Intervenciones quirúrgicas para el estrabismo vertical en la parálisis del músculo oblicuo superior
Resumen
Antecedentes
La parálisis del músculo oblicuo superior es una causa frecuente de estrabismo vertical en adultos y niños. Los pacientes pueden estar sintomáticos debido a diplopía vertical binocular o a la inclinación compensatoria de la cabeza necesaria para mantener una visión única. La mayoría de los pacientes que están sintomáticos optan por someterse a una cirugía por estrabismo, pero no se conoce el tratamiento quirúrgico óptimo para el estrabismo vertical en los pacientes con parálisis del músculo oblicuo superior.
Objetivos
Evaluar los efectos relativos de los tratamientos quirúrgicos en comparación con otra intervención quirúrgica, intervención no quirúrgica u observación para el estrabismo vertical en pacientes con parálisis del músculo oblicuo superior.
Métodos de búsqueda
Se hicieron búsquedas en el Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials) (CENTRAL) (que contiene el registro de ensayos del Grupo Cochrane de Trastornos de los Ojos y la Visión [Cochrane Eyes and Vision Group]) (2016, número 12), MEDLINE Ovid (1946 hasta 13 diciembre 2016), Embase Ovid (1947 hasta 13 diciembre 2016), Latin American and Caribbean Health Sciences Literature Database (LILACS) (1982 hasta 13 diciembre 2016), el ISRCTN registry (www.isrctn.com/editAdvancedSearch); búsqueda 13 diciembre 2016, ClinicalTrials.gov (www.clinicaltrials.gov); búsqueda 13 diciembre 2016 y en la World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/search/en); búsqueda 13 diciembre 2016. No se aplicó ninguna restricción de fecha ni de idioma en las búsquedas electrónicas de ensayos.
Criterios de selección
Se incluyeron los ensayos aleatorios que compararon al menos un tipo de intervención quirúrgica con otra intervención quirúrgica o no quirúrgica u observación.
Obtención y análisis de los datos
Dos autores de la revisión completaron de forma independiente el examen de la elegibilidad, el resumen de los datos, la evaluación del "Riesgo de sesgo" y la calificación de la evidencia.
Resultados principales
Se identificaron dos ensayos aleatorios que compararon cuatro tratamientos quirúrgicos diferentes para esta afección, dos métodos en cada ensayo. Los estudios incluyeron un total de 45 niños y adultos. Todos los tratamientos quirúrgicos fueron procedimientos para debilitar el músculo oblicuo inferior ipsilateral. Un estudio comparó la miectomía del músculo oblicuo inferior con la recesión de 10 mm; el otro estudio comparó la desinserción del músculo oblicuo inferior con la transposición anterior (2 mm anterior al borde temporal de la inserción del recto inferior).
Se consideró que ambos estudios tuvieron riesgo incierto de sesgo debido al informe incompleto de los métodos y a otras deficiencias metodológicas.
Ningún estudio informó datos sobre el resultado primario de esta revisión, que fue la proporción de participantes con éxito quirúrgico posoperatorio, definido como hipertropía menor de 3 dioptrías del prisma (DP) en la mirada fija primaria. Sin embargo, ambos estudios informaron una reducción promedio de la hipertropía en la mirada fija primaria. Un estudio encontró que a los 12 meses después de la cirugía la disminución promedio en la hipertropía fue mayor en los participantes sometidos a miectomía del músculo oblicuo inferior en comparación con los pacientes sometidos a recesión; sin embargo, no hubo datos disponibles para la comparación estadística. El otro ensayo encontró que después de al menos seis meses de seguimiento, la disminución media en la hipertropía primaria de la posición fue menor en los participantes sometidos a desinserción del músculo oblicuo inferior que en los sometidos a transposición anterior (diferencia de medias [DM] ‐5,20 DP; intervalo de confianza [IC] del 95% ‐7,76 a ‐2,64; evidencia de calidad moderada).
Ambos ensayos también informaron la reducción posoperatoria promedio de la desviación vertical en la aducción. Un estudio informó que la reducción promedio de la hipertropía en aducción fue mayor en los participantes sometidos a miectomía del músculo oblicuo inferior en comparación con los sometidos a recesión, pero no hubo datos disponibles para la comparación estadística. El otro estudio encontró menos disminución en la hipertropía en la mirada fija contralateral de los participantes sometidos a desinserción del músculo oblicuo inferior en comparación con los sometidos a transposición anterior (DM ‐7,10 DP; IC del 95%: ‐13,85 a ‐0,35; evidencia de calidad moderada).
Los resultados secundarios con datos suficientes para el análisis incluyeron la proporción de participantes con inclinación preoperatoria de la cabeza que se resolvió después de la cirugía y la proporción de participantes sometidos a una segunda cirugía. Estos resultados se evaluaron en el ensayo que comparó transposición anterior con desinserción del músculo oblicuo inferior; ambos resultados favorecieron la transposición anterior (cociente de riesgos 7,00; IC del 95%: 0,40 a 121,39 para ambos resultados; evidencia de muy baja calidad). Ninguno de los participantes sometidos a transposición anterior o desinserción del músculo oblicuo inferior desarrollaron hipotropía o inversión de la desviación vertical posoperatorias. Todos los participantes sometidos a transposición anterior del músculo oblicuo inferior desarrollaron deficiencia de la elevación, que los autores consideraron clínicamente no significativa en todos los casos, mientras que ningún participante sometido a desinserción del músculo oblicuo inferior presentó esta complicación. Además, el ensayo que comparó miectomía del músculo oblicuo inferior con recesión informó que ningún participante de ninguno de los grupos necesitó otra cirugía por estrabismo durante el período posoperatorio.
Conclusiones de los autores
Los dos ensayos incluidos en esta revisión evaluaron cuatro procedimientos de debilitamiento del músculo oblicuo inferior para el tratamiento quirúrgico de la parálisis del músculo oblicuo superior. No se encontraron ensayos que compararan otros tipos de procedimientos quirúrgicos para este trastorno. Ambos estudios reclutaron un escaso número de participantes y proporcionaron evidencia de baja calidad debido a las limitaciones en la completitud y la aplicabilidad. Por lo tanto, no se encontró evidencia de alta calidad que apoyara las recomendaciones para el tratamiento quirúrgico óptimo de la parálisis del músculo oblicuo superior. Se necesitan ensayos aleatorios rigurosamente diseñados, realizados e informados para identificar el tratamiento quirúrgico óptimo para el estrabismo vertical en este trastorno.
PICOs
Resumen en términos sencillos
Tratamientos quirúrgicos para la desalineación vertical de los ojos (estrabismo) en la parálisis del músculo oblicuo superior
Objetivo de la revisión
El objetivo de esta revisión Cochrane fue determinar si, en los pacientes con parálisis del músculo oblicuo superior, la cirugía para el estrabismo vertical tiene mejores resultados que otras intervenciones quirúrgicas o no quirúrgicas. Se buscaron todos los estudios relevantes y se identificaron dos ensayos clínicos.
Mensajes clave
No existe evidencia de alta calidad con respecto a los efectos de la cirugía sobre el estrabismo vertical en los pacientes con parálisis del oblicuo superior. En consecuencia, no es posible determinar la mejor intervención quirúrgica para este trastorno. Se necesitan estudios cuidadosamente diseñados para poder establecer recomendaciones de tratamiento de este problema frecuente.
¿Qué se estudió en esta revisión?
Se compararon diferentes tipos de cirugías para reducir el estrabismo vertical en niños y adultos con un diagnóstico de parálisis del músculo oblicuo superior. La parálisis del músculo oblicuo superior ocurre cuando hay debilidad de uno de los músculos (oblicuo superior) involucrados en el movimiento de los ojos, lo que provoca un modelo característico de estrabismo o desalineación de los ojos, que habitualmente varía con la colocación de la cabeza. La parálisis del músculo oblicuo superior es una causa frecuente de estrabismo vertical y puede dar lugar a diplopía o colocación anormal de la cabeza para mantener una visión única.
Resultados principales
Los dos ensayos incluidos compararon dos procedimientos quirúrgicos diferentes para debilitar el músculo oblicuo inferior y, por lo tanto, equilibrar la debilidad del músculo oblicuo superior. Se estudiaron cuatro cirugías diferentes que debilitan el músculo oblicuo inferior: la miectomía (eliminar parte del músculo), la recesión (mover el músculo a una posición donde ejerce menos fuerza), la transposición anterior (mover el músculo a una posición donde se altera la dirección de la fuerza) y la desinserción (separar el músculo de la esclerótica).
Ninguno de los ensayos examinó el resultado principal que se deseaba estudiar en esta revisión (la proporción de participantes que se consideró que logró una realineación exitosa de los ojos después de la cirugía). Además, se consideró que la calidad de los datos en ambos estudios es baja.
¿Cuál es el grado de actualización de esta revisión?
Se buscaron los ensayos con datos de resultados publicados hasta el 13 de diciembre de 2016. Los ensayos incluidos se publicaron entre 2001 y 2003.
Authors' conclusions
Summary of findings
| Inferior oblique myectomy compared with inferior oblique recession for vertical strabismus in superior oblique palsy | ||||
| Patient or population: people with symptom‐producing and/or socially noticeable unilateral overacting inferior oblique muscle; all participants had longstanding unilateral superior oblique underaction Settings: eye hospital Intervention: inferior oblique myectomy Comparison: inferior oblique recession | ||||
| Outcomes | Relative effect | No. of participants | Quality of the evidence | Comments |
| Proportion of participants with postoperative surgical success (hypertropia less than 3 PD in primary gaze) | N/A | 23 (1 study) | N/A | This outcome measure was not reported in the study included in this comparison. However, median hypertropia in primary gaze at 12 months was 3 PD in the myectomy group and 1 PD in the recession group. The average reduction in hypertropia in primary position was 14 PD in the myectomy group and 8 PD in the recession group (P = 0.042). |
| Proportion of participants with anomalous head position preoperatively with residual head tilt postoperatively | N/A | 23 (1 study) | N/A | This outcome measure was not reported in the study included in this comparison. |
| Proportion of participants with postoperative hypertropia less than 3 PD in down gaze | N/A | 23 (1 study) | N/A | This outcome measure was not reported in the study included in this comparison. |
| Proportion of participants with postoperative hypertropia less than 3 PD in contralateral gaze | N/A | 23 (1 study) | N/A | This outcome measure was not reported in the study included in this comparison. |
| Proportion of participants who received additional strabismus surgery | N/A | 23 (1 study) | N/A | None of the participants in either group required a second strabismus surgery during the follow‐up interval. |
| Proportion of participants with reversal of vertical deviation postoperatively | N/A | 23 (1 study) | N/A | This outcome measure was not reported in the study included in this comparison. |
| Proportion of participants with postoperative orbital cellulitis | N/A | 23 (1 study) | N/A | This outcome measure was not reported in the study included in this comparison. |
| GRADE Working Group grades of evidence CI: confidence interval; N/A: not applicable; PD: prism diopters | ||||
| Inferior oblique disinsertion compared with inferior oblique anterior transposition for vertical strabismus in superior oblique palsy | ||||
| Patient or population: people with unilateral superior oblique palsy Settings: eye hospital Intervention: inferior oblique disinsertion Comparison: inferior oblique anterior transposition | ||||
| Outcomes | Relative effect | No. of participants | Quality of the evidence | Comments |
| Proportion of participants with postoperative surgical success (hypertropia less than 3 PD in primary gaze) | N/A | 22 (1 study) | Moderate | This outcome measure was not reported in the study included in this comparison. However, the mean reduction of hypertropia in primary position was 13.3 (SD 1.9) PD in the disinsertion group and 18.5 (SD 3.9) PD in the anterior transposition group (mean difference ‐5.20 PD, 95% CI ‐7.76 to ‐2.64). This difference favors inferior oblique anterior transposition. |
| Proportion of participants with anomalous head position preoperatively with residual head tilt postoperatively | RR 7.00 (0.40 to 121.39) | 22 (1 study) | Very low | This outcome favors inferior oblique anterior transposition. |
| Proportion of participants with postoperative hypertropia less than 3 PD in down gaze | N/A | 22 (1 study) | N/A | This outcome measure was not reported in the study included in this comparison. |
| Proportion of participants with postoperative hypertropia less than 3 PD in contralateral gaze | N/A | 22 (1 study) | Moderate | The mean reduction of hypertropia in adduction was 20.6 (SD 6.2) PD in the disinsertion group and 27.7 (SD 9.6) PD in the anterior transposition group (mean difference ‐7.10 PD, 95% CI ‐13.85 to ‐0.35). Anterior transposition resulted in a greater decrease in hypertropia in contralateral gaze, but it was unclear whether this difference favored the anterior transposition group, since the authors did not report the number of participants overcorrected in contralateral gaze. |
| Proportion of participants who received additional strabismus surgery | RR 7.00 (0.40 to 121.39) | 22 (1 study) | Very low | This outcome favors inferior oblique anterior transposition. |
| Proportion of participants with reversal of vertical deviation postoperatively | N/A | 22 (1 study) | N/A | None of the participants in either group developed postoperative reversal of vertical deviation. |
| Proportion of participants with postoperative orbital cellulitis | N/A | 22 (1 study) | N/A | This outcome measure was not reported in the study included in this comparison. |
| GRADE Working Group grades of evidence CI: confidence interval; N/A: not applicable; PD: prism diopters; RR: risk ratio; SD: standard deviation | ||||
Background
Description of the condition
Superior oblique palsy is considered to be the most common cyclovertical muscle palsy (Plager 1999). A recent epidemiological study found the annual incidence of adult‐onset superior oblique palsy to be 6.3 cases per 100,000 people, but significantly higher in men than women (Martinez‐Thompson 2014). In children younger than 19 years of age, the annual incidence was 3.4 cases per 100,000 (Tollefson 2006), with 31% of vertical strabismus in children attributed to superior oblique palsy, of equal incidence by gender.
Superior oblique palsy may be congenital or acquired. Possible causes of congenital superior oblique palsy include hypoplasia of the trochlear nucleus or nerve and anatomical defects or absence of the superior oblique tendon or trochlea (Chan 1999; Helveston 1992; Mansour 1986). Acquired cases have been presumed to be most frequently secondary to trauma, although the association is in many cases tenuous. Other causes of acquired superior oblique palsy include inflammation, infection, vascular malformation, infarct, tumor, myasthenia gravis, or iatrogenic denervation of muscle complicating sinus, orbital, or neurologic surgery (Plager 1999; Tamhankar 2013).
Clinical characteristics
The main clinical feature of superior oblique palsy is vertical binocular misalignment (strabismus), which occurs when the vertical angular orientation of one eye differs from that of the other eye. In superior oblique palsy, there is hypertropia (upward deviation) of the eye on the same side as the affected muscle, which may present with diplopia (double vision) or be compensated by an abnormal head position. The head is usually tilted in the direction of the shoulder opposite to the elevated eye, and the chin may be lowered or, less commonly, raised to minimize the vertical strabismus. There may also be excyclotorsion of the hypertropic eye, that is rotation of the eye about the line of sight so that the normally vertical meridian of the eye is tilted away from the midline of the face.
Diagnosis
Superior oblique palsy is typically considered to produce an incomitant strabismus in which the vertical misalignment varies in magnitude with different gaze positions relative to the head. However, there may be individual exceptions. The historical gold standard for diagnosis has been considered to be the Parks‐Bielschowsky three‐step test. The elements of the three‐step test for acute, unilateral (one eye) superior oblique palsy consist of: 1) hypertropia of the eye ipsilateral to the palsied superior oblique muscle; 2) increased magnitude of hypertropia in lateral gaze contralateral to the affected eye; and 3) increased magnitude of hypertropia when the head is tilted towards the shoulder corresponding to the affected eye (Bielschowsky 1935). Investigators of more recent magnetic resonance imaging (MRI) studies of superior oblique structure and function have challenged the three‐step test, demonstrating it to be only about 70% sensitive, Manchandia 2014, and 50% specific, Demer 2011, for deficient superior oblique function. Consequently, earlier studies that reported the clinical characteristics of superior oblique palsy as diagnosed by the three‐step test probably included a substantial fraction of misdiagnosed alternative causes of vertical strabismus, and also systematically omitted many cases of actual superior oblique weakness.
Historically, it has been hypothesized that when longstanding, as in congenital superior oblique palsy presenting in adulthood, the vertical strabismus may be more comitant, or similar in magnitude in all gaze directions. In general, children more often present with an anomalous head position rather than diplopia, because the developing brain suppresses central perception from one eye when the eyes are not aligned. Older children with acquired superior oblique palsy who see double may be unable to verbalize this symptom. Adults may present with an anomalous head position or diplopia from vertical misalignment or excyclotorsion.
Bilateral superior oblique palsy
Superior oblique palsy may be bilateral, involving both eyes. In this case, patients may have hypertropia that alternates with gaze position and head tilt, as well as crossing of the eyes (esotropia) increasing in down gaze with a V pattern. On right gaze, the left eye is hypertropic, while the right eye is hypertropic in left gaze. In addition, with the head tilted to the right, the right eye is hypertropic, while the left eye is hypertropic on left head tilt. The degree of excyclotorsion is typically larger in bilateral than in unilateral superior oblique palsy (Kushner 1988).
Congenital superior oblique palsy
Congenital superior oblique palsy may manifest in childhood or adulthood. Presentation may be precipitated by inability to sustain the effort required to compensate for the vertical misalignment. Clinical signs associated with a congenital superior oblique palsy include longstanding torticollis and facial asymmetry (Plager 1999), although the relationship between facial asymmetry and superior oblique palsy has been questioned (Velez 2000). People with congenital superior oblique palsy also may have a larger‐than‐normal vertical fusion amplitude. The vertical fusion amplitude refers to the greatest amount of vertical ocular misalignment that the brain can tolerate without the person experiencing diplopia. The normal vertical fusion amplitude for long‐distance viewing is less than or equal to 3 prism diopters (PD) (Bharadwaj 2007; Parks 2005); people with a vertical fusion amplitude greater than this are suspected of having congenital superior oblique palsy.
Acquired superior oblique palsy
Superior oblique palsy may also be acquired in either childhood or adulthood. The trochlear nerve, which innervates the superior oblique muscle, may be compromised anywhere along its long course from the dorsal midbrain to the orbit, traversing intracranial structures including the tentorium cerebelli and cavernous sinus (Plager 1999). The superior oblique tendon itself may also suffer injury, particularly during sinus or orbital surgery. People with acquired superior oblique palsy may present with an anomalous head position or vertical or torsional diplopia. Such patients typically have normal vertical fusional amplitudes and do not have facial asymmetry. Because the normal vertical fusion amplitude is less than or equal to 3 PD, patients may be significantly disabled by small degrees of hypertropia caused by acquired superior oblique palsy.
Challenges to diagnosing superior oblique palsy
Although the Parks‐Bielschowsky three‐step test has been considered the gold standard for diagnosing superior oblique palsy, 30% of people with superior oblique palsy confirmed by MRI may not fulfill all three of these criteria (Manchandia 2014). Recent studies utilizing MRI have shown that many cases diagnosed clinically as superior oblique palsy may be related to connective tissue abnormalities rather than dysfunction of cranial nerves (Demer 2011). Specifically, heterotopic extraocular muscle pulleys can cause patterns of incomitant strabismus that may be attributed to oblique muscle dysfunction (Clark 1998; Suh 2016). Because neurogenic atrophy occurs rapidly and reliably after denervation of extraocular muscles (Demer 2010), superior oblique atrophy observed on MRI may be used to confirm the clinical diagnosis of superior oblique palsy (Demer 1995). In cases of head tilt‐dependent hypertropia with absence of superior oblique atrophy, MRI demonstrates abnormal shifts of extraocular muscle pulleys during head tilt (Demer 2011). Magnetic resonance imaging studies have also shown that compartmental palsy of the superior oblique can occur, which may account for the heterogeneity of clinical presentation in this disorder (Shin 2015). Notwithstanding this objective evidence that clinical ocular motility patterns are not specifically interpretable for oblique extraocular muscle dysfunction, clinical terminology remains deeply grounded in the belief that underdepression of the eye in adduction is a pathognomonic reflection of “superior oblique muscle underaction,” while overelevation in adduction is a pathognomonic reflection of “inferior oblique muscle overaction.” The studies reviewed here were based upon the historical diagnostic concepts, and employed the historical terminology.
Description of the intervention
People with superior oblique palsy may seek treatment due to symptomatic vertical or torsional diplopia or the anomalous head posture adopted to minimize vertical ocular misalignment. Children with a constant head tilt can develop permanent contracture of the neck muscles, particularly the sternocleidomastoid muscle (Lau 2009). Various non‐surgical and surgical treatment options exist. When patients are asymptomatic or minimally symptomatic, observation without treatment may be considered. In cases where the vertical deviation is small and comitant, prisms may be sufficient to improve symptoms. However, the majority of people treated for symptomatic superior oblique palsy undergo surgery (Plager 1999), the main goal of which is to reduce the vertical ocular misalignment such that diplopia or anomalous head position, when present preoperatively, is improved or resolved.
Surgical options for hypertropia in superior oblique palsy include: ipsilateral superior oblique tendon plication ('tucking') (Bhola 2005; Durnian 2011); superior oblique tendon resection and advancement (Luton 1998; Wheeler 1934); procedures to weaken the ipsilateral inferior oblique, including recession (Hendler 2013; Parks 1972), myectomy (Bahl 2013; Lee 2015), myotomy (Lee 2015), marginal myotomy (Mellott 2002), disinsertion (Parks 1972; Yanyali 2001), anterior transposition (Elliott 1981; Farvardin 2002), anterior nasal transposition (Hussein 2007; Stager 2003), and orbital fixation (Ela‐Dalman 2007); ipsilateral superior rectus recession (Ahn 2012); and contralateral inferior rectus recession (Mahmoud 2009).
In patients symptomatic from excyclotorsion, surgical options include Harada‐Ito advancement of the anterior portion of the superior oblique tendon (Harada 1964; Nishimura 2002), inferior oblique weakening as listed above, and transposition of vertical rectus muscles (Nemoto 2000). We have not included surgical options to address excyclotorsion in this review; we have focused on surgical procedures to address symptomatic hypertropia.
How the intervention might work
Strabismus surgery works by changing the forces or pulling directions of the extraocular muscles, or both, as influenced by their associated orbital connective tissues (pulleys). A variety of surgical approaches are used to treat superior oblique palsy. Advancement, resection, or plication of the superior oblique tendon shorten a lax tendon, which may improve action of the superior oblique muscle. Weakening the superior oblique's opponent, the ipsilateral inferior oblique muscle, decreases the activity of the antagonist. Recession of the ipsilateral superior rectus muscle reduces the upward force elevating the hypertropic eye. Recession of the contralateral inferior rectus reduces the force rotating the contralateral eye downward, shifting it upward to match the position of the eye hypertropic due to the palsied superior oblique muscle.
Why it is important to do this review
Although many people with symptomatic superior oblique palsy undergo surgical treatment, there is no consensus as to which, if any, surgical procedure is most effective for remediating strabismus due to this condition, or whether different surgical approaches may be optimal for differing clinical presentations of superior oblique palsy. Moreover, although certain surgical procedures are subject to particular complications (e.g. iatrogenic Brown syndrome in superior oblique tuck, or anti‐elevation syndrome in inferior oblique anterior transposition), there are few data comparing the rates of complications between the various surgical procedures used to treat superior oblique palsy. A comprehensive review was needed to guide practitioners in choosing effective surgical interventions.
Objectives
To assess the relative effects of surgical treatments compared with another surgical intervention, non‐surgical intervention, or observation for vertical strabismus in people with superior oblique palsy.
Methods
Criteria for considering studies for this review
Types of studies
We included only randomized controlled trials. We did not exclude studies on the basis of publication status or language of publication.
Types of participants
We included studies of adults and children with acquired or congenital vertical strabismus considered compatible with the diagnosis of unilateral superior oblique palsy. We did not limit inclusion based on the angle of deviation, as patients may be symptomatic at different degrees of hypertropia based on their vertical fusional amplitudes. We excluded studies of people who underwent surgical intervention for any strabismus before entering the trial. We also excluded studies of people undergoing surgical interventions primarily for torsion, as this review was focused on vertical strabismus. We also excluded studies of people who underwent simultaneous concomitant horizontal rectus muscle surgery.
Types of interventions
We included trials that compared any type of surgical procedure to another type of surgical procedure. The types of surgical procedures for comparison included the following.
-
Superior oblique plication ('tuck')
-
Superior oblique resection
-
Superior oblique advancement
-
Inferior oblique recession
-
Inferior oblique myectomy
-
Inferior oblique myotomy
-
Inferior oblique marginal myotomy
-
Inferior oblique disinsertion
-
Inferior oblique anterior transposition temporal to the inferior rectus insertion
-
Inferior oblique anterior transposition nasal to the inferior rectus insertion
-
Inferior oblique orbital fixation
-
Inferior oblique denervation and extirpation
-
Superior rectus recession
-
Inferior rectus recession
-
Posterior fixation suture
-
Combinations of any of the above
We included studies that utilized unilateral or bilateral surgical procedures.
Additionally, we included studies that compared any surgical procedure to observation or non‐surgical treatment.
Types of outcome measures
Primary outcomes
The primary outcome measure was the proportion of participants with postoperative surgical success, defined as hypertropia at distance and near in primary position (with the head upright and looking straight ahead) of less than 3 PD, as measured by alternate cover testing with prism, without reversal of the direction of hypertropia, at one‐year postoperatively. When no one‐year outcome data were available, we considered the proportion of surgical success at the longest postoperative follow‐up time (minimum six weeks).
Secondary outcomes
We evaluated all secondary outcomes at one‐year postoperatively, or at longest postoperative follow‐up when no outcome data were available at one year.
The secondary outcome measures were as follows.
-
Proportion of participants with an anomalous head position preoperatively who had a residual head tilt greater than 15 degrees in central gaze postoperatively
-
Proportion of participants with postoperative hypertropia less than 3 PD, as measured by alternate cover testing with prism, in down gaze
-
Proportion of participants with postoperative hypertropia less than 3 PD, as measured by alternate cover testing with prism, in contralateral gaze (adduction of affected eye)
-
Proportion of participants with symptomatic cyclotorsion postoperatively
-
Proportion of participants who received another strabismus surgery
-
Proportion of participants who reported relief of symptoms (e.g., diplopia), assessed by questionnaire or other instrument
-
Scores from vision‐specific quality of life instruments, such as the National Eye Institute Visual Function Questionnaire‐25 (NEI VFQ‐25) for adults, Adult Strabismus‐20 Questionnaire (AS‐20) for adults, and vision‐specific pediatric quality of life instruments for children
Adverse effects
Adverse effects documented and compared were as follows.
-
Orbital cellulitis
-
Endophthalmitis
-
Retinal perforation
-
Iatrogenic Brown syndrome
-
Anti‐elevation syndrome
-
Reversal of vertical deviation.
Search methods for identification of studies
Electronic searches
The Cochrane Eyes and Vision Information Specialist conducted systematic searches in the following databases for randomized controlled trials and controlled clinical trials. There were no language or publication year restrictions. The date of the search was 13 December 2016.
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2016, Issue 12) (which contains the Cochrane Eyes and Vision Trials Register) in the Cochrane Library (searched 13 December 2016) (Appendix 1)
-
MEDLINE Ovid (1946 to 13 December 2016) (Appendix 2)
-
Embase Ovid (1947 to 13 December 2016) (Appendix 3)
-
LILACS (Latin American and Caribbean Health Sciences Literature Database) (1982 to 13 December 2016) (Appendix 4)
-
ISRCTN registry (www.isrctn.com/editAdvancedSearch; searched 13 December 2016) (Appendix 5)
-
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov; searched 13 December 2016) (Appendix 6)
-
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp; searched 13 December 2016) (Appendix 7)
Searching other resources
We did not conduct manual searches of conference proceedings or abstracts specifically for this review because proceedings and abstracts from major eye conferences are searched annually by Cochrane Eyes and Vision and trials identified are added to CENTRAL.
Data collection and analysis
Selection of studies
Two review authors independently assessed the titles and abstracts of all reports identified by the electronic search. We classified the studies corresponding to the abstracts as (a) definitely relevant, (b) possibly relevant, or (c) definitely not relevant. For studies classified as (a) or (b) based on review of abstracts, we obtained and assessed the full‐text reports. Using the full‐text reports, we classified each study as (1) include, (2) awaiting assessment, or (3) exclude. Any disagreements at either stage of screening were resolved by a third review author. We assessed studies identified as 'included' for risk of bias. We documented studies excluded after review of the full‐text report with reasons for exclusion. The review authors were unmasked to the report authors, institutions, and trial results during the selection of studies.
Data extraction and management
Two review authors independently extracted data for study methods and characteristics, such as details of participants, interventions, outcomes, and other relevant information for all included studies, and quantitative outcome results onto data collection forms developed by Cochrane Eyes and Vision. We did not pilot test the forms as specified in the protocol for this review as we included only two trials, which was the number of trials recommended for pilot testing the form (Chang 2016). Any discrepancies were resolved by discussion. Wherever possible, and for included trials for which we were unable to obtain data from the investigators, we extracted data from figures in the published papers. One review author entered data into Review Manager 5 (Review Manager 2014), and a second review author verified the data entry.
Assessment of risk of bias in included studies
Two review authors independently assessed each included trial for risk of bias according to methods set out in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We considered the following domains: selection bias (sequence generation, allocation concealment before randomization), performance bias (masking (blinding) of participants and personnel), detection bias (masking of outcome assessors), attrition bias (incompletely reported outcome data), reporting bias (selective outcome reporting), and any other sources of bias. We judged each study for each domain as being at high, low, or unclear risk of bias. A third review author resolved any disagreements in the bias assessments. We recorded our assessments in the Cochrane 'Risk of bias' table.
Measures of treatment effect
For primary and secondary dichotomous outcomes, we calculated risk ratios with 95% confidence intervals. Dichotomous outcomes included the proportion of participants with postoperative surgical success, residual head tilt greater than 15 degrees in central gaze, hypertropia less than 3 PD in down gaze and contralateral gaze, and symptomatic cyclotorsion; the proportion of participants who received another strabismus surgery; and the proportion of participants with adverse effects.
We calculated mean differences with 95% confidence intervals for continuous outcomes including quality of life scores and measures of postoperative change in vertical deviation, which were reported by the included studies but not prespecified as outcomes for this review.
Unit of analysis issues
The unit of analysis was the individual participant; all participants had unilateral superior oblique palsy.
Dealing with missing data
Since the studies included in this review were published 14 or more years ago, we used the data available. We did not impute data for the purposes of this review.
Assessment of heterogeneity
We assessed clinical and methodological heterogeneity by comparing participant characteristics, inclusion/exclusion criteria, and assessments of primary and secondary outcomes. As each included study evaluated different surgeries and outcomes, meta‐analysis was not feasible. Had we performed any meta‐analysis, we planned to test for statistical heterogeneity using the Chi2 test and evaluate the I2 value, with an I2 value greater than 50% indicating the presence of substantial statistical heterogeneity. We also planned to examine the overlap of effect estimates and confidence intervals among studies, with poor overlap suggestive of heterogeneity.
Assessment of reporting biases
We did not examine funnel plots for asymmetry to identify potential publication (reporting) bias because no meta‐analysis was performed. We assessed selective outcome reporting as part of the 'Risk of bias' assessment for individual trials.
Data synthesis
Data analysis followed the guidelines in Chapter 9 of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011). We planned to use a fixed‐effect model when there were fewer than three trials in a meta‐analysis, and a random‐effects model when there were three or more trials in an analysis. Due to clinical and methodological heterogeneity, we did not perform meta‐analysis, and have presented a narrative summary.
Subgroup analysis and investigation of heterogeneity
Data were insufficient to conduct our planned subgroup analyses. We had planned to analyze outcomes within subgroups based on participant age (adults 18 years of age and older versus children); etiology of superior oblique palsy (congenital versus acquired); and clinical presentation (primarily symptomatic due to head tilt versus diplopia in various gaze positions).
Sensitivity analysis
Data were insufficient to conduct our planned sensitivity analyses to examine the impact on effect estimates of exclusion of studies at high risk of bias, industry‐funded studies, and unpublished studies.
Summary of findings
We prepared a 'Summary of findings' table that includes relevant outcomes in the included studies. We based the seven outcomes selected for presentation in the table on clinical and patient importance. We reported the following outcomes in the 'Summary of findings' table.
-
Proportion of participants with postoperative surgical success, as defined above
-
Proportion of participants with an anomalous head position preoperatively who had a residual head tilt greater than 15 degrees in central gaze postoperatively
-
Proportion of participants with postoperative hypertropia less than 3 PD, as measured by alternate cover testing with prism, in down gaze
-
Proportion of participants with postoperative hypertropia less than 3 PD, as measured by alternate cover testing with prism, in contralateral gaze (adduction of affected eye)
-
Proportion of participants who received additional strabismus surgery
-
Proportion of participants with reversal of the vertical deviation at distance or near postoperatively
-
Proportion of participants with the postoperative complication of orbital cellulitis.
We used the GRADE approach to grade the overall certainty of evidence for each outcome (GRADEpro 2014). We assessed the certainty of evidence for each outcome as high, moderate, low, or very low according to the following criteria as described in Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2011).
-
High risk of bias among included studies
-
Indirectness of evidence
-
Unexplained heterogeneity or inconsistency of results
-
Imprecision of results (i.e. wide confidence intervals)
-
High probability of publication bias
Results
Description of studies
Results of the search
The electronic searches yielded a total of 927 records (Figure 1). The Cochrane Information Specialist scanned the search results and removed 214 duplicate records. We screened the remaining 713 reports and obtained five full‐text reports for further assessment. We identified two studies that met the inclusion criteria for this review (Shipman 2003; Yanyali 2001), and excluded the remaining three studies (Bahl 2013; Muchnick 1998; Ziffer 1993). Our searches of clinical trials registries did not yield any ongoing studies.
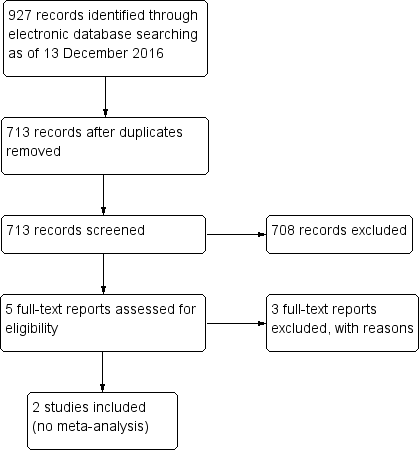
Study flow diagram.
Included studies
We have described the characteristics of each of the two included studies in detail in the Characteristics of included studies tables. Neither study had been registered in a clinical trial registry, likely because registration was uncommon at the time of publication of the trial reports.
Types of participants
The two included studies involved a total of 45 children and adults of both genders. One study was conducted in the UK, and the other in Turkey. Both studies included people diagnosed with unilateral superior oblique palsy with ipsilateral overelevation in adduction ("inferior oblique overaction"). The surgical procedures were all performed on the inferior oblique muscle, and included 12 myectomies, 11 recessions, 11 disinsertions, and 11 anterior transpositions.
Shipman 2003 recruited 24 adults and children with symptom‐producing and/or socially noticeable unilateral overelevation in adduction. The inclusion criteria did not specify superior oblique palsy, but all participants had decompensated longstanding unilateral underdepression in adduction. Exclusion criteria were prior or simultaneous extraocular muscle surgery, inability to co‐operate with testing, and visual acuity of 20/60 or worse in either eye. An additional post hoc exclusion criterion was failure to attend any postoperative visit. Participants were randomized to undergo inferior oblique myectomy or recession. Twelve participants were randomized to each group, but one participant who underwent recession failed to complete one‐year follow‐up, so a total of 23 participants were analyzed. The average age was 30.8 years (range 12 to 77 years) in the myectomy group and 28.5 years (range 13.7 to 69 years) in the recession group. The study authors reported that preoperative hypertropia in the primary position was 15 PD and 10 PD in the myectomy and recession groups, respectively; preoperative hypertropia in contralateral gaze, "inferior oblique overaction," and "superior oblique underaction" were balanced between the groups.
Yanyali 2001 enrolled 22 adults and children with unilateral superior oblique palsy diagnosed based on ipsilateral hypertropia in the primary position that was greater on contralateral gaze and ipsilateral head tilt, in addition to ipsilateral underdepression in adduction ("superior oblique underaction") and overelevation in adduction ("inferior oblique overaction"). Candidates who had prior extraocular muscle surgery or hypertropia less than 8 PD in primary position were excluded. Participants were randomized to undergo inferior oblique disinsertion or anterior transposition. Eleven participants were assigned to each group, and all completed at least six months of follow‐up, thus all 22 participants were included in the analysis. The groups were similar in preoperative characteristics including age, gender, and percentage of participants with head tilt and diplopia, and vertical deviation in primary and contralateral gaze positions.
Types of interventions
The two included studies each compared two different surgeries for overelevation in adduction ("inferior oblique overaction") and hypertropia in people who had unilateral underdepression in adduction ("superior oblique underaction"). All surgeries were procedures to weaken the ipsilateral inferior oblique muscle. Shipman 2003 compared inferior oblique myectomy at the temporal border of the inferior rectus muscle to 10‐millimeter inferior oblique recession, with the muscle sutured 3 mm posterior and 2.5 mm lateral to the temporal pole of the inferior rectus muscle insertion. Total follow‐up time was 12 months. Yanyali 2001 compared inferior oblique disinsertion to inferior oblique anterior transposition, with the muscle sutured 2 mm anterior to the temporal border of the inferior rectus muscle insertion. The entire muscle, anterior and posterior, was "bunched up" and anteriorized at this location. Participants were expected to complete at least six months of follow‐up, and outcomes were assessed at the last follow‐up visit rather than at a specific follow‐up time point.
Types of outcomes
The studies reported different outcome measures. Shipman 2003 reported the average postoperative reduction in vertical deviation in ipsilateral, primary, and contralateral gaze positions, in addition to median postoperative vertical deviations in these positions. The study authors also reported the change in vertical deviation in these gaze positions between 2 weeks and 12 months postoperatively. Additionally, the median postoperative improvement in overelevation in adduction ("inferior oblique overaction") and undepression in adduction ("superior oblique underaction") were reported. All outcomes were assessed at 2 weeks, 4 months, and 12 months postoperatively. Subgroup analyses were performed on participants with large preoperative vertical deviations, that is those with primary gaze hypertropia of 15 PD or more and those with ipsilateral gaze hypertropia of 10 PD or more. The study did not report adverse events.
Yanyali 2001 reported the reduction of vertical deviation in primary and contralateral gaze positions after surgery. Secondary outcomes included the proportion of participants who had postoperative resolution of preoperative diplopia, the proportion of participants with postoperative resolution of head tilt, and the proportion of participants requiring a second surgery. Adverse outcomes assessed included postoperative development of clinically significant or insignificant elevation deficiency, and postoperative hypotropia in primary position (reversal of vertical deviation). Outcomes were assessed at the last follow‐up visit; the mean follow‐up time was 18.8 months (range 6 to 40 months).
Neither study reported data for the following outcome measures that were specified in our review: the primary outcome of proportion of participants with surgical success (defined as hypertropia of less than 3 PD in primary position), and secondary outcomes including proportion of participants with postoperative hypertropia less than 3 PD in down gaze and contralateral gaze, proportion of participants with symptomatic cyclotorsion postoperatively, proportion of participants who reported relief of symptoms, quality of life scores, and proportion of participants with adverse events of orbital cellulitis, endophthalmitis, retinal perforation, or iatrogenic Brown syndrome.
Funding sources
Neither group of investigators reported funding sources for their trials (Shipman 2003; Yanyali 2001).
Excluded studies
We excluded three studies for reasons shown in the Characteristics of excluded studies table. We excluded two studies because they were retrospective reviews of cases rather than randomized controlled trials (Bahl 2013; Ziffer 1993). We excluded the third study, Muchnick 1998, because the authors did not state whether the design was retrospective or prospective and did not specify the method of assigning participants to the two different surgeries being evaluated.
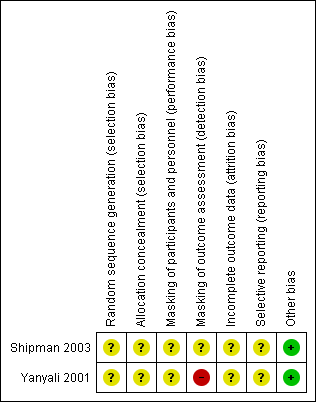
Risk of bias in included studies
See Figure 2.
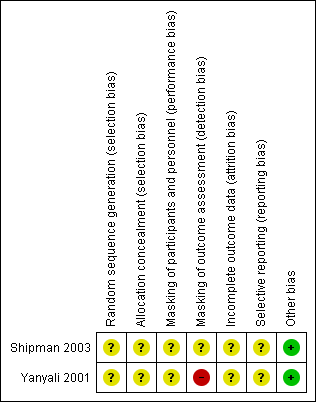
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Neither study reported methods of randomization or allocation concealment, therefore we judged the risk of selection bias to be unclear.
Masking (performance bias and detection bias)
Surgeons could not be masked to random assignments in these trials. Neither study reported whether participants were masked to treatment group, so we judged both studies to have an unclear risk of performance bias.
Shipman 2003 reported that outcomes were assessed by an orthoptist, but did not specify whether this orthoptist was masked. We therefore judged this study to have an unclear risk of detection bias.
Yanyali 2001 reported that the same surgeons performed the surgery and assessed preoperative and postoperative measures. This lack of masking led to a judgement of high risk of detection bias for this study.
Incomplete outcome data
We judged both studies to have an unclear risk of attrition bias. Shipman 2003 reported that one participant randomized to the recession group failed to complete one year of follow‐up and was excluded from analysis. However, the characteristics of this participant were not described, other than reporting that the participant was “asymptomatic in the early postoperative period.” Yanyali 2001 reported no participants lost to follow‐up, but outcomes were not assessed at standardized postoperative times, which would have been necessary for complete and accurate comparison. The last follow‐up visit was used, which ranged from 6 to 40 months postoperatively.
Selective reporting
Neither study reported that outcomes had been specified prior to study initiation, therefore we judged both studies to have an unclear risk of reporting bias.
Other potential sources of bias
We identified no other potential sources of bias for either study.
Effects of interventions
See: Summary of findings for the main comparison Inferior oblique myectomy versus recession for vertical strabismus in superior oblique palsy; Summary of findings 2 Inferior oblique disinsertion versus anterior transposition for vertical strabismus in superior oblique palsy
Four different surgical techniques were compared, two in each of the two included studies. The Shipman 2003 study compared inferior oblique myectomy (at the temporal border of the inferior rectus) to recession (of 10 mm); the Yanyali 2001 study compared inferior oblique disinsertion to anterior transposition (2 mm anterior to the temporal border of the inferior rectus insertion). Shipman 2003 reported outcomes at 2 weeks, 4 months, and 12 months, data for the last of which we used for our analysis. Yanyali 2001 reported data at last follow‐up (6 to 40 months postoperatively). The follow‐up time was not reported separately for the two surgical groups, and the authors did not specify whether follow‐up time differed significantly between the groups.
Inferior oblique myectomy versus recession
See summary of findings Table for the main comparison for comparison between inferior oblique myectomy and recession. These two surgeries were compared in the Shipman 2003 study. At 12‐month follow‐up, data were available for 12 participants in the myectomy group and 11 participants in the recession group.
Surgical success
The Shipman 2003 study did not report the proportion of participants with surgical success, as defined in this review by hypertropia less than 3 PD in primary gaze. However, data extracted from the published graphs indicated that the median hypertropia in primary gaze at 12 months was 3 PD in the myectomy group and 1 PD in the recession group. The authors also reported that the average reduction in hypertropia in primary position was 14 PD in the myectomy group and 8 PD in the recession group (P = 0.042). No additional data were available for analysis.
In a subgroup analysis of six participants with preoperative primary position hypertropia of 15 PD or more, the median postoperative vertical deviation in primary gaze at 12 months was 1 PD hypertropia (range orthotropia to 6 PD hypertropia). The study authors did not specify whether these participants had undergone inferior oblique myectomy or recession.
Head tilt
The Shipman 2003 study did not report preoperative or postoperative data on head positioning.
Hypertropia in down gaze
The Shipman 2003 study did not report preoperative or postoperative data on vertical deviation in down gaze.
Hypertropia in contralateral gaze
Although the Shipman 2003 study did not specify the proportion of participants with hypertropia less than 3 PD in contralateral gaze, the study authors did report that the median vertical deviation in adduction at 12 months' postoperatively was 1.75 PD hypertropia (range 5 PD hypotropia to 16 PD hypertropia) in the myectomy group and 3 PD hypertropia (range orthotropia to 9 PD hypertropia) in the recession group. The average reduction of vertical deviation in contralateral gaze at 12 months' postoperatively was 18.5 PD in the myectomy group and 16 PD in the recession group (P = 0.05).
Cyclotorsion
The Shipman 2003 study did not report preoperative or postoperative data on cyclotorsion.
Second surgery
The Shipman 2003 study reported that no participant in either group required a second strabismus surgery during the follow‐up period.
Relief of symptoms
The Shipman 2003 study did not report the proportion of participants who reported relief of symptoms.
Quality of life
The Shipman 2003 study did not evaluate quality of life with any standard instrument or method.
Adverse effects
The Shipman 2003 study did not evaluate any of the adverse effects specified for this review. However, tables in the study report indicated that the vertical deviation in contralateral gaze at 12 months' postoperatively ranged from 5 PD hypotropia to 16 PD hypertropia in the myectomy group, and from orthotropia to 9 PD hypertropia in the recession group. These data suggest that there may have been some participants with hypotropia (reversal of vertical deviation) in primary gaze in the myectomy group. The total number of participants, if any, who developed reversal of the vertical deviation, anti‐elevation syndrome, orbital cellulitis, endophthalmitis, and retinal perforation was not reported. The final adverse effect to be evaluated by this review, iatrogenic Brown syndrome, was not discussed in the study report, but would not be expected to have been discussed because surgery was not performed on the superior oblique muscle.
Inferior oblique disinsertion versus anterior transposition
See summary of findings Table 2 for comparison between inferior oblique disinsertion and anterior transposition. These two surgical techniques were compared by the Yanyali 2001 investigators. Data were available for 11 participants in the disinsertion group and 11 participants in the anterior transposition group at final follow‐up visit (range 6 to 40 months).
Surgical success
The Yanyali 2001 study did not specify the proportion of participants with surgical success, as defined in this review by hypertropia less than 3 PD in primary gaze. However, the authors reported that the mean reduction of hypertropia in primary position was 13.3 (standard deviation (SD) 1.9) PD in the disinsertion group and 18.5 (SD 3.9) PD in the anterior transposition group (mean difference (MD) ‐5.20 PD, 95% confidence interval (CI) ‐7.76 to ‐2.64). This difference favors the anterior transposition group, since no participant in either group was overcorrected postoperatively. We rated the quality of the data for this outcome as moderate due to risk of bias in the study design.
Head tilt
The Yanyali 2001 study reported that all participants had head tilt preoperatively. Postoperatively, three of 11 (27%) participants who underwent inferior oblique disinsertion had residual head tilt, and all participants who underwent anterior transposition had resolution of head tilt (risk ratio (RR) 7.00, 95% CI 0.40 to 121.39). However, the authors did not report the angle of head tilt preoperatively or postoperatively. We rated the quality of the data for this outcome as very low due to bias in the study design as well as imprecision, reflected by the large confidence interval.
Hypertropia in down gaze
The Yanyali 2001 study did not report preoperative or postoperative data on hypertropia in down gaze.
Hypertropia in contralateral gaze
The Yanyali 2001 study did not specify the proportion of participants with a hypertropia of less than 3 PD in contralateral gaze. However, the study investigators reported that the mean reduction of hypertropia in adduction was 20.6 (SD 6.2) PD in the disinsertion group and 27.7 (SD 9.6) PD in the anterior transposition group (MD ‐7.10 PD, 95% CI ‐13.85 to ‐0.35). Anterior transposition resulted in a greater decrease in hypertropia in contralateral gaze, but it was unclear whether this difference favored the anterior transposition group, since the authors did not report the number of participants overcorrected in contralateral gaze. We rated the quality of the data for this outcome as moderate due to bias in the study design.
Cyclotorsion
The Yanyali 2001 study did not report preoperative or postoperative data on cyclotorsion.
Second surgery
In the Yanyali 2001 study, none of the participants who underwent anterior transposition required reoperation during the follow‐up period. However, three of 11 (27%) participants who underwent disinsertion of the inferior oblique muscle required a second surgery, which was a recession of the contralateral inferior rectus muscle in all cases (RR 7.00, 95% CI 0.40 to 121.39). We rated the quality of the data for this outcome as very low due to bias in the study design as well as imprecision, as indicated by the large confidence interval.
Relief of symptoms
The Yanyali 2001 study reported that one of 11 (9%) participants who underwent inferior oblique disinsertion had diplopia in primary position preoperatively. Two of 11 (18%) participants who underwent inferior oblique anterior transposition had preoperative diplopia. All three participants with preoperative diplopia had resolution of diplopia postoperatively.
Quality of life
The Yanyali 2001 study did not provide any data on quality of life using standard instruments or methods.
Adverse effects
In the Yanyali 2001 study, elevation deficiency was defined as clinically significant when it caused diplopia or restriction of elevation of the abducting eye with secondary upshoot of the contralateral adducting eye. No participant who underwent disinsertion had clinically significant or insignificant elevation deficiency. All participants who underwent anterior transposition had marked elevation deficiency on the first postoperative day, which decreased throughout the follow‐up period and was clinically insignificant in all participants at last follow‐up.
No participant who underwent inferior oblique disinsertion or anterior transposition developed postoperative hypotropia or reversal of the vertical deviation.
The Yanyali 2001 study did not report rates of orbital cellulitis, endophthalmitis, or retinal perforation. Iatrogenic Brown syndrome, the final adverse effect specified by this review, was not discussed in this study, but would not have been expected to occur because surgery was not performed on the superior oblique muscle.
Discussion
Superior oblique palsy is a common cause of vertical strabismus, and there are a number of surgical treatment options for the condition. However, data comparing these treatments are few or absent. We found only two randomized trials of surgical procedures for this disorder from our search of multiple publication databases and registers of clinical trials. The two trials each compared two different surgical techniques for weakening the ipsilateral inferior oblique muscle, so we analyzed a total of four surgical treatments in this review (inferior oblique myectomy versus recession, and disinsertion versus anterior transposition).
Summary of main results
Because the two studies included in this review compared the effects of two different pairs of surgical procedures, we were unable to combine data in a meta‐analysis for any outcome targeted for this review. Furthermore, neither of the studies provided data on our primary outcome, the proportion of participants with postoperative surgical success, defined as hypertropia less than 3 PD in primary gaze. The limited data preclude any conclusion regarding optimal surgical treatment of superior oblique palsy.
Instead of the proportion of participants with postoperative surgical success, both studies reported on the mean postoperative reduction in hypertropia in primary gaze. The Shipman 2003 study reported an average decrease in hypertropia of 14 PD in participants who underwent inferior oblique myectomy, compared to 8 PD after inferior oblique recession. However, the amount of recession performed (10 mm) is considered submaximal, and this study did not address how maximal inferior oblique recession would compare to inferior oblique myectomy. Yanyali 2001 reported that mean reduction in hypertropia in primary gaze was 18.5 (SD 3.9) PD after inferior oblique anterior transposition, compared to 13.3 (SD 1.9) PD after inferior oblique disinsertion.
Similarly, although neither study specifically addressed our secondary outcome of proportion of participants with hypertropia less than 3 PD in contralateral gaze, both studies reported the average postoperative reduction in vertical deviation in adduction. In the Shipman 2003 study, the mean decrease in hypertropia in contralateral gaze was 18.5 PD after myectomy and 16 PD after recession. Yanyali 2001 reported that the average reduction in hypertropia in adduction was 20.6 (SD 6.2) PD after disinsertion and 27.7 (SD 9.6) PD after anterior transposition. This outcome was similar in each pair of comparisons, and the reduction was large following each type of surgery.
None of the participants in either trial required a second surgery during the follow‐up period, except for three of 11 (27%) of those who underwent inferior oblique disinsertion (Yanyali 2001).
The Shipman 2003 study did not address any of the other secondary outcomes specified in this review, including proportion of participants with postoperative resolution of head tilt, postoperative hypertropia in down gaze, cyclotorsion, relief of symptoms, and quality of life.
Of the aforementioned secondary outcomes, the Yanyali 2001 study addressed the proportion of participants with postoperative resolution of head tilt. The Yanyali 2001 study reported that all participants who underwent inferior oblique anterior transposition had resolution of head tilt, in comparison to only eight of 11 (73%) after inferior oblique disinsertion. Additionally, all participants in the Yanyali 2001 study who had preoperative diplopia in primary gaze experienced resolution of diplopia after surgery.
Most of the adverse effects specified for this review (orbital cellulitis, endophthalmitis, retinal perforation, and iatrogenic Brown syndrome) were not addressed by either study. However, the Yanyali 2001 study reported that no participants who underwent inferior oblique anterior transposition or disinsertion experienced clinically significant anti‐elevation syndrome or reversal of vertical deviation in primary gaze postoperatively.
Overall completeness and applicability of evidence
Both studies included in this review had limitations in completeness and applicability.
The reporting in the Shipman 2003 study was more complete than the Yanyali 2001 study, due to prespecified time points at which outcomes were evaluated (2 weeks, 4 months, and 12 months). One participant who underwent recession failed to complete 12 months of follow‐up and was excluded from analysis. The characteristics of this participant were not described other than indicating that the participant was “asymptomatic in the early postoperative period.” It is therefore unclear whether the exclusion of this one participant could have introduced bias in the study. Because only 12 participants were randomized to inferior oblique recession, the absence of data from one participant could change the final results.
The main problem with applicability of the Shipman 2003 study lies in the subjectivity of the inclusion criteria. Participants were included if they experienced “symptom producing and/or socially noticeable unilateral overacting inferior oblique muscle.” Although the study authors reported that all participants had decompensated longstanding unilateral "superior oblique underaction," this was not stated to have been an inclusion criterion. There were no objective inclusion criteria, such as vertical deviation fulfilling one or more conditions of the Parks three‐step test, or evidence of superior oblique atrophy on neuroimaging. It is thus difficult to determine to what patient population the study’s results would be applicable.
Furthermore, the Shipman 2003 study failed to report preoperative data that could be used to compare the two study groups preoperatively, the investigators merely reporting that there was no significant difference in hypertropia in contralateral gaze and degree of "superior oblique underaction."
The reporting of outcomes in the Yanyali 2001 study was incomplete due to varying lengths of follow‐up time and absence of specific postoperative time points at which outcomes were assessed. Follow‐up of at least 6 months was expected, but follow‐up time ranged from 6 to 40 months (average 18.8 months), and outcome data were reported from "final follow‐up." The study authors did not specify whether follow‐up times differed between the two surgery groups. The Shipman 2003 study demonstrated that postoperative vertical deviation improved with longer follow‐up time after inferior oblique muscle surgery, therefore unreported differences in follow‐up time between the two surgical groups in the Yanyali 2001 study could confound interpretation of the results.
The inclusion criteria in the Yanyali 2001 study were stringent, requiring that participants demonstrate all three components of the Parks three‐step test for diagnosis of superior oblique palsy (hypertropia in primary position increasing on contralateral gaze and ipsilateral head tilt), in addition to ipsilateral overelevation in adduction and underdepression in adduction. Participants were also required to have a hypertropia of at least 8 PD in primary gaze. The study authors included this criterion to avoid postoperative hypotropia, due to the reportedly powerful effect of inferior oblique anterior transposition. The strict inclusion criteria were helpful in reducing the chance of misdiagnosis in the participants, but limit the generalizability of the study findings, as many people diagnosed with superior oblique palsy in clinical practice do not meet all criteria of the Parks three‐step test or have a primary position hypertropia of less than 8 PD, or both.
Quality of the evidence
We graded the overall quality of the evidence as low in both of the included studies. Both studies were characterized by poor reporting of methods, which created uncertainty in our assessments of the risk of most types of bias. Additionally, neither study reported data on our primary outcome, the proportion of participants with postoperative surgical success. Furthermore, both studies had a small sample size (22 and 23 participants), which contributed to imprecision in our statistical analysis (e.g. the confidence interval for the risk ratio for reoperation and resolution of head tilt in the Yanyali 2001 study ranged from 0.40 to 121.39). Neither study reported an a priori sample size calculation or computation of post hoc power to detect or rule out differences between surgeries in outcome estimates.
The Shipman 2003 study used a single, subjective inclusion criterion of symptomatic and/or socially noticeable overelevation in adduction. Although the authors stated that all participants had decompensated longstanding unilateral superior oblique palsy, the inclusion criteria are not supportive of this diagnosis. The study authors did not report method of randomization, and did not perform statistical comparisons of the two surgical groups on the measure of interest (vertical deviation in primary gaze) preoperatively. It is therefore unknown whether preoperative differences between the groups could account for the results. Furthermore, there was no indication that the participants or the orthoptist who performed preoperative and postoperative measurements was masked. The authors did not report the proportion of participants with surgical success, but instead indicated that the mean reduction in vertical deviation in primary gaze was greater in the myectomy group compared to the recession group. This difference was of borderline statistical significance. However, because of the purported self titrating effect of inferior oblique surgery, the absolute decrease in vertical deviation may be less clinically useful than the proportion of participants who achieve postoperative alignment within the vertical fusional range. The authors did report outcomes at prespecified time points, allowing comparisons between groups at 12 months' postoperatively.
In the Yanyali 2001 study, the inclusion and exclusion criteria were well‐defined, but there were no prespecified time points for outcome assessment, and the findings at the last follow‐up visit were reported. The authors did not report whether the follow‐up time differed between groups, therefore it is unknown whether differences in follow‐up time confounded interpretation of outcome comparisons. Additionally, the method of randomization was not specified, so the risk of selection and allocation bias is unclear. However, the authors provided statistical analysis showing that basic preoperative characteristics were similar between the groups. The authors did not indicate whether participants were masked, but the surgeons performed all preoperative and postoperative measurements, introducing a high risk of detection bias. Finally, the outcome measure reported in this study was the same as in the Shipman 2003 study, that is mean reduction in hypertropia in primary gaze. As discussed above, this outcome may be of limited clinical applicability as it may be dependent upon the preoperative vertical deviation.
Potential biases in the review process
We did not identify any potential biases in the review process.
Agreements and disagreements with other studies or reviews
The existing literature on surgical treatment of superior oblique palsy is mainly limited to case reports or retrospective case series, either describing the effects of one surgical treatment or comparing two surgical procedures that were not assigned in a random fashion. For instance, one group published a retrospective review of their results for isolated superior oblique tucking in people with superior oblique palsy over 17 years (Durnian 2011). The authors reported that, among 75 adults with congenital or acquired superior oblique palsy who underwent ipsilateral superior oblique tendon tuck, 71% achieved postoperative success, defined as absence of diplopia requiring reoperation. Similarly, another group published a retrospective non‐comparative study of their surgical results after inferior oblique anterior transposition for superior oblique palsy over an 11‐year period (Clifford 2015). These authors reported that 82% of 96 patients experienced postoperative success, defined as hypertropia measuring less than 5 PD in primary gaze, with absence of diplopia. These studies, although having the advantage of larger patient numbers since cases were reviewed over a long period of time, are non‐comparative and provide lower‐quality data due to their retrospective nature. Retrospective studies comparing different surgical procedures for superior oblique palsy have also been published. For example, one study reported the outcomes of 123 patients who underwent one‐ or two‐muscle surgery for superior oblique palsy (Simons 1998). The authors found that oblique muscle surgery (superior oblique tuck or inferior oblique weakening) was more frequently associated with an excellent outcome (hypertropia measuring 3 PD or less in primary gaze and reading position) than vertical rectus muscle surgery or combined oblique‐rectus muscle surgery. The authors also found that excellent results were more likely to be achieved with one‐muscle surgery when the preoperative vertical deviation measured less than 15 PD; multiple‐muscle surgery was more successful in patients with larger deviations. This retrospective study, along with other similar reports, is subject to bias due to lack of randomization, masking, and complete follow‐up at prespecified time points.
Additionally, many studies do not provide clear inclusion criteria to establish the diagnosis of superior oblique palsy, which would likely lead to the inclusion of participants with an alternative etiology of vertical strabismus, such as sagging eye syndrome (Chaudhuri 2013). The methodological limitations of these studies preclude meaningful comparison with the current review. We did not identify any prior systematic review or meta‐analysis of randomized trials of surgical treatment for vertical strabismus in superior oblique palsy.
Several authors, including the investigators in the Simons 1998 study, suggest performing oblique muscle surgery as the initial surgical procedure for superior oblique palsy. This surgery would consist of superior oblique tendon plication ('tuck') when the superior oblique tendon is found to be lax intraoperatively, or an inferior oblique weakening procedure when the superior oblique tendon is normal. Vertical rectus muscle surgery (contralateral inferior rectus recession or ipsilateral superior rectus recession) has been recommended as a secondary procedure. However, there are no data from randomized trials or well‐designed prospective studies to support these recommendations.
Similar to this review, retrospective studies have reported that the risk of elevation deficiency is higher in inferior oblique anterior transposition compared to other inferior oblique weakening procedures. The risk of hypotropia in primary gaze, as well as other adverse effects, varies in the literature.
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
| Inferior oblique myectomy compared with inferior oblique recession for vertical strabismus in superior oblique palsy | ||||
| Patient or population: people with symptom‐producing and/or socially noticeable unilateral overacting inferior oblique muscle; all participants had longstanding unilateral superior oblique underaction Settings: eye hospital Intervention: inferior oblique myectomy Comparison: inferior oblique recession | ||||
| Outcomes | Relative effect | No. of participants | Quality of the evidence | Comments |
| Proportion of participants with postoperative surgical success (hypertropia less than 3 PD in primary gaze) | N/A | 23 (1 study) | N/A | This outcome measure was not reported in the study included in this comparison. However, median hypertropia in primary gaze at 12 months was 3 PD in the myectomy group and 1 PD in the recession group. The average reduction in hypertropia in primary position was 14 PD in the myectomy group and 8 PD in the recession group (P = 0.042). |
| Proportion of participants with anomalous head position preoperatively with residual head tilt postoperatively | N/A | 23 (1 study) | N/A | This outcome measure was not reported in the study included in this comparison. |
| Proportion of participants with postoperative hypertropia less than 3 PD in down gaze | N/A | 23 (1 study) | N/A | This outcome measure was not reported in the study included in this comparison. |
| Proportion of participants with postoperative hypertropia less than 3 PD in contralateral gaze | N/A | 23 (1 study) | N/A | This outcome measure was not reported in the study included in this comparison. |
| Proportion of participants who received additional strabismus surgery | N/A | 23 (1 study) | N/A | None of the participants in either group required a second strabismus surgery during the follow‐up interval. |
| Proportion of participants with reversal of vertical deviation postoperatively | N/A | 23 (1 study) | N/A | This outcome measure was not reported in the study included in this comparison. |
| Proportion of participants with postoperative orbital cellulitis | N/A | 23 (1 study) | N/A | This outcome measure was not reported in the study included in this comparison. |
| GRADE Working Group grades of evidence CI: confidence interval; N/A: not applicable; PD: prism diopters | ||||
| Inferior oblique disinsertion compared with inferior oblique anterior transposition for vertical strabismus in superior oblique palsy | ||||
| Patient or population: people with unilateral superior oblique palsy Settings: eye hospital Intervention: inferior oblique disinsertion Comparison: inferior oblique anterior transposition | ||||
| Outcomes | Relative effect | No. of participants | Quality of the evidence | Comments |
| Proportion of participants with postoperative surgical success (hypertropia less than 3 PD in primary gaze) | N/A | 22 (1 study) | Moderate | This outcome measure was not reported in the study included in this comparison. However, the mean reduction of hypertropia in primary position was 13.3 (SD 1.9) PD in the disinsertion group and 18.5 (SD 3.9) PD in the anterior transposition group (mean difference ‐5.20 PD, 95% CI ‐7.76 to ‐2.64). This difference favors inferior oblique anterior transposition. |
| Proportion of participants with anomalous head position preoperatively with residual head tilt postoperatively | RR 7.00 (0.40 to 121.39) | 22 (1 study) | Very low | This outcome favors inferior oblique anterior transposition. |
| Proportion of participants with postoperative hypertropia less than 3 PD in down gaze | N/A | 22 (1 study) | N/A | This outcome measure was not reported in the study included in this comparison. |
| Proportion of participants with postoperative hypertropia less than 3 PD in contralateral gaze | N/A | 22 (1 study) | Moderate | The mean reduction of hypertropia in adduction was 20.6 (SD 6.2) PD in the disinsertion group and 27.7 (SD 9.6) PD in the anterior transposition group (mean difference ‐7.10 PD, 95% CI ‐13.85 to ‐0.35). Anterior transposition resulted in a greater decrease in hypertropia in contralateral gaze, but it was unclear whether this difference favored the anterior transposition group, since the authors did not report the number of participants overcorrected in contralateral gaze. |
| Proportion of participants who received additional strabismus surgery | RR 7.00 (0.40 to 121.39) | 22 (1 study) | Very low | This outcome favors inferior oblique anterior transposition. |
| Proportion of participants with reversal of vertical deviation postoperatively | N/A | 22 (1 study) | N/A | None of the participants in either group developed postoperative reversal of vertical deviation. |
| Proportion of participants with postoperative orbital cellulitis | N/A | 22 (1 study) | N/A | This outcome measure was not reported in the study included in this comparison. |
| GRADE Working Group grades of evidence CI: confidence interval; N/A: not applicable; PD: prism diopters; RR: risk ratio; SD: standard deviation | ||||

