Position in the second stage of labour for women with epidural anaesthesia
Information
- DOI:
- https://doi.org/10.1002/14651858.CD008070.pub3Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 24 February 2017see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Pregnancy and Childbirth Group
- Copyright:
-
- Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
Marion Kibuka designed and wrote the first version of the protocol. Claire Kingswood revised the protocol. Jim Thornton revised the protocol. Emily Kemp and Jim Thornton identified, and classified studies, abstracted and entered data, carried out the analysis and wrote the initial version of this review.
For this update, Marion Kikbuka assessed the studies. Jim Thornton reviewed the final version. Also see Acknowledgements in relation to the assistance we received from Anna Cuthbert.
Sources of support
Internal sources
-
University of Nottingham, UK.
Claire Kingswood and Emily Kemp worked on the 2013 version of this review as part of their BMedSci projects in 2009 and 2010
External sources
-
UNDP‐UNFPA‐UNICEF‐WHO‐World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization, Switzerland.
Declarations of interest
Marion Kibuka: none known
Jim G Thornton: none known.
Acknowledgements
We are grateful to Emily Kemp and Claire J Kingswood for their contribution to the initial version of this review (Kemp 2013).
We would also like to thank Bita Mesgarpour for translating and assessing Amiri 2012.
This project was supported by the National Institute for Health research, via Cochrane Infrastructure funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
We are grateful to Anna Cuthbert (Research Associate with Cochrane Pregnancy and Childbirth) for her help in preparing this 'no new studies' update. Anna assessed studies for inclusion and prepared the updated review.
Version history
| Published | Title | Stage | Authors | Version |
| 2018 Nov 09 | Maternal position in the second stage of labour for women with epidural anaesthesia | Review | Kate F Walker, Marion Kibuka, Jim G Thornton, Nia W Jones | |
| 2017 Feb 24 | Position in the second stage of labour for women with epidural anaesthesia | Review | Marion Kibuka, Jim G Thornton | |
| 2013 Jan 31 | Position in the second stage of labour for women with epidural anaesthesia | Review | Emily Kemp, Claire J Kingswood, Marion Kibuka, Jim G Thornton | |
| 2009 Oct 07 | Position in the second stage of labour for women with epidural anaesthesia | Protocol | Marion Kibuka, Jim G Thornton, Claire J Kingswood | |
Differences between protocol and review
The methods have been updated and the current standard methods text for Cochrane Pregnancy and Childbirth has been incorporated. This includes the use of GRADE and inclusion of a 'Summary of findings' table. We have restructured the Plain Language Summary using the standardised headings developed by Cochrane Pregnancy and Childbirth.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Female; Humans; Pregnancy;
PICOs

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Comparison 1 Upright position versus recumbent position, Outcome 1 Operative birth (caesarean or instrumental vaginal).

Comparison 1 Upright position versus recumbent position, Outcome 2 Duration of second stage labour (minutes) (from time of randomisation to birth).
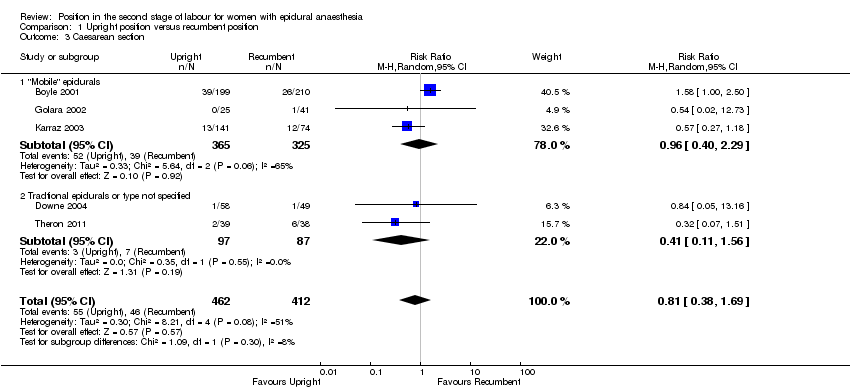
Comparison 1 Upright position versus recumbent position, Outcome 3 Caesarean section.
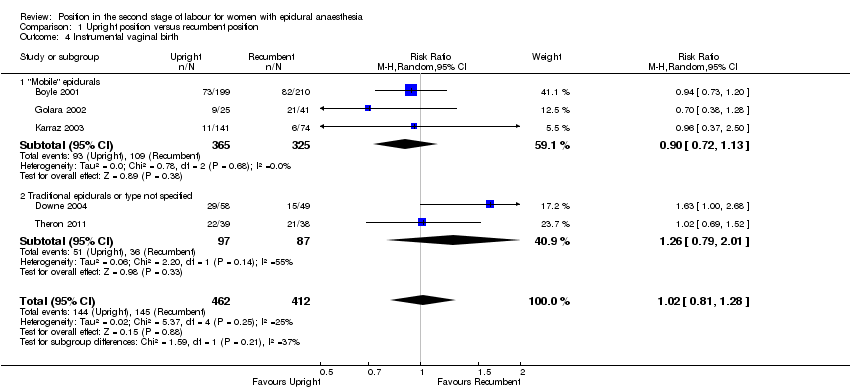
Comparison 1 Upright position versus recumbent position, Outcome 4 Instrumental vaginal birth.
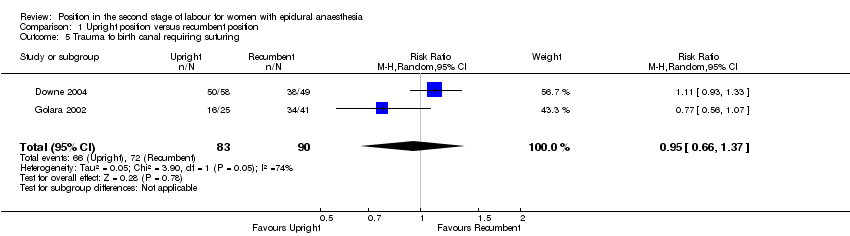
Comparison 1 Upright position versus recumbent position, Outcome 5 Trauma to birth canal requiring suturing.

Comparison 1 Upright position versus recumbent position, Outcome 6 Abnormal fetal heart rate patterns, requiring intervention.
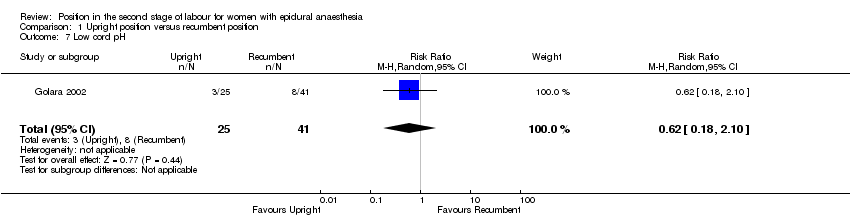
Comparison 1 Upright position versus recumbent position, Outcome 7 Low cord pH.

Comparison 1 Upright position versus recumbent position, Outcome 8 Admission to neonatal intensive care unit.
| Upright position compared to recumbent position for the second stage of labour for women with epidural anaesthesia | ||||||
| Patient or population: women with epidural anaesthesia in the second stage of labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with recumbent position | Risk with upright position | |||||
| Operative birth (caesarean or instrumental vaginal) | Study population | RR 0.97 | 874 | ⊕⊕⊕⊝ | ||
| 464 per 1000 | 450 per 1000 | |||||
| Duration of second stage labour (minutes) (from time of randomisation to birth) | The mean duration of second stage labour was 22.98 minutes less for women in the upright position (99.09 minutes less to 53.13 minutes more) | 322 | ⊕⊝⊝⊝ | |||
| Trauma to birth canal requiring suturing | Study population | RR 0.95 | 173 | ⊕⊝⊝⊝ | ||
| 800 per 1000 | 760 per 1000 | |||||
| Blood loss (greater than 500 mL) (or as defined by trial authors) | Study population | ‐ | (0 studies) | ‐ | No trial reported this outcome | |
| see comment | see comment | |||||
| Abnormal fetal heart rate patterns, requiring intervention | Study population | RR 1.69 | 107 | ⊕⊝⊝⊝ | ||
| 41 per 1000 | 69 per 1000 | |||||
| Low cord pH less than 7.1 (or as defined by trial authors) | Study population | RR 0.61 | 66 | ⊕⊝⊝⊝ | ||
| 195 per 1000 | 119 per 1000 | |||||
| Admission to neonatal intensive care unit | Study population | RR 0.54 | 66 | ⊕⊝⊝⊝ | ||
| 24 per 1000 | 13 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1All studies had design limitations. One trial contributing 24.2% weight had serious design limitations (‐1). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Operative birth (caesarean or instrumental vaginal) Show forest plot | 5 | 874 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.76, 1.25] |
| 1.1 "Mobile" epidurals | 3 | 690 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.61, 1.26] |
| 1.2 Traditional epidurals or type not specified | 2 | 184 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.62, 2.12] |
| 2 Duration of second stage labour (minutes) (from time of randomisation to birth) Show forest plot | 2 | 322 | Mean Difference (IV, Random, 95% CI) | ‐22.98 [‐99.09, 53.13] |
| 2.1 "Mobile" epidurals | 1 | 215 | Mean Difference (IV, Random, 95% CI) | ‐63.0 [‐97.94, ‐28.06] |
| 2.2 Traditional epidurals or type not specified | 1 | 107 | Mean Difference (IV, Random, 95% CI) | 14.70 [‐8.14, 37.54] |
| 3 Caesarean section Show forest plot | 5 | 874 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.38, 1.69] |
| 3.1 "Mobile" epidurals | 3 | 690 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.40, 2.29] |
| 3.2 Tradtional epidurals or type not specified | 2 | 184 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.11, 1.56] |
| 4 Instrumental vaginal birth Show forest plot | 5 | 874 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.81, 1.28] |
| 4.1 "Mobile" epidurals | 3 | 690 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.72, 1.13] |
| 4.2 Traditional epidurals or type not specified | 2 | 184 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [0.79, 2.01] |
| 5 Trauma to birth canal requiring suturing Show forest plot | 2 | 173 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.66, 1.37] |
| 6 Abnormal fetal heart rate patterns, requiring intervention Show forest plot | 1 | 107 | Risk Ratio (M‐H, Random, 95% CI) | 1.69 [0.32, 8.84] |
| 7 Low cord pH Show forest plot | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.18, 2.10] |
| 8 Admission to neonatal intensive care unit Show forest plot | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.02, 12.73] |


