Rehabilitación pulmonar para la enfermedad pulmonar obstructiva crónica
Appendices
Appendix 1. Archive of previous search methods and results
Search strategy used for review versions published up to 2004
We searched all records in the Cochrane Airways Group Register coded as 'COPD' for original articles published in any language using the following strategy: rehabilitat* or fitness* or exercis* or physical* or train*
In the first version of this review (Lacasse 1996), 522 publications were retrieved from the computerised search. The review authors reduced this list to 68 potentially eligible papers (quadratic weighted Kappa 0.53, 95% CI 0.45 to 0.61) that were assessed in detail. From this study list, 47 were excluded as the result of wrong population studies (n = 4), intervention not meeting the definition of rehabilitation (n = 7), control group not receiving conventional community care (n = 29), trials not randomised (n = 7). Both primary review authors agreed to include 17 papers in the meta‐analysis (quadratic Kappa 0.89, 95% CI 0.65 to 1.00). Six of the 14 RCTs included in the original meta‐analysis (Lacasse 1996) were not uncovered by this literature search. Therefore, a total of 23 randomised controlled trials were included. This represents an addition of nine RCTs to the meta‐analysis published in 1996 (Lacasse 1996). We contacted the authors of these trials for any additional information required; response rate was 91% (21/23).
An updated search for the review was undertaken in October 2004, which identified an additional 998 references. These were filtered to a list of 139 references, which were considered in the update of the review. Of these, 93 studies failed to meet the inclusion criteria. The original version of the review as previously indicated had included 23 trials. From the updated search (2004), eight additional RCTs (represented by 17 references) met the inclusion criteria of the review (Behnke 2000a; Boxall 2005; Casaburi 2004; Chlumsky 2001; Finnerty 2001; Güell 1998; Singh 2003; Xie 2003). Six papers were awaiting assessment (Corrado 1995: published as conference abstract; Fernández 1998: paper not available; Shu 1998: published as conference abstract; Tregonning 2000: published as conference abstract; Ward 1999: published as conference abstract; Wright 2002: unclear study methods). One trial was ongoing (Whiteford 2004). As an outcome of the update in 2004, a total of 31 RCTs (represented by 65 references) contributed to the meta‐analysis.
Appendix 2. Sources and search methods for the Cochrane Airways Group Specialised Register (CAGR)
Electronic searches: core databases
| Database | Frequency of search |
| CENTRAL | Monthly |
| MEDLINE (Ovid) | Weekly |
| EMBASE (Ovid) | Weekly |
| PsycINFO (Ovid) | Monthly |
| CINAHL (EBSCO) | Monthly |
| AMED (EBSCO) | Monthly |
Handsearches: core respiratory conference abstracts
| Conference | Years searched |
| American Academy of Allergy, Asthma and Immunology (AAAAI) | 2001 onwards |
| American Thoracic Society (ATS) | 2001 onwards |
| Asia Pacific Society of Respirology (APSR) | 2004 onwards |
| British Thoracic Society Winter Meeting (BTS) | 2000 onwards |
| Chest Meeting | 2003 onwards |
| European Respiratory Society (ERS) | 1992, 1994, 2000 onwards |
| International Primary Care Respiratory Group Congress (IPCRG) | 2002 onwards |
| Thoracic Society of Australia and New Zealand (TSANZ) | 1999 onwards |
MEDLINE search strategy used to identify trials for the CAGR
COPD search
1. Lung Diseases, Obstructive/
2. exp Pulmonary Disease, Chronic Obstructive/
3. emphysema$.mp.
4. (chronic$ adj3 bronchiti$).mp.
5. (obstruct$ adj3 (pulmonary or lung$ or airway$ or airflow$ or bronch$ or respirat$)).mp.
6. COPD.mp.
7. COAD.mp.
8. COBD.mp.
9. AECB.mp.
10. or/1‐9
Filter to identify RCTs
1. exp "clinical trial [publication type]"/
2. (randomised or randomised).ab,ti.
3. placebo.ab,ti.
4. dt.fs.
5. randomly.ab,ti.
6. trial.ab,ti.
7. groups.ab,ti.
8. or/1‐7
9. Animals/
10. Humans/
11. 9 not (9 and 10)
12. 8 not 11
The MEDLINE strategy and RCT filter are adapted to identify trials in other electronic databases
Appendix 3. Search strategy to identify relevant trials from the CAGR
#1 MeSH DESCRIPTOR Pulmonary Disease, Chronic Obstructive Explode All
#2 MeSH DESCRIPTOR Bronchitis, Chronic
#3 (obstruct*) near3 (pulmonary or lung* or airway* or airflow* or bronch* or respirat*)
#4 COPD:MISC1
#5 (COPD OR COAD OR COBD):TI,AB,KW
#6 #1 OR #2 OR #3 OR #4 OR #5
#7 MeSH DESCRIPTOR Rehabilitation
#8 MeSH DESCRIPTOR Respiratory Therapy
#9 rehabilitat*
#10 fitness*
#11 exercis*
#12 train*
#13 #7 or #8 or #9 or #10 or #11 or #12
#14 #6 and #13
[Note: in search line #4, MISC1 denotes the field in which the reference has been coded for condition, in this case, COPD]
Appendix 4. Exclusion criteria used to sort and categorise references
| Exclusion criteria |
| Less than 90% of participants have a diagnosis of COPD |
| Not a programme, or programme does NOT contain any exercise component |
| Has an exercise component but is NOT aerobically demanding |
| Programme of less than 4 weeks' duration |
| Control received more than conventional care |
| Includes ventilated patients (hospital ventilated) |
| Within 4 weeks post exacerbation |
| This citation linked to main study paper already being screened |
| Duplicate citation (identical to a citation previously included) |
| The intervention is a medication |
Appendix 5. Eligibility classification allocated to studies
| Classification | Action |
| Excluded | Study excluded |
| Important article but not to be included in review | Study excluded |
| Included but needs translation | Study included and proceeds to next stage |
| Included | Study included and proceeds to next stage |
| More information needed before inclusion decision | Awaiting additional information before study proceeds |
Appendix 6. Risk of bias domains and judgements
Sequence generation (possible selection bias)
A detailed description of the methods used to generate the allocation sequence was developed for each study to facilitate an assessment of whether it should produce comparable groups.
Risk of bias for sequence generation was graded based on the following:
-
low risk (any truly random process, e.g. random number table; computer random number generator);
-
high risk (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number); or
-
unclear risk.
Allocation concealment (possible selection bias)
A description of the methods used to conceal the allocation sequence for each study was presented, and this determined whether the intervention allocation might have been anticipated in advance of, or during, recruitment, or changed after assignment.
Risk of bias associated with allocation concealment was graded as follows:
-
low risk (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
-
high risk (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth); or
-
unclear risk.
Blinding of participants and personnel (possible performance bias)
The nature of the interventions involved in pulmonary rehabilitation would make it highly unlikely or impossible to blind participants or personnel delivering the interventions.
However, it would be possible to blind outcome assessors. Therefore, we assessed the risk of bias for blinding of outcome assessors as:
-
high risk;
-
low risk; or
-
unclear risk.
Blinding of outcome assessment (checking for possible detection bias)
We will describe for each included study the methods used, if any, to blind outcome assessors from knowledge
of which intervention participants received. We will assess the risk of bias for blinding of outcome assessment as:
-
low risk;
-
high risk; or
-
unclear risk.
Incomplete outcome data (possible attrition bias associated with withdrawals, drop‐outs, deviations from original protocol)
A description of completeness of data for each outcome at all stages of the study was presented. This included examining attrition and exclusions from the analysis. Each study was examined to identify whether attrition and exclusions were reported (comparing the numbers presented at each stage with the total number of randomised participants). The studies were also examined for rationale and justifications explaining any attrition or exclusions. In instances where enough information could be identified or was obtained from the trial authors, we re‐included missing data in the analyses. We assessed the risk of bias for completeness of data as follows:
-
low risk (20% or less missing data);
-
high risk (more than 20% missing data); or
-
unclear risk.
Selective reporting bias
Studies were examined for selective outcome reporting bias by cross‐checking that all outcomes identified in the methods section of the results publication were reported in the results section of the trial publication(s).
The risk of bias for selective reporting was graded as follows:
-
high risk (where not all of the study’s prespecified outcomes had been reported; one or more reported primary outcomes were not prespecified; outcomes of interest were reported incompletely and so cannot be used; study failed to include results of a key outcome that would have been expected to have been reported);
-
low risk (where it was clear that all of the study’s prespecified outcomes and all expected outcomes of interest to the review have been reported); or
-
unclear risk.
Other sources of bias (bias due to problems not covered by the items above)
If the review authors believed that any other possible sources of bias were matters of concern, these were recorded.
The level at which studies were seen to be free of other problems that could put them at risk of bias was graded as:
-
low risk;
-
high risk; or
-
unclear risk.
Overall risk of bias
An overall judgement was made in relation to whether studies were at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) and identified above. The magnitude of the overall bias, along with the degree to which the bias was likely to have impacted the findings, was assessed for each study using the following grades:
-
low risk;
-
high risk; or
-
unclear risk.
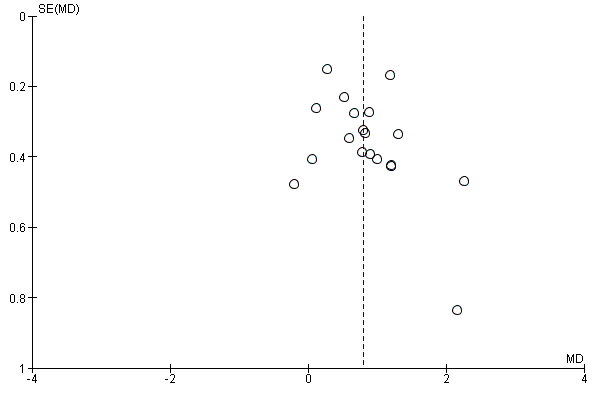
Funnel plot of comparison: 1 Rehabilitation versus usual care, outcome: 1.4 QoL ‐ Change in CRQ (Dyspnoea) (see Table 1 for Egger and Begg‐Mazumdar: Kendall's test results).

Funnel plot of comparison: 1 Rehabilitation versus usual care, outcome: 1.5 QoL ‐ Change in SGRQ (Total) (see Table 1 for Egger and Begg‐Mazumdar: Kendall's test results).

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Comparison 1 Rehabilitation versus usual care, Outcome 1 QoL ‐ Change in CRQ (Fatigue).

Comparison 1 Rehabilitation versus usual care, Outcome 2 QoL ‐ Change in CRQ (Emotional Function).
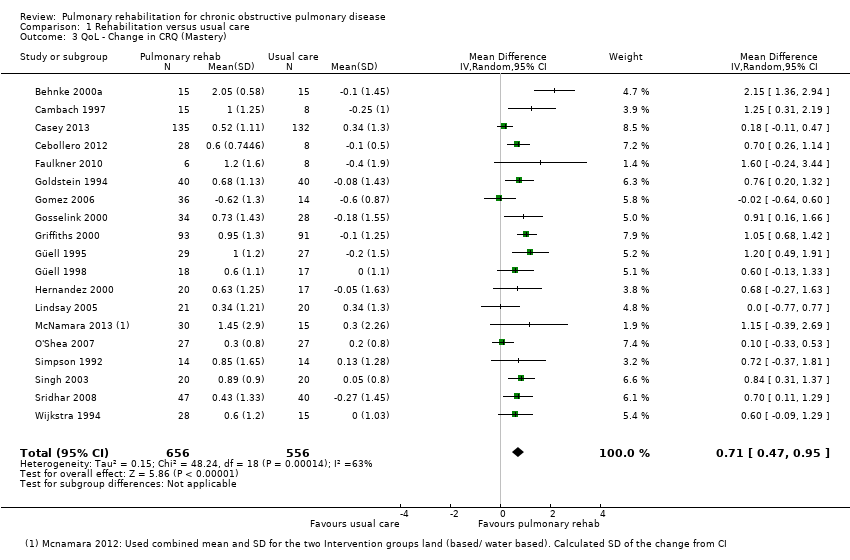
Comparison 1 Rehabilitation versus usual care, Outcome 3 QoL ‐ Change in CRQ (Mastery).

Comparison 1 Rehabilitation versus usual care, Outcome 4 QoL ‐ Change in CRQ (Dyspnoea).

Comparison 1 Rehabilitation versus usual care, Outcome 5 QoL ‐ Change in SGRQ (Total).

Comparison 1 Rehabilitation versus usual care, Outcome 6 QoL ‐ Change in SGRQ (Symptoms).
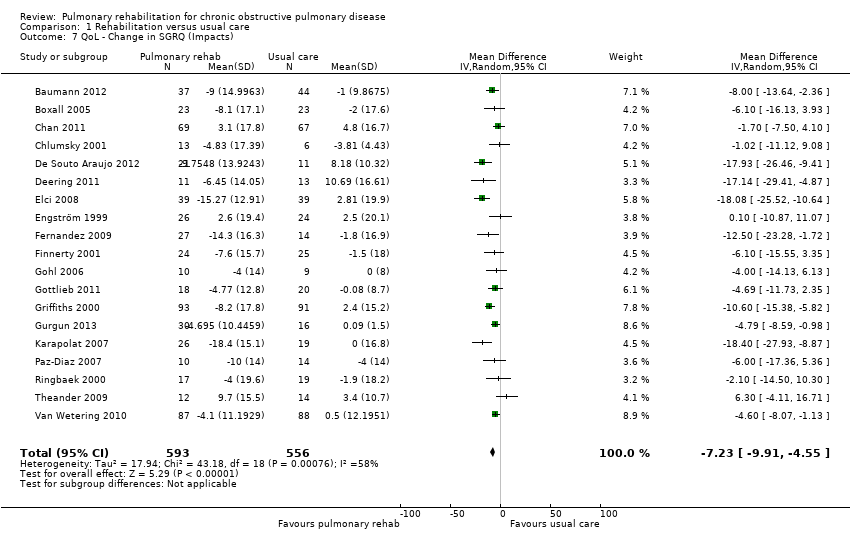
Comparison 1 Rehabilitation versus usual care, Outcome 7 QoL ‐ Change in SGRQ (Impacts).

Comparison 1 Rehabilitation versus usual care, Outcome 8 QoL ‐ Change in SGRQ (Activity).

Comparison 1 Rehabilitation versus usual care, Outcome 9 Maximal Exercise (Incremental shuttle walk test).

Comparison 1 Rehabilitation versus usual care, Outcome 10 Maximal Exercise Capacity (cycle ergometer).
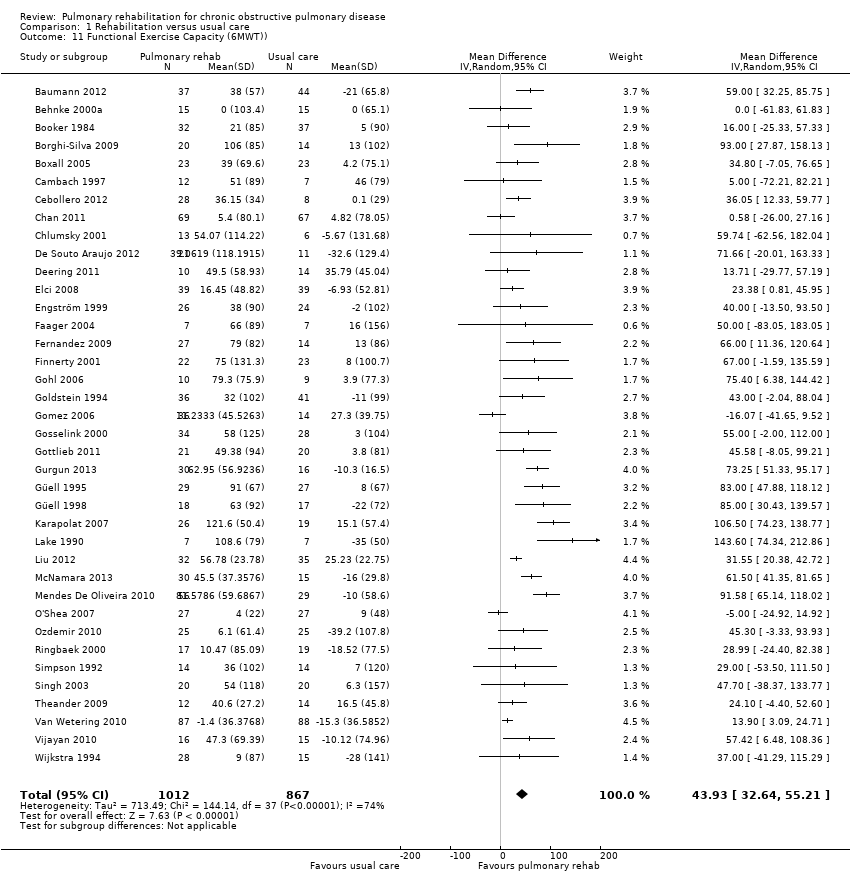
Comparison 1 Rehabilitation versus usual care, Outcome 11 Functional Exercise Capacity (6MWT)).

Comparison 2 Rehabilitation versus usual care (subgroup analysis hospital vs community), Outcome 1 QoL ‐ Change in CRQ (Fatigue).
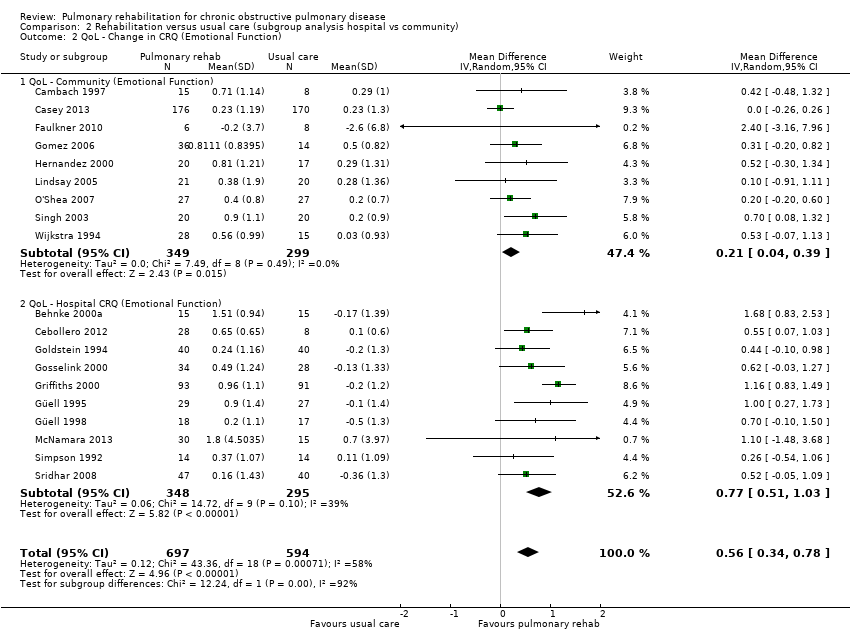
Comparison 2 Rehabilitation versus usual care (subgroup analysis hospital vs community), Outcome 2 QoL ‐ Change in CRQ (Emotional Function).

Comparison 2 Rehabilitation versus usual care (subgroup analysis hospital vs community), Outcome 3 QoL ‐ Change in CRQ (Mastery).

Comparison 2 Rehabilitation versus usual care (subgroup analysis hospital vs community), Outcome 4 QoL ‐ Change in CRQ (Dyspnoea).

Comparison 2 Rehabilitation versus usual care (subgroup analysis hospital vs community), Outcome 5 QoL ‐ Change in SGRQ (Total).

Comparison 2 Rehabilitation versus usual care (subgroup analysis hospital vs community), Outcome 6 QoL ‐ Change in SGRQ (Symptoms).

Comparison 2 Rehabilitation versus usual care (subgroup analysis hospital vs community), Outcome 7 QoL ‐ Change in SGRQ (Impacts).
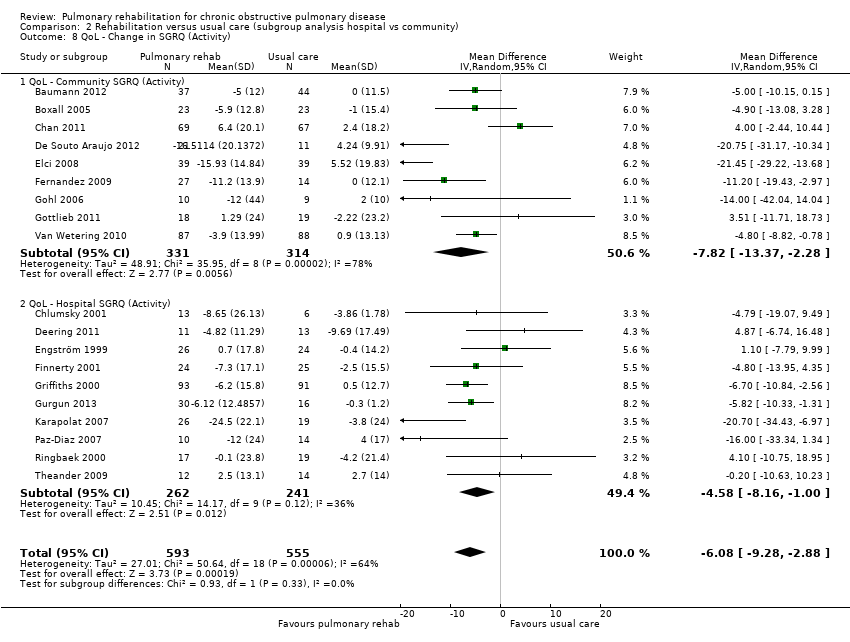
Comparison 2 Rehabilitation versus usual care (subgroup analysis hospital vs community), Outcome 8 QoL ‐ Change in SGRQ (Activity).

Comparison 3 Rehabilitation versus usual care (subgroup analysis exercise only vs exercise and other), Outcome 1 QoL ‐ Change in CRQ (Fatigue).
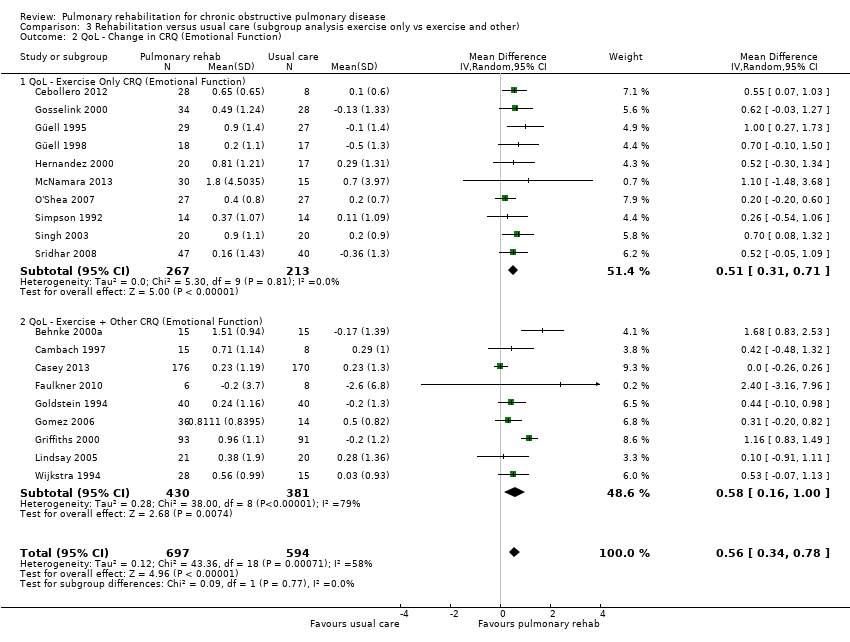
Comparison 3 Rehabilitation versus usual care (subgroup analysis exercise only vs exercise and other), Outcome 2 QoL ‐ Change in CRQ (Emotional Function).

Comparison 3 Rehabilitation versus usual care (subgroup analysis exercise only vs exercise and other), Outcome 3 QoL ‐ Change in CRQ (Mastery).

Comparison 3 Rehabilitation versus usual care (subgroup analysis exercise only vs exercise and other), Outcome 4 QoL ‐ Change in CRQ (Dyspnoea).
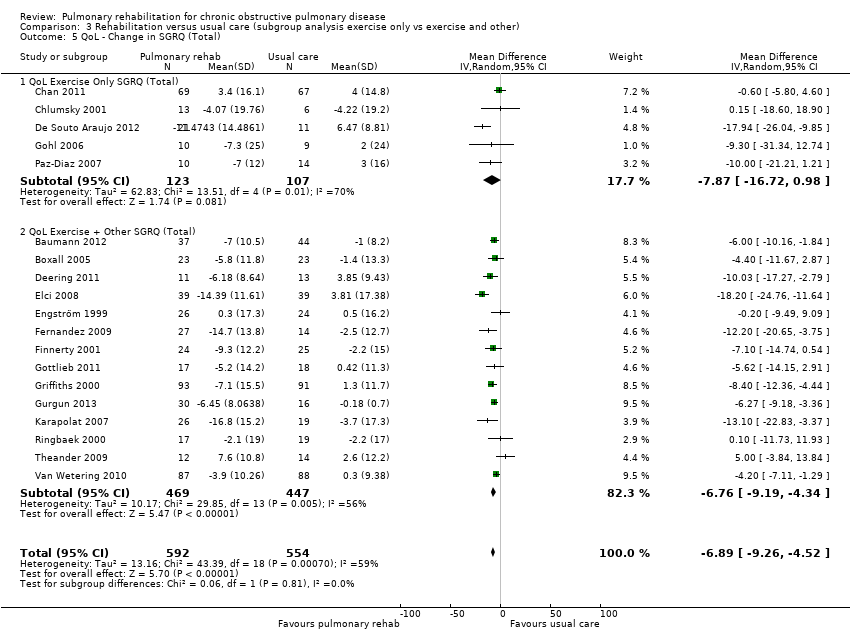
Comparison 3 Rehabilitation versus usual care (subgroup analysis exercise only vs exercise and other), Outcome 5 QoL ‐ Change in SGRQ (Total).

Comparison 3 Rehabilitation versus usual care (subgroup analysis exercise only vs exercise and other), Outcome 6 QoL ‐ Change in SGRQ (Symptoms).

Comparison 3 Rehabilitation versus usual care (subgroup analysis exercise only vs exercise and other), Outcome 7 QoL ‐ Change in SGRQ (Impacts).

Comparison 3 Rehabilitation versus usual care (subgroup analysis exercise only vs exercise and other), Outcome 8 QoL ‐ Change in SGRQ (Activity).
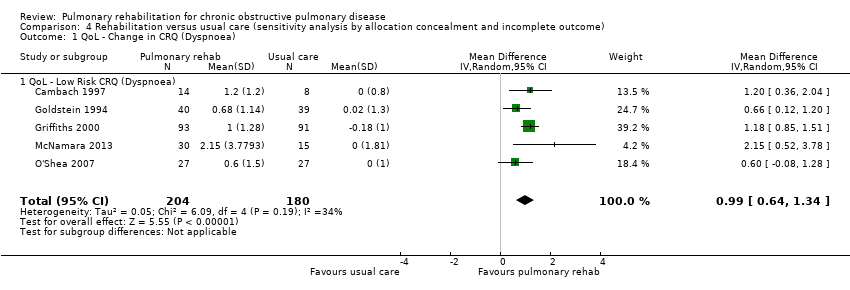
Comparison 4 Rehabilitation versus usual care (sensitivity analysis by allocation concealment and incomplete outcome), Outcome 1 QoL ‐ Change in CRQ (Dyspnoea).

Comparison 4 Rehabilitation versus usual care (sensitivity analysis by allocation concealment and incomplete outcome), Outcome 2 QoL ‐ Change in CRQ (Emotional Function).

Comparison 4 Rehabilitation versus usual care (sensitivity analysis by allocation concealment and incomplete outcome), Outcome 3 QoL ‐ Low Risk CRQ (Fatigue).

Comparison 4 Rehabilitation versus usual care (sensitivity analysis by allocation concealment and incomplete outcome), Outcome 4 QoL ‐ Low Risk CRQ (Mastery).

Comparison 4 Rehabilitation versus usual care (sensitivity analysis by allocation concealment and incomplete outcome), Outcome 5 QoL ‐ Low Risk SGRQ (Total).

Comparison 4 Rehabilitation versus usual care (sensitivity analysis by allocation concealment and incomplete outcome), Outcome 6 QoL ‐ Low Risk SGRQ (Symptoms).

Comparison 4 Rehabilitation versus usual care (sensitivity analysis by allocation concealment and incomplete outcome), Outcome 7 QoL ‐ Low Risk SGRQ (Impacts).
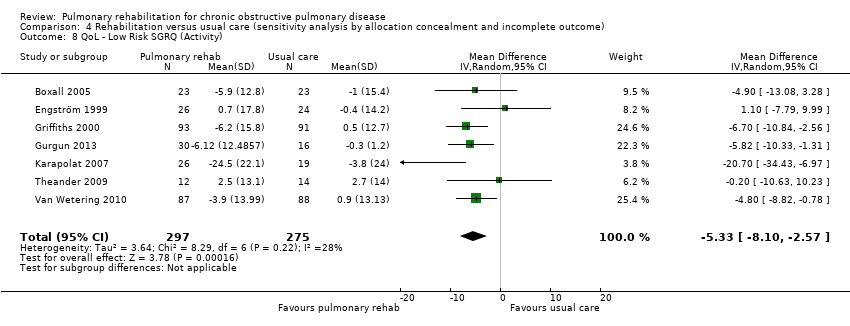
Comparison 4 Rehabilitation versus usual care (sensitivity analysis by allocation concealment and incomplete outcome), Outcome 8 QoL ‐ Low Risk SGRQ (Activity).
| Rehabilitation versus usual care for chronic obstructive pulmonary disease | |||||
| Patient or population: patients with chronic obstructive pulmonary disease | |||||
| Outcomes | Illustrative comparative effects* (95% CI) | Number of participants | Quality of the evidence | Comments | |
| Response on control | Treatment effect | ||||
| Usual care | Rehabilitation versus usual care | ||||
| QoL ‐ Change in CRQ (dyspnoea) (Higher is better and 0.5 unit is an important difference) | Median change = 0 units | Mean QoL ‐ change in CRQ (Dyspnoea) in the intervention groups was | 1283 | ⊕⊕⊕⊝ | Sensitivity analysis from studies at lower risk of bias was similar (MD 0.99, 95% CI 0.64 to 1.34; participants = 384; studies = 5; I2 = 34%) |
| QoL ‐ Change in SGRQ (total) (Lower is better and 4 units is an important difference) | Median change = 0.42 units | Mean QOL ‐ change in SGRQ (total) in the intervention groups was | 1146 | ⊕⊕⊕⊝ | Sensitivity analysis from studies at lower risk of bias was similar (MD ‐5.15, 95% CI ‐7.95 to ‐2.36; participants = 572; studies = 7; I2 = 51%) |
| Change in maximal exercise (Incremental Shuttle walk test (ISWT)) | Median change = 1 metre | Mean maximal exercise (incremental shuttle walk test) in the intervention groups was | 694 | ⊕⊕⊕⊝ | |
| Change in functional exercise capacity (6MWT)) | Median change = 3.4 metres | Mean functional exercise capacity (6MWT)) in the intervention groups was | 1879 | ⊕⊝⊝⊝ | |
| Change in maximal exercise capacity (cycle ergometer) | Median change = ‐0.05 watts | Mean maximal exercise capacity (cycle ergometer) in the intervention groups was | 779 | ⊕⊕⊝⊝ | |
| *The basis for the response on control is the median control group response across studies. | |||||
| GRADE Working Group grades of evidence. | |||||
| 117 studies reported random sequence generation (1 unclear), 12 reported allocation concealment 2 did not have allocation concealment and it is unclear in 5 studies. 4 studies did not blind assessors, 11 blinded assessors and 4 were unclear as to assessor blinding. 6 studies had attrition bias greater than 20%. | |||||
| CRQ Fatigue | Bias indicators Begg‐Mazumdar: Kendall's tau = 0.22807; P value 0.1863 Egger: bias = 1.61189 (95% CI = ‐0.194745 to 3.418525); P value 0.077 |
| CRQ Emotional | Bias indicators Begg‐Mazumdar: Kendall's tau = 0.204678; P value 0.2378 Egger: bias = 0.997332 (95% CI = ‐0.618039 to 2.612702); P value 0.2101 |
| CRQ Mastery | Bias indicators Begg‐Mazumdar: Kendall's tau = 0.146199; P value 0.4063 Egger: bias = 1.531134 (95% CI = ‐0.268167 to 3.330434); P value 0.0904 |
| CRQ Dyspnoea (see Figure 1 for funnel plot) | Bias indicators Begg‐Mazumdar: Kendall's tau = 0.274854; P value 0.1082 Egger: bias = 1.275427 (95% CI = ‐0.761574 to 3.312427); P value 0.204 |
| SGRQ Total (see Figure 2 for funnel plot) | Bias indicators Begg‐Mazumdar: Kendall's tau = ‐0.052632; P value 0.73 Egger: bias = ‐0.459813 (95% CI = ‐2.086751 to 1.167125); P value 0.5588 |
| SGRQ Symptoms | Bias indicators Begg‐Mazumdar: Kendall's tau = 0.017544; P value 0.945 Egger: bias = 0.076734 (95% CI = ‐1.241745 to 1.395213); P value 0.9037 |
| SQRQ Activity | Bias indicators Begg‐Mazumdar: Kendall's tau = ‐0.052632; P value 0.73 Egger: bias = ‐0.336937 (95% CI = ‐2.10096 to 1.427086); P value 0.692 |
| 6MWT | Bias indicators Begg‐Mazumdar: Kendall's tau = 0.16074; P value 0.1601 Egger: bias = 1.24304 (95% CI = 0.183967 to 2.302131); P value 0.0227 |
| Incremental Shuttle Walk Test | Bias indicators Begg‐Mazumdar: Kendall's tau = 0.0776906; P value 0.846 Egger: bias = ‐0.21 2523 (95% CI = ‐2.7776 to 2.351859); P value 0.846 |
| Cycle Ergometer | Bias indicators Begg‐Mazumdar: Kendall's tau = ‐0.2666667; P value 0.139 |
| Study | Rehab sample size | Male | Female | Mean age (SD) | FEV1 (SD) | Control sample size | Male | Female | Mean age (SD) | FEV1 (SD) |
| 35 | na | na | 63.7 | 41.9 | 36 | na | na | 65.9 | 43.3 | |
| 37 | na | na | 65 | 45 | 44 | na | na | 63 | 47 | |
| 23 | 12 | 3 | 64.0 (1) | 34.1 (7.4) | 23 | 11 | 4 | 68.0 (2.2) | 37.5 (6.6) | |
| 27 | 7 | 9 | 64 (3) | 1.02 L/min (0.06) | 20 | 7 | 9 | 65 (2) | 1.04 L/min (0.07) | |
| 32 | na | na | 66 (8) | 0.85 L (0.29) | 37 | na | na | 65 (7) | 0.97 L (0.37) | |
| 20 | 13 | 7 | 67 (10) | 33 (9) | 14 | 12 | 8 | 67(10) | 35 (11) | |
| 23 | 11 | 12 | 77.6 (7.6) | 40.5 (15.9) | 23 | 15 | 8 | 75.8 (8.1) | 37.7 (15.0) | |
| 7 | 5 | 2 | 65 (16) | 26% (9) | 7 | 6 | 1 | 66 (16) | 27% (11) | |
| 15 | 7 | 8 | 62 (5) | 59% (16) | 8 | 6 | 2 | 62 (9) | 60% (23) | |
| 12 | 12 | 0 | 69 (10) | 36% (9) | 12 | 12 | 0 | 68 (9) | 39% (12) | |
| 178 | 117 | 61 | 68.8 (10.2) | 57.6 (14.3) | 172 | 106 | 66 | 68.4 (10.3) | 59.7 (13.8) | |
| 28 | 28 | 0 | 68 (7) | 47.8 (5) | 8 | 8 | 0 | 69(5) | 38.7 (5) | |
| 69 | 61 | 8 | 73.6 (7.5) | 91 (0.39) | 67 | 58 | 9 | 73.6 (7.4) | 89 (0.39) | |
| 13 | 12 | 1 | 63 (11) | 43% (21) | 6 | 5 | 1 | 65 (13) | 51% (17) | |
| 32 | na | na | 58 (8) | 1.72 L (0.83) | 16 | na | na | 55 (8) | 1.44 L (0.59) | |
| 74 | 32 | 42 | na | na | 50 | 18 | 32 | na | na | |
| 18 | 18 | 0 | 61 (5) | 1.53 L (0.70) | 16 | 16 | 0 | 60 (5) | 1.32 L (0.44) | |
| 21 | 12 | 9 | 59 | 39.2 (11.4) /43.9 (10.3) | 11 | 8 | 3 | 71.1 | 45.1 (12.6) | |
| 25 | 11 | 14 | 67.7 (5.3) | 77.0 (19) | 19 | 8 | 8 | 68.6 (5.5) | 45.8 (18.3) | |
| 39 | 33 | 6 | 59.67 (8.6) | 47.7 | 39 | 33 | 6 | 58.08 (11.45) | 46.28 | |
| 25 | 15 | 14 | 65 (6) | 1.29 L (0.63) | 25 | 12 | 13 | 67 (7) | 1.02 L (0.37) | |
| 26 | 14 | 12 | 66 (5) | 31% (11) | 24 | 12 | 12 | 67 (5) | 34% (10) | |
| 10 | 3 | 7 | 72 (9) | 26 (7) | 10 | 3 | 7 | 70 (8) | 28 (6) | |
| 10 | na | na | na | na | 10 | na | na | na | na | |
| 30 | 29 | 1 | 66 (8) | 33 (10) | 20 | 20 | 0 | 70 (5) | 38 (12) | |
| 36 | 25 | 11 | 70 (8) | 41% (19) | 29 | 19 | 10 | 68 (10) | 41% (16) | |
| 17 | 6 | 4 | 62.5 (7) | 53.4 (10.7) | 17 | 7 | 2 | 53.7 (5.8) | 63.2 (8.5) | |
| 38 | 21 | 17 | 66 (7) | 35% (15) | 40 | 17 | 23 | 65 (8) | 35% (12) | |
| 37 | 31 | 6 | 60 (9) | 41% (16) | 33 | 30 | 3 | 63 (7) | 43% (12) | |
| 35 | 7 | 15 | 74.1 (66–82) | 64.27 (7.9) | 26 | 7 | 13 | 73.2 (67–88) | 67.05 (8.8) | |
| 93 | 57 | 37 | 68 (8) | 40% (16) | 91 | 54 | 37 | 68 (8) | 39% (16) | |
| 30 | 28 | 28 | 64.0 (10.8) | 41.9 (10.8) | 16 | 15 | 1 | 67.8 (6.6) | 39.3 (9.3) | |
| 30 | 30 | 30 | 64 (7) | 31% (12) | 30 | 30 | 0 | 66 (6) | 39% (14) | |
| 18 | 16 | 2 | 68 (8) | 32% (11) | 17 | 17 | 0 | 66 (8) | 38% (15) | |
| 20 | 20 | 0 | 64 (8) | 71.1 (18.9) | 17 | 17 | 0 | 63 (7) | 74.7 (14.7) | |
| 6 | 4 | 2 | 62.8 (1.4) | 49.9 (4.6) | 6 | 4 | 2 | 60.6 (3.0) | 45.2 (6.0) | |
| 8 | 6 | 2 | 64 (6) | 0.78 L (0.27) | 6 | 1 | 5 | 63 (8) | 0.68 L (0.12) | |
| 26 | 21 | 5 | 64.81 (9.4) | 55.50% | 19 | 18 | 1 | 67.21 (6.72) | 58% | |
| 7 | 6 | 1 | 66.3 (6.8) | 0.83 L (0.25) | 7 | 4 | 3 | 65.7 (3.5) | 0.97 L (0.29) | |
| 25 | 20 | 5 | 69.5 (9.3) | 0.9 L (0.3) | 25 | 18 | 7 | 69.8 (10.3) | 0.8 L (0.4) | |
| 36 | 26 | 10 | 61.34 (8.3) | 61.27 (5.86) | 36 | 29 | 7 | 62.2 (6.34) | 61.43 (6.17) | |
| 12 | 12 | 0 | 61 (6) | 0.97 L (0.33) | 12 | 12 | 0 | 57 (8) | 1.15 L (0.72) | |
| 38 | 18 | 15 | 72 (10) | 60 (10) | 15 | 8 | 7 | 70 (9) | 55 (20) | |
| 20 | 11 | 9 | 52.1 (10.7) | na | 18 | 7 | 11 | 52.17 (11.6) | na | |
| 56 | 46 | 10 | 66.4/71.3 | 47.5/ 51.5 | 29 | 19 | 10 | 70.8 | 41.4 | |
| 14 | 11 | 3 | 73.5 | 58.5 (48‐65) | 15 | 13 | 2 | 68 | 57 (44‐66) | |
| 27 | na | na | 66.9 (7) | 49 | 27 | na | na | 68.4 (9.9) | 52 | |
| 25 | 25 | 0 | 60.9 (8.8) | 54.5 (15.6) | 25 | 25 | 0 | 64.1 (8.9) | 54.1 (20.2) | |
| 10 | 6 | 4 | 67 (5) | 34 (11) | 14 | 12 | 2 | 62 (7) | 30 (9) | |
| 149 | 80 | 69 | 68.8 (9.2) | na | 73 | 40 | 33 | 66.8 (9.9) | na | |
| 10 | 5 | 5 | 66 (8) | 35% (10) | 10 | 5 | 5 | 66 (7) | 33% (15) | |
| 24 | 1 | 23 | 62 (7) | 50% (17) | 21 | 6 | 15 | 65 (8) | 44% (14) | |
| 64 | 39 | 9 | 64.1/64.9 | 74 (66.5‐81.5) | 33 | 19 | 4 | 63.4 | 60.1 (55.6‐64.4) | |
| 14 | 5 | 9 | 73 (5) | 40% (19) | 14 | 10 | 4 | 70 (6) | 39% (21) | |
| 20 | na | na | na | 28 (7.5) | 20 | na | na | na | 26 (7.1) | |
| 61 | 30 | 31 | 69.9 (9.6) | 42.9 (15.5) | 61 | 30 | 31 | 69.68 (10.4) | 48.9 (18.69) | |
| 15 | 14 | 1 | 61 (6) | 40% (20) | 15 | 12 | 3 | 63 (5) | 43% (9) | |
| 15 | 3 | 9 | 66 | 35.1 (7.6) | 15 | 10 | 4 | 64 | 32.3 (9.5) | |
| 10 | 7 | 3 | 60 (9) | 57.2 | 10 | 8 | 2 | 58 (6) | 55.7 | |
| 102 | 72 | 30 | 65.9 (8.8) | 58 (17) | 97 | 69 | 28 | 67.2 (8.9) | 60 (15) | |
| 16 | na | na | na | na | 15 | na | na | na | na | |
| 12 | 6 | 6 | 67 (9) | 32.8 (3) | 12 | 5 | 7 | 61 (9) | 39.2 (2.8) | |
| 32 | 31 | 1 | 67 (7)/68 (7) | 46 (10)/50 (14) | 9 | 9 | 0 | 66(10) | 52 (14) | |
| 28 | 23 | 5 | 64 (5) | 44% (11) | 15 | 14 | 1 | 62 (5) | 45% (9) | |
| 25 | 22 | 3 | 54 (6) | 42% (16) | 25 | 21 | 4 | 54 (6) | 40% (17) | |
| na: not available. | ||||||||||
| Study | Follow‐up | Duration (weeks) | Setting | Programme type |
| 14 weeks | 14 | Outpatient | Exercise + other | |
| 6 months | 8 | Community | Exercise + other | |
| 3, 6 months | 24 | Inpatient | Exercise + other | |
| 12, 24 weeks | 12 | Outpatient | Exercise | |
| 3, 6, 12 months | 9 | Home | Exercise + other | |
| 6 weeks | 6 | Outpatient | Exercise | |
| 12 weeks | 12 | Home | Exercise + other | |
| 18 weeks | 18 | Home | Exercise | |
| 3 months | 12 | Community | Exercise + other | |
| 10 weeks | 10 | Outpatient | Exercise + other | |
| 12 weeks | 8 | Community | Exercise + other | |
| 12 weeks | 12 | Outpatient | Exercise | |
| 3 months | 12 | Community | Exercise | |
| 8 weeks | 8 | Outpatient | Exercise | |
| 12 weeks | 12 | Home | Exercise | |
| 6 weeks, 6 months, 12 months | 6 | Outpatient | Exercise + other | |
| 2, 6 months | 6 | Outpatient | Exercise | |
| 8 weeks | 8 | Community | Exercise | |
| 8 weeks | 7 | Outpatient | Exercise + other | |
| 1, 3 months | 12 | Community /Home | Exercise + other | |
| 10 weeks | 10 | Outpatient | Exercise + other | |
| 12 months | 52 | Outpatient /Home | Exercise + other | |
| 8 weeks, 6 months | 8 | Inpatient /Home | Exercise + other | |
| week 9 | 8 | Community | Exercise + other | |
| 1 year | 52 | Home | Exercise + other | |
| 12, 24 weeks | 6 | Outpatient | Exercise + other | |
| 12 months | 52 | Community | Exercise | |
| 24 weeks | 8 | Inpatient | Exercise + other | |
| 6, 18 months | 24 | Outpatient | Exercise | |
| 6 months | 7 | Community | Exercise + other | |
| 1 year | 6 | Outpatients /Home | Exercise + other | |
| 3, 6 months | 12 | Community | Exercise + other | |
| 3, 6, 9, 12, 18, 24 months | 12 | Outpatient /Home | Exercise | |
| 8 weeks | 8 | Outpatient | Exercise | |
| 8 weeks, 6 months | 8 | Outpatient | Exercise + other | |
| 12 weeks | 12 | Home | Exercise | |
| 8 weeks | 8 | Outpatient | Exercise | |
| 10 weeks | 10 | Home | Exercise | |
| 8, 12 weeks | 8 | Outpatient | Exercise + other | |
| 8 weeks | 8 | Outpatient | Exercise | |
| 6 weeks, 3 months | 6 | Community | Exercise + other | |
| 6 months | 24 | Inpatient /Home | Exercise | |
| 14 weeks | ?12 | Home | Exercise | |
| 8 weeks | 8 | Outpatient | Exercise | |
| 4 weeks | 4 | Outpatient | Exercise | |
| 12 weeks | 12 | Outpatient /Home | Exercise + other | |
| 3, 6 months | 24 | Nursing home | Exercise + other | |
| 3, 6 months | 12 | Outpatient /Home | Exercise | |
| 1 month | 4 | Outpatient | Exercise | |
| 8 weeks | 8 | Outpatient | Exercise | |
| 8 weeks | 8 | Home | Exercise + other | |
| 6 weeks | 6 | Outpatient | Exercise + other | |
| 8 weeks | 8 | Outpatient | Exercise + other | |
| 8 weeks | 8 | Outpatient | Exercise | |
| 4 weeks | 4 | Home | Exercise | |
| 6 months | 6 | Outpatients /Home | Exercise + other | |
| 3, 6, 12, 18 months | 12 | Outpatient | Exercise + other | |
| 12 weeks | 12 | Outpatient /Home | Exercise + other | |
| 8 weeks | 8 | Inpatient | Exercise | |
| 4 months | 12 | Community | Exercise + other | |
| Unclear | 6 | Unclear | Exercise | |
| 6 months | 24 | Outpatient | Exercise | |
| 12 weeks | 12 | Outpatient | Exercise | |
| 12 weeks | 12 | Outpatient /Home | Exercise + other | |
| 12 weeks | 12 | Home | Exercise |
| Pulmonary rehabilitation versus usual care. Subgroup: community versus hospital‐delivered programme | |||||
| Outcome | Subscale | Subgroups | Heterogeneity | MD [95% CI] | Test for subgroup differences |
| CRQ | Fatigue | Community | Tau² = 0.10; I² = 52% | 0.44 [0.14, 0.75] | Chi² = 3.98, df = 1 (P value 0.05), I² = 74.9% |
| Hospital | Tau² = 0.09; I² = 51% | 0.86 [0.58, 1.14] | |||
| CRQ | Emotional Function | Community | Tau² = 0.00; I² = 0% | 0.21 [0.04, 0.39] | Chi² = 12.24, df = 1 (P value 0.0005), I² = 91.8% |
| Hospital | Tau² = 0.06; I² = 39% | 0.77 [0.51, 1.03] | |||
| CRQ | Mastery | Community | Tau² = 0.07; I² = 45% | 0.40 [0.12, 0.67] | Chi² = 8.58, df = 1 (P value 0.003), I² = 88.3% |
| Hospital | Tau² = 0.05; I² = 31% | 0.95 [0.70, 1.20] | |||
| CRQ | Dyspnoea | Community | Tau² = 0.03; I² = 26% | 0.58 [0.34, 0.81] | Chi² = 4.05, df = 1 (P value 0.04), I² = 75.3% |
| Hospital | Tau² = 0.17; I² = 60% | 0.99 [0.66, 1.32] | |||
| SGRQ | Total | Community | Tau² = 24.00; I² = 73% | ‐8.15 [‐12.16, ‐4.13] | Chi² = 0.69, df = 1 (P value 0.41), I² = 0% |
| Hospital | Tau² = 6.41; I² = 35% | ‐6.05 [‐8.91, ‐3.20] | |||
| SGRQ | Symptoms | Community | Tau² = 6.28; I² = 24% | ‐3.66 [‐7.07, ‐0.24] | Chi² = 1.65, df = 1 (P value 0.20), I² = 39.2% |
| Hospital | Tau² = 4.96; I² = 15% | ‐6.91 [‐10.51, ‐3.30] | |||
| SGRQ | Impact | Community | Tau² = 19.91; I² = 63% | ‐8.17 [‐12.00, ‐4.34] | Chi² = 0.46, df = 1 (P value 0.50), I² = 0% |
| Hospital | Tau² = 22.39; I² = 58% | ‐6.21 [‐10.33, ‐2.09] | |||
| SGRQ | Activity | Community | Tau² = 48.91; I² = 78% | ‐7.82 [‐13.37, ‐2.28] | Chi² = 0.93, df = 1 (P value 0.33), I² = 0% |
| Hospital | Tau² = 10.45; I² = 36% | ‐4.58 [‐8.16, ‐1.00] | |||
| Pulmonary rehabilitation versus usual care. Subgroup: exercise only programme versus exercise plus additional elements in programme | |||||
| Outcome | Subscale | Subgroups | Heterogeneity | MD [95% CI] | Test for subgroup differences |
| CRQ | Fatigue | Exercise only | Tau² = 0.00; I² = 0% | 0.73 [0.54, 0.92] | Chi² = 0.26, df = 1 (P value 0.61), I² = 0% |
| Exercise + other | Tau² = 0.29; I² = 79% | 0.61 [0.18, 1.03] | |||
| CRQ | Emotional Function | Exercise only | Tau² = 0.00; I² = 0% | 0.51 [0.31, 0.71] | Chi² = 0.09, df = 1 (P value 0.77), I² = 0% |
| Exercise + other | Tau² = 0.28; I² = 79% | 0.58 [0.16, 1.00] | |||
| CRQ | Mastery | Exercise only | Tau² = 0.01; I² = 11% | 0.66 [0.44, 0.88] | Chi² = 0.12, df = 1 (P value 0.73), I² = 0% |
| Exercise + other | Tau² = 0.31; I² = 79% | 0.74 [0.31, 1.18] | |||
| CRQ | Dyspnoea | Exercise only | Tau² = 0.06; I² = 31% | 0.83 [0.56, 1.10] | Chi² = 0.13, df = 1 (P value 0.72), I² = 0% |
| Exercise + other | Tau² = 0.25; I² = 77% | 0.74 [0.35, 1.13] | |||
| SGRQ | Total | Exercise only | Tau² = 62.83; I² = 70% | ‐7.87 [‐16.72, 0.98] | |
| Exercise + other | Tau² = 10.17; I² = 56% | ‐6.76 [‐9.19, ‐4.34] | Chi² = 0.06, df = 1 (P value 0.81), I² = 0% | ||
| SGRQ | Symptoms | Exercise only | Tau² = 0.00; I² = 0% | ‐7.38 [‐12.33, ‐2.44] | |
| Exercise + other | Tau² = 13.88; I² = 41% | ‐4.38 [‐7.62, ‐1.15] | Chi² = 0.99, df = 1 (P value 0.32), I² = 0% | ||
| SGRQ | Impact | Exercise only | Tau² = 33.34; I² = 63% | ‐6.11 [‐12.60, 0.38] | |
| Exercise + other | Tau² = 17.12; I² = 59% | ‐7.61 [‐10.64, ‐4.57] | Chi² = 0.17, df = 1 (P value 0.68), I² = 0% | ||
| SGRQ | Activity | Exercise only | Tau² = 139.67; I² = 78% | ‐9.33 [‐21.66, 2.99] | Chi² = 0.30, df = 1 (P value 0.59), I² = 0% |
| Exercise + other | Tau² = 18.51; I² = 60% | ‐5.79 [‐8.95, ‐2.64] | |||
| CRQ: Chronic Respiratory Disease Questionnaire; MD: mean difference; SGRQ: St. George's Respiratory Questionnaire. | |||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 QoL ‐ Change in CRQ (Fatigue) Show forest plot | 19 | 1291 | Mean Difference (IV, Random, 95% CI) | 0.68 [0.45, 0.92] |
| 2 QoL ‐ Change in CRQ (Emotional Function) Show forest plot | 19 | 1291 | Mean Difference (IV, Random, 95% CI) | 0.56 [0.34, 0.78] |
| 3 QoL ‐ Change in CRQ (Mastery) Show forest plot | 19 | 1212 | Mean Difference (IV, Random, 95% CI) | 0.71 [0.47, 0.95] |
| 4 QoL ‐ Change in CRQ (Dyspnoea) Show forest plot | 19 | 1283 | Mean Difference (IV, Random, 95% CI) | 0.79 [0.56, 1.03] |
| 5 QoL ‐ Change in SGRQ (Total) Show forest plot | 19 | 1146 | Mean Difference (IV, Random, 95% CI) | ‐6.89 [‐9.26, ‐4.52] |
| 6 QoL ‐ Change in SGRQ (Symptoms) Show forest plot | 19 | 1153 | Mean Difference (IV, Random, 95% CI) | ‐5.09 [‐7.69, ‐2.49] |
| 7 QoL ‐ Change in SGRQ (Impacts) Show forest plot | 19 | 1149 | Mean Difference (IV, Random, 95% CI) | ‐7.23 [‐9.91, ‐4.55] |
| 8 QoL ‐ Change in SGRQ (Activity) Show forest plot | 19 | 1148 | Mean Difference (IV, Random, 95% CI) | ‐6.08 [‐9.28, ‐2.88] |
| 9 Maximal Exercise (Incremental shuttle walk test) Show forest plot | 8 | 694 | Mean Difference (IV, Random, 95% CI) | 39.77 [22.38, 57.15] |
| 10 Maximal Exercise Capacity (cycle ergometer) Show forest plot | 16 | 779 | Mean Difference (IV, Random, 95% CI) | 6.77 [1.89, 11.65] |
| 11 Functional Exercise Capacity (6MWT)) Show forest plot | 38 | 1879 | Mean Difference (IV, Random, 95% CI) | 43.93 [32.64, 55.21] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 QoL ‐ Change in CRQ (Fatigue) Show forest plot | 19 | 1291 | Mean Difference (IV, Random, 95% CI) | 0.68 [0.45, 0.92] |
| 1.1 QoL ‐ Community CRQ (Fatigue) | 9 | 648 | Mean Difference (IV, Random, 95% CI) | 0.44 [0.14, 0.75] |
| 1.2 QoL ‐ Hospital CRQ (Fatigue) | 10 | 643 | Mean Difference (IV, Random, 95% CI) | 0.86 [0.58, 1.14] |
| 2 QoL ‐ Change in CRQ (Emotional Function) Show forest plot | 19 | 1291 | Mean Difference (IV, Random, 95% CI) | 0.56 [0.34, 0.78] |
| 2.1 QoL ‐ Community (Emotional Function) | 9 | 648 | Mean Difference (IV, Random, 95% CI) | 0.21 [0.04, 0.39] |
| 2.2 QoL ‐ Hospital CRQ (Emotional Function) | 10 | 643 | Mean Difference (IV, Random, 95% CI) | 0.77 [0.51, 1.03] |
| 3 QoL ‐ Change in CRQ (Mastery) Show forest plot | 19 | 1212 | Mean Difference (IV, Random, 95% CI) | 0.71 [0.47, 0.95] |
| 3.1 QoL ‐ Community CRQ (Mastery) | 9 | 569 | Mean Difference (IV, Random, 95% CI) | 0.40 [0.12, 0.67] |
| 3.2 QoL ‐ Hospital CRQ (Mastery) | 10 | 643 | Mean Difference (IV, Random, 95% CI) | 0.95 [0.70, 1.20] |
| 4 QoL ‐ Change in CRQ (Dyspnoea) Show forest plot | 19 | 1283 | Mean Difference (IV, Random, 95% CI) | 0.82 [0.59, 1.05] |
| 4.1 QoL ‐ Community Based CRQ (Dyspnoea) | 8 | 633 | Mean Difference (IV, Random, 95% CI) | 0.58 [0.34, 0.81] |
| 4.2 QoL ‐ Hospital Based CRQ (Dyspnoea) | 11 | 650 | Mean Difference (IV, Random, 95% CI) | 0.99 [0.66, 1.32] |
| 5 QoL ‐ Change in SGRQ (Total) Show forest plot | 19 | 1146 | Mean Difference (IV, Random, 95% CI) | ‐6.89 [‐9.26, ‐4.52] |
| 5.1 QoL ‐ Community in SGRQ (Total) | 9 | 643 | Mean Difference (IV, Random, 95% CI) | ‐8.15 [‐12.16, ‐4.13] |
| 5.2 QoL ‐ Hospital SGRQ (Total) | 10 | 503 | Mean Difference (IV, Random, 95% CI) | ‐6.05 [‐8.91, ‐3.20] |
| 6 QoL ‐ Change in SGRQ (Symptoms) Show forest plot | 19 | 1153 | Mean Difference (IV, Random, 95% CI) | ‐5.09 [‐7.69, ‐2.49] |
| 6.1 QoL ‐ Community SGRQ (Symptoms) | 9 | 649 | Mean Difference (IV, Random, 95% CI) | ‐3.66 [‐7.07, ‐0.24] |
| 6.2 QoL ‐ Hospital SGRQ (Symptoms) | 10 | 504 | Mean Difference (IV, Random, 95% CI) | ‐6.91 [‐10.51, ‐3.30] |
| 7 QoL ‐ Change in SGRQ (Impacts) Show forest plot | 19 | 1149 | Mean Difference (IV, Random, 95% CI) | ‐7.23 [‐9.91, ‐4.55] |
| 7.1 QoL ‐ Community SGRQ (Impacts) | 9 | 646 | Mean Difference (IV, Random, 95% CI) | ‐8.17 [‐10.00, ‐4.34] |
| 7.2 QoL ‐ Hospital SGRQ (Impacts) | 10 | 503 | Mean Difference (IV, Random, 95% CI) | ‐6.21 [‐10.33, ‐2.09] |
| 8 QoL ‐ Change in SGRQ (Activity) Show forest plot | 19 | 1148 | Mean Difference (IV, Random, 95% CI) | ‐6.08 [‐9.28, ‐2.88] |
| 8.1 QoL ‐ Community SGRQ (Activity) | 9 | 645 | Mean Difference (IV, Random, 95% CI) | ‐7.82 [‐13.37, ‐2.28] |
| 8.2 QoL ‐ Hospital SGRQ (Activity) | 10 | 503 | Mean Difference (IV, Random, 95% CI) | ‐4.58 [‐8.16, 1.00] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 QoL ‐ Change in CRQ (Fatigue) Show forest plot | 19 | 1291 | Mean Difference (IV, Random, 95% CI) | 0.68 [0.45, 0.92] |
| 1.1 QoL ‐ Exercise Only CRQ (Fatigue) | 10 | 480 | Mean Difference (IV, Random, 95% CI) | 0.73 [0.54, 0.92] |
| 1.2 QoL ‐ Exercise + Other CRQ (Fatigue) | 9 | 811 | Mean Difference (IV, Random, 95% CI) | 0.61 [0.18, 1.03] |
| 2 QoL ‐ Change in CRQ (Emotional Function) Show forest plot | 19 | 1291 | Mean Difference (IV, Random, 95% CI) | 0.56 [0.34, 0.78] |
| 2.1 QoL ‐ Exercise Only CRQ (Emotional Function) | 10 | 480 | Mean Difference (IV, Random, 95% CI) | 0.51 [0.31, 0.71] |
| 2.2 QoL ‐ Exercise + Other CRQ (Emotional Function) | 9 | 811 | Mean Difference (IV, Random, 95% CI) | 0.58 [0.16, 1.00] |
| 3 QoL ‐ Change in CRQ (Mastery) Show forest plot | 19 | 1212 | Mean Difference (IV, Random, 95% CI) | 0.71 [0.47, 0.95] |
| 3.1 QoL ‐ Exercise Only CRQ (Mastery) | 10 | 480 | Mean Difference (IV, Random, 95% CI) | 0.66 [0.44, 0.88] |
| 3.2 QoL ‐ Exercise + Other CRQ (Mastery) | 9 | 732 | Mean Difference (IV, Random, 95% CI) | 0.74 [0.31, 1.18] |
| 4 QoL ‐ Change in CRQ (Dyspnoea) Show forest plot | 19 | 1283 | Mean Difference (IV, Random, 95% CI) | 0.79 [0.56, 1.03] |
| 4.1 QoL ‐ Exercise Only CRQ (Dyspnoea) | 10 | 474 | Mean Difference (IV, Random, 95% CI) | 0.83 [0.56, 1.09] |
| 4.2 QoL ‐ Exercise + Other CRQ (Dyspnoea) | 9 | 809 | Mean Difference (IV, Random, 95% CI) | 0.74 [0.35, 1.13] |
| 5 QoL ‐ Change in SGRQ (Total) Show forest plot | 19 | 1146 | Mean Difference (IV, Random, 95% CI) | ‐6.89 [‐9.26, ‐4.52] |
| 5.1 QoL Exercise Only SGRQ (Total) | 5 | 230 | Mean Difference (IV, Random, 95% CI) | ‐7.87 [‐16.72, 0.98] |
| 5.2 QoL Exercise + Other SGRQ (Total) | 14 | 916 | Mean Difference (IV, Random, 95% CI) | ‐6.76 [‐9.19, ‐4.34] |
| 6 QoL ‐ Change in SGRQ (Symptoms) Show forest plot | 19 | 1153 | Mean Difference (IV, Random, 95% CI) | ‐5.09 [‐7.69, ‐2.49] |
| 6.1 QoL ‐ Exercise Only SGRQ (Symptoms) | 5 | 230 | Mean Difference (IV, Random, 95% CI) | ‐7.38 [‐12.33, ‐2.44] |
| 6.2 QoL ‐ Exercise + Other SGRQ (Symptoms) | 14 | 923 | Mean Difference (IV, Random, 95% CI) | ‐4.38 [‐7.62, ‐1.15] |
| 7 QoL ‐ Change in SGRQ (Impacts) Show forest plot | 19 | 1149 | Mean Difference (IV, Random, 95% CI) | ‐7.23 [‐9.91, ‐4.55] |
| 7.1 QoL ‐ Exercise Only SGRQ (Impacts) | 5 | 230 | Mean Difference (IV, Random, 95% CI) | ‐6.11 [‐12.60, 0.38] |
| 7.2 QoL ‐ Exercise + Other SGRQ (Impacts) | 14 | 919 | Mean Difference (IV, Random, 95% CI) | ‐7.61 [‐10.64, ‐4.57] |
| 8 QoL ‐ Change in SGRQ (Activity) Show forest plot | 19 | 1148 | Mean Difference (IV, Random, 95% CI) | ‐6.08 [‐9.28, ‐2.88] |
| 8.1 QoL ‐ Exercise Only SGRQ (Activity) | 5 | 230 | Mean Difference (IV, Random, 95% CI) | ‐9.33 [‐21.66, 2.99] |
| 8.2 QoL ‐ Exercise + Other SGRQ (Activity) | 14 | 918 | Mean Difference (IV, Random, 95% CI) | ‐5.79 [‐8.95, ‐2.64] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 QoL ‐ Change in CRQ (Dyspnoea) Show forest plot | 5 | 384 | Mean Difference (IV, Random, 95% CI) | 0.99 [0.64, 1.34] |
| 1.1 QoL ‐ Low Risk CRQ (Dyspnoea) | 5 | 384 | Mean Difference (IV, Random, 95% CI) | 0.99 [0.64, 1.34] |
| 2 QoL ‐ Change in CRQ (Emotional Function) Show forest plot | 5 | 386 | Mean Difference (IV, Random, 95% CI) | 0.60 [0.09, 1.11] |
| 2.1 QoL ‐ Low Risk (Emotional Function) | 5 | 386 | Mean Difference (IV, Random, 95% CI) | 0.60 [0.09, 1.11] |
| 3 QoL ‐ Low Risk CRQ (Fatigue) Show forest plot | 5 | 386 | Mean Difference (IV, Random, 95% CI) | 0.90 [0.41, 1.39] |
| 4 QoL ‐ Low Risk CRQ (Mastery) Show forest plot | 5 | 386 | Mean Difference (IV, Random, 95% CI) | 0.77 [0.28, 1.26] |
| 5 QoL ‐ Low Risk SGRQ (Total) Show forest plot | 7 | 572 | Mean Difference (IV, Random, 95% CI) | ‐5.15 [‐7.95, ‐2.36] |
| 6 QoL ‐ Low Risk SGRQ (Symptoms) Show forest plot | 7 | 572 | Mean Difference (IV, Random, 95% CI) | ‐4.12 [‐8.45, 0.21] |
| 7 QoL ‐ Low Risk SGRQ (Impacts) Show forest plot | 7 | 572 | Mean Difference (IV, Random, 95% CI) | ‐5.92 [‐10.01, ‐1.82] |
| 8 QoL ‐ Low Risk SGRQ (Activity) Show forest plot | 7 | 572 | Mean Difference (IV, Random, 95% CI) | ‐5.33 [‐8.10, ‐2.57] |


