Return‐to‐work coordination programmes for improving return to work in workers on sick leave
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Design: RCT, parallel, 2 arms Country: Denmark Sample size: 119 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: April 2004 to April 2005 Method of recruitment: 4 participating municipalities, invitation to an information meeting Follow‐up: 3, 6, 12 months | |
| Participants | Health problem: low back pain, neck pain, musculoskeletal disorders Age in years: mean 43.7 (SD 11.3) Female in %: 55 Intervention group: 68 participants Control group: 51 participants Inclusion criteria: absent from work 4‐12 weeks, aged 18‐65 years, understanding and speaking Danish, reimbursement request indicating low back pain or musculoskeletal disorders as the main cause of sick leave Exclusion criteria: mental health disorders, alcohol or drug addiction, pregnancy, quit their job or had been fired before randomisation Duration and type of sick leave: 1‐3 months, mean 39.3 days (SD 20.9); full sick leave Type of sick leave compensation: employer paid according to public sickness benefit scheme | |
| Interventions | Intervention: coordinated and tailored work rehabilitation Components of intervention:
Team: occupational physician, occupational physiotherapist, chiropractor, psychologist, social worker Involvement of the employer: yes Providers of intervention: rehabilitation team, experience and training not reported Theoretical basis: Canadian multidisciplinary work rehabilitation programme (i.e. the Sherbrooke model, Loisel 2002) Duration: maximum 3 months Control: conventional case management as provided by the municipality; same information about the study and the same (follow‐up) questionnaires, no additional assessment or action | |
| Outcomes | Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
| |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation without stratification |
| Allocation concealment (selection bias) | Low risk | Concealed (author information) |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) | Low risk | Blind for return‐to‐work outcomes Not blind for patient‐reported outcomes |
| Incomplete outcome data (attrition bias) | Low risk | 6 participants withdrew their consent after randomisation; for the rest complete data on return‐to‐work outcomes, 33% loss to follow‐up on patient‐related outcomes, non‐response analysis: “A non‐response analysis revealed that nonrespondents in both groups and at both time points were more likely to be men. Moreover, in the CTWR [coordinated and tailored work rehabilitation] group, non‐respondents at 3 month follow‐up tended to have less vocationally education and more sickness absence hours. Otherwise, non‐respondents in both groups did not differ significantly from respondents with respect to other sociodemographic, health status, and work absence variables tested at 3 and 12 months follow‐up.” (p. 86) |
| Selective reporting (reporting bias) | Unclear risk | No study protocol published, “pain intensity last week” was considered to be less relevant and was not reported (author information) |
| Other bias | Low risk | No indications of other sources of bias |
| Methods | Design: RCT, parallel, 2 arms Country: Scotland, North‐East England Sample size: 50 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: not reported Method of recruitment: the 4 participating insurance companies identified potential clients from the personal injury claims files, invitation by letter Follow‐up: 6, 12 months (after 6 months: intervention for both groups, therefore only 6 months follow‐up data analysed) | |
| Participants | Health problem: injuries likely to result in absence from work of 6 months or more Age in years: mean 39.4, range 18‐61 Female in %: 18 Intervention group: 33 participants Control group: 17 participants Inclusion criteria: residents in Scotland or North‐East England, aged 16‐65 years, in the labour market at the time of injury, injuries likely to result in absences from work ≥ 6 months and/or permanent disability Exclusion criteria: people with catastrophic injuries Duration and type sick leave: median 20 months, mean 21 months, range 3‐50 months; full sick leave Type of sick leave compensation: personal injury insurance (private insurance) | |
| Interventions | Intervention: rehabilitation coordinator service Components of intervention:
Team: physiotherapist, psychologist, consultant in rehabilitation medicine, occupational therapist Involvement of the employer: no Providers of intervention: a physiotherapist as coordinator with experience in care coordination, 3‐month induction programme Theoretical basis: Chamberlain 1991, Thornicroft 1991 Duration: 6 months Control: no restrictions; the intervention group received help for 12 months, beginning immediately after the initial assessment, while the control group had no contact with the coordinator for 6 months, then received help for 6 months between their 6 and 12 month reassessments | |
| Outcomes | Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
| |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Concealed in sequentially numbered, sealed, opaque envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) | Low risk | Blind for return‐to‐work outcomes Not blind for patient‐reported outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No losses to follow‐up, complete data at 6 months |
| Selective reporting (reporting bias) | Unclear risk | Unclear, insufficient information |
| Other bias | Low risk | No indications of other sources of bias |
| Methods | Design: RCT, parallel, 2 arms Country: Belgium Sample size: 710 in 60 clusters Unit of allocation: cluster Unit of analysis: individuals Date of recruitment: October 1996 to June 1997 Method of recruitment: patients of all medical advisors of Christian Sickness Fund who introduced a claim for benefits after surgery for disc herniation Follow‐up: 6, 12 months | |
| Participants | Health problem: surgery for disc herniation Age in years: mean 39.2 Female in %: 35 Intervention group: 345 participants (30 medical advisors) Control group: 365 participants (30 medical advisors) Inclusion criteria: absent from work before surgery < 1 year, aged 15‐64 years, worker Exclusion criteria: self‐employment Duration and type of sick leave: 2‐2.5 months; full sick leave Type of sick leave compensation: a claim for benefits after surgery for disc herniation | |
| Interventions | Intervention: new guideline for medical advisers Components of intervention: intervention guidelines for the medical adviser:
Team: general practitioner, social insurance agent, social insurance physician, other healthcare personnel (not reported) Involvement of the employer: no Providers of intervention: 30 medical advisers (social insurance physicians), experience and training not reported Theoretical basis: a number of rehabilitation guidelines Duration: as long as participant is on disability benefit Control: medical practice as in the past; focus on corporal damage, few rehabilitation efforts | |
| Outcomes | Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement): none Outcomes not analysed (measurement): none | |
| Notes | Each medical advisor was responsible for a specific region, baseline characteristics of medical advisors not reported (unit of randomisation) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | No concealment of allocation reported (usually not relevant in cluster randomised trials, as all clusters are randomised at once) |
| Blinding of participants and personnel (performance bias) | High risk | No blinding, but participants were probably not aware of the intervention, case mangers were not blind |
| Blinding of outcome assessment (detection bias) | High risk | Not blind for return‐to‐work outcomes Unclear if blind for patient related outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No losses to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No protocol published |
| Other bias | Low risk | No indications of other sources of bias, recruitment‐bias implausible: participants were blind during recruitment process, no analysis of cluster effect reported |
| Methods | Design: RCT, parallel, 2 arms Country: USA Sample size: 205 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: July 1999 to December 2000 Method of recruitment: invitation by letter from the medical director of the Office of Worker's Compensation Programs Follow‐up: 4, 10, 16 months | |
| Participants | Health problem: work‐related upper extremity disorder Age in years: mean 46 (SD 8.6) Female in %: 78 Intervention group: initial number of participants not reported; 58 participants answered the patient satisfaction questionnaire Control group: initial number of participants not reported; 73 participants answered the patient satisfaction questionnaire Inclusion criteria: aged 18‐65 years, accepted single worker's compensation claim according to work‐related upper extremity disorder, no claims in the previous 2 years, claims adjudicated and accepted as work‐related within 90 days of filing (only those still out of work or on modified duty at the time of claim adjudication were eligible) Exclusion criteria: none Duration and type of sick leave: 1‐6 months; full‐ and part‐time sick leave Type of sick leave compensation: claims of the US Department of Labor's Office of Worker's Compensation Programs | |
| Interventions | Intervention: integrated case management Components of intervention:
Team: “e.g. supervisor, injury compensation specialist, medical providers, claims examiner” (p. 383 Shaw 2001) Involvement of the employer: yes Providers of intervention: 32 nurse case managers: 2 years experience providing case management service, 2‐day training in ergonomic assessment and workplace accommodations, problem‐solving approach, experience in coordination of medical care Theoretical basis: Shaw 2001 Duration: 4 months, variable Control: usual practice; 33 nurse case managers, focus on medical care, no training in a structured protocol | |
| Outcomes | Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
| |
| Notes | Return‐to‐work data was not published, but provided by one of the authors | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “[P]articipants were randomly assigned” (p. 805) |
| Allocation concealment (selection bias) | High risk | No concealed allocation (author information) |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) | High risk | Probably not blind for return‐to‐work outcomes Probably not blind for patient related outcomes |
| Incomplete outcome data (attrition bias) | High risk | 40% losses to follow‐up for return‐to‐work outcomes, 36%‐61% losses to follow‐up for patient‐reported outcomes (author information) |
| Selective reporting (reporting bias) | High risk | Return‐to‐work outcomes not published, one author provided outcomes as far as possible |
| Other bias | Low risk | No indications of other sources of bias |
| Methods | Design: RCT, parallel, 2 arms with 2 subgroups Subgroups: those with influence on the planning of their own work and no perceived risk of losing job and/or being a work injury claimant; those without influence on the planning of their own work or feeling at risk of losing job and not a work injury claimant Country: Denmark Sample size: 351 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: November 2004 to June 2007 Method of recruitment: referred by their general practitioner, recruited at the Spine Center Follow‐up: 12, 24 months | |
| Participants | Health problem: low back pain Age in years: mean 42.0 (SD 10.5) Female in %: 52 Intervention group: 176 participants Control group: 175 participants Inclusion criteria: absent from work for 3‐16 weeks, aged 16‐60 years, ability to read and speak Danish Exclusion criteria: unemployed, continuing or progressive symptoms indicating plans for surgery, surgery in the spine within the past 12 months, diagnosis of specific back disease (e.g. tumour), diagnosis of primary psychiatric disease, pregnancy, known substance abuse Duration and type of sick leave: range 3‐16 weeks; full‐ and part‐time sick leave Type of sick leave compensation: municipalities, financed by tax payers | |
| Interventions | Intervention: multidisciplinary intervention (same as Stapelfeldt 2011) Components of intervention:
Team: specialist of social medicine, a rheumatologist, a physiotherapist, a social worker, and an occupational therapist Involvement of the employer: yes Providers of intervention: 3 case managers; experience and training not reported Theoretical basis: Canadian multidisciplinary work rehabilitation programme (i.e. the Sheerbrooke model, Loisel 2002) Duration: median 18 weeks Control: municipality case management and brief intervention:
Same control group interventions as Stapelfeldt 2011 and Myhre 2014 (without municipality case management) | |
| Outcomes | Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
| |
| Notes | The proportion at work at end of the follow‐up was reported to 'last job' or 'modified job or training'; we analysed the proportion returned to last job followed by a sensitivity analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated block‐randomisation |
| Allocation concealment (selection bias) | Low risk | Allocation was carried out by a secretary |
| Blinding of participants and personnel (performance bias) | High risk | Blinding was not possible; only the first clinical examination was carried out double‐blind |
| Blinding of outcome assessment (detection bias) | Low risk | Author information |
| Incomplete outcome data (attrition bias) | Low risk | Complete data for return‐to‐work outcomes; for patient‐reported outcomes 39% losses to follow‐up after 12 months |
| Selective reporting (reporting bias) | Low risk | Study protocol published; all outcomes reported; after 24 months no reporting of patient‐reported outcomes |
| Other bias | Low risk | No indications of other sources of bias |
| Methods | Design: RCT, parallel, 2 arms Country: Netherlands Sample size: 134 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: November 2005 to April 2007 Method of recruitment: in each hospital a competent hospital employee identified the source population weekly from the computerised patient record system, invitation by mail Follow‐up: 3, 6, 12 months | |
| Participants | Health problem: non‐specific chronic low back pain Age in years: mean 46.2 (SD 9.1) Female in %: 42 Intervention group: 66 participants Control group: 68 participants Inclusion criteria: aged 18‐65 years, low back pain > 12 weeks, visited an outpatient clinic in one of the participating hospitals, absent or partially absent from work, paid employment or self‐employed (> 8 hours/week) Exclusion criteria: absent from work > 2 years, temporarily work for an employment agency without detachment, lumbar spine surgery in the past 6 weeks or surgery or invasive examinations within 3 months, serious psychiatric or cardiovascular illness, specific low back pain (due to infection, tumour, osteoporosis, rheumatoid arthritis, fracture or inflammatory process), pregnancy Duration and type of sick leave: mean 22 weeks; full‐ and part‐time sick leave Type of sick leave compensation: employer is responsible for 2 years (is obliged to have a company insurance) | |
| Interventions | Intervention: integrated care Components of intervention:
Team: clinical occupational physician, patients occupational physician, general practitioner, medical specialist, occupational therapist, physiotherapist Involvement of the employer: yes Providers of intervention: 2 case managers (occupational physicians), 2 days training programme Theoretical basis: not reported Duration: 67 calender days (SD 32) Control: usual practice; guidance from health professionals, average 0.2 visits to case managers | |
| Outcomes | Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
| |
| Notes | EQ‐5D scores by author information | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random‐sequence table |
| Allocation concealment (selection bias) | Low risk | Opaque, sequentially numbered, and sealed coded envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) | Low risk | Blind for return‐to‐work outcomes Not blind for patient‐reported outcomes |
| Incomplete outcome data (attrition bias) | Low risk | 13% losses to follow‐up for return‐to‐work outcomes, 7% losses to follow‐up for patient‐reported outcomes, missing outcome data balanced in numbers across groups, with similar reasons for missing outcome data and plausible effect size among missing data (assuming a smaller effect in same direction) not enough to introduce clinically relevant bias) |
| Selective reporting (reporting bias) | Low risk | Study protocol published, all outcomes reported |
| Other bias | Low risk | No indications of other sources of bias |
| Methods | Design: RCT, parallel, 2 arms with 2 subgroups Subgroups: Swedes; immigrants Country: Sweden Sample size: 611 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: not reported Method of recruitment: 7 social insurance offices in Gotenburg reported cases reaching a continuous sick leave of 90 days; invitation by letter Follow‐up: 3 months intervals up to 60 months | |
| Participants | Health problem: non‐specific chronic musculoskeletal pain Age in years: mean 39.5, range 20‐55 Female in %: 62 Intervention group: 351 participants Control group: 296 participants Inclusion criteria: absent from work < 180 days sick listed in the preceding 2 years, age < 56 years Exclusion criteria: ongoing rehabilitation, partial sick leave, pregnancy Duration and type of sick leave: 3 months or more; full sick leave Type of sick leave compensation: sick benefit through the Swedish social insurance system | |
| Interventions | Intervention: multidisciplinary rehabilitation programme Components of intervention: outpatient regime with:
Team: rehabilitation physician, nurse, physical therapist, psychotherapist, psychologist, occupational therapist, social worker, vocational counsellor Involvement of the employer: no Providers of intervention: rehabilitation team, experience and training not reported Theoretical basis: not reported Duration: individually Control: usual practice; physical therapy and other rehabilitation measures | |
| Outcomes | Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement): none Outcomes not analysed (measurement): none | |
| Notes | No information about attrition after randomisation Contradicting information, whether time point 0 in the graph corresponds to time of randomisation or sick listing (we assumed randomisation) Contradicting information between figures and text Since follow‐up was much longer than in other studies, we analysed the data on the 24 months follow‐up and conducted a sensitivity analysis using 60 months outcome. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No method reported |
| Allocation concealment (selection bias) | Unclear risk | No concealment reported |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) | Low risk | Blind for return‐to‐work outcomes |
| Incomplete outcome data (attrition bias) | High risk | High level of attrition directly after randomisation: 77 (24%) in the intervention group returned to work between randomisation and first visit; to correct for possible selection bias a similar proportion in the control group was randomly excluded A further 80 patients never received the study intervention because of their doctor's refusal (n = 24), other rehabilitation (n = 38), withdraw (n = 11) or other (n = 7); these 80 patients were included in the analysis (intention‐to‐treat), it seems plausible that further patients were lost to follow‐up after the intervention started |
| Selective reporting (reporting bias) | Low risk | Results presented in subgroups (Swedes and immigrants), we extracted return‐to‐work rates from graphs and recombined subgroups |
| Other bias | Unclear risk | Unclear |
| Methods | Design: RCT, parallel, 2 arms Country: Norway Sample size: 405 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: August 2009 to August 2011 Method of recruitment: patients referred for diagnostic consideration or multidisciplinary treatment of neck and/or back pain were screened for eligibility at their first consultation at the outpatient clinic Follow‐up: 4, 12 months | |
| Participants | Health problem: neck pain (10%) and low back pain (90%) Age in years: mean 40.59 (SD 9.86) Female in %: 46 Intervention group: 203 participants Control group: 202 participants Inclusion criteria: absent from work 4‐52 weeks, employed or self‐employed Exclusion criteria: need for surgical treatment, cauda equina syndrome, symptomatic spinal deformities, osteoporosis with fractures, inflammatory rheumatic diseases, pregnancy, legal labour disputes, insufficient Norwegian language skills, cardiac/pulmonary/metabolic disease with functional restrictions, mental disorders. Duration and type of sick leave: mean 112 days (IQR 71‐182); full‐ and part‐time sick leave Type of sick leave compensation: sickness benefits, a work assessment allowance pension, or a disability pension from the Norwegian Labour and Welfare Administration | |
| Interventions | Intervention: work‐focused intervention Components of intervention:
Team: physician, physical therapist, case worker, medical specialist, group discussions, lecturer Involvement of the employer: yes Providers of intervention: caseworkers, experience and training not reported Theoretical basis: not reported Duration: 3 weeks Control: usual practice:
| |
| Outcomes | Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
| |
| Notes | Secondary outcomes from Marchand 2015; authors provided additional outcome data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “An independent statistician generated a random block sequence stratified by hospital.” (p. 2001) |
| Allocation concealment (selection bias) | Low risk | Concealed (author information) |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) | Low risk | Blind for return‐to‐work outcomes Not blind for patient‐reported outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No losses to follow‐up for return‐to‐work outcomes, 26% losses to follow‐up for patient‐reported outcomes “Patients lost to follow‐up at 12 months had higher baseline disability scores (mean difference 3.60, p = 0.018), reported higher baseline pain (mean difference 0.52, p = 0.039) and higher baseline FABQ‐P scores (mean difference 1.57, p =0.015). There were also a significantly higher number of men, smokers, patients with a foreign mother tongue, and patients with low education in patients lost to follow‐up. The response rate was 74% at the 12‐month follow‐up. There were a similar number of patients lost to follow‐up in both groups” (Marchand 2015; p. 5) |
| Selective reporting (reporting bias) | Unclear risk | No protocol published |
| Other bias | Low risk | No indications of other sources of bias |
| Methods | Design: RCT, parallel, 4 arms Country: United Kingdom Sample size: 1423 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: April 2003 for 2 years Method of recruitment: potential clients spoke with the central telephone contact centre, brief explanation of the trial, check for eligibility Follow‐up: 20‐36 weeks | |
| Participants | Health problem: any condition likely to result in a 50% chance to return to work (musculoskeletal, mental and behavioural problems, injuries) Age in years: mean 44.0 Female in %: 57 Intervention group: 571 (weighted: 713 participants) Control group: 458 (weighted: 710 participants) Inclusion criteria: absent from work 6‐26 weeks, employed/self‐employed and working for > 16 hours/week, living and working within one of the pilot areas Exclusion criteria: not be within 18 weeks of planned retirement Duration and type of sick leave: 1.5‐6 months; full sick leave Type of sick leave compensation: 30.4% incapacity benefit, rest unclear | |
| Interventions | Intervention: job retention and rehabilitation Components of intervention:
Team: psychologist, psychotherapist, physical therapist, podiatrists, chiropractors, osteopaths, dieticians Involvement of the employer: yes Providers of intervention: case managers, experience and training not reported Theoretical basis: not reported Duration: 20 to 36 weeks Control: usual practice; no systematic aid, low levels of work support | |
| Outcomes | Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
| |
| Notes | Authors presented data only for the weighted numbers of patients: “These unequal numbers per group inevitably leads to some concerns that the randomisation groups may not be strictly balanced: to address this a thorough non‐response analysis has been carried out and the data has been weighted to help minimise any non‐response bias.” (p. 2) Return to work was reported for at least 2 weeks, 6 weeks or 13 weeks: due to the limited follow‐up of 20‐36 weeks, we disregarded the 13 weeks outcome which most participants probably could not achieve in this timeframe; to ensure the longest follow‐up, we used the data for the 2 weeks outcome and conducted sensitivity analyses using 6 and 13 weeks outcome | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Concealed |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) | High risk | Outcome survey for return‐to‐work outcomes with risk of recall in both groups Not blind for patient‐reported outcomes |
| Incomplete outcome data (attrition bias) | High risk | High rates of non‐response (20% intervention group, 35% control group) |
| Selective reporting (reporting bias) | Unclear risk | No protocol published |
| Other bias | High risk | Low compliance (88% received return‐to‐work‐plan, 72% of those followed the plan), probably bias through weighting: “The weighting strategy could have introduced bias into the impact estimates. A comparison . . . showed that . . . the estimates have not been affected substantially. We conclude that the weighting has not distorted the measurement of the impact in a way that adversely affects the comparison of the randomisation groups or the interpretation of the estimates.” (p. 142) |
| Methods | Design: RCT, parallel, 2 arms Country: Canada Sample size: 110 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: June 1995 to December 1996 Method of recruitment: invitation by letter and by telephone to all consecutive cases eligible for inclusion in the computer system of Quebec Worker's Compensation Board in Montreal office Follow‐up: 3, 6 months | |
| Participants | Health problem: any work‐related injury to the middle or lower vertebral column, not surgery or multiple injuries Age in years: mean 37.6 (SD 10.1) Female in %: 28 Intervention group: 54 participants Control group: 56 participants Inclusion criteria: absent from work 4‐8 weeks from the date of filing a claim, compensation for any work‐related injury to the thoracic, lumbar, and/or sacral portions of the vertebral column Exclusion criteria: history of compensation for the back in the previous year or history of spinal surgery at any time in the past, multiple injuries involving sites other than mid‐ or lower spine, workers with claims labelled as a recurrent by the Quebec Worker's Compensation Board or in litigation at the time of recruitment, pregnancy, no communication in French or in English Duration and type of sick leave: cumulative 40 days of absence from work; full sick leave Type of sick leave compensation: Quebec Worker's Compensation Board (public insurance) | |
| Interventions | Intervention: programme for coordination of primary health care (CORE) Components of intervention:
Team: treating physician, chiropractor, physiotherapist Involvement of the employer: no direct contact, but workplace accommodations on occasion Providers of intervention: a team of 2 primary care physicians and a nurse, experience and training not reported Theoretical basis: clinical guideline for the management of back pain Duration: until return to work Control: usual practice; instruction to continue with their treating physician | |
| Outcomes | Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
| |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Consecutively numbered sealed envelopes, allocation was probably concealed |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) | Low risk | Blind for return‐to‐work outcomes Not blind for patient‐reported outcomes |
| Incomplete outcome data (attrition bias) | Low risk | For return‐to‐work outcomes, no attrition according to author, for patient related outcomes 18% missing data, “The number of nonreturned questionnaires at 6 months was relatively large but equal in both groups, and the baseline functional scores were similar to those who returned their questionnaire” (p. 256), plausible effect size among missing data (assuming a smaller effect in same direction), not enough to introduce clinically relevant bias (as the observed effects for patient‐reported outcomes were clearly beneficial) |
| Selective reporting (reporting bias) | Unclear risk | Healthcare satisfaction only incompletely reported |
| Other bias | High risk | Some baseline imbalances between the groups: fewer men in the CORE group (66.7% vs. 76.8%), more subjects with a history of compensation for back pain in the CORE group (42.6% vs. 28.6%) and more subjects with disabling back pain in the previous month in the CORE group (27% vs. 8.9%) |
| Methods | Design: quasi‐RCT, parallel, 2 arms Country: Switzerland Sample size: 8050 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: 2002 to 2006 Method of recruitment: cases covered by the Swiss National Accident Insurance Fund (which includes occupational and non‐occupational accident insurance, and insurance for the unemployed) and registered within 12 months of the accident where eligible for randomisation Follow‐up: 12, 24, 36, 48, 60, 72 months | |
| Participants | Health problem: severe accidents, occupational and non‐occupational Age in years: mean 40.21 Female in %: 18 Intervention group: 4039 participants (unweighted: 3863) Control group: 4013 participants (unweighted: 4187) Inclusion criteria: medical complexity, difficulties with return to work, risk of permanent disability Exclusion criteria: no coverage by the Swiss compulsory accident insurance, cases registered more than 12 months after accident, patients with occupational diseases Duration and type of sick leave: no information about duration of sick leave, at least 4 weeks seemed plausible; full‐ and part‐time sick leave Type of sick leave compensation: Swiss National Accident Insurance Fund (public insurance) | |
| Interventions | Intervention: intensive case management Components of intervention: highly structured approach with defined steps:
Team: independent physician, insurance physician, outpatient care provider, inpatient care provider, physiotherapist, ergotherapist, other care provider Involvement of the employer: yes Providers of intervention: case manager, “specially trained” Theoretical basis: not reported Duration: as long as considered appropriate, average 21.9 months (median 18 months) Control: standard case management:
| |
| Outcomes | Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement): none Outcomes not analysed (measurement):
| |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random procedure based on custom software |
| Allocation concealment (selection bias) | Low risk | Concealed (author information) |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel not blind (author information) |
| Blinding of outcome assessment (detection bias) | Low risk | Blind for return‐to‐work outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No losses to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No protocol published |
| Other bias | Low risk | No indications of other sources of bias |
| Methods | Design: RCT, parallel, 2 arms with 2 subgroups Subgroups: 1) those with influence on the planning of their own work and no perceived risk of losing job and/or being a work injury claimant, 2) those without influence on the planning of their own work or feeling at risk of losing job and not a work injury claimant Country: Denmark Sample size: 120 Unit of allocation: individuals Unit of analysis: individuals Date of recruitment: August 2007 to July 2008 Method of recruitment: referred by their general practitioner, recruited at the Spine Center Follow‐up: 12 months | |
| Participants | Health problem: low back pain Age in years: mean 40.7 (SD 10.0) Female in %: 58 Intervention group: 60 participants Control group: 60 participants Inclusion criteria: absent from work for 3‐16 weeks, aged 16‐60 years, ability to read and speak Danish Exclusion criteria: unemployed, continuing or progressive symptoms indicating plans for surgery, surgery in the spine within the past 12 months, diagnosis of specific back disease (e.g. tumour), diagnosis of primary psychiatric disease, pregnancy, known substance abuse Duration and type of sick leave: range 3‐16 weeks; full‐ and part‐time sick leave Type of sick leave compensation: municipalities, financed by taxpayers (public insurance) | |
| Interventions | Intervention: multidisciplinary intervention (same as Jensen 2012) Components of intervention: brief intervention like control group; case management containing:
Team: specialist of social medicine, a rheumatologist, a physiotherapist, a social worker and an occupational therapist Involvement of the employer: yes Providers of intervention: 3 case managers; experience and training not reported Theoretical basis: Canadian multidisciplinary work rehabilitation programme (i.e. the Sherbrooke model, Loisel 2002) Duration: median 18 weeks Control: municipality case management and brief intervention:
Same control group interventions as Jensen 2012 and Myhre 2014 (without municipality case management) | |
| Outcomes | Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement): none Outcomes not analysed (measurement): none | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated block‐randomisation |
| Allocation concealment (selection bias) | Low risk | Allocation was carried out by a secretary |
| Blinding of participants and personnel (performance bias) | High risk | Blinding was not possible, only the first clinical examination was carried out double blind |
| Blinding of outcome assessment (detection bias) | Low risk | Author information |
| Incomplete outcome data (attrition bias) | Low risk | Complete data for return‐to‐work outcomes |
| Selective reporting (reporting bias) | Low risk | Study protocol published; all outcomes reported |
| Other bias | Low risk | No indications of other sources of bias |
| Methods | Design: RCT, parallel, 2 arms Country: Netherlands Sample size: 60 in 24 clusters Unit of allocation: cluster Unit of analysis: individuals Date of recruitment: not reported, duration 3 years Method of recruitment: recruitment of occupational physicians and consultant psychiatrists in cooperation with ArboNed and Arbounie (2 companies providing company medical care; together they cover almost half of the working population in the Netherlands); recruitment of patients who visited an occupational physician within the past 6 months, selected from the medical files, invitation by letter Follow‐up: 3, 6 months | |
| Participants | Health problem: anxiety, depression, somatoform disorder Age in years: mean 42, range 24‐59 Female in %: 58 Intervention group: 29 participants (12 occupational physicians) Control group: 31 participants (12 occupational physicians) Inclusion criteria: absent from work > 6 weeks, a positive screen on either the Patient Health Questionnaire or the Whitely Index, no plan to return to work within another 6 weeks Exclusion criteria: suicidal, addicted to drugs or alcohol, psychotic, suffering from dementia, insufficient knowledge of the Dutch language, involved in a legislative procedure for unemployment compensation or on sick leave > 52 weeks Duration and type of sick leave: mean 144 days, range 1‐46 (conflicting information to inclusion criteria); full sick leave Type of sick leave compensation: government | |
| Interventions | Intervention: psychiatric consultation model Components of intervention:
Team: occupational physician, consulting psychiatrist, and in some cases the general practitioner Involvement of the employer: no Providers of intervention: 12 occupational physicians, training in diagnosis and treatment of mental disorders, consulted by 2 psychiatrists trained in improvement of work functioning Theoretical basis: Van der Feltz‐Cornelis 1996 Duration: until return to work Control: usual practice; care from occupational physicians and mental healthcare professionals | |
| Outcomes | Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
| |
| Notes | Baseline characteristics of the occupational physicians not reported (unit of randomisation) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Consecutive envelopes, the sequence was concealed until interventions were assigned by an independent blinded research assistant |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) | Low risk | Blind for return‐to‐work outcomes Not blind for patient‐reported outcomes |
| Incomplete outcome data (attrition bias) | High risk | 18% losses to follow‐up for return‐to‐work outcomes, 27% losses to follow‐up for patient‐reported outcomes |
| Selective reporting (reporting bias) | High risk | Primary outcome was not pre‐specified: changed from “level of functioning” in the protocol to “time until RTW for at least 4 weeks”; reasons for change of primary outcomes were not discussed in final report; “level of functioning” not reported |
| Other bias | Low risk | No indications of other sources of bias; no indication of design effect: “As this is a cluster randomized trial, a correction for possible doctor variance (practices) was made. It was shown that it did not make any difference to the effect size which doctor gave the treatment. Apparently the effect of the intervention stands for itself.” (p. 383) |
| Methods | Design: RCT, parallel, 2 arms Country: Netherlands Sample size: 220 in 12 clusters Unit of allocation: cluster Unit of analysis: individuals Date of recruitment: not reported Method of recruitment: screening of sick‐listed employees visiting their occupational physician, invitation by letter and telephone Follow‐up: 3, 6, 9, 12 months | |
| Participants | Health problem: common mental disorders Age in years: 44.46 (SD 10.04) Female in %: 59 Intervention group: 131 participants (32 occupational physicians) Control group: 89 participants (30 occupational physicians) Inclusion criteria: absent from work 4‐26 weeks, aged ≥18 years, screened positive (score ≥ 10) on either the scale of the Patient Health Questionnaire 9, Patient Health Questionnaire 15 or the Generalised Anxiety Disorder Questionnaire Exclusion criteria: insufficient knowledge of the Dutch language, pregnancy, involved in legal action against their employer, no Internet access Duration and type of sick leave: 4‐26 weeks, median 73 days (intervention group) and 70 days (control group); full‐ and part‐time sick leave Type of sick leave compensation: government | |
| Interventions | Intervention: e‐health module embedded in Collaborative Occupational health care (ECO) Components of intervention: the ECO intervention included
Team: occupational physician, general practitioner, mental health professional Additional resource: Return@Work eHealth module, email decision aid for the occupational physician Involvement of the employer: no Providers of intervention: 29 occupational physicians at Arbo Vitale (a large occupational health service) and one occupational physician at GGz Breburg (a large mental health service employer); half a day training on sickness guidance, the e‐health module and contact to other stakeholders Theoretical basis: none Duration: not reported (up to 16 sessions) Control: usual practice with contact to occupational physician, general practitioner and mental health professional, contact to other healthcare professionals not restricted (same utilisation as in intervention group) | |
| Outcomes | Return‐to‐work outcomes (measurement/data collection):
Patient‐reported outcomes (measurement):
Outcomes not analysed (measurement):
| |
| Notes | Authors provided additional data for secondary outcomes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | “The research assistants and the participants were blind to the allocation when assessing the eligibility of sick‐listed employees for participating in this study.” (p. 3) |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel not blind |
| Blinding of outcome assessment (detection bias) | Low risk | Blind for return‐to‐work outcomes Not blind for patient‐reported outcomes |
| Incomplete outcome data (attrition bias) | Low risk | 2% losses to follow‐up for return‐to‐work outcomes “For the self‐reported secondary outcomes, follow‐up questionnaires were returned by 158 of 220 participants (71.8%) at 3 months, 158 participants (71.8%) at 6 months, 137 participants (62.3%) at 9 months, and 131 participants (59.5%) at 12 months. At 9 months, the loss to follow‐up rate was significantly higher in the ECO condition (44.3%, 58/131) than in the CAU condition (28%, 25/89, P=.02). However, the participants who did return the questionnaire at 9 months did not differ significantly at baseline on sickness absence duration, depression, somatization, or anxiety symptoms from the participants who did not return the questionnaire. This was the case in the ECO condition and in the control condition. From these results, we concluded that there was no evidence for selective dropout in this study.” (p. 7) |
| Selective reporting (reporting bias) | Low risk | Study protocol published, all outcomes reported |
| Other bias | High risk | Low adherence to intervention: “in the intervention group, 31 participants (23.7%) never logged in at Return@Work. Of the 100 participants who did log in at Return@Work, 10.0% (10/100) did not finish the introduction (which included information about Return@Work and a questionnaire). The mean number of total log‐ins of the 90 participants who finished the introduction and actually started Return@Work was 7.8 (SD 6.1). Furthermore, 40% (36/90) of the participants minimally completed half of the modules of Return@Work.” (p. 11) no indication of a cluster effect: “The results, however, showed that there was no evidence of a clustering effect at the level of occupational physician regions (P = 0.92).” (p. 9) |
IQR: interquartile range; SD: standard deviation; SF‐12/36: 12/36‐item Short Form Health Survey.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not a commissioned programme, not an individually tailored programme | |
| Not a commissioned programme, not an individually tailored programme | |
| Not a commissioned programme, not an individually tailored programme | |
| Not a commissioned programme, not an individually tailored programme | |
| Sick leave was not inclusion criteria | |
| Sick leave less than 4 weeks | |
| Sick leave duration unclear | |
| Not a commissioned programme, not an individually tailored programme | |
| Sick leave less than 4 weeks | |
| Not an individually tailored programme | |
| Sick leave was not an inclusion criterion | |
| Not an individually tailored programme | |
| Not a commissioned programme, not an individually tailored programme | |
| Only vocational advice service | |
| Not an individually tailored programme, less than 80% on sick leave | |
| Not an individually tailored programme, duration of sick leave unclear | |
| Prevention programme | |
| Sick leave less than 4 weeks | |
| Sick leave less than 4 weeks | |
| Not an individually tailored programme | |
| Not coordinated | |
| Not an individually tailored programme | |
| Not an RCT | |
| Not an individually tailored programme | |
| Aim was not return to work | |
| Sick leave less than 4 weeks | |
| Sick leave was not an inclusion criterion | |
| Not an individually tailored programme | |
| Prevention programme | |
| Prevention programme | |
| Prevention programme | |
| Unemployed participants, not an individually tailored programme | |
| Not an individually tailored programme, no return‐to‐work plan | |
| Not an individually tailored programme | |
| Not a commissioned programme, not an individually tailored programme | |
| Not an RCT | |
| Advice only | |
| Sick leave less than 4 weeks | |
| Investigates self‐management | |
| Not an individually tailored programme | |
| Less than 80% on sick leave | |
| Not an individually tailored programme | |
| Unemployed participants | |
| Sick leave less than 4 weeks, no individually tailored programme | |
| Not a controlled design | |
| Not a commissioned programme, not an individually tailored programme | |
| No face‐to‐face contact, not an individually tailored programme | |
| No face‐to‐face contact, not an individually tailored programme | |
| Not an individually tailored programme | |
| Not an individually tailored programme | |
| Not an individually tailored programme | |
| Prevention programme | |
| No face‐to‐face contact, aim was to assess the feasibility of the programme | |
| Sick leave less than 4 weeks | |
| Not an individually tailored programme | |
| Sick leave duration unclear, no commissioned programme | |
| Not an RCT | |
| Sick leave less than 4 weeks | |
| Not an individually tailored programme | |
| Not an RCT | |
| No prospective design | |
| No prospective design | |
| Not an RCT | |
| Not an individually tailored programme | |
| Not a commissioned programme, not an individually tailored programme | |
| Not an individually tailored programme | |
| Not coordinated, no return‐to‐work plan | |
| Prevention programme | |
| More than 20% unemployed participants | |
| Not an RCT | |
| Not an RCT | |
| Aim was not return to work; participants not on sick leave | |
| Participants not on sick leave | |
| Aim was not return to work | |
| Control group received the intervention after 3 weeks | |
| Not an individually tailored programme; participants not on sick leave | |
| Not a commissioned programme, not an individually tailored programme | |
| Not a commissioned programme, not an individually tailored programme | |
| Sick leave less than 4 weeks | |
| Sick leave was 4 weeks during 1 year | |
| Not an individually tailored programme | |
| Not an individually tailored programme | |
| Not an individually tailored programme | |
| No prospective design, more than 20% unemployed participants | |
| No prospective design, more than 20% unemployed participants | |
| Quasi‐randomised trial, more than 20% unemployed participants | |
| Less than 80% on sick leave | |
| Not an RCT | |
| Not an individually tailored programme | |
| Not an individually tailored programme | |
| Not an RCT | |
| Not an individually tailored programme | |
| More than 20% unemployed participants | |
| Sick leave less than 4 weeks | |
| Not an individually tailored programme | |
| Not an individually tailored programme | |
| Not an individually tailored programme | |
| Prevention programme | |
| Unemployed participants | |
| Not an individually tailored programme, no return‐to‐work plan | |
| Health promotion programme | |
| Not all participants on sick leave | |
| Sick leave less than 4 weeks | |
| More than 20% unemployed participants | |
| Study protocol, no multidisciplinary intervention, not individually tailored | |
| Sick leave less than 4 weeks | |
| Sick leave less than 4 weeks | |
| Sick leave less than 4 weeks | |
| Not an individually tailored programme | |
| Study protocol, not an individually tailored programme | |
| Not a commissioned programme, not an individually tailored programme | |
| Not a commissioned programme; more than 20% unemployed participants | |
| More than 20% unemployed participants | |
| Unemployed participants | |
| Evaluation study | |
| Not an RCT | |
| Not an individually tailored programme | |
| Not an RCT | |
| Participants not on sick leave | |
| Not an individually tailored programme | |
| Not an RCT | |
| No face‐to‐face contact, not an individually tailored programme | |
| No face‐to‐face contact, not an individually tailored programme | |
| Not an RCT | |
| Sick leave less than 4 weeks | |
| Sick leave less than 4 weeks | |
| Sick leave less than 4 weeks | |
| Sick leave less than 4 weeks | |
| No controlled design | |
| Multidisciplinary rehabilitation for both groups | |
| Aim was not return to work | |
| Not an individually tailored programme | |
| Not a coordinated programme | |
| Not an individually tailored programme | |
| Not a commissioned programme, more than 20% unemployed participants, sick leave duration unclear | |
| Not an RCT | |
| Sick leave less than 4 weeks | |
| Not an individually tailored programme, sick leave less than 4 weeks | |
| Sick leave duration 2‐8 weeks | |
| Sick leave duration 2‐8 weeks | |
| Other outcomes | |
| Unemployed participants | |
| More than 20% unemployed participants | |
| Not an individually tailored programme | |
| Study was not conducted | |
| Not an individually tailored programme | |
| Sick leave less than 4 weeks | |
| No face‐to‐face contact, participants not on sick leave | |
| Sick leave less than 4 weeks, less than 80% on sick leave | |
| Not a commissioned programme, not an individually tailored programme | |
| Less than 80% on sick leave | |
| No prospective design, not an individually tailored programme | |
| Not an individually tailored programme, sick leave duration unclear | |
| Unemployed participants | |
| Not an individually tailored programme |
RCT: randomised controlled trial.
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Design: RCT, parallel, 2 arms Country: Sweden Sample size: unknown Method of recruitment: patients at high risk for long‐term sick leave are identified within primary care Follow‐up: unknown |
| Participants | Patients at high risk for long‐term sick leave |
| Interventions | Intervention: standard care and return‐to‐work coordination (individually adapted patient coaching and coordination Control: standard care |
| Outcomes | Cumulative sickness absence Average sick‐claim rates |
| Notes | Some inclusion and exclusion criteria not verifiable, poster presentation, no full‐text available |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 9 | Hazard Ratio (Random, 95% CI) | Subtotals only | |
| Analysis 1.1  Comparison 1 Return‐to‐work outcomes, Outcome 1 Time to return to work. | ||||
| 1.1 Short‐term, follow‐up 6 months | 2 | 161 | Hazard Ratio (Random, 95% CI) | 1.32 [0.93, 1.88] |
| 1.2 Long‐term, follow‐up 12 months | 6 | 1935 | Hazard Ratio (Random, 95% CI) | 1.25 [0.95, 1.66] |
| 1.3 Very long‐term, follow‐up longer than 12 months | 2 | 474 | Hazard Ratio (Random, 95% CI) | 0.93 [0.74, 1.17] |
| 2 Time to return to work, sensitivity analysis (low risk of bias studies only) Show forest plot | 7 | Hazard Ratio (Random, 95% CI) | Subtotals only | |
| Analysis 1.2  Comparison 1 Return‐to‐work outcomes, Outcome 2 Time to return to work, sensitivity analysis (low risk of bias studies only). | ||||
| 2.1 Short‐term, follow‐up 6 months | 1 | 110 | Hazard Ratio (Random, 95% CI) | 1.17 [0.76, 1.79] |
| 2.2 Long‐term, follow‐up 12 months | 6 | 1935 | Hazard Ratio (Random, 95% CI) | 1.25 [0.95, 1.66] |
| 2.3 Very long‐term, follow‐up longer than 12 months | 1 | 351 | Hazard Ratio (Random, 95% CI) | 0.86 [0.68, 1.09] |
| 3 Cumulative sickness absence in work days Show forest plot | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.3  Comparison 1 Return‐to‐work outcomes, Outcome 3 Cumulative sickness absence in work days. | ||||
| 3.1 Short‐term, follow‐up 6 months | 1 | 113 | Mean Difference (IV, Random, 95% CI) | ‐16.18 [‐32.42, 0.06] |
| 3.2 Long‐term, follow‐up 12 months | 6 | 1339 | Mean Difference (IV, Random, 95% CI) | ‐14.84 [‐38.56, 8.88] |
| 3.3 Very long‐term, follow‐up longer than 12 months | 1 | 8052 | Mean Difference (IV, Random, 95% CI) | 7.0 [‐15.17, 29.17] |
| 4 Proportion at work at end of the follow‐up Show forest plot | 7 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.4  Comparison 1 Return‐to‐work outcomes, Outcome 4 Proportion at work at end of the follow‐up. | ||||
| 4.1 Short‐term, follow‐up 6 months | 5 | 1388 | Risk Ratio (IV, Random, 95% CI) | 1.06 [0.86, 1.30] |
| 4.2 Long‐term, follow‐up 12 months | 5 | 3061 | Risk Ratio (IV, Random, 95% CI) | 1.06 [0.99, 1.15] |
| 4.3 Very long‐term, follow‐up longer than 12 months | 2 | 815 | Risk Ratio (IV, Random, 95% CI) | 0.94 [0.82, 1.07] |
| 5 Proportion at work at end of the follow‐up, sensitivity analysis (low risk of bias studies only) Show forest plot | 4 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.5  Comparison 1 Return‐to‐work outcomes, Outcome 5 Proportion at work at end of the follow‐up, sensitivity analysis (low risk of bias studies only). | ||||
| 5.1 Short‐term, follow‐up 6 months | 3 | 873 | Risk Ratio (IV, Random, 95% CI) | 1.20 [1.10, 1.30] |
| 5.2 Long‐term, follow‐up 12 months | 3 | 1174 | Risk Ratio (IV, Random, 95% CI) | 1.08 [0.94, 1.23] |
| 5.3 Very long‐term, follow‐up longer than 12 months | 1 | 351 | Risk Ratio (IV, Random, 95% CI) | 0.95 [0.80, 1.13] |
| 6 Proportion who had ever returned to work Show forest plot | 12 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.6  Comparison 1 Return‐to‐work outcomes, Outcome 6 Proportion who had ever returned to work. | ||||
| 6.1 Short‐term, follow‐up 6 months | 4 | 675 | Risk Ratio (IV, Random, 95% CI) | 0.87 [0.63, 1.19] |
| 6.2 Long‐term, follow‐up 12 months | 8 | 3822 | Risk Ratio (IV, Random, 95% CI) | 1.03 [0.97, 1.09] |
| 6.3 Very long‐term, follow‐up longer than 12 months | 3 | 938 | Risk Ratio (IV, Random, 95% CI) | 0.95 [0.88, 1.02] |
| 7 Proportion who had ever returned to work, sensitivity analysis (low risk of bias studies only) Show forest plot | 8 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.7  Comparison 1 Return‐to‐work outcomes, Outcome 7 Proportion who had ever returned to work, sensitivity analysis (low risk of bias studies only). | ||||
| 7.1 Short‐term, follow‐up 6 months | 2 | 160 | Risk Ratio (IV, Random, 95% CI) | 1.06 [0.86, 1.31] |
| 7.2 Long‐term, follow‐up 12 months | 6 | 1935 | Risk Ratio (IV, Random, 95% CI) | 1.04 [0.96, 1.11] |
| 7.3 Very long‐term, follow‐up longer than 12 months | 1 | 351 | Risk Ratio (IV, Random, 95% CI) | 0.97 [0.87, 1.08] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 10.0 Show forest plot | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.1  Comparison 2 Patient‐reported outcomes, Outcome 1 Pain ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 10.0. | ||||
| 1.1 Short‐term, follow‐up 6 months | 4 | 427 | Mean Difference (IV, Random, 95% CI) | ‐4.76 [‐14.89, 5.36] |
| 1.2 Long‐term, follow‐up 12 months | 6 | 2319 | Mean Difference (IV, Random, 95% CI) | ‐2.98 [‐5.33, ‐0.63] |
| 1.3 Very long‐term, longer than 12 months | 1 | 80 | Mean Difference (IV, Random, 95% CI) | ‐7.20 [‐15.76, 1.36] |
| 2 Pain ‐ pooled RDs of workers with an improvement greater than the MID of 10.0 Show forest plot | 7 | Risk Difference (Random, 95% CI) | Subtotals only | |
| Analysis 2.2  Comparison 2 Patient‐reported outcomes, Outcome 2 Pain ‐ pooled RDs of workers with an improvement greater than the MID of 10.0. | ||||
| 2.1 Short‐term, follow‐up 6 months | 4 | Risk Difference (Random, 95% CI) | ‐0.03 [‐0.11, 0.05] | |
| 2.2 Long‐term, follow‐up 12 months | 6 | Risk Difference (Random, 95% CI) | ‐0.03 [‐0.06, ‐0.00] | |
| 2.3 Very long‐term, longer than 12 months | 1 | Risk Difference (Random, 95% CI) | ‐0.02 [‐0.11, 0.07] | |
| 3 Overall function ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 10.0 Show forest plot | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.3  Comparison 2 Patient‐reported outcomes, Outcome 3 Overall function ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 10.0. | ||||
| 3.1 Short‐term, follow‐up 6 months | 3 | 295 | Mean Difference (IV, Random, 95% CI) | 8.13 [3.95, 12.32] |
| 3.2 Long‐term, follow‐up 12 months | 5 | 2235 | Mean Difference (IV, Random, 95% CI) | 2.74 [‐0.15, 5.64] |
| 4 Overall function ‐ pooled RDs of workers with an improvement greater than the MID of 10.0 Show forest plot | 6 | Risk Difference (Random, 95% CI) | Subtotals only | |
| Analysis 2.4  Comparison 2 Patient‐reported outcomes, Outcome 4 Overall function ‐ pooled RDs of workers with an improvement greater than the MID of 10.0. | ||||
| 4.1 Short‐term, follow‐up, 6 months | 3 | Risk Difference (Random, 95% CI) | 0.16 [‐0.04, 0.37] | |
| 4.2 Long‐term, follow‐up 12 months | 5 | Risk Difference (Random, 95% CI) | 0.00 [‐0.09, 0.09] | |
| 5 Physical function ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 8.4 Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.5  Comparison 2 Patient‐reported outcomes, Outcome 5 Physical function ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 8.4. | ||||
| 5.1 Short‐term, follow‐up 6 months | 3 | 336 | Mean Difference (IV, Random, 95% CI) | 3.47 [‐3.26, 10.20] |
| 5.2 Long‐term, follow‐up 12 months | 4 | 1860 | Mean Difference (IV, Random, 95% CI) | 2.19 [‐2.29, 6.67] |
| 5.3 Very long‐term, follow‐up longer than 12 months | 1 | 78 | Mean Difference (IV, Random, 95% CI) | 1.85 [‐2.25, 5.95] |
| 6 Physical function ‐ pooled RDs of workers with an improvement greater than the MID of 8.4 Show forest plot | 5 | Risk Difference (Random, 95% CI) | Subtotals only | |
| Analysis 2.6  Comparison 2 Patient‐reported outcomes, Outcome 6 Physical function ‐ pooled RDs of workers with an improvement greater than the MID of 8.4. | ||||
| 6.1 Short‐term, follow‐up 6 months | 3 | Risk Difference (Random, 95% CI) | 0.03 [‐0.07, 0.13] | |
| 6.2 Long‐term, follow‐up 12 months | 4 | Risk Difference (Random, 95% CI) | 0.01 [‐0.02, 0.03] | |
| 6.3 Very long‐term, follow‐up longer than 12 months | 1 | Risk Difference (Random, 95% CI) | 0.0 [‐0.02, 0.02] | |
| 7 Social function ‐ scale to 0 to 100 (higher score indicates improvement) ‐ MID 11.7 Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.7  Comparison 2 Patient‐reported outcomes, Outcome 7 Social function ‐ scale to 0 to 100 (higher score indicates improvement) ‐ MID 11.7. | ||||
| 7.1 Long‐term, follow‐up 12 months | 2 | 1636 | Mean Difference (IV, Random, 95% CI) | 2.84 [‐0.09, 5.77] |
| 8 Social function ‐ pooled RDs of workers with an improvement greater than the MID of 11.7 Show forest plot | 2 | Risk Difference (Random, 95% CI) | Subtotals only | |
| Analysis 2.8  Comparison 2 Patient‐reported outcomes, Outcome 8 Social function ‐ pooled RDs of workers with an improvement greater than the MID of 11.7. | ||||
| 8.1 Long‐term, follow‐up 12 months | 2 | Risk Difference (Random, 95% CI) | 0.01 [‐0.02, 0.04] | |
| 9 Mental function ‐ scale to 0 to 100 (higher score indicates improvement) ‐ MID 7.3 Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.9  Comparison 2 Patient‐reported outcomes, Outcome 9 Mental function ‐ scale to 0 to 100 (higher score indicates improvement) ‐ MID 7.3. | ||||
| 9.1 Short‐term, follow‐up 6 months | 1 | 125 | Mean Difference (IV, Random, 95% CI) | 1.85 [‐2.67, 6.37] |
| 9.2 Long‐term, follow‐up 12 months | 3 | 1737 | Mean Difference (IV, Random, 95% CI) | 3.14 [1.16, 5.11] |
| 9.3 Very long‐term, follow‐up longer than 12 months | 1 | 78 | Mean Difference (IV, Random, 95% CI) | 6.09 [0.56, 11.63] |
| 10 Mental function ‐ pooled RDs of workers with an improvement greater than the MID of 7.3 Show forest plot | 3 | Risk Difference (Random, 95% CI) | Subtotals only | |
| Analysis 2.10  Comparison 2 Patient‐reported outcomes, Outcome 10 Mental function ‐ pooled RDs of workers with an improvement greater than the MID of 7.3. | ||||
| 10.1 Short‐term, follow‐up 6 months | 1 | Risk Difference (Random, 95% CI) | 0.0 [‐0.01, 0.01] | |
| 10.2 Long‐term, follow‐up 12 months | 3 | Risk Difference (Random, 95% CI) | 0.00 [‐0.01, 0.01] | |
| 10.3 Very long‐term, follow‐up longer than 12 months | 1 | Risk Difference (Random, 95% CI) | 0.0 [‐0.01, 0.01] | |
| 11 Depression ‐ scale 0 to 27 (higher score indicates deterioration) ‐ MID 5.0 Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.11  Comparison 2 Patient‐reported outcomes, Outcome 11 Depression ‐ scale 0 to 27 (higher score indicates deterioration) ‐ MID 5.0. | ||||
| 11.1 Short‐term, follow‐up 6 months | 3 | 252 | Mean Difference (IV, Random, 95% CI) | 0.37 [‐2.81, 3.55] |
| 11.2 Long‐term, follow‐up 12 months | 2 | 420 | Mean Difference (IV, Random, 95% CI) | ‐0.00 [‐1.07, 1.07] |
| 12 Depression ‐ pooled RDs of workers with an improvement greater than the MID of 5.0 Show forest plot | 4 | Risk Difference (Random, 95% CI) | Subtotals only | |
| Analysis 2.12  Comparison 2 Patient‐reported outcomes, Outcome 12 Depression ‐ pooled RDs of workers with an improvement greater than the MID of 5.0. | ||||
| 12.1 Short‐term, follow‐up 6 months | 3 | Risk Difference (Random, 95% CI) | 0.03 [‐0.07, 0.12] | |
| 12.2 Long‐term, follow‐up 12 months | 2 | Risk Difference (Random, 95% CI) | 0.01 [‐0.04, 0.06] | |
| 13 Anxiety ‐ scale 0 to 21 (higher score indicates deterioration) ‐ MID 4.0 Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.13  Comparison 2 Patient‐reported outcomes, Outcome 13 Anxiety ‐ scale 0 to 21 (higher score indicates deterioration) ‐ MID 4.0. | ||||
| 13.1 Short‐term, follow‐up 6 months | 2 | 208 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐3.24, 3.21] |
| 13.2 Long‐term, follow‐up 12 months | 2 | 420 | Mean Difference (IV, Random, 95% CI) | 0.97 [‐0.17, 2.12] |
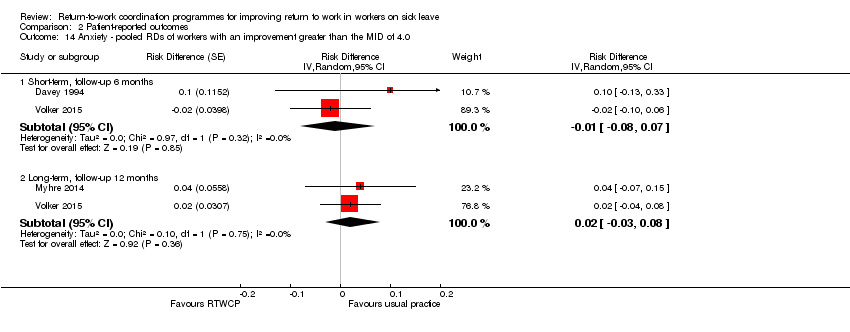
| 14 Anxiety ‐ pooled RDs of workers with an improvement greater than the MID of 4.0 Show forest plot | 3 | Risk Difference (Random, 95% CI) | Subtotals only | |
| Analysis 2.14  Comparison 2 Patient‐reported outcomes, Outcome 14 Anxiety ‐ pooled RDs of workers with an improvement greater than the MID of 4.0. | ||||
| 14.1 Short‐term, follow‐up 6 months | 2 | Risk Difference (Random, 95% CI) | ‐0.01 [‐0.08, 0.07] | |
| 14.2 Long‐term, follow‐up 12 months | 2 | Risk Difference (Random, 95% CI) | 0.02 [‐0.03, 0.08] | |
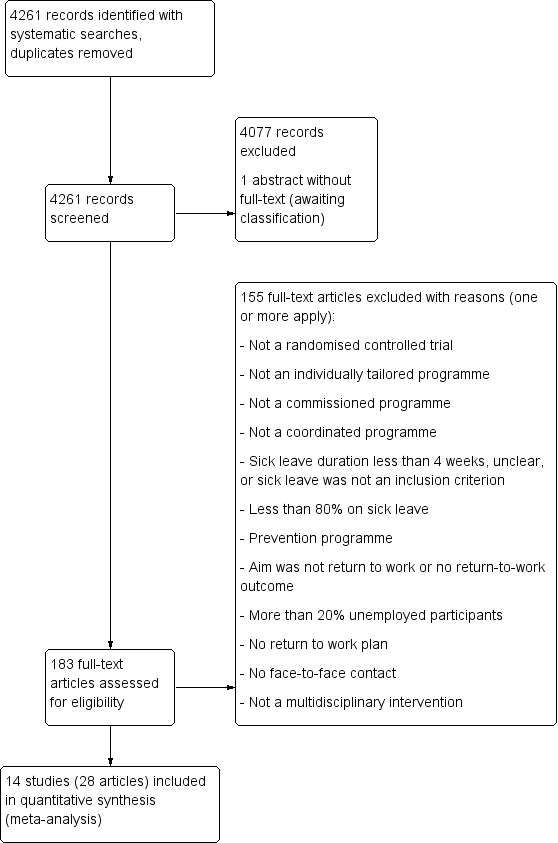
PRISMA Study flow diagram

Risk of bias graph: review author's judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: time to return to work. RTWCP = return‐to‐work coordination programmes

Forest plot of comparison: cumulative sickness absence in work days. RTWCP = return‐to‐work coordination programmes
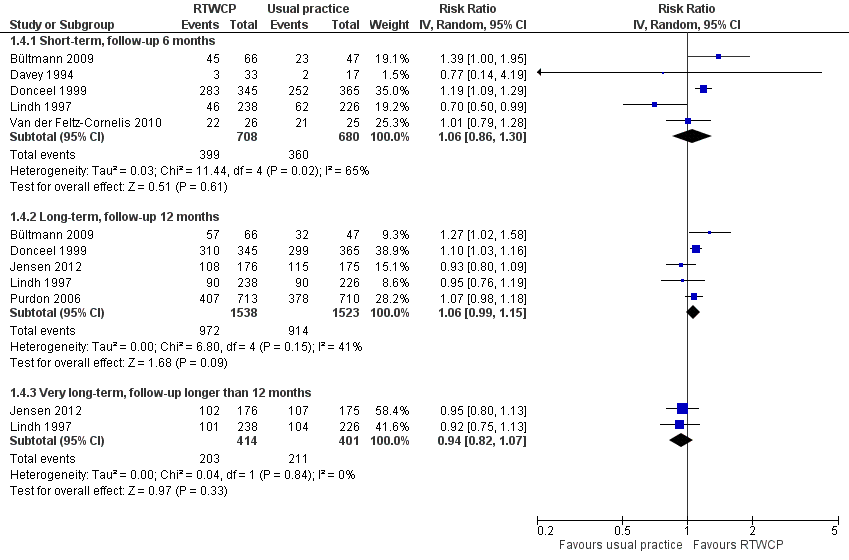
Forest plot of comparison: proportion at work at end of the follow‐up. RTWCP = return‐to‐work coordination programmes
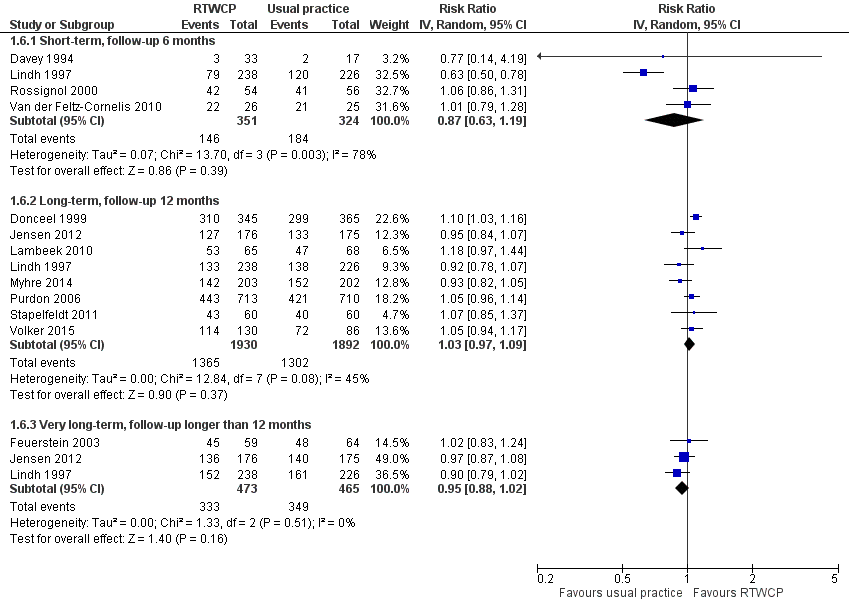
Forest plot of comparison: proportion who had ever returned to work. RTWCP = return‐to‐work coordination programmes

Comparison 1 Return‐to‐work outcomes, Outcome 1 Time to return to work.
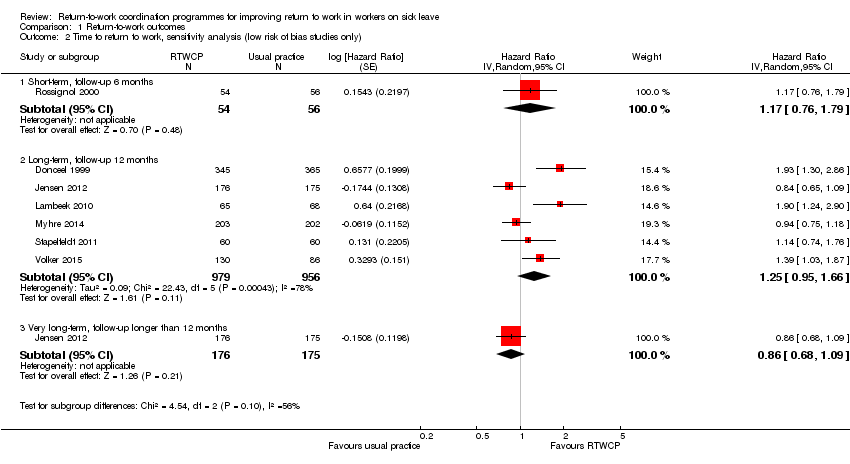
Comparison 1 Return‐to‐work outcomes, Outcome 2 Time to return to work, sensitivity analysis (low risk of bias studies only).

Comparison 1 Return‐to‐work outcomes, Outcome 3 Cumulative sickness absence in work days.
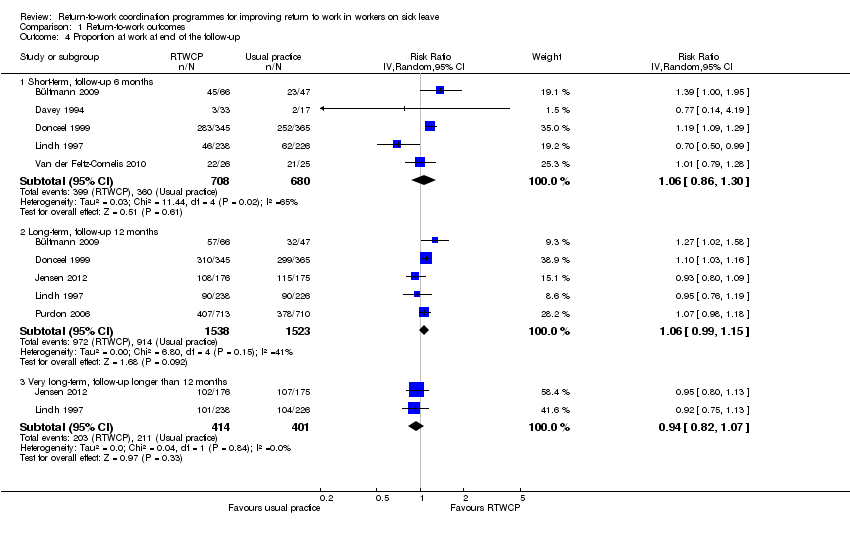
Comparison 1 Return‐to‐work outcomes, Outcome 4 Proportion at work at end of the follow‐up.
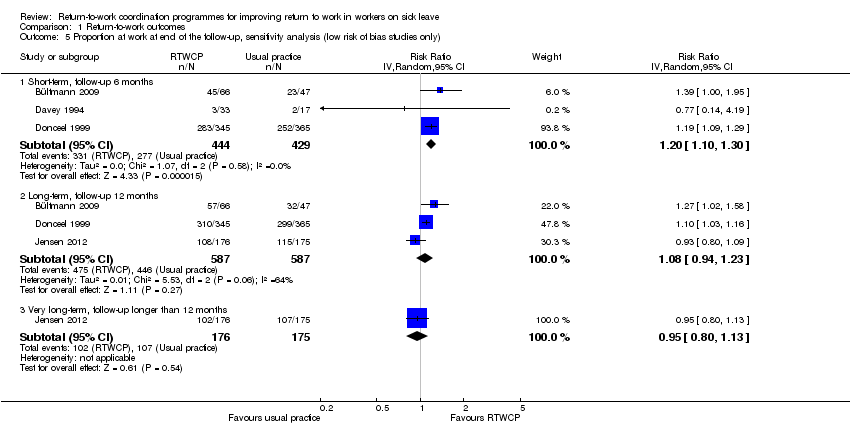
Comparison 1 Return‐to‐work outcomes, Outcome 5 Proportion at work at end of the follow‐up, sensitivity analysis (low risk of bias studies only).
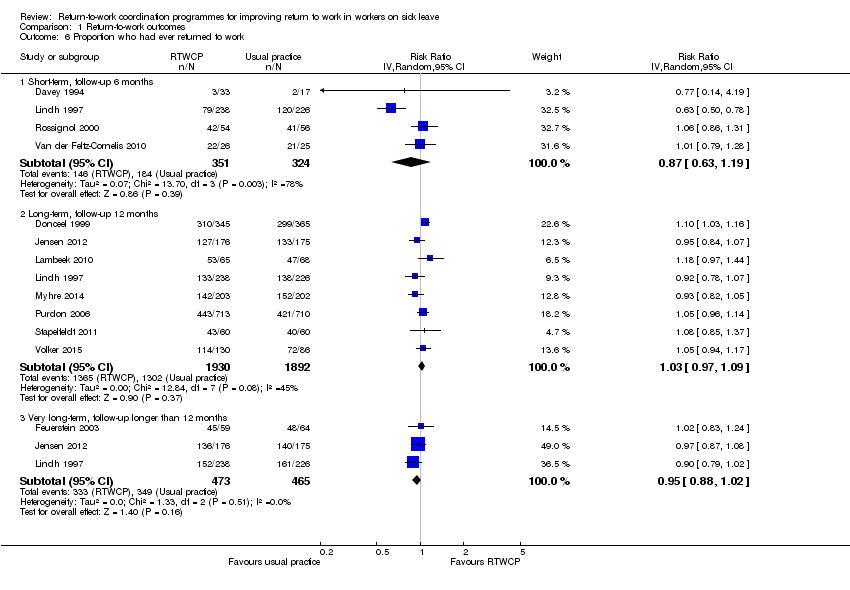
Comparison 1 Return‐to‐work outcomes, Outcome 6 Proportion who had ever returned to work.

Comparison 1 Return‐to‐work outcomes, Outcome 7 Proportion who had ever returned to work, sensitivity analysis (low risk of bias studies only).

Comparison 2 Patient‐reported outcomes, Outcome 1 Pain ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 10.0.

Comparison 2 Patient‐reported outcomes, Outcome 2 Pain ‐ pooled RDs of workers with an improvement greater than the MID of 10.0.

Comparison 2 Patient‐reported outcomes, Outcome 3 Overall function ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 10.0.

Comparison 2 Patient‐reported outcomes, Outcome 4 Overall function ‐ pooled RDs of workers with an improvement greater than the MID of 10.0.

Comparison 2 Patient‐reported outcomes, Outcome 5 Physical function ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 8.4.
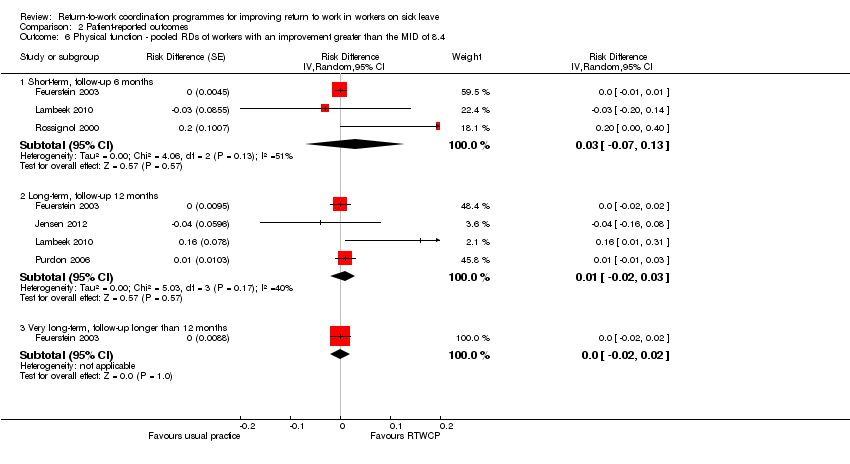
Comparison 2 Patient‐reported outcomes, Outcome 6 Physical function ‐ pooled RDs of workers with an improvement greater than the MID of 8.4.
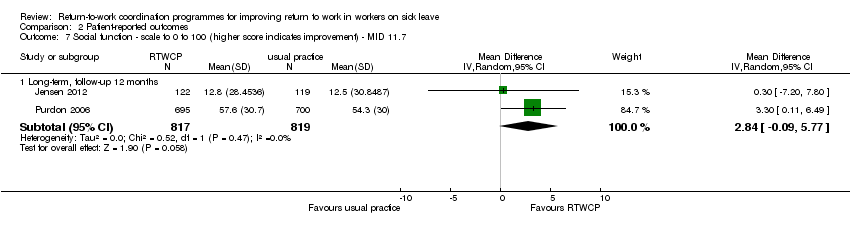
Comparison 2 Patient‐reported outcomes, Outcome 7 Social function ‐ scale to 0 to 100 (higher score indicates improvement) ‐ MID 11.7.
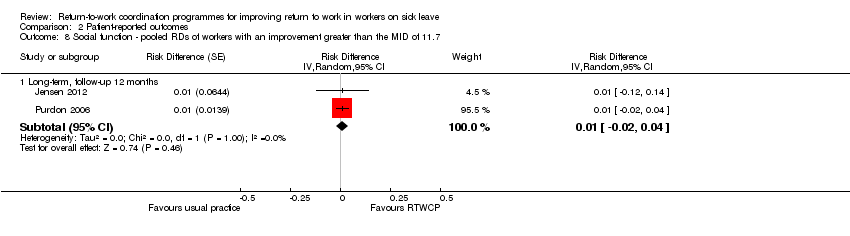
Comparison 2 Patient‐reported outcomes, Outcome 8 Social function ‐ pooled RDs of workers with an improvement greater than the MID of 11.7.

Comparison 2 Patient‐reported outcomes, Outcome 9 Mental function ‐ scale to 0 to 100 (higher score indicates improvement) ‐ MID 7.3.

Comparison 2 Patient‐reported outcomes, Outcome 10 Mental function ‐ pooled RDs of workers with an improvement greater than the MID of 7.3.
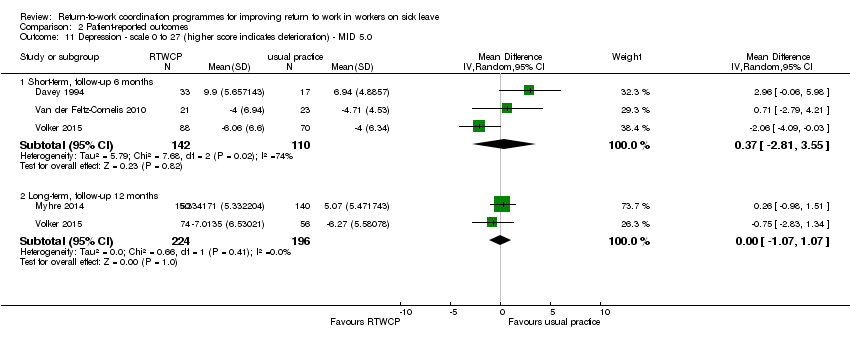
Comparison 2 Patient‐reported outcomes, Outcome 11 Depression ‐ scale 0 to 27 (higher score indicates deterioration) ‐ MID 5.0.

Comparison 2 Patient‐reported outcomes, Outcome 12 Depression ‐ pooled RDs of workers with an improvement greater than the MID of 5.0.
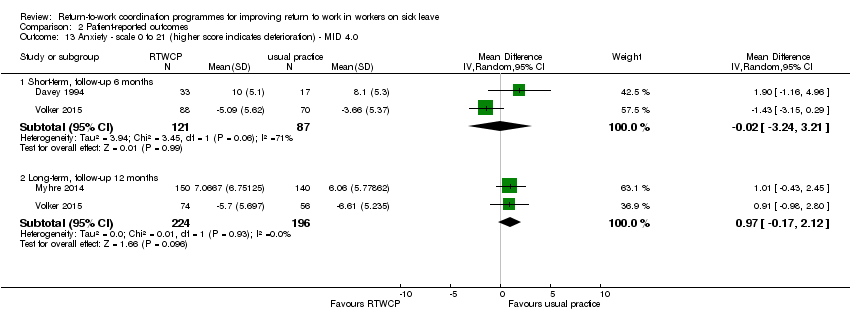
Comparison 2 Patient‐reported outcomes, Outcome 13 Anxiety ‐ scale 0 to 21 (higher score indicates deterioration) ‐ MID 4.0.
Comparison 2 Patient‐reported outcomes, Outcome 14 Anxiety ‐ pooled RDs of workers with an improvement greater than the MID of 4.0.
| Return to work coordination programmes compared to usual practice for improving return to work in workers on sick leave | |||||
| Patient or population: workers on sick leave | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | |
| Risk with usual practice | Risk with return‐to‐work coordination programmes | ||||
| Time to return to work ‐ short‐term | — | — | HR 1.32 | 161 | ⊕⊕⊝⊝ |
| Time to return to work ‐ long‐term | — | — | HR 1.25 | 1935 | ⊕⊕⊝⊝ |
| Time to return to work ‐ very long‐term | — | — | HR 0.93 | 474 | ⊕⊕⊝⊝ |
| Cumulative sickness absence in work days ‐ short‐term | The mean cumulative sickness absence was 79.14 work days | The mean cumulative | — | 113 | ⊕⊕⊕⊝ |
| Cumulative sickness absence in work days ‐ long‐term | The mean cumulative sickness absence was 144 work days | The mean cumulative | — | 1339 | ⊕⊕⊝⊝ |
| Cumulative sickness absence in work days ‐ very long‐term | The mean cumulative sickness absence was 466 work days | The mean cumulative | — | 8052 | ⊕⊕⊕⊝ |
| Proportion at work at end of the follow‐up ‐ short‐term | 53 per 100 | 56 per 100 | RR 1.06 | 1388 | ⊕⊕⊝⊝ |
| Proportion at work at end of the follow‐up ‐ long‐term | 60 per 100 | 64 per 100 | RR 1.06 | 3061 | ⊕⊕⊝⊝ |
| Proportion at work at end of the follow‐up ‐ very long‐term | 53 per 100 | 49 per 100 | RR 0.94 | 815 | ⊕⊕⊝⊝ |
| Proportion who had ever returned to work ‐ short‐term | 57 per 100 | 49 per 100 | RR 0.87 | 675 | ⊕⊝⊝⊝ |
| Proportion who had ever returned to work ‐ long‐term | 69 per 100 | 71 per 100 | RR 1.03 | 3822 | ⊕⊕⊕⊝ |
| Proportion who had ever returned to work ‐ very long‐term | 75 per 100 | 71 per 100 | RR 0.95 | 938 | ⊕⊕⊝⊝ |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| a Downgraded 1 level for risk of bias (attrition bias, reporting bias). | |||||
| Occupational or rehabilitation physician | General practitioner | (Occupational) physiotherapist | Psychologist, psychiatrist, psychotherapist | Occupational therapist | Social worker | Chiropractor | Other | |
| X | — | X | X | — | X | X | — | |
| X | — | X | X | X | — | — | — | |
| X (social insurance physician) | X | — | — | — | — | — | Other healthcare personnel, social insurance agent | |
| — | — | — | — | — | — | — | “[E].g. supervisor, injury compensation specialist, medical providers, claims examiner” | |
| X | X | X | — | X | X | — | — | |
| X | — | X | — | X | — | — | Medical specialist | |
| X | — | X | X | X | X | — | Nurse, vocational counsellor | |
| X | — | X | — | — | — | — | Case worker, medical specialist, group discussions, lecturer | |
| — | — | X | X | — | — | X | Podiatrists, osteopaths and dieticians | |
| X | — | X | — | — | — | X | — | |
| X (insurance physician) | X | X | — | X | — | — | Outpatient care provider, inpatient care provider, other care provider | |
| X | X | X | — | X | X | — | — | |
| X | X | — | X | — | — | — | — | |
| X | X | — | X | — | — | — | Web‐based eHealth Modules | |
| X = involved discipline | ||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 9 | Hazard Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Short‐term, follow‐up 6 months | 2 | 161 | Hazard Ratio (Random, 95% CI) | 1.32 [0.93, 1.88] |
| 1.2 Long‐term, follow‐up 12 months | 6 | 1935 | Hazard Ratio (Random, 95% CI) | 1.25 [0.95, 1.66] |
| 1.3 Very long‐term, follow‐up longer than 12 months | 2 | 474 | Hazard Ratio (Random, 95% CI) | 0.93 [0.74, 1.17] |
| 2 Time to return to work, sensitivity analysis (low risk of bias studies only) Show forest plot | 7 | Hazard Ratio (Random, 95% CI) | Subtotals only | |
| 2.1 Short‐term, follow‐up 6 months | 1 | 110 | Hazard Ratio (Random, 95% CI) | 1.17 [0.76, 1.79] |
| 2.2 Long‐term, follow‐up 12 months | 6 | 1935 | Hazard Ratio (Random, 95% CI) | 1.25 [0.95, 1.66] |
| 2.3 Very long‐term, follow‐up longer than 12 months | 1 | 351 | Hazard Ratio (Random, 95% CI) | 0.86 [0.68, 1.09] |
| 3 Cumulative sickness absence in work days Show forest plot | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Short‐term, follow‐up 6 months | 1 | 113 | Mean Difference (IV, Random, 95% CI) | ‐16.18 [‐32.42, 0.06] |
| 3.2 Long‐term, follow‐up 12 months | 6 | 1339 | Mean Difference (IV, Random, 95% CI) | ‐14.84 [‐38.56, 8.88] |
| 3.3 Very long‐term, follow‐up longer than 12 months | 1 | 8052 | Mean Difference (IV, Random, 95% CI) | 7.0 [‐15.17, 29.17] |
| 4 Proportion at work at end of the follow‐up Show forest plot | 7 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Short‐term, follow‐up 6 months | 5 | 1388 | Risk Ratio (IV, Random, 95% CI) | 1.06 [0.86, 1.30] |
| 4.2 Long‐term, follow‐up 12 months | 5 | 3061 | Risk Ratio (IV, Random, 95% CI) | 1.06 [0.99, 1.15] |
| 4.3 Very long‐term, follow‐up longer than 12 months | 2 | 815 | Risk Ratio (IV, Random, 95% CI) | 0.94 [0.82, 1.07] |
| 5 Proportion at work at end of the follow‐up, sensitivity analysis (low risk of bias studies only) Show forest plot | 4 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Short‐term, follow‐up 6 months | 3 | 873 | Risk Ratio (IV, Random, 95% CI) | 1.20 [1.10, 1.30] |
| 5.2 Long‐term, follow‐up 12 months | 3 | 1174 | Risk Ratio (IV, Random, 95% CI) | 1.08 [0.94, 1.23] |
| 5.3 Very long‐term, follow‐up longer than 12 months | 1 | 351 | Risk Ratio (IV, Random, 95% CI) | 0.95 [0.80, 1.13] |
| 6 Proportion who had ever returned to work Show forest plot | 12 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Short‐term, follow‐up 6 months | 4 | 675 | Risk Ratio (IV, Random, 95% CI) | 0.87 [0.63, 1.19] |
| 6.2 Long‐term, follow‐up 12 months | 8 | 3822 | Risk Ratio (IV, Random, 95% CI) | 1.03 [0.97, 1.09] |
| 6.3 Very long‐term, follow‐up longer than 12 months | 3 | 938 | Risk Ratio (IV, Random, 95% CI) | 0.95 [0.88, 1.02] |
| 7 Proportion who had ever returned to work, sensitivity analysis (low risk of bias studies only) Show forest plot | 8 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Short‐term, follow‐up 6 months | 2 | 160 | Risk Ratio (IV, Random, 95% CI) | 1.06 [0.86, 1.31] |
| 7.2 Long‐term, follow‐up 12 months | 6 | 1935 | Risk Ratio (IV, Random, 95% CI) | 1.04 [0.96, 1.11] |
| 7.3 Very long‐term, follow‐up longer than 12 months | 1 | 351 | Risk Ratio (IV, Random, 95% CI) | 0.97 [0.87, 1.08] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 10.0 Show forest plot | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Short‐term, follow‐up 6 months | 4 | 427 | Mean Difference (IV, Random, 95% CI) | ‐4.76 [‐14.89, 5.36] |
| 1.2 Long‐term, follow‐up 12 months | 6 | 2319 | Mean Difference (IV, Random, 95% CI) | ‐2.98 [‐5.33, ‐0.63] |
| 1.3 Very long‐term, longer than 12 months | 1 | 80 | Mean Difference (IV, Random, 95% CI) | ‐7.20 [‐15.76, 1.36] |
| 2 Pain ‐ pooled RDs of workers with an improvement greater than the MID of 10.0 Show forest plot | 7 | Risk Difference (Random, 95% CI) | Subtotals only | |
| 2.1 Short‐term, follow‐up 6 months | 4 | Risk Difference (Random, 95% CI) | ‐0.03 [‐0.11, 0.05] | |
| 2.2 Long‐term, follow‐up 12 months | 6 | Risk Difference (Random, 95% CI) | ‐0.03 [‐0.06, ‐0.00] | |
| 2.3 Very long‐term, longer than 12 months | 1 | Risk Difference (Random, 95% CI) | ‐0.02 [‐0.11, 0.07] | |
| 3 Overall function ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 10.0 Show forest plot | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Short‐term, follow‐up 6 months | 3 | 295 | Mean Difference (IV, Random, 95% CI) | 8.13 [3.95, 12.32] |
| 3.2 Long‐term, follow‐up 12 months | 5 | 2235 | Mean Difference (IV, Random, 95% CI) | 2.74 [‐0.15, 5.64] |
| 4 Overall function ‐ pooled RDs of workers with an improvement greater than the MID of 10.0 Show forest plot | 6 | Risk Difference (Random, 95% CI) | Subtotals only | |
| 4.1 Short‐term, follow‐up, 6 months | 3 | Risk Difference (Random, 95% CI) | 0.16 [‐0.04, 0.37] | |
| 4.2 Long‐term, follow‐up 12 months | 5 | Risk Difference (Random, 95% CI) | 0.00 [‐0.09, 0.09] | |
| 5 Physical function ‐ scale 0 to 100 (higher score indicates improvement) ‐ MID 8.4 Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Short‐term, follow‐up 6 months | 3 | 336 | Mean Difference (IV, Random, 95% CI) | 3.47 [‐3.26, 10.20] |
| 5.2 Long‐term, follow‐up 12 months | 4 | 1860 | Mean Difference (IV, Random, 95% CI) | 2.19 [‐2.29, 6.67] |
| 5.3 Very long‐term, follow‐up longer than 12 months | 1 | 78 | Mean Difference (IV, Random, 95% CI) | 1.85 [‐2.25, 5.95] |
| 6 Physical function ‐ pooled RDs of workers with an improvement greater than the MID of 8.4 Show forest plot | 5 | Risk Difference (Random, 95% CI) | Subtotals only | |
| 6.1 Short‐term, follow‐up 6 months | 3 | Risk Difference (Random, 95% CI) | 0.03 [‐0.07, 0.13] | |
| 6.2 Long‐term, follow‐up 12 months | 4 | Risk Difference (Random, 95% CI) | 0.01 [‐0.02, 0.03] | |
| 6.3 Very long‐term, follow‐up longer than 12 months | 1 | Risk Difference (Random, 95% CI) | 0.0 [‐0.02, 0.02] | |
| 7 Social function ‐ scale to 0 to 100 (higher score indicates improvement) ‐ MID 11.7 Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Long‐term, follow‐up 12 months | 2 | 1636 | Mean Difference (IV, Random, 95% CI) | 2.84 [‐0.09, 5.77] |
| 8 Social function ‐ pooled RDs of workers with an improvement greater than the MID of 11.7 Show forest plot | 2 | Risk Difference (Random, 95% CI) | Subtotals only | |
| 8.1 Long‐term, follow‐up 12 months | 2 | Risk Difference (Random, 95% CI) | 0.01 [‐0.02, 0.04] | |
| 9 Mental function ‐ scale to 0 to 100 (higher score indicates improvement) ‐ MID 7.3 Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 Short‐term, follow‐up 6 months | 1 | 125 | Mean Difference (IV, Random, 95% CI) | 1.85 [‐2.67, 6.37] |
| 9.2 Long‐term, follow‐up 12 months | 3 | 1737 | Mean Difference (IV, Random, 95% CI) | 3.14 [1.16, 5.11] |
| 9.3 Very long‐term, follow‐up longer than 12 months | 1 | 78 | Mean Difference (IV, Random, 95% CI) | 6.09 [0.56, 11.63] |
| 10 Mental function ‐ pooled RDs of workers with an improvement greater than the MID of 7.3 Show forest plot | 3 | Risk Difference (Random, 95% CI) | Subtotals only | |
| 10.1 Short‐term, follow‐up 6 months | 1 | Risk Difference (Random, 95% CI) | 0.0 [‐0.01, 0.01] | |
| 10.2 Long‐term, follow‐up 12 months | 3 | Risk Difference (Random, 95% CI) | 0.00 [‐0.01, 0.01] | |
| 10.3 Very long‐term, follow‐up longer than 12 months | 1 | Risk Difference (Random, 95% CI) | 0.0 [‐0.01, 0.01] | |
| 11 Depression ‐ scale 0 to 27 (higher score indicates deterioration) ‐ MID 5.0 Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 11.1 Short‐term, follow‐up 6 months | 3 | 252 | Mean Difference (IV, Random, 95% CI) | 0.37 [‐2.81, 3.55] |
| 11.2 Long‐term, follow‐up 12 months | 2 | 420 | Mean Difference (IV, Random, 95% CI) | ‐0.00 [‐1.07, 1.07] |
| 12 Depression ‐ pooled RDs of workers with an improvement greater than the MID of 5.0 Show forest plot | 4 | Risk Difference (Random, 95% CI) | Subtotals only | |
| 12.1 Short‐term, follow‐up 6 months | 3 | Risk Difference (Random, 95% CI) | 0.03 [‐0.07, 0.12] | |
| 12.2 Long‐term, follow‐up 12 months | 2 | Risk Difference (Random, 95% CI) | 0.01 [‐0.04, 0.06] | |
| 13 Anxiety ‐ scale 0 to 21 (higher score indicates deterioration) ‐ MID 4.0 Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 13.1 Short‐term, follow‐up 6 months | 2 | 208 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐3.24, 3.21] |
| 13.2 Long‐term, follow‐up 12 months | 2 | 420 | Mean Difference (IV, Random, 95% CI) | 0.97 [‐0.17, 2.12] |
| 14 Anxiety ‐ pooled RDs of workers with an improvement greater than the MID of 4.0 Show forest plot | 3 | Risk Difference (Random, 95% CI) | Subtotals only | |
| 14.1 Short‐term, follow‐up 6 months | 2 | Risk Difference (Random, 95% CI) | ‐0.01 [‐0.08, 0.07] | |
| 14.2 Long‐term, follow‐up 12 months | 2 | Risk Difference (Random, 95% CI) | 0.02 [‐0.03, 0.08] | |

