Thrombolytic strategies versus standard anticoagulation for acute deep vein thrombosis of the lower limb
Information
- DOI:
- https://doi.org/10.1002/14651858.CD002783.pub5Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 19 January 2021see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Vascular Group
- Copyright:
-
- Copyright © 2021 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
CB: assessed reference list, extracted data, updated review text
LW: assessed reference list, extracted data, updated review text
MPA: assessed reference list, updated review text, resolved differences where required
Contributions of editorial support
Marlene Stewart (MS; Managing Editor): co‐ordinated the editorial process; edited the review and assisted with full‐text article screening and data extraction.
Sources of support
Internal sources
-
No sources of support supplied
External sources
-
Chief Scientist Office, Scottish Government Health Directorates, The Scottish Government, UK
The Cochrane Vascular editorial base is supported by the Chief Scientist Office.
Declarations of interest
CB is a member of Cochrane Vascular's editorial base staff. Where appropriate, editorial tasks were carried out by other group members.
LW has declared that she received travel and accomodation fees from the European Society of Angiology for speaking at the 2012 meeting on this topic. LW is an editor for Cochrane Vascular but had no editor role for this review.
MPA: none known.
Acknowledgements
We would like to thank Dr Jonathon Michaels, who was involved with formulating the original protocol.
The review authors, and the Cochrane Vascular Editorial base wish to thank the peer referees for their comments: Scott M Stevens MD FRCP, Co‐Director Thrombosis Clinic & Thrombosis Research Group, Intermountain Medical Center, UT, USA; Avi Leader MD, Specialist in Internal Medicine and Hematology, Rabin Medical Center, Petah Tikva, Israel; Dr Ronald LG Flumignan, Sao Paulo, Brazil; Ahmed HS Ibrahim, Egypt.
Version history
| Published | Title | Stage | Authors | Version |
| 2021 Jan 19 | Thrombolytic strategies versus standard anticoagulation for acute deep vein thrombosis of the lower limb | Review | Cathryn Broderick, Lorna Watson, Matthew P Armon | |
| 2016 Nov 10 | Thrombolysis for acute deep vein thrombosis | Review | Lorna Watson, Cathryn Broderick, Matthew P Armon | |
| 2014 Jan 23 | Thrombolysis for acute deep vein thrombosis | Review | Lorna Watson, Cathryn Broderick, Matthew P Armon | |
| 2004 Jul 19 | Thrombolysis for acute deep vein thrombosis | Review | Lorna Watson, Matthew P Armon | |
| 2000 Apr 24 | Thrombolysis for acute deep vein thrombosis | Protocol | Matthew P Armon, J A Michaels | |
Differences between protocol and review
After consideration, the review authors decided to increase the inclusion period of acute symptoms of DVT from 14 to 21 days as this is more commonly used in recent studies. Trials previously excluded due to this were reassessed and included.
In the initial published version, the quality of the trials was investigated using the methods of Jadad (Jadad 1996) and Schulz (Schultz 1995). In keeping with updated Cochrane Collaboration requirements, methodological quality has now been assessed using the Cochrane risk of bias tool (Higgins 2011).
For the 2016 update, we changed the time point definitions to differentiate late outcomes after five years as two studies (Arnesen 1978; CAVENT) now reported results within this period. Due to this Arnesen 1978 data was re‐categorised from intermediate to late.
For the 2020 update, the review title was amended from 'Thrombolysis for acute DVT' to 'Thrombolytic strategies versus standard anticoagulation for acute deep vein thrombosis of the lower limb'. This was to reflect current clinical practice where thrombolysis is frequently carried out in combination with additional strategies to aid removal of the clot, not typically as a stand alone treatment. We added the term 'adult' to Types of participants to clarify only studies involving adult participants would be considered for inclusion. Outcomes were reordered to simplify and reflect those of most clinical relevance. To do this the previous primary outcomes of 'improvement in venous patency', 'stroke', 'venous ulceration rates' and 'mortality' were moved to secondary outcomes. Data were checked to ensure that event numbers for PTS included those patients reported as having ulcers, as two older studies reported these separately. Where necessary, PTS data were corrected to include ulcer events as this was considered clinically appropriate. Checks revealed PTS data for one previously included study (Schweizer 2000), and these data were added. We presented subgroup analysis for this update by delivery method to allow comparison between the routes. In the previous version these results were presented separately. We carried out additional subgroup analysis by level of DVT as it was possible to report this data from the ATTRACT study separately.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Acute Disease;
- Anticoagulants [*therapeutic use];
- Hemorrhage [chemically induced];
- Lower Extremity [*blood supply];
- Postthrombotic Syndrome [epidemiology];
- Randomized Controlled Trials as Topic;
- Thrombolytic Therapy [adverse effects, *methods];
- Time Factors;
- Treatment Outcome;
- Varicose Ulcer [prevention & control];
- Venous Thrombosis [complications, *drug therapy];
Medical Subject Headings Check Words
Humans;
PICOs

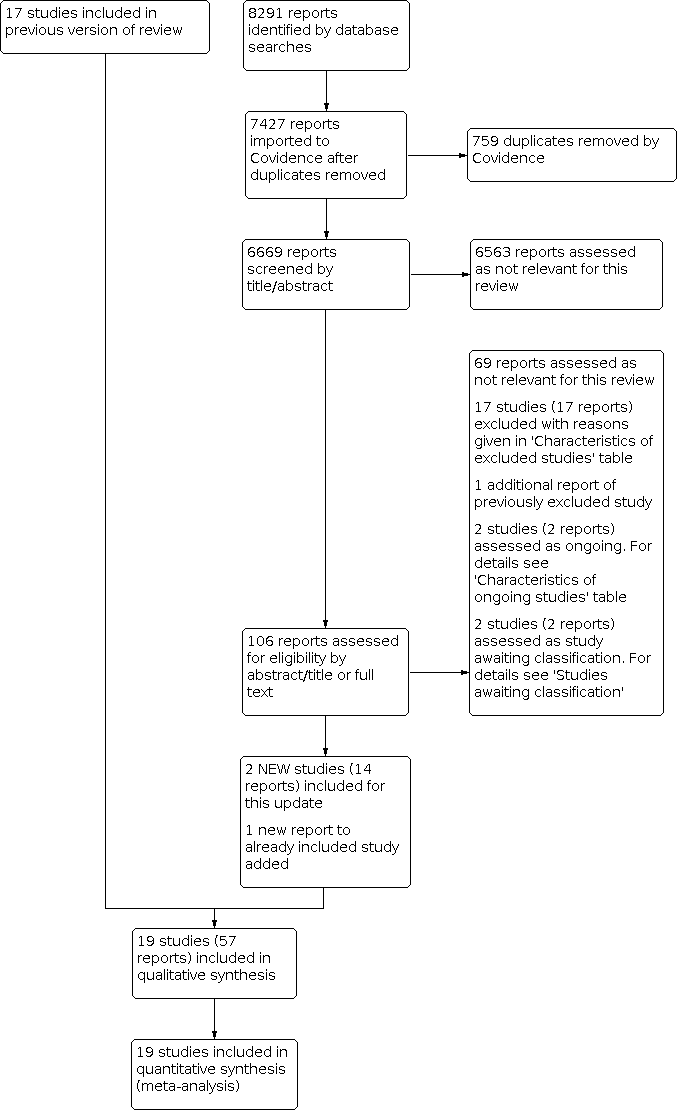
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Funnel plot of comparison: 1 Thrombolysis versus standard anticoagulation, outcome: 1.4 Bleeding (early, subgrouped by thrombolysis strategy).

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 1: Complete clot lysis (early, subgrouped by thrombolysis strategy)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 2: Complete clot lysis (intermediate, subgrouped by thrombolysis strategy)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 3: Complete clot lysis (late, subgrouped by thrombolysis strategy)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 4: Bleeding (early, subgrouped by thrombolysis strategy)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 5: PTS (intermediate, subgrouped by thrombolysis strategy)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 6: PTS by iliofemoral/fempop (intermediate, subgrouped by location)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 7: PTS (late, subgrouped by thrombolysis strategy)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 8: Any improvement in venous patency (early)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 9: Stroke (early, subgrouped by thrombolysis strategy)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 10: Leg ulceration (intermediate, subgrouped by thrombolysis strategy)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 11: Leg ulceration (late)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 12: Mortality (early, subgrouped by thrombolysis strategy)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 13: Mortality (intermediate, subgrouped by thrombolysis strategy)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 14: Mortality (late, subgrouped by thrombolysis strategy)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 15: Recurrent DVT (intermediate, subgrouped by thrombolysis strategy)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 16: Recurrent DVT (late, subgrouped by thrombolysis strategy)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 17: Pulmonary embolism (early, subgrouped by thrombolysis strategy)

Comparison 1: Thrombolysis versus standard anticoagulation, Outcome 18: Venous function (intermediate, subgrouped by thrombolysis strategy)
| Treatment with any thrombolysis clot removal strategy for acute DVT | ||||||
| Patient or population: patients diagnosed with acute DVT | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with standard anticoagulation | Risk with thrombolysis | |||||
| Complete clot lysis (intermediate, 6 months to under 5 years after treatment) | Study population | RR 2.42 (1.42 to 4.12) | 654 | ⊕⊕⊕⊝ | 78 of 244 patients treated with standard anticoagulation had complete clot lysis compared to 198 of 410 in the thrombolysis group | |
| 320 per 1000 | 774 per 1000 (454 to 1000) | |||||
| Bleeding (early, up to 1 month after treatment) | Study population | RR 2.45 | 1943 | ⊕⊕⊕⊝ | ||
| 23 per 1000 | 56 per 1000 (36 to 87) | |||||
| Post‐thrombotic syndrome (intermediate, 6 months to under 5 years after treatment) | Study population | RR 0.78 | 1393 | ⊕⊕⊕⊝ | 329 of 622 patients treated with standard anticoagulation developed PTS compared to 383 of 771 treated with thrombolysis. Additional subgroup analysis did not show any differences in PTS incidence between iliofemoral and femoropopliteal DVTs | |
| 529 per 1000 | 413 per 1000 (349 to 492) | |||||
| Post‐thrombotic syndrome (late, 5 years follow‐up after treatment) | Study population | RR 0.56 | 211 | ⊕⊕⊕⊝ | 75 of 107 patients treated with standard anticoagulation developed PTS compared to 41 of 104 treated with thrombolysis | |
| 701 per 1000 | 393 per 1000 (301 to 512) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Thrombolysis includes delivery of thrombolytics either systemically, loco‐regionally or by CDT. CDT may include the use of additional endovascular techniques | ||||||
| Study | Potential levels of leg vein included |
|---|---|
| proximal to calf | |
| proximal (femoral, common femoral, iliac vein with or without other involved ipsilateral veins) | |
| femoral and iliofemoral | |
| pelvic, iliofemoral, femoral | |
| not specified | |
| proximal | |
| femoral and iliofemoral | |
| popliteal or more proximal | |
| proximal | |
| not specified | |
| not specified | |
| calf up to iliac vein | |
| calf vein thrombosis only | |
| not specified | |
| leg or pelvic (popliteal or more proximal) | |
| not specified | |
| proximal | |
| popliteal up to inferior vena cava | |
| popliteal or more proximal |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Complete clot lysis (early, subgrouped by thrombolysis strategy) Show forest plot | 8 | 592 | Risk Ratio (M‐H, Random, 95% CI) | 4.75 [1.83, 12.33] |
| 1.1.1 Systemic | 7 | 432 | Risk Ratio (M‐H, Random, 95% CI) | 3.65 [1.40, 9.56] |
| 1.1.2 Loco‐regional | 1 | 125 | Risk Ratio (M‐H, Random, 95% CI) | 10.55 [0.66, 168.79] |
| 1.1.3 CDT | 1 | 35 | Risk Ratio (M‐H, Random, 95% CI) | 21.79 [1.38, 343.26] |
| 1.2 Complete clot lysis (intermediate, subgrouped by thrombolysis strategy) Show forest plot | 7 | 654 | Risk Ratio (M‐H, Random, 95% CI) | 2.42 [1.42, 4.12] |
| 1.2.1 Systemic | 4 | 239 | Risk Ratio (M‐H, Random, 95% CI) | 3.80 [1.46, 9.93] |
| 1.2.2 Loco‐regional | 2 | 191 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [1.03, 2.97] |
| 1.2.3 CDT | 2 | 224 | Risk Ratio (M‐H, Random, 95% CI) | 2.52 [0.52, 12.17] |
| 1.3 Complete clot lysis (late, subgrouped by thrombolysis strategy) Show forest plot | 2 | 206 | Risk Ratio (M‐H, Random, 95% CI) | 3.25 [0.17, 62.63] |
| 1.3.1 Systemic | 1 | 34 | Risk Ratio (M‐H, Random, 95% CI) | 16.76 [1.03, 272.11] |
| 1.3.2 Loco‐regional | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.3.3 CDT | 1 | 172 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.94, 1.33] |
| 1.4 Bleeding (early, subgrouped by thrombolysis strategy) Show forest plot | 19 | 1943 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.45 [1.58, 3.78] |
| 1.4.1 Systemic | 14 | 685 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.99 [1.24, 3.19] |
| 1.4.2 Loco‐regional | 2 | 191 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.07 [0.41, 23.05] |
| 1.4.3 CDT | 4 | 1067 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.30 [1.67, 31.98] |
| 1.5 PTS (intermediate, subgrouped by thrombolysis strategy) Show forest plot | 6 | 1393 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.66, 0.93] |
| 1.5.1 Systemic | 2 | 170 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.31, 0.92] |
| 1.5.2 Loco‐regional | 2 | 191 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.73, 1.07] |
| 1.5.3 CDT | 3 | 1032 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.74, 1.05] |
| 1.6 PTS by iliofemoral/fempop (intermediate, subgrouped by location) Show forest plot | 6 | 1393 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.71, 0.94] |
| 1.6.1 Iliofemoral DVT | 4 | 777 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.55, 1.01] |
| 1.6.2 Femoropopliteal DVT | 1 | 300 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.76, 1.27] |
| 1.6.3 Unspecified DVT | 2 | 316 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.69, 0.92] |
| 1.7 PTS (late, subgrouped by thrombolysis strategy) Show forest plot | 2 | 211 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.43, 0.73] |
| 1.7.1 Systemic | 1 | 35 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.14, 0.88] |
| 1.7.2 loco‐regional | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.7.3 CDT | 1 | 176 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.45, 0.79] |
| 1.8 Any improvement in venous patency (early) Show forest plot | 9 | 421 | Risk Ratio (M‐H, Random, 95% CI) | 2.48 [1.35, 4.57] |
| 1.8.1 Systemic | 8 | 386 | Risk Ratio (M‐H, Random, 95% CI) | 2.18 [1.28, 3.70] |
| 1.8.2 CDT | 1 | 35 | Risk Ratio (M‐H, Random, 95% CI) | 35.05 [2.28, 539.63] |
| 1.9 Stroke (early, subgrouped by thrombolysis strategy) Show forest plot | 19 | 1943 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.92 [0.34, 10.86] |
| 1.9.1 Systemic | 14 | 685 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.92 [0.34, 10.86] |
| 1.9.2 Loco‐regional | 2 | 191 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.9.3 CDT | 4 | 1067 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.10 Leg ulceration (intermediate, subgrouped by thrombolysis strategy) Show forest plot | 5 | 1033 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.39, 1.49] |
| 1.10.1 Systemic | 2 | 87 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 7.53] |
| 1.10.2 Loco‐regional | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [0.17, 13.60] |
| 1.10.3 CDT | 2 | 880 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.36, 1.54] |
| 1.11 Leg ulceration (late) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.12 Mortality (early, subgrouped by thrombolysis strategy) Show forest plot | 10 | 1220 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.31, 1.89] |
| 1.12.1 Systemic | 8 | 369 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.31, 1.89] |
| 1.12.2 Loco‐regional | 1 | 125 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.12.3 CDT | 2 | 726 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.13 Mortality (intermediate, subgrouped by thrombolysis strategy) Show forest plot | 4 | 1144 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.39, 1.69] |
| 1.13.1 Systemic | 2 | 176 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.27, 3.43] |
| 1.13.2 Loco‐regional | 1 | 125 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.13.3 CDT | 2 | 843 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.31, 1.86] |
| 1.14 Mortality (late, subgrouped by thrombolysis strategy) Show forest plot | 2 | 230 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.25, 1.50] |
| 1.14.1 Systemic | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.34, 5.24] |
| 1.14.2 CDT | 1 | 188 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.36 [0.10, 1.30] |
| 1.15 Recurrent DVT (intermediate, subgrouped by thrombolysis strategy) Show forest plot | 4 | 1067 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.96, 1.83] |
| 1.15.1 Systemic | 1 | 35 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.41 [0.37, 5.40] |
| 1.15.2 Loco‐regional | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.15.3 CDT | 3 | 1032 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.94, 1.84] |
| 1.16 Recurrent DVT (late, subgrouped by thrombolysis strategy) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.16.1 Systemic | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.16.2 CDT | 1 | 176 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.34, 1.18] |
| 1.17 Pulmonary embolism (early, subgrouped by thrombolysis strategy) Show forest plot | 6 | 433 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.33, 3.05] |
| 1.17.1 Systemic | 5 | 273 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.36, 4.10] |
| 1.17.2 Loco‐regional | 1 | 125 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.17.3 CDT | 1 | 35 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 7.26] |
| 1.18 Venous function (intermediate, subgrouped by thrombolysis strategy) Show forest plot | 3 | 255 | Risk Ratio (M‐H, Random, 95% CI) | 2.18 [0.86, 5.54] |
| 1.18.1 Systemic | 1 | 31 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.59, 1.83] |
| 1.18.2 Loco‐regional | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.18.3 CDT | 2 | 224 | Risk Ratio (M‐H, Random, 95% CI) | 3.18 [1.41, 7.19] |