Normobaric and hyperbaric oxygen therapy for the treatment and prevention of migraine and cluster headache
Information
- DOI:
- https://doi.org/10.1002/14651858.CD005219.pub3Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 28 December 2015see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Pain, Palliative and Supportive Care Group
- Copyright:
-
- Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
MB conceived and coordinated this review, wrote to authors of papers for additional information, provided additional data about articles, and entered data into RevMan 2014.
MB and AS performed manual literature searches.
MB and JW screened the search results.
MB and AS organized retrieval of papers.
MB, AS, and CF screened retrieved papers against inclusion criteria.
MB and SW extracted data from articles, appraised the quality of included trials, performed data management, and performed double‐entry of data in this review update; MB and AS did so for Bennett 2008.
MB and AS obtained and screened data on unpublished studies. MB and AS performed statistical analyses using RevMan 2014.
MB performed statistical inferences and other statistical analysis not using RevMan 2014.
MB, AS, PK, and SW interpreted data.
AS and MB wrote the review.
NR secured funding for the review.
MB and PK performed previous work that was the foundation of this review update.
MB is guarantor for this review.
CF, JW, and PK were responsible for reading and checking this review before submission.
Sources of support
Internal sources
-
No internal source of support, Other.
External sources
-
No external source of support, Other.
Declarations of interest
Michael Bennett has no relevant conflict of interest to declare.
Christopher French has no relevant conflict of interest to declare.
Alexander Schnabel has no relevant conflict of interest to declare.
Jason Wasiak has no relevant conflict of interest to declare.
Peter Kranke has no relevant conflict of interest to declare.
Stephanie Weibel has no relevant conflict of interest to declare.
Acknowledgements
We acknowledge the support and suggestions of the Cochrane Pain, Palliative and Supportive Care review group (PaPaS), particularly Frances Fairman, Becky Gray, and Doug McCrory (PaPaS staff), and Drs Claude Piantadosi and Peer Tfelt‐Hansen (peer reviewers) for their assistance in the preparation of the original review (Bennett 2005). We gratefully received the suggestions of Sheena Derry (Pain Research, University of Oxford) in preparing this review update.
Funding: The authors have received no funding for this review.
Cochrane Review Group funding acknowledgement: The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane PaPaS Group. Disclaimer: The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, National Health Service (NHS) or the Department of Health.
Version history
| Published | Title | Stage | Authors | Version |
| 2015 Dec 28 | Normobaric and hyperbaric oxygen therapy for the treatment and prevention of migraine and cluster headache | Review | Michael H Bennett, Christopher French, Alexander Schnabel, Jason Wasiak, Peter Kranke, Stephanie Weibel | |
| 2008 Jul 16 | Normobaric and hyperbaric oxygen therapy for migraine and cluster headache | Review | Michael H Bennett, Christopher French, Alexander Schnabel, Jason Wasiak, Peter Kranke | |
| 2005 Apr 20 | Normobaric and hyperbaric oxygen therapy for migraine and cluster headache | Protocol | Michael H Bennett, Christopher French, Peter Kranke, Alexander Schnabel, Jason Wasiak | |
Differences between protocol and review
For this 2015 update, we added an author (SW) and two new trials (Cohen 2009; Ozkurt 2012). We have also amended the title from 'Normobaric and hyperbaric oxygen therapy for migraine and cluster headache' to 'Normobaric and hyperbaric oxygen therapy for the treatment and prevention of migraine and cluster headache' for clarity.
We have formulated a summary of findings Table for the main comparison and estimated the quality of the evidence using the GRADE Pro Guideline Development Tool software and methodology (GRADEPro GDT 2015) .
Notes
The authors and editors have agreed that this review will be assessed for further updating in 2020. It is unlikely that new evidence will be published that has the potential to change the conclusions.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Humans;
PICOs

'Risk of bias' graph: each 'Risk of bias' item presented as percentages across all included studies.
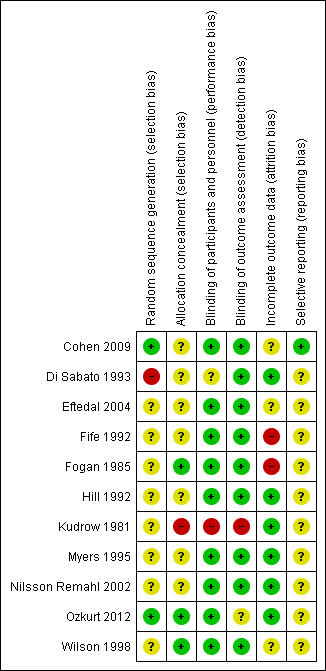
'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included study.
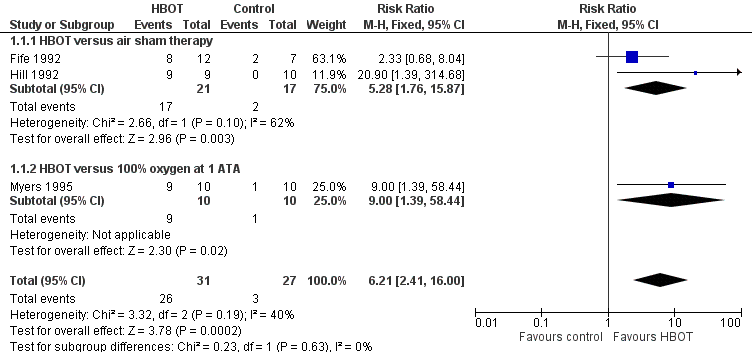
Forest plot of comparison: 1 HBOT versus control for acute migraine attack, outcome: 1.1 Substantial acute relief of headache.

Comparison 1 HBOT versus control for acute migraine attack, Outcome 1 Substantial acute relief of headache.
| Hyperbaric oxygen therapy for the relief of acute migraine | ||||||
| Patient or population: Acute migraine | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk with sham therapy | Risk with HBOT | |||||
| Chance of obtaining substantial headache relief (Relief). | Study population | RR 6.21 | 58 | Low¹ | We included 3 small RCTs but all showed large effect size with HBOT compared to either air or 100% oxygen sham. | |
| 111 per 1000 | 663 per 1000 | |||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| ¹The evidence has been downgraded from moderate to low due to two of these trials being incompletely reported crossover trials reported only in abstract. [Two of the three included studies were planned as crossover trials. In those two, many patients obtained relief during the first treatment period and were not crossed to the second period. For Hill 1992, where all patients are not clearly accounted for we have included the results only from the first treatment period.] | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Substantial acute relief of headache Show forest plot | 3 | 58 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.21 [2.41, 16.00] |
| 1.1 HBOT versus air sham therapy | 2 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.28 [1.76, 15.87] |
| 1.2 HBOT versus 100% oxygen at 1 ATA | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 9.0 [1.39, 58.44] |


