Cirugía de cataratas en pacientes con degeneración macular asociada a la edad
Information
- DOI:
- https://doi.org/10.1002/14651858.CD006757.pub4Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 16 February 2017see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Eyes and Vision Group
- Copyright:
-
- Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
Conceiving the review: NB
Designing the review: HC
Co‐ordinating the review: HC
Data collection for the review
-
Designing search strategies: Iris Gordon, HC
-
Undertaking searches: Iris Gordon
-
Screening search results: HC, NB, KL, IK, SS
-
Organizing retrieval of papers: HC, KL
-
Screening retrieved papers against inclusion criteria: HC, NB, KL, IK, SS
-
Appraising quality of papers: HC, KL, IK, SS
-
Extracting data from papers: HC, KL, IK, SS
-
Writing to authors of papers for additional information: HC, KL
-
Providing additional data about papers: HC, NB
-
Obtaining and screening data on unpublished studies: HC, NB
Data management for the review
-
Entering data into Review Manager 5: HC, KL
Analysis of data: HC, KL
Interpretation of data
-
Providing a methodological perspective: HC, NB, KL, IK, SS
-
Providing a clinical perspective: HC, NB, IK, SS
-
Providing a policy perspective: NB
-
Providing a consumer perspective: NB
Writing the review: HC, NB, KL
Providing general advice on the review: NB
Securing funding for the review: CEV US Project
Performing previous work that was the foundation of the current study: NB
Updating the review: HC, KL, IK, SS, NB
Sources of support
Internal sources
-
Johns Hopkins University, USA.
External sources
-
Grant 1 U01 EY020522, National Eye Institute, National Institutes of Health, USA.
-
National Institute for Health Research (NIHR), UK.
-
Richard Wormald, Co‐ordinating Editor for the Cochrane Eyes and Vision (CEV) acknowledges financial support for his CEV research sessions from the Department of Health through the award made by the NIHR to Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology for a Specialist Biomedical Research Centre for Ophthalmology.
-
The NIHR also funds the CEV editorial base in London.
The views expressed in this publication are those of the review authors and not necessarily those of the NIHR, the NHS or the Department of Health.
-
Declarations of interest
HC is retina specialist in private practice.
KL is the Project Director for the CEV US Project.
IK: None known.
SS: None known.
NB: None known.
Acknowledgements
We acknowledge Iris Gordon, Information Specialist for Cochrane Eyes and Vision (CEV), for devising and running the electronic searches. We thank Anupa Shah, the Managing Editor for CEV, as well as Jennifer Evans, Barbara Hawkins, Dayse Sena, and Gianni Virgili, for their assistance and comments.
Version history
| Published | Title | Stage | Authors | Version |
| 2017 Feb 16 | Surgery for cataracts in people with age‐related macular degeneration | Review | Heather Casparis, Kristina Lindsley, Irene C Kuo, Shameema Sikder, Neil M Bressler | |
| 2012 Jun 13 | Surgery for cataracts in people with age‐related macular degeneration | Review | Heather Casparis, Kristina Lindsley, Irene C Kuo, Shameema Sikder, Neil M Bressler | |
| 2009 Jan 21 | Surgery for cataracts in people with age‐related macular degeneration | Review | Heather Casparis, Kristina Lindsley, Neil B Bressler | |
| 2007 Oct 17 | Surgery for cataracts in people with age‐related macular degeneration | Protocol | Heather Casparis, Neil Bressler | |
Differences between protocol and review
In the protocol for this review (Casparis 2007), secondary outcomes were to be assessed at one‐, two‐, and three‐year follow‐up. As of 2012, we also assessed secondary outcomes at six months (Casparis 2012).
For this update, we included a 'Summary of findings' table and GRADE assessments in accordance with Cochrane standards.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Humans; Middle Aged;
PICOs
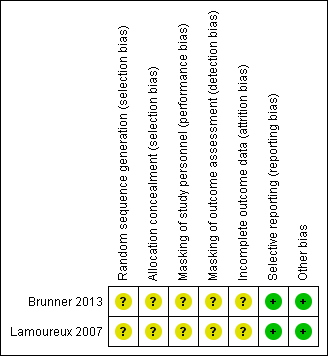
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
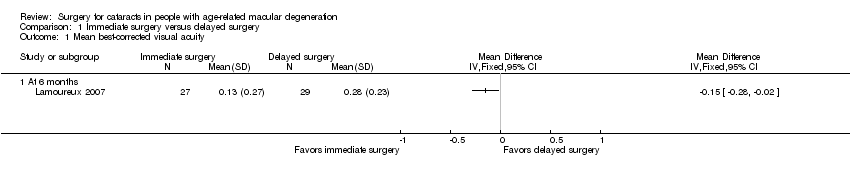
Comparison 1 Immediate surgery versus delayed surgery, Outcome 1 Mean best‐corrected visual acuity.

Comparison 1 Immediate surgery versus delayed surgery, Outcome 2 Mean change in cumulative drusen and geographic atrophy size at 12 months.
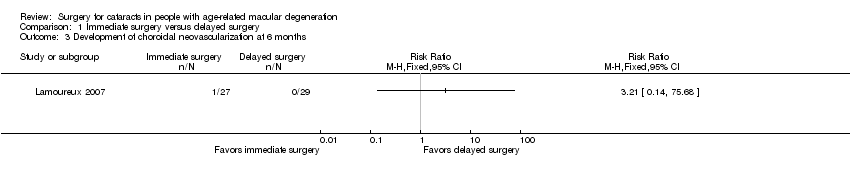
Comparison 1 Immediate surgery versus delayed surgery, Outcome 3 Development of choroidal neovascularization at 6 months.
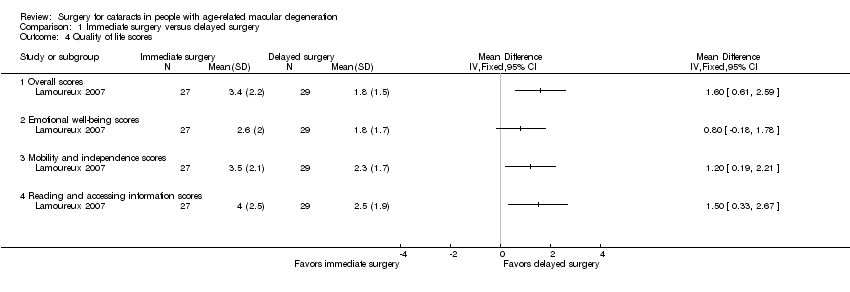
Comparison 1 Immediate surgery versus delayed surgery, Outcome 4 Quality of life scores.
| Immediate cataract surgery compared with delayed cataract surgery in eyes with age‐related macular degeneration | ||||||
| Population: people with cataract and age‐related macular degeneration Settings: ophthalmology clinics Intervention: immediate cataract surgery (within 2 weeks) Comparison: delayed cataract surgery (after 6 months) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Delayed cataract surgery | Immediate cataract surgery | |||||
| Mean best‐corrected visual acuity (BCVA) (measured on the LogMAR scale; 0 = good vision, higher scores = worse vision) | At 6 months' follow‐up | — | 56 | ⊕⊕⊕⊝ | Neither trial reported visual acuity outcomes as dichotomous or categorical outcomes. At 12 months, 1 trial reported mean distance visual acuity, but the unit of measure was not reported. | |
| Mean BCVA in the delayed‐cataract surgery group was 0.28 LogMAR units. | Mean BCVA in the immediate‐cataract surgery group was 0.15 LogMAR units lower (better) (0.28 lower to 0.02 lower). | |||||
| At 12 months' follow‐up | ||||||
| See comment | ||||||
| Mean change in cumulated drusen or geographic atrophy area size (CDGAS) | At 6 months' follow‐up | 1 trial did not report any outcome related to drusen or geographic atrophy. | ||||
| Not reported | ||||||
| At 12 months' follow‐up | — | 49 | ⊕⊕⊝⊝ | |||
| The mean change in CDGAS in the delayed‐cataract surgery group was ‐1.125 CDGAS units. | The mean change in CDGAS in the immediate‐cataract surgery group was 0.76 CDGAS units higher (8.49 lower to 10.00 higher). | |||||
| Development of choroidal neovascularization | At 6 months' follow‐up | RR 3.21 (0.14 to 75.68) | 56 | ⊕⊝⊝⊝ | At 6 months, none of 29 participants in the delayed‐cataract surgery group compared with 1 of 27 participants in the immediate‐cataract surgery group developed choroidal neovascularization. The other trial reported that no participant in either group developed exudative AMD up to 12 months' follow‐up. | |
| Not estimated (see comment) | ||||||
| At 12 months' follow‐up | ||||||
| See comment | ||||||
| Quality of life (measured by the Impact of Vision Impairment questionnaire; higher mean scores represent better quality of life in the analyses, scale of 0 to 5) | At 6 months' follow‐up | — | 56 | ⊕⊕⊝⊝ | The other trial measured quality of life using the Visual Function‐14 questionnaire to assess patient satisfaction at baseline and 12 months' follow‐up; however, no between‐group analysis of results could be performed. | |
| Mean overall score in the delayed‐cataract surgery group was 1.8. | Mean overall score in the immediate‐cataract surgery group was 1.60 higher (0.61 to 2.59 higher). | |||||
| At 12 months' follow‐up | ||||||
| See comment | ||||||
| Complications | Not reported | |||||
| *The basis for the assumed risk is the risk in the control group. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the control group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded (‐1) for unclear risks of bias such as selection bias (methods of randomization and allocation concealment not reported), performance and detection bias (effect of lack of masking on outcome unclear), and attrition bias (nine of 114 participants not included in analyses). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mean best‐corrected visual acuity Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 At 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Mean change in cumulative drusen and geographic atrophy size at 12 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Development of choroidal neovascularization at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Quality of life scores Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Overall scores | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Emotional well‐being scores | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Mobility and independence scores | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Reading and accessing information scores | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |


