Intervenciones para la prevención de embarazos no deseados en adolescentes
References
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias adicionales
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Jump to:
| Methods | Cluster‐randomis ed controlled study; method of generating allocation sequence not mentioned in the paper | |
| Participants | 582 students who enrolled in the 7th grade at the beginning of the study; enrolled in the 8th grade at the beginning of the 1996/1997 session; capable of reading and comprehending the questionnaire in English or Spanish; not truant or suspended during the trial; mean age of 12.8 years; 52% female and 48% male; 84% African American, 13% Hispanic, 2% other, low socio‐economic status | |
| Interventions | Intervention: t hree 45‐ minute reproductive health education classes by health professionals, five 45‐ minute sessions on postponing sexual involvement by peer leaders in 10th and 11th grades, health risk assessment questionnaire Control: conventional education programme | |
| Outcomes | Initiation of intercourse (age at initiation), use of birth control/condoms at last sex | |
| Notes | Duration of follow up: 15 months. Loss to follow up: 19% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method used for allocation sequence generation not provided |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Unclear risk | Did not control for cluster randomi sation during the analysis |
| Methods | Randomis ed controlled trial. Randomis ation was done at two levels; student (75% of sample) by picking names out of a hat or choosing every other name on an alphabetis ed list, and classroom (25% of sample) by a coin toss | |
| Participants | 695 students from 25 sites in the United States, 9th grade to 12th grade, mean age of 15.8 years, 85% female and 15% male; 67% African American, 19% White, 11% Hispanic and 3% other | |
| Interventions | Intervention: 20 hours per year of supervised community volunteer services and one hour per week of classroom‐ based discussion of service experiences, future life options, developmental tasks of adolescents and sex education Control: standard curriculum offerings | |
| Outcomes | Unintended pregnancy (women only) | |
| Notes | Duration of follow up: nine months Loss to follow up: 7.0% lost to follow up (5.3% among experimental students and 8.4% among control students) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Picking names out of a hat (for individual) or coin toss (for classrooms) |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | No information provided on this domain |
| Incomplete outcome data (attrition bias) | Unclear risk | Three sites were excluded from analysis. Higher attrition rate in the control groups. There were some differences between students lost and those retained in that students lost were more likely to have had or caused a prior pregnancy, been suspended, be younger and be male. |
| Selective reporting (reporting bias) | Low risk | Pre‐specifed outcomes were reported |
| Other bias | Low risk | The study appears to be free from other bias |
| Methods | Cluster ‐ randomis ed controlled trial; randomis ation was done using Enumeration Areas (EAs). | |
| Participants | Young women aged 12 years to 22 years and not married | |
| Interventions | Intervention: conditional cash transfer (CCT) as an incentive for school girls and young women to stay or return to school Control: no CCT provided | |
| Outcomes | Pregnancy, sexual behaviour (onset of sexual activity, number of sexual partners in the past 12 months, condom use, frequency of sexual activity) | |
| Notes | Duration of follow up: 12 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information on this domain was not provided |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | Attrition rate was low and balanced across treatment and control groups |
| Selective reporting (reporting bias) | Unclear risk | Outcomes to be measured were not clearly listed in the methods |
| Other bias | Unclear risk | Baseline differences between dropouts and school girls (dropouts were older, less literate and more likely to have started childbearing) |
| Methods | Cluster‐randomis ed controlled study. Method of generating allocation sequence not mentioned in the paper Unit of randomis ation: schools | |
| Participants | 7614, 8319 and 9489 9 (at baseline, 19 and 31 months); grade 9 to 12 students in schools in California and Texas, 47% male, 53% female, 18% African American, 17% Asian, 33% Hispanic, 27% White, 5% other | |
| Interventions | Intervention: 20 sessions of health education, skills‐ building, contraceptive education, social norms and peer education, parent education, community linkages Control: standard knowledge‐ based curriculum on contraception, HIV and other STDs | |
| Outcomes | Initiation of intercourse, contraception use | |
| Notes | Duration of follow up: 31 months Loss to follow up: not clear | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information on attrition/exclusion to permit judgement as number of participants in the study increased with each follow up. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Unclear risk | The sampling methods for including students not clear |
| Methods | Randomis ed controlled study. Method of allocation sequence not mentioned. Unit of randomis ation: individual | |
| Participants | 181 adolescent mothers in urban hospitals who were living with their mother, 13.5 years to 17.9 years at delivery, first‐time delivery, Black, no history of drugs, infants should be 37 weeks and birth weight of > 2500 g with no congenital problems, chronic illnesses, or disabilities. | |
| Interventions | Intervention: home mentoring programme (home visits every week until infant's first birthday, approximately 19 visits) Control: no intervention | |
| Outcomes | Second unintended pregnancy | |
| Notes | Duration of follow up: 24 months Loss to follow up: 18% Evaluators were blinded to intervention status | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Low risk | Evaluators only |
| Incomplete outcome data (attrition bias) | High risk | Only participants with both baseline and 24‐months' data were included in the analysis. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other bias |
| Methods | Cluster‐randomis ed controlled study. Quarterly marking period within schools was used to generate allocation sequence Unit of randomis ation: schools | |
| Participants | 351 8th grade students in Rochester, New York living in middle class suburban communities, 48% female and 52% male. 85% were white and non‐Hispanic. | |
| Interventions | Intervention: enhanced intervention; five one‐hour sessions on standard school‐ based curriculum ( health education; skills‐ building; abstinence; communication skills) plus five parent‐child homework assignments on sexuality and sexual behaviour led by trained youth leaders Control: standard school‐ based curriculum only | |
| Outcomes | Initiation of intercourse, knowledge on the risk of pregnancy | |
| Notes | Duration of follow up: seven weeks. No mention of loss to follow up | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quarterly marking period within schools |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | Only those who completed pre‐test and post‐test questionnaires were analys ed at baseline and end of the study. Analysis adjusted for clusters |
| Selective reporting (reporting bias) | Low risk | Pre‐stated outcomes were reported |
| Other bias | High risk | Selection bias as the proportion of students who had completed no assignments was higher among Black and Hi spanic adolescents than among non‐Hispanic White students (43% vs 18%; P < 0.05); higher among male than female students (27% vs 9%; P < 0.01) and was higher among adolescents who reported recent sexual intercourse than among those who did not (63% vs 17%; P < 0.001) |
| Methods | Matched‐pair individual‐allocation randomi sed trial. | |
| Participants | Girls aged 13 years to 15 years | |
| Interventions | Intervention: weekly three‐hour sessions in pre‐school nuseries to develop awareness of the responsibility involved in parenting, self‐awareness and confidence to reduce risk of teenage pregnancy, other issues addressed include self‐esteem and sense of control, emotional literacy and social skills, teenage sex, sexual health and consequences of unplanned pregnancy Control: not stated | |
| Outcomes | Last sex without contraception in the last three months, more than one episode of sex without contraception in the last three months, new pregnancy since baseline, last sex without condom in the last three months, more than one episode of sex without condom in the last three months | |
| Notes | Duration of follow up: 22 weeks and 12 months Loss to follow up; 9% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐ generated random number |
| Allocation concealment (selection bias) | Unclear risk | Children: Our Ultimate Investment (COUI) and school staff were blinded to allocation; however, neither intervention teachers, nor girls nor analyst were blinded to allocation status |
| Blinding (performance bias and detection bias) | High risk | Teachers and girls were not blinded to allocation status |
| Incomplete outcome data (attrition bias) | Low risk | Few number of participants lost to follow up; intention‐ to‐ treat analysis was employed |
| Selective reporting (reporting bias) | High risk | Pregnancy was based on self‐reporting |
| Other bias | Unclear risk | The study appears to be free from other bias |
| Methods | Cluster‐randomis ed controlled study. Method of allocation concealment not mentioned. Unit of randomization: schools | |
| Participants | 1295 students from 18 high schools in Rome, 51% male, 49% female, mean age 18.3 years | |
| Interventions | Intervention: HIV/AIDS education and skills‐ building by peer Control: same intervention by teachers | |
| Outcomes | Consistent condom use | |
| Notes | Duration of follow up: 5 months Loss to follow up: 20% for peer‐led group and 27% teacher‐led group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | Trial authors stated they used an intention‐to‐treat analysis, whereby classes which did not perform the interventions were included in the outcome evaluation. Analysis adjusted for clusters |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Cluster‐randomis ed controlled trial. Classrooms were randomised by blindly, taking letters of the class from a bag (simple balloting) Unit of randomis ation: classrooms | |
| Participants | 1259 9th grade female students in San Bernardo, Chile, aged 15 years to 16 years, White Hispanic, who had initiated high school in 1997 and 1998. | |
| Interventions | Intervention: one 45‐ minute class per week for a year on health education, contraceptive education, skills‐ building and abstinence Control: no intervention | |
| Outcomes | Unintended pregnancy | |
| Notes | Duration of follow up: 4 years Loss to follow up: 19% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple balloting (blindly taking letters from a bag) |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | Per‐ protocol analysis was carried out but missing outcome data balanced in numbers across intervention groups with similar reasons for missing data across groups (change of residence and financial problems) |
| Selective reporting (reporting bias) | Low risk | Stated outcomes were measured |
| Other bias | Low risk | The study appears to be free from other bias |
| Methods | Cluster‐randomis ed controlled study. Method of allocation sequence not mentioned Unit of randomis ation: class | |
| Participants | 211 African American 7th grade students, 11 years to 14 years of age, 55% male, 45% female, low income | |
| Interventions | Intervention: 10 sessions (once or twice per week for six weeks) on skills‐ building and career mentoring Control: standard health curriculum | |
| Outcomes | Initiation of intercourse | |
| Notes | Duration of follow up: 1 year Loss to follow up: 26% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Unclear risk | Only participant, the provided baseline, and end of study information were included in the one‐ year follow‐ up analysis |
| Selective reporting (reporting bias) | Low risk | Stated outcome reported |
| Other bias | Unclear risk | The study appears to be free from other sources of bias |
| Methods | Cluster‐randomis ed controlled study. Method of allocation sequence not mentioned in this study Unit of randomis ation: schools | |
| Participants | 3869 9th grade students from 20 urban high schools in Texas and California, mean age 15 years, 53% female and 47% male; 31% White, 27% Hispanic, 18% Asian or Pacific Islanders, 16% African‐American, < 1% African Indian, 7% other | |
| Interventions | Intervention: 20 sessions on health education, skills‐ building, contraceptive education, parent education, community linkages Control: standard knowledge‐ based HIV‐ prevention curriculum | |
| Outcomes | Initiation of intercourse, use of contraceptive at last sex | |
| Notes | Duration of follow up: 7 months Loss to follow up: 3% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | Whereas only those with data at baseline and at follow up were included in the analysis, there were no differences in the sexual behaviours between those lost to follow up and those who remained in the study across groups. |
| Selective reporting (reporting bias) | Low risk | Stated outcomes reported |
| Other bias | Low risk | Appears to be free from other bias |
| Methods | Randomis ed controlled study. Method of generating allocation sequence not mentioned in the paper Unit of randomis ation: schools | |
| Participants | 2829 6th grade students with an average age of 11.5 years from 19 schools in Northern California; 50% female and 50% male; 5.2% African American, 15.9% Asian, 59.3% Hispanic 16.5% White and 3.1% Other. | |
| Interventions | Intervention: 20‐ session curriculum ( five lessons in 6th grade on skills‐ building in non‐sexual situations, eight lessons in 7th grade on determining personal limits in intercourse, understanding consequences of unplanned sexual intercourse (including pregnancy and STD), skills‐ building, seven lessons in 8th grade on contraception education, HIV‐infected speaker and refusal skills in dating) Control: standard curriculum | |
| Outcomes | Initiation of intercourse | |
| Notes | Duration of follow up: 36 months; lost to follow up: 36% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | High risk | High attrition rate among participants |
| Selective reporting (reporting bias) | Low risk | Pre‐stated outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Cluster‐randomi sed controlled study. Method of generation of allocation was done using restricted randomi sation into matched sets. Unit of randomi sation: schools | |
| Participants | 988 students, 14 years to 18 years or older, in community day schools located in four urban counties in Northern California, 63% male, 37% female, 27% African American, 15% Asian American, 30% Hispanic, 12% White, 16% other | |
| Interventions | Intervention: 14 sessions (26 hrs) on HIV/STDs/ pregnancy education, skills‐ building, risks related to sexual behaviour, contraception education and service learning activities ( five visits to volunteer sites) Control: usual curriculum | |
| Outcomes | Unintended pregnancy, initiation of intercourse, use of contraceptives and condoms at last sex | |
| Notes | Duration of follow up: 18 months Loss to follow up: 58% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Restricted randomis ation into matched set |
| Allocation concealment (selection bias) | Unclear risk | No information provided on this domain |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | All students were included in the analysis regardless of programme dose. No statistically significant difference was found in the rates of attrition across groups |
| Selective reporting (reporting bias) | Low risk | All expected/stated outcomes reported |
| Other bias | Low risk | The study seems to be free from other bias |
| Methods | Randomis ed controlled study. Table of random numbers was used to generate allocation sequence. Unit of randomi sation: individual | |
| Participants | 522 female participants between the ages of 14 years to 18 years in four community health agencies in southern United States, African American, reporting vaginal intercourse in the preceding six months. | |
| Interventions | Intervention: four‐hour interactive group sessions on ethnic and gender pride, health/HIV education, skills‐ building and contraception education Control: four‐hour interactive group sessions on general health promotion condition (exercise and nutrition) | |
| Outcomes | Unintended pregnancy, consistent condom use and sexually transmitted disease | |
| Notes | Duration of follow up: 12 months. Loss to follow up: 12% (12.7% for intervention and 11.1% for the control). Assessors were blinded to participants' condition assignments. Allocation concealed in opaque envelopes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers |
| Allocation concealment (selection bias) | Low risk | Use of sealed opaque envelopes |
| Blinding (performance bias and detection bias) | Low risk | Assessors were blinded |
| Incomplete outcome data (attrition bias) | Low risk | Participants were analys ed in their groups irrespective of number of sessions attended. Missing outcome data balanced in numbers with similar reasons for missing data across groups |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Randomis ed controlled study. Computer‐generated random numbers used to generate allocation sequence. Unit of randomi sation: sites | |
| Participants | 582 adolescents from a community‐ based organi sation and their mothers, 11 years to 14 years, 60% male, 40% female, 98% African American | |
| Interventions | Intervention 1: seven sessions ( two hours) over 14 weeks ( four sessions for mother and adolescents together) on HIV education, communication skills, take‐ home activities and sexual decision making, consequences of early sexual intercourse Intervention 2: stress reduction exercise and specific type of at‐risk behaviours including early sexual intercourse, take‐ home assignments and community service (mothers and adolescents attended the first and last sessions together) Control: mothers and adolescents had a one‐hour HIV prevention session | |
| Outcomes | Condom use at last sex among participants who have ever had sex | |
| Notes | Duration of follow up: 24months. Loss to follow up: 10% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | Trial authors stated the use of intention‐ to‐ treat analysis; for the use of condoms, only respondents who indicated being sexually active were included in the analysis |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Randomis ed controlled study. Method for generating allocation sequence not mentioned in the paper Unit of randomi sation: sites | |
| Participants | 277 adolescent boys from seven sites in Atlanta, 11 years to 14 years, 96% African American | |
| Interventions | Intervention: seven two‐hour sessions, 6th session for fathers of participants only, and the last session for both on communication, parental monitoring and relationship with peers, HIV/AIDS education Control: seven sessions on nutrition and exercise | |
| Outcomes | Ever had sex without a condom among participants who have ever had sex | |
| Notes | Duration of follow up: 12 months Loss to follow up: 20% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method on allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | Intent‐to‐treat analysis carried out. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Randomis ed controlled study. Table of random numbers was used to generate the allocation sequence. Unit of randomis ation: individuals | |
| Participants | 300 female part icipants from four urban Pittsburgh area healthcare sites, who were aged 14 years to 18 years and had reported heterosexual vaginal sexual activity in the previous six months, 75% were African American, 15% Whites and 10% other or mixed race | |
| Interventions | Intervention: interactive video intervention on reproductive health/STD education, skills‐ building and contraceptive education delivered for 30 minutes at baseline and 15 minutes on each follow up visit Control 1: content‐matched control (same intervention in a book form) Control 2: topic‐matched control (same intervention using commercially available brochures) | |
| Outcomes | Unintended pregnancy, use of condoms, sexually transmitted disease | |
| Notes | Duration of follow up: 6 months Loss to follow up: 14% Individuals were randomised to one of the three groups ( interactive video intervention, content‐matched control and topic‐matched control) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | High risk | Only participants who provided data at six months were included in the analysis |
| Selective reporting (reporting bias) | High risk | Pre‐specifed outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Randomis ed controlled multicentre study. Method used to generate allocation sequence not mentioned in the paper Unit of randomi sation: individual and classroom | |
| Participants | 1444 8th to 9th grade students from six family planning agencies and one school in Texas and California; mean age 15.5 years; 52% female, 48% male; 15% White, 24% African‐American, 53% Hispanic and 8% Asian | |
| Interventions | Intervention: 12 hours to 15 hours on health education (reproductive biology), skills‐ building, contraceptive/STD education Control: usual sex education programmes which varied among sites | |
| Outcomes | Initiation of intercourse, consistent use of contraceptives | |
| Notes | Duration of follow up: one year Loss to follow up: 39% Randomis ation was done individually or by classroom units (71% by classroom and 29% by individual) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to assess this domain |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Cluster‐randomis ed controlled trial. Method used to generate allocation not mentioned in the paper. Unit of randomi sation: classrooms | |
| Participants | 450 students from 11 mixed‐sex public schools in Ibadan, Nigeria; mostly Yoruba; 55.2% female, 44.9% male. Low socioeconomic status | |
| Interventions | Intervention: six weekly (each lasted between two hours and six hours) of AIDS/HIV education, health education and contraceptive education Control: standard curriculum | |
| Outcomes | Initiation of intercourse, use of condoms at last sex, consistent use of condom, sexually transmitted disease | |
| Notes | Duration of follow up: 6 months Loss to follow up: 3.8% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | Participants lost to follow up were less than 5% of the total participants included in the study |
| Selective reporting (reporting bias) | Low risk | all pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Cluster‐randomis ed controlled study. Coin toss technique was used to generate allocation sequence | |
| Participants | 63 female African American students aged 12 years to 16 years who completed the Camp Horizon Adolescent Pregnancy Prevention Program, residing in one of the four public housing developments in Charlottesville, Virginia, not currently pregnant, had never given birth, 5th grade to 10th grade, low income | |
| Interventions | Intervention: two hours per week for eight weeks on health education, skills ‐building, contraceptive education, abstinence, ethnic/cultural values, family options, career counselling by peer counsellors | |
| Outcomes | Unintended pregnancy, initiation of intercourse, use of contraceptive at last sex | |
| Notes | Duration of follow up: 3 months. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Tossing a coin |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | High risk | Imbalance in numbers los t to follow up across intervention groups and reasons not stated. Per‐protocol analysis done with substantial departure from one of the groups |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Unclear risk | Baseline differences not reported |
| Methods | Cluster‐randomi sed controlled study. Computer‐ generated random numbers used to generate allocation sequence. Unit of randomis ation: schools | |
| Participants | 3794 adolescents from secondary schools in Avon, UK , 14 years to 15 years, 52% male, 48% female | |
| Interventions | Intervention: contraception (emergency contraceptives) education Control: usual sex education | |
| Outcomes | Use of contraceptives, initiation of intercourse | |
| Notes | Duration of follow up: 6 months Loss to follow up: 18% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐ generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | No information provided on this domain |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | High risk | Attrition rate > 10% |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Randomis ed controlled trial. Dyads (mothers and their adolescents) were randomly assigned. Method of randomis ation was not stated | |
| Participants | 2016 adolescents aged 11 years to 14 years, either African American or Hispanic, and accompanied to the clinic by a resident mother | |
| Interventions | Intervention: mothers met with a social work interventionist for 30 minutes and were then given a packet containing reference materials and family activities (teaching parent effective communication and parenting strategies for reducing sexual risk, communication aids) to implement with their daughter at home. They also received two booster calls as a reminder to implement materials. Control: mothers met with their adolescent's healthcare provider only at the clinic | |
| Outcomes | Vaginal sexual intercourse, frequency of sexual intercourse in the past 30 days and oral sex | |
| Notes | Duration of follow up: 9 months loss to follow up: 5.4% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information on this domain was not provided |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | High retention rate (98.6%) |
| Selective reporting (reporting bias) | Low risk | Reported stated outcome |
| Other bias | Unclear risk | There was no way of assessing if mothers did implement the intervention at home |
| Methods | Cluster‐randomis ed controlled study. Method used to generate allocation sequence not mentioned in the paper. Unit of randomis ation: schools | |
| Participants | 4196 female students in secondary schools in Scotland, 13 years to 15 years, | |
| Interventions | Intervention: SHARE (20 session package: 10 for 3rd year and 10 for 4th years of secondary school respectively) on health/sex education, skills‐ building, contraceptive education primarily through the use of interactive video. Control: conventional sex education | |
| Outcomes | Childbirth and abortion | |
| Notes | Duration of follow up: 4.5 years Loss to follow up: 0.5% One of the control schools demonstrated how to handle condoms (one of the lesson included in the intervention group). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information on this domain was not provided |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | Minimal participants lost to follow up (0.5%) |
| Selective reporting (reporting bias) | Low risk | Primary outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Randomis ed controlled study. Method used to generate allocation sequence was not mentioned in the paper. Unit of randomis ation:i Individual | |
| Participants | 417 female adolescents aged 12 years to 17 years from nine family planning clinics in Philadelphia, making their first visit to the clinics, residing in the area and with a family member. 53% African American, 47% White | |
| Interventions | Intervention 1: Family Support Group ( regular clinic services plus 50 minutes of family or individualis ed counselling services on sex and contraceptive education for six weeks) Intervention 2: Periodic Support Group ( regular clinic services plus staff supports through two to six telephone calls four to six weeks after initial clinic visit, to monitor teenage adjustment to the contraceptive received at the clinic) Control Group A and B: regular clinic services | |
| Outcomes | Unintended pregnancy and consistent use of contraceptives | |
| Notes | Duration of follow up: 15 months. Loss to follow up: 14% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Allocation sequence generation not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | High risk | The number of people assessed in each group was not clearly stated |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported |
| Other bias | Unclear risk | High rate of non‐compliance among participants randomis ed to the intervention |
| Methods | Cluster‐randomi sed controlled study. Method used to generate allocation sequence not mentioned in the paper | |
| Participants | 536 low‐ income minority students from 53 schools in Atlanta, 99% Black, 8th grade to 9th grade | |
| Interventions | Intervention: five sessions on health/STD education, skills‐ building, contraceptive education (first four sessions given fairly close together ‐ four classroom periods in a week or one each week for four weeks; the fifth session given one to three months later) | |
| Outcomes | Unintended pregnancy, initiation of intercourse | |
| Notes | Duration of follow up: 2 years | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Unclear risk | Information on this domain was not provided |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Randomis ed controlled study. Computer‐ generated random number was used to generate the allocation sequence Unit of randomis ation: individual | |
| Participants | 659 African American students in 6th to 7th grade from three middle schools serving low‐income African American communities in Philadelphia, PA.; mean age of 11.8 years; 53% female and 47% male. | |
| Interventions | Intervention 1: eight 1‐hour modules over two consecutive Saturdays on abstinence HIV intervention (health education, skills‐ building, contraception education with emphasis on abstinence) Intervention 2: eight 1‐hour modules over two consecutive Saturdays on safer sex HIV intervention (health education, skills‐ building, abstinence with emphasis on the use of contraceptives) Control: health issues unrelated to sexual behaviour Each intervention consisted of eight 1‐hour modules divided equally over two consecutive Saturdays | |
| Outcomes | Initiation of intercourse, consistent condom use ( sexual intercourse in past three months among all participants) | |
| Notes | Duration of follow up: 12 months Loss to follow up: 7.4% Individuals were randomly allocated to one of the three conditions (abstinence HIV intervention, safer sex HIV intervention and control) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐ generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Low risk | Proctors were blinded to participants' intervention group |
| Incomplete outcome data (attrition bias) | Unclear risk | Per‐protocol analys es were carried out, included only patient present at the end of the study regardless of the number of intervention sessions attended |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Cluster‐randomis ed controlled study. Computer‐generated random numbers were used to generate allocation sequence. Unit of randomis ation: schools | |
| Participants | 682 sexually experienced adolescent girls of a children's hospital, mean age 15.5 years, 68% African American, 32% Hispanic, low income | |
| Interventions | Intervention 1: HIV/STD education, contraceptive education Intervention 2: skills‐ building, HIV/STD education, contraceptive education Control: health promotion intervention | |
| Outcomes | Sexually transmitted diseases | |
| Notes | Duration of follow up: 12 months Loss to follow up: 11.4% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐ generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | Attrition was low (11.4%) and did not differ by condition |
| Selective reporting (reporting bias) | Low risk | Pre‐stated outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Cluster‐ randomi sed controlled trial using blocked (4 to 8 in size) computer‐generated random number sequences; unit of randomis ation: community‐ based organis ations (CBOs) in a 2 x 3 factorial design to the HIV/STD risk‐reduction intervention or control and to one of the three levels of facilitator training (manual only, standard training and enhanced training) | |
| Participants | 1707 adolescents aged 13 years to 18 years who read, wrote and spoke English with written parental or guardian consent in English or Spanish. Over 80% of the participants w ere Black or African American and half of the participants were female | |
| Interventions | Intervention: six 50‐ minute modules of developmentally appropriate interactive activities, films, small group discussions, experimental exercises and role‐play activities. Information provided included the aetiology, detection, transmission, prevention and possibilities of asymptomatic infection, attitudes toward condom use, skill and self‐efficacy in using condoms. It also teaches abstinence as the most effective way to prevent STDs Manual only: intervention package and no training Standard training: intervention package and two days' training Enhanced training: intervention package, two days' standard training and practice implementation of the intervention with group of adolescents Control: health promotion which focused on reducing behaviours linked to risk for heart disease, hypertension, lung disease and cancer | |
| Outcomes | Self‐reported consistent condom use in the previous three months, proportion of condom‐protected sex, frequency of sex in the past three months, condom use at most recent sex | |
| Notes | Duration of follow up: 3, 6 and 12 months; analysis on condoms and contraceptives were limited to those who were sexually active loss to follow up: 21.3% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number sequence |
| Allocation concealment (selection bias) | Low risk | Facilitators were not aware of which group were in the follow‐up sample and participants were blinded to intervention prior to enrolment |
| Blinding (performance bias and detection bias) | Low risk | Data collectors were blind to the participant's intervention |
| Incomplete outcome data (attrition bias) | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | High risk | Selection bias likely with respect to high decline from CBOs that support abstinence |
| Methods | Cluster‐randomised controlled trial. Method used to generate allocation sequence not mentioned in the paper. Unit of randomis ation: classrooms | |
| Participants | 1657 7th grade students from six schools in California, mean age of 12.3 years; 54% female and 46% male; 64% Hispanic, 13% Asian, 9% African American, 5% non‐ Hispanic , low socio‐economic status | |
| Interventions | Intervention: eight sessions for two weeks on health education, skills ‐building, contraceptive education, risks and consequences of teen sex and community resources Control: standard curriculum | |
| Outcomes | Unintended pregnancy, initiation of intercourse, use of condoms at last sex, sexually transmitted diseases | |
| Notes | Duration of follow up: 17 months; loss to follow up: 23% Subset of patients was assessed for certain outcomes such as initiation of intercourse (only students who had never had sex at pre‐test were analys ed); likewise pregnancy and Sexually Transmitted Diseases (STD) (included in the analysis only students who had never been pregnant or never had an STD respectively) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided. Authors simply stated "randomly assigned" |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Unclear risk | High attrition |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Randomis ed controlled study. Method of allocation sequence not mentioned in this paper Unit of randomi sation: schools, agency, classroom, individual | |
| Participants | 10,600 youths in 7th grade and 8th grade (mean age of 12.8 years) from schools and community‐based organi sations in California; 58% female and 42% male; 31% Hispanic, 38% White, 9% African‐American | |
| Interventions | Intervention 1: adult‐led intervention ( five sessions, 45‐50 minutes in length, delivered in classrooms or small group settings on health education, skills‐ building, contraceptive education) in addition to the available standard sexuality curriculum, taught by adults Intervention 2: youth‐led intervention (same intervention taught by peers) Control: standard sexuality curriculum | |
| Outcomes | Unintended pregnancy, initiation of intercourse, use of condoms, use of hormonal contraceptive, sexually transmitted diseases | |
| Notes | Duration of follow up: 17 months Loss to follow up: 17% Five randomis ations were reported (random assignment by classroom to adult‐led intervention, by classroom to youth‐led intervention, by school to adult‐led intervention, by individual to adult‐led intervention, and control) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Unclear risk | High attrition rate |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Unclear risk | The study appears to be free from other sources of bias |
| Methods | Cluster‐randomis ed controlled study. Method used to generate allocation sequence not mentioned in the paper. Unit of randomis ation: schools | |
| Participants | 3869 9th grade students from 20 urban high schools in Texas and California who completed the baseline survey in autumn 1993 and officially enrolled at first follow up (spring 1994), mean age 15 years, 53% female and 47% male; 30% White, 27% Hispanic, 18% Asian or Pacific Islanders, 17% Black and 7% other Exclusion: students who left the school during the 1993 to 1994 school year | |
| Interventions | Intervention: 20 sessions on health education, skills‐ building, contraceptive education, community linkages Control: standard knowledge‐ based HIV prevention curriculum | |
| Outcomes | Initiation of intercourse, use of contraceptive at last sex | |
| Notes | Duration of follow up: 31 months Loss to follow up: 21% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Unclear risk | Analysis was carried out on the number of students' observations for each outcomes. |
| Selective reporting (reporting bias) | Low risk | Pre‐stated outcomes we re reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Randomis ed controlled study; families were randomly assigned | |
| Participants | 506 African Americans aged 16 years, with 51% female | |
| Interventions | Intervention: Strong African American Families Teen (SAAF‐T) programme: a family‐ centred intervention made up of five sessions on optimal parenting, preparation for life after high school, content on sexual health, and an optional condom skills unit Control: family‐ centred intervention but designed to promote healthful behaviours (good nutrition, exercise, and informed consumer behaviour) | |
| Outcomes | Unprotected intercourse in the past three months, condom efficacy | |
| Notes | Duration of follow up: 5 and 22 months Loss to follow up: 5% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | Low attrition rate |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Three‐ armed randomis ed controlled trial, schools were randomis ed using a multi‐attribute randomis ation protocol | |
| Participants | 1258 students; 75% of students were classified as economically disadvantaged, 59.8% female, 39.3% African American and 48.4% Hispanic with a mean age of 12.6 years | |
| Interventions | Intervention 1 (Risk Avoidance): interactive skills‐training exercises, peer role model videos, emphasis ed interactions between personal, environmental and behavioral influences, beliefs and normative beliefs. it also included homework to facilitate parent‐child communication, incorporating elements of character development and future orientation. It was framed to reinforce abstinence‐until‐marriage beliefs Intervention 2 (Risk Reduction): contained similar activities as Risk Avoidance but reinforced abstinence‐until‐older beliefs. In addition, it promoted self‐resect and responsibility, activities addressing knowledge and self‐efficacy regarding condom and contraceptive use Control: regular health classes offered by the respective schools | |
| Outcomes | Sexual initiation (for virgins only), unprotected sex at last vaginal intercourse, frequency of sex in the past three months, frequency of sex without a condom in the past three months, number of lifetime sexual partners, number of sexual partners in the past three months | |
| Notes | Duration of follow up: 16 and 26 months Loss to follow up: 25%. In addition, 75 students were excluded because of missing or inconsistent responses | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomi sation not clearly explained |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Unclear risk | Sample sizes for each outcome varied due to missing data |
| Selective reporting (reporting bias) | Low risk | Pre‐stated outcomes reported |
| Other bias | Unclear risk | The presence of baseline imbalances in demographics and sexual behaviour between conditions |
| Methods | Randomis ed controlled study. Unit of randomisation: individuals; method of randomis ation was not stated | |
| Participants | 360 students aged 10 years to 20 years, all African | |
| Interventions | Intervention: reproductive health education on STDs, HIV/AIDS and family planning Control: no education or intervention | |
| Outcomes | Correct knowledge about STD (control measures), HIV/AIDS (transmission and cure) and family planning (methods and usage) | |
| Notes | Duration of follow up: 6 weeks Loss to follow up: None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Schools were selected using a basket method of random sampling, while students were selected using a systematic sampling method (every ninth student on the school register) |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | Due to the short duration in follow up, no participants were lost and there were no missing outcome data |
| Selective reporting (reporting bias) | Low risk | All stated outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Cluster‐ randomis ed study; social networks were randomi sed; method of randomis ation not stated but both participants and research interviewers were blinded to the assignment | |
| Participants | 162 youths , male and female, aged 16 years to 21 years (median age 16.8) who were Hispanic, residing in San Francisco, spoke English or Spanish, were not pregnant or parenting | |
| Interventions | Intervention: eight life skills sessions (communication and relationship‐ building skills) promoting sexual health with a focus on STI and unintended pregnancy prevention and early childbearing norms; job training, reproductive health wellness (such as clinic visit), cash payment to youth on completion of a given activity Control: standard community services | |
| Outcomes | Childbearing expectations, STIs, contraceptive self‐efficacy and motivation | |
| Notes | Duration of follow up: 6 months loss to follow up: 8% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information on this domain was not provided |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Low risk | Both participants and research interviewers were blinded to the assignment |
| Incomplete outcome data (attrition bias) | Unclear risk | Attrition rate < 10%, baseline differences between participants adherent to the intervention compared to those who did not participate or participated minimally with regards to risky behaviours (lower proportion had ever had sex (< 0.01), gang‐affiliated close friends (< 0.05) and used alcohol frequently (< 0.01) |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Cluster‐ randomised controlled trial. Table of random numbers was used to generate allocation sequence Unit of randomis ation: schools | |
| Participants | 3289 students in Grades 7 and 8 in 21 schools in Hamilton, Ontario‐Canada; mean age 12.6 years, 52% female, 48% male, most White Exclusion: non‐consent by parent or students; planning to move out of the area in the next few weeks; unable to speak or understand English, severe learning disabilities, reached 17th birthday, attendance at a private or separate school | |
| Interventions | Intervention: ten 1‐hour sessions on health education and skills building, media and peer pressure, parenting, teenage pregnancy and responsibility in relationships Control: conventional sex education | |
| Outcomes | Unintended pregnancy, initiation of intercourse, use of contraceptives | |
| Notes | Duration of follow up: 4 years Loss to follow up: 44% During the study, 10 students transferred from the control to the experimental school and one student from an experimental to a control school | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Unclear risk | High rate of attrition by the fourth year with close to half the participants lost to follow up. Analysis for each outcome included only student who responded to that outcome |
| Selective reporting (reporting bias) | Low risk | Pre‐stated outcomes were reported |
| Other bias | Unclear risk | Contamination of intervention groups as students who completed Grade 8 moved on to high schools that drew students from a variety of schools, thereby bringing together experimental and control group students |
| Methods | Cluster‐randomised controlled study. Block randomi sation was used to generate allocation sequence. Unit of randomis ation: s chools | |
| Participants | 2483 6th grade students in 21 middle schools in small cities and towns in Wisconsin; by 9th grade, participants included 48% male, 52% female, 96% White, 4% other | |
| Interventions | Intervention 1: age‐ appropriate: taught four weeks each year over three years in grade 6, 7 and 8: on social situations, refusal skills (skills‐ building), parental values, media, parent relationship, contraception education, risks, responsibility and sexuality Intervention 2: intensive; taught as a 12‐ week block in grade 7: same programme Control: usual curriculum | |
| Outcomes | Initiation of intercourse, use of condoms | |
| Notes | Duration of follow up: 3 years Loss to follow up: 20% Students were randomised into one of three interventions ( control, age ‐ appropriate intervention or intensive intervention. One of the seven schools dropped out of the intensive intervention (n = 590), data from these are excluded | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomis ation design nested within two self‐selected treatment options |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Unclear risk | No statistical difference between interventions in attrition by 9th grade (p = 0.21). But high percentage of participants were lost to follow up in the 10th grade (32%) and underrepresented the intensive subjects. Individuals were used as the unit of analysis even though clusters were randomised |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Randomis ed controlled trial, individual was randomi sed by block randomi sation, research assistant was blinded to conditions | |
| Participants | 738 girls aged 15 years to 19 years, unmarried, not pregnant, not given birth within the past three months, sexually active within the past three months; predominantly low income, 69% African American | |
| Interventions | Intervention: four weekly, 120‐ minute sessions and two 90‐ minute booster sessions at three months and six months post‐intervention. It provided HIV information, motivation to reduce risky behaviour, interpersonal and self‐management and communication skills facilitating sexual risk reduction and condom use Control: general health promotion (nutrition, breast health, anger management) with the same number of sessions and led by the same facilitators | |
| Outcomes | Frequency of sexual behaviour, protected vaginal sex, number of sexual partners, abstinence | |
| Notes | Duration of follow up: 3 months, 6 months and 12 months Loss to follow up: approx 14% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Block randomi sation of participants, but method of block randomi sation not stated |
| Allocation concealment (selection bias) | Unclear risk | No information on this domain was provided |
| Blinding (performance bias and detection bias) | Low risk | Condition was known only to the project director until each group was filled and facilitators assigned. Also, pregnancy and STI was confirmed by testing |
| Incomplete outcome data (attrition bias) | High risk | Attrition rate: 14%; Girls lost to follow up were older and may have been at more risk of the outcomes |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Randomi sed controlled trial; method of randomis ation not stated | |
| Participants | 198 college students that were at least 18 years of age, heterosexual, engaged in sexual intercourse at least once during the past three months; 70% females, 85% White and 15% non‐ White | |
| Interventions | Intervention: it includes information and myths, attitudes and social norms, teaching skills and building self‐efficacy regarding increasing condom use and safer sexual behaviour. with an exclusive focus on preventing unplanned pregnancy (Intervention A), STI (Intervention B) or HIV infection (Intervention C). Control: standard healthcare services received by students in college settings | |
| Outcomes | Condom use, including percentage, frequency and use at last sex; number of unprotected vaginal intercourse | |
| Notes | Duration of follow up: 4 weeks and 8 weeks; for certain outcomes, the different interventions were collapsed as one | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomis ation not stated |
| Allocation concealment (selection bias) | Unclear risk | No information on this domain was provided |
| Blinding (performance bias and detection bias) | Unclear risk | No information on this domain was provided |
| Incomplete outcome data (attrition bias) | Unclear risk | Attrition rates were not reported |
| Selective reporting (reporting bias) | Low risk | All stated outcomes w ere reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Cluster‐ randomis ed controlled trial. Classrooms within the intervention school were randomly assigned | |
| Participants | 1061 minority students, 7th & 8th graders, 79.2% African American, 47.2% male and 15.9% Hispanic, high‐risk health profile, high‐risk academic profile, with limited access to resources | |
| Interventions | Intervention: the intervention was split into two; the regular community youth service (CYS) classroom curriculum (40 lessons in 7th grade and 34 lessons in 8th grade on risk related to early and unprotected sex, violence, substance use, healthy development and sexuality) and CYS classroom curriculum enhanced by participation. In the latter, participants engaged in three hours per week community placement performing a variety of tasks associated with social skills and behaviours, assisting or observing doctors, recreation groups etc Control: intervention not explained | |
| Outcomes | Initiation of sex (virgins at baseline), recent sex in the last three months, use of protection during the most recent intercourse | |
| Notes | Duration of follow up: 6 months loss to follow up: 8.3% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomi sation was not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | Low loss to follow up (< 10%) |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Cluster‐randomis ed controlled study. Method used to generate allocation sequence not stated. Unit of randomis ation: classrooms | |
| Participants | 225 7th grade students from 18 classrooms attending a public middle school in New York, 71% non‐Hispanic African‐American, 26% Hispanic, low socio‐economic status | |
| Interventions | Intervention: thr ee hours per week Community Youth Service (CYS) plus classroom curriculum (40 lessons in 7th grade and 34 lessons in 8th grade on risk related to early and unprotected sex, violence, substance use, healthy development and sexuality) Control: standard classroom curriculum | |
| Outcomes | Pregnancy among all participants not reporting pregnancy at baseline | |
| Notes | Duration of follow up: 4 years Loss to follow up: 23% After year 1 of the programme, the school expanded the CYS component to more students resulting in 32 students transferring into the intervention group and 16 transferring to the control group because CYS did not fit their schedules. Analyses were divided into youths receiving two programme years, youths receiving one programme year (i.e. those who transferred in or out after year 1), and no‐exposure controls. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Unclear risk | Irrespective of the crossover of participants between intervention and control groups, analysis retained participants in their previous randomised group |
| Selective reporting (reporting bias) | Low risk | Pre‐specifed outcomes were reported |
| Other bias | Unclear risk | Crossover of students between groups could have contaminated the different groups. |
| Methods | Cluster‐randomised controlled study. Method used to generate allocation sequences not mentioned. Unit of randomis ation: schools | |
| Participants | 1896 students in secondary schools in Benin, Nigeria, 14 years to 20 years, 53% female, 47% male, 33% Ishan, 36% Bini, 5% Yoruba, 10% Ibo, 16% other | |
| Interventions | Health education, peer education on STD, individual or group counselling by trained peer educators, training of health providers on STD diagnosis and treatment around the intervention schools Control: no intervention | |
| Outcomes | Use of condoms | |
| Notes | Duration of follow up: 10 months Loss to follow up: 1% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Unclear risk | Individuals were used as the unit of analysis even though clusters (classrooms) were randomised. All participants lost to follow up were from the control group and per‐protocol analysis used |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Two‐arm nested randomis ation design. Randomi sation was carried out using a Multi‐attribute randomi sation method. Unit of randomi sation: s chools | |
| Participants | 1571 female participants with mean age of 14.3 years (standard deviation = 0.59), and was 59% female, 74% Hispanic, 17% African‐American, and 9% other race/ethnicity. Close to 20% of students reported ever engaging in any type of sex (vaginal, oral, or anal) | |
| Interventions | Intervention: computer‐based sexual health education, animated scenario with modelling and skills practices, peer‐modelling videos, quizzes, virtual role‐playing activities to stimulate student skills practice in real‐world situation, healthy/unhealthy dating relationship, anatomy of reproduction, social, emotional, physical consequences of sex, communication skills, internet communication safety, causes of teen pregnancies and STIs, knowledge and skills of condoms and contraception use and condom negotiation Control: state‐approved school health education | |
| Outcomes | Delayed initiation of any sexual activity, sexual behaviours such as use of condoms in the past three months and last sex, number of partners at different time points, knowledge of STIs and condoms, and beliefs (psychosocial measures) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Multi‐attribute randomi sation method |
| Allocation concealment (selection bias) | Unclear risk | Method not stated but it was stated that "participants were blinded to condition during allocation" |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) | Low risk | Attrition rate approx. 10%, which was similar across groups |
| Selective reporting (reporting bias) | High risk | Primary outcome was reported. However, most of the secondary pre‐specified outcomes such as condom use at last sex or in the last three months were not reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Randomis ed controlled study. Unit of randomi sation: individual | |
| Participants | 484 teenagers in New York not currently pregnant or a parent, 13 years to 15 years, 55% female, 45% male, 56% Black, 42% Hispanic, 2% other | |
| Interventions | Intervention: job clubs, academic skills, family and life sexuality education, developing personal art skills, recreational activities, group/individual counselling, contraceptive education, medical care ( five days per week for a school year) Control: alternative youth programme (recreational activities, homework help, art and crafts) | |
| Outcomes | Unintended pregnancy, childbirth, initiation of intercourse, use of condoms at last sex | |
| Notes | Duration of follow up: 3 years Loss to follow up: 21% Allocation concealment by the use of opaque envelopes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomis ation not stated |
| Allocation concealment (selection bias) | Low risk | Use of opaque envelopes |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain not provided |
| Incomplete outcome data (attrition bias) | Unclear risk | Analysis was based on number of participants present at the end of the three ‐year follow up (high attrition rate) |
| Selective reporting (reporting bias) | Low risk | Pre‐specfied outcomes reported |
| Other bias | Unclear risk | Possible contamination (exchange of information) between groups, since both programmes were conducted at the same site |
| Methods | Randomis ed controlled study. Computer‐generated randomi sation sequence was used. Unit of randomi sation: individual | |
| Participants | 2117 women attending four California clinics providing family planning services, who were not desiring pregnancy, 15 years to 24 years (mean 19.9), spoke English or Spanish, had sexual intercourse in the past six months, using long‐ term hormonal contraception or requesting EC, 20% Hispanic, 15% Black, 31% White, 22% Asian, 12% Other | |
| Interventions | intervention 1: pharmacy access group (instructions for obtaining levonorgestrel Intervention 2: (provision of three packets of levonorgestrel EC and its dosage) Control: clinic access (instructions to return to the clinic for EC, if needed) | |
| Outcomes | Unintended pregnancy, contraceptive use (consistent condom use, use of hormonal contraceptives, use of condom at last sex), sexually transmitted diseases | |
| Notes | Duration of follow up: 6 months Loss to follow up: 8% Single blinding ( research staff only) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐ generated numbers |
| Allocation concealment (selection bias) | Low risk | Sealed, sequential numbered boxes identical in appearance were used to conceal allocation |
| Blinding (performance bias and detection bias) | Low risk | Research staff only |
| Incomplete outcome data (attrition bias) | Low risk | Use of a Modified intention‐to treat where only participants who completed follow‐up in their respective randomised group were analys ed. Attrition analysis showed no difference in characteristics of women lost to follow up. |
| Selective reporting (reporting bias) | Low risk | All stated outcomes in the method section were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Randomis ed controlled study. Computer‐ generated random numbers were used in allocation sequence. Unit of randomis ation: individuals | |
| Participants | 1490 sexually active women not desiring pregnancy, 14 years to 24 years, 13% Hispanic, 70% White, 21% non‐ White | |
| Interventions | Intervention: contraception distribution ( two packages of pills dispensed in advance with unlimited resupply at no charge) Control: contraceptive distribution (pills dispensed when needed at usual charge) | |
| Outcomes | Unintended pregnancy, sexually transmitted diseases | |
| Notes | Duration of follow up: 1 year Loss to follow up: < 7% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐ generated number |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain not provided |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analysis |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcome reported |
| Other bias | Unclear risk | Higher proportion of people in the increased access group had a sexually transmitted disease which may lead to increased use of condoms |
| Methods | Randomis ed controlled trial. Table of random numbers was used to generate allocation sequence. Unit of randomis ation: individuals | |
| Participants | 123 female participants between the ages of 13 years to 22 years (median 17.2) with cervicitis or pelvic inflammatory disease in urban children's hospital, adolescent clinic and inpatient service in Boston, 49% non‐Hispanic Black, 18% Hispanic, 14% Non‐Hispanic White, 17% other Exclusion: p atient had treatment of STDs between laboratory confirmation; patient pregnant at treatment visit; patient already exposed to intervention through pilot study | |
| Interventions | Intervention: watch a seven ‐minute videotape featuring contraception education (condoms), contraception distribution, individual counselling on risk perception, STD education, pregnancy prevention and consequences of unprotected sex and a booster session at one , three and six months. Control: standard STD education and contraceptive education and distribution | |
| Outcomes | Sexually transmitted diseases | |
| Notes | Duration of follow up: 12 months Loss to follow up: 48% Assessors were blinded to participant allocation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain not provided |
| Blinding (performance bias and detection bias) | Low risk | Assessors only |
| Incomplete outcome data (attrition bias) | Unclear risk | High attrition rates of over 20% though it did not differ between the intervention and control groups. As‐treated analysis was done with substantial loss‐ to‐ follow‐ up of participants across groups. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | Study appears to be free from other sources of bias |
| Methods | Randomis ed controlled trial. Individuals were randomi sed to the intervention or control but the method of randomi sation was not stated. | |
| Participants | 253 girls aged between 13 years to 17 years, racially mixed ; American Indian, Asian, Hispanic, White/European, mixed and Black/African/African American. Black/African/African American made up over 40% of the population | |
| Interventions | Intervention: one‐on‐one case management addressing the following issues: emotional skills, healthy relationships, responsible sexual behaviours, positive family, school and community involvement and the peer leadership components which provided hands‐on skills‐ building experiences; plus usual clinic services Control: usual clinic services | |
| Outcomes | Contraceptive use (condom, hormonal and dual method) consistency with most recent sex partner, number of sex partners in the past six months | |
| Notes | Duration of follow up: ,12 & 24 months, intention‐to‐treat design Loss to follow up: 5.5% and 6.7% at 12 and 24 months respectively | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomis ation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain not provided |
| Incomplete outcome data (attrition bias) | Low risk | Attrition rate was low (< 10%) |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes not provided |
| Other bias | Low risk | The study seems to be free from other sources of bias |
| Methods | Randomis ed controlled study. Method used to generate allocation sequence not mentioned in the paper. Unit of randomis ation: individuals | |
| Participants | 120 9th grade students from the 1989 class of freshmen at a high school in Queens, New York. Mean age 15.1 years; 74.2% female and 25.8% male; 43.3% African American, 30.8% West Indian, 22.5% Hispanic and 3.3% other | |
| Interventions | Intervention: one session per week for 14 weeks on health/STD education, skills‐ building, contraceptive education and individual counselling on career mentorship Control: written materials on contraception and decision making pertaining to sexual‐ and fertility‐ related risk‐taking behaviour | |
| Outcomes | Initiation of intercourse ( absolute sexual frequency ‐ instances of completed sexual activity during past two months, among all participants) | |
| Notes | Duration of follow up: six months. Loss to follow up: 21% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | No information provided on this domain |
| Blinding (performance bias and detection bias) | Unclear risk | No information provided on this domain |
| Incomplete outcome data (attrition bias) | Unclear risk | Per‐protocol analysis was done with substantial departure of the intervention received from that assigned at randomis ation |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Cluster‐randomis ed controlled study. Schools were randomised within strata, using a computer‐generated sequence of allocation of block size ten. Unit of randomis ation: schools | |
| Participants | 8766 pupils in 29 schools in central and southern England, aged 13 years to 14 years; over 9000 pupils | |
| Interventions | Intervention: Three 1‐hour sessions on sexual communication and relationships, contraceptive education (condoms) (pressure role play on declining sex or insisting on the use of condoms), HIV/STD education (transmission and treatment) taught by peer leaders (16 years to 17years) Control: usual teacher‐led sex education | |
| Outcomes | Unintended pregnancy, heterosexual intercourse at age 16 years, use of contraceptives (at first and last sex), use of condoms, abortion and livebirth at age 20 years, self‐reported STD | |
| Notes | Duration of follow up: 18 months and 54 months Loss to follow up: 14% and > 40% at 18 months and 54 months respectively Data on abortion and livebirth are included in data & analysis, while others are reported in additional tables | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence of allocation of block size ten |
| Allocation concealment (selection bias) | Unclear risk | No information provided on this domain |
| Blinding (performance bias and detection bias) | Low risk | While blinding of participants/facilitators to allocation was not possible, matching of outcomes to sources was blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | All participants who experienced the outcome at baseline and who completed at least one follow‐up questionnaire were included in the analysis for the primary outcome (initiation of intercourse). High attrition rate at 54 months but intention ‐to‐ treat was employed for primary outcomes (childbirth and abortion by 20 years) at the second follow up |
| Selective reporting (reporting bias) | Low risk | Expected outcomes and those pre‐specified in the methods were reported |
| Other bias | Unclear risk | It is not known for sure if there was no contamination between pupils in the different groups |
| Methods | Randomised controlled study. Computer‐generated random numbers used to generate allocation sequence Unit of randomi sation: individuals | |
| Participants | 656 8th grade to 11th grade students in Northeast Philadelphia schools and community‐ based organis ations, aged 13 years to 18 years, 45% male, 55% female, 85.4% Hispanic | |
| Interventions | Intervention: six 50‐minute modules on Health/HIV education, skills‐ building, contraceptive education Control: health promotion education | |
| Outcomes | Initiation of intercourse in the past t hree months, consistent condom use in the past three months, | |
| Notes | Duration of follow up: 12 months Loss to follow up: 13% 103 students were excluded from the analysis because they were non‐ Hispanic | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐ generated numbers |
| Allocation concealment (selection bias) | Unclear risk | No information provided on this domain |
| Blinding (performance bias and detection bias) | Unclear risk | No information provided on this domain |
| Incomplete outcome data (attrition bias) | Low risk | Analyse s were conducted using an intention‐to‐treat approach in which participants were analy sed in their original randomised groups regardless of the number of sessions attended |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Cluster‐randomis ed controlled study. Method used to generate allocation sequence not mentioned in the paper. Unit of randomi sation: schools | |
| Participants | 10,954 10th grade to 12th grade high school students in Morelos, 15 years to 18 years, 48% male, 52% female | |
| Interventions | Intervention 1: HIV education, skills‐ building, cultural values, contraceptive promotion ( condoms). Intervention 2: HIV education, skills‐ building, cultural values plus contraceptive education (EC plus condoms and their access). Control: biology‐ based sex education | |
| Outcomes | Initiation of intercourse, use of condom at last sex, use of hormonal contraceptive | |
| Notes | Duration of follow up: 16 months Loss to follow up: 33.3% Two of the intervention schools were included in the control group because they did not teach the intervention course | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The statement "randomly assigned" was said but the method of allocation generation was not stated. |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain not provided |
| Blinding (performance bias and detection bias) | Unclear risk | Information on this domain not provided |
| Incomplete outcome data (attrition bias) | Unclear risk | Per‐protocol analysis was done. But analysis took the cluster sample design into account. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes not provided |
| Other bias | Low risk | The study appears to be free from other sources of bias |
| Methods | Cluster‐randomis ed controlled study. Method used to generate allocation sequence not mentioned. Unit of randomi sation: schools | |
| Participants | 7616 pupils from 25 secondary schools in east Scotland, 13 years to 15 years, 50% male, 50% female | |
| Interventions | Intervention: SHARE (20‐ session package: 10 for 3rd years and 10 for 4th years of secondary school respectively) on health/sex education, skills ‐building, contraceptive education primarily through the use of interactive video Control: conventional sex education | |
| Outcomes | Unintended pregnancy, initiation of intercourse, use of condoms at last sex | |
| Notes | Duration of follow up: 2 years Loss to follow up: 31% Single blinding ( assessors) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomis ation was not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain not provided |
| Blinding (performance bias and detection bias) | Low risk | Assessors only |
| Incomplete outcome data (attrition bias) | Unclear risk | Outcomes were analy sed based on the number of participants at the end of the two ‐year follow up. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Characteristics of excluded studies [ordered by study ID]
Jump to:
| Study | Reason for exclusion |
| Did not measure any of the desired outcomes | |
| Randomi sed controlled trial but participants were pregnant or parenting teens | |
| Participants above the required age range | |
| Had none of the required interventions | |
| Secondary prevention of adolescent pregnancy | |
| Unintended repeat pregnancies assessed | |
| No specified intervention | |
| Non‐randomis ed controlled trial | |
| Participants above the required age range | |
| Published protocol | |
| Control group received an intervention aimed at promoting contraceptive usage | |
| Non‐randomis ed controlled trial | |
| Non‐randomis ed controlled trial | |
| Non‐randomis ed controlled trial | |
| Participants aged 18 years to 32 years (above required age range) | |
| Reported information on baseline characteristics only | |
| None of the desired outcomes was measured | |
| Quasi‐experimental study | |
| C ross‐sectional st udy | |
| None of the desired outcomes was measured | |
| Non‐randomis ed controlled study | |
| Non‐randomis ed controlled study | |
| Non‐randomis ed controlled study | |
| Non‐randomis ed controlled study | |
| Non‐randomis ed controlled study | |
| Non‐randomis ed controlled study | |
| Participants were above the required age range | |
| Quasi‐randomis ed controlled study | |
| Non‐randomis ed controlled study | |
| Did not measure any of the desired outcomes | |
| Participants above the required age and different outcomes measured | |
| Non‐randomis ed controlled trial | |
| No control group | |
| Randomis ed controlled trial but participants included couples only | |
| Unintended repeat pregnancies assessed | |
| Non‐randomi sed controlled trial | |
| None of the desired outcomes was measured | |
| Participant above the required age range | |
| Did not measure any of the desired outcomes | |
| Non‐randomis ed controlled trial | |
| Participants above the required age range | |
| None of the desired outcomes was measured | |
| Age range above the required range | |
| Unintended repeat pregnancies assessed | |
| A Review | |
| Non‐randomis ed controlled trial | |
| An epidemiological study | |
| Non‐randomis ed controlled study | |
| Participants' age range was above the required range | |
| Non‐randomis ed controlled study | |
| Non‐randomis ed controlled trial | |
| Study did not measure any of the desired outcomes | |
| No intervention | |
| Method of randomis ation not adequate | |
| Participants were above the required age range | |
| Non‐randomis ed controlled trial | |
| None of the desired outcomes was measured | |
| Non‐randomis ed controlled trial | |
| Not a randomis ed controlled trial | |
| Participants above the required age range | |
| Participants above the required age range | |
| Participants above the required age range | |
| Not a randomis ed controlled trial | |
| Participants above the required age range | |
| Participants above the required age range | |
| Participants above the required age range | |
| Participants above the required age range | |
| A review | |
| Unintended repeat pregnancies assessed | |
| Participants above the required age range | |
| Non‐randomis ed controlled trial | |
| A quasi‐randomis ed study | |
| Non‐randomis ed controlled trial | |
| A review | |
| A review | |
| Quasi‐experimental design | |
| A review | |
| Non‐randomis ed controlled trial | |
| Non‐randomis ed controlled trial | |
| Study included participants greater than the age limit and it was not clearly stated what percentage was within the accepted age range | |
| Participants were not within the age limit | |
| Case‐control study | |
| Non‐randomis ed study | |
| Non‐randomis ed study | |
| Non‐randomis ed study | |
| Quasi‐experimental study |
Characteristics of studies awaiting assessment [ordered by study ID]
Jump to:
| Methods | Multi‐center, clinic‐based, randomised controlled trial |
| Participants | Female, aged 14 years to 19 years |
| Interventions | Seventeen Days (theory‐based interactive video intervention) |
| Outcomes | Unintended pregnancy and STIs |
| Notes | Full paper pending |
| Methods | Randomised controlled study |
| Participants | Male and female (14 years to 24 years) |
| Interventions | Interactive computer‐based intervention |
| Outcomes | STIs, unintended pregnancy, number of partners, rate of unprotected vaginal sex (without condoms) and rate of unprotected vaginal sex (without contraceptive) |
| Notes | Full paper pending |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Unintended pregnancy [individually randomised trials] Show forest plot | 4 | 1905 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.50, 0.87] |
| Analysis 1.1 ![Comparison 1 Multiple interventions, Outcome 1 Unintended pregnancy [individually randomised trials].](/cdsr/doi/10.1002/14651858.CD005215.pub3/media/CDSR/CD005215/image_n/nCD005215-CMP-001-01.png) Comparison 1 Multiple interventions, Outcome 1 Unintended pregnancy [individually randomised trials]. | ||||
| 2 Unintended pregnancy [cluster‐randomised trials] Show forest plot | 5 | 3149 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.23, 1.09] |
| Analysis 1.2 ![Comparison 1 Multiple interventions, Outcome 2 Unintended pregnancy [cluster‐randomised trials].](/cdsr/doi/10.1002/14651858.CD005215.pub3/media/CDSR/CD005215/image_n/nCD005215-CMP-001-02.png) Comparison 1 Multiple interventions, Outcome 2 Unintended pregnancy [cluster‐randomised trials]. | ||||
| 3 Initiation of sexual intercourse ‐ individually RCT Show forest plot | 4 | 1796 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.74, 1.32] |
| Analysis 1.3  Comparison 1 Multiple interventions, Outcome 3 Initiation of sexual intercourse ‐ individually RCT. | ||||
| 4 Initiation of sexual intercourse ‐ cluster RCT Show forest plot | 7 | 8608 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.68, 1.04] |
| Analysis 1.4 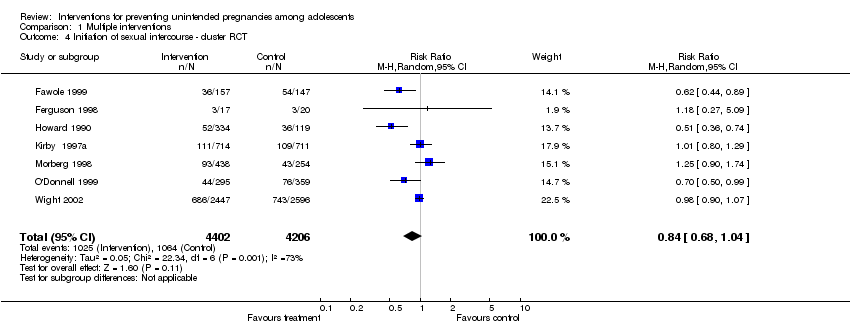 Comparison 1 Multiple interventions, Outcome 4 Initiation of sexual intercourse ‐ cluster RCT. | ||||
| 5 Use of birth control methods ‐ individually RCT Show forest plot | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.5  Comparison 1 Multiple interventions, Outcome 5 Use of birth control methods ‐ individually RCT. | ||||
| 5.1 Condom use in last sex | 3 | 796 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.95, 1.06] |
| 5.2 Consistent condom use | 5 | 1681 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.95, 1.54] |
| 5.3 Contraceptive use at last sex | 1 | 408 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.95, 1.03] |
| 5.4 Consistent contraceptive use | 1 | 253 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [1.06, 1.59] |
| 6 Use of birth control methods ‐ cluster RCT Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.6  Comparison 1 Multiple interventions, Outcome 6 Use of birth control methods ‐ cluster RCT. | ||||
| 6.1 Condom use at last sex | 4 | 2620 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.93, 1.09] |
| 6.2 Consistent condom use | 3 | 826 | Risk Ratio (M‐H, Random, 95% CI) | 1.95 [0.70, 5.44] |
| 6.3 Hormonal contraceptives | 3 | 3987 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.72, 1.43] |
| 7 Sexually Transmitted Diseases ‐ individually RCT Show forest plot | 2 | 699 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.65, 1.22] |
| Analysis 1.7  Comparison 1 Multiple interventions, Outcome 7 Sexually Transmitted Diseases ‐ individually RCT. | ||||
| 8 Sexually Transmitted Diseases ‐ cluster RCT Show forest plot | 2 | 420 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.27, 2.14] |
| Analysis 1.8  Comparison 1 Multiple interventions, Outcome 8 Sexually Transmitted Diseases ‐ cluster RCT. | ||||
| 9 Childbirth ‐ cluster RCT Show forest plot | 1 | 4776 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.52, 0.79] |
| Analysis 1.9 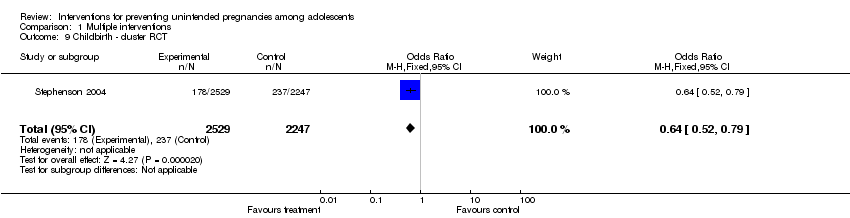 Comparison 1 Multiple interventions, Outcome 9 Childbirth ‐ cluster RCT. | ||||
| 10 Childbirth ‐ individually RCT Show forest plot | 1 | 484 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.31, 1.45] |
| Analysis 1.10 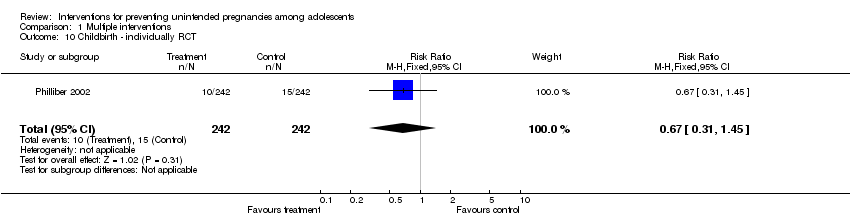 Comparison 1 Multiple interventions, Outcome 10 Childbirth ‐ individually RCT. | ||||
| 11 Second unintended pregnancy ‐ individually RCT Show forest plot | 1 | 149 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.22, 1.02] |
| Analysis 1.11  Comparison 1 Multiple interventions, Outcome 11 Second unintended pregnancy ‐ individually RCT. | ||||
| 12 Abortion (cluster RCT) Show forest plot | 1 | 4776 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.72, 1.21] |
| Analysis 1.12  Comparison 1 Multiple interventions, Outcome 12 Abortion (cluster RCT). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Unintended pregnancy ‐ cluster‐randomi sed trials Show forest plot | 2 | 497 | Risk Ratio (M‐H, Random, 95% CI) | 0.20 [0.10, 0.39] |
| Analysis 2.1 ![Comparison 2 Sensitivity analysis [Multiple interventions]: Unintended pregnancy, Outcome 1 Unintended pregnancy ‐ cluster‐randomi sed trials .](/cdsr/doi/10.1002/14651858.CD005215.pub3/media/CDSR/CD005215/image_n/nCD005215-CMP-002-01.png) Comparison 2 Sensitivity analysis [Multiple interventions]: Unintended pregnancy, Outcome 1 Unintended pregnancy ‐ cluster‐randomi sed trials . | ||||
| 2 Unintended pregnancy ‐ individually‐randomi sed trials Show forest plot | 3 | 1421 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.46, 1.00] |
| Analysis 2.2 ![Comparison 2 Sensitivity analysis [Multiple interventions]: Unintended pregnancy, Outcome 2 Unintended pregnancy ‐ individually‐randomi sed trials .](/cdsr/doi/10.1002/14651858.CD005215.pub3/media/CDSR/CD005215/image_n/nCD005215-CMP-002-02.png) Comparison 2 Sensitivity analysis [Multiple interventions]: Unintended pregnancy, Outcome 2 Unintended pregnancy ‐ individually‐randomi sed trials . | ||||
| 3 Unintended pregnancy ‐ cluster‐adjusted + individual Show forest plot | 5 | 1918 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.39, 0.72] |
| Analysis 2.3 ![Comparison 2 Sensitivity analysis [Multiple interventions]: Unintended pregnancy, Outcome 3 Unintended pregnancy ‐ cluster‐adjusted + individual .](/cdsr/doi/10.1002/14651858.CD005215.pub3/media/CDSR/CD005215/image_n/nCD005215-CMP-002-03.png) Comparison 2 Sensitivity analysis [Multiple interventions]: Unintended pregnancy, Outcome 3 Unintended pregnancy ‐ cluster‐adjusted + individual . | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Initiation of sexual intercourse ‐ individually RCT Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 3.1 ![Comparison 3 Sensitivity analysis [Multiple interventions]: Initiation of intercourse, Outcome 1 Initiation of sexual intercourse ‐ individually RCT.](/cdsr/doi/10.1002/14651858.CD005215.pub3/media/CDSR/CD005215/image_n/nCD005215-CMP-003-01.png) Comparison 3 Sensitivity analysis [Multiple interventions]: Initiation of intercourse, Outcome 1 Initiation of sexual intercourse ‐ individually RCT. | ||||
| 1.1 Gender mixed or not specified | 3 | 1312 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.67, 2.09] |
| 2 Initiation of sexual intercourse ‐ cluster RCT Show forest plot | 4 | 1687 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.57, 1.25] |
| Analysis 3.2 ![Comparison 3 Sensitivity analysis [Multiple interventions]: Initiation of intercourse, Outcome 2 Initiation of sexual intercourse ‐ cluster RCT.](/cdsr/doi/10.1002/14651858.CD005215.pub3/media/CDSR/CD005215/image_n/nCD005215-CMP-003-02.png) Comparison 3 Sensitivity analysis [Multiple interventions]: Initiation of intercourse, Outcome 2 Initiation of sexual intercourse ‐ cluster RCT. | ||||
| 2.1 Gender mixed or not specified | 4 | 1687 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.57, 1.25] |
| 3 Initiation of sexual intercourse ‐ cluster‐adjusted + individual Show forest plot | 7 | 2999 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.74, 1.05] |
| Analysis 3.3 ![Comparison 3 Sensitivity analysis [Multiple interventions]: Initiation of intercourse, Outcome 3 Initiation of sexual intercourse ‐ cluster‐adjusted + individual.](/cdsr/doi/10.1002/14651858.CD005215.pub3/media/CDSR/CD005215/image_n/nCD005215-CMP-003-03.png) Comparison 3 Sensitivity analysis [Multiple interventions]: Initiation of intercourse, Outcome 3 Initiation of sexual intercourse ‐ cluster‐adjusted + individual. | ||||
| 3.1 Gender mixed or not specified | 7 | 2999 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.74, 1.05] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Initiation of sexual intercourse ‐ cluster RCT Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.1  Comparison 4 Educational interventions , Outcome 1 Initiation of sexual intercourse ‐ cluster RCT. | ||||
| 1.1 Gender mixed or not specified | 2 | 672 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.71, 1.27] |
| 2 Use of birth control methods ‐ cluster RCT Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 4.2  Comparison 4 Educational interventions , Outcome 2 Use of birth control methods ‐ cluster RCT. | ||||
| 2.1 condom use at last sex | 2 | 1431 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [1.06, 1.32] |
| 3 Use of contraceptives ‐ individually RCT Show forest plot | 1 | 360 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.5 [1.39, 4.48] |
| Analysis 4.3 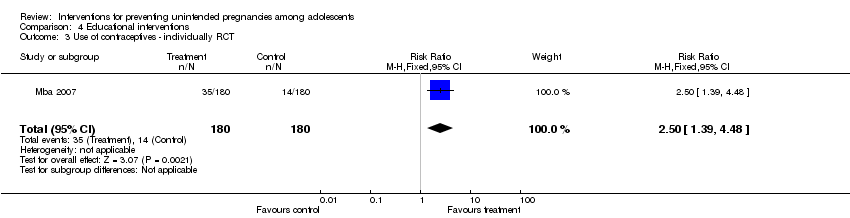 Comparison 4 Educational interventions , Outcome 3 Use of contraceptives ‐ individually RCT. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Unintended pregnancy ‐ individually RCT Show forest plot | 2 | 3440 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.81, 1.26] |
| Analysis 5.1 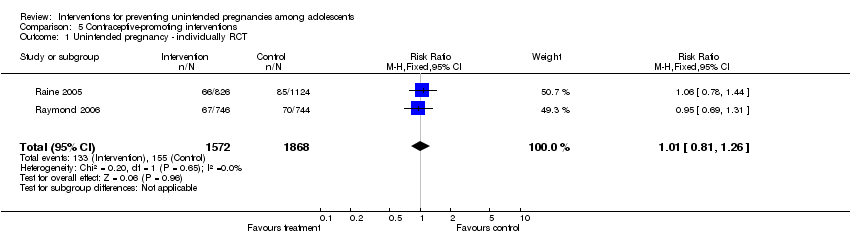 Comparison 5 Contraceptive‐promoting interventions, Outcome 1 Unintended pregnancy ‐ individually RCT. | ||||
| 2 Initiation of sexual intercourse ‐ cluster RCT Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.2  Comparison 5 Contraceptive‐promoting interventions, Outcome 2 Initiation of sexual intercourse ‐ cluster RCT. | ||||
| 2.1 Female | 1 | 1446 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.76, 1.04] |
| 2.2 Male | 1 | 1560 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.87, 1.21] |
| 3 Use of birth control methods ‐ cluster RCT Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.3 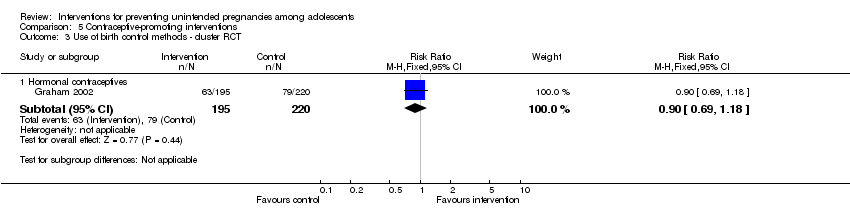 Comparison 5 Contraceptive‐promoting interventions, Outcome 3 Use of birth control methods ‐ cluster RCT. | ||||
| 3.1 Hormonal contraceptives | 1 | 415 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.69, 1.18] |
| 4 Use of birth control methods ‐ individually RCT Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 5.4 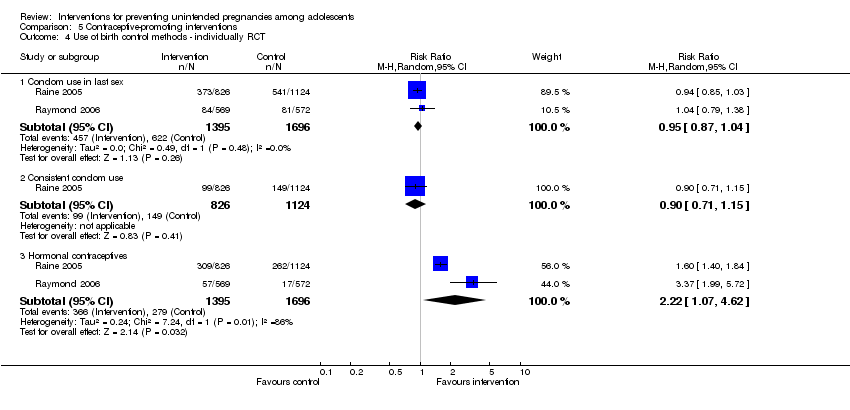 Comparison 5 Contraceptive‐promoting interventions, Outcome 4 Use of birth control methods ‐ individually RCT. | ||||
| 4.1 Condom use in last sex | 2 | 3091 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.87, 1.04] |
| 4.2 Consistent condom use | 1 | 1950 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.71, 1.15] |
| 4.3 Hormonal contraceptives | 2 | 3091 | Risk Ratio (M‐H, Random, 95% CI) | 2.22 [1.07, 4.62] |
| 5 Sexually Transmitted Diseases ‐ individually RCT Show forest plot | 2 | 3440 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.75, 1.13] |
| Analysis 5.5  Comparison 5 Contraceptive‐promoting interventions, Outcome 5 Sexually Transmitted Diseases ‐ individually RCT. | ||||

Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
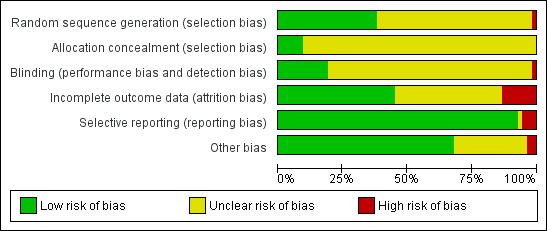
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
![Comparison 1 Multiple interventions, Outcome 1 Unintended pregnancy [individually randomised trials].](/cdsr/doi/10.1002/14651858.CD005215.pub3/media/CDSR/CD005215/image_n/nCD005215-CMP-001-01.png)
Comparison 1 Multiple interventions, Outcome 1 Unintended pregnancy [individually randomised trials].
![Comparison 1 Multiple interventions, Outcome 2 Unintended pregnancy [cluster‐randomised trials].](/cdsr/doi/10.1002/14651858.CD005215.pub3/media/CDSR/CD005215/image_n/nCD005215-CMP-001-02.png)
Comparison 1 Multiple interventions, Outcome 2 Unintended pregnancy [cluster‐randomised trials].

Comparison 1 Multiple interventions, Outcome 3 Initiation of sexual intercourse ‐ individually RCT.
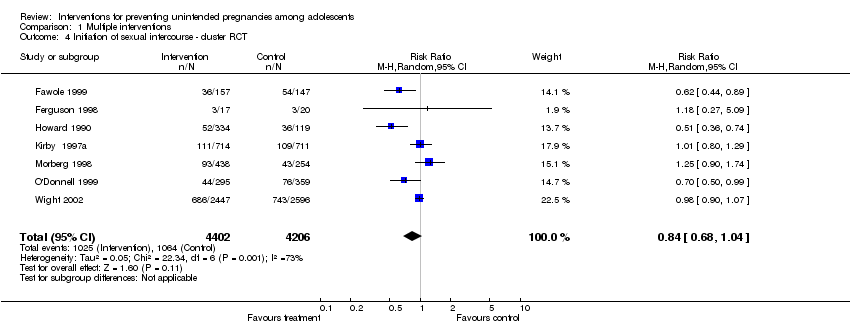
Comparison 1 Multiple interventions, Outcome 4 Initiation of sexual intercourse ‐ cluster RCT.

Comparison 1 Multiple interventions, Outcome 5 Use of birth control methods ‐ individually RCT.

Comparison 1 Multiple interventions, Outcome 6 Use of birth control methods ‐ cluster RCT.

Comparison 1 Multiple interventions, Outcome 7 Sexually Transmitted Diseases ‐ individually RCT.

Comparison 1 Multiple interventions, Outcome 8 Sexually Transmitted Diseases ‐ cluster RCT.
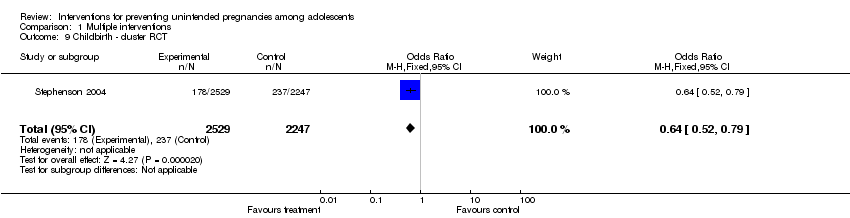
Comparison 1 Multiple interventions, Outcome 9 Childbirth ‐ cluster RCT.
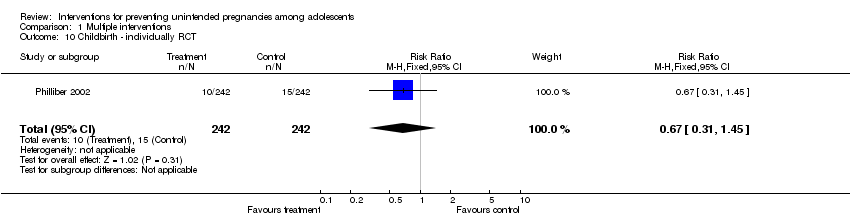
Comparison 1 Multiple interventions, Outcome 10 Childbirth ‐ individually RCT.

Comparison 1 Multiple interventions, Outcome 11 Second unintended pregnancy ‐ individually RCT.

Comparison 1 Multiple interventions, Outcome 12 Abortion (cluster RCT).
![Comparison 2 Sensitivity analysis [Multiple interventions]: Unintended pregnancy, Outcome 1 Unintended pregnancy ‐ cluster‐randomi sed trials .](/cdsr/doi/10.1002/14651858.CD005215.pub3/media/CDSR/CD005215/image_n/nCD005215-CMP-002-01.png)
Comparison 2 Sensitivity analysis [Multiple interventions]: Unintended pregnancy, Outcome 1 Unintended pregnancy ‐ cluster‐randomi sed trials .
![Comparison 2 Sensitivity analysis [Multiple interventions]: Unintended pregnancy, Outcome 2 Unintended pregnancy ‐ individually‐randomi sed trials .](/cdsr/doi/10.1002/14651858.CD005215.pub3/media/CDSR/CD005215/image_n/nCD005215-CMP-002-02.png)
Comparison 2 Sensitivity analysis [Multiple interventions]: Unintended pregnancy, Outcome 2 Unintended pregnancy ‐ individually‐randomi sed trials .
![Comparison 2 Sensitivity analysis [Multiple interventions]: Unintended pregnancy, Outcome 3 Unintended pregnancy ‐ cluster‐adjusted + individual .](/cdsr/doi/10.1002/14651858.CD005215.pub3/media/CDSR/CD005215/image_n/nCD005215-CMP-002-03.png)
Comparison 2 Sensitivity analysis [Multiple interventions]: Unintended pregnancy, Outcome 3 Unintended pregnancy ‐ cluster‐adjusted + individual .
![Comparison 3 Sensitivity analysis [Multiple interventions]: Initiation of intercourse, Outcome 1 Initiation of sexual intercourse ‐ individually RCT.](/cdsr/doi/10.1002/14651858.CD005215.pub3/media/CDSR/CD005215/image_n/nCD005215-CMP-003-01.png)
Comparison 3 Sensitivity analysis [Multiple interventions]: Initiation of intercourse, Outcome 1 Initiation of sexual intercourse ‐ individually RCT.
![Comparison 3 Sensitivity analysis [Multiple interventions]: Initiation of intercourse, Outcome 2 Initiation of sexual intercourse ‐ cluster RCT.](/cdsr/doi/10.1002/14651858.CD005215.pub3/media/CDSR/CD005215/image_n/nCD005215-CMP-003-02.png)
Comparison 3 Sensitivity analysis [Multiple interventions]: Initiation of intercourse, Outcome 2 Initiation of sexual intercourse ‐ cluster RCT.
![Comparison 3 Sensitivity analysis [Multiple interventions]: Initiation of intercourse, Outcome 3 Initiation of sexual intercourse ‐ cluster‐adjusted + individual.](/cdsr/doi/10.1002/14651858.CD005215.pub3/media/CDSR/CD005215/image_n/nCD005215-CMP-003-03.png)
Comparison 3 Sensitivity analysis [Multiple interventions]: Initiation of intercourse, Outcome 3 Initiation of sexual intercourse ‐ cluster‐adjusted + individual.

Comparison 4 Educational interventions , Outcome 1 Initiation of sexual intercourse ‐ cluster RCT.

Comparison 4 Educational interventions , Outcome 2 Use of birth control methods ‐ cluster RCT.
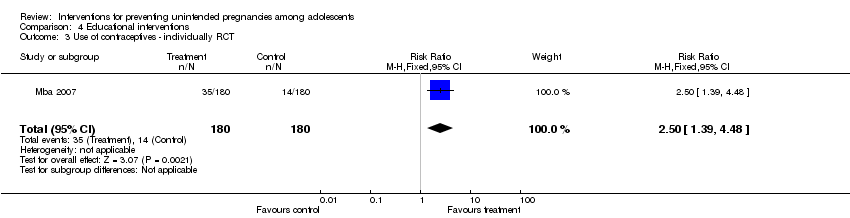
Comparison 4 Educational interventions , Outcome 3 Use of contraceptives ‐ individually RCT.
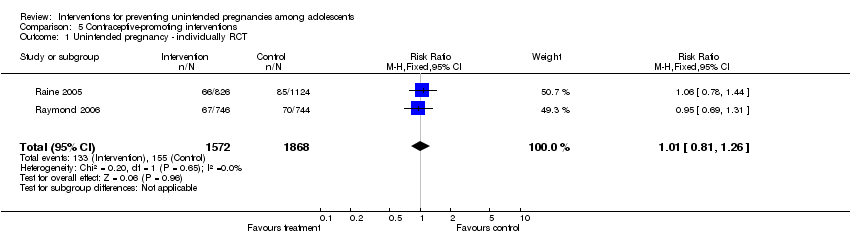
Comparison 5 Contraceptive‐promoting interventions, Outcome 1 Unintended pregnancy ‐ individually RCT.

Comparison 5 Contraceptive‐promoting interventions, Outcome 2 Initiation of sexual intercourse ‐ cluster RCT.
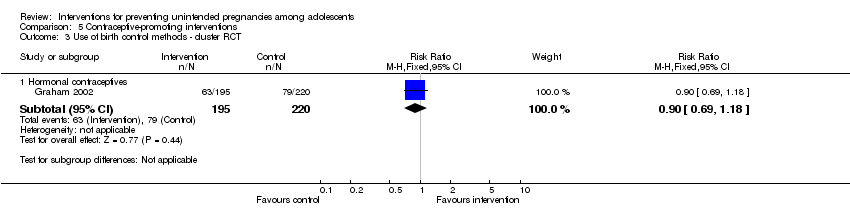
Comparison 5 Contraceptive‐promoting interventions, Outcome 3 Use of birth control methods ‐ cluster RCT.
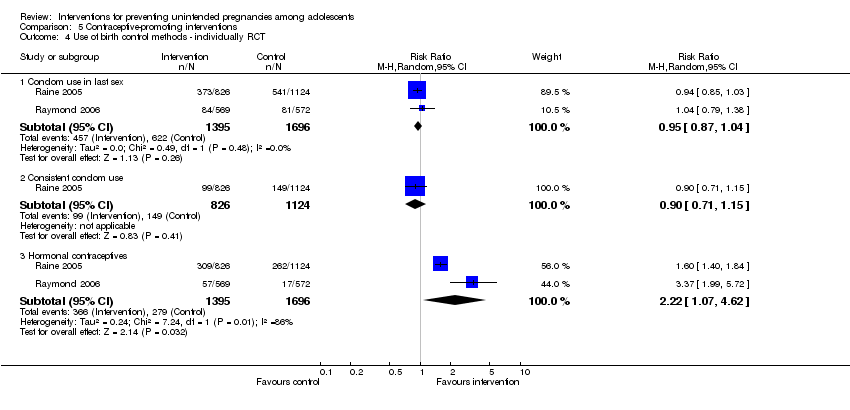
Comparison 5 Contraceptive‐promoting interventions, Outcome 4 Use of birth control methods ‐ individually RCT.

Comparison 5 Contraceptive‐promoting interventions, Outcome 5 Sexually Transmitted Diseases ‐ individually RCT.
| Contraceptive‐promoting interventions (individual RCTs) | |||||
| Patient or population: Male and female adolescents aged 10 years to 19 years | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | |
| Risk with No intervention/standard curriculum | Risk with Contraception Intervention | ||||
| Unintended pregnancy | Study population | RR 1.01 | 3440 | ⊕⊕⊕⊝ | |
| 83 per 1000 | 84 per 1000 | ||||
| Moderate | |||||
| 85 per 1000 | 86 per 1000 | ||||
| Use of birth control methods (condom use in last sex) | Study population | RR 0.95 | 3091 | ⊕⊕⊕⊕ | |
| 367 per 1000 | 348 per 1000 | ||||
| Moderate | |||||
| 312 per 1000 | 296 per 1000 | ||||
| Use of birth control methods (hormonal contraceptives) | Study population | RR 2.22 | 3091 | ⊕⊕⊕⊕ | |
| 165 per 1000 | 365 per 1000 | ||||
| Moderate | |||||
| 131 per 1000 | 292 per 1000 | ||||
| Sexually Transmitted Diseases | Study population | RR 0.92 | 3440 | ⊕⊕⊕⊕ | |
| 103 per 1000 | 95 per 1000 | ||||
| Moderate | |||||
| 98 per 1000 | 90 per 1000 | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1 Downgraded by 1 for imprecision: confidence interval fail to appreciable harm and included the null value | |||||
| Educational interventions (cluster RCTs) | |||||
| Patient or population: Male and female adolescents aged 10 years to 19 years | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | |
| Risk with No intervention/Standard curriculum | Risk with Educational intervention | ||||
| Use of birth control methods (condom use at last sex) | Study population | RR 1.18 | 1431 | ⊕⊕⊕⊝ | |
| 261 per 1000 | 308 per 1000 | ||||
| Moderate | |||||
| 534 per 1000 | 630 per 1000 | ||||
| Initiation of sexual intercourse (mixed gender) | Study population | RR 0.95 | 672 | ⊕⊕⊝⊝ | |
| 227 per 1000 | 215 per 1000 | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1 Several risk of bias assessment were unclear (not provided in the text) 2 Low number of events and confidence interval includes the null value | |||||
| Multiple interventions (cluster RCTs) | |||||
| Patient or population: Male and female adolescents aged 10 years to 19 years | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | |
| Risk with No Intervention/Standard curriculum | Risk with Multiple interventions | ||||
| Unintended pregnancy | Study population | RR 0.50 | 3149 | ⊕⊕⊝⊝ | |
| 67 per 1000 | 33 per 1000 | ||||
| Moderate | |||||
| 25 per 1000 | 13 per 1000 | ||||
| Initiation of sexual intercourse (mixed gender) | Study population | RR 0.84 | 8608 | ⊕⊝⊝⊝ | |
| 253 per 1000 | 212 per 1000 | ||||
| Moderate | |||||
| 212 per 1000 | 178 per 1000 | ||||
| Use of birth control methods (condom use at last sex) | Study population | RR 1.01 | 2620 | ⊕⊕⊕⊝ | |
| 585 per 1000 | 591 per 1000 | ||||
| Moderate | |||||
| 565 per 1000 | 570 per 1000 | ||||
| Use of birth control methods (consistent condom use) | Study population | RR 1.95 | 826 | ⊕⊕⊝⊝ | |
| 353 per 1000 | 689 per 1000 | ||||
| Moderate | |||||
| 133 per 1000 | 259 per 1000 | ||||
| Use of birth control methods (hormonal contraceptives) | Study population | RR 1.01 | 3987 | ⊕⊝⊝⊝ | |
| 244 per 1000 | 246 per 1000 | ||||
| Moderate | |||||
| 251 per 1000 | 254 per 1000 | ||||
| Sexually Transmitted Diseases | Study population | RR 0.76 | 420 | ⊕⊕⊝⊝ | |
| 37 per 1000 | 28 per 1000 | ||||
| Moderate | |||||
| 31 per 1000 | 24 per 1000 | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1 Downgraded by 1 for risk of bias; several assessments were unclear due to no information provided. Such potential limitations are likely to lower confidence in the estimate of effect 2 Downgraded by 1 for imprecision; low number of events, confidence interval includes appreciable benefit and null value 3 Heterogeneity could be explained (difference in comparison intervention and length of follow up) 4 Downgraded by 1 for imprecision: confidence interval includes appreciable benefit 5 Downgraded by 1 for inconsistency: unexplained large variations in effect 6 Confidence interval includes the null value, however, the sample size and number of events are fairly large and confidence interval is relatively narrow 7 Downgraded by 1 for imprecision: confidence interval includes appreciable benefit and harm 8 Downgraded by 1 for imprecision; low number of events, confidence interval includes appreciable benefit and harm | |||||
| Multiple interventions ( individual RCTs) | |||||
| Patient or population: Male and female adolescents aged 10 years to 9 years | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | |
| Risk with No Intervention/Standard curriculum | Risk with Multiple interventions | ||||
| Unintended pregnancy | Study population | RR 0.66 | 1905 | ⊕⊕⊕⊝ | |
| 116 per 1000 | 76 per 1000 | ||||
| Moderate | |||||
| 149 per 1000 | 98 per 1000 | ||||
| Initiation of sexual intercourse (mixed gender) | Study population | RR 0.99 | 1796 | ⊕⊕⊕⊝ | |
| 410 per 1000 | 406 per 1000 | ||||
| Moderate | |||||
| 236 per 1000 | 234 per 1000 | ||||
| Use of birth control methods (condom use in last sex) | Study population | RR 1.00 | 796 | ⊕⊕⊕⊝ | |
| 840 per 1000 | 840 per 1000 | ||||
| Moderate | |||||
| 837 per 1000 | 837 per 1000 | ||||
| Use of birth control methods (consistent condom use) | Study population | RR 1.21 | 1681 | ⊕⊕⊝⊝ | |
| 353 per 1000 | 427 per 1000 | ||||
| Moderate | |||||
| 476 per 1000 | 575 per 1000 | ||||
| Sexually Transmitted Diseases | Study population | RR 0.89 | 699 | ⊕⊝⊝⊝ | |
| 191 per 1000 | 170 per 1000 | ||||
| Moderate | |||||
| 270 per 1000 | 241 per 1000 | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1 Downgraded by 1 for risk of bias; several assessments were unclear due to no information provided. Such potential limitations are likely to lower confidence in the estimate of effect 2 Downgraded by 1 for imprecision; low number of events, confidence interval includes appreciable benefit and null value 3 Heterogeneity could be explained (difference in comparison intervention and length of follow up) 4 Downgraded by 1 for imprecision: confidence interval includes appreciable benefit 5 Downgraded by 1 for inconsistency: unexplained large variations in effect 6 Confidence interval includes the null value, however, the sample size and number of events are fairly large and confidence interval is relatively narrow 7 Downgraded by 1 for imprecision: confidence interval includes appreciable benefit and harm 8 Downgraded by 1 for imprecision; low number of events, confidence interval includes appreciable benefit and harm | |||||
| Intervention | Outcome | Study ID | Number Assessed | Case affected | Control affected | Test Statistics | 95% CI | p‐value |
| Educational intervention | Pregnancy | 1701 | ‐ | ‐ | OR: 0.97 | 0.93 to 1.0 | 0.04 | |
| Initiation of intercourse | 156 | ‐ | ‐ | Beta: 1.604 and SE: 1.00 | ‐ | < 0.11 | ||
| Aarons 2000 (females) | 139 | Adj. OR: 1.88 | 1.02 to 3.47 | 0.04 | ||||
| Aarons 2000 (males) | 123 | Adj. OR: 1.18 | 0.61 to 2.29 | 0.62 | ||||
| 1079 | ‐ | ‐ | OR: 1.00 | 0.70 to 1.41 | ||||
| Changes in knowledge and attitudes about the risk of unintended pregnancy | 351 | 92.9% | 91.8% | ns | ||||
| Use of birth control at last sex | Mitchell‐DiCenso 1997 (females) | 109 | 42.2% | 46.7% | OR: 1.03 | 1.00 to 1.07 | 0.03 | |
| Mitchell‐DiCenso 1997 (males) | 214 | 39.3% | 35.9% | OR: 1.06 | 1.02 to 1.77 | 0.005 | ||
| Aarons 2000 (females) | 135 | Adj. OR: 3.39 | 1.16 to 9.95 | 0.025 | ||||
| Aarons 2000 (males) | 125 | Adj. OR: 1.53 | 0.55 yo 4.26 | 0.42 | ||||
| Use of condom at last sex | 1896 | 39.1% | 31.9% | OR: 1.41 | 1.12 to 1.77 | ‐ | ||
| 221 | 77% | 73% | ||||||
| Unprotected intercourse in the past 3 monthsa | 502 | Beta: ‐0.375 and SE: 0.32 | >0.05 | |||||
| Ever had sex without condoms | Mean: 0.23 | Mean: 0.57 | ‐0.61 to ‐0.06 | 0.03 | ||||
| Multiple interventions | Pregnancy | 308 | ‐ | ‐ | OR; 0.84 | ‐ | 0.61 | |
| 460 | ‐ | ‐ | OR: 0.53 | 0.27 to 1.03 | 0.06 | |||
| 1172 | 2.3% | 3.3% | ‐ | ‐ | 0.07 | |||
| 2145 | ‐ | ‐ | OR: 1.34 | 0.98 to 1.84 | 0.07 | |||
| 417 | ‐ | ‐ | OR: 0.77 | 0.49 to 1.23 | 0.28 | |||
| 95 | ‐ | ‐ | ‐ | ‐ | < 0.05 | |||
| 195 | 6.8% | 18.5% | ||||||
| 323 | B=‐.823 OR: 0.44 | 0.009 | ||||||
| 560 | ‐ | ‐ | OR: 0.41 | ‐ | ‐ | |||
| Initiation of sexual intercourse (mixed gender) | 94 | ‐ | ‐ | OR: 1.23 | 0.51 to 2.97 | 0.65 | ||
| 95 | .Mean: 1.19 | .Mean: 2.74 | ||||||
| 8326 | ‐ | ‐ | OR: 1.03 | 0.88 to 1.21 | 0.69 | |||
| 627 | AOR:0.65 | 0.54,0.77 | <.01 | |||||
| 195 | 40.1% | 66.1% | OR: 0.39 | 0.20 to 0.76 | 0.005 | |||
| 735 | AOR:0.82 | 0.51,1.34 | >0.05 | |||||
| 2565 | OR:1.13 SE: 0.24 | 0.71 to 1.82 | 0.60 | |||||
| Initiation of sexual intercourse (male) | 1412 | 19.3% | 27.7% | model R2: 0.118 | ‐ | 0.02 | ||
| 809 | ‐ | ‐ | OR: 1.08 | 0.80 to 1.46 | 0.63 | |||
| 8156 | 32.7% | 31.1% | OR: 0.90 | 0.65 to 1.23 | 0.35 | |||
| 408 | 36% | 44% | ‐ | ‐ | ‐ | |||
| Initiation of sexual intercourse (female) | 1417 | 20.3% | 22.1% | model R2: 0.145 | ‐ | 0.53 | ||
| 1220 | ‐ | ‐ | OR: 0.88 | 0.59 to 1.31 | 0.54 | |||
| 8156 | 34.7% | 40.8% | OR: 0.80 | 0.66 to 0.97 | 0.008 | |||
| 480 | 27% | 22% | ‐ | ‐ | ‐ | |||
| Use of condoms at last sex | 2145 | ‐ | ‐ | OR: 1.38 | 1.06 to 1.79 | 0.02 | ||
| 359 | ‐ | ‐ | OR: 1.00 | 0.49 to 1.23 | 0.99 | |||
| 460 | ‐ | ‐ | OR: 3.94 | 2.58 to 6.03 | < .001 | |||
| 258 | ‐ | ‐ | OR: 2.13 | ‐ | 0.15 | |||
| 198 | OR: 0.93 | ‐0.75,0.62 | 0.85 | |||||
| 1018 | OR:191 SE:0.27 | 1.13 to 3.21 | 0.02 | |||||
| Childbirth | 4196 | 300/1000 | 274/1000 | OR: 14.6 | 0.32 | |||
| Abortion | 4196 | 127/1000 | 112/1000 | OR: 26.4 | 0.40 | |||
| Consistent condom use at 12 months | 253 | Mean: 0.96 (116/126) | Mean: 0.66 (81/127) | ARR:145 | 1.26 to 1.67 | 0.00 | ||
| Consistent condom use at 24 months | 204 | Mean:1.53 | Mean: 0.93 | ARR: 1.57 | 1.28,1.94 | |||
| Consistent hormonal contraceptive use at 12 months | 253 | Mean: 4.27 (74/126) | Mean: 2.91 (51/127) | ARR:1.46 | 1.13 to 1.89 | 0.00 | ||
| Consistent hormonal contraceptive use at 24 months | 203 | Mean: 3.29 | Mean: 2.34 | ARR: 1.30 | 1.06,1.58 | |||
| 162 | OR:0.42 | 0.12 | ||||||
| Use of condoms at first sex | 285 | OR:0.68 SE:0.48 | 0.26 to 1.75 | 0.42 | ||||
| Protected against pregnancy at last sex | 998 | OR:1.62 SE:0.22 | 1.05 to 2.50 | 0.03 | ||||
| Sexually Transmitted Infections | 323 | B=‐0.067 OR: ‐0.94 | 0.77 | |||||
| Mean:10.5 SE: 2.9 | Mean:18.2 SE:2.8 | 0.05 | ||||||
| Baird 2010: The following listed outcomes were reported. However, the method of reporting made difficult to extract correct estimates. 1. Pregnancy School girls and dropouts among the treatment group are 1.1 percentage points less likely to have become pregnant over the past year. Not statistically significant. | ||||||||
| a ‐ Binary outcome (did unprotected intercourse occur or not?) b ‐ Study (Stephenson 2008) same as Stephenson 2004, but with an extended follow up (7yrs) c ‐ Data comparing skills‐based intervention versus health‐promotion intervention Analyses assessing impact on delay of sexual initiation excluded individuals who reported any type of sexual intercourse at baseline Analyses assessing impact on other on sexual behaviours are limited to individuals that are sexually active ns ‐ non‐significant | ||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Unintended pregnancy [individually randomised trials] Show forest plot | 4 | 1905 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.50, 0.87] |
| 2 Unintended pregnancy [cluster‐randomised trials] Show forest plot | 5 | 3149 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.23, 1.09] |
| 3 Initiation of sexual intercourse ‐ individually RCT Show forest plot | 4 | 1796 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.74, 1.32] |
| 4 Initiation of sexual intercourse ‐ cluster RCT Show forest plot | 7 | 8608 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.68, 1.04] |
| 5 Use of birth control methods ‐ individually RCT Show forest plot | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Condom use in last sex | 3 | 796 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.95, 1.06] |
| 5.2 Consistent condom use | 5 | 1681 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.95, 1.54] |
| 5.3 Contraceptive use at last sex | 1 | 408 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.95, 1.03] |
| 5.4 Consistent contraceptive use | 1 | 253 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [1.06, 1.59] |
| 6 Use of birth control methods ‐ cluster RCT Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 Condom use at last sex | 4 | 2620 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.93, 1.09] |
| 6.2 Consistent condom use | 3 | 826 | Risk Ratio (M‐H, Random, 95% CI) | 1.95 [0.70, 5.44] |
| 6.3 Hormonal contraceptives | 3 | 3987 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.72, 1.43] |
| 7 Sexually Transmitted Diseases ‐ individually RCT Show forest plot | 2 | 699 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.65, 1.22] |
| 8 Sexually Transmitted Diseases ‐ cluster RCT Show forest plot | 2 | 420 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.27, 2.14] |
| 9 Childbirth ‐ cluster RCT Show forest plot | 1 | 4776 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.52, 0.79] |
| 10 Childbirth ‐ individually RCT Show forest plot | 1 | 484 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.31, 1.45] |
| 11 Second unintended pregnancy ‐ individually RCT Show forest plot | 1 | 149 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.22, 1.02] |
| 12 Abortion (cluster RCT) Show forest plot | 1 | 4776 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.72, 1.21] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Unintended pregnancy ‐ cluster‐randomi sed trials Show forest plot | 2 | 497 | Risk Ratio (M‐H, Random, 95% CI) | 0.20 [0.10, 0.39] |
| 2 Unintended pregnancy ‐ individually‐randomi sed trials Show forest plot | 3 | 1421 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.46, 1.00] |
| 3 Unintended pregnancy ‐ cluster‐adjusted + individual Show forest plot | 5 | 1918 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.39, 0.72] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Initiation of sexual intercourse ‐ individually RCT Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Gender mixed or not specified | 3 | 1312 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.67, 2.09] |
| 2 Initiation of sexual intercourse ‐ cluster RCT Show forest plot | 4 | 1687 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.57, 1.25] |
| 2.1 Gender mixed or not specified | 4 | 1687 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.57, 1.25] |
| 3 Initiation of sexual intercourse ‐ cluster‐adjusted + individual Show forest plot | 7 | 2999 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.74, 1.05] |
| 3.1 Gender mixed or not specified | 7 | 2999 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.74, 1.05] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Initiation of sexual intercourse ‐ cluster RCT Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Gender mixed or not specified | 2 | 672 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.71, 1.27] |
| 2 Use of birth control methods ‐ cluster RCT Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 condom use at last sex | 2 | 1431 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [1.06, 1.32] |
| 3 Use of contraceptives ‐ individually RCT Show forest plot | 1 | 360 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.5 [1.39, 4.48] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Unintended pregnancy ‐ individually RCT Show forest plot | 2 | 3440 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.81, 1.26] |
| 2 Initiation of sexual intercourse ‐ cluster RCT Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Female | 1 | 1446 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.76, 1.04] |
| 2.2 Male | 1 | 1560 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.87, 1.21] |
| 3 Use of birth control methods ‐ cluster RCT Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Hormonal contraceptives | 1 | 415 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.69, 1.18] |
| 4 Use of birth control methods ‐ individually RCT Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Condom use in last sex | 2 | 3091 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.87, 1.04] |
| 4.2 Consistent condom use | 1 | 1950 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.71, 1.15] |
| 4.3 Hormonal contraceptives | 2 | 3091 | Risk Ratio (M‐H, Random, 95% CI) | 2.22 [1.07, 4.62] |
| 5 Sexually Transmitted Diseases ‐ individually RCT Show forest plot | 2 | 3440 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.75, 1.13] |

