Capsaicina tópica (alta concentración) para el dolor neuropático crónico en adultos
Appendices
Appendix 1. CENTRAL search strategy
-
MeSH descriptor Capsaicin (400)
-
(capsaicin OR capsaicine OR capsici OR axsain OR capsidol OR capsig OR capsin OR capsina OR capsiplast OR capzasin‐P OR dolorac OR gelcen OR katrum OR "No pain‐HP" OR priltam OR "R‐gel" OR zacin OR zostrix OR capsicum):TI,AB,KY (763)
-
1 OR 2 (763)
-
exp MeSH descriptor Administration, topical (13012)
-
(topical* OR cutaneous OR dermal OR transcutaneous OR transdermal OR percutaneous OR skin OR massage OR embrocation OR gel OR ointment OR aerosol OR cream OR crème OR lotion OR foam OR liniment OR spray OR rub OR balm OR salve OR emulsion OR oil OR patch OR plaster):TI,AB,KY (79078)
-
4 OR 5 (81831)
-
MeSH descriptor Diabetic neuropathies EXPLODE ALL TREES (1017)
-
MESH DESCRIPTOR Peripheral Nervous System Diseases EXPLODE ALL TREES (2878)
-
MESH DESCRIPTOR Neuralgia EXPLODE ALL TREES (694)
-
((neuropath* OR diabet* post‐herpetic OR neuralgia OR phantom OR stump)):TI,AB,KY (7096)
-
7 OR 8 OR 9 OR 10 (8623)
-
3 AND 6 AND 11 (108)
-
2012 TO 2016:YR (192843)
-
12 AND 13 (40)
Appendix 2. MEDLINE search strategy (via Ovid)
-
Capsaicin/ (1149)
-
(capsaicin OR capsaicine OR capsici OR axsain OR capsidol OR capsig OR capsin OR capsina OR capsiplast OR capzasin‐P OR dolorac OR gelcen OR katrum OR "No pain‐HP" OR priltam OR "R‐gel" OR zacin OR zostrix OR capsicum).mp. (2436)
-
1 or 2 (2436)
-
exp Administration, topical/ (10094)
-
(topical* OR cutaneous OR dermal OR transcutaneous OR transdermal OR percutaneous OR skin OR massage OR embrocation OR gel OR ointment OR aerosol OR cream OR creme OR lotion OR foam OR liniment OR spray OR rub OR balm OR salve OR emulsion OR oil OR patch OR plaster).mp. (191041)
-
4 or 5 (193874)
-
exp Diabetic neuropathies/ (2906)
-
exp Peripheral Nervous System Diseases/ (166699)
-
exp Neuralgia/ (3473)
-
(neuropath* OR diabet* post‐herpetic OR neuralgia OR phantom OR stump).mp. (28080)
-
7 or 8 or 9 or 10 (36908)
-
randomized controlled trial.pt. (83324)
-
controlled clinical trial.pt. (6282)
-
randomized.ab. (75790)
-
placebo.ab. (25769)
-
drug therapy.fs. (304825)
-
randomly.ab. (49098)
-
trial.ab. (78401)
-
groups.ab. (275092)
-
12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 (637615)
-
3 AND 6 AND 11 AND 20 (94)
Appendix 3. EMBASE search strategy (via Ovid)
-
Capsaicin/ (13552)
-
(capsaicin or capsaicine or capsici or axsain or capsidol or capsig or capsin or capsina or capsiplast or capzasin‐P or dolorac or gelcen or katrum or "No pain‐HP" or priltam or "R‐gel" or zacin or zostrix or capsicum).mp. (17641)
-
1 or 2 (17641)
-
exp Topical Drug Administration/ (28821)
-
(topical* or cutaneous or dermal or transcutaneous or transdermal or percutaneous or skin or massage or embrocation or gel or ointment or aerosol or cream or creme or lotion or foam or liniment v spray or rub or balm or salve or emulsion or oil or patch or plaster).mp. (1410353)
-
4 or 5 (1417324)
-
exp Diabetic Neuropathies/ (14444)
-
exp Peripheral Nervous System Diseases/ (43680)
-
exp Neuralgia/ (63962)
-
(neuropath* or diabet* post‐herpetic or neuralgia or phantom or stump).mp. (252239)
-
7 or 8 or 9 or 10 (276770)
-
Randomized controlled trial/ (348956)
-
Double‐blind procedure/ (102583)
-
Crossover‐procedure/ (41951)
-
(random* or factorial* or crossover* or cross over* or cross‐over* or placebo* or (doubl* adj blind*) or assign* or allocat*).tw. (1194868)
-
12 or 13 or 14 or 15 (1262910)
-
3 and 6 and 11 and 16 (359)
-
limit 17 to yr="2012‐Current" (124)
Appendix 4. GRADE: criteria for assigning grade of evidence
The GRADE system uses the following criteria for assigning a quality level to a body of evidence (Chapter 12, Higgins 2011).
-
High: randomised trials; or double‐upgraded observational studies.
-
Moderate: downgraded randomised trials; or upgraded observational studies.
-
Low: double‐downgraded randomised trials; or observational studies.
-
Very low: triple‐downgraded randomised trials; or downgraded observational studies; or case series/case reports.
Factors that may decrease the quality level of a body of evidence are:
-
limitations in the design and implementation of available studies suggesting high likelihood of bias;
-
indirectness of evidence (indirect population, intervention, control, outcomes);
-
unexplained heterogeneity or inconsistency of results (including problems with subgroup analyses);
-
imprecision of results (wide confidence intervals);
-
high probability of publication bias.
Factors that may increase the quality level of a body of evidence are:
-
large magnitude of effect;
-
all plausible confounding would reduce a demonstrated effect or suggest a spurious effect when results show no effect;
-
dose‐response gradient.
Appendix 5. Summary of outcomes in individual studies: efficacy
| Study ID | Treatment | Clinical improvement |
|---|---|---|
| (1) Capsaicin patch 8%, n = 206 (2) Control patch, n = 196 | Over 2 to 12 weeks ≥ 30% pain reduction from baseline: (1) 91/206, (2) 69/196 (Participants with ≥ 50% pain reduction from baseline ‐ no significant difference between groups) ≥ 2 points reduction in pain from baseline: (1) 87/206, (2) 55/196 At 12 weeks PGIC (slightly/much/very much improved): (1) 114/206, (2) 85/196 Over 2 to 8 weeks ≥ 30% pain reduction from baseline: (1) 87/206, (2) 63/196 ≥ 2 points reduction in pain from baseline: (1) 82/206, (2) 51/196 At 8 weeks PGIC (slightly/much/very much improved): (1) 109/206, (2) 83/196 | |
| (1) Capsaicin patch 8% 60 min, n = 24 (23 treated) (2) Placebo patch 60 min, n = 22 | No responder outcomes reported. No significant difference in the summed pain intensity difference (from baseline) between groups at 4, 8, or 12 weeks after treatment in completers | |
| (1) Capsaicin patch 8% 30 min, n = 167 (2) Capsaicin patch 8% 60 min, n = 165 (3) Control patch 30 min, n = 73 (4) Control patch 60 min, n = 89 | Over 2 to 12 weeks ≥ 30% pain reduction from baseline: (1) 65/167, (2) 79/165, (3) 19/73, (4) 40/89 At 12 weeks PGIC (slightly, much, very much improved): (1) 109/167, (2) 114/165, (3) 33/73, (4) 56/89 | |
| (1) Capsaicin patch 8%, n = 212 (2) Control patch, n = 204 | At 12 weeks ≥ 50% pain reduction from baseline: (1) 64/212, (2) 43/204 ≥ 30% pain reduction from baseline: (1) 100/212, (2) 71/204 At 12 weeks PGIC (much and very much improved): (1) 83/212, (2) 50/204 ≥ 2 points reduction in pain from baseline: (1) 91/212, (2) 59/204 Over 2 to 8 weeks ≥ 50% pain reduction from baseline: (1) 61/212, (2) 41/204 ≥ 30% pain reduction from baseline: (1) 98/212, (2) 69/204 At 8 weeks PGIC (much and very much improved): (1) 71/212, (2) 49/204 ≥ 2 points reduction in pain from baseline: (1) 89/212, (2) 53/204 | |
| (1) Capsaicin patch 8% 30 min, n = 72 (2) Capsaicin patch 8% 60 min, n = 78 (3) Capsaicin patch 8% 90 min, n = 75 (4) Control patch, n = 82 | Over 2 to 12 weeks ≥ 30% pain reduction from baseline: (1) 30/72, (2) 19/78, (3) 27/75, (4) 15/82 (capsaicin combined 76/225) At 12 weeks PGIC (much and very much improved): (1) 23/72, (2) 18/78, (3) 20/75, (4) 9/82 (capsaicin combined 61/225) | |
| (1) Capsaicin patch 8%, 30 min, n = 186 (2) Placebo patch, n = 183 | Over 2 to 8 weeks ≥ 50% pain reduction from baseline: (1) 39/186, (2) 33/183 ≥ 30% pain reduction from baseline: (1) 74/186, (2) 60/183 At 8 weeks PGIC (much and very much improved), using ITT denominators: (1) 71/186, (2) 52/183 Over 2 to 12 weeks ≥ 50% pain reduction from baseline: (1) 41/186, (2) 35/183 ≥ 30% pain reduction from baseline: (1) 76/186, (2) 58/183 At 12 weeks PGIC (much and very much improved), using ITT denominators: (1) 68/186, (2) 51/183 | |
| (1) Capsaicin patch 8% 30 min, n = 72 (2) Capsaicin patch 8% 60 min, n = 77 (3) Capsaicin patch 8% 90 min, n = 73 (4) Control patch, 30, 60, 90 min pooled for analysis, n = 77 | Over 2 to 8 weeks ≥ 50% pain reduction from baseline: (1) 17/72, (2) 21/77, (3) 17/73, (4) 8/77 ≥ 30% pain reduction from baseline: (1) 27/72, (2) 27/77, (3) 29/73, (4) 22/77 At 12 weeks PGIC (slight, much and very much improved): (1+2+3) 122/222 (capsaicin combined), (4) 32/77 | |
| (1) Capsaicin patch 8%, n = 102 (2) Control patch, n = 53 | Over 2 to 12 weeks ≥ 50% pain reduction from baseline: (1) 40/102, (2) 19/53 ≥ 30% pain reduction from baseline: (1) 50/102, (2) 26/53 At 12 weeks PGIC (much and very much improved): (1) 41/102, (2) 15/53 Over 2 to 8 weeks ≥ 50% pain reduction from baseline: (1) 37/102, (2) 19/53 ≥ 30% pain reduction from baseline: (1) 50/102, (2) 24/53 At 8 weeks PGIC (much and very much improved): (1) 43/102, (2) 14/53 | |
| ITT: intention‐to‐treat; min: minute; n: number of participants in treatment arm; PGIC: Patient Global Impression of Change. | ||
Appendix 6. Summary of outcomes in individual studies: adverse events and withdrawals
| Study ID | Treatment | Local AEs | Systemic AEs | Serious AEs | Withdrawals/exclusions |
|---|---|---|---|---|---|
| (1) Capsaicin patch 8%, n = 206 (2) Control patch, n = 196 | Mostly transient, mild to moderate Erythema: (1) 193/205, (2) 128/197 Pain: (1) 114/205, (2) 43/197 Papules: (1) 20/205, (2) 6/197 Pruritus: (1) 10/205, (2) 6/197 Oedema: (1) 12/205, (2) 2/197 | Nausea, vomiting, nasopharyngitis, sinusitis, back pain, dizziness, headache, worsening of PHN, hypertension ‐ all reported at < 5% per group, with no clear difference between groups | (1) 10/205, (2) 6/197 (1 in capsaicin group judged related to medication) | AE: (1) 1/205, (2) 0/197 LoE: (1) 10/205, (2) 9/197 Lost to follow‐up: (1) 3/205, (2) 2/197 Other: (1) 5/205, (2) 7/197 | |
| (1) Capsaicin patch 8% 60 min, n = 24 (23 treated) (2) Placebo patch 60 min, n = 22 | Pain: (1) 12/23, (2) 6/20 Erythema: (1) 9/23, (2) 3/20 Burning sensation: (1) 12/23, (2) 1/20 | None | None | AE: (1) 1/23 (due to pain during application), (2) 0/22 LoE: (1) 0.23, (2) 2/22 (began new analgesic treatment) Lost to follow‐up: (1) 0/23, (2) 2/22 | |
| (1) Capsaicin patch 8% 30 min, n = 167 (2) Capsaicin patch 8% 60 min, n = 165 (4) Control patch 60 min, n = 89 | Generally mild or moderate. Groups combined Erythema: (1+2) 176/332, (3+4) 58/162 Pain: (1+2) 274/332, (3+4) 62/162 Papules: (1+2) 12/332, (3+4) 0/162 Pruritus: (1+2) 12/332, (3+4) 2/162 Oedema: (1+2) 4/332, (3+4) 5/162 | Diarrhoea, nausea, respiratory tract infection, pain, worsening neuropathy ‐ all reported, generally < 5% per group | Approximately 6% in all groups with "infections and infestations" 1 death in capsaicin 60 min group (judged unrelated) | AE: (1) 0/167, (2) 2/165 (1 death), (3) 0/72, (4) 1/90 LoE: (1) 0/167, (2) 1/165, (3) 0/73, (4) 1/89 Lost to follow‐up: (1) 3/167, (2) 2/165, (3) 2/73, (4) 0/89 Other: (1) 8/167, (2) 6/165, (3) 0/73, (4) 6/89 | |
| (1) Capsaicin patch 8%, n = 212 (2) Control patch, n = 204 | Most mild or moderate Erythema: (1) 194/212, (2) 141/204 Pain: (1) 134/212, (2) 57/204 Papules: (1) 15/212, (2) 5/204 Pruritus: (1) 6/212, (2) 3/204 Oedema: (1) 13/212, (2) 0/204 | Nausea, vomiting, sinusitis, respiratory tract infection, musculoskeletal disorders, dizziness, headache ‐ all reported, most < 5% per group | (1) 11/212 (1 death), (2) 8/204 None considered drug‐related | AE: (1) 4/212 (1 death), (2) 3/304 LoE: (1) 1/212, (2) 5/204 Lost to follow‐up: (1) 4/212, (2) 5/204 Other: (1) 11/212, (2) 5/204 | |
| (1) Capsaicin patch 8% 30 min, n = 72 (2) Capsaicin patch 8% 60 min, n = 78 (3) Capsaicin patch 8% 90 min, n = 75 (4) Control patch, n = 82 | Self‐limiting and mild to moderate Pain: (1) 47/225, (2) 7/82 Papules: (1) 11/225, (2) 1/82 Pruritus: (1) 39/225, (2) 5/82 Swelling: (1) 29/225, (2) 7/82 | Diarrhoea, nausea, vomiting, fatigue, infections, musculoskeletal disorders, dizziness, headache, psychiatric disorders ‐ all reported, < 5% per group | (1) 1/225, (2) 2/82 All deaths, all judged unrelated to study medication | AE: (1) 3/225 (1 death), (2) 3/82 (2 deaths) LoE: (1) 1/225, (2) 2/82 Lost to follow‐up: (1) 13/225, (2) 4/82 Other: (1) 5/225, (2) 2/82 | |
| (1) Capsaicin patch 8%, 30 min, n = 186 (2) Placebo patch, n = 183 | Mostly mild or moderate Application site pain and reactions overall: (1) 63/186, (2) 15/183 Pain: (1) 18/186, (2) 4/183 Burning sensation: (1) 26/186, (2) 5/183 | Musculoskeletal disorders, infections, respiratory disorders, gastrointestinal disorders | (1) 2/186, (2) 7/183 | AE: (1) 0/186, (2) 1/183 Lost to follow‐up: (1) 2/186, (2) 1/183 Participant decision: (1) 7/186, (2) 6/183 | |
| (1) Capsaicin patch 8% 30 min, n = 72 (2) Capsaicin patch 8% 60 min, n = 77 (3) Capsaicin patch 8% 90 min, n = 73 (4) Control patch, 30, 60, 90 min pooled for analysis, n = 77 | Transient and mild to moderate Pain: (1) 1/222, (2) 2/77 Papules: (1) 3/222, (2) 2/77 Pruritus: (1) 17/222, (2) 9/77 Swelling: (1) 3/222, (2) 5/77 | Diarrhoea, nausea, vomiting, infections, musculoskeletal disorders, dizziness, headache, cough ‐ all reported, mostly < 5% per group | (1+2+3) 10/222 (1 death), (4) 3/77 None considered related to study medication | AE: (1+2+3) 2/222, (4) 1/77 (death) LoE: (1+2+3) 4/222, (4) 0/77 Lost to follow‐up (1+2+3) 7/222, (4) 1/77 Other: (1+2+3) 9/222, (4) 2/77 | |
| (1) Capsaicin patch 8%, n = 102 (2) Control patch, n = 53 | Transient and mild to moderate Erythema: (1) 4/102, (2) 0/53 Pain: (1) 4/102, (2) 2/53 Papules: (1) 4/102, (2) 2/53 Pruritus: (1) 17/102, (2) 6/53 Swelling: (1) 10/102, (2) 1/53 | Nausea, infections, musculoskeletal disorders, dizziness, cough, nasopharyngitis, hypertension ‐ all reported, mostly < 5% per group | (1) 7/102, (2) 0/53 None considered related to study medication | AE: None in either group LoE: (1) 3/102, (2) 7/53 Lost to follow‐up: (1) 5/102, (2) 0/53 Other: (1) 3/102, (2) 3/53 | |
| AE: adverse event; LoE: lack of efficacy; n: number of participants in treatment arm; PHN: postherpetic neuralgia; SAE: serious adverse event | |||||
Appendix 7. Patch tolerability
| Study ID | Treatment | Completed < 90% application time | Dermal irritation score > 2 at 2 hours | Rescue medication days 0 to 5 |
|---|---|---|---|---|
| (1) Capsaicin patch 8%, n = 206 (2) Control patch, n = 196 | (1) 1/206, (2) 2/196 | "Common but mild, transient and self‐limited" | (1) 99/206, (2) 32/196 | |
| (1) Capsaicin patch 8% 60 min, n = 24 (23 treated) (2) Placebo patch 60 min, n = 22 | Not reported 1 participant in (1) had patch removed early | No data | No data | |
| (1) Capsaicin patch 8% 30 min, n = 167 (2) Capsaicin patch 8% 60 min, n = 165 (3) Control patch 30 min, n = 73 (4) Control patch 60 min, n = 89 | (1+2) 10/332, (3+4) 0/162 | (1+2) 13/332, (3+4) 0/162 | (1+2) 246/332, (3+4) 53/162 | |
| (1) Capsaicin patch 8%, n = 212 (2) Control patch, n = 204 | (1) 4/212, (2) 0/204 | (1) 6/212, (2) 1/204 | (1) 112/212, (2) 43/204 | |
| (1) Capsaicin patch 8% 30 min, n = 72 (2) Capsaicin patch 8% 60 min, n = 78 (3) Capsaicin patch 8% 90 min, n = 75 (4) Control patch, n = 82 | (1) 0/72, (2) 0/78, (3) 2/75, (4) 0/82 | > 0 at 2 hours: (1+2+3) 92/225, (4) 23/82 | (1+2+3) 124/225, (4) 19/82 | |
| (1) Capsaicin patch 8%, 30 min, n = 186 (2) Placebo patch, n = 183 | No data | Dermal irritation (scale 0 to 7) score ≥ 4 (definite oedema) at 15 and 60 min after patch removal (1) 0/186, (2) 2/183 | (1) 35/186, (2) 10/183 | |
| (1) Capsaicin patch 8% 30 min, n = 72 (2) Capsaicin patch 8% 60 min, n = 77 (3) Capsaicin patch 8% 90 min, n = 73 (4) Control patch, 30, 60, 90 min pooled for analysis, n = 77 | (1) 0/73, (2) 1/77, (3) 0/73, (4) 0/77 | > 0 at 2 hours: (1+2+3) 87/222, (4) 5/77 | (1+2+3) 12/222, (4) 3/77 | |
| (1) Capsaicin patch 8%, n = 102 (2) Control patch, n = 53 | (1) 4/102, (2) 0/53 | (1) 53/102, (2) 2/53 | (1) 12/102, (2) 1/53 | |
| min: minutes; n: number of participants in treatment arm | ||||

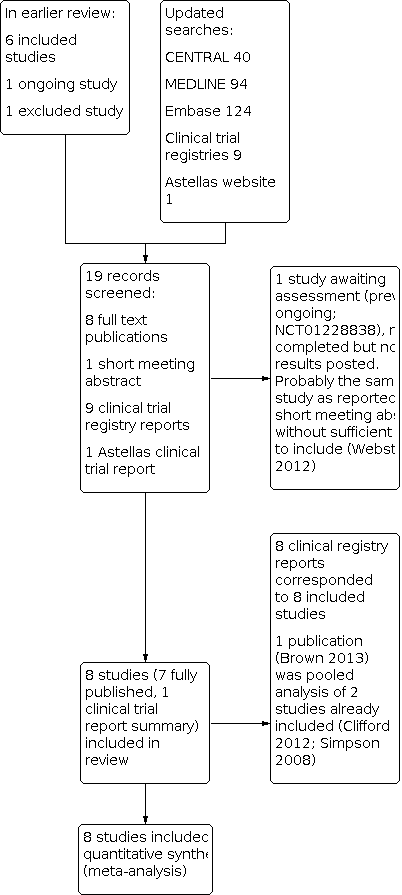
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 High‐concentration (8%) capsaicin versus control (single dose), outcome: 1.1 Postherpetic neuralgia ‐ at least 50% pain intensity reduction over weeks 2 to 8.

Forest plot of comparison: 1 High‐concentration (8%) capsaicin versus control (single dose), outcome: 1.5 Postherpetic neuralgia ‐ Patient Global Impression of Change much or very much improved at 8 and 12 weeks.

Forest plot of comparison: 1 High‐concentration (8%) capsaicin versus control (single dose), outcome: 1.6 HIV‐neuropathy ‐ at least 30% pain intensity reduction over weeks 2 to 12.

Forest plot of comparison: 1 High‐concentration (8%) capsaicin versus control (single dose), outcome: 1.10 Serious adverse events.

Comparison 1: High‐concentration (8%) capsaicin versus control (single dose), Outcome 1: Postherpetic neuralgia (PHN) ‐ at least 50% pain intensity reduction over weeks 2 to 8

Comparison 1: High‐concentration (8%) capsaicin versus control (single dose), Outcome 2: PHN ‐ at least 50% pain intensity reduction over 2 to 12 weeks

Comparison 1: High‐concentration (8%) capsaicin versus control (single dose), Outcome 3: PHN ‐ at least 30% pain intensity reduction over weeks 2 to 8

Comparison 1: High‐concentration (8%) capsaicin versus control (single dose), Outcome 4: PHN ‐ at least 30% pain intensity reduction over weeks 2 to 12

Comparison 1: High‐concentration (8%) capsaicin versus control (single dose), Outcome 5: PHN ‐ Patient Global Impression of ChangePGIC much or very much improved at 8 and 12 weeks

Comparison 1: High‐concentration (8%) capsaicin versus control (single dose), Outcome 6: HIV‐neuropathy ‐ at least 30% pain intensity reduction over weeks 2 to 12

Comparison 1: High‐concentration (8%) capsaicin versus control (single dose), Outcome 7: Local skin reactions ‐ group 1

Comparison 1: High‐concentration (8%) capsaicin versus control (single dose), Outcome 8: Local skin reactions ‐ group 2

Comparison 1: High‐concentration (8%) capsaicin versus control (single dose), Outcome 9: Patch tolerability

Comparison 1: High‐concentration (8%) capsaicin versus control (single dose), Outcome 10: Serious adverse events

Comparison 1: High‐concentration (8%) capsaicin versus control (single dose), Outcome 11: Withdrawals
| High‐concentration (8%) capsaicin patch compared with control patch (0.4%) for postherpetic neuralgia | ||||||
| Patient or population: adults with postherpetic neuralgia Settings: community Intervention: high‐concentration (8%) capsaicin patch, single application Comparison: control patch (0.4% capsaicin), single application | ||||||
| Outcomes | Outcome with intervention | Outcome with comparator | RR, NNT, NNH, NNTp (95% CI) | Number of | Quality of the evidence | Comments |
|---|---|---|---|---|---|---|
| Substantial benefit | ||||||
| PGICvery much improved, week 8 and week 12 | No data | No data | ‐ | ‐ | Very low | No data |
| Moderate benefit | ||||||
| PGICmuch or very much improved, week 8 | 360 in 1000 | 250 in 1000 | RR 1.4 (1.1 to 1.8) NNT 8.8 (5.3 to 26) | 2 studies, 571 participants, 178 events | Moderate | Downgraded 1 level due to susceptibility to publication bias |
| PGIC much or very much improved, week 12 | 390 in 1000 | 250 in 1000 | RR 1.6 (1.2 to 2.0) NNT 7.0 (4.6 to 15) | 2 studies, 571 participants, 189 events | Moderate | Downgraded 1 level due to susceptibility to publication bias |
| Harm ‐ all conditions combined | ||||||
| Withdrawals due to lack of efficacy | 15 in 1000 | 31 in 1000 | RR 0.58 (0.32 to 1.04) NNTp 64 (34 to 610) | 6 studies, 2073 participants, 44 events | Moderate | Downgraded 1 level due to imprecision (few events, wide CI) |
| Withdrawals due to adverse events | 8.0 in 1000 | 9.2 in 1000 | RR 0.80 (0.36 to 1.8) NNTp not calculated | 8 studies, 2487 participants, 21 events | Moderate | Downgraded 1 level due to sparse data (few events) |
| Serious adverse events | 35 in 1000 | 32 in 1000 | RR 1.1 (0.70 to 1.8) NNH not calculated | 7 studies, 1993 participants, 67 events | Moderate | Downgraded 1 level due to sparse data (few events) |
| Death | 4 events | 2 events | Not calculated | 8 studies, 2487 participants | Very low | Downgraded 3 levels as only six events, so no better grading possibleNo death was judged related to study medication by study authors |
| CI: confidence interval; NNH: number needed to treat for one additional harmful outcome; NNT: number needed to treat for one additional beneficial outcome; NNTp: number needed to treat to prevent one withdrawal event; PGIC: Patient Global Impression of Change; RR: risk ratio. | ||||||
| Descriptors for levels of evidence (EPOC 2015): † Substantially different: a large enough difference that it might affect a decision. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Postherpetic neuralgia (PHN) ‐ at least 50% pain intensity reduction over weeks 2 to 8 Show forest plot | 3 | 870 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.44 [1.12, 1.86] |
| 1.1.1 Using 30‐minute application | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.95 [0.73, 11.88] |
| 1.1.2 Using 60‐minute application | 3 | 674 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [1.03, 1.75] |
| 1.1.3 Using 90‐minute application | 1 | 99 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.02 [0.64, 6.33] |
| 1.2 PHN ‐ at least 50% pain intensity reduction over 2 to 12 weeks Show forest plot | 2 | 571 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [1.00, 1.71] |
| 1.3 PHN ‐ at least 30% pain intensity reduction over weeks 2 to 8 Show forest plot | 4 | 1268 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [1.13, 1.52] |
| 1.3.1 Using 30‐minute application | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [0.67, 2.69] |
| 1.3.2 Using 60‐minute application | 4 | 1072 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [1.12, 1.52] |
| 1.3.3 Using 90‐minute application | 1 | 99 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.74, 2.95] |
| 1.4 PHN ‐ at least 30% pain intensity reduction over weeks 2 to 12 Show forest plot | 3 | 973 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [1.07, 1.45] |
| 1.5 PHN ‐ Patient Global Impression of ChangePGIC much or very much improved at 8 and 12 weeks Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.5.1 At 8 weeks | 2 | 571 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [1.10, 1.84] |
| 1.5.2 At 12 weeks | 2 | 571 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.55 [1.20, 1.99] |
| 1.6 HIV‐neuropathy ‐ at least 30% pain intensity reduction over weeks 2 to 12 Show forest plot | 2 | 801 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [1.09, 1.68] |
| 1.6.1 Using 30‐minute application | 2 | 340 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [1.14, 2.46] |
| 1.6.2 Using 60‐minute application | 2 | 359 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.84, 1.44] |
| 1.6.3 Using 90‐minute application | 1 | 102 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.94 [0.83, 4.53] |
| 1.7 Local skin reactions ‐ group 1 Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.7.1 Erythema | 4 | 1355 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [1.32, 1.54] |
| 1.7.2 Pain | 4 | 1355 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.26 [1.98, 2.59] |
| 1.7.3 Papules | 3 | 1312 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.58 [1.87, 6.85] |
| 1.7.4 Pruritus | 3 | 1312 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.99 [0.98, 4.03] |
| 1.7.5 Oedema | 3 | 1312 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.98 [1.44, 6.18] |
| 1.8 Local skin reactions ‐ group 2 Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.8.1 Erythema | 1 | 129 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.31 [0.35, 114.82] |
| 1.8.2 Pain | 4 | 1105 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.39 [1.41, 4.05] |
| 1.8.3 Papules | 3 | 735 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.58 [0.59, 4.24] |
| 1.8.4 Pruritus | 3 | 735 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.57 [0.98, 2.50] |
| 1.8.5 Oedema | 3 | 735 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [0.75, 2.39] |
| 1.9 Patch tolerability Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.9.1 < 90% of application time | 6 | 2074 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.27 [1.17, 9.15] |
| 1.9.2 Dermal irritation score > 2 at 2 hours | 3 | 1065 | Risk Ratio (M‐H, Fixed, 95% CI) | 11.80 [4.04, 34.48] |
| 1.9.3 Dermal irritation score > 0 at 2 hours | 2 | 606 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.28 [1.60, 3.26] |
| 1.9.4 Pain medication 0 to 5 days | 7 | 2442 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.52 [2.18, 2.92] |
| 1.10 Serious adverse events Show forest plot | 7 | 1993 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.70, 1.86] |
| 1.11 Withdrawals Show forest plot | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.11.1 Adverse events | 8 | 2487 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.36, 1.78] |
| 1.11.2 Lack of efficacy | 6 | 2073 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.32, 1.02] |