Abordajes quirúrgicos de la histerectomía para las enfermedades ginecológicas benignas
Appendices
Appendix 1. MDSG search
MDSG Specialised Register SS for NJ473 11.11.10
Keywords CONTAINS "Hysterectomy" or Title CONTAINS "Hysterectomy"
AND
Keywords CONTAINS "Hysterectomy,abdominal" or "Hysterectomy, Vaginal" or "hysterectomy ‐laparoscopic" or "hysterectomy, laparoscopically assisted vaginal" or "Hysterectomy, subtotal" or "hysterectomy techniques" or "laparoscopic assisted vaginal hysterectomy" or "laparoscopic hysterectomy" or "LAVH" or Title CONTAINS "Hysterectomy,abdominal" or "Hysterectomy, Vaginal" or "hysterectomy ‐laparoscopic" or "hysterectomy, laparoscopically assisted vaginal" or "Hysterectomy, subtotal" or "hysterectomy techniques" or "laparoscopic assisted vaginal hysterectomy" or "laparoscopic hysterectomy" or "LAVH" or "TVH" or "TLH" or "vaginal hysterectomy"or "abdominal hysterectomy"or "abdominal myomectomy"or"laparoscopic"or"laparoscopic procedure"or"laparoscopic surgical treatment"or"laparoscopically assisted hysterectomy"or"laparoscopically assisted vaginal hysterectomy"or"laparoscopy"or "laparotomy"or"mini‐laparoscopy"or "mini‐laparotomy"or "abdominal hysterectomy"
Appendix 2. CENTRAL search
Cochrane Central Register of Controlled Trials (CENTRAL) in all fields (on Ovid platform)
1. Hysterectomy
2. Abdominal
3. Vaginal
4. Laparoscopic assisted
5. Laparo‐vaginal
6. Laparoscopic
7. 1 and 2 or 3 or 4 or 5 or 6
Appendix 3. MEDLINE search
Ovid MEDLINE(R) (1946 to 2014 week 32)
Search strategy:
1 exp HYSTERECTOMY/ (24605)
2 hysterectom$.tw. (26883)
3 1 or 2 (37348)
4 abdom$.tw. (253636)
5 vaginal$.tw. (74351)
6 (lap$ adj assist$).tw. (3843)
7 (lap$ adj5 vaginal$).tw. (1692)
8 LAVH.tw. (324)
9 LVH.tw. (3897)
10 (Ah or Vh or Lh).tw. (62452)
11 TLH.tw. (309)
12 exp Laparoscopy/ (69937)
13 Laparoscop$.tw. (84412)
14 route$.tw. (121604)
15 technique$.tw. (1094816)
16 approach$.tw. (1056843)
17 exp Laparotomy/ (15750)
18 laparotom$.tw. (38835)
19 minilaparotom$.tw. (927)
20 or/4‐19 (2520921)
21 3 and 20 (16470)
22 randomized controlled trial.pt. (385723)
23 controlled clinical trial.pt. (89662)
24 randomized.ab. (305899)
25 placebo.tw. (162963)
26 clinical trials as topic.sh. (172008)
27 randomly.ab. (220260)
28 trial.ti. (131972)
29 (crossover or cross‐over or cross over).tw. (62251)
30 or/22‐29 (950838)
31 exp animals/ not humans.sh. (3994784)
32 30 not 31 (876347)
33 21 and 32 (1715)
34 2014$.ed. (619882)
35 2014$.dp. (613080)
36 34 or 35 (1063755)
37 33 and 36 (106)
Appendix 4. EMBASE search
EMBASE (1980 to 2014 Week 32)
1 Controlled study/ or randomised controlled trial/
2 double blind procedure/
3 single blind procedure/
4 crossover procedure/
5 drug comparison/
6 placebo/
7 random$.ti,ab,hw,tn,mf.
8 latin square.ti,ab,hw,tn,mf.
9 crossover.ti,ab,hw,tn,mf.
10 cross‐over.ti,ab,hw,tn,mf.
11 placebo$.ti,ab,hw,tn,mf.
12 ((doubl$ or singl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).ti,ab,hw,tn,mf.
13 (comparative adj5 trial$).ti,ab,hw,tn,mf.
14 (clinical adj5 trial$).ti,ab,hw,tn,mf.
15 or/1‐14
16 nonhuman/
17 animal/ not (human/ and animal/)
18 or/16‐17
19 15 not 18
20 exp HYSTERECTOMY/
21 hysterectom$.tw.
22 20 or 21
23 abdom$.tw.
24 vaginal$.tw.
25 (Lap$ adj Assist$).tw.
26 (Lap$ adj Vaginal$).tw.
27 LAVH.tw.
28 LH.tw.
29 or/23‐28
30 exp Surgical Technique/
31 route$.tw.
32 technique$.tw.
33 approach$.tw.
34 or/30‐33
35 22 and 29
36 34 and 35
37 19 and 36
Appendix 5. CINAHL search
CINAHL search strategy for NJ473 28.01.14
# Query Results
S38 S22 AND S36
S37 S22 AND S36
S36 S23 OR S24 or S25 or S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35
S35 TX allocat* random*
S34 (MH "Quantitative Studies")
S33 (MH "Placebos")
S32 TX placebo*
S31 TX random* allocat*
S30 (MH "Random Assignment")
S29 TX randomi* control* trial*
S28 TX ( (singl* n1 blind*) or (singl* n1 mask*) ) or TX ( (doubl* n1 blind*) or (doubl* n1 mask*) ) or TX ( (tripl* n1 blind*) or (tripl* n1 mask*) ) or TX ( (trebl* n1 blind*) or (trebl* n1 mask*) )
S27 TX ( (trebl* n1 blind*) or (trebl* n1 mask*) )
S26 TX ( (trebl* n1 blind*) or (trebl* n1 mask*) )
S25 TX clinic* n1 trial*
S24 PT Clinical trial
S23 (MH "Clinical Trials+")
S22 S3 AND S21
S21 S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20
S20 TX minilaparotom*
S19 TX laparotom*
S18 (MM "Laparotomy")
S17 TX approach*
S16 TX technique*
S15 TX route*
S14 TX Laparoscop*
S13 (MM "Laparoscopy")
S12 TX TLH
S11 TX (Ah or Vh or Lh)
S10 TX LVH
S9 TX LAVH
S8 TX (lap* N2 vagina*)
S7 TX (lap* N2 assist*)
S6 TX vagina*
S5 (MM "Hysterectomy, Vaginal")
S4 TX abdomin*
S3 S1 OR S2
S2 TX Hysterectom*
S1 (MH "Hysterectomy+")
Appendix 6. Biological abstracts search
Biological Abstracts (1969 to August 2008, not included in searches beyond 2008)
1 exp HYSTERECTOMY/ (0)
2 hysterectom$.tw. (10663)
3 1 or 2 (10663)
4 abdom$.tw. (149794)
5 vaginal$.tw. (31662)
6 (lap$ adj assist$).tw. (691)
7 (lap$ adj5 vaginal$).tw. (540)
8 LAVH.tw. (71)
9 LVH.tw. (1654)
10 Laparoscop$.tw. (16487)
11 route$.tw. (373620)
12 technique$.tw. (3259392)
13 approach$.tw. (354093)
14 laparo$.tw. (29111)
15 or/4‐14 (3796162)
16 3 and 15 (7312)
17 limit 16 to yr="2007 ‐ 2008" (529)
18 from 17 keep 1‐529 (529)
Appendix 7. PsycINFO search
PsycINFO <1806 to August Week 1 2014>
Search strategy:
1 exp Hysterectomy/ (384)
2 hysterectom$.tw. (677)
3 or/1‐2 (698)
4 abdom$.tw. (4874)
5 vaginal$.tw. (3769)
6 (lap$ adj assist$).tw. (6)
7 (lap$ adj5 vaginal$).tw. (10)
8 LAVH.tw. (2)
9 LVH.tw. (23)
10 Laparoscop$.tw. (304)
11 route$.tw. (11033)
12 technique$.tw. (151513)
13 approach$.tw. (369519)
14 or/4‐13 (509044)
15 3 and 14 (149)
16 limit 15 to yr="2014 ‐Current" (2)
Appendix 8. Clinical Trials Register
1. Hysterectomy
2. Abdominal
3. Vaginal
4. Laparoscopic assisted
5. Laparo‐vaginal
6. Laparoscopic
7. 1 and 2 or 3 or 4 or 5 or 6
Appendix 9. Data extraction
-
Trial characteristics
-
Method of randomisation, in order of preference, as follows:
-
third party randomisation, for example by pharmacy, computer, or telephone;
-
true randomisation by carer, for example by opaque numbered envelope or register;
-
not stated.
-
-
Study design:
-
blinding;
-
duration of follow‐up;
-
type of follow‐up.
-
-
Size of study:
-
number of women recruited;
-
number of women randomised;
-
number of women excluded;
-
number of women withdrawn and lost to follow‐up;
-
number of women analysed.
-
-
Study setting:
-
single centre or multicentre;
-
location;
-
timing and duration;
-
source of funding stated or not.
-
-
Analyses:
-
whether a power calculation was performed and adhered to;
-
whether 'intention‐to‐treat' analysis was performed by authors, was possible from the data but not performed by authors, not possible or uncertain.
-
-
Criteria for hysterectomy:
-
indications specified;
-
data broken down by indications for hysterectomy.
-
-
-
Characteristics of the study participants
-
Baseline characteristics:
-
age;
-
parity;
-
indication for hysterectomy;
-
investigative work up, for example pelvic ultrasound scan, endometrial sampling;
-
previous treatments;
-
exclusion criteria.
-
-
Treatment characteristics:
-
pre‐operative preparation, for example pre‐operative medical treatment;
-
level of training of surgeons.
-
-
-
Interventions
-
Approach to hysterectomy, percentage of patients having subtotal hysterectomy
-
Subcategory in case of LH (i.e. LAVH, LH(a) and TLH)
-
Use of technique to support the vaginal vault
-
Proportion undergoing bilateral elective oophorectomy versus ovarian conservation
-
Other strategies to reduce the likelihood of complications
-
Absence of co‐interventions in treatment and control groups
-
If the trial compared a surgical approach performed by one (group of) surgeon(s) with another surgical approach performed by a second (group of) surgeon(s)
-
-
Outcomes
-
Primary outcomes:
-
1. Return to normal activities
-
2. Satisfaction and quality of life
-
3. Intra‐operative visceral injury: bladder injury, ureter injury, urinary tract (bladder or ureter) injury, bowel injury, vascular injury
-
4. Major long‐term complications: fistula, pelvi‐abdominal pain, urinary dysfunction, bowel dysfunction, pelvic floor condition (prolapse), sexual dysfunction
-
Secondary outcomes:
-
5. Operation time
-
6. Other intra‐operative complication: estimated blood loss, (sequelae of) bleeding, including substantial bleeding, haemoglobin or haematocrit drop, transfusion, pelvic haematoma, unintended laparotomy for approaches not involving routine laparotomy
-
7. Short‐term outcomes and complications: length of hospital stay, infections: vaginal cuff, abdominal wall or wound, urinary tract infection, chest infection, febrile episodes or unspecified infections, thromboembolism, perioperative mortality, postoperative ileus, wound dehiscence, pain scales and pain relief
-
8. Costs
-

'Risk of bias' summary: review authors' judgements about each methodological quality item for each included study.
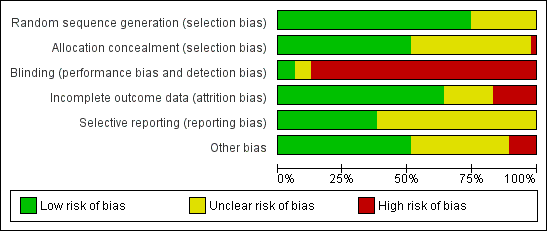
'Risk of bias' graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.

Forest plot of comparison: 1 VH versus AH, outcome: 1.1 Return to normal activities (days).

Forest plot of comparison: 2 LH versus AH, outcome: 2.1 Return to normal activities (days).
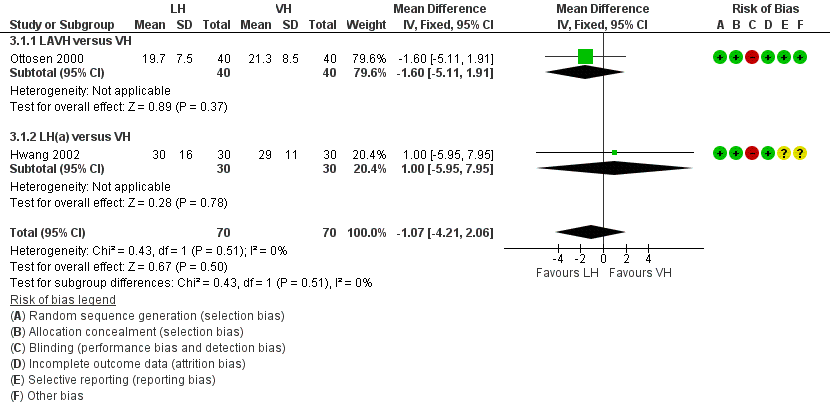
Forest plot of comparison: 3 LH versus VH, outcome: 3.1 Return to normal activities (days).
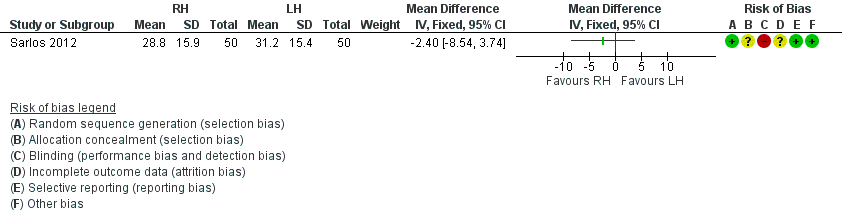
Forest plot of comparison: 4 RH versus LH, outcome: 4.1 Return to normal activities (days).

Comparison 1 VH versus AH, Outcome 1 Return to normal activities (days).

Comparison 1 VH versus AH, Outcome 2 Long‐term outcomes: satisfaction (dichotomous).
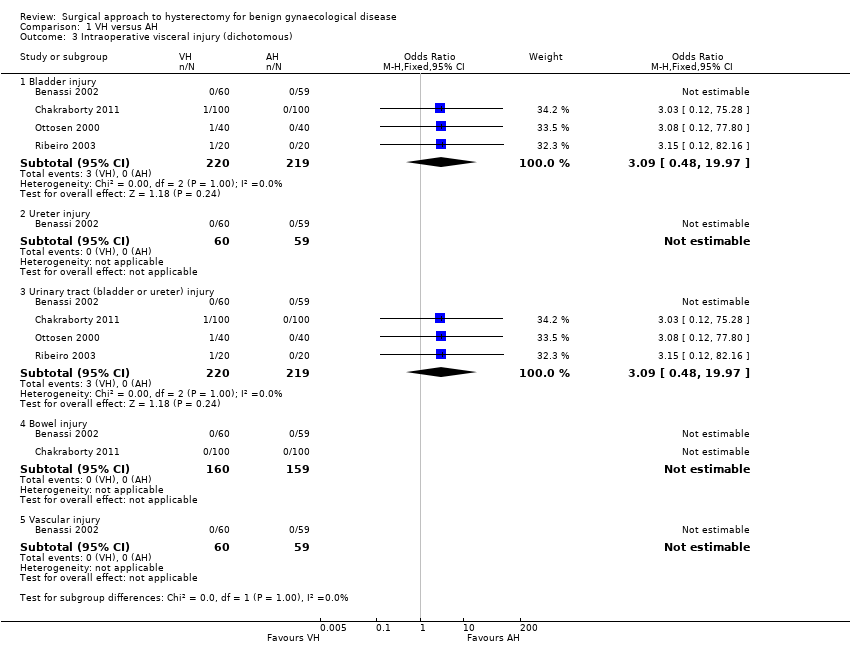
Comparison 1 VH versus AH, Outcome 3 Intraoperative visceral injury (dichotomous).
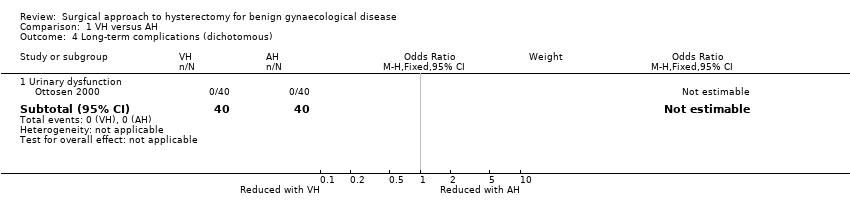
Comparison 1 VH versus AH, Outcome 4 Long‐term complications (dichotomous).

Comparison 1 VH versus AH, Outcome 5 Operation time (mins).
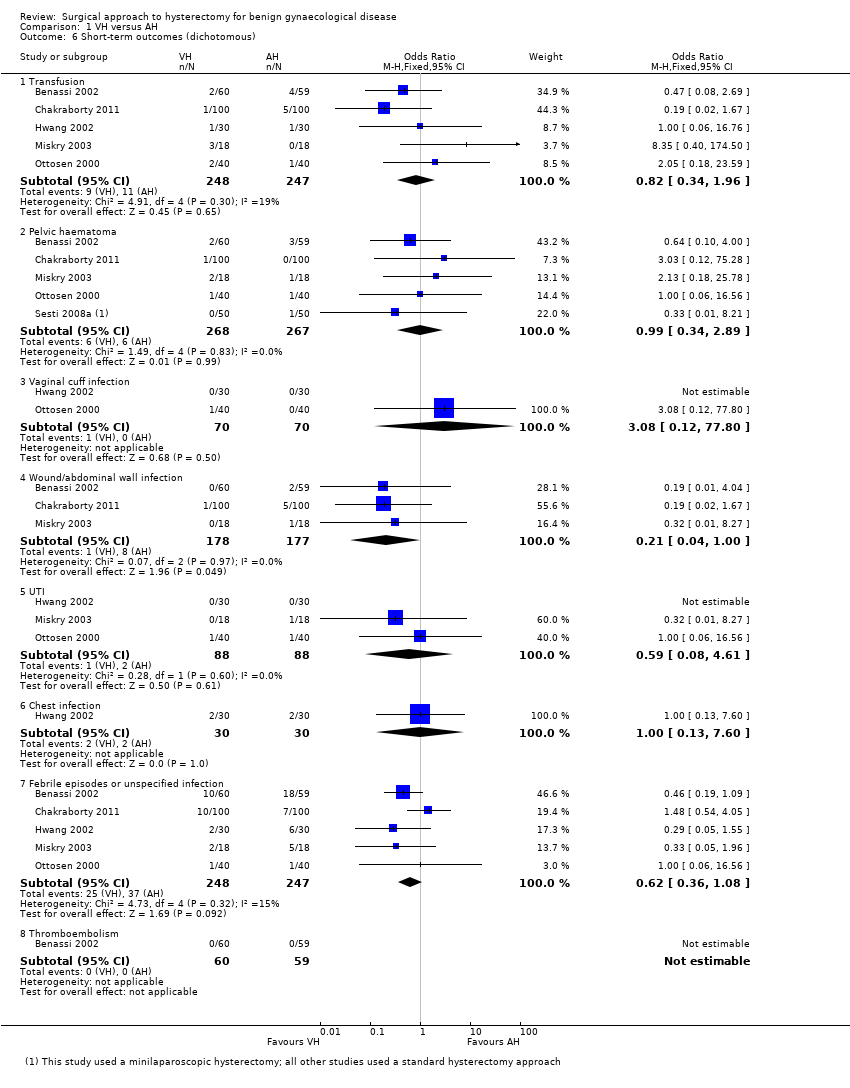
Comparison 1 VH versus AH, Outcome 6 Short‐term outcomes (dichotomous).

Comparison 1 VH versus AH, Outcome 7 Length of hospital stay (days).
| Study | VH | AH | Comments | |
| Quality of life (descriptive data) | ||||
| Silva Filho 2006 | Questionnaire SF‐36. Only data from functional capacity, physical aspect and pain are presented. A high score is a better quality of life | n = 30 | n = 30 | Functional capacity: VH mean = 95, IQ‐range = 75 to 100. AH mean = 72.5, IQ‐range = 55 to 90 A higher rate of patients in VH would choose the same therapeutic modality (90 % versus 65.5 %, P value = 0.021) |
| Operation time (descriptive data) | ||||
| Hwang 2002 | With 2nd procedure: | With 2nd procedure: | Not tested separately | |
| Miskry 2003 | Mean 68.8 (range 30 to 180) mins | Mean 68.2 (range 45 to 174) mins | — | |
| Ribeiro 2003 | Mean 78 mins | Mean 109 mins | No measure of spread stated | |
| Length of hospital stay (descriptive data) | ||||
| Hwang 2002 | n = 30 | n = 30 | Not tested separately | |
| Ribeiro 2003 | n = 20 | n = 20 | — | |
Comparison 1 VH versus AH, Outcome 8 All outcomes, descriptive data.

Comparison 2 LH versus AH, Outcome 1 Return to normal activities (days).
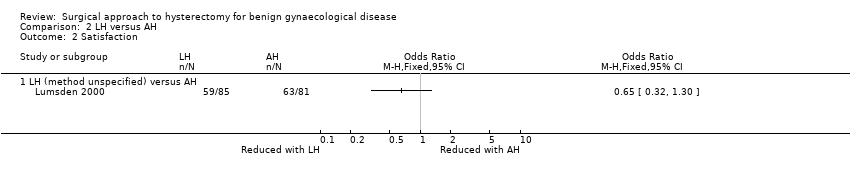
Comparison 2 LH versus AH, Outcome 2 Satisfaction.
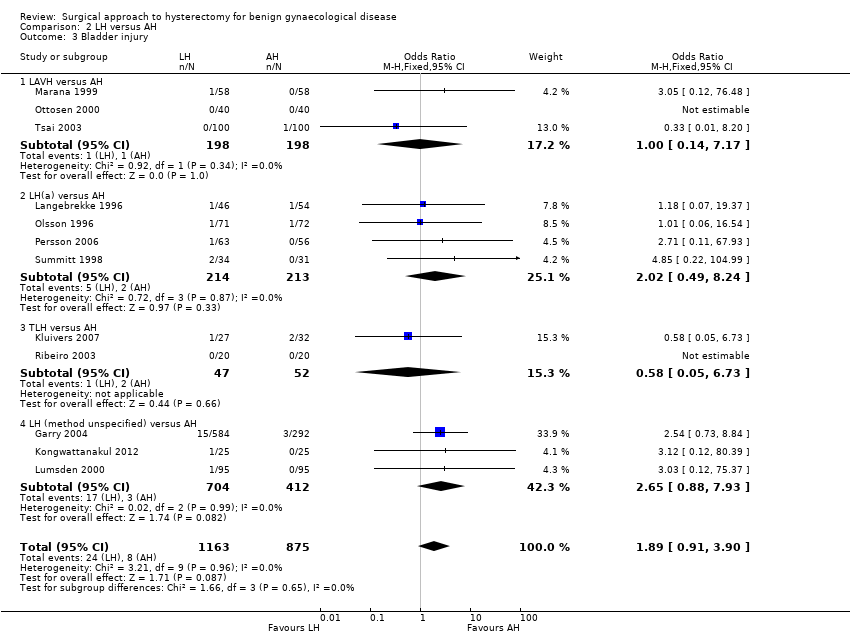
Comparison 2 LH versus AH, Outcome 3 Bladder injury.

Comparison 2 LH versus AH, Outcome 4 Ureter injury.
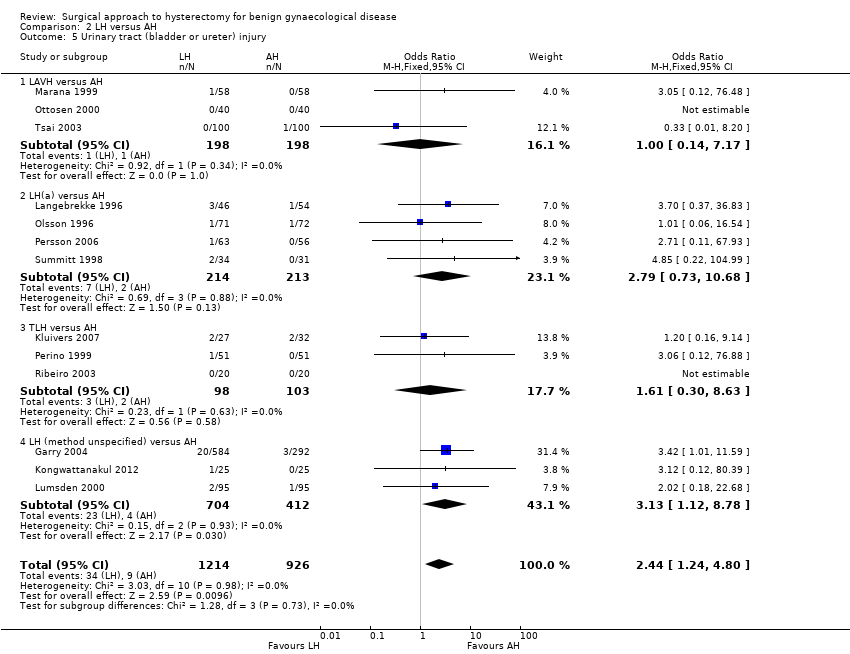
Comparison 2 LH versus AH, Outcome 5 Urinary tract (bladder or ureter) injury.

Comparison 2 LH versus AH, Outcome 6 Bowel injury.

Comparison 2 LH versus AH, Outcome 7 Vascular injury.

Comparison 2 LH versus AH, Outcome 8 Fistula.
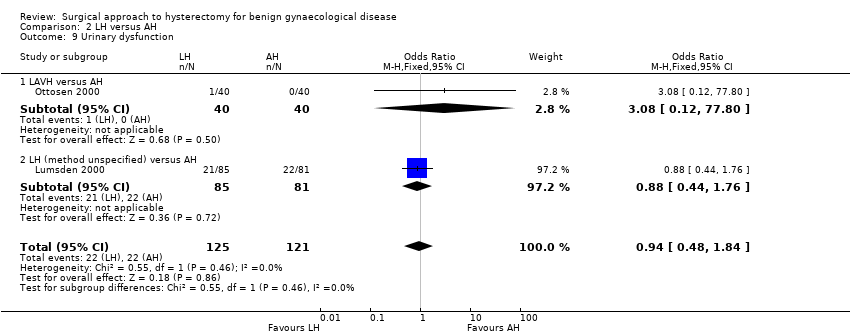
Comparison 2 LH versus AH, Outcome 9 Urinary dysfunction.
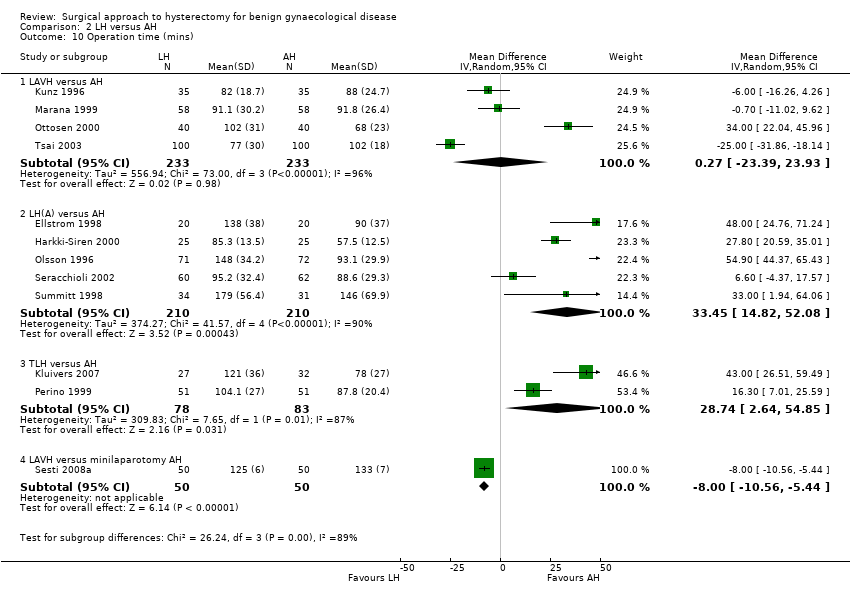
Comparison 2 LH versus AH, Outcome 10 Operation time (mins).

Comparison 2 LH versus AH, Outcome 11 Bleeding.
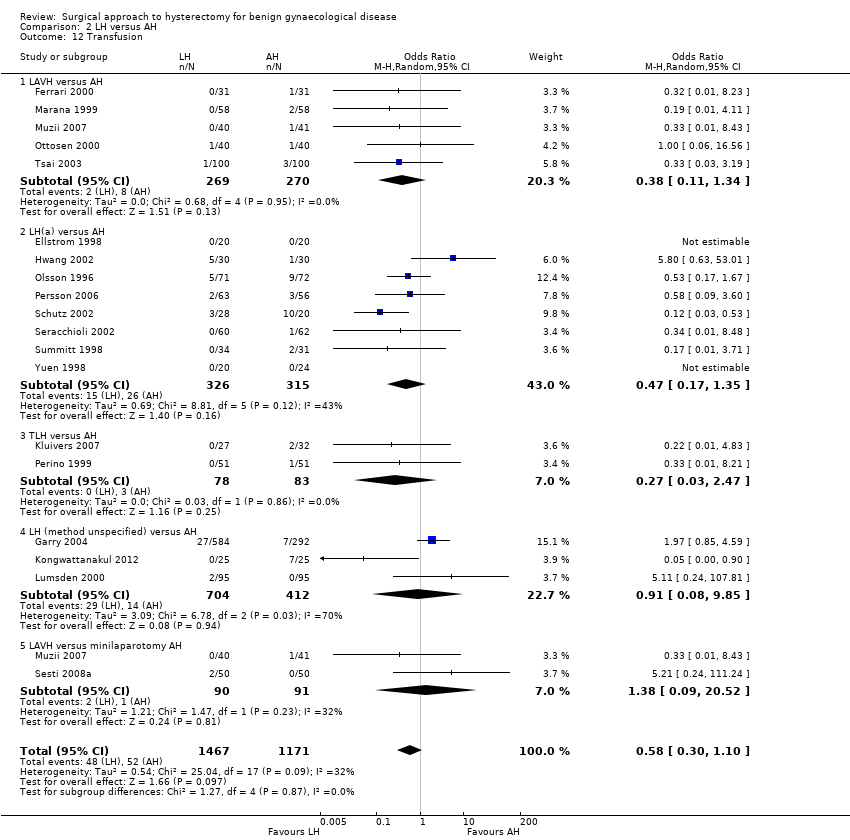
Comparison 2 LH versus AH, Outcome 12 Transfusion.

Comparison 2 LH versus AH, Outcome 13 Pelvic haematoma.
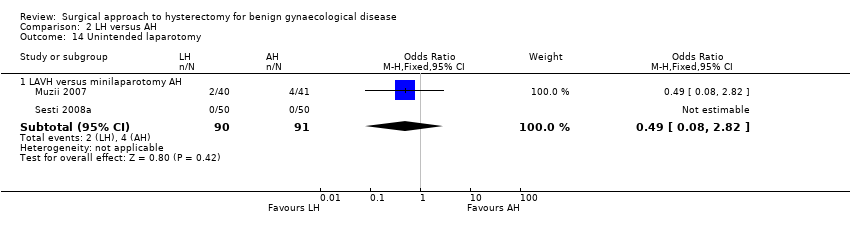
Comparison 2 LH versus AH, Outcome 14 Unintended laparotomy.
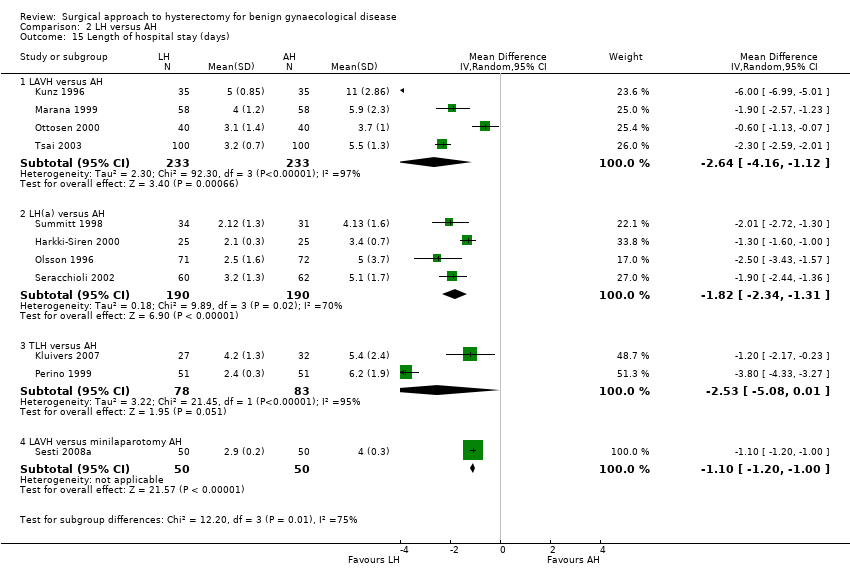
Comparison 2 LH versus AH, Outcome 15 Length of hospital stay (days).
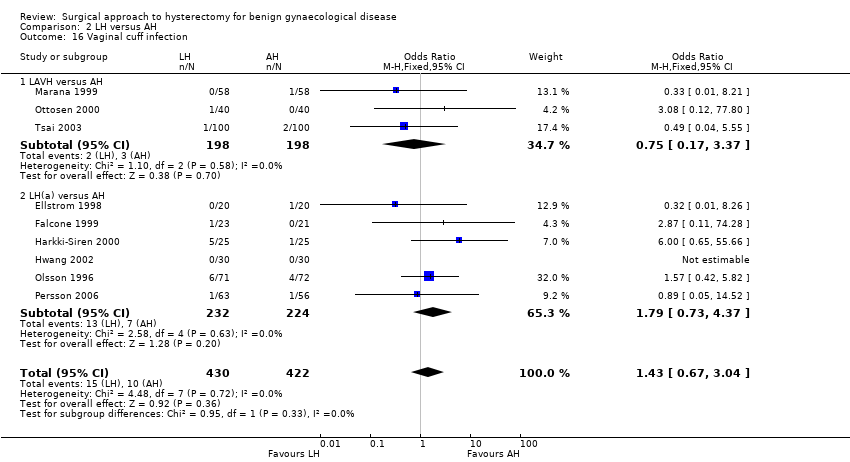
Comparison 2 LH versus AH, Outcome 16 Vaginal cuff infection.

Comparison 2 LH versus AH, Outcome 17 Wound/abdominal wall infection.

Comparison 2 LH versus AH, Outcome 18 Urinary tract infection.

Comparison 2 LH versus AH, Outcome 19 Chest infection.

Comparison 2 LH versus AH, Outcome 20 Febrile episodes or unspecified infection.
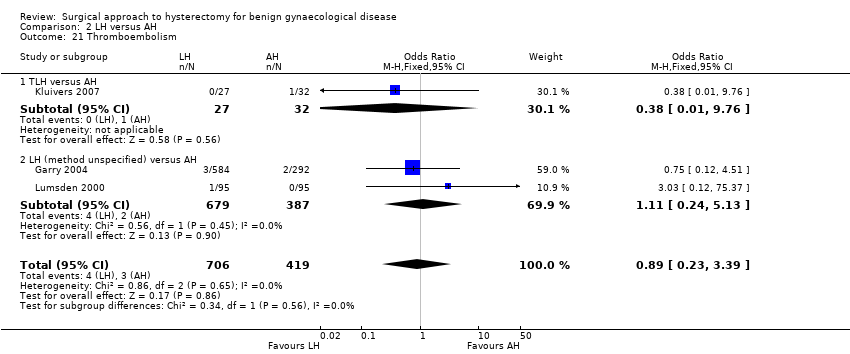
Comparison 2 LH versus AH, Outcome 21 Thromboembolism.
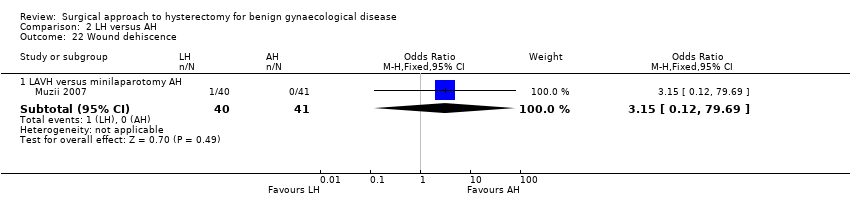
Comparison 2 LH versus AH, Outcome 22 Wound dehiscence.
| Study | LH | AH | Comments |
| Langebrekke 1996 | n = 46 | n = 54 | P value < 0.001 |
| Persson 2006 | n = 63 | n = 56 | P value = 0.0081 |
| Raju 1994 | n = 40 | n = 40 | P value < 0.0001 |
| Schutz 2002 | n = 28 | n = 20 | — |
Comparison 2 LH versus AH, Outcome 23 Return to normal activities (descriptive data).
| Study | Description | LH | AH | Comments |
| Garry 2004 | Questionnaire assessment of sexual activity, body image (BIS) and health status (SF‐12) before and after surgery (6 weeks, 4 months and 1 year) | SF scores | SF scores | SF scores |
| Kluivers 2007 | Questionnaire RAND‐36. A high score is a better quality of life. Statistical analysis with use of linear mixed model to evaluate the differences between 2 and 12 weeks while accounting for baseline value In Nieboer 2012, the same patients were evaluated with use of the same questionnaire 4 years after surgery | n = 27 at baseline n = 23 at 4 years | n = 32 at baseline n = 26 at 4 years | Difference (95%CI) in favour of LH (the score range on subscales is 100, score range on total RAND‐36 scales is 800) over the first 12 weeks: Analysis over 4 years follow up after surgery: Total RAND‐36 scores overall mean difference 50.4 points (95% confidence interval 1.0 –99.7) in favour of LH. Statistically significant higher scores were also found on the domains physical role functioning, social role functioning and vitality |
| Lumsden 2000 | EuroQol Health Questionnaire used to measure women's evaluation of their health state post surgery (1, 6 and 12 months after surgery). Use of a visual analogue thermometer (0 is worst imaginable health state and 100 is best imaginable health state). | 1 month (post‐op minus pre‐op): n = 74. Mean = 7, SD = 24.1. Median = 10, range (‐50 to 50) 6 months: n = 62. Mean = 11.3, SD = 23.9. Median = 15, range (‐50 to 60) | 1 month: n = 76. Mean = 6.8, SD = 19.2. Median = 8, range (‐50 to 60). | Mean difference: 1 month: ‐1.6 (‐7.2 to 6.9) |
| Olsson 1996 | 6 to 8 weeks after surgery participants were asked in an anonymous questionnaire if they considered the duration of their post‐operative stay adequate | 9% of women in the LAVH group considered their time in hospital following surgery to be too short | 17% of women in the AH group considered their time in hospital following surgery to be too short | — |
| Persson 2006 | Questionnaires: Psychological General Wellbeing (PGWI), Women Health Questionnaire (WHQ), Spielberger Trait Anxiety Inventory (STAI) and Beck's Depression Inventory (BDI) Persson 2008 analysed wellbeing on a 0 to 100 VAS and stress coping ability | n = 63 | n = 56 | Main effect between groups: PGWB P value = 0.719, WHQ P value = 0.800, STAI P value = 0.418, BDI P value = 0.788. Main effect over time: PGWB P value < 0.0001, WHQ P value < 0.0001, STAI P value = 0.0002, BDI P value = 0.0002 In Persson 2008: No significant difference was found in the day‐by‐day recovery of the general wellbeing between the operating methods. Stress coping ability did significantly influence the day‐by‐day recovery of general wellbeing |
Comparison 2 LH versus AH, Outcome 24 Long‐term outcomes: quality of life (descriptive data).
| Study | LH | AH | Comments |
| Falcone 1999 | n = 23 | n = 21 | LH(a) vs AH |
| Ferrari 2000 | n = 31 | n = 31 | LAVH vs AH |
| Garry 2004 | n = 584 | n = 292 | non‐categorisable LH vs AH |
| Hwang 2002 | With 2nd procedure | With 2nd procedure | LH(a) vs AH |
| Langebrekke 1996 | n = 46 | n = 54 | LH(a) vs AH |
| Muzii 2007 | n = 40 median = 86 mins range (60 to 120) | n = 41 median = 58 mins range (45 to 75) | LAVH vs minilaparotomy AH |
| Persson 2006 | n = 63 | n = 56 | LH(a) vs AH |
| Raju 1994 | n = 40 | n = 40 | LAVH vs AH |
| Ribeiro 2003 | n = 20 | n = 20 | TLH vs AH |
| Schutz 2002 | n = 28 | n = 20 | LH(a) vs AH |
| Yuen 1998 | n = 20 | n = 24 | LH(a) vs AH |
Comparison 2 LH versus AH, Outcome 25 Operation time (descriptive data).
| Study | LH | AH | Comments |
| Falcone 1999 | n = 23 | n = 21 | P value = 0.038 |
| Ferrari 2000 | n = 31 | n = 31 | P value < 0.001 |
| Garry 2004 | n = 584 | n = 292 | — |
| Hwang 2002 | n = 30 | n = 30 | Not tested separately |
| Langebrekke 1996 | n = 46 | n = 54 | P value < 0.001 |
| Muzii 2007 | n = 40 median = 2 days range (1 to 3) | n = 41 median = 3 days range = (1 to 5) | P value = 0.53 |
| Persson 2006 | n = 63 | n = 56 | P value = 0.0006 In the same population (described in Persson 2008), duration of sick leave was associated with the occurrence of postoperative complications but not with stress‐coping ability |
| Raju 1994 | n = 40 | n = 40 | P value < 0.0001 |
| Ribeiro 2003 | n = 20 | n = 20 | — |
| Schutz 2002 | n = 28 | n = 20 | — |
| Yuen 1998 | n = 20 | n = 24 | P value < 0.001 |
Comparison 2 LH versus AH, Outcome 26 Length of hospital stay (descriptive data).
| Study | Description | LH | AH | Conclusions |
| Pain scales | ||||
| Ellstrom 1998 | Pain during rest and when coughing. 100 mm visual analogue scale, endpoints 'no pain' and 'worst pain possible'. Day 0, Day 1 (10am and 6pm) and Day 2 | n = 40 | n = 40 | Lower pain score following LAVH compared to AH at 10am on 1st and 2nd day when coughing (P value < 0.05 and P value < 0.01 respectively). No significant difference with the pain scores at rest |
| Falcone 1999 | Weekly visual analogue scales for pain (from "no pain" to "most severe pain". Reported in graph form | n = 22 | n = 20 | No significant difference in change over time (group by time interaction) between groups. No difference in mean pain scores over the postoperative interval (P value = 0.38). The number of weeks before a pain score of less than 1 was recorded was not significantly different between the 2 groups (P value = 0.95) |
| Garry 2004 | Daily diary using a visual analogue scale, scored on day 0 (operation day), and days 2, 7 and 21. Analysis of covariance used to adjust pain scores over days 0 to 6 by the number of days that opiates were used | VH: n = 168 | AH: n = 292 | A higher proportion of AH participants used opiates than aLH. AH is more painful than aLH and LH has a tendency to be less painful than vLH |
| Marana 1999 | 10‐point visual analogue scale. Evaluation of pain on postoperative days 1, 2 and 3 | n = 58 | n = 58 | Significant difference between 2 groups at 3 evaluations. Lower pain score following LAVH compared to AH |
| Muzii 2007 | VAS scores (no further description) Postoperative day 1 and 2 | n = 40 Day 1 median = 2.8 Range (0 to 6) Day 2 median = 0.8 Range (0 to 3.7) | n = 41 Day 1 median = 4.4 Range (2 to 6.2) Day 2 median = 2.9 Range (2 to 5.5) | Day 1 P value < 0.05 Day 2 P value < 0.05 |
| Olsson 1996 | Visual analogue scale (range 0 to 7), 2 days after surgery | n = 71 | n = 72 | Postoperative pain 2 days after surgery was significantly less following LAVH compared to AH |
| Perino 1999 | 10‐point visual analogue scale, 0 = no pain to 10 = maximum pain. Assessed pain for 3 days after surgery | n = 51 | n = 51 | Participants who underwent LH had less intense postoperative pain than those in the AH group |
| Schutz 2002 | 10‐point visual analogue scale on days 1, 3 and 5. Pain index on 4th postoperative day (WHO scale) | n = 28 | n = 20 | Pain index was 0 on postoperative day 4 in the LH group and 5 in the AH group, LH was significantly less painful than AH |
| Postoperative analgesics | ||||
| Falcone 1999 | Length of time PCA pump was required (hours) and number of narcotic (oxycodone) or acetaminophen pills used in the hospital and after discharge was recorded | n = 23 | n = 21 | Participants in the LH group required less PCA time |
| Ferrari 2000 | Analgesic requirement recorded daily for 3 groups (number who require analgesia for more than 24 hours after surgery): | Group 1: n = 31 | Group 1: n = 31. Median = 24, n% = 77, P value < 0.001. | LAVH was associated with a significantly lower administration of analgesics after the first 24 postoperative hours. Group 2, uteri weighing less than 500 g, LAVH was associated with less analgesic administration |
| Kluivers 2007 | Number of participants receiving opioids during the first 3 days after surgery were recorded | n = 27 | n = 32 | Less women in LH versus AH group required opioids (P value < 0.01) |
| Langebrekke 1996 | Number of participants receiving analgesics (parenterally, oral and rectal analgesics) during the hospital stay and 5 days postoperatively | n = 46 | n = 54 | The need for both kinds of analgesics was reduced in the LH group |
| Raju 1994 | Duration of postoperative analgesia (days) | n = 40 | n = 40 | Participants in the LAVH group required fewer days of analgesia than participants in the AH group |
| Summitt 1998 | Use of intramuscular narcotics and oral pain medication | n = 34 | n = 31 | A statistically greater number of patients in the AH group required IM narcotics on the day of surgery compared to those in the LH group |
| Recovery from pain (days) | ||||
| Raju 1994 | Number of days until participants are free from pain | n = 40 | n = 40 | Participants who had LAVH recovered from pain quicker than those who had AH |
Comparison 2 LH versus AH, Outcome 27 Pain relief (descriptive data).
| Study | Description | LH | AH | Comments |
| Ellstrom 1998 | Analysis of cost over a period of 12 weeks, starting on the day the participant entered the hospital. Direct costs (hospital costs) and indirect costs (loss of production value) were analysed separately. Units of currency = Swedish crowns (SEK) | n = 38 | n = 38 | The change in costs between LH and AH are negligible as approximately 50% of hospital costs are fixed costs |
| Falcone 1999 | Hospital costs (amount a provider must pay for goods and services) were assessed through the hospital accounting system. The direct and indirect costs were calculated for each patient from 3 different components: operating room costs, anaesthesia costs and ward costs | n = 24 | n = 24 | Total hospital costs were not significantly higher in the LH group than the AH group |
| Lumsden 2000 | Single set of unit costs applied to each unit of resource to provide a NHS cost for each woman. 1997/98 prices | n = 95 | n = 95 | AH had significantly lower total costs than LH, resulting principally from the difference in operation costs. When the cost of disposable equipment was removed, the difference was non‐significant |
| Raju 1994 | Cost analysis of each type of procedure on the major points of difference between either operation: cost of disposable consumables and the comparative costs of postoperative lengths of stay in hospital | n = 40 | n = 40 | — |
| Summitt 1998 | Hospital charges for both groups | n = 34 | n = 31 | Lack of a statistical difference in total hospital charges |
Comparison 2 LH versus AH, Outcome 28 Cost (descriptive data).

Comparison 3 LH versus VH, Outcome 1 Return to normal activities (days).
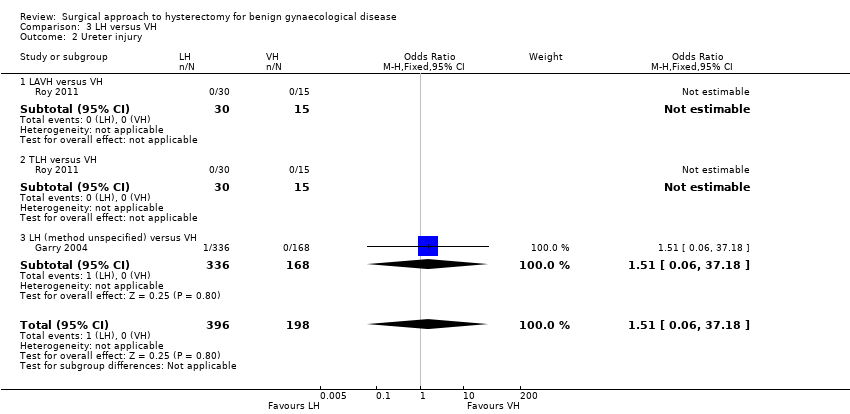
Comparison 3 LH versus VH, Outcome 2 Ureter injury.

Comparison 3 LH versus VH, Outcome 3 Bladder injury.

Comparison 3 LH versus VH, Outcome 4 Urinary tract (bladder or ureter) injury.
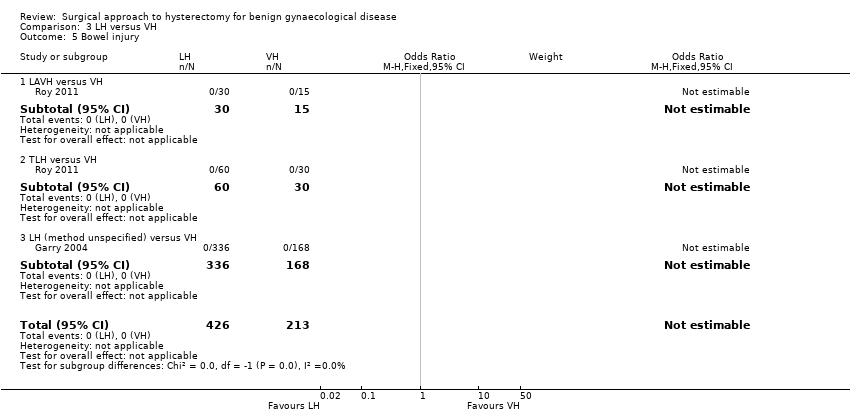
Comparison 3 LH versus VH, Outcome 5 Bowel injury.
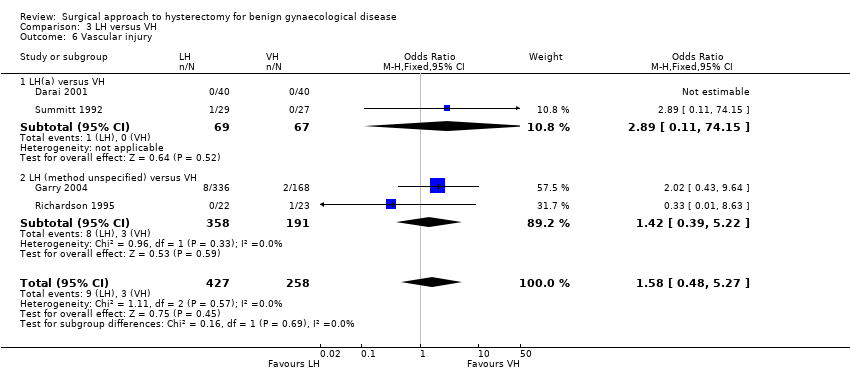
Comparison 3 LH versus VH, Outcome 6 Vascular injury.

Comparison 3 LH versus VH, Outcome 7 Fistula.

Comparison 3 LH versus VH, Outcome 8 Urinary dysfunction.

Comparison 3 LH versus VH, Outcome 9 Operation time (mins).
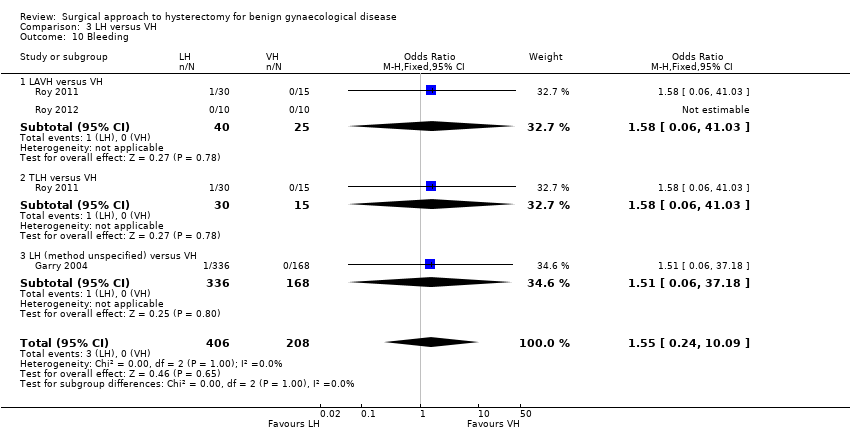
Comparison 3 LH versus VH, Outcome 10 Bleeding.

Comparison 3 LH versus VH, Outcome 11 Transfusion.

Comparison 3 LH versus VH, Outcome 12 Pelvic haematoma.
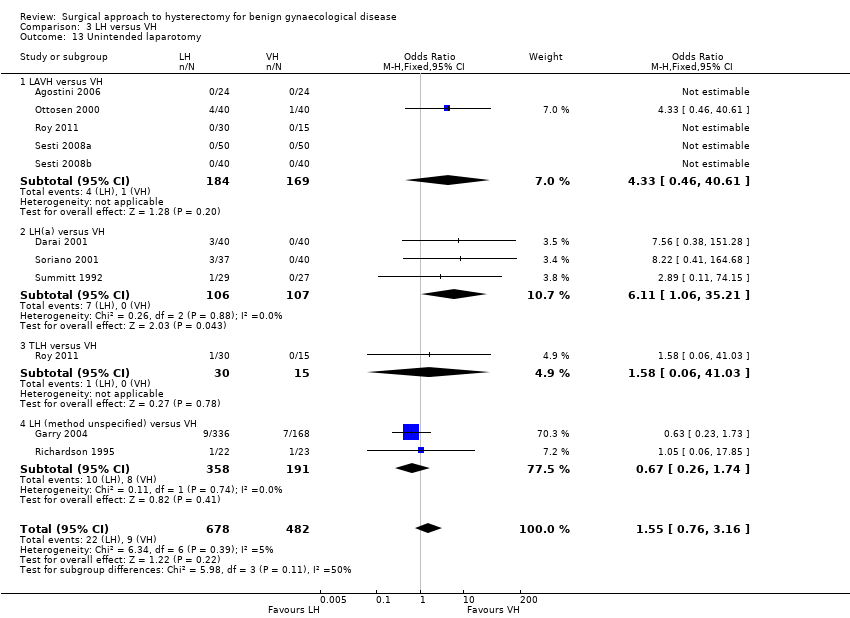
Comparison 3 LH versus VH, Outcome 13 Unintended laparotomy.
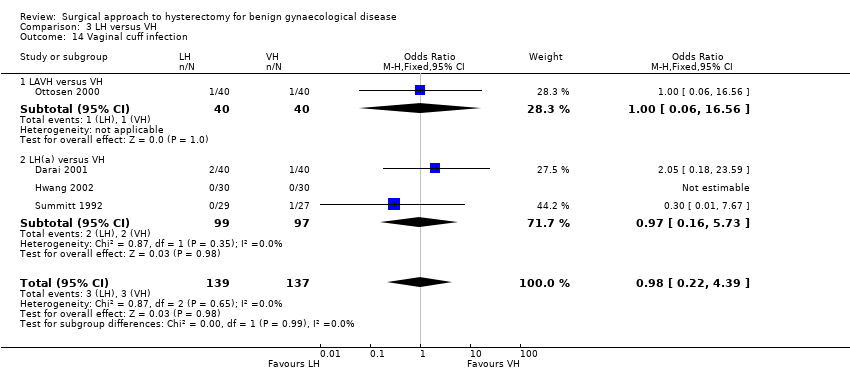
Comparison 3 LH versus VH, Outcome 14 Vaginal cuff infection.

Comparison 3 LH versus VH, Outcome 15 Wound/abdominal wall infection.

Comparison 3 LH versus VH, Outcome 16 Urinary tract infection.
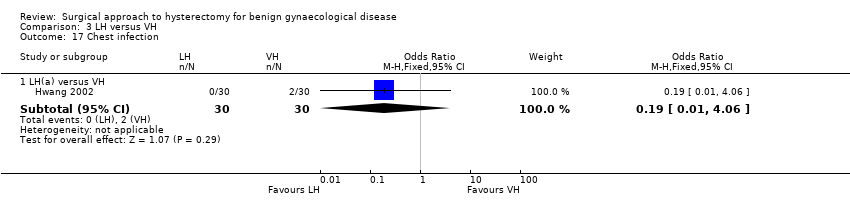
Comparison 3 LH versus VH, Outcome 17 Chest infection.
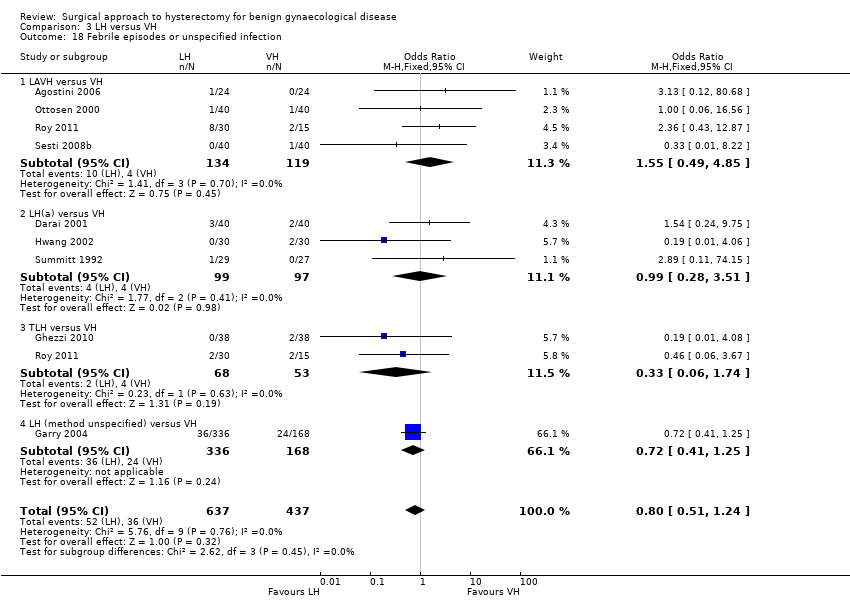
Comparison 3 LH versus VH, Outcome 18 Febrile episodes or unspecified infection.
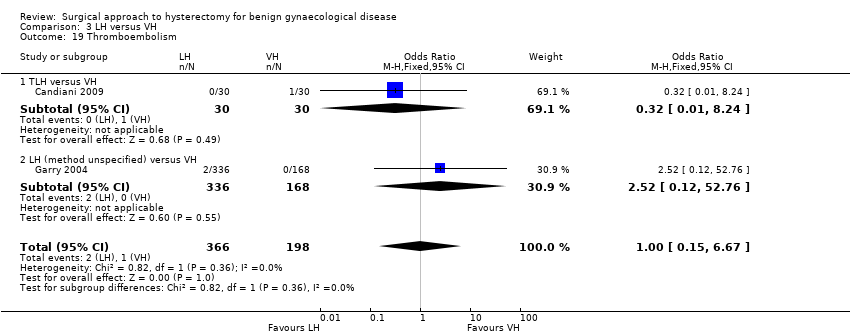
Comparison 3 LH versus VH, Outcome 19 Thromboembolism.

Comparison 3 LH versus VH, Outcome 20 Length of hospital stay (days).
| Study | LH | VH | Comments |
| Richardson 1995 | n = 22 | n = 23 | |
| Roy 2011 | TLH: n = 30 median = 15 days min‐max = 7 to 30 days LAVH: n = 30 median = 20 days min‐max = 8 to 40 days | n = 30 median = 14 days min‐max = 7 to 25 days | P value = 0.7 |
| Roy 2012 | n = 10 median = 20 days min‐max = 10 to 30 days | n = 10 median = 16 days min‐max = 12 to 24 days | P value = 0.05 |
Comparison 3 LH versus VH, Outcome 21 Return to normal activities (descriptive data).
| Study | Description | LH | VH | Comment |
| Roy 2011 | Patient satisfaction was evaluated using HRQOL (Health Related Quality Of Life) questionnaire and SF‐12 (12‐item Short Form health survey) and follow‐up visits in outpatient clinic were done at 1, 3 and 6 months | TLH: n = 30 LAVH: n = 30 | n = 30 | After 6 months of surgery, there was significant higher satisfaction rate among patients who underwent TLH and NDVH (non‐descent vaginal hysterectomy) than those who underwent LAVH (P value = 0.003). The satisfaction was similar between the TLH and NDVH group |
Comparison 3 LH versus VH, Outcome 22 Long‐term outcomes: quality of life (descriptive data).
| Study | LH | VH | Comments |
| Hwang 2002 | With 2nd proc: | With 2nd proc: | Kruskal Wallis test: |
| Ribeiro 2003 | n = 20 | n = 20 | — |
| Richardson 1995 | n = 22 | n = 23 | Some of these cases include oophorectomies. Oophorectomy (mean): LH 129.7 mins, VH 95.3 mins; no oophorectomy (mean): LH 132.7 mins, VH 64.7 mins |
| Roy 2012 | n = 10 median = 90 mins min‐max = 60 to 165 mins | n = 10 median = 75 min‐max = 40 to 105 | Not statistically significant |
Comparison 3 LH versus VH, Outcome 23 Operation time (descriptive data).
| Study | LH | VH | Comments |
| Hwang 2002 | n = 30 | n = 30 | Not tested separately |
| Richardson 1995 | n = 22 | n = 23 | — |
| Roy 2011 | TLH: n = 30 median = 2 days min‐max = 2 to 12 days LAVH: n = 30 median = 3 days min‐max = 4 days | VH: n = 30 median = 2 days min‐max = 1 to 4 days | P value = 0.15 |
| Roy 2012 | n = 10 median = 3 days min‐max = 2 to 4 days | n = 10 median = 2 days min‐max = 2 to 4 days | Not statistically significant |
Comparison 3 LH versus VH, Outcome 24 Length of hospital stay (descriptive data).
| Study | Description | LH | VH | Conclusion |
| Pain scales | ||||
| Ghezzi 2010 | VAS pain scores at several times post surgery | n = 41 VAS score after 1 h: mean = 4.7, SD = 2.6 VAS score after 3 h: mean = 3.2, SD = 2.5 VAS score after 8 h: mean = 2.1, SD = 2.2 VAS score after 24 h: mean = 1.8, SD = 1.7 | n = 41 VAS score after 1 h: mean = 7.8, SD = 1.7 VAS score after 3 h: mean = 6.6, SD = 2.0 VAS score after 8 h: mean = 5.3, SD = 2.1 VAS score after 24 h: mean = 3.6, SD = 2.6 | P value < 0.0001 P value < 0.0001 P value < 0.0001 P value = 0.001 |
| Sesti 2008b | VAS pain 24 hours post surgery | 6 patients (15%) reported absence of pain 24 hours post surgery | 20 patients (50%) reported absence of pain (VAS = 0) 24 hours post surgery | Patients undergoing LAVH had more postoperative pain compared with patients undergoing VH |
| Postoperative analgesics | ||||
| Ghezzi 2010 | The need for additional use of analgesics after the operation | n = 41 7 (17.1%) | n = 41 32 (78.0%) | P value < 0.0001 |
| Richardson 1995 | The number of postoperative opoid injections and the number of days analgesia was required was recorded | n = 22 | n = 23 | The number of opoid injections and analgesia requirements were similar in each group |
| Soriano 2001 | Total consumption of paracetamol, NSAID and subcutaneous opoid | n = 37 | n = 40 | No significant difference in the total consumption of paracetamol, NSAID and subcutaneous opoid between the 2 groups |
| Summitt 1992 | Pain control was assessed by documenting the intramuscular narcotic use on the day of surgery and the number of pain tablets used on the day of surgery and the first 2 postoperative days | n = 28 | n = 27 | — |
Comparison 3 LH versus VH, Outcome 25 Pain relief (descriptive data).
| Study | Description | LH | VH |
| Summitt 1992 | Mean total hospital charge when surgery was performed on an outpatient basis. Charges consisted of: operating room fee, operating room time, anaesthesia time, charges for disposable staples, scissors, graspers and a charge for recovery in the ambulatory surgery unit, including laboratory fees | n = 29 | n = 27 |
Comparison 3 LH versus VH, Outcome 26 Cost (descriptive data).

Comparison 4 RH versus LH, Outcome 1 Return to normal activities (days).

Comparison 4 RH versus LH, Outcome 2 Intraoperative visceral injury (dichotomous).

Comparison 4 RH versus LH, Outcome 3 Operation time.

Comparison 4 RH versus LH, Outcome 4 Transfusion.
| Study | Description | RH | LH | Comment |
| Paraiso 2013 | Percentage to return to normal baseline activities at 1, 2, 3, 4, 5 and 6 weeks postoperatively | 1 week (n = 17): 22% 2 weeks (n = 17): 46% 3 weeks (n = 17): 54% 4 weeks (n = 17): 60% 5 weeks (n = 17): 66% 6 weeks (n = 16): 72% | 1 week (n = 19): 29% 2 weeks (n = 19): 46% 3 weeks (n = 18): 58% 4 weeks (n = 18): 64% 5 weeks (n = 17): 73% 6 weeks (n = 17): 82% | P value (overall) = 0.25 |
Comparison 4 RH versus LH, Outcome 5 Return to normal activities (descriptive data).
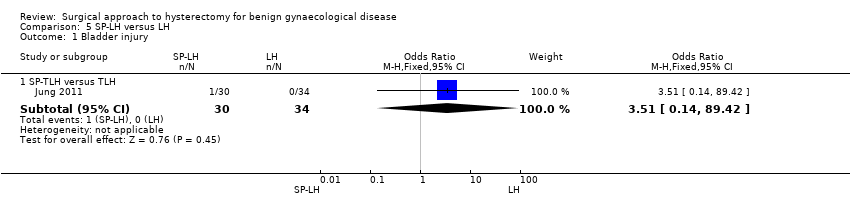
Comparison 5 SP‐LH versus LH, Outcome 1 Bladder injury.

Comparison 5 SP‐LH versus LH, Outcome 2 Operation time (mins).
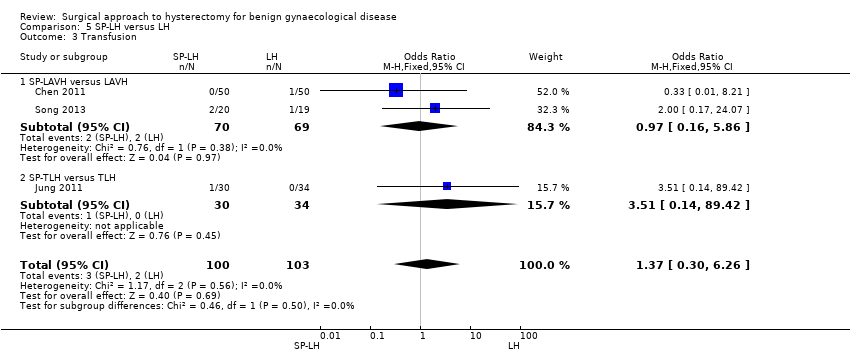
Comparison 5 SP‐LH versus LH, Outcome 3 Transfusion.

Comparison 5 SP‐LH versus LH, Outcome 4 Pelvic haematoma.

Comparison 5 SP‐LH versus LH, Outcome 5 Wound/abdominal wall infection.
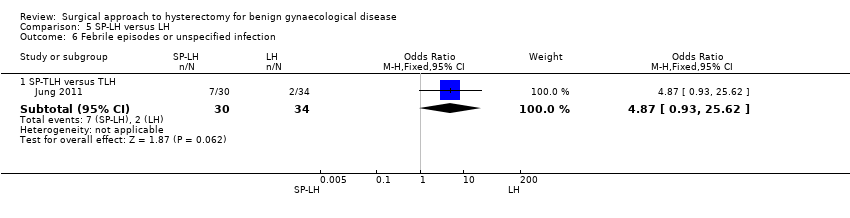
Comparison 5 SP‐LH versus LH, Outcome 6 Febrile episodes or unspecified infection.

Comparison 5 SP‐LH versus LH, Outcome 7 Postoperative ileus.
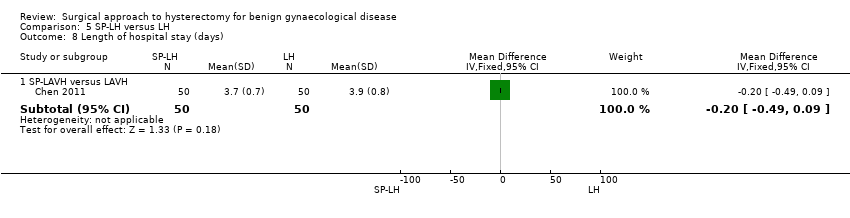
Comparison 5 SP‐LH versus LH, Outcome 8 Length of hospital stay (days).
| Study | SP‐LH | Conventional LH | Comments |
| Song 2013 | n = 20 SP‐LAVH Mean = 92 min Range 57 to 220 min | n = 19 LAVH Mean = 95 min Range 70 to 154 min | P value = 0.47 |
Comparison 5 SP‐LH versus LH, Outcome 9 Operation time (descriptive data).
| Study | SP‐LH | LAVH | Comments |
| Jung 2011 | n = 30 SP‐TLH Median postoperative hospital stay = 3.4 days Range 3.0 to 4.3 days | n = 34 TLH Median postoperative hospital stay = 3.0 days Range 3.0 to 3.0 days | P value = 0.075 |
| Song 2013 | n = 20 SP‐LAVH Mean = 3 days Range 2 to 4 days | n = 19 LAVH Mean = 3 days Range 2 to 4 days | P value = 0.95 |
Comparison 5 SP‐LH versus LH, Outcome 10 Length of hospital stay (descriptive data).
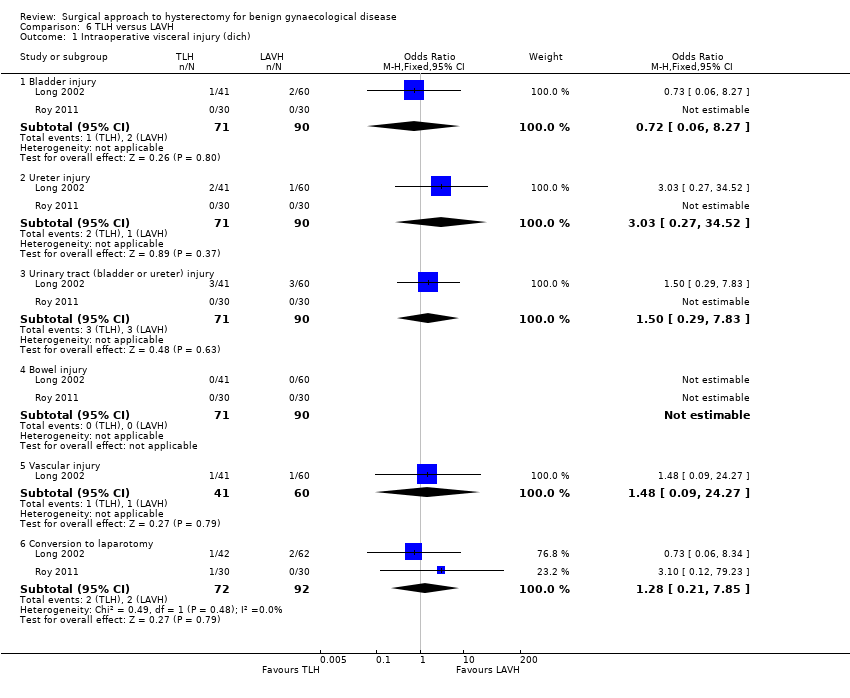
Comparison 6 TLH versus LAVH, Outcome 1 Intraoperative visceral injury (dich).
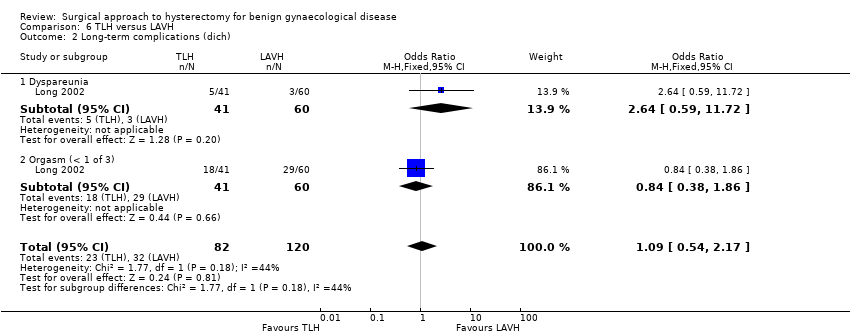
Comparison 6 TLH versus LAVH, Outcome 2 Long‐term complications (dich).
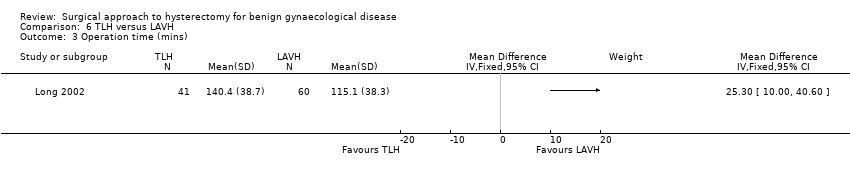
Comparison 6 TLH versus LAVH, Outcome 3 Operation time (mins).
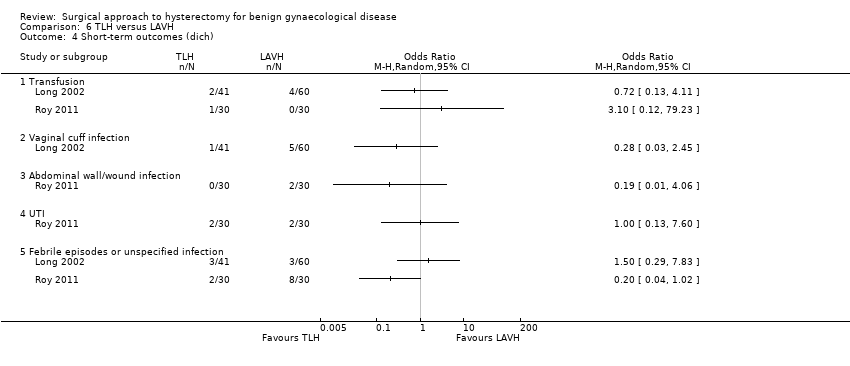
Comparison 6 TLH versus LAVH, Outcome 4 Short‐term outcomes (dich).
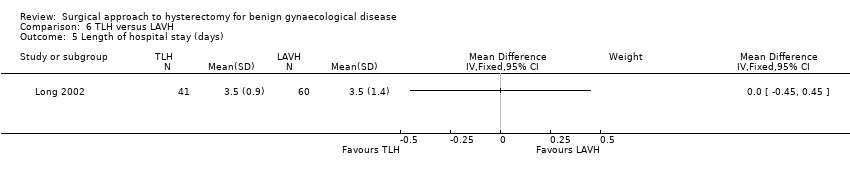
Comparison 6 TLH versus LAVH, Outcome 5 Length of hospital stay (days).
| Study | Mini‐TLH | Conventional TLH | Comments |
| Ghezzi 2011 | n = 38 Median = 58 mins Range: 30 to 135 mins | n = 38 Median = 60 mins Range: 30 to 155 mins | P value = 0.55 |
Comparison 7 Mini‐LH versus TLH, Outcome 1 Operation time (descriptive data).
| Study | mini‐TLH | Conventional TLH | Comment |
| Ghezzi 2011 | n = 38 Median = 1 day Range: 0 to 2 | n = 38 Median = 1 day Range: 1 to 2 | P value = 0.73 |
Comparison 7 Mini‐LH versus TLH, Outcome 2 Length of hospital stay (descriptive data).
| Vaginal hysterectomy versus abdominal hysterectomy for benign gynaecological disease | ||||||
| Patient or population: patients with benign gynaecological disease | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Abdominal hysterectomy | Vaginal hysterectomy | |||||
| Return to normal activities (days) | The mean return to normal activities (days) in the AH group was | The mean return to normal activities (days) in the VH group was | — | 176 | ⊕⊕⊕⊝ | — |
| Urinary tract (bladder or ureter) injury | 0 per 1000 | 0 per 1000 | OR 3.09 | 439 | ⊕⊕⊕⊝ | There were no urinary tract injuries in one study |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1There was a large difference in return to normal activities between the different studies; the analysis had high heterogeneity (I2 = 75%) but consistent direction of effect. | ||||||
| Laparoscopic hysterectomy versus abdominal hysterectomy for benign gynaecological disease | ||||||
| Patient or population: patients with benign gynaecological disease | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Abdominal hysterectomy | Laparoscopic hysterectomy | |||||
| Return to normal activities (days) | The mean return to normal activities (days) in the AH group was | The mean return to normal activities (days) in the LH group was | — | 520 | ⊕⊕⊝⊝ | — |
| Urinary tract (bladder or ureter) injury | 10 per 1000 | 24 per 1000 | OR 2.44 | 2140 | ⊕⊕⊝⊝ | — |
| Bowel injury | 7 per 1000 | 1 per 1000 | OR 0.21 | 1175 | ⊕⊕⊕⊝ | — |
| Vascular injury | 9 per 1000 | 16 per 1000 | OR 1.76 | 956 | ⊕⊕⊕⊝ | — |
| Bleeding | 16 per 1000 | 6 per 1000 | OR 0.45 | 1266 | ⊕⊕⊝⊝ | — |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1In some studies there was doubt about the method used for random sequence generation or allocation of patients. Furthermore, one study did not perform an intention‐to‐treat analysis. | ||||||
| Laparoscopic hysterectomy versus vaginal hysterectomy for benign gynaecological disease | ||||||
| Patient or population: patients with benign gynaecological disease | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Vaginal hysterectomy | Laparoscopic hysterectomy | |||||
| Return to normal activities (days) | The mean return to normal activities (days) in the VH group was | The mean return to normal activities (days) in the LH group was | — | 140 | ⊕⊕⊕⊝ | — |
| Urinary tract (bladder or ureter) injury | 16 per 1000 | 16 per 1000 | OR 1.0 | 865 | ⊕⊕⊝⊝ | — |
| Vascular injury | 12 per 1000 | 18 per 1000 | OR 1.58 | 745 | ⊕⊕⊝⊝ | — |
| Bleeding | 29 per 1000 | 25 per 1000 | OR 2.45 | 644 | ⊕⊕⊝⊝ | — |
| Unintended laparotomy | 24 per 1000 | 37 per 1000 | OR 1.55 | 1160 | ⊕⊕⊝⊝ | — |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Wide confidence intervals crossing the line of no effect. | ||||||
| Type of LH | LH versus AH RCTs | LH versus VH RCTs | LH versus LH RCTs |
| LAVH | Ferrari 2000 | Agostini 2006 | Chen 2011 |
| Kunz 1996 | Ottosen 2000 | Roy 2011 | |
| Marana 1999 | Roy 2011 | Song 2013 | |
| Muzii 2007 | Roy 2012 | ||
| Ottosen 2000 | Sesti 2008(a) | ||
| Raju 1994b | Sesti 2008(b) | ||
| Sesti 2008(a) | |||
| Tsai 2003 | |||
| LH(a) | Ellstrom 1998 | Darai 2001 | |
| Falcone 1999 | Hwang 2002 | ||
| Harkki‐Siren 2000 | Soriano 2001 | ||
| Hwang 2002 | Summitt 1992 | ||
| Langebrekke 1998 | Zhu 2009 | ||
| Olsson 1996 | |||
| Persson 2006 | |||
| Schutz 2002 | |||
| Seracchioli 2002 | |||
| Summitt 1998 | |||
| Yuen 1998 | |||
| Zhu 2009 | |||
| TLH | Kluivers 2007 | Candiani 2009 | Ghezzi 2011 |
| Perino 1999 | Ghezzi 2010 | Jung 2011 | |
| Ribeiro 2003 | Morelli 2007 | Paraiso 2013 | |
| Ribeiro 2003 | Roy 2011 | ||
| Roy 2011 | Sarlos 2012 | ||
| Non‐categorisable LH | Garry 2004 | Garry 2004 | |
| Kongwattanakul 2012 | Richardson 1998 | ||
| Lumsden 2000 | |||
| AH: abdominal hysterectomy | |||
| Stage | Laparoscopic content |
| 0 | Laparoscopy done but no laparoscopic procedure before vaginal hysterectomy |
| 1 | Procedure includes laparoscopic adhesiolysis and/or excision of endometriosis |
| 2 | Either or both adnexa freed laparoscopically |
| 3 | Bladder dissected from the uterus laparoscopically |
| 4 | Uterine artery transected laparoscopically |
| 5 | Anterior and/or posterior colpotomy or entire uterus freed laparoscopically |
| Step | Laparoscopic content |
| 1 | Severing the round ligaments and dissection of the upper portion of the broad ligament |
| 2 | Severing the tubo‐uterine junction and the utero‐ovarian ligament if the adnexa are to be preserved, or severing the infundibulopelvic ligaments |
| 3 | Severing the uterine vessels |
| 4 | Preparation of the bladder flap |
| 5 | Severing the cardinal uterosacral ligaments complex |
| 6 | Performing anterior and posterior culdotomy and separation of the cervix |
| 7 | Closure of the vaginal cuff |
| Trial | No. dropouts | Details |
| Chen 2011 | 2 | Excluded from analysis postoperatively, because they underwent accessory adnexal surgery |
| Falcone 1999 | 4 (1 LH; 3 AH) | Withdrew pre‐operatively |
| Garry 2004 | 34 (23 LH (11 aLH; 12 vLH); 6 AH; 5 VH) | Withdrew pre‐operatively |
| Long 2002 | 13 | 3 laparotomy conversions were excluded from analysis; 7 incomplete records; 3 combined procedures that were excluded post‐randomisation |
| Lumsden 2000 | 10 | 10 dropouts were not analysed. 7 women did not attend surgery and 3 records were not available |
| Kluivers 2007 | 1 | Refused assignment procedure |
| Lumsden 2000 | 10 | 7 withdrew pre‐operatively; 3 case records not available |
| Paraiso 2013 | 6 | 6 withdrew after randomisation but before the intervention was performed |
| Persson 2006 | 6 | 5 allocated to AH and 1 to LH withdrew after informed consent prior to the operation or withdrew in the postoperative period before the 5‐week follow‐up |
| Roy 2011 | 9 | 5 excluded because they needed adenectomy during surgery and 4 excluded from all analyses because they did not show up for follow‐up after intervention |
| Roy 2012 | 1 | 1 LH patient excluded from analysis due to conversion |
| Sarlos 2012 | 5 | After randomisation 5 did not complete the study and were excluded from the analysis |
| Song 2013 | 1 | 1 lost to follow‐up because of dissatisfaction with hospital care |
| Summitt 1998 | 2 | Refused assignment procedure |
| Yuen 1998 | 6 | 4 declined operation; 2 refused to participate postoperatively |
| AH: abdominal hysterectomy | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Return to normal activities (days) Show forest plot | 3 | 176 | Mean Difference (IV, Random, 95% CI) | ‐12.33 [‐19.89, ‐4.77] |
| 2 Long‐term outcomes: satisfaction (dichotomous) Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3 Intraoperative visceral injury (dichotomous) Show forest plot | 4 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Bladder injury | 4 | 439 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.09 [0.48, 19.97] |
| 3.2 Ureter injury | 1 | 119 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.3 Urinary tract (bladder or ureter) injury | 4 | 439 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.09 [0.48, 19.97] |
| 3.4 Bowel injury | 2 | 319 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.5 Vascular injury | 1 | 119 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Long‐term complications (dichotomous) Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Urinary dysfunction | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Operation time (mins) Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 VH versus standard AH | 3 | 259 | Mean Difference (IV, Random, 95% CI) | ‐11.01 [‐35.09, 13.08] |
| 5.2 VH versus minilaparotomy AH | 1 | 100 | Mean Difference (IV, Random, 95% CI) | ‐63.0 [‐65.11, ‐60.89] |
| 6 Short‐term outcomes (dichotomous) Show forest plot | 6 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Transfusion | 5 | 495 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.34, 1.96] |
| 6.2 Pelvic haematoma | 5 | 535 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.34, 2.89] |
| 6.3 Vaginal cuff infection | 2 | 140 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.08 [0.12, 77.80] |
| 6.4 Wound/abdominal wall infection | 3 | 355 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.04, 1.00] |
| 6.5 UTI | 3 | 176 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.08, 4.61] |
| 6.6 Chest infection | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.13, 7.60] |
| 6.7 Febrile episodes or unspecified infection | 5 | 495 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.36, 1.08] |
| 6.8 Thromboembolism | 1 | 119 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Length of hospital stay (days) Show forest plot | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 VH versus standard AH | 4 | 295 | Mean Difference (IV, Fixed, 95% CI) | ‐1.07 [‐1.22, ‐0.92] |
| 7.2 VH versus minilaparotomy AH | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | ‐2.1 [‐2.19, ‐2.01] |
| 8 All outcomes, descriptive data Show forest plot | Other data | No numeric data | ||
| 8.1 Quality of life (descriptive data) | Other data | No numeric data | ||
| 8.2 Operation time (descriptive data) | Other data | No numeric data | ||
| 8.3 Length of hospital stay (descriptive data) | Other data | No numeric data | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Return to normal activities (days) Show forest plot | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 LAVH versus AH | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐8.40 [‐12.15, ‐4.65] |
| 1.2 LH(a) versus AH | 5 | 440 | Mean Difference (IV, Fixed, 95% CI) | ‐15.17 [‐17.21, ‐13.14] |
| 2 Satisfaction Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 LH (method unspecified) versus AH | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Bladder injury Show forest plot | 12 | 2038 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.89 [0.91, 3.90] |
| 3.1 LAVH versus AH | 3 | 396 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.14, 7.17] |
| 3.2 LH(a) versus AH | 4 | 427 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.02 [0.49, 8.24] |
| 3.3 TLH versus AH | 2 | 99 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.05, 6.73] |
| 3.4 LH (method unspecified) versus AH | 3 | 1116 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.65 [0.88, 7.93] |
| 4 Ureter injury Show forest plot | 7 | 1417 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.46 [0.94, 12.71] |
| 4.1 LH(a) versus AH | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 6.12 [0.29, 130.87] |
| 4.2 TLH versus AH | 3 | 201 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.35 [0.34, 32.97] |
| 4.3 LH (method unspecified) versus AH | 3 | 1116 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.82 [0.44, 18.03] |
| 5 Urinary tract (bladder or ureter) injury Show forest plot | 13 | 2140 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.44 [1.24, 4.80] |
| 5.1 LAVH versus AH | 3 | 396 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.14, 7.17] |
| 5.2 LH(a) versus AH | 4 | 427 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.79 [0.73, 10.68] |
| 5.3 TLH versus AH | 3 | 201 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.61 [0.30, 8.63] |
| 5.4 LH (method unspecified) versus AH | 3 | 1116 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.13 [1.12, 8.78] |
| 6 Bowel injury Show forest plot | 4 | 1175 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.03, 1.33] |
| 6.1 LAVH versus AH | 1 | 50 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.25] |
| 6.2 TLH versus AH | 1 | 59 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 LH (method unspecified) versus AH | 2 | 1066 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.02, 1.60] |
| 7 Vascular injury Show forest plot | 2 | 956 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.76 [0.52, 5.87] |
| 7.1 LAVH versus AH | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 5.26 [0.24, 113.11] |
| 7.2 LH (method unspecified) versus AH | 1 | 876 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.34 [0.35, 5.08] |
| 8 Fistula Show forest plot | 2 | 245 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.07 [0.32, 29.96] |
| 8.1 LH(a) versus AH | 1 | 143 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.09 [0.12, 77.01] |
| 8.2 TLH versus AH | 1 | 102 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.06 [0.12, 76.88] |
| 9 Urinary dysfunction Show forest plot | 2 | 246 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.48, 1.84] |
| 9.1 LAVH versus AH | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.08 [0.12, 77.80] |
| 9.2 LH (method unspecified) versus AH | 1 | 166 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.44, 1.76] |
| 10 Operation time (mins) Show forest plot | 12 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 10.1 LAVH versus AH | 4 | 466 | Mean Difference (IV, Random, 95% CI) | 0.27 [‐23.39, 23.93] |
| 10.2 LH(A) versus AH | 5 | 420 | Mean Difference (IV, Random, 95% CI) | 33.45 [14.82, 52.08] |
| 10.3 TLH versus AH | 2 | 161 | Mean Difference (IV, Random, 95% CI) | 28.74 [2.64, 54.85] |
| 10.4 LAVH versus minilaparotomy AH | 1 | 100 | Mean Difference (IV, Random, 95% CI) | ‐8.0 [‐10.56, ‐5.44] |
| 11 Bleeding Show forest plot | 5 | 1266 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.15, 1.37] |
| 11.1 LAVH versus AH | 2 | 197 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.08, 4.64] |
| 11.2 LH(a) versus AH | 2 | 193 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.02, 1.34] |
| 11.3 LH (method unspecified) versus AH | 1 | 876 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.50 [0.16, 14.51] |
| 12 Transfusion Show forest plot | 19 | 2638 | Odds Ratio (M‐H, Random, 95% CI) | 0.58 [0.30, 1.10] |
| 12.1 LAVH versus AH | 5 | 539 | Odds Ratio (M‐H, Random, 95% CI) | 0.38 [0.11, 1.34] |
| 12.2 LH(a) versus AH | 8 | 641 | Odds Ratio (M‐H, Random, 95% CI) | 0.47 [0.17, 1.35] |
| 12.3 TLH versus AH | 2 | 161 | Odds Ratio (M‐H, Random, 95% CI) | 0.27 [0.03, 2.47] |
| 12.4 LH (method unspecified) versus AH | 3 | 1116 | Odds Ratio (M‐H, Random, 95% CI) | 0.91 [0.08, 9.85] |
| 12.5 LAVH versus minilaparotomy AH | 2 | 181 | Odds Ratio (M‐H, Random, 95% CI) | 1.38 [0.09, 20.52] |
| 13 Pelvic haematoma Show forest plot | 8 | 782 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.38, 1.47] |
| 13.1 LAVH versus AH | 3 | 276 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.05, 2.10] |
| 13.2 LH(a) versus AH | 4 | 406 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.44, 1.97] |
| 13.3 LAVH versus minilaparotomy AH | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.21] |
| 14 Unintended laparotomy Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 LAVH versus minilaparotomy AH | 2 | 181 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.08, 2.82] |
| 15 Length of hospital stay (days) Show forest plot | 11 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 15.1 LAVH versus AH | 4 | 466 | Mean Difference (IV, Random, 95% CI) | ‐2.64 [‐4.16, ‐1.12] |
| 15.2 LH(a) versus AH | 4 | 380 | Mean Difference (IV, Random, 95% CI) | ‐1.82 [‐2.34, ‐1.31] |
| 15.3 TLH versus AH | 2 | 161 | Mean Difference (IV, Random, 95% CI) | ‐2.53 [‐5.08, 0.01] |
| 15.4 LAVH versus minilaparotomy AH | 1 | 100 | Mean Difference (IV, Random, 95% CI) | ‐1.1 [‐1.20, ‐1.00] |
| 16 Vaginal cuff infection Show forest plot | 9 | 852 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.43 [0.67, 3.04] |
| 16.1 LAVH versus AH | 3 | 396 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.17, 3.37] |
| 16.2 LH(a) versus AH | 6 | 456 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [0.73, 4.37] |
| 17 Wound/abdominal wall infection Show forest plot | 6 | 611 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.12, 0.71] |
| 17.1 LAVH versus AH | 1 | 81 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.01, 4.19] |
| 17.2 LH(a) versus AH | 4 | 259 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.12, 1.03] |
| 17.3 LH (method unspecified) versus AH | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.24 [0.03, 2.21] |
| 17.4 LAVH versus minilaparotomy AH | 1 | 81 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.01, 4.19] |
| 18 Urinary tract infection Show forest plot | 8 | 659 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.54, 2.00] |
| 18.1 LAVH versus AH | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.22] |
| 18.2 LH(a) versus AH | 5 | 339 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.55, 2.95] |
| 18.3 LH (method unspecified) versus AH | 2 | 240 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.26, 2.69] |
| 19 Chest infection Show forest plot | 3 | 294 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.07, 1.35] |
| 19.1 LH(a) versus AH | 2 | 104 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.10, 3.93] |
| 19.2 LH (method not specified) versus AH | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.01, 2.01] |
| 20 Febrile episodes or unspecified infection Show forest plot | 16 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 20.1 LAVH versus AH | 4 | 339 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.09, 0.73] |
| 20.2 LH(a) versus AH | 7 | 572 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.33, 0.90] |
| 20.3 TLH versus AH | 2 | 161 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.36 [0.11, 1.21] |
| 20.4 LH (method unspecified) versus AH | 3 | 1116 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.65, 1.37] |
| 20.5 LAVH versus minilaparotomy AH | 1 | 81 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.72] |
| 21 Thromboembolism Show forest plot | 3 | 1125 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.23, 3.39] |
| 21.1 TLH versus AH | 1 | 59 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.01, 9.76] |
| 21.2 LH (method unspecified) versus AH | 2 | 1066 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.24, 5.13] |
| 22 Wound dehiscence Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 22.1 LAVH versus minilaparotomy AH | 1 | 81 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.15 [0.12, 79.69] |
| 23 Return to normal activities (descriptive data) Show forest plot | Other data | No numeric data | ||
| 24 Long‐term outcomes: quality of life (descriptive data) Show forest plot | Other data | No numeric data | ||
| 25 Operation time (descriptive data) Show forest plot | Other data | No numeric data | ||
| 26 Length of hospital stay (descriptive data) Show forest plot | Other data | No numeric data | ||
| 27 Pain relief (descriptive data) Show forest plot | Other data | No numeric data | ||
| 27.1 Pain scales | Other data | No numeric data | ||
| 27.2 Postoperative analgesics | Other data | No numeric data | ||
| 27.3 Recovery from pain (days) | Other data | No numeric data | ||
| 28 Cost (descriptive data) Show forest plot | Other data | No numeric data | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Return to normal activities (days) Show forest plot | 2 | 140 | Mean Difference (IV, Fixed, 95% CI) | ‐1.07 [‐4.21, 2.06] |
| 1.1 LAVH versus VH | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐1.60 [‐5.11, 1.91] |
| 1.2 LH(a) versus VH | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐5.95, 7.95] |
| 2 Ureter injury Show forest plot | 2 | 594 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.51 [0.06, 37.18] |
| 2.1 LAVH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 TLH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 LH (method unspecified) versus VH | 1 | 504 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.51 [0.06, 37.18] |
| 3 Bladder injury Show forest plot | 7 | 895 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.32, 2.56] |
| 3.1 LAVH versus VH | 2 | 125 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.22] |
| 3.2 LH(a) versus VH | 2 | 136 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.98 [0.30, 29.43] |
| 3.3 TLH versus VH | 2 | 85 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.26] |
| 3.4 LH (method unspecified) versus VH | 2 | 549 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.18, 3.79] |
| 4 Urinary tract (bladder or ureter) injury Show forest plot | 7 | 895 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.36, 2.75] |
| 4.1 LAVH versus VH | 2 | 125 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.22] |
| 4.2 LH(a) versus VH | 2 | 136 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.98 [0.30, 29.43] |
| 4.3 TLH versus VH | 2 | 85 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.26] |
| 4.4 LH (method unspecified) versus VH | 2 | 549 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.23, 4.38] |
| 5 Bowel injury Show forest plot | 2 | 639 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 LAVH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 TLH versus VH | 1 | 90 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.3 LH (method unspecified) versus VH | 1 | 504 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Vascular injury Show forest plot | 4 | 685 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.58 [0.48, 5.27] |
| 6.1 LH(a) versus VH | 2 | 136 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.89 [0.11, 74.15] |
| 6.2 LH (method unspecified) versus VH | 2 | 549 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.42 [0.39, 5.22] |
| 7 Fistula Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 LH(a) versus VH | 1 | 56 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.01, 7.67] |
| 8 Urinary dysfunction Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 LAVH versus VH | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.08 [0.12, 77.80] |
| 9 Operation time (mins) Show forest plot | 9 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 LAVH versus VH | 5 | 377 | Mean Difference (IV, Random, 95% CI) | 33.60 [20.13, 47.07] |
| 9.2 LH(a) versus VH | 3 | 213 | Mean Difference (IV, Random, 95% CI) | 53.58 [43.67, 63.49] |
| 9.3 TLH versus VH | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 17.30 [3.34, 31.26] |
| 10 Bleeding Show forest plot | 3 | 614 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.24, 10.09] |
| 10.1 LAVH versus VH | 2 | 65 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.58 [0.06, 41.03] |
| 10.2 TLH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.58 [0.06, 41.03] |
| 10.3 LH (method unspecified) versus VH | 1 | 504 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.51 [0.06, 37.18] |
| 11 Transfusion Show forest plot | 8 | 1039 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.60 [0.80, 3.18] |
| 11.1 LAVH versus VH | 4 | 273 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.16, 3.41] |
| 11.2 LH(a) versus VH | 3 | 217 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.49 [0.63, 9.86] |
| 11.3 TLH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.58 [0.06, 41.03] |
| 11.4 LH (method unspecified) versus VH | 1 | 504 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.74 [0.63, 4.79] |
| 12 Pelvic haematoma Show forest plot | 4 | 308 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.36, 4.03] |
| 12.1 LAVH versus VH | 3 | 228 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.70 [0.40, 7.26] |
| 12.2 LH(a) versus VH | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.04, 5.60] |
| 13 Unintended laparotomy Show forest plot | 10 | 1160 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.76, 3.16] |
| 13.1 LAVH versus VH | 5 | 353 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.33 [0.46, 40.61] |
| 13.2 LH(a) versus VH | 3 | 213 | Odds Ratio (M‐H, Fixed, 95% CI) | 6.11 [1.06, 35.21] |
| 13.3 TLH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.58 [0.06, 41.03] |
| 13.4 LH (method unspecified) versus VH | 2 | 549 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.26, 1.74] |
| 14 Vaginal cuff infection Show forest plot | 4 | 276 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.22, 4.39] |
| 14.1 LAVH versus VH | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.06, 16.56] |
| 14.2 LH(a) versus VH | 3 | 196 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.16, 5.73] |
| 15 Wound/abdominal wall infection Show forest plot | 2 | 170 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.88 [0.31, 27.06] |
| 15.1 LAVH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.72 [0.12, 60.29] |
| 15.2 LH(a) versus VH | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.08 [0.12, 77.80] |
| 15.3 TLH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Urinary tract infection Show forest plot | 3 | 230 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.66 [0.40, 6.82] |
| 16.1 LAVH versus VH | 2 | 125 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.15, 6.89] |
| 16.2 LH(a) versus VH | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.10 [0.12, 79.23] |
| 16.3 TLH versus VH | 1 | 45 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.72 [0.12, 60.29] |
| 17 Chest infection Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 17.1 LH(a) versus VH | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.01, 4.06] |
| 18 Febrile episodes or unspecified infection Show forest plot | 9 | 1074 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.51, 1.24] |
| 18.1 LAVH versus VH | 4 | 253 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.49, 4.85] |
| 18.2 LH(a) versus VH | 3 | 196 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.28, 3.51] |
| 18.3 TLH versus VH | 2 | 121 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.06, 1.74] |
| 18.4 LH (method unspecified) versus VH | 1 | 504 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.41, 1.25] |
| 19 Thromboembolism Show forest plot | 2 | 564 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.15, 6.67] |
| 19.1 TLH versus VH | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.24] |
| 19.2 LH (method unspecified) versus VH | 1 | 504 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.52 [0.12, 52.76] |
| 20 Length of hospital stay (days) Show forest plot | 7 | 525 | Mean Difference (IV, Random, 95% CI) | 0.88 [0.73, 1.03] |
| 20.1 LAVH versus VH | 4 | 308 | Mean Difference (IV, Random, 95% CI) | 0.91 [0.76, 1.06] |
| 20.2 LH(a) versus VH | 2 | 157 | Mean Difference (IV, Random, 95% CI) | 0.40 [‐0.42, 1.22] |
| 20.3 TLH versus VH | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐0.5 [‐2.41, 1.41] |
| 21 Return to normal activities (descriptive data) Show forest plot | Other data | No numeric data | ||
| 22 Long‐term outcomes: quality of life (descriptive data) Show forest plot | Other data | No numeric data | ||
| 23 Operation time (descriptive data) Show forest plot | Other data | No numeric data | ||
| 24 Length of hospital stay (descriptive data) Show forest plot | Other data | No numeric data | ||
| 25 Pain relief (descriptive data) Show forest plot | Other data | No numeric data | ||
| 25.1 Pain scales | Other data | No numeric data | ||
| 25.2 Postoperative analgesics | Other data | No numeric data | ||
| 26 Cost (descriptive data) Show forest plot | Other data | No numeric data | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Return to normal activities (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2 Intraoperative visceral injury (dichotomous) Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Ureter injury | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.21] |
| 2.2 Vascular injury | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.06, 16.44] |
| 2.3 Wound/abdominal wall infection | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.21] |
| 2.4 Wound dehiscence | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.21] |
| 3 Operation time Show forest plot | 2 | 152 | Mean Difference (IV, Random, 95% CI) | 44.09 [5.31, 82.88] |
| 4 Transfusion Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5 Return to normal activities (descriptive data) Show forest plot | Other data | No numeric data | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Bladder injury Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 SP‐TLH versus TLH | 1 | 64 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.51 [0.14, 89.42] |
| 2 Operation time (mins) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 SP‐LAVH versus LAVH | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 SP‐TLH versus TLH | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Transfusion Show forest plot | 3 | 203 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.30, 6.26] |
| 3.1 SP‐LAVH versus LAVH | 2 | 139 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.16, 5.86] |
| 3.2 SP‐TLH versus TLH | 1 | 64 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.51 [0.14, 89.42] |
| 4 Pelvic haematoma Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 SP‐LAVH versus LAVH | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.06 [0.12, 76.95] |
| 5 Wound/abdominal wall infection Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 SP‐LAVH versus LAVH | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.21] |
| 6 Febrile episodes or unspecified infection Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 SP‐TLH versus TLH | 1 | 64 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.87 [0.93, 25.62] |
| 7 Postoperative ileus Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 SP‐TLH versus TLH | 1 | 64 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.36 [0.20, 27.39] |
| 8 Length of hospital stay (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 SP‐LAVH versus LAVH | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.49, 0.09] |
| 9 Operation time (descriptive data) Show forest plot | Other data | No numeric data | ||
| 10 Length of hospital stay (descriptive data) Show forest plot | Other data | No numeric data | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intraoperative visceral injury (dich) Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Bladder injury | 2 | 161 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.06, 8.27] |
| 1.2 Ureter injury | 2 | 161 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.03 [0.27, 34.52] |
| 1.3 Urinary tract (bladder or ureter) injury | 2 | 161 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.29, 7.83] |
| 1.4 Bowel injury | 2 | 161 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.5 Vascular injury | 1 | 101 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.09, 24.27] |
| 1.6 Conversion to laparotomy | 2 | 164 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.21, 7.85] |
| 2 Long‐term complications (dich) Show forest plot | 1 | 202 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.54, 2.17] |
| 2.1 Dyspareunia | 1 | 101 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.64 [0.59, 11.72] |
| 2.2 Orgasm (< 1 of 3) | 1 | 101 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.38, 1.86] |
| 3 Operation time (mins) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4 Short‐term outcomes (dich) Show forest plot | 2 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Transfusion | 2 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Vaginal cuff infection | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Abdominal wall/wound infection | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 UTI | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.5 Febrile episodes or unspecified infection | 2 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Length of hospital stay (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Operation time (descriptive data) Show forest plot | Other data | No numeric data | ||
| 2 Length of hospital stay (descriptive data) Show forest plot | Other data | No numeric data | ||


