Planificación anticipada de la atención para adultos con insuficiencia cardíaca
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Study design: individual RCT (pair of patients and surrogates) Total duration of study: not reported Number of study centres and location: 1 centre (2 clinics and 1 dialysis unit)/La Crosse, WI Study setting: clinic and renal dialysis unit, a 325‐bed clinically affiliated organisation Date of study: not reported | |
| Participants | Randomised (n): 27 pairs of patients and surrogates (intervention: 13 pairs (CHF: 4; ESRD: 5; pre‐OHS: 4); control: 14 pairs (CHF: 5; ESRD: 5; OHS: 4)) Lost to follow‐up/withdrawn from studies (n): 0 withdrawals Analysed (n): intervention: 13 pairs (CHF: 4; ESRD: 5; OHS: 4); control: 14 pairs (CHF: 5; ESRD: 5; OHS: 4) Mean age (years): all patients: 68.7; all surrogates: 50 Age range: not reported Gender (n and % men): intervention: 5 (38.5%) in patients, 3 (23.1%) in surrogates; control: 11 (78.6%) in patients, 4 (28.6%) in surrogates Severity of condition and diagnostic criteria: not reported Inclusion criteria:
Exclusion criteria: not reported | |
| Interventions | Intervention: patients and their surrogates participated in scheduled 1‐hour PC‐ACP interview implemented by experienced advance care planning facilitator. Interview consisted of 5 stages. Comparison: participants were approached on admission and asked if they had an advance directive or if they would like more information (or both). They were given an information card describing their right to have an advance directive and materials that explained the process of advance care planning and completion of an advance directive if they desired. Referrals were made to trained advance care planning facilitators for additional discussion and assistance. Completed advance directive documents were placed in a specific place in the medical record as determined by organisational policy. | |
| Outcomes | Primary outcomes and time points: planned outcomes not reported Secondary outcomes and time points:
Adverse outcomes: not reported | |
| Notes | Funding for trial: not reported Notable conflicts of interest of trial authors: not reported We contacted the trialists for further details of study data, and received the data regarding quality of communication. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "…Systematic assignment was used within disease categories by alternating group assignment after assignment of the first patient‐surrogate pair was randomly determined by flipping a coin…" Comment: study generated random sequence generation by alternating group assignment. Only allocation of the first patient–surrogate pair was determined by coin tossing. |
| Allocation concealment (selection bias) | High risk | Quote: "alternating group assignment." Personnel may have been able to predict participants' allocation. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Intervention was PC‐ACP interview, and participants may have been able to know their allocation. However, details of interventionist were not reported. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Outcome measures included self‐reported outcome, and participants may have been able to know allocation. However, uncertain whether investigators were aware of assignment. |
| Incomplete outcome data (attrition bias) | Low risk | No withdrawals in either groups. |
| Selective reporting (reporting bias) | Low risk | Study protocol and trial register were not reported; all outcomes listed in the 'Methods' section of the study were reported in the 'Results' section. |
| Other bias | Unclear risk | There were more women (61.5%) than men (38.5%) in the intervention group. In the control group, 21.4% were women and 78.6% were men. Unclear whether gender imbalance would affect intervention effects. |
| Methods | Study design: cross‐over RCT Total duration of study: not reported Number of study centres and location: not reported/UK Study setting: participant recruitment undertaken in cardiology, medical and care of hospital wards for elderly people Date of study: screened between 1 October 2013 and 31 September 2014 | |
| Participants | Randomised (n): patients: 50 (intervention: 25; control: 25); carers: 32 (intervention: 19; control: 13). Patients were randomised in 1:1 ratio based on cross‐over design using random permuted blocks to receive either 12 weeks of an FCP at discharge followed by crossover to 12 weeks of usual care (early group) or to receive 12 weeks of usual care followed by crossover to 12 weeks of FCP (delayed group). Lost to follow‐up/withdrawn from studies (n): intervention: 2 participants died after allocation and did not receive intervention, 2 participants lost to follow‐up (1 died, 1 withdrew) at 12 weeks' follow‐up; control: 2 participants withdrew at 12 weeks' follow‐up Analysed (n): intervention: 21 participants were analysed at 12 weeks' follow‐up; control: 23 participants were analysed at 12 weeks' follow‐up Mean age (years): all participants: 81.1 (SD 8.6); intervention: 81.9 (SD 7.1); control: 80.2 (SD 10.0) Age range: not reported Gender (n and % men): intervention: 17 (68%) men; control: 13 (52%) men Severity of condition and diagnostic criteria: not reported (quote: "an unscheduled hospital admission with HF and or ACS based on European Society of Cardiology guidelines"). Inclusion criteria: predicted 12‐month mortality risk ≥ 20% estimated using the GRACE score for ACS and the EFFECT score for HF; people with aortic stenosis who presented with HF Exclusion criteria: moderate/severe dementia; prognosis < 30 days and people already on a palliative care register | |
| Interventions | Intervention: 1. Initial, 1‐hour semi‐structured meeting with trial cardiologist and trial nurse specialists involving patient and their carer; followed by 2 × 1‐hour meetings with trial nurse in patient's home at 6 and 12 weeks. Comparison: usual care | |
| Outcomes | Primary outcome and time point:
Secondary outcome and time point:
Adverse outcomes: not reported | |
| Notes | Funding for trial: Marie Curie Research Notable conflicts of interest of trial authors: authors declared no competing financial interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "1:1 ratio using random permuted blocks" Additional information about block size or how permuted blocks were generated was not described. |
| Allocation concealment (selection bias) | Unclear risk | Details not reported |
| Blinding of participants and personnel (performance bias) | High risk | Trial cardiologist and trial nurse specialists implemented semi‐structured meeting with participants and their carer. |
| Blinding of outcome assessment (detection bias) | High risk | Since the intervention was semi‐structured discussion with trial cardiologist and trial nurse, participants may have been aware of their allocation. Primary outcome, QoL, was subjective self‐reported outcome. |
| Incomplete outcome data (attrition bias) | Low risk | Intervention: 4/25 (16%) participants discontinued at 12 weeks (3 died and 1 withdrew consent); control: 2/25 (8%) participants discontinued at 12 weeks (2 withdrew due to progressive illness). |
| Selective reporting (reporting bias) | Unclear risk | Planned outcomes as prespecified in the trial register record (NCT02302014) were reported. However, we noted that participants' screening and enrolment commenced before trial registry entry. |
| Other bias | Low risk | None identified. |
| Methods | Study design: individual RCT Total duration of study: not reported Number of study centres and location: 7 centres/USA Study setting: teaching hospitals Date of study: enrolment 28 June 2012 to 7 February 2015 | |
| Participants | Randomised (n): 246 (intervention: 123; control: 123) Lost to follow‐up/withdrawn from studies (n): intervention: 50 participants withdrawn at 1 month, and 7 at 3 months; control: 60 participants withdrawn at 1 month, and 11 at 3 months Analysed (n): intervention: 73 participants analysed at 1 month, and 66 at 3 months; control: 63 participants analysed at 1 month, and 52 at 3 months Mean age (years): intervention: 81 (SD 8) at baseline; control: 81 (SD 9) at baseline Age range: not reported Gender (n and % women): intervention: 50 (41%); control: 47 (38%) Severity of condition and diagnostic criteria: intervention: NYHA class II: 2 (2%); NYHA class III: 111 (90%); NYHA class IV: 10 (8%); control: NYHA class II: 0 (0%); NYHA class III: 112 (91%); NYHA class IV: 11 (9%); diagnostic criteria not reported Inclusion criteria:
Exclusion criteria: not an established HF patient, candidate for transplant or mechanical circulatory support, been referred to or enrolled in hospice care, psychiatric illness as determined by physician that would make this study inappropriate; any patient that had been excluded for transplant or circulatory support for psychological or psychiatric comorbidities | |
| Interventions | Intervention:
Comparison: participants listened to a description of the 3 goals of care used in the intervention arm read out loud by the research assistants. | |
| Outcomes | Primary outcomes and time points: planned outcomes that we prespecified for this review not reported Secondary outcomes and time points: planned outcomes that we prespecified for this review not reported Adverse outcomes: not reported | |
| Notes | Funding for trial: the National Heart, Lung, and Blood Institute Notable conflicts of interest of trial authors: Dr Paasche‐Orlow received compensation as a consultant to Nous Foundation, Inc, a not‐for‐profit foundation that disseminates educational videos. Dr Volandes was the President of the not‐for‐profit foundation. Dr Volandes had financial interests in the not‐for‐profit foundation, which were reviewed and managed by Massachusetts General Hospital and Partners HealthCare in accordance with their conflict of interest policies. The other authors reported no conflicts. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "computer‐generated 2:2 block randomization design stratified on the basis of use of an implantable cardioverter‐defibrillator at each institution." |
| Allocation concealment (selection bias) | Low risk | Quote: "assignments concealed in numbered envelopes." |
| Blinding of participants and personnel (performance bias) | High risk | The trained research assistants explained goals of care, and showed a goals‐of‐care video to participants. |
| Blinding of outcome assessment (detection bias) | High risk | Data collection was implemented by trained research assistants. Quote: "data collectors were not blinded to the randomization." |
| Incomplete outcome data (attrition bias) | High risk | In the follow‐up interview at 1 and 3 months after intervention, participants were asked whether they had discussed goals of care with their clinician. In the intervention group, 50 participants (40.7%) lost to follow‐up at 1 month and 57 participants (46.3%) at 3 months. In the control group, 60 participants (48.8%) lost to follow‐up at 1 month and 71 participants (57.7%) at 3 months. Other self‐reported outcomes (patients' goals‐of‐care preferences, CPR and intubation preferences, and patients' knowledge of goals of care) were assessed postintervention, and nobody lost to follow‐up. |
| Selective reporting (reporting bias) | High risk | Not all outcomes that were mentioned in the trial register (NCT01589120) were reported. The outcomes of decisional conflict, QoL, referral to hospice, place of death, and carer bereavement score were not reported. |
| Other bias | Low risk | None identified. |
| Methods | Study design: individual RCT (pair of patients and surrogates) Total duration of study: not reported Number of study centres and location: 2 centres (6 clinics)/La Crosse, Madison and Milwaukee, Wisconsin Study setting: clinics and dialysis units Date of study: recruited from 1 January 2004 to 31 July 2007 | |
| Participants | Randomised (n): all participants: 338 (intervention: 164 pairs of patients and surrogates; control: 174 pairs of patients and surrogates); CHF: 197 pairs (intervention: 93 pairs; control: 104 pairs) Lost to follow‐up/withdrawn from studies (n): all participants (intervention: 2 patients died, 2 participants withdrawn; control: 21 participants withdrawn), CHF (intervention: 2 patients died, 1 participant withdrawn; control: 15 participants withdrawn) Analysed (n): all participants (intervention:160 pairs; control: 153 pairs), CHF (intervention: 90 pairs; control: 89 pairs) Mean age (years): intervention: 71.4 (all patients), 59.5 (surrogates); control: 70.6 (all patients), 57.4 (surrogates) Age range (years): 37–93 (all patients) Gender (n and % men): intervention: 96 (60.0%) patients, and 43 (26.9%) surrogates; control: 89 (58.2%) patients, 41 (26.8%) surrogates (all participants) Severity of condition and diagnostic criteria: not reported Inclusion criteria: patients receiving medical care but had clinical symptoms and signs that indicated a risk of serious complication or death in next 2 years; NYHA II, III, or IV; patients with ESRD had serum albumin < 3.7 g/dL and comorbidity such as diabetes mellitus, CHF, COPD, history of acute myocardial infarction, or above‐the‐knee amputation; aged ≥ 18 years; had decision‐making capacity; able to speak and understand English Exclusion criteria: not reported | |
| Interventions | Intervention: trained facilitator implemented PC‐ACP interview. Purposes of interview were to assess patient's and surrogate's understanding of patient's illness, experiences, hopes, fears, and concerns; to provide individualised information about disease‐specific treatment choices and their benefit and burdens; to assist in documentation of disease‐specific goals of care; and to prepare surrogate to understand the patient's choices and make future decisions to honour these choices. Interview consisted of 5 stages. Comparison: all patients received care provided by their local health organisation for the completion of ADs. For the La Crosse centre, usual care included ACP facilitation with patient but not the indepth, patient‐centred intervention in the presence of the surrogate decision‐maker. For all sites, usual care included standard AD counselling, assessment of an AD on admission to the organisation, and questions as to whether they would like more information | |
| Outcomes | Primary outcomes and time points:
2 reviewers blinded to group allocation determined what treatment the patient received. Patients identified previously whether they want to receive treatment in the situation of a low chance of survival. Then, the treatment was compared with patients' preferences of treatment. Secondary outcomes and time points:
Adverse outcomes: not reported | |
| Notes | Funding for trial: Agency of Health Care Research and Quality, the Clinical and Translational Science Award (CTSA) program of the National Center for Research Resources, National Institutes of Health Notable conflicts of interest of trial authors: Dr Kirchhoff received Agency of Health Care Research and Quality award. Dr Hammes and Ms Briggs were employed by the Gundersen Lutheran Medical Foundation, Inc. which owns the rights to the Respecting Choices programme, of which the intervention used in the current study, Disease‐Specific Advance Care Planning, was part. Dr Kehl was supported by the Clinical and Translational Science Award program of the National Center for Research Resources, National Institutes of Health, during the final year of this project. Dr Brown had no conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "the allocation sequence using a computerized random number generator." |
| Allocation concealment (selection bias) | Low risk | Quote: "using the sealed‐envelope method within each setting and disease condition." |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "the PC‐ACP facilitator was not blinded to group assignment." Intervention was PC‐ACP interview, therefore, participants were not blinded to investigators. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Since the intervention was structured interview, participants may have been aware of their allocation. For outcomes of concordance between participants' preferences and end‐of‐life care after patients' death (quote): "two reviewers blinded to group determined what treatment the patient received". Other details of outcome assessors not reported. |
| Incomplete outcome data (attrition bias) | High risk | For participants with HF in the intervention group, 2 participants died and there was 1 withdrawal/refusal by surrogate carers. In the control group, 15 participants withdrew or refused by surrogate carers. More participants in the control group withdrew or refused, and there was an imbalance of the reason and the number of lost to follow‐up between groups. |
| Selective reporting (reporting bias) | Unclear risk | The efficacy of PC‐ACP was mentioned in the trial register (NCT00204802) as the primary outcome. The details of outcome measures were not mentioned in the trial register. |
| Other bias | Low risk | None identified |
| Methods | Study design: individual RCT Total duration of study: not reported Number of study centres and location: not reported/Houston (TX) Study setting: Veterans Affairs Medical Center Date of study: not reported | |
| Participants | Randomised (n): all participants: 120 (intervention: 60; control: 60) Lost to follow‐up/withdrawn from studies (n): intervention: 3 participants; control: 0 withdrawn Analysed (n): all participants: 117 (intervention: 57; control: 60); CHF: 53 (intervention: 28; control: 25) Mean age (years): intervention: 66.4; control: 68.4 Age range (years): intervention: 55–85; control: 56–84 Gender: all men Severity of condition and diagnostic criteria: CHF; ejection fraction < 25%/diagnostic criteria not reported Inclusion criteria: CHF with an ejection fraction < 25% and ≥ 1 previous hospitalisation; COPD/emphysema, requiring mechanical ventilation, with ≥ 2 previous hospitalisations; chronic liver disease with cirrhosis and ascites; any metastatic solid tumour (e.g. colon carcinoma with liver metastases) and non‐small‐cell lung cancer, stage IIIb or IV; ESRD on haemodialysis Exclusion criteria: dementia (Mini‐Mental State Examination score ≤ 24, diagnosis of dementia listed in the patients' chart) | |
| Interventions | Intervention: received explicit verbal instructions to use the values inventory as a starting point for future care planning with their physician during their visit and explicit instructions to discuss the values inventory at the beginning of the visit. A values inventory (VI) is a tool used in self‐assessment that allows patients to rate different values according to their relative importance. It gives the treating physician information about what is important to the patient and can thus be used as a discussion aid about ACP Comparison: usual care | |
| Outcomes | Primary outcomes and time points: planned outcomes that we prespecified for this review not reported Secondary outcomes and time points: planned outcomes that we prespecified for this review not reported Adverse outcomes: not reported | |
| Notes | Funding for trial: Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service, grant IIR‐02‐224 Notable conflicts of interest of trial authors: quote: "Neither the principal investigator nor any coauthors have any conflicts of interest." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 6 participants in each clinical department were randomised using a simple random number table, and 120 participants were randomised as a whole. |
| Allocation concealment (selection bias) | Unclear risk | Details not reported. |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "Physicians were not blinded to patients' assignments, but they did not know a priori if the patient had been assigned to the VI [value inventory] or usual‐care group at the outset of the encounter." A value inventory (VI) which intervention group used was a self‐assessment tool, and it was used as a discussion about ACP. Participants was supported to show their physician the VI and discuss ACP. Therefore, personnel were able to aware which participants allocated eventually. |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "All patient–physician encounters were audiotaped with a small and unobtrusive boundary microphone." This audiotaped data was analysed. Therefore, investigators will be able to anticipate which group participants were allocated. |
| Incomplete outcome data (attrition bias) | Low risk | In the intervention group, 3/60 (5%) participants withdrew. In the control group, 0 withdrew. |
| Selective reporting (reporting bias) | Low risk | Outcomes mentioned in trial register (NCT00122135) were reported. |
| Other bias | Unclear risk | Physicians' characteristics and experience who provided end‐of‐life discussion not reported. Physicians' characteristics may have affected the contents of end‐of life discussion. |
| Methods | Study design: individual RCT (pair of patients and surrogates) Total duration of study: not reported Number of study centres and location: 1 centre/North Carolina Study setting: academic medical centre Date of study: recruited from November 2014 to June 2015 | |
| Participants | Randomised (n): 29 pairs of patients and surrogates (intervention: 14 pairs; control: 15 pairs) Lost to follow‐up/withdrawn from studies (n): 0 lost to follow‐up Analysed (n): 29 pairs (intervention: 14 pairs; control: 15 pairs) Mean age (years): intervention: 62.6 (SD 7.6) (patients), 56.2 (SD 12.4) (surrogates); control: 62.3 (SD 12.3) (patients), 56.5 (SD 17.6) (surrogates) Age range (years): intervention: 44–74 (patients), surrogates not reported; control: 43–85 (patients), 28–85 (surrogates) Gender( n and % men): intervention: 11 (78.6%) patients, 2 (14.3%) surrogates; control: 9 (60.0%) patients, 2 (13.3%) surrogates Severity of condition and diagnostic criteria: not reported (intervention: 3 were bridge to transplant, 11 were destination therapy; control: 5 were bridge to transplant, 10 were destination therapy) Inclusion criteria: English‐speaking adults, ≥ 30 days post‐LVAD placement and medically stable; had access to telephone, and had a willing surrogate to participate in study with the patient. Surrogates were English‐speaking adults with access to a telephone Exclusion criteria: people hospitalised in critical condition | |
| Interventions | Intervention: usual care + SPIRIT‐HF. SPIRIT‐HF was a structured, guided discussion, delivered by a trained interventionist in a single, approximately 1‐hour session. 5 steps: 1. assessing representations; 2. identifying gaps and concerns; 3. creating conditions for conceptual change; 4. introducing replacement information; 5. setting goals, planning, and summarising. During SPIRIT‐HF, interventionist gained an understanding of the patient's experiences, thoughts, attitudes, and beliefs, related to his/her HF and LVAD, which in turn, facilitated the delivery of targeted, individualised information. Patient was given opportunity to consider his/her values and preferences related to end‐of‐life care. The inclusion of the surrogate ensured that surrogate had an opportunity to learn about patient's illness experiences, and end‐of‐life concerns, and to prepare for the role of surrogate decision‐maker. Participants were provided a copy of the Goals of Care used during the discussion, a written summary of the discussion, and information on resources regarding advance directives. Comparison: usual care, which consisted of a pre‐VAD evaluation by clinicians in psychology, social work, nutrition, nursing, cardiology, and cardiac surgery. Information about advance directives was provided during the LVAD evaluation. However, palliative care consultations and ACP discussions were not routinely part of usual care | |
| Outcomes | Primary outcomes and time points: planned outcomes that we prespecified for this review were not reported Secondary outcomes and time points:
Adverse outcomes: not reported | |
| Notes | Funding for trial: Sigma Theta Tau International/Hospice and Palliative Nurses 2014 Foundation End of Life Nursing Care Research Grant; National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award; Sigma Theta Tau International, Alpha Chapter Postdoc Award Notable conflicts of interest of trial authors: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "using a computer‐generated random scheme." |
| Allocation concealment (selection bias) | Low risk | Quote: "The interventionist was blinded to group assignment until she opened a sequentially numbered opaque envelope containing the enrolled dyad's assignment." |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "The interventionist was blinded to group assignment until she opened a sequentially numbered opaque envelope containing the enrolled dyad's assignment." The intervention was a 5‐step discussion between interventionist and participants. Neither the participants nor the study personnel were blinded. |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "A trained research assistant (not the interventionist) assessed all outcomes by telephone." Since the intervention was a structured interview delivered by interventionist and outcomes were assessed by research assistant, it is likely that they were aware of the type of intervention allocation. Participants' decisional conflict assessed using subjective self‐reported questionnaire. |
| Incomplete outcome data (attrition bias) | Low risk | No missing data in either group. |
| Selective reporting (reporting bias) | Low risk | Study protocol and trial register were not reported; all outcomes listed in the 'Methods' section of the study were reported in the 'Results' section. |
| Other bias | Low risk | None identified |
| Methods | Study design: individual RCT Total duration of study: not reported Number of study centres and location: 1 centre/Boston (MA) Study setting: hospital Date of study: recruited from September 2014 to December 2015, analyses began in July 2016 | |
| Participants | Randomised (n): 50 (intervention: 26; control: 24) Lost to follow‐up/withdrawn from studies (n): intervention: 10 participants died; control: 9 participants died Analysed (n): outcome of documentation of AC preferences (intervention: 26; control: 24); outcomes of QoL and depression (intervention: 16; control: 15) Mean age (years): intervention: 74.7 (SD 11.2); control: 69.2 (SD 10.2) Age range: not reported Gender (n and % men): intervention: 14 (53.9%); control: 15 (62.5%) Severity of condition (n and %) and diagnostic criteria: intervention: 16 (61.5%) were NYHA III or IV; control: 16 (66.7%) were NYHA III or IV/diagnostic criteria not reported Inclusion criteria: symptomatic HF (NYHA II‐IV); ≥ 1 risk factor for poor prognosis from following: prior hospitalisation for HF within 1 year, aged ≥ 80 years, chronic kidney disease (estimated GFR ≤ 45 mL/min/m2), systolic blood pressure ≤ 100 mmHg, serum sodium ≤ 130 meq/L, cardiogenic shock (Cardiac Index ≤ 2.0), serious non‐cardiovascular Illness (e.g. advanced stage cancer, COPD); ability to provide informed consent; permission of attending physician Exclusion criteria: anticipated major cardiac surgery, including VAD or transplant, within 3 months of enrolment; already enrolled in hospice or receiving outpatient palliative care | |
| Interventions | Intervention: social worker‐led intervention began as a structured goals of care conversation. Conversation prepared the patient for future decisions and solicit permission to proceed; assessed prognostic understanding and preferences regarding receipt of prognostic information; discussed prognosis and its implications for decision‐making; explored key topics including patient goals and priorities, fears and worries, sources of strength, perceived critical abilities, tradeoffs between length and QoL, and family awareness of preferences and prognosis; and summarised impressions and recommendations. All patients were reviewed with a palliative care physician who provided guidance regarding strategies for facilitation of further discussions and directed specific interventions (formal palliative care physician consultation, Medical Orders for Life Sustaining Treatment, hospice referral, etc.) where indicated. Social worker then contacted the patient by telephone or during subsequent scheduled clinic visits over the 6‐month follow‐up period to further develop the conversation begun with the patient during the initial visit. Comparison: all patients received printed materials containing information about ACP as provided routinely by Brigham and Women's Hospital and the Brigham and Women's Heart Failure guide. Palliative care and advanced planning discussions in these patients were initiated at discretion of treating team. Results of the questionnaires detailed symptoms burden, anxiety, and depression were available to the care team so that additional consultative resources (social work, psychiatry, palliative care) could be deployed as appropriate. | |
| Outcomes | Primary outcome and time points:
Secondary outcomes and time points:
Adverse outcomes: not reported | |
| Notes | Funding for trial: Watkins Discovery Award from Brigham and Women's Hospital, made possible through a philanthropic gift from the E. G. Watkins Family Foundation Notable conflicts of interest of trial authors: no conflicts of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly allocated 1:1 to a structured, social worker–led palliative care intervention or usual care using a permuted block randomization scheme" Comment: additional information about block size or how permuted blocks were generated was not described. |
| Allocation concealment (selection bias) | Low risk | Quote: "All patients were identified and enrolled by the study coordinator, who was blinded to the allocation sequence." |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "Patients allocated to the intervention group received a structured goals of care discussion based on the framework of the Serious Illness Conversation Guide conducted by a social worker (A.E.O.)" Comment: participants were provided the intervention by investigator. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Since the intervention was a structured discussion, participants may have been aware of their allocation. Documentation about advance care preferences were assessed by (quote) "blinded review of the electronic health record by 2 nonstudy clinicians." Other details of outcome assessors not reported. |
| Incomplete outcome data (attrition bias) | High risk | Outcome of documentation of –1 preferences was analysed all participants (n = 50). However, when outcomes of QoL and depression were analysed, 10/26 (38.5%) participants in the intervention group and 9/24 (37.5%) participants in the control group were lost to follow‐up due to participants' death. Although the reasons were balanced across groups, the rate of losses were high. |
| Selective reporting (reporting bias) | Unclear risk | Planned outcomes as indicated in the trial register entry (NCT02805712) were reported. However, participants' recruitment commenced before the trial was registered. |
| Other bias | Low risk | None identified. |
| Methods | Study design: RCT Total duration of study: duration of intervention phase 6 months, but patients in both groups were followed until death or end of the study Number of study centres and location: 1 centre/US Study setting: not reported Date of study: 15 August 2012 to 25 June 2015 | |
| Participants | Randomised (n): 150 (intervention: 75; control: 75) Lost to follow‐up/withdrawals (n): QoL measurement: intervention: 34 lost to follow‐up (23 died) at 6 months; control: 35 lost to follow‐up (20 died) at 6 months. Depressive measurement: intervention: 34 lost to follow‐up (23 died) at 6 months; control: 36 lost to follow‐up (20 died) 6 months Analysed (n): QoL measurement at: 2 weeks: 123 (intervention: 63; control: 60); 6 weeks: 110 (intervention: 53; control: 57); 3 months: 90 (intervention: 47; control: 43); 6 months 81 (intervention: 41; control: 40). Depressive measurement at: 2 weeks: 113 (intervention: 59; control: 54); 3 months: 89 (intervention: 46; control: 43); 6 months: 80 (intervention: 41; control: 39) Mean age (years): intervention: 71.9 (SD 12.4); control: 69.8 (SD 13.4) Age range: not reported Gender (n and % men): intervention: 42 (56.0%); control: 37 (49.3%) Severity of condition (n and %) and diagnostic criteria: intervention: 54 (72.0%) were NYHA III, 15 (20.0%) were NYHA IV; control: 58 (77.3%) were NYHA III, 5 (6.7%) were NYHA IV/diagnostic criteria not reported Inclusion criteria: aged > 18 years, hospitalisation for acute HF (either systolic HF or HF with preserved ejection fraction) or within 2 weeks of discharge of a hospitalisation for acute HF, dyspnoea at rest or minimal exertion plus ≥ 1 sign of volume overload, previous HF hospitalisation within the past 1 year, ESCAPE risk score ≥ 4 indicating 50% predicted 6‐month mortality, anticipated discharge from hospital with anticipated ability to return to outpatient follow‐up appointments, hospitalised with acute HF with signs/symptoms of volume overload who did not meet all other eligibility criteria may also be considered for enrolment if they could be categorised into 1 of the following high‐risk groups.
Exclusion criteria: ACS within 30 days, cardiac resynchronisation therapy within the past 3 months or current plan to implant, active myocarditis, constrictive pericarditis, severe stenotic valvular disease amendable to surgical intervention, anticipated heart transplant or VAD within 6 months, renal replacement therapy, non‐cardiac terminal illness, pregnant or planning to become pregnant, inability to comply with study protocol | |
| Interventions | Intervention: Palliative Care in Heart Failure (PAL‐HF). Study team assessed and managed the multiple domains of QoL for patients with advanced HF, including physical symptoms, psychosocial and spiritual concerns, and advance care planning Intervention co‐ordinated by a certified palliative care nurse practitioner. Performed in collaboration with each patient's clinical cardiology team and focused on shared goal‐setting to combine HF symptom amelioration with palliative care goals. After hospital discharge, the palliative nurse practitioner actively participated in the ongoing management of patients in outpatient environment. Comparison: managed by a cardiologist‐directed team with HF expertise. Inpatient care was focused on symptom relief and use of evidence‐based therapies as detailed in current guidelines. After discharge, patients received outpatient follow‐up with their general practitioners and an HF cardiologist or nurse practitioner with care focused on guidelines‐based medication titration and serial monitoring of end‐organ function. | |
| Outcomes | Primary outcomes and time points:
Secondary outcomes and time points:
Adverse outcomes: not reported | |
| Notes | Funding for trial: National Institute of Nursing Research (NINR) Notable conflicts of interest of trial authors: "Dr. Mentz has received research support from the National Institutes of Health (U10HL110312 and R01AG045551‐01A1), Amgen, AstraZeneca, Bristol‐Myers Squibb, GlaxoSmithKline, Gilead, Medtronic, Novartis, Otsuka, and ResMed; honoraria from HeartWare, Janssen, Luitpold Pharmaceuticals, Novartis, ResMed, and Thoratec/St. Jude; and has served on an advisory board for Luitpold Pharmaceuticals, Inc., and Boehringer Ingelheim. Dr. Granger has received research funding from Novartis, Sanofi, Daiichi, Boe[h]ringer Ingelheim, and AstraZeneca. Dr. Johnson has received research support from projects funded by the National Institute on Aging (RO1AG042130; K08AG028975). Dr. Krishnamoorthy has worked on projects funded by research grants to the Duke Clinical Research Institute from the NIH, Novartis, Daiichi‐Sankyo, and Eli Lilly; and has received support to attend educational conferences from HeartWare, Thoratec, and Medtronic. Dr. Mark has received consulting fees from Medtronic; and has received research funding from Eli Lilly, Bristol‐Myers Squibb, Pfizer, AstraZeneca, Merck and Company, Oxygen Therap[e]utics, and Gilead. Dr. Tulsky has received research funding from PCORI (SC 14‐1403‐13975). All other authors have reported that they have no relationships relevant to the contents of this paper to disclose." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described in design paper that participants were assigned using a complete randomisation scheme, but details not reported. |
| Allocation concealment (selection bias) | Unclear risk | Described in the design paper that participants were assigned using a complete randomisation scheme, but details were not reported. |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "The trial was unblinded because blinding of the intervention was not feasible." Comment: study team assessed and managed the participants' multiple domains of QoL. Therefore, participants were not blinded to investigators. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: "Spiritual concerns were assessed by the study nurse practitioner;" "Goals of care were iteratively assessed by the intervention nurse practitioner." Comment: other details of outcome assessors not reported. |
| Incomplete outcome data (attrition bias) | High risk | QoL measurement (n and %): intervention: 23 (30.7%) died, 11 (14%) lost to follow‐up; control group: 20 (26.7%) died, 15 (20%) lost to follow‐up. Depressive measurement (n and %): intervention: 23 (30.7%) died, 11 (14%) lost to follow‐up; control: 20 (26.7%) died, 16 (21%) lost to follow‐up. |
| Selective reporting (reporting bias) | High risk | Not all outcomes that were described in the design and methods paper were reported. The outcomes of a structured interview with HF patient's carer regarding overall quality of care, and costs and resource utilisation which we prespecified were not reported. |
| Other bias | Low risk | None identified. |
| Methods | Study design: individual RCT Total duration of study: not reported Number of study centres and location: 1 centre/Minnesota Study setting: hospital Date of study: recruited April 2012 to February 2013 | |
| Participants | Randomised (n): 232 (intervention: 116; control: 116) Lost to follow‐up/withdrawals (n): Intervention: 4 withdrew at time of intervention, and 11 discharged prior to intervention after randomisation Intervention: 26 lost to follow‐up at 1 month (7 died, 4 withdrew, 15 surveys were not completed for reasons unknown); 22 lost to follow‐up at 3 months (7 died, 1 withdrew, 14 surveys were not completed for reasons unknown) Control: 27 lost to follow‐up at 1 month (4 died, 2 withdrew, 21 surveys were not completed for reasons unknown), 22 lost to follow‐up at 3 months (1 died, 3 withdrew, 18 surveys not completed for reasons unknown) Analysed (n): intervention: 65; control: 78 (completed all surveys) Mean age (years): intervention: 76.0 (SD 13.0); control: 70.9 (SD 13.6) Age range: not reported Gender (n and % men): intervention: 55 (47.4%); control: 67 (57.8%) Severity of condition and diagnostic criteria: not reported Inclusion criteria: adult inpatients with a diagnosis of acute HF Exclusion criteria: in ICU, on a ventilator, undergoing evaluation for a heart transplant or a LVAD, post‐transplant to post‐LVAD, determined to be actively dying, or if they had cognitive impairments such that informed consent and data collection would not be possible or if they spoke limited English; patients who had already had a palliative care order request by their attending physician during hospital stay | |
| Interventions | Intervention: order for palliative care immediately entered, and triaged by palliative care team with goal of conducting palliative care consult within 24 hours of order. Providers did an initial consult and then determined whether further appointments were necessary and discussed that with the patient. Baseline study measures of symptom burden, depression, and QoL were available to providers to review at time of consultation. Study paid only for initial palliative care consultation and any subsequent visits were billed to patient's insurance as standard care. Actions of palliative care providers during visits generally included assessment of symptom burdens; emotional, spiritual, and psychosocial aspects of care; co‐ordination of care orders; recommendations for change in current or future treatment; referrals; and future care planning assessment and discussions Comparison: usual care | |
| Outcomes | Primary outcome and time points:
Secondary outcomes and time points:
Adverse outcomes: not reported | |
| Notes | Funding for trial: Abbott Northwestern Hospital Foundation Notable conflicts of interest of trial authors: "No competing financial interests exist." We contacted the trialists for further details of study data, and received some data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not reported. |
| Allocation concealment (selection bias) | Unclear risk | Details not reported. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Details not reported. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: "questionnaires were administered via mailed surveys at 1 and 3 months after enrollment. Patients who did not return mailed surveys within a week after the 1‐ or 3‐month follow‐up date were called by the research nurse and encouraged to return the survey or were offered the option to complete the survey over the phone." Comment: outcome data collected from self‐reported measures or electronic health record data. Since blinding of participants and personnel was unclear, it was unknown whether the outcomes of QoL and depression were affected. |
| Incomplete outcome data (attrition bias) | High risk | Intervention group: 65/116 (56%) participants completed all surveys. Control: 78/116 (67.2%) participants completed all surveys. |
| Selective reporting (reporting bias) | Low risk | Study protocol and trial register were not reported; all outcomes listed in the 'Methods' section of the study were reported in the 'Results' section. |
| Other bias | High risk | Quote: "Patients in the intervention group were average 5.1 years older than patients in the control group." Comment: intervention: mean age 76.0 (SD 11.9) years, control: 70.9 (SD 13.6) years. |
AC: advanced care; ACP: advanced care planning; ACS: acute coronary syndrome; AD: advanced directive; CHF: congestive heart failure; COPD: chronic obstructive pulmonary disease; CPR: cardiopulmonary resuscitation; EFFECT: Enhanced Feedback for Effective Cardiac Treatment; EGFR: estimated glomerular filtration rate; EQ5D: EuroQol‐5D; ESCAPE: Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness; ESRD: end‐stage renal disease; FACIT–Pal: Functional Assessment of Chronic Illness Therapy–Palliative Care scale; FCP: Future Care Plan; n: number of participants; GRACE: Global Registry of Acute Coronary Syndrome; HADS: Hospital Anxiety and Depression Survey; HF: heart failure; ICU: intensive care unit; KCCQ: Kansas City Cardiomyopathy Questionnaire; LVAD: left ventricular assist device; NYHA: New York Heart Association; MLHF: Minnesota Living with Heart Failure; NTproBNP: N‐terminal‐pro B‐type natriuretic peptide; OHS: open‐heart surgery; PC‐ACP: Patient‐Centered Advance Care Planning; PHQ‐8: 9‐item Patient Health Questionnaire; QoL: quality of life; RCT: randomised controlled trial; SD: standard deviation; SPIRIT‐HF: SPIRonolactone In the Treatment of Heart Failure; SPMQ: Short Portable Mental Status Questionnaire; STP: Statement of Treatment Preferences; VAD: ventricular assist device.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Wrong intervention | |
| Wrong study design | |
| Wrong intervention | |
| Ineligible participants. Study included participants of various diagnoses such as respiratory disease. We planned that we would include studies if the majority of participants had a diagnosis of heart failure, but this study included people with heart failure only about 30%. | |
| Wrong intervention | |
| Wrong participant population | |
| Wrong intervention | |
| Wrong intervention | |
| Wrong intervention | |
| Wrong intervention | |
| Wrong study design | |
| Wrong study design | |
| Wrong intervention | |
| Wrong study design | |
| Wrong intervention | |
| Wrong intervention | |
| Wrong intervention | |
| Wrong study design | |
| Wrong study design | |
| Wrong intervention | |
| Wrong participant population | |
| Wrong study design | |
| Ineligible participants. Study included participants of various diagnoses such as chronic obstructive pulmonary disease and diabetes with renal disease. Study did not indicate the rate of each diagnosis. | |
| Wrong intervention | |
| Ineligible participants. Study included participants of various diagnoses such as cancer and lung disease. We planned that we would include studies if the majority of participants had a diagnosis of heart failure, but this study included only about 17% of people with heart disease. Study was published as a series of studies about Skorstengaard 2017 that classified as awaiting studies. | |
| Wrong study design | |
| Wrong participant population | |
| Wrong study design | |
| Wrong intervention |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | RCT |
| Participants | Inclusion criteria: people with HF or lung disease at risk of dying within 12 months Exclusion criteria: high risk of death with 3 months |
| Interventions | Intervention: single case conference of 30–40 minutes between general practitioner, palliative care physician, and specialist nurse to develop a care plan for people with life‐limiting heart or lung disease. Case conference provided a comprehensive review of the case from a palliative care perspective, including symptom control, psychosocial issues for patient and carer, ACP, and service delivery, with an emphasis on care co‐ordination between specialist and community‐based care. Comparison: normal care of specialist medical services focusing on maximising function, general practitioner providing day‐to‐day care but not in close liaison with specialists, and nurses providing case management at home, and palliative care not involved at all. |
| Outcomes | Primary outcome:
Secondary outcomes:
|
| Notes | Last updated: December 2013 |
| Methods | RCT |
| Participants | Inclusion criteria: aged ≥ 18 years; being 'Supportive and Palliative Care Indicators Tool' positive in accordance to the tools criteria, i.e. positive for section 1 (general indicators of poor or deteriorating health) and positive for an indicator in section 2 (clinical indicators of life‐limiting conditions) of the tool. Exclusion criteria: patient already having been referred to the intervention supportive care clinic |
| Interventions | Intervention: multidisciplinary supportive care clinic management and ongoing follow‐up as clinically required. Clinic consisted of palliative care, renal medicine, general medicine, cardiac failure medicine, social work, ACP, and complex care nurse practitioners working in a combined clinic using a multidisciplinary clinic paradigm to manage chronic disease and care plan. Face‐to‐face consultations with patients and their carers with a palliative care physician or general medicine physician (or both), nurse practitioner, and social worker. Medical issues will be reviewed, symptoms managed, and care planning issues reviewed. Comparator: standard care includes all usual health care provided in settings other than the interventional clinic, such as the usual outpatient speciality clinics within Monash Health, usual inpatient care and emergency department care, and community care including general practice. |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Notes | Last updated: June 2018 |
| Methods | individual RCT, 2 academic medical centres |
| Participants | 56 dyads Inclusion criteria: dyads of adults with cardiovascular implantable electronic device and NYHA level II or III HF; an adult family member whom they might involve in heart care decision‐making Exclusion criteria: patients or family members with cognitive impairment |
| Interventions | Intervention: TAILORED intervention, which is a brief, nurse‐facilitated, patient‐family discussion involving assessment of patient preference for family involvement in healthcare decision and support for family members involved in proxy decision‐making. Comparison: unknown |
| Outcomes |
|
| Notes | Trial report available as conference abstract. Although we sent the corresponding trial author an e‐mail requesting further information whether article was published, we did not get a response. |
| Methods | RCT |
| Participants | Estimated enrolment: 140 participants Inclusion criteria: ejection fraction ≤ 35% and NYHA classification III or IV; surrogates of patients meeting this criteria. Exclusion criteria: unknown |
| Interventions | Intervention: Fair Care Program Comparison: usual care |
| Outcomes |
|
| Notes | Actual study completion date in ClinicalTrials.gov: September 2004. Study results are not available. |
| Methods | RCT |
| Participants | Enrolment: 240 participants Inclusion criteria: diagnosis of either: class III or IV NYHA Functional Classification or Stage D based on American Heart Association/American College of Cardiology Heart Failure Classification; renal failure and on dialysis; or metastatic lung, gastrointestinal (including pancreatic), or gynaecological cancer and receiving chemotherapy, radiotherapy, or palliative care; aged ≥ 19 years; able to communicate in English; reside within 100 km of Edmonton or Calgary; owns a telephone Exclusion criteria: cognitive impairment that would impact ability to give informed consent; in crisis; first visit or in the case of renal patients, in the first month of dialysis; participated in ACP pilot study; visual or hearing impairment (or both) that would impact their ability to see or hear (or both) the videos, or complete the assessments including the telephone follow‐up interviews. |
| Interventions | Intervention: 2 Conversations Matter videos: ACP and GCD Comparison: usual care (to receive no intervention) |
| Outcomes | Primary outcomes:
|
| Notes | Actual study completion date in ClinicalTrials.gov: November 2016. Study results not available. |
| Methods | RCT |
| Participants | Estimated enrolment: 1185 participants Inclusion criteria: aged ≥ 18 years; diagnosis of HF, COPD, or advanced cancer; ≥ 1 hospitalisations or emergency department visits in the previous year; Palliative Performance Scale score ≤ 70%; English‐ or Spanish‐speaking; PCP assessment that he/she "would not be surprised" if the patient died within 1 year Exclusion criteria: receiving hospice care; has end‐stage renal disease; lives in a nursing home |
| Interventions | Intervention: home‐based palliative care consisting of home visits by an interdisciplinary primary care team (physician, nurse, social worker, and chaplain) that provides pain and symptom management, psychosocial support, ACP, disease management education, spiritual and grief counselling, and other services as needed. Comparison: enhanced usual care consisting of usual primary care provided by a PCP who has received special training in the core elements of palliative care. |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Notes | Last updated on ClinicalTrials.gov: April 2017 |
| Methods | RCT |
| Participants | Estimated enrolment: 20 participants Inclusion criteria: aged > 18 years; a regular patient in trialists' clinic; able to read and write English; familiar with the use and have access to a personal computer, e‐mail, and Internet Exclusion criteria: none |
| Interventions | Intervention: HF‐ACP Website, which leads participants through 4 e‐learning modules. Each module contains 3 core elements: educational content that provides information and support to help patients complete the module, interactive tools for documenting their thoughts and progress, and motivational video clips that encourage behaviour change by validating participants ambivalence, suggesting strategies to help participants complete the task and to encourage and reassure participants that they can do this. Comparison: usual care. The standard of care for ACP at the trialists' institution is the "Speak Up" booklet and the Power of Attorney workbook from the Attorney General's Office – Ontario. Patients randomised to the control arm will be asked to register on a separate research portal where they will have electronic access to both booklets and a link to the Speak Up online Interactive workbook. There is no specific information on HF or HF treatments. They will be asked to complete the ACP using the interactive workbook. They will not receive any additional communication from the research team about their progress. |
| Outcomes | Primary outcome:
Secondary outcomes:
|
| Notes | Last updated on ClinicalTrials.gov: May 2018 |
| Methods | RCT |
| Participants | Estimated enrolment: 1129 participants Inclusion criteria: residents of participating nursing homes; aged ≥ 65 years; at high risk of death in the next 6–12 months, as indicated by data collected on the Resident Assessment Instrument that is completed quarterly in most Canadian nursing homes. Specifically the high‐risk elements are any of: CHESS score ≥ 3, cancer, congestive H, leave > 25% of their food uneaten; resident and resident's substitute decision‐maker provide informed consent to participate Exclusion criteria: resident and substitute decision‐maker do not speak English or French; residents who are deemed not be competent to make their own medical decisions AND their substitute decision‐maker is a legally assigned public guardian, or they have no substitute decision‐maker; residents who are transferred to a BABEL study home from another BABEL study home, with the date of transfer being after study initiation. Residents who transferred into a study home from a non‐study home are eligible. |
| Interventions | Intervention: BABEL Approach to Advance Care Planning in Nursing Homes. Eligible residents will: receive the BABEL Approach to Advance Care Planning; after these ACP discussions occur, the resident's PCP will be notified of the residents' ACP wishes; a brightly coloured document will be placed in a standard location of the nursing home chart that identifies the resident's ACP wishes; paramedics will be educated to know about these sheets and where to find them, and that they should be taken with any resident transferred to another care setting. Comparison: control group will receive the prevalent approach to ACP in that nursing home. No elements of the BABEL Approach to Advance Care Planning will be introduced |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Notes | Last updated on ClinicalTrials.gov: September 2018 |
| Methods | Baseline survey for RCT |
| Participants | 29 people with HF, further details not reported |
| Interventions | Intervention: in collaboration with HF specialists, the intervention consists of an interdisciplinary palliative care intervention focused on symptom management, ACP, and psychosocial support. The initial palliative care visit is conducted in hospital, followed by ≥ 3 in‐person and 3 telephone consultations over 6 months. |
| Outcomes | Not reported |
| Notes | We contacted the trialists for further details whether article was published. Their article was in the process of submission, and we were unable to get further information on the article. |
| Methods | RCT |
| Participants | 360 participants Inclusion criteria: eligible patients from the departments of oncology, cardiology, and respiratory medicine at Aarhus University Hospital; aged > 18 years; acceptable Danish language skills Exclusion criteria: cognitive impairment; expected to die within the next month; has no relatives |
| Interventions | Intervention: ACP conversation between a health professional and a patient about end‐of‐life discussions Comparison: usual care |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Notes | Study completed. We contacted the trial authors and were informed that publication of study findings is in progress. Although 2 articles were published, 1 study design was cross‐sectional study and the other had ineligible participants. The trialists are planning to publish 1 more article. Mrs Marianne H Skorstengaard, E‐mail: [email protected] Trial registration: NCT01944813 (first posted: 18 September 2013) |
ACP: advance care planning; AD: advance directive; CHESS: Changes in Health, End‐stage disease and Symptoms and Sign; COPD: chronic obstructive pulmonary disease; GAD‐7: 7‐item Generalized Anxiety Disorder Scale; GCD: Goals of Care Designations; HF: heart failure; NYHA: New York Heart Association; PCP: primary care physician; PHQ‐9: 9‐item Patient Health Questionnaire; QoL: quality of life; RCT: randomised controlled trial; SF‐12: 12‐item Short Form.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | A randomised control trial for advance care planning and symptom management for patients identified in the emergency department and followed up at home |
| Methods | RCT |
| Participants | Estimated enrolment: 500 participants Inclusion criteria: people presenting to the Prince of Wales Hospital Emergency Department with any advanced progressive life‐threatening illness as identified by clinical staff using the iPAL‐EM screening tool guide who do not presently require referral to specialist palliative care. Exclusion criteria: aged < 18 years, prisoners, pregnant women, and people with unstable psychotic illnesses or serious mood disorders |
| Interventions | Intervention: ACP + Symptom Management and Support, a 2‐pronged intervention. ACP: series of nurse‐lead discussions that explore and identify values and concerns relating to the participant's health care and management of care at EOL. Discussions will include patient and patient's carer if available and willing to participate in discussion. Anticipated that discussions will take place over ≤ 4 visits lasting 1–1.5 hours each. SMS: education component provided to participants' GPs and other healthcare providers. This includes: in‐service style training by a member of research team conducted at baseline and repeated at 6 months; individualised education regarding palliative care; provision of a symptom management resource list; letter to GP with information about Plan Early and ACP, written information about referral to specialist palliative care, and 6‐weekly follow‐up telephone calls to GP and family; education and training of RACF staff and GPs in the SELHD Terminal Care Plan. Comparison: usual care, which is standard evidence‐based care provided at the discretion of patient's GP and other healthcare providers. As health conditions will vary among participants in control group, usual care is expected to vary. |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Starting date | Date registered: June 2014 Date of first enrolment: February 2014 |
| Contact information | Dr Megan Sands, E‐mail: [email protected] Prince of Wales Hospital Barker Street Randwick NSW 2031, Australia |
| Notes | Last updated: 4 June 2014 |
| Trial name or title | FINnish PALliative care education trial (FINPAL) to improve nursing home residents' quality of life |
| Methods | Cluster RCT |
| Participants | Estimated enrolment: 300 participants Inclusion criteria: Finnish speaking; permanent resident in a nursing home/assisted‐living facility in city of Helsinki/Vantaa, Finland; ≥ 1 condition evaluated to affect severely health and prognosis (severe dementia, heart failure, COPD, diabetes mellitus, coronary heart disease, cancer, cachexia, chronic inflammation, frailty, disability, malnutrition); volunteer; able to give informed consent Exclusion criteria: aged < 65 years; evaluated prognosis > 1‐year terminal disease; end‐stage dementia; end‐stage COPD; end‐stage heart failure; end‐stage renal failure; malignant cancer; severe stroke; permanent institutionalisation; severe disability |
| Interventions | Intervention: staff working in units that are randomised to intervention group will be able to take part in educational sessions in palliative and end‐of‐life care over 3 months. Educational sessions will be performed in small groups of 10–20 staff members. Teaching method will be interactive encouraging discussions and questions. Sessions will encourage staff members to share and learn from previous experiences and patient cases in their own units to help them improve teamwork. Comparison: usual care, information leaflet to staff on current care guidelines on terminal care. |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Starting date | Date registered: July 2017 Date of first enrolment: September 2017 |
| Contact information | Prof Kaisu Pitkälä, E‐mail: [email protected] University of Helsinki Department of General Practice, PO Box 20. 00014 University of Helsinki, Finland |
| Notes | URL: www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=372296 Last updated: July 2017 |
| Trial name or title | Reducing disparities in the quality of palliative care for older African Americans through improved advance care planning: study design and protocol |
| Methods | Study design: RCT Number of study centres and location: 10 clinics in 5 US states/Alabama, Georgia, North Carolina, Texas, and South Carolina Study setting: clinic |
| Participants | Inclusion criteria: aged ≥ 65 years; non‐Hispanic, African‐American, or white; English speaking; residence in a non‐institutional setting; ≥ 2 visits at 1 of the participating clinics in last year; serious, chronic illness (≥ 1 of metastatic solid tumour or haematological cancer, end‐stage renal disease, advance liver disease or cirrhosis, COPD or interstitial lung disease on home oxygen, or hospitalised for condition in the last year, diabetes with severe complications (ischaemic heart disease, peripheral vascular disease, and renal disease); NYHA Stage III or IV congestive heart failure with hospitalisation in the last year; ≥ 2 unplanned hospitalisations in the last year; dependence in ≥ 1 activities of daily; aged ≥ 80 years; referral by provider at a participating clinic if provider considered patient would die in next 12 months. Exclusion criteria: residence in nursing home or assisted living facility; deafness; blindness; diagnosis of dementia; significant cognitive impairment; EMR documentation or patient report of ACP (living will, health care proxy, MOST form, and provider note); current or prior use of hospice or home‐based palliative care |
| Interventions | Intervention: 2 ACP approaches for comparison: a structured ACP approach using Respecting Choices First Steps and a patient‐driven, self‐management approach, including a Five Wishes form. Both approaches are delivered by lay ACP facilitators. In addition, all participants receive state advance directive forms and a contact card with telephone number and picture of their assigned lay ACP facilitator. Participants receive Respecting Choices materials that include general information about ACP and choosing a healthcare agent. Within 2 weeks, patient is contacted by a lay ACP facilitator who sets up a meeting with patient and surrogate decision maker for a 60–90‐minute ACP session. Conversation focuses on identifying cultural, spiritual, and personal beliefs that influence treatment preferences, identifying a healthcare agent, and exploring goals for medical care. Meetings occur in person if possible (by telephone if not). Lay ACP facilitator follows up with telephone call 2 weeks after meeting to answer questions. Patients may request 1 additional follow‐up call. Comparison: patients at clinics randomised to the patient‐driven, self‐management ACP approach receive the Five Wishes advance directive form and the Five Wishes Conversation Guide for Individuals and Families. Document allows patients to share their 'wishes' for the person they would like to serve as surrogate decision maker; the type of medical care that they would like to receive; how comfortable they want to be; how they want people to treat them; and what they want their loved ones to know. |
| Outcomes | Primary outcome:
Secondary outcomes:
|
| Starting date | Not reported |
| Contact information | Deborah B Ejem, E‐mail: [email protected] Division of Preventive Medicine, School of Medicine, University of Alabama at Birmingham, Birmingham, Alabama |
| Notes |
| Trial name or title | Advancing Symptom Alleviation with Palliative Treatment (ADAPT) trial to improve quality of life: a study protocol for a randomized clinical trial |
| Methods | Study design: RCT Number of study centres and location: 2 Veterans Health Administration facilities/Eastern Colorado, Puget Sound Study setting: community‐based outpatient clinics |
| Participants | Estimated enrolment: 300 participants Inclusion criteria: diagnosis of CHF or COPD within 2 years prior to enrolment; diagnosis of interstitial lung disease within 2 years prior to enrolment; among those with CHF or COPD, high risk for hospitalisation and death; poor quality of life; symptomatic; primary care or other provider who is willing to facilitate intervention medical recommendations; able to read and understand English; consistent access to and able to use a standard telephone Exclusion criteria: diagnosis of dementia; active substance abuse; comorbid metastatic cancer; diagnosis of obesity hypoventilation syndrome; nursing home resident; heart or lung transplant or LVAD; participation in the intervention arm of the CASA (Collaborative Care to Alleviate Symptoms and Adjust to Illness in Chronic Heart Failure) trial (NCT01739686); enrolled in palliative care, hospice, or home‐based primary care; prisoner; pregnant |
| Interventions | Intervention: multidisciplinary, team‐based approach to addressing symptoms and psychosocial needs of participants. Personnel include a registered nurse and Master's level social worker. They integrate into a larger collaborative care team that includes a representative primary care provider and palliative care specialist. Specialist support with a cardiologist or pulmonologist is available for the team for additional management recommendations if needed. Each site has a team that meets weekly for 30–60 minutes, integrating palliative symptom management with disease‐specific care plans. Comparison: usual care at the discretion of their care providers. No limitations on care recommendations or referrals, which may include management by subspecialists, mental health providers, or palliative care at the discretion of their primary care providers. |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Starting date | Recruitment began 1 September 2016 |
| Contact information | Bridget A Graney, E‐mail: [email protected] Division of Pulmonary Sciences and Critical Care Medicine, Department of Medicine, University of Colorado School of Medicine, Anschutz Medical Campus, Aurora, CO, USA |
| Notes | Trial registration: NCT02713347. Registered 18 March 2016. Last updated 16 August 2019 |
| Trial name or title | Impact of advance care planning on the care of patients with heart failure: study protocol for a randomized controlled trial |
| Methods | Study design: RCT Number of study centres and location: 2 centres/Singapore Study setting: hospital |
| Participants | 282 participants Inclusion criteria: people with advanced CHF (NYHA classes III and IV); hospitalised; aged ≥ 21 years; able to give informed consent Exclusion criteria: psychiatric or cognitive disorders; previously documented ACP; people who have undergone ACP facilitation |
| Interventions | Intervention: ACP facilitator will assist in determining patients' preferences for future medical care, and will provide patients and their families with emotional support to make end‐of‐life decisions. Family members will be encouraged to be present during ACP discussion so that whole family unit will be able to explore goals, values, and beliefs towards patient's medical care. Patients will be encouraged to appoint a substitute healthcare decision‐maker who will make decisions on their behalf when they are no longer able to do so. These patients' preferences will be noted in the ACP document, and copy of ACP document will be provided to patients, their substitute healthcare decision‐makers, and the healthcare team. The ACP document will be recorded electronic medical records in the National IT System, and will be shared with another hospital in Singapore. The ACP facilitator will review patients' preferences regularly. If patients' preferences about future medical care change, the ACP facilitator will discuss patients' preferences with patients and their families or substitute healthcare decision‐makers, and will update the ACP document. Comparison: usual care with no ACP discussions and documentation. |
| Outcomes | Primary outcome:
Secondary outcomes:
|
| Starting date | February 2015 |
| Contact information | Chetna Malhotra, E‐mail: chetna.malhotra@duke‐nus.edu.sg Duke‐NUS Graduate Medical School, Singapore |
| Notes | Trial registration: NCT02299180. Registered 18 November 2014 |
| Trial name or title | Feasibility and outcomes of older patients' hospitalization (official title not provided) |
| Methods | RCT |
| Participants | Estimated enrolment: 300 participants Inclusion criteria: aged > 65 years; haemodynamic, nutritional, and respiratory stability; eligibility for subacute hospitalisation Exclusion criteria: oncological active disease; uncorrectable hypoxaemia (oxygen saturation 90%); suspected myocardial ischaemia; presence of an acute illness, other than the target illness |
| Interventions | Not known |
| Outcomes | Not known |
| Starting date | July 2007 |
| Contact information | Doron Nezer, E‐mail: [email protected] |
| Notes | Last updated on ClinicalTrials.gov: 21 June 2007 Although we contacted the trialists for further details whether study was completed and article was published, we received no response. |
| Trial name or title | Preparing family caregivers to make medical decisions for their loved ones |
| Methods | RCT |
| Participants | Enrolment: 570 participants Inclusion criteria: aged ≥ 18 years; diagnosis of kidney disease (e.g. chronic kidney disease, end‐stage renal disease) OR advanced cancer (Stage IV disease or having an estimated survival < 2 years) OR severe heart failure (e.g. NYHA class III or IV) OR severe lung disease (e.g. Stage III or IV COPD by modified GOLD Spirometric Classification, idiopathic pulmonary fibrosis); able to read and understand English at 8th grade level (word 26 on either blue or tan version of the Wide Range Achievement Test‐3 reading subtest); neuro‐cognitively able to engage in ACP (Mini‐Mental State Examination score > 23); no active suicidal ideations (i.e. score of 0 or 1 on item 9 of the Beck Depression Inventory‐II) Exclusion criteria: failure on any of the above inclusion criteria |
| Interventions | Group 1: standard ACP/patient alone Group 2: decision aid/patient alone Group 3: standard ACP/patients and carers together Group 4: decision aid/patients and carers together |
| Outcomes | Primary outcome:
Secondary outcomes:
|
| Starting date | June 2013 |
| Contact information | Dr Benjamin H Levi, E‐mail: [email protected] Milton S. Hershey Medical Center/Penn State College of Medicine, H134 Humanities Hershey, PA, USA |
| Notes | Last updated on ClinicalTrials.gov: November 2017 |
| Trial name or title | Pragmatic trial of video education in nursing homes (PROVEN) |
| Methods | RCT |
| Participants | Inclusion criteria: facilities within Genesis HealthCare or PruittHealth healthcare systems; facilities have facility identifiers that indicate that they are Medicare/Medicaid‐certified nursing facilities in the US; facilities serve both short and long‐stay patients; facilities have > 50 beds; facilities have an electronic medical records system; facilities had ≥ 20 admissions and 20 annual Minimum Data Set assessments (regardless of whether they were discharged alive) in 2013. Exclusion criteria: facilities excluded per corporate leaders in healthcare system because of recent turnover in nursing home administrator or Director of Nursing; facilities excluded per corporate leaders in health care system because of recent bad state or federal quality assurance survey (e.g. restriction on admissions, levied large civil monetary penalty, etc.); facilities excluded per corporate leaders in healthcare system because of current new initiatives/competing demands. |
| Interventions | Intervention: ACP Video Program, which consists of 5 videos that address ACP decisions: General Goals of Care, Goals of Care for Advanced Dementia, Hospice, Hospitalization, and ACP for Healthy Patients. Nursing home staff will offer videos to patients at these clinical triggers: within 7 days of admission or readmission; every 6 months for long‐stay patients; when there is a significant change in clinical status; when a treatment decision arises for which there is a specific video; and special circumstances when goals of care are being considered (e.g. family visiting). Comparison: usual ACP procedures |
| Outcomes | Primary outcome:
Secondary outcomes:
|
| Starting date | March 2016 |
| Contact information | Vincent Mor, E‐mail: [email protected] Health Services, Policy & Practice, Brown University, Rhode Island, USA |
| Notes | Last updated on ClinicalTrials.gov: May 2018 |
| Trial name or title | Primary palliative care in heart failure: a pilot trial |
| Methods | RCT |
| Participants | Enrolment: 30 participants Inclusion criteria: NYHA class III or IV heart failure; ≥ 2 hospitalisations in the past year due to heart failure Exclusion criteria: aged < 40 years; currently awaiting a transplant; received outpatient palliative care within the past 12 months; pregnant or intends to be within next 12 months; no regular telephone access; not fluent in English; failed the Callahan 6‐item Screener; does not intent to regularly attend clinic for the next 12 months |
| Interventions | Intervention: 4 primary mechanisms 1. An existing heart failure nurse will deliver the intervention to patients during regularly scheduled visits. 2. Telephone calls will reinforce topics. 3. Patients will regularly report symptoms through the MyUPMC patient portal. 4. The nurse will act as a liaison to communicate concerns to the patient's cardiologist and primary care physician, as well as facilitating other resources The intervention will span 4 domains: symptom management (e.g. dyspnoea), psychosocial support (e.g. anxiety), ACP (e.g. understanding prognosis and electing a proxy), and care co‐ordination (e.g. communication across providers). Comparison: usual care, which will include standard of high‐quality heart failure care provided to all patients. |
| Outcomes | Primary outcome:
Secondary outcomes:
|
| Starting date | October 2017 |
| Contact information | Dio Kavalieratos, PhD, Assistant Professor of Medicine, E‐mail: [email protected] University of Pittsburgh, 230 McKee Place Suite 600 Pittsburgh, PA 15213, USA |
| Notes | Recruitment status: active, not recruiting Last verified: June 2019 Estimated study completion date: 31 May 2020 |
| Trial name or title | Reducing disparities in the quality of advance care planning for older adults (EQUALACP) |
| Methods | Cluster randomised trial, 4 locations |
| Participants | Estimated enrolment: 800 participants Inclusion criteria: African‐American or white people; aged ≥ 65 years; English‐speaking; residing in non‐institutional setting; cognitively able to participate in ACP; serious or chronic illness including: metastatic cancer, end‐stage renal disease, advanced liver disease, heart disease, lung disease, amyotrophic lateral sclerosis, severe Parkinson's disease; ≥ 2 unplanned hospitalisations in last year; requiring assistance with any basic activity of daily living. Exclusion criteria: residence in nursing home or assisted living facility; diagnosis of dementia or unable to consent; documented ACP (living will, health care proxy, MOST form, provider note); current or prior use of hospice; current or prior use of non‐hospice palliative care except inpatient palliative care consultation |
| Interventions | Intervention: structured ACP. Patients will participate in 60‐ to 90‐minute facilitated ACP conversation with a trained person using Respecting Choices (First Steps) guide and receive a state advance directive form. The ACP facilitator will follow‐up as needed after the session to answer additional questions. Comparison: patient‐driven ACP. Patients will receive a Five Wishes Form (easy to understand advance directive written in plain language), a state advance directive form, and ≥ 2 follow‐up telephone calls with an ACP contact who will answer questions. |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Starting date | January 2019 |
| Contact information | Kimberly S Johnson, E‐mail: [email protected] Duke University, Durham, NC, USA |
| Notes | Last updated on ClinicalTrials.gov: October 2018 |
ACP: advance care planning; ALS: advanced life support; CHF: chronic heart failure; COPD: chronic obstructive pulmonary disease; CPR: cardiopulmonary resuscitation; EMR: electronic medical record; EOL: end of life; GOLD: Global Initiative for Chronic Obstructive Lung Disease; GP: general practitioner; iPAL‐EM: Improving Palliative Care in Emergency Medicine; MDS‐RAI: Resident Assessment Instrument‐Minimum Data Set; MOST: Medical Orders for Scope of Treatment; NWAU: National Weighted Activity Unit; NYHA: New York Heart Association; PACE: Programs of All‐Inclusive Care for the Elderly; RACF: residential aged care facilities; RCT: randomised controlled trial; SELHD: South Eastern Sydney Local Health District.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants' quality of life (overall analysis: EQ‐5D, Kansas City Cardiomyopathy Questionnaire) Show forest plot | 3 | 156 | Std. Mean Difference (Fixed, 95% CI) | 0.06 [‐0.26, 0.38] |
| Analysis 1.1  Comparison 1 Advance care planning (ACP) versus usual care, Outcome 1 Participants' quality of life (overall analysis: EQ‐5D, Kansas City Cardiomyopathy Questionnaire). | ||||
| 2 Participants' quality of life (subgroup analysis by follow‐up periods: EQ‐5D, Kansas City Cardiomyopathy Questionnaire) Show forest plot | 3 | 156 | Std. Mean Difference (Fixed, 95% CI) | 0.06 [‐0.26, 0.38] |
| Analysis 1.2  Comparison 1 Advance care planning (ACP) versus usual care, Outcome 2 Participants' quality of life (subgroup analysis by follow‐up periods: EQ‐5D, Kansas City Cardiomyopathy Questionnaire). | ||||
| 2.1 Follow‐up periods ≤ 3 months | 1 | 44 | Std. Mean Difference (Fixed, 95% CI) | ‐0.05 [‐0.65, 0.54] |
| 2.2 Follow‐up periods > 3 months | 2 | 112 | Std. Mean Difference (Fixed, 95% CI) | 0.11 [‐0.27, 0.48] |
| 3 Completion of documentation by medical staff regarding discussions with participants about ACP processes Show forest plot | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.68 [1.23, 2.29] |
| Analysis 1.3  Comparison 1 Advance care planning (ACP) versus usual care, Outcome 3 Completion of documentation by medical staff regarding discussions with participants about ACP processes. | ||||
| 4 Participants' depression (overall analysis) Show forest plot | 3 | 278 | Std. Mean Difference (Fixed, 95% CI) | ‐0.58 [‐0.82, ‐0.34] |
| Analysis 1.4  Comparison 1 Advance care planning (ACP) versus usual care, Outcome 4 Participants' depression (overall analysis). | ||||
| 5 Participants' depression (subgroup analysis by follow‐up periods) Show forest plot | 3 | 278 | Std. Mean Difference (Fixed, 95% CI) | ‐0.58 [‐0.82, ‐0.34] |
| Analysis 1.5  Comparison 1 Advance care planning (ACP) versus usual care, Outcome 5 Participants' depression (subgroup analysis by follow‐up periods). | ||||
| 5.1 Follow‐up periods ≤ 3 months | 1 | 167 | Std. Mean Difference (Fixed, 95% CI) | ‐0.69 [‐1.01, ‐0.38] |
| 5.2 Follow‐up periods > 3 months | 2 | 111 | Std. Mean Difference (Fixed, 95% CI) | ‐0.41 [‐0.79, ‐0.03] |
| 6 Participants' decisional conflict Show forest plot | 2 | 38 | Mean Difference (IV, Fixed, 95% CI) | ‐0.26 [‐0.55, 0.02] |
| Analysis 1.6  Comparison 1 Advance care planning (ACP) versus usual care, Outcome 6 Participants' decisional conflict. | ||||
| 7 All‐cause mortality Show forest plot | 5 | 795 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [1.04, 1.67] |
| Analysis 1.7  Comparison 1 Advance care planning (ACP) versus usual care, Outcome 7 All‐cause mortality. | ||||
| 8 All‐cause mortality (sensitivity analysis excluding Kirchhoff 2010) Show forest plot | 4 | 482 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.44 [0.99, 2.09] |
| Analysis 1.8  Comparison 1 Advance care planning (ACP) versus usual care, Outcome 8 All‐cause mortality (sensitivity analysis excluding Kirchhoff 2010). | ||||

Study flow diagram.
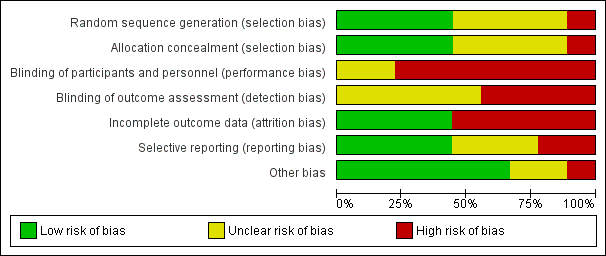
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
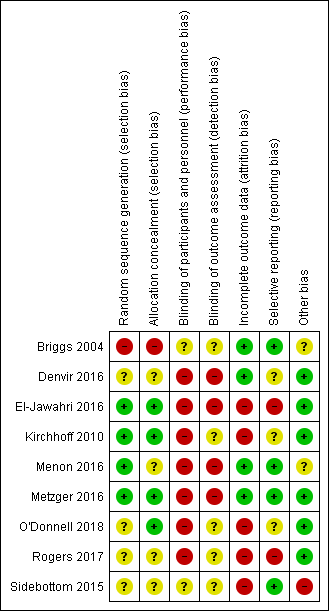
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
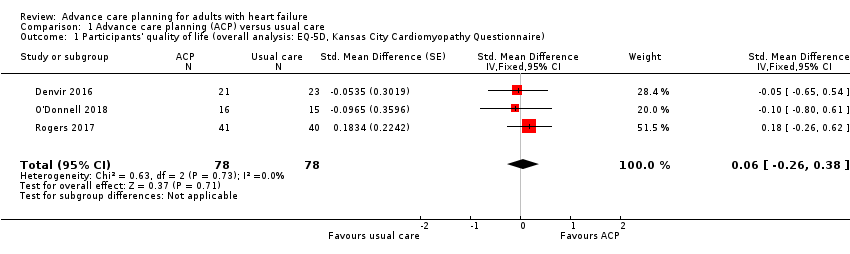
Comparison 1 Advance care planning (ACP) versus usual care, Outcome 1 Participants' quality of life (overall analysis: EQ‐5D, Kansas City Cardiomyopathy Questionnaire).
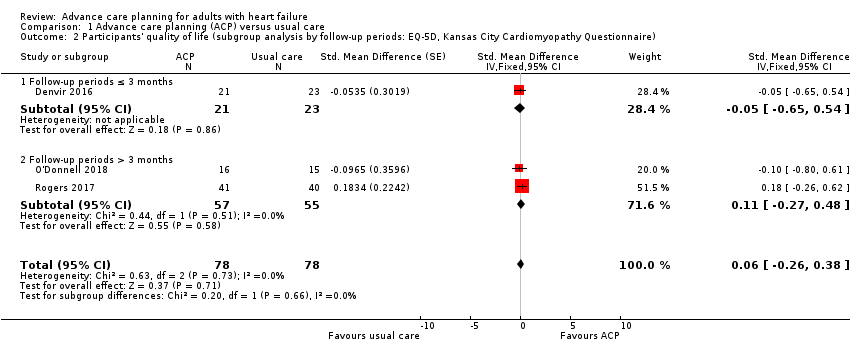
Comparison 1 Advance care planning (ACP) versus usual care, Outcome 2 Participants' quality of life (subgroup analysis by follow‐up periods: EQ‐5D, Kansas City Cardiomyopathy Questionnaire).
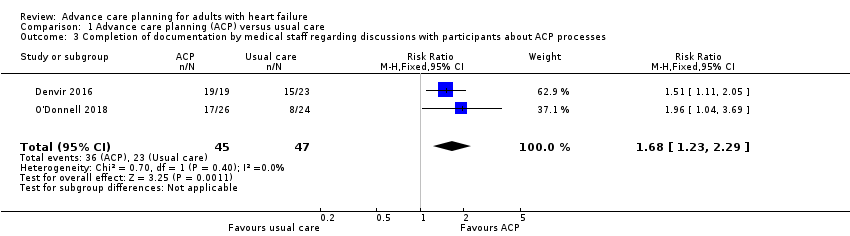
Comparison 1 Advance care planning (ACP) versus usual care, Outcome 3 Completion of documentation by medical staff regarding discussions with participants about ACP processes.

Comparison 1 Advance care planning (ACP) versus usual care, Outcome 4 Participants' depression (overall analysis).
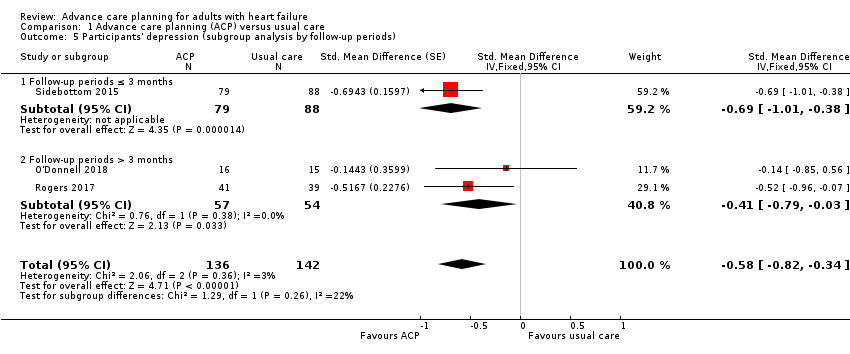
Comparison 1 Advance care planning (ACP) versus usual care, Outcome 5 Participants' depression (subgroup analysis by follow‐up periods).

Comparison 1 Advance care planning (ACP) versus usual care, Outcome 6 Participants' decisional conflict.
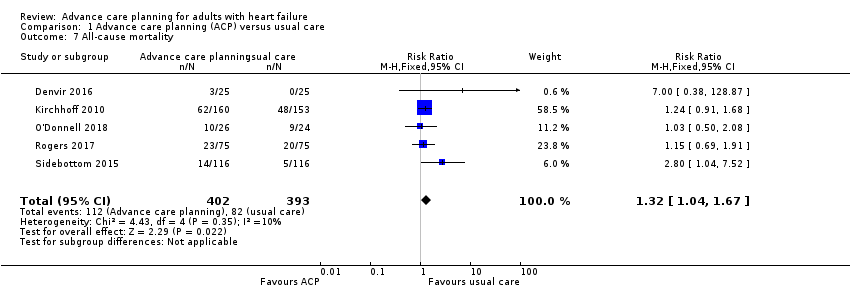
Comparison 1 Advance care planning (ACP) versus usual care, Outcome 7 All‐cause mortality.
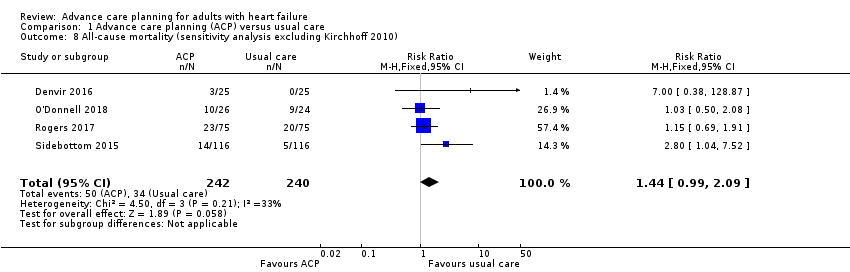
Comparison 1 Advance care planning (ACP) versus usual care, Outcome 8 All‐cause mortality (sensitivity analysis excluding Kirchhoff 2010).
| Advance care planning compared with usual care for patients with heart failure | ||||||
| Patient or population: people with heart failure with or without their surrogate decision‐makers/carers Settings: inpatient and outpatient hospitals and clinics Intervention: ACP Comparison: usual care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Usual care | ACP | |||||
| Concordance between participants' preferences and end‐of‐life care (yes/no) Post‐death data: mean days to death, ACP group (388.8 ± 255.7); | 625 per 1000 | 744 per 1000 | RR 1.19 (0.91 to 1.55) | 110 | ⊕⊝⊝⊝ | — |
| Participants' quality of life Measured by EQ‐5D and KCCQ. Higher scores indicate high‐quality of life. Follow‐up: 2 weeks to 6 months | The quality of life score in the ACP groups was on average 0.06 SDs higher (0.26 lower to 0.38 higher) than in the usual care groups. | — | 156 | ⊕⊕⊝⊝ | 1 additional study reported quality of life using the MLHF Questionnaire. The study showed that the quality of life score was improved by 14.86 points in the intervention group compared with 11.80 points in the usual care group at 3 months. Generally, 0.2 SD represents a small difference, 0.5 moderate, and 0.8 large. | |
| Patients' satisfaction with care/treatment (yes/no) | — | — | — | — | — | Outcome not reported. |
| Completion of documentation by medical staff regarding discussions with participants about ACP processes (yes/no) Follow‐up: 3–6 months | 489 per 1000 | 822 per 1000 | RR 1.68 (1.23 to 2.29) | 92 | ⊕⊕⊝⊝ | 1 additional study reported completion of documentation with HR (HR 2.87, 95% CI 1.09 to 7.59; P = 0.033). |
| Participants' depression Measured on PHQ‐8, PHQ‐9, and HADS. Higher scores indicate high depression Follow‐up: 2 weeks to 6 months | The depression score in the ACP groups was on average 0.58 SDs (0.82 to 0.34) lower than in the usual care groups. | — | 278 | ⊕⊕⊝⊝ Lowc,e | Generally, 0.2 SD represents a small difference, 0.5 moderate, and 0.8 large. | |
| Caregivers' satisfaction with care/treatment (yes/no) | — | — | — | — | — | Outcome not reported. |
| Quality of communication Measured on Quality of Patient‐Clinician Communication About End‐of‐Life Care. Higher score indicates high satisfaction with the quality of communication Assessed after intervention | 11.2 ± 0.8 (mean ± SD) | MD 0.4 lower (1.61 lower to 0.81 higher) | — | 9 | ⊕⊝⊝⊝ | — |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ACP: advanced care planning; CI: confidence interval; EQ‐5D: EuroQol‐5D; HADS: Hospital Anxiety and Depression Survey; HR: hazard ratio; KCCQ: Kansas City Cardiomyopathy Questionnaire; MD: mean difference; MLHF: Minnesota Living with Heart Failure; PHQ: Patient Health Questionnaire; RCT: randomised controlled trial; RR: risk ratio; SD: standard deviation; SMD: standardised mean difference. | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded one level for indirectness because the study included participants other than people with heart failure. bSince the outcome included only one study, the sample size was too small, and had wide confidence intervals. Therefore, we downgraded two levels for imprecision. cDowngraded one level for risk of bias because most included studies showed unclear selection bias and high attrition bias. dDowngraded one level for imprecision due to small sample size and wide confidence intervals. eDowngraded one level for imprecision due to small sample size. fDowngraded one level for risk of bias due to high risk of selection bias. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants' quality of life (overall analysis: EQ‐5D, Kansas City Cardiomyopathy Questionnaire) Show forest plot | 3 | 156 | Std. Mean Difference (Fixed, 95% CI) | 0.06 [‐0.26, 0.38] |
| 2 Participants' quality of life (subgroup analysis by follow‐up periods: EQ‐5D, Kansas City Cardiomyopathy Questionnaire) Show forest plot | 3 | 156 | Std. Mean Difference (Fixed, 95% CI) | 0.06 [‐0.26, 0.38] |
| 2.1 Follow‐up periods ≤ 3 months | 1 | 44 | Std. Mean Difference (Fixed, 95% CI) | ‐0.05 [‐0.65, 0.54] |
| 2.2 Follow‐up periods > 3 months | 2 | 112 | Std. Mean Difference (Fixed, 95% CI) | 0.11 [‐0.27, 0.48] |
| 3 Completion of documentation by medical staff regarding discussions with participants about ACP processes Show forest plot | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.68 [1.23, 2.29] |
| 4 Participants' depression (overall analysis) Show forest plot | 3 | 278 | Std. Mean Difference (Fixed, 95% CI) | ‐0.58 [‐0.82, ‐0.34] |
| 5 Participants' depression (subgroup analysis by follow‐up periods) Show forest plot | 3 | 278 | Std. Mean Difference (Fixed, 95% CI) | ‐0.58 [‐0.82, ‐0.34] |
| 5.1 Follow‐up periods ≤ 3 months | 1 | 167 | Std. Mean Difference (Fixed, 95% CI) | ‐0.69 [‐1.01, ‐0.38] |
| 5.2 Follow‐up periods > 3 months | 2 | 111 | Std. Mean Difference (Fixed, 95% CI) | ‐0.41 [‐0.79, ‐0.03] |
| 6 Participants' decisional conflict Show forest plot | 2 | 38 | Mean Difference (IV, Fixed, 95% CI) | ‐0.26 [‐0.55, 0.02] |
| 7 All‐cause mortality Show forest plot | 5 | 795 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [1.04, 1.67] |
| 8 All‐cause mortality (sensitivity analysis excluding Kirchhoff 2010) Show forest plot | 4 | 482 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.44 [0.99, 2.09] |

