Butóxido de piperonilo (BOP) combinado con piretroides en los mosquiteros tratados con insecticida para prevenir el paludismo en África
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [author‐defined order]
| Study characteristics | ||
| Methods | Cluster‐randomized controlled village trial | |
| Participants | Households with at least 1 adult resident and 1 child aged 2 to 10 years, Anopheles species | |
| Interventions | Control: LLIN, PermaNet 2.0 Intervention: LLIN, PermaNet 3.0 Control: LLIN, Olyset Net Intervention: LLIN, Olyset Plus | |
| Outcomes | Primary outcomes; parasite prevalence (proportion of thick blood smears that are positive for asexual parasites) in children ages 2 to 10 years, assessed before net distribution and 3 times after nets are distributed Secondary outcomes: prevalence of anaemia; mean haemoglobin in children ages 2 to 10 years; vector density; measures of LLIN ownership; coverage, use, and integrity | |
| Mosquito resistance status | Resistance ‐ high | |
| Net treatment | Nets unholed and unwashed | |
| Location(s) | Uganda ‐ East and West, 104 sub‐districts | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Recruitment bias | Low risk | No participants were recruited after clusters had been randomized |
| Were the mosquitoes in LLIN and LLIN + PBO groups comparable | Unclear risk | Resistance monitoring was not conducted at all study sites due to the size of the RCT |
| Collectors blinded | High risk | LLIN allocation was not masked; therefore risk of detection bias was high for entomological outcomes |
| Household blinded | Low risk | LLIN allocation was not masked, but this is unlikely to affect the primary outcome (parasite prevalence) |
| Treatment allocation (sequence randomly/adequately generated) | Low risk | Randomization was used to allocate clusters to study groups |
| Allocation concealment (selection bias) | Low risk | Randomization was carried out to allocate treatments to clusters |
| Were incomplete outcome data adequately addressed | Low risk | No outcome data were incomplete; intention‐to‐treat analysis was conducted |
| Were the raw data reported for LLIN and LLIN + PBO groups | Low risk | No outcome data were missing |
| Clusters lost to follow‐up | Unclear risk | 14 clusters were lost to follow‐up in the final time point (25 months) due to the COVID‐19 pandemic |
| Selective reporting (reporting bias) | Low risk | All intended outcomes stated in the pre‐published protocol were reported in the final publication |
| Correct statistical methods; adjusted for clustering | Low risk | Clustering was not taken into account and adjusted for during statistical analysis. Trial authors did however provide us with an ICC, so we could adjust for clustering |
| Trial authors' conflicting interest | Low risk | Trial authors declared no conflicting interests |
| Study characteristics | ||
| Methods | Village trial | |
| Participants | Ilara ‐ An gambiae (100% S‐form) | |
| Interventions | Control: LLIN, PermaNet 2.0 Intervention: LLIN, PermaNet 3.0 | |
| Outcomes | Mosquito mortality, blood feeding, sporozoite rate, mosquito density, parity rate | |
| Mosquito resistance status | Ilara ‐ resistant ‐ low (deltamethrin, 72.5% mortality, N = 120) | |
| Net treatment | Nets unholed and unwashed | |
| Location(s) | Ilara, Nigeria ‐ untreated net | |
| Notes | Trial conducted: March 2012 to March 2013 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Recruitment bias | Low risk | Recruiment bias is related to human participants and so is not applicable to this study |
| Were the mosquitoes in LLIN and LLIN + PBO groups comparable | Unclear risk | Mosquito species composition varied slightly pre‐trial and post‐trial between treatment villages. However, resistance level was the same |
| Collectors blinded | High risk | Not stated whether collectors where blinded; therefore judged as high risk, as this is likely to impact searching efforts |
| Household blinded | Low risk | Unclear whether households were blinded – not stated in the publication. We judged this as low risk, as it is unlikely to affect the outcome |
| Treatment allocation (sequence randomly/adequately generated) | Low risk | Villages were randomly assigned to treatment arms |
| Allocation concealment (selection bias) | Low risk | Allocation concealment procedures were not adhered to; however this is unlikely to affect the results |
| Were incomplete outcome data adequately addressed | Low risk | There were no incomplete data |
| Were the raw data reported for LLIN and LLIN + PBO groups | Low risk | All necessary data were reported |
| Clusters lost to follow‐up | Low risk | No clusters were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | It appears that all measured outcomes were reported |
| Correct statistical methods; adjusted for clustering | High risk | Study did not take clustering into account for statistical methods |
| Trial authors' conflicting interest | Low risk | Trial authors declared no conflicting interests; however the study was funded by Vestergaard (net manufacturers). Views and findings in the publication are stated to be those of the trial authors |
| Study characteristics | ||
| Methods | Experimental hut trial | |
| Participants | An coluzzii | |
| Interventions | Control: LLIN, DawaPlus 2.0 Intervention: LLIN, DawaPlus 3.0, DawaPlus 4.0 | |
| Outcomes | Mosquito mortality, blood feeding, deterrence, exophily | |
| Mosquito resistance status | Resistant ‐ high (6% mortality, N = 98) | |
| Net treatment | Nets holed, nets unwashed and washed (x 20) | |
| Location(s) | Vallée du Kou, Burkina Faso | |
| Notes | Trial conducted: August 2016 to October 2016 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Were the mosquitoes in LLIN and LLIN + PBO groups comparable | Low risk | The hut trial was conducted in the same area; therefore characteristics are similar |
| Collectors blinded | Unclear risk | Paper does not state whether collectors were blinded |
| Sleepers blinded | Unclear risk | Paper does not state whether sleepers were blinded |
| Sleeper bias | Low risk | Sleepers were rotated between huts according to a Latin square design |
| Treatment allocation (sequence randomly/adequately generated) | Low risk | Treatments were not randomly allocated to huts; however the trial completed a full rotation through the huts |
| Treatment rotation | Low risk | Treatments were rotated between huts according to a Latin square design + 2 weeks |
| Standardized hut design | Low risk | Huts were built previously according to standard West African design |
| Hut cleaning between treatments | Unclear risk | Trial authors do not state whether huts were cleaned between treatments |
| Were incomplete outcome data adequately addressed | Low risk | No data were incomplete |
| Were the raw data reported for LLIN and LLIN + PBO groups | Low risk | All necessary data were reported |
| Trial authors' conflicting interest | Low risk | Trial authors declare no conflicting interest in the WHOPES report |
| Study characteristics | ||
| Methods | Village trial | |
| Participants | An gambiae s.s. | |
| Interventions | Control: LLIN, Olyset Net, PermaNet 2.0 Intervention: LLIN, Olyset Plus, PermaNet 3.0 | |
| Outcomes | Sporozoite rate, mosquito density, parity rate | |
| Mosquito resistance status | Olyset Net villages ‐ resistance ‐ high (1% mortality, N = 305) | |
| Net treatment | Nets unholed and unwashed | |
| Location(s) | Sikasso region, Mali PermaNet 2.0 villages ‐ Beko East, Dalabani, Berila, Dierila | |
| Notes | Trial conducted: January 2014 to January 2015 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Recruitment bias | Low risk | Recruiment bias is related to human participants and so is not applicable to this study |
| Were the mosquitoes in LLIN and LLIN + PBO groups comparable | Unclear risk | Mosquito species composition is constant between villages; however resistance level varies slightly |
| Collectors blinded | High risk | Not stated whether collectors where blinded; therefore judged as high risk, as this is likely to affect searching efforts |
| Household blinded | Low risk | Unclear whether households were blinded – not stated in the publication. We judged this as low risk, as this is unlikely to affect the outcome |
| Treatment allocation (sequence randomly/adequately generated) | Low risk | Villages were randomly assigned to treatment arms |
| Allocation concealment (selection bias) | Low risk | Allocation concealment procedures were not adhered to; however this is unlikely to affect study results |
| Were incomplete outcome data adequately addressed | Low risk | No data were incomplete |
| Were the raw data reported for LLIN and LLIN + PBO groups | Low risk | All necessary data were reported |
| Clusters lost to follow‐up | Low risk | No clusters were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | It appears that all measured outcomes were reported |
| Correct statistical methods; adjusted for clustering | High risk | Study did not take clustering into account for statistical methods |
| Trial authors' conflicting interest | Low risk | Trial authors have no competing interests |
| Study characteristics | ||
| Methods | Experimental hut trial | |
| Participants | Vallée du Kou, Burkina Faso ‐ 100% An gambiae: M‐form (15%), S‐form (85%) Malanville, Benin ‐ 95% An gambiae: M‐form (100%), 5% An arabiensis Pitoa, Cameroon ‐ 5% An gambiae: S‐form (100%), 95% An arabiensis | |
| Interventions | Control: LLIN, PermaNet 2.0 Intervention: LLIN, PermaNet 3.0 | |
| Outcomes | Mosquito mortality, blood feeding, deterrence, exophily | |
| Mosquito resistance status | Vallée du Kou, Burkina Faso ‐ resistant – high (deltamethrin, 23% mortality, N = 100) Malanville, Benin ‐ resistant – low (deltamethrin, 85% mortality, N = 100) Pitoa, Cameroon ‐ resistant – low (deltamethrin, 70% mortality, N = 100) | |
| Net treatment | Nets holed, nets unwashed and washed (x 20) | |
| Location(s) | Vallée du Kou, Burkina Faso Malanville, Benin Pitoa, Cameroon | |
| Notes | Trial conducted: Vallée du Kou, Burkina Faso ‐ September 2007 to November 2007 Malanville, Benin ‐ July 2008 to September 2008 Pitoa, Cameroon ‐ July 2008 to September 2008 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Were the mosquitoes in LLIN and LLIN + PBO groups comparable | Low risk | Huts situated in the same area: mosquito characteristics will be the same |
| Collectors blinded | Unclear risk | Unclear whether collectors were blinded – not stated in the publication |
| Sleepers blinded | Unclear risk | Unclear whether sleeper was blinded – not stated in the publication |
| Sleeper bias | Low risk | Sleepers were rotated between huts according to a Latin square design |
| Treatment allocation (sequence randomly/adequately generated) | Low risk | Treatments were randomly allocated to huts |
| Treatment rotation | Low risk | Treatments were rotated between huts according to a Latin square design |
| Standardized hut design | Low risk | Huts were built according to a standard West African design |
| Hut cleaning between treatments | Unclear risk | Unclear whether huts were cleaned between treatments – not stated in the publication |
| Were incomplete outcome data adequately addressed | Low risk | No outcome data were incomplete |
| Were the raw data reported for LLIN and LLIN + PBO groups | Low risk | All necessary data were reported |
| Trial authors' conflicting interest | Low risk | Trial authors have no competing interests |
| Study characteristics | ||
| Methods | Experimental hut trial | |
| Participants | An gambiae s.s. | |
| Interventions | Control: LLIN, PermaNet 2.0 Intervention: LLIN, PermaNet 3.0 | |
| Outcomes | Mosquito mortality, deterrence, exophily | |
| Mosquito resistance status | Resistant ‐ high (deltamethrin, 10.6% mortality, N = 80 min) | |
| Net treatment | Nets not holed, nets unwashed and washed (x 20) | |
| Location(s) | Yaokoffikro, Côte d'Ivoire | |
| Notes | Trial conducted: April 2009 to July 2009 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Were the mosquitoes in LLIN and LLIN + PBO groups comparable | Low risk | Huts situated in the same area – mosquito characteristics will be the same |
| Collectors blinded | Unclear risk | Unclear whether collectors were blinded – not stated in the publication |
| Sleepers blinded | Unclear risk | Unclear whether sleeper was blinded – not stated in the publication |
| Sleeper bias | Low risk | Sleepers were rotated between huts according to a Latin square design |
| Treatment allocation (sequence randomly/adequately generated) | Low risk | Treatments were not randomly allocated to the huts However, results from trials performed before this trial show no significant differences in attractiveness of the different huts |
| Treatment rotation | Low risk | Treatments were rotated between huts according to a Latin square design |
| Standardized hut design | Low risk | Huts were built according to a standard West African design |
| Hut cleaning between treatments | Low risk | All huts were cleaned between treatments |
| Were incomplete outcome data adequately addressed | Low risk | No outcome data were incomplete |
| Were the raw data reported for LLIN and LLIN + PBO groups | Low risk | All necessary data were reported |
| Trial authors' conflicting interest | Low risk | Trial authors declared they had no conflicting interests |
| Study characteristics | ||
| Methods | Experimental hut trial | |
| Participants | An arabiensis (100%), An funestus group (95% s.s.) | |
| Interventions | Control: LLIN, MAGNet LN Intervention: LLIN, Veeralin LN | |
| Outcomes | Mosquito mortality, blood feeding, deterrence, exophily | |
| Mosquito resistance status | An arabiensis ‐ susceptible (alpha‐cypermethrin, 100% mortality, N = 97) An funestus ‐ unclassified | |
| Net treatment | Nets holed, nets unwashed and washed (x 20) | |
| Location(s) | Ifakara, Tanzania | |
| Notes | Although additional data provided, they show resistance to deltamethrin and permethrin in An gambiae s.l. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Were the mosquitoes in LLIN and LLIN + PBO groups comparable | Low risk | The hut trial was conducted in the same area; therefore characteristics are similar |
| Collectors blinded | Unclear risk | Paper does not state whether collectors were blinded |
| Sleepers blinded | Unclear risk | Paper does not state whether sleepers were blinded |
| Sleeper bias | Low risk | Sleepers were rotated between huts according to a Latin square design |
| Treatment allocation (sequence randomly/adequately generated) | Low risk | Treatments were not randomly allocated to huts; however the trial completed a full rotation through the huts |
| Treatment rotation | Low risk | Treatments were rotated between huts according to a Latin square design |
| Standardized hut design | Low risk | Study used the standard design of the Ifakara experimental huts |
| Hut cleaning between treatments | Unclear risk | The paper does not state whether huts were cleared between treatments |
| Were incomplete outcome data adequately addressed | Low risk | No outcome data were incomplete |
| Were the raw data reported for LLIN and LLIN + PBO groups | Low risk | No outcome data were missing |
| Trial authors' conflicting interest | Low risk | Trial authors declared they received prescribed standard fees from Vestergaard Frandsen for evaluating its pesticide products; however this is standard practice |
| Study characteristics | ||
| Methods | Village trial | |
| Participants | An gambiae s. l., An funestus group | |
| Interventions | Control: LLIN, Olyset Net, PermaNet 2.0 Intervention: LLIN, Olyset Plus, PermaNet 3.0 | |
| Outcomes | Mosquito density, parity rate | |
| Mosquito resistance status | An funestus (Balaka district) Permethrin ‐ resistant ‐ moderate (55.5% mortality, N = unknown) Deltamethrin ‐ resistant ‐ high (14.9% mortality, N = unknown) An gambiae (Balaka district) Permethrin ‐ resistant ‐ low (84.4% mortality, N = unknown) (Machinga district) Deltamethrin ‐ resistant ‐ moderate (54.5% mortality, N = unknown) | |
| Net treatment | Nets unholed and unwashed | |
| Location(s) | Balaka district, Malawi (12 villages) | |
| Notes | Trial conducted: December 2012 to June 2014 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Recruitment bias | Low risk | Recruiment bias is related to human participants and so is not applicable to this study |
| Were the mosquitoes in LLIN and LLIN + PBO groups comparable | Unclear risk | Mosquito species composition and resistance status are not recorded per village. Village names are not provided in the study; instead villages are grouped by treatment type |
| Collectors blinded | High risk | Not stated whether collectors were blinded; therefore judged as high risk, as this is likely to affect searching effort |
| Household blinded | Low risk | Unclear whether households were blinded – not stated in the publication. We judged this as low risk, as this is unlikely to affect the outcome |
| Treatment allocation (sequence randomly/adequately generated) | Low risk | Villages were randomly assigned to treatment arms |
| Allocation concealment (selection bias) | Low risk | Allocation concealment procedures were not adhered to; however this is unlikely to affect the results |
| Were incomplete outcome data adequately addressed | Low risk | No outcome data were incomplete |
| Were the raw data reported for LLIN and LLIN + PBO groups | Low risk | All necessary data were reported |
| Clusters lost to follow‐up | Low risk | No clusters were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | It appears that all measured outcomes were reported |
| Correct statistical methods; adjusted for clustering | High risk | Study did not take clustering into account when statistical methods were performed |
| Trial authors' conflicting interest | Unclear risk | No information on trial authors' possible conflicting interests is provided |
| Study characteristics | ||
| Methods | Experimental hut trial | |
| Participants | An gambiae | |
| Interventions | Control: LLIN, PermaNet 2.0 Intervention: LLIN, PermaNet 3.0 | |
| Outcomes | Mosquito mortality, blood feeding, deterrence, exophily | |
| Mosquito resistance status | Proxy data. Adjara, Benin: resistant ‐ moderate (deltamethrin, 50% mortality, N = 56) (Aïzoun 2013) | |
| Net treatment | Nets holed, nets unwashed and washed (x 20) | |
| Location(s) | Akron, Benin | |
| Notes | Trial conducted: October 2008 to January 2009 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Were the mosquitoes in LLIN and LLIN + PBO groups comparable | Low risk | Huts were situated in the same area – mosquito characteristics will be the same |
| Collectors blinded | Unclear risk | Unclear whether collectors were blinded – not stated in the publication |
| Sleepers blinded | Unclear risk | Unclear whether sleeper was blinded – not stated in the publication |
| Sleeper bias | Low risk | Sleepers were rotated between huts according to a Latin square design |
| Treatment allocation (sequence randomly/adequately generated) | Low risk | Treatments were randomly allocated to huts |
| Treatment rotation | Low risk | Treatments were rotated between huts according to a Latin square design |
| Standardized hut design | Low risk | Huts were built according to a standard West African design |
| Hut cleaning between treatments | Low risk | All huts were cleaned between treatments |
| Were incomplete outcome data adequately addressed | Low risk | No outcome data were incomplete |
| Were the raw data reported for LLIN and LLIN + PBO groups | Low risk | All necessary data were reported |
| Trial authors' conflicting interest | Unclear risk | The trial was sponsored by Vestergaard (net manufacturers), which also commented on the manuscript |
| Study characteristics | ||
| Methods | Experimental hut trial | |
| Participants | 95% An gambiae: M‐form (100%), 5% An arabiensis (Corbel 2010) | |
| Interventions | Control: LLIN, Olyset Net Intervention: LLIN, Olyset Plus | |
| Outcomes | Mosquito mortality, blood feeding, deterrence, exophily | |
| Mosquito resistance status | Proxy data. Resistant ‐ high (permethrin, 22% mortality, N = 100) (Djègbè 2011) | |
| Net treatment | Nets holed, nets unwashed and washed (x 20) | |
| Location(s) | Malanville, Benin | |
| Notes | Trial conducted: September 2011 to December 2011 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Were the mosquitoes in LLIN and LLIN + PBO groups comparable | Low risk | Huts situated in the same area – mosquito characteristics will be the same |
| Collectors blinded | Unclear risk | Unclear whether collectors were blinded – not stated in the publication |
| Sleepers blinded | Unclear risk | Unclear whether sleeper was blinded – not stated in the publication |
| Sleeper bias | Low risk | Sleepers were rotated between huts according to a Latin square design |
| Treatment allocation (sequence randomly/adequately generated) | Low risk | Treatments were not randomized to huts but instead were rotated fully between all huts according to a Latin square design |
| Treatment rotation | Low risk | Treatments were rotated between huts according to a Latin square design |
| Standardized hut design | Low risk | Huts were built according to a standard West African design |
| Hut cleaning between treatments | Low risk | All huts were cleaned between treatments |
| Were incomplete outcome data adequately addressed | Low risk | No outcome data were incomplete |
| Were the raw data reported for LLIN and LLIN + PBO groups | Low risk | All necessary data were reported |
| Trial authors' conflicting interest | Low risk | Funders of the trial stated that they had no part in data collection, data analysis, or manuscript preparation |
| Study characteristics | ||
| Methods | Cluster‐randomized controlled village trial | |
| Participants | 3966 children analysed (21 months after intervention) aged 6 months to 14 years (excluding the severely ill), Anopheles species (pooled). Total core cluster population ranged from 14,845 to 16,358 | |
| Interventions | Control: LLIN, Olyset Net Intervention: LLIN, Olyset Plus | |
| Outcomes | Malaria parasite prevalence, sporozoite rate, mosquito density | |
| Mosquito resistance status | Resistance ‐ high (17.8% mortality, N = 107) | |
| Net treatment | Nets unholed and unwashed | |
| Location(s) | Muleba District, Tanzania | |
| Notes | Trial conducted: March 2014 to December 2016 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Recruitment bias | Low risk | No participants were recruited after clusters had been randomized |
| Were the mosquitoes in LLIN and LLIN + PBO groups comparable | Unclear risk | Resistance level was available only for the whole district ‐ not at the village level |
| Collectors blinded | Low risk | Field workers were masked to net treatment |
| Household blinded | Low risk | Inhabitants were masked to net treatment |
| Treatment allocation (sequence randomly/adequately generated) | Low risk | Restricted randomization was used to allocate clusters to study groups |
| Allocation concealment (selection bias) | Low risk | Restricted randomization was used to allocate treatments to clusters |
| Were incomplete outcome data adequately addressed | Low risk | No outcome data were incomplete |
| Were the raw data reported for LLIN and LLIN + PBO groups | Low risk | No outcome data were missing |
| Clusters lost to follow‐up | Low risk | No clusters were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | It appears that all measured outcomes were reported |
| Correct statistical methods; adjusted for clustering | Low risk | Clustering was taken into account and was adjusted for during statistical analysis |
| Trial authors' conflicting interest | Low risk | Trial authors declared no conflicting interests |
| Study characteristics | ||
| Methods | Village trial | |
| Participants | An gambiae | |
| Interventions | Control: LLIN, PermaNet 2.0 Intervention: LLIN, PermaNet 3.0 | |
| Outcomes | Sporozoite rate, mosquito density, parity rate | |
| Mosquito resistance status | Futa ‐ resistant ‐ moderate (33.3% mortality, N = 96) | |
| Net treatment | Nets unholed and unwashed | |
| Location(s) | Futa, Ghana ‐ no net control | |
| Notes | Trial conducted: November 2010 to August 2011 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Recruitment bias | Low risk | Recruiment bias is related to human participants and so is not applicable to this study |
| Were the mosquitoes in LLIN and LLIN + PBO groups comparable | Unclear risk | Mosquito species composition varied slightly. Resistance level varies between villages. However, pre‐trial and post‐trial data are provided |
| Collectors blinded | High risk | Not stated whether collectors were blinded; therefore judged as high risk, as this is likely to affect searching efforts |
| Household blinded | Low risk | Unclear whether households were blinded – not stated in the publication. We judged this as low risk, as this is unlikely to impact the outcome |
| Treatment allocation (sequence randomly/adequately generated) | Low risk | Villages were randomly assigned to treatment arms |
| Allocation concealment (selection bias) | Low risk | Allocation concealment procedures were not adhered to; however this is unlikely to affect the results |
| Were incomplete outcome data adequately addressed | Low risk | No outcome data were incomplete |
| Were the raw data reported for LLIN and LLIN + PBO groups | Low risk | All necessary data were reported |
| Clusters lost to follow‐up | Low risk | No clusters were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | It appears that all measured outcomes were reported |
| Correct statistical methods; adjusted for clustering | High risk | Study did not take clustering into account for statistical methods |
| Trial authors' conflicting interest | Unclear risk | Study data were collected for use in Vestergaard PermaNet 3.0 product dossier |
| Study characteristics | ||
| Methods | Experimental hut trial | |
| Participants | An coluzzii | |
| Interventions | Control: LLIN, PermaNet 2.0, Olyset Net Intervention: LLIN, PermaNet 3.0, Olyset Plus | |
| Outcomes | Mosquito mortality, blood feeding, deterrence, exophily | |
| Mosquito resistance status | Vallée du Kou 5 ‐ resistant – high (deltamethrin, 2.5% mortality, N = 163; permethrin, 5% mortality, N = 153) Tengrela ‐ resistant – high (deltamethrin, 34% mortality, N = 85; permethrin, 14% mortality, N = 101) | |
| Net treatment | Nets holed, nets unwashed | |
| Location(s) | Vallée du Kou 5, Burkina Faso Tengrela, Burkina Faso | |
| Notes | Trial conducted: September 2014 to October 2014 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Were the mosquitoes in LLIN and LLIN + PBO groups comparable | Low risk | Huts situated in the same area – mosquito characteristics will be the same |
| Collectors blinded | Unclear risk | Unclear whether collectors were blinded – not stated in the publication |
| Sleepers blinded | Unclear risk | Unclear whether sleeper was blinded – not stated in the publication |
| Sleeper bias | Low risk | Sleepers were rotated between huts according to a Latin square design |
| Treatment allocation (sequence randomly/adequately generated) | Low risk | Treatments were not randomized to huts but instead were rotated fully between all huts according to a Latin square design |
| Treatment rotation | Low risk | Treatments were rotated between huts according to a Latin square design |
| Standardized hut design | Low risk | Huts were built according to a standard West African design |
| Hut cleaning between treatments | Unclear risk | Unclear whether huts were cleaned between treatments – not stated in the publication |
| Were incomplete outcome data adequately addressed | Low risk | No outcome data were incomplete |
| Were the raw data reported for LLIN and LLIN + PBO groups | Low risk | All necessary data were reported |
| Trial authors' conflicting interest | Low risk | Trial authors had no competing interests |
| Study characteristics | ||
| Methods | Experimental hut trial | |
| Participants | An gambiae | |
| Interventions | Control: LLIN, PermaNet 2.0 Intervention: LLIN, PermaNet 3.0 | |
| Outcomes | Mosquito mortality, blood feeding, deterrence, exophily | |
| Mosquito resistance status | Susceptible (deltamethrin, 100% mortality, N = not stated) | |
| Net treatment | Nets holed, nets unwashed and washed (x 20) | |
| Location(s) | Zeneti, Muheza, Tanzania | |
| Notes | Trial conducted: July 2008 to October 2008 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Were the mosquitoes in LLIN and LLIN + PBO groups comparable | Low risk | Huts situated in the same area – mosquito characteristics will be the same |
| Collectors blinded | Unclear risk | Unclear whether collectors were blinded – not stated in the publication |
| Sleepers blinded | Unclear risk | Unclear whether sleeper was blinded – not stated in the publication |
| Sleeper bias | Low risk | Sleepers were rotated between huts according to a Latin square design |
| Treatment allocation (sequence randomly/adequately generated) | Low risk | Treatments were randomly allocated to huts |
| Treatment rotation | Low risk | Treatments were rotated between huts according to a Latin square design |
| Standardized hut design | Low risk | Huts were built according to a standard West African design |
| Hut cleaning between treatments | Low risk | All huts were cleaned between treatments |
| Were incomplete outcome data adequately addressed | Low risk | No outcome data were incomplete |
| Were the raw data reported for LLIN and LLIN + PBO groups | Low risk | All necessary data were reported |
| Trial authors' conflicting interest | Low risk | Trial authors had no competing interests |
| Study characteristics | ||
| Methods | Experimental hut trial | |
| Participants | An funestus | |
| Interventions | Control: LLIN, PermaNet 2.0, Olyset Net Intervention: LLIN, PermaNet 3.0, Olyset Plus | |
| Outcomes | Mosquito mortality, blood feeding, exophily | |
| Mosquito resistance status | Moderate | |
| Net treatment | Nets unwashed and holed | |
| Location(s) | Mibellon, Cameroon | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Were the mosquitoes in LLIN and LLIN + PBO groups comparable | Low risk | Huts situated in the same area – mosquito characteristics will be the same |
| Collectors blinded | Unclear risk | Unclear whether collectors were blinded – not stated in the publication |
| Sleepers blinded | Unclear risk | Unclear whether collectors were blinded – not stated in the publication |
| Sleeper bias | Low risk | Sleepers were rotated between huts according to a Latin square design |
| Treatment allocation (sequence randomly/adequately generated) | Low risk | Treatments were not randomized to huts but instead were rotated fully between all huts according to a Latin square design |
| Treatment rotation | Low risk | Treatments were rotated between huts according to a Latin square design |
| Standardized hut design | Low risk | Huts were built according to a standard West African design |
| Hut cleaning between treatments | Low risk | All huts were cleaned between treatments |
| Were incomplete outcome data adequately addressed | Low risk | No outcome data were incomplete |
| Were the raw data reported for LLIN and LLIN + PBO groups | Low risk | No outcome data were missing |
| Correct statistical methods; adjusted for clustering | Low risk | Clustering was not taken into account and adjusted for during statistical analysis. We adjusted for clustering by using an ICC value of 0.1 |
| Trial authors' conflicting interest | Low risk | Trial authors state that they have no competing interests |
| Study characteristics | ||
| Methods | Experimental hut trial | |
| Participants | An gambiae | |
| Interventions | Control: LLIN, MAGNet LN Intervention: LLIN, Veeralin LN | |
| Outcomes | Mosquito mortality, blood feeding, deterrence, exophily | |
| Mosquito resistance status | Low resistance | |
| Net treatment | Nets holed, nets unwashed and washed (x 20) | |
| Location(s) | M'be Côte d'Ivoire | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Were the mosquitoes in LLIN and LLIN + PBO groups comparable | Low risk | Huts situated in the same area – mosquito characteristics will be the same |
| Collectors blinded | Unclear risk | Unclear whether collectors were blinded – not stated in the publication |
| Sleepers blinded | Unclear risk | Unclear whether collectors were blinded – not stated in the publication |
| Sleeper bias | Low risk | Sleepers rotated between huts according to a Latin square design |
| Treatment allocation (sequence randomly/adequately generated) | Low risk | Treatments were randomly allocated to huts |
| Treatment rotation | Low risk | Treatment were rotated between huts according to a Latin Square design |
| Standardized hut design | Low risk | Huts were built previously according to standard West African hut design |
| Hut cleaning between treatments | Low risk | Huts were thoroughly cleaned and aired for a day at the end of each rotation |
| Were incomplete outcome data adequately addressed | Low risk | No outcome data were incomplete |
| Were the raw data reported for LLIN and LLIN + PBO groups | Low risk | No outcome data were missing |
| Correct statistical methods; adjusted for clustering | Low risk | Clustering was not taken into account and adjusted for during statistical analysis. We adjusted for clustering using an ICC value of 0.1 |
| Trial authors' conflicting interest | Low risk | Trial authors state that they have no conflicting interests |
An arabiensis: Anopheles arabiensis; An coluzzii: Anopheles coluzzii; An funestus: Anopheles funestus; An gambiae: Anopheles gambiae; ITN: insecticide‐treated net; LLIN: long‐lasting insecticidal net; PBO: piperonyl butoxide.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Study included laboratory data only | |
| Study included laboratory data only |
Characteristics of studies awaiting classification [ordered by study ID]
| Methods | Village trial |
| Participants | Bouaké ‐ 100% An gambiae: (70% S‐form, 30% M‐form) |
| Interventions | Control: LLIN, PermaNet 2.0 Extra Intervention: LLIN, PermaNet 3.0 |
| Outcomes | Blood feeding, mosquito density |
| Mosquito Resistance Status | Bouaké ‐ resistant ‐ moderate (43.9% mortality, N = 114) |
| Net Treatment | Nets unholed and unwashed |
| Location(s) | Bouaké, Côte d’Ivoire |
| Notes | Trial conducted: November 2009 to January 2012 |
| Methods | Not available |
| Participants | An funestus: Anopheles funestus; An gambiae: Anopheles gambiae |
| Interventions | |
| Outcomes | Not available |
| Mosquito Resistance Status | Not available |
| Net Treatment | Control: LLIN, Olyset Net Intervention: LLIN, Olyset Plus |
| Location(s) | Not available |
| Notes |
| Methods | Experimental hut trial |
| Participants | An funestus |
| Interventions | Control: LLIN, DawaPlus 2.0 Intervention: LLIN, DawaPlus 3.0, DawaPlus 4.0 |
| Outcomes | Mosquito mortality, blood feeding, deterrence, exophily |
| Mosquito Resistance Status | |
| Net Treatment | Nets holed, nets unwashed and washed (x 20) |
| Location(s) | Muheza, Tanzania |
| Notes |
Characteristics of ongoing studies [ordered by study ID]
| Study name | Comparative evaluation of standard insecticide‐treated bed nets and co‐treated bed nets on malaria prevalence in Sud Ubangi, Democratic Republic of Congo: a cluster‐randomised trial |
| Methods | Cluster‐randomized trial |
| Participants | Women (> 15 years) attending first ANC appointment at a clinic that is taking part in the study, who consent to be enrolled in the study 20 visitors per month at each of 7 antenatal clinics (held monthly) in each of 17 study clusters, which gives a total of approximately 2400 participants per month, 28,500 per year, and 86,000 in total |
| Interventions | Control: bed net treated with pyrethroid only Intervention: bed net treated with both pyrethroid and PBO |
| Outcomes | 1. Determination of parasite prevalence in women visiting monthly antenatal clinics 2. Entomological collections for surveillance of insecticide resistance and mosquito abundance and parasite infection 3. Assessment of bed net durability (physical and chemical analysis) and bio‐efficacy (against mosquitoes) over time |
| Starting date | November 2019 (recruitment start date 01/06/2020) |
| Contact information | Dr David Weetman |
| Notes |
| Study name | Effectiveness study of new‐generation bed nets in the context of conventional insecticide resistance in the Democratic Republic of the Congo (Net‐PBO) |
| Methods | Cluster‐randomized trial |
| Participants | 1680 participants; 0 to 10‐year‐old subjects in 30 villages |
| Interventions | Control: bed net treated with pyrethroid only Intervention: bed net treated with both pyrethroid and PBO (IRS and LSM included in trial) |
| Outcomes | Incidence rate of laboratory‐confirmed clinical cases of malaria (time frame: participants will be actively followed up for 12 months, and any suspected case of clinical malaria will immediately lead to microscopy and RDT for confirmation). Microscopy to confirm the diagnosis of malaria sporozoite rate (time frame: Anopheles mosquitoes will be captured every 3 months during 1 year), sporozoite detection by ELISA to determine infectivity of Anopheles |
| Starting date | 2 October 2017 |
| Contact information | |
| Notes |
| Study name | HS#2017‐3512. Adaptive interventions for optimizing malaria control: a cluster‐randomized SMART trial |
| Methods | Cluster‐randomized trial |
| Participants | 122,872 participants (6 months and older, all sexes) |
| Interventions | Other: regular long‐lasting insecticidal nets (Olyset) Other: LLIN plus piperonyl butoxide‐treated LLIN (Olyset Plus) |
| Outcomes | Annual clinical malaria incidence rate Malaria parasite prevalence Malaria vector density Malaria transmission intensity |
| Starting date | 01/12/2019 |
| Contact information | Dr Guiyun Yan |
| Notes |
| Study name | A preliminary study on designing a cluster randomized control trial of two mosquito nets to prevent malaria parasite infection |
| Methods | Cluster‐randomized trial |
| Participants | 1360 target participants Children targeted for malaria transmission survey are aged between 7 and 131 months Children between 60 and 131 months old are schoolchildren; 170 children are randomly selected from each cluster for survey |
| Interventions | Control: bed net treated with pyrethroid only Intervention: bed net treated with both pyrethroid and PBO |
| Outcomes | Plasmodium falciparum parasite infection after distribution of bed nets with PBO: PCR‐based infection Slide‐based infection Haemoglobin amount |
| Starting date | |
| Contact information | Dr Noboru Minakawa |
| Notes |
ELISA: enzyme‐linked immunosorbent assay; PBO: piperonyl butoxide.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Parasite prevalence (pyrethroid‐PBO nets vs non‐PBO LLINs, latest end points in RCT) Show forest plot | 2 | Odds Ratio (IV, Fixed, 95% CI) | 0.79 [0.67, 0.95] | |
| Analysis 1.1  Comparison 1: Commercial pyrethroid‐PBO nets versus commercial LLINs: village trials, Outcome 1: Parasite prevalence (pyrethroid‐PBO nets vs non‐PBO LLINs, latest end points in RCT) | ||||
| 1.2 Parasite prevalence (pyrethroid‐PBO nets vs non‐PBO LLINs, shown at 4 different time points) Show forest plot | 2 | Odds Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.2  Comparison 1: Commercial pyrethroid‐PBO nets versus commercial LLINs: village trials, Outcome 2: Parasite prevalence (pyrethroid‐PBO nets vs non‐PBO LLINs, shown at 4 different time points) | ||||
| 1.2.1 4 to 6 months | 2 | Odds Ratio (IV, Fixed, 95% CI) | 0.74 [0.62, 0.89] | |
| 1.2.2 9 to 12 months | 2 | Odds Ratio (IV, Fixed, 95% CI) | 0.72 [0.61, 0.86] | |
| 1.2.3 16 to 18 months | 2 | Odds Ratio (IV, Fixed, 95% CI) | 0.88 [0.74, 1.04] | |
| 1.2.4 21 to 25 months | 2 | Odds Ratio (IV, Fixed, 95% CI) | 0.79 [0.67, 0.95] | |
| 1.3 Mosquito sporozoite‐positive (adjusted ICC 0.1) Show forest plot | 4 | 424 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.24, 2.75] |
| Analysis 1.3  Comparison 1: Commercial pyrethroid‐PBO nets versus commercial LLINs: village trials, Outcome 3: Mosquito sporozoite‐positive (adjusted ICC 0.1) | ||||
| 1.4 Mosquito parous (adjusted ICC 0.1) Show forest plot | 3 | 220 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.82, 1.13] |
| Analysis 1.4  Comparison 1: Commercial pyrethroid‐PBO nets versus commercial LLINs: village trials, Outcome 4: Mosquito parous (adjusted ICC 0.1) | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Mosquito mortality (pooled) hut/night (adjusted ICC 0.1) Show forest plot | 10 | 15614 | Risk Ratio (M‐H, Random, 95% CI) | 1.43 [1.26, 1.62] |
| Analysis 2.1  Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 1: Mosquito mortality (pooled) hut/night (adjusted ICC 0.1) | ||||
| 2.1.1 Unwashed | 10 | 8647 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [1.29, 2.05] |
| 2.1.2 Washed | 8 | 6967 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [1.04, 1.38] |
| 2.2 Mosquito blood‐feeding success (pooled) hut/night (adjusted ICC 0.1) Show forest plot | 9 | 12351 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.66, 0.85] |
| Analysis 2.2  Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 2: Mosquito blood‐feeding success (pooled) hut/night (adjusted ICC 0.1) | ||||
| 2.2.1 Unwashed | 9 | 7261 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.57, 0.80] |
| 2.2.2 Washed | 7 | 5090 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.74, 1.02] |
| 2.3 Mosquito exophily (pooled) hut/night (adjusted ICC 0.1) Show forest plot | 10 | 13214 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.94, 1.06] |
| Analysis 2.3  Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 3: Mosquito exophily (pooled) hut/night (adjusted ICC 0.1) | ||||
| 2.3.1 Unwashed | 10 | 7699 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.91, 1.10] |
| 2.3.2 Washed | 8 | 5515 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.93, 1.07] |
| 2.4 Mosquito mortality (high resistance) hut/night (adjusted ICC 0.1) Show forest plot | 5 | 7997 | Risk Ratio (M‐H, Random, 95% CI) | 1.58 [1.34, 1.86] |
| Analysis 2.4  Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 4: Mosquito mortality (high resistance) hut/night (adjusted ICC 0.1) | ||||
| 2.4.1 Unwashed | 5 | 4896 | Risk Ratio (M‐H, Random, 95% CI) | 1.84 [1.60, 2.11] |
| 2.4.2 Washed | 4 | 3101 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.88, 1.63] |
| 2.5 Mosquito blood‐feeding success (high resistance) hut/night (adjusted ICC 0.1) Show forest plot | 4 | 7134 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.57, 0.76] |
| Analysis 2.5  Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 5: Mosquito blood‐feeding success (high resistance) hut/night (adjusted ICC 0.1) | ||||
| 2.5.1 Unwashed | 4 | 4458 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.50, 0.71] |
| 2.5.2 Washed | 3 | 2676 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.72, 0.92] |
| 2.6 Mosquito mortality (moderate resistance) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1027 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [1.21, 1.78] |
| Analysis 2.6  Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 6: Mosquito mortality (moderate resistance) hut/night (adjusted ICC 0.1) | ||||
| 2.6.1 Unwashed | 2 | 751 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.68 [1.33, 2.11] |
| 2.6.2 Washed | 1 | 276 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.74, 1.54] |
| 2.7 Mosquito blood‐feeding success (moderate resistance) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1034 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.78, 1.05] |
| Analysis 2.7  Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 7: Mosquito blood‐feeding success (moderate resistance) hut/night (adjusted ICC 0.1) | ||||
| 2.7.1 Unwashed | 2 | 752 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.72, 1.11] |
| 2.7.2 Washed | 1 | 282 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.74, 1.13] |
| 2.8 Mosquito mortality (low resistance) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1970 | Risk Ratio (M‐H, Random, 95% CI) | 1.30 [1.09, 1.56] |
| Analysis 2.8  Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 8: Mosquito mortality (low resistance) hut/night (adjusted ICC 0.1) | ||||
| 2.8.1 Unwashed | 2 | 948 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.99, 1.57] |
| 2.8.2 Washed | 2 | 1022 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [0.95, 2.04] |
| 2.9 Mosquito blood‐feeding success (low resistance) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1970 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.56, 1.57] |
| Analysis 2.9  Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 9: Mosquito blood‐feeding success (low resistance) hut/night (adjusted ICC 0.1) | ||||
| 2.9.1 Unwashed | 2 | 948 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.27, 2.11] |
| 2.9.2 Washed | 2 | 1022 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.49, 2.33] |
| 2.10 Mosquito mortality (susceptible) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1916 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.96, 1.15] |
| Analysis 2.10  Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 10: Mosquito mortality (susceptible) hut/night (adjusted ICC 0.1) | ||||
| 2.10.1 Unwashed | 2 | 948 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.64, 2.26] |
| 2.10.2 Washed | 2 | 968 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.92, 1.25] |
| 2.11 Mosquito blood‐feeding success (susceptible) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1916 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.40, 1.89] |
| Analysis 2.11  Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 11: Mosquito blood‐feeding success (susceptible) hut/night (adjusted ICC 0.1) | ||||
| 2.11.1 Unwashed | 2 | 948 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.12, 2.22] |
| 2.11.2 Washed | 2 | 968 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.82, 1.91] |
| 2.12 Mosquito mortality (high resistance/Permanet) hut/night (adjusted ICC 0.1) Show forest plot | 3 | 2806 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [1.26, 2.01] |
| Analysis 2.12  Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 12: Mosquito mortality (high resistance/Permanet) hut/night (adjusted ICC 0.1) | ||||
| 2.12.1 Not Washed | 3 | 1877 | Risk Ratio (M‐H, Random, 95% CI) | 1.81 [1.56, 2.10] |
| 2.12.2 Washed | 2 | 929 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.61, 2.28] |
| 2.13 Mosquito blood‐feeding success (high resistance/Permanet) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1943 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.45, 0.76] |
| Analysis 2.13  Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 13: Mosquito blood‐feeding success (high resistance/Permanet) hut/night (adjusted ICC 0.1) | ||||
| 2.13.1 Unwashed | 2 | 1439 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.40, 0.69] |
| 2.13.2 Washed | 1 | 504 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.61, 0.93] |
| 2.14 Mosquito mortality (high resistance/Olyset) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1410 | Risk Ratio (M‐H, Random, 95% CI) | 1.73 [1.51, 1.97] |
| Analysis 2.14  Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 14: Mosquito mortality (high resistance/Olyset) hut/night (adjusted ICC 0.1) | ||||
| 2.14.1 Unwashed | 2 | 1257 | Risk Ratio (M‐H, Random, 95% CI) | 1.72 [1.48, 1.99] |
| 2.14.2 Washed | 1 | 153 | Risk Ratio (M‐H, Random, 95% CI) | 1.81 [1.25, 2.61] |
| 2.15 Mosquito blood‐feeding success (high resistance/Olyset) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1470 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.40, 0.98] |
| Analysis 2.15  Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 15: Mosquito blood‐feeding success (high resistance/Olyset) hut/night (adjusted ICC 0.1) | ||||
| 2.15.1 Unwashed | 2 | 1257 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.38, 1.18] |
| 2.15.2 Washed | 1 | 213 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.27, 0.93] |
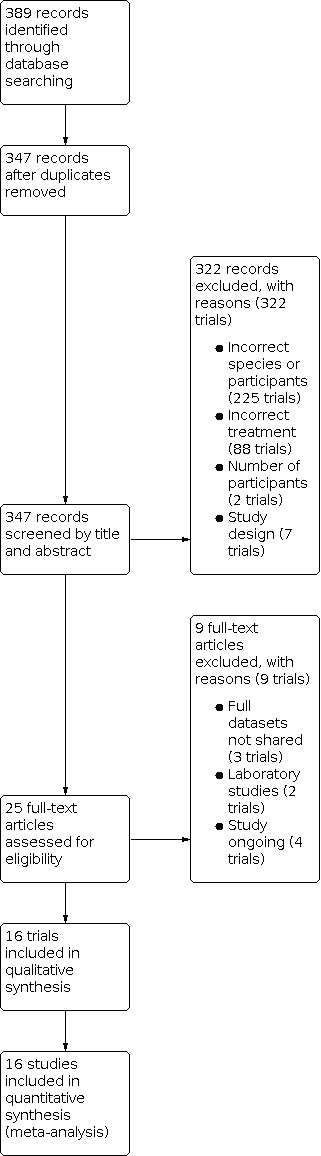
Study flow diagram.

‘Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1: Commercial pyrethroid‐PBO nets versus commercial LLINs: village trials, Outcome 1: Parasite prevalence (pyrethroid‐PBO nets vs non‐PBO LLINs, latest end points in RCT)

Comparison 1: Commercial pyrethroid‐PBO nets versus commercial LLINs: village trials, Outcome 2: Parasite prevalence (pyrethroid‐PBO nets vs non‐PBO LLINs, shown at 4 different time points)

Comparison 1: Commercial pyrethroid‐PBO nets versus commercial LLINs: village trials, Outcome 3: Mosquito sporozoite‐positive (adjusted ICC 0.1)

Comparison 1: Commercial pyrethroid‐PBO nets versus commercial LLINs: village trials, Outcome 4: Mosquito parous (adjusted ICC 0.1)

Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 1: Mosquito mortality (pooled) hut/night (adjusted ICC 0.1)

Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 2: Mosquito blood‐feeding success (pooled) hut/night (adjusted ICC 0.1)

Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 3: Mosquito exophily (pooled) hut/night (adjusted ICC 0.1)

Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 4: Mosquito mortality (high resistance) hut/night (adjusted ICC 0.1)

Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 5: Mosquito blood‐feeding success (high resistance) hut/night (adjusted ICC 0.1)

Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 6: Mosquito mortality (moderate resistance) hut/night (adjusted ICC 0.1)

Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 7: Mosquito blood‐feeding success (moderate resistance) hut/night (adjusted ICC 0.1)

Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 8: Mosquito mortality (low resistance) hut/night (adjusted ICC 0.1)

Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 9: Mosquito blood‐feeding success (low resistance) hut/night (adjusted ICC 0.1)

Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 10: Mosquito mortality (susceptible) hut/night (adjusted ICC 0.1)

Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 11: Mosquito blood‐feeding success (susceptible) hut/night (adjusted ICC 0.1)

Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 12: Mosquito mortality (high resistance/Permanet) hut/night (adjusted ICC 0.1)

Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 13: Mosquito blood‐feeding success (high resistance/Permanet) hut/night (adjusted ICC 0.1)

Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 14: Mosquito mortality (high resistance/Olyset) hut/night (adjusted ICC 0.1)

Comparison 2: Commercial pyrethroid‐PBO nets versus commercial LLINs: hut trials, Outcome 15: Mosquito blood‐feeding success (high resistance/Olyset) hut/night (adjusted ICC 0.1)
| Pyrethroid‐piperonyl butoxide (PBO) nets compared to long‐lasting insecticidal nets (LLINs) for malaria control when insecticide resistance is high | ||||||
| Patient or population: adults and childen living in malaria‐endemic areas, Anopheles gambiae complex or Anopheles funestus group | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants, | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with LLIN | Risk with pyrethroid‐PBO nets | |||||
| Parasite prevalence (4‐ to 6‐month follow‐up) | 254 per 1000a | 201 per 1000 (174 to 233)a | OR 0.74 (0.62 to 0.89) | 11,582 people (2 trials, 2 comparisons, 61 PBO clusters, 64 non‐PBO clusters) | ⊕⊕⊕⊕ | Pyrethroid‐PBO nets at 4‐ to 6‐month follow‐up reduce parasite prevalence in areas of high insecticide resistance |
| Parasite prevalence (9‐ to 12‐month follow‐up) | 224 per 1000a | 172 per 1000 (150 to 199)a | OR 0.72 (0.61 to 0.86) | 11,370 people (2 trials, 2 comparisons, 61 PBO clusters, 64 non‐PBO clusters) | ⊕⊕⊕⊝ due to inconsistency | Pyrethroid‐PBO nets at 9‐ to 12‐month follow‐up reduce parasite prevalence in areas of high insecticide resistance |
| Parasite prevalence (16‐ to 18‐month follow‐up) | 248 per 1000a | 225 per 1000 (196 to 255)a | OR 0.88 (0.74 to 1.04) | 11,822 people (2 trials, 2 comparisons, 61 PBO clusters, 64 non‐PBO clusters) | ⊕⊕⊕⊝ due to inconsistency | Pyrethroid‐PBO nets at 16‐ to 18‐month follow‐up reduce parasite prevalence in areas of high insecticide resistance |
| Parasite prevalence (21‐ to 25‐month follow‐up) | 350 per 1000a | 298 per 1000 (265 to 338)a | OR 0.79 (0.67 to 0.95) | 10,603 people (2 trials, 2 comparisons, 54 PBO clusters, 60 non‐PBO clusters) | ⊕⊕⊕⊝ due to inconsistency | Pyrethroid‐PBO nets at 21‐ to 25‐month follow‐up reduce parasite prevalence in areas of high insecticide resistance |
| Mosquito mortality (unwashed nets) | 238 per 1000a | 438 per 1000 | RR 1.84 | 14,620 mosquitoes | ⊕⊕⊕⊕ | Mosquito mortality is higher with unwashed pyrethroid‐PBO nets compared to standard unwashed LLINs in areas of high insecticide resistance |
| Mosquito mortality (washed nets) | 201 per 1000a | 242 per 1000 | RR 1.20 | 10,268 mosquitoes | ⊕⊝⊝⊝ due to imprecision and inconsistency | We do not know whether pyrethroid‐PBO nets have an effect on mosquito mortality in areas of high insecticide resistance when the nets have been washed |
| Blood‐feeding success (unwashed nets) | 438 per 1000a | 263 per 1000 | RR 0.60 (0.50 to 0.71)
| 14,000 mosquitoes | ⊕⊕⊕⊕ | Mosquito blood‐feeding success is decreased with unwashed pyrethroid‐PBO nets compared to standard unwashed LLINs in areas of high insecticide resistance |
| Blood‐feeding success (washed nets) | 494 per 1000a | 400 per 1000 | RR 0.81 | 9674 mosquitoes | ⊕⊕⊕⊕ | Mosquito blood‐feeding success is decreased with washed pyrethroid‐PBO nets compared to standard washed LLINs in areas of high insecticide resistance |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aOriginal numbers were used in this table; however in pooled analysis, events and total numbers were generated from cluster‐adjusted results, which use the effective sample size. Note that cluster adjustments do not change the point estimate of the effect size ‐ just the standard error. | ||||||
| Pyrethroid‐piperonyl butoxide (PBO) nets compared to long‐lasting insecticidal nets (LLINs) for malaria control when insecticide resistance is moderate | ||||||
| Patient or population:Anopheles gambiae complex or Anopheles funestus group | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of mosquitoes | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with LLIN | Risk with pyrethroid‐PBO nets | |||||
| Mosquito mortality (unwashed nets) | 180 per 1000a | 303 per 1000 | RR 1.68 | 1007 | ⊕⊕⊕⊝ due to imprecision | Mosquito mortality is probably higher with unwashed pyrethroid‐PBO nets compared to standard unwashed LLINs in areas of moderate insecticide resistance |
| Mosquito mortality (washed nets) | 287 per 1000a | 307 per 1000 | RR 1.07 | 329 | ⊕⊕⊝⊝ due to imprecision and indirectness | There may be little to no difference in the effect of washed pyrethroid‐PBO nets on mosquito mortality compared to standard washed LLINs (washed) in areas of moderate insecticide resistance |
| Blood‐feeding success (unwashed nets) | 258 per 1000a | 232 per 1000 | RR 0.90 | 1006 | ⊕⊕⊕⊝ due to imprecision | There is probably little to no difference in the effect of pyrethroid‐PBO nets (unwashed) on mosquito blood‐feeding success compared to standard LLINs in areas of moderate insecticide resistance |
| Blood‐feeding success (washed nets) | 586 per 1000a | 533 per 1000 | RR 0.91 | 329 | ⊕⊕⊝⊝ due to imprecision and indirectness | There may be little to no difference in the effect of washed pyrethroid‐PBO nets on mosquito blood‐feeding success compared to standard washed LLINs in areas of moderate insecticide resistance |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aOriginal numbers are used in this table; however for the pooled analysis, we generated events and total numbers from cluster‐adjusted results, which used the effective sample size. Note that cluster adjustments do not change the point estimate of the effect size, just the standard error. | ||||||
| Pyrethroid‐piperonyl butoxide (PBO) nets compared to long‐lasting insecticidal nets (LLINs) for malaria control when insecticide resistance is low | ||||||
| Patient or population:Anopheles gambiae complex or Anopheles funestus group | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of mosquitoes | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with LLINs | Risk with pyrethroid‐PBO nets | |||||
| Mosquito mortality (unwashed nets) | 527 per 1000a | 659 per 1000 | RR 1.25 | 1580 | ⊕⊕⊕⊝ due to imprecision | There is probably little to no difference in the effect of unwashed pyrethroid‐PBO nets on mosquito mortality compared to standard unwashed LLINs in areas of low insecticide resistance |
| Mosquito mortality (washed nets) | 394 per 1000a | 547 per 1000 | RR 1.39 | 1774 | ⊕⊝⊝⊝ due to imprecision and inconsistency | We do not know if pyrethroid‐PBO nets have an effect on mosquito mortality in areas of low insecticide resistance when the nets have been washed |
| Blood‐feeding success (unwashed nets) | 201 per 1000a | 151 per 1000 | RR 0.75 | 1580 | ⊕⊝⊝⊝ due to imprecision and inconsistency | We do not know if unwashed pyrethroid‐PBO nets have an effect on mosquito blood‐feeding success in areas of low insecticide resistance |
| Blood‐feeding success (washed nets) | 161 per 1000a | 172 per 1000 | RR 1.07 | 1774 | ⊕⊕⊝⊝ due to inconsistency | Mosquito blood‐feeding success may decrease with washed pyrethroid‐PBO nets compared to standard washed LLINs in areas of low insecticide resistance |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aOriginal numbers are used in this table; however for the pooled analysis, events and total numbers were generated from cluster‐adjusted results, which use the effective sample size. Note that cluster adjustments do not change the point estimate of the effect size, just the standard error. | ||||||
| Pyrethroid‐piperonyl butoxide (PBO) nets compared to long‐lasting insecticidal nets (LLINs) for malaria control when mosquitoes are susceptible | ||||||
| Patient or population:Anopheles gambiae complex or Anopheles funestus group Intervention: pyrethroid‐PBO nets | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of mosquitoes | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with LLINs | Risk with pyrethroid‐PBO nets | |||||
| Mosquito mortality (unwashed nets) | 392 per 1000a | 471 per 1000 | RR 1.20 | 2791 | ⊕⊕⊝⊝ due to imprecision | There may be little to no difference in the effect of unwashed pyrethroid‐PBO nets on mosquito mortality compared to standard unwashed LLINs in areas of no insecticide resistance |
| Mosquito mortality (washed nets) | 457 per 1000a | 489 per 1000 | RR 1.07 | 2644 | ⊕⊕⊝⊝ due to imprecision | There may be little to no difference in the effect of washed pyrethroid‐PBO nets on mosquito mortality compared to standard washed LLINs in areas of no insecticide resistance |
| Blood‐feeding success (unwashed nets) | 57 per 1000a | 29 per 1000 | RR 0.52 | 2791 | ⊕⊝⊝⊝ due to imprecision and inconsistency | We do not know if unwashed pyrethroid‐PBO nets have an effect on mosquito blood‐feeding success in areas of no insecticide resistance |
| Blood‐feeding success (washed nets) | 64 per 1000a | 82 per 1000 | RR 1.25 | 2644 | ⊕⊝⊝⊝ due to imprecision and inconsistency | We do not know if washed pyrethroid‐PBO nets have an effect on mosquito blood‐feeding success in areas of no insecticide resistance |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aOriginal numbers are used in this table; however for the pooled analysis, events and total numbers were generated from cluster‐adjusted results, which use the effective sample size. Note that cluster adjustments do not change the point estimate of the effect size, just the standard error. | ||||||
| WHOPES Phase | Definition |
|---|---|
| WHOPES Phase I. Laboratory bioassays | Cone bioassays: these studies are conducted in the laboratory setting and use standard WHO protocols (WHO 2013, Section 2.2.1), when mosquitoes are exposed to a suitable LLIN (treated intervention or untreated control) for three minutes using a standard plastic WHO cone. Following net exposure, mosquitoes are transferred to a holding container and are maintained on a sugar solution diet while entomological outcomes (mosquitoes knocked down 1 hour post exposure, and mosquito mortality 24 hours post exposure) are measured. Tunnel tests: these studies are conducted in the laboratory setting and use standard WHO protocols (WHO 2013, Section 2.2.2). Mosquitoes are released into a glass tunnel covered at each end with untreated netting. The intervention or control LLIN net sample is placed one‐third down the length of the tunnel, and the net contains 9 holes that enable mosquitoes to pass through. A suitable bait is immobilized in the shorter section of the tunnel, where it is available for mosquito biting. Mosquitoes are released into the opposite end of the tunnel and must make contact with the net and locate holes before they are able to feed on the bait. After 12 to 15 hours, mosquitoes are removed from both sections of the tunnel, and entomological outcomes (the number of mosquitoes in each section, mortality, and blood‐feeding inhibition at the end of the assay and 24 hours post exposure) are recorded. Wire‐ball bioassays: these studies are conducted in the laboratory setting, where mosquitoes are introduced into a wire‐ball frame that has been covered with the intervention or control LLIN. Mosquitoes are exposed for 3 minutes, after which they are transferred to a holding container, and entomological outcomes (mosquitoes knocked down 1 hour post exposure, and mosquito mortality 24 hours post exposure) are measured. |
| WHOPES Phase II. Experimental hut trials | WHOPES Phase II experimental hut trials are field trials conducted in Africa where wild mosquito populations or local colonized populations are evaluated. Volunteers or livestock sleep in experimental huts under a purposefully holed LLIN, with 1 person or animal per hut. Huts are designed to resemble local housing based on a West or East African design (WHO 2013; Section 3.3.1‐2). However these trials have identical design features, such as eave gaps or entry slits to allow mosquitoes to enter, and exit traps to capture exiting mosquitoes. LLINs and volunteers are randomly allocated to huts and are rotated in a Latin square to avoid bias, with huts cleaned between rotations to avoid contamination. Several nets, including an untreated control net, can be tested at the same time. Dead and live mosquitoes are collected each morning from inside the net, inside the hut, and inside the exit traps. They are then scored as blood‐fed or non‐blood‐fed, and as alive or dead, and live mosquitoes are maintained for a further 24 hours to assess delayed mosquito mortality. |
| WHOPES Phase III. Village trials | WHOPES Phase III village trials are conducted in Africa where wild mosquito populations are evaluated. Villages chosen to be included in the study are similar in terms of size, housing structure, location, and data available on insecticide resistance status of local malaria vectors. Households are assigned as conventional LLINs or PBO‐LLINs. Randomization can be done at the household or village level. Adult mosquitoes are collected from study houses, and mosquito density is measured. An indication of malaria transmission is measured at the study sites by recording infections in mosquitoes, parasite prevalence, or malaria incidence. |
| LLIN: long‐lasting insecticidal nets; PBO: piperonyl butoxide; WHOPES: World Health Organization Pesticide Evaluation Scheme. | |
| Product name | Product type | Status of WHO recommendation |
|---|---|---|
| DawaPlus 2.0 | Deltamethrin coated on polyester | Interim |
| DawaPlus 3.0 | Combination of deltamethrin coated onto polyester (side panels) and deltamethrin and PBO incorporated into polyester (roof) | Interim |
| DawaPlus 4.0 | Deltamethrin and PBO incorporated into polyester | Interim |
| Duranet | Alpha‐cypermethrin incorporated into polyethylene | Full |
| Interceptor | Alpha‐cypermethrin coated on polyester | Full |
| Interceptor G2 | Alpha‐cypermethrin and chlorfenapyr incorporated into polyester | Interim |
| LifeNet | Deltamethrin incorporated into polypropylene | Interim |
| MAGNet | Alpha‐cypermethrin incorporated into polyethylene | Full |
| MiraNet | Alpha‐cypermethrin incorporated into polyethylene | Interim |
| Olyset Net | Permethrin incorporated into polyethylene | Full |
| Olyset Plus | Permethrin (20 g/kg) and PBO (10 g/kg) incorporated into polyethylene | Interim |
| Panda Net 2.0 | Deltamethrin incorporated into polyethylene | Interim |
| PermaNet 2.0 | Deltamethrin coated on polyester | Full |
| PermaNet 3.0 | Combination of deltamethrin coated on polyester with strengthened border (side panels) and deltamethrin and PBO incorporated into polyethylene (roof) | Interim |
| Royal Sentry | Alpha‐cypermethrin incorporated into polyethylene | Full |
| SafeNet | Alpha‐cypermethrin coated on polyester | Full |
| Veeralin | Alpha‐cypermethrin and PBO incorporated into polyethylene | Interim |
| Yahe | Deltamethrin coated on polyester | Interim |
| Yorkool | Deltamethrin coated on polyester | Full |
| LLIN: long‐lasting insecticidal net; PBO: piperonyl butoxide; WHO: World Health Organization. | ||
| Insecticide | Formulation | Dosagea |
|---|---|---|
| Alpha‐cypermethrin | SC 10% | 20 to 40 |
| Cyfluthrin | EW 5% | 50 |
| Deltamethrin | SC 1% | 15 to 25 |
| Etofenprox | EW 10% | 200 |
| Lambda‐cyhalothrin | CS 2.5% | 10 to 15 |
| Permethrin | EC 10% | 200 to 500 |
| EC: emulsifiable concentrate; EW: emulsion, oil in water; CS: capsule suspension; SC: suspension concentrate; WT: water dispersible tablet. | ||
| Outcome | Confirmed resistance | Suspected resistance | Susceptible | Unclassified |
|---|---|---|---|---|
| WHO mosquito mortalitya | < 90% | 90% to 97% | 98% to 100% | Unknown |
| CDC knock‐downb | < 90% | 80% to 97% | 98% to 100% | Unknown |
| CDC: Centers for Disease Control and Prevention; WHO: World Health Organization. | ||||
| Outcome | Low | Moderate | High | Unclassified |
|---|---|---|---|---|
| Mosquito mortalitya | 61% to 90% | 31% to 60% | < 30% | Unknown |
| a24‐hour post‐exposure mortality (%). | ||||
| Criteria | Assessment | Comments | ||
|---|---|---|---|---|
| Yes | No | Unclear | ||
| Mosquito population | ||||
| Did the study test Anopheles gambiae complex or Anopheles funestus group mosquitoes? | ↓ | — | ↓ | State mosquito species |
| Were a minimum of 50 mosquitoes tested per study arm? | ↓ | — | ↓ | |
| Intervention | ||||
| Did the study include a long‐lasting insecticidal net (LLIN) or insecticide‐treated net (ITN)? | ↓ | — | ↓ | State net LLIN or ITN |
| Was the intervention net either of the following?
| ↓ | — | ↓ | State net type |
| Was the control net either of the following?
| ↓ | — | ↓ | State which objective study meets |
| Study design | ||||
| Was the study one of the following?
| ↓ | — | ↓ | State study type |
| For experimental hut study and village trial. Was the study conducted in Africa? | ↓ | — | ↓ | State country |
| Outcome | ||||
| Did the study include at least 1 of the following outcome measures?
| ↓ | — | ↓ | |
| Decision | ||||
| Is the study eligible for inclusion? | — | — | ↓ | State reason(s) for exclusion |
| Discuss with authors | ||||
| ITN: insecticide‐treated net; LLIN: long‐lasting insecticidal net; PBO: piperonyl butoxide; WHO: World Health Organization. | ||||
| Study ID | Locality | Net type | Net washed | Total number in ITN hut | Total number in UTN hut | Deterrence (%) reported | Deterrence (%) calculated |
|---|---|---|---|---|---|---|---|
| Vallée du Kou | DawaPlus 2.0 | No | 1548 | 1848 | 16.23 | 16.23 | |
| Vallée du Kou | DawaPlus 2.0 | Yes | 2155 | 1848 | 0 | ‐16.61 | |
| Vallée du Kou | DawaPlus 3.0 | No | 1365 | 1848 | 26.13 | 26.14 | |
| Vallée du Kou | DawaPlus 3.0 | Yes | 1981 | 1848 | 0 | ‐7.20 | |
| Vallée du Kou | DawaPlus 4.0 | No | 846 | 1848 | 54.22 | 54.22 | |
| Vallée du Kou | DawaPlus 4.0 | Yes | 1646 | 1848 | 10.93 | 10.93 | |
| Malanville | Permanet 2.0 | Yes | 195 | 285 | 31.58 | 31.58 | |
| Malanville | Permanet 3.0 | Yes | 210 | 285 | 26.32 | 26.32 | |
| Malanville | Permanet 2.0 | No | 243 | 285 | 14.74 | 14.74 | |
| Malanville | Permanet 3.0 | No | 214 | 285 | 24.91 | 24.91 | |
| Pitoa | Permanet 2.0 | Yes | 310 | 401 | 22.69 | 22.69 | |
| Pitoa | Permanet 3.0 | Yes | 163 | 401 | 59.35 | 59.35 | |
| Pitoa | Permanet 2.0 | No | 105 | 401 | 73.82 | 73.82 | |
| Pitoa | Permanet 3.0 | No | 146 | 401 | 63.59 | 63.59 | |
| Vallée du Kou | Permanet 2.0 | Yes | 788 | 908 | 13.22 | 13.22 | |
| Vallée du Kou | Permanet 3.0 | Yes | 724 | 908 | 20.26 | 20.26 | |
| Vallée du Kou | Permanet 2.0 | No | 329 | 908 | 63.77 | 63.77 | |
| Vallée du Kou | Permanet 3.0 | No | 463 | 908 | 49.01 | 49.01 | |
| Yaokoffikro | Permanet 3.0 | No | 303 | 796 | 62.1 | 61.93 | |
| Yaokoffikro | Permanet 2.0 | No | 317 | 796 | 60.4 | 60.18 | |
| Yaokoffikro | Permanet 3.0 | Yes | 313 | 796 | 60.1 | 60.68 | |
| Yaokoffikro | Permanet 2.0 | Yes | 281 | 796 | 64.4 | 64.70 | |
| Mibellon | PermaNet 2.0 | No | 237 | 390 | 39.2 | 39.2 | |
| Mibellon | PermaNet 3.0 | No | 153 | 390 | 60.8 | 60.8 | |
| Mibellon | Olyset Net | No | 176 | 390 | 54.9 | 54.9 | |
| Mibellon | Olyset Plus | No | 199 | 390 | 49 | 49 | |
| Ifakara | Veeralin LN | No | 722 | 810 | 11 | 10.86 | |
| Ifakara | Veeralin LN | Yes | 727 | 810 | 10 | 10.25 | |
| Ifakara | MAGNet LN | No | 1070 | 810 | 0 | ‐32.10 | |
| Ifakara | MAGNet LN | Yes | 773 | 810 | 5 | 4.57 | |
| Ifakara | Veeralin LN | No | 89 | 170 | 48 | 47.65 | |
| Ifakara | Veeralin LN | Yes | 85 | 170 | 50 | 50.00 | |
| Ifakara | MAGNet LN | No | 114 | 170 | 33 | 32.94 | |
| Ifakara | MAGNet LN | Yes | 103 | 170 | 39 | 39.41 | |
| Akron | Permanet 3.0 | No | 128 | 185 | 31 | 30.81 | |
| Akron | Permanet 3.0 | Yes | 155 | 185 | NR | 16.22 | |
| Akron | Permanet 2.0 | No | 114 | 185 | 38 | 38.38 | |
| Akron | Permanet 2.0 | Yes | 174 | 185 | NR | 5.95 | |
| Malanville | Olyset Plus | No | 67 | 69 | NR | 2.90 | |
| Malanville | Olyset Plus | Yes | 101 | 69 | NR | ‐46.38 | |
| Malanville | Olyset Net | No | 96 | 69 | NR | ‐39.13 | |
| Malanville | Olyset Net | Yes | 124 | 69 | NR | ‐79.71 | |
| Tengrela | Olyset Net | No | 923 | 480 | ‐92.29 | ‐92.29 | |
| Tengrela | Olyset Plus | No | 695 | 480 | ‐44.79 | ‐44.79 | |
| Tengrela | Permanet 2.0 | No | 858 | 480 | ‐78.75 | ‐78.75 | |
| Tengrela | Permanet 3.0 | No | 794 | 480 | ‐65.42 | ‐65.42 | |
| VK5 | Olyset Net | No | 1458 | 1095 | ‐33.15 | ‐33.15 | |
| VK5 | Olyset Plus | No | 1278 | 1095 | ‐16.71 | ‐16.71 | |
| VK5 | Permanet 2.0 | No | 1075 | 1095 | 1.83 | 1.83 | |
| VK5 | Permanet 3.0 | No | 657 | 1095 | 40 | 40.00 | |
| Zeneti | PermaNet 3.0 | No | 425 | 723 | 41 | 41.22 | |
| Zeneti | PermaNet 2.0 | No | 574 | 723 | 21 | 20.61 | |
| Zeneti | PermaNet 3.0 | Yes | 558 | 723 | 23 | 22.82 | |
| Zeneti | PermaNet 2.0 | Yes | 586 | 723 | 19 | 18.95 | |
| ITN: insecticide‐treated net; LLIN: long‐lasting insecticidal net; NR: not reported; PBO: piperonyl butoxide; UTN: untreated net; WHO: World Health Organization. | |||||||
| Study ID | Net type | Species | Density measurement | Collection method | Baseline density | Post‐intervention density | Reduction (%) |
|---|---|---|---|---|---|---|---|
| Untreated | An gambiae s.l. | Mean number caught per house | WT, IRC | 16.2 | 17.1 | ‐5.56 | |
| PermaNet 2.0 | An gambiae s.l. | Mean number caught per house | WT, IRC | 21.3 | 7.2 | 66.20 | |
| PermaNet 3.0 | An gambiae s.l. | Mean number caught per house | WT, IRC | 20.1 | 1.4 | 93.03 | |
| PermaNet 2.0 | An gambiae s.l. | Resting density per room per day | IRC | ‐ | 1.92 | ‐ | |
| PermaNet 3.0 | An gambiae s.l. | Resting density per room per day | IRC | ‐ | 3.05 | ‐ | |
| Olyset | An gambiae s.l. | Resting density per room per day | IRC | ‐ | 3.21 | ‐ | |
| Olyset Plus | An gambiae s.l. | Resting density per room per day | IRC | ‐ | 3.7 | ‐ | |
| Olyset | An gambiae | Mean number caught per catch | PSC | ‐ | 0.10 | ‐ | |
| Olset Plus | An gambiae | Mean number caught per catch | PSC | ‐ | 0.12 | ‐ | |
| PermaNet 2.0 | An gambiae | Mean number caught per catch | PSC | ‐ | 0.13 | ‐ | |
| PermaNet 3.0 | An gambiae | Mean number caught per catch | PSC | ‐ | 0.09 | ‐ | |
| Olyset | An funestus | Mean number caught per catch | PSC | ‐ | 0.08 | ‐ | |
| Olyset Plus | An funestus | Mean number caught per catch | PSC | ‐ | 0.16 | ‐ | |
| PermaNet 2.0 | An funestus | Mean number caught per catch | PSC | ‐ | 0.27 | ‐ | |
| PermaNet 3.0 | An funestus | Mean number caught per catch | PSC | ‐ | 0.13 | ‐ | |
| Olyset | An gambiae | Mean number caught per catch | LT | ‐ | 1.23 | ‐ | |
| Olset Plus | An gambiae | Mean number caught per catch | LT | ‐ | 0.27 | ‐ | |
| PermaNet 2.0 | An gambiae | Mean number caught per catch | LT | ‐ | 0.96 | ‐ | |
| PermaNet 3.0 | An gambiae | Mean number caught per catch | LT | ‐ | 1.44 | ‐ | |
| Olyset | An funestus | Mean number caught per catch | LT | ‐ | 2.02 | ‐ | |
| Olset Plus | An funestus | Mean number caught per catch | LT | ‐ | 2.1 | ‐ | |
| PermaNet 2.0 | An funestus | Mean number caught per catch | LT | ‐ | 5.76 | ‐ | |
| PermaNet 3.0 | An funestus | Mean number caught per catch | LT | ‐ | 3.76 | ‐ | |
| Olyset (2015) | Anopheles species | Mean number caught per house per night | LT | ‐ | 2.61 | ‐ | |
| Olyset Plus (2015) | Anopheles species | Mean number caught per house per night | LT | ‐ | 1.85 | ‐ | |
| Olyset (2016) | Anopheles species | Mean number caught per house per night | LT | ‐ | 3.60 | ‐ | |
| Olyset Plus (2016) | Anopheles species | Mean number caught per house per night | LT | ‐ | 2.68 | ‐ | |
| Permanet 2.0 (6 months) | An gambiae s.l. | Mean density per house | IRC | 0.3 | 0.67 | ||
| Permanet 3.0 (6 months) | An gambiae s.l. | Mean density per house | IRC | 0.8 | 0.17 | 78.75 | |
| Olyset (6 months) | An gambiae s.l. | Mean density per house | IRC | 0.3 | 0.81 | ||
| Olyset Plus (6 months) | An gambiae s.l. | Mean density per house | IRC | 0.1 | 0.16 | ||
| Permanet 2.0 (12 months) | An gambiae s.l. | Mean density per house | IRC | 0.3 | 1.35 | ||
| Permanet 3.0 (12 months) | An gambiae s.l. | Mean density per house | IRC | 0.8 | 0.52 | 35 | |
| Olyset (12 months) | An gambiae s.l. | Mean density per house | IRC | 0.3 | 1.1 | ||
| Olyset Plus (12 months) | An gambiae s.l. | Mean density per house | IRC | 0.1 | 0.23 | ||
| Permanet 2.0 (18 months) | An gambiae s.l. | Mean density per house | IRC | 0.3 | 1.65 | ||
| Permanet 3.0 (18 months) | An gambiae s.l. | Mean density per house | IRC | 0.8 | 1.57 | ||
| Olyset (18 months) | An gambiae s.l. | Mean density per house | IRC | 0.3 | 0.66 | ||
| Olyset Plus (18 months) | An gambiae s.l. | Mean density per house | IRC | 0.1 | 0.19 | ||
| No intervention | An gambiae s.s. | Mean number caught per village | IRC | 230 | 79 | 65.65 | |
| Permanet 2.0 | An gambiae s.s. | Mean number caught per village | IRC | 39 | 36 | 7.69 | |
| Permanet 2.0 | An gambiae s.s. | Mean number caught per village | IRC | 82 | 45 | 45.12 | |
| Permanet 3.0 | An gambiae s.s. | Mean number caught per village | IRC | 77 | 12 | 84.42 | |
| Permanet 3.0 | An gambiae s.s. | Mean number caught per village | IRC | 178 | 15 | 91.57 | |
| No intervention | An gambiae s.s. | Mean number caught per person per night per village | Indoor & outdoor HLC | 415 | 72 | 82.65 | |
| Permanet 2.0 | An gambiae s.s. | Mean number caught per person per night per village | Indoor & outdoor HLC | 33 | 31 | 6.06 | |
| Permanet 2.0 | An gambiae s.s. | Mean number caught per person per night per village | Indoor & outdoor HLC | 79 | 64 | 18.99 | |
| Permanet 3.0 | An gambiae s.s. | Mean number caught per person per night per village | Indoor & outdoor HLC | 98 | 19 | 80.61 | |
| Permanet 3.0 | An gambiae s.s. | Mean number caught per person per night per village | Indoor & outdoor HLC | 156 | 36 | 76.92 | |
| An funestus: Anopheles funestus; An gambiae: Anopheles gambiae; HLC: human landing catch; IRC: indoor resting catch; LT: light trap; PSC: pyrethrum spray catch; WT: window trap. | |||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Parasite prevalence (pyrethroid‐PBO nets vs non‐PBO LLINs, latest end points in RCT) Show forest plot | 2 | Odds Ratio (IV, Fixed, 95% CI) | 0.79 [0.67, 0.95] | |
| 1.2 Parasite prevalence (pyrethroid‐PBO nets vs non‐PBO LLINs, shown at 4 different time points) Show forest plot | 2 | Odds Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 1.2.1 4 to 6 months | 2 | Odds Ratio (IV, Fixed, 95% CI) | 0.74 [0.62, 0.89] | |
| 1.2.2 9 to 12 months | 2 | Odds Ratio (IV, Fixed, 95% CI) | 0.72 [0.61, 0.86] | |
| 1.2.3 16 to 18 months | 2 | Odds Ratio (IV, Fixed, 95% CI) | 0.88 [0.74, 1.04] | |
| 1.2.4 21 to 25 months | 2 | Odds Ratio (IV, Fixed, 95% CI) | 0.79 [0.67, 0.95] | |
| 1.3 Mosquito sporozoite‐positive (adjusted ICC 0.1) Show forest plot | 4 | 424 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.24, 2.75] |
| 1.4 Mosquito parous (adjusted ICC 0.1) Show forest plot | 3 | 220 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.82, 1.13] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Mosquito mortality (pooled) hut/night (adjusted ICC 0.1) Show forest plot | 10 | 15614 | Risk Ratio (M‐H, Random, 95% CI) | 1.43 [1.26, 1.62] |
| 2.1.1 Unwashed | 10 | 8647 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [1.29, 2.05] |
| 2.1.2 Washed | 8 | 6967 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [1.04, 1.38] |
| 2.2 Mosquito blood‐feeding success (pooled) hut/night (adjusted ICC 0.1) Show forest plot | 9 | 12351 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.66, 0.85] |
| 2.2.1 Unwashed | 9 | 7261 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.57, 0.80] |
| 2.2.2 Washed | 7 | 5090 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.74, 1.02] |
| 2.3 Mosquito exophily (pooled) hut/night (adjusted ICC 0.1) Show forest plot | 10 | 13214 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.94, 1.06] |
| 2.3.1 Unwashed | 10 | 7699 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.91, 1.10] |
| 2.3.2 Washed | 8 | 5515 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.93, 1.07] |
| 2.4 Mosquito mortality (high resistance) hut/night (adjusted ICC 0.1) Show forest plot | 5 | 7997 | Risk Ratio (M‐H, Random, 95% CI) | 1.58 [1.34, 1.86] |
| 2.4.1 Unwashed | 5 | 4896 | Risk Ratio (M‐H, Random, 95% CI) | 1.84 [1.60, 2.11] |
| 2.4.2 Washed | 4 | 3101 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.88, 1.63] |
| 2.5 Mosquito blood‐feeding success (high resistance) hut/night (adjusted ICC 0.1) Show forest plot | 4 | 7134 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.57, 0.76] |
| 2.5.1 Unwashed | 4 | 4458 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.50, 0.71] |
| 2.5.2 Washed | 3 | 2676 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.72, 0.92] |
| 2.6 Mosquito mortality (moderate resistance) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1027 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [1.21, 1.78] |
| 2.6.1 Unwashed | 2 | 751 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.68 [1.33, 2.11] |
| 2.6.2 Washed | 1 | 276 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.74, 1.54] |
| 2.7 Mosquito blood‐feeding success (moderate resistance) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1034 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.78, 1.05] |
| 2.7.1 Unwashed | 2 | 752 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.72, 1.11] |
| 2.7.2 Washed | 1 | 282 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.74, 1.13] |
| 2.8 Mosquito mortality (low resistance) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1970 | Risk Ratio (M‐H, Random, 95% CI) | 1.30 [1.09, 1.56] |
| 2.8.1 Unwashed | 2 | 948 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.99, 1.57] |
| 2.8.2 Washed | 2 | 1022 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [0.95, 2.04] |
| 2.9 Mosquito blood‐feeding success (low resistance) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1970 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.56, 1.57] |
| 2.9.1 Unwashed | 2 | 948 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.27, 2.11] |
| 2.9.2 Washed | 2 | 1022 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.49, 2.33] |
| 2.10 Mosquito mortality (susceptible) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1916 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.96, 1.15] |
| 2.10.1 Unwashed | 2 | 948 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.64, 2.26] |
| 2.10.2 Washed | 2 | 968 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.92, 1.25] |
| 2.11 Mosquito blood‐feeding success (susceptible) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1916 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.40, 1.89] |
| 2.11.1 Unwashed | 2 | 948 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.12, 2.22] |
| 2.11.2 Washed | 2 | 968 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.82, 1.91] |
| 2.12 Mosquito mortality (high resistance/Permanet) hut/night (adjusted ICC 0.1) Show forest plot | 3 | 2806 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [1.26, 2.01] |
| 2.12.1 Not Washed | 3 | 1877 | Risk Ratio (M‐H, Random, 95% CI) | 1.81 [1.56, 2.10] |
| 2.12.2 Washed | 2 | 929 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.61, 2.28] |
| 2.13 Mosquito blood‐feeding success (high resistance/Permanet) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1943 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.45, 0.76] |
| 2.13.1 Unwashed | 2 | 1439 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.40, 0.69] |
| 2.13.2 Washed | 1 | 504 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.61, 0.93] |
| 2.14 Mosquito mortality (high resistance/Olyset) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1410 | Risk Ratio (M‐H, Random, 95% CI) | 1.73 [1.51, 1.97] |
| 2.14.1 Unwashed | 2 | 1257 | Risk Ratio (M‐H, Random, 95% CI) | 1.72 [1.48, 1.99] |
| 2.14.2 Washed | 1 | 153 | Risk Ratio (M‐H, Random, 95% CI) | 1.81 [1.25, 2.61] |
| 2.15 Mosquito blood‐feeding success (high resistance/Olyset) hut/night (adjusted ICC 0.1) Show forest plot | 2 | 1470 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.40, 0.98] |
| 2.15.1 Unwashed | 2 | 1257 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.38, 1.18] |
| 2.15.2 Washed | 1 | 213 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.27, 0.93] |

