重症病患的康复日记
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Pragmatic, randomized controlled trial in six European countries, with two ICUs per country. | |
| Participants | 352 adult ICU patients randomized, 322 completed study. Inclusion criteria: Admitted to ICU for > 72 hours; ventilated for > 24 hours. Exclusion criteria: Too confused to give informed consent; pre‐existing psychotic illness (e.g. schizophrenia); diagnosed PTSD. | |
| Interventions | ICU diary: a daily record of the patient's ICU stay, written in everyday language and accompanied by photographs. Authored by multidisciplinary healthcare staff and family. Diaries standardized via the provision of guidelines to each centre. The diary was introduced to the patient by a research nurse or doctor who ensured that they understood its contents but did not give any advice on what to do with it. This was done either face‐to‐face or over the phone. Controls: Received standard care at each setting. At several of the study sites, this involved giving patients verbal information about their illness prior to discharge from hospital. All control participants received the ICU diary after the final outcome assessment. | |
| Outcomes | Patient ICU memory recall: assessed using ICUMT at randomization (1‐month post ICU discharge) and 3‐month follow‐up. Patient post‐traumatic stress symptomatology: assessed using post‐traumatic stress‐14 at randomization and 3‐month follow‐up. Patient PTSD: assessed using post‐traumatic diagnostic scale with a blinded clinician within a 'diagnostic' interview at the 3‐month follow‐up. Not included within this systematic review. | |
| Notes | ICU: Intensive care unit | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomised in blocks of six through computerised random number generation" (p. 4) |
| Allocation concealment (selection bias) | Low risk | Quote: "Assigned to treatment or control at one‐month using closed, non‐transparent envelope technique" (p. 4) |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "Impractical to guarantee blinding of allocation of the diary as patients would volunteer their use" (p. 3). |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: "In order to reduce bias and ensure blinding of the diagnosis of post traumatic stress disorder at the three‐month follow‐up, the researchers were only trained to interview and administer the post‐traumatic diagnostic scale but were not made aware of the scoring calculation or in what way each question contributed to the score and final diagnosis" (p. 3). For the outcomes included within this review, assessment was made via questionnaire by the participants, who were not blinded to the intervention. It is not known whether the researchers summarising these questionnaire results were blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Less than 10% attrition. Well described reasons for participant withdrawal from the study. (p. 4) |
| Selective reporting (reporting bias) | Low risk | Research protocol well described, clinical trial registered. All outcomes reported. (p. 1, 3, 5) |
| Other bias | Low risk | Nil |
| Methods | Pragmatic, randomized controlled trial in two European ICUs. | |
| Participants | 36 family members of adult ICU patients randomized; 30 completed the study. Inclusion criteria: Family members of those recruited to Jones 2010. That is, patients who were admitted to ICU for > 72 hours; ventilated for > 24 hours. Exclusion criteria: Too confused to give informed consent; pre‐existing psychotic illness (e.g. schizophrenia); diagnosed post‐traumatic stress disorder. | |
| Interventions | ICU diary: a daily record of the family members' experiences of patients' ICU stay, written in everyday language and accompanied by photographs. Authored by multidisciplinary healthcare staff and family. Diaries standardized via the provision of guidelines to each centre. The diary was introduced to the family member by a research nurse or doctor who ensured that they understood its contents but did not give any advice on what to do with it. This was done either face‐to‐face or over the phone. Controls: Received standard care at each setting. At several of the study sites, this involved giving family members verbal information. All control participants received the ICU diary after the final outcome assessment. | |
| Outcomes | Family member post‐traumatic stress symptomatology: assessed using post‐traumatic stress‐14 at randomization and 3‐month follow‐up. | |
| Notes | ICU: Intensive care unit | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Just before randomization to the study group" (p. 174): Random sequence generation as reported by Jones 2010: Quote: "Randomised in blocks of six through computerised random number generation" (p. 4) |
| Allocation concealment (selection bias) | Low risk | Allocation concealment as reported by Jones 2010: Quote: "Assigned to treatment or control at one‐month using closed, non‐transparent envelope technique" (p. 4) |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not able to blind participants and personnel to their allocation, as reported by Jones 2010. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Assessment was made via questionnaire by the participants, who were not blinded to the intervention. It is not known whether the researchers summarising these questionnaire results were blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Less than 10% attrition. Well described reasons for participant withdrawal from the study. (p. 174) |
| Selective reporting (reporting bias) | Low risk | Research protocol well described, clinical trial registered. All outcomes reported. (p. 173, 4, 5) |
| Other bias | Low risk | Nil |
| Methods | Pragmatic, randomized controlled trial in a single British ICU. | |
| Participants | 36 adult ICU patients. Inclusion criteria: Admitted to ICU for > 48 hours. Exclusion criteria: Age < 18 years or > 85 years; admitted following a deliberate suicide attempt; currently experiencing clinically significant psychological symptomatology which predated their admission to ICU; history of dementia or other organic memory problems. | |
| Interventions | ICU diary: a daily record of the patient's ICU stay, authored by multidisciplinary healthcare staff. Diaries standardized under the headings: patient's appearance and condition, events on the ward, details of any treatment or procedures administered in lay language and the names of any visitors. The diary was handed over by the ICU nurse consultant who read it with the patient and answered questions in a verbal feedback session. Controls: Received standard care. All control participants received the ICU diary after the final outcome assessment. | |
| Outcomes | Anxiety: assessed using Hospital Anxiety and Depression Scale; at initial assessment (1‐month post ICU discharge) and 3 weeks later. Depression: assessed using Hospital Anxiety and Depression Scale; at initial assessment (1‐month post ICU discharge) and 3 weeks later. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomly allocated" (p. 185) |
| Allocation concealment (selection bias) | Low risk | Quote: "Presealed envelopes" (p.185) Private correspondence with authors: "Opaque envelopes were used". |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "ICU staff were blind to the patients' group membership, but the participants themselves... were not". (p. 185) |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "The principal investigator (who conducted the psychological assessment) was not (blinded)". (p. 185) |
| Incomplete outcome data (attrition bias) | Low risk | Flow diagram regarding recruitment and attrition provided. No loss to follow‐up. (p. 186) |
| Selective reporting (reporting bias) | High risk | No protocol or clinical trial registry. Not all outcomes reported. Quote: "findings from the other assessment tools will be presented in a separate paper" (p. 186). No subsequent publication located. |
| Other bias | Unclear risk | Significant differences between control and experimental groups including ICU length of stay, APACHE II (p. 186‐187) which are associated with increased risk of PTSD. |
Abbreviations:
APACHE II = Acute Physiology and Chronic Health Evaluation II; ICU = intensive care unit; ICUMT = intensive care unit memory tool; P = page; PTSD = post‐traumatic stress disorder.
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Commentary paper on Jones 2012 | |
| Observational study | |
| Prospective cohort study with retrospective reference group | |
| Observational study | |
| Time‐series design | |
| Observational study | |
| Observational study | |
| Observational study | |
| Observational study |
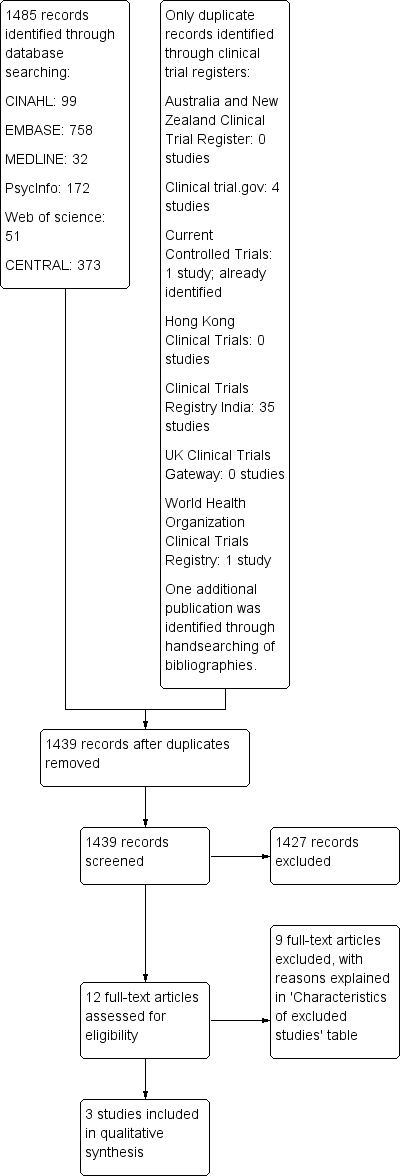
Study flow diagram.
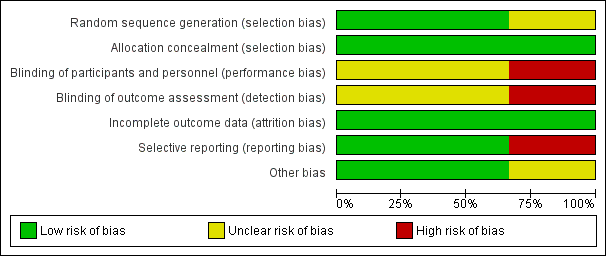
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
| Outcomes | Study | Incidence | Number of participants | Quality of the evidence: GRADE |
| Risk of anxiety in patients recovering from admission to ICU Hospital Anxiety and Depression Scale (Zigmond 1983) | Patient diary: 2 of 18 participants (11.1%) had the likely presence of clinically significant anxiety. No patient diary: 7 of 18 participants (38.9%) had the likely presence of clinically significant anxiety. | 36 | ⊕⊝⊝⊝ very low 1,2 | |
| Risk of depression in patients recovering from admission to ICU Hospital Anxiety and Depression Scale (Zigmond 1983) | Patient diary: 3 of 18 participants (16.7%) had the likely presence of clinically significant depression. No patient diary: 8 of 18 participants (44.4%) had the likely presence of clinically significant depression. | 36 | ⊕⊝⊝⊝ very low 1,2 | |
| Risk of memory recall of ICU in patients recovering from admission to ICU Intensive Care Unit Memory Tool (Jones 2000) | Patient diary: 85 of 162 participants (55%) had recall of delusional ICU memories. No patient diary: 81 of 160 participants (52%) had recall of delusional ICU memories. | 322 | ⊕⊕⊝⊝ low 2 | |
| Post‐traumatic stress symptomatology in patients recovering from admission to ICU Post‐Traumatic Stress Disorder‐Related Symptoms Screening Tool 14 (Twigg 2008) | Patient diary: The median post‐traumatic stress symptomatology in the patient diary group was 24 (SD 11.6)3 No patient diary: The median post‐traumatic stress symptomatology in the no patient diary group was 24 (SD 11.6) 3 | 322 | ⊕⊕⊝⊝ low 2 | |
| Post‐traumatic stress symptomatology in family members of patients recovering from admission to ICU Post‐Traumatic Stress Disorder‐Related Symptoms Screening Tool 14 (Twigg 2008) | Patient diary: The median post‐traumatic stress symptomatology in the patient diary group was 19 (range 14 to 28) 3 No patient diary: The median post‐traumatic stress symptomatology in the no diary group was 28 (range 14 to 38) 3 | 30 | ⊕⊕⊝⊝ low 2 | |
| GRADE Working Group grades of evidence | ||||
| CI: Confidence interval | ||||
| 1 Results are from a single study at risk of bias regarding blinding of outcome assessment and participants. | ||||

