Ultrasound‐guided arterial cannulation for paediatric patients
Abstract
This is a protocol for a Cochrane Review (Intervention). The objectives are as follows:
To assess the benefits and harms of using ultrasound guidance technique for arterial line placement in the paediatric population, as compared to other traditional techniques (palpation, Doppler auditory assistance, and others), at all potential sites for arterial cannulation (left or right radial, ulnar, brachial, femoral, or dorsalis pedis artery).
Background
Description of the condition
Arterial line cannulation is a common intervention performed in major surgeries and in the intensive care unit for continuous blood pressure monitoring and arterial blood sampling in children. Children are distinct from adults because of the size of their arteries. The most commonly used site for arterial cannulation is the radial artery, other sites include the femoral, axillary, brachial, ulnar, dorsal pedis, tibial posterior, and temporal arteries.
Description of the intervention
Many techniques for arterial cannulation have been described in the paediatric age group (Ueda 2013). These techniques include the use of palpation, ultrasound guidance, and Doppler auditory assistance.
Palpation of the pulse
Using pulse palpation as a landmark is the traditional approach for the insertion of an arterial catheter. The site of cannulation is usually selected, positioned and prepped. The artery is localized by palpating the pulse, and the procedure is initiated. Accurate localization of the small artery is technically difficult, especially in small children and infants (Varga 2013). This may complicate the placement and the threading of the catheter (Schindler 2005). The situation can be further complicated in case of dehydration or haemodynamic instability by making the pulse weak and difficult to find.
Ultrasound guidance
Ultrasound guidance is an alternative to the traditional palpation technique for the insertion of arterial catheters. It is commonly used for the placement of central venous catheters (CVCs). Numerous randomized controlled trials (RCTs) and meta‐analyses have found that the use of ultrasound reduces complications and increases first‐attempt success for CVC placement when compared with traditional landmark techniques (Hind 2003; Milling 2005; Randolph 1996). As for arterial cannulation, only one meta‐analysis studied the effect of ultrasound versus palpation and showed an improved first‐attempt success rate with the use of real‐time two‐dimensional ultrasound guidance (Shiloh 2011). This meta‐analysis gathered data from both adult and paediatric populations; therefore, the results cannot be extrapolated to paediatric patients only.
Doppler auditory assistance
Doppler auditory assistance has also been described as an alternative to the traditional palpation technique for the insertion of arterial catheters. The doppler tone changes to a higher pitch at the exact location of the artery which might facilitate arterial cannulation. The success rates using this technique were reported to be 46% (Ueda 2013)
Potential complications
Although rare, devastating complications from arterial line cannulation such as permanent ischaemic damage, sepsis and pseudoaneurysm formation may occur (Scheer 2002). Arterial occlusion, haematoma, or nerve injuries are seen more frequently (King 2008).
How the intervention might work
Intervention
Real‐time ultrasound guidance technique: using an out‐of‐plane technique, the artery is centred in the middle of the screen with the probe held with the left hand perpendicular to the skin. A cannula of an appropriate size is introduced with the right hand below the ultrasound probe at its centre while watching for tissue movement on the ultrasound screen. The cannula is redirected or the manoeuvre repeated until adequate arterial flow is obtained that allows easy insertion of the guidewire or the angiocath.
Comparator
Palpation technique: refers to the use of the nondominant hand palpating the artery, while the dominant hand manipulates the intravascular needle/catheter. The intravascular needle/catheter is inserted at a 30 to 45 degree angle and advanced slowly until pulsatile blood return is obtained. The outer catheter is then advanced into the artery directly from the needle or with the aid of a guidewire.
Doppler auditory assistance: the doppler probe identifies the artery by locating the area with the maximum sound. During the cannulation, the Doppler probe is used to identify the exact position of the artery, and guides the needle/catheter insertion.
Ultrasound guidance may improve the success rate and reduce potential complications of arterial line cannulation in children.
Why it is important to do this review
The importance of this Cochrane systematic review stems from the large number of arterial lines placed in the paediatric population undergoing major surgeries, or hospitalized in intensive care units, or both. UK guidelines for the placement of CVCs have recommended the use of an ultrasound‐guided technique, given the associated reduction in the rate of failure and mechanical complications (NICE 2002). The American Society of Anesthesiology task force has issued practice guidelines for central venous access in which they recommended the use of real‐time ultrasound guidance for vessel localization and venipuncture when the internal jugular vein is selected for cannulation (ASA 2012). The use of ultrasound for arterial line insertion has been controversial, as some studies advocate for its use (Schwemmer 2006), while others refute it (Ganesh 2009). There are no guidelines for ultrasound‐use for arterial line placement in the paediatric population. RCTs have been published on this topic (for example, Schwemmer 2006), but we have not identified a meta‐analysis for the paediatric population. This Cochrane systematic review will provide an objective assessment of the benefits and harms of using an ultrasound guidance technique for arterial line placement in the paediatric population, as compared to other traditional techniques (palpation, Doppler auditory assistance, and others). This will serve to assist doctors in making educated choices and reducing the potential complications that may stem from arterial line placement.
Objectives
To assess the benefits and harms of using ultrasound guidance technique for arterial line placement in the paediatric population, as compared to other traditional techniques (palpation, Doppler auditory assistance, and others), at all potential sites for arterial cannulation (left or right radial, ulnar, brachial, femoral, or dorsalis pedis artery).
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled clinical trials (RCTs).
Types of participants
We will limit participants of interest to paediatric patients, infants, and adolescents (one month to 18 years old) undergoing arterial line placement. We will exclude neonates.
Types of interventions
-
Ultrasound guidance
-
Palpation of the pulse
-
Doppler auditory assistance
Types of outcome measures
Primary outcomes
-
First‐attempt success rate
-
Rate of complications: i) haematoma, ii) Ischaemic damage
Secondary outcomes
-
Rate of successful cannulation
-
Time to successful cannulation
-
Number of attempts to successful cannulation
-
Number of cannulas used
-
Need for assistance by another operator (primary operator fails insertion and asks for help)
Search methods for identification of studies
Electronic searches
We will use the OVID platform to search the following sources from inception to the present: The Cochrane Library (CENTRAL), MEDLINE, and EMBASE. We will also search databases of ongoing trials (ClinicalTrials.gov (www.clinicaltrials.gov/), Current Controlled Trials metaRegister (www.controlled‐trials.com/), the EU Clinical Trials register (www.clinicaltrialsregister.eu/), and the WHO International Clinical Trials Registry Platform (http://apps.who.int/trialsearch/)). We will provide information, including trial identifier, about potentially relevant ongoing studies in the table ’Characteristics of ongoing studies’.
Please see Appendix 1 for our MEDLINE search.
We will continuously apply PubMed’s ’My NCBI’ (National Center for Biotechnology Information) email alert service for identification of newly published studies using a basic search strategy. We will perform a complete updated search on all specified databases four weeks before we submit the final review draft to the Cochrane Anesthesia Group for editorial approval. If we detect additional relevant key words during any of the electronic or other searches we will modify the electronic search strategies to incorporate these terms and document the changes. We will place no restrictions on the language of publication.
Searching other resources
We will try to identify other potentially eligible trials or ancillary publications by searching the reference lists of retrieved included trials, related systematic or other reviews, and health‐technology assessment reports.
Data collection and analysis
Selection of studies
Two review authors (CR, FF) will assess independently, and in duplicate, the abstract and title of every retrieved citation for potential eligibility. We will retrieve the full texts for all citations judged by at least one of the two authors as potentially eligible. The two authors will then assess the full texts for eligibility, in a duplicate and independent manner, using a standardized and pilot‐tested screening form (Appendix 2). They will then compare their results and resolve any disagreements by consensus, or with the help of a third author (MA), when needed. Before starting the selection process, CR and FF will conduct calibration exercises to ensure the validity of the process. We will present a PRISMA (preferred reporting items for systematic reviews and meta‐analyses) flowchart of study selection (Figure 1) (Liberati 2009). We will translate studies available in languages other than English, Arabic, or French.
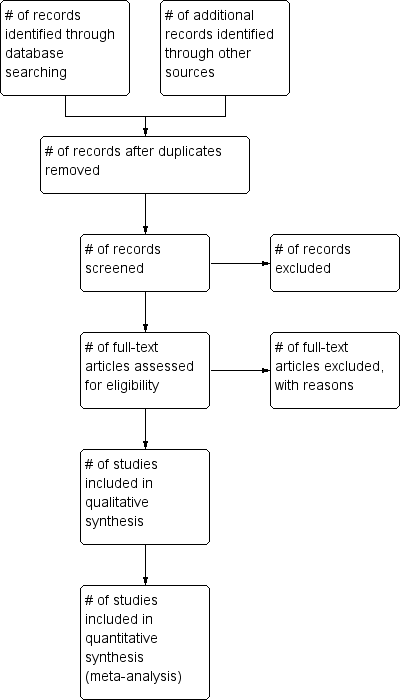
Study flow diagram.
Data extraction and management
Two reviewers (CR, FF) will independently, and in duplicate, abstract relevant data using standard data extraction forms. We will resolve any disagreements by discussion, or if required, by a third author (MA). We will seek relevant missing information on the trial from the primary author(s) of the article, if required.
We will abstract data on the characteristics of the population, intervention, control, and outcomes. We will also abstract statistical data needed for the meta‐analysis.
Dealing with duplicate publications and companion papers
In the event of duplicate publications, companion documents, or multiple reports of a primary study, we will maximize yield of information by collating all available data. We will attempt to resolve any remaining uncertainties by contacting the authors whenever possible.
Assessment of risk of bias in included studies
Two review authors (CR, FF) will assess the risk of bias of each included study, independently, and in duplicate. We will resolve disagreements by consensus, or by consultation with a third author (MA). We will assess risk of bias using The Cochrane Collaboration’s tool (Higgins 2011; Higgins 2011b). We will use the following domains.
-
Random sequence generation (selection bias)
-
Allocation concealment (selection bias)
-
Blinding of participants, providers, data collectors, outcome adjudicators, and data analysts (performance bias and detection bias)
-
Incomplete outcome data (attrition bias)
-
Selective outcome reporting (outcome reporting bias)
-
Other bias
We will assess outcome reporting bias (Kirkham 2010) by comparing the outcomes listed in a trial protocol, registration, and methods section, with the outcomes for which data are reported in the results section. We will judge risk of bias criteria as ’low risk’, ’high risk’, or ’unclear risk’ and evaluate individual bias items as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). For blinding of participants and personnel (performance bias), detection bias (blinding of outcome assessors), and attrition bias (incomplete outcome data) we intend to evaluate risk of bias separately for subjective and objective outcomes (Hróbjartsson 2013). We will consider the implications of missing outcome data from individual participants.
Measures of treatment effect
We will express dichotomous data as risk ratios (RRs) or hazard ratios (HRs) with 95% confidence intervals (CIs). We will express continuous data as mean differences (MDs) with 95% CIs when all studies report the outcome using the same scale, and as standardized mean difference when studies report the outcome using different scales.
Unit of analysis issues
The unit of analysis will be the individual patient. We will take into account the level at which randomizations occurred, such as cluster‐randomized trials and multiple observations for the same outcome.
Dealing with missing data
We will attempt to obtain relevant missing data from authors. If unsuccessful, we will use a complete case approach in the main analysis. We will then conduct sensitivity analyses using plausible assumptions about the outcomes of participants with missing outcome data to test the robustness of statistically significant results. For both continuous and dichotomous data, we will impute plausible treatment effects using progressively stringent criteria, as outlined in Akl 2013 and Ebrahim 2013.
Assessment of heterogeneity
We will assess statistical heterogeneity (inconsistency) by visual inspection of the forest plots and by using a standard Chi2 test with a significance level of 0.1. In view of the low power of this test, we will also consider the I2 statistic, which quantifies inconsistency across studies to assess the impact of heterogeneity on the meta‐analysis (Higgins 2002; Higgins 2003); where an I2 statistic of 50% or more indicates a considerable level of statistical heterogeneity (Higgins 2011).
In the event of a considerable level of statistical heterogeneity, we will conduct subgroup analyses to explore whether any clinical or methodological factor explains statistical heterogeneity (see Subgroup analysis and investigation of heterogeneity below). If the subgroup analysis identified a subgroup effect (i.e., statistical heterogeneity is explained), we will present the results stratified by the relevant subgroups. If the subgroup analysis does not identify a subgroup effect (i.e., statistical heterogeneity remains unexplained), we will not meta‐analyse the studies.
We expect the following characteristics to introduce clinical heterogeneity.
-
Expertise of the anaesthesiologist
-
Academic versus non‐academic setting
-
Age group of the patients (infant versus children versus adolescents)
-
Site of cannulation (radial or other arteries)
-
Expertise with ultrasound usage
-
Studies at low versus high risk of bias
Assessment of reporting biases
We will examine funnel plots to assess the potential for publication bias if we have 10 or more studies reporting on a particular outcome. As there are several explanations for funnel plot asymmetry we will interpret the results carefully (Sterne 2011).
Data synthesis
We will calculate the agreement between the two independent review authors for the assessment of eligibility using the kappa statistic. For categorical data, we will calculate the relative risk separately for each study for the event rate of outcomes by treatment arm. We will then pool the results of the different studies using a random‐effects model. For continuous data, we will pool data from different studies using random‐effects models with the inverse variance approach.
Subgroup analysis and investigation of heterogeneity
If we find heterogeneity, we will attempt to determine potential reasons by conducting subgroup analyses. We plan to conduct subgroup analyses, and investigate interaction, based on the following characteristics.
-
Expertise of the anaesthesiologist
-
Academic versus non‐academic setting
-
Age group of the patients (infant versus children versus adolescents)
-
Site of cannulation (radial or other arteries)
-
Expertise with ultrasound usage
Sensitivity analysis
We will perform sensitivity analyses in order to explore the influence of the following factors (when applicable) on effect sizes.
-
Restricting the analysis to published studies
-
Restricting the analysis to studies with low risk of bias
-
Making plausible assumptions about the outcome of participants with missing data
Summary of findings
We will grade the overall quality of the evidence for each outcome using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach (Guyatt 2011). The approach classifies the quality of evidence into four categories: high, moderate, low, and very low. It takes into account the study design as well as the following factors: risk of bias, imprecision, inconsistency, indirectness, publication bias, large effect size, dose‐response effect, and confounding. We will use the principles of the GRADE system to assess the quality of the body of evidence associated with the following specific outcomes in our review.
-
First‐attempt success rate
-
Rate of successful cannulation
-
Time to successful cannulation
-
Number of attempts to successful cannulation
-
Number of cannulas used
-
Need for assistance by another operator
-
Rate of complications: i) haematoma, ii) ischaemic damage
We will construct a 'Summary of findings' (SoF) table using the GRADE software.
The GRADE approach appraises the quality of a body of evidence based on the extent to which one can be confident that an estimate of effect or association reflects the item
being assessed. The quality of a body of evidence considers within‐study risk of bias (methodologic quality), the directness of the evidence, heterogeneity of the data, precision of effect estimates, and risk of publication bias.

