Tratamiento inmediato versus tardío para la estenosis de la arteria carótida con síntomas recientes
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomized Multicenter | |
| Participants | 40 participants within 7 days of the onset of symptoms Partial anterior circulation infarction More than 70% ipsilateral carotid stenosis Barthel score > 18 | |
| Interventions | Early surgery (usually within 2 to 6 hours) Late surgery (6 to 8 weeks) | |
| Outcomes | Outcome measures were recorded using Barthel Activities of Daily Living score for disability and Modified Rankin scale for independence | |
| Notes | Study dates not reported Nine of the 21 participants randomized to the late surgery group did not undergo surgery | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomized by computer |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of study participants and personnel could not be done as 1 treatment group had surgery arranged as soon as possible while the other group did not |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | High risk | Allocation to the delayed surgical group was retained in accordance with the 'intention‐to‐treat' principle |
| Selective reporting (reporting bias) | Low risk | Data on pre‐specified primary and secondary outcomes were presented |
| Other bias | High risk | Size: sample size less than 50 per treatment arm |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Non‐acute study (participants in the early group received carotid endarterectomy between 15 and 30 days) | |
| Confounded with no control group; not randomized | |
| Not randomized |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | SPREAD‐STACI study |
| Methods | Randomized Multicenter Blind follow‐up at 90 days |
| Participants | People presenting with TIA, amaurosis fugax or minor stroke within only a few hours of their first symptom Stenosis ranging between 51% and 99% of the carotid artery |
| Interventions | CEA within 48 hours or between 48 hours and 15 days from their initial ischemic symptom |
| Outcomes | Primary outcome: any type of stroke, myocardial infarction, and death due to the procedures Secondary outcome: ipsilateral stroke, identification of predictive risk factors, confirmation of the safety of urgent CEA |
| Starting date | 2010 |
| Contact information | Dr Gaetano Lanza – U.O. Chirurgia Vascolare, Ospedale MultiMedica, V.le Piemonte, 70, 21053 Castellanza (Va) |
| Notes | Size: 456 participants |
CEA: carotid endarterectomy
TIA: transient ischemic attack
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Stroke and death < 30days Show forest plot | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.32 [0.38, 29.23] |
| Analysis 1.1  Comparison 1 Stroke, Outcome 1 Stroke and death < 30days. | ||||
| 2 Perioperative death and all strokes Show forest plot | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.14, 1.58] |
| Analysis 1.2  Comparison 1 Stroke, Outcome 2 Perioperative death and all strokes. | ||||

Study flow diagram.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
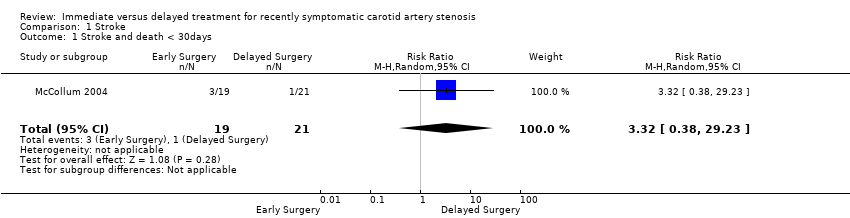
Comparison 1 Stroke, Outcome 1 Stroke and death < 30days.

Comparison 1 Stroke, Outcome 2 Perioperative death and all strokes.
| Very early cerebral revascularization compared with delayed treatment for recently symptomatic carotid artery stenosis | ||||||
| Patient or population: people with recently symptomatic carotid artery stenosis Settings: hospital Intervention: very early cerebral revascularization (within two days) Comparison: delayed treatment (after two days) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Very early cerebral revascularization | Delayed Treatment | |||||
| Stroke and Death < 30 days | This outcome was poorly reported | RR 3.3 (0.4 to 29.2) | 40 (1 study) | ⊝⊝⊝ | ||
| Perioperative death and strokes | This outcome was poorly reported | RR 0.5 (0.1 to 1.6) | 40 (1 study) | ⊝⊝⊝ | ||
| Lenght of hospital stay | This outcome was poorly reported: One study reported no difference between groups. No standard deviation was reported. | |||||
| Myocardial infarction < 30 days | This outcome was not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level: one study with small sample size 2Downgraded one level due to risk of bias: incomplete outcome data 3Downgraded one level due to uncertainty in outcome measurement | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Stroke and death < 30days Show forest plot | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.32 [0.38, 29.23] |
| 2 Perioperative death and all strokes Show forest plot | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.14, 1.58] |

