Fototerapia para la prevención del trastorno afectivo estacional
Resumen
Antecedentes
El trastorno afectivo estacional (TAE) es un patrón estacional de episodios depresivos graves y recurrentes que ocurre con más frecuencia durante el otoño o el invierno y remiten en primavera. La prevalencia del TAE varía del 1,5% al 9%, según la latitud. El aspecto estacional previsible del TAE brinda la posibilidad alentadora de la prevención. Esta revisión (una de cuatro revisiones sobre la eficacia y la seguridad de las intervenciones para prevenir el TAE) se centra en la fototerapia como una intervención preventiva. La fototerapia es un tratamiento no farmacológico en el que los pacientes se exponen a la luz artificial. La forma de administración (p.ej. visores, cajas de luz) y la forma de la luz (p.ej. luz blanca brillante) varían.
Objetivos
Evaluar la eficacia y la seguridad de la fototerapia (en comparación con ningún tratamiento, otros tipos de fototerapia, antidepresivos de segunda generación, melatonina, agomelatina, terapias psicológicas, intervenciones en el estilo de vida y generadores de iones negativos) para prevenir el TAE y mejorar los resultados centrados en el paciente en adultos con antecedentes de TAE.
Métodos de búsqueda
Una búsqueda en el registro especializado del Grupo Cochrane de Depresión, Ansiedad y Neurosis (Cochrane Depression, Anxiety and Neurosis Review Group [CCDANCTR]) incluyó todos los años hasta el 11 de agosto de 2015. El CCDANCTR contiene informes de ensayos controlados aleatorios relevantes derivados de EMBASE (1974 hasta la fecha), MEDLINE (1950 hasta la fecha), PsycINFO (1967 hasta la fecha) y el Registro Central Cochrane de Ensayos Controlad0s (CENTRAL). Además se buscó en Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Knowledge, The Cochrane Library y la Allied and Complementary Medicine Database (AMED) (hasta el 26 de mayo de 2014). También se realizó una búsqueda en la literatura gris y se realizaron búsquedas manuales en las listas de referencias de todos los estudios y artículos de revisión relevantes incluidos.
Criterios de selección
Para la eficacia se incluyeron los ensayos controlados aleatorios en adultos con antecedentes de TAE tipo invierno que no presentaban síntomas al comienzo del estudio. Para los eventos adversos también se planificó incluir estudios no aleatorios. Se intentó incluir los estudios que compararon cualquier tipo de fototerapia (p.ej. luz blanca brillante, administrada por visores o cajas de luz, luz infrarroja, estimulación al amanecer) versus ningún tratamiento / placebo, antidepresivos de segunda generación (ASG), terapias psicológicas, melatonina, agomelatina, cambios en el estilo de vida, generadores de iones negativos u otras de las fototerapias ya mencionadas. También se planificó incluir los estudios que consideraron la fototerapia en combinación con cualquier intervención de comparación y compararon esta combinación con la misma intervención de comparación como monoterapia.
Obtención y análisis de los datos
Dos autores de la revisión examinaron los resúmenes y las publicaciones de texto completo frente a los criterios de inclusión. Dos autores de la revisión, de forma independiente, extrajeron los datos y evaluaron el riesgo de sesgo de los estudios incluidos.
Resultados principales
Se identificaron 2986 citas después de extraer los duplicados de los resultados de la búsqueda. Se excluyeron 2895 registros durante la revisión del título y el resumen. Se evaluaron 91 artículos de texto completo para inclusión en la revisión, pero solamente un estudio que proporcionó datos de 46 pacientes cumplió con los criterios de elegibilidad. El ensayo controlado aleatorio (ECA) incluido tuvo limitaciones metodológicas. Se consideró de alto riesgo de sesgo de realización y de detección debido a la falta de cegamiento y de alto riesgo de sesgo de desgaste porque los autores del estudio no informaron los motivos de los abandonos y no integraron los datos de los abandonos en el análisis.
El ECA incluido comparó el uso preventivo de luz blanca brillante (2500 lux mediante visores), luz infrarroja (0,18 lux mediante visores) y ninguna fototerapia. En general, ambas formas de fototerapia preventiva redujeron numéricamente la incidencia de TAE en comparación con ninguna fototerapia. En total, el 43% (6/14) de los participantes del grupo de luz brillante desarrollaron TAE, así como el 33% (5/15) del grupo de luz infrarroja y el 67% (6/9) del grupo ningún tratamiento. La fototerapia con luz brillante redujo el riesgo de incidencia de TAE en el 36%; sin embargo, el intervalo de confianza (IC) del 95% fue muy amplio e incluyó tamaños posibles de efecto a favor de la fototerapia con luz brillante y a favor de ninguna fototerapia (cociente de riesgos [CR] 0,64; IC del 95%: 0,30 a 1,38). La luz infrarroja redujo el riesgo de TAE en el 50% en comparación con ninguna fototerapia, pero en este caso también el IC fue demasiado amplio para permitir estimaciones precisas del tamaño del efecto (CR 0,50; IC del 95%: 0,21 a 1,17). La comparación de ambas formas de fototerapia preventiva entre sí produjo tasas similares de incidencia de episodios depresivos en ambos grupos (CR 1,29; IC del 95%: 0,50 a 3,28). La calidad de las pruebas para todos los resultados fue muy baja. Las razones de la disminución de la calidad de las pruebas incluyeron alto riesgo de sesgo del estudio incluido, imprecisión y otras limitaciones como la autocalificación de los resultados, la falta de verificación del cumplimiento durante todo el estudio y el informe insuficiente de las características de los participantes.
Los investigadores no aportaron datos sobre los eventos adversos. No fue posible encontrar estudios que compararan fototerapia versus otras intervenciones de interés como ASG, terapias psicológicas, melatonina o agomelatina.
Conclusiones de los autores
Las pruebas sobre la fototerapia como tratamiento preventivo para los pacientes con antecedentes de TAE son limitadas. Las limitaciones metodológicas y el tamaño pequeño de la muestra del único estudio disponible han impedido que los revisores establezcan conclusiones sobre los efectos de la fototerapia en el TAE. Debido a que las pruebas comparativas de la fototerapia versus otras opciones preventivas son limitadas, la decisión a favor o en contra de iniciar el tratamiento preventivo del TAE y el tratamiento seleccionado se deben basar firmemente en las preferencias de los pacientes.
PICOs
Resumen en términos sencillos
Fototerapia para la prevención de la depresión de invierno
¿Por qué es importante esta revisión?
Muchas personas en las latitudes septentrionales sufren de tristeza durante el invierno, que se presenta como una reacción a la reducción de la luz solar. Tres cuartas partes de los afectados son mujeres. La letargia, la sobrealimentación, la necesidad imperiosa de carbohidratos y el estado de ánimo deprimido son síntomas frecuentes. En algunas personas, la tristeza del invierno se convierte en depresión, que afecta seriamente sus vidas cotidianas. Hasta dos terceras partes presentan síntomas depresivos cada invierno.
¿Quién estará interesado en esta revisión?
Alguna persona que ha experimentado depresión de invierno, o que tiene familiares y amigos que han experimentado depresión de invierno.
¿Qué preguntas pretende contestar esta revisión?
Debido al patrón estacional y la alta tasa de recurrencia, la fototerapia durante los meses de otoño e invierno podría ayudar a prevenir la aparición del estado de ánimo deprimido. El objetivo de esta revisión fue determinar si la fototerapia puede prevenir la aparición de la depresión en el invierno cuando se utiliza en pacientes sanos con antecedentes de depresión de invierno, y si es segura. Hasta la fecha, esta pregunta no se ha examinado de manera sistemática, pero es importante para los que han presentado depresión de invierno.
¿Qué estudios se incluyeron en la revisión?
Se efectuaron búsquedas en las bases de datos hasta agosto de 2015 de estudios sobre fototerapia para prevenir la depresión de invierno. Entre 2986 registros se encontró un estudio controlado aleatorio que incluyó 46 pacientes que recibieron fototerapia o ningún tratamiento. Todos los pacientes en estos estudios tenían antecedentes de depresión de invierno.
¿Qué revelan las pruebas de la revisión?
La calidad de las pruebas de todos los resultados fue muy baja, por lo que no fue posible establecer conclusiones acerca de si la fototerapia es eficaz para prevenir la depresión de invierno. El estudio incluido no proporcionó información sobre los efectos secundarios de la fototerapia.
Los médicos deben analizar con los pacientes que consideran el tratamiento preventivo las ventajas y desventajas de la fototerapia y otros tratamientos potencialmente preventivos para la depresión de invierno, como la farmacoterapia, las terapias psicológicas o las intervenciones sobre el estilo de vida. Como no hay estudios disponibles que hayan comparado estos tratamientos, hay que considerar las preferencias de los pacientes.
¿Qué debe suceder a continuación?
Los revisores recomiendan que los estudios futuros comparen directamente la fototerapia versus otros tratamientos como la farmacoterapia, las terapias psicológicas o las intervenciones sobre el estilo de vida para determinar el mejor tratamiento para la prevención de la depresión de invierno.
Authors' conclusions
Summary of findings
| Bright white light therapy compared with no light therapy for prevention of SAD | ||||||
| Patient or population: All participants were known SAD patients who had been successfully treated with conventional light therapy in previous winters | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No light therapy | Light therapy | |||||
| Incidence of SAD (SIGH‐SAD score ≥ 20) (follow‐up 26 weeks) | Low | RR 0.64 | 23 | ⊕⊝⊝⊝ | ||
| 300 per 1000 | 192 per 1000 | |||||
| Moderate | ||||||
| 500 per 1000 | 320 per 1000 (150 to 690) | |||||
| High | ||||||
| 600 per 1000 | 276 per 1000 (210 to 966) | |||||
| Incidence of severe SAD (SIGH‐SAD‐SR (≥ 40)) (follow‐up 26 weeks) | Study population | RR 0.21 | 23 | ⊕⊝⊝⊝ | ||
| 333 per 1000 | 70 per 1000 | |||||
| Overall discontinuation (follow‐up 26 weeks) | Study population | RR 2.22 | 28 | ⊕⊝⊝⊝ | ||
| 100 per 1000 | 222 per 1000 | |||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded 2 steps because of severe risk of bias due to non‐blinding and unclear randomisation process and allocation concealment; no intention‐to‐treat analysis was reported, outcomes were self rated, compliance throughout study duration was not checked and participant characteristics were not reported comprehensively bDowngraded 1 step because of small sample size (lack of power and random error could have influenced results) | ||||||
| Infrared light therapy compared with no light therapy for prevention of SAD | ||||||
| Patient or population: All participants were known SAD patients who had been successfully treated with conventional light therapy in previous winters | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No light therapy | Infrared light therapy | |||||
| Incidence of SAD (SIGH‐SAD score ≥ 20) (follow‐up 26 weeks) | Low | RR 0.50 | 24 | ⊕⊝⊝⊝ | ||
| 300 per 1000 | 150 per 1000 (63 to 351) | |||||
| Moderate | ||||||
| 500 per 1000 | 250 per 1000 (105 to 585) | |||||
| High | ||||||
| 600 per 1000 | 300 per 1000 (126 to 702) | |||||
| Incidence of severe SAD (SIGH‐SAD‐SR (≥ 40)) (follow‐up 26 weeks) | Study population | RR 0.20 | 24 | ⊕⊝⊝⊝ | ||
| 333 per 1000 | 67 per 1000 | |||||
| Overall discontinuation (follow‐up 26 weeks) | Study population | RR 1.67 | 28 | ⊕⊝⊝⊝ | ||
| 100 per 1000 | 167 per 1000 | |||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded 2 steps because of severe risk of bias due to non‐blinding and unclear randomisation process and allocation concealment; no intention‐to‐treat analysis was reported, outcomes were self rated, compliance throughout study duration was not checked and participant characteristics were not reported comprehensively bDowngraded 1 step because of small sample size (lack of power and random error could have influenced results) | ||||||
| Light therapy (bright white or infrared) compared with no light therapy for prevention of SAD | ||||||
| Patient or population: All participants were known SAD patients who had been successfully treated with conventional light therapy in previous winters | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No light therapy | Infrared light therapy | |||||
| Incidence of SAD (SIGH‐SAD score ≥ 20) (follow‐up 26 weeks) | Low | RR 0.57 | 38 | ⊕⊝⊝⊝ | ||
| 300 per 1000 | 171per 1000 (90 to 330) | |||||
| Moderate | ||||||
| 500 per 1000 | 285 per 1000 (150 to 550) | |||||
| High | ||||||
| 600 per 1000 | 342 per 1000 (180 to 660) | |||||
| Incidence of severe SAD (SIGH‐SAD‐SR (≥ 40)) (follow‐up 26 weeks) | Study population | RR 0.21 | 38 | ⊕⊝⊝⊝ | ||
| 333 per 1000 | 70 per 1000 | |||||
| Overall discontinuation (follow‐up 26 weeks) | Study population | RR 1.94 | 46 | ⊕⊝⊝⊝ | ||
| 100 per 1000 | 194 per 1000 | |||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded 2 steps because of severe risk of bias due to non‐blinding and unclear randomisation process and allocation concealment; no intention‐to‐treat analysis was reported, outcomes were self rated, compliance throughout study duration was not checked and participant characteristics were not reported comprehensively bDowngraded 1 step because of small sample size (lack of power and random error could have influenced results) | ||||||
| Bright white light therapy compared with infrared light therapy for prevention of SAD | ||||||
| Patient or population: All participants were known SAD patients who had been successfully treated with conventional light therapy in previous winters | ||||||
| Outcomes | Risk in both groups | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk in this treatment group | Risk in this treatment group | |||||
| Infrared light therapy | Bright white light therapy | |||||
| Incidence of SAD (SIGH‐SAD score ≥ 20) (follow‐up 26 weeks) | Study population | RR 1.29 | 29 | ⊕⊝⊝⊝ | ||
| 333 per 1000 | 357 per 1000 | |||||
| Incidence of severe SAD (SIGH‐SAD‐SR (≥ 40)) (follow‐up 26 weeks) | Study population | RR 1.07 | 29 | ⊕⊝⊝⊝ | ||
| 67 per 1000 | 71 per 1000 | |||||
| Overall discontinuation (follow‐up 26 weeks) | Study population | RR 1.33 | 36 | ⊕⊝⊝⊝ | ||
| 167 per 1000 | 222 per 1000 | |||||
| CI: Confidence interval; RCT: Randomised controlled trial; RR: Risk ratio, SIGH‐SAD‐SR: Structured Interview Guide for the Hamilton Depression Rating Scale‐Seasonal Affective Disorders self rating version | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded 2 steps because of severe risk of bias due to non‐blinding and unclear randomisation process and allocation concealment; no intention‐to‐treat analysis was reported, outcomes were self rated, compliance throughout study duration was not checked and participant characteristics were not reported comprehensively bDowngraded 1 step because of small sample size (lack of power and random error could have influenced results) | ||||||
Background
Description of the condition
Seasonal affective disorder (SAD) is a seasonal pattern of recurrent major depressive episodes that most commonly occurs during autumn or winter and remits in spring or summer (Rosenthal 1984). In addition to the predictable seasonal pattern of depression, persons suffering from SAD commonly experience atypical symptoms including hypersomnia, carbohydrate craving with increased appetite and weight gain and extreme fatigue (Sohn 2005). Prevalence in the United States ranges from 1.5% in southern Florida to 9% in northern regions (Rosen 1990). In northern latitudes, the prevalence of SAD is estimated to be about 10% (Byrne 2008). SAD is a multi‐factorial condition. Chronobiological mechanisms related to circadian rhythms, melatonin, serotonin turnover and photoperiodism (length of dark hours relative to light hours in a 24‐hour period) are all thought to play a role in SAD (Ciarleglio 2011; Levitan 2007). A quintessential and especially harmful quality of this illness is its high risk of recurrence and persistence. Approximately two‐thirds of those diagnosed with SAD will face recurrence of these distressing symptoms the following winter (Rodin 1997). In the five to 11 years following initial diagnosis, 22% to 42% of patients still suffer from SAD, and 33% to 44% develop a non‐seasonal pattern in subsequent episodes; the disorder resolves completely in only 14% to 18% of patients (Magnusson 2005; Schwartz 1996). Indeed, many patients who suffer from SAD experience this type of depression every year, which makes it particularly amenable to preventive treatment (Westrin 2007).
Description of the intervention
Various interventions such as second‐generation antidepressants (SGAs), light therapy, melatonin or agomelatine, psychological therapies and lifestyle interventions have been used for prevention of SAD. Of those, light therapy (e.g. bright white light, dawn simulation) is a non‐pharmacological treatment that has proved effective and is often used as first‐line therapy for individuals with SAD (Terman 2005). It is commonly applied with use of a light box; however, application with a light visor (a portable head‐mounted light source) is possible (Pail 2011). To achieve an effect on circadian rhythms, the dosage of bright light given should be greater than the artificial lighting usually used in homes ‐ about 5000 lux per day (2500 lux for two hours, or 10,000 lux for 30 minutes) (Levitan 2005). Dawn simulation, on the other hand, increases light exposure from 0 to around 200 to 300 lux, over 1.5 to 2.5 hours (Golden 2005). A recent meta‐analysis found that the odds ratio (OR) for remission was similar to that of many pharmaceutical treatments for depression (OR 2.9, 95% confidence interval (CI) 1.6 to 5.4) (Golden 2005). Patients should be treated with light therapy units that are specifically designed to treat SAD with the goal of achieving strong response. Otherwise, these units may not provide adequate brightness and may not allow appropriate ultraviolet light filtration (Levitan 2005). Patients do not need to stare directly into the light (Pail 2011). However, it is important that the light meets the eye because it is hypothesised that the effect of light therapy is mediated through the eyes by retinal cells that are not part of the visual system (Pail 2011). Other forms of light therapy (e.g. infrared light) are available, but their effectiveness for patients with SAD is not known.
How the intervention might work
Much research into the origin of SAD has focused on the role of circadian rhythms and melatonin (Lam 2006). Decreased seasonal exposure to light through phase shifts in circadian rhythms, resulting in alterations of serotonin metabolism, is thought to be a reason for development of SAD. The circadian system is influenced primarily by the zeitgeber light, and exposure to light acts as a signal for the circadian clock (Quera‐Salva 2011). As a consequence, light therapy has been studied intensively as treatment for SAD (Partonen 1998). Underlying hypotheses on the pathophysiology of SAD, such as the depressogenic effects of melatonin, support the rationale for light therapy. Light therapy helps to suppress the release of melatonin and lengthens the photoperiod (Golden 2005). Timing, duration and intensity play an important role in light therapy. Studies have shown that light therapy is most effective when administered early in the day (Levitan 2005) because the typical depressed patient is phase‐delayed, and therapy administered early in the morning regulates the circadian pattern of melatonin secretion. However, in some patients, evening light therapy may be more successful, because phase‐advanced individuals may benefit more from the corrective phase delay provided by evening light therapy (Lewy 1987; Lewy 2006). Seasonal recurrence of depressive episodes provides the rationale for light therapy provided as preventive treatment for SAD.
Why it is important to do this review
The predictable seasonal aspect of SAD provides a specific and promising opportunity for prevention. However, both patients and clinicians face much uncertainty in their collaborative decisions about the choice of a preventive intervention (Westrin 2007). Although a recent Cochrane review assessed the efficacy and risk of harms of light therapy compared with SGAs for short‐term treatment of SAD (Thaler 2010), to date no review has determined the efficacy, effectiveness and risk of harms of light therapy for preventing recurrent SAD.
Our findings are intended to provide insights into (1) available evidence on the benefits and harms of competing interventions in the prevention of SAD, with respect to patient‐centred outcomes, and (2) gaps in the evidence base that will inform future research needs.
This is one of four reviews of interventions to prevent SAD. The others focus on SGAs (Gartlehner 2014), agomelatine and/or melatonin (Kaminski‐Hartenthaler 2014) and psychological therapies (Forneris 2014) as preventive interventions.
Objectives
To assess the efficacy and safety of light therapy (in comparison with no treatment, other types of light therapy, second‐generation antidepressants, melatonin, agomelatine, psychological therapies, lifestyle interventions and negative ion generators) in preventing SAD and improving patient‐centred outcomes among adults with a history of SAD.
Methods
Criteria for considering studies for this review
Types of studies
Efficacy (beneficial effects)
We included randomised controlled trials (RCTs; including cross‐over studies and cluster‐randomised trials) on light therapy for prevention of SAD.
Adverse effects
We planned to include the following.
-
RCTs (including cross‐over studies and cluster‐randomised trials) of light therapy for prevention of SAD.
-
Non‐randomised controlled studies such as non‐randomised trials, prospective cohort studies or case‐control studies of light therapy for prevention of SAD.
Types of participants
Participant characteristics
Male and female adults (≥ 18 years of age) of all races, ethnicities and cultural groups, with a history of SAD, who do not fulfil the criteria for a current major depressive episode.
Diagnosis
We defined SAD according to the Diagnostic and Statistical Manual of Mental Disorders (DSM‐5) (APA 2013) as a seasonal pattern of recurrent major depressive episodes. However, we restricted our focus to winter‐type SAD (i.e. major depression in the autumn/winter with full remission in the spring/summer), and we did not include patients with bipolar disorder with a seasonal pattern. We included studies that used definitions from prior versions of the DSM (APA 1980; APA 1987; APA 2000).
Co‐morbidities
We excluded studies that enrolled participants with depressive disorder due to another medical condition. We planned to include populations at risk of SAD with common co‐morbidities (e.g. diabetes, cardiovascular disease) that are not the cause of the depressive episode.
Setting
We included studies conducted in all settings.
Subset data
We intended to include studies that provided data on subsets of participants of interest, as long as the subset met our eligibility criteria. We did not include studies with 'mixed' populations if investigators did not adequately stratify data with respect to our population of interest.
Types of interventions
Experimental interventions
We included the following forms of light therapy.
-
Bright white light.
-
Infrared light.
-
Dawn simulation.
We did not limit light therapy in terms of dosage, mode of delivery or duration. We intended to include combination therapies of light therapy with any of the comparator interventions listed below. We did not limit light therapy in terms of dosage or duration.
Comparator interventions
We planned to compare any light therapy with:
-
another light therapy from the list above;
-
placebo, no treatment or waiting list;
-
second‐generation antidepressants;
-
melatonin or agomelatine;
-
psychological therapies;
-
lifestyle interventions (e.g. exercising, making the environment sunnier (open blinds), spending regular time outside, adapting nutrition (consuming a low‐fat diet, reducing refined sugars)); and
-
negative ion generators.
We also planned to compare light therapy in combination with any of the comparator interventions listed above with the same comparator intervention as monotherapy (see Data extraction and management).
Types of outcome measures
We included studies that met the above inclusion criteria regardless of whether they reported on the following outcomes. In consultation with clinical experts, we selected the following outcomes a priori.
Primary outcomes
1. The primary outcome for benefit was the incidence of SAD, measured as the proportion of participants with a SIGH‐SAD (Structured Interview Guide for the Hamilton Depression Rating Scale, Seasonal Affective Disorders (Williams 2002)) score of 20 or higher.
2. The primary outcome for harms was the overall rate of adverse events related to preventive interventions.
Secondary outcomes
3. Severity of the SAD episode or SAD‐related symptoms, as measured by a validated tool (e.g. Hamilton Depression Rating Scale (Hamilton 1960)).
4. Quality of life, as measured by a validated quality of life tool (e.g. Short Form (SF)‐36 (Ware 1992)).
5. Quality of interpersonal and social functioning, as measured by a validated tool (e.g. the Range of Impaired Functioning Tool (LIFE–RIFT) (Leon 1999)).
6. Proportion of participants with serious adverse events.
7. Rates of discontinuation of preventive intervention due to adverse events.
8. Overall rate of discontinuation.
Timing of outcome assessment
Depending on available data, we planned to synthesise outcomes at different time points (i.e. short‐term, medium‐term and long‐term) throughout an entire six‐month period of risk during an autumn‐winter season.
Hierarchy of outcome measures
Our main focus was patient‐centred outcomes (i.e. outcomes that patients notice and care about). If several measures assessed the same outcome, we consulted a priori with clinical experts regarding the validity and reliability of individual outcome measures and prioritised accordingly.
Search methods for identification of studies
The Cochrane Depression, Anxiety and Neurosis Group (CCDAN) maintains two clinical trials registers at its editorial base in Bristol, UK: a references‐based register and a studies‐based register. The CCDAN Specialised Register (CCDANCTR)‐References contains more than 39,000 reports of randomised controlled trials (RCTs) on depression, anxiety and neurosis. Approximately 60% of these references have been tagged to individual, coded trials. The coded trials are held in the Specialised CCDANCTR‐Studies Register, and records are linked between the two registers through the use of unique Study ID tags. Coding of trials is based on the EU‐Psi coding manual and use of a controlled vocabulary (the CCDAN Trials Search Co‐ordinator can provide further details). Reports of trials for inclusion in the Group Registers are collated from routine (weekly), generic searches of MEDLINE (1950‐), EMBASE (1974‐) and PsycINFO (1967‐); quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL); and review‐specific searches of additional databases. Reports of trials are also obtained from international trials registers through trials portals of the World Health Organization (the International Clinical Trials Registry Platform (ICTRP)) and pharmaceutical companies and by handsearching of key journals, conference proceedings and other (non‐Cochrane) systematic reviews and meta‐analyses.
Details of CCDAN's generic search strategies (used to identify RCTs) can be found on the Group website.
Electronic searches
-
The CCDAN Trials Search Co‐ordinator (TSC) ran an initial search of the Specialised Registers (CCDANCTR‐Studies and CCDANCTR‐References) (all years to 12 April 2013) using terms for conditions only.
-
-
("seasonal affective disorder*" or "seasonal depression" or "seasonal mood disorder*" or "winter depression" or SIGH‐SAD*).
-
-
-
Updated searches were performed to 11 August 2015.
-
-
-
On both occasions, we screened search results for reports of trials involving light therapy.
-
-
In addition, we conducted our own searches of the following electronic databases (to 26 May 2014) to ensure that no studies had been missed by the CCDANCTR (Appendix 1).
-
-
International Pharmaceutical Abstracts.
-
CINAHL (Cumulative Index to Nursing and Allied Health Literature).
-
Web of Knowledge (includes Web of Science, Current Contents Connect, Conference Proceedings Citation Index, BIOSIS, Derwent Innovations Index, Data Citation Index, SciELO Citation Index).
-
The Cochrane Library.
-
AMED (Allied and Complementary Medicine Database).
-
-
We searched international trials registries via the World Health Organization trials portal (ICTRP) and ClinicalTrials.gov to identify unpublished and ongoing studies. The CCDAN TSC searched these registries again to 11 August 2015.
We did not restrict searches by date, language or publication status.
Searching other resources
Grey literature
To detect additional studies, we checked the following sources.
-
IFPMA (International Federation of Pharmaceutical Manufacturers and Associations) Clinical Trials Portal.
-
OpenGrey.
-
GreyMatters.
-
National Institute of Health RePORTER.
-
Health Services Research Projects in Progress (HSRPROJ).
-
Hayes Inc. Health Technology Assessment.
-
The New York Academy of Medicine Grey Literature Index.
-
Conference Papers Index.
-
National Registry of Evidence‐Based Programs and Practices (NREPP).
Reference lists
We handsearched the references of all included studies and pertinent review articles.
Correspondence
We contacted trialists and subject matter experts to ask for information on unpublished and ongoing studies, or to request additional trial data.
Data collection and analysis
Selection of studies
Two review authors independently screened the titles and abstracts of all studies identified by the searches. We retrieved full‐text copies of all studies that potentially met the inclusion criteria as determined by this initial assessment, and two review authors independently screened them to determine their eligibility.
If the two review authors did not reach consensus, they discussed disagreements and resolved them through consultation with a third party. We contacted study authors if relevant information was missing. We tracked all results in an EndNote X5 database.
We recorded the selection process in sufficient detail to complete a PRISMA (Preferred Reporting Items for Systematic Reviews and Meta‐Analyses) flow diagram and Characteristics of included studies tables.
Data extraction and management
We used a data collection form. Two review authors independently extracted study characteristics and outcome data from included studies (JW, BN). We resolved discrepancies by reaching consensus or by involving another review author. We reported whether studies were detected by a search of databases of published studies, by handsearch or by a search of grey literature.
We extracted the following study characteristics.
-
Methods: study design, duration of study, details of any 'run‐in' period, duration of treatment period, number of study centres and locations, study settings, withdrawals and dates of studies.
-
Participants: number of participants, mean age, age range, proportion of women, number of prior depressive episodes, diagnostic criteria, inclusion criteria and exclusion criteria.
-
Interventions: intervention, comparison, concomitant interventions and excluded interventions.
-
Outcomes: primary and secondary outcomes specified and collected and time points reported.
-
Notes: funding for studies and notable conflicts of interest of study authors.
We noted in the Characteristics of included studies table if outcome data were not reported in a useable way. We resolved disagreements by reaching consensus or by involving a third person (BG). One review author (BN) transferred data into the Review Manager file (RevMan 2012). We double‐checked that data were entered correctly by comparing data presented in the systematic review versus the study reports. A second review author (AG) spot‐checked study characteristics for accuracy against the trial report.
Main planned comparisons
-
Light therapy versus placebo, no treatment or waiting list.
-
Light therapy versus other light therapy.
-
Light therapy versus second‐generation antidepressants.
-
Light therapy versus melatonin or agomelatine.
-
Light therapy versus psychological therapies.
-
Light therapy versus lifestyle intervention.
-
Light therapy versus negative ion generators.
-
Light therapy + comparator intervention (as listed in Types of interventions) versus placebo or no treatment control group or waiting list.
-
Light therapy + comparator intervention (as listed in Types of interventions) versus the same comparator intervention as monotherapy (e.g. light therapy + psychological therapy vs psychological therapy alone).
Assessment of risk of bias in included studies
Two review authors (JW, BN) independently assessed risk of bias of included randomised trials using the Cochrane 'Risk of bias' tool, as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). This tool includes assessment of random sequence generation; allocation concealment; blinding of participants, personnel and outcome assessors; incomplete outcome data; selective reporting and other potential threats to validity. Specifically, we assessed attrition in these trials and reasons for attrition, particularly when attrition rates between two groups in a trial differed substantially. In addition, we assessed whether all relevant outcomes for the trial were reported in the published articles. We assigned each domain high risk of bias, low risk of bias or unclear risk of bias.
For non‐randomised studies, we planned to use the Newcastle‐Ottawa Scale, involving selection of cases or cohorts and controls, adjustment for confounders, methods of outcome assessment, length of follow‐up and statistical analysis (Wells 2009). Review authors resolved discrepancies by reaching consensus or by consulting with a third review author.
Measures of treatment effect
We used data extracted from the original studies to construct 2 × 2 tables for dichotomous outcomes. When multiple studies allowed for quantitative analysis, we planned to calculate the risk ratio (RR) with 95% confidence intervals (CIs) for each outcome. We chose risk ratio as an effect measure because for decision makers, risk ratios are easier to interpret than odds ratios, particularly when event rates are high.
We planned to pool continuous data using the mean difference (MD) if an outcome was measured on the same scale, or the standardised mean difference (SMD) if an outcome was measured on different scales. If available, we intended to use final measurements rather than changes from baseline to estimate differences between treatments. When it was considered necessary to use both change and post‐intervention scores within a comparison, we would have presented these by subgroup using the MD rather than the SMD.
For time‐to‐event data, we planned to calculate a pooled hazard ratio when this was available, or to dichotomise data at multiple time points into response/no response (e.g. at one week, at two weeks, at four weeks, etc.).
We intended to use the same time points as specified under 'Timing of outcomes assessment' to form the basis for dichotomisation into response/no response.
For non‐randomised studies, we planned to use adjusted treatment effects if available.
Unit of analysis issues
Cluster‐randomised trials
To incorporate cluster‐randomised trials, we intended to reduce the size of each trial to its 'effective sample size'. If intracluster correlation coefficients had not been reported, we planned to find external estimates from similar studies. We intended to undertake sensitivity analysis to assess the impact of including such trials.
Cross‐over trials
To avoid carry‐over effects, we planned to include data only from the first period of cross‐over studies.
Studies with multiple treatment groups
For included trials that consisted of multiple treatment groups (e.g. differing dosing regimens of light therapy), we planned to include data for the treatment arms and to halve the data from the placebo arm, or to collapse the data for different doses into one group when this was clinically appropriate (Hansen 2009).
Dealing with missing data
We used intention‐to‐treat (ITT) analysis when data were missing for participants who dropped out of trials before completion. We calculated two ITT analyses: one assuming that all dropouts developed SAD, the other assuming that all dropouts stayed free of depressive symptoms. When data regarding an outcome of interest were not reported, we planned to contact the authors of publications to obtain missing results, as long as the study was published over the past 20 years. We documented all correspondence with trialists and reported responses in the full review.
Assessment of heterogeneity
We planned to use the Cochran Chi2 test (Q‐test) to assess heterogeneity. A P value less than 0.10 is considered statistically significant. We planned to use the I2 statistic to estimate the degree of heterogeneity. This measure describes the percentage of total variation across studies that results from heterogeneity rather than from chance. We planned to interpret the importance of any heterogeneity in terms of its magnitude and direction of effects. We planned to not consider thresholds; instead we intended to adopt the overlapping bands, as suggested in the Cochrane Handbook for Systematic Reviews of Interventions. For example, we planned to consider an I2 value between 0% and 40% as probably not important, between 30% and 60% as representing moderate heterogeneity, between 50% and 90% as representing substantial heterogeneity and between 75% and 100% as representing considerable heterogeneity (Higgins 2011).
Assessment of reporting biases
If we had found more than 10 studies, we planned to perform a funnel plot analysis. A funnel plot is a graph used to detect publication bias. We intended to look at whether the largest studies were near the average and small studies spread on both sides of the average. Variations from this assumption can indicate the existence of publication bias, but asymmetry may not necessarily be caused by publication bias. In addition, we planned to use Kendell's tau (Begg 1994), Egger's regression intercept (Egger 1997) and Fail‐Safe N (Rosenthal 1979) to assess reporting biases.
Data synthesis
We analysed data using Review Manager software (RevMan 2012). We planned to pool data for meta‐analysis when participant groups were similar, and when studies assessed the same treatments with the same comparator and had similar definitions of outcome measures over a similar duration of treatment.
In general, we planned to use random‐effects models to combine results because we did not expect the true effect to be the same for all included studies. We intended to also employ fixed‐effect models to determine differences in treatment effects between random‐effects and fixed‐effect results. Studies would have been weighted using the Mantel‐Haenszel method. We rated the strength of the evidence using the system developed by the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) Working Group (GRADEpro 2015).
We planned to perform qualitative analysis of data on adverse effects by comparing crude rates. We planned to conduct quantitative analysis of the rates of adverse effects only if we located a sufficient number of prospective observational studies or randomised trials that gathered data on adverse effects that were suitable for pooling.
Subgroup analysis and investigation of heterogeneity
Sex, age, history of non‐seasonal major depressive episodes and psychiatric co‐morbidities are potential effect measure modifiers for prevention of SAD. Timing, duration, type and intensity of light therapy may also modify the preventive effect on SAD. If data were sufficient, we would have conducted subgroup analyses for the primary outcome measures. Subgroup analyses should be performed and interpreted with caution because multiple analyses could lead to false‐positive conclusions. We planned to conduct subgroup analyses based on:
-
men versus women;
-
history of non‐seasonal major depressive episodes versus no history of non‐seasonal major depressive episodes;
-
younger than 65 years of age versus 65 years of age older; and
-
Axis I, Axis II co‐morbidities versus no Axis I, Axis II co‐morbidities.
Sensitivity analysis
Sensitivity analyses were conducted to test the robustness of decisions made during the review process.
We planned to conduct sensitivity analyses:
-
excluding small studies (i.e. studies with fewer than 30 participants);
-
excluding studies with high risk of bias (i.e. studies that had been rated as high risk of bias in one or more domains);
-
excluding studies published only in abstract form;
-
with adjusted versus unadjusted results; and
-
excluding cluster‐randomised trials.
'Summary of findings' tables
We assessed the quality of the evidence using the GRADE approach and presented the results in 'Summary of findings' tables for our main comparisons and outcomes (as listed in Types of outcome measures). We did not expect to be able to stratify populations into low‐, medium‐ or high‐risk populations. For 'assumed risk', we used prevalence studies from countries in northern latitudes (e.g. Scandinavia, Canada, northern United States) in which SAD leads to substantial burden of disease.
We used the GRADEpro Guideline Development Tool to rate the quality of evidence and to prepare the 'Summary of findings' tables (GRADEpro 2015).
Results
Description of studies
Results of the search
We identified 2986 citations through electronic searches and reviews of reference lists after de‐duplication of search results. We excluded 2895 records during title and abstract reviews. We included 91 articles for full‐text review, of which one publication met eligibility criteria for this review. We excluded most of the 91 articles because the intervention did not meet our eligibility criteria; in most studies, participants already had depressive symptoms when the therapeutic intervention was started. Our focus was on prevention. Therefore, we included only studies that included patients with a history of SAD who were free of symptoms at the beginning of the study. Another major reason for exclusion was that patients had major depressive disorder rather than SAD, and that the study design did not match our inclusion criteria (e.g. studies without a control group). The PRISMA flow chart (Figure 1) documents the disposition of the literature in this review. Under Excluded studies, we describe the reasons for excluding these studies in greater detail.
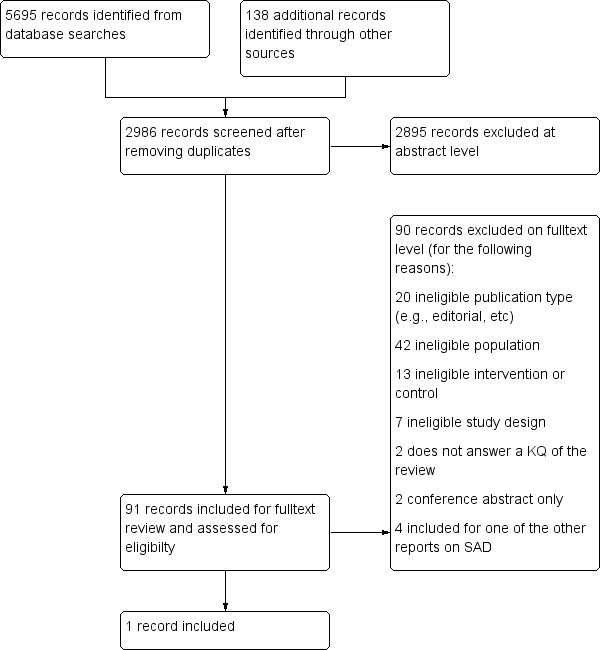
PRISMA flow diagram.
Included studies
We included one RCT comparing three study arms for prevention of SAD: bright white visor light versus infrared visor light versus no light therapy (Meesters 1999). Bio Bright, Inc., sponsored the equipment, and study authors reported no other information on funding. We found no non‐randomised studies for assessment of risk of harms.
In the following section, we present study characteristics and results in greater detail (see also Characteristics of included studies).
Design
The included RCT was a single‐centre, non‐blinded study that was composed of two winter seasons (1993‐94 and 1994‐95) that started each year in October and ended in April.
Sample size
During both winter seasons, the study included a total of 46 participants with a history of SAD who had no depressive symptoms when the study started. Initially, investigators had recruited 50 outpatients (30 in winter season 1993‐94; 20 in winter season 1994‐95); however, four developed depression between the time of giving consent and the start of the study. Therefore, these patients were not included in the study.
Setting
The study was conducted in the Netherlands and included patients from an outpatient clinic. The intervention was implemented at participants' homes.
Participants
Participants were adult outpatients with a history of SAD who had been successfully treated with conventional light treatment in previous winter seasons. Patients were non‐depressed at the start of the study. All participants were free of drugs and were diagnosed with SAD according to the criteria of Rosenthal et al. (Rosenthal 1984), and in keeping with an older version (1987) of the DSM (DSM‐III‐R). A total of 50 adults with a history of SAD gave consent to participate in the study. Four developed symptoms of depression before the study started. In all, 46 participants took part in the study and were randomly assigned to one of three study arms. Eighteen participants were randomly assigned to bright white visor light (2500 lux); four dropped out (no information on age or gender reported). Of the remaining 14 participants, 12 were women with a mean age of 39.5 years (standard deviation (SD) ± 9.3), and two were men with a mean age of 41.0 years (SD ± 12.7). Eigtheen participants were randomly assigned to the infrared visor light (0.18 lux); three dropped out (no information on age or gender reported). Of the remaining 15 participants in the infrared light group, 10 were women with a mean age of 36.6 years (SD ± 4.9), and five were men with a mean age of 35.4 years (SD ± 6.9). Ten participants were randomly assigned to no light exposure; one person dropped out (no information on age or gender reported). Of the remaining nine patients in the no treatment group, five were women with a mean age of 39.4 years (± 8.0), and four were men with a mean age of 47.5 years (SD ± 7.0). Study authors reported no other participant characteristics.
Interventions
Participants were randomly assigned to three study arms: bright white visor light (bright light inclusive infrared light), pure infrared visor light (visible light filtered out) and no light exposure. Participants in the bright white light therapy group used a bright white visor light. Those in the infrared light group were exposed to infrared light by means of a light visor equipped with a Kodak Wratten filter (type 89b, 720 mm). The light visors ‐ portable head‐mounted devices ‐ were manufactured by Bio Bright, Inc., and contained two krypton incandescent bulbs. Participants used them at home and were instructed to use them 30 minutes daily (except on Saturdays and Sundays) between 6:00 AM and 9:00 AM. As participants used the treatment at home on their own, they were able to choose the exact treatment time on their own and to integrate treatments into their daily routine. Participants in the control group received no type of light therapy (no visors were provided) and represented a waiting list control.
Outcomes
The primary outcome reported in this study was development of depression, according to a translated version of the Structured Interview Guide for the Hamilton Depression Rating Scale‐Seasonal Affective Disorders self rating version (SIGH‐SAD‐SR, 29‐item version) and according to the Beck Depression Inventory (BDI, 21‐item version). As the primary outcome for this Cochrane review was defined using SIGH‐SAD (see Types of outcome measures), we focus only on the SIGH‐SAD‐SR data reported. According to SIGH‐SAD‐SR criteria, individuals with a score ≥ 20 were considered depressive. A secondary outcome of this Cochrane review was severity of depression defined as "Severity of the SAD episode or SAD‐related symptoms, as measured by a validated tool (e.g. Hamilton Depression Rating Scale (Hamilton 1960))." Severity is usually reported as a continuous outcome, however in the included study it was dichotomized by the authors. Patients with a SIGH‐SAD‐SR score ≥ 40 were considered severely depressed. Therefore we reported this outcome as a dichotomous outcome in this review.
Researchers did not assess adverse events.
Excluded studies
Overall we assessed 91 studies at full‐text level and excluded 90 of them. We excluded most studies because they were treatment ‐ not prevention ‐ studies and/or because they focused on major depression ‐ not on SAD. Some studies were intended to prevent SAD, but we had to exclude them for different reasons.
Two studies included participants with a history of SAD and investigated the preventive effects of light therapy (Meesters 1994; Partonen 1996). We excluded these studies because they had no control group and therefore did not meet our eligibility criteria. Two controlled studies investigated whether starting light therapy at an early stage of a depressive episode can prevent a full‐blown winter depressive episode (Meesters 1991; Meesters 1993). We excluded these studies because participants already had depressive symptoms when the study started. One study also investigated whether starting light therapy at an early stage of a depressive episode can prevent a full‐blown SAD; however, in this study participants already had symptoms when the study started, and a control group was missing (Terman 1994).
Characteristics of excluded studies show all records that narrowly missed the inclusion criteria for this systematic review and mention those studies that were included in the review on SGA (Gartlehner 2014). In the Characteristics of excluded studies section, we explain why we did not include these studies in this review.
Ongoing studies
We identified no ongoing studies of interest..
Studies awaiting classification
We found no studies currently awaiting classification.
Risk of bias in included studies
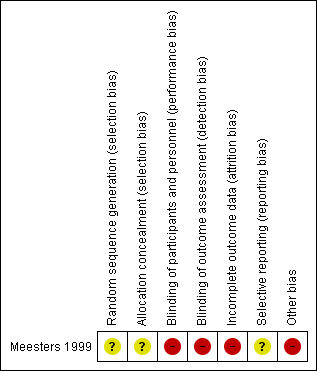
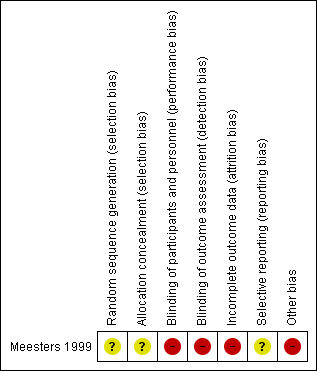
For details of the risk of bias judgement, see Characteristics of included studies. We present graphical representations of the overall risk of bias in the included study in Figure 2 and Figure 3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across included studies.
Risk of bias summary: review authors' judgements about each risk of bias item for the included study.
Allocation
Study authors state that participants were randomly assigned to treatment groups. However, they do not provide detailed information about the randomisation scheme and do not explain how allocation concealment was achieved. The only participant characteristics reported are age and sex (only for the per‐protocol population). Study authors do not report details on participants' history of SAD nor on their prior experience with light therapy, socioeconomic status of included participants or whether treatment groups were similar in terms of participant characteristics.
Blinding
Participants were not blinded to type of treatment. As participants were using a self reporting scale, they were assessing outcomes too.
Incomplete outcome data
Eight of 46 participants (17%) dropped out of the study (four in the bright light group, three in the infrared light group and one in the control group) and were not included in the analysis (no ITT). Investigators reported no characteristics (e.g. age, sex) of participants who dropped out.
Selective reporting
We could not identify a protocol for this study. Therefore, we rated this domain as unclear.
Other potential sources of bias
Participants self administered the intervention in their own homes. Whether they used the intervention properly is unknown.
Effects of interventions
See: Summary of findings for the main comparison Bright white light therapy compared with no light therapy for prevention of SAD; Summary of findings 2 Infrared light therapy compared with no light therapy for prevention of SAD; Summary of findings 3 Light therapy compared with no light therapy for prevention of SAD; Summary of findings 4 Bright white light therapy compared with infrared light therapy for prevention of SAD
Comparison 1. Light therapy versus placebo, no treatment or waiting list
One study including 46 participants contributed data for this comparison (Meesters 1999). In this study, investigators compared bright white visor light (2500 lux) (n = 18) and infrared visor light (0.18 lux) (n = 18) with no light exposure (n = 10). Because study authors reported only per‐protocol analyses, we additionally conducted two types of intention‐to‐treat analyses. In one, we assumed that participants who dropped out of the study were depressed; in the other, we assumed that participants who dropped out of the study were not depressed. We chose this approach because with eight dropouts in such a small study, assumptions about the dropouts can determine analytical results. Therefore, we decided to report per‐protocol results as well.
We conducted three comparisons as summarised in this section: bright light therapy versus no light therapy, infrared light therapy versus no light therapy and "light therapy" (both bright white light therapy and infrared light therapy) versus no light therapy.
We did not synthesise outcomes at different time points because data were presented only in figures and were not ready to included in analyses.
Primary outcomes
1.1 Incidence of SAD
We defined a priori the incidence of SAD as the proportion of participants with a SIGH‐SAD score of 20 or higher.
For the first comparison, risk of developing a depressive episode (SIGH‐SAD‐SR ≥ 20) was numerically smaller for participants in the bright light group than for those in the non‐treatment group. According to the per‐protocol analysis, 43% (6/14) of those in the bright light group developed a depressive episode compared with 67% (6/9) of participants in the non‐treatment group. The risk of developing a depressive episode during the winter was 36% smaller for individuals in the bright light group than for those in the non‐treatment group; however, the confidence interval was very broad, implying that with 95% confidence, the true effect lies within 0.30 to 1.38 (RR 0.64, 95% CI 0.30 to 1.38; see Analysis 1.1).
When we assumed that none of the participants who dropped out developed a depressive episode, ITT analysis showed that 33% (6/18) of individuals in the bright light group and 60% (6/10) of those in the non‐treatment group developed depression. The risk of developing depression under bright light therapy was 44% smaller than in the non‐treatment group; however, the broad confidence interval suggests with 95% certainty that the true effect lies between 0.24 and 1.27 (RR 0.56, 95% CI 0.24 to 1.27; see Analysis 1.2).
If we assumed on the other hand that all dropouts developed depression, ITT analysis showed that 56% (10/18) of participants in the bright light group developed depression compared with 70% (7/10) in the non‐treatment group. The risk of developing depression was 21% smaller in the bright light group than in the non‐treatment group; however, the broad confidence interval suggests with 95% certainty a possible true value between 0.44 and 1.42 (RR 0.79, 95% CI 0.44 to 1.42; see Analysis 1.3).
For the second comparison, a favourable effect of the light condition was observed in the infrared light group; however, confidence intervals always included possible true values favouring infrared light and favouring no treatment, no matter what type of analysis we applied (per‐protocol: 33% (5/15) vs 67% (6/9), RR 0.50, 95% CI 0.21 to 1.17; see Analysis 2.1; ITT with no dropouts depressed: 28% (5/18) vs 60% (6/10), RR 0.46, 95% CI 0.19 to 1.14; see Analysis 2.2; ITT with all dropouts depressed: 44% (8/18) vs 70% (7/10), RR 0.63, 95% CI 0.33 to 1.22; see Analysis 2.3).
For the third comparison, when we compared both types of light therapy given to one treatment arm, we observed a numerically favourable effect of light therapy versus no light therapy; however, confidence intervals always included possible true values favouring light and no light therapy, no matter if we used per‐protocol or ITT analysis (per‐protocol: 38% (11/29) vs 67% (6/9), RR 0.57, 95% CI 0.30‐1.10; see Analysis 3.1; ITT with no dropouts depressed: 31% (11/36) vs 60% (6/10), RR 0.51, 95% CI 0.25‐1.03; see Analysis 3.2; ITT with all dropouts depressed: 50% (18/36) vs 70% (7/10), RR 0.71, 95% CI 0.42‐1.20; see Analysis 3.3).
1.2 Overall rate of adverse events
The included RCT reported no data on adverse events. We found no additional eligible evidence addressing this outcome.
Secondary outcomes
1.3 Severity of SAD or SAD‐related symptoms
For the first comparison, when we looked only at those participants who developed severe depression using SIGH‐SAD‐SR (≥ 40) as the criterion for severe depression, the broad confidence interval showed that the difference between bright white light therapy and no light therapy again was not statistically significant (per‐protocol: 7% (1/14) vs 33% (3/9), RR 0.20, 95% CI 0.02 to 1.64; see Analysis 1.4; ITT with no dropout depressed: 6% (1/18) vs 30% (3/10), RR 0.19, 95% CI 0.02 to 1.55; see Analysis 1.5; ITT with all dropouts depressed: 28% (5/18) vs 40% (4/10), RR 0.56, 95% CI 0.18 to 1.76; see Analysis 1.6).
For the second comparison, infrared light therapy versus no light therapy showed no statistically significant differences when we used SIGH‐SAD‐SR (per‐protocol: 7% (1/15) vs 33% (3/9), RR 0.20, 95% CI 0.02 to 1.64; see Analysis 2.4; ITT with no dropout depressed: 6% (1/18) vs 30% (3/10), RR 0.19, 95% CI 0.02 to 1.55; see Analysis 2.5; ITT with all dropouts depressed: 22% (4/18) vs 40% (4/10), RR 0.56, 95% CI 0.18 to 1.76; see Analysis 2.6).
For the third comparison, combining bright white light and infrared light versus "light therapy" and comparing it versus no light therapy showed numerically favourable results for light therapy; however, again the 95% confidence interval was very broad. In the per‐protocol analysis, the true effect could favour both light therapy and no light therapy (7% (2/29) vs 33% (3/9), RR 0.21, 95% CI 0.04 to 1.05; see Analysis 3.4). In the ITT analysis, when we assumed that all dropouts were not depressed, the 95% CI shows a true favourable effect of light therapy in reducing the risk of development of a severe depressive episode (6% (2/36) vs 30% (3/10), RR 0.63, 95% CI 0.24 to 1.61; see Analysis 3.5). However, when we assumed that all dropouts had developed a severe episode of depression, this was no longer the case (25% (9/36) vs 40% (4/10), RR 0.63, 95% CI 0.22 to 1.61; see Analysis 3.6).
1.4 Quality of life
We found no eligible evidence addressing this outcome.
1.5 Quality of interpersonal and social functioning
We found no eligible evidence addressing this outcome.
1.6 Proportion of participants with serious adverse events
We found no eligible evidence addressing this outcome.
1.7 Rates of discontinuation due to adverse events
We found no eligible evidence addressing this outcome.
1.8 Overall rate of discontinuation
Eight participants dropped out during the study period (four in the bright light group, three in the infrared light group and one in the control group) for the following reasons: One person failed to wear the light visor, one started to use medication, one in the "non‐treatment group" started with light therapy on her own and five stopped because they lacked motivation to keep scoring self rating scales when suffering from no symptoms, moving to a new home and other reasons that study authors did not describe in detail.
Additionally, researchers offered light treatment in the clinic to all participants who developed severe depression (SIGH‐SAD‐SR ≥ 40) and left the study at that moment. As this type of discontinuation is part of the main outcome, we did not take it into account when we compared discontinuation rates between groups receiving light therapy and those receiving no light therapy.
For the first comparison, four of 18 (22%) participants randomly assigned to bright light therapy dropped out during the study period compared with one person in the no treatment group (10%) (RR 2.22, 95% CI 0.29 to 17.27; see Analysis 1.7).
For the second comparison, the infrared light therapy group dropout rate was higher than that of the non‐treatment group (17% (3/18) vs 10% (1/10), RR 1.67, 95% CI 0.2 to 13.98; see Analysis 2.7), but the difference was small and was not statistically significant.
For the third comparison, both types of light therapy together versus no light therapy showed that the dropout rate in the light therapy group was numerically higher (19% (7/36) vs 10% (1/10), RR 1.94, 95% CI 0.27 to 14.01; see Analysis 3.7).
Comparison 2. Light therapy versus other light therapy
One study contributed data from 36 participants to this comparison; 18 were randomly assigned to bright white visor light, and 18 to infrared visor light (Meesters 1999). As explained in Comparison 1, we reported per‐protocol results as well as results derived from two types of ITT analyses. In one, we assumed that participants who dropped out of the study were depressed; in the other, we assumed that those who dropped out of the study were not depressed.
Primary outcomes
2.1 Incidence of SAD
In the bright light condition, the rate of participants developing depression (SIGH‐SAD‐SR ≥ 20) was numerically higher than that of participants in the infrared light therapy group; however, confidence intervals always included possible true values favouring light and no light therapy, no matter whether we performed per‐protocol or ITT analysis (per‐protocol: 43% vs 33%, RR 1.29, 95% CI 0.50 to 3.28; see Analysis 4.1; ITT with no dropouts depressed: 33% vs 28%, RR 1.20, 95% CI 0.45 to 3.23; see Analysis 4.2; ITT with all dropouts depressed: 56% vs 44%, RR 1.25, 95% CI 0.65 to 2.42; see Analysis 4.3).
2.2 Overall rate of adverse events
We did not find any eligible evidence addressing this outcome.
Secondary outcomes
2.3 Severity of SAD or SAD‐related symptoms
When we looked only at participants who developed severe depression (SIGH‐SAD‐SR ≥ 40), we observed no differences between individuals in the bright light therapy group and those in the infrared light therapy group ‐ both light conditions seemed to be similar (per‐protocol: 7% vs 7%, RR 1.07, 95% CI 0.07 to 15.54; see Analysis 4.4; ITT with no dropouts depressed: 6% vs 6%, RR 1.00, 95% CI 0.07 to 14.79; see Analysis 4.5; ITT with all dropouts depressed: 28% vs 22%, RR 1.25, 95% CI 0.40 to 3.91; see Analysis 4.6).
2.4 Quality of life
We found no eligible evidence addressing this outcome.
2.5 Quality of interpersonal and social functioning
We found no eligible evidence addressing this outcome.
2.6 Proportion of participants with serious adverse events
We found no eligible evidence addressing this outcome.
2.7 Rates of discontinuation due to adverse events
We found no eligible evidence addressing this outcome.
2.8 Overall rate of discontinuation
Discontinuation was similar in the two light therapy groups; 22% (4/18) of participants randomly assigned to bright light therapy dropped out during the study period compared with 17% (3/18) of those in the infrared light therapy group (RR 1.33, 95% CI 0.35 to 5.13; see Analysis 4.7).
Comparison 3. Light therapy versus second‐generation antidepressants
We found no eligible studies assessing this comparison.
Comparison 4. Light therapy versus melatonin or agomelatine
We found no eligible studies assessing this comparison.
Comparison 5. Light therapy versus psychological therapy
We found no eligible studies assessing this comparison.
Comparison 6. Light therapy versus lifestyle intervention
We found no eligible studies assessing this comparison.
Comparison 7. Light therapy versus negative ion generators
We found no eligible studies assessing this comparison.
Comparison 8. Light therapy + comparator intervention (as listed under Types of interventions) versus placebo or no treatment control group or waiting list
We found no eligible studies assessing this comparison.
Comparison 9. Light therapy + comparator intervention (as listed under Types of interventions) versus the same comparator intervention as monotherapy (e.g. light therapy + psychological therapy vs psychological therapy alone)
We found no eligible studies assessing this comparison.
Subgroup analyses
Data were insufficient for subgroup analyses.
Sensitivity analyses
Data were insufficient for subgroup analyses.
Reporting bias
As we identified only one study, statistical approaches to assessment of publication bias are not possible. It is unclear whether reporting bias is a problem of the included study, as we could not identify a protocol for the study.
Discussion
Summary of main results
Overall, bright white visor light and infrared visor light numerically reduced the incidence of SAD, as well as the incidence of severe SAD, as compared with no light therapy; however, 95% confidence intervals were very broad and included both possible true effects favouring light therapy and possible true effects favouring no treatment. Comparison of both light conditions versus each other showed no differences in SAD incidence and in the incidence of severe SAD.
Overall the number of dropouts (not including those who stopped the study because of depression) was similar between study arms.
summary of findings Table for the main comparison, summary of findings Table 2, summary of findings Table 3 and summary of findings Table 4 show that quality of evidence for all outcomes was very low.
Overall completeness and applicability of evidence
A major limitation of our report is that evidence is limited to one RCT with a very small number of participants (n = 46) that is rated as having high risk of bias in several domains. Therefore, results of this RCT can be influenced by lack of power and by random error.
The population included in this study that met our eligibility criteria was only loosely described (age, gender); therefore, it is difficult to say whether the results can be applied to a broad spectrum of patients who experience SAD.
As no results on adverse events were reported, we cannot estimate potential harms of the intervention.
Quality of the evidence
We graded the quality of evidence for available efficacy outcomes (incidence of SAD, severity of SAD, overall discontinuation) as very low. Reasons for downgrading the quality of evidence included high risk of bias of the included study and imprecision due to lack of optimal information size. Other limitations of the included study were that outcomes were self rated, compliance throughout study duration was not checked, participant characteristics were not reported comprehensively, no safety data were reported (especially important because infrared light can cause such events as eye damage) and the wavelength of infrared light used was not specified, which is important because absorption of infrared light in the eye depends on the wavelength (Berg 1997). We did not downgrade for indirectness because we drew conclusions only on the efficacy of these two special types of light therapy (bright white visor light and infrared visor light). Drawing conclusions about light therapy per se is not possible because different types of administration of light therapy may lead to different results.
Potential biases in the review process
Our eligibility criteria included non‐randomised studies for assessment of harms because methods research indicates that rare but potentially serious adverse events are not covered well in RCTs. Despite extensive literature searches, we could identify no non‐randomised studies. We identified only one RCT that was published in 1999 and did not report on adverse events. As the study was conducted 20 years ago, we did not contact the study author to ask for more detailed information. Other studies that investigated light therapy as treatment ‐ not as prevention ‐ have reported possible side effects from light therapy, including headache (13% to 21%), eye strain or visual disturbance (19% to 27%), nausea (7%), sweating (7%), sedation (6% to 7%) and agitation (6% to 13%) (Lam 1999). However, based on the evidence included in this systematic review, we do not know whether light therapy as preventive treatment is associated with side effects.
In this systematic review, we considered all types of bright white therapy, infrared light therapy and dawn simulation therapy to be eligible (no limitations on dosage, duration or mode of delivery) because we wanted to base our systematic review on all available evidence on preventive use of any type of light therapy. The included study (Meesters 1999) investigated two types of light therapy that nowadays generally are not accepted as treatment for patients with SAD. Three studies showed that bright white light delivered by visors is not more effective than placebo (Joffe 1993; Rosenthal 1993; Teicher 1995). Therefore, experts often do not consider visors as a legitimate light therapy intervention. This might explain why bright white light was not more effective than no light therapy in reducing the incidence of SAD in Meesters 1999. Nowadays, dim red light producing only a visually negligible lux of red light is often considered sham treatment rather than active light therapy. This must be considered when results of the included study are interpreted.
Finally, publication bias and selective outcomes reporting are potential limitations of any systematic review. Although we searched for grey and unpublished literature, the extent and impact of reporting biases of this body of evidence is impossible to determine.
Agreements and disagreements with other studies or reviews
One uncontrolled study included participants with a history of SAD and showed no preventive effects of light therapy on SAD when administered before the winter season (Meesters 1994). Another uncontrolled study observing participants who received light therapy before symptoms started showed a preventive effect ‐ none of the six individuals developed a depressive episode during the winter season, according to SIGH‐SAD‐SR (Partonen 1996). Two controlled studies showed that light therapy at an early stage of a depressive episode can prevent a full‐blown winter depressive episode (Meesters 1991; Meesters 1993). Another study showed that treating individuals with light therapy at an early stage could postpone a subsequent episode of SAD (Terman 1994).
We could identify no systematic reviews on the effects of light therapy as preventive treatment for patients with a history of SAD. A systematic review and meta‐analysis of light therapy as treatment for mood disorders showed that bright light therapy and dawn simulation were efficacious in reducing the severity of SAD symptoms (Golden 2005).

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across included studies.
Risk of bias summary: review authors' judgements about each risk of bias item for the included study.
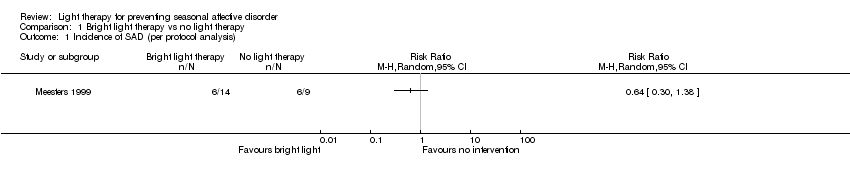
Comparison 1 Bright light therapy vs no light therapy, Outcome 1 Incidence of SAD (per protocol analysis).
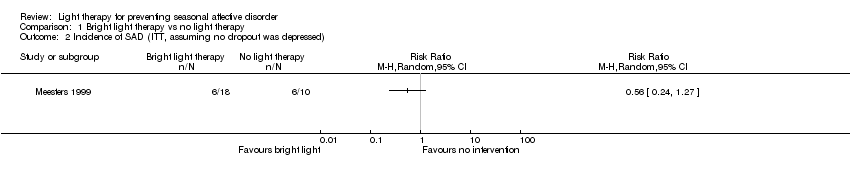
Comparison 1 Bright light therapy vs no light therapy, Outcome 2 Incidence of SAD (ITT, assuming no dropout was depressed).
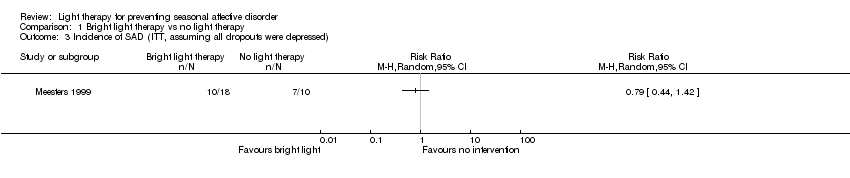
Comparison 1 Bright light therapy vs no light therapy, Outcome 3 Incidence of SAD (ITT, assuming all dropouts were depressed).

Comparison 1 Bright light therapy vs no light therapy, Outcome 4 Incidence of severe SAD (per protocol analysis).

Comparison 1 Bright light therapy vs no light therapy, Outcome 5 Incidence of severe SAD (ITT, assuming no dropout was depressed).

Comparison 1 Bright light therapy vs no light therapy, Outcome 6 Incidence of severe SAD (ITT, assuming all dropouts were depressed).
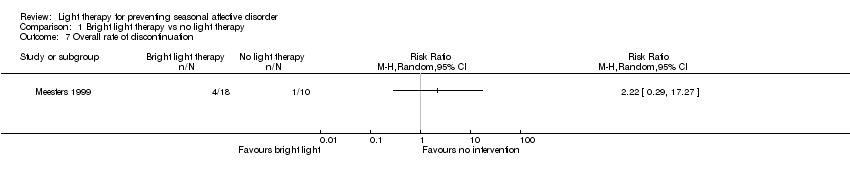
Comparison 1 Bright light therapy vs no light therapy, Outcome 7 Overall rate of discontinuation.

Comparison 2 Infrared light therapy vs no light therapy, Outcome 1 Incidence of SAD (per protocol analysis).

Comparison 2 Infrared light therapy vs no light therapy, Outcome 2 Incidence of SAD (ITT, assuming no dropout was depressed).

Comparison 2 Infrared light therapy vs no light therapy, Outcome 3 Incidence of SAD (ITT, assuming all dropouts were depressed).

Comparison 2 Infrared light therapy vs no light therapy, Outcome 4 Incidence of severe SAD (per protocol analysis).

Comparison 2 Infrared light therapy vs no light therapy, Outcome 5 Incidence of severe SAD (ITT, assuming no dropout was depressed).

Comparison 2 Infrared light therapy vs no light therapy, Outcome 6 Incidence of severe SAD (ITT, assuming all dropouts were depressed).
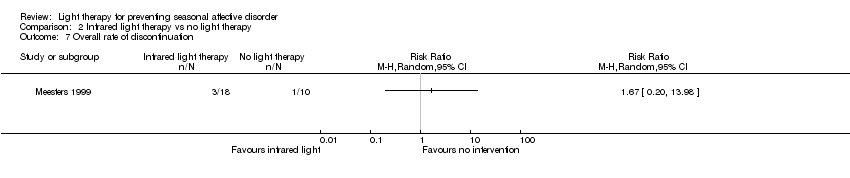
Comparison 2 Infrared light therapy vs no light therapy, Outcome 7 Overall rate of discontinuation.

Comparison 3 Light therapy (bright white and infrared) vs no light therapy, Outcome 1 Incidence of SAD (per protocol analysis).

Comparison 3 Light therapy (bright white and infrared) vs no light therapy, Outcome 2 Incidence of SAD (ITT, assuming no dropout was depressed).

Comparison 3 Light therapy (bright white and infrared) vs no light therapy, Outcome 3 Incidence of SAD (ITT, assuming all dropouts were depressed).

Comparison 3 Light therapy (bright white and infrared) vs no light therapy, Outcome 4 Incidence of severe SAD (per protocol analysis).

Comparison 3 Light therapy (bright white and infrared) vs no light therapy, Outcome 5 Incidence of severe SAD (ITT, assuming no dropout was depressed).
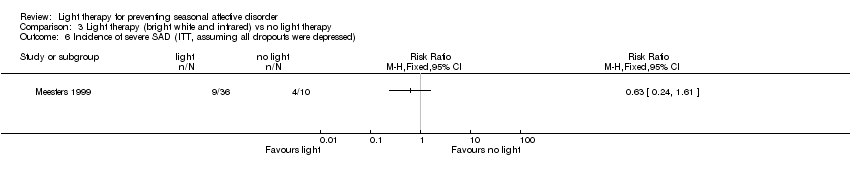
Comparison 3 Light therapy (bright white and infrared) vs no light therapy, Outcome 6 Incidence of severe SAD (ITT, assuming all dropouts were depressed).

Comparison 3 Light therapy (bright white and infrared) vs no light therapy, Outcome 7 Overall discontinuation.
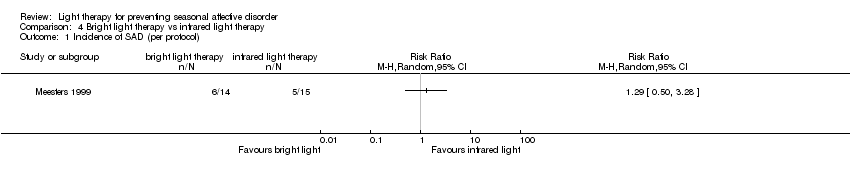
Comparison 4 Bright light therapy vs infrared light therapy, Outcome 1 Incidence of SAD (per protocol).
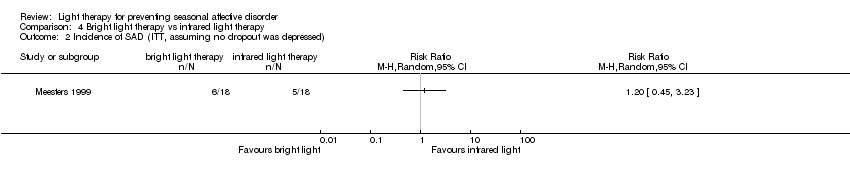
Comparison 4 Bright light therapy vs infrared light therapy, Outcome 2 Incidence of SAD (ITT, assuming no dropout was depressed).

Comparison 4 Bright light therapy vs infrared light therapy, Outcome 3 Incidence of SAD (ITT, assuming all dropouts were depressed).

Comparison 4 Bright light therapy vs infrared light therapy, Outcome 4 Incidence of severe SAD (per protocol).

Comparison 4 Bright light therapy vs infrared light therapy, Outcome 5 Incidence of severe SAD (ITT, assuming no dropout was depressed).

Comparison 4 Bright light therapy vs infrared light therapy, Outcome 6 Incidence of severe SAD (ITT, assuming all dropouts were depressed).

Comparison 4 Bright light therapy vs infrared light therapy, Outcome 7 Overall discontinuation.
| Bright white light therapy compared with no light therapy for prevention of SAD | ||||||
| Patient or population: All participants were known SAD patients who had been successfully treated with conventional light therapy in previous winters | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No light therapy | Light therapy | |||||
| Incidence of SAD (SIGH‐SAD score ≥ 20) (follow‐up 26 weeks) | Low | RR 0.64 | 23 | ⊕⊝⊝⊝ | ||
| 300 per 1000 | 192 per 1000 | |||||
| Moderate | ||||||
| 500 per 1000 | 320 per 1000 (150 to 690) | |||||
| High | ||||||
| 600 per 1000 | 276 per 1000 (210 to 966) | |||||
| Incidence of severe SAD (SIGH‐SAD‐SR (≥ 40)) (follow‐up 26 weeks) | Study population | RR 0.21 | 23 | ⊕⊝⊝⊝ | ||
| 333 per 1000 | 70 per 1000 | |||||
| Overall discontinuation (follow‐up 26 weeks) | Study population | RR 2.22 | 28 | ⊕⊝⊝⊝ | ||
| 100 per 1000 | 222 per 1000 | |||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded 2 steps because of severe risk of bias due to non‐blinding and unclear randomisation process and allocation concealment; no intention‐to‐treat analysis was reported, outcomes were self rated, compliance throughout study duration was not checked and participant characteristics were not reported comprehensively bDowngraded 1 step because of small sample size (lack of power and random error could have influenced results) | ||||||
| Infrared light therapy compared with no light therapy for prevention of SAD | ||||||
| Patient or population: All participants were known SAD patients who had been successfully treated with conventional light therapy in previous winters | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No light therapy | Infrared light therapy | |||||
| Incidence of SAD (SIGH‐SAD score ≥ 20) (follow‐up 26 weeks) | Low | RR 0.50 | 24 | ⊕⊝⊝⊝ | ||
| 300 per 1000 | 150 per 1000 (63 to 351) | |||||
| Moderate | ||||||
| 500 per 1000 | 250 per 1000 (105 to 585) | |||||
| High | ||||||
| 600 per 1000 | 300 per 1000 (126 to 702) | |||||
| Incidence of severe SAD (SIGH‐SAD‐SR (≥ 40)) (follow‐up 26 weeks) | Study population | RR 0.20 | 24 | ⊕⊝⊝⊝ | ||
| 333 per 1000 | 67 per 1000 | |||||
| Overall discontinuation (follow‐up 26 weeks) | Study population | RR 1.67 | 28 | ⊕⊝⊝⊝ | ||
| 100 per 1000 | 167 per 1000 | |||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded 2 steps because of severe risk of bias due to non‐blinding and unclear randomisation process and allocation concealment; no intention‐to‐treat analysis was reported, outcomes were self rated, compliance throughout study duration was not checked and participant characteristics were not reported comprehensively bDowngraded 1 step because of small sample size (lack of power and random error could have influenced results) | ||||||
| Light therapy (bright white or infrared) compared with no light therapy for prevention of SAD | ||||||
| Patient or population: All participants were known SAD patients who had been successfully treated with conventional light therapy in previous winters | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No light therapy | Infrared light therapy | |||||
| Incidence of SAD (SIGH‐SAD score ≥ 20) (follow‐up 26 weeks) | Low | RR 0.57 | 38 | ⊕⊝⊝⊝ | ||
| 300 per 1000 | 171per 1000 (90 to 330) | |||||
| Moderate | ||||||
| 500 per 1000 | 285 per 1000 (150 to 550) | |||||
| High | ||||||
| 600 per 1000 | 342 per 1000 (180 to 660) | |||||
| Incidence of severe SAD (SIGH‐SAD‐SR (≥ 40)) (follow‐up 26 weeks) | Study population | RR 0.21 | 38 | ⊕⊝⊝⊝ | ||
| 333 per 1000 | 70 per 1000 | |||||
| Overall discontinuation (follow‐up 26 weeks) | Study population | RR 1.94 | 46 | ⊕⊝⊝⊝ | ||
| 100 per 1000 | 194 per 1000 | |||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded 2 steps because of severe risk of bias due to non‐blinding and unclear randomisation process and allocation concealment; no intention‐to‐treat analysis was reported, outcomes were self rated, compliance throughout study duration was not checked and participant characteristics were not reported comprehensively bDowngraded 1 step because of small sample size (lack of power and random error could have influenced results) | ||||||
| Bright white light therapy compared with infrared light therapy for prevention of SAD | ||||||
| Patient or population: All participants were known SAD patients who had been successfully treated with conventional light therapy in previous winters | ||||||
| Outcomes | Risk in both groups | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk in this treatment group | Risk in this treatment group | |||||
| Infrared light therapy | Bright white light therapy | |||||
| Incidence of SAD (SIGH‐SAD score ≥ 20) (follow‐up 26 weeks) | Study population | RR 1.29 | 29 | ⊕⊝⊝⊝ | ||
| 333 per 1000 | 357 per 1000 | |||||
| Incidence of severe SAD (SIGH‐SAD‐SR (≥ 40)) (follow‐up 26 weeks) | Study population | RR 1.07 | 29 | ⊕⊝⊝⊝ | ||
| 67 per 1000 | 71 per 1000 | |||||
| Overall discontinuation (follow‐up 26 weeks) | Study population | RR 1.33 | 36 | ⊕⊝⊝⊝ | ||
| 167 per 1000 | 222 per 1000 | |||||
| CI: Confidence interval; RCT: Randomised controlled trial; RR: Risk ratio, SIGH‐SAD‐SR: Structured Interview Guide for the Hamilton Depression Rating Scale‐Seasonal Affective Disorders self rating version | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded 2 steps because of severe risk of bias due to non‐blinding and unclear randomisation process and allocation concealment; no intention‐to‐treat analysis was reported, outcomes were self rated, compliance throughout study duration was not checked and participant characteristics were not reported comprehensively bDowngraded 1 step because of small sample size (lack of power and random error could have influenced results) | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Incidence of SAD (per protocol analysis) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Incidence of SAD (ITT, assuming no dropout was depressed) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Incidence of SAD (ITT, assuming all dropouts were depressed) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Incidence of severe SAD (per protocol analysis) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Incidence of severe SAD (ITT, assuming no dropout was depressed) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6 Incidence of severe SAD (ITT, assuming all dropouts were depressed) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7 Overall rate of discontinuation Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Incidence of SAD (per protocol analysis) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Incidence of SAD (ITT, assuming no dropout was depressed) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Incidence of SAD (ITT, assuming all dropouts were depressed) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Incidence of severe SAD (per protocol analysis) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Incidence of severe SAD (ITT, assuming no dropout was depressed) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6 Incidence of severe SAD (ITT, assuming all dropouts were depressed) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7 Overall rate of discontinuation Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Incidence of SAD (per protocol analysis) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Incidence of SAD (ITT, assuming no dropout was depressed) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Incidence of SAD (ITT, assuming all dropouts were depressed) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Incidence of severe SAD (per protocol analysis) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Incidence of severe SAD (ITT, assuming no dropout was depressed) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Incidence of severe SAD (ITT, assuming all dropouts were depressed) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7 Overall discontinuation Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Incidence of SAD (per protocol) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Incidence of SAD (ITT, assuming no dropout was depressed) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Incidence of SAD (ITT, assuming all dropouts were depressed) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Incidence of severe SAD (per protocol) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Incidence of severe SAD (ITT, assuming no dropout was depressed) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6 Incidence of severe SAD (ITT, assuming all dropouts were depressed) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7 Overall discontinuation Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |

