Intervenciones para las exacerbaciones de otoño del asma en niños
Resumen
Antecedentes
Las exacerbaciones del asma en los niños en edad escolar alcanzan un punto máximo en el otoño, poco después del retorno de los niños a la escuela después de las vacaciones de verano. Lo anterior podría reflejar una combinación de factores de riesgo que incluye el cumplimiento deficiente del tratamiento, el aumento de los alérgenos y la exposición a los virus, y la modificación de la tolerancia inmunitaria. Debido a que este incremento máximo es previsible, las intervenciones dirigidas a los factores de riesgo modificables podrían reducir la morbilidad asociada con la exacerbación y la sobrecarga para los recursos sanitarios. El incremento máximo ocurre en septiembre en el hemisferio norte y en febrero en el hemisferio sur.
Objetivos
Evaluar los efectos de la farmacoterapia y las intervenciones conductuales implementadas en previsión del retorno a la escuela durante el otoño, que están diseñadas para reducir las exacerbaciones del asma en los niños durante este período.
Métodos de búsqueda
Se hicieron búsquedas en el registro de ensayos del Grupo Cochrane de Vías Respiratorias (Cochrane Airways Group Trials Register), ClinicalTrials.gov, la World Health Organization International Clinical Trials Registry Platform, listas de referencias de estudios primarios y revisiones existentes, y los registros de ensayos de los fabricantes (Merck, Novartis and Ono Parmaceuticals). Se realizaron búsquedas en las bases de datos desde su inicio hasta el 1 diciembre 2017 y no se aplicaron restricciones en el idioma de publicación.
Criterios de selección
Se incluyeron todos los ensayos controlados aleatorios que compararon intervenciones dirigidas específicamente a la reducción de las exacerbaciones de otoño, con la atención habitual (ningún cambio sistemático en el tratamiento como preparación para el retorno a la escuela). Se incluyeron estudios con datos sobre niños de 18 años o menos.
Obtención y análisis de los datos
Se utilizaron los procedimientos metodológicos estándar previstos por la Colaboración Cochrane. Dos autores de la revisión de forma independiente examinaron los registros identificados mediante la búsqueda y luego extrajeron los datos y evaluaron el sesgo de los ensayos que cumplieron los criterios de inclusión. Un tercer autor de la revisión verificó la presencia de exactitud y medió para alcanzar consenso cuando hubo desacuerdos. El resultado primario fue la proporción de niños que presentaron una o más exacerbaciones del asma que requirieron hospitalización o corticosteroides orales durante el período de otoño.
Resultados principales
Las búsquedas obtuvieron 546 ensayos, de los cuales cinco cumplieron los criterios de inclusión. Estos estudios asignaron al azar a 14 252 niños a recibir una intervención o la atención habitual. Todos los estudios se realizaron en el hemisferio norte. Tres intervenciones utilizaron un antagonista de los receptores de leucotrieno, una utilizó omalizumab o un refuerzo de corticosteroides inhalados, y el estudio más grande (12 179 niños) utilizó una carta de recordatorio de la medicación. Aunque el riesgo de sesgo en los estudios individuales fue generalmente bajo, la calidad de la evidencia se disminuyó debido a la imprecisión asociada con el escaso número de participantes, la consistencia deficiente entre los estudios y la falta de direccionalidad en la determinación de los resultados.
Un estudio de los EE.UU. que incluyó 513 niños con asma leve/grave y sensibilización alérgica fue el único que proporcionó datos para el resultado primario. En este estudio la proporción de participantes que presentaron una exacerbación que requirió corticosteroides orales o ingreso hospitalario en los 90 días posteriores al retorno a la escuela se redujo significativamente al 11,3% en los pacientes que recibieron omalizumab en comparación con el 21,0% en los que recibieron placebo (odds ratio 0,48; intervalo de confianza del 95%: 0,25 a 0,92; evidencia de calidad moderada). Los estudios restantes utilizaron definiciones alternativas de exacerbación. Cuando los datos de dos estudios de antagonistas de los receptores de leucotrieno con resultados equivalentes se combinaron en un modelo de efectos aleatorios, no hubo evidencia de un efecto sobre las exacerbaciones. No hubo evidencia de que una carta estacional de recordatorio de la medicación reduce las consultas no programadas debido a un diagnóstico respiratorio entre septiembre y diciembre.
Cuatro estudios registraron eventos adversos. No hubo evidencia de que la proporción de participantes que presentaron al menos un evento adverso difiere entre los grupos de intervención y atención habitual. La falta de datos impidió realizar los análisis de subgrupos y de sensibilidad programados.
Conclusiones de los autores
El tratamiento estacional con omalizumab de cuatro a seis semanas antes del retorno a la escuela podría reducir las exacerbaciones de otoño del asma. No se encontró evidencia de que esta estrategia se asocie con un aumento en los efectos adversos diferentes del dolor en el sitio de inyección, pero es costosa. No hubo datos con los que se pudiera valorar el efecto de ésta u otras intervenciones estacionales sobre el control del asma, la calidad de vida o la muerte relacionada con el asma. En los estudios futuros se deben proporcionar y estandarizar las definiciones de exacerbaciones, cuando sea posible. Para investigar los posibles efectos diferenciales según los subgrupos, los participantes de los ensayos futuros se deben caracterizar de manera adecuada en cuanto a la gravedad inicial del asma y los antecedentes de exacerbaciones, además de la edad y el sexo.
PICOs
Resumen en términos sencillos
Intervenciones para prevenir las crisis asmáticas en niños con el retorno a la escuela en el otoño
Antecedentes
El asma es una afección a largo plazo que afecta a los pulmones. Es la afección a largo plazo más frecuente que afecta a los niños. Uno de cada 11 niños en el Reino Unido presenta asma. Los pacientes con asma pueden presentar "crisis" de asma con tos, sibilancias y dificultad para respirar.
Cada año hay un punto máximo en las crisis asmáticas después del retorno a la escuela en el otoño. Un probable motivo para lo anterior es que los niños están expuestos a más virus que pueden desencadenar el asma. Los niños también pueden haber tomado su medicación regular de forma menos sistemática debido a la interrupción en la rutina durante el verano.
Como este aumento de las crisis al comienzo del año escolar es previsible, y de cierta forma se comprenden los motivos, podría ser prevenible. Los enfoques para reducir las crisis asmáticas de otoño incluyen la administración extra de fármacos cuando retornan a la escuela o recordatorios de la medicación durante las vacaciones escolares.
Principales hallazgos
Las búsquedas encontraron 546 ensayos, de los cuales cinco fueron relevantes. Se asignó al azar un total de 14 252 niños a recibir una intervención para las crisis asmáticas de otoño o atención habitual. Cuatro estudios pequeños (aproximadamente 200 a 1200 niños en cada uno) les administraron a los niños medicación extra para el asma; estos fármacos adicionales fueron omalizumab, comprimidos de antagonistas de los receptores de leucotrieno o un aumento en las dosis de esteroides inhalados. Un estudio envió una carta de recordatorio de la medicación durante las vacaciones de verano a los padres de los niños con asma.
Un ensayo administró a los niños omalizumab o placebo. Omalizumab es un anticuerpo diseñado para modificar la respuesta inmunitaria. Se administró mediante inyección de manera regular durante cuatro a seis semanas antes del retorno a la escuela (es decir, durante la mayor parte de las vacaciones de verano). Se sabía que los niños de este estudio presentaban asma alérgica. El estudio mostró que omalizumab podría reducir las crisis de otoño. El 11% de los niños que recibieron omalizumab presentaron una crisis asmática durante los primeros 90 días en comparación con el 21% de los que recibieron placebo.
Tres estudios administraron comprimidos de antagonistas de los receptores de leucotrieno, montelukast o pranlukast. Aunque los resultados de un estudio indicaron que el montelukast estacional podría reducir las crisis de otoño, no hubo evidencia de una reducción en las crisis en los otros dos ensayos posteriores, incluido un segundo ensayo más grande de montelukast.
No hubo evidencia de que el envío de una carta de recordatorio reduzca el número de niños que requieren atención sanitaria no planificada.
Ningún estudio aportó evidencia de que el número total de niños que presentaron eventos adversos fuera mayor en el grupo de intervención que en el grupo de atención habitual.
Limitaciones
Los resultados de esta revisión fueron limitados debido al escaso número de estudios identificados y porque estos estudios utilizaron diferentes intervenciones y definiciones de exacerbaciones del asma. Se necesitan estudios de investigación adicionales para comprender mejor cómo prevenir las crisis estacionales, incluidas intervenciones apropiadas para los niños con asma leve, donde los tratamientos costosos y dolorosos no están justificados.
Authors' conclusions
Summary of findings
| Omalizumab compared to usual care for autumn asthma exacerbations in children | ||||||
| Patient or population: autumn asthma exacerbations in children Setting: community | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with usual care | Risk with omalizumab | |||||
| Exacerbations | 210 per 1000 | 113 per 1000 (62 to 197) | OR 0.48 (0.25 to 0.92) | 348 (1 RCT) | ⊕⊕⊕⊝ | Absolute effects calculated using control risk of 21.0% from Teach 2015a. |
| Exacerbations | 326 per 1000 | 152 per 1000 | OR 0.37 | 184 | ⊕⊕⊕⊝ | Absolute effects calculated using control risk of 32.6% from Teach 2015a. |
| Exacerbations | 127 per 1000 | 83 per 1000 | OR 0.63 | 164 | ⊕⊕⊕⊝ | Absolute effects calculated using control risk of 12.7% from Teach 2015a. |
| Adverse events | 548 per 1000 | 546 per 1000 | OR 0.99 | 361 | ⊕⊕⊕⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded once for imprecision because few children studied. | ||||||
| A boost of inhaled corticosteroids compared to usual care for autumn asthma exacerbations in children | ||||||
| Patient or population: autumn asthma exacerbations in children Setting: community | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with usual care | Risk with a boost of inhaled corticosteroids | |||||
| Exacerbations | 127 per 1000 | 111 per 1000 | OR 0.86 | 173 | ⊕⊕⊕⊝ | Absolute effects calculated using control risk of 12.7% from Teach 2015a. |
| Adverse events | 533 per 1000 | 434 per 1000 | OR 0.67 | 176 | ⊕⊕⊕⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded once for imprecision because few children studied. | ||||||
| Leukotriene receptor antagonist (LTRA) compared to usual care for autumn asthma exacerbations in children | ||||||
| Patient or population: autumn asthma exacerbations in children Setting: community | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with usual care | Risk with montelukast | |||||
| Exacerbations assessed with: oral corticosteroid or hospitalisation | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Exacerbations | 146 per 1000 | 79 per 1000 | OR 0.50 | 1326 | ⊕⊕⊝⊝ | Absolute effects calculated using control risk of 14.6% from Johnston 2007. |
| Adverse events | 328 per 1000 | 307 per 1000 | OR 0.91 | 1326 | ⊕⊕⊕⊕ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded once for inconsistency because asthma severity of children differed between included studies, and thresholds for medical contact or oral steroids appeared to differ between studies. | ||||||
| Behavioural intervention compared to usual care for autumn asthma exacerbations in children | ||||||
| Patient or population: autumn asthma exacerbations in children | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with usual care | Risk with behavioural intervention | |||||
| Exacerbations | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Exacerbations | 167 per 1000 | 185 per 1000 | OR 1.13 | 10,481 | ⊕⊕⊕⊝ | Absolute effects calculated using control rate of 16.7% from Julious 2016. |
| Adverse events | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded once for indirectness because studies contained no data on hospitalisation and need for oral steroids, so unscheduled contacts for a respiratory diagnosis used as a proxy outcome. | ||||||
Background
Description of the condition
Asthma is a chronic disease of the airways characterised by recurrent episodes of wheezing, breathlessness, and cough, together with variable expiratory airflow limitation. Symptoms are frequently associated with airway inflammation and bronchial hyper‐responsiveness (GINA 2017). Asthma can affect people of all ages, although childhood onset is common. Asthma is diagnosed clinically based upon evaluation of symptoms and response to pharmacotherapy. There is no specific diagnostic test, although spirometric measurement of reversible airflow limitation and indirect or direct tests of airway hyper‐responsiveness can be useful (GINA 2017).
The number of people with asthma globally is currently estimated to be approximately 300 million, and is expected to grow to closer to 400 million by 2025 (WHO 2007). Asthma is the most common chronic disease among children (Asher 2014). The International Study of Asthma and Allergies in Childhood (ISAAC), conducted between 2002 and 2003, found the highest prevalence of childhood wheeze in Latin and North America, and in English‐speaking countries in Australasia and Europe (Asher 2006). More than 1 million children (1 in 11) in the United Kingdom are currently believed to be living with asthma (Asthma UK 2016).
Symptom exacerbations can be triggered by a number of environmental challenges, including pollutants (Lierl 2003; Schildcrout 2006), physical activity (Randolph 2013), and respiratory infections or allergens (Brandt 2015; Ito 2015; Murray 2006; Olenec 2010). People whose airway inflammation is not adequately controlled are more vulnerable to exacerbations than those on adequate therapy with good treatment adherence. Poorly controlled day‐to‐day asthma symptoms can limit activities, including schooling, and impair sleep quality and overall quality of life (Kiotseridis 2013; Teyhan 2015; van Maanen 2013). However, it is asthma exacerbations or 'attacks' ‐ acute or subacute progressive worsening of symptoms ‐ which pose the greatest danger to people with asthma (NAEPP 2007). Asthma exacerbations are also associated with reduced school or work attendance and are the most important contributor to the economic and social costs of asthma (Bahadori 2009; Hoskins 2000; Ismaila 2013).
A seasonal peak in exacerbation rates has been consistently demonstrated in the autumn months (September to November) across multiple Northern Hemisphere countries (Fleming 2000; Gergen 2002). More specifically, exacerbation rates peak in September following the summer school holiday and in line with the start of the autumn term (Johnston 2006). Equivalent peaks during February have been reported in Southern Hemisphere countries (Lincoln 2006; Lister 2001). The autumn peak in asthma exacerbations is temporally linked to children returning to school and most pronounced in school‐aged children (Corne 2002). Hospitalisations and emergency department visits attributable to asthma demonstrate an initial peak in school‐aged children; however, this is followed within days by increased hospitalisations in preschool children and a more blunted peak in adults up to the age of 50 years (Sears 2008). There is evidence that viral infections, particularly rhinovirus, may contribute to this seasonality (Johnston 1996; Johnston 2005; Thumerelle 2003), but suboptimal asthma treatment and changes in tolerance may also be contributing factors (Johnston 2005; Tovey 2011). Not only do viral infections trigger asthma exacerbations, but there is also evidence that asthmatic individuals are more susceptible to rhinovirus infection than those without asthma (Baraldo 2012; Wark 2005). Individuals at particular risk of asthma exacerbation have been identified as those with more severe disease, greater degree of atopy, and recent exacerbations (Teach 2015b).
Description of the intervention
A number of interventions including asthma education programmes, action plans, self monitoring, and self initiation of oral corticosteroid (OCS) treatment have been shown to reduce both symptom exacerbations and need for unscheduled acute care in children with asthma (Bhogal 2006; Guevara 2003; Vuillermin 2011). Given that the seasonality of asthma exacerbations in school‐aged children is predictable and repeatable, it is reasonable to assume that management strategies that anticipate increased risk in the autumn might reduce exacerbation frequency during this period. Whilst the exact aetiology of the seasonal peak in asthma exacerbations is not fully understood, any change in management aimed at improving asthma control in anticipation of the autumn school return, if successful, could offer protection against the increased risk recognised to be associated with this event. Therapies that have been demonstrated to reduce the seasonal excess of exacerbations in the autumn, in addition to the annual number of exacerbations, include year‐round treatment with the anti‐immunoglobulin E (IgE) monoclonal antibody omalizumab (Busse 2011); or with high‐dose inhaled corticosteroids (ICS) (Szefler 2008). However, omalizumab is an expensive and sometimes painful treatment, whilst high‐dose ICS are associated with adverse effects upon growth and bone health (Pruteanu 2014; Wong 2000).
Given the pragmatic difficulties associated with minimising viral or allergen exposure, two main potential strategies remain that might reduce autumn asthma exacerbations whilst minimising treatment costs and adverse effects. The first strategy would be to add on, or increase, asthma pharmacotherapy before the autumn period; the second strategy would be to focus upon treatment adherence and achieving symptom control before and during the autumn. It is anticipated that school‐aged children would gain the greatest benefit from an intervention targeting seasonal exacerbations, since the autumn peak in exacerbations is most pronounced in this age group. Similarly, greater benefit might be demonstrable in those at increased risk of exacerbation due to poor treatment adherence, severe disease, allergic phenotype, or recent exacerbation.
Add‐on therapies include those aimed at reducing airway inflammation, such as corticosteroid preparations, macrolide antibiotics, or leukotriene receptor antagonists (LTRAs). Alternatively, agents such as biologics which more specifically target the interaction between the immune response, allergens, and viral infection might be selected (Beck 2004; Durrani 2012; Gill 2010). Important considerations with respect to choice of intervention include onset of action and ease of administration, in addition to cost and adverse effect profile.
Strategies to improve treatment adherence require adherence status to be assessed, and barriers leading to non‐adherence to be identified and addressed. The success of adherence interventions can be increased by a number of strategies, including the provision of biofeedback, Feldman 2012, and increasing motivation via motivational interviewing techniques (Borrelli 2007). Nevertheless, it is difficult to achieve sustained adherence (Jonasson 2000). Targeting adherence interventions to periods of increased exacerbation risk might increase their overall benefit.
How the intervention might work
Upon return to school in the autumn children are exposed to allergens and respiratory infections by close contact with their classmates (Cai 2011; Krop 2014). During the autumn months mould spores, which can act as a trigger for allergic asthma, are more abundant than at other times of the year (de Ana 2006). However, the sequential periods of peak risk demonstrated by school‐aged children, younger children, and adults suggest a transmissible agent is responsible. In support of this are findings from virological studies that demonstrate increased viral isolations during autumn, notably rhinovirus, from children with asthma compared to those without, with the highest rates of isolation measured in those admitted to hospital with an asthma exacerbation (Johnston 2005; Thumerelle 2003).
Changes in routine during the summer holidays and lower perceived risk of cold weather or respiratory infection might be associated with both intentional reduction in preventer medication and unintentional poor adherence (Johnston 2005; Sears 2008). A higher rate of exacerbation has been reported in people prescribed bronchodilator therapy alone than in those prescribed an inhaled steroid or other preventer medication (Johnston 2005; Murray 2006). Furthermore, within a trial of seasonal omalizumab treatment, school‐aged children with mild asthma but poor control, as evidenced by an exacerbation during the run‐in period of four to nine months, experienced a significant reduction in exacerbation frequency (Teach 2015a). Exacerbation frequency could not be significantly reduced in those with mild asthma but without a recent admission (Teach 2015a). Any intervention based upon reinforcing or increasing adherence to regular treatment, monitoring symptoms to assess control, or a seasonal enhancement of treatment might potentially reduce ongoing airway inflammation and the likelihood of viral infection triggering an exacerbation.
Why it is important to do this review
Although the asthma epidemic observed in the 1980s and 1990s appears to have stabilised, a study from the Northern Hemisphere demonstrates that emergency care contacts due to asthma remain significantly higher in September than in other months (Larsen 2016). Despite this, current national and international guidelines offer no guidance on strategies to reduce seasonal exacerbations after autumn school return. Following the recent successful trial of seasonal omalizumab, which demonstrated reduced exacerbations amongst children with severe or poorly controlled asthma (Teach 2015a), it is important to identify whether a similar effect can be achieved with less invasive and less expensive medications. This is particularly the case in countries such as the United Kingdom where omalizumab can only be prescribed to children meeting strict severity criteria. A quarter of annual hospitalisations for asthma are estimated to occur in September (Johnston 2001), and acute exacerbations are the principal driver of the economic and social costs of asthma (Bahadori 2009; Hoskins 2000; Ismaila 2013). Interventions based upon an anticipatory change in asthma management, if successful, could therefore substantially reduce both the overall exacerbation rate and the strain placed upon health services during autumn.
Objectives
To assess the effects of pharmacotherapy and behavioural interventions enacted in anticipation of school return during autumn that are designed to reduce asthma exacerbations in children during this period.
Methods
Criteria for considering studies for this review
Types of studies
We restricted inclusion to randomised controlled trials with a control arm of usual care since currently there is no recommended management strategy for autumn exacerbations. Studies reported as full text, those published as abstract only, and unpublished data were all eligible for inclusion.
Types of participants
We included studies presenting data relating to children with asthma. Studies needed to recruit children aged 18 years or younger, including preschool‐age as well as school‐aged children.
Types of interventions
We included studies comparing interventions aimed specifically at reducing autumn exacerbations with usual care where there is no systematic change in management in preparation for school return. Eligible interventions included pharmacotherapy trials and behavioural or educational‐based initiatives.
Types of outcome measures
Primary outcomes
The primary outcome was number of children (adjusted for the number of participants per group) experiencing one or more asthma exacerbations during the autumn period (the first three‐month period following the autumn school return) or during the intervention period if this included the autumn months. An exacerbation was defined as increased asthma symptoms requiring treatment with OCS or hospitalisation.
Secondary outcomes
-
Number of children experiencing exacerbations of asthma requiring hospitalisation.
-
Number of children experiencing exacerbations of asthma requiring paediatric intensive care unit admission.
-
Number of asthma‐related deaths.
-
Asthma control, measured by standardised tool (e.g. Childhood Asthma Control Test (cACT) or Asthma Control Test (ACT)).
-
Asthma‐related quality of life measured by standardised tool (e.g. Paediatric Asthma Quality of Life Questionnaire (PAQLQ) or Asthma Quality of Life Questionnaire (AQLQ)).
-
Days of schooling (or employment, for those beyond school age) missed.
-
Adverse events (including serious adverse events).
For each outcome data were collected throughout the autumn period or the intervention period (as for the primary outcome) in both the intervention group and the usual therapy group.
We did not require report of the primary outcome as an inclusion criterion for the review.
Search methods for identification of studies
Electronic searches
We identified trials from the Cochrane Airways Group's Trials Register, which is maintained by the Information Specialist for the Group. The Register contains trial reports identified through systematic searches of several sources:
-
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL), through the Cochrane Register of Studies Online (crso.cochrane.org);
-
weekly searches of MEDLINE Ovid SP 1946 to date;
-
weekly searches of Embase Ovid SP 1974 to date;
-
monthly searches of PsycINFO Ovid SP 1967 to date;
-
monthly searches of CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature) 1937 to date;
-
monthly searches of AMED EBSCO (Allied and Complementary Medicine) all years to date;
-
handsearches of the proceedings of major respiratory conferences.
Studies contained in the Trials Register are identified through search strategies based on the scope of Cochrane Airways. Details of these strategies, as well as a list of handsearched conference proceedings, can be found in Appendix 1. See Appendix 2 for search terms used to identify studies for this review.
We also conducted a search of ClinicalTrials.gov (www.clinicaltrials.gov) and the World Health Organization International Clinical Trials Registry Platform (www.who.int/ictrp/en/). We searched all databases from their inception to 1 December 2017, and imposed no restriction on language of publication.
Searching other resources
We checked reference lists of all primary studies and review articles for additional references. We searched relevant manufacturers' websites for trial information (Merck, Novartis and Ono Pharmaceuticals).
On 1 December 2017 we searched for errata or retractions from included studies published in full text on PubMed (www.ncbi.nlm.nih.gov/pubmed).
Data collection and analysis
Selection of studies
Two review authors (KCP, MA) independently screened for potential inclusion titles and abstracts of all the studies identified as a result of the search and coded them as 'retrieve' (eligible or potentially eligible/unclear) or 'do not retrieve'. We retrieved the full‐text study reports/publications, and two review authors (KCP, MA) independently screened the full texts and identified studies for inclusion and recorded reasons for exclusion of the ineligible studies. Any disagreements were resolved through discussion or, if required, by consultation with a third review author (DK). We identified and excluded duplicates and collated multiple reports of the same study so that each study, rather than each report, was the unit of interest in the review. We recorded the selection process using EPPI‐Reviewer 4 and completed a PRISMA flow diagram and Characteristics of included studies table (EPPI‐Reviewer 4 2010; Moher 2009).
Data extraction and management
We used a data collection form for study characteristics and outcome data that was piloted on two studies in the review. Three review authors (KCP, KMH, MA) extracted study characteristics from included studies in triplicate. We extracted the following study characteristics.
-
Methods: study design, total duration of study, details of any 'run‐in' period, number of study centres and location, study setting, withdrawals, and date of study.
-
Participants: number, mean age, age range, gender, severity of condition, diagnostic criteria, baseline lung function, smoking history, inclusion criteria, and exclusion criteria.
-
Interventions: intervention type, comparison, concomitant medications, and excluded medications.
-
Outcomes: primary and secondary outcomes specified and collected, and time points reported.
-
Notes: funding for trial, and notable conflicts of interest of trial authors.
Two review authors (KCP, MA) independently extracted outcome data from the included studies. We noted in the Characteristics of included studies table if outcome data were not reported in a usable way. Any disagreements were resolved by consensus or by involving a third review author (KMH) when necessary. One review author (KCP) transferred data into the Review Manager 5 file (RevMan 2014). We double‐checked that data were entered correctly by comparing the data presented in the systematic review with the data in the study reports. A second review author (DK) spot‐checked study characteristics for accuracy against the trial report.
Assessment of risk of bias in included studies
Two review authors (KCP, MA) independently assessed the risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Any disagreements were resolved by discussion or by involving another review author (KMH) when necessary. We assessed the risk of bias according to the following domains.
-
Random sequence generation.
-
Allocation concealment.
-
Blinding of participants and personnel.
-
Blinding of outcome assessment.
-
Incomplete outcome data.
-
Selective outcome reporting.
-
Other bias.
We graded each potential source of bias as high, low, or unclear and provided a quote from the study report together with a justification for our judgement in the 'Risk of bias' tables included within the Characteristics of included studies table. We summarised the 'Risk of bias' judgements across different studies for each of the domains listed. We considered blinding separately for different key outcomes where necessary (e.g. for unblinded outcome assessment, risk of bias for asthma‐related mortality may be very different than for a patient‐reported asthma control scale). Where information on risk of bias related to unpublished data or correspondence with a trialist, we noted this in the Characteristics of included studies table.
When considering treatment effects, we took into account the risk of bias for the studies that contributed to that outcome.
Assessment of bias in conducting the systematic review
We conducted the review according to the published protocol (Pike 2016) and reported deviations from it in the Differences between protocol and review section.
Measures of treatment effect
We analysed dichotomous data as odds ratios.
We undertook meta‐analyses only where this was meaningful, such as when the interventions, participants, outcomes, and underlying clinical question were similar enough for pooling to make sense.
Unit of analysis issues
We considered asthma exacerbation a dichotomous outcome using participants as the unit of analysis. The odds of exacerbation in the intervention group during the intervention were compared to the odds of exacerbation in individuals receiving usual therapy. Where multiple changes in management strategy were included in the original studies (e.g. seasonal omalizumab or a steroid boost in addition to usual therapy), the odds of exacerbation in each group that included a change in management were compared to the group receiving usual care only or usual care with a placebo. For large‐scale behavioural interventions (e.g. those involving contacting families in late summer to remind them of the need for treatment adherence), the unit of allocation may be at the level of primary care practice level rather than the individual. Where this was the case, we included results only if the original trial accounted for clustering or if it was possible to adjust for this by calculating a design effect.
Dealing with missing data
We contacted investigators or study sponsors in order to verify key study characteristics and to obtain missing numerical outcome data where possible (e.g. if an odds ratio was presented without a confidence interval).
Assessment of heterogeneity
We used the I² statistic to measure heterogeneity among the trials in each analysis. Where possible we intended to report the I² statistic, and if we identified substantial heterogeneity (I² > 50%) to explore possible causes by prespecified subgroup analyses.
Assessment of reporting biases
Had we been able to pool more than 10 trials, we intended to create and examine a funnel plot to explore possible small‐study and publication biases.
Data synthesis
We used an inverse variance model for outcomes where odds ratios from the original studies were adjusted for covariables. We used a Mantel‐Haenszel model for outcomes where confounding covariables were not identified and where absolute numbers of children experiencing the outcome were reported or could be calculated. We used Review Manager 5 software to calculate random‐effects models for all outcomes (RevMan 2014), as we expected variation in effects due to differences in study populations and methods (Mantel 1959). We performed a sensitivity analysis with a fixed‐effect model when we encountered significant heterogeneity.
'Summary of findings' tables
We created 'Summary of findings' tables for each intervention type using the following outcomes: exacerbation occurrence (requiring oral steroids or hospitalisation), exacerbation occurrence (defined according to alternative definition), and adverse events. We used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias) to assess the quality of a body of evidence as it relates to the studies that contributed data for the prespecified outcomes. We used methods and recommendations described in Section 8.5 and Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), employing GRADEpro GDT software. We justified all decisions to down‐ or upgrade the quality of studies using footnotes and made comments to aid the reader's understanding of the review where necessary.
Subgroup analysis and investigation of heterogeneity
We recognised that intervention type and/or disease severity might affect effect sizes, and therefore planned to carry out the following subgroup analyses for all outcomes.
-
An analysis separating studies based on pharmacological interventions from those based on non‐pharmacological interventions.
-
Analyses considering separately those with mild to moderate disease (intermittent bronchodilator only; or low/moderate ICS with or without a single add‐on therapy) and those with severe asthma (two or more add‐on therapies; or high‐dose ICS ‐ daily beclomethasone equivalents for children 5 to 12 years: ≥ 800 mcg; for children older than 12 years: ≥ 2000 mcg).
We planned to use identical primary and secondary outcomes in subgroup analyses as in the main analysis.
We planned to use the formal test for subgroup interactions in Review Manager 5 to determine statistical significance of subgroup analyses (RevMan 2014).
Sensitivity analysis
We planned to carry out the following sensitivity analyses.
-
An analysis including only studies without missing data.
-
An analysis excluding cluster‐randomised trials (in case any benefit in cluster‐randomised trials arises due to the 'herd' effect of an intervention).
We also planned to re‐run analyses and compare results after sequential exclusion of each study from any meta‐analysis.
Results
Description of studies
We included detailed descriptions of studies fulfilling the criteria specified in the protocol in the Characteristics of included studies section. Studies for which full texts were reviewed but were eventually excluded were collated along with reasons for exclusion in the Characteristics of excluded studies section.
Results of the search
Electronic searches run in December 2017 identified 546 records. We removed four duplicates and four abstracts where full texts describing the same study were also identified. After screening full texts and abstracts, we evaluated 31 full texts against the inclusion criteria. We assessed 22 as not meeting the inclusion criteria, leaving nine references to five studies for inclusion in the review (Figure 1).

Study flow diagram.
Included studies
Five studies (nine citations) met the inclusion criteria. All five reported upon the effect of an intervention specifically designed to reduce asthma exacerbations in predominantly school‐aged children following return to school in the autumn. Two studies were funded by Merck (Johnston 2007; Weiss 2010), two by national funding bodies, (Julious 2016 (funded by the National Institute for Health Research) and Teach 2015a (funded by the National Institute of Allergy and Infectious Diseases, the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, Department of Health and Human Services)), and one did not list a funding source (Morita 2017). Between‐study variation in participant inclusion criteria, intervention type, and outcome definition limited the opportunity for meta‐analysis. For full details see the Characteristics of included studies tables.
Design and duration
The five included studies randomised 14,252 children to receive either an intervention or usual care. All studies were conducted in the Northern Hemisphere. The largest study randomised 12,179 children in a cluster‐randomised trial of a primary care‐based public health intervention (Julious 2016). Data were collected from August 2013 until the end of September 2014 from the Clinical Practice Research Datalink (CPRD), a computerised database of anonymised longitudinal medical records for primary care. The remaining studies were randomised controlled clinical trials employing a pharmacological intervention; three were blinded and one was an open study. Johnston 2007, Weiss 2010, and Morita 2017 studied interventions based upon LTRA administration from school return, whilst Teach 2015a compared administration of the anti‐IgE monoclonal omalizumab to a doubling of ICS dose or placebo initiated four to six weeks before school return. Three pharmacological studies recruited across multiple sites (Morita 2017; Teach 2015a; Weiss 2010), whilst in Johnston 2007 participation was at a single site. In Johnston 2007, 194 children were followed up for 45 days with no run‐in period. In Weiss 2010, 1162 children were followed up for 10 weeks after a 2‐ to 12‐week screening period. The 513 children in Teach 2015a received guideline‐based treatment to gain asthma control during a 4‐ to 9‐month run‐in period and were followed up until 90 days after school return. In Morita 2017, 204 children were enrolled and randomised two to six weeks before entering a 60‐day study period.
Inclusion and exclusion criteria
All studies referenced age and asthma diagnosis in their inclusion criteria. Julious 2016 included children aged 4 to 16 years with a coded diagnosis of asthma within their primary care record and a prescription for asthma medication within the last year. Four‐year‐old children were analysed separately since, whilst they are of school age in the United Kingdom, a diagnosis of asthma in this age group was judged to be more controversial than in older children. Children with neoplastic disease and those judged unsuitable for the intervention by their general practitioner were excluded. Johnston 2007 included children aged 2 to 14 years with doctor‐diagnosed asthma. Additional inclusion criteria were use of a reliever inhaler in the last year, school absence due to asthma in the last year or significant activity limitation, history of asthma exacerbations associated with respiratory viral infections, and ability to communicate in English. Children with significant cardiorespiratory comorbidity were excluded, as were those with an asthma exacerbation during the month before study inception and those using regular OCS or an LTRA. Weiss 2010 included children aged 6 to 14 years with a history of chronic asthma needing asthma medication in the six months preceding screening, at least one asthma exacerbation in the previous year in conjunction with a cold, and an alteration in environment differing from their typical school or education environment throughout August/September. Morita 2017 recruited 1‐ to 14‐year‐old children with physician‐diagnosed asthma, needing a rescue inhaler in the last year, and with a history of asthma exacerbations associated with apparent respiratory viral infections. Exclusion criteria were significant cardiorespiratory comorbidity, regular OCS use, or an asthma exacerbation in the month before the treatment period. Teach 2015a recruited children aged 6 to 17 years with an asthma diagnosis or symptoms for more than a year and at least one asthma exacerbation (requiring systemic corticosteroids or hospitalisation) within the prior 19 months. Additional inclusion criteria were positive perennial allergen skin test response, body weight and total serum IgE levels suitable for omalizumab, school attendance the following August or September, residence in a low‐income census tract, and insurance covering standard medications. There were no exclusions for this study beyond not meeting these inclusion criteria.
Baseline characteristics of participants
All five studies recruited more male than female participants: in each study 60% to 65% of participants were male. No study reported smoking status or exposure to environmental tobacco smoke. Only two studies reported baseline lung function: in Weiss 2010 mean forced expiratory volume in the first second of expiration (FEV1) was 89.8% predicted in the intervention group and 90.1% in the usual care group, and in Teach 2015a mean FEV1 across both groups at randomisation was 90.2% predicted. Only Teach 2015a systematically reported asthma severity: 195 randomised children were classified as step 5 according to a severity scale based on the National Heart, Lung and Blood Institute Expert Panel Report‐3 (severe persistent symptoms requiring high‐dose ICS and one adjunctive therapy), and 318 met the criteria for asthma severity steps 2 to 4 (mild‐moderate persistent symptoms requiring preventer medication but no more than medium‐dose ICS and one adjunctive therapy). Johnston 2007 reported that 90% of children were routinely receiving ICS, suggesting moderate severity, whilst only 30% of participants in Weiss 2010 and 50% in Morita 2017 routinely received ICS at randomisation. It is likely that the general practice‐based population in Julious 2016 included more people with mild asthma than the studies recruiting from secondary care.
Description of the intervention
The behavioural public health intervention was a letter sent to parents/carers of school‐aged children with asthma from the child's general practitioner reminding them to maintain their child’s medication and to collect a prescription if they were running low on medication. The letter was sent out during the week commencing 29 July and highlighted that school return is a time when asthma can worsen. The comparison group did not receive a letter (Julious 2016). In the pharmacological studies the interventions were added to usual care and compared with a placebo in addition to usual care. In Johnston 2007, an age‐specific dose of montelukast was given from 1 September to 15 October, whilst participants in Weiss 2010 received 5 mg montelukast from the night before the first day of school for eight weeks. Children in the intervention group in Morita 2017 received pranlukast 7 mg/kg twice daily between 15 September and 14 November. In Teach 2015a, children were randomised 3:3:1 to a standard dose of omalizumab based on serum IgE levels and weight, a doubling of their ICS dose, or placebo from 4 to 6 weeks before the start of the autumn term, continuing for 90 days after school return. Only children at steps 2 to 4 were entered into the ICS boost arm because of concerns that very high‐dose ICS provides limited additional efficacy and increases the risk of side effects.
Outcomes and analysis
Julious 2016 studied a number of outcomes, but the primary outcome was the proportion of children aged 5 to 16 years with unscheduled contacts during September 2013. Secondary outcomes measured in September included number of unscheduled contacts and proportion and total number of contacts (scheduled and unscheduled) and unscheduled contacts for a respiratory diagnosis. These outcomes were also measured throughout September to December 2013, September 2013 to August 2014, and in September 2014 in an 'echo study' to see if there was a maintained effect in the year following the main study and in which there was no study intervention. Between September 2013 and August 2014 time to first contact, first unscheduled contact, and first unscheduled contact for a respiratory diagnosis were also measured. The proportion of children with scheduled contacts was measured in August 2013, August 2014, and between August 2013 and July 2014. The number of participants collecting prescriptions was measured in August for both years. Quality‐adjusted life years (QALYs) gained and NHS health costs were measured between August 2013 and July 2014. Primary analyses were conducted on an intention‐to‐treat basis.
The primary outcome in Johnston 2007 was percentage of days during the intervention period with worsening asthma symptoms. Data were inputted daily by parents/carers into a prospectively completed sticker chart, and further data were collected by questionnaire two weeks after the end of the intervention period. The secondary outcome was number of unscheduled care visits. Analysis was intention‐to‐treat. In Weiss 2010, the primary outcome was percentage of days with worsening asthma symptoms, defined as one or more of increased beta‐agonist use, increased daytime symptoms score, night wakening, increased ICS use, OCS rescue or unanticipated visits to a doctor, emergency department, or hospital for asthma. Secondary outcomes were individual components of the composite primary endpoint and adverse events. Data were collected at 4, 8, and 10 weeks of the study and analysed in the full‐analysis population (all children who received at least one dose of study medication and had a valid measurement of the percentage of days with worsening asthma during the study period, derived from at least seven days of diary data). In Morita 2017, the primary outcome was total asthma score during the 60 study days, calculated based on asthma symptoms, need for medication, and need for an unscheduled physician visit or OCS. The secondary outcomes were days with worse asthma symptoms, number of colds, and days with fever. Data were analysed per protocol only from those compliant with treatment and returning adequate outcome data via a daily sticker chart. Teach 2015a conducted a modified intention‐to‐treat analysis, analysing data from children who were randomised, began study treatment, and had at least one study contact during the 90‐day outcome period. The primary outcome was asthma exacerbation, defined as worsening of asthma control requiring systemic corticosteroids or hospitalisation, during the 90‐day period from the first day of each child's school year. Secondary analyses considered exacerbations during the 90‐day intervention period according to subgroups based upon: exacerbation during run‐in, eosinophil count, total IgE, roach IgE, age, fractional exhaled nitric oxide (FeNO), FEV1, body mass index, ethnicity and gender. Interferon alpha responses to rhinovirus were measured in peripheral blood mononuclear cells from a subset of children.
Excluded studies
During screening of titles and abstracts, we excluded studies using a hierarchy of screening criteria. We asked first whether the study focused on asthma, followed by seasonal asthma exacerbations, and then considered whether the majority of the participants were school‐aged children, whether the paper focused on exacerbations at the beginning of the autumn school term, and compared an intervention to prevent these exacerbations to usual care. We excluded most studies due to no mention of seasonal asthma exacerbation or incorrect seasonal focus because the search terms picked up many studies of seasonal rhinitis in conjunction with asthma. Since a focus on asthma was the first stage in the screening hierarchy, this was also a common reason for exclusion. We excluded 22 records after viewing full texts, in most cases because the study did not focus on seasonal asthma exacerbations or did not present data from children. We excluded two studies because they did not employ an intervention specifically designed to reduce asthma exacerbations in children in autumn (Busse 2011; Gerald 2012), and two studies because they did not compare an intervention with usual care in which there is no systematic change in management in anticipation of children returning to school in the autumn (Prazma 2015; Yoshihara 2014); we prespecified both study designs as exclusionary in our protocol. We outlined details of reasons for exclusion of studies in the Characteristics of excluded studies section.
Risk of bias in included studies
Details of our 'Risk of bias' assessment for each included study and the reasoning behind our ratings can be found in the Characteristics of included studies section; a summary of 'Risk of bias' judgements by study and domain (selection bias, performance bias, detection bias, attrition bias, reporting bias, other bias) is presented in Figure 2. Most ratings in most domains for the included studies were low risk, with the exception of high risk of attrition bias in Morita 2017 as well as performance and detection bias due to lack of blinding. There was also unclear selection and performance bias in Julious 2016, unclear allocation bias in Weiss 2010 and Morita 2017, and unclear selective reporting bias in Johnston 2007.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
All of the included studies were described as randomised. Each study described random sequence generation in sufficient detail in their report or in response to contact from the review authors to warrant a rating of low risk of bias. All included studies used computer‐generated randomisation. However, information on allocation concealment was incomplete for Weiss 2010 and Morita 2017, so this was rated unclear. Due to the nature of the intervention it was not possible in the primary care study to blind participating practices or children (Julious 2016), which might have led to some performance bias since practices were able to choose not to send the letter to individual patients or not to send any letters at all. There may have been systematic bias in the children or practices excluded in this manner, so we rated this study as at high risk of bias. Almost a quarter of the intervention group did not receive the intervention as intended. In contrast, since a letter reminding parents to pick up asthma medications for their child did not form part of usual care, all of the control group received the control intervention (no letter) according to the protocol.
Blinding
Morita 2017 was an open, unblinded study and was therefore at high risk of performance and detection bias. We found no evidence of risk of bias related to blinding of children or observers in the other pharmacological studies. These three studies were described as double‐blind, and study authors described measures such as matched placebos to hide group allocation from children and study personnel. In the primary care study (Julious 2016), the risk of detection bias was low since outcome data were collected via the Clinical Practice Research Datalink and designated as "scheduled", "unscheduled", or "irrelevant" by an independent adjudication panel comprised of experienced general practitioners who were blinded to the treatment group. However, there may have been some performance bias if coding of medical contacts was influenced by general practitioners knowing whether or not their practice was sending reminder letters. For this reason we rated performance bias for this study as unclear.
Incomplete outcome data
Risk of bias due to high or unbalanced dropout was low across all studies except Morita 2017. There was 14% attrition from the pranlukast group after commencing the study medication and only 3% attrition from the placebo arm. All children in Johnston 2007 completed the study, and rates of treatment adherence and diary card completion documenting outcome data were high. In Teach 2015a, the primary analysis was modified intention‐to‐treat, restricted to children who were randomised, began study treatment, and had one or more study contact during the outcome period. A number of sensitivity analyses were presented including best‐ and worst‐case analyses and an analysis using multiple imputation of missing data. There was good retention and similar dropout rates and reasons between groups. Weiss 2010 also conducted a modified intention‐to‐treat primary analysis, including all children who received at least one dose of study medication and had a valid measurement of the percentage of days with worsening asthma during the study period, derived from at least seven days of diary data. There was no imputation of missing data, but dropout rates and reasons were similar between groups. In Julious 2016, withdrawal rates were similar in the intervention and control arms. The trialists felt imputation was not required since outcome data were missing only where practices changed their computer system to one that did not support data collection. This was assumed to be unrelated to treatment allocation, however rates of withdrawal were at least 25% in both groups.
Selective reporting
All named outcomes were reported in the published reports of Weiss 2010, Teach 2015a, and Julious 2016; we rated these studies as at low risk of bias. For Johnston 2007, it was unclear if all a priori defined outcomes were reported. The protocol submitted at trial registration stated that OCS use would be an outcome considered separately from unscheduled medical contacts. Medical contacts were reported as an outcome, but OCS use was not. Although it was reported that all prescriptions of OCS occurred as a consequence of an unscheduled visit to a doctor, it was not clear whether all visits resulted in OCS prescription.
Other potential sources of bias
We identified no other sources of bias in any included study.
Effects of interventions
See: Summary of findings for the main comparison Omalizumab compared to usual care for autumn asthma exacerbations in children; Summary of findings 2 A boost of inhaled corticosteroids compared to usual care for autumn asthma exacerbations in children; Summary of findings 3 Leukotriene receptor antagonist compared to usual care for autumn asthma exacerbations in children; Summary of findings 4 Behavioural intervention compared to usual care for autumn asthma exacerbations in children
Primary outcomes
Proportion of children experiencing one or more asthma exacerbations during the autumn period
Only Teach 2015a compared the number of children experiencing asthma exacerbations exactly as defined in the primary outcome of this review. Evidence relevant to this outcome is summarised in summary of findings Table for the main comparison and summary of findings Table 2. During the 90‐day period from the first day of each child’s school year, the omalizumab intervention was associated with exacerbation (worsening of asthma control requiring systemic corticosteroids or hospitalisation) in 11.3% of children compared with 21.0% in the placebo arm, odds ratio (OR) 0.48, 95% confidence interval (CI) 0.25 to 0.92 (adjusted for study centre, dosing schedule, and asthma severity step) (Analysis 1.1, Figure 3). Considering those with stage 5 asthma, omalizumab was associated with a reduced odds of exacerbation (OR 0.37, 95% CI 0.17 to 0.81). In contrast, considering only steps 2 to 4 where children were allocated to omalizumab, placebo, or a third arm of a doubling of ICS, exacerbation rates were experienced by 8.4%, 12.7%, and 11.1% of children, respectively. The odds of exacerbation did not differ significantly between any pair of groups (omalizumab versus placebo OR 0.63, 95% CI 0.22 to 1.78; omalizumab versus inhaled steroid boost OR 0.73, 95% CI 0.33 to 1.64; inhaled steroid boost versus placebo OR 0.86, 95% CI 0.32 to 2.30). However, when those experiencing a recent exacerbation (during the four‐ to nine‐month run‐in ending four to six weeks before school return) were considered separately from those without a recent exacerbation, reduced odds of exacerbation were seen across all severity steps 2 to 5 in the omalizumab group compared to placebo (OR 0.12, 95% CI 0.02 to 0.64) and compared to ICS boost across steps 2 to 4 (OR 0.05, 95% CI 0.003 to 0.98). For those without an exacerbation during run‐in, the odds of exacerbation were OR 0.88, 95% CI 0.35 to 2.18 compared to placebo across steps 2 to 5 and OR 1.34, 95% CI 0.56 to 3.25 compared to ICS boost across steps 2 to 4.
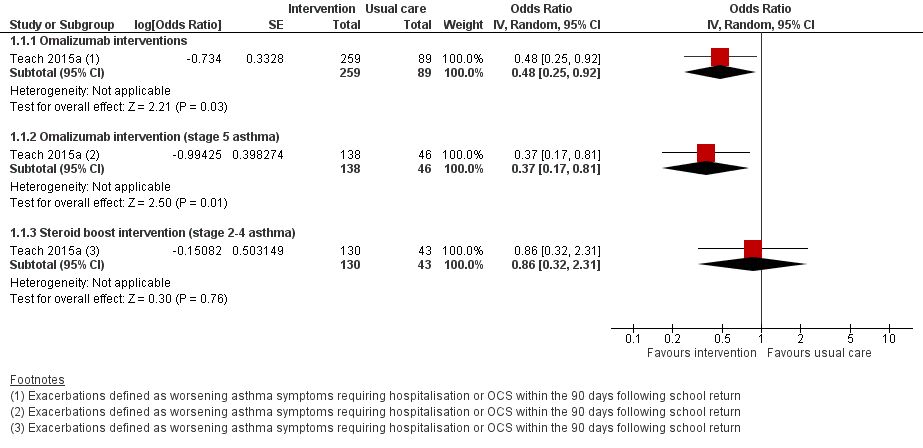
Forest plot of comparison: 1 Interventions for autumn exacerbations of asthma versus usual care, outcome: 1.1 Exacerbations defined according to the review's primary outcome.
Exacerbations reported according to alternative definitions
Johnston 2007 and Weiss 2010 considered the percentage of days with worsening asthma symptoms as the primary outcome, whilst Morita 2017 used a total asthma score based upon symptoms, medication need, and healthcare utilisation. These outcomes were not suitable for expression as an odds ratio. Johnston 2007 defined worsening asthma symptoms as symptoms that were worse than usual or needed extra asthma medication, or required an unscheduled visit to a doctor or treatment with oral corticosteroids; a 53% reduction in days with worsening asthma symptoms was reported compared with placebo during the 45‐day intervention (3.9% versus 8.3%, P = 0.02). Boys aged 2 to 5 years showed greater benefit from montelukast than did older boys, whereas among girls the treatment effect was most evident in 10‐ to 14‐year‐olds. The proportion of participants reporting one or more unscheduled visits to a doctor for asthma symptoms was markedly reduced in the montelukast group compared to the placebo group (4.1% versus 14.6%; OR 0.25, 95% CI 0.08 to 0.79), and it was reported that all prescriptions of OCS for asthma exacerbation occurred as a consequence of an unscheduled visit to a doctor. Weiss 2010 defined worsening asthma symptoms as one or more of the following actions: increased beta‐agonist use; increased daytime symptoms score; being awake 'all night' due to asthma; increased ICS use; OCS rescue; or unanticipated visits to a doctor, emergency department, or hospital for asthma. Analyses were adjusted for treatment, school start date, investigator site type, ICS use at entry, age, and sex. We found no significant difference in worsening symptoms between groups or for any component of this outcome, including OCS use (26.0% versus 30.3%; OR 0.79, 95% CI 0.59 to 1.06) and unanticipated medical contacts (11.8% versus 14.7%; OR 0.77, 95% CI 0.53 to 1.13). There was a consistent direction of effect favouring the intervention for five of the six outcomes, but none reached significance. Prespecified subgroup analyses found significantly fewer days of worsening symptoms in boys and in children aged 10 to 14 years, although interaction terms for age and gender were non‐significant. Morita 2017 based total asthma score on asthma symptoms, need for increased asthma medication, unscheduled physician visit or OCS; an adjustment was made in multivariable analysis for ICS use. There were no significant differences between pranlukast and control group in total asthma score (5.5 versus 7.8, P = 0.35) or days of worsening asthma symptoms (1.5 versus 1.8, P = 0.67). Significantly lower asthma scores and number of colds were seen for boys age one to five years. A higher number of colds and days of fever were seen in the control group compared to the pranlukast group, but only the latter reached significance (P = 0.06 and P = 0.04, respectively). Unscheduled visits to a doctor or OCS did not differ between groups (5.9% versus 8.6%; OR 0.67, 95% CI 0.16 to 2.80, Analysis 1.2, Figure 4). Evidence relevant to LTRA‐based interventions is summarised in summary of findings Table 3.

Forest plot of comparison: 1 Interventions for autumn exacerbations of asthma versus usual care, outcome: 1.2 Exacerbations defined according to study‐specific definitions.
In Julious 2016, exacerbations were not directly measured, but numbers of unscheduled contacts were reported as a proxy for this, and the study also reported unscheduled contacts coded with a respiratory diagnosis. Neither outcome significantly favoured the intervention. Data were reported between September and December rather than for the three months following school return; during September to December unscheduled contacts for a respiratory diagnosis were recorded for a greater proportion of children receiving the intervention letter than for those in the control group (18.4% versus 16.7%; OR 1.13, 95% CI 0.95 to 1.33), but this difference was not significant (summary of findings Table 4). Unscheduled contacts for any diagnosis also did not differ significantly between the intervention and usual care groups (80.1% versus 79.1%; OR 1.10, 95% CI 0.96 to 1.26). The primary outcome period for this study was September; during this period no significant between‐group differences were reported for the proportion of children for whom any medical contact or any unscheduled contact was recorded. Unscheduled contacts for a respiratory diagnosis were recorded in significantly higher numbers in the intervention than in the usual care arm (5.3% versus 4.2%; OR 1.30, 95% CI 1.03 to 1.66). Analyses were modelled using age, sex, number of contacts the previous September and the trial arm as fixed‐effect, and the design/cluster effect of general practice as random‐effects. The study authors suggested that contacts following the intervention might have occurred as a result of appointments needed to assess children's need for preventer medication.
Asthma exacerbations and the period during which children were considered at risk of exacerbation after school return were defined differently in each trial. Moreover, the interventions trialled rarely used the same approach or medication. For these reasons, we limited meta‐analysis to studies with comparable interventions based upon seasonal administration of montelukast. Even amongst these three trials, participant populations and outcomes varied slightly: in Johnston 2007 the intervention period was fixed for 45 days from 1 September, whilst in Weiss 2010 the intervention period was for eight weeks from the night before each child's school return, and in Morita 2017 children were randomised two to six weeks before a fixed 60‐day study period starting from 15 September. The participant populations in these trials differed according to both age and asthma severity: participants were both younger and more likely to be receiving ICS in Johnston 2007 and Morita 2017 than in Weiss 2010. Despite the higher proportion of children receiving ICS at trial outset in Johnston 2007 and Morita 2017, higher rates of oral steroid prescription occurred in Weiss 2010. It was not possible to assess the review's primary outcome in these studies since, although each separately reported OCS prescription and unscheduled medical contact, the proportion of children with an exacerbation needing hospitalisation or OCS was not reported. Where evidence was based on single studies, the quality was moderate, downgraded due to small numbers of participants randomised or use of an indirect outcome (unscheduled respiratory contacts in Julious 2016 rather than hospitalisation or oral steroid requirement). When results from Johnston 2007 and Weiss 2010 were included in a random‐effects model, the odds ratio for unscheduled medical contacts was 0.50, 95% CI 0.17 to 1.46. We judged the evidence to be of low quality due to poor consistency between studies and concerns about the indirect outcome of unscheduled medical contact, the threshold for which appeared to differ between studies. The I² statistic was 70%, so we deemed a fixed‐effect model to be inappropriate.
Secondary outcomes
Hospital and paediatric intensive care unit admissions and asthma‐related deaths
Although Johnston 2007, Weiss 2010, Teach 2015a, and Morita 2017 reported medical contact data, including hospital admission, no study presented data on hospitalisation or paediatric intensive care unit admission separately from total unscheduled contacts or OCS use. No study reported any asthma‐related deaths.
Asthma control, quality of life, and impact on schooling
No study reported asthma control measured by a standardised tool (e.g. Childhood Asthma Control Test (cACT) or Asthma Control Test (ACT)). Weiss 2010 mentioned increased symptom score, but the scale on which this was measured was not defined. We found no significant between‐group differences for this outcome. No study measured asthma‐related quality of life or absence from school (or employment for those beyond school age).
Adverse events
In the pharmacological studies, there was no evidence that either adverse events or serious adverse event rate differed between the intervention and the usual care group. Adverse events were not formally reported in the primary care intervention study (Julious 2016). Morita 2017 reported that no children discontinued study medication due to an adverse event, and the authors of this study confirmed that no adverse events occurred in either group. In Johnston 2007, minor adverse events occurred in 20.4% of children in the montelukast group and in 28.1% of children in the placebo group (OR 0.66, 95% CI 0.34 to 1.27) (summary of findings Table 3). Adverse events caused two children to discontinue the placebo: one child experienced behavioural change and the other tiredness and appetite changes. A significant behavioural disorder requiring emergency treatment was identified in a participant from the montelukast group at the follow‐up interview. No adverse events were described as serious. Teach 2015a reported adverse events during the period between randomisation and 30 days after the end of the intervention period. Of those children receiving at least one dose of the study drug, 54.5% in the omalizumab arm and 54.8% in the placebo arm experienced an adverse event (OR 0.99, 95% CI 0.61 to 1.58, Analysis 1.3, Figure 5) (summary of findings Table for the main comparison). Considering only children eligible for the ICS boost (steps 2 to 4), one or more adverse events were reported by 43.5% of children in the ICS boost arm and 53.3% of children in the placebo arm (OR 0.67, 95% CI 0.34 to 1.33). Two serious adverse events occurred: a seventh nerve palsy in the placebo group and an episode of anaphylaxis in the ICS boost arm (summary of findings Table 2). In Weiss 2010, 33.9% of children in the montelukast group and 33.6% of those in the placebo group reported at least one adverse event (OR 1.02, 95% CI 0.79 to 1.30) (summary of findings Table 3); the most common adverse events were upper respiratory tract disorders and infections. Four serious adverse events occurred in the intervention group and one in the placebo group (0.7% versus 0.2%). Consequently, there was no evidence in any study that total adverse events occurred more frequently in the intervention than in the usual care arm. Moreover, we found no evidence of a significant difference between these groups when data from the montelukast studies were pooled in a random‐effects model (OR 0.91, 95% CI 0.63 to 1.32; I² = 32%). However, significantly more children experienced local administration site reactions in the intervention group in Teach 2015a compared to the usual care group (15.3% versus 6.5%, P = 0.03). We graded the quality of the evidence for this outcome as high for the pooled montelukast data and moderate for omalizumab or steroid boost intervention, downgrading the evidence due to the imprecision inherent to low participant numbers.
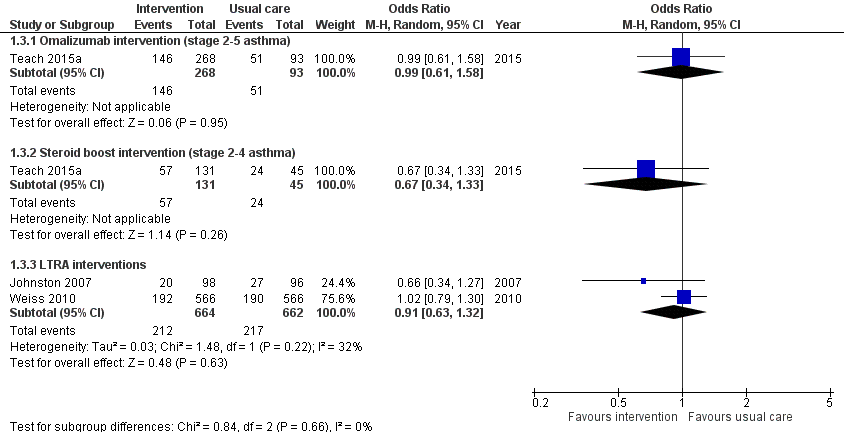
Forest plot of comparison: 1 Interventions for autumn exacerbations of asthma versus usual care, outcome: 1.3 Adverse effects.
Subgroup analyses
We had planned analyses separating studies of pharmacological interventions from studies of non‐pharmacological interventions, and to consider separately those with mild‐to‐moderate disease and those with severe asthma. Due to the low numbers of studies identified and the likely heterogeneity introduced by combining different pharmacological interventions, the planned subgroup analyses were not justified. We identified only one non‐pharmacological study, and baseline medication use and asthma severity were not always well described.
Sensitivity analyses
We had planned an analysis including only studies without missing data and an analysis excluding cluster‐randomised trials. Due to the low numbers of studies identified, these subgroup analyses were not possible.
Discussion
Summary of main results
Five randomised controlled trials met the inclusion criteria. Three were double‐blinded pharmacological studies; one was an open pharmacological study; and the remaining study was a cluster‐randomised trial of a public health intervention delivered in primary care. Three studies compared seasonal LTRA administration to a placebo, and one study compared seasonal omalizumab or an ICS boost to placebo. The primary care intervention was a letter sent to parents of children with asthma explaining the need to have adequate inhaled medication ready at the start of the autumn school term.
Two pharmacological studies reported a reduction in asthma exacerbations associated with the intervention. A 50% reduction (from 21% to 11.3%) in the proportion of children experiencing an exacerbation was found in allergen‐sensitised children with mild‐severe asthma and IgE > 30 IU/mL receiving omalizumab compared to placebo (Teach 2015a) (summary of findings Table for the main comparison). In subgroup analyses within this study, a reduction in exacerbation risk was demonstrated in children receiving treatment for severe asthma where there is little scope for additional therapy other than OCS and in those with a recent exacerbation. A 70% reduction (from 14.6% to 4.1%) was found in children with moderate‐severe asthma receiving montelukast (Johnston 2007). However, neither a second larger trial of montelukast (Weiss 2010), nor pooled data from both studies found evidence for a significant between‐group difference in the proportion of children experiencing exacerbations (summary of findings Table 3). Exacerbations requiring admission or a course of OCS were not reported in the primary care intervention study. However, there was no evidence that the proportion of participants who had at least one unscheduled medical contact between September and December differed between the intervention and the control group (Julious 2016) (summary of findings Table 4). Of the planned secondary outcomes, we could only assess adverse events and serious adverse events; there was no evidence of a significant difference between intervention and usual care groups for either of these outcomes.
Overall completeness and applicability of evidence
Due to the small number of studies identified and variation in their inclusion criteria, interventions, and outcomes, it was not possible to perform subgroup analysis or sensitivity analyses. Insufficient data for subgroup analyses prevented us from reaching conclusions about the relative efficacy of pharmacological and non‐pharmacological interventions or about efficacy according to asthma severity or other characteristics such as age or gender. Whilst all included studies reported asthma exacerbations or worsening of symptoms, none considered the burden associated with worsening asthma symptoms in terms of absence from education or employment or used a validated measure of asthma control or quality of life. Consideration of these important clinical outcomes would have increased the applicability for a clinical audience. Outcomes such as paediatric intensive care unit admission and asthma‐related death are rare and were not reported in the included studies. All included studies were conducted in the Northern Hemisphere. Inclusion of studies from the Southern Hemisphere would increase the generalisability of the results. Similarly, it may not be possible to generalise the findings of Teach 2015a beyond the largely minority, low‐income population in which this study was conducted or to children with asthma who are not allergen‐sensitised. Lack of clarity regarding the efficacy of strategies aiming to prevent autumn exacerbations is reflected in current guidelines. Whilst the Global Initiative for Asthma guidelines recognise the autumn season as a risk period for exacerbation, and seasonality of symptoms is mentioned in the British Thoracic Society/Scottish Intercollegiate Guidelines Network guideline for the management of asthma, current guidelines do not offer management advice to tackle this problem (BTS 2016; GINA 2017).
Quality of the evidence
The five included studies randomised 14,252 children to receive either an intervention designed to reduce asthma exacerbations in children during autumn after school return or to usual care. The largest study randomised 12,179 children, and the smallest 194. Children were predominantly school‐age, although two studies enrolled a small number of preschool‐aged children (Johnston 2007; Morita 2017). Because the interventions investigated differed between studies, inconsistencies between the studies' results might reflect the relative efficacy of the interventions. For example, greater efficacy of pharmacological than non‐pharmacological interventions might explain why the intervention was found to be superior to placebo in Johnston 2007 and Teach 2015a and also approached significance for many outcomes in Weiss 2010 and Morita 2017, but no outcome favoured the intervention in Julious 2016. However, asthma severity and exacerbations also varied between and within studies. Differences in rates of asthma exacerbations did not always reflect difference in baseline severity. For example, higher rates of OCS use were reported in the population studied by Weiss 2010 than in those studied by Johnston 2007 and Morita 2017, despite lower baseline severity in the former study. Worsening asthma symptoms, inclusion criteria, intervention period, and outcomes were not uniformly defined across studies. Weiss 2010, Julious 2016, and Morita 2017 included children with relatively mild asthma, and this might have limited the potential for the interventions in these studies to reduce exacerbation rates below an already low baseline. Moreover, as a consequence of using routinely collected data, the study by Julious 2016 was also limited by considerable uncertainty around the adjudication of some of the contacts as scheduled, unscheduled, or irrelevant.
We assessed the quality of the evidence in this review using GRADEpro software and have presented this information in 'Summary of findings' tables. Overall, the evidence for exacerbation outcomes ranged from low to moderate according to the nature of the intervention, whilst the quality of the adverse event data was moderate or high. We downgraded evidence due to the small number of studies included and hence wide confidence intervals. Moreover, interventions differed qualitatively between studies, and in some cases surrogate outcomes were reported.
When pooling data from the montelukast studies, we used inverse variance random‐effects modelling for the exacerbation outcome due to constraints in the extracted data. While we would have preferred Mantel‐Haenszel modelling for both models, since it provides better estimates for infrequent events, this was not possible to implement with Review Manager 5 and the data available.
Potential biases in the review process
We used standard Cochrane methodology to conduct this review. We performed extensive literature searches and did not limit study selection by language of publication. Two review authors independently screened published data and conference abstracts. Discrepancies were resolved through discussion or, if necessary, by consultation with a third review author. Given our use of a thorough search strategy, it is unlikely that the study selection process missed any available published studies. We recognise that the clinical problem of asthma exacerbations associated with school return is complex and that consistent terminology does not exist to describe this problem or interventions designed to prevent it. To mitigate against this problem, the search terms used included 'February', 'autumn' or 'fall' and 'seasonal' in addition to 'September'. Two review authors independently extracted study characteristics and numerical data. Any discrepancies were resolved through discussion or, if necessary, by consultation with a third review author. Similarly, two review authors independently made decisions about risk of bias, resolving any discrepancies through discussion or, if necessary, by consultation with a third review author. We also attempted to contact all study authors to obtain additional information about outcomes and to clarify study methods to ensure accurate 'Risk of bias' decisions. We received three detailed replies and additional data from one study author, while one author was unable to provide the requested information relating to risk of bias. Review authors reported no conflicts of interest.
Agreements and disagreements with other studies or reviews
We identified no other systematic reviews relating to this issue.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
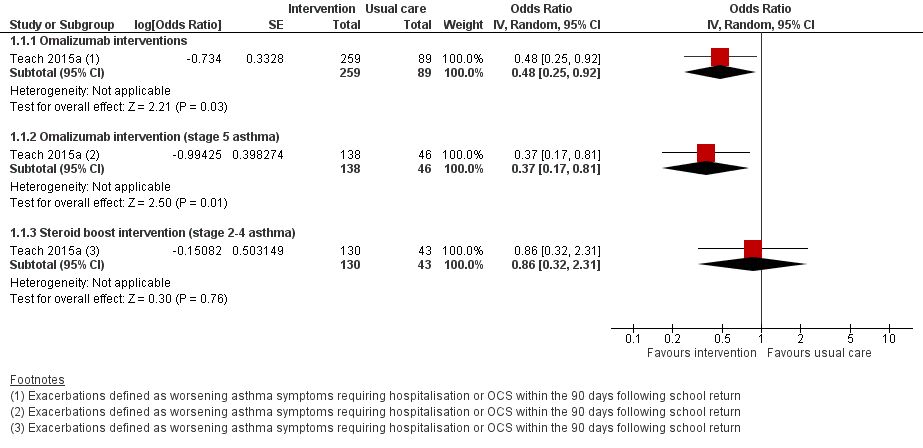
Forest plot of comparison: 1 Interventions for autumn exacerbations of asthma versus usual care, outcome: 1.1 Exacerbations defined according to the review's primary outcome.

Forest plot of comparison: 1 Interventions for autumn exacerbations of asthma versus usual care, outcome: 1.2 Exacerbations defined according to study‐specific definitions.
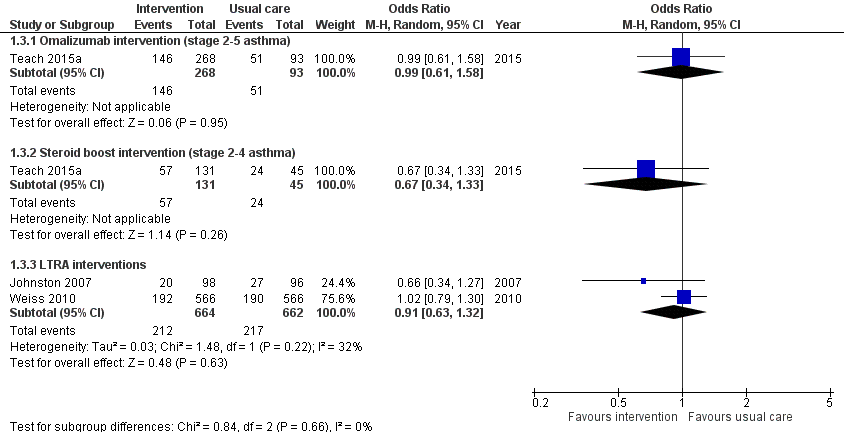
Forest plot of comparison: 1 Interventions for autumn exacerbations of asthma versus usual care, outcome: 1.3 Adverse effects.
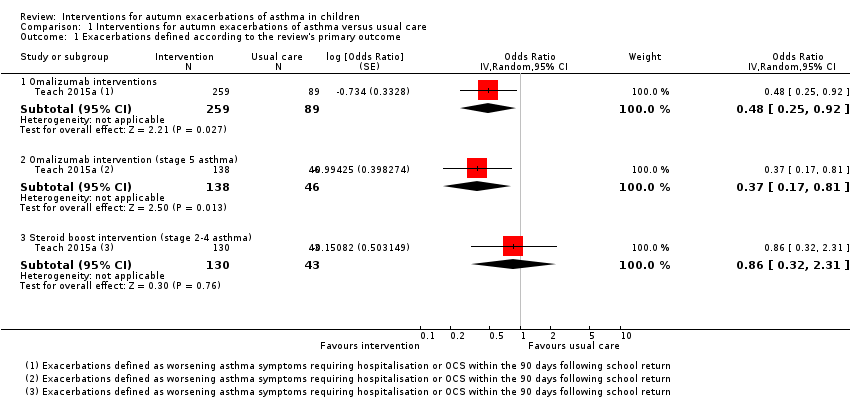
Comparison 1 Interventions for autumn exacerbations of asthma versus usual care, Outcome 1 Exacerbations defined according to the review's primary outcome.
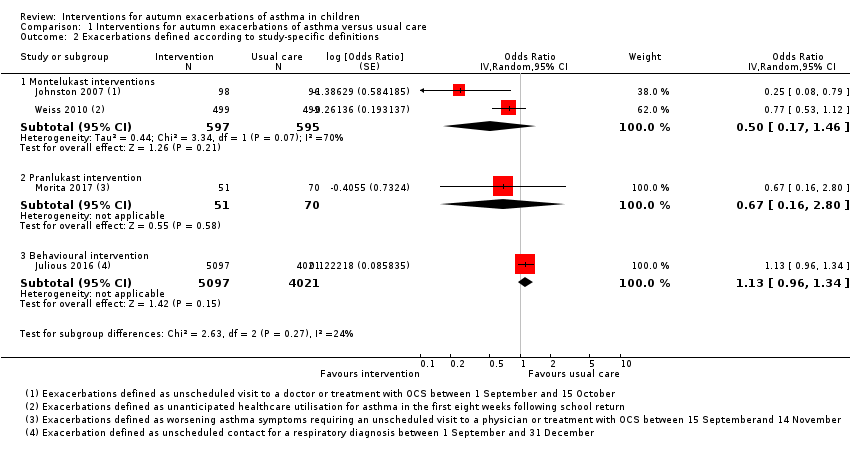
Comparison 1 Interventions for autumn exacerbations of asthma versus usual care, Outcome 2 Exacerbations defined according to study‐specific definitions.

Comparison 1 Interventions for autumn exacerbations of asthma versus usual care, Outcome 3 Adverse effects.
| Omalizumab compared to usual care for autumn asthma exacerbations in children | ||||||
| Patient or population: autumn asthma exacerbations in children Setting: community | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with usual care | Risk with omalizumab | |||||
| Exacerbations | 210 per 1000 | 113 per 1000 (62 to 197) | OR 0.48 (0.25 to 0.92) | 348 (1 RCT) | ⊕⊕⊕⊝ | Absolute effects calculated using control risk of 21.0% from Teach 2015a. |
| Exacerbations | 326 per 1000 | 152 per 1000 | OR 0.37 | 184 | ⊕⊕⊕⊝ | Absolute effects calculated using control risk of 32.6% from Teach 2015a. |
| Exacerbations | 127 per 1000 | 83 per 1000 | OR 0.63 | 164 | ⊕⊕⊕⊝ | Absolute effects calculated using control risk of 12.7% from Teach 2015a. |
| Adverse events | 548 per 1000 | 546 per 1000 | OR 0.99 | 361 | ⊕⊕⊕⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded once for imprecision because few children studied. | ||||||
| A boost of inhaled corticosteroids compared to usual care for autumn asthma exacerbations in children | ||||||
| Patient or population: autumn asthma exacerbations in children Setting: community | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with usual care | Risk with a boost of inhaled corticosteroids | |||||
| Exacerbations | 127 per 1000 | 111 per 1000 | OR 0.86 | 173 | ⊕⊕⊕⊝ | Absolute effects calculated using control risk of 12.7% from Teach 2015a. |
| Adverse events | 533 per 1000 | 434 per 1000 | OR 0.67 | 176 | ⊕⊕⊕⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded once for imprecision because few children studied. | ||||||
| Leukotriene receptor antagonist (LTRA) compared to usual care for autumn asthma exacerbations in children | ||||||
| Patient or population: autumn asthma exacerbations in children Setting: community | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with usual care | Risk with montelukast | |||||
| Exacerbations assessed with: oral corticosteroid or hospitalisation | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Exacerbations | 146 per 1000 | 79 per 1000 | OR 0.50 | 1326 | ⊕⊕⊝⊝ | Absolute effects calculated using control risk of 14.6% from Johnston 2007. |
| Adverse events | 328 per 1000 | 307 per 1000 | OR 0.91 | 1326 | ⊕⊕⊕⊕ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded once for inconsistency because asthma severity of children differed between included studies, and thresholds for medical contact or oral steroids appeared to differ between studies. | ||||||
| Behavioural intervention compared to usual care for autumn asthma exacerbations in children | ||||||
| Patient or population: autumn asthma exacerbations in children | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with usual care | Risk with behavioural intervention | |||||
| Exacerbations | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Exacerbations | 167 per 1000 | 185 per 1000 | OR 1.13 | 10,481 | ⊕⊕⊕⊝ | Absolute effects calculated using control rate of 16.7% from Julious 2016. |
| Adverse events | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded once for indirectness because studies contained no data on hospitalisation and need for oral steroids, so unscheduled contacts for a respiratory diagnosis used as a proxy outcome. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Exacerbations defined according to the review's primary outcome Show forest plot | 1 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Omalizumab interventions | 1 | 348 | Odds Ratio (Random, 95% CI) | 0.48 [0.25, 0.92] |
| 1.2 Omalizumab intervention (stage 5 asthma) | 1 | 184 | Odds Ratio (Random, 95% CI) | 0.37 [0.17, 0.81] |
| 1.3 Steroid boost intervention (stage 2‐4 asthma) | 1 | 173 | Odds Ratio (Random, 95% CI) | 0.86 [0.32, 2.31] |
| 2 Exacerbations defined according to study‐specific definitions Show forest plot | 4 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 2.1 Montelukast interventions | 2 | 1192 | Odds Ratio (Random, 95% CI) | 0.50 [0.17, 1.46] |
| 2.2 Pranlukast intervention | 1 | 121 | Odds Ratio (Random, 95% CI) | 0.67 [0.16, 2.80] |
| 2.3 Behavioural intervention | 1 | 9118 | Odds Ratio (Random, 95% CI) | 1.13 [0.96, 1.34] |
| 3 Adverse effects Show forest plot | 3 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Omalizumab intervention (stage 2‐5 asthma) | 1 | 361 | Odds Ratio (M‐H, Random, 95% CI) | 0.99 [0.61, 1.58] |
| 3.2 Steroid boost intervention (stage 2‐4 asthma) | 1 | 176 | Odds Ratio (M‐H, Random, 95% CI) | 0.67 [0.34, 1.33] |
| 3.3 LTRA interventions | 2 | 1326 | Odds Ratio (M‐H, Random, 95% CI) | 0.91 [0.63, 1.32] |

