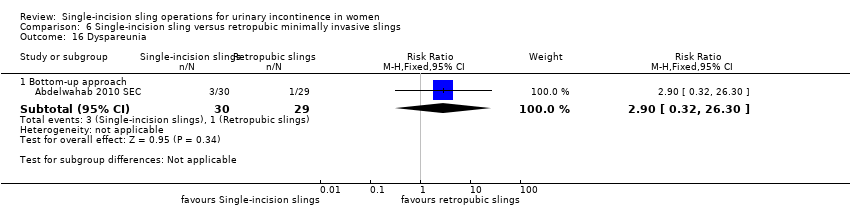 Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 16 Dyspareunia. | ||||
| 16.1 Bottom‐up approach | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.9 [0.32, 26.30] |
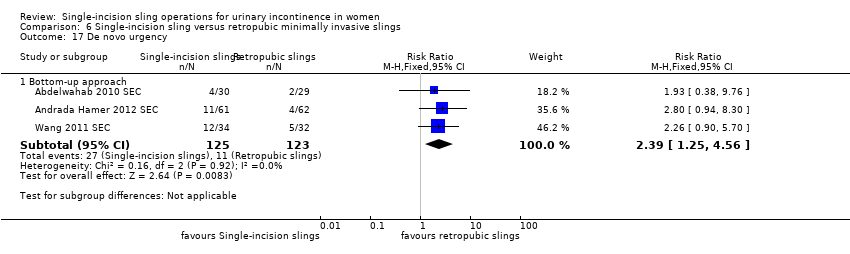
| 17 De novo urgency Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.17 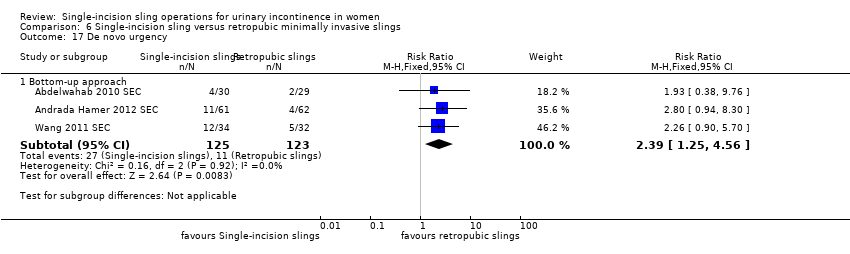 Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 17 De novo urgency. | ||||
| 17.1 Bottom‐up approach | 3 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.39 [1.25, 4.56] |
| 18 New‐onset detrusor overactivity Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.18  Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 18 New‐onset detrusor overactivity. | ||||
| 18.1 Bottom‐up approach | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.13, 5.98] |
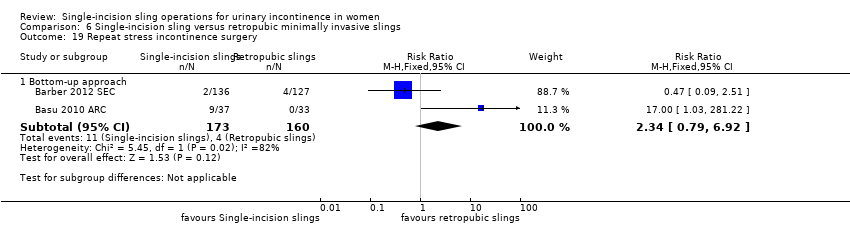
| 19 Repeat stress incontinence surgery Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.19 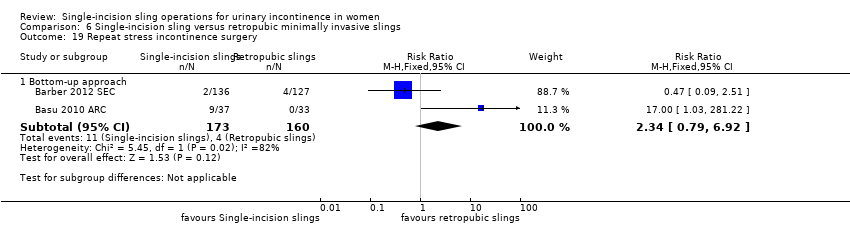 Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 19 Repeat stress incontinence surgery. | ||||
| 19.1 Bottom‐up approach | 2 | 333 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.34 [0.79, 6.92] |
| 20 Need for any other additional or new surgical procedure to treat complications Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.20  Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 20 Need for any other additional or new surgical procedure to treat complications. | ||||
| 20.1 Bottom‐up approach | 2 | 333 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.29, 4.74] |
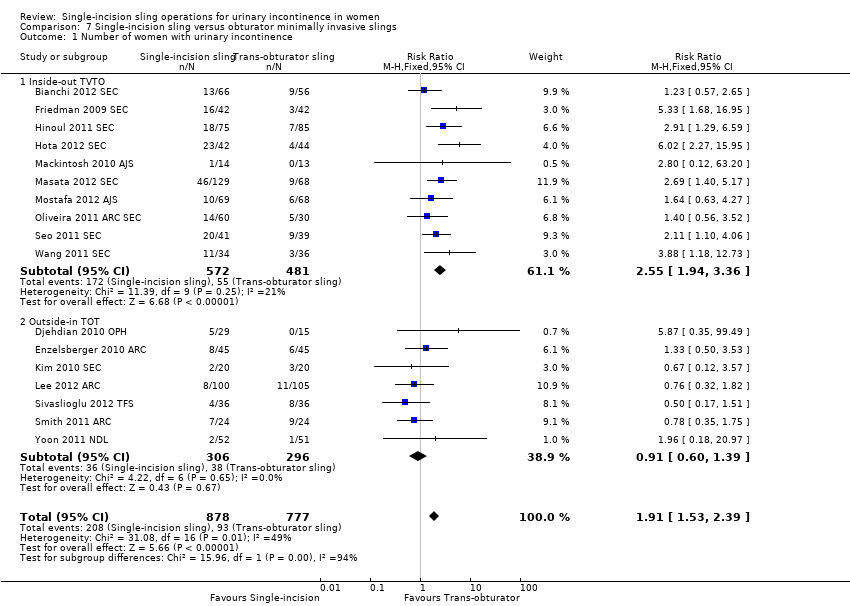
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women with urinary incontinence Show forest plot | 17 | 1655 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.91 [1.53, 2.39] |
| Analysis 7.1 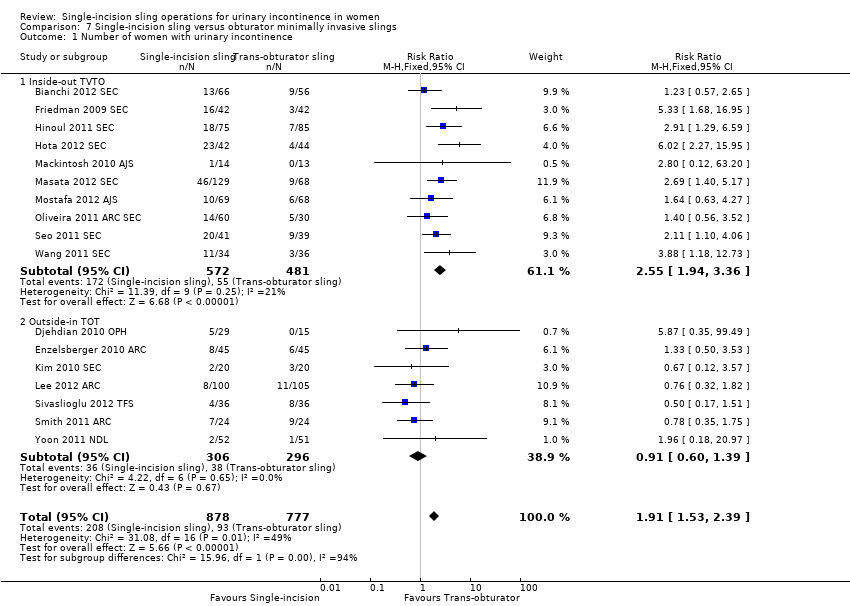 Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 1 Number of women with urinary incontinence. | ||||
| 1.1 Inside‐out TVTO | 10 | 1053 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.55 [1.94, 3.36] |
| 1.2 Outside‐in TOT | 7 | 602 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.60, 1.39] |
| 2 Number of women with no improvement Show forest plot | 5 | 642 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.29 [1.29, 4.06] |
| Analysis 7.2 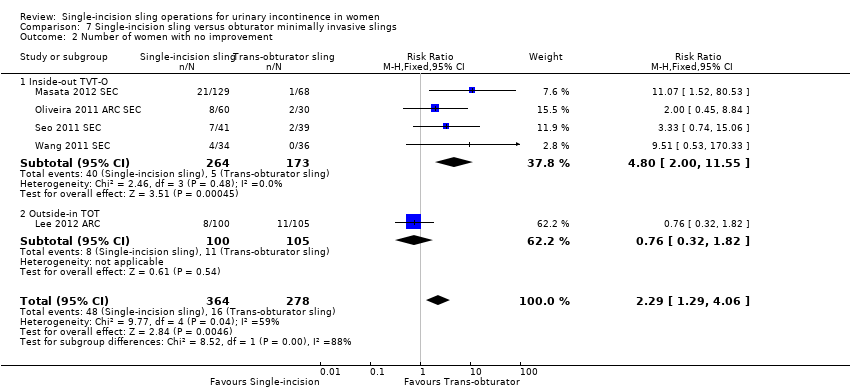 Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 2 Number of women with no improvement. | ||||
| 2.1 Inside‐out TVT‐O | 4 | 437 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.80 [2.00, 11.55] |
| 2.2 Outside‐in TOT | 1 | 205 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.32, 1.82] |
| 3 Objective measurement of incontinence Show forest plot | 12 | 1198 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.88 [1.49, 2.36] |
| Analysis 7.3  Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 3 Objective measurement of incontinence. | ||||
| 3.1 Inside‐out TVT‐O | 7 | 804 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.91 [2.00, 4.25] |
| 3.2 Outside‐in TOT | 5 | 394 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.90, 1.55] |
| 4 Incontinence episodes Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.4  Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 4 Incontinence episodes. | ||||
| 4.1 Outside‐in TOT | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Pad test (weights) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 7.5  Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 5 Pad test (weights). | ||||
| 5.1 Outside‐in TOT | 2 | 268 | Mean Difference (IV, Fixed, 95% CI) | ‐1.64 [‐6.24, 2.96] |
| 6 Condition‐specific health measures Show forest plot | 3 | 334 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.16 [‐0.06, 0.38] |
| Analysis 7.6 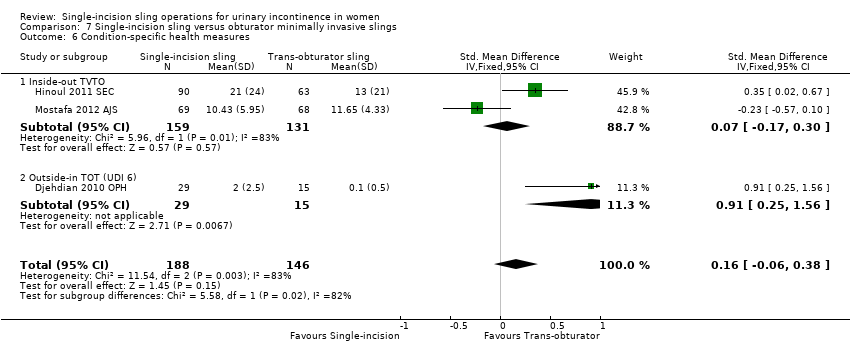 Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 6 Condition‐specific health measures. | ||||
| 6.1 Inside‐out TVTO | 2 | 290 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.17, 0.30] |
| 6.2 Outside‐in TOT (UDI 6) | 1 | 44 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.91 [0.25, 1.56] |
| 7 Duration of operation (minutes) Show forest plot | 9 | 1176 | Mean Difference (IV, Fixed, 95% CI) | ‐1.17 [‐1.60, ‐0.75] |
| Analysis 7.7  Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 7 Duration of operation (minutes). | ||||
| 7.1 Inside‐out TVTO | 6 | 759 | Mean Difference (IV, Fixed, 95% CI) | ‐1.06 [‐1.50, ‐0.61] |
| 7.2 Outside‐in TOT | 3 | 417 | Mean Difference (IV, Fixed, 95% CI) | ‐2.14 [‐3.43, ‐0.84] |
| 8 Operative blood loss (mL) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 7.8  Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 8 Operative blood loss (mL). | ||||
| 8.1 Inside‐out TVTO | 2 | 320 | Mean Difference (IV, Fixed, 95% CI) | 18.79 [3.70, 33.88] |
| 9 Length of in‐patient stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 7.9  Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 9 Length of in‐patient stay. | ||||
| 9.1 Inside‐out TVTO | 1 | 188 | Mean Difference (IV, Fixed, 95% CI) | ‐0.08 [‐0.33, 0.17] |
| 10 Major vascular or visceral injury Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 7.10 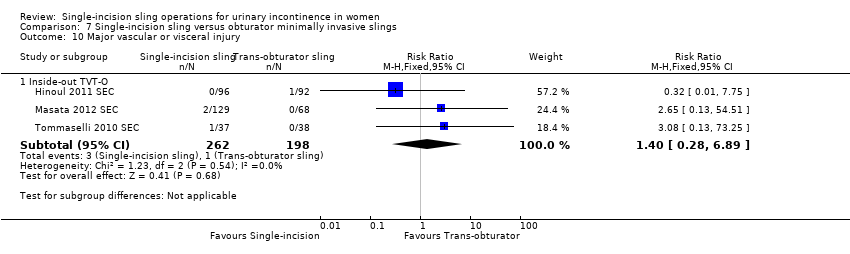 Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 10 Major vascular or visceral injury. | ||||
| 10.1 Inside‐out TVT‐O | 3 | 460 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.28, 6.89] |
| 11 Bladder or urethral perforation Show forest plot | 9 | 961 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.32, 5.02] |
| Analysis 7.11 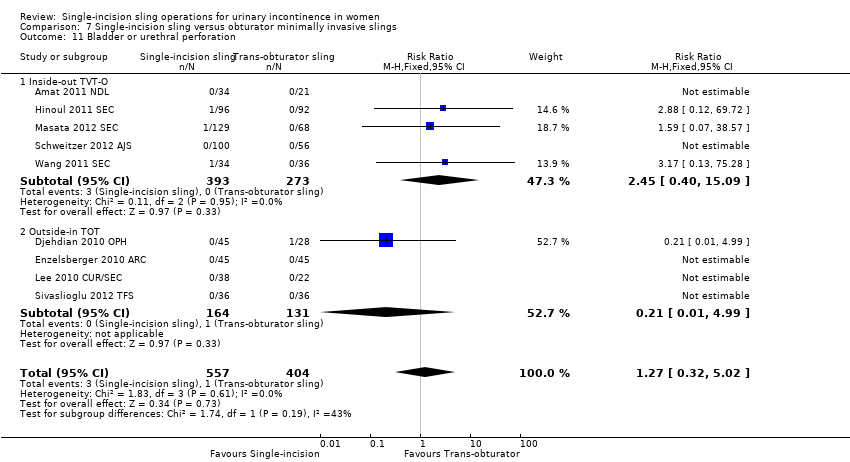 Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 11 Bladder or urethral perforation. | ||||
| 11.1 Inside‐out TVT‐O | 5 | 666 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.45 [0.40, 15.09] |
| 11.2 Outside‐in TOT | 4 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.01, 4.99] |
| 12 Vaginal wall perforation Show forest plot | 6 | 788 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.41, 6.81] |
| Analysis 7.12 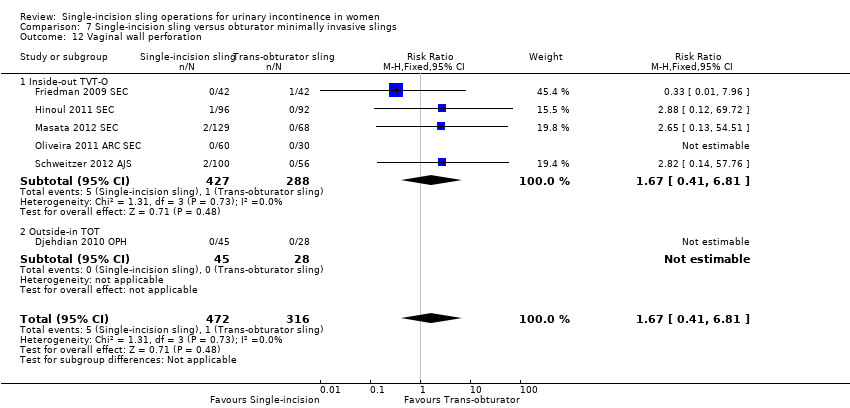 Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 12 Vaginal wall perforation. | ||||
| 12.1 Inside‐out TVT‐O | 5 | 715 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.41, 6.81] |
| 12.2 Outside‐in TOT | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Urinary retention and need for catheterisation Show forest plot | 15 | 1477 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.28, 1.15] |
| Analysis 7.13  Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 13 Urinary retention and need for catheterisation. | ||||
| 13.1 Inside‐out TVTO | 10 | 996 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.34, 1.52] |
| 13.2 Outside‐in TOT | 5 | 481 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.08, 3.44] |
| 14 Infection related to use of synthetic mesh Show forest plot | 2 | 412 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.09, 2.69] |
| Analysis 7.14  Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 14 Infection related to use of synthetic mesh. | ||||
| 14.1 Inside‐out TVT‐O | 1 | 188 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.88 [0.12, 69.72] |
| 14.2 Outside‐in TOT | 1 | 224 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.73] |
| 15 Vaginal mesh exposure Show forest plot | 9 | 819 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.59 [1.21, 5.56] |
| Analysis 7.15  Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 15 Vaginal mesh exposure. | ||||
| 15.1 Inside‐out TVT‐O | 5 | 562 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.75 [1.42, 9.86] |
| 15.2 Outside‐in TOT | 4 | 257 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.27, 4.28] |
| 16 Mesh extrusion into the bladder or urethra Show forest plot | 2 | 146 | Risk Ratio (M‐H, Fixed, 95% CI) | 17.79 [1.06, 298.88] |
| Analysis 7.16  Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 16 Mesh extrusion into the bladder or urethra. | ||||
| 16.1 Inside‐out TVT‐O | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 17.79 [1.06, 298.88] |
| 16.2 Outside‐in TOT | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Postoperative pain or discomfort Show forest plot | 9 | 1102 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.19, 0.37] |
| Analysis 7.17 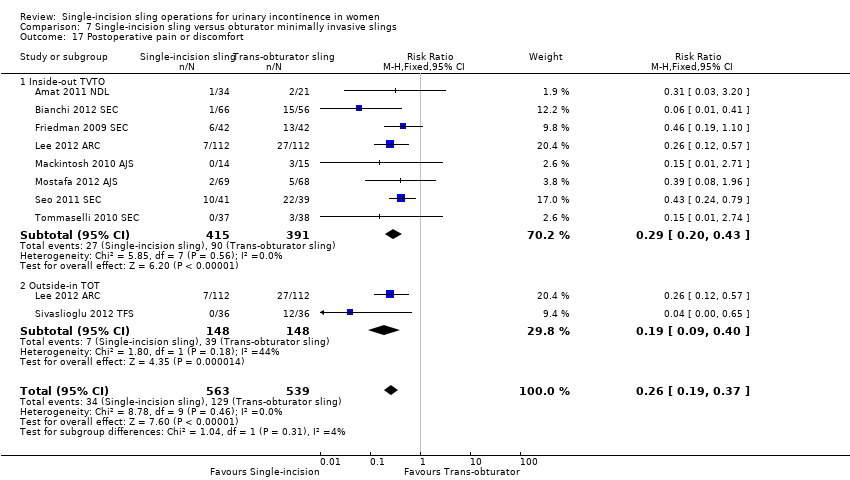 Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 17 Postoperative pain or discomfort. | ||||
| 17.1 Inside‐out TVTO | 8 | 806 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.20, 0.43] |
| 17.2 Outside‐in TOT | 2 | 296 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.09, 0.40] |
| 18 Long‐term pain or discomfort Show forest plot | 5 | 351 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.04, 0.54] |
| Analysis 7.18  Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 18 Long‐term pain or discomfort. | ||||
| 18.1 Inside‐out TVT‐O | 3 | 235 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.03, 1.07] |
| 18.2 Outside‐in TOT | 2 | 116 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.02, 0.82] |
| 19 De novo urgency Show forest plot | 10 | 927 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.41 [0.98, 2.03] |
| Analysis 7.19 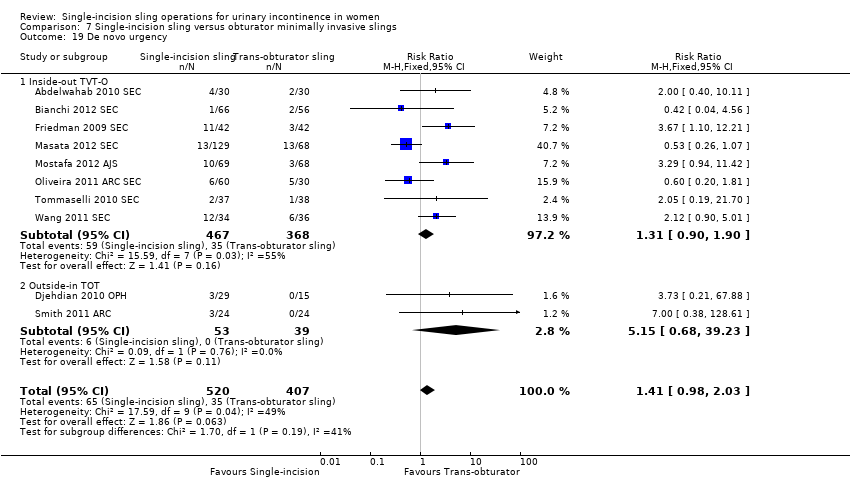 Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 19 De novo urgency. | ||||
| 19.1 Inside‐out TVT‐O | 8 | 835 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.90, 1.90] |
| 19.2 Outside‐in TOT | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.15 [0.68, 39.23] |
| 20 Repeat stress incontinence surgery Show forest plot | 6 | 764 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.09 [1.48, 6.49] |
| Analysis 7.20 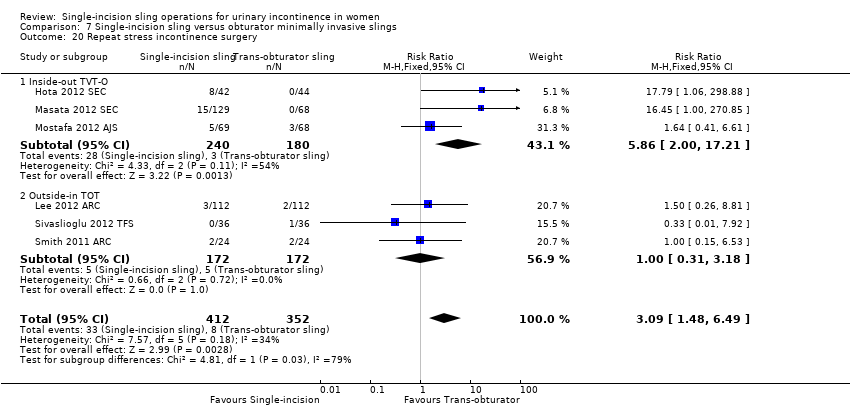 Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 20 Repeat stress incontinence surgery. | ||||
| 20.1 Inside‐out TVT‐O | 3 | 420 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.86 [2.00, 17.21] |
| 20.2 Outside‐in TOT | 3 | 344 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.31, 3.18] |
| 21 Need for any other additional or new surgical procedure to treat complications Show forest plot | 8 | 989 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.03 [1.09, 3.78] |
| Analysis 7.21  Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 21 Need for any other additional or new surgical procedure to treat complications. | ||||
| 21.1 Inside‐out TVT‐O | 5 | 645 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.15 [1.04, 4.43] |
| 21.2 Outside‐in TOT | 3 | 344 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.75 [0.52, 5.85] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women with urinary incontinence Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.1  Comparison 8 One single‐incision sling versus another, Outcome 1 Number of women with urinary incontinence. | ||||
| 1.1 TVT‐SECUR versus MiniArc | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.95, 1.29] |
| 1.2 U‐type versus H‐type TVT‐Secur | 3 | 496 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.78, 1.40] |
| 1.3 MiniArc versus Ajust | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.91 [0.63, 13.32] |
| 2 Number of women with no improvement Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.2  Comparison 8 One single‐incision sling versus another, Outcome 2 Number of women with no improvement. | ||||
| 2.1 TVT‐Secur versus MiniArc | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.25 [0.84, 12.66] |
| 2.2 U‐type versus H‐type TVT‐Secur | 1 | 129 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.33, 1.63] |
| 2.3 MiniArc versus Ajust | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.21 [0.21, 23.08] |
| 3 Objectve measurement of incontinence Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.3 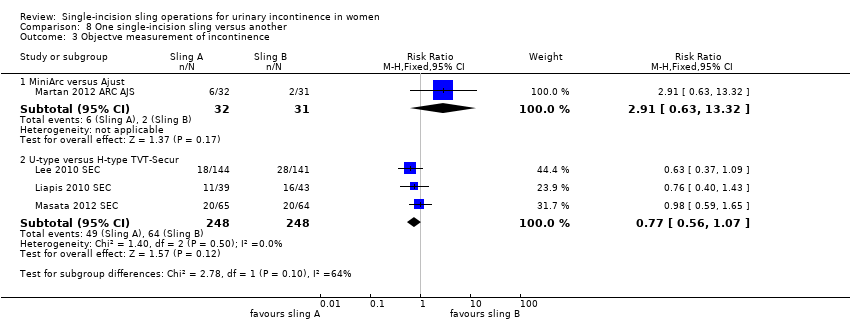 Comparison 8 One single‐incision sling versus another, Outcome 3 Objectve measurement of incontinence. | ||||
| 3.1 MiniArc versus Ajust | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.91 [0.63, 13.32] |
| 3.2 U‐type versus H‐type TVT‐Secur | 3 | 496 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.56, 1.07] |
| 4 Condition‐specific health measures Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.4  Comparison 8 One single‐incision sling versus another, Outcome 4 Condition‐specific health measures. | ||||
| 4.1 MiniArc versus AJUST | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.13 [‐1.58, 1.32] |
| 4.2 U‐type versus H‐type TVT‐Secur | 2 | 414 | Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐2.15, 1.55] |
| 5 Duration of operation (minutes) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.5  Comparison 8 One single‐incision sling versus another, Outcome 5 Duration of operation (minutes). | ||||
| 5.1 TVT‐Secur versus MiniArc | 2 | 190 | Mean Difference (IV, Fixed, 95% CI) | 1.70 [‐4.11, 7.51] |
| 5.2 Ajust versus MiniArc | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐4.67, 7.07] |
| 6 Operative blood loss Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.6  Comparison 8 One single‐incision sling versus another, Outcome 6 Operative blood loss. | ||||
| 6.1 U‐type versus H‐type TVT‐Secur | 2 | 459 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Ajust versus MiniArc | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐1.20 [‐10.04, 7.64] |
| 6.3 TVT‐Secur versus MiniArc | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 4.30 [‐5.53, 14.13] |
| 7 Major vascular or visceral injury Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.7  Comparison 8 One single‐incision sling versus another, Outcome 7 Major vascular or visceral injury. | ||||
| 7.1 U‐type versus H‐type TVT‐Secur | 2 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.19] |
| 8 Bladder or urethral perforation Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.8  Comparison 8 One single‐incision sling versus another, Outcome 8 Bladder or urethral perforation. | ||||
| 8.1 U‐type versus H‐type TVT‐Secur | 2 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 8.2 TVT‐Secur versus MiniArc | 1 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.18 [0.21, 85.11] |
| 9 Vaginal wall perforation Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.9  Comparison 8 One single‐incision sling versus another, Outcome 9 Vaginal wall perforation. | ||||
| 9.1 TVT‐S versus MiniArc | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 U‐type versus H‐type TVT‐Secur | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Urinary retention and need for catheterisation Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.10  Comparison 8 One single‐incision sling versus another, Outcome 10 Urinary retention and need for catheterisation. | ||||
| 10.1 TVT‐Secur versus MiniArc | 3 | 250 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.05 [0.47, 8.95] |
| 10.2 U‐type versus H‐type TVT‐Secur | 1 | 330 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.11, 3.94] |
| 10.3 Ajust versus MiniArc | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.25, 100.97] |
| 11 Vaginal mesh exposure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.11  Comparison 8 One single‐incision sling versus another, Outcome 11 Vaginal mesh exposure. | ||||
| 11.1 U‐type versus H‐type TVT‐Secur | 2 | 414 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.22, 2.80] |
| 12 Postoperative pain or discomfort Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.12  Comparison 8 One single‐incision sling versus another, Outcome 12 Postoperative pain or discomfort. | ||||
| 12.1 Ajust versus MiniArc | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 TVT‐Secur versus MiniArc | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 De novo urgency Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.13  Comparison 8 One single‐incision sling versus another, Outcome 13 De novo urgency. | ||||
| 13.1 TVT‐Secur versus MiniArc | 3 | 250 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.24, 2.02] |
| 13.2 U‐type versus H‐type TVT‐Secur | 2 | 367 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.53, 2.25] |
| 13.3 Ajust versus MiniArc | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.26, 8.50] |
| 14 Repeat stress incontinence surgery Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.14  Comparison 8 One single‐incision sling versus another, Outcome 14 Repeat stress incontinence surgery. | ||||
| 14.1 U‐type versus H‐type TVT‐Secur | 2 | 414 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.54, 2.51] |
| 15 Need for any other additional or new surgical procedure to treat complications Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.15 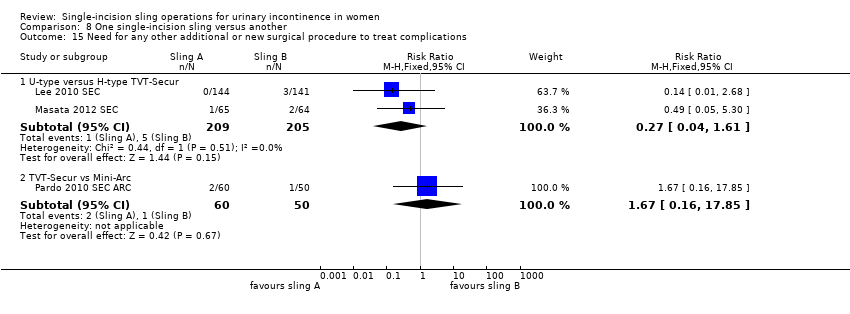 Comparison 8 One single‐incision sling versus another, Outcome 15 Need for any other additional or new surgical procedure to treat complications. | ||||
| 15.1 U‐type versus H‐type TVT‐Secur | 2 | 414 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.04, 1.61] |
| 15.2 TVT‐Secur vs Mini‐Arc | 1 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.16, 17.85] |

PRISMA study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 1 Number of women with urinary incontinence.
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 2 Number of women with no improvement.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 3 Objectve measurement of incontinence.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 4 Condition‐specific health measures.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 5 Duration of operation (in minutes).
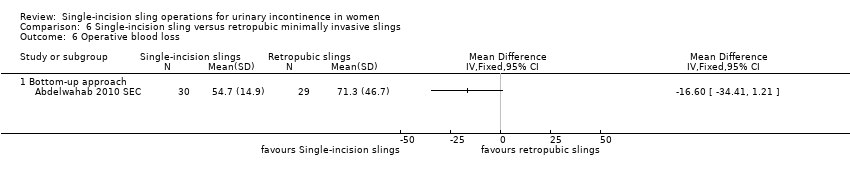
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 6 Operative blood loss.
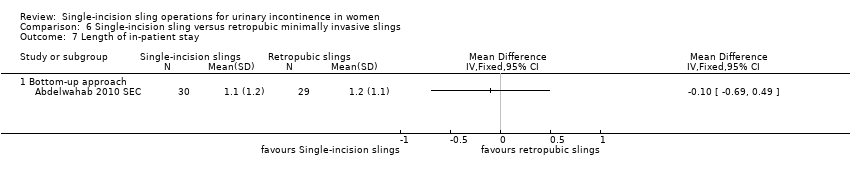
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 7 Length of in‐patient stay.
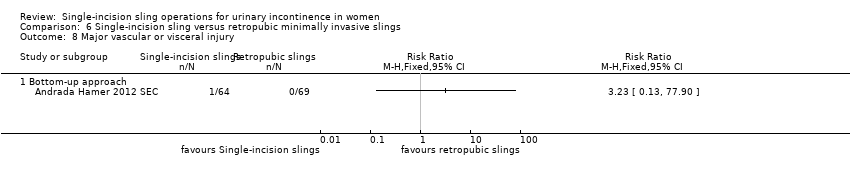
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 8 Major vascular or visceral injury.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 9 Vaginal wall perforation.
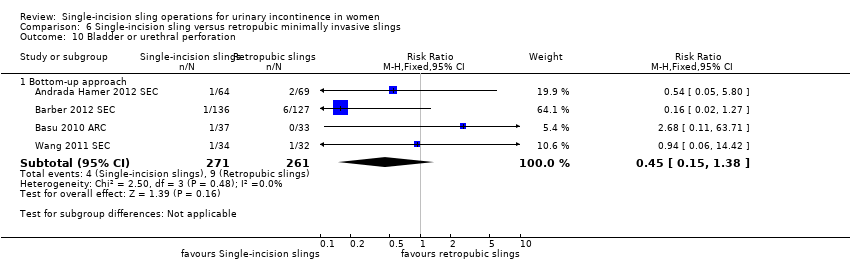
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 10 Bladder or urethral perforation.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 11 Urinary retention and need for catheterisation.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 12 Infection related to use of synthetic mesh.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 13 Vaginal mesh exposure.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 14 Mesh extrusion into the bladder or urethra.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 15 Long‐term pain or discomfort.
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 16 Dyspareunia.
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 17 De novo urgency.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 18 New‐onset detrusor overactivity.
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 19 Repeat stress incontinence surgery.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 20 Need for any other additional or new surgical procedure to treat complications.
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 1 Number of women with urinary incontinence.
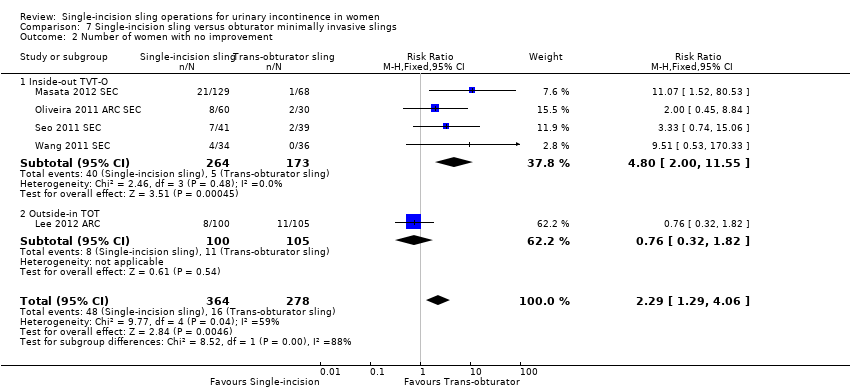
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 2 Number of women with no improvement.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 3 Objective measurement of incontinence.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 4 Incontinence episodes.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 5 Pad test (weights).
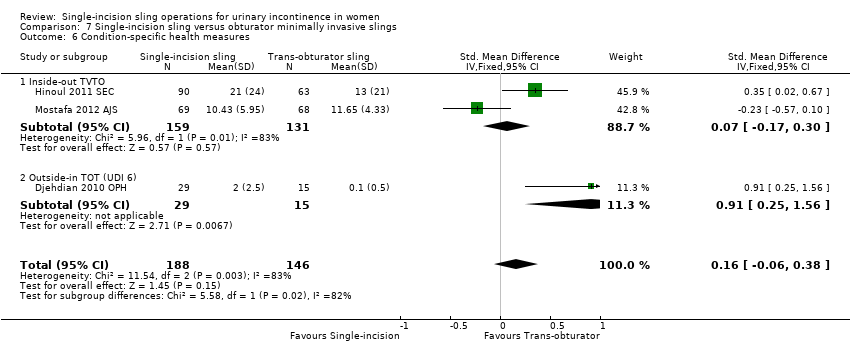
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 6 Condition‐specific health measures.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 7 Duration of operation (minutes).

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 8 Operative blood loss (mL).

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 9 Length of in‐patient stay.
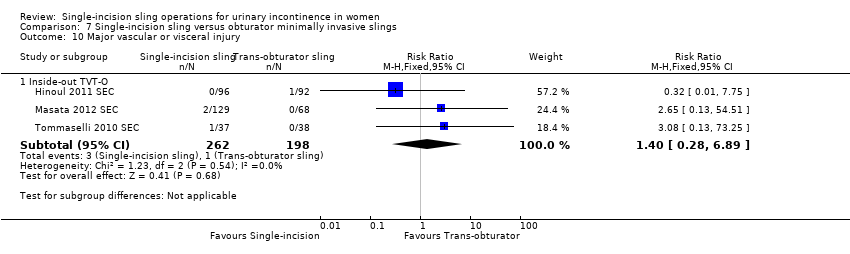
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 10 Major vascular or visceral injury.
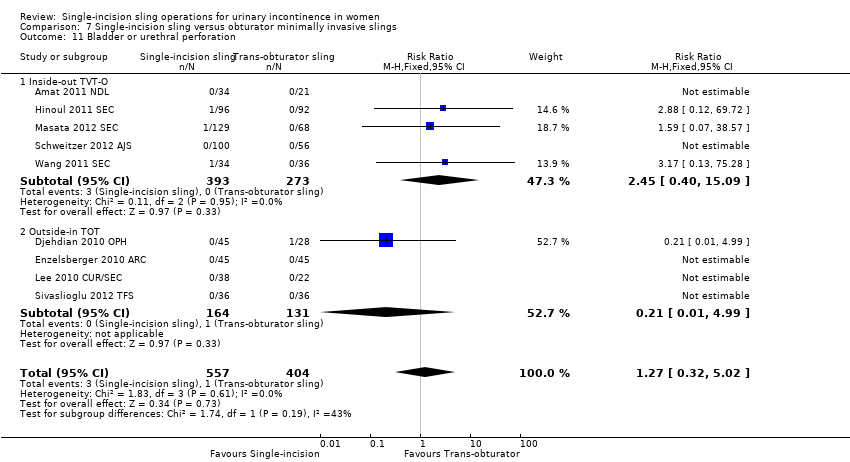
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 11 Bladder or urethral perforation.
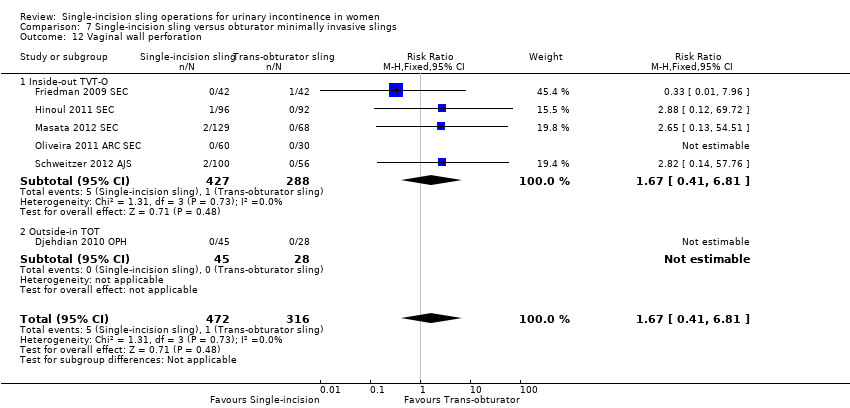
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 12 Vaginal wall perforation.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 13 Urinary retention and need for catheterisation.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 14 Infection related to use of synthetic mesh.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 15 Vaginal mesh exposure.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 16 Mesh extrusion into the bladder or urethra.
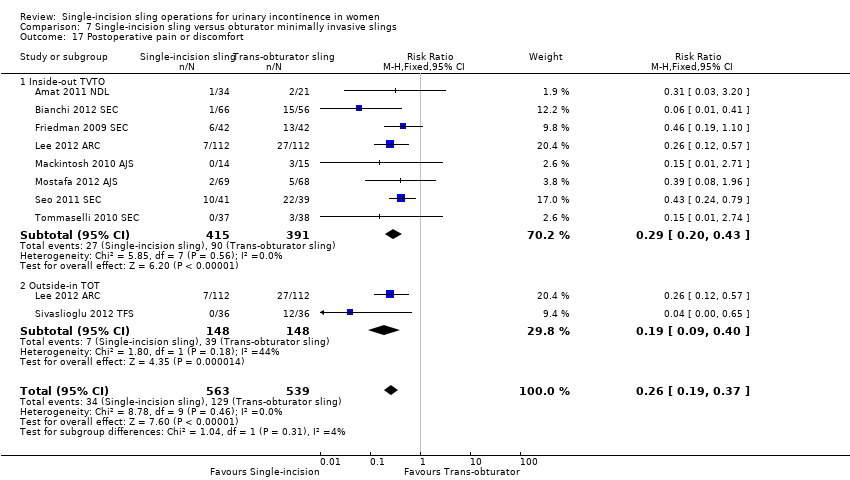
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 17 Postoperative pain or discomfort.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 18 Long‐term pain or discomfort.
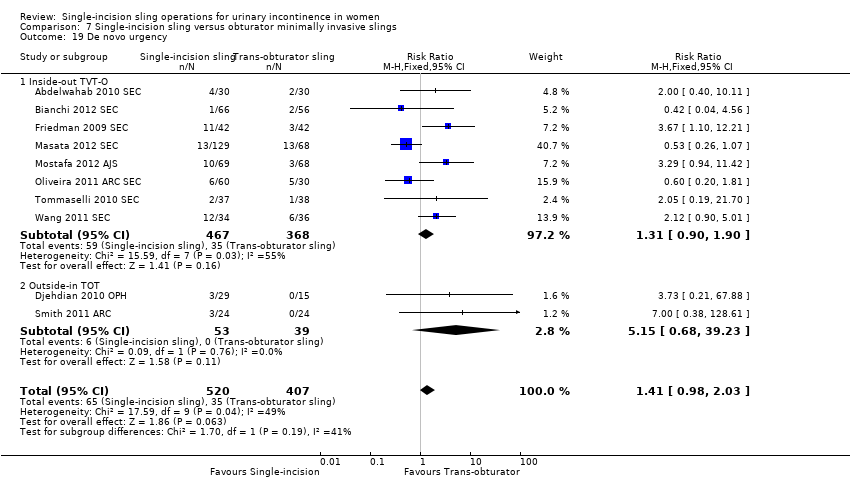
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 19 De novo urgency.
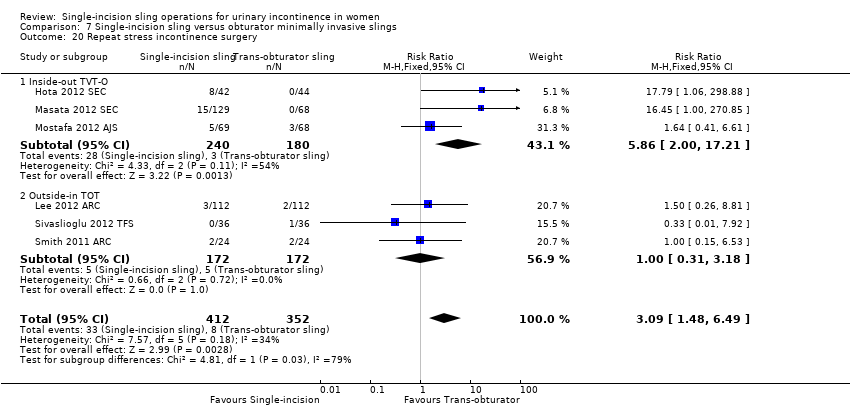
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 20 Repeat stress incontinence surgery.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 21 Need for any other additional or new surgical procedure to treat complications.

Comparison 8 One single‐incision sling versus another, Outcome 1 Number of women with urinary incontinence.

Comparison 8 One single‐incision sling versus another, Outcome 2 Number of women with no improvement.
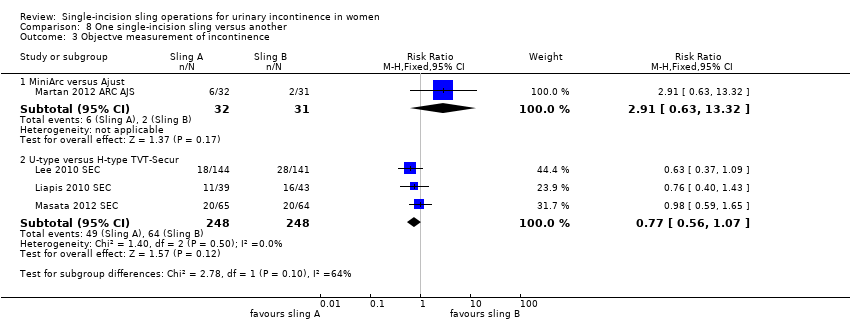
Comparison 8 One single‐incision sling versus another, Outcome 3 Objectve measurement of incontinence.

Comparison 8 One single‐incision sling versus another, Outcome 4 Condition‐specific health measures.

Comparison 8 One single‐incision sling versus another, Outcome 5 Duration of operation (minutes).

Comparison 8 One single‐incision sling versus another, Outcome 6 Operative blood loss.

Comparison 8 One single‐incision sling versus another, Outcome 7 Major vascular or visceral injury.

Comparison 8 One single‐incision sling versus another, Outcome 8 Bladder or urethral perforation.

Comparison 8 One single‐incision sling versus another, Outcome 9 Vaginal wall perforation.

Comparison 8 One single‐incision sling versus another, Outcome 10 Urinary retention and need for catheterisation.

Comparison 8 One single‐incision sling versus another, Outcome 11 Vaginal mesh exposure.

Comparison 8 One single‐incision sling versus another, Outcome 12 Postoperative pain or discomfort.

Comparison 8 One single‐incision sling versus another, Outcome 13 De novo urgency.

Comparison 8 One single‐incision sling versus another, Outcome 14 Repeat stress incontinence surgery.
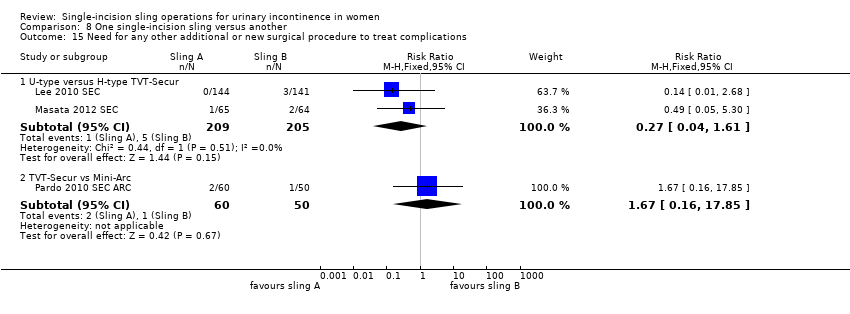
Comparison 8 One single‐incision sling versus another, Outcome 15 Need for any other additional or new surgical procedure to treat complications.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women with urinary incontinence Show forest plot | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Bottom‐up approach | 5 | 573 | Risk Ratio (M‐H, Random, 95% CI) | 2.08 [1.04, 4.14] |
| 2 Number of women with no improvement Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Bottom‐up approach | 3 | 246 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.38 [0.55, 3.46] |
| 3 Objectve measurement of incontinence Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Bottom‐up approach | 2 | 188 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.44 [2.06, 9.56] |
| 4 Condition‐specific health measures Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Bottom‐up approach | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Duration of operation (in minutes) Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Bottom‐up approach | 3 | 386 | Mean Difference (IV, Random, 95% CI) | ‐17.33 [‐32.09, ‐2.57] |
| 6 Operative blood loss Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 Bottom‐up approach | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Length of in‐patient stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 Bottom‐up approach | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Major vascular or visceral injury Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 Bottom‐up approach | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Vaginal wall perforation Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.1 Bottom‐up approach | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Bladder or urethral perforation Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 Bottom‐up approach | 4 | 532 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.15, 1.38] |
| 11 Urinary retention and need for catheterisation Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11.1 Bottom‐up approach | 5 | 578 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.38, 1.99] |
| 12 Infection related to use of synthetic mesh Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 12.1 Bottom‐up approach | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.22, 17.89] |
| 13 Vaginal mesh exposure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 Bottom‐up approach | 2 | 333 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.23, 8.16] |
| 14 Mesh extrusion into the bladder or urethra Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 Bottom‐up approach | 3 | 445 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.19, 3.01] |
| 15 Long‐term pain or discomfort Show forest plot | 2 | 329 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15.1 Bottom‐up approach | 2 | 329 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Dyspareunia Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 16.1 Bottom‐up approach | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.9 [0.32, 26.30] |
| 17 De novo urgency Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 17.1 Bottom‐up approach | 3 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.39 [1.25, 4.56] |
| 18 New‐onset detrusor overactivity Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 18.1 Bottom‐up approach | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.13, 5.98] |
| 19 Repeat stress incontinence surgery Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 19.1 Bottom‐up approach | 2 | 333 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.34 [0.79, 6.92] |
| 20 Need for any other additional or new surgical procedure to treat complications Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 20.1 Bottom‐up approach | 2 | 333 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.29, 4.74] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women with urinary incontinence Show forest plot | 17 | 1655 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.91 [1.53, 2.39] |
| 1.1 Inside‐out TVTO | 10 | 1053 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.55 [1.94, 3.36] |
| 1.2 Outside‐in TOT | 7 | 602 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.60, 1.39] |
| 2 Number of women with no improvement Show forest plot | 5 | 642 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.29 [1.29, 4.06] |
| 2.1 Inside‐out TVT‐O | 4 | 437 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.80 [2.00, 11.55] |
| 2.2 Outside‐in TOT | 1 | 205 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.32, 1.82] |
| 3 Objective measurement of incontinence Show forest plot | 12 | 1198 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.88 [1.49, 2.36] |
| 3.1 Inside‐out TVT‐O | 7 | 804 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.91 [2.00, 4.25] |
| 3.2 Outside‐in TOT | 5 | 394 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.90, 1.55] |
| 4 Incontinence episodes Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Outside‐in TOT | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Pad test (weights) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Outside‐in TOT | 2 | 268 | Mean Difference (IV, Fixed, 95% CI) | ‐1.64 [‐6.24, 2.96] |
| 6 Condition‐specific health measures Show forest plot | 3 | 334 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.16 [‐0.06, 0.38] |
| 6.1 Inside‐out TVTO | 2 | 290 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.17, 0.30] |
| 6.2 Outside‐in TOT (UDI 6) | 1 | 44 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.91 [0.25, 1.56] |
| 7 Duration of operation (minutes) Show forest plot | 9 | 1176 | Mean Difference (IV, Fixed, 95% CI) | ‐1.17 [‐1.60, ‐0.75] |
| 7.1 Inside‐out TVTO | 6 | 759 | Mean Difference (IV, Fixed, 95% CI) | ‐1.06 [‐1.50, ‐0.61] |
| 7.2 Outside‐in TOT | 3 | 417 | Mean Difference (IV, Fixed, 95% CI) | ‐2.14 [‐3.43, ‐0.84] |
| 8 Operative blood loss (mL) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Inside‐out TVTO | 2 | 320 | Mean Difference (IV, Fixed, 95% CI) | 18.79 [3.70, 33.88] |
| 9 Length of in‐patient stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 Inside‐out TVTO | 1 | 188 | Mean Difference (IV, Fixed, 95% CI) | ‐0.08 [‐0.33, 0.17] |
| 10 Major vascular or visceral injury Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 Inside‐out TVT‐O | 3 | 460 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.28, 6.89] |
| 11 Bladder or urethral perforation Show forest plot | 9 | 961 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.32, 5.02] |
| 11.1 Inside‐out TVT‐O | 5 | 666 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.45 [0.40, 15.09] |
| 11.2 Outside‐in TOT | 4 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.01, 4.99] |
| 12 Vaginal wall perforation Show forest plot | 6 | 788 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.41, 6.81] |
| 12.1 Inside‐out TVT‐O | 5 | 715 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.41, 6.81] |
| 12.2 Outside‐in TOT | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Urinary retention and need for catheterisation Show forest plot | 15 | 1477 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.28, 1.15] |
| 13.1 Inside‐out TVTO | 10 | 996 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.34, 1.52] |
| 13.2 Outside‐in TOT | 5 | 481 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.08, 3.44] |
| 14 Infection related to use of synthetic mesh Show forest plot | 2 | 412 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.09, 2.69] |
| 14.1 Inside‐out TVT‐O | 1 | 188 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.88 [0.12, 69.72] |
| 14.2 Outside‐in TOT | 1 | 224 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.73] |
| 15 Vaginal mesh exposure Show forest plot | 9 | 819 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.59 [1.21, 5.56] |
| 15.1 Inside‐out TVT‐O | 5 | 562 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.75 [1.42, 9.86] |
| 15.2 Outside‐in TOT | 4 | 257 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.27, 4.28] |
| 16 Mesh extrusion into the bladder or urethra Show forest plot | 2 | 146 | Risk Ratio (M‐H, Fixed, 95% CI) | 17.79 [1.06, 298.88] |
| 16.1 Inside‐out TVT‐O | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 17.79 [1.06, 298.88] |
| 16.2 Outside‐in TOT | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Postoperative pain or discomfort Show forest plot | 9 | 1102 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.19, 0.37] |
| 17.1 Inside‐out TVTO | 8 | 806 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.20, 0.43] |
| 17.2 Outside‐in TOT | 2 | 296 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.09, 0.40] |
| 18 Long‐term pain or discomfort Show forest plot | 5 | 351 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.04, 0.54] |
| 18.1 Inside‐out TVT‐O | 3 | 235 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.03, 1.07] |
| 18.2 Outside‐in TOT | 2 | 116 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.02, 0.82] |
| 19 De novo urgency Show forest plot | 10 | 927 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.41 [0.98, 2.03] |
| 19.1 Inside‐out TVT‐O | 8 | 835 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.90, 1.90] |
| 19.2 Outside‐in TOT | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.15 [0.68, 39.23] |
| 20 Repeat stress incontinence surgery Show forest plot | 6 | 764 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.09 [1.48, 6.49] |
| 20.1 Inside‐out TVT‐O | 3 | 420 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.86 [2.00, 17.21] |
| 20.2 Outside‐in TOT | 3 | 344 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.31, 3.18] |
| 21 Need for any other additional or new surgical procedure to treat complications Show forest plot | 8 | 989 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.03 [1.09, 3.78] |
| 21.1 Inside‐out TVT‐O | 5 | 645 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.15 [1.04, 4.43] |
| 21.2 Outside‐in TOT | 3 | 344 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.75 [0.52, 5.85] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women with urinary incontinence Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 TVT‐SECUR versus MiniArc | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.95, 1.29] |
| 1.2 U‐type versus H‐type TVT‐Secur | 3 | 496 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.78, 1.40] |
| 1.3 MiniArc versus Ajust | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.91 [0.63, 13.32] |
| 2 Number of women with no improvement Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 TVT‐Secur versus MiniArc | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.25 [0.84, 12.66] |
| 2.2 U‐type versus H‐type TVT‐Secur | 1 | 129 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.33, 1.63] |
| 2.3 MiniArc versus Ajust | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.21 [0.21, 23.08] |
| 3 Objectve measurement of incontinence Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 MiniArc versus Ajust | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.91 [0.63, 13.32] |
| 3.2 U‐type versus H‐type TVT‐Secur | 3 | 496 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.56, 1.07] |
| 4 Condition‐specific health measures Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 MiniArc versus AJUST | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.13 [‐1.58, 1.32] |
| 4.2 U‐type versus H‐type TVT‐Secur | 2 | 414 | Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐2.15, 1.55] |
| 5 Duration of operation (minutes) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 TVT‐Secur versus MiniArc | 2 | 190 | Mean Difference (IV, Fixed, 95% CI) | 1.70 [‐4.11, 7.51] |
| 5.2 Ajust versus MiniArc | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐4.67, 7.07] |
| 6 Operative blood loss Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 U‐type versus H‐type TVT‐Secur | 2 | 459 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Ajust versus MiniArc | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐1.20 [‐10.04, 7.64] |
| 6.3 TVT‐Secur versus MiniArc | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 4.30 [‐5.53, 14.13] |
| 7 Major vascular or visceral injury Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 U‐type versus H‐type TVT‐Secur | 2 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.19] |
| 8 Bladder or urethral perforation Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 U‐type versus H‐type TVT‐Secur | 2 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 8.2 TVT‐Secur versus MiniArc | 1 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.18 [0.21, 85.11] |
| 9 Vaginal wall perforation Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.1 TVT‐S versus MiniArc | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 U‐type versus H‐type TVT‐Secur | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Urinary retention and need for catheterisation Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 TVT‐Secur versus MiniArc | 3 | 250 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.05 [0.47, 8.95] |
| 10.2 U‐type versus H‐type TVT‐Secur | 1 | 330 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.11, 3.94] |
| 10.3 Ajust versus MiniArc | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.25, 100.97] |
| 11 Vaginal mesh exposure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11.1 U‐type versus H‐type TVT‐Secur | 2 | 414 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.22, 2.80] |
| 12 Postoperative pain or discomfort Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 Ajust versus MiniArc | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 TVT‐Secur versus MiniArc | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 De novo urgency Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 TVT‐Secur versus MiniArc | 3 | 250 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.24, 2.02] |
| 13.2 U‐type versus H‐type TVT‐Secur | 2 | 367 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.53, 2.25] |
| 13.3 Ajust versus MiniArc | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.26, 8.50] |
| 14 Repeat stress incontinence surgery Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 U‐type versus H‐type TVT‐Secur | 2 | 414 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.54, 2.51] |
| 15 Need for any other additional or new surgical procedure to treat complications Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 15.1 U‐type versus H‐type TVT‐Secur | 2 | 414 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.04, 1.61] |
| 15.2 TVT‐Secur vs Mini‐Arc | 1 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.16, 17.85] |

