Transferencia de embriones frescos versus congelados en la reproducción asistida
Resumen
Antecedentes
En general, la fecundación in vitro (FIV) o la inyección intracitoplasmática de espermatozoides (ICSI) implica una única transferencia de embriones frescos y una o más transferencias de embriones congelados‐descongelados. Alternativamente, la estrategia de "criotransferencia" implica la transferencia de embriones congelados‐descongelados solamente, sin transferencia de embriones frescos. En la práctica, ambas estrategias pueden variar técnicamente, lo que incluye diferencias en las técnicas de congelación y en el momento de la trasferencia de la criopreservación, es decir, vitrificación versus congelación lenta, congelación de dos embriones pronucleados (2pn) versus embriones en estadio de división versus blastocistos, y la transferencia de embriones en estadio de división versus blastocistos.
En la estrategia de criotransferencia las transferencias de embriones se desvinculan de la estimulación ovárica en el ciclo de tratamiento inicial. Lo anterior podría evitar un efecto negativo de la hiperestimulación ovárica sobre el endometrio y mejoraría así la implantación de los embriones. También podría reducir el riesgo del síndrome de hiperestimulación ovárica (SHEO) en el ciclo de estimulación ovárica al evitar un embarazo.
Se compararon los efectos beneficiosos y los riesgos de las dos estrategias de tratamiento.
Objetivos
Evaluar la efectividad y la seguridad de la estrategia de criopreservación en comparación con la estrategia convencional de FIV/ICSI en pacientes sometidas a tecnología de reproducción asistida.
Métodos de búsqueda
Se hicieron búsquedas en el registro de ensayos del Grupo Cochrane de Ginecología y Fertilidad (Cochrane Gynaecology and Fertility Group Trials Register), Registro Cochrane Central de Estudios (Cochrane Central Register of Studies, CRSO), MEDLINE, Embase, PsycINFO, CINAHL y en dos registros de ensayos en curso en noviembre 2016 y además se verificaron las referencias y se contactó con los autores de los estudios y expertos en el tema para identificar estudios adicionales.
Criterios de selección
Se incluyeron los ensayos clínicos aleatorios que compararon una estrategia de criopreservación con una estrategia convencional de FIV/ICSI que incluye la transferencia de embriones frescos a pacientes sometidas a tratamiento de FIV o ICSI.
Obtención y análisis de los datos
Se utilizaron los procedimientos metodológicos estándar recomendados por la Colaboración Cochrane. Los resultados primarios de la revisión fueron la tasa acumulativa de nacidos vivos y el SHEO. Los resultados secundarios incluyeron otros efectos adversos (tasa de abortos espontáneos).
Resultados principales
Se incluyeron cuatro ensayos clínicos aleatorios que analizaron a 1892 mujeres y compararon una estrategia de criopreservación con una estrategia convencional de FIV/ICSI. La evidencia fue de calidad moderada a baja debido al riesgo de sesgo grave y (en algunos resultados) a imprecisión grave. El riesgo de sesgo se asoció con el cegamiento poco claro de los investigadores a los resultados preliminares de los estudios, error en la unidad de análisis y falta de reglas adecuadas para la terminación de los estudios.
No hubo evidencia clara de una diferencia en la tasa acumulativa de nacidos vivos entre la estrategia de criopreservación y la estrategia convencional de FIV/ICSI (odds ratio [OR] 1,09; intervalo de confianza [IC] del 95%: 0,91 a 1,31; cuatro ensayos; 1892 mujeres; I2 = 0%; evidencia de calidad moderada). Lo anterior indica que si la tasa acumulativa de nacidos vivos es del 58% después de una estrategia convencional de FIV/ICSI, la tasa después de una estrategia de criopreservación estaría entre el 56% y el 65%.
La prevalencia de SHEO fue inferior después de la estrategia de criopreservación en comparación con la estrategia convencional de FIV/ICSI (OR 0,24; IC del 95%: 0,15 a 0,38; dos ensayos; 1633 mujeres; I2 = 0%; evidencia de baja calidad). Lo anterior indica que si la tasa de SHEO es del 7% después de una estrategia convencional de FIV/ICSI, la tasa después de una estrategia de criopreservación estaría entre el 1% y el 3%.
La estrategia de criopreservación se asoció con menos abortos espontáneos (OR 0,67; IC del 95%: 0,52 a 0,86; cuatro ensayos; 1892 mujeres; I2 = 0%; evidencia de baja calidad) y una tasa mayor de complicaciones del embarazo (OR 1,44; IC del 95%: 1,08 a 1,92; dos ensayos; 1633 mujeres; evidencia de baja calidad). No hubo diferencias en los embarazos múltiples por paciente después de la primera transferencia (OR 1,11; IC del 95%: 0,85 a 1,44; dos ensayos; 1630 mujeres; evidencia de baja calidad) y no se informaron datos del tiempo hasta el embarazo.
Conclusiones de los autores
Se encontró evidencia de calidad moderada que indicó que una estrategia no es superior a la otra en cuanto a las tasas acumulativas de nacidos vivos. No se informó el tiempo hasta el embarazo, pero se puede suponer que es más corto cuando se utiliza una estrategia convencional de FIV/ICSI en el caso de tasas acumulativas de nacidos vivos similares, ya que la transferencia de embriones se retrasa en una estrategia de criopreservación. Evidencia de baja calidad indica que no realizar una transferencia de embriones frescos disminuye el riesgo de SHEO en las pacientes con riesgo de SHEO.
PICOs
Resumen en términos sencillos
Transferencias de embriones frescos versus congelados para la reproducción asistida
Pregunta de la revisión
Se examinó la evidencia acerca de la efectividad y seguridad de una estrategia de "criopreservación" en pacientes sometidas a fecundación in vitro (FIV) o inyección intracitoplasmática de espermatozoides (ICSI), comparada con una estrategia convencional de FIV/ICSI, en cuanto a la tasa acumulativa de nacidos vivos y el riesgo del síndrome de hiperestimulación ovárica (SHEO).
Antecedentes
En la FIV/ICSI la transferencia de embriones se puede realizar con el uso de embriones frescos o congelados‐descongelados. Por lo tanto, hay dos estrategias para la transferencia de embriones en la FIV: 1) la estrategia convencional de FIV/ICSI con una transferencia única de embriones frescos y una o más transferencias de embriones congelados‐descongelados, y 2) la estrategia de "criopreservación", en la que se transfieren solo embriones congelados‐descongelados y no se transfieren embriones frescos. Existen diferencias en la técnica de congelación y en el momento de la criopreservación y la transferencia entre ambas estrategias de transferencia. En la estrategia de criopreservación, la transferencia de embriones se desvincula de la estimulación ovárica en el ciclo de estimulación ovárica. Esta estrategia puede ser beneficiosa, ya que se ha indicado que la hiperestimulación ovárica tiene un efecto negativo sobre la receptividad del endometrio para la implantación de los embriones. La estrategia de criopreservación disminuiría el riesgo de SHEO porque los embarazos no ocurren en el ciclo con estimulación ovárica.
Características de los estudios
Se incluyeron cuatro estudios que compararon una estrategia de criopreservación con una estrategia convencional de FIV/ICSI en 1892 mujeres sometidas a tecnología de reproducción asistida. La evidencia se actualizó hasta noviembre de 2016.
Resultados clave
Se encontró evidencia que mostró que al parecer no hay diferencias entre las estrategias en cuanto a la tasa acumulativa de nacidos vivos por paciente. Los hallazgos indican que si la tasa acumulativa de nacidos vivos es del 58% después de una estrategia convencional de FIV/ICSI, la tasa después de una estrategia de criopreservación estaría entre el 56% y el 65%. El tiempo hasta el embarazo no se informó como un resultado en los estudios incluidos, pero es de suponer que es más corto cuando se utiliza una estrategia convencional de FIV/ICSI que incluye la transferencia de embriones frescos cuando las tasas acumulativas de nacidos vivos son similares, ya que la transferencia de embriones se retrasa en una estrategia de criopreservación. No realizar una transferencia de embriones frescos (estrategia de criopreservación) disminuye el riesgo de SHEO en las pacientes con riesgo de SHEO. Estos hallazgos indican que si la tasa de SHEO es del 7% después de una estrategia convencional de FIV/ICSI, la tasa después de una estrategia de criopreservación estaría entre el 1% y el 3%.
Calidad de la evidencia
La evidencia fue de calidad moderada a baja debido al riesgo de sesgo grave y (en algunos resultados) a imprecisión grave. El riesgo de sesgo se asoció con el cegamiento poco claro de los investigadores a los resultados preliminares de los estudios, error en la unidad de análisis y falta de reglas adecuadas para la terminación de los estudios.
Authors' conclusions
Summary of findings
| Fresh versus frozen embryo transfers in assisted reproduction | ||||||
| Patient or population: women undergoing assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with fresh and frozen embryo transfers | Risk with frozen embryo transfers only | |||||
| Live birth rate cumulatively for all embryo stages of transfer | 579 per 1000 | 600 per 1000 | OR 1.09 | 1892 | ⊕⊕⊕⊝ | |
| Ovarian hyperstimulation syndrome per cycle with ovarian hyperstimulation | 70 per 1000 | 18 per 1000 | OR 0.24 | 1633 | ⊕⊕⊝⊝ | |
| Multiple pregnancy per woman after first ET | 161 per 1000 | 176 per 1000 (141 to 217) | OR 1.11 (0.85 to 1.44) | 1630 (2 RCTs) | ⊕⊕⊝⊝ | |
| Miscarriage per woman after first ET | 184 per 1000 | 131 per 1000 (105 to 162) | OR 0.67 (0.52 to 0.86) | 1892 | ⊕⊕⊝⊝ | |
| Pregnancy complications per woman after first ET | 110 per 1000 | 151 per 1000 (118 to 191) | OR 1.44 (1.08 to 1.92) | 1633 | ⊕⊕⊝⊝ | |
| Time to pregnancy | Not reported in any of the included studies | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level due to serious risk of bias associated with lack of power calculation (unclear what determined end of study) and/or use of interim analysis that was calculated per transfer (unit of analysis error) with absence of adequate stopping rules (possible overestimation of treatment effect). | ||||||
Background
Description of the condition
Subfertility is defined as the failure to conceive after one year of unprotected intercourse (Van Voorhis 2007). One in six couples experience subfertility at least once during their reproductive lifetime, and approximately 10% of couples worldwide are subfertile (ESHRE 2010; CDC 2011). Common causes of subfertility include poor semen quality, obstruction of the fallopian tubes, absence of ovulation, and endometriosis (Hull 1985). Poor semen quality can manifest itself as low sperm concentration, low motility, or low numbers of sperm with normal morphology. Fallopian tubes can be blocked or damaged by infection, or there can be adhesions of the tubes or ovaries caused by surgery, chlamydia, or endometriosis. Couples who fail to conceive naturally are diagnosed as having unexplained infertility if no cause can be found after standard fertility tests.
Description of the intervention
Assisted reproductive technology has rapidly evolved as an intervention to improve pregnancy rates. It involves the handling of gametes and embryos outside the human body and consists of in vitro fertilisation (IVF) with or without intracytoplasmic sperm injection (ICSI). After fertilisation, fresh transfer of the morphologically best embryo(s) into the uterine cavity is performed. Embryos suitable for transfer, but not transferred fresh, are frozen for future use.
Even so, many women fail to achieve a pregnancy after transfer of one or more fresh embryos. Recent technical improvements in cryopreservation have led to increased chances of embryo survival after thawing and subsequently increased pregnancy rates per frozen‐thawed embryo transfer (CDC 2011; Wong 2014). In fact, pregnancy rates after frozen‐thawed embryo transfer are now almost equal to pregnancy rates after fresh transfer when calculated per transfer. This has fuelled the call for a new IVF/ICSI strategy where no fresh embryo transfer is conducted and all available embryos are cryopreserved, thawed, and transferred in a subsequent cycle. This would reduce any residual chance of ovarian hyperstimulation syndrome (OHSS) and possibly increase the cumulative live birth rates (Mastenbroek 2011; Maheshwari 2013).
How the intervention might work
In contrast to the conventional strategy, in a 'freeze‐all' strategy there are no fresh embryo transfers in the cycle with ovarian stimulation, but only frozen‐thawed embryo transfers in subsequent cycles without ovarian stimulation. This avoids possible adverse effects of ovarian stimulation. The underlying reason here is the claim that ovarian stimulation reduces endometrial receptivity for the implanting embryo (Kolibianakis 2002; Bourgain 2003). Studies on the molecular level comparing stimulated with unstimulated endometrium samples have shown distinct gene‐expression profiles between the two conditions (Haouzi 2009). Transfer of frozen‐thawed embryos only would thus circumvent a possible negative effect of gonadotropins on the endometrium in the cycle with ovarian stimulation, and consequently increase live birth rates, the main outcome of interest to subfertile couples.
Ovarian stimulation with exogenous gonadotropins in IVF also increases the risk of OHSS when a pregnancy occurs in such a cycle with ovarian stimulation. Avoiding a pregnancy in the cycle with ovarian stimulation by only transferring frozen‐thawed embryos in subsequent unstimulated cycles would eliminate the residual risks of OHSS, and OHSS would therefore be self limiting. Mild OHSS symptoms can still occur as a result of the human chorionic gonadoptropin trigger in the hyperstimulated cycle in the freeze‐all strategy, but OHSS in its severe form should be rare.
Why it is important to do this review
Nowadays, an increasing number of clinics apply the freeze‐all strategy as a standard treatment strategy in their practice. However, the relative effectiveness and safety of IVF treatment with the freeze‐all strategy compared to the conventional IVF/ICSI strategy is unclear. A previous non‐Cochrane systematic review reported that a freeze‐all strategy was associated with higher ongoing and clinical pregnancy rates, and lower miscarriage rates than the conventional IVF/ICSI strategy (Roque 2013). However, this review did not report live birth or safety outcomes. This review aimed to provide a systematic, up‐to‐date summary of reliable evidence of the benefits and risks of a freeze‐all strategy.
Objectives
To evaluate the effectiveness and safety of the freeze‐all strategy compared to the conventional IVF/ICSI strategy in women undergoing assisted reproductive technology.
Methods
Criteria for considering studies for this review
Types of studies
We included published randomised clinical trials and excluded quasi‐ and pseudo‐randomised clinical trials. We excluded trials published only as abstract. We planned to include cross‐over trials for completeness, but would only pool the data from the first phase in the meta‐analysis (Vail 2003).
Types of participants
All women undergoing IVF or ICSI.
Types of interventions
Trials comparing the freeze‐all strategy with transfer of frozen‐thawed embryos only versus the conventional IVF/ICSI strategy with transfer of fresh and subsequent frozen‐thawed embryos until a live birth occurred or until all embryos from the initial cycle were transferred.
Types of outcome measures
Primary outcomes
-
Effectiveness: cumulative live birth rate per randomised woman, i.e. the rate of live birth following the transfer of all (fresh or frozen‐thawed) embryos available from the stimulated cycle.
-
Safety: OHSS per randomised woman.
Secondary outcomes
-
Cumulative ongoing pregnancy rate, defined as the number of ongoing pregnancies per woman randomised (demonstrated by the presence of a gestational sac with fetal heartbeat on ultrasound at ≥ 12 weeks of gestation).
-
Clinical pregnancy, defined as the cumulative number of clinical pregnancies per woman randomised (demonstrated by a pregnancy confirmed by ultrasonographic visualisation of one or more gestational sacs.
-
Time to pregnancy, defined as the time between the first day of the last menstrual period and clinical pregnancy.
-
Multiple‐pregnancy rate, defined as the number of multiple pregnancies per woman.
-
Miscarriage rate, defined as the number of miscarriages per woman.
-
Pregnancy complications (including ectopic pregnancy, foetal growth disorders, preterm birth < 37 weeks, pregnancy‐induced hypertension, (pre‐) eclampsia, women with haemolysis, elevated liver enzymes, and low platelets in the blood (HELLP syndrome) per woman.
-
Birth weight of babies born per baby.
-
Congenital disorders, defined as the number of congenital abnormalities at birth per live‐born children plus number of foetuses therapeutically terminated.
We also calculated multiple pregnancy, miscarriage, pregnancy complications, and birth weight per clinical pregnancy in a secondary analysis.
Search methods for identification of studies
We searched for all published randomised clinical trials on the freeze‐all strategy, without language restriction and in consultation with the Cochrane Gynaecology and Fertility Group (CGF) Information Specialist.
Electronic searches
We searched the following electronic databases, trial registers, and websites from inception to 14 November 2016 without language restriction and in consultation with the CGF Information Specialist: Cochrane Gynaecology and Fertility Group Specialised Register, Cochrane Central Register of Studies (CENTRAL CRSO), MEDLINE, Embase, PsycINFO, and CINAHL. These search strategies are presented in Appendix 1; Appendix 2; Appendix 3; Appendix 4; Appendix 5; Appendix 6.
Other electronic sources of trials included:
-
trial registers for ongoing and registered trials: ClinicalTrials.gov, a service of the US National Institutes of Health (clinicaltrials.gov/ct2/home) and the World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) (www.who.int/trialsearch/Default.aspx); see Appendix 7; Appendix 8.
-
DARE (Database of Abstracts of Reviews of Effects) in the Cochrane Library for reference lists from relevant non‐Cochrane reviews (onlinelibrary.wiley.com/o/cochrane/cochrane_cldare_articles_fs.html);
-
conference abstracts in the Web of Knowledge (wokinfo.com/);
-
OpenGrey (System for Information on Grey Literature in Europe) (www.opengrey.eu/);
-
PubMed (www.ncbi.nlm.nih.gov/pubmed/).
Searching other resources
We examined the reference lists of eligible articles and contacted study authors where necessary to obtain additional relevant data. We also handsearched relevant journals and conference abstracts that were not covered in the CGF Register.
Data collection and analysis
Selection of studies
Two review authors (KMW and SM) screened the titles and abstracts retrieved by the search and retrieved the full texts of all potentially eligible studies. We independently examined these full‐text articles for compliance with the inclusion criteria and selected studies eligible for inclusion in the review. We corresponded with study investigators as required to clarify study eligibility. Disagreements as to study eligibility were resolved by discussion or by consulting a third review author (SR). We documented the selection process with a PRISMA flow chart (Figure 1).

Study flow diagram.
Data extraction and management
Two review authors (KMW and SM) independently extracted data from the eligible studies using a data extraction form designed and pilot‐tested by the authors. Any discrepancies were resolved by discussion. The data extraction forms included methodological quality and allocation information. We included this information in the review and presented it in the Characteristics of included studies and Characteristics of excluded studies tables.
We corresponded with study investigators to request further data on methods or results, or both, as required.
Assessment of risk of bias in included studies
Two review authors (KMW and SM) independently assessed the included studies for risk of bias using the Cochrane 'Risk of bias' assessment tool for the following domains (Higgins 2011).
Sequence generation
We allocated a low risk of bias if the investigators described a random component in the sequence generation process, such as:
-
using a computerised random number generator;
-
using a random numbers table.
Allocation concealment
We allocated a low risk of bias if the participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation:
-
central computer randomisation;
-
serially numbered, sealed, opaque envelopes.
Blinding
We allocated a low risk of bias if blinding of participants, scientists, and clinicians or nurses had been ensured. However, in this study design it was ethically not possible to blind participants and clinicians. Lack of blinding may not increase the risk of bias if follow‐up is complete and outcomes are unequivocal (live birth).
Completeness of outcome data
We allocated a low risk of bias if there were no missing data, which meant live birth rate and length of follow‐up were stated, loss to follow‐up was accounted for, and an intention‐to‐treat analysis had been carried out.
Selective outcome reporting
We allocated a low risk of bias if all of the study's primary, secondary, and additional outcomes that were of interest in the review had been reported in a prespecified way.
Other sources of bias
We allocated a low risk of bias if the study:
-
was free of commercial funding;
-
reported multiple‐pregnancy rate in the case of an embryo transfer policy of multiple embryos per treatment cycle;
-
had no other source of bias identified (e.g. imbalance in prognostic factors at baseline).
Two review authors (KMW and SM) assessed these domains and resolved any disagreements by consensus or by consulting a third review author (SR). We described the judgements and presented the conclusions in the 'Risk of bias' figures. We took into account all judgements in the interpretation of review findings.
Measures of treatment effect
For dichotomous data (e.g. live birth rates), we used the numbers of events in the freeze‐all strategy and in the conventional IVF/ICSI strategy group of each study to calculate Mantel‐Haenszel odds ratios (ORs) with 95% confidence intervals (CI). We used Peto ORs where the event was very rare (less than 1%) or in the case of zero cell counts. For continuous data (e.g. birth weight), we calculated mean difference (MD) between treatment groups provided that the same measure was used. We reversed the direction of effect of individual studies if required to ensure consistency across trials. We treated ordinal data as continuous data. Where data to calculate ORs or MDs were not available, we utilised the most detailed numerical data available that would facilitate similar analyses of included studies (e.g. test statistics, P values). We compared the magnitude and direction of effect reported by studies with how they were presented in the review, taking into account legitimate differences.
We planned to analyse the outcome 'time to pregnancy' using hazard ratios (HRs).
Unit of analysis issues
We performed the analyses with data per woman randomised, apart from birth weight, which we analysed per baby. If data of the primary analysis were reported per embryo, per oocyte, per cycle, or per transfer, we contacted the authors of the studies for per‐woman data for completeness.
We counted reported multiple live births as one live birth event.
We planned to include only first‐phase data from cross‐over trials.
We also performed secondary analyses for multiple pregnancy, miscarriage, pregnancy complications, and birth weight per clinical pregnancy since these conditions only occur in pregnant women.
Dealing with missing data
We analysed the data on an intention‐to‐treat basis, and contacted the authors of three included studies, Shapiro 2011a, Shapiro 2011b, and Ferraretti 1999, and one excluded study, Absalan 2013, for missing data. We queried the study authors about these missing data and about bias (e.g. randomisation and blinding). One author did not reply to our request for information (Absalan 2013). The remaining authors very kindly responded to our request for additional information, and we were able to include these data in our analysis.
We assumed that live births had not occurred in women without a reported outcome. If studies reported sufficient detail to calculate MDs, but provided no information on associated standard deviations (SD), we assumed that the outcome had a SD equal to the highest SD from other studies within the same analysis.
Assessment of heterogeneity
We considered heterogeneity when the clinical and methodological characteristics of the included studies were sufficiently similar for a meta‐analysis to provide a clinically meaningful summary. We performed statistical analyses in accordance with the guidelines developed by Cochrane (Higgins 2003; Higgins 2011). We assessed heterogeneity between the results of different studies by the I2 statistic, considering an I2 value greater than 50% to indicate substantial heterogeneity (Higgins 2003; Higgins 2011).
Assessment of reporting biases
We aimed to minimise the potential impact of publication and reporting biases by performing a comprehensive search for eligible studies and looking for duplication of data. We planned to perform a funnel plot to investigate the possibility of small‐study effects if 10 or more studies were included in an analysis.
If included studies reported neither the primary outcome measure of live birth nor interim outcomes such as clinical pregnancy, we undertook informal assessment as to whether studies reporting the primary outcome measures reflected typical findings for the interim outcomes. We considered within‐study reporting bias by looking at the protocols.
We addressed the assessment of reporting biases in the Risk of bias in included studies section of the Results.
Data synthesis
We used Review Manager 5 software to perform the meta‐analyses with a fixed‐effect model to calculate pooled ORs and 95% CIs (RevMan 2014). To aid interpretation, we translated findings for primary outcomes to absolute risks, expressed as percentages based on the 95% CIs. We combined results for continuous outcomes using MDs.
Prospectively, we planned to present the analyses as:
-
cumulative live birth rates for IVF/ICSI cycles with frozen‐thawed embryo transfers until live birth was achieved or when all frozen embryos originating from the cycle with ovarian stimulation were transferred in the freeze‐all strategy versus IVF/ICSI cycles with fresh and subsequent frozen‐thawed embryo transfers until live birth was achieved or when all frozen embryos originating from the cycle with ovarian stimulation were transferred in the conventional IVF/ICSI strategy;
-
pregnancy and live birth rates for one IVF/ICSI cycle with the first frozen‐thawed embryo transfer in the freeze‐all strategy versus one IVF/ICSI cycle with the first fresh embryo transfer in the conventional IVF/ICSI strategy (as an additional table).
Subgroup analysis and investigation of heterogeneity
We had planned to perform subanalyses on timing of cryopreservation (e.g. day of embryo development) and method of cryopreservation (e.g. slow freezing or vitrification). However, data were insufficient to conduct all planned subgroup analyses. Should more data become available in the future, we will conduct additional subgroup analyses in later updates of this review.
Sensitivity analysis
We conducted sensitivity analyses for the primary outcome. These analyses included consideration of whether the review conclusions would have differed if:
-
eligibility was restricted to studies without high risk of bias;
-
a random‐effects model had been adopted;
-
the summary effect measure was risk ratio rather than OR.
Overall quality of the body of evidence: 'Summary of findings' table
We prepared a 'Summary of findings' table using GRADEpro software and Cochrane methods (GRADEpro GDT 2014; Higgins 2011). This table evaluates the overall quality of the body of evidence for the main review outcomes. Two review authors independently evaluated the overall quality of the evidence for the outcomes (live birth, OHSS, multiple pregnancy, miscarriage, pregnancy complications and time to pregnancy) using GRADE criteria (study limitations such as risk of bias, consistency of effect, imprecision, indirectness, and publication bias). We justified, documented, and took into account judgements about evidence quality (high, moderate, low, or very low) in the results for each outcome.
Results
Description of studies
Results of the search
Our searches on 14 November 2016 revealed 2401 reports, of which 785 were duplicates, leaving 1622 reports. After screening the title and abstract, we found 12 reports to be potentially eligible, and retrieved these reports in full text.
We excluded four studies: one randomised women to a different intervention that was not clear from the abstract (Boostanfar 2016); two were considered not properly randomised (Absalan 2013; Yang 2015); and one has been retracted (Aflatoonian 2010).
Three studies were ongoing trials and awaiting data (ACTRN12612000422820; NCT02148393; NTR3187).
One study did not clearly report the methods used; it has been classified as awaiting classification and will be reassessed in the next iteration of this review (Chandel 2016).
We included four studies in the review.
See the study flow diagram (Figure 1) and study tables (Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies).
Included studies
Study design and setting
We included four parallel‐design randomised clinical trials (RCTs) in the review. Three were single‐centre studies, conducted in reproductive medical centres in Italy and the United States (Ferraretti 1999; Shapiro 2011a; Shapiro 2011b), and one was a multicentre trial conducted in 14 reproductive medical centres throughout China (Chen 2016).
Participants
The four studies enrolled a total of 1892 women, with 934 women undergoing the freeze‐all strategy and 958 women undergoing the conventional IVF/ICSI strategy. The inclusion criteria of the two studies of Shapiro and colleagues were based on the number of antral follicles observed at baseline ultrasound examination: Shapiro 2011a included normal responders (8 to 15 antral follicles), and Shapiro 2011b included high responders (> 15 antral follicles). Ferraretti 1999 included women at risk of developing OHSS, based on level of oestradiol (E2) and number of retrieved eggs (≥ 15 oocytes). In all trials, the baseline characteristics were similar between the two strategies. Chen 2016 included women with polycystic ovary syndrome. The ages of the women included by Shapiro ranged from 18 to 41 years. The mean age for the women included in Ferraretti 1999 ranged from 31.6 to 31.4 years. Women in Chen 2016 were between the ages of 20 and 34 years. For details, see Characteristics of included studies.
Interventions
All four studies compared the freeze‐all strategy versus the conventional IVF/ICSI strategy.
Women in the Ferraretti 1999 study received a down‐regulation protocol with gonadotropin‐releasing hormone (GnRH) analogue (0.3 mg subcutaneous buserelin acetate (Suprefact) two times a day) and ovarian stimulation with urinary gonadotropin (4 ampoules of follicle‐stimulating hormone (FSH) on the first and second days of treatment, and 2 ampoules of FSH plus 2 ampoules of human menopausal gonadotropins (hMG) on the third and fourth treatment days, followed by an adjusted dosage of gonadotropins according to the individual response measured by plasma concentration of E2 and follicular growth assessed by ultrasound) (Ferraretti 1996). All women received 7500 IU of human chorionic gonadotropin (hCG) 34 to 36 hours before follicle aspiration followed by 20 g of intravenous albumin. Embryos were frozen at the pronuclear stage. All embryos were transferred at the early cleavage stage (day 3) in artificial cycles. The scheme included oral administration of oestradiol valerate, 2 mg daily for the first 5 days of the cycle; 4 mg/day from day 6 to day 10; 6 mg/day from day 11 to day 13; then 4 mg/day from day 14 onward. On day 15 of the cycle, 50 mg of progesterone in oil was administered daily, and on day 17 the dose was increased to 100 mg/day.
In Shapiro 2011a and Shapiro 2011b, women received down‐regulation with a GnRH antagonist and a combination of recombinant FSH and highly purified urinary FSH. Human chorionic gonadotropin (5 to 15 IU per pound body weight (11 to 33 IU/kg)) was administered 34 to 36 hours prior to follicle aspiration. In those women with greater ovarian response, 4 mg leuprolide acetate was added concomitant to the hCG. Embryos were vitrified at the pronuclear stage. All embryos were transferred as blastocysts in artificial cycles. Women with fresh embryo transfers received 6.0 mg daily E2 and daily progesterone injections (typically 100 mg), with progesterone supplementation beginning one to two days after follicle aspiration and E2 initiated as needed. Women with frozen‐thawed embryo transfers were down‐regulated with leuprolide acetate in a subsequent cycle and received oral 6.0 mg daily E2 and E2 patches as needed starting 10 to 14 days before thawing to achieve a target endometrial thickness of at least 8 mm. Daily progesterone injections (typically 100 mg) were started the day before thawing. In both groups, E2 and progesterone supplements were adjusted as needed to sustain serum levels of at least 200 pg/mL and 15 ng/mL, respectively, until increasing serum levels indicated placental production, typically at 9 to 10 weeks’ gestation.
In Chen 2016, women received recombinant FSH at a daily dose of 112.5 IU for those weighing less than 60 kg and 150 IU for those weighing over 60 kg starting on day 2 or 3 of the menstrual cycle. This was adjusted following ovarian response. Human menopausal gonadotropin could be added when considered to appropriate. On the day of oocyte retrieval, women had to have more than 3 and fewer than 30 oocytes with a low risk of OHSS to be randomised. Intramuscular progesterone at a daily dose of 80 mg was administered for luteal‐phase support in the fresh‐transfer group. Embryos were cryopreserved at day 3 of development. Oral oestradiol valerate was used for endometrial preparation on day 2 or 3 of the second menstrual cycle after oocyte retrieval. Intramuscular progesterone (80 mg/day) was added when endometrial thickness reached 8 mm or more or at the physician’s discretion. On day 4 of progesterone administration, two day 3 frozen embryos were thawed and transferred. Luteal‐phase support with oestradiol valerate and intramuscular progesterone for endometrium preparation continued until 10 weeks after conception.
Outcomes
Data were extracted from study reports or provided by authors for the following outcomes.
Primary outcomes
-
Effectiveness: Cumulative live birth per woman. Two studies did not report on live birth in their published article (Shapiro 2011a; Shapiro 2011b), but we were able to obtain these data by personal communication with the authors. One study did not report on live birth rate after the first embryo transfer (Ferraretti 1999), but we were able to obtain these data by personal communication with the authors. Chen 2016 reported these data.
-
Safety: OHSS. One study reported OHSS per woman if hospitalisation was required (Ferraretti 1999). Two studies did not report on OHSS (Shapiro 2011a; Shapiro 2011b), but we were able to obtain these data by personal communication with the authors. However, we did not include the data from these two studies in the analysis, as women with high risk of OHSS were excluded and standardly received the freeze‐all strategy. Chen 2016 reported these data.
Secondary outcomes
-
Two studies reported ongoing pregnancy rate determined at 10 weeks of gestational age (Shapiro 2011a; Shapiro 2011b).
-
Three studies reported clinical pregnancy rate (Ferraretti 1999; Shapiro 2011a; Shapiro 2011b), but only one study reported this outcome cumulative per woman (Ferraretti 1999).
-
None of the studies reported time to pregnancy or the results for each menstrual cycle following randomisation.
-
Two studies reported multiple‐pregnancy rate (Shapiro 2011b; Chen 2016).
-
All four studies reported the number of miscarriages (Ferraretti 1999; Shapiro 2011a; Shapiro 2011b; Chen 2016).
-
One study reported on congenital disorders (Chen 2016).
-
Two studies reported pregnancy complications (Ferraretti 1999; Chen 2016).
-
One study reported birth weight of the newborn (Chen 2016).
Excluded studies
We excluded four potentially eligible studies from the review, for the following reasons.
-
Aflatoonian 2010, as this study was retracted.
-
Absalan 2013, as it was unclear whether it was truly a RCT. This study compared the clinical and delivery rates between the freeze‐all strategy and the conventional strategy in women at risk for OHSS. In their abstract it was stated that women with OHSS were randomly divided into two groups, with fresh embryo transfer and with frozen transfer. However, nothing is mentioned in the methods section about the method of randomisation (sequence generation or allocation concealment) or which method was used to divide women into the two groups. Nothing was reported on the occurrence of OHSS in these women. The authors did not respond to our request for additional information.
-
Yang 2015, as one‐third of all randomised women chose to be in group 3 (fresh transfer of a day 3 embryo followed by frozen‐thawed embryos) after randomisation. We did not consider the study to be a properly randomised RCT.
-
Boostanfar 2016 randomised women to a different intervention that was not clear from the abstract.
Awaiting classification
Chandel 2016 is awaiting classification (see Characteristics of studies awaiting classification); we await more information from the study authors.
Ongoing studies
We identified 12 ongoing studies from trial registers that may have results for inclusion in future versions of this review (ACTRN12612000422820; ACTRN12616000643471; ISRCTN61225414; NCT02000349; NCT02133950; NCT02148393; NCT02471573; NCT02570386; NCT02681367; NCT02712840; NCT02746562; NTR3187). Note that studies that were registered in the trial registers but that were not started or that were withdrawn or stopped were not included in this review.
Risk of bias in included studies
See the 'Risk of bias’ summary (Figure 2) and graph (Figure 3) for the four included trials. See also Characteristics of included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
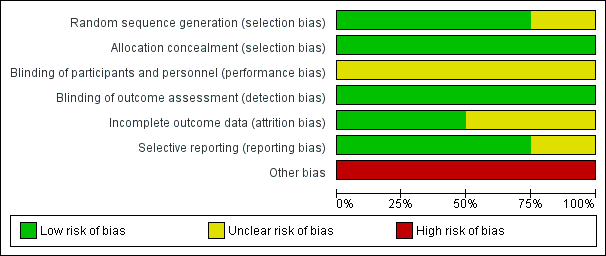
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
Sequence generation
The randomisation procedure was well described in Shapiro 2011a. In the second study of Shapiro 2011b, the authors referred to the randomisation procedure in Shapiro 2011a. These two studies used randomly chosen envelopes, and we judged these two studies to be at low risk of selection bias related to sequence generation. Ferraretti 1999 did not describe the method of randomisation in the published article, but replied in a personal communication that the method of randomisation was performed with random sealed envelopes; we judged this study to be at unclear risk of this bias, as random sequence was used but it was unclear whether envelopes were opaque and sequentially numbered. Randomisation in Chen 2016 was well described; an online central randomisation system was used. We considered risk of selection bias related to sequence generation to be low.
Allocation concealment
Shapiro 2011a and Shapiro 2011b performed allocation concealment by using identical, opaque, unmarked, sealed envelopes, and we therefore judged both studies to be at low risk of selection bias related to allocation concealment. The first author of the Ferraretti 1999 study provided additional information on allocation concealment. This study performed participant allocation by sealed envelopes, and we therefore judged it to be at low risk of bias for this domain. There was low risk of selection bias related to allocation concealment in Chen 2016 due to the use of an online central randomisation system.
Blinding
As described in the Methods section, blinding of the participant or the clinician is technically not possible due to the nature of the intervention in this study design. We felt that lack of blinding was not likely to influence findings for the primary outcomes live birth or OHSS. However, blinding for the primary outcome was not reported for the investigators of the four studies, which could have influenced the decision to terminate a trial. The risk of performance bias was unclear in all four studies.
Incomplete outcome data
Three studies did not report intention‐to‐treat analysis in the methodological or analysis sections (Ferraretti 1999; Shapiro 2011a; Shapiro 2011b), while one study did report intention‐to‐treat analysis (Chen 2016).
We judged the studies by Shapiro 2011a and Shapiro 2011b to be at high risk of attrition bias. These studies did not take into account withdrawals or exclusions of randomised women in the reported analyses. Both studies also analysed the outcomes per embryo transferred instead of per woman. However, sufficient data were available for analysis per woman in meta‐analysis. We prespecified ongoing pregnancy as a viable pregnancy at 12 weeks' gestation. These two studies defined ongoing pregnancy at 10 weeks' gestation, which could slightly overestimate the results for this outcome. Taken these issues into account, we considered the risk of bias to be unclear in these two studies.
Ferraretti 1999 and Chen 2016 did analyse all randomised women. Risk of attrition bias was low.
Selective reporting
One study was registered in a prospective trial register under number NCT01841528, including an automatically indexed link on the published report on the study, and the study protocol was published beforehand (Chen 2016). Prespecified outcomes were generally reported, although some prespecified outcomes (e.g. time to pregnancy) were missing from the report. Considering this, we judged this study to be at low risk of reporting bias. Two studies were registered in a prospective trial register with the respective trial numbers NCT00963625 and NCT00963079 (Shapiro 2011a; Shapiro 2011b). Data on the follow‐up of the studies were available in the trial register. The prespecified outcomes of interest were reported in the two studies, and we judged these studies to be at low risk of this bias. We could not assess reporting bias for Ferraretti 1999, as trial registers did not exist at that time, therefore the risk of reporting bias for this study was unclear.
Other potential sources of bias
Three of the studies did not clearly report their prespecified criteria for early termination of their trial. Ferraretti 1999 did not prespecify rules as to when to terminate the study. In the two studies by Shapiro 2011a and Shapiro 2011b, an interim analysis was planned after 100 completed blastocyst transfers. While women were randomised, the interim analyses were based on completed blastocyst transfers (unit of analysis error). They did not report whether the interim analysis was performed by an independent committee that was blinded for the primary outcome. In addition, Shapiro 2011b pre‐terminated the study after an interim analysis based on differences in embryo quality between the two strategies. This reason was not mentioned as one of the criteria to terminate the study. All three studies cryopreserved embryos at the two pro‐nucleate (2pn) stage with slow freezing, which is not currently a common freezing protocol in IVF centres.
After freezing and thawing, the four studies transferred embryos at a different developmental stage: Ferraretti 1999 and Chen 2016 transferred cleavage embryos, and Shapiro 2011a and Shapiro 2011b transferred blastocysts. None of the four studies reported time to pregnancy or (separate or incremental) data per subsequent menstrual or cryo‐transfer cycle (relevant for time‐to‐pregnancy comparison). The difference in technical protocols (some of which are not common practice) between studies in day of cryopreservation and embryo developmental stage of transfer, together with the differences in study population, complicates the comparison between freeze‐all and conventional IVF/ICSI strategies and could introduce heterogeneity between studies. We therefore judged all studies to be at high risk of this bias.
Effects of interventions
We included four studies involving 1892 women in this review. See summary of findings Table for the main comparison.
1. Comparison of the freeze‐all strategy versus the conventional IVF/ICSI strategy
Primary outcomes
1.1 Effectiveness: Cumulative live birth per woman
All studies collected data on cumulative live birth rates (Ferraretti 1999; Shapiro 2011a; Shapiro 2011b; Chen 2016). There was no clear evidence of a difference between the freeze‐all strategy and the conventional IVF/ICSI strategy in cumulative live birth rates (OR 1.09, 95% CI 0.91 to 1.31; 4 trials; 1892 women; I2 = 0%; moderate‐quality evidence).
It was unclear whether there was any difference between the two strategies in cumulative live birth rate when the studies were analysed per cleavage stage (OR 1.11, 95% CI 0.91 to 1.35; 2 trials; 1633 women; low‐quality evidence) or blastocyst transfer stage (OR 0.99, 95% CI 0.60 to 1.62; 2 trials; 259 women; low‐quality evidence) (Analysis 1.1; Figure 4).

Forest plot of comparison: 1 Freeze‐all vs conventional IVF, outcomes per woman, outcome: 1.1 Live birth rate.
1.2 Safety: Ovarian hyperstimulation syndrome per woman
One study reported OHSS per woman if hospitalisation was required (Ferraretti 1999). Two studies did not report on OHSS, but we were able to obtain these data by personal communication with the authors (Shapiro 2011a; Shapiro 2011b). However, we did not include the data from these two studies in the analysis as women with high risk of OHSS were excluded and standardly received the freeze‐all strategy. Chen 2016 reported these data. The prevalence of OHSS was lower after the freeze‐all strategy compared to the conventional IVF/ICSI strategy (OR 0.24, 95% CI 0.15 to 0.38; 2 trials; 1633 women; I2 = 0%; low‐quality evidence) (Analysis 1.2; Figure 5).

Forest plot of comparison: 1 Freeze‐all vs conventional IVF, outcomes per woman, outcome: 1.2 OHSS.
Secondary outcomes
1.3 Ongoing pregnancy rate per woman
Two studies reported on the cumulative ongoing pregnancy rates (Shapiro 2011a; Shapiro 2011b). There was no evidence of a difference between the two strategies in the cumulative ongoing pregnancy rate (OR 1.05, 95% CI 0.64 to 1.73; 2 trials; 259 women; I2 = 0%; low‐quality evidence) (Analysis 1.3; Figure 6).

Forest plot of comparison: 1 Freeze‐all vs conventional IVF, outcomes per woman, outcome: 1.3 Ongoing pregnancy rate.
1.4 Clinical pregnancy rate per woman
One study reported the cumulative clinical pregnancy rates (Ferraretti 1999), therefore pooling was not possible. There was no evidence of a difference between the two strategies in clinical pregnancy rate (OR 1.08, 95% CI 0.54 to 2.19; 1 trial; 125 women; low‐quality evidence) (Analysis 1.4; Figure 7).

Forest plot of comparison: 1 Freeze‐all vs conventional IVF, outcomes per woman, outcome: 1.4 Clinical pregnancy rate.
1.5 Time to pregnancy
No study reported the time to pregnancy or (separate or incremental) data per subsequent menstrual or cryo‐transfer cycle (relevant for time‐to‐pregnancy comparison).
1.6 Multiple‐pregnancy rate
Two studies reported on the multiple‐pregnancy rate (Shapiro 2011b; Chen 2016). There was no evidence of a difference between the two strategies in multiple‐pregnancy rate (OR 1.11, 95% CI 0.85 to 1.44; 2 trials; 1630 women; low‐quality evidence) (Analysis 1.5; Figure 8).

Forest plot of comparison: 1 Freeze‐all vs conventional IVF, outcomes per woman, outcome: 1.5 Multiple pregnancy rate.
1.7 Miscarriage rate
All studies reported the miscarriage rate (Ferraretti 1999; Shapiro 2011a; Shapiro 2011b; Chen 2016). Miscarriage rate was lower in the freeze‐all group (OR 0.67, 95% CI 0.52 to 0.86; 4 trials; 1892 women; I2 = 0%, low‐quality evidence) (Analysis 1.6; Figure 9).

Forest plot of comparison: 1 Freeze‐all vs conventional IVF, outcomes per woman, outcome: 1.6 Miscarriage rate.
1.8 Pregnancy complications
Two studies reported on pregnancy complications (Ferraretti 1999; Chen 2016). There were more pregnancy complications in the freeze‐all group (OR 1.44, 95% CI 1.08 to 1.92; 2 trials; 1633 women; low‐quality evidence) (Analysis 1.7; Figure 10).

Forest plot of comparison: 1 Freeze‐all vs conventional IVF, outcomes per woman, outcome: 1.7 Pregnancy complications.
1.9 Birth weight
One study reported on birth weight (Chen 2016). A higher birth weight of singleton babies born was reported for the freeze‐all strategy (MD 161.8 g, 95% CI 57.1 to 266.5; 1 trial; 462 singletons; low‐quality evidence). Birth weight of multiples was similar between strategies (MD ‐2.00 g, 95% CI ‐94.08 to 90.08; 1 trial; 453 multiples; low‐quality evidence) (Analysis 1.8; Figure 11).

Forest plot of comparison: 1 Freeze‐all vs conventional IVF, outcomes per woman, outcome: 1.8 Birth weight of babies born.
1.10 Congenital abnormalities
One study reported on congenital abnormalities (Chen 2016). There was no evidence of a difference between the two strategies for congenital abnormalities per live‐born children plus number of fetuses therapeutically terminated (OR 1.25, 95% CI 0.66 to 2.37; 1 trial; 923 live‐born children plus number of fetuses therapeutically terminated; low‐quality evidence) (Analysis 3.1; Figure 12).

Forest plot of comparison: 3 Freeze‐all vs conventional IVF, congenital abnormalities per live‐born children plus number of foetuses therapeutically terminated, outcome: 3.1 Congenital abnormalities.
Other analyses
We also analysed the adverse events multiple pregnancy, miscarriage and pregnancy complications per clinical pregnancy (Analysis 2.1 , Analysis 2.2 , Analysis 2.3). There was no evidence of a difference between the two strategies for multiple pregnancy per clinical pregnancy after the first transfer (OR 1.02, 95% CI 0.77 to 1.37; 2 trials; 939 clinical pregnancies) (Analysis 2.1). Miscarriage rate was lower in the freeze‐all group per clinical pregnancy after the first transfer (OR 0.56, 95% CI 0.41 to 0.77; 4 trials; 1058 clinical pregnancies) (Analysis 2.2).There were more pregnancy complications in the freeze‐all group per clinical pregnancy after the first transfer (OR 1.43, 95% CI 1.05 to 1.95; 2 trials; 914 clinical pregnancies) (Analysis 2.3).
Sensitivity analysis
We did not undertake sensitivity analysis by risk of bias because all studies in the analyses were at high risk of bias in at least one domain. We undertook sensitivity analyses of the primary outcome using 1) adoption of a random‐effects model and 2) using the summary effect measure of risk ratio (RR) rather than OR. Neither of the sensitivity analyses made any material difference to the findings (Table 1).
| Studies, number of participants | OR, 95% CI, fixed effect | OR, 95% CI, random effect | RR, 95% CI, fixed effect | RR, 95% CI, random effect |
| Ferraretti 1999 (n = 125) Shapiro 2011a (n = 103) Shapiro 2011b (n = 122) Chen 2016 (n = 1508) | 1.09 (0.91, 1.31) | 1.09 (0.91, 1.31) | 1.04 (0.96, 1.12) | 1.04 (0.96, 1.12) |
CI: confidence interval
OR: odds ratio
RR: risk ratio
Discussion
Summary of main results
There was no clear evidence of a difference between the freeze‐all strategy and the conventional IVF/ICSI strategy in cumulative live birth rates per woman, but the prevalence of OHSS appears to be lower after the freeze‐all strategy. The freeze‐all strategy appears to be associated with fewer miscarriages and a higher birth weight of singleton babies (MD 161.80 g, 95% CI 57.11 to 266.49), but also with an increased rate of pregnancy complications.
Overall completeness and applicability of evidence
All trials provided data on the primary outcome live birth rate, but for OHSS we could use data from only two studies.
Three out of four included studies involved a small number of women. All studies had specific and differing technical protocols, and studies had differing inclusion criteria leading to the inclusion of select groups of women ('normal responders', 'high responders', women with polycystic ovary syndrome, women with high OHSS risk). No study included women with low ovarian response.
Quality of the evidence
We rated the quality of evidence using GRADE methods and judged it to be moderate to low, due to serious risk of bias and (for some outcomes) serious imprecision. Risk of bias was associated with unclear blinding of investigators for preliminary outcomes of the study, unit of analysis error, and absence of adequate study termination rules.
The four included studies involved a total of 934 women undergoing the freeze‐all strategy and 958 women undergoing the conventional IVF/ICSI strategy. Varying protocols between studies (some not common in routine practice), varying study population (select groups of women undergoing IVF), one study without power calculation reported (unclear what determined the end of study), and two studies with interim analysis that was calculated per transfer (unit of analysis error) with absence of adequate stopping rules (possible overestimation of treatment effect) resulted in an overall judgement of the evidence as low quality.
Our searches identified 12 ongoing studies. We anticipate that the evidence from these will provide a more definitive answer on the relative effectiveness and safety of a freeze‐all strategy.
Potential biases in the review process
We tried to reduce potential bias in the review process to a minimum by identifying all eligible trials for inclusion in this meta‐analysis. We were able to retrieve additional information on three included trials where required, which helped us in providing accurate study outcomes.
Agreements and disagreements with other studies or reviews
Three out of four included studies reported higher pregnancy or live birth rates for the freeze‐all strategy than for conventional IVF/ICSI treatment including fresh transfer in the published manuscripts (Shapiro 2011b; Shapiro 2011a; Chen 2016), while our review concluded that there was no difference in live birth rates between the strategies. This discrepancy in conclusion is attributed to the fact that these publications focussed on outcomes that were reported per first transfer, whereas in our review we focused on the cumulative live birth rate per woman randomised. The live birth rate calculated per first transfer possibly shows differences in outcome for a stimulated and an unstimulated uterus, although this does not take into account the number of embryos that were thawed for transfer. But for women undergoing treatment, the live birth rate per first transfer is less relevant since at the same time of first transfer in a freeze‐all strategy, they would already have received the second transfer (in case of sufficient number of embryos) in a conventional strategy including fresh transfer. We therefore used the cumulative live birth rate as a primary outcome. In case cumulative live birth rates are comparable, as found in our review, then the difference between strategies could be time to pregnancy. Unfortunately, this outcome was not reported in any of the included studies, but by design time to pregnancy is shorter in the conventional strategy than in the freeze‐all strategy when the cumulative live birth rate is comparable. For illustrative purposes we also calculated and presented the live birth rate per first transfer (Table 2).
| Outcome | Number of studies | Number of participants | Analysis method | OR |
| Live birth rate after first embryo transfer for all embryo stages of transfer | 4 | 1892 | Odds ratio (Mantel‐Haenszel, fixed, 95% confidence interval) | 1.34 (1.12, 1.61) |
| Live birth rate after first transfer with cleavage‐stage embryos | 2 | 1633 | Odds ratio (Mantel‐Haenszel, fixed, 95% confidence interval) | 1.31 (1.08, 1.59) |
| Live birth rate after first transfer with blastocyst‐stage embryo | 2 | 259 | Odds ratio (Mantel‐Haenszel, fixed, 95% confidence interval) | 1.54 (0.94, 2.52) |
Live birth rate calculated per first transfer is added for illustrative purposes as this comparison is often reported in the literature. It possibly shows differences in outcome for a stimulated and an unstimulated uterus, although this does not take into account the number of embryos that were thawed for transfer. This outcome is less relevant for women undergoing treatment since at the same time of first transfer in a freeze‐all strategy, they would already have received the second transfer (in case of sufficient number of embryos) in a conventional strategy that includes fresh transfer.
The same difference in primary outcome (cumulative live birth rate versus live birth rate per first transfer) explains the difference from previous reviews that found improved IVF/ICSI outcomes with the freeze‐all strategy, such as Roque 2013, although the included studies also differed. Roque and colleagues did not include the study of Ferraretti 1999 in their analysis, for reasons that are unclear. The authors did include the retracted study of Aflatoonian 2010 in their analysis. The Chen 2016 study was not yet published when this review was written.
Although we reported pregnancy and live birth rates only cumulatively for the above reasons, for other outcomes, such as the number of multiples and the number of miscarriages, we did report the numbers per first transfer, as cumulative rates for these outcomes were not available from any of the studies.
The lower rate of OHSS found in our review is in agreement with previous studies, and is to be expected, as avoiding a pregnancy in the initial cycle with ovarian stimulation by only transferring frozen‐thawed embryos in subsequent unstimulated cycles would eliminate the residual risks of OHSS, and OHSS would therefore be self limiting. Mild OHSS symptoms can still occur as a result of the hCG trigger in the hyperstimulated cycle in the freeze‐all strategy, but OHSS in its severe form should be rare.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
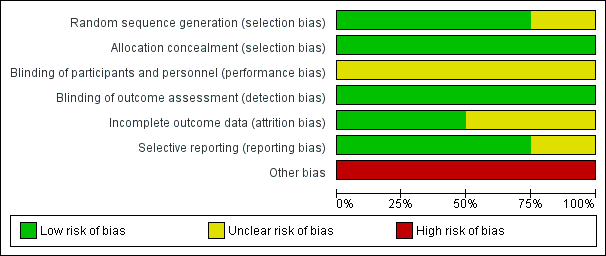
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Forest plot of comparison: 1 Freeze‐all vs conventional IVF, outcomes per woman, outcome: 1.1 Live birth rate.

Forest plot of comparison: 1 Freeze‐all vs conventional IVF, outcomes per woman, outcome: 1.2 OHSS.

Forest plot of comparison: 1 Freeze‐all vs conventional IVF, outcomes per woman, outcome: 1.3 Ongoing pregnancy rate.

Forest plot of comparison: 1 Freeze‐all vs conventional IVF, outcomes per woman, outcome: 1.4 Clinical pregnancy rate.

Forest plot of comparison: 1 Freeze‐all vs conventional IVF, outcomes per woman, outcome: 1.5 Multiple pregnancy rate.

Forest plot of comparison: 1 Freeze‐all vs conventional IVF, outcomes per woman, outcome: 1.6 Miscarriage rate.

Forest plot of comparison: 1 Freeze‐all vs conventional IVF, outcomes per woman, outcome: 1.7 Pregnancy complications.

Forest plot of comparison: 1 Freeze‐all vs conventional IVF, outcomes per woman, outcome: 1.8 Birth weight of babies born.

Forest plot of comparison: 3 Freeze‐all vs conventional IVF, congenital abnormalities per live‐born children plus number of foetuses therapeutically terminated, outcome: 3.1 Congenital abnormalities.

Comparison 1 Freeze‐all versus conventional IVF, outcomes per woman, Outcome 1 Live birth rate.
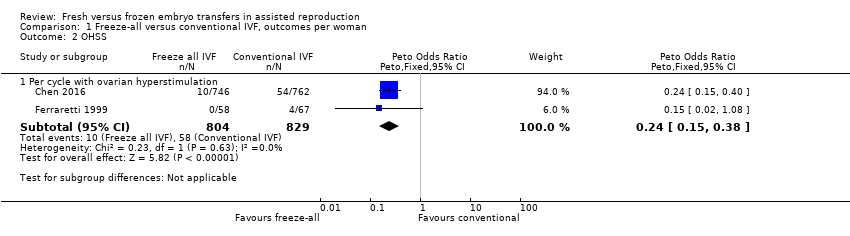
Comparison 1 Freeze‐all versus conventional IVF, outcomes per woman, Outcome 2 OHSS.

Comparison 1 Freeze‐all versus conventional IVF, outcomes per woman, Outcome 3 Ongoing pregnancy rate.

Comparison 1 Freeze‐all versus conventional IVF, outcomes per woman, Outcome 4 Clinical pregnancy rate.

Comparison 1 Freeze‐all versus conventional IVF, outcomes per woman, Outcome 5 Multiple pregnancy rate.

Comparison 1 Freeze‐all versus conventional IVF, outcomes per woman, Outcome 6 Miscarriage rate.

Comparison 1 Freeze‐all versus conventional IVF, outcomes per woman, Outcome 7 Pregnancy complications.

Comparison 1 Freeze‐all versus conventional IVF, outcomes per woman, Outcome 8 Birth weight of babies born.

Comparison 2 Freeze‐all versus conventional IVF, adverse events per clinical pregnancy, Outcome 1 Multiple pregnancy.

Comparison 2 Freeze‐all versus conventional IVF, adverse events per clinical pregnancy, Outcome 2 Miscarriage.

Comparison 2 Freeze‐all versus conventional IVF, adverse events per clinical pregnancy, Outcome 3 Pregnancy complications.

Comparison 3 Freeze‐all versus conventional IVF, congenital abnormalities per live‐born children plus number of foetuses therapeutically terminated, Outcome 1 Congenital abnormalities.
| Fresh versus frozen embryo transfers in assisted reproduction | ||||||
| Patient or population: women undergoing assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with fresh and frozen embryo transfers | Risk with frozen embryo transfers only | |||||
| Live birth rate cumulatively for all embryo stages of transfer | 579 per 1000 | 600 per 1000 | OR 1.09 | 1892 | ⊕⊕⊕⊝ | |
| Ovarian hyperstimulation syndrome per cycle with ovarian hyperstimulation | 70 per 1000 | 18 per 1000 | OR 0.24 | 1633 | ⊕⊕⊝⊝ | |
| Multiple pregnancy per woman after first ET | 161 per 1000 | 176 per 1000 (141 to 217) | OR 1.11 (0.85 to 1.44) | 1630 (2 RCTs) | ⊕⊕⊝⊝ | |
| Miscarriage per woman after first ET | 184 per 1000 | 131 per 1000 (105 to 162) | OR 0.67 (0.52 to 0.86) | 1892 | ⊕⊕⊝⊝ | |
| Pregnancy complications per woman after first ET | 110 per 1000 | 151 per 1000 (118 to 191) | OR 1.44 (1.08 to 1.92) | 1633 | ⊕⊕⊝⊝ | |
| Time to pregnancy | Not reported in any of the included studies | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level due to serious risk of bias associated with lack of power calculation (unclear what determined end of study) and/or use of interim analysis that was calculated per transfer (unit of analysis error) with absence of adequate stopping rules (possible overestimation of treatment effect). | ||||||
| Studies, number of participants | OR, 95% CI, fixed effect | OR, 95% CI, random effect | RR, 95% CI, fixed effect | RR, 95% CI, random effect |
| Ferraretti 1999 (n = 125) Shapiro 2011a (n = 103) Shapiro 2011b (n = 122) Chen 2016 (n = 1508) | 1.09 (0.91, 1.31) | 1.09 (0.91, 1.31) | 1.04 (0.96, 1.12) | 1.04 (0.96, 1.12) |
| CI: confidence interval | ||||
| Outcome | Number of studies | Number of participants | Analysis method | OR |
| Live birth rate after first embryo transfer for all embryo stages of transfer | 4 | 1892 | Odds ratio (Mantel‐Haenszel, fixed, 95% confidence interval) | 1.34 (1.12, 1.61) |
| Live birth rate after first transfer with cleavage‐stage embryos | 2 | 1633 | Odds ratio (Mantel‐Haenszel, fixed, 95% confidence interval) | 1.31 (1.08, 1.59) |
| Live birth rate after first transfer with blastocyst‐stage embryo | 2 | 259 | Odds ratio (Mantel‐Haenszel, fixed, 95% confidence interval) | 1.54 (0.94, 2.52) |
| Live birth rate calculated per first transfer is added for illustrative purposes as this comparison is often reported in the literature. It possibly shows differences in outcome for a stimulated and an unstimulated uterus, although this does not take into account the number of embryos that were thawed for transfer. This outcome is less relevant for women undergoing treatment since at the same time of first transfer in a freeze‐all strategy, they would already have received the second transfer (in case of sufficient number of embryos) in a conventional strategy that includes fresh transfer. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Live birth rate Show forest plot | 4 | 1892 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.91, 1.31] |
| 1.1 Live birth rate: cumulatively for cleavage stage transfer | 2 | 1633 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.91, 1.35] |
| 1.2 Live birth rate: cumulatively for blastocyst stage transfer | 2 | 259 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.60, 1.62] |
| 2 OHSS Show forest plot | 2 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 2.1 Per cycle with ovarian hyperstimulation | 2 | 1633 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.24 [0.15, 0.38] |
| 3 Ongoing pregnancy rate Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Cumulatively | 2 | 259 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.64, 1.73] |
| 4 Clinical pregnancy rate Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Cumulatively | 1 | 125 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.54, 2.19] |
| 5 Multiple pregnancy rate Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 After first ET | 2 | 1630 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.85, 1.44] |
| 6 Miscarriage rate Show forest plot | 4 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 After first ET | 4 | 1892 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.52, 0.86] |
| 7 Pregnancy complications Show forest plot | 2 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 7.1 After first ET | 2 | 1633 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.44 [1.08, 1.92] |
| 8 Birth weight of babies born Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Birth weight of singletons | 1 | 462 | Mean Difference (IV, Fixed, 95% CI) | 161.80 [57.11, 266.49] |
| 8.2 Birth weight of multiples | 1 | 453 | Mean Difference (IV, Fixed, 95% CI) | ‐2.0 [‐94.08, 90.08] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Multiple pregnancy Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 After first ET | 2 | 939 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.77, 1.37] |
| 2 Miscarriage Show forest plot | 4 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 After first ET | 4 | 1058 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.41, 0.77] |
| 3 Pregnancy complications Show forest plot | 2 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 3.1 After first ET | 2 | 914 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.43 [1.05, 1.95] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Congenital abnormalities Show forest plot | 1 | 923 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.66, 2.37] |

