Pelvimetría para presentaciones cefálicas fetales a término o cerca del término para decidir el modo de parto
Information
- DOI:
- https://doi.org/10.1002/14651858.CD000161.pub2Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 30 March 2017see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Pregnancy and Childbirth Group
- Copyright:
-
- Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
V Vannevel assisted RC Pattinson with the 2016 update. V Vannevel analysed and interpreted the results, and prepared the update. A Cuthbert assessed studies for inclusion and prepared the 'Summary of findings' table.
Sources of support
Internal sources
-
University of Pretoria, South Africa
External sources
-
South African Medical Research Council, South Africa
-
Department of Reproductive Health and Research, World Health Organization, Switzerland
-
UNDP‐UNFPA‐UNICEF‐WHO‐World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization, Switzerland
Declarations of interest
Robert C Pattinson: no conflict of interest.
Anna Cuthbert: no conflict of interest.
Valerie Vannevel: no conflict of interest.
Acknowledgements
Professor Justus Hofmeyr and Ms Cheryl Nikodem for assisting me with the study and teaching me (V Vannevel) the use of Review Manager. Thanks to Therese Dowswell (Cochrane Pregnancy and Childbirth) for her contribution in assessing studies and help preparing the 'Summary of findings' table for this update (2016).
This research was supported by a grant from the Department of Reproductive Health and Research, World Health Organization (WHO). The findings, interpretations and conclusions expressed in this paper are entirely those of the authors and should not be attributed in any manner whatsoever to WHO.
We thank El‐Marie Farrell for contributions to the previous update.
As part of the pre‐publication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team), a member of Cochrane Pregnancy and Childbirth's international panel of consumers and the Group's Statistical Adviser.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Version history
| Published | Title | Stage | Authors | Version |
| 2017 Mar 30 | Pelvimetry for fetal cephalic presentations at or near term for deciding on mode of delivery | Review | Robert C Pattinson, Anna Cuthbert, Valerie Vannevel | |
| 1997 Apr 21 | Pelvimetry for fetal cephalic presentations at or near term | Review | Robert C Pattinson, El‐Marie E Farrell | |
Differences between protocol and review
Title: We changed the title from Pelvimetry for fetal cephalic presentations at or near term to Pelvimetry for fetal cephalic presentations at or near term for deciding on mode of delivery.
Objectives: We removed assessing the effects of postnatal pelvimetry from the objectives as this could not impact on mode of delivery.
We also removed the following hypothesis.
-
Information provided by pelvimetry in women without previous caesarean section is useful because it decreases the morbidity and mortality in the women and fetuses or neonates.
-
Information provided by pelvimetry in women with previous caesarean section is useful because it decreases the morbidity and mortality in the women and fetuses or neonates.
We have clarified aspects in the section on Criteria for considering studies for this review, as follows:
Types of studies
All acceptably randomised comparisons of the use of pelvimetry in cephalic presentations in:
-
women without previous caesarean section;
-
women with previous caesarean section.
has changed to:
We included all randomised controlled trials (including quasi‐randomised) comparing pelvimetry in cephalic presentations versus no pelvimetry or comparing different types of pelvimetry. We would have included cluster trials if they had been identified during the search. Cross‐over studies were not eligible for this review.
If an abstract was of interest, we would have contacted the authors for further information about their trial.
Types of participants
-
Women without caesarean section;
-
Women with previous caesarean section.
has changed to:
Pregnant women with singleton, cephalic presentation fetus who have or have not had a previous caesarean section. Studies which recruited women before, or during labour were included as well as women for spontaneous labour, induction or trial of scar after previous caesarean section.
Types of interventions
Policy of elective caesarean section or trial of labour or scar depending on the prediction of pelvimetry as opposed to trial of labour or scar in all.
has changed to:
The main intervention of interest is pelvimetry as a predictor of cephalo‐pelvic disproportion. Control groups could include women who did not have pelvimetry or who had different types of pelvimetry.
We planned to include studies comparing different methods of clinical or radiological pelvimetry such as X‐rays, computerised tomography (CT) scanning or magnetic resonance imaging (MRI). We reported women who have had one previous caesarean section and women who have had no previous section, or are nulliparous, in separate clinical subgroups.
Outcomes: We changed 'Caesarean section/symphysiotomy' to 'Caesarean section'.Crichton 1962 only, reported the composite outcome of caesarean section/symphysiotomy, and did not report data for these outcomes separately. It is not clear how many symphysiotomies were performed in this trial and we could not report the data as two separate outcomes. We have documented this in the results section and in footnotes in Analysis 1.1.
'Summary of findings' table: We assessed the trial quality by using GRADE assessment. This is documented in summary of findings Table 1.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Apgar Score;
- Blood Transfusion [statistics & numerical data];
- Cesarean Section [statistics & numerical data];
- Delivery, Obstetric [*methods];
- *Labor Presentation;
- Pelvimetry [*methods];
- Perinatal Mortality;
- Randomized Controlled Trials as Topic;
- Surgical Wound Dehiscence [epidemiology];
- Surgical Wound Infection [epidemiology];
- *Term Birth;
Medical Subject Headings Check Words
Female; Humans; Pregnancy;
PICOs

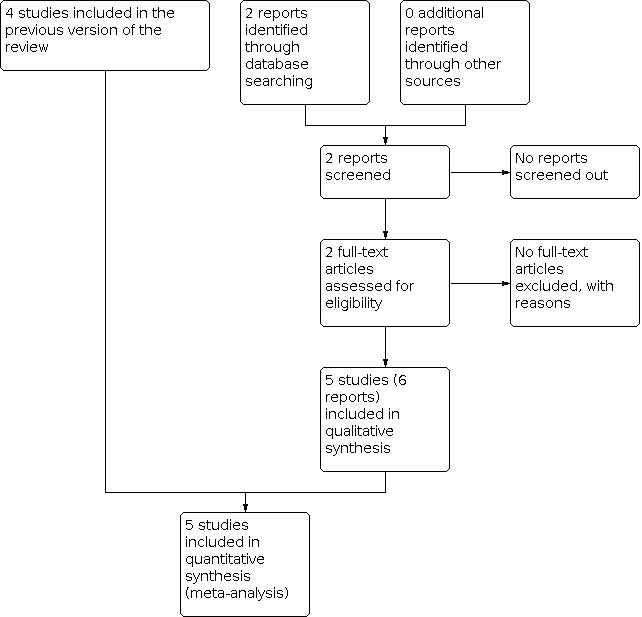
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Comparison 1: X‐ray pelvimetry versus no X‐ray pelvimetry, Outcome 1: Caesarean section

Comparison 1: X‐ray pelvimetry versus no X‐ray pelvimetry, Outcome 2: Perinatal mortality

Comparison 1: X‐ray pelvimetry versus no X‐ray pelvimetry, Outcome 3: Puerperal pyrexia

Comparison 1: X‐ray pelvimetry versus no X‐ray pelvimetry, Outcome 4: Wound sepsis

Comparison 1: X‐ray pelvimetry versus no X‐ray pelvimetry, Outcome 5: Blood transfusion

Comparison 1: X‐ray pelvimetry versus no X‐ray pelvimetry, Outcome 6: Scar dehiscence

Comparison 1: X‐ray pelvimetry versus no X‐ray pelvimetry, Outcome 7: Perinatal asphyxia

Comparison 1: X‐ray pelvimetry versus no X‐ray pelvimetry, Outcome 8: Admission to special care baby units
| X‐ray pelvimetry compared to no X‐ray pelvimetry in fetal cephalic presentations at or near term | ||||||
| Patient or population: pregnant women at or near term with fetal cephalic presentations | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with no pelvimetry in cephalic presentations | Risk with X‐ray pelvimetry | |||||
| Caesarean section | Study population | RR 1.34 | 1159 | ⊕⊕⊝⊝ | One study Crichton 1962 reported caesarean section and symphysiotomy together | |
| 388 per 1000 | 520 per 1000 | |||||
| Perinatal mortality | Study population | RR 0.53 | 1159 | ⊕⊝⊝⊝ | ||
| 17 per 1000 | 9 per 1000 | |||||
| Wound sepsis | Study population | RR 0.83 | 288 | ⊕⊝⊝⊝ | ||
| 42 per 1000 | 35 per 1000 | |||||
| Blood transfusion | Study population | RR 1.00 | 288 | ⊕⊝⊝⊝ | ||
| 56 per 1000 | 56 per 1000 | |||||
| Scar dehiscence | Study population | RR 0.59 | 390 | ⊕⊝⊝⊝ | ||
| 26 per 1000 | 15 per 1000 | |||||
| Admission to special care baby units | Study population | RR 0.20 | 288 | ⊕⊝⊝⊝ | ||
| 14 per 1000 | 3 per 1000 | |||||
| Apgar score < 7 at 5 minutes | Study population | ‐ | (0 studies) | ‐ | No data reported for this outcome | |
| see comment | see comment | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Most studies contributing data had design limitations. Two studies had serious design limitations (high risk of bias for sequence generation and allocation concealment) one of which contributed 37.4% of weight (‐2). 2 Most studies contributing data had design limitations. (‐1) 3 Wide confidence interval crossing the line of no effect, small sample size, few events and lack of precision. (‐2) 4 One study contributing data with serious design limitations. (‐2) 5 Very wide confidence intervals crossing the line of no effect, small sample size and few events. (‐2) 6 Study contributing 79.7% total weight has serious design limitations. (‐2) | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Caesarean section Show forest plot | 5 | 1159 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [1.19, 1.52] |
| 1.1.1 No previous caesarean section | 3 | 769 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [1.02, 1.52] |
| 1.1.2 Previous caesarean section | 2 | 390 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [1.26, 1.67] |
| 1.2 Perinatal mortality Show forest plot | 5 | 1159 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.19, 1.45] |
| 1.2.1 No previous caesarean section | 3 | 769 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.21, 1.90] |
| 1.2.2 Previous caesarean section | 2 | 390 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.01, 3.91] |
| 1.3 Puerperal pyrexia Show forest plot | 1 | 288 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.22, 2.92] |
| 1.3.1 No previous caesarean section | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.3.2 Previous caesarean section | 1 | 288 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.22, 2.92] |
| 1.4 Wound sepsis Show forest plot | 1 | 288 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.26, 2.67] |
| 1.4.1 No previous caesarean section | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.4.2 Previous caesarean section | 1 | 288 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.26, 2.67] |
| 1.5 Blood transfusion Show forest plot | 1 | 288 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.39, 2.59] |
| 1.5.1 No previous caesarean section | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.5.2 Previous caesarean section | 1 | 288 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.39, 2.59] |
| 1.6 Scar dehiscence Show forest plot | 2 | 390 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.14, 2.46] |
| 1.7 Perinatal asphyxia Show forest plot | 1 | 305 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.39, 1.10] |
| 1.8 Admission to special care baby units Show forest plot | 1 | 288 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.01, 4.13] |
| 1.8.1 No previous caesarean section | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.8.2 Previous caesarean section | 1 | 288 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.01, 4.13] |