Appendix stump closure during laparoscopic appendectomy
References
Additional references
Jump to:
References to other published versions of this review
Jump to:
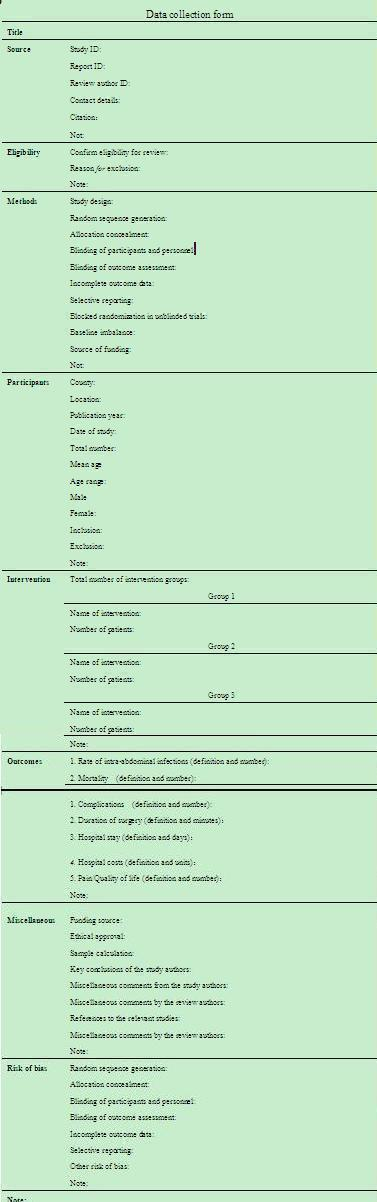
Data collection form (Microsoft Word)
| Domain | Support for judgement | Review authors’ judgement |
| Random sequence generation. | Describe the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups. | Selection bias (biased allocation to interventions) due to inadequate generation of a randomised sequence: High risk/Low risk/Unclear risk? |
| Allocation concealment. | Describe the method used to conceal the allocation sequence in sufficient detail to determine whether intervention allocations could have been foreseen in advance of, or during, enrolment. | Selection bias (biased allocation to interventions) due to inadequate concealment of allocations prior to assignment: High risk/Low risk/Unclear risk? |
| Blinding of participants and personnel. | Describe all measures used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. Provide any information relating to whether the intended blinding was effective. | Performance bias due to knowledge of the allocated interventions by participants and personnel during the study: High risk/Low risk/Unclear risk? |
| Blinding of outcome assessment. | Describe all measures used, if any, to blind outcome assessors from knowledge of which intervention a participant received. Provide any information relating to whether the intended blinding was effective. | Detection bias due to knowledge of the allocated interventions by outcome assessors: High risk/Low risk/Unclear risk? |
| Incomplete outcome data. | Describe the completeness of outcome data for each main outcome, including attrition and exclusions from the analysis. State whether attrition and exclusions were reported, the numbers in each intervention group (compared with total randomised participants), reasons for attrition/exclusions where reported, and any re‐inclusions in analyses performed by the review authors. | Attrition bias due to amount, nature or handling of incomplete outcome data: High risk/Low risk/Unclear risk? |
| Selective reporting. | State how the possibility of selective outcome reporting was examined by the review authors, and what was found. | Reporting bias due to selective outcome reporting: High risk/Low risk/Unclear risk? |
| Other sources of bias. | State any important concerns about bias not addressed in the other domains in the tool. | Bias due to problems not covered elsewhere in the table: High risk/Low risk/Unclear risk? |

