Uso de la episiotomía selectiva versus sistemática para el parto vaginal
References
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Jump to:
| Methods | RCT | |
| Participants | Women after admission to the labour ward, I00 primigravidae in each group Inclusion criteria: primigravidae in labour at term with a singleton fetus in cephalic presentation. Exclusion criteria: participants with gross fetal malformations. | |
| Interventions | Intervention group: episiotomy was avoided and was only given for fetal distress or when severe perineal trauma was judged to be imminent. Control group: right mediolateral episiotomy was made in all primigravidae according to hospital policy. | |
| Outcomes | Severe perineal trauma, rate of episiotomy | |
| Notes | Right mediolateral episiotomies. Epsiotomy rates were 32% for the selective group and 100% for the routine group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Low risk | Woman was asked to open one of the two envelopes each envelope containing intervention for the either group as mentioned above (routine and selective use of episiotomy groups) for randomised selection |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | High risk | No description of loss to follow‐up. Exactly 100 in each group. Table of patient variables does not give numbers of women on which these data are based. There appears to be a differential loss to follow‐up (at 7th day postpartum), 19 women were lost from the selective group, and 12 from the routine group. |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated were reported but unable to fully judge |
| Other bias | Unclear risk | The authors claim no "severe perineal trauma" but table 2 indicates there is 100% in both groups, leading to questions about the integrity of the data. |
| Methods | Generation of randomisation by computer from a random sample generator programme, organised in balanced blocks of 100, with stratification by centre and by parity (nulliparous and primiparous) Allocation concealment by sequentially‐numbered, sealed, opaque envelopes, divided according to parity. | |
| Participants | N: 2606 women; 1298 women in the intervention group and 1308 women in the control group. 1555 were nulliparous (778 in the selective group and 777 in the routine group) and 1051 primiparous (520 in the selective and 531 in the routine group). | |
| Interventions | Intervention: selective ‐ try to avoid an episiotomy if possible and only do it for fetal indications or if severe perineal trauma was judged to be imminent Control: routine ‐ do an episiotomy according to the hospital’s policy prior to the trial | |
| Outcomes | Severe perineal trauma (primary outcome); middle/upper vaginal tears; anterior trauma; any posterior surgical repair; posterior perineal surgical repair; perineal pain at discharge; haematoma at discharge; healing complications, infection and dehiscence at 7 days. Apgar score less than 7 at 1st minute. | |
| Notes | Mediolateral episiotomies. Epsiotomy rates were 30% for the restricted group and 80.6% for the routine group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The description "Random treatment assignments were derived from a random sample generator programme and was organized in balanced blocks of 100, with stratification by centre and parity". |
| Allocation concealment (selection bias) | Low risk | The description "Each centre was supplied with a set of sequentially‐ numbered, sealed, opaque envelopes, which contained the trial instructions". |
| Blinding of participants and personnel (performance bias) | Unclear risk | The description "Healing and morbidity were assessed at the time of discharge from hospital and on the seventh postpartum day by an independent physician who did not know the trial allocation". However, it was not clear whether the primary outcome "perineal trauma" "assessed by the attending physician at the time of delivery" was done with blinding. It was not clear whether participants were blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | The description "Healing and morbidity were assessed at the time of discharge from hospital and on the seventh postpartum day by an independent physician who did not know the trial allocation". The assessment was blinded, but no details reported for other outcomes, e.g. severe perineal trauma at delivery. |
| Incomplete outcome data (attrition bias) | High risk | The primary outcome was with a 5% loss to follow‐up at delivery. 93.0% of women in the selective group and 92.9% in the routine were assessed when discharged from hospital. This is high. However, 42.7% and 43.1% followed up for the selective and routine group respectively on the seventh day postpartum. More than half of women in both groups were not assessed, but no detailed information about this |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated were reported but unable to fully judge as no trial protocol |
| Other bias | Unclear risk | Not enough information to judge |
| Methods | Random generation: not stated Allocation concealment: sealed opaque envelopes | |
| Participants | Number randomised: 146 (selective 70, routine 76) Inclusion criteria: primiparous, > 34 weeks of gestation, with an uncomplicated pregnancy and with a live singleton fetus. Women were intending to have a vaginal delivery. Exclusion criteria: previous surgery at the pelvic floor, or neurologic disorder | |
| Interventions | Intervention: restrictive ‐ try to avoid an episiotomy even if severe perineal trauma was judged to be imminent and only do it for fetal indications. Control: liberal ‐ in addition to fetal indications use of episiotomy when a tear is judged to be imminent. | |
| Outcomes | Reduction of episiotomies, increase of intact perinea and only minor perineal trauma, perineal pain (displayed in score) in the postpartum period, percentage change in overall anterior perineal trauma, difference of the PH of the umbilical artery, percentage of umbilical artery PH less than 7.15, percentage of Apgar scores less than 7 at 1 and 5 minutes, maternal blood loss at delivery (measured by mean difference pre/post haemoglobin), percentage of severe perineal trauma, dyspareunia, urinary incontinence | |
| Notes | Mediolateral episiotomies. Episiotomy rates were 70% for restricted group and 79% for the routine group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Low risk | The description "Random treatment assignments were carried out using two opaque envelopes with the different policies enclosed for every particular participant" |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Unclear risk | Loss to follow‐up reported with reason, but unable to fully judge. For follow‐up approximately 6 months or more later, the overall dropout was around 40%, 45% in selective, and 32% in routine |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated were reported but unable to fully judge |
| Other bias | Unclear risk | No enough information to judge |
| Methods | Random generation: not stated | |
| Participants | N: 200 women (100 in each) Inclusion criteria: primigravid women with live, singleton fetus, cephalic presentation of at least 37 weeks of gestational age, having a spontaneous vaginal delivery. Women were not suffering from any important medical or psychiatric disorder. | |
| Interventions | Intervention: selective ‐ the intention was not to perform an episiotomy unless it was absolutely necessary for maternal or fetal reasons | |
| Outcomes | First‐, second‐, third‐ and fourth‐degree tears, anterior trauma, need for suturing, and neonatal outcomes: Apgar score at 1 and 5 minutes, and stay in NICU | |
| Notes | Mediolateral episiotomies. Epsiotomy rates were 53% for the restricted group and 83% for the routine group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details reported |
| Allocation concealment (selection bias) | Low risk | The description "Entry to the trial, which was signalled by opening a sealed opaque envelope, was postponed until the attending midwife had decided to 'scrub up' in expectation of a spontaneous vaginal delivery" |
| Blinding of participants and personnel (performance bias) | Unclear risk | No details reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | No details reported |
| Incomplete outcome data (attrition bias) | Unclear risk | No detailed reported |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated were reported but unable to fully judge |
| Other bias | Unclear risk | No enough information to judge |
| Methods | Generation method of randomisation not established Concealment allocation method not established "Allocated randomly" | |
| Participants | N: 181 (intervention, N = 92; control, N = 89). Inclusion criteria: women primigravid, vaginal delivery, at least 16 years old, no less than 38 weeks’ gestational age, not suffering from any important medical or psychiatric conditions or eclampsia | |
| Interventions | Intervention: not to undergo episiotomy unless it was considered to be medically essential by the person in charge, that is the accoucheur could see that a woman was going to sustain a greater damage or if the intact perineum was thought to be hindering the achievement of a safe normal or operative delivery. Control: to undergo mediolateral episiotomy | |
| Outcomes | Severe maternal trauma. Any posterior perineal trauma. Need for suturing perineal trauma | |
| Notes | Mediolateral episiotomies. Epsiotomy rates were 7.6% for restricted group and 100% for the routine group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details reported |
| Allocation concealment (selection bias) | Unclear risk | No details reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | No details reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | No details reported |
| Incomplete outcome data (attrition bias) | High risk | Data were not reported by randomisation group |
| Selective reporting (reporting bias) | Unclear risk | No enough information to judge |
| Other bias | Unclear risk | No enough information to judge |
| Methods | Generation method of randomisation not established Concealment method of allocation by envelopes | |
| Participants | Number of participants not established. There is only information for 165 women available to follow‐up but information about women lost to follow‐up is lacking, either because 1 of the study authors was not available, or because of the early discharge scheme. 98 primigravidae and 67 multigravidae. 94 in the intervention and 71 in the control group. Inclusion criteria: women were at least 37 weeks’ gestational age, cephalic presentation and vaginal delivery. Exclusion criteria: lack of consent, labour at less than 37 weeks pregnant, presentation other than vertex, caesarean section and the unavailability of an accoucheur willing to abide by the research protocol. Women who subsequently had a forceps delivery were not excluded | |
| Interventions | Intervention: restrict ‐ not to perform specifically to prevent laceration Control: liberal ‐ to receive standard current management whereby perineal damage was avoided by control of the descent of the head and supporting the perineum at crowning. An episiotomy was made if there was fetal distress, or for maternal reasons to shorten the 2nd stage such as severe exhaustion, inability to complete expulsion or unwillingness to continue pushing. Episiotomy was performed if the perineum appeared to be too tight or rigid to permit delivery without laceration, or if a laceration appeared imminent. | |
| Outcomes | Second‐degree tear. Third‐degree tear. Need for perineal suturing. Any perineal pain at 3 days. Healing at 3 days. Tenderness at 3 days. Perineal infection at 3 days. Blood loss during delivery | |
| Notes | Mediolateral episiotomies. Epsiotomy rate for restricted group were 18% and for the routine group were 69% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details reported |
| Allocation concealment (selection bias) | Low risk | Judge from the description "This involved the selection of envelopes containing a questionnaire and management group" |
| Blinding of participants and personnel (performance bias) | Low risk | The description "Women were not informed of the management group allocated" |
| Blinding of outcome assessment (detection bias) | Unclear risk | No details reported |
| Incomplete outcome data (attrition bias) | Unclear risk | The study involved above 165 women over a 12‐month period. Authors did not provide how many participants were recruited at the recruitment |
| Selective reporting (reporting bias) | Unclear risk | No enough information to judge |
| Other bias | Unclear risk | Unclear risk of bias of measuring blood loss at delivery since the study used visual inspection for blood loss estimation without specific training. Not enough information to judge for other bias |
| Methods | Generation method of randomisation not established Concealment method of randomisation not stated. Experimental study, controlled, with random allocation of women to the control group who were given routine episiotomy or to the experimental group who were given a selective episiotomy | |
| Participants | N: 402 (intervention, N = 200; control, N = 202) | |
| Interventions | Intervention: selective episiotomy (by fetal or maternal indication) | |
| Outcomes | Weight gain during gestation, maternal weight at the time of delivery | |
| Notes | Medio‐lateral; 118 of 200 women had episiotomy in the selective group; 169 of 202 women had episiotomy in the control group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details reported |
| Allocation concealment (selection bias) | Unclear risk | No details reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | No details reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | There was the description "On the third day after puerperium, a different midwife carried out a personalised survey and assessed the perineum". However, it was not clear whether the midwife was blinded for the group allocation |
| Incomplete outcome data (attrition bias) | Low risk | 402 women began the study. 14 women who received an early discharge which impeded them from being interviewed during hospital puerperium; at 3 months postpartum, 21 participants were excluded due to not being able to be contacted; at 3 years after childbirth, 37 participants from the initial sample were excluded due to the fact that it was impossible to contact women |
| Selective reporting (reporting bias) | Unclear risk | No details reported |
| Other bias | Unclear risk | No details reported |
| Methods | Generation method of randomisation not established Concealment of allocation by opaque, sequentially‐numbered envelopes | |
| Participants | N: 703 randomised (N = 353; control, N = 350). Inclusion criteria: women had a parity of 0, 1, or 2, between the ages of 18 and 40 years, carried a single fetus, spoke English or French, and were of medical and obstetrical low risk as determined by their physician. Exclusion criteria: prematurity, that is gestation less than 37 weeks, medical conditions developing late in pregnancy, fetal distress, caesarean deliveries and planned forceps | |
| Interventions | Intervention: restricted ‐ "Try to avoid an episiotomy". The physician should only use episiotomy for fetal indications (late fetal distress: fetal bradycardia, tachycardia, or meconium‐stained amniotic fluid) or rarely for maternal perineal indications (severe tear anticipated) Control: liberal ‐ "Try to avoid a tear". The physician was expected to use episiotomy liberally as the usual or routine method for preventing tears | |
| Outcomes | Perineal trauma including first, second, third and fourth degree and sulcus tears. Perineal pain at 1, 2, 10 days. Dyspareunia. Urinary incontinence and perineal bulging. Time on resumption and pain of sexual activity. Pelvic floor function. Admission to special care baby unit | |
| Notes | Midline episiotomies. Epsiotomy rates were 43.8% for restricted group and 65% for the routine group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details reported |
| Allocation concealment (selection bias) | Low risk | The description "Usage of opaque envelopes that were sequentially numbered, and contained instructions printed on opaque cards" |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not blinded. As stated in the text "Blinding of the staff to subject group membership was not possible. The subjects, while they usually knew if they had received an episiotomy, were generally naive as to their study group membership (base on intention to treat)" |
| Blinding of outcome assessment (detection bias) | Unclear risk | No details reported |
| Incomplete outcome data (attrition bias) | Low risk | A loss to follow‐up rate around 1% at delivery and 3 months postpartum. |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated were reported but unable to fully judge |
| Other bias | Unclear risk | No details reported |
| Methods | RCT. Random allocation to: A. restrictive use of episiotomy for instrumental vaginal delivery B. routine use of episiotomy for instrumental vaginal delivery | |
| Participants | N: 200 women (intervention, N = 101; control, N = 99) Inclusion criteria: primigravid women in the third trimester of pregnancy (> 36 weeks) with a singleton cephalic pregnancy who were English speakers and had no contra‐indication to vaginal birth Exclusion criteria: women who were: non‐English speakers; who had contra‐indication to vaginal birth; multiple pregnancy; malpresentation; multiparous women as the rate of instrumental delivery is significantly lower in these women making the effort of recruitment unjustified; women who had not given written informed consent prior to the onset of labour. | |
| Interventions | Intervention: restrictive use of episiotomy for instrumental vaginal delivery (only if tearing becomes apparent) Control: routine use of episiotomy for instrumental vaginal delivery (in all cases) | |
| Outcomes | Extensive perineal tearing involving the anal sphincter (third‐ or fourth‐degree tears) Postpartum haemorrhage, shoulder dystocia, the mother's perception of pain, the length of postnatal hospital stay, urinary or bowel symptoms and the rate of healing complications, low Apgar scores, low arterial blood gases, admission to the neonatal intensive care unit and trauma, estimated blood loss | |
| Notes | Unclear for the mediolateral or midline episiotomies | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The description "The randomisation was performed by computer program using a randomisation sequence generated by a statistician unconnected with the study. Allocation was stratified by maternity unit using randomly permuted blocks of 10" |
| Allocation concealment (selection bias) | Low risk | The description "The allocation was revealed immediately prior to commencing the OVD. Some randomisation were allocated using opaque envelopes due to technical difficulties with the programme. Adherence to the allocation was confirmed by the research midwife each day" |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Unclear risk | Loss to follow‐up reported without reasons (described as unobtained), unable to fully judge |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated were reported but unable to fully judge |
| Other bias | Unclear risk | No details reported |
| Methods | Ralloc software (Boston College Department of Economics, Boston, MA) was used to create a random sequence of numbers in blocks with 2, 4, and 6 size permutations. | |
| Participants | N: 446 randomised, 223 in each group (intervention, N = 222 analysed; control, N = 223). Inclusion criteria: nulliparous women with pregnancies more than 28 weeks of gestation who had vaginal deliveries Exclusion criteria: women with multiple pregnancies, and with breech presentations and those who did not sign the informed consent or refused to participate in the study | |
| Interventions | Intervention: selective ‐ to undergo the procedure only in cases of forceps delivery, fetal distress, or shoulder dystocia or when the operator considered that a severe laceration was impending and could only be avoided by performing an episiotomy. | |
| Outcomes | The primary outcome of severe laceration to perineal tissues was defined as a third‐degree laceration when the extent of the lesion included the external anal sphincter totally or partially, and fourth‐degree laceration when the rectal mucosa was involved. | |
| Notes | Midline episiotomies. Epsiotomy rates were 24.3% for restricted group and 100% for the routine group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random sequence of numbers was established, and block size reported |
| Allocation concealment (selection bias) | Unclear risk | Inadequate information to judge as it was described "randomisation sequence was kept at the institution" |
| Blinding of participants and personnel (performance bias) | Unclear risk | No details reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | No details reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Reported numbers of loss with reason, but unable to fully judge |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated were reported but unable to fully judge |
| Other bias | Unclear risk | No enough information to judge |
| Methods | Generation method of randomisation not established Concealment of allocation by opaque sealed envelopes | |
| Participants | N: 1000 (intervention, N = 498; control, N = 502) Inclusion criteria: women randomised with spontaneous vaginal deliveries, live singleton fetus, at least 37 completed weeks of gestational age, cephalic presentation From the 1000 original women randomised in the original trial, 922 were available for follow‐up and 674 of them responded to a postal questionnaire which are the women included in the analysis | |
| Interventions | Intervention: restrict policy ‐ “Try to avoid episiotomy”: the intention should be to avoid an episiotomy and performing it only for fetal indications (fetal bradycardia, tachycardia, or meconium‐stained liquor) Control: liberal policy ‐ “Try to prevent a tear”: the intention being that episiotomy should be used more liberally to prevent tears | |
| Outcomes | Severe maternal trauma: extension through the anal sphincter or to the rectal mucosa or to the upper 3rd of the vagina | |
| Notes | Mediolateral episiotomies. Epsiotomy rates were 10.2% for restricted group and 51.4% for the routine group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details reported |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelope was used for group allocation |
| Blinding of participants and personnel (performance bias) | Unclear risk | Although 1 of the outcomes was described as "Perineal discomfort three months after delivery reported by mothers who in most cases blind to the allocation", but not enough information to judge how they were blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Perineal pain 10 days after delivery, admission to special care baby unit in first 10 days of life, were assessed by community midwife blind to the allocation; not enough information to judge |
| Incomplete outcome data (attrition bias) | Unclear risk | "One thousand women (93% of those who met the criteria for entry) were allocated at random to one of two management policies. But 885 were assessed on 10 days postpartum, and 895 assessed on three months postpartum." The follow‐up rate at both 10 days and 3 months after delivery was 89%. For 3‐years' follow‐up, the loss to follow‐up was about 33%. There was the description "no attempt was made to contact 15 women: eight were known to speak little English; two had refused to adoption; open baby had been taken into care; and one baby had died in the neonatal period. 481 (49%) of the remaining 985 participants had changed their address in the three years since the original study, of whom 303 (31%) were still living within West Berkshire Health Authority. The new address of 100 of the remaining 178 women was not known". Another 63 women were unable to trace because they had "registered in different name (one woman had changed her name six times during the three days), or failed to reregister for medical care in a different area, or because their husbands had been transferred to military posts overseas; one mother had died" |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated were reported but unable to fully judge |
| Other bias | Unclear risk | Not enough information to judge |
| Methods | Generation method of randomisation not established | |
| Participants | N: 209 randomised, 171 analysed (intervention, N = 89; control, N = 82). Inclusion criteria: Women live singleton pregnancy with cephalic presentation, gestation beyond 37 weeks, primigravida, women with no history of severe perineal injuries, no life‐threatening medical or psychiatric conditions | |
| Interventions | Intervention: selective ‐ women in the selective group were not to undergo episiotomy unless considered essential for various reasons such as fetal distress or imminent extended perineal injury Control: routine‐ all women in the routine group were to undergo the usual hospital protocol | |
| Outcomes | Prevalence of obstetrical anal sphincter injuries, incidence of first‐, second‐, third‐ and fourth‐degree perineal tears, blood loss, mean birthweight, and newborns with pH less than 7.2 and admission to the NICU, blood loss, intact perineum | |
| Notes | Mediolateral. Half in the selective group had episiotomy and all (100%) women in the routine group were subjected to an episiotomy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details reported |
| Allocation concealment (selection bias) | Low risk | The description "Randomization into selective and routine episiotomy group was performed by opening a sealed opaque envelope" |
| Blinding of participants and personnel (performance bias) | Unclear risk | No details reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | No details reported |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated were reported but unable to fully judge |
| Other bias | Unclear risk | Unclear risk of bias of measuring blood loss at delivery since the study used visual inspection for blood loss estimation without specific training. Not enough information to judge for other bias |
NICU: neonatal intensive care unit
RCT: randomised controlled trial
Characteristics of excluded studies [ordered by study ID]
Jump to:
| Study | Reason for exclusion |
| This study examined a policy of no episiotomy versus selective episiotomy; this comparison was not covered in this review which focused on selective versus routine episiotomy | |
| Quasi‐randomised controlled trial, participants were allocated by the last digit of their hospital numbers and the appropriate episiotomy was performed if needed | |
| This study did not compare the restrictive use of episiotomy versus the routine use of episiotomy. It compared median and medio‐lateral episiotomy. | |
| This study focused on 2 approaches of mediolateral episiotomy (with different angles), rather than the comparison between restrictive and routine episiotomy. There was no description on the process of randomisation and how pain was scored. | |
| This paper compared 2 incision angles of mediolateral episiotomy, not the restrictive use of episiotomy and routine use of episiotomy. | |
| Only translated abstract was available. Degrees of perineal trauma not clear from the abstract. The abstract only included the overall proportion of perineal trauma. | |
| As described in the Summary, it was a quasi‐randomised study. (Design: The study was a population‐based observational study. 2 approaches were used in the analyses: At first we considered the women giving birth as quasi randomised to 1 of 3 equally sized groups of midwives, where episiotomy was used to different extents. Next, we studied the effect of episiotomy on the state of the anal sphincter as well as birthweight, parity and the duration of the second stage of labour.) | |
| The study compared the use of episiotomy or not, rather than the restrictive use and routine use of episiotomy. | |
| The comparison was not conducted between the restrictive use of episiotomy and routine use of episiotomy, but to compare the use of episiotomy or not. Furthermore, participants were not randomly allocated to the 2 groups. (Page 107, 300 primigravida were selected randomly by lottery system but when a patient included in group B, who was not to undergo episiotomy, needed that due to fetal indication, she was shifted to the other group A who were to undergo episiotomy, medio‐lateral in every case.) | |
| The studies aimed to compare mediolateral versus lateral episiotomy, and to compare the effect of episiotomy performed before and at time of crowning in primiparous women, not for restrictive use of episiotomy and routine use of episiotomy. | |
| To compare the use of episiotomy and non‐use of episiotomy | |
| The study compared the use of episiotomy or not, not comparing the selective use and routine use of episiotomy. | |
| To compare episiotomy suture angles with Braun‐Stadler episiotomy scissors with the new fixed angle EPISCISSORS‐60. | |
| Only abstract is available, excluded | |
| This study did not compare restrictive use of episiotomy and routine use of episiotomy. It compared curved versus straight scissors to avoid 3rd and 4th degree tears. | |
| The study compared midline versus mediolateral episiotomy rather than selective versus routine episiotomy. There is no reference about the method of randomisation used. The effects are not shown in a quantitative format making the data uninterpretable. |
Characteristics of ongoing studies [ordered by study ID]
Jump to:
| Trial name or title | The effect of episiotomy on maternal and fetal outcomes (EPITRIAL) |
| Methods | RCT |
| Participants | 14,842 women in 7 northern public Israeli hospitals from February 2015‐February 2019 Inclusion criteria Women who are able to understand and sign the informed consent forms |
| Interventions | Intervention: avoidance of episiotomy Episiotomy will not be performed in this group. Deviation from protocol (i.e. episiotomy performance) will be allowed only according to the discretion of obstetrician in charge of the delivery, in cases of unequivocal benefit to the fetus. Control: no episiotomy The decision to perform episiotomy in this group will be based on routine delivery care, i.e. indistinguishable from any other delivery not participating in the trial. |
| Outcomes | Obstetric anal sphincter injury (time frame: from the delivery to 1 h after delivery) (Designated as safety issue: no |
| Starting date | February 2015 |
| Contact information | Lena Sagi‐Dain, email: [email protected] |
| Notes |
| Trial name or title | Restrictive versus routine episiotomy: a randomised controlled trial. |
| Methods | RCT |
| Participants | 3 study hospitals will be included, Srinagarind Hospital, a super tertiary care university hospital; Khon Kaen Hospital, a regional tertiary care hospital; Kalasin Hospital. Women who agree to participate in the trial after having signed the consent form will be randomly allocated to be delivered with either restrictive or routine episiotomy. A total of 3006 women will be recruited ‐ for primi‐parity group 1100 women (550 per arm); for multi‐parity group 1906 women (953 per arm) Inclusion criteria Age > 18 years old and able to read and write Singleton pregnancy Gestational age at least 37 weeks Cephalic presentation Planned vaginal delivery Exclusion criteria Women planned for cesarean delivery |
| Interventions | Intervention: restrictive episiotomy ‐ to avoid episiotomy unless indicated for fetal indications and/or to avoid severe laceration Control: routine episiotomy ‐ all women receive episiotomy, either medio‐lateral or midline according to attending personnel |
| Outcomes | Primary outcome: severe perineal trauma (third‐degree and fourth‐degree laceration) Secondary outcomes
|
| Starting date | Pending (not yet recruiting as of August 2016) |
| Contact information | Jadsada Thinkhamrop; email: [email protected] |
| Notes |
RCT: randomised controlled trial
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe perineal/vaginal trauma Show forest plot | 11 | 6177 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.52, 0.94] |
| Analysis 1.1  Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 1 Severe perineal/vaginal trauma. | ||||
| 2 Severe perineal/vaginal trauma (grouped by trial implementation success) Show forest plot | 11 | 6177 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.52, 0.94] |
| Analysis 1.2  Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 2 Severe perineal/vaginal trauma (grouped by trial implementation success). | ||||
| 2.1 Difference in episiotomy rate < 30% | 3 | 1300 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.63, 1.69] |
| 2.2 Difference in episiotomy rate 30% + | 8 | 4877 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.38, 0.81] |
| 3 Blood loss at delivery (mL) Show forest plot | 2 | 336 | Mean Difference (IV, Random, 95% CI) | ‐27.16 [‐74.80, 20.49] |
| Analysis 1.3  Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 3 Blood loss at delivery (mL). | ||||
| 4 Newborn Apgar score < 7 at 5 minutes Show forest plot | 2 | 511 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.01, 0.01] |
| Analysis 1.4 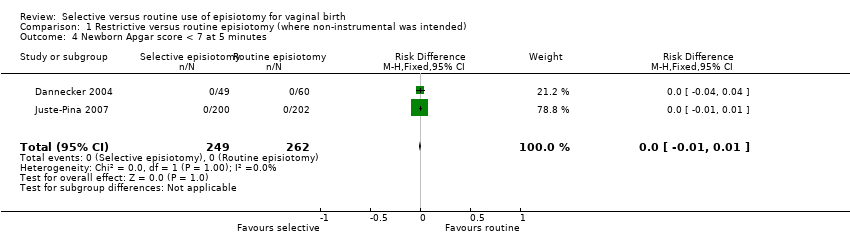 Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 4 Newborn Apgar score < 7 at 5 minutes. | ||||
| 5 Perineal infection Show forest plot | 3 | 1467 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.45, 1.82] |
| Analysis 1.5  Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 5 Perineal infection. | ||||
| 6 Moderate or severe pain (visual analogue scale) Show forest plot | 1 | 165 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.48, 1.05] |
| Analysis 1.6  Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 6 Moderate or severe pain (visual analogue scale). | ||||
| 7 Dyspareunia long term (≥ 6 m) Show forest plot | 3 | 1107 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.84, 1.53] |
| Analysis 1.7  Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 7 Dyspareunia long term (≥ 6 m). | ||||
| 8 Genital prolapse long term (≥ 6 m) Show forest plot | 1 | 365 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.06, 1.41] |
| Analysis 1.8  Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 8 Genital prolapse long term (≥ 6 m). | ||||
| 9 Urinary incontinence long term (≥ 6 m) Show forest plot | 3 | 1107 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.67, 1.44] |
| Analysis 1.9  Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 9 Urinary incontinence long term (≥ 6 m). | ||||
| 10 Need for perineal suturing Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 1.10  Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 10 Need for perineal suturing. | ||||
| 11 Admission to special care baby unit Show forest plot | 5 | 2471 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.56, 1.07] |
| Analysis 1.11 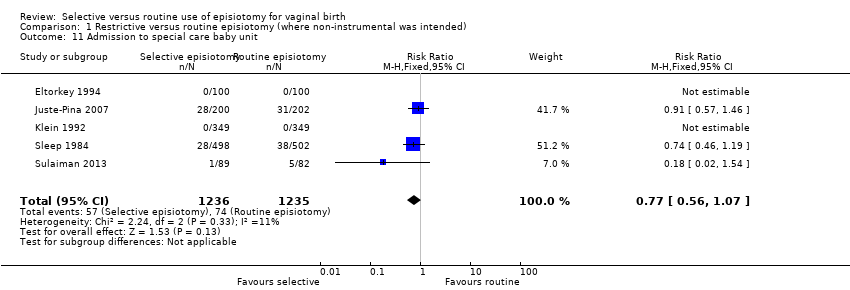 Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 11 Admission to special care baby unit. | ||||
| 12 Pain at different time points (any measure) Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.12  Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 12 Pain at different time points (any measure). | ||||
| 12.1 Any perineal pain at discharge | 2 | 2587 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.25, 2.86] |
| 12.2 Any pain at 10 days | 1 | 885 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.78, 1.27] |
| 12.3 Moderate‐severe pain in first 10 days | 3 | 1127 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.61, 2.12] |
| 12.4 Severe or moderate pain at 3 months postpartum | 1 | 895 | Risk Ratio (M‐H, Random, 95% CI) | 1.51 [0.65, 3.49] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe perineal/vaginal trauma Show forest plot | 11 | 6177 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.52, 0.94] |
| Analysis 2.1  Comparison 2 Restrictive versus routine episiotomy (non‐instrumental, subgroup by parity), Outcome 1 Severe perineal/vaginal trauma. | ||||
| 1.1 Primiparae | 11 | 4137 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.50, 0.93] |
| 1.2 Multiparae | 4 | 2040 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.35, 2.01] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe vaginal/perineal trauma Show forest plot | 10 | 5977 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.52, 0.94] |
| Analysis 3.1  Comparison 3 Restrictive versus routine episiotomy (non‐instrumental, subgroup midline‐midlateral), Outcome 1 Severe vaginal/perineal trauma. | ||||
| 1.1 Midline | 2 | 1143 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.51, 1.07] |
| 1.2 Mediolateral | 8 | 4834 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.37, 1.04] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
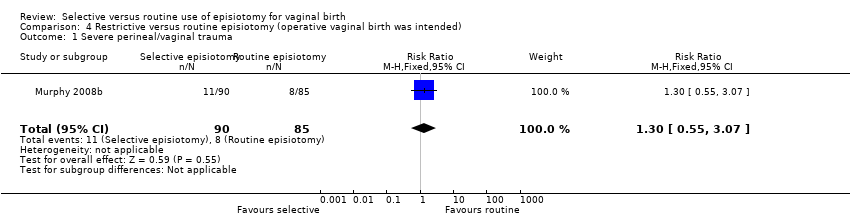
| 1 Severe perineal/vaginal trauma Show forest plot | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.55, 3.07] |
| Analysis 4.1 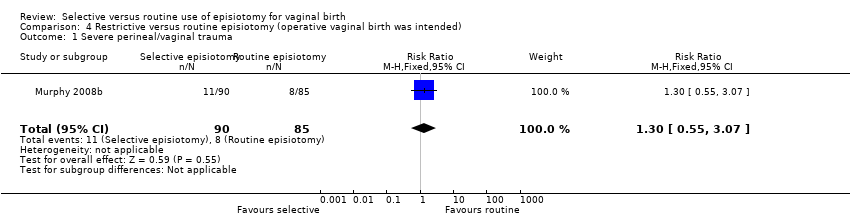 Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 1 Severe perineal/vaginal trauma. | ||||
| 2 Apgar < 7 at 5 minutes Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.2  Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 2 Apgar < 7 at 5 minutes. | ||||
| 3 Perineal infection Show forest plot | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.04, 5.11] |
| Analysis 4.3  Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 3 Perineal infection. | ||||
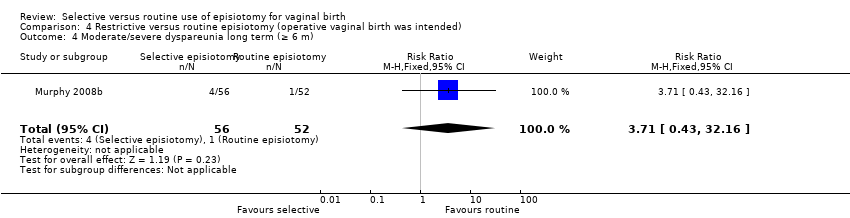
| 4 Moderate/severe dyspareunia long term (≥ 6 m) Show forest plot | 1 | 108 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.71 [0.43, 32.16] |
| Analysis 4.4 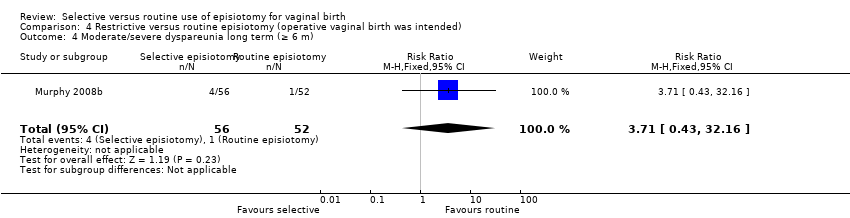 Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 4 Moderate/severe dyspareunia long term (≥ 6 m). | ||||
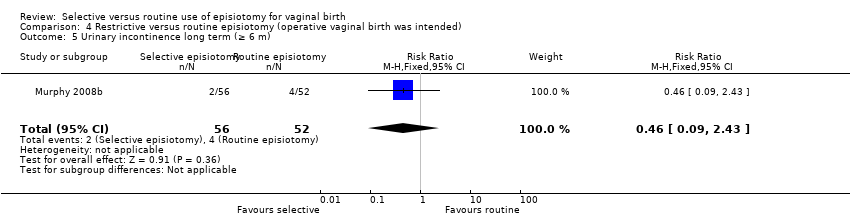
| 5 Urinary incontinence long term (≥ 6 m) Show forest plot | 1 | 108 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.09, 2.43] |
| Analysis 4.5 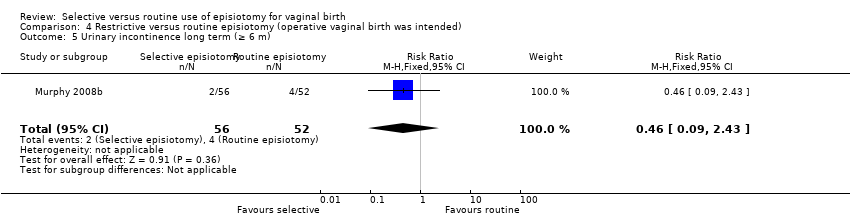 Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 5 Urinary incontinence long term (≥ 6 m). | ||||
| 6 Admission to special care baby unit Show forest plot | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.13 [0.68, 6.64] |
| Analysis 4.6  Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 6 Admission to special care baby unit. | ||||

The rationale commonly used to justify routine episiotomy

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
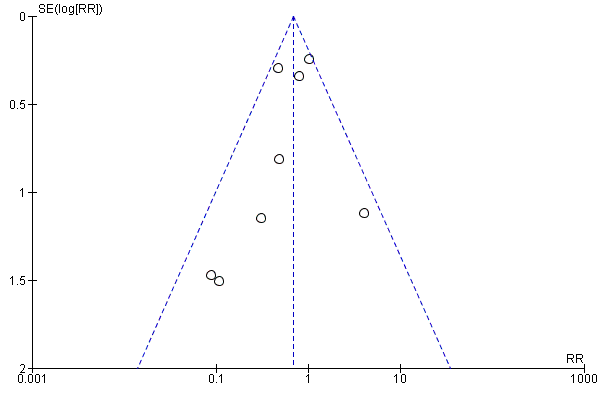
Funnel plot of comparison: 1 Restrictive versus routine episiotomy (planned non‐instrumental), outcome: 1.1 Severe perineal/vaginal trauma

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 1 Severe perineal/vaginal trauma.

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 2 Severe perineal/vaginal trauma (grouped by trial implementation success).

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 3 Blood loss at delivery (mL).
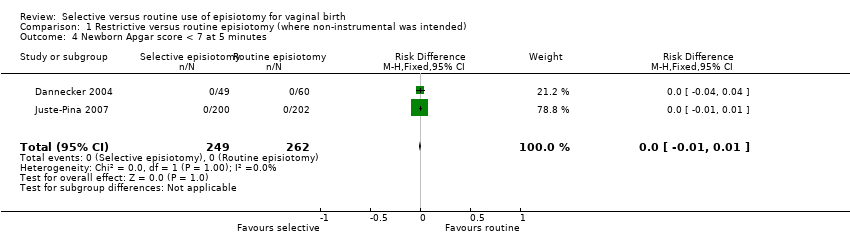
Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 4 Newborn Apgar score < 7 at 5 minutes.

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 5 Perineal infection.

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 6 Moderate or severe pain (visual analogue scale).

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 7 Dyspareunia long term (≥ 6 m).

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 8 Genital prolapse long term (≥ 6 m).

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 9 Urinary incontinence long term (≥ 6 m).

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 10 Need for perineal suturing.
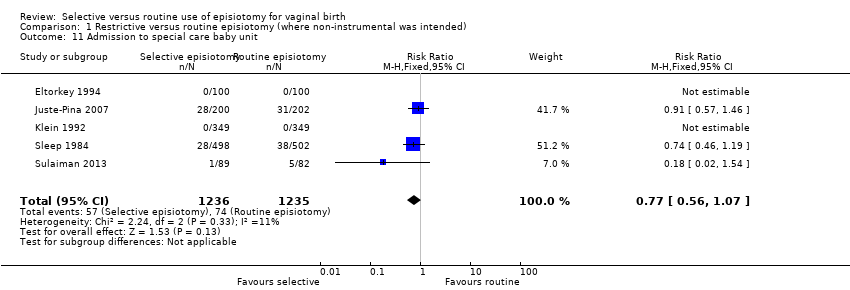
Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 11 Admission to special care baby unit.

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 12 Pain at different time points (any measure).

Comparison 2 Restrictive versus routine episiotomy (non‐instrumental, subgroup by parity), Outcome 1 Severe perineal/vaginal trauma.

Comparison 3 Restrictive versus routine episiotomy (non‐instrumental, subgroup midline‐midlateral), Outcome 1 Severe vaginal/perineal trauma.
Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 1 Severe perineal/vaginal trauma.

Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 2 Apgar < 7 at 5 minutes.

Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 3 Perineal infection.
Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 4 Moderate/severe dyspareunia long term (≥ 6 m).
Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 5 Urinary incontinence long term (≥ 6 m).

Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 6 Admission to special care baby unit.
| Selective versus routine episiotomy: all vaginal births where operative vaginal delivery was not anticipated | ||||||
| Patient or population: Women in labour where operative delivery was not anticipated. (Women were above 16 years old and between 28 gestational weeks and full term, with a live singleton fetus, without severe medical or psychiatric conditions, and had vaginal birth.) Intervention: Selective episiotomy (episiotomy rates in the selective group ranged from 8% to 59%). Comparison: Routine episiotomy (episiotomy rates in the routine group ranged from 61% to 100%; episiotomy rate differences between the groups within trials varied from 21% to 91%). | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with routine episiotomy | Risk with selective episiotomy | |||||
| Severe perineal/vaginal trauma | 3.6 per 100 | 2.5 per 100 | RR 0.70 | 5375 | ⊕⊕⊝⊝ due to imprecision and inconsistency | Selective episiotomy compared to routine may reduce severe perineal/vaginal trauma |
| Blood loss at delivery | The mean blood loss at delivery was 278 mL | 27 mL less (95% CI from 75 mL less to 20 mL more) | 336 | ⊕⊝⊝⊝ very low4,5,6 due to risk of bias, imprecision and inconsistency | We do not know if selective episiotomy compared to routine affects blood loss at delivery | |
| Babies with newborn Apgar score < 7 at 5 minutes | 0 per 100 | 0 per 100 | no events | 501 | ⊕⊕⊕⊝ moderate7,8 Due to imprecision | Both selective episiotomy and routine probably has little or no effect on Apgar < 7 at 5 minutes |
| Perineal infection | 2 per 100 | 2 per 100 | RR 0.90 | 1467 | ⊕⊕⊝⊝ Due to imprecision | Selective episiotomy compared to routine may result in little or no difference in perineal infection |
| Women with moderate or severe pain (measured by visual analogue scale) | 45.1 per 100 | 32 per 100 | RR 0.71 | 165 | ⊕⊝⊝⊝ Due to imprecision and indirectness | We do not know if selective episiotomy compared to routine results in fewer women with moderate or severe perineal pain |
| Women with long‐term dyspareunia (≥ 6 months) | 12.9 per 100 | 14.8 per 100 | RR 1.14 | 1107 | ⊕⊕⊕⊝ Due to imprecision | Selective episiotomy compared to routine probably results in little or no difference in women with dyspareunia at > 6 months |
| Women with long‐term urinary incontinence (≥ 6 months) | 32.2 per 100 | 31 per 100 | RR 0.98 | 1107 | ⊕⊕⊝⊝ Due to risk of bias and imprecision | Selective episiotomy compared to routine results may have little or no difference in the number of women with urinary incontinence > 6 months |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded by 1 for imprecision: confidence intervals range from no important difference to large difference. | ||||||
| Trial | Primigravidae | Follow‐up | |||
| N | per cent (%) | Immediate (< 1 month) | Short‐term (1‐6 months) | Long‐term (≥ 6 months) | |
| 200 | 100 | Discharge & day 7 | No data | No data | |
| 1555/2606 | 60a | Discharge & day 7 | No data | No data | |
| 146 | 100 | Discharge | Several months | A mean follow‐up time of 7.3 months (SD 3.4) | |
| 200 | 100 | Delivery only | No data | No data | |
| 181 | 100 | 4 days | 6 weeks | No data | |
| 98/165 | 59 | 3 days | 3 months | No data | |
| 402 | 100 | No data | 3 months | 3 years 365/402 (91%) | |
| 356/703 | 51 | Discharge | 3 months | No data | |
| 200 | 100 | Discharge | 6 weeks | 1 year | |
| 446 | 100 | Delivery only | N | No data | |
| 420/1000 | 42 | 2 & 10 days | 3 months | 3 years | |
| 209 | 100 | Delivery only | No data | No data | |
| aStratified analysis (primary outcome only) | |||||
| Trial | Selective | Routine | Difference (%) | ||
| n/N | % | n/N | % | ||
| 124/349 | 36 | 198/349 | 57 | 21 | |
| 118/200 | 59 | 169/202 | 84 | 25 | |
| 53/100 | 53 | 83/100 | 83 | 30 | |
| 20/49 | 41 | 46/60 | 77 | 36 | |
| 51/498 | 10 | 258/502 | 51 | 41 | |
| 17/94 | 18 | 49/71 | 69 | 51 | |
| 391/1298 | 30 | 1080/1308 | 83 | 53 | |
| 39/89 | 44 | 82/82 | 100 | 56 | |
| 32/100 | 32 | 100/100 | 100 | 68 | |
| 54/222 | 24 | 223/223 | 100 | 76 | |
| 7/92 | 8 | 89/89 | 100 | 92 | |
| Trial | OVD Included In trial | Total | Included in analysis | Intervention | Control |
| Y | 56/2599 | Y | 24/1302 | 32/1297 | |
| Y | 13/109 | Y | 4/49 | 9/60 | |
| Y | 9/200 | Y | 4/100 | 5/100 | |
| Y | Unknown | Y | 4/92 | Unknown | |
| Y | 20/165 | Y | 10/94 | 10/71 | |
| Unclear | / | / | / | / | |
| Y | 20/703 | Y | Unknown | Unknown | |
| ALL | 200/200 | 101/101 | 99/99 | ||
| Y | 7/445 | Y | 3/222 | 4/223 | |
| Unknown | / | / | / | / | |
| Ali 2004 | Unknown | / | / | / | / |
| Unclear | / | / | / | / |
| Trial | Primary outcome | Outcome related to review primary outcome | Description | Match? |
| Severe perineal trauma | Same | "Extension through the anal sphincter and/or the anal or rectal mucosa (3rd or 4th degree lacerations)" | Matches | |
| Severe perineal trauma | Same | Severe perineal trauma (3rd and 4th degree tear) | Matches | |
| Not specified | Severe perineal trauma | "extension through the anal sphincter or rectal mucosa" | Matches | |
| Not specified | Third‐degree tear | "complete tear including the anal sphincter" | Matches | |
| Not specified | Third‐degree tear | "a complete tear including the anal sphincter, usually extending 2 cm or more up the anal canal" | Matches | |
| Not specified | Third‐degree tear | "one in which the anal sphincter was involved" | Matches | |
| Not specified | Serious case of perineal trauma | "third or fourth degree tear" | Matches | |
| Not specified | Third‐ or fourth‐degree tear | As stated | Matches | |
| Third‐/fourth‐degree tear | Same | Extensive perineal tearing involving the anal sphincter | Matches | |
| Severe laceration to perineal tissues | Same | Third‐degree laceration when the extent of the lesion including the external anal sphincter totally or partially and 4th degree laceration when the rectal mucosa was involved | Matches | |
| Not known | Severe maternal trauma | Extension through the anal sphincter or to the rectal mucosa or to the upper 3rd of the vagina | Matches | |
| Obstetrical anal sphincter injuries | 3rd/4th degree | No further details given | Matches | |
| aMurphy included only women where operative delivery was anticipated and this is described and analysed separately. | ||||
| Trial | Parity | Time assessed | Outcome | Selective n/N (%) | Routine n/N (%) |
| All parities | day 3 | Moderate and severe pain (defined by score categories) | 30/94 (32%) | 32/71 (45%) | |
| Primigravida | day 2 | Average score | Score 1.4, SD 0.8 (N 150) | Score 1.3, SD 0.7 (N 156) | |
| Multigravida | day 2 | Average score | Score 0.9, SD 0.8 (N 156) | Score 0.9, SD 0.7 (N 145) | |
| Primigravida | 1‐5 days | Average score | Score 51, SD 25, 22 (N 49) | Score 69, SD 23, 31 (N 60) |
| Trial | Parameter measured | Collection | Selective n/N (%) | Routine n/N (%) |
| Pain during sex in the last 4 weeks | Questionnaire. Follow up average time of 7.3 months in about 65% of those randomised. | 6/29 (21%) | 13/39 (33%) | |
| Dyspareunia at 3 months; and pain with coitus at 3 years postpartum | Telephone survey 3 months postpartum and interview by telephone at 3 years postpartum. Loss to follow up was 6% in the selective, 5% in the routine group at 3 months; and 8% in the selective, 11% in the routine group at 3 years postpartum. | 3 months postpartum: 42/189 (22%) 3 years postpartum: 20/185 (11%) | 3 months postpartum:67/192 (35%) 3 years postpartum: 15/180 (8%) | |
| Not reported | Collected but not reported | NA | NA | |
| Reported dyspareunia at 3 months postpartum | Self administered postal questionnaire. Follow up rate 66% in selective, and 69% in routine at 3 years postpartum. | 3 months postpartum: 87/394 (22%) 3 years postpartum: 52/329 (16%) | 3 months postpartum: 74/411 (18%) 3 years postpartum: 45/345 (13%) |
| Trial | Parameter measured | Collection | Selective n/N (%) | Routine n/N (%) |
| Urinary incontinence was considered as present whenever a participant gave an answer other than 'never' when replying to "How often do you leak urine involuntarily?" | Questionnaire. Follow‐up average time of 7.3 months in about 65% of those randomised | 13/27 (48%) | 11/41 (27%) | |
| Urinary incontinence at 3 years postpartum | Telephone survey 3 years postpartum. Loss to follow‐up was 8% in the selective, 11% in the routine group at 3 years postpartum | 34/180 (19%) | 49/185 (26%) | |
| Urinary incontinence at 3 months | Questions employing a 4‐point scale | 57/337 (17%) | 60/337 (18%) | |
| Reported urinary incontinence at 3 months after delivery; Reported incontinence of urine at 3 years postpartum | Standardised postal questionnaire administered by mothers at 3 months and 3 years postpartum. Follow‐up rate 62% in selective, and 67% in routine at 3 months postpartum; follow‐up rate 66% in selective, and 69% in routine at 3 years postpartum | 3 months postpartum: 83/438 (19%) 3 years postpartum: 112/329 (34%) | 3 months postpartum: 87/457 (19%) 3 years postpartum: 124/345 (36%) |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe perineal/vaginal trauma Show forest plot | 11 | 6177 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.52, 0.94] |
| 2 Severe perineal/vaginal trauma (grouped by trial implementation success) Show forest plot | 11 | 6177 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.52, 0.94] |
| 2.1 Difference in episiotomy rate < 30% | 3 | 1300 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.63, 1.69] |
| 2.2 Difference in episiotomy rate 30% + | 8 | 4877 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.38, 0.81] |
| 3 Blood loss at delivery (mL) Show forest plot | 2 | 336 | Mean Difference (IV, Random, 95% CI) | ‐27.16 [‐74.80, 20.49] |
| 4 Newborn Apgar score < 7 at 5 minutes Show forest plot | 2 | 511 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.01, 0.01] |
| 5 Perineal infection Show forest plot | 3 | 1467 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.45, 1.82] |
| 6 Moderate or severe pain (visual analogue scale) Show forest plot | 1 | 165 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.48, 1.05] |
| 7 Dyspareunia long term (≥ 6 m) Show forest plot | 3 | 1107 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.84, 1.53] |
| 8 Genital prolapse long term (≥ 6 m) Show forest plot | 1 | 365 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.06, 1.41] |
| 9 Urinary incontinence long term (≥ 6 m) Show forest plot | 3 | 1107 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.67, 1.44] |
| 10 Need for perineal suturing Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 11 Admission to special care baby unit Show forest plot | 5 | 2471 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.56, 1.07] |
| 12 Pain at different time points (any measure) Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 12.1 Any perineal pain at discharge | 2 | 2587 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.25, 2.86] |
| 12.2 Any pain at 10 days | 1 | 885 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.78, 1.27] |
| 12.3 Moderate‐severe pain in first 10 days | 3 | 1127 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.61, 2.12] |
| 12.4 Severe or moderate pain at 3 months postpartum | 1 | 895 | Risk Ratio (M‐H, Random, 95% CI) | 1.51 [0.65, 3.49] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe perineal/vaginal trauma Show forest plot | 11 | 6177 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.52, 0.94] |
| 1.1 Primiparae | 11 | 4137 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.50, 0.93] |
| 1.2 Multiparae | 4 | 2040 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.35, 2.01] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe vaginal/perineal trauma Show forest plot | 10 | 5977 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.52, 0.94] |
| 1.1 Midline | 2 | 1143 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.51, 1.07] |
| 1.2 Mediolateral | 8 | 4834 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.37, 1.04] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe perineal/vaginal trauma Show forest plot | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.55, 3.07] |
| 2 Apgar < 7 at 5 minutes Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3 Perineal infection Show forest plot | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.04, 5.11] |
| 4 Moderate/severe dyspareunia long term (≥ 6 m) Show forest plot | 1 | 108 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.71 [0.43, 32.16] |
| 5 Urinary incontinence long term (≥ 6 m) Show forest plot | 1 | 108 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.09, 2.43] |
| 6 Admission to special care baby unit Show forest plot | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.13 [0.68, 6.64] |


