Cannabis para el tratamiento de la enfermedad de Crohn
Resumen
Antecedentes
La enfermedad de Crohn (EC) es una afección crónica mediada por el sistema inmunitario, con inflamación transmural del tracto gastrointestinal, asociada a una morbilidad significativa y una disminución en la calidad de vida. El sistema endocannabinoide proporciona un objetivo terapéutico potencial del cannabis y los cannabinoides, y en modelos animales, se ha demostrado el efecto beneficioso para disminuir la inflamación. Sin embargo, también hay evidencia que indica eventos adversos transitorios como debilidad, mareos y diarrea, y un mayor riesgo de cirugía en los pacientes con EC que consumen cannabis.
Objetivos
Los objetivos fueron evaluar la eficacia y la seguridad del cannabis y los cannabinoides para la inducción y el mantenimiento de la remisión en los pacientes con EC.
Métodos de búsqueda
Se hicieron búsquedas en MEDLINE, Embase, AMED, PsychINFO, registro especializado de ensayos del Grupo Cochrane de Enfermedad Inflamatoria Intestinal y Trastornos Funcionales del Intestino (EII/TFI) (Cochrane Inflammatory Bowel Disease and Functional Bowel Disorders Group, IBD/FBD Group), CENTRAL, ClinicalTrials.Gov y en el European Clinical Trials Register hasta el 17 octubre 2018. Se realizaron búsquedas en los resúmenes de congresos, las referencias y también se estableció contacto con los investigadores en este campo para obtener publicaciones futuras.
Criterios de selección
Se incluyeron los ensayos controlados aleatorizados que compararon cualquier forma de cannabis o derivados de cannabinoide (natural o sintético) con placebo o un tratamiento activo para pacientes adultos con enfermedad de Crohn.
Obtención y análisis de los datos
Dos autores de la revisión, de forma independiente, examinaron los resultados de la búsqueda, extrajeron los datos y evaluaron el sesgo mediante la herramienta Cochrane riesgo de sesgo. Los resultados primarios fueron la remisión clínica y la recurrencia. La remisión se define comúnmente con un Crohn's disease activity index (CDAI) de < 150. La recaída se define con un CDAI > 150. Los resultados secundarios fueron: la respuesta clínica, la remisión endoscópica, la mejoría endoscópica, la mejoría histológica, la calidad de vida, la proteína C reactiva (PCR) y las mediciones de calprotectina fecal, los eventos adversos (EA), los EA grave, los retiros debido a EA y la dependencia del cannabis y los efectos de la abstinencia. Se calcularon los riesgos relativos (RR) y el intervalo de confianza del 95% (IC del 95%) correspondiente para los resultados dicotómicos. Para los datos continuos, se calculó la diferencia de medias (DM) y el IC del 95%. Los datos se combinaron para el metanálisis cuando las intervenciones, los grupos de pacientes y los resultados fueron suficientemente similares (decidido por consenso). Los datos se analizaron sobre una base de intención de tratar y la certeza general de la evidencia que apoyaba los resultados se evaluó con los criterios GRADE.
Resultados principales
Tres estudios (93 participantes) que evaluaron el cannabis en pacientes con EC activa cumplieron con los criterios de inclusión. También se identificó un estudio en curso. Los participantes de dos de los estudios fueron pacientes adultos con enfermedad de Crohn activa en quienes había fracasado al menos un tratamiento médico. Los criterios de inclusión del tercer estudio no estaban claros. No se identificaron estudios que evaluaran el tratamiento con cannabis en la EC inactiva. Los estudios no se agruparon debido a las diferencias en el fármaco de intervención.
Un estudio pequeño (N = 21) comparó ocho semanas de tratamiento con cigarrillos de cannabis que contenían 115 mg de D9‐tetrahidrocannabinol (THC) con los cigarrillos placebo que contenían cannabis sin THC en pacientes con EC activa. Este estudio se consideró con alto riesgo de sesgo por el cegamiento y otros sesgos (los participantes que recibieron cannabis eran mayores que los que recibieron placebo). Los efectos del cannabis sobre la remisión clínica no estuvieron claros. El 45% (5/11) del grupo de cannabis logró la remisión clínica en comparación con el 10% (1/10) del grupo placebo (RR 4,55; IC del 95%: 0,63 a 32,56; evidencia de muy baja certeza). Se observó una diferencia en las tasas de respuesta clínica (disminución en la puntuación CDAI > 100 puntos). El 91% (10/11) del grupo de cannabis logró una respuesta clínica en comparación con el 40% (4/10) del grupo placebo (RR 2,27; IC del 95%: 1,04 a 4,97; evidencia de muy baja certeza). Se observaron más EA en el grupo de cigarrillos de cannabis en comparación con placebo (RR 4,09; IC del 95%: 1,15 a 14,57; evidencia de certeza muy baja). Estos EA se consideraron leves e incluyeron somnolencia, náuseas, dificultad para concentrarse, pérdida de memoria, confusión y mareos. Este estudio no informó EA graves ni retiros debido a EA.
Un estudio pequeño (N = 22) comparó aceite de cannabis (cannabidiol 5%) con aceite placebo en los pacientes con EC activa. Este estudio se consideró con alto riesgo de sesgo de otros sesgos (fue más probable que los participantes que recibieron cannabis fueran fumadores que los participantes que recibieron placebo). No hubo diferencias en las tasas de remisión clínica. El 40% (4/10) de los participantes que recibieron aceite de cannabis lograron la remisión a las ocho semanas en comparación con el 33% (3/9) de los participantes que recibieron placebo (RR 1,20; IC del 95%: 0,36 a 3,97; evidencia de muy baja certeza). No hubo diferencias en la proporción de participantes que presentaron un evento adverso grave. El 10% (1/10) de los participantes del grupo de aceite de cannabis presentaron un evento adverso grave en comparación con el 11% (1/9) de los participantes que recibieron placebo (CR 0,90; IC del 95%: 0,07 a 12,38; evidencia de certeza muy baja). Los EA graves fueron casos de empeoramiento de la enfermedad de Crohn que requería intervención de rescate. Este estudio no informó de la respuesta clínica, PCR, la calidad de vida ni los retiros debido a EA.
Un estudio pequeño (N = 50) comparó aceite de cannabis (15% de cannabidiol y 4% de THC) con placebo en pacientes con EC activa. Este estudio se consideró con riesgo bajo de sesgo. Se observaron diferencias en las puntuaciones de CDAI y la calidad de vida medidas con el SF‐36. La media de la puntuación de calidad de vida después de ocho semanas de tratamiento fue 96,3 en el grupo de aceite de cannabis en comparación con 79,9 en el grupo placebo (DM 16,40; IC del 95%: 5,72 a 27,08; evidencia de certeza baja). Después de ocho semanas de tratamiento, la media de la puntuación de CDAI fue 118,6 en el grupo de aceite de cannabis en comparación con 212,6 en el grupo placebo (DM ‐94,00; IC del 95%: ‐148,86 a ‐39,14; evidencia de certeza baja). Este estudio no informó de la remisión clínica, la respuesta clínica, la PCR ni los EA.
Conclusiones de los autores
Los efectos del cannabis y del aceite de cannabis en la enfermedad de Crohn no están claros. Por lo tanto, no se pueden establecer conclusiones firmes con respecto a la eficacia y la seguridad del cannabis ni del aceite de cannabis en pacientes adultos con enfermedad de Crohn activa. No se han investigado los efectos del cannabis ni del aceite de cannabis en la enfermedad de Crohn inactiva. Se necesitan estudios adicionales con un gran número de participantes para evaluar los efectos beneficiosos y perjudiciales potenciales del cannabis en la enfermedad de Crohn. Los estudios futuros deben evaluar los efectos del cannabis en los pacientes con enfermedad de Crohn activa e inactiva. Se deben investigar diferentes dosis y vías de administración del cannabis.
PICO
Resumen en términos sencillos
Cannabis y aceite de cannabis para el tratamiento de la enfermedad de Crohn
¿Qué es la enfermedad de Crohn?
La enfermedad de Crohn es una afección a largo plazo que provoca la inflamación del tracto gastrointestinal, en cualquier sitio desde la boca al ano. Los síntomas frecuentes son: fiebre, diarrea, dolor abdominal y pérdida de peso. La enfermedad de Crohn se caracteriza por períodos de recurrencia en que los pacientes presentan síntomas de actividad y períodos de remisión sin síntomas.
¿Qué son el cannabis y los cannabinoides?
El cannabis es un fármaco de uso extendido que actúa en el sistema endocannabinoide. El cannabis contiene componentes múltiples llamados cannabinoides. El uso de cannabis y aceite de cannabis (que contiene cannabinoides específicos) produce efectos mentales y físicos como alteración de la percepción sensorial y euforia cuando se consumen. Algunos cannabinoides, como el cannabidiol, no tienen efectos psicoactivos. El cannabis y el cannabidiol tienen algunas propiedades antiinflamatorias que quizás ayuden a los pacientes con enfermedad de Crohn.
¿Qué examinaron los investigadores?
Los investigadores estudiaron si el cannabis es mejor que placebo (p.ej., una pastilla de azúcar) para el tratamiento de los pacientes adultos con enfermedad de Crohn activa o enfermedad de Crohn activa en remisión.
¿Qué encontraron los investigadores?
Los investigadores realizaron búsquedas exhaustivas en la literatura hasta el 17 de octubre de 2018 y encontraron tres estudios (93 participantes) que cumplieron con los criterios de inclusión. También se identificó un estudio en curso. Todos los estudios fueron de tamaño pequeño y con algunos problemas de calidad. Un estudio pequeño (21 participantes) comparó ocho semanas de tratamiento con cigarrillos de cannabis que contenían 115 mg de D9‐tetrahidrocannabinol (THC) con cigarrillos placebo que contenían cannabis con THC extraído, en pacientes con enfermedad de Crohn activa en quienes había fracasado al menos un tratamiento médico. Aunque no se observaron diferencias en las tasas de remisión clínica, más participantes del grupo de cannabis presentaron mejoría de los síntomas de enfermedad de Crohn que los participantes del grupo placebo. Se observaron más efectos secundarios en el grupo del cigarrillo de cannabis en comparación con placebo. Estos efectos secundarios se consideraron leves e incluyeron somnolencia, náuseas, dificultad para concentrarse, pérdida de memoria, confusión y mareos. Los participantes del grupo del cigarrillo de cannabis informaron de mejoría en el dolor, el apetito y la satisfacción con el tratamiento.
Un estudio pequeño (22 participantes) comparó aceite de cannabis (10 mg de cannabidiol dos veces al día) con aceite placebo (es decir, aceite de oliva) en pacientes con enfermedad de Crohn activa en quienes había fracasado al menos un tratamiento médico. No se observaron diferencias en las tasas de remisión clínica. No hubo diferencias en los efectos secundarios graves. Entre los efectos secundarios graves, se incluyó el empeoramiento de la enfermedad de Crohn en un participante de cada grupo.
Un estudio pequeño (50 participantes) comparó aceite de cannabis (compuesto de 15% de cannabidiol y 4% de THC) con aceite placebo en participantes con enfermedad de Crohn activa. Se observaron diferencias positivas en la calidad de vida y en el índice de actividad de la enfermedad de Crohn.
Conclusiones
Los efectos del cannabis y del aceite de cannabis en la enfermedad de Crohn no están claros. No se pueden establecer conclusiones firmes con respecto a los efectos beneficiosos y perjudiciales (p.ej., efectos secundarios) del cannabis y del aceite de cannabis en pacientes adultos con enfermedad de Crohn. No se han investigado los efectos del cannabis y el aceite de cannabis en los pacientes con enfermedad de Crohn en remisión. Se necesitan estudios adicionales con un gran número de participantes para evaluar los efectos beneficiosos y perjudiciales potenciales del cannabis en la enfermedad de Crohn. Los estudios futuros deben evaluar los efectos del cannabis en los pacientes con enfermedad de Crohn activa e inactiva. Se deben investigar diferentes dosis y formas farmacéuticas del cannabis (p.ej., aceite de cannabis o comprimidos).
Authors' conclusions
Summary of findings
| Cannabis cigarettes (115 mg THC) compared to placebo cigarettes for the treatment of active Crohn's disease | ||||||
| Patient or population: participants with active Crohn's disease | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with placebo cigarettes | Risk with cannabis cigarettes (115 mg THC) | |||||
| Proportion of patients achieving clinical remission Follow‐up: 8 weeks | 100 per 1,000 | 455 per 1,000 | RR 4.55 | 21 | ⊕⊝⊝⊝ | Remission was defined as a CDAI score < 150 |
| Proportion of patients achieving clinical response Follow‐up: 8 weeks | 400 per 1,000 | 908 per 1,000 | RR 2.27 | 21 | ⊕⊝⊝⊝ | Response was defined as a 100‐point reduction of CDAI from baseline |
| CRP (mg/dL) at end of study Follow‐up: 8 weeks | 200 per 1,000 | 272 per 1,000 | RR 1.36 | 21 | ⊕⊕⊝⊝ | This study reported on the proportion of participants with a decrease in CRP of more than 0.5mg/dL from week 0 to week 8 |
| Quality of life Short‐Form 36 health survey (SF‐36) Follow‐up: 8 weeks | See comments | SF‐36 scores range from 0 to 100 with a higher score indicating better quality of life This study reported a 28 point increase in the SF‐36 score from baseline in the cannabis group compared to a 5 point increase in the placebo group (standard deviations were not reported) | ||||
| Adverse events Follow‐up: 8 weeks | 200 per 1,000 | 818 per 1,000 | RR 4.09 | 21 | ⊕⊝⊝⊝ | Adverse events included sleepiness, nausea, difficulty with concentration, memory loss, confusion and dizziness |
| Serious adverse events | Not reported | This outcome was not reported | ||||
| Withdrawal due to adverse events | Not reported | This outcome was not reported | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to high risk of bias for blinding of participants and other bias (cannabis participants were about 10 years older than placebo participants) 2 Downgraded two levels due to very serious imprecision (6 events) 3 Downgraded two levels due to very serious imprecision (14 events) 4 We did not downgrade for risk of bias as this would have no impact on CRP which is an objective outcome 5 Downgraded two levels due to very serious imprecision (5 events) 6 Downgraded two levels due to very serious imprecision (11 events) | ||||||
| Cannabis oil (5% cannabidiol sublingual oil) compared to placebo for the treatment of active Crohn's disease | ||||||
| Patient or population: participants with active Crohn's disease | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with placebo | Risk with cannabis oil (5% cannabidiol sublingual oil) | |||||
| Proportion of patients achieving clinical remission Follow‐up: 8 weeks | 333 per 1,000 | 400 per 1,000 | RR 1.20 | 19 | ⊕⊝⊝⊝ | Remission was defined as a CDAI score < 150 |
| Proportion of patients achieving clinical response | Not reported | This outcome was not reported | ||||
| CRP (mg/dL) at end of study | Not reported | This outcome was not reported | ||||
| Quality of life | Not reported | This outcome was not reported | ||||
| Adverse events Follow‐up: 8 weeks | See comments | Adverse events were rated on a scale from one to seven and included headache, sleepiness, nausea and dizziness The proportion of participants in each group who had an adverse event was not reported | ||||
| Serious adverse events Follow‐up: 8 weeks | 111 per 1,000 | 100 per 1,000 | RR 0.90 | 19 | ⊕⊝⊝⊝ | There was one serious adverse event in each group. Both were worsening Crohn's disease that required rescue intervention |
| Withdrawal due to adverse events | Not reported | This outcome was not reported | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to high risk of bias for other bias (60% of cannabis participants were smokers compared to none of the placebo participants) 2 Downgraded two levels due to very serious imprecision (7 events) 3 Downgraded two levels due to very serious imprecision (2 events) | ||||||
| Cannabis oil (15% cannabidiol and 4% THC) compared to placebo oil for the treatment of active Crohn's disease | ||||||
| Patient or population: participants with active Crohn's disease | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with placebo oil | Risk with cannabis oil (15% cannabidiol and 4% THC) | |||||
| Proportion of patients achieving clinical remission | Not reported | This outcome was not reported | ||||
| Proportion of patients achieving clinical response | Not reported | This outcome was not reported | ||||
| CRP (mg/dL) at end of study | Not reported | This outcome was not reported | ||||
| Quality of life Short‐Form 36 health survey (SF‐36) Follow‐up: 8 weeks | The mean SF‐36 score at 8 weeks was 79.9 | MD 16.4 higher | ‐ | 39 | ⊕⊕⊝⊝ | SF‐36 scores range from 0 to 100 with a higher score indicating better quality of life |
| Adverse events | Not reported | This outcome was not reported | ||||
| Serious adverse events | Not reported | This outcome was not reported | ||||
| Withdrawal due to adverse events | Not reported | This outcome was not reported | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to very serious imprecision (39 participants) | ||||||
Background
Cannabis is a widely used recreational drug which alters sensory perception and causes euphoria (Tibirica 2010). It has been promoted as a treatment for a variety of diseases such as cancer, glaucoma and autoimmune diseases (Hill 2015). Cannabis has also been hypothesized to improve disease activity in Crohn’s disease via modulation of the endocannabinoid system (Tibirica 2010). The endocannabinoid system has been shown to help regulate brain function and the immune system (Klein 2006).
Studies have found a higher prevalence of cannabis use in people with IBD who claim it relieves symptoms such as abdominal pain, diarrhoea, and reduced appetite (Lal 2011; Weiss 2015). It is unclear if this is due to the known psychotropic effects of cannabis such as analgesia and euphoria or if it is related to anti‐inflammatory effects demonstrated in recent studies and experimental animal models (Hasenoehrl 2016; Klein 2006; Singh 2012). There is also evidence that cannabis use in people with Crohn's disease has potential for harm. Cannabis has been associated with higher risk of surgery in people with Crohn's disease (Storr 2014). Cannabinoids have been associated with an increased risk of transient adverse events including weakness, dizziness, and diarrhea (Whiting 2015). Despite these conflicting data, physicians are often asked to prescribe cannabis in the context of a rapidly growing medical cannabis industry (Fletcher 2013).
There were no placebo‐controlled trials evaluating the use of cannabis in people with IBD until the first randomized, prospective, placebo‐controlled trial was published in 2013 (Naftali 2013). This study raised important questions regarding the exact role of cannabis in treating people with Crohn's disease: Does cannabis lead to symptomatic improvement only or does it also objectively reduce inflammation? Is cannabis safe when used by people with Crohn's disease?
Description of the condition
Crohn’s disease (CD) is a chronic immune‐mediated condition of transmural inflammation in the gastrointestinal tract. CD is associated with significant morbidity and decreased quality of life (Lahat 2012; Rubin 2004). In North America, the prevalence of CD is estimated to range from 26 to 199 cases per 100,000 person‐years (Friedman 2012).
CD can affect anywhere from the mouth to the perianal area. The pathophysiology of this condition is multifactorial and people may have a genetic predisposition (Friedman 2012). CD is thought to arise from a dysregulated immune response towards commensal microbiota and dietary contents in the gastrointestinal tract (Friedman 2012). This leads to an inappropriate inflammatory cascade of activated T cells secreting excessive pro‐inflammatory cytokines such as interleukin‐1 (IL‐1), IL‐6, and tumor necrosis factor‐alpha (TNF‐α) (Friedman 2012). This results in damage to previously healthy tissues.
CD is characterized by periods of relapse and remission (Friedman 2012). Symptoms may include low grade fevers, malaise, diarrhea, crampy abdominal pain, or hematochezia (Friedman 2012). The site of inflammation influences the symptoms. Complications of CD include fistula and abscess formation, perforations and fibrotic strictures (Friedman 2012; Lahat 2012).
Usual treatment options for CD include anti‐inflammatory and immunosuppressant agents (Friedman 2012). Commonly used drugs are aminosalicylates, sulfasalazine, corticosteroids, thiopurine drugs, methotrexate and biologic therapies such as anti‐TNF‐α agents (Friedman 2012). Management includes control of acute exacerbations, induction of remission, and maintenance of remission.
Description of the intervention
Cannabis sativa consists of numerous compounds called cannabinoids, of which delta 9‐tetrahydrocannabinol (THC) is the main psychotropic component (Klein 2006). Many natural and synthetic cannabinoids have been found and studied including cannabidiol, cannabinol, cannabigerol, and dronabinol (Klein 2006). Some of these cannabinoids are psychoactive, whereas others are not (Klein 2006). Multiple experimental animal models have shown anti‐inflammatory properties of various cannabinoids (Klein 2006).
How the intervention might work
The endocannabinoid system helps regulate the central nervous sytem, peripheral tissues, and multiple immune cells (Tibirica 2010). This system consists of cannabinoid (CB) receptors 1 and 2, several endogenous ligands called 'endocannabinoids', and associated enzymes (Hasenoehrl 2016; Klein 2006). Multiple studies have shown that the endocannabinoid system helps control physiologic functions of the gut including motility, secretion and epithelial barrier integrity (Coutts 1998; Hasenoehrl 2016; Pinto 2002; Vianna 2012). This makes the endocannabinoid system a potential therapeutic target for gastrointestinal diseases. Cannabis and cannabinoids appear to influence this system via CB1 and CB2 receptors and other mechanisms (Hasenoehrl 2016; Klein 2006).
CB1 receptors are widely expressed in the gastrointestinal tract, central nervous system and peripheral tissues such as blood vessels (Hasenoehrl 2016; Klein 2006). In the GI tract, the CB1 receptors are found in the enteric nervous system, the epithelial lining, plasma cells, and smooth muscle cells of blood vessels (Hasenoehrl 2016). CB1 receptor activation may reduce gastric emptying, intestinal transit time, as well as reduce colonic propulsion (Pinto 2002). The brain‐gut axis also influences motility and CB1 receptors in the vagus nerve are part of normal motility (Vianna 2012). CB1 receptors modulate the release of multiple neurotransmitters in the central nervous system causing central effects such as a reduction in pain and nausea (Klein 2006; Tibirica 2010). Activation of the CB1 receptor may enhance epithelial wound closure in the colon (Wright 2005). There is also evidence that upregulation of CB1 receptors and activation of CB1 receptors physiologically protects the colon during excessive inflammation in the colon (Massa 2004).
CB2 receptors are mainly expressed in immune cells, myenteric plexus neurons, and in epithelial cells during ulcerative colitis (Hasenoehrl 2016; Klein 2006; Marquez 2009). CB2 receptors are expressed on immune cells such B‐cells, NK cells and macrophages (Klein 2006). CB2 activation leads to T‐cell apoptosis and decreased proliferation in colitis (Singh 2012). CB2 activation also decreases the recruitment of neutrophils, T cells and macrophages to the inflamed colon (Singh 2012).
Other receptors in the GI tract have been found to be endocannabinoid‐responsive through mechanisms separate from CB1 and CB2 receptors (Hasenoehrl 2016). These include the peroxisome proliferator‐activated receptor alpha, the G‐protein coupled receptor 55, and transient receptor potential cation channel subfamily V member 1 (Hasenoehrl 2016). Cannabinoids also help modulate chemokine and cytokine release (Klein 2006).
Why it is important to do this review
This review was undertaken to evaluate the strength of evidence for the use of cannabis and cannabinoids as treatment for CD. It will help clarify if this therapy leads to objective physiological improvement beyond subjective and psychotropic scores. Further, we hope to evaluate various modes of consumption and assess for adverse effects.
Objectives
The primary objective was to assess the efficacy and safety of cannabis for induction and maintenance of remission in people with Crohn’s disease.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled intervention trials were considered for inclusion. Studies published as abstracts were only included if the authors could be reached for further information to allow for evaluation of quality and main outcomes.
Types of participants
Adults (> 18 years of age) with Crohn’s disease (as defined by the included studies) were considered for inclusion. Clinical remission or quiescent disease was defined by the Crohn's Disease Activity Index (CDAI). Participants with active (e.g. CDAI > 150) or quiescent disease (defined as mild or absent symptoms prior to entering the study or by a CDAI < 150) were included. People with surgically‐induced remission were excluded.
Types of interventions
Studies comparing any form of cannabis or its cannabinoid derivatives (natural or synthetic) to placebo or an active therapy for Crohn’s disease were included. We also included studies that assessed different cannabis or cannabinoid doses. An attempt was made to analyze dose response if data were available.
Types of outcome measures
Primary outcomes
The primary outcome was remission at study endpoint for induction of remission studies (as defined by a CDAI < 150) and relapse (e.g. CDAI > 150) at study endpoint for maintenance studies. Any validated scoring system such as the CDAI or Disease Activity Score (DAS) was included.
Secondary outcomes
Secondary outcomes included:
1. Clinical response;
2. Endoscopic remission;
3. Endoscopic improvement;
4. Histological response;
5. Quality of life;
6. CRP and fecal calprotectin measurements;
7. Adverse events;
8. Serious adverse events;
9. Withdrawal due to adverse events; and
10. Cannabis dependence and withdrawal effects.
Search methods for identification of studies
Electronic searches
We searched the following databases from inception up to 17 October 2018: MEDLINE, Embase, AMED (Allied & Alternative Medicine), PsychINFO, the Cochrane IBD Group Specialized Register, CENTRAL, ClinicalTrials.Gov, and the European Clinical Trials Register.
We searched abstracts from major gastroenterological meetings to identify research published in abstract form. We also contacted authors in this field for upcoming publications. The electronic search strategy is reported in Appendix 1.
Searching other resources
Conference proceedings were searched to identify studies published in abstract form. We also searched the references of applicable studies and systematic reviews to identify additional studies. We searched ClinicalTrials.gov and the EU Clinical Trials Register to identify ongoing studies.
Data collection and analysis
Selection of studies
Study papers and abstracts were identified by the literature search and reviewed. Two authors (TK and NC) independently screened the search results to identify potentially relevant studies for full text evaluation. The studies selected for full text review were independently assessed by two authors (TK and NC) and consensus for study inclusion and exclusion was reached through discussion. Any conflicts regarding inclusion or exclusion were resolved through discussion and by consultation with a third author (JKM) as necessary. Studies published in abstract form were only be included if the authors could be reached for further information.
Data extraction and management
Two authors (TK and NC) independently extracted the outcome data of interest from each study. Any conflicts were resolved by discussion and consensus or by consultation with a third author (JKM) as necessary. If data were missing or unclear, the study authors were contacted for clarification.
Other information extracted from the studies included:
a. Study characteristics and design;
b. Characteristics of participants;
c. Inclusion and exclusion criteria;
d. Interventions; and
e. Outcomes scoring methods.
Assessment of risk of bias in included studies
Two authors (TK and NC) independently assessed the methodological quality of included studies using the Cochrane risk of bias tool (Higgins 2011a). Any conflicts were resolved by discussion and consensus or by consultation with a third author (JKM) as necessary. Items assessed included:
1. Random sequence generation;
2. Allocation sequence concealment;
3. Blinding of participants, personnel and assessment of outcome;
4. Incomplete outcome data;
5. Selective outcome reporting; and
6. Other potential sources of bias.
Each category was evaluated as low, high or unclear risk. Judgment justification was provided in the Characteristics of included studies section of the review.
GRADE Analysis
The overall quality of the evidence supporting the primary outcome and selected secondary outcomes was evaluated using the GRADE criteria (Guyatt 2008; Schünemann 2011). Using this approach, outcome data were rated high, moderate, low or very low certainty. Outcome data from randomized controlled trials begins as high certainty, but could be downgraded based on several criteria. These criteria included:
1. Risk of bias from the studies;
2. Indirect evidence (by comparison, population, setting);
3. Inconsistency (i.e. unexplained heterogeneity);
4. Imprecision in data (i.e. few events and wide confidence intervals); and
5. Likelihood of publication bias.
Measures of treatment effect
For dichotomous outcomes, we calculated the risk ratio (RR) and corresponding 95% confidence interval (CI). For continuous outcomes, we calculated the mean difference (MD) and corresponding 95% CI .
Unit of analysis issues
For multi‐arm trials with a single placebo group and two treatment dose groups, we planned to split the placebo group in half to avoid a unit of analysis error (Higgins 2011b). To avoid potential carry‐over effects, we planned to only include the first part of the study (i.e. before the cross‐over) for any cross‐over studies (Higgins 2011b).
For studies where events reoccurred, we included the proportion of participants who experienced at least one event (i.e. the first event). When there were repeated observations on participants, we used the primary endpoint defined by the study. We did not find study designs applicable to cannabis in Crohn’s disease where multiple treatment attempts were used. We did not find any available cluster‐randomized studies.
Dealing with missing data
Data were analyzed on an intention‐to‐treat basis. Studies were evaluated for missing data and where explanations were not provided, the patient outcome was considered to be a treatment failure. For dichotomous outcomes, we dealt with missing data by treating missing participants as treatment failures. We counted failures as a relapse for maintenance studies and as failure to enter remission for induction studies.
We conducted an available case analysis for missing continuous outcomes. For missing standard deviations of continuous outcomes, we imputed standard deviations where reasonably possible. Sensitivity analysis was used to assess the impact of any imputation.
Assessment of heterogeneity
We planned to assess statistical heterogeneity using the Chi2 test and I2 statistic. For the Chi2 test, a P value of less than 0.1 would be considered statistically significant. We planned to use the I2 statistic to assess the degree of statistical heterogeneity. We planned to investigate heterogeneity by visually inspecting the forest plots to identify outliers. If outliers were identified, we would conduct sensitivity analysis to explore potential explanations for the heterogeneity. If significant heterogeneity was identified, a random‐effects model would be used. We planned to not pool data for meta‐analysis when a high degree of heterogeneity was detected (e.g. I2 > 75%).
Assessment of reporting biases
We assessed selective reporting by comparing outcomes pre‐specified in study protocols to those reported in study manuscripts. If protocols were not available for the included studies, we assessed reporting bias by comparing the outcomes specified in the methods section of the manuscript to those reported in the results section. If there were more than 10 included studies in a pooled analysis, we planned to investigated publication bias by constructing funnel plots (Egger 1997).
Data synthesis
We planned to combine data from individual trials when the interventions, patient groups and outcomes were sufficiently similar (determined by consensus). When pooling studies was not possible, we narratively summarized the results of individual trials. For dichotomous outcomes, we planned to calculate the pooled RR and 95% CI using a fixed‐effect model. For continuous outcomes, we planned to calculate the pooled MD and corresponding 95% CI. For continuous outcomes that utilized different scales to measure the same underlying construct, we planned to calculate the standardized mean difference (SMD) and corresponding 95% CI.
Subgroup analysis and investigation of heterogeneity
We attempted to perform subgroup analyses by dose and formula (e.g. based on dose of THC, dose of cannabidiol , or combination formula) when the data allowed for such comparisons. Other subgroup analyses considered included an effect based on disease location, cigarette smoking status, history of biologic therapy and failure of biologic therapy.
Sensitivity analysis
We planned to perform a sensitivity analysis based on risk of bias. However, there were no studies were pooled for analysis because of differences in the interventions.
Results
Description of studies
Results of the search
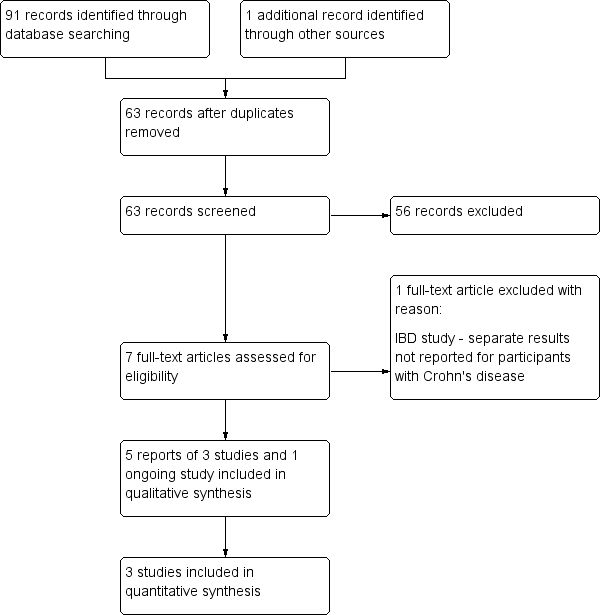
A literature search conducted on 17 October 2018 identified 91 studies. After duplicates were removed, a total of 63 studies remained for screening. Fifty‐six of these studies were not applicable. Seven studies remained for full‐text review. One study was excluded (Naftali 2013b). Five reports of three studies (93 participants) met the inclusion criteria and were included in the review (See Figure 1). One ongoing study was also identified (NCT03467620).

Flow diagram.
Included studies
Naftali 2013a was a randomized, single‐centre, double‐blind, placebo‐controlled trial. The purpose of the study was to determine whether cannabis can induce remission in participants with active Crohn’s disease. Participants were given either cannabis cigarettes containing 115 mg of THC twice daily or placebo cigarettes composed of cannabis flowers from which the THC had been extracted. Participants were treated for eight weeks. Twenty‐two people were randomized, but 21 participants were studied (cannabis n = 11; placebo n = 10). One person declined participation after signing consent, but before receiving any study drugs. Inclusion criteria were an established diagnosis of Crohn’s disease, at least 20 years of age, and active Crohn’s disease (with a calculated CDAI score between 200 and 450 points) at study entry. All participants had failed at least one form of medical treatment for the disease including mesalamine, corticosteroids, thiopurines, methotrexate, or anti–TNF‐α. Anti–TNF‐α failure was declared after at least four doses. Participants receiving corticosteroids had to be receiving a stable dose for at least one month prior to study entry, and participants receiving thiopurines had to be receiving a stable dose for at least three months prior to entry. Participants were followed at weeks 0, 2, 8, and 10 (2 weeks after treatment done). The primary outcome was induction of remission, defined as a CDAI score of 150 or less after 8 weeks of cannabis treatment. Secondary outcomes included response rate, defined as a 100‐point reduction of CDAI from baseline, a reduction of at least 0.5 mg in C‐reactive protein (CRP), or improvement in quality of life of at least 50 points, as measured by the Short‐Form 36 (SF‐36) health survey. Adverse effects were assessed by questionnaire and severity was assessed on a scale from one to seven, with one meaning no symptoms and seven corresponding with severe symptoms.
Naftali 2017a was a randomized, single‐centre, double‐blind, placebo‐controlled trial. The purpose of the study was to assess the effects of cannabidiol in participants with active Crohn’s disease. Participants were given either 2 ml twice daily of cannabis oil at a concentration of 5 mg/ml (i.e. 20 mg/day or approximately 5% cannabidiol) or placebo containing pure olive oil 2 ml twice daily. Twenty‐one participants were recruited, one withdrew consent before any consumption of the study drug and one was withdrawn due to colitis. Nineteen participants completed the study. Participants were at least 20 years of age, had active Crohn’s disease with a calculated CDAI score between 200 and 450 points, and received at least one form of medical treatment for Crohn’s disease with no effect. Previous treatments included mesalamine, corticosteroids, thiopurines, methotrexate, or anti‐TNF‐α. Participants receiving corticosteroids had to be on a stable dose for at least one month. Participants receiving thiopurines had to be on a stable dose for at least three months, and participants receiving anti‐TNF‐α had received at least four infusions before failure was declared. Participants were visited at weeks 0, 2, 8, and 10. The primary outcome was a reduction of 70 points in CDAI from week 0 to week 8. Secondary outcomes included any adverse events within the time frame of eight weeks, ability to stop steroids in participants who were treated with steroids at the beginning of the study, and reduction in at least 1 mg/dl in the CRP level. Adverse effects were assessed by questionnaire as described for Naftali 2013a
Naftali 2017b was an abstract presented at the International Association of Cannabis Medicine in September 2017. This study was sent to us by the first author. It is a randomized, double‐blind, placebo‐controlled trial looking at the effect of cannabis on Crohn's disease. Participants were randomized to either cannabis oil (15% cannabidiol and 4% THC) or placebo oil for eight weeks of treatment. The cannabis oil group had 24 participants and the placebo oil group had 26 participants. Inclusion criteria were not specified. Outcomes included the CDAI, inflammatory markers and quality of life as measured by the Short‐Form 36 (SF‐36) health survey. These outcomes were assessed before, during and after treatment.
Excluded studies
Naftali 2013b was excluded because we were not able to acquire separate data for participants with Crohn's disease and ulcerative colitis. The study included 10 people with ulcerative colitis and 22 people with Crohn's disease.
Risk of bias in included studies
Bias was assessed using the Cochrane risk of bias tool. The risk of bias results are summarized in Figure 2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Random sequence generation was rated as low risk of bias for all three studies given the use of the block randomization.
Allocation concealment was rated as unclear risk of bias for Naftali 2013a as the methods for allocation concealment were not described. Naftali 2017a and Naftali 2017b were rated as low risk of bias for allocation concealment. Both studies used sequentially numbered drug containers of identical appearance. .
Blinding
Blinding was performed for both participants and investigators in all three studies. Both Naftali 2017a and Naftali 2017b used identical placebos and were rated as low risk of bias. However, blinding was not effective in Naftali 2013a due to the psychotropic effects of cannabis. Almost all participants were aware of their study allocation with the exception of two participants in the placebo group, before the end of the study. As a result we decided to rate Naftali 2013a as high risk of bias for blinding of participants. Outcome assessors were blinded in all three studies and this item was rated as low risk of bias.
Incomplete outcome data
Incomplete outcome data were rated as unclear for Naftali 2013a and low risk of bias for Naftali 2017a and . Naftali 2017b. There was a higher drop out rate in the placebo group of the Naftali 2013a study compared to the cannabis group (three placebo versus one cannabis). Alternatively, there were no drop outs for the Naftali 2017a and Naftali 2017b studies and therefore, incomplete outcome data was rated as low risk of bias.
Selective reporting
All three studies were rated as unclear risk of bias for selective reporting. The protocol for the Naftali 2013a study pre‐specified the primary outcome as clinical response (reduction in CDAI of 70‐points from baseline). In the manuscript the authors reported on clinical remission (CDAI < 150) as the primary outcome. We note that clinical remission is a more stringent outcome than clinical response and that this is not strong evidence of selective reporting to bias the results in favour of the intervention. The study protocol also included change in IL‐10, IL‐2, and TGF beta as secondary outcomes and these outcomes were not reported in the final study manuscript. The protocol for the Naftali 2017a study also pre‐specified the primary outcome as clinical response (reduction in CDAI of 70‐points from baseline). In the manuscript the authors reported on clinical remission (CDAI < 150) as the primary outcome. Again we note that clinical remission is a more stringent outcome than clinical response and that this is not strong evidence of selective reporting to bias the results in favour of the intervention. The study protocol also included a reduction of at least 1mg/dL in the serum CRP levels and this was not reported in the final manuscript. The Naftali 2017b was published as an abstract. The abstract reported on a pre‐specified secondary outcome (quality of life) but did not report on the pre‐specified primary outcome from the study protocol (clinical response defined by a 100‐point reduction in CDAI) or other pre‐specified outcomes (e.g. clinical remission). However, these outcomes could be reported on in the full study manuscript.
Other potential sources of bias
Naftali 2013a was rated as high risk of bias for other potential sources of bias because participants in the cannabis participants were significantly older than participants in the placebo group. Naftali 2017a was rated as high risk of bias because there were significantly more smokers in the cannabis oil group than the placebo group. Sixty per cent of the cannabis oil group smoked compared to none of the placebo group. The Naftali 2017b study was rated as low risk of bias..
Effects of interventions
See: Summary of findings for the main comparison Cannabis cigarettes (115 mg THC) compared to placebo cigarettes for the treatment of active Crohn's disease; Summary of findings 2 Cannabis oil (5% cannabidiol sublingual oil) compared to placebo oil for the treatment of active Crohn's disease; Summary of findings 3 Cannabis oil (15% cannabidiol and 4% THC) compared to placebo oil for the treatment of active Crohn's disease
Data from the three included studies were not pooled due to the different routes of administration and formula composition for the two studies that used cannabis oil. The Naftali 2013a study participants took 115 mg of THC in the form of cigarettes (twice daily) and the Naftali 2017a study participants took cannabis oil at a concentration of 5% cannabidiol. The Naftali 2017b study utilized cannabis oil at a concentration of 15% cannabidiol and 4% THC.
Cannabis cigarettes (115 mg THC) versus placebo cigarettes at 8 weeks:
Clinical remission rates at eight weeks were higher in the cannabis cigarettes group compared to placebo cigarettes (Naftali 2013a). Clinical remission was reported in 45.5% (5/11) of participants in the treatment group compared to 10% (1/10) of participants in the placebo group (RR 4.55, 95% CI 0.63 to 32.56; very low certainty evidence). Clinical response was reported in 90.9% (10/11) of participants in the treatment group compared to 40% (4/10) of participants in the placebo group (RR 2.27, 95% CI 1.04 to 4.97; very low certainty evidence). There was no difference in serum CRP levels measured at the end of the study. A decrease in CRP of more than 0.5mg/dL from week 0 to week 8 was found in 27% (3/11) of participants in the treatment group compared to 20% (2/10) of participants in the placebo group (RR 1.36, 95% CI 0.28 to 6.56; low certainty evidence). There was an increase in the quality of life scores in the treatment group compared to the placebo group. There was an increase of 28 points in the treatment group from baseline to week 8, compared to a difference of 5 points in the placebo group from baseline to week 8. None of the participants experienced difficulty or withdrawal symptoms when they stopped the cannabis treatment after eight weeks. We acquired the prevalence of adverse effects from the author, and the cannabis group had more adverse events compared to the placebo. Eighty‐two per cent (9/11) of participants in the cannabis group had an adverse event compared to 20% (2/10) of placebo participants (RR 4.09, 95% CI 1.15 to 14.57; very low certainty evidence). However, these adverse events were considered to be mild in nature and included sleepiness, nausea, difficulty with concentration, memory loss, confusion and dizziness. Participants in the cannabis group reported improvements in pain, appetite and satisfaction. Endoscopic remission, endoscopic response, histological response, serious adverse events and withdrawal due to adverse events were not reported in this study.
Cannabis oil (5% cannabidiol sublingual oil) versus placebo oil at 8 weeks:
There was no difference in remission rates at eight weeks in the small study (n = 19) that compared cannabis oil (5% cannabidiol sublingual oil) to placebo oil (Naftali 2017a). Clinical remission was reported in 40% (4/10) of participants in the cannabis oil group compared to 33.3% (3/9) of participants in the placebo group (RR 1.20, 95% CI 0.36 to 3.97; very low certainty evidence). There was no difference in the proportion of participants who had a serious adverse event. Ten per cent (1/10) of participants in the cannabis oil group had a serious adverse event compared to 11% (1/9) of placebo participants (RR 0.90, 95% CI 0.07 to 12.38; very low certainty evidence). In both cases the serious adverse event was worsening Crohn's disease that required rescue intervention. The participants did not report any withdrawal symptoms when treatment was stopped. Although the study protocol stated they were going to assess clinical response (reduction of 70 points in the CDAI from week 0 to 8) as the primary outcome, and reduction in CRP level, the final data for these outcomes were not reported. Additionally, endoscopic remission, endoscopic response and histological response were not assessed in this study. Adverse effects were rated on a scale from one to seven and included headache, sleepiness, nausea and dizziness. The authors reported that adverse effects did not differ between the cannabis oil and placebo groups.
Cannabis oil (15% cannabidiol and 4% THC) versus placebo oil at 8 weeks:
The small study (n = 39) comparing cannabis oil (15% cannabidiol and 4% THC) to placebo oil found differences in CDAI scores and quality of life scores as measured by the SF‐36 instrument. The mean quality of life score after 8 weeks of treatment was 96.3 in the cannabis oil group compared to 79.9 in the placebo group (MD 16.40, 95% CI 5.72 to 27.08, low certainty evidence). After 8 weeks of treatment, the mean CDAI score was 118.6 in the cannabis oil group compared to 212.6 in the placebo group (MD ‐94.00, 95%CI ‐148.86 to ‐39.14, low certainty evidence). The abstract did not report on any other outcomes.
Discussion
Summary of main results
This systematic review included three small randomized controlled trials (93 participants) that evaluated the efficacy and safety of cannabis and cannabis oil (cannabidiol) in Crohn's disease. Overall, there were sparse data and heterogenous outcomes. Each study used a different dose of cannabis or cannabidiol formula. Naftali 2013a compared cannabis cigarettes (115 mg THC) to placebo cigarettes. Naftali 2017a compared cannabis oil composed of 5% cannabidiol sublingual oil to a placebo oil. Naftali 2017b compared cannabis oil composed of 15% cannabidiol and 4% THC to a placebo oil. We were only able to extract limited data on quality of life (SF‐36) and CDAI scores from this study. None of the studies were pooled due to the different routes of administration and cannabidiol formulas. No studies were identified that assessed cannabis or cannabis oil therapy in people with quiescent Crohn's disease.
In the Naftali 2013a study, clinical remission and response rates were higher in the cannabis cigarette group than the placebo cigarette group at eight weeks. This study found no difference in serum CRP levels after eight weeks of treatment. Participants in the cannabis group were more likely than placebo participants to experience an adverse event. However, these adverse events were considered to be mild in nature and included sleepiness, nausea, difficulty with concentration, memory loss, confusion and dizziness. Participants in the cannabis group reported improvements in pain, appetite and satisfaction with treatment. These results should be interpreted with caution as the GRADE analysis indicated that the overall certainty of the evidence supporting these results was very low due to sparse data and high risk of bias. Thus, we are uncertain about the effects of cannabis cigarettes on Crohn's disease. Further research is needed before any strong conclusions can be drawn on the efficacy and safety of cannabis cigarettes in Crohn's disease.
The Naftali 2017a study found no difference in clinical remission rates at eight weeks or serious adverse events. One serious adverse event was reported in each group. In both cases the serious adverse event was worsening Crohn's disease that required rescue intervention. Reported adverse events included headache, sleepiness, nausea and dizziness. The GRADE analysis indicated that the overall certainty of the evidence supporting these results was very low due to sparse data and high risk of bias. Thus, we are uncertain about the effects of cannabis oil (5% cannabidiol) on Crohn's disease. Further research is needed before any strong conclusions can be drawn on the efficacy and safety of cannabis oil (5% cannabidiol) in Crohn's disease.
Lastly, the Naftali 2017b study compared cannabis oil (15% cannabidiol and 4% THC) to placebo. This study was presented as an abstract and only reported on quality of life and CDAI scores. Mean quality of life scores were higher in the cannabis oil group (96.3) compared to placebo (79.9). The mean difference between the cannabis oil and placebo groups was 16.4 points and this is likely to be a clinically meaningful improvement in health‐related quality of life in people with Crohn's disease (Irvine 1994; Irvine 2008). However, the GRADE analysis indicated that the overall certainty of the evidence for this outcome was low due to due to serious imprecision. Further research is needed before any firm conclusions can be drawn about potential quality of life benefits with cannabis oil (15% cannabidiol and 4% THC) therapy in Crohn's disease. Mean CDAI scores were lower in cannabis oil participants (118.6) compared to placebo participants (212.6). Although, the difference in CDAI is clinically meaningful (Brant 1999; Feagan 2004), this result should be interpreted with caution given the small number of participants who were assessed. Further research is needed before any firm conclusions can be drawn about potential benefits of cannabis oil in terms of improved disease activity.
There are significant risks of bias with the included studies and a paucity of data on adverse events (short‐term and long‐term). The existing studies excluded people with a history of mental illness, drug abuse, or previous cannabis consumption, or if in their physician’s judgement they might be vulnerable to drug addiction or mental instability (Naftali 2013a; Naftali 2017a). Hence, given the high prevalence of cannabis use and mental health disorders such as anxiety and depression in the Crohn's disease population, it is challenging to generalize the results of these small studies to all people with Crohn's disease.
We must weigh the possibility of small benefit of cannabis and cannabinoids in Crohn's disease against the well‐established harms and concerns of cannabis including mental health related concerns (Triantafillidis 2013). Cannabis use is associated with increased emergency department visits in people with gastrointestinal diseases (Gubatan 2015).
Co‐use of tobacco and cannabis is highly prevalent among cannabis users (Schauer 2016; Schauer 2017). Tobacco smoking in people with Crohn's disease leads to increased morbidity and smoking cessation improves outcomes (Johnson 2005). Further, there is concern that cannabis and tobacco are often combined in the same product (Schauer 2017). This is particularly worrisome in adolescents and young adults because of potential mental health symptoms (Ramo 2012). Mental health disorders such as anxiety and depression are prevalent among people with IBD and can negatively influence the course of IBD (Triantafillidis 2013). It is not known if cannabis smoking will increase concomitant tobacco use. People with Crohn's disease who use cannabis or cannabis oil may benefit from screening for tobacco use and counselling on smoking cessation. Close monitoring for adverse events in people with Crohn's disease who use cannabis may be beneficial given the lack of robust data and conversely, the presence of large body of data suggesting evidence of harm with cannabis use (Asbridge 2012; Gubatan 2015; Hackam 2015; Schauer 2016).
Overall completeness and applicability of evidence
This review included three small studies with a total of 93 participants, so completeness of evidence is a concern. More research is needed to be able to draw any firm conclusions about the efficacy and safety of cannabis in people with Crohn's disease. Although the results of this review may be applicable to persons with Crohn's disease there are some concerns with applicability because the included studies excluded people with a history of mental illness, drug abuse, or previous cannabis consumption. Both cannabis use and mental illness such as depression and anxiety are prevalent among people with IBD in North America (Hauser 2014; Weiss 2015).
Quality of the evidence
The Naftali 2013a study was rated as high risk of bias for blinding of participants and other bias (cannabis participants were older than placebo participants). Although the authors took care to assign placebo participants to identical placebo cigarettes, the majority of participants were able to figure out which group they were assigned to due to the psychotropic effects of cannabis. The Naftali 2017a study was rated as high risk of bias due to other bias. Sixty per cent of cannabis participants were smokers compared to none of the placebo participants. The Naftali 2017b study was rated as low risk of bias. Our assessment based on GRADE analyses suggests that the certainty of the evidence supporting the outcomes in this review is low to very low. As a result of this uncertainty no firm conclusions regarding the efficacy and safety of cannabis for Crohn's can be drawn.
Potential biases in the review process
We performed a comprehensive literature search to minimize bias related to study selection. Two authors (TK and NC) reviewed the studies for inclusion and exclusion, extracted data independently, and reviewed study quality. Limitations of this systematic review include a small number of studies with a small number of participants and sparse data. Two of the included studies were judged to be at high risk of bias (Naftali 2013a; Naftali 2017a). In addition, all three eligible studies were conducted by the same investigator (Naftali).
Agreements and disagreements with other studies or reviews
We found two systematic reviews that assessed the use of cannabis in Crohn's disease (Langhorst 2015; Volz 2016). Langhorst 2015 assessed all complementary and alternative medical treatments for inflammatory bowel disease and Volz 2016 assessed the use of cannabis in inflammatory bowel disease, irritable bowel syndrome and chronic pancreatitis. Both reviews included the Naftali 2013a study and both reviews had similar conclusions. Langhorst 2015 concluded that complementary and alternative therapies might be effective for the treatment of inflammatory bowel disease. Volz 2016 concluded that cannabis may be useful for symptom relief. Studies with higher methodological quality and larger numbers of participants are required to allow for more definitive conclusions on the efficacy and safety of cannabis for Crohn's disease.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Cannabis cigarettes (115 mg THC) versus placebo cigarettes, Outcome 1 Clinical remission at 8 weeks.

Comparison 1 Cannabis cigarettes (115 mg THC) versus placebo cigarettes, Outcome 2 Clinical response at 8 weeks.

Comparison 1 Cannabis cigarettes (115 mg THC) versus placebo cigarettes, Outcome 3 Adverse events.

Comparison 1 Cannabis cigarettes (115 mg THC) versus placebo cigarettes, Outcome 4 Decrease in CRP of more than 0.5 mg/dL from week 0 to week 8.

Comparison 2 Cannabis oil (5% cannabidiol sublingual oil) versus placebo oil, Outcome 1 Clinical remission at 8 weeks.

Comparison 2 Cannabis oil (5% cannabidiol sublingual oil) versus placebo oil, Outcome 2 Serious adverse events.

Comparison 3 Cannabis oil (15% cannabidiol and 4% THC) versus placebo oil, Outcome 1 Quality of life at 8 weeks.

Comparison 3 Cannabis oil (15% cannabidiol and 4% THC) versus placebo oil, Outcome 2 CDAI at 8 weeks.
| Cannabis cigarettes (115 mg THC) compared to placebo cigarettes for the treatment of active Crohn's disease | ||||||
| Patient or population: participants with active Crohn's disease | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with placebo cigarettes | Risk with cannabis cigarettes (115 mg THC) | |||||
| Proportion of patients achieving clinical remission Follow‐up: 8 weeks | 100 per 1,000 | 455 per 1,000 | RR 4.55 | 21 | ⊕⊝⊝⊝ | Remission was defined as a CDAI score < 150 |
| Proportion of patients achieving clinical response Follow‐up: 8 weeks | 400 per 1,000 | 908 per 1,000 | RR 2.27 | 21 | ⊕⊝⊝⊝ | Response was defined as a 100‐point reduction of CDAI from baseline |
| CRP (mg/dL) at end of study Follow‐up: 8 weeks | 200 per 1,000 | 272 per 1,000 | RR 1.36 | 21 | ⊕⊕⊝⊝ | This study reported on the proportion of participants with a decrease in CRP of more than 0.5mg/dL from week 0 to week 8 |
| Quality of life Short‐Form 36 health survey (SF‐36) Follow‐up: 8 weeks | See comments | SF‐36 scores range from 0 to 100 with a higher score indicating better quality of life This study reported a 28 point increase in the SF‐36 score from baseline in the cannabis group compared to a 5 point increase in the placebo group (standard deviations were not reported) | ||||
| Adverse events Follow‐up: 8 weeks | 200 per 1,000 | 818 per 1,000 | RR 4.09 | 21 | ⊕⊝⊝⊝ | Adverse events included sleepiness, nausea, difficulty with concentration, memory loss, confusion and dizziness |
| Serious adverse events | Not reported | This outcome was not reported | ||||
| Withdrawal due to adverse events | Not reported | This outcome was not reported | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to high risk of bias for blinding of participants and other bias (cannabis participants were about 10 years older than placebo participants) 2 Downgraded two levels due to very serious imprecision (6 events) 3 Downgraded two levels due to very serious imprecision (14 events) 4 We did not downgrade for risk of bias as this would have no impact on CRP which is an objective outcome 5 Downgraded two levels due to very serious imprecision (5 events) 6 Downgraded two levels due to very serious imprecision (11 events) | ||||||
| Cannabis oil (5% cannabidiol sublingual oil) compared to placebo for the treatment of active Crohn's disease | ||||||
| Patient or population: participants with active Crohn's disease | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with placebo | Risk with cannabis oil (5% cannabidiol sublingual oil) | |||||
| Proportion of patients achieving clinical remission Follow‐up: 8 weeks | 333 per 1,000 | 400 per 1,000 | RR 1.20 | 19 | ⊕⊝⊝⊝ | Remission was defined as a CDAI score < 150 |
| Proportion of patients achieving clinical response | Not reported | This outcome was not reported | ||||
| CRP (mg/dL) at end of study | Not reported | This outcome was not reported | ||||
| Quality of life | Not reported | This outcome was not reported | ||||
| Adverse events Follow‐up: 8 weeks | See comments | Adverse events were rated on a scale from one to seven and included headache, sleepiness, nausea and dizziness The proportion of participants in each group who had an adverse event was not reported | ||||
| Serious adverse events Follow‐up: 8 weeks | 111 per 1,000 | 100 per 1,000 | RR 0.90 | 19 | ⊕⊝⊝⊝ | There was one serious adverse event in each group. Both were worsening Crohn's disease that required rescue intervention |
| Withdrawal due to adverse events | Not reported | This outcome was not reported | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to high risk of bias for other bias (60% of cannabis participants were smokers compared to none of the placebo participants) 2 Downgraded two levels due to very serious imprecision (7 events) 3 Downgraded two levels due to very serious imprecision (2 events) | ||||||
| Cannabis oil (15% cannabidiol and 4% THC) compared to placebo oil for the treatment of active Crohn's disease | ||||||
| Patient or population: participants with active Crohn's disease | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with placebo oil | Risk with cannabis oil (15% cannabidiol and 4% THC) | |||||
| Proportion of patients achieving clinical remission | Not reported | This outcome was not reported | ||||
| Proportion of patients achieving clinical response | Not reported | This outcome was not reported | ||||
| CRP (mg/dL) at end of study | Not reported | This outcome was not reported | ||||
| Quality of life Short‐Form 36 health survey (SF‐36) Follow‐up: 8 weeks | The mean SF‐36 score at 8 weeks was 79.9 | MD 16.4 higher | ‐ | 39 | ⊕⊕⊝⊝ | SF‐36 scores range from 0 to 100 with a higher score indicating better quality of life |
| Adverse events | Not reported | This outcome was not reported | ||||
| Serious adverse events | Not reported | This outcome was not reported | ||||
| Withdrawal due to adverse events | Not reported | This outcome was not reported | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to very serious imprecision (39 participants) | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical remission at 8 weeks Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Clinical response at 8 weeks Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Decrease in CRP of more than 0.5 mg/dL from week 0 to week 8 Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical remission at 8 weeks Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Serious adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Quality of life at 8 weeks Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 CDAI at 8 weeks Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |