Lavado de manos sin enjuague para reducir el ausentismo entre los niños en edad preescolar y escolar
Resumen
Antecedentes
El ausentismo relacionado con la enfermedad es un problema importante entre los niños en edad preescolar y escolar de los países de ingresos bajos, medios y altos. La higiene apropiada de las manos es una estrategia investigada y aplicada comúnmente para reducir la propagación de enfermedades y, por consiguiente, el número de días de ausentismo. La mayoría de las estrategias de higiene de las manos implican lavarse las manos con agua y jabón, sin embargo, este procedimiento se asocia a una serie de factores que actúan como una barrera para su uso, como la necesidad de agua corriente, y la necesidad de secarse las manos después de la limpieza. Un método alternativo consiste en lavarse las manos utilizando un lavado de manos sin enjuague. Esta técnica tiene una serie de beneficios sobre las estrategias tradicionales de higiene de las manos y puede resultar beneficiosa para reducir el ausentismo por enfermedad en los niños en edad preescolar y escolar.
Objetivos
1. Evaluar la efectividad del lavado de manos sin enjuague para reducir el ausentismo por enfermedad en niños en edad preescolar y escolar en comparación con ningún lavado de manos, el lavado de manos convencional con agua y jabón u otras estrategias de lavado de las manos.
2. Determinar qué productos para el lavado de manos sin enjuague son los más efectivos (si existen comparaciones directas), y qué efecto tienen las estrategias adicionales en combinación con el lavado de manos sin enjuague en los resultados de interés.
Métodos de búsqueda
En febrero 2020 se hicieron búsquedas en CENTRAL, MEDLINE, Embase, CINAHL, otras 12 bases de datos y tres registros de ensayos clínicos. También se revisaron las listas de referencia de los estudios incluidos y se estableció un contacto directo con los principales autores de los estudios para recabar información adicional según fuera necesario. No se aplicaron restricciones de fecha o de idioma.
Criterios de selección
Ensayos controlados aleatorizados (ECA), independientemente del estado de publicación, que compararan el lavado de manos sin enjuague en cualquier forma (higiene de las manos mediante frotación, desinfectante de manos, gel, espuma, etc.) con el lavado de manos convencional con agua y jabón, otros programas de lavado de manos (como educación sola) o ninguna intervención. La población de interés incluyó a niños de entre dos y 18 años de edad que asistían a un nivel preescolar (guardería, jardín de infancia, etc.) o a la escuela (primaria, secundaria, etc.). Los resultados primarios incluyeron el ausentismo de niños o estudiantes por cualquier razón, el ausentismo debido a cualquier enfermedad y las reacciones cutáneas adversas.
Obtención y análisis de los datos
Siguiendo los métodos estándar de Cochrane, dos autores de la revisión (ZM, CT, CL, CS o TB), seleccionaron de forma independiente los estudios para su inclusión, evaluaron el riesgo de sesgo y extrajeron los datos relevantes. Las ausencias fueron extraídas como el número de días de ausencia de los estudiantes del total de días. Estos datos fueron informados algunas veces con los números brutos y otras veces como el cociente de tasas de incidencia (CTI), que también fue extraído. Para los datos de los eventos adversos, se calcularon los tamaños del efecto como riesgos relativos (RR) y se presentan con intervalos de confianza (IC) del 95%. Se utilizaron los procedimientos metodológicos estándar previstos por Cochrane para el análisis de los datos y se siguieron los criterios GRADE para establecer la certeza de los hallazgos.
Resultados principales
Esta revisión incluye 19 estudios con 30 747 participantes. La mayoría de los estudios se realizaron en los Estados Unidos (ocho estudios), dos en España y uno en China, Colombia, Finlandia, Francia, Kenya, Bangladesh, Nueva Zelandia, Suecia y Tailandia. Seis estudios se realizaron en centros preescolares o guarderías (niños de 0 a < 5 años), y los 13 restantes en escuelas primarias (niños de 5 a 14 años).
Se consideró que los estudios incluidos presentaban un riesgo alto de sesgo en varios dominios, sobre todo en los dominios del sesgo de realización y de detección, debido a la dificultad para cegar a quienes realizaban la intervención o a quienes evaluaban el resultado. Además, todos los resultados de interés se calificaron como de certeza baja o muy baja de la evidencia, principalmente debido al riesgo alto de sesgo, así como a la imprecisión de las estimaciones de los efectos y la incoherencia entre los datos agrupados. Para el resultado del ausentismo por cualquier motivo, la estimación agrupada para el lavado de manos sin enjuague fue un CTI de 0,91 (IC del 95%: 0,82 a 1,01; 2 estudios; evidencia de certeza muy baja), lo que indica que puede haber poca o ninguna diferencia entre los grupos. Para el ausentismo por cualquier enfermedad, el CTI agrupado fue de 0,82 (IC del 95%: 0,69 a 0,97; 6 estudios; evidencia de certeza muy baja), lo que indica que el lavado de manos sin enjuague puede reducir el ausentismo (13 días de ausencia por cada 1000) en comparación con los del grupo de «ningún lavado de manos sin enjuague» (16 días de ausencia por cada 1000). Para el resultado del ausentismo por enfermedades respiratorias agudas, el CTI agrupado fue 0,79 (IC del 95%: 0,68 a 0,92; 6 estudios; evidencia de certeza muy baja ), lo que indica que el lavado de manos sin enjuague puede reducir el ausentismo (33 días de ausencia por cada 1000) en comparación con los del grupo de «ningún lavado de manos sin enjuague» (42 días de ausencia por cada 1000). Cuando se evaluó el ausentismo por enfermedades gastrointestinales agudas, la estimación agrupada encontró un CTI de 0,79 (IC del 95%: 0,73 a 0,85; 4 estudios; evidencia de certeza baja), que indica que el lavado de manos sin enjuague puede reducir el ausentismo (seis días de ausencia por cada 1000) en comparación con los del grupo de «ningún lavado de manos sin enjuague» (ocho días de ausencia por cada 1000). Es posible que haya poca o ninguna diferencia entre el grupo de lavado de manos sin enjuague y el grupo de «ningún lavado de manos sin enjuague» con respecto a las reacciones cutáneas adversas con un RR de 1,03 (IC del 95%: 0,8 a 1,32; 3 estudios, 4365 participantes; evidencia de certeza muy baja). En general, el cumplimiento de la intervención pareció oscilar entre un cumplimiento moderado y alto (9 estudios, 10 749 participantes; evidencia de certeza muy baja); en la narrativa, ningún autor informó de problemas considerables relacionados con el cumplimiento. En general, la mayoría de los estudios que incluyeron datos sobre la percepción informaron de que los profesores y los estudiantes percibieron de forma positiva el lavado de manos sin enjuague y estaban dispuestos a seguir utilizándolo (3 estudios, 1229 participantes; evidencia de certeza muy baja).
Conclusiones de los autores
Los resultados de esta revisión pueden haber identificado un efecto pequeño pero potencialmente beneficioso de los regímenes de lavado de manos sin enjuague en el ausentismo por enfermedad. Sin embargo, la certeza de la evidencia que contribuyó a esta conclusión fue baja o muy baja según los criterios GRADE y, por lo tanto, es incierta. Es necesario realizar más investigaciones en todos los niveles de la enseñanza para evaluar los regímenes de lavado de manos sin enjuague a fin de obtener evidencia más concluyente y de mayor certeza con respecto a su impacto. Al considerar el uso de un programa de lavado de manos sin enjuague en un entorno local, es necesario tener en cuenta las tasas actuales de ausentismo por enfermedad y si los pequeños efectos beneficiosos que se observan aquí se traducirán en una reducción significativa en todos sus entornos.
PICO
Resumen en términos sencillos
Lavado de manos sin enjuague para reducir el ausentismo entre los niños en edad preescolar y escolar
Antecedentes
El ausentismo escolar es costoso para los padres, las escuelas y los gobiernos y la ausencia sostenida es perjudicial para el aprendizaje de los estudiantes. El ausentismo por enfermedad es un factor importante que contribuye al ausentismo escolar, pero también puede dar lugar al ausentismo laboral de los padres debido a que ellos mismos pueden contraer la enfermedad o pueden tener que quedarse en casa para cuidar de sus hijos. En la actualidad se utilizan varias estrategias para reducir el ausentismo por enfermedad, un método común es la aplicación de prácticas adecuadas de higiene de las manos. Sin embargo, la higiene de las manos con agua y jabón no siempre es práctica, y las alternativas pueden resultar más efectivas para reducir la tasa general de ausentismo por enfermedad. Una de dichas alternativas es el uso de un lavado de manos sin enjuague.
Pregunta de la revisión
Esta revisión se diseñó para investigar si el uso del lavado de manos sin enjuague puede reducir el número de días de ausencia de la escuela en niños en edad preescolar y escolar en comparación con el uso de ningún lavado de manos sin enjuague.
Características de los estudios
Las búsquedas arrojaron 19 estudios relevantes con un total de 30 747 participantes. Ocho estudios se realizaron en los Estados Unidos, dos en España y uno en China, Colombia, Finlandia, Francia, Kenya, Bangladesh, Nueva Zelandia, Suecia y Tailandia. Seis estudios se realizaron en centros preescolares o guarderías (niños de 0 a 5 años), y los 13 restantes en escuelas primarias (niños de 5 a 14 años). Estos estudios fueron muy variados en cuanto a la composición y la aplicación del programa de lavado de manos sin enjuague. Solo dos estudios incluyeron información sobre el resultado primario (ausentismo por cualquier motivo), mientras que para el ausentismo por cualquier enfermedad hubo seis estudios que proporcionaron información. La evidencia presentada está actualizada hasta febrero de 2020.
Resultados clave
La aplicación y la adherencia a un programa de lavado de manos sin enjuague pueden estar asociados con efectos pequeños, pero potencialmente beneficiosos en cuanto a la reducción del número de días en que los estudiantes se ausentan de la escuela por enfermedad, en comparación con un programa de higiene de ningún lavado de manos sin enjuague. Sin embargo, el lavado de manos sin enjuague puede no ser diferente a los controles para reducir el ausentismo por cualquier motivo. También es posible que no haya diferencia en el número de irritaciones de la piel entre los estudiantes que recibieron el lavado de manos sin enjuague en comparación con los que usaron agua y jabón. La mayoría de los estudiantes y profesores respondieron de manera favorable al uso del lavado de manos sin enjuague y cumplieron relativamente bien con su uso.
Certeza de la evidencia
La certeza de la evidencia incluida en esta revisión fue baja o muy baja, principalmente debido a que los estudios incluidos utilizaron métodos deficientes, proporcionaron datos imprecisos y fueron muy inconsistentes entre sí. Este hecho significa que existe poca y muy poca certeza, o confianza, en estos resultados.
Authors' conclusions
Summary of findings
| Rinse‐free hand wash compared to no rinse‐free hand wash program for reducing absenteeism among preschool and school children | ||||||
| Patient or population: children aged from birth to 14 years old | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with control | Risk with rinse‐free hand wash | |||||
| Absenteeism for any reason (within the study period) Calculated as: an incident rate per child‐days possible Length of time observed: range = 5 to 6 months | Baseline risk (Priest 2014)aa | Incidence rate ratio 0.91 | (2 RCTs) | ⊕⊝⊝⊝ | ‐ | |
| 32 days absent per 1000 | 29 per 1000 | |||||
| Absenteeism due to any illness (within the study period) Calculated as: an incident rate per child‐days possible Length of time observed: range = 1 to 11 months | Baseline risk (Priest 2014)bb | Incidence rate ratio 0.82 | (6 RCTs) | ⊕⊝⊝⊝ | ‐ | |
| 16 days absent per 1000 | 13 per 1000 | |||||
| Adverse skin reactions (within the study period) Calculated as: number of events Length of time observed: range = 5 to 8 months | Study population | RR 1.03 | 4365 (3 RCTs) | ⊕⊝⊝⊝ | ‐ | |
| 47 per 1000 | 49 per 1000 | |||||
| Absenteeism due to acute respiratory illness (within the study period) Calculated as: an incident rate per child‐days possible Length of time observed: range = 1 to 8 months | Baseline risk (Azor Martinez 2018)cc | Incidence rate ratio 0.79 | (6 RCTs) | ⊕⊝⊝⊝ | ‐ | |
| 42 days absent per 1000 | 33 per 1000 | |||||
| Absenteeism due to acute gastrointestinal illness (within the study period) Calculated as: an incident rate per child‐days possible Length of time observed: range = 1 to 8 months | Baseline risk (Prazuck 2010)dd | Incidence rate ratio 0.79 | (4 RCTs) | ⊕⊕⊝⊝ | ‐ | |
| 8 days absent per 1000 | 6 per 1000 | |||||
| Compliance with the intervention or program Assessed with: different measures of compliance Length of time observed: range = 1 to 12 months | 9 studies addressed compliance using diverse approaches. Broadly, compliance with the intervention appeared to range from moderate to high compliance. Narrativley, no authors reported substantial issues with compliance. | 10,749 | ⊕⊝⊝⊝ | ‐ | ||
| Perception of the hand hygiene strategy or satisfaction with the hand hygiene strategy Assessed with: different measures of perception Length of time observed: range = 3 to 11 months | 3 studies addressed perception. Of these, 2 studies, Pickering 2013 and Vessey 2007, conducted semi‐structured interviews with staff and students. No numerical data were reported by Pickering 2013; however, rinse‐free hand wash was perceived favorably by the teaching staff. Vessey 2007 reported that 100% of interviewed staff would prefer rinse‐free hand wash over soap at their school; 91% of students interviewed stated they would preferentially choose rinse‐free hand wash over soap and water to wash their hands. 1 study, Correa 2012, reported that teachers of rinse‐free hand wash‐assigned schools perceived rinse‐free hand wash positively and were willing to continue its use. | 1229 | ⊕⊝⊝⊝ | ‐ | ||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| a Downgraded two levels due to a high risk of performance bias and detection bias, as the students, parents of students and teachers were aware of treatment assignment. Both studies are also at high risk of attrition bias. Downgraded one level due to confidence intervals ranging from a potentially important difference (0.82) to a negligible difference (1.01). aaBaseline risk for absenteeism for any reason was calculated using the values provided in the study by Priest 2014 as 3.2% (days spent absent over child‐days possible). | ||||||
Background
Description of the condition
Absenteeism due to sickness (particularly gastrointestinal or minor respiratory illness) is an important problem for schools in low‐, middle‐ and high‐income countries (Day 1993; Early 1998; Guinan 1997; Kimel 1996; Master 1997; Monsma 1992; Niffenegger 1997). The common cold alone has been shown to result in approximately 22 million days absent from school per year in the USA (Adams 1999), and young children are likely to have between six and eight colds per year, decreasing to between two and four colds per year in adults (Heikkinen 2003). Not only are children adversely affected by repeated respiratory infections, family members can also be affected due to infections transmitted by an infected child (Neuzil 2002). When a child is ill, this can result in work‐related absence due to parental illness or due to the need to remain at home to care for their child (Neuzil 2002).
Many strategies for reducing the spread of infectious diseases in children have been studied, such as hand washing (Lee 2010), education or training (Lee 2010; Roberts 2000), safe water supply (Esrey 1985; Lee 2010), environmental cleaning (Harris 2010; Lee 2010), exclusion periods (Lee 2010; Richardson 2001), and vigilance during food preparation (Lee 2010). While conventional hand washing with soap and water is an effective method of hand hygiene for the prevention of the spread of infectious diseases, it is difficult to maintain compliance with conventional hand washing, and its consistency and effectiveness among preschool (three to five‐year olds) (Niffenegger 1997) and school students is variable (Day 1993; Early 1998; Guinan 2002; Kimel 1996; Monsma 1992). There may also be other factors that can either lead to increased or decreased absenteeism due to sickness, including infection control measures in the home, or school specific factors such as local hygiene measures, equipment, geographic location, etc.
Description of the intervention
Rinse‐free hand wash (also known as hand gel, hand foam, hand sanitizer or hand rub) is increasingly being used in both healthcare settings and the community as a measure to improve hand hygiene (Gould 2017; Harbarth 2002; Maury 2000). The active ingredients of the majority of rinse‐free hand wash products are alcohols (such as isopropanol, ethanol, or n‐propanol). Other rinse‐free antimicrobial hand washes are not as common (Boyce 2002; Meadows 2004; Morton 2004). Some evidence suggests there are only minimal adverse effects (e.g. dry skin or irritation) associated with the use of rinse‐free hand wash (Meadows 2004; Sandora 2005); while some studies have shown rinse‐free hand wash reduces skin irritation and dryness compared to traditional soap and water methods, and has been shown to be more acceptable than traditional methods (Boyce 2000); however, single studies are not considered a reliable source of evidence for policy or practice. Rinse‐free hand wash with a concentration of ethanol between 60% and 95%, with a 3 mL to 5 mL application, is considered to be effective and safe for reducing the amount of bacteria present on the hand (Kampf 2008).
Rinse‐free hand wash can be considered as more convenient than traditional hand washing with soap and water for the following reasons: (1) it can be easily transported or carried on oneself; (2) it can be located within classroom or day care settings without the need for running water; (3) hands do not require traditional paper‐towel or air blower drying after use; and (4) it is quicker to complete than traditional hand washing. As rinse‐free hand wash may be a simpler method for hand hygiene compared to conventional hand washing with soap and water, it may be more effective than traditional measures. Rinse‐free hand wash may be applied by the children themselves, by a helper or under the direction of a helper, and may be implemented alongside an educational initiative to promote hand hygiene. For this review, education alone was not considered an intervention.
How the intervention might work
Respiratory‐tract viruses, such as influenza or rhinoviruses, are commonly spread between people through direct contact with droplets or aerosol containing the pathogen to the respiratory mucosa of another person (Heikkinen 2003; Musher 2003; Warren‐Gash 2013). Gastrointestinal illnesses and diarrhea‐causing pathogens are transmitted via the faecal‐oral route, by exposure to faecal matter, direct contact with a person, or via ingestion of food and water contaminated with faecal matter (Warren‐Gash 2013).
Hand hygiene is commonly recommended as a decontamination measure to reduce transmission via direct contact of gastrointestinal and respiratory infections and has shown promise in community settings (Aiello 2008; Warren‐Gash 2013). Once the hands come into contact with a pathogen, this can be transferred to respiratory or oral mucosa when the person brings their hand to their face. Hand hygiene may reduce transmission through reducing and removing or eliminating pathogens from the hand (Ejemot‐Nwadiaro 2015; Warren‐Gash 2013).
The active component of the vast majority of rinse‐free hand washes is alcohol. Alcohol has the ability to denature proteins, and therefore, acts as a skin disinfectant against viruses and bacteria (Bessonneau 2010). However, there may be a range of costs associated with its use, related to, for instance, perceptions and compliance, and financial cost, which we discuss in the Discussion section.
Why it is important to do this review
When children acquire an illness, this can spread through the family and result in days lost from school, and from work. Student school attendance is positively related to improved performance on standardized tests (Lamdin 1996), whilst significant or chronic absence from schooling can have a detrimental effect on a student's academic achievement (Chang 2008). Although lost days to an infectious illness like the common cold or gastroenteritis are not likely to result in a significant amount of attendance days lost from school, as compared to a chronic illness, there may still be an effect on learning and academic achievement (Gottfried 2009).
A Cochrane systematic review (Ejemot‐Nwadiaro 2015), which evaluated hand washing with water and soap to reduce diarrhea in children and adults in community settings (day care centres, schools, communities or hospitals) in both high‐income countries and low‐ and middle‐income countries (LMICs), found a reduction in diarrhea episodes of "around one‐third (rate ratio 0.70; 95% CI 0.58 to 0.85)" (Ejemot‐Nwadiaro 2015). However, the authors explicitly excluded rinse‐free hand wash as an intervention and respiratory illnesses as an outcome (Ejemot‐Nwadiaro 2015). Another systematic review, published in 2004, evaluated the effectiveness of rinse‐free hand sanitizers for reducing absenteeism related to illness in elementary school children. The review authors found six trials of low quality and poor reporting (Meadows 2004). Since that review there have been a number of new studies published. A systematic review was published in 2016 on hand hygiene interventions for children in educational settings (Willmott 2016). The authors of this review concluded that the evidence is equivocal regarding the effectiveness of hand hygiene interventions although they may decrease respiratory tract infections amongst children. There are some important differences between our review inclusion criteria and the Willmott 2016 review, the main being that our review focuses explicitly on rinse‐free interventions. Willmott 2016 stated the following as one of the limitations of their review: this "review does not distinguish between handwashing with soap or hand sanitizer use even though these methods may have different resource implications and be differentially effective in eliminating certain pathogens.” Additionally, the search for the Willmott 2016 review was conducted in September 2014 and there have been a number of new studies published after this date. Given the convenience of rinse‐free hand washing compared to traditional approaches, the number of recent dedicated studies addressing rinse‐free hand wash, and the potential policy implications for hand hygiene practices, a review on rinse‐free hand wash in preschools and schools is required.
This systematic review aims to provide an up‐to‐date examination of the effects of rinse‐free hand wash on illness‐related absenteeism amongst preschool and school children in low‐, middle‐ and high‐income countries.
Objectives
-
To assess the effectiveness of rinse‐free hand washing for reducing absenteeism (due to illness or for any reason) in preschool and school children compared to no hand washing, conventional hand washing with soap and water or other hand hygiene strategies.
-
To determine which rinse‐free hand washing products are the most effective (if head‐to‐head comparisons exist), and what effect additional strategies in combination with rinse‐free hand washing have on the outcomes of interest.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials (RCTs), including cluster‐RCTs, irrespective of publication status. We also considered for inclusion quasi‐RCTs, where allocation has been systematic but not random (for example, by days of the week).
Types of participants
Children aged between two and 18 years attending preschool (childcare, day care, kindergarten, etc.), or school (primary, secondary, elementary, etc.). We included children attending preschool or school in urban or rural settings regardless of whether they reside in a low‐, middle‐ or high‐income country.
Types of interventions
Rinse‐free hand wash in any form (hand rub, hand sanitizer, gel, foam etc.), based on alcohol or another active ingredient, irrespective of dose or frequency of use.
It may be used alone or as part of a comprehensive hand hygiene program that includes, for example, education on rinse‐free hand wash as an intervention. The rinse‐free hand wash may be applied by the child or by a helper (such as a childcare worker, caregiver or teacher) or under direction of the helper.
Comparators included conventional hand washing with soap and water, other hand hygiene programs (such as education alone), or no intervention.
Types of outcome measures
Primary outcomes
-
Student absenteeism for any reason. Absenteeism is defined as time absent from preschool or school when the student is scheduled to be attending, and does not include planned holidays or leave, or student‐free days.
-
Student absenteeism due to any illness.
-
Adverse skin reactions (such as a rash or irritation) within the trial period.
Illness may be confirmed by a physician or by self‐report.
The outcome measures could be assessed on a per week, month, term, trial period, or year basis. These could be reported as average or median days absent per group, as total days absent within each group, or as an incidence rate (i.e. two absences per 100 student days) per group. This is not a time‐bound intervention and, as such, outcomes will not be reported in terms of short‐term, mid‐term and long‐term follow‐up.
Secondary outcomes
-
Child or student absenteeism due to acute respiratory illness (an infection of the respiratory system such as influenza or rhinovirus).
-
Child or student absenteeism due to acute gastrointestinal illness (an illness with gastrointestinal symptoms such as diarrhea, vomiting and nausea).
-
Compliance with the intervention or program.
-
Perception of the hand hygiene strategy or satisfaction with the hand hygiene strategy.
Search methods for identification of studies
Electronic searches
The following electronic databases were searched initially in November 2016, and top‐up searches were performed in February 2019 and February 2020.
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2020 Issue 2) in the Cochrane Library, and which includes the Cochrane Developmental, Psychosocial and Learning Problems Specialised Register (searched 19 February 2020).
-
MEDLINE Ovid (1946 to 1 February 2020).
-
MEDLINE In‐Process & Other Non‐Indexed Citations Ovid (searched 19 February 2020).
-
MEDLINE Epub Ahead of Print Ovid (searched 19 February 2020).
-
Embase Ovid (1974 to 18 February 2020).
-
CINAHLPlus EBSCOhost (Cumulative Index to Nursing and Allied Health Literature; 1937 to 19 February 2020).
-
ERIC EBSCOhost (Education Resources Information Center; 1966 to 19 February 2020).
-
Science Citation Index Web of Science (SCI; 1970 to 19 February 2020).
-
Social Sciences Citation Index Web of Science (SSCI; 1970 to 19 February 2020).
-
Conference Proceedings Citation Index ‐ Social Science & Humanities Web of Science (CPCI‐SS&H; 1990 to 19 February 2020).
-
Conference Proceedings Citation Index ‐ Science Web of Science (CPCI‐S; 1990 to 19 February 2020).
-
LILACS (Latin American and Caribbean Health Sciences Literature; lilacs.bvsalud.org/en; searched 19 February 2020).
-
Cochrane Database of Systematic Reviews (CDSR; 2020 Issue 2), part of the Cochrane Library (searched 22 February 2020).
-
Database of Abstracts of Reviews of Effects (DARE; 2015 Issue 2; final issue searched 3 November 2016), part of the Cochrane Library. Archived version available at www.york.ac.uk/crd).
-
Epistemonikos (www.epistemonikos.org; searched 19 February 2020)
-
Database of Promoting Health Effectiveness Reviews (DoPHER; eppi.ioe.ac.uk/webdatabases4/Intro.aspx?ID=9; searched 22 February 2019).
-
ClinicalTrials.gov (clinicaltrials.gov; searched 2 March 2020)
-
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP; apps.who.int/trialsearch; searched 2 March 2020).
-
Australian New Zealand Clinical Trials Registry (www.anzctr.org.au; searched 2 March 2020).
The search strategies used for each source are available in Appendix 1. We did not place any language restrictions on the search and we assessed non‐English studies for their need for translation on a case‐by‐case basis (Higgins 2011a).
Searching other resources
We searched the reference lists of studies selected for inclusion for additional references and made direct contact with lead authors of studies to collect additional information as required.
Data collection and analysis
We reported only the methods we used. Other pre‐planned methods (Munn 2017) are reported as in Table 1.
| Section of review | Unused methods | Justification |
| Electronic searches | We had planned to search International Initiative for Impact Evaluation (3ie) Systematic Reviews Database. | We did not search International Initiative for Impact Evaluation (3ie) Systematic Reviews Database as planned. |
| Measures of treatment effect | Time‐to‐event data We had planned to analyze time‐to‐event data as dichotomous data, where appropriate. If hazard ratios had been reported and had been suitable for synthesis, we planned to compute RR for other similar studies, so that a synthesis across studies could occur. | Due to the reporting of the data in the primary studies, this did not eventuate. |
| Continuous data As absenteeism can occur on multiple occasions, it may have been that mean days absent were reported. We had planned to calculate effect sizes as mean differences and to present these with 95% confidence intervals. If different scales had been used, we had planned to report effect sizes using standardized mean differences (SMD). | Absenteeism was not reported in any of the papers as continuous data. | |
| Assessment of reporting biases | If there had been an adequate number of studies (at least 10), we would have created funnel plots to investigate reporting bias (Sterne 2011). In the case of 10 or more studies, for continuous data, we would have used Egger's test (Egger 1997). | We did not have any analyses that included 10 or more studies. |
| If effect sizes appeared to depend on the size of the trial, we would have explored whether this association was due to heterogeneity or publication bias. | We did not have enough studies to adequately investigate small study effects and publication bias. | |
| Subgroup analysis and investigation of heterogeneity | We had intended to explore heterogeneity by conducting the subgroup analyses listed below. 2. The frequency of the intervention (i.e. only after meals, before and after meals and toilet breaks, on arrival at preschool or school, etc.). 3. The person delivering the intervention or responsible for the intervention (teachers or caregivers compared to a child‐initiated intervention). 4. The means of recording absence (teacher reported compared to other measures). 5. The provision of hand‐wash alone versus the provision of hand wash plus additional strategies (such as education). 6. By gross national income per capita, based on World Banks classification of low‐, middle‐ and high‐income countries. | Insufficent details or information was able to be extracted from the included studies, preventing subgroup analysis. |
| Sensitivity analysis | We had intended to carry out sensitivity analyses, when necessary, to assess the robustness of our results to the exclusion of studies at high risk of bias (determined by both the allocation concealment and blinding of outcome assessment 'Risk of bias' criteria being rated as high) | All studies were at an overall high risk of bias; therefore, we did not perform this sensitivity analysis. |
Selection of studies
We collated and uploaded all identified citations to the review management software, Covidence (Covidence), removing any duplicates. Two review authors (from ZM, CT, CL, CS, TB) then independently screened titles and abstracts for assessment against the inclusion criteria for the review (Criteria for considering studies for this review). We obtained the full text of any paper that was clearly eligible for inclusion or where there was any doubt about eligibility. Two review authors (from ZM, CT, CL, CS, TB) independently assessed the full text against the inclusion criteria. We excluded full‐text reports that did not meet the inclusion criteria and provide reasons for exclusion in the review and in the 'Characteristics of excluded studies' tables. Any disagreements that arose between the review authors were resolved through discussion, or with a third, independent review author (from either ZM, CT, CL, CS, TB). We recorded our decisions in a study flow diagram Figure 1 (Moher 2009).
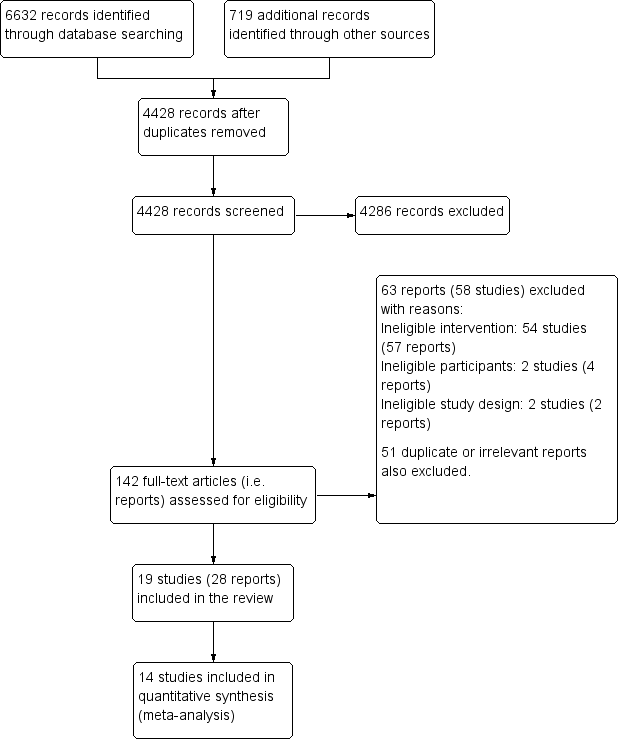
PRISMA study flow diagram.
Data extraction and management
Two review authors from the review team (from ZM, CT, CL, CS, TB) independently extracted data from included studies using a standardized data extraction tool. This tool was piloted and modified accordingly in Covidence. We extracted specific data on the population, intervention, study methods and outcomes of significance to the review question and specific objectives, as listed below.
-
Participants: number randomized (including the number of withdrawals and whether data were imputed and the imputation method), age distribution, gender, type of schooling, class sizes, time or months of the year (season), sociodemographics (race, ethnicity, language spoken) and country.
-
Intervention: the rinse‐free hand wash manufacturer, composition, active ingredient, dosage or frequency, application (who delivered it) and, when possible, cost and length of study. Details around any education regarding the use of the rinse‐free hand wash such as who delivered the education and the format for delivery (online or in person) was also extracted for each treatment group.
-
Outcomes: outcome definition and unit of measurement (such as how absence was measured), the number of participants allocated to each group, the sample size for each outcome.
-
Results: events per groups and subgroups.
Any disagreements that arose between the review authors were resolved through discussion, or with a third review author (from either ZM, CT, CL, CS, TB).
Assessment of risk of bias in included studies
Two independent review authors from the review team (from ZM, CT, CL, CS) critically appraised selected studies at the outcome level for risk of bias as detailed in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). This tool assesses the following domains of bias; selection (random sequence generation and allocation concealment), performance, detection, attrition, reporting and other sources of bias. We assessed the domains as high, low or unclear risk of bias, following the guidance in Table 8.5.d in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a), and as described in Appendix 2. Any disagreements that arose between the review authors was resolved through discussion, or with a third, independent review author (from ZM, CT, CL, CS, TB). We report the results of the this appraisal in the Risk of bias in included studies section.
Measures of treatment effect
We pooled studies, where possible, in a statistical meta‐analysis using Review Manager 5 (RevMan 5) (Review Manager 2014).
Dichotomous data
We collected dichotomous data such as reporting whether a student was absent or not, the amount of student days absent out of total days, and the amount of absent episodes. This was sometimes reported with the raw numbers and other times as an incidence rate ratio (IRR), which was also extracted. For adverse event data, we extracted this and calculated effect sizes as risk ratio (RR) and present these with 95% confidence intervals (CIs). Where there were no events in a treatment arm, Review Manager 2014 added a fixed value of 0.5 to the empty cell. If there were no events in the study, the study was excluded from the meta‐analysis (Higgins 2011b). As specified in the protocol (Munn 2017), we planned to analyze time‐to‐event data as dichotomous data, where appropriate, and if hazard ratios were reported and suitable for synthesis, we planned to compute RR for other similar studies, so that a synthesis across studies could occur. However, due to the reporting of the data in the primary studies, this was not undertaken (see Table 1).
Unit of analysis issues
Cluster‐randomised trials
We were likely to encounter unit of analysis issues in this systematic review, as groups of individuals were likely to be randomized and assigned together (in clusters such as classrooms or schools) (Higgins 2011b). We attempted to take appropriate measures to address unit of analysis issues, such as using the generic inverse variance method in Review Manager 2014, when studies analyzed their data and providing adjusted estimates accounting for their cluster design. It was likely that study authors would have taken steps to control for clustering in their analysis; however, if not, we requested the individual participant data to calculate an estimate of the intracluster correlation coefficient (ICC). However, these data were not provided, and as such, we either used the IRR provided by the study or calculated our own based on the data provided in the report.
Dealing with missing data
We requested missing or additional data from authors of studies, where required. Where authors could be contacted or did not respond to requests, we have highlighted this in the Results section of the review. We did not impute missing data with replacement values. We analyzed only available data. However, where possible, we made calculations based on available data or effect sizes to enable subsequent meta‐analysis. This is described on a per study basis in the Effects of interventions section. We have addressed the potential impact of missing data in the Discussion section of the review (Higgins 2011a).
Assessment of heterogeneity
We assessed clinical and methodological heterogeneity by evaluating the similarities and differences across studies in terms of the population (including age ranges, urban or rural, country (including low‐ and middle‐income countries compared to high‐income countries) and type of schooling), the intervention (dose and frequency), and study design. We assessed statistical heterogeneity visually by inspection of the forest plot and statistically by Cochran's Q (P value ≤ 0.10), and by I², which is a statistic used for quantifying inconsistency in meta‐analysis. In our meta‐analyses which use a random‐effects model, we also report tau2, an estimate of between‐study variability. We interpreted the I2 according to the guidance in theCochrane Handbook for Systematic Reviews of Interventions, bearing in mind the limitations of concrete thresholds for I2 (Deeks 2011):
-
0% to 40%: might not be important;
-
30% to 60%: may represent moderate heterogeneity;
-
50% to 90%: may represent substantial heterogeneity; or
-
75% to 100%: considerable heterogeneity.
Assessment of reporting biases
To address publication bias, we sought both published and unpublished literature. Too few studies were included to allow for the creation of a funnel plot to investigate reporting bias (Sterne 2011).
Data synthesis
Regardless of how the data were reported in the included studies (such as average or median days absent per group, as total days absent within each group, or as an incidence rate (e.g. two absences per 100 child days per group), we transformed the data to a common effect size, where possible, to facilitate meta‐analysis, as specified in the protocol (Munn 2017). For absenteeism, we used incidence rate ratios (IRRs) in the majority of cases, except for the comparisons evaluated in Pandejpong 2012 where rate difference was reported. This often required calculation of an IRR from the raw data, which was completed using StatsDirect software. For adverse effects, we used relative risks.
As we intended to generalize the results beyond the included studies, we used the random‐effects model as the default model, as this is a more appropriate approach than the fixed‐effect model for this purpose (Tufanaru 2015). We used the inverse variance method, available in Review Manager 2014, for both dichotomous and continuous data. We only used the fixed‐effect model when it was not appropriate to use the random‐effects model (for example, where fewer than five studies were included in the meta‐analysis) (Cooper 1994; Guolo 2017; Murad 2015; Tufanaru 2015).
We synthesized the data in a meta‐analysis when they were clinically comparable, and presented them in forest plots using Review Manager 2014, where possible. When synthesis in a meta‐analysis was not possible, due to significant clinical or methodological heterogeneity, we provided a narrative description of the results.
Summary of findings
We created a 'Summary of findings' table using GRADEPro GDT software (GRADEpro GDT 2016), based on review data exported from Review Manager 2014, for the following comparison: rinse‐free hand wash compared to no rinse‐free hand wash program for reducing absenteeism among preschool and school children. Following the GRADE approach (Schünemann 2011; Schünemann 2013), two authors from the review team (ZM, CL, CS, TB) assessed the certainty of the evidence for both the primary and secondary outcomes, based on the risk of bias, directness, heterogeneity, precision and risk of publication bias. We present the following information in the 'Summary of findings' table, when appropriate: absolute risks for the treatment and control, estimates of relative risk, and a ranking of the certainty of the evidence.
Subgroup analysis and investigation of heterogeneity
In order to explore heterogeneity, we subgrouped the data according to the age of the children (coinciding with level of education). According to our protocol (Munn 2017) we also planned to subgroup based on the frequency of the intervention; the person delivering the intervention; the means of recording absence; the provision of hand wash alone versus the provision of hand wash plus additional strategies; and by gross national income per capita. The justification for not performing these subgroup analyses have been reported in Table 1.
Sensitivity analysis
We did carry out sensitivity analysis on all analyses presented in this review to investigate the impact of the type of model (fixed or random) on the overall estimate of effect. We did not do this for exclusion of studies at high risk of bias, as all studies were at an overall high risk of bias as reported in Table 1.
Results
Description of studies
Results of the search
We ran searches in December 2016, February 2019 and February 2020. In total, we retrieved 7351 records, 6632 records from the database searches and 719 records from other sources. The duplicates were removed in Covidence, leaving 4428 records that we screened by title and abstract. From these, we identified 4286 clearly irrelevant records. We retrieved 142 full‐text articles and from these included 19 studies (reported in 28 publications) in the review (Figure 1).
We contacted 15 of the authors for additional information. Despite following up all email addresses and searching for authors via Google, we were unable to make contact or never heard back from the authors of the following reports: Ban 2015; Lau 2012; Morton 2004; Pandejpong 2012; Pickering 2013; Prazuck 2010; Snow 2008; Uhari 1999; White 2001;Biswas 2019. Responses were received from Correa 2012 and Sandora 2008, both of whom provided clarification on the presentation of their data. Gerald 2012 also responded, confirming that they did not collect any data on absences. Lennell 2008 responded, clarifying to the review team that absences for reasons other than infectious illness were excluded from the analysis. These authors were also unwilling to share the individual participant data for ethical concerns. Finally, Vessey 2007 responded and provided the review team with the complete raw data set, which we used for the analyses presented in this review.
Included studies
This review includes 19 studies from 28 reports involving 30,747 patients. From the 19 trials, five provided data that did not contribute to any of the meta‐analyses. Study characteristics are reported in detail in the Characteristics of included studies tables and summarized below.
Study types
Of the 19 included studies, all were randomized trials other than the study by Lau 2012, which was a controlled trial. All 19 of the studies employed a cluster‐trial design. Three of the studies also used a cross‐over design (Gerald 2012; Morton 2004; Vessey 2007). The duration of the trials ranged from two months (White 2001) to 14 months (Uhari 1999). The sample size ranged from 253 (Morton 2004) to 10885 (Biswas 2019), with the average sample size across studies being 1618 (standard deviation (SD) = 2312).
Populations and Settings
There were more studies conducted in the USA (eight studies:Gerald 2012; Lau 2012; Morton 2004; Sandora 2008; Snow 2008; Stebbins 2011; Vessey 2007; White 2001 ) compared to any other single country. Spain was the only other country where multiple studies has been conducted (two studies: Azor Martinez 2014; Azor Martinez 2018). The rest of the studies were conducted in China (Ban 2015), Colombia (Correa 2012), Bangladesh (Biswas 2019), Finland (Uhari 1999), France (Prazuck 2010), Kenya (Pickering 2013), New Zealand (Priest 2014), Sweden (Lennell 2008) and Thailand (Pandejpong 2012).
In terms of the educational setting, six studies were conducted in preschools or day‐care centres (Azor Martinez 2018; Ban 2015; Correa 2012; Lennell 2008; Pandejpong 2012; Uhari 1999); the remaining 13 studies were conducted in elementary or primary schools (Azor Martinez 2014; Biswas 2019; Gerald 2012; Lau 2012; Morton 2004; Pickering 2013; Prazuck 2010; Priest 2014; Sandora 2008; Snow 2008; Stebbins 2011; Vessey 2007; White 2001). For the schools, it was not always clear whether they were conducted in public or private institutions, and two studies (White 2001 and Biswas 2019) included both. Five studies stated they were conducted in public settings (Azor Martinez 2014; Gerald 2012; Lau 2012; Snow 2008; Stebbins 2011).
Given the mix of day‐care centres and elementary schools, the overall age across studies included in this review ranged from birth (Azor Martinez 2018) to 13 to 14 years (Pickering 2013).
Interventions
Studies did not always specify the type of rinse‐free hand wash used. The most common, commercial organization was GOJO industries, named in four studies (Correa 2012; Gerald 2012; Pickering 2013; Stebbins 2011). Studies did not always provide the active ingredient/s, although where they were provided, most (13 studies) used ethanol (alcohol) at a range of 60% to 75% (Azor Martinez 2014; Azor Martinez 2018; Ban 2015; Biswas 2019; Correa 2012; Gerald 2012; Lennell 2008; Morton 2004; Pandejpong 2012; Prazuck 2010; Priest 2014; Sandora 2008; Stebbins 2011). Two studies, Lau 2012 and White 2001, used a product from Woodward Laboratories Inc (CA, USA), where the active ingredient was benzalkonium chloride (stated at concentration levels of 0.13% in Lau 2012). In three studies, the hand sanitizer applied was unclear (Snow 2008; Uhari 1999; Vessey 2007).
The instructions and guidance for using the rinse‐free hand wash also differed across the studies. The study with the most strict application regimen was Pandejpong 2012, where participants were assigned to an intervention group of use every 60 or 120 minutes. The majority of the remaining studies provided a protocol or recommendations for when rinse‐free hand washing should be used. This commonly included: on presentation to the classroom or arrival at school (nine studies: Azor Martinez 2014; Azor Martinez 2018; Biswas 2019; Gerald 2012; Lau 2012; Morton 2004; Prazuck 2010; Stebbins 2011; White 2001); before or after (or both) mealtimes or scheduled breaks (13 studies: Azor Martinez 2014; Azor Martinez 2018; Biswas 2019; Gerald 2012; Lau 2012; Lennell 2008; Morton 2004; Prazuck 2010; Priest 2014; Sandora 2008; Stebbins 2011; Vessey 2007; White 2001); upon leaving for the day (six studies: Azor Martinez 2014; Azor Martinez 2018; Biswas 2019; Lau 2012; Stebbins 2011; White 2001); after coughing/sneezing or blowing/rubbing noses (eight studies: Azor Martinez 2014; Azor Martinez 2018; Biswas 2019; Gerald 2012; Lau 2012; Morton 2004; Priest 2014; White 2001); when a teacher asked them (one study: Morton 2004); after using the restroom (seven studies:Biswas 2019; Gerald 2012; Lennell 2008; Morton 2004; Prazuck 2010; Sandora 2008; Vessey 2007); after changing diapers (one study: Azor Martinez 2018); when dirty (two studies: Lennell 2008; Vessey 2007); after a field trip (one study: Lau 2012); or after using the gym/physical education lessons (two studies: Azor Martinez 2014; Lau 2012). Four studies did not specify a particular protocol or it was not described (Correa 2012; Pickering 2013; Snow 2008; Uhari 1999). In the case of one study, Ban 2015, it was simply stated that rinse‐free hand wash was used under supervision. All studies (with the exception of Pandejpong 2012) provided some form of education regarding hand hygiene or hand sanitizer use, in the form of either teacher‐ or researcher‐directed classroom lessons or presentations. In all studies, the children applied the rinse‐free hand wash themselves, although in six studies students may have been assisted by teachers or carers also (Azor Martinez 2014; Azor Martinez 2018; Correa 2012; Lennell 2008; Pandejpong 2012; Uhari 1999).
Outcomes
The main outcome, absenteeism, was reported and measured differently amongst the studies. Some of the studies (n = 4) stated that they relied on parental reporting to the school (Azor Martinez 2018; Lau 2012; Lennell 2008; Morton 2004), others (n = 11) in records kept by the school and collected by school personal (Azor Martinez 2014; Priest 2014; Sandora 2008; Stebbins 2011; Vessey 2007), by teachers using calendars or templates (Ban 2015; Pandejpong 2012; White 2001), student self‐reporting (Pickering 2013), or by parents using templates (Prazuck 2010; Uhari 1999). Absenteeism was not reported or it was unclear how it was reported in four studies (Correa 2012; Biswas 2019; Gerald 2012; Snow 2008).
The definition for diarrhea of three or more loose/watery stools in 24 hours (Ban 2015;Correa 2012; Pickering 2013), or a definition very similar (i.e. two watery stools in a 24‐hour period or three stools in 48 hours (Azor Martinez 2014; Pickering 2013; Prazuck 2010; Sandora 2008) was used in studies that have contributed outcome data towards gastrointestinal‐related absenteeism. Other studies (n = 13) also stated that a combination of particular symptoms, such as vomiting (Azor Martinez 2014; Priest 2014; White 2001), diarrhea (Ban 2015; Prazuck 2010; Priest 2014; White 2001), fever (Ban 2015; Prazuck 2010), abdominal pain (Ban 2015; Prazuck 2010; White 2001) and nausea (Prazuck 2010) could indicate gastrointestinal illness.
In studies that collected data on respiratory illness, one study used the Centers for Disease Control (CDC) definition for influenza‐like illness (Stebbins 2011). Whilst others (nine studies) stated a combination of symptoms could be diagnosed as a respiratory illness, symptoms considered included runny nose (Azor Martinez 2014; Azor Martinez 2018; Ban 2015; Correa 2012; Pandejpong 2012; Sandora 2008), blocked or stuffy nose (Azor Martinez 2014; Azor Martinez 2018; Ban 2015; Correa 2012; Pandejpong 2012; Priest 2014; Sandora 2008; White 2001), cough/expectoration (Azor Martinez 2014; Azor Martinez 2018; Ban 2015; Biswas 2019; Correa 2012; Pandejpong 2012; Priest 2014; Sandora 2008; White 2001), fever or chills (Azor Martinez 2014; Ban 2015; Biswas 2019; Correa 2012; Pandejpong 2012; Priest 2014; Sandora 2008; White 2001), sore throat (Azor Martinez 2014; Azor Martinez 2018; Correa 2012; Pandejpong 2012; Priest 2014; Sandora 2008), sneezing (Azor Martinez 2014; Azor Martinez 2018; Priest 2014; Sandora 2008; White 2001), ear pain (Correa 2012), bronchitis (White 2001), pink eye (White 2001), headache (Pandejpong 2012; Priest 2014; White 2001), and asthma exacerbation (White 2001).
Funding of studies
Not all studies reported their funding support. Of those that did, eight studies were funded by a commercial body who manufactures rinse‐free hand wash or who provided support or free samples for the duration of the study (Ban 2015; Correa 2012; Lau 2012; Morton 2004; Pickering 2013; Prazuck 2010; Sandora 2008; Vessey 2007).
Excluded studies
Following the full‐text review of 142 reports, we excluded 114 reports, 51 of which were excluded as they were either duplicates or irrelevant. The reasons for the exclusions of the remaining 63 reports (58 studies) are described in the Characteristics of excluded studies tables, but were mainly due to studies using interventions that were incompatible with the review question.
Risk of bias in included studies
We assessed risk of bias using the Cochrane 'Risk of bias' tool. For further information of individual studies' risk of bias, please see Characteristics of included studies tables. For 'Risk of bias' summary figures, see Figure 2 and Figure 3.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
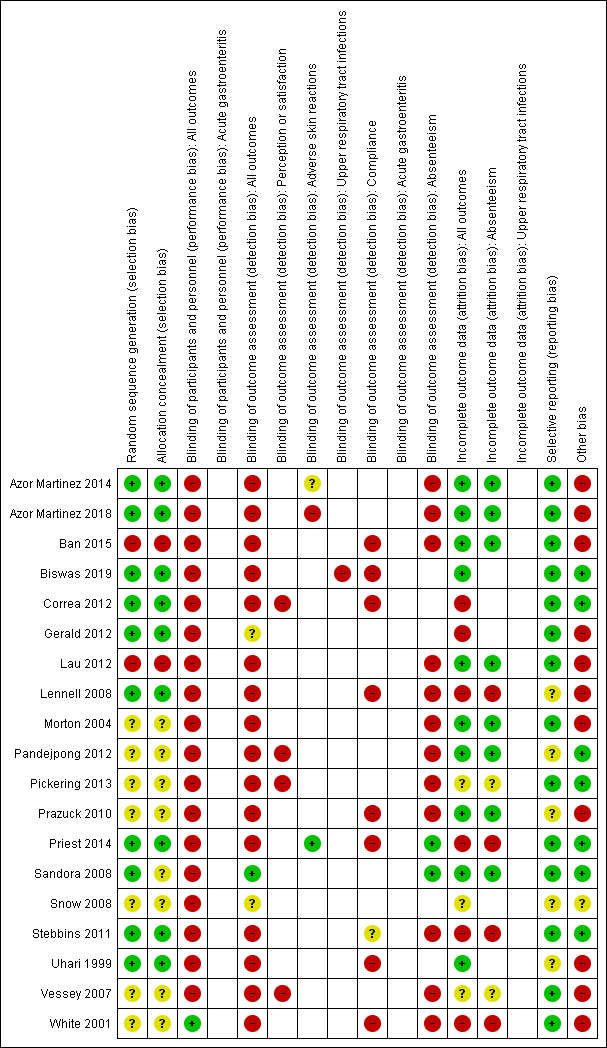
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Random sequence generation
Of the studies, 10 demonstrated a low risk of bias for this domain (Azor Martinez 2014; Azor Martinez 2018; Biswas 2019Correa 2012; Gerald 2012; Lennell 2008; Priest 2014; Sandora 2008; Stebbins 2011; Uhari 1999). For these studies the method of randomization was clearly described by the study authors. Seven studies (Morton 2004; Pandejpong 2012; Pickering 2013; Prazuck 2010; Snow 2008; Vessey 2007; White 2001) were assessed as being unclear as the authors stated that randomization occurred, however the specific method of randomization was not specified. Two studies were at high risk of bias for this domain (Ban 2015; Lau 2012). The Ban 2015 study included only two kindergartens and it was unclear how (and if) randomization actually occurred. Consequently, we rated it as high risk. The Lau 2012 study was a controlled study where allocation was systematic but not random and as such, this was also judged to be at a high risk.
Allocation concealment
In cluster‐randomized trials, clusters are often randomized and allocated at the same time, meaning there is likely to be a low risk of bias related to allocation concealment (Higgins 2011a). As such, if a study provided sufficient details as to how randomization of the sequence occurred (therefore judged as being at a low risk of bias ‐ as above), it was regarded as low risk. The exception to this was the study by Sandora 2008, even though this study was at low risk of bias for random sequence generation, it is not clear whether the investigators were unaware of the allocation schedule prior to recruitment and selection of groups, thus being judged as an unclear risk of bias. To summarize, nine studies (Azor Martinez 2014; Azor Martinez 2018; Biswas 2019; Correa 2012; Gerald 2012; Lennell 2008; Priest 2014; Stebbins 2011; Uhari 1999) were judged as being at low risk, and eight studies were judged as being at an unclear risk (Morton 2004; Pandejpong 2012; Pickering 2013; Prazuck 2010; Sandora 2008; Snow 2008; Vessey 2007; White 2001). Allocation concealment was judged to be a potential concern in two studies where randomization was deemed an issue and as such were judged as being at high risk (Ban 2015; Lau 2012).
Blinding
Performance bias
Due to the nature of the intervention used it was often difficult to blind participants (students; school staff and parents), and as such, all but one study was judged to have been at a high risk of performance bias. Only one study, White 2001, performed adequate blinding of participants through the use of a placebo hand wash which is to be expected for this type of intervention. As such, this was the only study judged to be at a low risk of bias.
Detection bias
Of the studies, only two adequately blinded outcome assessors/reporters (Priest 2014; Sandora 2008). This was achieved in the Priest 2014 study by having telephone interviewers collecting data who were blinded to the group allocation until after the analysis was complete. Similarly, in the Sandora 2008 study, the person collecting data on absences was also blinded. Fifteen studies were at a high risk of bias. Thirteen of these (Azor Martinez 2014; Azor Martinez 2018; Biswas 2019; Correa 2012; Lennell 2008; Lau 2012; Morton 2004; Pickering 2013; Prazuck 2010; Stebbins 2011; Uhari 1999; Vessey 2007; White 2001) reported that the outcomes were recorded by either the parent, teacher or reported by study personnel themselves. As all of these people were unblinded in their respective studies, we have judged this to be at a high risk of bias. The other two studies (Ban 2015; Pandejpong 2012) were judged as being at high risk as they failed to provide sufficient information as to if the outcome assessors were blinded or not, however as these studies were also at high risk of performance bias, we have judged them to also have been at high risk of detection bias.Two studies were judged to have been at an unclear risk (Gerald 2012; Snow 2008) due to the study authors not providing enough information as to how the outcomes themselves were measured, thus precluding them from assessing how outcome assessors may, or may not have been blinded.
Incomplete outcome data
Six trials (Correa 2012; Gerald 2012; Lennell 2008; Priest 2014; Stebbins 2011; White 2001) were at a high risk of attrition bias, all these studies experiencing large losses to follow‐up and high drop out rates. Nine studies were judged to be at a low risk of bias. Of these, seven studies (Azor Martinez 2014; Azor Martinez 2018; Ban 2015; Lau 2012; Morton 2004; Pandejpong 2012; Uhari 1999) did experience loss to follow‐up, however these losses were relatively small and were evenly balanced between treatment groups. Three studies (Biswas 2019; Prazuck 2010; Sandora 2008), also judged to be at low risk of attrition bias reported that no or minimal losses to follow‐up were experienced in the study. Three studies (Pickering 2013; Snow 2008; Vessey 2007) were judged to be at a unclear risk of bias, as insufficient information was provided by the authors in regards to participant flow within the study and whether losses to follow‐up were experienced.
Selective reporting
Fourteen studies (Azor Martinez 2014; Azor Martinez 2018; Ban 2015; Biswas 2019; Correa 2012; Gerald 2012; Lau 2012; Morton 2004; Pickering 2013; Priest 2014; Sandora 2008; Stebbins 2011; Vessey 2007; White 2001) were at low risk of reporting bias, as they provide full and complete reporting of all pre‐specified outcomes, or when a protocol could not be retrieved, all outcomes as specified in the methods section were included in the results. Finally, five studies (Lennell 2008; Pandejpong 2012; Prazuck 2010; Snow 2008; Uhari 1999) were judged to be unclear, as a study protocol could not be retrieved, and insufficient information was provided in the text to allow for a low judgment.
Other potential sources of bias
Eleven studies (Azor Martinez 2014; Azor Martinez 2018; Ban 2015; Gerald 2012; Lau 2012; Lennell 2008; Morton 2004; Prazuck 2010; Uhari 1999; Vessey 2007; White 2001) were judged to be at high risk for other potential sources of bias. Potential sources of bias that could pose additional risk include: when there is clear imbalance in baseline characteristics between groups (for cross‐over trials), loss of clusters in cluster trials, incorrect analysis (such as not accounting for clustering), or evidence of individuals being preferentially recruited to clusters following the randomization of clusters (Higgins 2011a). In the studies by Ban 2015 and Gerald 2012, there were important differences in baseline characteristics between groups. In the Lennell 2008 study, clusters were lost during the trial. In the Morton 2004 and White 2001 studies, which were both crossover trials, there was insufficient washout periods (1‐2 weeks). Finally, the Prazuck 2010 and Uhari 1999 studies did not take into account clustering in their analysis, additionally, as we calculated crude incident rate ratios (IRRs) for Azor Martinez 2014; Azor Martinez 2018; Ban 2015; Lau 2012; Pickering 2013; Prazuck 2010; Vessey 2007; White 2001, this was considered as a risk of bias. Morton 2004 also used an insufficient washout period in their study. Seven studies (Biswas 2019; Correa 2012; Pandejpong 2012; Pickering 2013; Priest 2014; Sandora 2008; Stebbins 2011) were judged at low risk of other potential bias, and only one study (Snow 2008) was at an unclear risk. This was due to the overall poor reporting quality of this paper that precluded a judgment of either high or low.
Effects of interventions
Rinse‐free hand wash versus control
Sixteen studies were included in this comparison (Azor Martinez 2014; Azor Martinez 2018; Ban 2015; Correa 2012; Gerald 2012; Lennell 2008; Morton 2004; Pickering 2013; Prazuck 2010; Priest 2014; Sandora 2008; Snow 2008; Stebbins 2011; Uhari 1999; Vessey 2007; White 2001) All rinse‐free hand wash use was supplemented with an educational regimen that focused on the importance of hand washing and infection control. Some studies also included direct instruction for rinse‐free hand wash usage. The particular details of these concurrent activities is expanded for each outcome. In all but three studies (Azor Martinez 2014; Ban 2015; Sandora 2008), rinse‐free hand wash provision was compared against normal practice supplemented with an educational regimen or activities that encouraged good hand hygiene. Where possible, we calculated and presented the number of total possible study days (henceforth referred to as child‐days possible) in appropriate meta‐analyses. Due to the significant heterogeneity between studies in how they reported their outcomes, we provide specific details for each study below. Where studies did not report the age distribution of the participating children, we have made estimates based on the year levels included and the geographical location the trial took place. A summary of these results can be found in summary of findings Table for the main comparison.
Primary outcomes
Child or student absenteeism for any reason
Two studies contributed data towards this outcome (Priest 2014; Stebbins 2011). Both studies reported an incidence rate ratio (IRR) of absence episodes against the child‐days possible. The provision of rinse‐free hand wash was not effective at reducing the incidence rate of absenteeism for any reason compared to control (IRR 0.91, 95% confidence interval (CI) 0.82 to 1.01, P = 0.07; very low‐certainty evidence; Analysis 1.1). There may be some issues with heterogeneity between studies (Chi2 = 2.43, P = 0.12, I2 = 59%).
Child or student absenteeism due to any illness
Six studies contributed data towards this outcome Ban 2015; Lennell 2008; Pickering 2013; Priest 2014; Vessey 2007; White 2001. The data presented in four of these studies (Ban 2015; Pickering 2013; Vessey 2007; White 2001) was subjected to transformation by the review team in order to convert to a common effect size. This process has been detailed in Appendix 3. When considering all groups, the combined effects show that provision of rinse‐free hand wash is effective in reducing the incidence of absenteeism as a result of any illness (IRR 0.82, 95% CI 0.69 to 0.97, P = 0.02; very low‐certainty evidence; Analysis 1.2). We stratified the data by subgroups based on the age of children. The provision of rinse‐free hand wash was no more of less effective in reducing the incidence of absenteeism in students younger than five years, compared to control (IRR 0.76, 95% CI 0.55 to 1.07, P = 0.11). This was also the case for students aged five to 12 years old (IRR 0.92, 95% CI 0.75 to 1.14, P = 0.45). For each analysis, there was substantial heterogeneity between studies (Analysis 1.2.1: Chi2 = 4.40, P = 0.04, I2=77%; Analysis 1.2.2: Chi2 = 10.72, P = 0.005, I2 = 81%; and Analysis 1.2.3: Chi2 = 28.24, P < 0.001, I2 = 82%). However, given the small number of included studies, this needs to be interpreted with caution. We conducted a sensitivity analysis on these data to investigate the choice of model used (fixed versus random). There was a difference for the subgroup of preschool age (< five years old), with an effect estimate for the fixed‐effect model of 0.85 (95% CI 0.78 to 0.94) and the random‐effects model of 0.76 (95% CI 0.55 to 1.07). We have presented the results for the random‐effects model as these are more conservative and align with the directive of the protocol (Munn 2017).
Adverse skin reactions
Pooled results
Three studies (n = 4365) contributed data towards this outcome (Azor Martinez 2014; Azor Martinez 2018; Priest 2014). This analysis has been further separated into subgroups based on the age of the participating students. For students aged birth and three years, there was no important difference in the occurrences of adverse skin reactions for those assigned to rinse‐free hand wash versus control (RR 2.64, 95% CI 0.11 to 64.59, P = 0.55). There was also no difference in students aged five to 11 years (RR 1.02, 95% CI 0.79 to 1.31, P = 0.89). The overall effect again, shows no important differences between groups (RR 1.03, 95% CI 0.80 to 1.32, P = 0.84 Analysis 1.3). There was no concern for heterogeneity between studies (Chi2= 0.34, P = 0.56, I2 = 0%). Priest 2014 reported 115 students randomized to receive rinse‐free hand wash developed an adverse skin reaction, compared to 100 randomized to the control group. Azor Martinez 2014 reported that one child who received rinse‐free hand wash showed worsening atopic dermatitis and was excluded from the group, and no reactions were observed in the control group. A similar result was also reported in a later study by the same authors; one student with existing dermatitis on the hand showed an exacerbation while no adverse events were observed in controls (Azor Martinez 2018).
Single study results
The majority of studies only provided a narrative report of the findings on this outcome. Ban 2015 make no specific mention of adverse events, but state 15 children (control n = 9; intervention n = 6) were lost to follow‐up. No further detail was provided to determine if this loss was related to adverse events. Morton 2004 reported that 10 children were removed from the study after developing skin irritations; however, as this was a cross‐over trial, the authors provided no detail as to what arm these students were in at the time the skin irritation developed. In the study by Vessey 2007, one student withdrew due to both the rinse‐free hand wash and soap control being too irritating. White 2001 report that seven students were removed from the study post‐randomization, after teachers or parents, or both, reported changes in skin conditions such as chapping or redness, or both; however, no information is provided if these children were in the active rinse‐free hand wash or the placebo group.
No adverse events were reported in the studies by Correa 2012; Gerald 2012; Pickering 2013; Prazuck 2010 and Sandora 2008. While no adverse events were reported by Lennell 2008, there were 10 reports of side‐effects due to the discoloration of clothing. Adverse events were not discussed in Snow 2008; Biswas 2019; Stebbins 2011 and Uhari 1999.
Secondary outcomes
Child or student absenteeism due to acute respiratory illness
Six studies contributed data towards this outcome (Azor Martinez 2014; Azor Martinez 2018; Biswas 2019; Sandora 2008; Stebbins 2011; White 2001). The data presented in three of these studies was subjected to transformation by the review team in order to convert to a common effect size (Azor Martinez 2014; Azor Martinez 2018; White 2001). This process has been detailed in Appendix 3. The overall effect shows that the provision of rinse‐free hand wash reduces the incidence of absenteeism due to respiratory illness (IRR 0.79, 95% CI 0.68 to 0.92, P = 0.005; very low‐certainty evidence; Chi2 = 27.45, P < 0.0001, I2 = 82%; Analysis 1.4). We stratified the data based on the age of the participating students. For students aged between birth and three years, the provision of rinse‐free hand wash resulted in reduced respiratory illness‐related absenteeism (IRR 0.77, 95% CI 0.72 to 0.82, P < 0.001; 1 study). For primary school students (five to 14 years old), there was no observed effect (IRR 0.79, 95% CI 0.61 to 1.03, P = 0.08); however, statistical heterogeneity was identified (Chi2 = 27.13, P < 0.001, I2 = 85%). Once again, there are some concerns of heterogeneity between all included studies (Chi2 = 27.45, P < 0.0001, I2 = 82%). We conducted a sensitivity analysis on this data to investigate the choice of model used (fixed versus random). There was a difference for the subgroup of primary school age (five to 14 years old), with an effect estimate for the fixed effect model of 0.75 (95% CI 0.70 to 0.80), and the random‐effects model of 0.79 (95% CI 0.61 to 1.03). We have presented the results for the random‐effects model as these are more conservative and align with the directive of the protocol (Munn 2017).
It is important to note, that Sandora 2008 report that 285 students underwent randomization (Figure 1 of primary literature), but this is inconsistent with the reporting of Table 1 (primary literature), which does not add up to 285 (292) and includes a footnote "numbers may not sum to group totals for all of the variables because of missing responses" (quote; control group says 144 but Figure 1 says 139). Due to the poor reporting by the study authors, these findings are unreliable. Additionally, for the Biswas 2019 study, only episodes of influenza like illness was presented, which we have used as a proxy for respiratory related absenteeism.
Absenteeism due to gastrointestinal illness
Four studies contributed data towards this outcome (Azor Martinez 2014; Prazuck 2010; Sandora 2008; White 2001). The data presented in two of these studies was subjected to transformation by the review team in order to convert to a common effect size (Prazuck 2010; White 2001). This process has been detailed in Appendix 3. The analysis shows that the provision of rinse‐free hand wash resulted in reduced incidence of absenteeism compared to the control groups (IRR 0.79, 95% CI 0.73 to 0.85, P < 0.00001; Analysis 1.5); however, there are some concerns over study heterogeneity (Chi2 = 21.48, P < 0.001, I2 = 86%). That being said, it should be noted that the control groups in Azor Martinez 2014 and Sandora 2008 did not provide any formal education program on hand washing, whilst both Prazuck 2010 and White 2001 did. Subgrouping was not pre‐specified in the protocol to occur based on the provision (or lack thereof) of co‐interventions within the comparison group. In addition, the findings presented in the study by Sandora 2008 are unreliable, for the same reasons as presented above.
Compliance with the hand hygiene strategy
Compliance with the intervention appeared to range from moderate to high compliance (9 studies, 10,749 participants; very‐low certainty evidence). No study authors reported substantial issues with compliance. The individual study results are discussed further below.
Ban 2015 reported the consumption of intervention products to evaluate compliance for the intervention group. Over the course of the study (20 September 2010 to 28 September 2011), the intervention group utilized 20,600 × 20 mL bottles of instant hand sanitizer. They also calculated the average person usage (mL used/person day) of rinse‐free hand wash as 1.4.
Biswas 2019 reported the number of handwashing events against the total number of handwashing opportunities as observed by a member of the study team. In 921 opportunities, school children in the intervention group washed their hands in 604 opportunities (66%). In 802 opportunities, school children in the control group washed their hands in 171 (21%). Of these handwashing opportunities, school children in the intervention group used hand sanitizer in 91% of the observed handwashing events. However, it is important to note, that a member of the study team was not present to observe every potential opportunity for school children to wash their hands and the data reported are simply those from when a study member observed a handwashing event towards the end of the intervention period. It was also reported that the average consumption of hand sanitizer per child was 4.3 mL (95% CI = 1.5 mL to 7.1 mL).
Lennell 2008 reported that use of rinse‐free hand wash varied among intervention day care centres. With total usage ranging from 19 L to 60 L per 50 children; the study authors estimated that students used the rinse‐free hand wash two to six times per day.
Prazuck 2010 reported that the 300 mL rinse‐free hand wash container was replaced three times on each table (roughly every four weeks) for each classroom fitted with the rinse‐free hand wash. This indicated to the study authors that compliance to the sanitization regimen was high.
There were limited data regarding compliance in the study by Priest 2014, who stated that they had to change their rinse‐free hand wash for 41 of the 396 classrooms, as some children had become reluctant to use the initial hand sanitizer product before eating their lunch, complaining of the taste of the sanitizer persisting on their fingers and food. A substitute was provided by the authors at week 10 of the study. This substitute had no ‘‘flavor’’ (quote) and both brands contained 60% ethanol. Following this change to the product, the median classroom difference in sanitizer usage between the first 10 weeks and the second 10 weeks (only in classrooms that switched products) was 2220 mL; the interquartile range of the usage difference was 2420 mL to 645 mL. All schools in the intervention group complied with the protocol of dispensing a volume equivalent to at least 45 mlLper child of hand sanitizer solution over the trial period. The average volume of hand sanitizer solution dispensed per child over the 34 schools was 94 mL.
Snow 2008 compared two forms of education with a control. In the control group, teachers simply instructed their students to “Wash your hands then line up for lunch” (quote). This was compared to teachers of classrooms who after instructing students to “Wash your hands then line up for lunch” (quote), walked over to the sink and began washing their hands (intervention one). The final intervention group was a guest educator teaching a 30‐minute grade‐appropriate lesson on hand hygiene principles and when rinse‐free hand wash is appropriate to use, coupled with the teacher demonstration that occurred in intervention one (intervention two). The study authors only reported outcome data on the rates of hand hygiene, each group (even controls) had access to the rinse‐free hand wash. The study authors reported narratively that both interventions one and two improved the rate at which alcohol‐based hand rubs (rinse‐free hand wash) were used for hand hygiene in children. However, each group (even controls) had some access to rinse‐free hand wash. These outcome data simply inform us that education improves use of alcohol‐based hand rubs in children, as recorded by the study authors.
Stebbins 2011 collected numerical outcome data regarding compliance. These results were reported in the earlier study (Stebbins 2010); however, these two individual papers reported on the same data set. Teachers were asked to complete surveys on their students' hand hygiene. Of the 16‐question survey, four questions were directly related to student compliance:
-
students wash hands more than three times a day;
-
students use hand sanitizer two times a day;
-
students use hand sanitizer four times a day; and
-
average number of times students wash/sanitize per day (direct report).
The study authors observed no difference between the mean scores for teacher observations for the rinse‐free hand wash group and control for questions one (rinse‐free hand wash: mean = 3.71 versus control: mean = 3.35, P = 0.042) and four (rinse‐free hand wash: mean = 3.95 versus control: 3.08, P = 0.144). However, teachers in the rinse‐free hand wash group observed their students using hand sanitizer at least twice a day (mean = 4.38) and four times a day (mean = 3.18), compared to controls (twice a day: mean = 2.82, P < 0.001; four times a day: mean = 1.89, P < 0.001).
In the study by Uhari 1999, the study nurse estimated in the course of her visits to the child day care centres that the children, in general, complied with all the instructions and washed their hands diligently. The compliance was calculated as the percentage of events where instructions were followed. The overall estimates of compliance varied from about 60% to 90% between the intervention day care centres, with a mean of 80%.
Of the 72 initial classes involved in the study by White 2001 (1626 student participants), 32 classes (16 active and 16 control; 769 student participants) were retained for analysis. The remainder of the classes were dropped from the data analysis because of noncompliance with minimum adequate product use standards (less than three uses per day).
Perception of the hand hygiene strategy
Teachers and students perceived rinse‐free hand wash positively and were willing to continue its use (3 studies, 1229 participants; very‐low certainty evidence). The individual study results are discussed further below.
Correa 2012 reported that all intervention centre teachers perceived the use of the alcohol‐based hand rubs (rinse‐free hand wash) as a more convenient hand hygiene method and manifested a willingness to continue its use.
Pickering 2013 conducted semi‐structured interviews with staff and students of participating schools. In regards to the perception of rinse‐free hand wash, 100% of teachers at intervention schools said they would prefer the permanent provision of rinse‐free hand wash over the provision of soap at their schools. One teacher stated that “I find it [sanitizer] easy to use than soap… If both were given, then you will find the hand sanitizer being used more than soap and water” (quote). For students, 91% stated that they would choose sanitizer to clean their hands over soap and water. Students at sanitizer schools reported that they perceived cleaning hands with rinse‐free hand wash to take a shorter time than hand washing with soap and water. Additionally, 80% of students in sanitizer schools said they disagreed with the statement that the sanitizer has an unpleasant odor, and 87% of students disagreed that using sanitizer made their hands feel dry.
Vessey 2007 conducted semi‐structured interviews with teachers to observe their perceptions of student rinse‐free hand wash use. No numerical data were available.
Many of the participants' observations indicated that they preferred the use of the hand sanitizer over soap and water as it better matched the pragmatics of the school day. The amount of time required was a key consideration, as noted in these comments: “....they [the students] would try to skip it [hand washing with soap and water] or wouldn't do it properly ...it took up to probably an extra 10 minutes to get out to lunch. I liked the hand sanitizer because it took so long to get the kids out to lunch [when hand washing with soap and water] and my kids would use it [hand sanitizer] because it was quick” (quote).
Improved adherence and better hand cleaning by students during the study period were also noted in teachers' comments:
-
“We have the sanitizer by the door and it was funny, the kids walk by it and subconsciously would just take a squirt...Lots of time I don't think they were paying attention to what they were doing”;
-
“It [hand sanitizer] was easy, it smelled good. It didn't make their food taste funny...in the lunchroom...”; and
-
“you can't let the water run...they touch [the faucet] with their dirty hands...touch it again with their clean hands...” (all direct quotes).
The ability to observe student behavior and maintain classroom decorum were other perceived benefits of hand sanitizers:
-
“We teach them a lot about coughing and sneezing into their hands and then to go wash their hands but many times they are in the classrooms and they can't leave. But if you have the gel, they can go over and use it.”; and
-
“When you have them go to in the bathroom with soap and water you can't tell if they are really using it...” (both direct quotes).
Rinse‐free hand wash and instruction versus rinse‐free hand wash and no instruction
One included study, Lau 2012, investigated the provision of rinse‐free hand wash with education and instruction versus rinse‐free hand wash provision alone. The data presented in this study were subjected to transformation by the review team in order to convert to a common effect size. This process has been detailed in Appendix 3.
Primary outcomes
Child or student absenteeism for any reason
There was no clear evidence of a difference with the provision of education and instruction with rinse‐free hand wash on the number of days spent absent for any reason (IRR 1.07, 95% CI 0.97 to 1.18, P = 0.18; Analysis 2.1).
Child or student absenteeism due to any illness
The provision of education and instruction produced no effect on the incidence of absence days compared to no education or instruction (IRR 0.99, 95% CI 0.89 to 1.10, P = 0.86; Analysis 2.2)
Adverse skin reactions
This study did not report on adverse skin reactions.
Secondary outcomes
This study did not report on any of the secondary outcomes.
Rinse‐free hand wash every 120 minutes versus rinse‐free hand wash once before lunch
Only one study was included for this comparison (Pandejpong 2012), However, the overall reporting of these findings is poor. Attempts were made to contact the study authors and despite the study authors stating that there was no loss to follow‐up, they also stated that they only analyzed data for 538 of the 540 students randomized to the control group. The rates of absenteeism due to confirmed respiratory illness were 0.026 and 0.025 for the rinse‐free hand wash before lunch group and the rinse‐free hand wash every 120 minutes group, respectively. However, these data have mainly been presented as a rate difference, which has been inputted directly to RevMan 5 (Review Manager 2014) (as a risk difference (RD).
Primary outcomes
Child or student absenteeism for any reason
This study did not collect data on this outcome.
Child or student absenteeism due to any illness
This study did not collect data on this outcome.
Adverse skin reactions
The study reported narratively that no adverse events occurred during the study.
Secondary outcomes
Child or student absenteeism due to acute respiratory illness
For the rinse‐free hand wash every 120 minutes compared to rinse‐free hand wash at lunch time, there was no difference between the two interventions RD 0.001, 95% CI 0.0005 to 0.007 (Analysis 3.1).
Perception of the hand hygiene strategy
Pandejpong 2012 stated that the usage of the hand sanitizer was reported by the authors as a seemingly enjoyable activity for the children.
Rinse‐free hand wash every 60 minutes versus rinse‐free hand wash every 120 minutes
One study, Pandejpong 2012, compared rinse‐free hand wash with instructions to use it every 60 minutes for one group (n = 452) and every 120 minutes in the another group (n = 447) .
Primary outcomes
Child or student absenteeism for any reason
This study did not collect data on this outcome.
Child or student absenteeism due to any illness
This study did not collect data on this outcome.
Adverse skin reactions
The study reported narratively that no adverse events occurred during the study.
Secondary outcomes
Child or student absenteeism due to acute respiratory illness
There was no difference between the two instruction regimens on absenteeism due to acute respiratory illness: RD 0.009, 95% CI 0.002 to 0.015 (Analysis 4.1).
Perception of the hand hygiene strategy
Pandejpong 2012 stated that the usage of the hand sanitizer was reported by the authors as a seemingly enjoyable activity for the children.
Rinse‐free hand wash every 60 minutes versus rinse‐free hand wash once before lunch
One study, Pandejpong 2012, compared rinse‐free hand wash with instructions to use it every 60 minutes for one group (n = 452) and before lunch for the other (n = 538)
Primary outcomes
Child or student absenteeism for any reason
This study did not collect data on this outcome.
Child or student absenteeism due to any illness
This study did not collect data on this outcome.
Adverse skin reactions
The study reported narratively that no adverse events occurred during the study.
Secondary outcomes
Child or student absenteeism due to acute respiratory illness
For rinse‐free hand wash every 60 minutes compared to rinse‐free hand wash at lunch, the RD was 0.0096 (95% CI 0.004 to 0.016; Analysis 5.1).
Perception of the hand hygiene strategy
Pandejpong 2012 stated that the usage of the hand sanitizer was reported by the authors as a seemingly enjoyable activity for the children.
Discussion
Summary of main results
Our review found 19 studies that met the inclusion criteria with 30,747 participants across different types of schools in 11 countries. For the main outcome (child or student absenteeism for any reason), only two studies reported data. The pooled estimate for rinse‐free hand washing was incidence rate ratio (IRR) 0.91 (95% confidence interval (CI) 0.82 to 1.01; I2 = 59%), with very low‐certainty evidence. For child or student absenteeism due to any illness, we included six studies in the meta‐analysis with a pooled IRR of 0.82 (95% CI of 0.69 to 0.97; I2 = 82%), once again with very low‐certainty evidence. When evaluating child or student absenteeism due to acute respiratory illness, the pooled results from six studies was an IRR of 0.79 (95% CI 0.68 to 0.92; I2 = 82%), very low‐certainty evidence. When evaluating child or student absenteeism due to acute gastrointestinal illness, the pooled estimate from four studies was IRR 0.79 (95% CI 0.73 to 0.85; I2 = 86%), low‐certainty evidence. It did not appear that rinse‐free hand washing was associated with an important increase in skin reactions. Compliance with the intervention varied between moderate and high (9 studies, 10,749 participants; very‐low certainty evidence), and teachers and students perceived rinse‐free hand wash positively and were willing to continue its use (3 studies, 1229 participants; very‐low certainty evidence). Summarising the main results of this review, there was no evident impact on absenteeism for any illness; however, rinse‐free hand washing did appear to have a small and potentially beneficial effect on reducing overall illness‐related absenteeism and respiratory and gastrointestinal illness‐related absenteeism, and this effect may be more pronounced in a younger student cohort.
Overall completeness and applicability of evidence
In this review, we were able to address some our first objective, the effectiveness of rinse‐free hand washing for reducing absenteeism (due to illness or for any reason) in preschool and school children compared to no hand washing, conventional hand washing with soap and water or other hand hygiene strategies.
Although not many of our included studies addressed the main outcome of interest, substantially more investigated illness‐related absenteeism. Where statistically and clinically appropriate, we combined results across studies in meta‐analysis. To enable this pooling, at times, we needed to contact study authors to request their data in a different format; other times, we needed to use the data presented in the papers and convert these to a form suitable for pooling. Occasionally, the data were simply not accessible in a format that facilitated meta‐analysis, despite requests to study authors. Where possible, we chose to combine studies in this review in a meta‐analysis, although the interventions and settings differed somewhat in terms of their intensity, co‐interventions and settings. This enabled us to assess statistical heterogeneity between trials and also generate a pooled estimate of the effect for use in the 'Summary of findings' table and to inform practice.
Given the paucity of the evidence, we were unable to address our second objective for this review, where we aimed to determine which rinse‐free hand washing products are the most effective (if head‐to‐head comparisons exist), whether there is any supervision and what effect additional strategies in combination with rinse‐free hand washing have on the outcomes of interest. Studies did not always clearly report what the active ingredient was for the rinse‐free hand wash or the product name, or how it was applied.
In terms of applicability of the results of this review, the included trials were pragmatic rather than explanatory (Treweek 2009), taking place in real settings with reasonable inclusion and exclusion criteria. When considering the applicability of the interventions in the real world, most of the rinse‐free hand washing programs were accompanied by education sessions or material, with clear guidance on how (and when) it should be used. The intervention may be reasonably easy (and potentially convenient) to implement. Some of the advantages of rinse‐free hand washing were established by Vessey 2007, who stated that if schools do not have sinks in the classrooms, students must leave class every time their hands need washing; and they also mentioned the issues of appropriately adjusting the water temperature. Hand sanitizers are able to eliminate these problems. Additionally, Vessey 2007 noted that ease of dispenser installation, low malfunctioning rates, easy identification of need for refills, and dispenser placement (in a highly visible and readily accessible locations) are aspects that are important when a hand gel sanitizer is used. When considering applicability, it will also be important for end users to consider their own rates of gastrointestinal and respiratory illness, and consider whether the investment in rinse‐free hand washing is worth it based on the relatively small beneficial impact of the programs. In this review, the largest impact was seen for younger children and as such the intervention may be more justified for younger age groups. Importantly, rinse‐free hand wash may result in additional costs to any educational facility that will need to be considered in any implementation program.
Due to a lack of reporting (or poor reporting), it is difficult to judge the impact of rinse‐free hand washing on adverse events in our review. Other studies have noted similar concerns, and Morton 2004 noted that with rinse‐free products the primary risk is eye irritation if the gel gets in the eye. They also recommended that children with underlying eczema or other underlying chronic skin conditions do not use the gel. In addition, poor reporting made it difficult to assess the age of the children that participated in each study, and in some cases, age had to be estimated based on the region and year levels (or grade) that children belonged.
Students and teachers seem receptive to rinse‐free hand washing and compliance appears to be high, although there was minimal information in the included studies addressing compliance and how to address compliance. Uhari 1999 noted that the study nurse found that the children in intervention centres generally complied with all instructions and washed their hands diligently, especially on arrival and before eating, even without reminders. The overall estimates of compliance (compliance was calculated as the percentage of events where instructions were followed) varied from about 60% to 90% in the intervention centres, with a mean of 80%. Vessey 2007 reported that teachers preferred that the dispensers be placed in the classroom, or outside the restroom door, and also in the cafeteria area.
Quality of the evidence
Overall, the certainty of the evidence was either low or very low. For each outcome presented in the summary of findings Table for the main comparison, we downgraded the certainty of the evidence for poor methodological quality. In terms of selection bias, neither randomization nor allocation concealment were a concern in many of the studies; however, there were obvious and understandable risks with regards to performance and detection bias across the studies. Only one study, White 2001, performed adequate blinding of participants by using a placebo formulation in the control group. We downgraded multiple outcomes for imprecision and, as such, further trials (especially investigating the main outcome of interest) are required. There were also multiple occurrences of inconsistency between study results contributing to an outcome. Additionally, there were concerns regarding detection bias, with 15 of the included studies being considered at high risk of bias for this domain, largely due to self‐reporting of outcomes. On no occasion did we downgrade an outcome for indirectness or publication bias.
Potential biases in the review process
We did not identify any potential biases in the review process. We conducted a comprehensive search for published and unpublished studies; we included studies in languages other than English; and we had two members of the team independently screen, select and extract data from studies.
Agreements and disagreements with other studies or reviews
There are other reviews that have a similar focus to ours, although this review is the first to focus specifically on all types of rinse‐free hand washing in schools and preschools. A review by Ejemot‐Nwadiaro 2015, which evaluated hand washing with water and soap to reduce diarrhea in children, found a reduction in diarrhea episodes of "around one‐third (RR 0.70; 95% CI 0.58 to 0.85)" (quote). Another systematic review, published in 2004, evaluated the effectiveness of rinse‐free hand sanitizers for reducing absenteeism related to illness in elementary school children. The review authors found six trials of low quality and poor reporting (Meadows 2004) and stated that although all included studies found a beneficial effect, the review authors could not say conclusively that the intervention was beneficial, due to the poor quality of included studies.
More recently, a systematic review was published in 2016 on hand hygiene interventions for children in educational settings (Willmott 2016). The authors of that review concluded that the evidence is inconsistent regarding the effectiveness of hand hygiene interventions, although they may decrease respiratory tract infections amongst children. Although this review did not focus explicitly on rinse‐free interventions they found a similar result to our review in that the intervention appears to have more benefit in younger children.

PRISMA study flow diagram.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
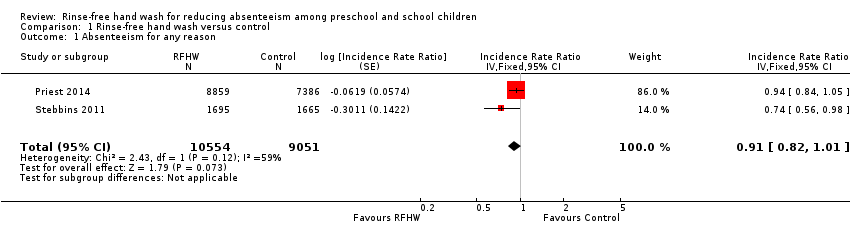
Comparison 1 Rinse‐free hand wash versus control, Outcome 1 Absenteeism for any reason.

Comparison 1 Rinse‐free hand wash versus control, Outcome 2 Absenteeism due to any illness.
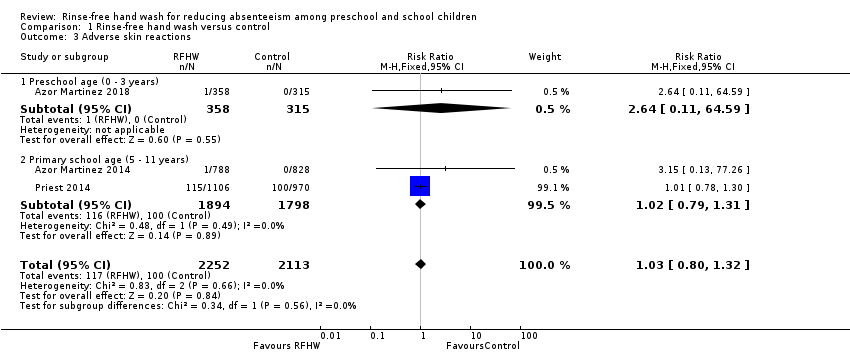
Comparison 1 Rinse‐free hand wash versus control, Outcome 3 Adverse skin reactions.

Comparison 1 Rinse‐free hand wash versus control, Outcome 4 Absenteeism due to acute respiratory illness.

Comparison 1 Rinse‐free hand wash versus control, Outcome 5 Absenteeism due to acute gastrointestinal illness.

Comparison 2 Rinse‐free hand wash with instruction versus rinse‐free hand wash with no instruction, Outcome 1 Absenteeism for any reason.
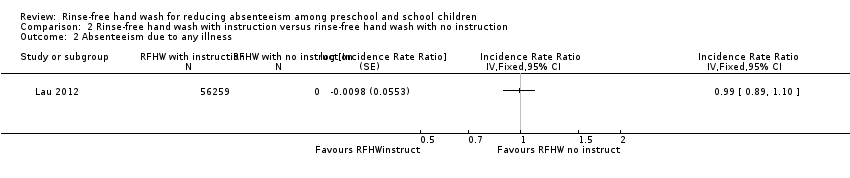
Comparison 2 Rinse‐free hand wash with instruction versus rinse‐free hand wash with no instruction, Outcome 2 Absenteeism due to any illness.
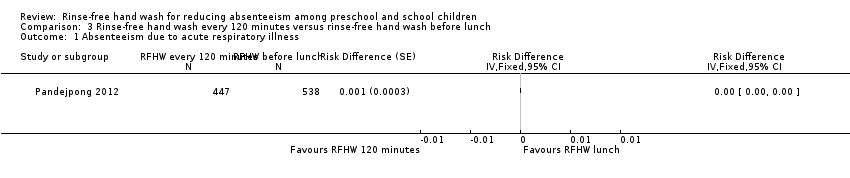
Comparison 3 Rinse‐free hand wash every 120 minutes versus rinse‐free hand wash before lunch, Outcome 1 Absenteeism due to acute respiratory illness.

Comparison 4 Rinse‐free hand wash every 60 minutes versus rinse‐free hand wash every 120 minutes, Outcome 1 Absenteeism due to acute respiratory illness.

Comparison 5 Rinse‐free hand wash every 60 minutes versus rinse‐free hand wash before lunch, Outcome 1 Absenteeism due to acute respiratory illness.
| Rinse‐free hand wash compared to no rinse‐free hand wash program for reducing absenteeism among preschool and school children | ||||||
| Patient or population: children aged from birth to 14 years old | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with control | Risk with rinse‐free hand wash | |||||
| Absenteeism for any reason (within the study period) Calculated as: an incident rate per child‐days possible Length of time observed: range = 5 to 6 months | Baseline risk (Priest 2014)aa | Incidence rate ratio 0.91 | (2 RCTs) | ⊕⊝⊝⊝ | ‐ | |
| 32 days absent per 1000 | 29 per 1000 | |||||
| Absenteeism due to any illness (within the study period) Calculated as: an incident rate per child‐days possible Length of time observed: range = 1 to 11 months | Baseline risk (Priest 2014)bb | Incidence rate ratio 0.82 | (6 RCTs) | ⊕⊝⊝⊝ | ‐ | |
| 16 days absent per 1000 | 13 per 1000 | |||||
| Adverse skin reactions (within the study period) Calculated as: number of events Length of time observed: range = 5 to 8 months | Study population | RR 1.03 | 4365 (3 RCTs) | ⊕⊝⊝⊝ | ‐ | |
| 47 per 1000 | 49 per 1000 | |||||
| Absenteeism due to acute respiratory illness (within the study period) Calculated as: an incident rate per child‐days possible Length of time observed: range = 1 to 8 months | Baseline risk (Azor Martinez 2018)cc | Incidence rate ratio 0.79 | (6 RCTs) | ⊕⊝⊝⊝ | ‐ | |
| 42 days absent per 1000 | 33 per 1000 | |||||
| Absenteeism due to acute gastrointestinal illness (within the study period) Calculated as: an incident rate per child‐days possible Length of time observed: range = 1 to 8 months | Baseline risk (Prazuck 2010)dd | Incidence rate ratio 0.79 | (4 RCTs) | ⊕⊕⊝⊝ | ‐ | |
| 8 days absent per 1000 | 6 per 1000 | |||||
| Compliance with the intervention or program Assessed with: different measures of compliance Length of time observed: range = 1 to 12 months | 9 studies addressed compliance using diverse approaches. Broadly, compliance with the intervention appeared to range from moderate to high compliance. Narrativley, no authors reported substantial issues with compliance. | 10,749 | ⊕⊝⊝⊝ | ‐ | ||
| Perception of the hand hygiene strategy or satisfaction with the hand hygiene strategy Assessed with: different measures of perception Length of time observed: range = 3 to 11 months | 3 studies addressed perception. Of these, 2 studies, Pickering 2013 and Vessey 2007, conducted semi‐structured interviews with staff and students. No numerical data were reported by Pickering 2013; however, rinse‐free hand wash was perceived favorably by the teaching staff. Vessey 2007 reported that 100% of interviewed staff would prefer rinse‐free hand wash over soap at their school; 91% of students interviewed stated they would preferentially choose rinse‐free hand wash over soap and water to wash their hands. 1 study, Correa 2012, reported that teachers of rinse‐free hand wash‐assigned schools perceived rinse‐free hand wash positively and were willing to continue its use. | 1229 | ⊕⊝⊝⊝ | ‐ | ||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| a Downgraded two levels due to a high risk of performance bias and detection bias, as the students, parents of students and teachers were aware of treatment assignment. Both studies are also at high risk of attrition bias. Downgraded one level due to confidence intervals ranging from a potentially important difference (0.82) to a negligible difference (1.01). aaBaseline risk for absenteeism for any reason was calculated using the values provided in the study by Priest 2014 as 3.2% (days spent absent over child‐days possible). | ||||||
| Section of review | Unused methods | Justification |
| Electronic searches | We had planned to search International Initiative for Impact Evaluation (3ie) Systematic Reviews Database. | We did not search International Initiative for Impact Evaluation (3ie) Systematic Reviews Database as planned. |
| Measures of treatment effect | Time‐to‐event data We had planned to analyze time‐to‐event data as dichotomous data, where appropriate. If hazard ratios had been reported and had been suitable for synthesis, we planned to compute RR for other similar studies, so that a synthesis across studies could occur. | Due to the reporting of the data in the primary studies, this did not eventuate. |
| Continuous data As absenteeism can occur on multiple occasions, it may have been that mean days absent were reported. We had planned to calculate effect sizes as mean differences and to present these with 95% confidence intervals. If different scales had been used, we had planned to report effect sizes using standardized mean differences (SMD). | Absenteeism was not reported in any of the papers as continuous data. | |
| Assessment of reporting biases | If there had been an adequate number of studies (at least 10), we would have created funnel plots to investigate reporting bias (Sterne 2011). In the case of 10 or more studies, for continuous data, we would have used Egger's test (Egger 1997). | We did not have any analyses that included 10 or more studies. |
| If effect sizes appeared to depend on the size of the trial, we would have explored whether this association was due to heterogeneity or publication bias. | We did not have enough studies to adequately investigate small study effects and publication bias. | |
| Subgroup analysis and investigation of heterogeneity | We had intended to explore heterogeneity by conducting the subgroup analyses listed below. 2. The frequency of the intervention (i.e. only after meals, before and after meals and toilet breaks, on arrival at preschool or school, etc.). 3. The person delivering the intervention or responsible for the intervention (teachers or caregivers compared to a child‐initiated intervention). 4. The means of recording absence (teacher reported compared to other measures). 5. The provision of hand‐wash alone versus the provision of hand wash plus additional strategies (such as education). 6. By gross national income per capita, based on World Banks classification of low‐, middle‐ and high‐income countries. | Insufficent details or information was able to be extracted from the included studies, preventing subgroup analysis. |
| Sensitivity analysis | We had intended to carry out sensitivity analyses, when necessary, to assess the robustness of our results to the exclusion of studies at high risk of bias (determined by both the allocation concealment and blinding of outcome assessment 'Risk of bias' criteria being rated as high) | All studies were at an overall high risk of bias; therefore, we did not perform this sensitivity analysis. |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Absenteeism for any reason Show forest plot | 2 | 19605 | Incidence Rate Ratio (Fixed, 95% CI) | 0.91 [0.82, 1.01] |
| 2 Absenteeism due to any illness Show forest plot | 6 | Incidence Rate Ratio (Random, 95% CI) | 0.82 [0.69, 0.97] | |
| 2.1 Preschool age (< 5 years) | 2 | Incidence Rate Ratio (Random, 95% CI) | 0.76 [0.55, 1.07] | |
| 2.2 Primary school age (5 ‐ 12 years) | 3 | Incidence Rate Ratio (Random, 95% CI) | 0.92 [0.75, 1.14] | |
| 2.3 Mixed age range (2 ‐ 13 years) | 1 | Incidence Rate Ratio (Random, 95% CI) | 0.55 [0.38, 0.80] | |
| 3 Adverse skin reactions Show forest plot | 3 | 4365 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.80, 1.32] |
| 3.1 Preschool age (0 ‐ 3 years) | 1 | 673 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.64 [0.11, 64.59] |
| 3.2 Primary school age (5 ‐ 11 years) | 2 | 3692 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.79, 1.31] |
| 4 Absenteeism due to acute respiratory illness Show forest plot | 6 | 414197 | Incidence Rate Ratio (Random, 95% CI) | 0.79 [0.68, 0.92] |
| 4.1 Preschool age (0 ‐ 3 years) | 1 | 96187 | Incidence Rate Ratio (Random, 95% CI) | 0.77 [0.72, 0.82] |
| 4.2 Primary school age (5 ‐ 14 years) | 5 | 318010 | Incidence Rate Ratio (Random, 95% CI) | 0.79 [0.61, 1.03] |
| 5 Absenteeism due to acute gastrointestinal illness Show forest plot | 4 | 222754 | Incidence Rate Ratio (Fixed, 95% CI) | 0.79 [0.73, 0.85] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Absenteeism for any reason Show forest plot | 1 | Incidence Rate Ratio (Fixed, 95% CI) | Totals not selected | |
| 2 Absenteeism due to any illness Show forest plot | 1 | Incidence Rate Ratio (Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Absenteeism due to acute respiratory illness Show forest plot | 1 | Risk Difference (Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Absenteeism due to acute respiratory illness Show forest plot | 1 | Risk Difference (Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Absenteeism due to acute respiratory illness Show forest plot | 1 | Risk Difference (Fixed, 95% CI) | Totals not selected | |

