生殖補助医療で採卵を受ける女性に対する鎮痛
References
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomisation: random numbers Allocation concealment: sealed in consecutive envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 50 No. analysed: 50 Intention‐to‐treat analysis: yes Power and sample calculations not described Duration of trial: not stated | |
| Participants | Women scheduled for oocyte retrieval Mean age: 34 years; cause of infertility not reported Similar baseline characteristics of age, height, and weight | |
| Interventions |
No premedication in either group | |
| Outcomes |
Other outcomes reported: no. of oocytes retrieved, cleavage rate, arousability, response to painful stimuli | |
| Notes | Israel Single centre HaEmek Mecical Centre Funding: not stated Definition of pregnancy not documented | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed envelopes |
| Blinding (performance bias and detection bias) | Unclear risk | Blinding not possible because of the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) | Low risk | No apparent dropout |
| Selective reporting (reporting bias) | Low risk | All pre‐stated outcomes reported |
| Other bias | Unclear risk | Comparable baseline characteristics of age, height, and weight but not cause of infertility |
| Methods | Randomisation: computer‐generated random numbers Allocation concealment: sealed in consecutively numbered envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 81 No. analysed: 81 Intention‐to‐treat analysis: yes Power and sample calculations described Duration of trial: not stated | |
| Participants | Women undergoing vaginal oocyte recovery Mean age: 33 years Mean duration of infertility 5.5 years; 26% tubal disease Similar baseline demographic and infertility characteristics | |
| Interventions |
All women received a preliminary IV loading dose of midazolam 4 mg. | |
| Outcomes |
Other outcomes reported: perioperative blood pressure, pulse, oxygen, doses of fentanyl | |
| Notes | Scotland Single centre Aberdeen University Funding: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed numbered envelopes |
| Blinding (performance bias and detection bias) | Unclear risk | Blinding not possible because of the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
| Methods | Randomisation: method unclear Allocation concealment: sealed envelopes Blinding of participants/investigators: no Blinding of assessors: yes No. randomised: 47 No. analysed: 47 Intention‐to‐treat analysis: yes Power and sample calculations: not reported Duration of trial: not stated | |
| Participants | Women presenting for transvaginal oocyte retrieval Mean age and weight similar in both groups (no data given) Cause of infertility: not reported Comparison of baseline characteristics: age/weight only | |
| Interventions |
IV alfentanil administered at 3 points: before insertion of vaginal speculum, before needle entry into each ovary, on request | |
| Outcomes | Secondary: patient satisfaction (VAS), adverse outcomes Other outcomes reported: sedation levels, psychometric tests | |
| Notes | England Single centre London University Funding: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Methods unclear |
| Allocation concealment (selection bias) | Low risk | Adequate, sealed envelopes |
| Blinding (performance bias and detection bias) | Unclear risk | Blinding not feasible because of the different appearance of drugs Assessors blind |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Comparable baseline characteristics of age and weight but not cause of infertility |
| Methods | Randomisation: computer‐generated Allocation concealment: quote "enclosed" numbers Blinding of participants/investigators: no Blinding of assessors: yes (for postop side effects) No. randomised: 69 No. analysed: 69 Intention‐to‐treat analysis: yes Power and sample calculations: described Duration of trial: not stated | |
| Participants | Women scheduled for transvaginal oocyte retrieval Mean age: 33 to 35 years Cause of infertility: not reported Comparison of baseline characteristics: age, weight, and height only Similar demographic characteristics at baseline | |
| Interventions |
TCI = A system that maintains a particular target plasma drug concentration via standard pharmacokinetic equations | |
| Outcomes |
Other outcomes reported: sedation score, amount of sedation required, recovery score, blood pressure | |
| Notes | Turkey Single centre Gazi University Funding: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Low risk | Quote "enclosed" numbers |
| Blinding (performance bias and detection bias) | Unclear risk | Blinding not reported Blinding of assessors for postop side effects only |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Comparable baseline characteristics of age, height, and weight but not cause of infertility |
| Methods | Ransomisation: method unclear Allocation concealment: serially numbered, sealed opaque envelopes Blinding of participants/investigators: yes Blinding of assessors: not reported No. randomised: 52 No. analysed: 52 Intention‐to‐treat analysis: awaiting response from trial author Power and sample calculations described Duration of trial: from September 2014 to April 2015 | |
| Participants | Women with ASA I/II undergoing ultrasound‐guided oocyte retrieval in an IVF programme Mean age: 25 to 38 years Cause of infertility: tubal disease, endometriosis, anovulation, male factor, unexplained Similar demographic (age, height, weight, BMI) and infertility characteristics at baseline Inclusion criteria: women in their first IVF cycle and showing bilateral ovarian follicular response Exclusion criteria: psychological abnormalities; cardiorespiratory, renal, or liver disease; requesting general anaesthesia; fewer than 3 dominant follicles present in either ovary; chronic alcohol/drug abusers; allergic to any of the medications used in the study | |
| Interventions | 1. Intervention 1: IV fentanyl (1 µg/kg) plus paracervical block (100 mg lidocaine 1%) plus IV dexmedetomidine (1 µg/kg) (N = 26) 2. Intervention 2: IV fentanyl (1 µg/kg) plus paracervical block (100 mg lidocaine 1%) plus IV midazolam (0.06 mg/kg) (N = 26) | |
| Outcomes |
Other outcomes reported: intraoperative vital signs, no. of oocytes obtained, embryos transferred per woman, amount of rescue propofol used | |
| Notes | Egypt University Hospital No funding received | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method unclear |
| Allocation concealment (selection bias) | Low risk | Adequate: serially numbered and sealed opaque envelopes |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind (investigators and participants) Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) | Low risk | No losses to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
| Methods | Randomisation: computer‐generated list Allocation concealment: unclear Blinding of participants/investigators: yes Blinding of assessors: yes No. randomised: 160 No. analysed: 158 Intention‐to‐treat analysis: reported both as intention‐to‐treat and ‘as per protocol’ Power and sample calculations described Duration of trial: 19 months, from March 2002 to October 2003 | |
| Participants | Women undergoing oocyte aspiration Mean age: 33 to 34 years (range 23 to 39 years) Cause of infertility: tubal factor, hormonal factor, endometriosis, male factor, unexplained Similar demographic and infertility characteristics at baseline | |
| Interventions | In a 1:1 ratio,
Control group received premedication (oral flunitrazepam 0.5 mg and rectal paracetamol 1 g); EA group did not receive premedication. | |
| Outcomes |
Other outcomes reported: well‐being, number of embryos transferred, pregnancy per cycle | |
| Notes | Sweden Single centre University Hospital Goteborg Funding: Research & Development Council, Goteborg and Bohuslan, the Hjarmar Sevensson Foundation, the Organon Foundation, the Wilhelm & Marina Lundgren's Foundation Loss to follow‐up (N = 2) in intervention group due to ovulation before aspiration and missing VAS assessment Definition of pregnancy not documented | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer randomisation |
| Allocation concealment (selection bias) | Unclear risk | Methods unclear |
| Blinding (performance bias and detection bias) | Low risk | Blinding of participants not feasible owing to the nature of the intervention Person who assessed the VAS blinded to the groups to which participants belonged Other midwives not involved in administering EA assisted in the analgesia procedure during oocyte retrieval. |
| Incomplete outcome data (attrition bias) | Low risk | Two lost to follow‐up. Data available for intention‐to‐treat and ‘per protocol’ |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
| Methods | Randomisation: computer generation Allocation concealment: method unclear Blinding of participants/investigators: no Blinding of assessors: yes No. randomised: 65 No. analysed: 65 (IVF outcomes); 45 (satisfaction) Intention‐to‐treat analysis: yes for IVF outcomes, no for satisfaction outcomes Power and sample calculations not reported Duration of trial: 18 months, from March 1999 to September 2002 | |
| Participants | Women undergoing oocyte retrieval Age range 24 to 39 years Cause of infertility: not reported Similar baseline characteristics of age/height/weight | |
| Interventions |
No premedication given to any groups | |
| Outcomes |
Other outcomes reported: serum prolactin levels, follicular cortisol levels, oocyte recovery rate | |
| Notes | Spain Single centre Hospital Universitario La Paz, Madrid Funding: not stated Definition of pregnancy not documented Fourth group (non‐randomised) receiving remifentanil: data not used for the review Paper in Spanish | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Unclear risk | Methods unclear |
| Blinding (performance bias and detection bias) | Unclear risk | Blinding not possible owing to the nature of the interventions Analysis conducted by an independent person not involved in the trial Oocyte and fertilisation data collected by a blinded investigator |
| Incomplete outcome data (attrition bias) | Low risk | Complete for pain but incomplete for satisfaction |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Comparable baseline characteristics of age, height, and weight but not cause of infertility |
| Methods | Randomisation: methods unclear Allocation concealment: sealed envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 40 No. analysed: 40 Intention‐to‐treat analysis: yes Power and sample calculations briefly described Duration of trial: not stated | |
| Participants | Women scheduled to undergo transvaginal oocyte retrieval Mean age: 32 to 33 years Cause of infertility: not reported Similar baseline characteristics of age, height, and weight | |
| Interventions |
| |
| Outcomes |
Other outcomes reported: plasma remifentanil levels, pulmonary function | |
| Notes | Turkey Single centre Gazi University Funding: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Methods unclear |
| Allocation concealment (selection bias) | Low risk | Closed envelope allocation |
| Blinding (performance bias and detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Comparable baseline characteristics of age, height, and weight but not cause of infertility |
| Methods | Randomisation: computer‐generated Allocation concealment: sealed unlabelled envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 200 No. analysed: 200 Intention‐to‐treat analysis: yes Power and sample calculations described Duration of trial: 9 months, from April to December 2002 | |
| Participants | Women in IVF programme undergoing transvaginal oocyte retrieval Mean age: 31 to 32 years (range 22 to 39) Cause of infertility: male, tubal disease, endometriosis, anovulation, unexplained Similar demographic and infertility characteristics at baseline | |
| Interventions |
Conscious sedation and analgesia group received premedication (oral benzodiazepine 10 mg); EA group did not | |
| Outcomes |
Other outcomes reported: no. of cycles, no. of embryos transferred, implantation rate | |
| Notes | Denmark Single centre Skiive Hospital Funding: not stated Definition of pregnancy not documented | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed unlabelled envelopes |
| Blinding (performance bias and detection bias) | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
| Methods | Randomisation: computer‐generated list Allocation concealment: not reported Blinding of participants/investigators: open‐label design, study not blind to participants nor to physicians and investigators Blinding of assessors: open‐label design, study not blind to participants nor to physicians and investigators No. randomised: 76 No. analysed: 76 Intention‐to‐treat analysis: yes Power and sample calculations described Duration of trial: 5 days after oocyte retrieval; duration of treatment: from 8 to 8.4 minutes | |
| Participants | Women who had an indication for IVF/intracytoplasmic sperm injection (ICSI) Mean age: 35 ± 5 years Mean BMI: 24 ± 4 Causes of infertility (primary, secondary, endometriosis): similar in both groups IVF or ICSI: similar in both groups No. of previous cycles: similar in both groups | |
| Interventions | 1. Control: patient‐controlled analgesia with IV remifentanil (0.5 µg/kg per bolus) via a pump; diclofenac suppository 50 mg given 30 minutes before remifentanil (N = 36) 2. Intervention: anaesthetist‐administered standard pethidine therapy with IM pethidine (2 mg/kg body weight) and midazolam (5 mg per os), given 30 minutes before oocyte retrieval; no diclofenac suppository given (N = 40) Both groups received atropine 0.5 mg IM 30 minutes before oocyte retrieval. | |
| Outcomes | 1. Primary: intraoperative and postoperative pain via NRS (numeric rating scale) 2. Secondary: ongoing pregnancy rate, side effects of analgesia, postoperative complications, patient satisfaction | |
| Notes | The Netherlands University Medical Centre Funding: VU University Medical Center (registered at the Netherlands Trial Registration (NTR 2431)) Pregnancy defined by positive foetal cardiac activity at 12 weeks' gestation on ultrasound | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | Unclear risk | Open‐label design, not blinded |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
| Methods | Randomisation: computer‐generated Allocation concealment: sealed opaque envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 110 No. analysed: 106 Intention‐to‐treat analysis: no Power and sample calculations described Duration of trial: not stated | |
| Participants | Women undergoing transvaginal oocyte retrieval Mean age: 33 to 35 years Cause of infertility: tubal disease, male factor, endometriosis, anovulation, unexplained Women in control group 2 years younger than women in intervention group (P = 0.01); other baseline characteristics similar | |
| Interventions |
No premedication in either group | |
| Outcomes |
| |
| Notes | China Single centre Chinese University of Hong Kong Funding: not stated Loss to follow‐up (N = 4) in intervention group due to pump failure (n = 1) and personal reasons (n = 3) Definition of pregnancy not documented | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed envelopes |
| Blinding (performance bias and detection bias) | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Four lost to follow‐up (3%) |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Significant differences in age between the 2 groups Comparable infertility characteristics at baseline |
| Methods | Randomisation: random numbers table Allocation concealment: methods unclear Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 80 No. analysed: 80 Intention‐to‐treat analysis: yes Power and sample calculations not described Duration of trial: 8 months from February to September 2006 | |
| Participants | Women undergoing oocyte retrieval Mean age: 31 to 33 years Cause of infertility: tubal disease, PCOS, endometriosis, male factor, unexplained Similar demographic and infertility characteristics at baseline | |
| Interventions |
| |
| Outcomes |
Other outcomes reported: changes in blood pressure | |
| Notes | China Single centre Zhejiang University, Hangzhou, China Funding: not stated Paper in Chinese | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation table |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
| Methods | Randomisation: group allocation envelopes randomly selected by co‐investigators (additional information from trial author) Allocation concealment: group allocations in sealed envelopes kept in locked office (additional information from trial author) Blinding of participants/investigators: no, owing to the nature of the intervention Blinding of assessors: yes, assessors blind to group allocation (additional information from trial author) No. randomised: 58 No. analysed: 58 Intention‐to‐treat analysis: yes Power and sample calculations not described Duration of trial: not stated | |
| Participants | Women scheduled for ultrasound transvaginal oocyte retrieval Mean age 34 to 35.5 years Mean body weight: 62 kg Cause of infertility: 51 cases of primary infertility, 7 cases of secondary infertility Similar demographic and infertility characteristics at baseline | |
| Interventions | 1. Control: conscious sedation/analgesia with remifentanil (a bolus dose 1 μg.kg ‐1 of remifentanil administered slowly during 1 minute following by a continuous IV infusion at a rate of 0.15 to 0.4 μg.kg ‐1.min ‐1) (N = 29) 2. Intervention: general anaesthesia with IV propofol 2 mg.kg‐1 and alfentanil 15 μg.kg ‐1, maintained with propofol continuous infusion at a rate of 2 to 4 mg.kg ‐1.h ‐1 (N = 29). All participants unpremedicated and received midazolam 2 mg IV just before start of the procedure | |
| Outcomes | Secondary: clinical pregnancy rate, fertilisation rate, side effects, postoperative complications, patient satisfaction Other outcomes reported: implantation and cleavage rates | |
| Notes | Greece Single centre University Hospital Funding: not stated Definition of pregnancy: over 16 weeks of gestation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Group allocation envelopes randomly selected by co‐investigators |
| Allocation concealment (selection bias) | Low risk | Group allocations in sealed envelopes kept in locked office (additional information from trial author) |
| Blinding (performance bias and detection bias) | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) | Low risk | No apparent loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
| Methods | Randomisation: random numbers table Allocation concealment: method unclear Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 316 No. analysed: 316 Intention‐to‐treat analysis: yes Power and sample calculations not reported Duration of trial: 5 months, from March to July 2007 | |
| Participants | Women undergoing transvaginal oocyte retrieval Mean age: 31 years (23 to 46 years) Cause of infertility: tubal disease, PCOS, endometriosis, male factor, unexplained Similar demographic and infertility characteristics at baseline | |
| Interventions |
| |
| Outcomes |
Other outcomes reported: changes in pulse and blood pressure | |
| Notes | China Single centre Nanjing university of TCM Funding: not stated Paper in Chinese | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation table |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | Unclear risk | Blinding not possible owing to the nature of the interventions Assessors blinded to group allocation |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
| Methods | Randomisation: random number table Allocation concealment: methods unclear Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 700 No. analysed: 694 Intention‐to‐treat analysis: no Power and sample calculations not reported Duration of trial: 8 months, from June 2007 to January 2008 | |
| Participants | Women undergoing transvaginal oocyte retrieval Mean age: 30 to 31 years Cause of infertility: not reported, duration of infertility < 5 years Similar demographic and infertility characteristics at baseline | |
| Interventions |
| |
| Outcomes | Primary: pain (unclear whether intraoperative or postoperative) according to pain thresholds | |
| Notes | China Single centre Nanjing University of TCM Funding: not stated No reason given for dropout (N = 6) Paper in Chinese | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation table |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Six lost to follow‐up (2 in control group; 4 in intervention group), no reason given |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
| Methods | Randomisation: computer‐generated Allocation concealment: sealed envelopes Blinding of participants/investigators: yes Blinding of assessors: yes No. randomised: 150 No. analysed: 150 Intention‐to‐treat analysis: yes Power and sample calculations described Duration of trial: not stated | |
| Participants | Women undergoing egg collection Mean age: 35 years (range 27 to 43 years) Cause of infertility: tuboperitoneal, male factor, endometriosis, unexplained Similar demographic and infertility characteristics at baseline | |
| Interventions |
Both groups received premedication (IM pethidine 50 mg and promethazine 25 mg) | |
| Outcomes |
Other outcomes reported: no. of embryos transferred, implantation rate, multiple pregnancy rate | |
| Notes | China Single centre University of Hong Kong Funding: not stated Definition of pregnancy not documented | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed envelopes |
| Blinding (performance bias and detection bias) | Low risk | Both participant and doctor carrying out the procedure were blind to the sedation given Nurses not involved in the Unit asked participants about pain levels |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
| Methods | Randomisation: method unclear Allocation concealment: method unclear Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 58 No. analysed: 58 Intention‐to‐treat analysis: yes Power and sample calculations not reported Duration of study: not stated | |
| Participants | Women admitted for vaginal oocyte retrieval Mean age: 31 to 33 years (range 25 to 41 years) Cause of infertility: not reported Similar baseline characteristics of age | |
| Interventions |
| |
| Outcomes | Primary: intraoperative pain score (Likert scale) | |
| Notes | Turkey Single centre Istanbul University Funding: not stated Paper in Turkish | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method unclear |
| Allocation concealment (selection bias) | Unclear risk | Method unclear |
| Blinding (performance bias and detection bias) | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) | Low risk | No apparent loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Comparable age but not cause of infertility
|
| Methods | Randomisation: method unclear Allocation concealment: sealed envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 100 No. analysed: 100 Intention‐to‐treat analysis: yes Power and sample calculations not reported Duration of study: not stated | |
| Participants | Women scheduled to undergo transvaginal oocyte retrieval Mean age: 33 to 35 years Cause of infertility: tuboperitoneal, male factor, anovulation, unexplained Similar demographic and infertility characteristics at baseline | |
| Interventions |
All women not premedicated | |
| Outcomes |
Other outcomes reported: remifentanil consumption, duration of anaesthesia, duration of procedure, no. of oocytes retrieved, retrieval rate | |
| Notes | Turkey Single centre Gazi University, Ankara Funding: not stated Definition of pregnancy not documented | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method unclear |
| Allocation concealment (selection bias) | Low risk | Closed envelope |
| Blinding (performance bias and detection bias) | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) | Low risk | No apparent loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
| Methods | Randomisation: by pharmacy Allocation concealment: sealed envelopes kept in medicine cupboard Blinding of participants/investigators: yes Blinding of assessors: no No. randomised: 30 No. analysed: 24 Intention‐to‐treat analysis: no Power and sample calculations not reported Duration of trial: 1 month, July 1989 | |
| Participants | Women undergoing follicular aspiration Mean age: not reported Cause of infertility: not reported Baseline characteristics comparison not reported | |
| Interventions |
| |
| Outcomes | Primary: intraoperative pain (VAS) | |
| Notes | England Single centre Sheffield Univerity Funding: not stated 6 women (20%) excluded after randomisation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation by pharmacy |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed envelope |
| Blinding (performance bias and detection bias) | Unclear risk | Neither medical and nursing personnel nor the patient knew which ampoule was used Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) | High risk | 6 women (20%) lost to follow‐up, reasons given |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Baseline demographic and infertility characteristics comparison not reported |
| Methods | Randomisation: computer‐generated Allocation concealment: method unclear Blinding of participants/investigators: yes Blinding of assessors: yes No. randomised: 94 No. analysed: 93 Intention‐to‐treat analysis: no Power and sample calculations described Duration of trial: 7 months, from April to December 2004 | |
| Participants | Women undergoing oocyte aspiration Mean age: 33 to 34 years Cause of infertility: male factor, tubal disease, endometriosis, PCOS, unexplained Similar demographic and infertility characteristics at baseline | |
| Interventions | Randomised in proportions of 1:1:1 to control and 2 interventions
All participants received IV metamizole 1 g 15 minutes before procedure. | |
| Outcomes | Primary: intraoperative and postoperative pain scores (VAS 0 to 100) | |
| Notes | Austria Single centre Medical University of Vienna Funding: not stated Definition of pregnancy not documented | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Methods unclear |
| Blinding (performance bias and detection bias) | Low risk | Participants and investigators blinded to the randomisation A second gynaecologist performed oocyte retrieval, and another doctor asked for outcome parameters to ensure blinding. |
| Incomplete outcome data (attrition bias) | Low risk | One participant in control group excluded owing to impaired compliance |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
| Methods | Randomisation: random number table Allocation concealment: sealed envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 150 No. analysed: 149 Intention‐to‐treat analysis: no Power and sample calculations not reported Duration of trial: 8 months, from September 1996 to May 1997 | |
| Participants | Women undergoing oocyte aspiration Mean age: 33 to 34 years (range 35 to 46 years) Cause of infertility: male factor, tubal disease, endometriosis, unexplained Similar demographic and infertility characteristics at baseline | |
| Interventions |
No premedication in either group | |
| Outcomes |
| |
| Notes | Sweden Multi‐centre (3 IVF centres) Goteburg University Funding: Foundation for Acupuncture and Alternative Biological Treatment Methods, and the Swedish Research Council PCB (10 mL lidocaine): given at 5 mg/mL at one IVF centre and at 10 mg/mL at the other 2 IVF centres One participant in the control group (0.7%) was excluded after randomisation because of protocol violation (received premedication) Definition of pregnancy not documented | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Each centre used its own randomisation. Method: random numbers table |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed envelopes |
| Blinding (performance bias and detection bias) | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) | Low risk | One participant lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
| Methods | Randomisation: in blocks of 20 to each group, random numbers table Allocation concealment: sealed unlabelled envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 286 No. analysed: 274 Intention‐to‐treat analysis: no Power and sample calculations described Duration of trial: from 1999 to 2001 | |
| Participants | Women undergoing oocyte aspiration Mean age: 33 years (range 22 to 38 years) Cause of infertility: male factor, tubal disease, endometriosis, PCOS, unexplained Similar demographic and infertility characteristics at baseline | |
| Interventions |
No premedication in either group | |
| Outcomes |
| |
| Notes | Sweden Multi‐centre (5 IVF centres) Goteburg University Funding: Hjalmar Svensson's Foundation, the Wilhelm and Martina Lundgren's Foundation Twelve women (4%) dropped out (7 in control group, 5 in intervention group): Definition of pregnancy not documented | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Each centre used its own randomisation Method: random numbers table |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed envelopes |
| Blinding (performance bias and detection bias) | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | 12 participants lost to follow‐up (4%) |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
| Methods | Randomisation: computer‐generated Allocation concealment: sealed opaque envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 112 No. analysed: 112 Intention‐to‐treat analysis: yes Power and sample calculations described Duration of trial: not stated | |
| Participants | Women undergoing outpatient oocyte recovery Mean age: 32 to 34 years Cause of infertility: not reported Similar baseline characteristics of age, height and weight, and history of previous oocyte recovery | |
| Interventions |
| |
| Outcomes |
| |
| Notes | Scotland Single centre Aberdeen University Funding: not stated Definition of pregnancy not documented | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed envelopes |
| Blinding (performance bias and detection bias) | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
| Methods | Randomisation: method unclear Allocation concealment: method unclear Blinding of participants/investigators: no Blinding of assessors: yes No. randomised: 80 No. analysed: 80 Intention‐to‐treat analysis: yes Power and sample calculations not reported Duration of trial: not stated | |
| Participants | Women presenting for outpatient oocyte retrieval Mean age: 32 to 34 years Cause of infertility: not reported Similar baseline characteristics of age, height, and weight | |
| Interventions |
All participants premedicated with midazolam 0.02 mg/kg | |
| Outcomes |
| |
| Notes | USA Single centre University of Texas Funding: Janssen‐Cilag | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method unclear |
| Allocation concealment (selection bias) | Unclear risk | Method unclear |
| Blinding (performance bias and detection bias) | Unclear risk | Blinding not possible owing to the nature of the interventions Postoperative side effects recorded by staff unaware of treatment groups |
| Incomplete outcome data (attrition bias) | Low risk | No apparent loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Comparable baseline characteristics of age, height, and weight but not cause of infertility |
Types of analgesic
Diazepam ‐ sedative and anxiolytic
Diclofenac suppository ‐ analgesic
Dolantin ‐ analgesic, same as pethidine
Electro‐acupuncture ‐ pain‐relieving method that activates endogenous pain‐inhibiting systems such as the spinal/segmental gate mechanism and the endogenous opoid systems. Any acupuncture effect rests on physiological and/or psychological mechanisms
Fentanyl/alfentanil/remifentanil ‐ analgesia
Isodesox ‐analgesic and sedative inhalational agent
Midazolam ‐ sedative and anxiolytic
Pethidine ‐ analgesic
Pirosikam ‐ analgesic (non‐steroidal anti‐inflammatory drug ‐ NSAID)
Propofol ‐ sedative and anxiolytic
Abbreviations
ASA = American Society of Anesthesiologists
BMI = body mass index
EA = electro‐acupuncture
IM = intramuscular
IV = intravenous
IVF = in vitro fertilisation
µg = microgram
mg = milligram
mg/kg = milligrams per kilogram
min = minute
mL = millilitre
no. = number
PCB = paracervical block. This involves injecting local anaesthetic adjacent to the cervix. Epidural analgesia involves injecting local anaesthetic into the epidural space close to the spinal cord to numb the lower part of the body
PCS = patient‐controlled sedation and analgesia
PAS = physician‐administered sedation and analgesia
PCOS = polycystic ovary syndrome
TCI = system that maintains a particular target plasma drug concentration via standard pharmacokinetic equations
VAS = visual analogue scale, usually a 100‐mm linear analogue scale
yr = year
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Unable to obtain evidence of randomisation | |
| Conscious sedation and analgesia not one of the comparators | |
| Conscious sedation and analgesia not one of the comparators | |
| Conscious sedation and analgesia not one of the comparators | |
| Conscious sedation and analgesia not one of the comparators | |
| Conscious sedation and analgesia not one of the comparators | |
| Unable to obtain evidence of randomisation | |
| General anaesthesia. Conscious sedation not one of the comparators | |
| Conscious sedation and analgesia among low‐ and high‐anxiety patients. No comparison with another technique | |
| Spinal anaesthesia dose finding. Conscious sedation and analgesia not one of the comparators | |
| Spinal anaesthesia. Conscious sedation and analgesia not one of the comparators | |
| Subperitoneal xylocaine. Spinal anaesthesia dose finding. Conscious sedation and analgesia not one of the comparators | |
| Paracervical block with lignocaine vs normal saline vs no paracervical block. Conscious sedation and analgesia not one of the comparators | |
| Paracervical block dose finding. Conscious sedation and analgesia not one of the comparators | |
| Premedication versus no premedication. Conscious sedation and analgesia not one of the comparators | |
| Paracervical block dose finding. Conscious sedation and analgesia not one of the comparators | |
| Conscious sedation and analgesia not one of the comparators | |
| Conscious sedation and analgesia not one of the comparators | |
| Conscious sedation and analgesia not one of the comparators | |
| Conscious sedation and analgesia not one of the comparators | |
| Population not clarified. No response from trial author when contacted | |
| Unable to obtain evidence of randomisation | |
| Spinal anaesthesia. Conscious sedation not one of the comparators | |
| Paracervical block vs vaginal anaesthetic cream. Conscious sedation and analgesia not one of the comparators | |
| Conscious sedation and analgesia not one of the comparators |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Randomisation: random numbers table used to divide into 2 groups Allocation concealment: not reported Blinding of participants/investigators: not reported Blinding of assessors: not reported No. randomised: 134 No. analysed: 134 Intention‐to‐treat analysis: yes Power and sample calculations: not described Duration of trial: not stated |
| Participants | Patients undergoing IVF‐E |
| Interventions | 1. Control: intramuscular (IM) Dolantin 50 milligrams (mg) 30 minutes before oocyte retrieval (N = 67) 2. Intervention: IM Dolantin 50 mg 30 minutes before electro‐acupuncture (N = 67) |
| Outcomes | 1. Primary: intraoperative pain (World Health Organization pain scale: Grade I (scores 1 to 3, minimal pain), Grade II (scores 4 to 6, mild pain), Grade III (scores 7 to 9, moderate pain), Grade IV (scores 10 to 12, severe pain)): postoperative (1 hour (h), 2 hours postoperatively) abdominal pain 2. Secondary: side effects of analgesia |
| Notes | China Reproductive Medicine Centre Funding: Gansu Province Paper in Chinese NB. Data unclear, awaiting response from trial authors |
IM = intramuscular
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | A randomised controlled trial of oral acetaminophen for analgesic control after transvaginal oocyte retrieval |
| Methods | Double‐blind randomised controlled trial |
| Participants | Women undergoing IVF |
| Interventions | Transvaginal oocyte retrieval |
| Outcomes | Post‐procedure pain |
| Starting date | Not clear |
| Contact information | Email of co‐author: [email protected] |
| Notes | Conference abstract published 2015. Trial authors/co‐authors contacted, no response |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain during needle insertion (VAS 0 to 10) Show forest plot | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐1.70 [‐2.38, ‐1.02] |
| Analysis 1.1  Comparison 1 Conscious sedation + analgesia (CSA) versus placebo, Outcome 1 Pain during needle insertion (VAS 0 to 10). | ||||
| 2 Pain during follicle aspiration (VAS 0 to 10) Show forest plot | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐1.30 [‐1.88, ‐0.72] |
| Analysis 1.2  Comparison 1 Conscious sedation + analgesia (CSA) versus placebo, Outcome 2 Pain during follicle aspiration (VAS 0 to 10). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intraoperative pain Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.1  Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 1 Intraoperative pain. | ||||
| 1.1 CSA vs CSA + acupuncture (VAS 0 to 10) | 1 | 62 | Mean Difference (IV, Random, 95% CI) | 1.0 [0.18, 1.82] |
| 1.2 CSA vs CSA + electro‐acupuncture (VAS 0 to 10) | 1 | 62 | Mean Difference (IV, Random, 95% CI) | 3.00 [2.23, 3.77] |
| 1.3 CSA vs CSA + electro‐acupuncture (Pain scale 1 to 12) | 1 | 316 | Mean Difference (IV, Random, 95% CI) | 1.70 [1.07, 2.33] |
| 2 Postoperative pain Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.2  Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 2 Postoperative pain. | ||||
| 2.1 CSA vs CSA + acupuncture (VAS 0 to 10) | 1 | 61 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [‐0.10, 1.30] |
| 2.2 CSA vs CSA + electro‐acupuncture (VAS 0 to 10) | 1 | 61 | Mean Difference (IV, Fixed, 95% CI) | 2.1 [1.40, 2.80] |
| 2.3 CSA vs general anaesthesia (Likert 0 to 3) | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | ‐1.90 [‐2.24, ‐1.56] |
| 3 Pregnancy Show forest plot | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.3  Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 3 Pregnancy. | ||||
| 3.1 CSA vs CSA + acupuncture | 1 | 61 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.20, 1.86] |
| 3.2 CSA vs CSA + electro‐acupuncture | 1 | 61 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.07, 0.66] |
| 3.3 CSA vs general anaesthesia | 2 | 108 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.43, 2.35] |
| 4 Postop vomiting and/or vomiting Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.4  Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 4 Postop vomiting and/or vomiting. | ||||
| 4.1 CSA vs CSA + acupuncture | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 CSA vs general anaesthesia | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Satisfaction Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.5  Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 5 Satisfaction. | ||||
| 5.1 CSA vs general anaesthesia | 2 | 108 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.11, 4.04] |
| 6 Postoperative complications (airway obstruction) Show forest plot | 1 | 58 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.02, 1.22] |
| Analysis 2.6 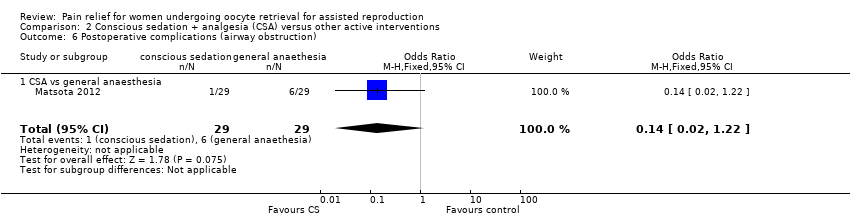 Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 6 Postoperative complications (airway obstruction). | ||||
| 6.1 CSA vs general anaesthesia | 1 | 58 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.02, 1.22] |
| 7 Postoperative complications (mask ventilation) Show forest plot | 1 | 58 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.01, 0.20] |
| Analysis 2.7  Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 7 Postoperative complications (mask ventilation). | ||||
| 7.1 CSA vs general anaesthesia | 1 | 58 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.01, 0.20] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intraoperative pain (VAS 0 to 10) Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.1  Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 1 Intraoperative pain (VAS 0 to 10). | ||||
| 1.1 CSA + paracervical block versus electro‐acupuncture + paracervical block | 4 | 781 | Mean Difference (IV, Fixed, 95% CI) | ‐0.66 [‐0.93, ‐0.39] |
| 2 Postoperative pain Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.2  Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 2 Postoperative pain. | ||||
| 2.1 CSA + paracervical block vs general anaesthesia | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 0.49 [‐0.13, 1.11] |
| 2.2 CSA + paracervical block vs spinal anaesthesia | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | 1.02 [0.48, 1.56] |
| 3 Live birth or ongoing pregnancy Show forest plot | 2 | 393 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.78, 1.86] |
| Analysis 3.3  Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 3 Live birth or ongoing pregnancy. | ||||
| 3.1 CSA + paracervical block vs electro‐acupuncture + paracervical block | 1 | 149 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.35 [1.09, 5.05] |
| 3.2 CSA + paracervical block vs electro‐acupuncture + paracervical block | 1 | 244 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.50, 1.47] |
| 4 Pregnancy Show forest plot | 7 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.4  Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 4 Pregnancy. | ||||
| 4.1 CSA + paracervical block vs general anaesthesia | 1 | 51 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.22, 2.26] |
| 4.2 CSA + paracervical block vs spinal anaesthesia | 1 | 38 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.24, 3.65] |
| 4.3 CSA + paracervical block vs paracervical block only | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.44, 1.96] |
| 4.4 CSA + paracervical block vs electro‐acupuncture + paracervical block | 4 | 783 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.72, 1.29] |
| 4.5 CSA + paracervical block vs CSA alone | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.28, 1.36] |
| 5 Fertilisation rate per woman Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.5  Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 5 Fertilisation rate per woman. | ||||
| 5.1 CSA + paracervical block vs paracervical block only | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.42, 1.66] |
| 6 Postoperative nausea and/or vomiting Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.6  Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 6 Postoperative nausea and/or vomiting. | ||||
| 6.1 CSA + paracervical block vs CS only | 2 | 140 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.18, 0.97] |
| 7 Patient satisfaction by Likert scale: report of 'excellent and satisfactory' Show forest plot | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.63 [0.68, 3.89] |
| Analysis 3.7  Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 7 Patient satisfaction by Likert scale: report of 'excellent and satisfactory'. | ||||
| 7.1 CSA + paracervical block vs paracervical block only | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.63 [0.68, 3.89] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intraoperative pain score (VAS 0 to 10) Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.1 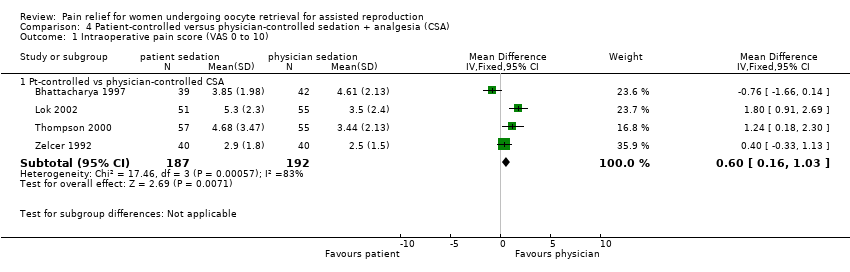 Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 1 Intraoperative pain score (VAS 0 to 10). | ||||
| 1.1 Pt‐controlled vs physician‐controlled CSA | 4 | 379 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.16, 1.03] |
| 2 Intraoperative pain score excluding inhalational sedation/analgesia (VAS 0 to 10) Show forest plot | 3 | 267 | Mean Difference (IV, Fixed, 95% CI) | 0.47 [‐0.01, 0.95] |
| Analysis 4.2  Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 2 Intraoperative pain score excluding inhalational sedation/analgesia (VAS 0 to 10). | ||||
| 2.1 Pt‐controlled vs physician‐controlled CSA | 3 | 267 | Mean Difference (IV, Fixed, 95% CI) | 0.47 [‐0.01, 0.95] |
| 3 Postoperative pain score (VAS 0 to 10) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.3  Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 3 Postoperative pain score (VAS 0 to 10). | ||||
| 3.1 Pt‐controlled vs physician‐controlled CSA | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | 1.2 [0.26, 2.14] |
| 4 Pregnancy rate per woman Show forest plot | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.4  Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 4 Pregnancy rate per woman. | ||||
| 4.1 Pt‐controlled vs physician‐controlled CSA | 3 | 294 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.51, 1.60] |
| 5 Fertilisation rate per woman Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.5  Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 5 Fertilisation rate per woman. | ||||
| 5.1 Pt‐controlled vs physician‐controlled CSA | 1 | 106 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.54, 2.50] |
| 6 Postoperative nausea: no. of patients Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.6  Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 6 Postoperative nausea: no. of patients. | ||||
| 6.1 Pt‐controlled vs physician‐controlled CSA | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.19, 5.28] |
| 7 Patient satisfaction by LIkert scale: report of 'very and moderately satisfied' Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.7  Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 7 Patient satisfaction by LIkert scale: report of 'very and moderately satisfied'. | ||||
| 7.1 Pt‐controlled vs physician‐controlled CSA | 1 | 81 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.95 [0.34, 11.28] |
| 8 Patient satisfaction (VAS 0 to 10) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.8  Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 8 Patient satisfaction (VAS 0 to 10). | ||||
| 8.1 Pt‐controlled vs physician‐controlled CSA | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.64, 1.04] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intraoperative pain score at 5 minutes (VAS 0 to 10) Show forest plot | 1 | 52 | Mean Difference (IV, Fixed, 95% CI) | ‐0.74 [‐1.48, 0.00] |
| Analysis 5.1  Comparison 5 Conscious sedation (CSA) + analgesia via different agents or dosages, Outcome 1 Intraoperative pain score at 5 minutes (VAS 0 to 10). | ||||
| 2 Intraoperative pain score at 10 minutes (VAS 0 to 10) Show forest plot | 1 | 52 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.64, ‐0.16] |
| Analysis 5.2  Comparison 5 Conscious sedation (CSA) + analgesia via different agents or dosages, Outcome 2 Intraoperative pain score at 10 minutes (VAS 0 to 10). | ||||
| 3 Postoperative pain score at 20 minutes (VAS 0 to 10) Show forest plot | 1 | 52 | Mean Difference (IV, Fixed, 95% CI) | 0.42 [‐0.04, 0.88] |
| Analysis 5.3  Comparison 5 Conscious sedation (CSA) + analgesia via different agents or dosages, Outcome 3 Postoperative pain score at 20 minutes (VAS 0 to 10). | ||||
| 4 Patient satisfaction rate Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.4  Comparison 5 Conscious sedation (CSA) + analgesia via different agents or dosages, Outcome 4 Patient satisfaction rate. | ||||
| 4.1 CSA with propofol vs CSA with midazolam | 1 | 47 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.04, 4.94] |
| 4.2 CSA with dexmedetomidine vs CSA with midazolam (very satisfied) | 1 | 52 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.07 [0.98, 9.59] |

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
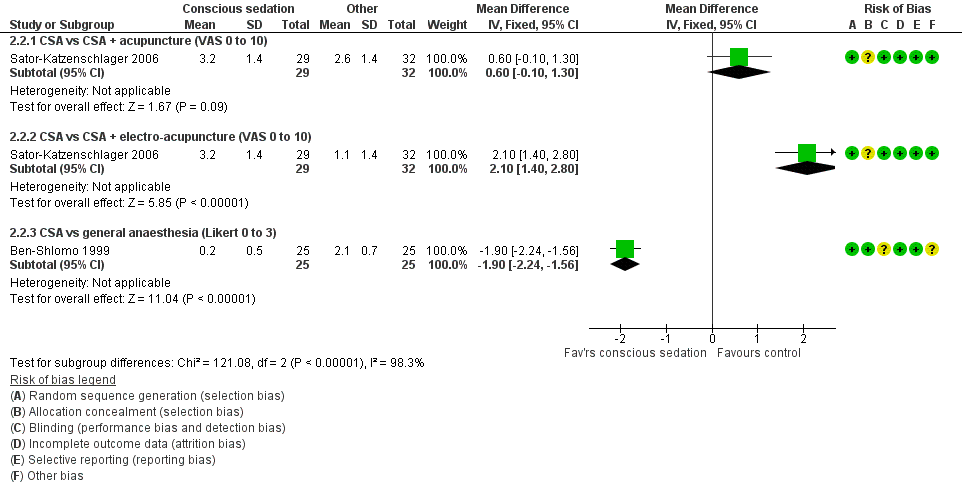
Forest plot of comparison: 2 Conscious sedation + analgesia (CSA) versus other active interventions, outcome: 2.2 Postoperative pain.

Forest plot of comparison: 3 Conscious sedation + paracervical block versus other interventions, outcome: 3.1 Intraoperative pain (VAS).

Forest plot of comparison: 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), outcome: 4.1 Intraoperative pain score (VAS 0 to 10).

Comparison 1 Conscious sedation + analgesia (CSA) versus placebo, Outcome 1 Pain during needle insertion (VAS 0 to 10).

Comparison 1 Conscious sedation + analgesia (CSA) versus placebo, Outcome 2 Pain during follicle aspiration (VAS 0 to 10).

Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 1 Intraoperative pain.

Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 2 Postoperative pain.

Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 3 Pregnancy.

Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 4 Postop vomiting and/or vomiting.

Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 5 Satisfaction.
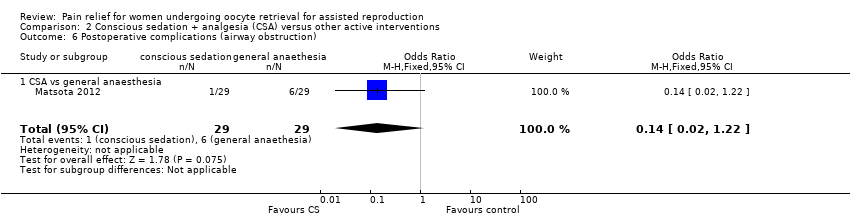
Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 6 Postoperative complications (airway obstruction).

Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 7 Postoperative complications (mask ventilation).

Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 1 Intraoperative pain (VAS 0 to 10).

Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 2 Postoperative pain.

Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 3 Live birth or ongoing pregnancy.

Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 4 Pregnancy.

Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 5 Fertilisation rate per woman.

Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 6 Postoperative nausea and/or vomiting.

Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 7 Patient satisfaction by Likert scale: report of 'excellent and satisfactory'.
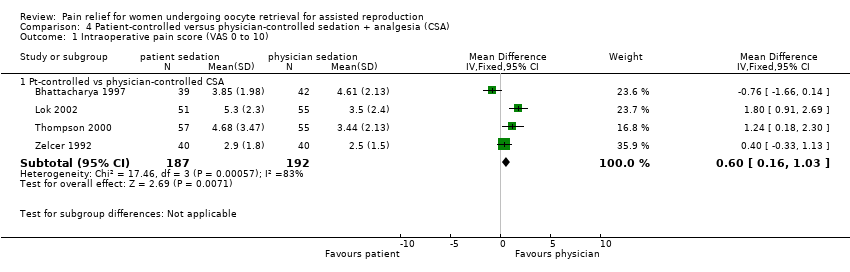
Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 1 Intraoperative pain score (VAS 0 to 10).

Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 2 Intraoperative pain score excluding inhalational sedation/analgesia (VAS 0 to 10).

Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 3 Postoperative pain score (VAS 0 to 10).

Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 4 Pregnancy rate per woman.

Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 5 Fertilisation rate per woman.

Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 6 Postoperative nausea: no. of patients.

Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 7 Patient satisfaction by LIkert scale: report of 'very and moderately satisfied'.

Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 8 Patient satisfaction (VAS 0 to 10).

Comparison 5 Conscious sedation (CSA) + analgesia via different agents or dosages, Outcome 1 Intraoperative pain score at 5 minutes (VAS 0 to 10).

Comparison 5 Conscious sedation (CSA) + analgesia via different agents or dosages, Outcome 2 Intraoperative pain score at 10 minutes (VAS 0 to 10).

Comparison 5 Conscious sedation (CSA) + analgesia via different agents or dosages, Outcome 3 Postoperative pain score at 20 minutes (VAS 0 to 10).

Comparison 5 Conscious sedation (CSA) + analgesia via different agents or dosages, Outcome 4 Patient satisfaction rate.
| Conscious sedation and analgesia (CSA) compared with CSA+acupuncture for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with CSA + acupuncture | Risk with CSA only (95% CI) | |||||
| Intraoperative pain | Mean intraoperative pain score in the comparison group was 4.9 points on a 0 to 10 VAS. | Mean score in the CSA‐only group was 1 point higher | ‐ | 62 | ⊕⊝⊝⊝ | |
| Postoperative pain | Mean postoperative pain score in the comparison group was 3.2 on a 0 to 10 VAS. | Mean score in the CSA‐only group was 0.6 points higher | ‐ | 61 | ⊕⊝⊝⊝ | |
| Pregnancy | 344 per 1000 | 242 per 1000 (95 to 493) | OR 0.61 (0.20 to 1.86) | 61 | ⊕⊝⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | 156 per 1000 | 233 per 1000 | OR 1.64 | 62 | ⊕⊝⊝⊝ | |
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded two levels for very serious imprecision: very small sample size and low event rate and/or wide confidence intervals compatible with benefit in either group or no effect. | ||||||
| Conscious sedation and analgesia (CSA) compared with CSA + electro‐acupuncture for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with CSA + electro‐acupuncture | Risk with CSA only (95% CI) | |||||
| Intraoperative pain | Mean intraoperative pain score in the comparison group was 2.9 points on a 0 to 10 VAS. | Mean score in the CSA‐only group was 3 points higher | ‐ | 62 | ⊕⊝⊝⊝ | |
| Postoperative pain | Mean postoperative pain score in the comparison group was 1.1 on a 0 to 10 VAS. | Mean score in the CSA‐only group was 2.1 points higher | ‐ | 61 | ⊕⊝⊝⊝ | |
| Pregnancy | 594 per 1000 | 243 per 1000 (95 to 491) | OR 0.22 (0.07 to 0.66) | 61 | ⊕⊝⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | 218 per 1000 | 233 per 1000 | OR 1.09 | 62 | ⊕⊝⊝⊝ | |
| Postoperative complications | Airway obstruction: No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Need for mask ventilation: No studies reported this outcome. | Not estimable | ‐ | ‐ | |||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded two levels for very serious imprecision: very small sample size and event rate. | ||||||
| Conscious sedation and analgesia (CSA) compared to general analgesia for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with GA | Risk with CSA only (95% CI) | |||||
| Intraoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative pain | Mean postoperative pain score in the comparison group was 2.1 points on a 0 to 3 Likert scale. | Mean score in the CSA‐only group was 1.9 points lower | ‐ | 50 | ⊕⊝⊝⊝ | |
| Pregnancy | 278 per 1000 | 278 per 1000 (142 to 475) | OR 1.00 (0.43 to 2.35) | 108 | ⊕⊝⊝⊝ | |
| Patient satisfaction (report of 'satisfactory') | 981 per 1000 | 972 per 1000 (854 to 995) | OR 0.66 (0.11 to 4.04) | 108 | ⊕⊝⊝⊝ | |
| Side effects (postoperative vomiting and/or vomiting) | 160 per 1000 | 81 per 1000 | OR 0.46 | 50 | ⊕⊝⊝⊝ | |
| Postoperative complications | Airway obstruction: 207 per 1000 | 35 per 1000 | OR 0.14 | 58 | ⊕⊝⊝⊝ | |
| Need for mask ventilation: 793 per 1000 | 161 per 1000 | OR 0.05 | 58 | ⊕⊝⊝⊝ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded two levels for very serious imprecision: very small sample size and event rate and/or wide confidence intervals compatible with benefit in either group or no effect. bDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. | ||||||
| Conscious sedation and analgesia (CSA) plus PCB compared with electro‐acupuncture plus PCB for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with electro‐acupuncture + PCB | Risk with CSA + PCB (95% CI) | |||||
| Intraoperative pain | Mean intraoperative pain score in the comparison group was 2.6 to 4.85 points on a 0 to 10 VAS. | Mean score in the CSA‐only group was 0.66 points lower | ‐ | 781 | ⊕⊕⊝⊝ | |
| Postoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Pregnancy | 367 per 1000 | 358 per 1000 (295 to 428) | OR 0.96 (0.72 to 1.29) | 783 | ⊕⊕⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded one level for serious inconsistency (I2 = 76%). cDowngraded one level for serious imprecision: wide confidence intervals compatible with benefit in either group or no effect. | ||||||
| Conscious sedation and analgesia (CSA) plus paracervical block (PCB) compared with general anaesthetic (GA) for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with GA | Risk with CSA + PCB (95% CI) | |||||
| Intraoperative pain | ||||||
| Postoperative pain | Mean postoperative pain score in the comparison group was 0.68 points on a 0 to 10 VAS. | Mean score in the CSA‐only group was 0.49 points higher | ‐ | 50 | ⊕⊝⊝⊝ | |
| Pregnancy | 375 per 1000 | 296 per 1000 (117 to 576) | OR 0.70 (0.22 to 2.26) | 51 | ⊕⊝⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded two levels for very serious imprecision: small sample size and low event rate, wide confidence intervals compatible with benefit in either group or no effect. | ||||||
| Conscious sedation and analgesia (CSA) plus paracervical block (PCB) compared with spinal anaesthesia for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with spinal anaesthesia | Risk with CSA + PCB (95% CI) | |||||
| Intraoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative pain | Mean postoperative pain score in the comparison group was 0.15 on a 0 to 10 VAS, | Mean score in the CSA‐only group was 1.02 points higher | ‐ | 36 | ⊕⊝⊝⊝ | |
| Pregnancy | 375 per 1000 | 358 per 1000 (126 to 687) | OR 0.93 (0.24 to 3.65) | 38 | ⊕⊝⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded two levels for very serious imprecision: very small sample size and low event rate, wide confidence intervals compatible with benefit in either group or no effect. | ||||||
| Conscious sedation and analgesia (CSA) plus paracervical block (PCB) compared with PCB only for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with PCB only | Risk with CSA + PCB (95% CI) | |||||
| Intraoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ‐ | |
| Postoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ‐ | |
| Pregnancy | 253 per 1000 | 240 per 1000 (130 to 399) | OR 0.93 (0.44 to 1.96) | 150 | ⊕⊕⊝⊝ | |
| Patient satisfaction | 800 per 1000 | 867 per 1000 | OR 1.63 (0.68 to 3.89) | 150 | ⊕⊕⊝⊝ | |
| Side effects (postoperative vomiting and/or vomiting) | No studies reported this outcome | Not estimable | ‐ | ‐ | ||
| Postoperative complications | No studies reported this outcome | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded two levels for very serious imprecision: low event rates and wide confidence intervals compatible with benefit in either group or no effect. | ||||||
| Conscious sedation and analgesia (CSA) plus paracervical block (PCB) compared with CSA alone | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with CSA alone | Risk with CSA + PCB (95% CI) | |||||
| Intraoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Pregnancy | 600 per 1000 | 482 per 1000 (296 to 671) | OR 0.62 (0.28 to 1.36) | 100 | ⊕⊝⊝⊝ | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | 300 per 1000 | 153 per 1000 | OR 0.42 | 140 | ⊕⊝⊝⊝ | |
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains. bDowngraded two levels for very serious imprecision: small sample size, very low event rates, and wide confidence intervals compatible with benefit in the CSA + PCB group or with no meaningful effect. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain during needle insertion (VAS 0 to 10) Show forest plot | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐1.70 [‐2.38, ‐1.02] |
| 2 Pain during follicle aspiration (VAS 0 to 10) Show forest plot | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐1.30 [‐1.88, ‐0.72] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intraoperative pain Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 CSA vs CSA + acupuncture (VAS 0 to 10) | 1 | 62 | Mean Difference (IV, Random, 95% CI) | 1.0 [0.18, 1.82] |
| 1.2 CSA vs CSA + electro‐acupuncture (VAS 0 to 10) | 1 | 62 | Mean Difference (IV, Random, 95% CI) | 3.00 [2.23, 3.77] |
| 1.3 CSA vs CSA + electro‐acupuncture (Pain scale 1 to 12) | 1 | 316 | Mean Difference (IV, Random, 95% CI) | 1.70 [1.07, 2.33] |
| 2 Postoperative pain Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 CSA vs CSA + acupuncture (VAS 0 to 10) | 1 | 61 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [‐0.10, 1.30] |
| 2.2 CSA vs CSA + electro‐acupuncture (VAS 0 to 10) | 1 | 61 | Mean Difference (IV, Fixed, 95% CI) | 2.1 [1.40, 2.80] |
| 2.3 CSA vs general anaesthesia (Likert 0 to 3) | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | ‐1.90 [‐2.24, ‐1.56] |
| 3 Pregnancy Show forest plot | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 CSA vs CSA + acupuncture | 1 | 61 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.20, 1.86] |
| 3.2 CSA vs CSA + electro‐acupuncture | 1 | 61 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.07, 0.66] |
| 3.3 CSA vs general anaesthesia | 2 | 108 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.43, 2.35] |
| 4 Postop vomiting and/or vomiting Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 CSA vs CSA + acupuncture | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 CSA vs general anaesthesia | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Satisfaction Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 CSA vs general anaesthesia | 2 | 108 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.11, 4.04] |
| 6 Postoperative complications (airway obstruction) Show forest plot | 1 | 58 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.02, 1.22] |
| 6.1 CSA vs general anaesthesia | 1 | 58 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.02, 1.22] |
| 7 Postoperative complications (mask ventilation) Show forest plot | 1 | 58 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.01, 0.20] |
| 7.1 CSA vs general anaesthesia | 1 | 58 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.01, 0.20] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intraoperative pain (VAS 0 to 10) Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 CSA + paracervical block versus electro‐acupuncture + paracervical block | 4 | 781 | Mean Difference (IV, Fixed, 95% CI) | ‐0.66 [‐0.93, ‐0.39] |
| 2 Postoperative pain Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 CSA + paracervical block vs general anaesthesia | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 0.49 [‐0.13, 1.11] |
| 2.2 CSA + paracervical block vs spinal anaesthesia | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | 1.02 [0.48, 1.56] |
| 3 Live birth or ongoing pregnancy Show forest plot | 2 | 393 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.78, 1.86] |
| 3.1 CSA + paracervical block vs electro‐acupuncture + paracervical block | 1 | 149 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.35 [1.09, 5.05] |
| 3.2 CSA + paracervical block vs electro‐acupuncture + paracervical block | 1 | 244 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.50, 1.47] |
| 4 Pregnancy Show forest plot | 7 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 CSA + paracervical block vs general anaesthesia | 1 | 51 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.22, 2.26] |
| 4.2 CSA + paracervical block vs spinal anaesthesia | 1 | 38 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.24, 3.65] |
| 4.3 CSA + paracervical block vs paracervical block only | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.44, 1.96] |
| 4.4 CSA + paracervical block vs electro‐acupuncture + paracervical block | 4 | 783 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.72, 1.29] |
| 4.5 CSA + paracervical block vs CSA alone | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.28, 1.36] |
| 5 Fertilisation rate per woman Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 CSA + paracervical block vs paracervical block only | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.42, 1.66] |
| 6 Postoperative nausea and/or vomiting Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 CSA + paracervical block vs CS only | 2 | 140 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.18, 0.97] |
| 7 Patient satisfaction by Likert scale: report of 'excellent and satisfactory' Show forest plot | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.63 [0.68, 3.89] |
| 7.1 CSA + paracervical block vs paracervical block only | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.63 [0.68, 3.89] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intraoperative pain score (VAS 0 to 10) Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Pt‐controlled vs physician‐controlled CSA | 4 | 379 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.16, 1.03] |
| 2 Intraoperative pain score excluding inhalational sedation/analgesia (VAS 0 to 10) Show forest plot | 3 | 267 | Mean Difference (IV, Fixed, 95% CI) | 0.47 [‐0.01, 0.95] |
| 2.1 Pt‐controlled vs physician‐controlled CSA | 3 | 267 | Mean Difference (IV, Fixed, 95% CI) | 0.47 [‐0.01, 0.95] |
| 3 Postoperative pain score (VAS 0 to 10) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Pt‐controlled vs physician‐controlled CSA | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | 1.2 [0.26, 2.14] |
| 4 Pregnancy rate per woman Show forest plot | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Pt‐controlled vs physician‐controlled CSA | 3 | 294 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.51, 1.60] |
| 5 Fertilisation rate per woman Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Pt‐controlled vs physician‐controlled CSA | 1 | 106 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.54, 2.50] |
| 6 Postoperative nausea: no. of patients Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Pt‐controlled vs physician‐controlled CSA | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.19, 5.28] |
| 7 Patient satisfaction by LIkert scale: report of 'very and moderately satisfied' Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Pt‐controlled vs physician‐controlled CSA | 1 | 81 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.95 [0.34, 11.28] |
| 8 Patient satisfaction (VAS 0 to 10) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Pt‐controlled vs physician‐controlled CSA | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.64, 1.04] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intraoperative pain score at 5 minutes (VAS 0 to 10) Show forest plot | 1 | 52 | Mean Difference (IV, Fixed, 95% CI) | ‐0.74 [‐1.48, 0.00] |
| 2 Intraoperative pain score at 10 minutes (VAS 0 to 10) Show forest plot | 1 | 52 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.64, ‐0.16] |
| 3 Postoperative pain score at 20 minutes (VAS 0 to 10) Show forest plot | 1 | 52 | Mean Difference (IV, Fixed, 95% CI) | 0.42 [‐0.04, 0.88] |
| 4 Patient satisfaction rate Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 CSA with propofol vs CSA with midazolam | 1 | 47 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.04, 4.94] |
| 4.2 CSA with dexmedetomidine vs CSA with midazolam (very satisfied) | 1 | 52 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.07 [0.98, 9.59] |


