Intervenciones para la prevención y el tratamiento de la enfermedad hepática avanzada en la fibrosis quística
Resumen
Antecedentes
La fibrosis quística es un defecto autosómico recesivo hereditario en el gen regulador de la conductancia transmembrana de la fibrosis quística (CFTR, por sus siglas en inglés) lo que resulta en la regulación anormal del movimiento de las sales y el agua a través de las membranas. En el hígado esta afección da lugar a fibrosis biliar focal que resulta en la hipertensión portal progresiva y a enfermedades hepáticas terminales en algunos individuos. Este trastorno puede ser asintomático, aunque puede dar lugar a esplenomegalia y hiperesplenismo, al desarrollo de várices y hemorragia de las várices y a ascitis; tiene un impacto negativo sobre el estado nutricional general y la función respiratoria en esta población. El pronóstico es deficiente una vez que se establece una hipertensión portal significativa. Actualmente no se ha identificado la función ni el resultado de diversas intervenciones para el tratamiento de las enfermedades hepáticas avanzadas (enfermedad no maligna en estadio final) en los pacientes con fibrosis quística.
Objetivos
Examinar y evaluar la eficacia de las opciones de tratamiento actualmente disponibles para la prevención y el tratamiento de las enfermedades hepáticas avanzadas en niños y adultos con fibrosis quística.
Métodos de búsqueda
Se realizaron búsquedas en el registro de ensayos del Grupo Cochrane de Fibrosis Quística y Enfermedades Genéticas (Cochrane Cystic Fibrosis and Genetic Disorders Group), compilado a partir de búsquedas en bases de datos electrónicas y búsquedas manuales en revistas y libros de resúmenes de congresos.
Fecha de la última búsqueda: 6 abril 2017.
También se hicieron búsquedas en las listas de referencias de artículos y revisiones relevantes y en los registros de ensayos en línea. Fecha de la última búsqueda: 4 enero 2017.
Criterios de selección
Cualquier ensayo controlado aleatorio publicado y no publicado y cualquier ensayo controlado cuasialeatorio de la enfermedad hepática avanzada en pacientes con fibrosis quística y cirrosis o insuficiencia hepática, hipertensión portal o hemorragia de las várices (o ambos).
Obtención y análisis de los datos
Los autores de la revisión examinaron de forma independiente títulos y resúmenes para identificar ensayos potencialmente relevantes, pero ninguno era elegible para su inclusión en esta revisión.
Resultados principales
Una búsqueda exhaustiva de la literatura no identificó ningún ensayo controlado aleatorio elegible publicado.
Conclusiones de los autores
Para desarrollar la mejor fuente de evidencia, se deben realizar ensayos controlados aleatorios de las intervenciones para la prevención y el tratamiento de las enfermedades hepáticas avanzadas en adultos y niños con fibrosis quística.
PICOs
Resumen en términos sencillos
Intervenciones para el tratamiento de la enfermedad hepática avanzada en la fibrosis quística
Pregunta de la revisión
Se procuró encontrar la mejor evidencia acerca de la prevención y el tratamiento de las enfermedades hepáticas avanzadas en adultos y niños con fibrosis quística mediante la comparación de diferentes opciones de tratamiento.
Antecedentes
En los pacientes con fibrosis quística y enfermedades hepáticas avanzadas, el tejido hepático normal es reemplazado por tejido cicatrizal. A medida que la enfermedad progresa, el hígado se vuelve duro y la sangre no puede fluir fácilmente a través del órgano, lo cual da lugar a una mayor presión en un vaso sanguíneo importante del hígado llamado vena portal (hipertensión portal). Más adelante, las venas de alrededor de la parte inferior del esófago se hinchan y desgarran, lo cual da lugar a una hemorragia potencialmente mortal (hemorragia de las várices). Hay varios tratamientos actualmente disponibles para la hemorragia de las várices y la hipertensión portal; tratamientos farmacológicos (betabloqueantes no selectivos), tratamiento endoscópico (p.ej. ligadura con banda en la que se colocan bandas elásticas muy pequeñas alrededor de las venas ampliadas para atarlas y que no puedan sangrar) o escleroterapia (en la que se inyecta una solución directamente en una vena que coagula la sangre e irrita el recubrimiento del vaso sanguíneo para que se hinche y se consolide). La inserción de una derivación portosistémica intrahepática transyugular (también conocida como TIPSS, por sus siglas en inglés) (un canal artificial dentro del hígado que permite el movimiento entre las venas por las que ingresa y egresa el flujo de sangre) ha sido empleada en la hemorragia recurrente o como un puente al trasplante hepático. Las derivaciones quirúrgicas portosistémicas también se han usado en los pacientes seleccionados con función hepática preservada. El trasplante hepático se realiza en los pacientes con fibrosis quística y cirrosis descompensada o enfermedades hepáticas terminales.
Las guías sobre la detección y el tratamiento de la hipertensión portal han estado disponibles para la población en general (sin fibrosis quística). Sin embargo, todavía no se ha definido el tratamiento óptimo para las enfermedades hepáticas avanzadas en la fibrosis quística, lo cual da lugar a una variedad amplia de prácticas entre diferentes centros.
Fecha de la búsqueda
La evidencia está actualizada hasta: 4 enero de 2017.
Características de los estudios
Se realizaron búsquedas de ensayos de alta calidad que comparaban los tratamientos descritos anteriormente en niños y adultos con enfermedades hepáticas avanzadas y fibrosis quística. Lamentablemente, no se encontró ningún ensayo para incluir en esta revisión.
Resultados clave
Debido a que no se encontró ningún ensayo para esta revisión, no es posible realizar recomendaciones específicas ni formular guías sobre la mejor práctica en este estadio. La revisión destacó una necesidad clara de ensayos controlados aleatorios de los tratamientos para la prevención y el tratamiento de las enfermedades hepáticas avanzadas en adultos y niños con fibrosis quística.
Authors' conclusions
Background
A subject‐specific glossary and a statistical glossary are available in the appendices (Appendix 1; Appendix 2).
Description of the condition
Cystic fibrosis (CF) is a life‐limiting autosomal recessive disorder caused by mutations in the CF transmembranes conductance regulator (CFTR) gene on chromosome 7, which is expressed on epithelial cells. It is a multi‐organ disease primarily affecting the lungs, pancreas, sweat glands, reproductive tract (Wolffian ducts in males), gastro‐intestinal tract and liver (Davis 2006). The incidence of CF varies between Asia, Europe and the USA. In Asia, while the condition is severely under‐diagnosed, its prevalence is rare. The incidence of CF is 1 in 2000 to 3000 newborns in the European countries; 1 in every 3500 births in the USA (WHO 2015). Further, a mean prevalence of CF was 0.737 per 10,000 people in some of the countries in the European Union, 0.797 per 10,000 in the USA, and 2.98 per 10,000 in the Republic of Ireland (Farrell 2008). The mortality data for the white population in the USA from 1999 to 2006 was 3708 people (CDC 2010).
Cystic fibrosis‐associated liver disease (CFLD) is an early complication of CF which occurs mostly in the first decade of life, particularly in people with a history of meconium ileus or pancreatic insufficiency and severe (class I to III) mutations (Colombo 2002; Nagel 1989). Advanced liver disease presents mainly during pre‐puberty and puberty with a median age at diagnosis of 12 years (Lindblad 1999). The incidence rate (number of new cases per year) of CFLD is 1.8% (Colombo 2002).
With increased life expectancy, CFLD has emerged as a significant cause for morbidity and mortality (Simmonds 2008) and evidence of clinically significant liver disease is found in around 25% of people with CF. Between 3% and 5% develop pulmonary hypertension (PHT) due to severe cirrhosis during the first decade of life, with a median age of diagnosis of 10 to 11 years of age; 90% of those affected are diagnosed before 20 years of age (Bartlett 2009; Debray 1999; Gooding 2005). A prevalence rate for CFLD of 41% at 12 years of age has been reported (Lamireau 2004). CFLD may progress to chronic obstructive cholangiopathy, focal biliary cirrhosis and multilobular cirrhosis with associated PHT with or without variceal bleeding and end‐stage liver disease. Cirrhosis and PHT can negatively impact on respiratory function due to organomegaly (abnormal enlargement of organs), ascites and intra‐pulmonary shunting (Smith 2004). PHT is an increase in the blood pressure within a system of veins called the portal venous system. Clinically significant PHT is defined as a hepatic venous pressure gradient of 10 mm Hg or more (Bari 2012). Most people with CFLD are asymptomatic. Approximately 10% of people with CFLD and PHT progress to advanced liver disease (Rowland 2011). Liver failure may occur subsequently (Melzi 2006).
Diagnosis of CFLD should be made when at least two of the following variables are present (Debray 2011):
-
abnormal physical examination: a palpable liver edge more than 2 cm below the bottom edge of the rib cage on the mid‐clavicular line and a prominent left lobe palpable in the epigastrium, confirmed by ultrasound;
-
abnormal liver function tests: an increase in transaminases (aspartate aminotransferase (AST) and alanine aminotransferase (ALT)) and gamma‐glutamyl transpeptidase (GGT) levels above the upper normal limits on at least three consecutive occasions over 12 months, after other causes of liver disease;
-
ultrasonographic evidence of liver involvement (an increased parenchymal echogenicity, irregular margins, nodularity) or PHT (splenomegaly, increased think ness of lesser omentum, spontaneous spleno‐renal anastomosis, large collateral veins, ascites) or biliary abnormalities (bile duct dilatation);
-
a liver biopsy may be indicated if there is diagnostic doubt.
There is a developing role for transient elastography (also known as Fibroscan®) for investigating CFLD, despite the absence of adequate validation against histology and other long‐term outcomes such as PHT, bleeding risk, cirrhosis, synthetic failure and transplantation (Ledder 2014). This method is widely used to stage liver fibrosis as an alternative to a liver biopsy; it measures liver stiffness, and it is also a valuable tool to detect and quantify CFLD in children and adults with CFLD (Ledder 2014; Malbrunot‐Wagner 2011; Menten 2010; Sadler 2015; Witters 2009). Liver stiffness is an accurate non‐invasive indicator in assessing the progression of liver disease in people with CF (Kitson 2013).
Description of the intervention
The principle of managing PHT in people with CFLD is not dissimilar to its management in those without CFLD.
In adults with evidence of PHT and the presence of varices, non‐selective beta‐blockers (NSBB) should be considered to prevent or reduce the number of bleeding events (Cheng 2005). The two most commonly used NSBB for preventing bleeding are propranolol and nadolol. Their dose is titrated to achieve the resting heart rate of 55 beats per minute or a reduction of heart rate by 25% from baseline, and adjusted to maximal tolerated doses. Propranolol is usually started at a dose of 20 mg twice daily and nadolol at a daily dose of 40 mg (Garcia‐Tsao 2007). However, in people with CF with a broncho‐constrictive element to their lung disease, NSBB may be contraindicated. Some studies in children suggest a possible benefit with few side effects, but there are no control data from these studies (Shashidhar 1999).
In adults and children with acute bleeding varices, the preferred initial intervention is upper gastro‐intestinal endoscopy with band ligation or sclerotherapy (Brigman 2006; Debray 1999; Efrati 2003; Price 1996; Stringer 1993). Endoscopic therapies have no effect on either portal flow or resistance (Garcia‐Tsao 2007). Endoscopic variceal band ligation is indicated as the primary variceal prophylaxis as well as the preferred therapy for variceal haemorrhage (Gluud 2012) and a single‐ or multi‐band ligator may be used (Wong 2000). Endoscopic variceal band ligation is very effective with a high success rate in both acute variceal bleeding episodes as well as for primary prophylaxis (Funakoshi 2012; Mileti 2011). Band ligation must be repeated periodically until the varices have been ablated (Gooding 2005). During sclerotherapy, a chemically irritating compound (ethanolamine or tetradecyl sulphate) is injected into (intravariceal) or adjacent to (paravariceal) a varix to control active bleeding or for variceal decompression (Gugig 2012; Kahan 1989). Sclerotherapy has been shown to be inferior to band ligation and is recommended only in specific cases, such as very young children, in whom banding is not possible (due to size of gastroscope and banding device) (Brigman 2006). Sclerotherapy is no longer used in the secondary prophylaxis of variceal haemorrhage in adults.
A balloon tamponade (Sengstaken Tube) is indicated only in cases of massive variceal bleeding in the absence, or failure, of definitive endoscopic treatment.
In a small number of individuals, for example those with severe PHT and refractory variceal haemorrhage in whom therapeutic endoscopy treatment has failed, a transjugular intrahepatic porto‐systemic stent shunt (TIPSS) should be considered either as a long‐term treatment option or as a bridge to transplant (Brigman 2006). An interventional radiologist generally inserts the TIPSS; a catheter is placed into the jugular vein and advanced into the hepatic vein, where a needle is used to form a tract between the left portal vein and the right hepatic vein. This tract is expanded with a balloon angioplasty catheter and a stent is then placed, forming a permanent porto‐systemic (PS) shunt (Efrati 2003; Gugig 2012). The diameter of the stent is generally between 8 mm and 10 mm.
Surgical PS shunting could be considered in selected individuals with preserved liver function and without severe respiratory disease or deterioration (Debray 1999; Efrati 2003). This procedure is indicated for large varices at a high risk of bleeding and failure to respond to a banding programme (Ledder 2014). For individuals with non‐cirrhotic PHT, in particular with extrahepatic portal vein thrombosis, PS shunt surgery represents the only effective therapy to prevent recurrent bleeding and repeated endoscopies for many years. Non‐selective shunts (mesocaval, portocaval), selective shunts (distal spleno‐renal) and intermediate shunts may be used (Gugig 2012).
Liver transplantation is the treatment of choice for decompensated or end‐stage CFLD or uncontrollable variceal bleeding despite an intensive therapeutic endoscopic programme (Cox 1987; Kobelska‐Dubiel 2014; Mack 1995; Noble‐Jamieson 1996). Whole‐liver, reduced‐liver or split‐liver transplant techniques are used (Melzi 2006).
How the intervention might work
Treatment with NSBB lowers cardiac output and causes vasoconstriction in the gastrointestinal tract, thereby reducing portal and collateral blood flow in the abdomen. However, this treatment is reserved for selected individuals only and should be avoided in those with CFLD who have a broncho‐constrictive element to their respiratory disease. These agents have been shown to prevent bleeding in more than 50% of people with medium or large varices (Garcia‐Tsao 2007).
Individuals undergoing variceal band ligation will have endoscopy sessions at regular intervals until the varices are ablated. In children this will generally be carried out under general anaesthesia and consequently, if frequent endoscopy sessions are required, may potentially have a negative impact on respiratory function.
A TIPSS places a stent between the intrahepatic portions of the portal vein and the hepatic vein and leads to a reduction of portal venous pressure and thus a reduction of pressure in oesophageal and gastric varices, preventing further variceal haemorrhage; it is reported to successfully control active and potentially life‐threatening variceal bleeding in more than 90% of cases. This technique is associated with low complication rates, but major risks include TIPSS dysfunction with stenosis, occlusion or thrombosis and new‐onset or worsened encephalopathy. In the long term, regular radiographic examination (ultrasound scans or TIPSS venogram, or both) are necessary to ensure that the TIPSS is functioning correctly and not suffering from blockages (Pozler 2003).
Surgical PS shunting aims to divert portal blood flow and as such decrease portal pressure leading to a reduced risk of bleeding (Ledder 2014). Surgical PS shunting improves hypersplenism without deteriorating liver function or encephalopathy (Wolff 2003). The non‐selective shunts, communicate with the entire portal system and have been associated with higher rates of hepatic encephalopathy compared with the selective shunts. The distal spleno‐renal shunt is a selective shunt which connects the distal end of the splenic vein to the left renal vein with interruption of all collateral vessels (e.g. coronary vein and gastroepiploic veins). In effect it separates the portal venous circulation into a decompressed gastrosplenic venous circuit (thus reducing the pressure on gastric and oesophageal varices) and a high‐pressure superior mesenteric venous system that continues to perfuse the liver. Liver function is preserved by a distal spleno‐renal shunt which is associated with a lower incidence of portal systemic encephalopathy (D’Amico 1995). Potential complications include onset or worsening of hepatic encephalopathy, shunt thrombosis or occlusion (Debray 1999; Efrati 2003). Hepatic encephalopathy is the most common adverse event developed after treatment with PS shunting for PHT (Flass 2013).
Liver transplantation is indicated in people with CFLD with progressive hepatic dysfunction, development of ascites and jaundice, intractable variceal bleeding, hepato‐pulmonary and porto‐pulmonary syndrome, severe malnutrition unresponsive to intensive nutritional support, deteriorating quality of life (QoL) related to liver disease or deteriorating pulmonary function or both (Debray 2011; Fridell 2003; Ikegami 2008; Melzi 2006; Nash 2008). Based on these factors, two scoring systems are currently available to evaluate the need for liver transplantation in adults with CFLD (Milkiewicz 2012; Noble‐Jamieson 1996). No such specific scoring systems exist for children. Liver transplantation in this group does not improve long‐term nutritional status, but short‐term improvement in pulmonary function after liver transplantation has been reported. Some of the initial improvement in lung function may reflect the resolution of the effects of severe PHT such as pulmonary oedema, intrapulmonary shunting ascites and organomegaly, in addition to reduced infection resulting from improved immune function, particularly neutrophil function (Dowman 2012). One further study showed there is improvement in QoL after liver transplantation (Moyer 2009).
Why it is important to do this review
Evidence‐based guidelines from the European and American Board of Gastroenterology recommend screening for and treating large varices in adults with severe PHT without a history of variceal bleeding (Shneider 2012). They suggest the use of NSBB as a first‐step therapy in adults with grade two or grade three varices, band ligation if beta‐blockers are contra‐indicated or have failed (secondary prophylaxis), and the placement of a TIPSS in cases of ligation failure (tertiary prophylaxis) (De Franchis 2005). In contrast, there is a paucity of data to recommend specific approaches for the management of PHT in children; and extrapolation of care models for adults to children may not be appropriate (Shneider 2012).
There are currently no clear recommendations for treating advanced liver disease in people with CF (Debray 2011). Furthermore, for people with CFLD, no specific recommendations exist with respect to the prevention and treatment of variceal haemorrhage. In addition, because of their lung disease, the use of beta‐blockers is usually contra‐indicated. Regular screening or therapeutic endoscopies may require general anaesthesia (particularly when carried out in children) and may lead to a reduction in lung function or predisposition to infection.
Objectives
To assess the various treatment options for preventing and managing advanced liver disease in children and adults with CFLD.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) and quasi‐RCTs.
Types of participants
Children and adults of all ages and either gender, diagnosed with CFLD with cirrhosis or liver failure, PHT or variceal bleeding (or both).
Types of interventions
We planned to evaluate the effects of the following comparisons.
-
Pharmacological interventions (e.g. NSBB) for any duration compared to placebo or no intervention
-
Endoscopic interventions (e.g. band ligation, sclerotherapy) compared to active control
-
TIPSS compared to active control
-
Surgical interventions (e.g. surgical PS shunt, liver transplantation) compared to active control
Types of outcome measures
Primary outcomes
-
Change in variceal bleeding and portal pressure
-
development of first bleeding episode (primary prevention)
-
re‐bleeding following endoscopic treatment (secondary prevention)
-
-
Adverse effects
-
of non‐surgical interventions (e.g. aggravated congestive cardiac failure, respiratory distress, hypotension from non‐selective beta‐blockers, stenosis, occlusion, thrombosis, worsened encephalopathy after TIPSS, perforation of oesophagus, oesophageal ulceration, oesophageal stricture after sclerotherapy)
-
of surgical interventions (e.g. thrombosis, occlusion, onset or worsening of encephalopathy, infection, rejection)
-
Secondary outcomes
-
Nutritional status
-
body mass index (BMI) calculated as weight (kg)/height² (m)
-
standard deviation (SD) score (z score) for weight (zW)
-
SD score (z score) for height (zH)
-
-
Respiratory outcomes
-
forced expiratory volume in one second (FEV₁)
-
forced vital capacity (FVC)
-
SD score (z scores ) for FEV₁/FVC ratio
-
-
Quality of life (QoL) as measured by a validated scoring system, e.g. Cystic Fibrosis Questionnaire Revised (CFQ‐R) (Quittner 2009)
-
Need for liver transplantation
-
Mortality (bleeding‐related mortality, all‐cause mortality)
Search methods for identification of studies
There will be no restrictions regarding language or publication status.
Electronic searches
We attempted to identify relevant trials from the Cystic Fibrosis and Genetic Disorders Group's Cystic Fibrosis Trials Register using the search term: liver.
The Cystic Fibrosis Trials Register is compiled from electronic searches of the Cochrane Central Register of Controlled Trials (CENTRAL) (updated each new issue of the Cochrane Library), weekly searches of MEDLINE,a search of Embase to 1995 and the prospective handsearching of two journals ‐ Pediatric Pulmonology and the Journal of Cystic Fibrosis. Unpublished work is identified by searching the abstract books of three major cystic fibrosis conferences: the International Cystic Fibrosis Conference; the European Cystic Fibrosis Conference and the North American Cystic Fibrosis Conference. For full details of all searching activities for the register, please see the relevant section of the Cochrane Cystic Fibrosis and Genetic Disorders Group's website.
Date of the last search: 06 April 2017.
We also searched the following trial registries for the latest clinical investigations and treatment in order to identify unpublished studies, ongoing studies and potential relevant trials. Searched terms can be found in Appendix 3.
-
ClinicalTrials.gov (https://clinicaltrials.gov)
-
metaRegister of Current Controlled Trials (mRCT) (www.controlled‐trials.com/mrct/)
-
World Health Organisation International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/en/)
Date of last search: 04 January 2017.
Data collection and analysis
Selection of studies
Two review authors aimed to independently check the titles and abstracts identified from the searches. However, no eligible RCTs were found. For future updates, the authors will adhere to the protocol described below.
Two review authors (SK and AWT) will independently assess all the potentially relevant trials obtained from the Information Specialist as well as from the handsearches undertaken by the authors. If there is disagreement between two authors, the third review author (NNT) will arbitrate and the three authors will discuss and finalise the selection of trials. The authors will select the trials if they meet the inclusion criteria, regardless of publication status (published, unpublished, in press and in progress). They will also include trials recorded and published in languages other than English. The authors will record details of any excluded trials together with the reasons for exclusion (Higgins 2011a).
Data extraction and management
Two review authors (SK and SM) will independently extract and record the data from included trials using standardised data extraction forms; one review author (SK) will prepare the forms based on the checklist for data collection described in theCochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). The data extraction form will include trial characteristics, such as trial design, participants, interventions, primary and secondary outcome measures and the analysis performed in original trials. If there are differences in the data extracted by the first two review authors, a third review author (SM) will check these and arbitrate. If there are insufficient or missing data, the authors will contact the corresponding trial investigators for additional information. One of the review authors (SK) will enter data into the Review Manager (RevMan) software for analysis, which another review author (IVM) will check (RevMan 2014).
We will analyse surgical and non‐surgical interventions separately.
Assessment of risk of bias in included studies
Two review authors (SK and SM) will independently assess the risk of bias for each included trial using the criteria outlined in theCochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). If there is disagreement, the third author (NNT) will be involved and the three authors will discuss until they achieve consensus. The authors will use Cochrane's tool to assess risk of bias in the included studies with regard to: random sequence generation; blinding of participants, personnel, and outcome assessors; completeness of outcome data for each main outcome; selective outcome reporting; and other sources of bias. The authors will grade studies using judgements of 'low risk', 'high risk' or 'unclear risk' of bias according to the specific criteria for each domain. They will record all judgements in the 'Risk of bias' tables together with the characteristics of each included trial and will also prepare the 'Risk of bias' summary figure. The authors will contact the trial investigators for details of the procedures involved in the conduct of trials and will keep their replies as evidence.
Measures of treatment effect
Dichotomous data
The review authors will use the Mantel‐Haenszel risk ratio (RR) with 95% confidence intervals (CI) for dichotomous outcome data (such as number of active variceal bleeding, stenosis, occlusion, thrombosis, worsened encephalopathy and mortality). They will further calculate the number needed to treat (NNT) for dichotomous outcomes to reflect the number of participants necessary to obtain a beneficial or harmful outcome with the intervention.
Continuous data
The review authors will use the fixed‐effect mean differences (MD) with 95% CI for continuous data variables (such as biochemical investigation results, measurements from ultrasound, measurements from hepatic scintigraphy, QoL, nutritional status, respiratory outcomes) provided the same scales are used to measure the outcomes in all the included trials. If trials assess the same outcome, but measure it in different ways, then the authors will use the standardised mean difference (SMD) as a summary statistic in meta‐analysis. If this is the case, they will prefer to report the MD based on change from baseline over the MD based on absolute values (Deeks 2011).
Unit of analysis issues
For dichotomous data, the participant will be the unit of analysis. For continuous data, the authors will use MD which will be the average change from baseline and not the absolute mean. For outcomes that may occur more than once, such as active variceal bleeding, the review authors will analyse count data as continuous data to prevent any unit of analysis errors. They will not include any cross‐over trials or cluster‐randomised trials. For trials with two treatment arms of different interventions, the review authors will analyse the outcomes for each arm separately.
Dealing with missing data
If data are missing the review authors will contact trial investigators or sponsors in order to verify key trial characteristics and obtain any missing numerical outcome data whenever possible. If this is not possible and if they assume that these data are 'missing at random', they will perform an available case analysis (i.e. ignoring the missing data) and discuss the impact of missing data on our results. When the review authors assume that the missing outcome data are 'not missing at random', they will conduct an intention‐to‐treat (ITT) analysis by imputing the missing data with replacement values, and treating these as if they were observed (e.g. last observation carried forward, imputing an assumed outcome such as assuming all were poor outcomes, imputing the mean, imputing based on predicted values from a regression analysis). The review authors also plan to perform a sensitivity analysis to assess the impact of any unknown status or assumptions made about missing data on participants who withdrew from trials on the overall pooled result of the meta‐analysis (Higgins 2011d).
Assessment of heterogeneity
The review authors plan to assess heterogeneity between the included trials by checking for overlap of horizontal lines representing each trial on the forest plot and the Chi² test, with a 10% level of significance. They will use the I² statistic to measure the percentage of inconsistency in results due to inter‐trial variability in each analysis. In line with guidance in the Cochrane Handbook for Systematic Reviews of Interventions, the review authors will consider I² values from 0% to 40% to be not important; values from 30% to 60% as moderate heterogeneity; values from 50% to 90% as substantial heterogeneity; and values over 75% as considerable heterogeneity (Deeks 2011). If they find I² values over 50% (considered as substantial heterogeneity), they will explore it by pre‐specified subgroup analyses (see below).
Assessment of reporting biases
The review authors plan to use funnel plots to assess reporting biases if the meta‐analysis includes 10 or more trials (Sterne 2011). They will also attempt to trace the original protocol of the trial and compare the sample size; they will check that outcomes listed in the methods in the protocol appear in the final reports.
Data synthesis
The review authors will analyse any relevant data using RevMan (RevMan 2014). For the pooling of outcomes, the review authors will use a fixed‐effect model if the I² statistic is homogeneous (i.e. I² is under 50%). They will apply a random‐effects model for data synthesis when they identify substantial heterogeneity (I² at least 50%) which can not be explained by subgroup analyses.
Subgroup analysis and investigation of heterogeneity
If the review authors identify significant heterogeneity (i.e. I² greater than 50%), they will conduct the following subgroup analyses for each group of interventions.
Pharmalogical therapy
-
Children with CFLD (aged up to 18 years) versus adults with CFLD (aged over 18 years)
-
Different types of NSBB
-
Different doses of NSBB
-
Short‐term therapy (less than six months) versus long‐term therapy (six months and over)
Endoscopic therapy
-
Children with CFLD (aged up to 18 years) versus adults with CFLD (aged over 18 years)
-
Banding versus sclerotherapy
TIPSS
-
Children with CFLD (aged up to 18 years) versus adults with CFLD (aged over 18 years)
Surgical therapy
-
Children with CFLD (aged up to 18 years) versus adults with CFLD (aged over 18 years)
-
PS shunts (selective or nonselective or partial) versus liver transplantation
Sensitivity analysis
The review authors will perform a sensitivity analysis by repeating the meta‐analysis after exclusion of trials with an overall high risk of bias and those with unclear methodological data from the overall analysis.
They also plan to perform a sensitivity analysis to assess the impact of any unknown status or assumptions made about missing data on participants who withdrew from trials on the overall pooled result of the meta‐analysis (Higgins 2011d).
Summary of findings table
For future updates, the authors will create a 'Summary of findings' table for each comparison presented using the methods and recommendations described in chapter 11 of theCochrane Handbook for Systematic Reviews of Interventions (Higgins 2011c) and using GRADEpro software for overall grading of the quality of the evidence (Deeks 2011).
In the summary of the finding tables, the review authors will report change in variceal bleeding (first bleeding episode and re‐bleeding) and portal pressure after various interventions such as pharmacotherapy, endoscopy and surgical interventions, which included the development of first bleeding episode and re‐bleeding following endoscopic treatment.
They will also report the adverse effects after the interventions as detailed in the outcome measures above.
Lastly, they will report the all‐cause mortality and QoL in the summary of findings tables.
Results
Description of studies
Results of the search
No RCTs were identified in the comprehensive searches undertaken for this review (Figure 1).
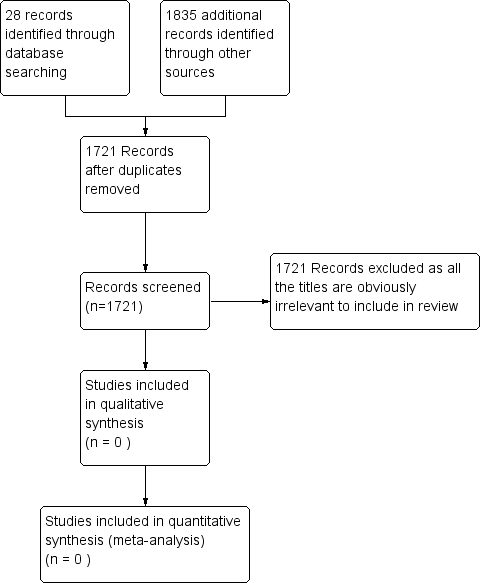
Figure 1 PRISMA study flow diagram
Included studies
The authors did not identify any trials which were eligible for inclusion in this review.
Excluded studies
We identified 25 potentially relevant trials, all of which were excluded after checking the abstracts or full text as these trials did not meet with the eligible criteria for inclusion in our review. Out of the 25 trials, nine were excluded as they were not RCTs. A further 16 trials were excluded as they did not examine the types of interventions we planned to evaluate.The reasons for exclusion of studies are described in the table of 'Characteristics of excluded studies'.
Risk of bias in included studies
No trials met the inclusion criteria; therefore, there were no trials for which risk of bias could be assessed in this review.
Effects of interventions
There are no trials eligible for inclusion in this review.
Discussion
No randomised controlled trials (RCTs) were identified which met the inclusion criteria for this review.
Agreements and disagreements with other studies or reviews
A relatively common, serious complication in cystic fibrosis‐related liver disease (CFLD) is portal hypertension and consequent acute bleeding of oesophageal varices. Cirrhosis and cholangiocarcinoma, while rare, are probably more serious. Studies related to preventing and managing of acute variceal bleeding secondary to portal hypertension in people with CFLD are scarce. We identified only some small retrospective studies on the management of CFLD. Clear guidelines and recommendations for treatment based on high‐level evidence for the management of this population are currently not available.
Pharmacological interventions
The efficacy and safety of non‐selective beta blockers (NSBB) in preventing variceal bleeding has not been evaluated in people with cystic fibrosis (CF) because of their potential adverse effects on pulmonary disease. Moreover, the repeated general anaesthesia required for screening of therapeutic endoscopic procedures may also reduce lung function and predispose to infection unless managed with intravenous antibiotics and vigorous physiotherapy (Debray 2011). A few small studies and case series have shown no effects of NSBB in children with decompensated portal hypertension. (Ozsoylu 1985; Ozsoylu 2000; Shashidhar 1999).
Endoscopic interventions
Sclerotherapy
Prophylactic sclerotherapy is not beneficial in CF because it carries a risk of bleeding during or following the procedure (D’Amico 1995). The preferred initial intervention for bleeding varices is oesophagogastroduodenoscopy with injection sclerotherapy or band ligation (Brigman 2006; Debray 1999; Efrati 2003; Price 1996; Stringer 1993). Injection sclerotherapy is associated with an 86% success rate without significant morbidity in people with CF (D’Amico 1995; Stringer 1993).
Band ligation
Endoscopic variceal band ligation is the treatment of choice for primary variceal prophylaxis (Funakoshi 2012; Mileti 2011). Band ligation is also the preferred approach for secondary variceal prophylaxis (Flass 2013), especially in older children and adults (Brigman 2006). This method can also be used to manage the difficult variceal bleeding in people with CF (Garcia‐Tsao 2007). However, band ligation can also carry a risk of bleeding both during and following the procedure which may result in repeated general anaesthesia with increased morbidity in people with CF.
Transjugular intrahepatic porto‐systemic stent shunt (TIPSS)
Use of TIPSS may be reserved for individuals with variceal haemorrhage refractory to sclerotherapy. It can also be used on an emergency basis in individuals who are actively bleeding, or in those who exhibit rapid progression to liver failure (Debray 1999). Both as a long‐term therapy for portal hypertension and as a bridge for liver transplantation, TIPSS can effectively control variceal bleeding (Brigman 2006); indeed, TIPSS controls active variceal bleeding in more than 90% of cases. Shunt stenosis is the principal limiting factor of TIPSS. The technique and complications in children are comparable to those in adults.
Surgical porto‐systemic (PS) shunt
A surgical PS shunt may also be reserved for refractory cases as a secondary measure. Partial splenectomy with splenorenal shunt was reported to have a favourable outcome in 15 of 19 individuals with CF with portal hypertension, with the improvement in liver function and portal hypertensive symptoms, significantly delaying or obviating the need for liver transplantation (Louis 2007). Surgical PS shunting can permanently reduce portal pressure and relieve portal hypertension in those without progressive liver and lung failure (Debray 1999; Efrati 2003). Surgical PS shunting has been used to preserve liver function, but carries the risk of acute liver failure and hepatic encephalopathy (Debray 2011); it offers a prolonged alternative treatment for refractory bleeding (Efrati 2003).
Liver transplantation
The established indications for liver transplant in CF include cirrhosis with evidence for hepatic decompensation or uncontrollable variceal bleeding. Some retrospective reviews have shown that there was a significant survival advantage in both adults and children with CF cirrhosis receiving liver transplant compared to those with cirrhosis who did not receive a transplant (Lu 2010; Mendizabal 2011).
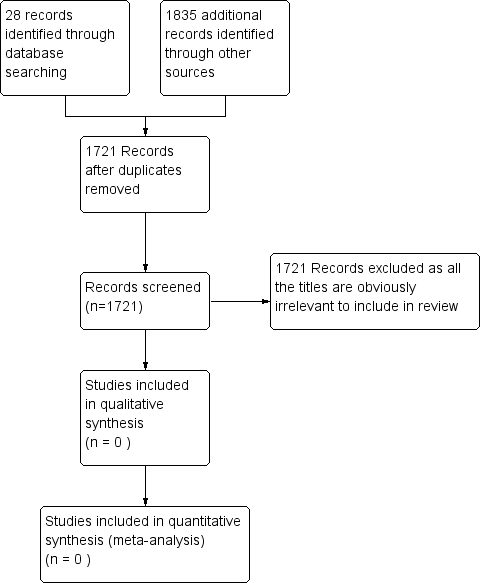
Figure 1 PRISMA study flow diagram

