Realidad virtual para la rehabilitación del accidente cerebrovascular
References
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT | |
| Participants | Recruited from 10 stroke centres in the UK 235 participants: 117 intervention, 118 control Inclusion criteria: ischaemic or haemorrhagic stroke within the last 6 months, arm weakness owing to stroke, defined as MRC Scale power < 5 in any joint plane and able to manipulate the Wii™ remote control Exclusion criteria: severe comorbidity that could impair participation, symptomatic shoulder subluxation, or a pacemaker Mean (SD) age: intervention group 66.8 (14.6) years, control group 68.0 (11.9) years 56% men Stroke details: 89% ischaemic Timing post stroke: intervention group mean (SD) 57.3 (48.3) d, control group mean 56.3 (50.1) d | |
| Interventions | VR intervention: therapists visited the participants home and installed the Wii and taught participants how to use it. Participants were given the choice of any of the Wii sports games. Performed in a seated position Control intervention: participant‐tailored arm exercises (based on the GRASP program) in a seated position Sessions: participants in both groups were instructed to warm up for 15 min and then perform the intervention for up to 45 min/d for 6 weeks | |
| Outcomes | Outcomes were assessed at baseline, 6 weeks, and 6 months Action Research Arm Test Canadian Occupational Performance Measure Stroke Impact Scale Modified Rankin Scale EQ5D Motor Activity Log Arm Function Test (6 months) Adverse events | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated |
| Allocation concealment (selection bias) | Low risk | Web‐based service |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded assessor |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis conducted |
| Selective reporting (reporting bias) | Low risk | Clinical trial registration and accurate reporting |
| Methods | RCT | |
| Participants | Recruited from 1 rehabilitation unit in Belgium 83 participants: 42 intervention, 41 control Inclusion criteria: within 3 months of first stroke, actively driving before stroke, in possession of an active driver's licence Exclusion criteria: ≥ 75 years, history of epilepsy within previous 6 months, severe motor or sensory aphasia Mean (SD) age: intervention group 54 (12) years, control group 54 (11) years 81% men Stroke details: 77% ischaemic, 44% right hemiparesis Timing post stroke: intervention group mean (SD) 53 (6) d, control group 54 (6) d | |
| Interventions | VR intervention: driving simulator in full‐sized, automatic gear transmission Ford Fiesta; a variety of 5 km driving scenarios were used including positioning on straight and curvy roads, stopping at crossings and avoiding pedestrians, overtaking and road sign recognition Control intervention: driving‐related cognitive tasks: these included route finding on a paper map, recognition of road signs, commercially available games including 'rush hour' and 'tantrix' Sessions were 60 min, 3 times a week for 5 weeks (15 h total) | |
| Outcomes | Outcomes recorded at baseline, post‐intervention and at 6 months with some participants followed up at 5 years Cognitive outcome measures: Useful Field of View Test Activity limitation outcome measures: on‐road driving test (using Test Ride for Investigating Practical Fitness to Drive checklist), decision of fitness to drive, Barthel Index (assessed at baseline and 5 years only) Other outcome measures: binocular acuity, kinetic vision, components of the Stroke Driver Screening Assessment Other outcome measures assessed at baseline and 5 years only: Hospital Anxiety and Depression Scale, number of km driven/year, number of self‐reported traffic tickets and accidents and driving status (actively driving or stopped driving) | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised number generation |
| Allocation concealment (selection bias) | Low risk | Allocation managed by an independent person |
| Blinding of outcome assessment (detection bias) | Low risk | Blind to allocation |
| Incomplete outcome data (attrition bias) | Low risk | A large amount of missing data due to the number of participants who withdrew (14% withdrew from their allocated intervention, 29% of participants were lost at 6‐month follow‐up); however, the authors completed an ITT analysis and found that dropout was random and balanced evenly across groups |
| Selective reporting (reporting bias) | Low risk | No other outcomes were collected |
| Methods | RCT | |
| Participants | Recruited from the physical therapy clinic at a university in Brazil 20 participants: 10 intervention, 10 control Inclusion criteria: people after stroke receiving weekly physical therapy sessions at the university; able to sit unsupported; able to understand the visual biofeedback; absence of osteoarticular deformities Exclusion criteria: unspecified comorbidities Mean (SD) age: intervention group 65.2 (12.5) years, control group 63.5 (14.5) years 45% men Stroke details: 65% right hemiparesis Timing post stroke: intervention group mean (SD) 12.3 (7.1) months, control group 15.2 (6.6 months) | |
| Interventions | VR intervention: conventional physical therapy plus an additional 30 min of balance training with visual feedback using 3 of the Nintendo Wii Fit program games Control intervention: convention physical therapy (stretching, joint movement, muscle strengthening, balance training, training of functional activities) Sessions were twice/week over 5 weeks. Conventional therapy lasted 60 min; the intervention sessions were an additional 30 min (approximately 5 h duration of additional training in total) | |
| Outcomes | Outcomes recorded at baseline and post intervention Gait outcomes: Timed Up and Go Test Balance outcomes: Berg Balance Scale, centre of pressure data, body symmetry Activity outcomes: Functional Independence Measure | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation table at central office |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded assessment |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Selective reporting (reporting bias) | Unclear risk | No access to study protocol |
| Methods | RCT | |
| Participants | Recruited from a rehabilitation facility in Melbourne, Australia 16 participants: 8 intervention, 8 control Inclusion criteria: adults with stroke who were able to sit unsupported for longer than 10 seconds (Motor Assessment Scale ‐ Sitting Balance ≥ 2) Exclusion criteria: severe dysphasia, significant cognitive deficits (Mini‐Mental State Examination < 20), other medical conditions (e.g. progressive neurological condition, severe arthritis, unstable heart condition) impacting on their ability to participate in the study, or visual problems such that they were not able to adequately see the games when displayed on the television screen Mean (SD) age: intervention group 60.8 (16.1) years, control 60.9 (14.0) years 69% men Timing post stroke, median (IQR) intervention group 12.8 (3.9 to 137.8) weeks, control group 24.7 (5.8 to 51.1) weeks | |
| Interventions | VR intervention: customised games developed for the research study. The system used a laptop, depth sensing camera and display on a television screen. The games were designed to encourage dynamic balance and upper limb activities and to be adaptable to users with different levels of balance, motor control and perceptual problems. Games included 'ball maze', 'fridge frenzy', 'tentacle dash' and 'bubble fish' Control intervention: usual care only (thus the VR therapy group received a greater overall dose of therapy) The intervention group completed eight 40‐min sessions over 4 weeks | |
| Outcomes | Assessed at baseline and post intervention Lower limb function and activity: 6MWT, step test Balance: functional reach Global Motor Function: Motor Assessment Scale Functional Independence Measure (transfers, walking, stairs) Adverse events | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random sequence |
| Allocation concealment (selection bias) | Low risk | External management |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded to allocation |
| Incomplete outcome data (attrition bias) | Low risk | Very low rate of withdrawals. ITT analysis conducted |
| Selective reporting (reporting bias) | Low risk | Registered clinical trial. All outcomes reported |
| Methods | RCT | |
| Participants | Recruited via the University of California, USA 15 participants completed the study: 5 intervention, 5 intervention, 5 control Inclusion criteria: stroke survivors > 6 months post stroke, 25‐75 years of age. Participants were independent in self care and independent in the community with minimal‐moderate voluntary function in the upper limb (Upper Limb Fugl Meyer score 16‐39). Participants needed to speak English or attend with an interpreter Exclusion criteria: people were excluded if they suffered from a neurological disease other than stroke, had co‐morbidities that would impact on participation, were in severe pain, were not mentally alert or had a skin condition that would prevent wearing the robotic orthosis Mean (SD) age: intervention group 65.2 (5.4) years, control group 54.2 (20.5) years Stroke details: 70% right hemiparesis Timing post stroke: intervention group 8.4 (4.2), control group 10.2 (5.0) months | |
| Interventions | This trial had 3 arms: 2 of the intervention groups performed VR tasks; 1 of the VR groups performed bilateral tasks and the other group performed unilateral tasks VR intervention: the participant wore a robotic orthosis. Each session started with a motor‐control evaluation task and then followed with treatment in which participants performed repetitive movements while playing task‐specific games Control intervention: repetitive task practice involved reaching, grasping, object manipulation and self‐care activities. Dynamic orthoses were not included in training Sessions were 90 min for 12 treatment sessions (approximately 18 h total) | |
| Outcomes | Outcomes recorded at baseline and post‐intervention Upper limb function outcomes: Fugl Meyer, Motor Proficiency Speed (abbreviated Wolf Motor Function Test and Digital Reaction Time Test) Hand function outcomes: motor skill performance (Box and Block test and Tapper test) Activity limitation outcomes: functional independence (CAFE40) Quality of life outcomes: Stroke Impact Scale Adverse events | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Allocated prospectively using a computer program |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded assessment |
| Incomplete outcome data (attrition bias) | Low risk | Reporting for all participants following intervention |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Methods | RCT | |
| Participants | Recruited from a hospital in Korea 29 participants: 15 intervention, 14 control Inclusion criteria: no VR intervention in the previous 2 years, no surgery in the previous 2 months and no specific medical problems, including psychological problems Exclusion criteria: none described Mean (SD) age: intervention group 64 (7.1) years, control group 63.7 (8.8) years 62% men Stroke details: 41% hemiparesis Timing post stroke: not reported | |
| Interventions | VR intervention: the Interactive Rehabilitation and Exercise System (IREX) was used for training. The participant performed 6 programs; each program was performed for 5 min Control intervention: no intervention Sessions were 60 min, 5 times/week for 4 weeks (approximately 20 h total) | |
| Outcomes | Outcomes recorded at baseline and post‐intervention Upper limb function outcomes: Wolf Motor Function Test Other outcomes: Motor Free Visual Perception Test | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random‐sampling numbers |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | High risk | Withdrawals not clearly explained |
| Selective reporting (reporting bias) | Unclear risk | Protocol not publicly available |
| Methods | RCT | |
| Participants | Recruited from outpatient physiotherapy at the Hong Kong Buddhist Hospital 14 participants (size of each group not reported) Inclusion criteria: diagnosis of stroke Exclusion criteria: not reported Mean (SD) age: intervention group 69.14 years (2.73), control group 68.86 (8.25) years Stroke details: not reported Timing post stroke: not reported | |
| Interventions | VR intervention: Xbox360 Kinect in addition to conventional physiotherapy training Control intervention: conventional physiotherapy training Sessions were 60 min, twice/week for 6 weeks | |
| Outcomes | Outcomes recorded at baseline and post intervention Gait and balance function: 10 metre walk test, Berg Balance scale Activity limitation: Modified Barthel Index Other: Sensory organisation test | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported (conference abstract) |
| Allocation concealment (selection bias) | Unclear risk | Not reported (conference abstract) |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported (conference abstract) |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported (conference abstract) |
| Selective reporting (reporting bias) | Unclear risk | Not reported (conference abstract) |
| Methods | RCT | |
| Participants | Recruited from a stroke unit in Glasgow, UK 12 participants: 4 high‐intensity intervention, 4 low‐intensity intervention, 4 control Inclusion criteria: ≥ 18 years with a clinical diagnosis of stroke and grade 1‐4 on MRC scale of arm impairment. Medically stable and within 10 d post stroke. Able to give informed consent, understand and follow simple instruction and sitting balance sufficient to use the device safely Exclusion criteria: orthosis could not be fitted to the affected limb due to previous stroke or other condition, bone instability of affected upper limb, no functional use of affected upper limb due to previous stroke or other condition. Pronounced fixed contractures of affected upper limb, open skin lesions on affected upper limb; major sensory deficit of affected upper limb; shoulder instability or excessive pain; severe spasticity; severe spontaneous movements; confused or non‐co‐operative; isolation due to infection; visual, perceptual or cognitive problems precluding participation in study involvement or involvement in any other intervention study Mean (SD) age: high‐intensity intervention group 65 (14) years, low‐intensity 72 (10), control 59 (16) years 66% men Stroke details: 42% right hemiparesis Timing post stroke: high‐intensity intervention 8 (1) d, low‐intensity 9 (2), control 8 (3) | |
| Interventions | VR intervention: Low‐intensity: standard care plus Armeo®Spring arm orthosis and VR games for arm rehabilitation used for 40 min/d, 3 d/week High‐intensity: standard care plus Armeo®Spring arm orthosis and VR games for arm rehabilitation used for 60 min/d, 5 d/week Games included catching rain drops, picking apples and cleaning a cooker Control intervention: standard care including standard physiotherapy and OT targeted at arm recovery Sessions were for 2 weeks or until discharge from the stroke unit (whichever was soonest) | |
| Outcomes | Outcomes recorded at baseline, completion of intervention and 3 months following completion Upper limb function: Action Research Arm Test, Fugl Meyer UE Activity restriction: Barthel Index Other outcomes related to feasibility, acceptability, safety, arm pain, perceived exhaustion and adverse events | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence |
| Allocation concealment (selection bias) | Low risk | Sealed, numbered, opaque envelopes |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded to allocation |
| Incomplete outcome data (attrition bias) | Low risk | Few withdrawals and balanced across groups for reasons not clearly related to the study |
| Selective reporting (reporting bias) | Low risk | All outcomes reported in thesis |
| Methods | RCT | |
| Participants | Recruited from 2 hospital stroke units and members of Stroke Association Clubs in Northern Ireland 18 participants: 9 intervention, 9 control Inclusion criteria: within 2 years of first stroke, medically stable, can follow 2‐stage commands, score of ≥ 25 on the upper limb Motricity Index Exclusion criteria: mental score < 7/10, neglect (star cancellation < 48/52), comorbid conditions impacting on rehabilitation potential, cardiac pacemaker, severe arm pain reported on visual analogue scale Mean (SD) age: intervention group 56 (15) years, control group 65 (7) years 55% men Stroke details: 39% right hemiparesis Timing post stroke: intervention group mean (SD) 10 (6) months, control group 12 (8) months | |
| Interventions | VR intervention: the participant chose from a variety of activities involving reaching and grasping of virtual objects at a variety of heights, speeds and with varied number of targets; the participant wore a head‐mounted device and data glove Control intervention: therapy provided based on the Bobath approach Sessions were 35‐45 min, 3 times/week over 3 weeks (approximately 6 h total) | |
| Outcomes | Outcomes recorded at baseline, post‐intervention and at 6 weeks Upper limb function and activity outcomes: Action Research Arm Test, Upper Limb Motricity Index Adverse events were reported Other outcome measures: an exit questionnaire including questions about enjoyment and perception of improvement | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An independent colleague generated the sequence using a computer random number generator |
| Allocation concealment (selection bias) | Low risk | Group allocation cards were concealed in sealed, opaque envelopes |
| Blinding of outcome assessment (detection bias) | Low risk | Masked to allocation |
| Incomplete outcome data (attrition bias) | Low risk | An ITT analysis was completed. Missing data points were dealt with using the simple mean imputation method |
| Selective reporting (reporting bias) | Low risk | No other outcomes were collected |
| Methods | RCT | |
| Participants | Recruited from a subacute rehabilitation unit in Spain 19 participants: 13 intervention, 6 control Inclusion criteria: recruited within 3 weeks of first stroke, severe‐moderate upper limb impairment, no moderate‐severe aphasia, no other cognitive deficits as assessed by the MMSE and aged ≤ 80 years Exclusion criteria: none specified Mean (SD) age: intervention group 63.7 (11.83) years, control group 59.4 (10.62) years, control group (Wii) 58 (14) years 47% men Stroke details: 37% right hemiparesis Timing post stroke: intervention group mean (SD) 11.5 (5.1) d, control group 16.8 (5.0) d, control group (Wii) 13 (4.7) d | |
| Interventions | VR intervention: Rehabilitation Gaming System (RGS). The main elements of the system are the vision‐based analysis and tracking system that capture upper limb movements through colour detection, data gloves to capture finger flexion and a virtual environment where an avatar mimics the movements of the user Control intervention (OT): OT with emphasis on motor tasks similar to those in the RGS (i.e. object displacement, grasp and release) Control intervention (Wii): used the Wii gaming system. This intervention involved the gaming features but not the neuro‐scientific hypothesis regarding recovery Sessions were 20 min, 3 times/week for 12 weeks (approximately 12 h total). This was provided in addition to standard rehabilitation | |
| Outcomes | Outcomes recorded at baseline, weeks 5, 12 and 24 Upper limb outcomes: Fugl Meyer, Chedoke Arm and Hand Activity Inventory Activity outcomes: Barthel Index Other outcomes: participant satisfaction | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated program |
| Allocation concealment (selection bias) | Low risk | Managed externally |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded to allocation |
| Incomplete outcome data (attrition bias) | High risk | Outliers excluded from the data analysis |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Methods | RCT | |
| Participants | Recruited from an outpatient setting in Sao Paolo, Brazil 30 participants: 15 intervention, 15 control Inclusion criteria: aged 18‐60 years with a diagnosis of stroke (based on neurologist assessment) and hemiparesis. Able to ambulate and hold the game controller without assistive devices. ≥ 6 months post stroke Exclusion criteria: associated disorders (such as hemineglect or pusher syndrome), intellectual disability that made it difficult to understand the games or a history of orthopaedic diseases that promoted dysfunction in the limbs or prevented the performance of the proposed activity Mean (SD) age: intervention group 53.7 (6.1) years, control group 52.8 (8.6) years 37% men Stroke details: 57% right hemiparesis Timing post stroke, mean (SD): intervention group 42.1 (26.9) months, control group 60.4 (44.) months | |
| Interventions | VR intervention: Nintendo Wii projected onto the wall. After full body stretching for 10 min the participants spent 50 min using the Nintendo Wii. The tennis and hula hoop games were used during the 1st session and soccer and boxing used during the second weekly session. The difficulty level of the games was increased as participants progressed Control intervention: conventional physiotherapy including stretching, passive, active and resisted mobilisation activities, balance and gait activities and gripping activities Sessions were 60 min, twice/week for 2 months with a physiotherapist | |
| Outcomes | Outcomes assessed post intervention Upper limb function and activity: Fugl Meyer Participation and quality of life: SF36 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number allocation (performed online) |
| Allocation concealment (selection bias) | Unclear risk | Used envelopes but unclear if opaque or not |
| Blinding of outcome assessment (detection bias) | Low risk | Masked to allocation |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear |
| Selective reporting (reporting bias) | Unclear risk | Trial register not reported |
| Methods | RCT | |
| Participants | Recruited from a suburban hospital and affiliated nursing home in Taiwan 20 participants: allocated to 4 different treatment groups Inclusion criteria: aged 20‐85 years with evidence of a cerebrovascular accident (confirmed by CT or MRI). Onset for symptoms for ≥ 6 months and MMSE score of > 24. Able to produce active shoulder movements on the side of the hemiparesis (Fugl Meyer of ≥ 21). Visual analogue scale of < 4, Modified Ashworth Scale of ≤ 2 and no rehabilitation in the past 3 months Exclusion criteria: uncontrolled hypertension, unstable angina, history of seizure, artificial pacemaker and participation in other research Mean (SD) age: varied from 57‐67 years across the 4 intervention groups Stroke details: 90% ischaemic, 45% right hemiplegia Timing post stroke: ranged from an average of 1.8‐2.6 years across the 4 intervention groups | |
| Interventions | VR intervention: used available games including the Nintendo Wii Sports Resort. Participants were supervised by a research staff member. The consoles and controller were not modified in the study. Participants were advised to take ≥ 5‐10‐min breaks between games Control intervention: OT involving Bobath and proprioceptive neuromuscular facilitation. Equipment included bean bags, target bags and cones Control intervention: leisure activities including mahjong, cards and checkers Control intervention: usual care Sessions were 60 min, 3 times/week for 3 weeks | |
| Outcomes | Outcomes assessed at baseline, post intervention and 4 weeks after treatment Arm function: Jebsen Taylor Hand Function Test Stroke Impact Scale Intrinsic Motivation Inventory | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer random‐number generator |
| Allocation concealment (selection bias) | Unclear risk | Details not reported |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessor blinded |
| Incomplete outcome data (attrition bias) | High risk | There were a relatively high proportion of withdrawals |
| Selective reporting (reporting bias) | Unclear risk | Unclear. Trial registry not reported |
| Methods | RCT | |
| Participants | Recruited from a physiotherapy clinic in Brazil 27 participants: intervention 17, control 10 Inclusion criteria: stroke, hemiparesis, aged 30‐70 years Exclusion criteria: failure to meet above criteria Mean (SD) age: 55.06 (11.52) years, control 60.8 (10.83) years | |
| Interventions | VR intervention: exercises with the Nintendo Wii Control intervention: conventional therapy Sessions were 75 min for the Wii group and 60 min for the conventional therapy group and a total of 10 sessions were provided | |
| Outcomes | Outcomes were assessed post intervention Fugl Meyer UL Motor Activity Log | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer randomisation program |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque, sealed envelopes |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | Detail not reported |
| Selective reporting (reporting bias) | Unclear risk | Detail not reported |
| Methods | RCT | |
| Participants | NCT01304017 Recruited from the community in Israel 47 participants: 23 intervention, 24 control Inclusion criteria: community dwelling, aged 18‐8 years and sustained a stroke ≥ 6 months prior to the study. Able to walk ≥ 10 m (with or without aid) and had weakness of the UE and no significant cognitive deficits (score of ≥ 21 or more on the MMSE) Exclusion criteria: other neurological conditions or epilepsy Mean (SD) age: intervention group 56.7 (9.3) years, control group 62.0 (9.3) years 60% men Stroke details: 85% ischaemic, 57% right hemiparesis Timing post stroke: intervention group mean 3 (1.8) years, control group mean 2.6 (1.8) years | |
| Interventions | VR intervention: interactive video games (Kinect, Sony Play Station Eyetoy 2, Sony Playstation 3 MOVE, Nintendo Wii Fit and SeeMe VR system) were set up in 3 workstations. Each session started with a 5‐min group warm up playing a Wii Fit walking game. Participants were then divided into workstations. They played games on 1 console then rotated to another console with a new partner. All games were played in pairs while standing. Partners either took turns or played simultaneously Control intervention: exercises and functional activities from existing community group programs such as the Fitness and Mobility Exercise Program, the GRASP program and task oriented intervention. The session started with a 5‐min group warm up and then participants were divided into pairs or triads to perform functional activities such as picking up and transferring objects from 1 side of the room to the other Sessions were 60 min, twice/week for 3 months. Intervention in both groups delivered by an occupational therapist | |
| Outcomes | Outcomes measured at baseline, post intervention and 3 months' follow‐up (after the end of intervention) 10‐metre walk test Hand grip strength Action Research Arm Test Other outcome measures: number of steps walked per day Adverse events | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Detail not reported |
| Allocation concealment (selection bias) | Unclear risk | Detail not reported |
| Blinding of outcome assessment (detection bias) | Low risk | Assessor masked to allocation |
| Incomplete outcome data (attrition bias) | Low risk | Low dropouts. ITT analysis conducted with the last observation carried forward method |
| Selective reporting (reporting bias) | High risk | Measures reported on the clinical trial registry were not reported in the paper |
| Methods | RCT | |
| Participants | Recruited from a tertiary hospital in Korea 12 participants: 6 intervention, 6 control Inclusion criteria: impaired standing balance (Berg Balance Scale < 40) however can stand for ≥ 1 min Exclusion criteria: none reported Mean (SD) age: total sample 60.1 (17.6) years 50% men Stroke details: not reported Timing post stroke: not reported | |
| Interventions | VR intervention: IREX system (games: Birds and Balls, Soccer, Conveyor, Drums, Sharkbait) Control intervention: balance training using tetrataxiometric posturography Sessions were 30 min/day, 3 d/week for 3 weeks | |
| Outcomes | Outcomes assessed post intervention Balance: Berg Balance Scale Modified Barthel Index Tetraataxiometric posturography | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported (conference abstract) |
| Allocation concealment (selection bias) | Unclear risk | Not reported (conference abstract) |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported (conference abstract) |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported (conference abstract) |
| Selective reporting (reporting bias) | Unclear risk | Not reported (conference abstract) |
| Methods | RCT | |
| Participants | Recruited from 1 rehabilitation institute in Chicago, USA 34 participants: 17 intervention, 17 control Inclusion criteria: single stroke ≥ 6 months ago, Fugl Meyer UE score 10‐30 Exclusion criteria: significant pain or instability of the shoulder, current participation in upper limb therapy program, severe cognitive dysfunction, aphasia, neglect, apraxia Mean (SD) age: intervention group 54 (12) years, control group 56 (13) years 64% men Stroke details: 61% ischaemic, 29% right hemiparesis Timing post stroke: intervention group mean (SD) 85 (96) months, control group 112 (129) months | |
| Interventions | VR intervention: a custom‐designed software package ('Vu Therapy') provided activities including grocery shopping, cleaning a stove and playing basketball. The participant wore an arm orthosis (T‐WREX), which supports the weight of the arm allowing movement in the horizontal and vertical plane. Position sensors at each joint enable interaction with the virtual environment Control intervention: UE exercises including passive and active ranging, stretching, strengthening and using the arm in functional tasks Both groups involved 3 sessions of direct training followed by semi‐autonomous practice in the research clinic Sessions were 60 min, approximately 3 times/week for 6 weeks (approximately 24 h total) | |
| Outcomes | Outcomes recorded at baseline, post‐intervention and at 6 months Upper limb function and activity outcomes: Fugl Meyer UE Scale, Rancho Functional test UE, Reaching ROM (deficit) Hand function and activity: grip strength (dynamometer) Participation restriction and quality of life: Motor Activity Log (amount of use and quality of movement) Adverse events reported | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly assigned using a lottery system in which the supervising therapist (with an independent witness) drew a labelled tile from an opaque container. Randomisation occurred in blocks of 4 to ensure equal numbers in each group |
| Allocation concealment (selection bias) | High risk | Participants were allocated in strict sequential order of enrolment. However, with small blocks of 4 and the use of tiles it might have been possible to predict allocation in advance in some cases |
| Blinding of outcome assessment (detection bias) | Low risk | Rater was blinded to allocation |
| Incomplete outcome data (attrition bias) | Low risk | Small number of dropouts balanced across groups with similar reasons for dropout |
| Selective reporting (reporting bias) | Low risk | No other outcomes were collected |
| Methods | RCT | |
| Participants | Recruited from an outpatient rehabilitation setting in Taiwan 30 participants: 15 intervention group, 15 control group Inclusion criteria: stroke with resulting hemiplegia ≥ 6 months prior to enrolment. Aged > 18 years and had a Berg Balance Scale score < 56. Able to understand verbal instructions and watch a television screen satisfactorily. Able to walk independently with or without a device for 10 m Exclusion criteria: bilateral lesions, receptive aphasis, significant visual field deficits or hemineglect and concomitant other neurological diagnoses or conditions that would prevent adherence to the exercise protocol Mean (SD) age: intervention group 55.38 (9.95) years, control group 53.40 (10.03) years 60% men Stroke details: 53% ischaemic, 37% right hemiparesis Timing post stroke: intervention group mean (SD) 21 (11.26) months, control group 15.93 (8.02) months | |
| Interventions | VR intervention: Nintendo Wii Fit. 7 games (Table tilt, Ski Slalom, Soccer, Balance Bubble, Penguin Slide, Basic Step and Warrior) were selected. At each session the therapist supervised 2‐4 games for participants according to their ability, needs and favourites. A walker was placed in front of the balance board for safety. Control intervention: weight shift and balance exercises Sessions were twice/week for 12 weeks and were run by an occupational therapist | |
| Outcomes | Outcomes assessed post intervention and at 3 months' follow‐up Tetrax Interactive Balance Systems Timed Up and Go Test Forward Reach Test Falls Efficacy Scale International Adverse events | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque, sealed envelopes |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded to allocation |
| Incomplete outcome data (attrition bias) | Low risk | Low attrition with clear rationale. Used data of actual number contributing |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trial registration reported |
| Methods | RCT | |
| Participants | Recruited from community stroke association meetings in California, USA 20 participants: 10 intervention, 10 control Inclusion criteria: > 6 months post stroke with a diagnosis of hemiplegia secondary to single documented lesion, walked independently or with an aid and had an asymmetric gait pattern and short step‐length with either step (< 95th percentile of normal step length), scores representing average or minimally impaired in all Cognistat categories unless performance was markedly limited by aphasia making assessment of cognition difficult Exclusion criteria: neurological diagnoses of spinal cord injury, multiple sclerosis or brainstem lesion; any progressive critical or long‐term illness or unstable cardiovascular, orthopaedic, musculoskeletal or neurological condition that precluded exercise or was not controlled by medication or required oxygen during ambulation Mean (SD) age: intervention group 58 (11) years, control group 63 (8) years 60% men Stroke details: 50% right hemiparesis Timing post stroke: intervention group 4 years (SD 2), control group 4 years (SD 3) | |
| Interventions | VR intervention: participants walked on a treadmill at a self‐selected walking speed and were secured by an overhead harness. The participant wore a head‐mounted display that showed real‐time video images of their feet walking and virtual objects. The participant was asked to step over the virtual objects and visual, vibrotactile and auditory feedback was provided during any collisions Control intervention: participants wore a gait belt and stepped over foam obstacles in a hallway. The sessions were videotaped and reviewed for collisions with the obstacles after the session was completed Sessions were approximately 60 min, for 6 sessions over 2 weeks (6 h total) | |
| Outcomes | Outcomes recorded at baseline, post‐intervention and 2 weeks post‐intervention Lower limb function and activity outcomes: 6‐m walk test, obstacle test, 6MWT, the researcher's own balance test (adapted from others) that included natural stance, eyes closed, on toes, tandem stance, left and right leg stand Adverse events reported | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An Excel spreadsheet was generated with a pre‐determined computerised randomisation sequence |
| Allocation concealment (selection bias) | High risk | The allocation in the spreadsheet was not visible due to black font and black background shading; however, there is the possibility that staff with access to the spreadsheet could have checked this |
| Blinding of outcome assessment (detection bias) | Low risk | Unaware of allocation |
| Incomplete outcome data (attrition bias) | Low risk | No outcome data were missing (according to personal correspondence with the researcher) |
| Selective reporting (reporting bias) | Unclear risk | Unclear ‐ not privy to protocol |
| Methods | RCT | |
| Participants | Study took place in Korea 10 participants: 5 intervention, 5 control Inclusion criteria: > 6 months post first stroke, able to move the elbow against gravity Exclusion criteria: severe spasticity (Modified Ashworth Score of > 2) or tremor. Severe visual and cognitive impairments Mean (SD) age: intervention group 60 (8) years, control group 54 (12) years 60% men Stroke details: 60% ischaemic, 50% right hemiparesis Timing post stroke: intervention group 14 months, control group 13 months | |
| Interventions | VR intervention: IREX VR system using a video capture system to capture the participant's whole body movement. The participant was able to view their body movements in real time on a screen in front of them immersed in a virtual environment. The games included soccer and moving objects from a conveyor belt and focused on reaching, lifting and grasping Control intervention: no intervention provided Sessions for the VR intervention group were 60 min, 5 times/week for 4 weeks (20 h total) | |
| Outcomes | Outcomes recorded at baseline and post‐intervention Upper limb (arm) function and activity outcomes: Fugl Meyer UE Scale, Manual Function Test Upper limb (hand) function and activity outcomes: Box and Block Test Participation restriction and quality of life: Motor Activity Log (amount of use and quality of movement) Other outcomes: functional MRI (laterality index and activated voxels) | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unclear |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Methods | RCT | |
| Participants | Recruited from a rehabilitation centre in the Netherlands 10 participants: 5 intervention, 5 control Inclusion criteria: not reported Exclusion criteria: not reported Mean (SD) age: intervention group 62 (3) years, control group 58 (13) years Timing post stroke: intervention group mean (SD) 89 d (31), control group 112 d (50) | |
| Interventions | VR intervention: the participant sat on an electric scooter with customised interface and completed training in a traffic garden, residential area and a grocery store. The virtual environment was displayed using a head‐mounted device as well as a computer display. Training included 50% of the time using the VR simulation program and 50% training in the real world Control intervention: real‐world scooter training program Sessions were 30 min, twice/week for 5 weeks (5 h total) | |
| Outcomes | Outcomes recorded at baseline and 5 weeks after training Other outcome measures: Functional Evaluation Rating Scale, Subjective Experience Questionnaire | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unclear |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Methods | RCT | |
| Participants | Recruited from outpatient community centre in Korea 21 participants: 11 intervention, 10 control Inclusion criteria: participants within 6 months after first stroke with a history of falling. Able to walk independently for > 30 min with no cognitive impairment, Brunnstrom Stage > 4 and no cardiovascular, orthopaedic or other neurological conditions that may interfere with study procedures Exclusion criteria: not reported Mean (SD) age: intervention group 60.5 (8.6) years, control group 63.6 (5.1) years 62% men Stroke details: 52% right‐sided hemiparesis Timing post stroke: intervention group mean (SD) 12.6 (3.3) months, control group 15.4 (4.7) months | |
| Interventions | VR intervention: treadmill training while viewing a virtual scene through a head‐mounted device. The VR program simulated a park stroll Control intervention: treadmill training without the VR program Sessions were 30 min/d, 5 times a week for 3 weeks (approximately 7.5 h total) | |
| Outcomes | Outcomes recorded at baseline and post‐intervention Gait outcomes: Timed Up and Go Test Other outcomes: Activity Specific Balance Confidence Scale | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Drawing lots |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded assessment |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Methods | RCT | |
| Participants | Study took place in Korea 16 participants: 8 intervention, 8 control Inclusion criteria: left hemiplegia after stroke, MMSE score of > 18/30 and Motor Free Visual Perception Test standard score < 109 Exclusion criteria: significant multiple small lacunar infarct, significantly decreased visual acuity or visual impairment from diabetic retinopathy or senile cataract, hearing difficulty or cranial nerve dysfunction Mean (SD) age: intervention group 60 (11) years, control group 63 (10) years Timing post stroke: intervention group mean (SD) 64 (37) d, control group 58 (30) d | |
| Interventions | VR intervention: participants were seated and participated in visual spatial and motor tasks using their unaffected arm. Software recognised and displayed the movements of the hand through a camera and displayed the images on a computer screen Control intervention: training using the PSS CogRehab program Sessions were 30 min, 3 times/week for 4 weeks (6 h total) | |
| Outcomes | Outcomes recorded at baseline and post‐intervention Cognitive outcome measures: MMSE Activity limitation outcomes: Modified Barthel Index Other outcome measures: motor free visual perception test, interest in performing the task | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation using block randomisation process. Envelopes were shuffled and the participant drew 1 after enrolment |
| Allocation concealment (selection bias) | Unclear risk | Whether the envelopes were opaque is unclear |
| Blinding of outcome assessment (detection bias) | Low risk | Blind |
| Incomplete outcome data (attrition bias) | Low risk | There does not appear to be any attrition and all outcome measures appear to be reported in full |
| Selective reporting (reporting bias) | Unclear risk | Unclear ‐ not privy to protocol |
| Methods | RCT | |
| Participants | Study took place in Korea 24 participants: 12 intervention, 12 control Inclusion criteria: ≥ 1 year post stroke with plateau in motor recovery after conventional rehabilitation and the ability to stand for 30 min and walk indoors independently (approximately 30 m) Exclusion criteria: severe visual or cognitive impairment or musculoskeletal disorders that could interfere with tests Mean (SD) age: intervention group 52 (10) years, control group 52 (7) years 54% men Timing post stroke: intervention group mean (SD) 26 (10) months, control group 24 (9) months | |
| Interventions | VR intervention: IREX VR system using a video capture system to capture the participant's whole body movement. The participant was able to view their body movements in real time on a screen in front of them immersed in a virtual environment. Games included stepping up/down, shark bait (capturing stars while avoiding eels and sharks by weight shift) and snowboarding. Participants were challenged by increasing resistance (e.g. adding weights) or increasing the speed. Control intervention: conventional physiotherapy designed to facilitate standing balance function during walking. Included practice of weight shift, muscle strengthening, functional reach or picking up objects Sessions for VR group: 30 min, 4 times/week for 4 weeks (8 h) of VR plus conventional physiotherapy 40 min, 4 times/week for 4 weeks (approximately 10.5 h) (approximately 18.5 h total) Sessions for control group: 40 min, 4 times/week for 4 weeks (approximately 10.5 h total) | |
| Outcomes | Outcomes recorded at baseline and post intervention Lower limb function and activity outcomes: 10‐m walk test, GAIT‐RITE gait analysis system, Berg balance scale, Balance performance monitor Global motor function outcomes: modified Motor Assessment Scale | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The sequence was generated using a lottery system |
| Allocation concealment (selection bias) | Low risk | Using sealed, opaque envelopes |
| Blinding of outcome assessment (detection bias) | Low risk | Blind |
| Incomplete outcome data (attrition bias) | Low risk | Does not appear to have any missing data |
| Selective reporting (reporting bias) | Low risk | No other outcomes were collected |
| Methods | RCT | |
| Participants | Recruited from a rehabilitation hospital in Korea 28 participants: 15 intervention, 13 control Inclusion criteria: not stated Exclusion criteria: people with a MMSE‐K score of < 10; people presenting with severe cognitive impairment of aphasia and unable to understand instructions. People with poor sitting balance such that they could not sit on a chair with back and armrests. People with limited ROM of the neck due to orthopaedic problems, and people with loss of visual acuity such that they could not perceive content on a computer screen Mean (SD) age: intervention group 66.5 (11) years, control group 62 (15.8) years 39% men Stroke details: 39% right hemiparesis Timing post stroke: intervention group mean (SD) 18.2 (11.3) d, control group 24 (31.1) d | |
| Interventions | VR intervention: IREX system (30 min 3 times/week) plus computer‐assisted cognitive rehabilitation (30 min twice/week) Control intervention: computer‐assisted rehabilitation (30 min 5 times/week) Sessions were 30 min, 5 times/week over 4 weeks (approximately 6 h of VR in total) | |
| Outcomes | Outcomes recorded at baseline and post intervention Upper limb function outcomes: Motricity index Lower limb function outcomes: Motricity index Cognitive function: computerised neuropsychological test and Tower of London test Activity limitation outcome: Korean modified Barthel Index | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | High risk | Not blinded |
| Incomplete outcome data (attrition bias) | Low risk | No withdrawals |
| Selective reporting (reporting bias) | Low risk | No other outcome data collected |
| Methods | RCT | |
| Participants | Recruited from Department of Rehabilitation, Korea 24 participants: 12 intervention, 12 control Inclusion criteria: participants diagnosed with unilateral spatial neglect through the line bisection test or star cancellation test Exclusion criteria: severe cognitive impairment or aphasia; insufficient sitting balance to sit on a chair with a back and armrests; restricted neck movement, poor eyesight or unable to recognise objects on a screen Mean (SD) age: intervention group 62.3 (10.2) years, control group 67.2 (13.9) years 58% men Timing post stroke: intervention group 22.8 (7.6) d, control group 25.5 (18.5) d | |
| Interventions | VR intervention: IREX Control intervention: conventional rehabilitation tasks such as visual tracking, reading and writing, drawing and puzzles Sessions were 30 min, 5 d/week for 3 weeks (approximately 7.5 h total) | |
| Outcomes | Outcomes recorded at baseline and post‐intervention Activity limitation outcomes: Korean Modified Barthel Index Other outcomes: Star cancellation test, Line bisection test, Catherine Bergego Scale | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded to allocation |
| Incomplete outcome data (attrition bias) | Low risk | No withdrawals |
| Selective reporting (reporting bias) | Low risk | No other outcome data collected |
| Methods | RCT | |
| Participants | Recruited from an inpatient setting in Korea 20 participants: 10 intervention, 10 control Inclusion criteria: > 6 months post diagnosis of stroke. Score of ≥ 19/30 on the MMSE. Able to maintain upright posture without any assistance Exclusion criteria: orthopaedic surgery, history of arthritis, hand or upper limb pain, epilepsy, psychiatric illnesses Mean age: not reported Timing post stroke: intervention group mean (SD) 12.6 (7.12) months, control group 12.85 (6.06) months | |
| Interventions | VR intervention: Nintendo Wii Sports (boxing and tennis) Control intervention: no intervention Sessions were 30 min, 3 times/week for 3 weeks | |
| Outcomes | Outcomes recorded at baseline and post intervention Gait outcomes: postural assessment scale Global motor function outcomes: modified Motor Assessment Scale Activity limitation outcomes: Functional Independence Measure | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported in adequate detail to make judgement |
| Selective reporting (reporting bias) | Unclear risk | No access to protocol |
| Methods | RCT | |
| Participants | Recruited from an institute of rehabilitation, Italy 80 participants: 40 intervention, 40 control Inclusion criteria: diagnosis of stroke within 1 year of enrolment and score of > 24/30 on the MMSE Exclusion criteria: clinical evidence of cognitive impairment, apraxia, neglect, language disturbance, complete paralysis of the UE, upper limb sensory disorders or post‐traumatic injury, which prevented the execution of exercises Mean (SD) age: 64 (16.4) years 58% men Time since onset of stroke: mean (SD) 5.7 (3.5) months | |
| Interventions | VR intervention: reinforced feedback in virtual environment (RFVE). Participants in the intervention group received 1 h of traditional rehabilitation and 1 h of RFVE. The RFVE involved sitting in front of a wall screen grasping a sensorised real object (ball, disc or cube) with the affected hand. The target objects were displayed on the wall screen. The physiotherapist created a sequence of virtual tasks that the participant had to perform on his workstation (e.g. pouring water from a glass, using a hammer) Control intervention: traditional neuromotor rehabilitation including postural control, exercises for hand pre‐configuration, manipulative and functional skills, proximal‐distal exercises Sessions were 1 h/d, 5 d/week for 4 weeks (approximately 20 h total) | |
| Outcomes | Outcomes recorded at baseline and post intervention Upper limb function outcomes: Fugl Meyer Activity limitation outcomes: Functional Independence Measure Other outcomes: Modified Ashworth Scale (spasticity) Adverse events reported | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes |
| Blinding of outcome assessment (detection bias) | Low risk | Masked to allocation |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | Author confirmed no other outcomes collected |
| Methods | RCT | |
| Participants | 77 participants: 39 VR group, 38 control group Recruited from 4 clinical settings in Switzerland Main inclusion criteria: diagnosis of 1, first ever cerebrovascular accident verified by brain imaging (MRI or CT); chronic impairment after stroke (minimum 6 months); moderate‐severe arm paresis, as indicated by a score of 8‐38 on arm section of Fugl‐Meyer assessment (which has a maximum of 66 points); aged ≥ 18 years; able to sit in a chair without any additional support and without leaning on the back rest; passive ROM in the shoulder as assessed with the neutral zero method: anteversion/retroversion 80°/0°/20°, abduction/adduction 60°/0°/10°, inner and outer rotation 20°/0°/20°; passive ROM in the elbow as assessed with the neutral zero method; flexion/extension 100°/40°/40°; no excessive spasticity of the affected arm (modified Ashworth Scale ≤ 3); no serious medical or psychiatric disorder as assessed by their physician; no cybersickness (nausea when looking at a screen or playing computer games); no pacemaker or other implanted electric devices; bodyweight < 120 kg; no serious cognitive defects or aphasia Mean age (SD): intervention group 55 (13), control group 58 (14) years 60% men Timing post stroke: mean (SD) 52 (44) months intervention group, 40 (45) months control group | |
| Interventions | VR intervention: during the robotic therapy with ARM in, each of 3 therapy modes (mobilisation, games, and training for ADL) had to be done for ≥ 10 min Control intervention: common neurorehabilitation treatment given to patients after stroke in outpatient facilities, namely OT or physiotherapy. Therapists were asked to give regular therapy, usually including mobilisation, games, ADL, or any combination of the 3. Their only restriction was not to use automated technical devices that might be available in therapy settings. For both groups, therapy was given 3 times/week in the centres for a period of 8 weeks (total 24 sessions) and sessions were ≥ 45 min | |
| Outcomes | Outcomes assessed 3‐4 weeks before assignment, immediately before therapy (baseline), after 4 weeks of therapy, at the end of 8 weeks of therapy, and 16 weeks and 34 weeks after baseline Upper limb function: Fugl Meyer UE, Wolf Motor Function Test, Motor Activity Log (quality of movement) Quality of life and participation: Stroke Impact Scale, Goal attainment scale Adverse events reported | |
| Notes | NCT00719433 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list |
| Allocation concealment (selection bias) | Low risk | Tamper‐evident envelopes |
| Blinding of outcome assessment (detection bias) | Low risk | Assessors were masked to treatment allocation |
| Incomplete outcome data (attrition bias) | Low risk | Few withdrawals. ITT analysis conducted |
| Selective reporting (reporting bias) | Low risk | Registered on clinical trial |
| Methods | RCT | |
| Participants | Recruited via a hospital in Korea 52 participants: 26 intervention, 26 control Inclusion criteria: 1865 years old and diagnosed with stroke within the last 6 months; able to walk > 10 m without or with assisting devices such as orthotics, a walker, or a cane; no symptoms with any lower motor neuron lesion and orthopedic diseases; a score > 24 points on the MMSE; and able to read the words on a monitor 60 cm away at eye level Exclusion criteria: failure to meet inclusion criteria Mean (SD) age: intervention group 48.1 (4.4) years, control group 45.3 (4.2) years 69% men | |
| Interventions | VR intervention: the Space Balance 3D training system is equipped with 2 wireless force plates. 3 kinds of balance training were implemented using Space Balance 3D, which can be used for both training and testing. According to the participants’ movement, the real‐time tilting angle and foot plates are indicated on a computer screen. The participant moves to 'hit' a predetermined target. Intervention was provided in addition to conventional rehabilitation exercises Control intervention: conventional rehabilitation only Sessions were 30 min, 5 times/week for 3 weeks. The control group only participated in usual rehabilitation thus there was a difference between groups in the amount of therapy received | |
| Outcomes | Outcomes assessed post intervention Balance: Berg Balance Scale Postural Assessment Scale for Stroke Patients Timed Up and Go Test | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Method not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Unclear risk | Details not described |
| Selective reporting (reporting bias) | Unclear risk | Protocol or clinical trial register not mentioned |
| Methods | RCT | |
| Participants | Recruited from inpatients in a tertiary rehabilitation setting in Singapore 105 participants Inclusion criteria: within first 6 weeks after stroke Exclusion criteria: none reported Mean (SD) age: 57.5 (9.8) years in the total sample Timing post stroke: mean 13.7 (8.9) d in the total sample | |
| Interventions | VR intervention: Nintendo Wii gaming therapy in addition to standard conventional rehabilitation Control intervention: conventional therapy in addition to standard rehabilitation Control intervention: usual care Sessions were 4 times/week for 3 weeks | |
| Outcomes | Outcomes assessed post intervention and at 4 and 8 weeks after the completion of intervention Upper limb: Fugl Meyer Assessment Upper limb: Action Research Arm Test Functional Independence Measure Stroke Impact Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated |
| Allocation concealment (selection bias) | Low risk | Managed externally |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded |
| Incomplete outcome data (attrition bias) | Low risk | Low attrition. ITT analysis with baseline values used |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Methods | RCT | |
| Participants | Recruited from a hospital in Korea 26 participants: 13 intervention, 13 control Inclusion criteria: adults within 3 months of stroke with the capacity to understand and follow simple instructions. Able to grasp and release affected hand, with manual muscle test ≥ grade 3. Able to maintain standing or sitting position independently and no visual deficit Exclusion criteria: failure to meet above criteria Mean (SD) age: intervention group 57.15 (15.42) years, control group 57.92 (12.32) years Timing post stroke: intervention group mean (SD) 24.69 (15.59) d, control group 23.92 (20.70) d | |
| Interventions | VR intervention: conventional therapy plus additional therapy time using IREX Control intervention: conventional therapy alone Sessions were 30 min, 5 d/week for 4 weeks | |
| Outcomes | Outcomes recorded at baseline and post‐intervention Upper limb function outcomes: Fugl Meyer, Manual Function Test Activity limitation outcomes: Korean Modified Barthel | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded to allocation |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported in adequate detail to make judgement |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available |
| Methods | RCT | |
| Participants | Recruited from rehabilitation units in Hong Kong 58 participants: 20 VR, 16 video‐based program, 22 no treatment Inclusion criteria: 50‐85 years old, medically stable with no previous psychiatric history, able to follow simple instructions and write with a pen in Chinese or English, consistent volitional motor response, good visual tracking, discrimination ability and figure ground skills, sustained attention span of ≥ 10 min Exclusion criteria: computer‐related phobia or previous training in Mass Transit Railway Skills Mean (SD) age: VR group 71 (16) years, video‐based program group 71 (15) years, no treatment group 73 (10) years 31% men Timing post stroke: VR group mean (SD) 4 (4) years, video‐based program group 3 (3) years, no treatment group 5 (3) years | |
| Interventions | VR intervention: a VR program designed to retrain skills using the Mass Transit Railway. Activities included crossing the road and using the facilities at the station Video based program intervention: a video‐based program included instruction, modelling, demonstration, role playing, coaching and feedback on using the Mass Transit Railway No treatment group: no treatment 10 sessions of unspecified duration were provided for the participants in the VR and video program group | |
| Outcomes | Outcomes recorded at baseline and post‐intervention Other outcomes: behavioural rating scale, Mass Transit Railway Self Efficacy Scale | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly allocated into 2 groups using a statistical package random number generator tool |
| Allocation concealment (selection bias) | Low risk | Allocation was computer‐generated |
| Blinding of outcome assessment (detection bias) | Low risk | Blind |
| Incomplete outcome data (attrition bias) | Low risk | There were no missing data |
| Selective reporting (reporting bias) | Low risk | No other outcomes were collected |
| Methods | RCT | |
| Participants | Recruited from inpatients at a hospital in Seoul 22 Participants: 12 intervention group, 10 control group Inclusion criteria: > 6 months after stroke; could sit independently for ≥ 30 min, who had a MMSE‐K score of > 21 points, who had not participated in any balance training program during the previous 6 months, who had no orthopedic problems, such as a fracture, deformity, or severe osteoarthritis, and who were not taking any drugs for balance maintenance were included Exclusion criteria: failure to meet above criteria Mean (SD) age: intervention group 60.6 (8.8) years, control group 63.7 (4.7) years 27% men | |
| Interventions | VR intervention: Visual Feedback Training (VFT) was performed individually in a dedicated room containing the required equipment. VFT was performed using BIORescue (RM INGENIERIE, Rodez, France) equipment, which consists of a computer, a monitor, and a force plate. This force plate detects the posture and movements made by participants and this information is transferred to the computer, and processed for display on the monitor. This system encourages adoption of the correct posture by providing visual feedback and allows for design of customised exercise programs based on pre‐test data. The system also allows different exercise times and intensities for selected games, and within‐session variable rest times. In the study, the participants sat 1 m‐1.5 m away from the monitor on a pressure platform. Four types of exercise were performed during each session. The first exercise was training for stability and weight shift by balancing the amount of water in a flask. The second was training for stability and weight shift by driving a vehicle. The third exercise was skiing, which involved shifting the body in the anterior, posterior, left, and right directions in three‐dimensional space; and the fourth exercise used a memory recall program, during which the participant had to remember 4 pictures and to match the picture Control intervention: general physical therapy Both groups received general physical therapy. In addition, those in the intervention group received additional 30‐min sessions, 5 d/week for 4 weeks | |
| Outcomes | Outcomes assessed following intervention Static balance measured using the Good Balance System Balance: Functional Reach Test Visual perception: Motor Free Visual Perception Test | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation software |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | High risk | Some dropouts but details of this and method for dealing with this not described |
| Selective reporting (reporting bias) | Unclear risk | Protocol or clinical trial register not mentioned |
| Methods | RCT | |
| Participants | Recruited from a hospital in Korea 21 participants: 10 intervention group, 11 control group Inclusion criteria: > 6 months post stroke, not taking medication that can affect balance, MMSE score of < 24/30, no pain or disability associated with acute musculoskeletal conditions, sitting to sidelying with moderate assistance, sitting for > 10 s without support and standing without support for 1 min Exclusion criteria: Pusher syndrome Mean (SD) age: intervention group 47.9 (12) years, control group 54 (11.9) years 67% men Timing post stroke: intervention group mean (SD) 11.7 (4.5) months, control group mean 11.0 (4.7) months | |
| Interventions | VR intervention: augmented reality had 3 stages and 16 scopes. The stages progressed from exercise programs in lying position to sitting to standing using a therapeutic ball or foothold. The VR included videos of postural control training for guiding the participants to perform ideal postural control motions. The head‐mounted device showed 2 views: the modelled movement was on one side and the actual movement on the other side. The participant could watch the modelled movement and listen to a recorded sound in order to compare the normal movement with his/her own movement. This was completed in addition to usual physiotherapy sessions Control intervention: no intervention except for usual physiotherapy sessions Sessions were 30 min/d for 4 weeks | |
| Outcomes | Outcomes assessed post intervention Timed Up and Go Test Berg Balance Scale Gait (measured using the GAITRite system ‐ gait velocity, cadence, step length, and stride length) | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Drawing lots |
| Allocation concealment (selection bias) | High risk | Participant selection from box (paper had either number 1 or 2 on) |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded outcome assessor |
| Incomplete outcome data (attrition bias) | Low risk | Low number of dropouts and ITT analysis performed (last observation carried forward) |
| Selective reporting (reporting bias) | Unclear risk | No mention of protocol or clinical trial registry |
| Methods | RCT | |
| Participants | Recruited from a hospital in Seoul 24 participants: 12 intervention, 12 control Inclusion criteria: stroke of > 6 months duration; a score of > 24 points on the MMSE‐K; ability to walk a distance of 10 m with or without an auxiliary device; no history of orthopedic conditions involving the lower limbs; ability to follow instructions and perform the exercise programs; and no visual or hearing impairment Exclusion criteria: failure to meet above criteria Mean (SD) age: intervention group 45.91 (12.28) years control group 49.16 (12.85) years 66% men | |
| Interventions | VR intervention: Wii and Wii Balance Board provided by Nintendo (Kyoto, Japan) and the Wii Fit Plus software were used. The VR‐based program was selected depending on the participants' interests and motivation, and the levels of difficulty were decided based on information provided in previous studies regarding suitable levels for balance improvement. The program consisted of: (1) sitting posture, (2) the knee bend and the other leg knee extend, (3) tightrope walking, (4) penguin teeter‐totter seesaw, (5) balance skiing, (6) rolling marble board, and (7) balance Wii Control intervention: the duration of the task‐oriented training program was 30 min. Each task took 3 min to perform, and a 1‐min break was provided between tasks. Each of the warm‐up and cooldown phases lasted for 2 min. The level of difficulty and frequency for each task were gradually increased during the 6 weeks with the participants’ consent, starting with 3 sets (12 times/set) All the participants also received general exercise therapy for 60 min/d, 5 d/week for 6 weeks. They participated in the VR‐based training program or task‐oriented training for an additional 30 min/d, 3 d/week for 6 weeks. | |
| Outcomes | Measured outcomes post intervention Balance: Functional reach test | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Not reported |
| Methods | RCT | |
| Participants | Recruited from a general hospital in Korea 18 participants: 10 intervention, 8 control Inclusion criteria: diagnosed with stroke and hemiparesis; able to follow verbal instructions; ≥ 6 months post‐stroke diagnosed by a physician; able to communicate (i.e. MMSE language section score from 24‐30), and a Modified Ashworth Scale (MAS) score < 2 for the UE Exclusion criteria: diplegia or a visual field defect Mean (SD) age: intervention group 69.2 (5.5) years, control group 73.1 (8.9) years 45% men, 55% right hemiparesis Timing post stroke: intervention group mean (SD) 16.2 (6.5) months, control group 17 (6.5) months | |
| Interventions | VR intervention: the VR‐based bilateral training (VRBT) involved a visual expression technique using animations and provided cognitive information for feedback. The animation consisted of symmetric and asymmetric upper‐extremity training as well as symmetric and asymmetric upper‐extremity training at 45° in a VR environment. The participants performed each movement for 4 min and then rested for 1 min to minimise fatigue. Depending on the severity of the deficits, the participant either grasped the handles or the affected hand was strapped to the handle. An UE instrument was used to control the inclination and width. A laptop, webcam, and monitor were used to create the VR environment Control intervention: the therapy program involved only bilateral UE exercises Both groups received conventional physical therapy: sessions were 30 min, 3 times/week for 6 weeks Both groups received additional therapy (either intervention or control) for 30 min, 3 times/week for 6 weeks | |
| Outcomes | Outcomes were assessed post intervention Electroencephalography | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Not reported |
| Methods | RCT | |
| Participants | Recruited from an outpatient rehabilitation centre in Israel 12 participants: 6 intervention, 6 control Inclusion criteria: unilateral left‐ or right‐sided stroke > 3 months previously. No hemispatial neglect or uncorrected visual field deficits including hemianopia and could understand and follow instructions (no receptive aphasia, MMSE evaluation) Exclusion criteria: shoulder or arm pain, lack of endurance as judged by their treating physician Mean (SD) age: intervention group 58.1 (14.6) years, control group 59.8 (15.1) years 50% men Stroke details: 58% right hemiplegia Timing post stroke: intervention group mean 2.6 (1.2) years, control group mean 3.8 (0.9) years | |
| Interventions | VR intervention: goal‐directed reaching tasks using the affected arm in a virtual environment (virtual supermarket, birds and balls, soccer, volleyball, VMall). Practice involved reaching but not grasp or manipulation. Task difficulty was matched to capabilities Control intervention: OT including exercises reaching for and holding cones, cups and other objects with and without external loading Sessions were 45 min for 9 sessions over a 3‐week period | |
| Outcomes | Assessed post intervention and 4 weeks after the end of intervention Fugl Meyer Arm Scale Composite Spasticity Index Reach Performance Scale for Stroke Upper limb activity: box and blocks test Upper limb activity: Wolf Motor Function Test Motor Activity Log Adverse events | |
| Notes | NCT01388400 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Coin toss |
| Allocation concealment (selection bias) | Low risk | As above ‐ coin toss |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded assessor |
| Incomplete outcome data (attrition bias) | Low risk | Small number of withdrawals |
| Selective reporting (reporting bias) | Low risk | Reported on clinical trial registry |
| Methods | RCT | |
| Participants | Recruited from outpatient services in the USA 99 participants: 51 intervention, 48 control Inclusion criteria: unilateral stroke within the previous 6 months with some voluntary UE movement (score of 11‐55 on the Fugl Meyer Assessment). Limited access to an organised stroke rehabilitation program and preserved cognitive function Exclusion criteria: lack of independence before the stroke (Modified Rankin Scale score of > 1) and injection to manage hypertonicity in the UE since stroke. Neglect (measured by > 3 errors on the star cancellation test), sensory loss score of ≥ 2 on the sensory item of the National Institutes of Health Stroke Scale and score of ≥ 3 on the Modified Ashworth Scale Mean (SD) age: intervention group 59.4 (13.6) years, control group 55.5 (12.6) years 65% men Stroke details: 49% right hemiplegia Timing post stroke: intervention group mean 117 (50.9) d, control group 125 (47) d | |
| Interventions | VR intervention: Hand Mentor Pro Robot assisted device uses a pneumatic pump to facilitate active‐assisted movement of the wrist and fingers. The device consists of 3 components: a computer control box, an arm unit and data‐collection device and a communications module. The arm unit stabilises the forearm so that the user is able to isolate the wrist and finger movement with the assistance of the pneumatic pump and the computer control box provides targeted goals with corresponding visual and auditory feedback. Feedback from the session is displayed on the screen and stored (including time of use, attempted and successful repetitions, wrist angle and pneumatic pressure) Control intervention: UE home exercise program prescribed by a therapist from a pool of exercises and activities. Weekly telephone calls were made to progress the program. Each participant was given an exercise book with instructions Robotic sessions were 2 h/d, 5 d/week for 8 weeks within a 12‐week period Home exercise program was 1 h/d, 5 d/week for 8 weeks within a 12‐week period Sessions were conducted with a physiotherapist or occupational therapist | |
| Outcomes | Outcomes assessed post intervention Stroke Impact Scale Center for Epidemiologic Studies Depression Scale (CES‐D) | |
| Notes | Disclosure: one author was Chairman of the Scientific Advisory Board and was previously a paid consultant for Kinetic Muscles. A second author was a paid consultant for Kinetic Muscles for this study NCT01144715 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated program |
| Allocation concealment (selection bias) | Low risk | Computer‐based program |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded assessor |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis conducted |
| Selective reporting (reporting bias) | High risk | Paper only reports 2 outcomes but others were described in the protocol |
| Methods | RCT | |
| Participants | Recruited from an outpatient rehabilitation unit in Spain 20 participants: 10 intervention, 10 control Inclusion criteria: people with stroke attending a rehabilitation program. Had hemiparesis and were aged 40+ years but ≤ 70 years. Had a stroke > 6 months ago and had absence of cognitive impairment (MMSE of ≥ 24/30). Able to follow instructions and able to maintain stride‐standing position for 30 s without assistance from another person Exclusion criteria: severe dementia or aphasia (Mississippi Aphasia Screening Test < 45), visual or hearing impairment restricting ability to interact with the intervention, hemispatial neglect and ataxia or cerebellar symptoms Mean (SD) age: intervention group 58.3 (11.6) years, control group 55.0 (11.6) years 45% men Stroke details: 65% ischaemic Timing post stroke: intervention group mean 407 (232) d, control group mean 587 (222) d | |
| Interventions | Intervention: 30 min conventional training plus 30 min of virtual rehabilitation. The set‐up consisted of a computer, audiovisual output system and motion tracking system. The output system consisted of a video display and audio system. The participant was immersed in a 3D environment; their feet were represented by 2 shoes that mimicked their movement in the real world. The objective of the task was to reach the items with 1 foot while maintaining the other foot within the circle. Conducted by a physiotherapist Control intervention: 1 h of conventional physiotherapy including balance exercises, task‐specific reaching, stepping and walking under different conditions. Conducted by a physiotherapist Sessions were 60 min, 5 times/week for 4 weeks | |
| Outcomes | Outcomes assessed post intervention Berg Balance Scale Balance and gait subscales of the Tinetti Performance Oriented Mobility Assessment Brunel Balance Assessment 10 m walking test Adverse events reported | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence |
| Allocation concealment (selection bias) | Unclear risk | Concealed in envelopes. Not clear whether they were opaque or not |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded therapist |
| Incomplete outcome data (attrition bias) | Low risk | Low withdrawals and analysis included only those contributing data |
| Selective reporting (reporting bias) | Unclear risk | No mention of protocol or trial registration |
| Methods | RCT | |
| Participants | 20 participants: 10 intervention, 10 control Inclusion criteria: diagnosis of stroke and medically stable Mean age 60.4 (13.3) years (total sample) 65% men Timing post stroke: 14.21 (5.5) d | |
| Interventions | VR intervention: locally developed VR program Control intervention: usual care The VR group received an additional 30 min of daily VR therapy for 2 weeks | |
| Outcomes | Fugl Meyer Motor Scale (upper limb) Action Research Arm Test Berg Balance Scale Functional Independence Measure Gait speed | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported (conference abstract) |
| Allocation concealment (selection bias) | Unclear risk | Not reported (conference abstract) |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported (conference abstract) |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported (conference abstract) |
| Selective reporting (reporting bias) | Unclear risk | Not reported (conference abstract) |
| Methods | RCT | |
| Participants | Recruited from rehabilitation centres in Manila, Phillipines 16 participants: 8 intervention, 8 control Inclusion and exclusion criteria: not reported Mean age: 55.69 (9.88) for the total sample 69% men Timing post stroke: mean 38.56 (14.51) months | |
| Interventions | VR intervention: Nintendo Wii Control intervention: not reported Intervention was provided twice/week for 6 weeks | |
| Outcomes | Outcomes assessed post intervention Fugl Meyer Motor Assessment Scale Fast Fourier Transform (FFT) analysis | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | States that participants were randomised using the 'fishbowl' method |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding of outcome assessment (detection bias) | Low risk | Assessor blinded |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Details not reported (conference abstract) |
| Methods | RCT | |
| Participants | Recruited from an inpatient hospital in China 23 participants: 11 intervention, 12 control Inclusion criteria: stroke (confirmed by CT or MRI), stable vital signs, aged 40‐78 years, able to walk independently for 10 m, unilateral hemipareses for < 3 months resulting from first stroke and residual gait impairment (reduced walking speed) and adequate mental and physical capacity to attempt the tasks as instructed Exclusion criteria: history of recent deep vein thrombosis of the lower limbs, other neurological or orthopedic pathology, or serious visual deficits Mean (SD) age: intervention group 58.18 (11.15) years, control group 63.09 (11.51) years 78% men Timing post stroke: intervention group mean 48.91 (17.01) d, control group mean 48.91 (17.92) d | |
| Interventions | VR intervention: a series of videos (e.g. climbing a mountain, crossing a street) was shown on screen and synced with treadmill velocity. The participant wore a harness to support body weight Control intervention: individualised walking training on the ground according to neurodevelopmental therapy Both of the groups received training of 20‐40 min/d, 5 d/week, for 3 weeks | |
| Outcomes | Outcomes assessed post intervention Motion analysis system (Vicon) to measure pelvic tilt, obliquity and rotation | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer randomisation program |
| Allocation concealment (selection bias) | Low risk | Sequentially‐numbered, opaque, sealed envelopes |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinded to allocation |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described in sufficient detail to make judgement |
| Selective reporting (reporting bias) | Low risk | Registered on clinical trial and all measures reported |
| Methods | RCT | |
| Participants | Recruited from a rehabilitation inpatient unit in Japan 28 participants No further details reported | |
| Interventions | VR intervention: 10 sessions of upper limb exercises via a Nintendo Wii over 2 weeks in addition to conventional rehabilitation Control intervention: conventional rehabilitation | |
| Outcomes | Outcomes assessed post intervention and 2 weeks after the end of intervention Fugl Meyer Assessment of Upper Limb Motor Function Wolf Motor Function Test Box and Block Test Motor Activity Log | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not reported (conference abstract) |
| Allocation concealment (selection bias) | Unclear risk | Details not reported (conference abstract) |
| Blinding of outcome assessment (detection bias) | Unclear risk | Details not reported (conference abstract) |
| Incomplete outcome data (attrition bias) | Unclear risk | Details not reported (conference abstract) |
| Selective reporting (reporting bias) | Unclear risk | Details not reported (conference abstract) |
| Methods | RCT | |
| Participants | Recruited from a rehabilitation hospital in Quebec, 2 driving evaluation centres in Montreal and from a private driving evaluation clinic 39 participants: 20 intervention, 19 control Inclusion criteria (for stroke participants): people with a diagnosis of stroke that did not pass the driving tests at a recognised driving evaluation service. Had licence to drive and were driving prior to the stroke and desire to return to driving Exclusion criteria: medical condition precluding driving (for example, hemianopia, seizures), received their driving evaluation > 2 years post diagnosis, unable to communicate in English or French, inadequate communication of basic verbal instructions or judged as dangerous by the therapist in the on‐road evaluation Mean (SD) age: intervention group 68 (14) years, control group 69 (9) years Stroke details: 31% right hemiparesis Timing post stroke: intervention group mean (SD) 1.4 (1) years, control group 1.7 (1) years | |
| Interventions | VR intervention: driving simulator. Simulator is a car frame with 3 large screens providing a large field of view. Participants were progressed through 4 increasingly complex scenarios. In level 1, participants were familiarised with the simulator and controls; level 2 involved a simulated road circuit without traffic; level 3 focused on performing different driving manoeuvres and level 4 involved a variety of traffic conditions (for example, rain, wind, reduced visibility, pedestrians). Instant feedback was provided by the simulator when errors were made Control intervention: no intervention provided Sessions were 60 min, twice/week for 8 weeks (16 h total) | |
| Outcomes | Outcomes recorded at baseline and post‐intervention (or after 8 weeks for the control group) Activity limitation outcomes: DriveAble Testing Ltd Driver Evaluation | |
| Notes | Note that this study also recruited 6 participants with traumatic brain injury. However, data for participants with stroke were able to be separated. This review reports on the stroke data only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a computer program to generate |
| Allocation concealment (selection bias) | Low risk | Opaque, sealed envelopes |
| Blinding of outcome assessment (detection bias) | Low risk | Blind |
| Incomplete outcome data (attrition bias) | Low risk | 7 participants (5 control group, 2 simulator group) did not complete the outcome evaluation and were therefore considered to have dropped out from the study. Analysis was completed based on the actual number of participants contributing data. ITT analyses were conducted |
| Selective reporting (reporting bias) | Low risk | No other outcomes were collected |
| Methods | RCT | |
| Participants | Recruited from hospitals in Australia 41 participants: 21 intervention group, 20 control group Inclusion criteria: ischaemic lesion or haemorrhagic stroke with upper limb motor impairment; 2‐48 months post stroke; ≥ 10° active movement at the shoulder, elbow, wrist and ≥ 2 digits; English speaking and ≥ 18 years Exclusion criteria: MMSE score of < 24/30; peripheral neuropathy significantly affecting sensorimotor function; unstable blood pressure; and formal upper limb therapy during the trial. Mean (SD) age: intervention group 59.9 (13.8) years, control group 56.1 (17) years 76% men Stroke details: 79% ischaemic Timing post stroke: intervention group mean (SD) 11.0 (3.1) months, control group 6.5 (2.1) months | |
| Interventions | VR intervention: Nintendo Wii Sports (golf, boxing, baseball, bowling and tennis) with the controller used in the person's more affected hand. Rather than playing each game, specific drills were introduced and varied. For people with poor grip strength, a self‐adhesive wrap was applied. Therapy was performed in standing position wherever possible Control intervention: modified constraint‐induced movement therapy: participants wore the mitt on the less affected hand for up to 90% of waking hours. Therapy included shaping practice tailored to each person's motor function with increasing task complexity, strength, dexterity, movement distance and speed. Training tasks included everyday activities using the more affected arm for 15‐20 min of continuous activity Therapy for both groups was delivered in the research institute or the person's home by a trained therapist. Dose was matched Sessions were 60 min on 10 consecutive weekdays augmented by progressively increasing home practice | |
| Outcomes | Outcomes assessed post intervention and at 6 months Upper limb outcomes: Wolf Motor Function Test timed tasks Motor Activity Log Quality of Movement Scale Fugl Meyer assessment Wolf Motor Function Test, maximal strength and submaximal strength Active and passive ROM Modified Ashworth Scale Box and Block Test Self‐perceived improvement and participant satisfaction questionnaire Adverse events reported | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated schedule |
| Allocation concealment (selection bias) | Low risk | Allocations were concealed in numbered, opaque envelopes prior to trial commencement by a person not involved with assessments or therapy and opened by the therapist after baseline assessments |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded therapist |
| Incomplete outcome data (attrition bias) | Low risk | Transparent reporting and ITT analysis conducted |
| Selective reporting (reporting bias) | Unclear risk | Could not find reference to study protocol or trial registration |
| Methods | RCT | |
| Participants | Study took place in New Jersey, USA 18 participants: 9 intervention, 9 control Inclusion criteria: chronic hemiparesis after stroke with residual gait deficits, partial antigravity dorsiflexion, able to walk 15 metres without the assistance of another person, sufficient communication and cognitive ability to participate Exclusion criteria: motion sickness and receiving concurrent therapy Mean (SD) age: intervention group 62 (10) years, control group 61 (8) years 83% men Stroke details: 44% right hemiparesis Timing post stroke: intervention group mean (SD) 38 (25) months, control group 58 (26) months | |
| Interventions | VR intervention: Rutgers ankle rehabilitation system (a 6‐degree‐of‐freedom platform force‐feedback system) that allows participants to exercise the lower extremity by navigating through a virtual environment displayed on a desktop computer. Participants executed the exercises by using the foot movements to navigate a plane or a boat through a virtual environment that consisted of a series of targets Control intervention: Rutgers ankle rehabilitation system without the virtual environment. Participants were instructed by the therapist on which direction to move their foot and were paced by a metronome cueing them to complete a comparable number of repetitions Sessions were 60 min, 3 times/week for 4 weeks (12 h total) | |
| Outcomes | Outcomes recorded at baseline, post intervention and at 3 months Lower limb function and activity outcomes: gait speed over 7‐m walkway, 6MWT, Patient Activity Monitor (distance walked, number of steps/d, average speed, step length, top speed) | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was performed based on the table of numbers method (generated by a computer) |
| Allocation concealment (selection bias) | Low risk | Allocation was done by an external person to the project and held in a database spreadsheet on a computer in his office which was password protected |
| Blinding of outcome assessment (detection bias) | Low risk | Blind |
| Incomplete outcome data (attrition bias) | Low risk | 1 participant in the robotic‐VR group was lost to follow‐up because of personal reasons. 1 outlier was identified in the robotic‐VR group following the descriptive analysis of the endurance test (6MWT), the values presented for this individual were 2 SD from the mean therefore he was excluded from the analysis |
| Selective reporting (reporting bias) | Low risk | No other outcomes were collected |
| Methods | RCT | |
| Participants | Recruited from a rehabilitation unit in Italy 50 participants: 25 intervention, 25 control Inclusion criteria: hemiparesis in the subacute phase (< 3 months from onset), with moderate gait deficits (FAC ≥ 2) caused by a first ever stroke and aged 18‐85 years Exclusion criteria: motor or cognitive sequale from prior cardiovascular accidents, other chronic disabling pathologies, orthopaedic injuries that could impair locomotion, spasticity that limited lower extremity ROM to < 80%, sacral skin lesions, MMSE score < 24/30 and hemispatial neglect, attention or memory deficit Mean (SD) age: intervention group 58.36 (9.62) years, control group 61.96 (10.31) years Stroke details: 58% right hemiparesis Timing post stroke: intervention group mean (SD) 61 (36.47) d, control group mean (SD) 41.65 (36.89) d | |
| Interventions | VR intervention: balance therapy using the Nintendo Wii Fit. During the intervention, 3 games were carried out in order to train balance, co‐ordination and endurance under the supervision of a physiotherapist: hula hoop, bubble blower and sky slalom Control intervention: balance therapy focusing on trunk stabilisation, weight transfer to the paretic leg and exercise with Freeman board for balance and proprioception Sessions for the VR and control interventions were 20 min, 3 times/week for 4 weeks. This was in addition to usual physical therapy which was 40 min, twice/d | |
| Outcomes | Outcomes assessed post intervention and 1 month after the end of intervention Berg Balance Scale 10 mwalk test at a self‐selected speed Functional Ambulatory Category Barthel Index | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded assessor |
| Incomplete outcome data (attrition bias) | High risk | Multiple withdrawals and unbalanced across groups |
| Selective reporting (reporting bias) | Unclear risk | Protocol or trial registration not reported |
| Methods | RCT | |
| Participants | Recruited in Korea 20 participants: 10 intervention group, 10 control group Inclusion criteria: history of stroke onset of > 6 months prior to the study; ability to walk without using a walking aid for a minimum of 15 m; MMSE score of > 24/30; able to comprehend and follow simple instructions Exclusion criteria: other neurological condition, orthopaedic disease or visual impairment Participant details not reported | |
| Interventions | VR intervention: community‐based VR scene exposure combined with treadmill training. A VR video was displayed on a screen 3 m in front of the treadmill using a video projector. The VR video comprised images of community ambulation, such as walking on sidewalks, level walking, slope walking and walking over obstacles. 5 min of treadmill training was followed by 2 min rest to minimise fatigue Control intervention: muscle strengthening, balance training, indoor and outdoor gait training Both groups had conventional physical therapy for 60 min/d, 5 d/week for 4 weeks The VR and control intervention was an additional 30 min/d, 3 d/week for 4 weeks | |
| Outcomes | Outcomes assessed post intervention Static balance ability (postural sway path length and speed at the center of pressure) | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | High risk | Excluded participants with low participation rate |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Methods | RCT | |
| Participants | Study took place in Italy 38 participants: 25 intervention, 13 control Inclusion criteria: mild‐intermediate arm motor impairment due to ischaemic stroke in the MCA territory within the past 3 months Exclusion criteria: cognitive impairment, neglect, apraxia, aphasia interfering with comprehension Mean (SD) age: intervention group 62 (9) years, control group 61 (7) years 66% men Timing post stroke: intervention group mean (SD) 2.5 (1.5) months, control group 2.6 (1.6) months | |
| Interventions | VR intervention: magnetic receivers were positioned on the participant's arm. As the participant grasped and moved real objects, software created a virtual environment, which displayed virtual handling and target objects, for example an envelope and a mailbox, a hammer and a nail, a glass and a carafe. While performing the virtual tasks such as putting the envelope in the mailbox the participant moves the real envelope and sees on screen the trajectory of the corresponding virtual objects toward the virtual mailbox. Participants could see not only their own movement but also the correct trajectory that they had to execute, pre‐recorded by the therapist. This allowed participants to easily perceive motion errors and adjust them during the task Control intervention: 'conventional' rehabilitation focused on the upper limb Sessions were 60 min, 5 times/week for 5‐7 weeks (approximately 25‐35 h total) | |
| Outcomes | Outcomes recorded at baseline and post‐intervention Upper limb function and activity outcomes (arm): Fugl Meyer UE Scale Activity limitation outcomes: Functional Independence Measure Adverse events reported | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Personal correspondence with the study author reports the use of a simple computer‐generated sequence |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding of outcome assessment (detection bias) | Low risk | Blind |
| Incomplete outcome data (attrition bias) | High risk | There were 3 dropouts from the control group and the analysis was per‐protocol |
| Selective reporting (reporting bias) | Low risk | No other outcomes were collected |
| Methods | RCT | |
| Participants | Study took place in Italy 36 participants: 18 intervention, 18 control Inclusion criteria: single ischaemic stroke in the MCA region with mild to intermediate arm motor impairment (Fugl Meyer UE score 30‐55) Exclusion criteria: clinical evidence of cognitive impairment, apraxia (< 62 points on the 'De Renzi' test), neglect or language disturbance interfering with verbal comprehension (> 40 errors on the Token test) Mean (SD) age: intervention group 66 (8) years, control group 64 (8) years 58% men Stroke details: 44% right hemiparesis Timing post stroke: intervention group mean (SD) 15 (7) months, control group 12 (4) months | |
| Interventions | VR intervention: the telerehabilitation program used 1 computer workstation at the participant's home and 1 at the rehabilitation hospital. The system used a 3D motion tracking system to record arm movements through a magnetic receiver into a virtual image. The participant moved a real object following the trajectory of a virtual object displayed on the screen in accordance with the requested virtual task. 5 virtual tasks comprising simple arm movements were devised for training Control intervention: specific exercises for the upper limb with progressive complexity. Started with control of isolated movements without postural control, then postural control including touching different targets and manipulating objects Sessions were 60 min, 5 times/week for 4 weeks (20 h total) | |
| Outcomes | Outcomes recorded at baseline, post intervention and at 1 month Upper limb function and activity outcomes (arm): Fugl Meyer UE Scale Participation restriction and quality of life outcomes: Abilhand scale Other outcome measures: Modified Ashworth Scale | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Personal correspondence with the study author reports the use of a simple computer‐generated sequence |
| Allocation concealment (selection bias) | Low risk | Opaque, sequentially numbered envelopes |
| Blinding of outcome assessment (detection bias) | Low risk | Blind |
| Incomplete outcome data (attrition bias) | Low risk | There were no missing data |
| Selective reporting (reporting bias) | Low risk | No other outcomes were collected |
| Methods | RCT | |
| Participants | Recruited from a rehabilitation hospital in Rome, Italy 50 participants: 27 intervention, 23 control Inclusion criteria: single ischaemic stroke in the MCA territory > 6 months ago demonstrated by CT or MRI, received conventional physiotherapy early after stroke, mild‐intermediate motor impairments of the arm (score of 20‐60 on the Fugl Meyer UE Scale) Exclusion criteria: clinical history or evidence of cognitive impairments, neglect, apraxia or aphasia interfering with verbal comprehension Mean (SD) age: intervention group 59 (8) years, control group 62 (10) years 58% men Stroke details: 58% right hemiparesis Timing post stroke: intervention group mean 15 (13) months, control group 15 (12) months | |
| Interventions | VR intervention: participants were asked to perform motor tasks with real objects (for example an envelope or a glass), which were displayed as tasks within the virtual environment (for example putting an envelope in the mailbox, breaking eggs, moving a glass over a table, placing a ball in a basket). A 3D magnetic receiver was used to record the motions. Participants were asked to emulate the tasks as per the therapist's pre‐recorded movement Control intervention: participants were asked to perform specific exercises for the arm, for example touching different targets, manipulating objects and following trajectories on a plan Sessions were 60 min, 5 times/week for 4 weeks (20 h total) | |
| Outcomes | Outcomes recorded at baseline and post‐intervention Upper limb function and activity outcomes (arm): Fugl Meyer UE Scale Activity limitation outcomes: Functional Independence Measure Adverse events reported | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Personal correspondence with the study author reports the use of a simple computer‐generated sequence |
| Allocation concealment (selection bias) | Low risk | Sequentially‐numbered, opaque, sealed envelopes |
| Blinding of outcome assessment (detection bias) | Low risk | Blind |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis was completed. In the case of missing data the authors used a 'best, worst and likely' approach to data imputation. There was a small amount of attrition and the reasons for this were reported. |
| Selective reporting (reporting bias) | Low risk | No other outcomes were collected |
| Methods | RCT | |
| Participants | Recruited from an inpatient rehabilitation centre in the Netherlands 70 participants: 37 intervention, 33 control Inclusion criteria: first stroke 1‐12 weeks ago, medically stable, display limited arm function but have active control of the elbow/shoulder of ≥ 15°, be free from other conditions or pain, be able to follow instructions and understand (and see) the visual game display Exclusion criteria: treated with botulinum toxin and/or electrical stimulation to improve arm function before or during participation Mean (SD) age: intervention group 60.3 (9.7) years, 58 (11.4) years Stroke details: 78% ischaemic, 60% right hemiparesis Timing post stroke: intervention group mean 7.3 (3.4) years, control group mean 6.8 (3.1) years | |
| Interventions | VR intervention: training using a customised arm support program. Training consisted of playing games with the affected arm, supported by the device, working toward maximising movement ability with as little arm support as possible. The training involved mostly shoulder and elbow movements with exercises structured according to categorisation of the games for increasing difficulty (1D, 2D and 3D) Conventional therapy: standard set of exercises to reflect usual physiotherapy and OT Sessions were 30 min, 3 times/week for 6 weeks | |
| Outcomes | Outcomes assessed post intervention Fugl‐Meyer assessment UE Stroke Upper Limb Capacity Scale (SULCS) Visual Analogue Scale for arm pain | |
| Notes | NTR2539 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Low risk | Concealed envelopes |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded assessor |
| Incomplete outcome data (attrition bias) | Low risk | Only 2 withdrawals and both withdrew due to inadvertent concurrent treatment |
| Selective reporting (reporting bias) | Low risk | Outcomes reported as per trial registration |
| Methods | RCT | |
| Participants | Recruited from a community rehabilitation hospital in Singapore 19 participants: 10 intervention, 9 control Inclusion criteria: recent first stroke with moderate or moderate‐severe disability (Modified Rankin Scale Grade 3 or 4) Participants were haemodynamically stable and had a MMSE score of > 23 Exclusion criteria: terminal illness, uncontrolled hypertension and angina and severe spatial neglect or visual impairments Mean (SD) age: intervention group 58.67 (8.62) years, control group 65.33 (9.59) years 37% men Stroke details: 42% right hemiparesis Timing post stroke: intervention group mean (SD) 14.7 (7.5) d, control group 15.2 (6.3) d | |
| Interventions | VR intervention: used either a Nintendo Wii Fit or Microsoft Kinect program during rehabilitation. The Nintendo Wii Fit was performed in standing and the Kinect was performed in sitting and standing. Sessions involved 40 min of conventional therapy and 20 min of VR Control intervention: conventional therapy (not described). Sessions involved 60 min of conventional therapy Sessions were 60 min for 15 sessions (approximately 15 h) | |
| Outcomes | Outcomes recorded at baseline and post‐intervention Gait outcomes: Timed Up and Go Test Balance function: Berg Balance Scale, Functional Reach Test, centre of pressure | |
| Notes | Activity limitation outcomes: Modified Barthel Index | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Low risk | Blind |
| Incomplete outcome data (attrition bias) | Unclear risk | Unable to ascertain |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Methods | RCT | |
| Participants | Recruited from local hospitals and stroke support groups in Orange County, California 26 participants: 13 intervention, 13 control Inclusion criteria: single stroke and ≥ 3 months post stroke; moderate‐severe weakness in their affected upper limbs, defined by the upper limb Fugl Meyer Motor Scale (score of 10‐35/66) Exclusion criteria: significant pain, instability or subluxation of the affected shoulder, severe elbow or wrist contractures, concurrent severe medical problems, cognitive dysfunction to the extent that would interfere with therapy participation, visual deficits, severe neglect or apraxia and current enrolment in ongoing upper limb therapy Mean (SD) age: intervention group 60 (10) years, control group 61 (13) years Stroke details: 50% ischaemic, 31% haemorrhagic, 19% unknown Timing post stroke: intervention group mean (SD) 65 (47) months, control group 67 (56) months | |
| Interventions | VR intervention: Pneu‐WREX is a robotic device (4‐degree‐of‐freedom robot based on a passive arm support (WREX)). It is a lightweight exoskeleton that allows a wide ROM of the arm in a 3D space. The degrees of freedom are elbow flexion/extension, shoulder abduction/adduction, shoulder flexion/extension and shoulder forward/backward translation.The device can provide assistance as needed for a patient to actively participate and to be able to perform 3D tasks. Hand training through grasp and release is incorporated through a grip sensor that measures the pressure of a water‐filled cylinder bladder that the user holds, to detect even trace finger movement. A software package called Vu Therapy allowed for interface between the hardware and software. Tasks included grocery shopping, cleaning a window, playing basketball and driving a car. Auditory and visual feedback and a game score were provided to maintain attention and interest Control intervention: conventional exercises including ROM and task‐oriented movements Sessions were 60 min, 3 times/week for 8‐9 weeks (total = 24) for both groups | |
| Outcomes | Outcomes assessed post intervention and 3 months following the end of intervention Arm Motor section of the Fugl Meyer Scale Rancho Functional Test for the hemiplegic UE Motor Activity Log Box and Blocks Test Grip strength (Jamar) Adverse events reported | |
| Notes | Disclosure reported that the lead author has a financial interest in Hocoma, a company that makes robotic therapy devices | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Unclear risk | Method not described |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded assessor |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported in detail |
| Selective reporting (reporting bias) | Unclear risk | Unable to ascertain (does not mention protocol or trial registration) |
| Methods | RCT | |
| Participants | Recruited from a subacute rehabilitation facility in Toronto, Canada 22 participants: 11 intervention, 11 control Inclusion criteria: 18‐85 years with first time ischaemic or haemorrhagic stroke within the last 6 months, Chedoke McMaster scale (UE) score of > 3 in the arm or hand Exclusion criteria: unable to follow instructions, pre‐stroke Modified Rankin Score of ≥ 2, medically unstable or with uncontrolled hypertension, severe illness with life expectancy of < 3 months, unstable angina, recent MI (within 3 months), history of seizures or epilepsy, participating in another clinical trial involving an investigational drug or physical therapy, any condition that might put the patient at risk (for example, known shoulder subluxation) Mean age: intervention group 55 years, control group 67 years 64% men Stroke details: 45% right hemiparesis Timing post stroke: intervention group mean (SD) 27 (16) d, control group 23 (9) d | |
| Interventions | VR intervention: participants used the Nintendo Wii gaming console playing 'Wii sports' and 'Cooking Mama' Control intervention: leisure activities including cards, bingo and Jenga Sessions were 60 min for 8 sessions (8 h total) | |
| Outcomes | Outcomes recorded at baseline, post intervention and at 1 month Upper limb function and activity outcomes (arm): abbreviated version of the Wolf Motor Function Test Upper limb function and activity outcomes (hand): Box and Block test, Grip strength (kg) Participation restriction and quality of life: Stroke Impact Scale (hand function, composite function, perception of recovery) Adverse events reported Other outcomes: therapy time | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly allocated using a basic computer random number generator |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) | Low risk | Blind |
| Incomplete outcome data (attrition bias) | Low risk | Some attrition was reported. Outcomes were calculated based on the number of participants and there was no reporting of imputation of data. ITT analysis was completed |
| Selective reporting (reporting bias) | Low risk | Reports on all measures reported in the study protocol paper |
| Methods | RCT | |
| Participants | Recruited from rehabilitation units in 4 countries: Canada, Argentina, Peru, Thailand 141 participants: 71 intervention group, 70 control group Inclusion criteria: 18‐85 years with first time ischaemic stroke within 3 months of enrolment and with mild to moderate motor disability (Chedoke McMaster Stroke Assessment stage > 3) Exclusion criteria: no disability in the UE (arm components of the Chedoke McMaster scale = 7), were unable to follow instructions, pre‐stroke Modified Rankin score of ≥ 2, medically unstable or uncontrolled hypertension; severe illness with a life expectancy of < 3 months, unstable angina or MI within 3 months, history of seizures or epilepsy (except for febrile seizures of childhood); participating in another clinical trial involving an investigational drug or physical therapy or had any condition that might put the patient at risk (e.g. known shoulder subluxation) Mean (SD) age: intervention group 62 (13) years, control group 62 (12) years Stroke details: 100% ischaemic; right hemiparesis 47% Timing post stroke: intervention group mean 27 d, control group mean 24.5 d | |
| Interventions | VR intervention: Nintendo Wii Sports and Game Party 3. Progression through the intervention allowed participants to choose some specific activities within those games (last 3 min of the intervention) based on their capabilities and interest with the goals of enhancing flexibility, ROM, strength and co‐ordination of the affected arm Control intervention: recreational therapy with progression through activities such as cards, bingo, Jenga or a ball game Administered 1:1 by a rehabilitation therapist Sessions were 60 min, 5 times/week for 2 weeks | |
| Outcomes | Outcomes were recorded at 2 weeks (post intervention) and 4 weeks Abbreviated Wolf Motor Function Test Box and Block Test Quality of life after stroke ‐ Stroke Impact Scale Functional Independence Measure, Barthel Index, Modified Rankin Scale Grip strength (dynamometer) Hand function ‐ Stroke Impact Scale Adverse events reported | |
| Notes | NCT01406912 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated assignment |
| Allocation concealment (selection bias) | Low risk | Assignment at the point enrolment |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded assessor |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis conducted. Details of withdrawals reported transparently |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Methods | RCT | |
| Participants | Recruited from 2 rehabilitation units and the neurorehabilitation ward of a hospital in Korea 16 participants: 9 intervention, 7 control Inclusion criteria: hemiparetic upper limb dysfunction due to first‐ever stroke, mild‐to‐severe deficits of the paretic UE (2‐4 on the MRC Scale and 2‐5 on the Brunnstrom Stage of motor recovery) Exclusion criteria: pre‐existing arm impairment, any painful condition affecting the upper limbs, difficulty in sitting for ≥ 20 min, severe cognitive impairment (MMSE score < 10 points) and severe aphasia Mean (SD) age: intervention group 46.6 (5.8) years, control group 52.0 (11.9) years 50% men Stroke details: 38% right lesion Timing post stroke: intervention group mean (SD) 76.6 (28.5) d, control group 67.1 (45.3) d | |
| Interventions | VR intervention: RehabMaster™. The participant sits in a chair in front of a monitor. The therapist can control the program and level of difficulty. Rehabilitation games were designed to combine rehabilitation exercises with gaming elements. The 4 games suggested were goalkeeper, bug hunter, underwater fire and rollercoaster Control intervention: conventional OT Sessions were 20 min of OT. The intervention group received an additional 20 min of VR. The duration of intervention was 10 sessions over 2 weeks | |
| Outcomes | Outcomes recorded at baseline and post intervention Upper limb function outcomes: Fugl Meyer Activity limitation outcomes; Modified Barthel Index Other outcomes: passive ROM of the upper limb, MRC Score | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded to allocation |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All outcomes reported except for the SF36 measure, which will be reported in a subsequent publication |
| Methods | RCT | |
| Participants | Recruited from a rehabilitation hospital in Seoul, Korea 35 participants: 18 intervention, 17 control Inclusion criteria: aged ≥ 18 years with chronic hemiparetic upper limb dysfunction, secondary to a first ever stroke. MRC Scale scores of 2‐4 (inclusive) and a Brunnstrom motor recovery stage for the proximal UE of 2‐5 inclusive Exclusion criteria: severe cognitive impairment or aphasia, pre‐existing mental illness or arm impairment, difficulty in sitting for ≥ 30 min and/or uncontrolled medical illness Mean (SD) age: intervention group 53.3 (11.8) years, control group 54.6 (13.4) years 69% men Stroke details: 50% right hemiparesis Timing post stroke: intervention group mean (SD) 202 (89), control group 165 (87) d | |
| Interventions | VR intervention: game‐based VR using 10 min of rehabilitation training and 20 min of rehabilitation games selected by an occupational therapist to encourage active arm and trunk movements. Participants sat in a chair in front of the monitor and depth sensor and moved according to the training protocol. The difficulty was set by manipulating the ROM or speed of the activity or by manipulating the number, size, location, speed or trajectories of the targets Control intervention: conventional OT including exercises, table top activities and training for ADL Sessions for the VR group were 30 min of VR plus 30 min of conventional OT, 5 d/ week for 4 weeks Sessions for the control group were 60 min of OT, 5 d/week for 4 weeks | |
| Outcomes | Outcomes assessed post intervention Korean SF36 Korean Hamilton Depression Rating Scale Fugl Meyer Assessment UE Adverse events reported | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded outcome assessor |
| Incomplete outcome data (attrition bias) | Low risk | Minor loss to follow‐up. Method of dealing with this in the analysis is not reported |
| Selective reporting (reporting bias) | Unclear risk | No mention of protocol or trial registration |
| Methods | RCT | |
| Participants | Recruited from a rehabilitation hospital in Korea 35 participants: 18 intervention, 17 control Inclusion criteria: > 6 months post stroke, no problems with auditory or visual functioning, active ROM of the shoulder, elbow, wrist and fingers of > 10°, ability to walk > 10 m independently not taking any medication that could influence balance or gait and no severe cognitive disorders (MMSE score of > 16/30) Exclusion criteria: uncontrolled blood pressure or angina, history of seizure, any intervention other than conventional therapy, or refusal to use a video game Mean (SD) age: intervention group 71.78 (9.42) years, control group 75.59 (5.55) years 43% men Stroke details: 66% right hemiparesis Timing post stroke: intervention group mean (SD) 7.22 (1.21) months, control group 8.47 (2.98) months | |
| Interventions | VR intervention: use of Xbox Kinect for 30 min followed by conventional OT for 30 min. Kinect programs that required use of the UEs were selected Control intervention: conventional OT, which focused on retraining UE and hand function and ADL | |
| Outcomes | Outcomes recorded at baseline and post‐intervention Upper limb outcomes: Fugl Meyer UE, Box and Block test Other outcomes: UE Active ROM | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded to allocation |
| Incomplete outcome data (attrition bias) | Unclear risk | To be determined |
| Selective reporting (reporting bias) | Unclear risk | To be determined |
| Methods | RCT | |
| Participants | Recruited from a hospital in South Korea 40 participants: 20 intervention group, 20 control group Inclusion criteria: no visual field deficit, no abnormality in the vestibular organs, no orthopaedic disease, an unrestricted ROM, able to understand and perform the exercise as instructed by the researcher and a score of ≥ 24 on the MMSE‐K Exclusion criteria: none reported Mean (SD) age: intervention group mean (SD) 51.37 (40.6) years, control group 50.10 (7.83) years 55% men Stroke details: 48% right hemiparesis Timing post stroke: intervention group 14.75 (6.06) months, 14.30 (3.40) months | |
| Interventions | VR intervention: Xbox Kinect including Kinect Sport, Kinect Sport Season 2, Kinect Adventure, Kinect Gunstringer. Mostly sports programs such as bowling, skiing, golf, ground walking, walking over obstacles and climbing stairs were used for training Control intervention: ergometer bicycle training using a Motomed Viva 2. The Motomed provides detailed feedback, software‐controlled therapy programs and motivation and training games Sessions for both interventions were 30 min, 5 d/week for 8 weeks | |
| Outcomes | Outcomes assessed post intervention Balance (biofeedback analysis system) Timed Up and Go Test 10 Minute Walk Test | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Detail not reported |
| Allocation concealment (selection bias) | Unclear risk | Detail not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Detail not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Detail not reported |
| Selective reporting (reporting bias) | Unclear risk | No mention of protocol or trial registration |
| Methods | RCT | |
| Participants | Study took place in the UK 27 participants: 17 intervention, 10 control Inclusion criteria: ≥ 18 years, no longer receiving any other intensive rehabilitation and still had residual upper limb dysfunction Exclusion criteria: failure to meet above criteria Mean (SD) age: intervention group 59 (12.03) years, control group 63 (14.6) years 59% men Timing post stroke: intervention group mean (SD) 38 (41.28) weeks, control group 24 (36.26) weeks | |
| Interventions | VR intervention: virtual glove which translates the position of the hand into gameplay. Participants were instructed to use the program at home Control intervention: usual care (no specific intervention) Sessions were 20 min, 3 times/d for 8 weeks (approximately 52 h) | |
| Outcomes | Outcomes recorded at baseline, 4 weeks and post intervention (8 weeks) Upper limb function outcome: Wolf Motor Function Test, Nine Hole Peg Test Other: Motor Activity Log Activity outcomes: Nottingham Extended ADL Scale (NEADL) | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random number generator |
| Allocation concealment (selection bias) | Low risk | Managed externally |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded to allocation |
| Incomplete outcome data (attrition bias) | High risk | Large number of dropouts in the intervention group |
| Selective reporting (reporting bias) | Low risk | Unpublished data obtained via personal communication |
| Methods | RCT | |
| Participants | Study took place in Canada 32 participants: 16 intervention, 16 control Inclusion criteria: aged 40‐80 years, sustained single ischaemic or haemorrhagic stroke 6‐60 months previously, scored 3‐6 on the Chedoke McMaster Stroke Assessment arm subscale and had no other neurologic or neuromuscular/orthopaedic problems affecting the upper limb and trunk Exclusion criteria: brainstem or cerebellar lesions, comprehension difficulties and marked apraxia, attention or visual field deficits Mean (SD) age: intervention group 62 (9.7) years, control group 60 (11) years 72% men Stroke details: 47% right hemiparesis Timing post stroke: intervention group mean (SD) 3.7 (2.2) years, control group 3.0 (1.9) years | |
| Interventions | VR intervention: a 3D virtual environment (CAREN system) simulated a supermarket scene. Participants had to reach for objects in the virtual environment. Training was high in intensity with 72 trials of reaching in each session Control intervention: pointing at targets in a physical environment Sessions were 45 min for 12 d spaced over 4 weeks | |
| Outcomes | Outcomes were recorded at baseline, post intervention and 3 months following intervention Upper limb outcomes: Fugl Meyer, Reaching Performance Scale for Stroke, Wolf Motor Function Test Adverse events reported Other outcomes: Motor Activity Log‐AS Other outcomes: Motivation Task Evaluation Questionnaire Other outcomes: kinematic data | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Managed by external personnel |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded to allocation |
| Incomplete outcome data (attrition bias) | Low risk | All completed the assessments. Small number of intervention dropouts and balanced across groups |
| Selective reporting (reporting bias) | Low risk | All outcomes reported as per entry on clinical trial registry |
| Methods | Quasi RCT | |
| Participants | Recruited from the National Institute of Neurology in Mexico City, Mexico 22 participants: 11 intervention, 11 control Inclusion criteria: ≥ 6 months after stroke Exclusion criteria: none reported Mean age: intervention group 51 years, control group 52 years Timing post stroke: intervention group 22 months, control group 26 months | |
| Interventions | VR intervention: participants used a 'Gesture Therapy' program designed by the researchers. Movements of the participant's upper limbs are tracked by a camera and the person interacts with on‐screen games. Games included shopping in the supermarket, making breakfast, playing basketball, cleaning, painting and driving Control intervention: a variety of exercises guided by the therapist using equipment such as cones and balls Sessions were 60 min, 3 times/week for 5 weeks (15 h total) | |
| Outcomes | Outcomes recorded at baseline and post intervention Upper limb function and activity outcomes (arm): Fugl Meyer UE scale, Motricity Index Adverse events reported Other outcomes: level of interest, competence, effort, pressure and utility of the intervention | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate allocation based on odd or even numbers |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) | High risk | Not blinded |
| Incomplete outcome data (attrition bias) | Low risk | There were no missing data |
| Selective reporting (reporting bias) | Low risk | No additional outcomes were collected |
| Methods | RCT | |
| Participants | Recruited from an outpatient clinic in the USA 14 participants: 7 intervention, 7 control Inclusion criteria: chronic hemiparesis resulting from a single stroke ≥ 6 months prior with mild‐moderate hand impairment as evidenced by a score of 5 or 6 on the Hand subsection of the Chedoke McMaster Stroke Assessment scale. Limitations with fine motor control but able to perform 2 of 3 specified hand movements Exclusion criteria: receiving outpatient physical or OT, biomechanical limitations which limited passive digit extension to 20° of finger flexion; had received botulinum toxin < 6 months prior to enrolment; cognitive deficits limiting simple 1‐step commands or significant UE pain Mean (SD) age: intervention group 54 (7) years, control group 59 (6) years Stroke details: right hemiparesis 43% Timing post stroke: intervention group 46.6 (32.5) months, control group 47.9 (47.4) months | |
| Interventions | VR intervention: trained with the actuated virtual keyboard (AVK) system to practice movements of different combinations. Participants wore a PneuGlove and pressed virtual keys. Visual displays guided the user as did the therapist. Each key played a unique tone which would play whenever the key was struck Control intervention: high‐intensity task‐oriented OT centred on fine motor control, dexterity, in‐hand manipulation and isolated finger movements. Examples of activities included practise of buttoning, typing, tying knots, writing and using tools Both group had sessions of 60 min, 3 times a week for 6 weeks | |
| Outcomes | Outcomes assessed post intervention and 1 month after the end of intervention Action Research Arm Test Jebsen Taylor Hand Function Test Fugl Meyer (UE) Grip strength (Jamar dynamometer) Other: Kinematic actuation | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Drawing lots |
| Allocation concealment (selection bias) | Low risk | Drawing lots |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded therapist |
| Incomplete outcome data (attrition bias) | Low risk | Minimal dropout |
| Selective reporting (reporting bias) | Unclear risk | No mention of protocol or trial registration |
| Methods | RCT | |
| Participants | Recruited from an outpatient unit in Turkey 22 participants: 11 intervention, 11 control Inclusion criteria: adult male (> 18 years), capability to ambulate 10 m without personal assistance and not receiving any other physical therapy Exclusion criteria: body weight > 135 kg, FAC score < 3; unable to walk consistently or independently within the community, cognitive deficits, cardiac disease, spasticity of the lower limbs preventing them from robotic walking, traumatic stroke, intracranial space occupying lesion‐induced strokes and seizures Mean age: intervention group 56.2 years, control group 61.5 years 100% men Stroke details not reported | |
| Interventions | VR intervention: robotic (Lokomat) training with a computer monitor placed in front of the participants. It provided them with biofeedback of their performance Control intervention: conventional physiotherapy in the home environment. Home exercise focused on gait and body weight support on the paretic leg. Also included active assisted exercises, leg strengthening and balance training Both groups received 30‐min sessions, 5 d/week for 2 weeks | |
| Outcomes | Outcomes assessed post intervention 10 m Timed Walking Speed Test Timed Up and Go Test MMSE Hospital Anxiety and Depression Scale Functional Ambulation Category | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Detail not reported |
| Allocation concealment (selection bias) | Unclear risk | Detail not reported |
| Blinding of outcome assessment (detection bias) | High risk | Assessor not blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | Detail not reported in enough detail to make a judgement |
| Selective reporting (reporting bias) | Unclear risk | No mention of protocol or trial registration |
| Methods | RCT | |
| Participants | Recruited from a hospital in China 20 participants: 10 intervention, 10 control Inclusion criteria: aged 40‐80 years within 3 months of first onset of stroke. Abnormal 10 m walking time but could walk > 10 m with no more than the assistance of 1 person Exclusion criteria: cerebellum/brainstem infarct; impairment in all 4 limbs, reduced consciousness, respiratory or heart failure, Parkinson's Disease, recent MI, recent leg fracture, recent deep vein thrombosis, recent stroke with gait disorder Mean (SD) age: intervention group 57.1 (10.43) years, control group 62.2 (10.21) years 70% men Stroke details: 45% right hemiparesis Timing post stroke: intervention group mean (SD) 44.4 (14.78) d, control group 40.80 (16.52) d | |
| Interventions | VR intervention: VR enhanced body weight supported treadmill training Control intervention: muscle strength training, stretching and balance exercises Both groups participated in 15 sessions of conventional therapy; the VR intervention group received an additional 20‐40 min of training at each session | |
| Outcomes | Outcomes assessed post intervention 10 m walking speed Fugl Meyer (LE) Brunel Balance Assessment | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Detail not reported |
| Allocation concealment (selection bias) | Unclear risk | Detail not reported |
| Blinding of outcome assessment (detection bias) | High risk | Assessor not blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported in sufficient detail to make judgement |
| Selective reporting (reporting bias) | Unclear risk | Unable to find protocol or trial registration |
| Methods | RCT | |
| Participants | Study took place in Taiwan 24 participants: 12 intervention, 12 control Inclusion criteria: hemiparesis resulting from a single stroke occurring > 6 months earlier, limited household walker, unlimited household walker or most‐limited community walker by functional walking category, not presently receiving any rehabilitation services, no visual field deficit or hemianopia, stable medical condition to allow participation in the testing protocol and intervention, ability to understand instructions and follow commands Exclusion criteria: any comorbidity or disability other than stroke that would preclude gait training, uncontrolled health condition for which exercise was contraindicated, neurological or orthopaedic disease that might interfere with the study Mean (SD) age: intervention group 55 (12) years, control group 61 (9) years 50% men Stroke details: 45% right hemiparesis Timing post stroke: intervention group mean (SD) 6 (4) years, control group 6 (10) years | |
| Interventions | VR intervention: the participant walked on a treadmill as virtual environments were displayed on a screen in front of the person with a wide field of view. Speed and incline of the treadmill was able to be varied in conjunction with scenery changes. Leg movements were tracked by an electromagnetic system to detect collisions with virtual objects. The virtual environment was designed to simulate a typical community in Taipei. Scenarios consisted of lane walking, street crossing, negotiating obstacles and strolling through the park Control intervention: treadmill training. While walking on the treadmill the participant was asked to execute different tasks. The tasks included lifting the legs to simulate stepping over obstacles, uphill and downhill walking and fast walking Sessions were 20 min, 3 times/week for 3 weeks (3 h total) | |
| Outcomes | Outcomes recorded at baseline, post intervention and at 1 month Lower limb function and activity outcomes: walking speed (m/s), community walk test Participation restriction and quality of life: walking ability questionnaire, Activities Specific Balance Confidence Scale | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An independent person picked 1 of the sealed envelopes before the start of the intervention |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether envelopes were opaque |
| Blinding of outcome assessment (detection bias) | Low risk | Blind |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Methods | RCT | |
| Participants | Recruited from a hospital in Taiwan 14 participants: 7 intervention, 7 control Inclusion criteria: hemiplegia resulting from a stroke > 6 months ago. Able to understand the treadmill exercises Exclusion criteria: inability to walk independently (without using an assistive device), abnormal neuro‐opthalmologic findings after examination and visual acuity problems after correction Mean (SD) age: intervention group 56.3 (10.2) years, control group 65.7 (5.9) years Stroke details: 36% right hemiparesis Timing post stroke: intervention group mean (SD) 17 (8.6) months, control group 16.3 (10.4) months | |
| Interventions | VR intervention: standard OT and physiotherapy program plus VR treadmill training. The treadmill was co‐ordinated with the interactive scenes so that a stepping switch turned the scenes left or right as if the person was turning a corner. Participants had to make 16 turns/session Control intervention: treadmill training facing a window Sessions were 20 min, 3 times/week for 3 weeks (approximately 3 h total) | |
| Outcomes | Outcomes recorded at baseline and post‐intervention Gait outcomes: bilateral limb loading symmetric index, paretic limb stance time, number of steps of the paretic limb, contact areas of the paretic foot during quiet stance, sit‐to‐stand transfer and level walking Balance outcomes: centre of pressure | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded to allocation |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient detail reported to tell |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available |
| Methods | RCT | |
| Participants | Recruited from an inpatient rehabilitation centre in Turkey 20 participants: 10 intervention, 10 control Inclusion criteria: first episode of unilateral stroke with hemiparesis during the previous 12 months, score of 1‐4 on the Brunnstrom stages for the UE, able to understand and follow simple verbal instructions, no severe cognitive disorders that would interfere with the study's purpose (MMSE score of > 16/30) Mean (SD) age: intervention group 58 (10) years, control group 64 (11) years 45% men Stroke details: 45% right hemiparesis Timing post stroke: intervention group mean (SD) 3 (3) months, control group 5 (1) months | |
| Interventions | VR intervention: active use of the Playstation EyeToy games involving use of the upper limbs Control intervention: watched the Playstation EyeToy games but did not get physically involved Sessions were 30 min, 5 times/week for 4 weeks (10 h total) | |
| Outcomes | Outcomes recorded at baseline and post‐intervention Upper limb function and activity outcome measures (arm function): Brunnstrom UE stages Upper limb function and activity outcome measures (hand function): Brunnstrom hand stages Activity limitation outcome measures: Functional Independence Measure self care component Adverse events reported | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generated using a computer‐generated random number list |
| Allocation concealment (selection bias) | Low risk | An independent doctor operated the random number program |
| Blinding of outcome assessment (detection bias) | Low risk | Blind |
| Incomplete outcome data (attrition bias) | Low risk | There does not appear to be any attrition and all outcome measures appear to have been reported in full |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Methods | RCT | |
| Participants | Recruited from an inpatient rehabilitation unit in Singapore 23 participants: 11 intervention, 12 control Inclusion criteria: medically stable to participate in active rehabilitation, > 21 years old, able to stand unsupported for 30 s, Fugl Meyer Assessment for the UE score of < 62 and MMSE score of > 20 Exclusion criteria: epilepsy, photophobia or known side effects from watching digital media, were pregnant, had implanted electronic devices including pacemakers or defibrillators, joint pain that could limit participation, severe visual deficits and presented with a spasticity score of > 2 in the affected limb quantified by the Modified Ashworth Scale Median age: intervention group 62 years, control group 56 years 70% men Stroke details: 35% right hemiparesis Timing post stroke: intervention group median 15 d, control group median 14 d | |
| Interventions | VR intervention: the VR system comprised a hand‐held remote controller detected with a base movement sensor, laptop computer, customised rehabilitation gaming software and a 80 centimetre, liquid crystal display screen. The tasks were highly repetitive but functional tasks in an enriched motivating environment, with customisable but challenging difficulty levels.The virtual environment consisted of a local supermarket setting to increase familiarity and engagement of participants. Participants were instructed to pick a virtual fruit from a shelf and release it into a virtual basket as many times as possible within a 2‐min trial. This reaching practice was carried out standing, simulating real‐life Control intervention: conventional rehabilitation training The experimental group received 30 min of non‐immersive VR training for 9 weekdays within 2 weeks (5 d/week) in addition to conventional therapy. The control group received only conventional therapy. The total dose provided was comparable (17 h intervention vs 15.5 h control) | |
| Outcomes | Outcomes assessed post intervention and at 4 weeks Fugl Meyer Assessment Action Research Arm Test Motor Activity Log Functional Independence Measure Adverse events reproted | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not clear |
| Allocation concealment (selection bias) | Unclear risk | Allocation was concealed using opaque envelopes. Not clear if sealed |
| Blinding of outcome assessment (detection bias) | High risk | Not blinded |
| Incomplete outcome data (attrition bias) | Low risk | Minimal dropout |
| Selective reporting (reporting bias) | Unclear risk | No mention of protocol |
| Methods | RCT | |
| Participants | Study took place in Korea 10 participants: 5 intervention, 5 control Inclusion criteria: ≥ 1 year after first stroke, plateau in the maximum motor recovery after conventional neurorehabilitation, > 60° extension at the knee Exclusion criteria: severe spasticity (modified Ashworth scale > 2) or tremor, severe visual and cognitive impairment Mean age: intervention group 55 years, control group 55 years 70% men Stroke details: 30% right hemiparesis Timing post stroke: intervention group 18 months, control group 19 months | |
| Interventions | VR intervention: IREX VR system using a video capture system to capture the participant's whole body movement. The participant is able to view their body movements in real time on a screen in front of them immersed in a virtual environment. Games included stepping up/down, 'shark bait' and snowboarding Control intervention: no intervention provided Sessions for the VR group were 60 min, 5 times/week for 4 weeks (20 h total) | |
| Outcomes | Outcomes recorded at baseline and post intervention Lower limb function and activity outcomes: Functional Ambulation Category Global motor function: modified Motor Assessment Scale Imaging studies: functional MRI ‐ laterality index | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) | Low risk | Blind |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Methods | RCT (3 arms) | |
| Participants | Recruited from a neurorehabilitation ward in Italy 33 participants: 11 intervention, 11 control, 11 control Inclusion criteria: stroke in the MCA territory ≥ 6 months before enrolment, absence of ideomotor apraxia, neglect and aphasia interfering with verbal comprehension Exclusion criteria: apraxia, neglect and language disturbances Median (IQR) age: intervention group 60 (57.25‐76) years, control group 60 (49‐74.25) years, control group 64.5 (54.50‐69) years 39% men Timing post stroke: intervention group median (IQR) 10.05 (4.05‐17.90) months, control group 8.75 (2.75‐24.95) months, control group 5.05 (1.75‐17.90) months | |
| Interventions | VR intervention (Ever teacher group): Reinforced Feedback in Virtual Environment (RFVE). Participants were asked to manipulate sensorised objects (ball, plastic cup or cylinder). Specific feedback was provided (like a virtual teacher) to encourage the participant to emulate the correct movement VR intervention (No teacher group): VR intervention but with no feedback Control intervention: conventional rehabilitation programme Sessions were 60 min, 5 times/week for 4 weeks | |
| Outcomes | Outcomes recorded at baseline and post intervention Upper limb outcomes: Fugl Meyer UE, Reaching performance scale Other outcomes: Modified Ashworth Scale, kinematics Activity outcomes: Functional Independence Measure | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque, sealed envelopes |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded to allocation |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | No other outcomes collected |
6MWT: 6‐minute walk test
ADL: activities of daily living
CT: computerised tomography
ITT: intention‐to‐treat
IQR: interquartile range
MCA: middle cerebral artery
MI: myocardial infarction
MMSE(‐K): Mini Mental State Examination( ‐ Korean)
MRC: Medical Research Council
MRI: magnetic resonance imaging
OT: occupational therapy
RCT: randomised controlled trial
ROM: range of motion
SD: standard deviation
UE: upper extremity
VR: virtual reality
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Cross‐over design | |
| Both the intervention and control group receive VR | |
| Did not meet the definition of VR intervention | |
| Study design: not a RCT | |
| Compares different types of VR | |
| Did not meet the definition of VR (no real 'interaction' between the person and the virtual environment) | |
| Both intervention and control group received VR | |
| Study design: not a RCT | |
| Study design: not a RCT | |
| Study design: not a RCT | |
| Study design: not a RCT | |
| Compares different types of VR | |
| Not considered to be properly randomised or quasi‐randomised | |
| Did not meet the definition of a VR intervention | |
| Cross‐over design | |
| Did not meet the definition of a VR intervention | |
| Study design: not all participants were randomised | |
| Did not meet the definition of a VR intervention | |
| It did not appear that the participant had control over the interaction with the virtual environment. We emailed the study authors to clarify this but there was no response | |
| Not clear that the VR is synced with real interaction between the person and the system | |
| Study design: participants were not randomly allocated to groups | |
| Compared assymetric training with symmetric training. Both groups had VR | |
| Outlines two studies: both included participants with acquired brain injury and did not report the results for different diagnoses separately | |
| Not considered VR intervention matching the definition in this review | |
| Compares groups VR in standing with VR in sitting | |
| Secondary analysis of a subgroup of participants from a larger study | |
| Cross‐over design | |
| Study design: participants were not randomly allocated to groups | |
| Unable to obtain further information to confirm inclusion criteria or obtain basic study data | |
| Not randomised | |
| Examines VR with or without transcranial direct current stimulation | |
| Did not meet definition of VR used in this review | |
| There is not genuine interaction between the participant and the virtual environment | |
| Not VR intervention |
RCT: randomised controlled trial
VR: virtual reality
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | RCT |
| Participants | People post stroke |
| Interventions | Physical therapy associated with VR therapy |
| Outcomes | Berg Balance Scale |
| Notes | Conference abstract. Appears to be preliminary results for an ongoing trial. Study authors did not respond to queries regarding study |
| Methods | RCT |
| Participants | People with stroke ≥ 6 months earlier |
| Interventions | Intervention group: 18 individualised training sessions using the YouGrabber over 12 weeks Control group: usual rehabilitation within the gym |
| Outcomes | Interviews, other outcome measures not described |
| Notes |
| Methods | RCT |
| Participants | People in the chronic phase post stroke |
| Interventions | Nintendo Wii Fit |
| Outcomes | Fugl Meyer‐Lower Extremity, QOL |
| Notes | Conference paper. States preliminary results. Study authors did not respond to queries regarding study |
| Methods | RCT |
| Participants | Individuals within 6 months of stroke |
| Interventions | VR: VR motor‐cognitive task group performed a VR motor and cognitive attention/memory task customised to each user in terms of the positive content Control: standard rehabilitation group performed conventional motor and cognitive rehabilitation tasks |
| Outcomes | Primary outcome: Fugl Meyer |
| Notes | NCT02539914. Co‐investigator AL Faria |
| Methods | RCT |
| Participants | People in the chronic phase post stroke |
| Interventions | VR: VR reflection therapy in addition to usual rehabilitation Control group: conventional rehabilitation and placebo VR |
| Outcomes | Berg Balance Scale, Functional Reach test, Timed Up and Go Test |
| Notes |
| Methods | RCT |
| Participants | People with stroke |
| Interventions | Treadmill training‐based, real‐walk simulation |
| Outcomes | Motor‐Free Visual Perception Test, Berg Balance Scale |
| Notes | Conference abstract only and unable to source further study details |
| Methods | RCT |
| Participants | People in the chronic phase of stroke |
| Interventions | VR‐based rehabilitation group Group‐based rehabilitation group |
| Outcomes | Fugl Meyer‐Upper Extremity, manual function test, Box and Block Test, Modified Barthel Index, SF‐12 |
| Notes | ISRCTN04144761 |
| Methods | RCT |
| Participants | People following stroke |
| Interventions | VR group received additional 30 min of therapy utilising canoe‐based game Control group received conventional rehabilitation program |
| Outcomes | Trunk postural stability, balance and upper limb motor function |
| Notes |
| Methods | RCT |
| Participants | People in the chronic phase post stroke |
| Interventions | Computer‐aided interlimb force coupling training task with visual feedback |
| Outcomes | Barthel Index, Fugl Meyer Assessment, Motor Assessment Score, Wolf Motor Function Test |
| Notes | Contacted authors to clarify details of intervention and whether this met our criteria for inclusion but received no response |
| Methods | Quasi RCT |
| Participants | People after stroke with aphasia |
| Interventions | Intervention: daily language stimulation sessions in 'EVA Park' with a support worker Control group: waitlist control group |
| Outcomes | Communication ADL, Verbal fluency task, Word finding in conversation (POWERS), narrative production, Communication Confidence Rating Scale for Aphasia, Friendship Scale |
| Notes |
| Methods | RCT |
| Participants | People in the chronic phase following stroke |
| Interventions | Intervention: self‐administered, home‐based arm and hand training using either a passive or dynamic wrist and hand orthosis combined with computerised gaming exercises Control: prescribed conventional exercises from a book |
| Outcomes | Action Research Arm Test, Intrinsic Motivation Inventory, Fugl Meyer Assessment, Motor Activity Log, Stroke Impact Scale, grip strength |
| Notes |
| Methods | RCT |
| Participants | Adults following stroke |
| Interventions | Intervention: Nintendo Wii for upper limb and balance Control: Bobath NDT |
| Outcomes | Functional Independence Measure, Nottingham Health Profile |
| Notes |
| Methods | RCT |
| Participants | People following stroke |
| Interventions | Additional therapy using the Xbox Kinect Control group received usual therapy |
| Outcomes | Feasibility and safety (treatment attendance, patient feedback, adverse events, Borg Scale) |
| Notes |
| Methods | RCT |
| Participants | People with chronic stroke |
| Interventions | Participants were allocated to 3 weeks of home‐based MusicGlove therapy or conventional tabletop exercises |
| Outcomes | Primary outcome: Box and Blocks test |
| Notes |
NDT: neurodevelopmental treatment
OT: occupational therapy
QOL: quality of life
RCT: randomised controlled trial
VR: virtual reality
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | 'FIND Technology': investigating the feasibility, efficacy and safety of controller‐free interactive digital rehabilitation technology in an inpatient stroke population: study protocol for a randomized controlled trial |
| Methods | RCT |
| Participants | Inpatient stroke population |
| Interventions | Intervention group receive Jintronix JRS Wave in addition to their individualised targeted therapy Control group receive repetitive exercises in addition to their individualised targeted therapy |
| Outcomes | Activity (measured using accelerometer), Modified Motor Assessment Scale (upper extremity component), sitting balance, standing balance, dynamic balance, mobility |
| Starting date | April 2014 |
| Contact information | Dr Marie‐Louise Bird |
| Notes | ACTRN12614000427673 |
| Trial name or title | Interactive video gaming compared with optimal standard of care to improve balance and mobility |
| Methods | Single‐blind pilot RCT |
| Participants | Individuals post stroke (> 6 months), able to walk ≥ 50 m, follow instructions |
| Interventions | VR intervention: Wii‐based balance and mobility training Control: optimal standard of care Dosing 3 h/week for 4 weeks |
| Outcomes | Gait variables (gait rite), 6‐Minute Walk Test, Dynamic Gait Index, Timed Up and Go, Activities Balance Questionnaire, Canadian Occupational Performance Measure, Postural Control |
| Starting date | Commenced Summer 2008 |
| Contact information | Professor Judith Deutsch: [email protected] |
| Notes | Data collection completed with results to be presented at upcoming conferences |
| Trial name or title | The optimal dosage of the rehabilitation gaming system: the impact of a longer period of VR‐based and standard OT on upper limb recovery in the acute phase of stroke |
| Methods | RCT |
| Participants | People after acute stroke |
| Interventions | VR intervention: rehabilitation gaming system Control: OT |
| Outcomes | Unclear |
| Starting date | Unclear |
| Contact information | Professor Armin Duff |
| Notes | — |
| Trial name or title | Dual‐task training using virtual reality: influence on walking and balance in individuals post‐stroke |
| Methods | RCT |
| Participants | > 1 year following stroke |
| Interventions | VR intervention: 'SeeMe' video capture system Control intervention: unclear |
| Outcomes | Primary outcome: gait speed |
| Starting date | Unclear |
| Contact information | Dr Ayelet Dunsky |
| Notes | — |
| Trial name or title | Using a virtual reality gaming system to supplement upper extremity rehabilitation post stroke |
| Methods | RCT |
| Participants | People following stroke with upper extremity impairment |
| Interventions | Intervention group: upper extremity VR Control group: usual care |
| Outcomes | Fugl Meyer, Box and Blocks Test, Stroke Impact Scale |
| Starting date | Unknown |
| Contact information | Professor Dahlia Kairy |
| Notes | — |
| Trial name or title | Maximizing post‐stroke upper limb rehabilitation using a novel telerehabilitation interactive virtual reality system in the patient's home: study protocol of a randomized clinical trial |
| Methods | RCT |
| Participants | People following stroke with upper extremity impairment |
| Interventions | Intervention: telerehabilitation VR (Jintronix system) |
| Outcomes | Primary outcome: Fugl Meyer |
| Starting date | Unknown |
| Contact information | Professor Dahlia Kairy |
| Notes | — |
| Trial name or title | Wii‐based rehabilitation in stroke |
| Methods | RCT |
| Participants | Individuals post stroke |
| Interventions | VR intervention: traditional balance rehabilitation plus Nintendo Wii Fit Control intervention: traditional balance rehabilitation |
| Outcomes | Berg Balance Scale, Functional Reach Test, postural assessment scale for stroke patients |
| Starting date | Unknown |
| Contact information | Professor Gülçin Kaymak Karataş: [email protected] |
| Notes | — |
| Trial name or title | Reinforced feedback in virtual environment for rehabilitation of upper extremity dysfunction after stroke: preliminary data from a randomized controlled trial |
| Methods | RCT |
| Participants | People ≥ 1 year post stroke |
| Interventions | Intervention: reinforced feedback in virtual environment Control: traditional rehabilitation |
| Outcomes | Primary outcome: Fugl Meyer‐upper extremity |
| Starting date | Unsure |
| Contact information | Dr Pawel Kiper |
| Notes | — |
| Trial name or title | Evaluation of a tele‐health system for upper extremity stroke rehabilitation |
| Methods | RCT |
| Participants | People following stroke |
| Interventions | Intervention: quasi‐home‐based tele‐motion‐rehabilitation (TMR) program using the Gertner System Control: self‐training upper extremity home exercise group |
| Outcomes | Not reported in conference abstract |
| Starting date | — |
| Contact information | |
| Notes | — |
| Trial name or title | Virtual action planning in stroke: a control rehabilitation study |
| Methods | RCT |
| Participants | Individuals with stroke |
| Interventions | VR intervention: rehabilitation using the 'Virtual Action Planning supermarket' Control intervention: conventional rehabilitation |
| Outcomes | Primary outcome: ability to perform shopping test in real supermarket |
| Starting date | May 2011 |
| Contact information | Professor Pierre‐Alain Joseph: pierre‐alain.joseph@chu‐bordeaux.fr |
| Notes | Date accessed December 2013 |
| Trial name or title | Evaluation of the effects of rehabilitation using the 'Wii' on upper limb kinematics in chronic stroke patients |
| Methods | RCT |
| Participants | Post‐stroke hemiparetic patients (≥ 6 months post stroke) |
| Interventions | VR: Nintendo Wii based therapy Control: traditional physiotherapy |
| Outcomes | Primary outcome: degree of elbow extension during an active reaching task |
| Starting date | — |
| Contact information | Dr Djamel Bensmail |
| Notes | NCT01806883 |
| Trial name or title | The development of upper extremity rehabilitation program using virtual reality for the stroke patients |
| Methods | RCT |
| Participants | Individuals with stroke |
| Interventions | VR intervention Control intervention: standard OT |
| Outcomes | Primary outcome: Fugl Meyer Upper Extremity Scale |
| Starting date | October 2013 |
| Contact information | Professor Nam‐Jong Paik, Department of Rehabilitation Medicine, Seoul National University |
| Notes | Date accessed December 2013 |
| Trial name or title | VIrtual Reality Training for Upper Extremity after Stroke (VIRTUES) |
| Methods | RCT |
| Participants | 1‐12 weeks post stroke |
| Interventions | VR intervention: VR training using the YouGrabber® for participants with impaired arm motor function after stroke. The YouGrabber exercises focus on intensity, repetitions, and motivating tasks ,and are adapted to the patient's motor abilities Control: participants receive supervised self‐training exercises with focus on functional tasks adapted to their motor abilities |
| Outcomes | Primary outcome: Action Research Arm Test |
| Starting date | Unclear |
| Contact information | Dr Iris Brunner |
| Notes | NCT02079103 |
| Trial name or title | Comparing the cognition effects of two exergame systems and traditional weight shifting training in patients with chronic stroke: a pilot randomized comparison trial |
| Methods | RCT |
| Participants | People in the chronic phase after stroke |
| Interventions | Intervention arm 1: Wii Fit Intervention arm 2: Tetrax biofeedback Control: conventional weight shifting |
| Outcomes | Primary outcome measure: Cognitive Abilities Screening Instrument Scale Chinese version |
| Starting date | 2015 |
| Contact information | Dr Jen Wen Hung |
| Notes | NCT02553993 |
| Trial name or title | Effects of upper extremity rehabilitation using Smart Glove in stroke patients |
| Methods | RCT |
| Participants | People following stroke |
| Interventions | Intervention: participants will be treated with conventional OT for 30 min and smart glove treatment for 30 min. 5 treatments/week will be conducted for a total of 2 weeks Control: participants will be treated with conventional OT for 30 min and upper extremity rehabilitation homework which means the self‐training at bedside, for 30 min. 5 treatments/week will be conducted for a total of 2 weeks |
| Outcomes | Primary outcome measure: Fugl Meyer UE |
| Starting date | Unclear |
| Contact information | A/Prof Han Gil Seo |
| Notes | NCT02592759 |
| Trial name or title | Evaluating the MindMotionPRO for early post‐stroke upper‐limb rehabilitation (MOVE‐Rehab) |
| Methods | RCT |
| Participants | 1‐6 weeks following first stroke |
| Interventions | VR intervention: MindMotionPRO exercises in addition to standard practice for upper limb rehabilitation Control intervention: self‐directed prescribed exercises |
| Outcomes | Primary outcome: dose of therapy |
| Starting date | 2016 |
| Contact information | — |
| Notes | NCT02688413 |
| Trial name or title | A randomised controlled trial comparing the impact of virtual reality, paper and pencil and conventional methods on stroke rehabilitation |
| Methods | RCT |
| Participants | Post stroke |
| Interventions | VR: Reh@City Paper and Pencil Conventional therapy All provided for 30 min, 3 times/week until 12 sessions |
| Outcomes | Montreal Cognitive Assessment, Stroke Impact Scale, Positive and Negative Affect Scale |
| Starting date | August 2016 |
| Contact information | Ana Lúcia Faria, ana.faria@m‐iti.org |
| Notes | NCT02857803 |
| Trial name or title | Effect of virtual reality training on reach after stroke |
| Methods | RCT |
| Participants | Individuals in the chronic phase post stroke |
| Interventions | VR intervention: reach training using a VR program Control intervention: reach training in a traditional therapy setting |
| Outcomes | Primary outcomes: Action Research Arm test, Fugl‐Meyer assessment, Intrinsic Motivation Inventory |
| Starting date | April 2010 |
| Contact information | Dr Kottink: [email protected] |
| Notes | Date accessed December 2013 |
| Trial name or title | Effects of training in a virtual environment in chronic stroke patients |
| Methods | RCT |
| Participants | People in the chronic phase after stroke |
| Interventions | VR intervention: Nintendo Wii Fit Plus balance and mobility games Control intervention: conventional balance and mobility training |
| Outcomes | Balance, cognition and functional assessments |
| Starting date | Unknown |
| Contact information | Dr Maria Piemonte: [email protected] |
| Notes | — |
| Trial name or title | Home‐based self training using video games: preliminary data from a randomised controlled trial |
| Methods | RCT |
| Participants | People following stroke 6‐36 months earlier |
| Interventions | Intervention: video game self‐training group using PS2 EyeToy, PS3 MOVE or Xbox Kinect Control: self‐training program |
| Outcomes | Box and Block Test, ARAT, Functional Reach Test |
| Starting date | — |
| Contact information | |
| Notes | — |
| Trial name or title | Using mixed methods to evaluate efficacy and user expectations of a virtual reality based training system for upper limb recovery in patients after stroke: a study protocol for a randomised controlled trial |
| Methods | RCT |
| Participants | People after stroke |
| Interventions | Intervention: 16 YouGrabber training sessions Control: 16 conventional therapy sessions |
| Outcomes | Primary outcome: Box and Block Test |
| Starting date | Unclear |
| Contact information | c.schuster@reha‐rhf.ch |
| Notes | NCT01774669 |
| Trial name or title | Virtual reality exercise for stroke rehabilitation in inpatients who are unable to stand |
| Methods | RCT |
| Participants | Stroke inpatients unable to stand |
| Interventions | VR: each participant will engage in 10‐12 sessions of 30‐50 min each of VR training (VRT) using Jintronix Rehabilitation Software and 3‐dimensional motion capture technology. A camera captures the movements of the participant and allows him or her to control an avatar, which interacts with the game. Exercises challenge sitting balance control, reaching and shifting the base of support; for example, controlling a ball as it rolls down a maze or reaching to put dishes away in a virtual kitchen. The difficulty of the games is monitored to maintain a challenge to sitting balance. The participant sits on a CONFORMat pressure mat which continuously monitors his or her centre of pressure to ensure that the participant is adequately challenged during the VRT Control: each participant will engage in 10‐12 sessions of 30‐50 min each of VRT using Jintronix Rehabilitation Software and 3‐dimensional motion capture technology. A camera captures the movements of the participant and allows him or her to control an avatar, which interacts with the game. Control group exercises require limited hand and arm movements; for example, using an arm to move a fish along a simple pathway or using the arms to pop balloons without reaching. Control group participants are strapped into their chair to minimise trunk movement. The participant sits on a CONFORMat pressure mat which continuously monitors his or her centre during the VRT |
| Outcomes | Primary outcome: change in the Function in Sitting Test |
| Starting date | 2014 |
| Contact information | Dr Lisa Sheehy |
| Notes | — |
RCT: randomised controlled trial
VR: virtual reality
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Upper limb function post intervention (composite measure) Show forest plot | 22 | 1038 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.05, 0.20] |
| Analysis 1.1  Comparison 1 Virtual reality versus conventional therapy: effect on upper limb function post intervention, Outcome 1 Upper limb function post intervention (composite measure). | ||||
| 2 Upper limb function post intervention (Fugl Meyer) Show forest plot | 16 | 599 | Mean Difference (IV, Fixed, 95% CI) | 2.85 [1.06, 4.65] |
| Analysis 1.2  Comparison 1 Virtual reality versus conventional therapy: effect on upper limb function post intervention, Outcome 2 Upper limb function post intervention (Fugl Meyer). | ||||
| 3 Hand function post intervention (grip strength) Show forest plot | 6 | 266 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.27, 0.22] |
| Analysis 1.3  Comparison 1 Virtual reality versus conventional therapy: effect on upper limb function post intervention, Outcome 3 Hand function post intervention (grip strength). | ||||
| 4 Upper limb function post intervention: amount of use (subjective) Show forest plot | 5 | 161 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.11 [‐0.42, 0.21] |
| Analysis 1.4  Comparison 1 Virtual reality versus conventional therapy: effect on upper limb function post intervention, Outcome 4 Upper limb function post intervention: amount of use (subjective). | ||||
| 5 Upper limb function at short term follow‐up (up to 3 months) Show forest plot | 9 | 366 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.10, 0.32] |
| Analysis 1.5  Comparison 1 Virtual reality versus conventional therapy: effect on upper limb function post intervention, Outcome 5 Upper limb function at short term follow‐up (up to 3 months). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Dose of intervention Show forest plot | 22 | 1038 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.05, 0.20] |
| Analysis 2.1  Comparison 2 Virtual reality versus conventional therapy: upper limb function: subgroup analyses, Outcome 1 Dose of intervention. | ||||
| 1.1 Less than 15 hours of intervention | 9 | 430 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.01 [‐0.20, 0.18] |
| 1.2 More than 15 hours of intervention | 13 | 608 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.13 [‐0.03, 0.29] |
| 2 Time since onset of stroke Show forest plot | 20 | 930 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.04 [‐0.09, 0.17] |
| Analysis 2.2  Comparison 2 Virtual reality versus conventional therapy: upper limb function: subgroup analyses, Outcome 2 Time since onset of stroke. | ||||
| 2.1 Less than 6 months | 7 | 555 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.06 [‐0.23, 0.11] |
| 2.2 More than 6 months | 13 | 375 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.19 [‐0.02, 0.39] |
| 3 Specialised or gaming Show forest plot | 22 | 1038 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.05, 0.20] |
| Analysis 2.3  Comparison 2 Virtual reality versus conventional therapy: upper limb function: subgroup analyses, Outcome 3 Specialised or gaming. | ||||
| 3.1 Specialised | 15 | 506 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.17 [‐0.00, 0.35] |
| 3.2 Gaming | 7 | 532 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.20, 0.15] |
| 4 Severity of impairment Show forest plot | 21 | 998 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.06, 0.19] |
| Analysis 2.4  Comparison 2 Virtual reality versus conventional therapy: upper limb function: subgroup analyses, Outcome 4 Severity of impairment. | ||||
| 4.1 Mild to moderate impairment | 13 | 678 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.06, 0.25] |
| 4.2 Moderate to severe impairment | 8 | 320 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.22, 0.23] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Upper limb function (composite measure) Show forest plot | 10 | 210 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.49 [0.21, 0.77] |
| Analysis 3.1  Comparison 3 Additional virtual reality intervention: effect on upper limb function post intervention, Outcome 1 Upper limb function (composite measure). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Dose of intervention Show forest plot | 10 | 210 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.49 [0.21, 0.77] |
| Analysis 4.1  Comparison 4 Additional virtual reality intervention: effect on upper limb function post intervention: subgroup analyses, Outcome 1 Dose of intervention. | ||||
| 1.1 Less than 15 hours of intervention | 7 | 153 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.47 [0.14, 0.80] |
| 1.2 More than 15 hours of intervention | 3 | 57 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.54 [0.00, 1.07] |
| 2 Time since onset of stroke Show forest plot | 9 | 181 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.44 [0.14, 0.74] |
| Analysis 4.2 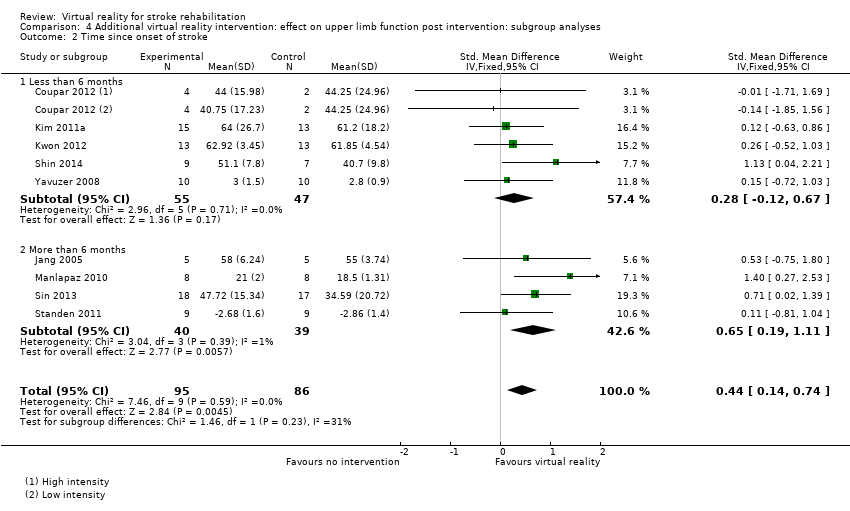 Comparison 4 Additional virtual reality intervention: effect on upper limb function post intervention: subgroup analyses, Outcome 2 Time since onset of stroke. | ||||
| 2.1 Less than 6 months | 5 | 102 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.28 [‐0.12, 0.67] |
| 2.2 More than 6 months | 4 | 79 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.65 [0.19, 1.11] |
| 3 Specialised or gaming Show forest plot | 10 | 210 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.49 [0.21, 0.77] |
| Analysis 4.3  Comparison 4 Additional virtual reality intervention: effect on upper limb function post intervention: subgroup analyses, Outcome 3 Specialised or gaming. | ||||
| 3.1 Specialised | 7 | 139 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.40 [0.06, 0.75] |
| 3.2 Gaming | 3 | 71 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.67 [0.18, 1.15] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gait speed Show forest plot | 6 | 139 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.04, 0.22] |
| Analysis 5.1  Comparison 5 Virtual reality versus conventional therapy: effect on lower limb activity post intervention, Outcome 1 Gait speed. | ||||
| 2 Timed Up and Go Test Show forest plot | 3 | 89 | Mean Difference (IV, Fixed, 95% CI) | ‐1.76 [‐4.67, 1.16] |
| Analysis 5.2  Comparison 5 Virtual reality versus conventional therapy: effect on lower limb activity post intervention, Outcome 2 Timed Up and Go Test. | ||||
| 3 Balance Show forest plot | 3 | 72 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.39 [‐0.09, 0.86] |
| Analysis 5.3 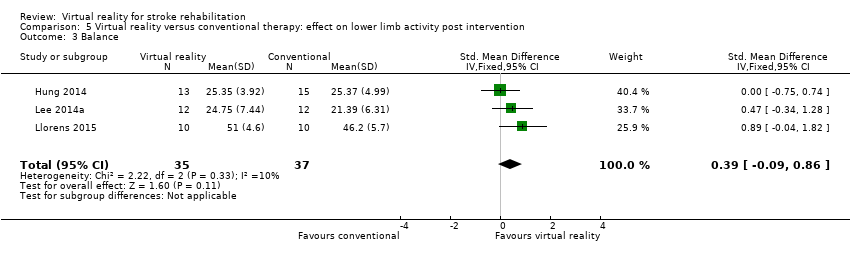 Comparison 5 Virtual reality versus conventional therapy: effect on lower limb activity post intervention, Outcome 3 Balance. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Dose of intervention: effect on gait speed Show forest plot | 6 | 139 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.04, 0.22] |
| Analysis 6.1 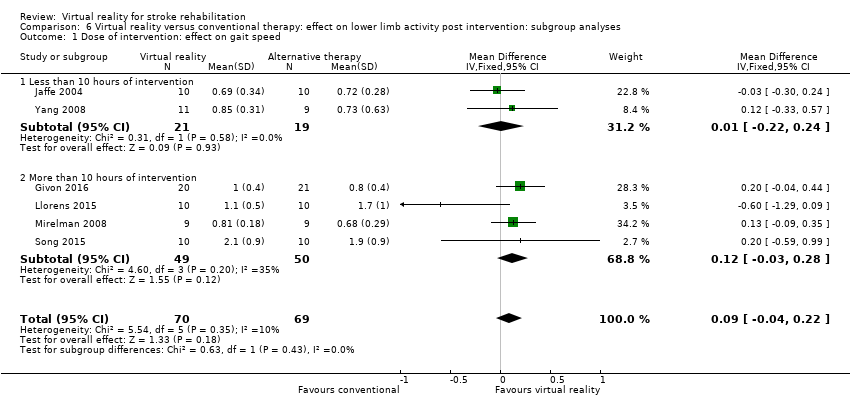 Comparison 6 Virtual reality versus conventional therapy: effect on lower limb activity post intervention: subgroup analyses, Outcome 1 Dose of intervention: effect on gait speed. | ||||
| 1.1 Less than 10 hours of intervention | 2 | 40 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.22, 0.24] |
| 1.2 More than 10 hours of intervention | 4 | 99 | Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.03, 0.28] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gait speed Show forest plot | 3 | 57 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.05, 0.21] |
| Analysis 7.1 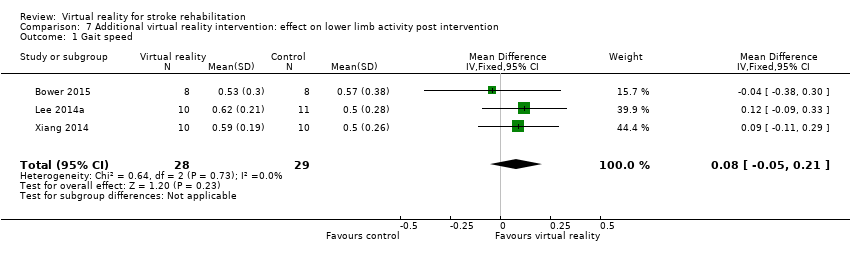 Comparison 7 Additional virtual reality intervention: effect on lower limb activity post intervention, Outcome 1 Gait speed. | ||||
| 2 Functional mobility (Timed Up and Go) Show forest plot | 3 | 93 | Mean Difference (IV, Fixed, 95% CI) | ‐4.76 [‐8.91, ‐0.61] |
| Analysis 7.2  Comparison 7 Additional virtual reality intervention: effect on lower limb activity post intervention, Outcome 2 Functional mobility (Timed Up and Go). | ||||
| 3 Balance Show forest plot | 7 | 173 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.59 [0.28, 0.90] |
| Analysis 7.3  Comparison 7 Additional virtual reality intervention: effect on lower limb activity post intervention, Outcome 3 Balance. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global motor function Show forest plot | 3 | 43 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.60, 0.61] |
| Analysis 8.1  Comparison 8 Additional virtual reality intervention: effect on global motor function post intervention, Outcome 1 Global motor function. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 ADL outcome Show forest plot | 10 | 466 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.25 [0.06, 0.43] |
| Analysis 9.1  Comparison 9 Virtual reality versus conventional therapy: effect on activity limitation, Outcome 1 ADL outcome. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 ADL outcome Show forest plot | 8 | 153 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.44 [0.11, 0.76] |
| Analysis 10.1  Comparison 10 Additional virtual reality intervention: effect on activity limitation, Outcome 1 ADL outcome. | ||||

Methodological quality summary: review authors' judgements about each methodological quality item for each included study
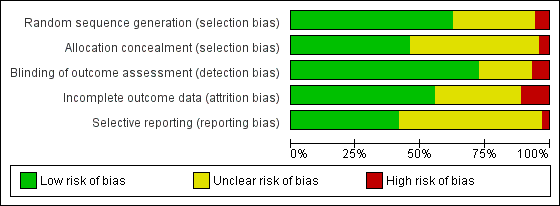
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies

Comparison 1 Virtual reality versus conventional therapy: effect on upper limb function post intervention, Outcome 1 Upper limb function post intervention (composite measure).

Comparison 1 Virtual reality versus conventional therapy: effect on upper limb function post intervention, Outcome 2 Upper limb function post intervention (Fugl Meyer).

Comparison 1 Virtual reality versus conventional therapy: effect on upper limb function post intervention, Outcome 3 Hand function post intervention (grip strength).

Comparison 1 Virtual reality versus conventional therapy: effect on upper limb function post intervention, Outcome 4 Upper limb function post intervention: amount of use (subjective).

Comparison 1 Virtual reality versus conventional therapy: effect on upper limb function post intervention, Outcome 5 Upper limb function at short term follow‐up (up to 3 months).

Comparison 2 Virtual reality versus conventional therapy: upper limb function: subgroup analyses, Outcome 1 Dose of intervention.

Comparison 2 Virtual reality versus conventional therapy: upper limb function: subgroup analyses, Outcome 2 Time since onset of stroke.

Comparison 2 Virtual reality versus conventional therapy: upper limb function: subgroup analyses, Outcome 3 Specialised or gaming.

Comparison 2 Virtual reality versus conventional therapy: upper limb function: subgroup analyses, Outcome 4 Severity of impairment.

Comparison 3 Additional virtual reality intervention: effect on upper limb function post intervention, Outcome 1 Upper limb function (composite measure).

Comparison 4 Additional virtual reality intervention: effect on upper limb function post intervention: subgroup analyses, Outcome 1 Dose of intervention.
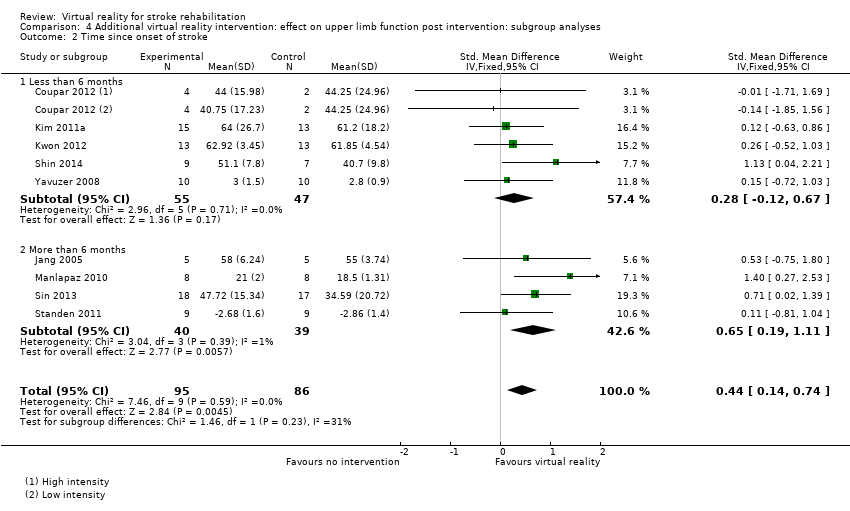
Comparison 4 Additional virtual reality intervention: effect on upper limb function post intervention: subgroup analyses, Outcome 2 Time since onset of stroke.

Comparison 4 Additional virtual reality intervention: effect on upper limb function post intervention: subgroup analyses, Outcome 3 Specialised or gaming.

Comparison 5 Virtual reality versus conventional therapy: effect on lower limb activity post intervention, Outcome 1 Gait speed.

Comparison 5 Virtual reality versus conventional therapy: effect on lower limb activity post intervention, Outcome 2 Timed Up and Go Test.
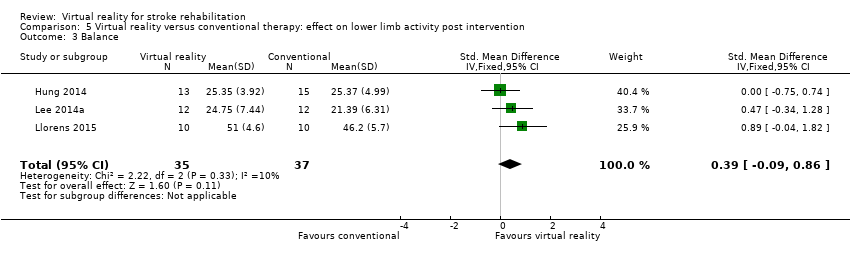
Comparison 5 Virtual reality versus conventional therapy: effect on lower limb activity post intervention, Outcome 3 Balance.
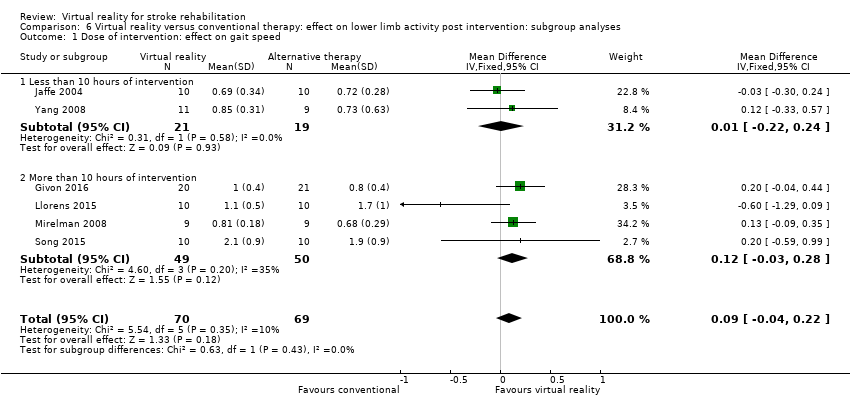
Comparison 6 Virtual reality versus conventional therapy: effect on lower limb activity post intervention: subgroup analyses, Outcome 1 Dose of intervention: effect on gait speed.
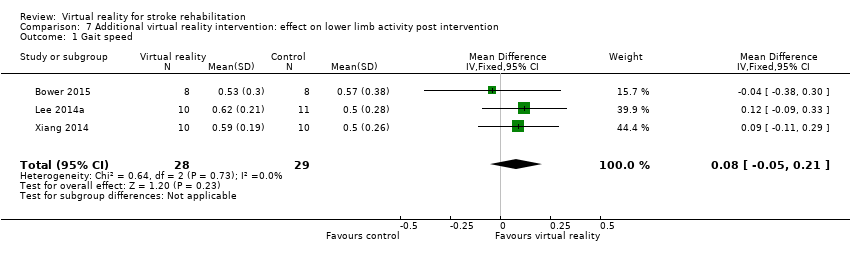
Comparison 7 Additional virtual reality intervention: effect on lower limb activity post intervention, Outcome 1 Gait speed.

Comparison 7 Additional virtual reality intervention: effect on lower limb activity post intervention, Outcome 2 Functional mobility (Timed Up and Go).

Comparison 7 Additional virtual reality intervention: effect on lower limb activity post intervention, Outcome 3 Balance.

Comparison 8 Additional virtual reality intervention: effect on global motor function post intervention, Outcome 1 Global motor function.

Comparison 9 Virtual reality versus conventional therapy: effect on activity limitation, Outcome 1 ADL outcome.

Comparison 10 Additional virtual reality intervention: effect on activity limitation, Outcome 1 ADL outcome.
| Virtual reality compared to conventional therapy for stroke rehabilitation | ||||||
| Patient or population: people receiving stroke rehabilitation Comparison: conventional therapy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Virtual reality | |||||
| Upper limb function | Same dose of conventional therapy | The mean upper limb function in the intervention groups was | 1038 | ⊕⊕⊝⊝ | No statistically significant difference between groups | |
| Quality of life | Same dose of conventional therapy | No significant benefit found on total score of the SF‐36 | 300 (3 studies) | ⊕⊕⊝⊝ low1,2,4 | Studies could not be pooled. None of the 3 studies found significant differences between groups in total score. 2 studies reported significant differences in domains of the SF36 | |
| Gait speed | Same dose of conventional therapy | The mean gait speed in the intervention groups was | 139 | ⊕⊕⊝⊝ | No statistically significant difference between groups | |
| ADL outcome | Same dose of conventional therapy | The mean ADL outcome in the intervention groups was | 466 | ⊕⊕⊕⊝ | Small effect in favour of those receiving virtual reality intervention | |
| ADL: activities of daily living; CI: confidence interval | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Risk of bias was unclear in a number of studies. | ||||||
| Virtual reality intervention compared with usual care (thus provided as additional therapy) for stroke rehabilitation | ||||||
| Patient or population: people receiving stroke rehabilitation Settings: hospital, clinic or home Intervention: virtual reality provided in addition to usual care Comparison: usual care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Virtual reality (provided in addition to usual care) | |||||
| Upper limb function | Usual care | The SMD in the intervention groups was 0.49 standard deviations higher (0.21 to 0.77) | ‐ | 210 (10 studies) | ⊕⊕⊝⊝ | Moderate effect in favour of providing virtual reality intervention in addition to usual care |
| Quality of life ‐ not measured in any of the studies | ‐ | ‐ | ‐ | ‐ | ‐ | Not measured in the studies |
| Gait speed | Usual care | The mean difference in the intervention groups was | ‐ | 57 (3 studies) | ⊕⊕⊝⊝ | No statistically significant difference between groups |
| Global motor function | Usual care | The SMD in the intervention groups was | ‐ | 43 (3 studies) | ⊕⊕⊝⊝ | No statistically significant difference between groups |
| ADL outcome | Usual care | The SMD in the intervention groups was 0.44 standard deviations higher (0.11 to 0.76) | ‐ | 153 (8 studies) | ⊕⊕⊝⊝ | Small to moderate effect in favour of virtual reality intervention |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ADL: activities of daily living; CI: confidence interval; MD: mean difference; RR: risk ratio; SMD: standardised mean difference | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Risk of bias was unclear in a number of studies. | ||||||
| Author and year | Upper limb function | Hand function | Lower limb activity | Balance and postural control | Global motor function | Cognitive function | Activity limitation | Participation restriction and QOL |
| Action Research Arm Test, Motor Activity Log Arm Function Test | Modified Rankin Scale | Stroke Impact Scale, EQ5D, Canadian Occupational Performance Measure | ||||||
| — | — | — | — | — | Useful Field of View test | On‐road driving test score, decision of fitness to drive | — | |
| — | — | Timed Up and Go | Berg Balance Scale, centre of pressure data, body symmetry data | — | — | Functional Independence Measure | — | |
| 6‐minute walk test, step test | Functional reach | Motor Assessment Scale | Functional Independence Measure (transfers, mobility, stairs) | |||||
| Fugl Meyer UE Scale, Motor Proficiency Speed (abbreviated Wolf Motor Function test + Digital reaction time test) | Motor skill performance (Box and Block and tapper test) | — | — | — | — | Functional Independence (CAFE40) | ||
| Wolf Motor Function Test | — | — | — | — | Motor Free Visual Perception Test | — | — | |
| 10‐m walk test | Berg Balance Scale | Modified Barthel Index | ||||||
| Action Research Arm Test, Upper Limb Motricity Index | — | — | — | — | — | — | — | |
| Fugl Meyer | Dynamic Gait Index | SF36 | ||||||
| Fugl Meyer UE, Chedoke Arm and Hand Inventory | — | — | — | — | — | Barthel Index | — | |
| Jebsen Taylor Hand Function Test | Stroke Impact Scale | |||||||
| Fugl Meyer, Motor Activity Log | ||||||||
| Action Research Arm Test | Grip strength | 10‐m walk test | ||||||
| Berg Balance Scale | Modified Barthel Index | |||||||
| Fugl Meyer UE Scale, Rancho Functional Test, Motor Activity Log (amount of use and quality of movement) | Grip strength (kg) | — | — | — | — | — | ‐ | |
| Timed Up and Go Test | Forward Reach Test | Falls Efficacy Scale International | ||||||
| — | — | 6‐m walk test, Obstacle Test, 6‐minute walk test | Customised balance test designed by the researchers | — | — | — | — | |
| Fugl Meyer UE Scale, Manual Function Test, Motor Activity Log (amount of use and quality of movement) | Box and Block Test | — | — | — | — | — | ||
| — | — | — | — | — | — | — | — | |
| — | — | Timed Up and Go | — | — | — | — | — | |
| — | — | — | — | — | Mini Mental State Examination | Modified Barthel Index | — | |
| — | — | 10‐m walk test, GAIT‐RITE gait analysis system | Berg Balance Scale, balance performance monitor | Modified Motor Assessment Scale | — | — | — | |
| Motricity Index | — | Motricity Index | — | — | Computerised neuropsychological test and Tower of London test | Korean Modified Barthel Index | — | |
| — | — | — | — | — | Measures of spatial neglect (star cancellation, line bisection test, Catherine Bergego Scale) | Korean Modified Barthel Index | — | |
| — | — | — | Postural assessment scale | Modified Motor Assessment Scale | — | Functional Independence Measure | — | |
| Fugl Meyer UE | — | — | — | — | — | Functional Independence Measure | — | |
| Fugl Meyer UE, Wolf Motor Function Test, Motor Activity Log (quality of movement) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | Stroke Impact Scale, Goal attainment scale | |
| Timed Up and Go Test | Berg Balance Scale | |||||||
| Fugl Meyer, Action Research Arm Test | Functional Independence Measure | Stroke Impact Scale | ||||||
| Fugl Meyer UE, Manual Function Test | — | — | — | — | — | Korean Modified Barthel Index | — | |
| — | — | — | — | — | — | — | — | |
| Functional Reach Test | ||||||||
| Timed Up and Go Test | Berg Balance Scale | |||||||
| Functional Reach Test | ||||||||
| Fugl Meyer UE Scale, Reach Performance Scale for Stroke, Box and Blocks Test, Wolf Motor Function Test, Motor Activity Log | ||||||||
| Stroke Impact Scale | ||||||||
| Tinetti Performance Oriented Mobility Assessment, 10‐m walk test | Berg Balance Scale, Brunel Balance Assessment | |||||||
| Fugl Meyer UE Scale, Action Research Arm Test | Gait speed | Berg Balance Scale | Functional Independence Measure | |||||
| Fugl Meyer UE Scale | Motor Assessment Scale | |||||||
| Gait analysis (gaitlab assessment) | ||||||||
| Fugl Meyer UE, Wolf Motor Function Test, Box and Block Test, Motor Activity Log | ||||||||
| — | — | — | — | — | — | DriveAble Testing Ltd Driver Evaluation | — | |
| Wolf Motor Function Test timed tasks and strength subtests, Motor Activity Log QOM scale, Fugl Meyer, Box and Block Test | ||||||||
| — | — | Gait speed over 7‐metre walkway, 6‐minute walk test, Patient Activity Monitor | — | — | — | — | — | |
| 10‐m walk test | Berg Balance Scale | Barthel Index | Functional Ambulation Category | |||||
| Static balance ability | ||||||||
| Fugl Meyer UE Scale | — | — | — | — | — | Functional Independence Measure | — | |
| Fugl Meyer UE Scale, Abilhand Scale | — | — | — | — | — | — | ‐ | |
| Fugl Meyer UE Scale | — | — | — | — | — | Functional Independence Measure | — | |
| Fugl Meyer UE, Stroke Upper Limb Capacity Sclae | ||||||||
| — | — | Timed Up and Go | Berg Balance Scale, functional reach, centre of pressure | — | — | — | — | |
| Fugl Meyer UE, Ranchos Functional Test for UE, Motor Activity Log, Box and Blocks Test | Grip strength | |||||||
| Abbreviated Wolf Motor Function Test | Box and Block Test, grip strength (kg) | — | — | — | — | — | Stroke Impact Scale (hand function, composite function, perception of recovery) | |
| Abbreviated Wolf Motor Function Test, Box and Block Test | Grip strength | Functional Independence Measure, Barthel Index, Modified Rankin Scale | Stroke Impact Scale | |||||
| Fugl Meyer UE | — | — | — | — | — | Modified Barthel Index | — | |
| Fugl Meyer UE | SF36 | |||||||
| Fugl Meyer UE, Box and Block Test | — | — | — | — | — | — | ||
| Timed Up and Go Test, 10‐minute walk test | Balance (Biofeedback system) | |||||||
| Wolf Motor Function Test, Motor Activity Log, Nine Hole Peg Test | — | — | — | — | Nottingham Extended Activities of Daily Living Scale | |||
| Fugl Meyer UE, Wolf Motor Function test, Reaching performance scale for stroke, Motor Activity Log | — | — | — | — | — | — | ||
| Fugl Meyer UE Scale, Upper Limb Motricity Index | — | — | — | — | — | — | — | |
| Action Research Arm Test, Jebsen Taylor Hand Function Test, Fugl Meyer UE | Grip strength | |||||||
| Timed walking speed test, Timed Up and Go | Mini Mental State Examination | Functional Ambulation Category | ||||||
| 10‐m walking speed, Fugl Meyer (LE) | Brunel Balance Assessment | |||||||
| — | — | Walking speed, Community Walk Test | — | — | — | — | Walking Ability Questionnaire, Activities Specific Balance Confidence Scale | |
| — | — | Gait analysis data | Balance analysis data | — | — | — | — | |
| Brunnstrom Upper Extremity Stages | Brunnstrom Hand Stages | — | — | — | — | Functional Independence Measure self‐care section | — | |
| Fugl Meyer, Action Research Arm Test, Motor Activity Log | Functional Independence Measure | |||||||
| — | — | Functional ambulation category | — | Modified Motor Assessment Scale | — | — | — | |
| Fugl Meyer UE, Reaching performance scale | — | — | — | — | — | Functional Independence Measure | — | |
| fMRI: functional magnetic resonance imaging | ||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Upper limb function post intervention (composite measure) Show forest plot | 22 | 1038 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.05, 0.20] |
| 2 Upper limb function post intervention (Fugl Meyer) Show forest plot | 16 | 599 | Mean Difference (IV, Fixed, 95% CI) | 2.85 [1.06, 4.65] |
| 3 Hand function post intervention (grip strength) Show forest plot | 6 | 266 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.27, 0.22] |
| 4 Upper limb function post intervention: amount of use (subjective) Show forest plot | 5 | 161 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.11 [‐0.42, 0.21] |
| 5 Upper limb function at short term follow‐up (up to 3 months) Show forest plot | 9 | 366 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.10, 0.32] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Dose of intervention Show forest plot | 22 | 1038 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.05, 0.20] |
| 1.1 Less than 15 hours of intervention | 9 | 430 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.01 [‐0.20, 0.18] |
| 1.2 More than 15 hours of intervention | 13 | 608 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.13 [‐0.03, 0.29] |
| 2 Time since onset of stroke Show forest plot | 20 | 930 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.04 [‐0.09, 0.17] |
| 2.1 Less than 6 months | 7 | 555 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.06 [‐0.23, 0.11] |
| 2.2 More than 6 months | 13 | 375 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.19 [‐0.02, 0.39] |
| 3 Specialised or gaming Show forest plot | 22 | 1038 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.05, 0.20] |
| 3.1 Specialised | 15 | 506 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.17 [‐0.00, 0.35] |
| 3.2 Gaming | 7 | 532 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.20, 0.15] |
| 4 Severity of impairment Show forest plot | 21 | 998 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.06, 0.19] |
| 4.1 Mild to moderate impairment | 13 | 678 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.06, 0.25] |
| 4.2 Moderate to severe impairment | 8 | 320 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.22, 0.23] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Upper limb function (composite measure) Show forest plot | 10 | 210 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.49 [0.21, 0.77] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Dose of intervention Show forest plot | 10 | 210 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.49 [0.21, 0.77] |
| 1.1 Less than 15 hours of intervention | 7 | 153 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.47 [0.14, 0.80] |
| 1.2 More than 15 hours of intervention | 3 | 57 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.54 [0.00, 1.07] |
| 2 Time since onset of stroke Show forest plot | 9 | 181 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.44 [0.14, 0.74] |
| 2.1 Less than 6 months | 5 | 102 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.28 [‐0.12, 0.67] |
| 2.2 More than 6 months | 4 | 79 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.65 [0.19, 1.11] |
| 3 Specialised or gaming Show forest plot | 10 | 210 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.49 [0.21, 0.77] |
| 3.1 Specialised | 7 | 139 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.40 [0.06, 0.75] |
| 3.2 Gaming | 3 | 71 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.67 [0.18, 1.15] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gait speed Show forest plot | 6 | 139 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.04, 0.22] |
| 2 Timed Up and Go Test Show forest plot | 3 | 89 | Mean Difference (IV, Fixed, 95% CI) | ‐1.76 [‐4.67, 1.16] |
| 3 Balance Show forest plot | 3 | 72 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.39 [‐0.09, 0.86] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Dose of intervention: effect on gait speed Show forest plot | 6 | 139 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.04, 0.22] |
| 1.1 Less than 10 hours of intervention | 2 | 40 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.22, 0.24] |
| 1.2 More than 10 hours of intervention | 4 | 99 | Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.03, 0.28] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gait speed Show forest plot | 3 | 57 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.05, 0.21] |
| 2 Functional mobility (Timed Up and Go) Show forest plot | 3 | 93 | Mean Difference (IV, Fixed, 95% CI) | ‐4.76 [‐8.91, ‐0.61] |
| 3 Balance Show forest plot | 7 | 173 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.59 [0.28, 0.90] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global motor function Show forest plot | 3 | 43 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.60, 0.61] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 ADL outcome Show forest plot | 10 | 466 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.25 [0.06, 0.43] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 ADL outcome Show forest plot | 8 | 153 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.44 [0.11, 0.76] |


