Intervenciones para la hipertensión intracraneal idiopática
References
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Jump to:
| Methods | Multicentre, open‐label, parallel‐group RCT. | |
| Participants | Participants had IIH that met Friedman's criteria (Friedman 2002). 50 participants from six UK centres. Two arms: 25 randomised to treatment with acetazolamide and 25 randomised to placebo. | |
| Interventions | Participants were randomised to either the acetazolamide group or the placebo group. All participants were encouraged to lose weight. | |
| Outcomes | Measured at baseline, 3, 6, 9 and 12 months. Primary outcomes were measured as an aggregate score (out of 15) on final visit (each outcome measure was ranked as being: absent (0); present, stable (1); deteriorating (2)):
Secondary outcomes (and methods):
Right and left eye data were reported separately. | |
| Notes | In addition, at 12 months, clinicians were asked to select the term that best described the participant from the following options:
Date study conducted:
Funding:
Conflict of interest:
Trial registration ID:
| |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants randomised by computer‐generated random list. No difference in baseline characteristics detected between arms. |
| Allocation concealment (selection bias) | Low risk | Neither participant or treating clinician was masked to allocation. Allocation was communicated to treating clinicians via telephone. |
| Blinding of participants and personnel (performance bias) | High risk | Neither participant or treating clinician was masked to allocation. Dosing schedules for acetazolamide decided by prescribing clinician. |
| Blinding of outcome assessment (detection bias) | High risk | No masking of assessor reported. |
| Incomplete outcome data (attrition bias) | High risk | Five participants from the placebo arm started on acetazolamide therapy. Two participants (one from each of the two arms) underwent surgical intervention. 12 participants from the acetazolamide arm discontinued treatment during the study period. |
| Selective reporting (reporting bias) | Low risk | Primary outcome data provided in full. Data not provided for anxiety, depression, patient reported health status assessment. |
| Methods | Multicentre, double‐masked, parallel‐group RCT | |
| Participants |
| |
| Interventions |
| |
| Outcomes | A study eye was decided: this was the eye with poorer visual acuity. Measurement of outcomes was performed at baseline, 1, 2, 3, 4, 5 and 6 months (apart from HIT‐6 and quality of life, which were only at six months). Primary outcomes (and methods):
Secondary outcomes (and methods):
| |
| Notes | Date study conducted:
Funding:
Conflict of interest:
Trial registration ID:
| |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation was performed per site, but the method has not been described. |
| Allocation concealment (selection bias) | Low risk | Both participants and clinicians were masked to allocation. |
| Blinding of participants and personnel (performance bias) | Low risk | Robust masking policy with the managing staff blinded to treatment status except for programmer who generated the randomization plan, a statistician and a member of staff involved with packaging the drugs. |
| Blinding of outcome assessment (detection bias) | Low risk | As above. |
| Incomplete outcome data (attrition bias) | High risk | 19% withdrawal rate. In the treatment group 16 patients withdrew for the following reasons: lost to follow‐up (6), withdrew consent (4), time commitment (3), desired active treatment (1), moved (1), and treatment failure later adjudicated to be performance failure (1). Sixteen patients in the placebo group were withdrawn for the following reasons: lost to follow‐up (9), time commitment (5), adverse event (1), needed disallowed medication (1). |
| Selective reporting (reporting bias) | Low risk | Data provided on all the secondary outcomes. |
Characteristics of excluded studies [ordered by study ID]
Jump to:
| Study | Reason for exclusion |
| Retrospective review of 25 patients treated with either lumboperitoneal shunt or ventriculoperitoneal shunt. | |
| Prospective study of 29 patients undergoing endovascular treatment of IIH. No control group. | |
| No control group. Retrospective study of 52 patients with IIH and venous sinus stenosis treated with transverse sinus stenting. | |
| Retrospective analysis of 86 adults with IIH who underwent transverse sinus stenting compared with 110 children treated with CSF shunting for hydrocephalus. | |
| No control group. Retrospective review of 19 patients who underwent venous sinus stenting. | |
| Retrospective review of 78 patients who underwent optic nerve fenestration and 20 control patients who did not. | |
| No control group. Retrospective review of 13 female patients who underwent venous sinus stenting. | |
| No control group. Retrospective study. 17 patients treated with ventriculo‐peritoneal shunting. | |
| No control group. Prospective study of four patients who underwent laparoscopic adjustable gastric banding. | |
| Case series of 33 patients undergoing either optic nerve sheath fenestration or cerebrospinal fluid diversion. No control group. | |
| No control group. Prospective following of seven patients and retrospective review of a different six patients. Total of 13 patients treated with CSF drainage at low pressure. | |
| No control group. Prospective study of 38 patients treated with venous sinus stenting. | |
| No control group. Late review of 14 patients (23 eyes) treated by optic nerve sheath fenestration. | |
| No control group. Retrospective review of 10 children treated with ventriculo‐peritoneal shunt (VPS) insertion using frameless stereotaxy. | |
| No control group. Retrospective study. 15 patients treated with acetazolamide and weight loss. | |
| No control group. Retrospective review and three‐year prospective follow‐up of 17 patients treated with custom‐designed electromagnetic image‐guided ventriculoperitoneal shunt placement. | |
| Technical validation of a novel 'bi‐corporal' pump to provide intermittent CSF drainage. | |
| No control group. Prospective trial of venous sinus stenting in IIH patients refractory to medical therapy. | |
| No control group. Single assignment trial of venous sinus stenting for refractory IIH. | |
| Retrospective review of the outcomes after three years in 39 cases of refenestration, 15 cases of acetazolamide and 14 cases of neurosurgical shunt insertion. | |
| No controls. Retrospective review of 21 patients treated with optic nerve sheath decompression. | |
| No control group. 4 patients treated with endoluminal stent insertion into transverse venous sinus. | |
| Retrospective review of 31 patients treated with CSF diversion surgery. | |
| Retrospective review of 32 patients. | |
| No control group. 8 patients (10 eyes) treated with optic nerve sheath fenestration. | |
| Prospective cohort study following 25 women adhering to a low energy diet. | |
| Prospective cohort study investigating outcomes before and after weight loss. No control group. | |
| No control group. 24 obese patients underwent surgery for weight loss. | |
| No control group, treatment not standardised, numbers small. 7 patients treated with external device to generate negative intra‐abdominal pressure. | |
| Single case report. | |
| Retrospective review of 34 patients who underwent CSF fluid diversion. | |
| Case series of 18 patients. No control group. | |
| Retrospective review of 22 patients. | |
| No placebo control group. No randomisation: 41 patients alternately allocated to treatment with acetazolamide or topiramate. |
Characteristics of ongoing studies [ordered by study ID]
Jump to:
| Trial name or title | Lowering Intracranial Pressure in Idiopathic Intracranial Hypertension: Assessing the Therapeutic Efficacy and Safety of an 11β‐hydroxysteroid Dehydrogenase Type 1 Inhibitor (AZD4017). Phase II Study. |
| Methods | Double‐blind, parallel assignment RCT |
| Participants |
|
| Interventions | AZD4017 (11b‐HSD1 inhibitor) 400 mg tablet twice daily for 12 weeks versus matched placebo tablet twice‐daily for 12 weeks |
| Outcomes | Primary outcome measures:
Secondary outcome measures:
Other outcome measures:
|
| Starting date | January 2014 |
| Contact information | Alexandra Sinclair; [email protected] |
| Notes | NCT02017444 |
| Trial name or title | A Randomised Controlled Trial of Bariatric Surgery Versus a Community Weight Loss Programme for the Sustained Treatment of Idiopathic Intracranial Hypertension: the IIH:WT Trial |
| Methods | Open‐label, parallel assignment RCT |
| Participants | Inclusion criteria:
|
| Interventions | Patients will be assigned to one of four arms:
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Other outcome measures:
|
| Starting date | March 2014 |
| Contact information | Alexandra Sinclair; [email protected] |
| Notes |
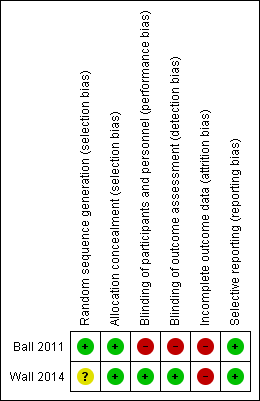
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
| Outcome | Acetalomazide | Placebo | MD (95% CI) adjusted for centre, baseline value of outcome and baseline papilloedema grade, with multiple imputation for missing data | ||||
| Mean | SD | N | Mean | SD | N | ||
| Wall 2014: Change in perimetric mean deviation (decibels) between baseline and 6 months | 1.43 | 2.23 | 86 | 0.71 | 2.49 | 69 | 0.71 (0 to 1.43) |
| Abbreviations: MD = mean difference; SD = standard deviation; CI = confidence interval. | |||||||
| Outcome | Acetalomazide | Placebo | MD (95% CI) | ||||
| Mean | SD | N | Mean | SD | N | ||
| Ball 2011: Change in logMAR acuity in the right eye between baseline and 12 months | Not reported | Not reported | 21 | Not reported | Not reported | 20 | 0.04 (‐0.08, 0.16) |
| Ball 2011: Change in logMAR acuity in the left eye between baseline and 12 months | Not reported | Not reported | 21 | Not reported | Not reported | 20 | 0.03 (‐0.09, 0.15) |
| Wall 2014a: Change in visual acuity (number of correct letters) between baseline and 6 months | 2.65 | Not reported (SE 0.49) | b | 2.64 | Not reported (SE 0.51) | b | 0.01 (‐1.45, 1.46) |
| aIn Wall 2014 MD adjusted for centre, baseline value of outcome and baseline papilloedema grade. | |||||||
| Outcome | Acetalomazide | Placebo | OR (95% CI) | ||
| n | N | n | N | ||
| Ball 2011: Visual loss (logMAR 0.2 or more) at 12 months | 0 | 21 | 2 | 20 | 0.17 (0.01, 3.82) |
| Abbreviations: MD = mean difference; SD = standard deviation; CI = confidence interval; n = number of events; N = number of participants; OR = odds ratio. | |||||
| Outcome | Acetalomazide | Placebo | MD (95% CI) adjusted for centre, baseline value of outcome and baseline papilloedema grade | ||||
| Mean | SD | N | Mean | SD | N | ||
| Wall 2014: Change in CSF pressure (mmH20) between baseline and 6 months | ‐112.3 | Not reported | 47 | ‐52.4 | Not reported | 38 | ‐59.9 (‐96.4 to ‐23.4) |
| Outcome | Acetalomazide | Placebo | MD (95% CI) adjusted for centre and baseline papilloedema grade | ||||
| Mean | SD | N | Mean | SD | N | ||
| Wall 2014: Change in papilloedema grade between baseline and 6 months, graded by fundus photographs | ‐1.31 | SE 0.11a | a | ‐0.61 | SE 0.11a | a | ‐0.70 (‐1.00 to ‐0.40) |
| Wall 2014: Change in papilloedema grade between baseline and 6 months, clinical grading | ‐1.75 | SE 0.13a | a | ‐0.85 | SE 0.14a | a | ‐0.91 (‐1.27 to ‐0.54) |
| aIt is unclear how many patients were included in these analyses. | |||||||
| Outcome | Acetalomazide | Placebo | MD (95% CI) adjusted for centre, baseline value of outcome and baseline papilloedema grade | ||||
| Mean | SD | N | Mean | SD | N | ||
| Ball 2011: Change in headache score as measured on a 10‐point visual analogue score at 12 months | Not reported | Not reported | 21 | Not reported | Not reported | 20 | 1.0 (‐1.80 to 3.70) |
| Wall 2014: Change in HIT‐6 total score between baseline and 6 months | ‐9.56 | Not reporteda | a | ‐9.11 | Not reporteda | a | ‐0.45 (‐3.50 to 2.60) |
| aIt is unclear how many patients were included in these analyses. | |||||||
| Outcome | Acetalomazide | Placebo | OR (95% CI) | ||
| n | N | n | N | ||
| Ball 2011: Number of people with headache at 12 months | 9 | 21 | 13 | 20 | 0.42 (0.12 to 1.41) |
| Abbreviations: CI = confidence interval; n = number of events; N = number of participants; OR = odds ratio. | |||||
| Outcome | Acetalomazide | Placebo | OR (95% CI) | ||
| n | N | n | N | ||
| Ball 2011: Number of people in remission at 12 months | 9 | 21 | 8 | 20 | 1.13 (0.32 to 3.90) |
| Abbreviations: CI = confidence interval; n = number of events; N = number of participants; OR = odds ratio. | |||||
| Outcome | Acetalomazide | Placebo | OR (95% CI) | ||
| n | N | n | N | ||
| Elevated ALT | 6 | 69 | 3 | 79 | 1.90 (0.46 to 7.87) |
| Decreased CO2 | 9 | 69 | 0 | 79 | 19.49 (1.12 to 340.66) |
| Diarrhea | 12 | 69 | 3 | 79 | 4.11 (1.11 to 15.15) |
| Dizziness | 8 | 69 | 3 | 79 | 2.60 (0.66 to 10.16) |
| Dysgeusia | 13 | 69 | 0 | 79 | 29.20 (1.71 to 500.07) |
| Dyspepsia | 7 | 69 | 1 | 79 | 6.91 (0.83 to 57.49) |
| Dyspnea | 7 | 69 | 2 | 79 | 3.41 (0.69 to 16.94) |
| Fatigue | 14 | 69 | 1 | 79 | 15.17 (1.94 to 118.27) |
| Headache | 13 | 69 | 11 | 79 | 1.10 (0.46 to 2.62) |
| Nasopharyngitis | 5 | 69 | 8 | 79 | 0.55 (0.17 to 1.75) |
| Nausea | 26 | 69 | 10 | 79 | 2.99 (1.33 to 6.70) |
| Paresthesia | 41 | 69 | 5 | 79 | 13.48 (4.96 to 36.64) |
| Post‐LP syndrome | 5 | 69 | 6 | 79 | 0.75 (0.22 to 2.56) |
| Rash | 7 | 69 | 2 | 79 | 3.41 (0.69 to 16.94) |
| Sinusitis | 3 | 69 | 6 | 79 | 0.44 (0.11 to 1.82) |
| Tinnitus | 11 | 69 | 3 | 79 | 3.72 (1.00 to 13.85) |
| Vomiting | 12 | 69 | 3 | 79 | 4.11 (1.11 to 15.15) |
| This data is from one study (Wall 2014). Abbreviations: CI = confidence interval; n = number of events; N = number of participants; OR = odds ratio. | |||||
| Outcome | Acetalomazide | Placebo | MD (95% CI) adjusted for centre, baseline value of outcome and baseline papilloedema grade | ||||
| Mean | SD | N | Mean | SD | N | ||
| Wall 2014: Change in VFQ‐25 total score between baseline and 6 months | 8.33 | SE 1.47a | a | 1.98 | SE 1.53a | a | 6.35 (2.22 to 10.47) |
| Wall 2014: Change in VFQ‐25 10‐item neuro‐ophthalmic supplement between baseline and 6 months | 9.82 | SE 1.55a | a | 1.59 | SE 1.62a | a | 8.23 (3.89 to 12.56) |
| Wall 2014: Change in SF‐36 Physical Component Summary between baseline and 6 months | 5.84 | SE 1.01a | a | 2.82 | SE 1.03a | a | 3.02 (0.34 to 5.70) |
| Wall 2014: Change in SF‐36 Mental Component Summary between baseline and 6 months | 5.62 | SE 1.16a | a | 2.17 | SE 1.17a | a | 3.45 (0.35 to 6.55) |
| aIt is unclear how many patients were included in these analyses. | |||||||


