Interventions for women in subsequent pregnancies following obstetric anal sphincter injury to reduce the risk of recurrent injury and associated harms
Abstract
Background
Perineal damage occurs frequently during childbirth, with severe damage involving injury to the anal sphincter reported in up to 18% of vaginal births. Women who have sustained anal sphincter damage are more likely to suffer perineal pain, dyspareunia (painful sexual intercourse), defaecatory dysfunction, and urinary and faecal incontinence compared to those without damage. Interventions in a subsequent pregnancy may be beneficial in reducing the risk of further severe trauma and may reduce the risk of associated morbidities.
Objectives
To examine the effects of Interventions for women in subsequent pregnancies following obstetric anal sphincter injury for improving health.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register (30 September 2014).
Selection criteria
Randomised controlled trials, cluster‐randomised trials and multi‐arm trials assessing the effects of any intervention in subsequent pregnancies following obstetric anal sphincter injury to improve health. Quasi‐randomised controlled trials and cross‐over trials were not eligible for inclusion.
Data collection and analysis
No trials were included. In future updates of this review, at least two review authors will extract data and assess the risk of bias of included studies.
Main results
No eligible completed trials were identified. One ongoing trial was identified.
Authors' conclusions
No relevant trials were included. The effectiveness of interventions for women in subsequent pregnancies following obstetric anal sphincter injury for improving health is therefore unknown. Randomised trials to assess the relative effects of interventions are required before clear practice recommendations can be made.
PICO
Plain language summary
Interventions for women in pregnancies following obstetric anal sphincter injury to reduce the risk of recurrent injury and harms
Three quarters of women who give birth vaginally sustain damage to the area between their vagina and anus (the perineum). Severe damage, involving the anal sphincter is less common, occurring in up to a fifth of vaginal births. Reported rates of anal sphincter damage vary widely which may be due to several reasons including: under and over reporting, use of different diagnostic criteria, different assessment methods and differences in training in the recognition of damage.
Sphincter damage is associated with an increased risk of short‐ and long‐term ill‐health including perineal pain, painful intercourse, bowel dysfunction, and urinary and faecal incontinence. Perineal pain following birth can affect maternal and infant bonding, ability to breastfeed and may increase the risk of urinary retention and painful intercourse, reduce well‐being and increase the risk of depression.
Women who have sustained sphincter damage during childbirth who become pregnant again, may benefit from a number of interventions to reduce the risk of repeated damage. These interventions include: antenatal pelvic floor exercises and biofeedback training to strengthen the pelvic floor; perineal massage or creams to reduce the risk of perineal tearing, or interventions during labour aimed at reducing the risk of sphincter damage including: earlier induction of labour to reduce the risk of a large baby, elective caesarean section to avoid perineal damage, vacuum extraction as opposed to forceps and selective episiotomy to reduce the risk of severe perineal damage.
Only one ongoing randomised trial was identified evaluating caesarean section compared with vaginal birth for women in subsequent pregnancies following obstetric anal sphincter injury to reduce the risk of recurrent injury and associated harms. High‐quality, adequately‐powered trials are therefore required to evaluate the relative effectiveness of different interventions to improve health in subsequent pregnancies following obstetric anal sphincter injury.
Authors' conclusions
Background
Perineal trauma (damage to the area between the vagina and anus) occurs in over three‐quarters of vaginal births (Albers 1999; McCandlish 1998). Obstetric anal sphincter injury (OASI) is perineal trauma involving the anal sphincter (the ring of muscle controlling the entrance to the rectum). OASI is the severe end of the spectrum of perineal trauma and is associated with increased morbidity. Primary OASI (OASI occurring for the first time), affects up to 18% (range 1.7% to 18%) of vaginal births (Harkin 2003; Hirayama 2012; Lowder 2007). Recurrent OASI (OASI in a subsequent pregnancy, previously affected by OASI) affects up to 7.2% of vaginal births (range 4.0% to 7.2%) (Dandolu 2005; Edozien 2014; Harkin 2003; Payne 1999; Peleg 1999). There is wide variation in reported rates of OASI between countries (Hirayama 2012), which may be due to under or over reporting, differences in training in the recognition of OASI and the variety of tools used to identify injury. Tools used include: clinical examination, endoanal ultrasonography (use of an ultrasound probe to identify sphincter damage), anal manometry (use of a pressure sensitive probe to measure muscle tone) and patient questionnaires (to assess symptoms and quality of life).
Incidence rate and predisposing risk factors
Incidence rate reporting is complex. The inclusion or exclusion of women with differing risk factors (for example, use of forceps or episiotomy) will alter the denominator population and influence the incidence rate of OASI reported (Abbott 2010). Also the rate is sometimes reported for the whole obstetric population (all primiparous and multiparous births, which will include women with previous OASI) (Hirayama 2012) and sometimes the rate is reported as a subset of the whole obstetric population, for example primiparous (Gurol‐Urganci 2013) or instrumental births only (de Leeuw 2007).
The incidence of OASI seems to be increasing (Gurol‐Urganci 2013; Laine 2009; McLeod 2003). Gurol‐Urganci 2013 reported that the OASI rate tripled in England between 2000 and 2012, (1.8% to 5.9%) and that improved recognition and standardised classification of perineal trauma and changes in second stage care practices such as the declining use of episiotomy, may be contributing to the increasing incidence.
The risk of recurrent OASI was found to be five‐fold higher than the risk for multiparous births with no history of OASI, the number of women included in this study were few and only two women (4.4% confidence interval (CI) 0.54 to 15.5) sustained a subsequent OASI (Harkin 2003). This finding however is supported by Edozien 2014 who reported a five‐fold increase in risk of recurrent OASI (adjusted odds ratio (OR) 5.5, 95% CI 5.2 to 5.9) using data from over 639,000 births. Dandolu 2005 examined 258,507 vaginal births and found that 18,888 (7.31%) women sustained a primary OAIS, 14,990 of these women went on to have a further vaginal birth and 864 (5.76%) sustained a recurrent OASI. Women with a primary fourth degree tear seemed at greater risk of OASI recurrence compared to women with a primary third degree tear (7.73% versus 4.69%) and overall, instrumental delivery accompanied by an episiotomy conveyed the greatest risk of OASI reoccurrence (17.7%). Episiotomy alone increased the risk of recurrent OASI by 50%. Jango 2012 reported a lower rate of primary OASI (7336/159,446, 4.6%) and higher rate of recurrent OASI (521/7336, 7.1%) compared to Dandolu 2005. Jango 2012 found increasing birth weight, ventouse (forceps was not performed in this population) and shoulder dystocia were associated with increased risk of a OASI but episiotomy use was not. The detrimental effect of episiotomy use in women with a previous OAS reported by Dandolu 2005 is opposite to the protective effect reported for episiotomy use during births of primiparous women or women without a history of OASI (de Leeuw 2007; Gurol‐Urganci 2013). The reasons for this difference are unclear, but may be due to increased risk of episiotomy extension from previous perineal scarring (Dandolu 2005).
Asian ethnicity seems to increase the risk of OASI, but this effect seems limited to South Asian women living outside Asia (Wheeler 2011). Increasing maternal age, primiparity, induction and augmentation of labour, length of second stage of labour (> two hours), forceps delivery, increased neonatal head circumference, occiput posterior position and birthweight greater than 4 kg are associated with an increased risk of primary and recurrent OASI (Dandolu 2005; Fizgerald 2007; Hirayama 2012; Kudish 2008; Payne 1999; Peleg 1999; Williams 2005).
Data regarding the incidence of primary and recurrent OASI and the influence of risk factors are limited and sometimes conflicting. The National Institute for Health and Care Excellence (NICE) intrapartum care guidance however, suggests the risk of recurrent severe trauma is similar to the risk of severe trauma at first vaginal birth, though this guidance is currently being updated (NICE 2007).
Adverse effects
OASI is associated with an increased risk of short‐ and long‐term morbidity which could seriously affect quality of life. Sequelae include: perineal pain (Macarthur 2004), dyspareunia (painful sexual intercourse) (Rathfisch 2010), defaecatory dysfunction, and urinary and faecal incontinence (Fenner 2003; MacArthur 1997; Richter 2006). Perineal pain is an immediate consequence that may adversely affect maternal and infant bonding, ability to breastfeed, increase the risk of urinary retention and dyspareunia (Barrett 2000; Buhling 2006), and could reduce well‐being and increase the risk of depression (Brown 2000).
Possibly the most distressing adverse effect of OASI is anal incontinence related to anal sphincter injury and pudendal nerve damage (Fynes 1998). Four per cent of women report faecal incontinence following vaginal birth (MacArthur 1997). The incidence of anal incontinence is related to the severity of the sphincter defect observed at follow‐up. For example, following clinically identified severe perineal trauma at the time of birth, 13% of women without identifiable sphincter defects on postnatal endo‐anal ultrasound (EAUS) reported anal incontinence, whereas 64% with internal and external defects on EAUS reported anal incontinence (Laine 2011). Incontinence rates may worsen with time and following subsequent births irrespective of degree of perineal trauma sustained (Baghestan 2012; Bek 1992). Various factors have been identified that may help determine the risk of anal incontinence following a subsequent birth; these include: age, parity, presence and severity of symptoms, EAUS‐identified injury and impaired sphincter function assessed by manometry.
Anal incontinence in the absence of identified OASI at the time of birth, may be in part due to pudendal nerve damage or unidentified anal sphincter damage. Sultan 1993 identified over 30% more anal sphincter injuries using EAUS compared with clinical examination alone. This difference may, however, be related to the experience of and/or technique used by the person undertaking the initial clinical examination rather than the superior or sensitivity of EAUS (Andrews 2006).
Identification of Injury
All women who have sustained perineal trauma should have a systematic examination of the vagina, perineum and rectum, including rectal examination before and after perineal repair by an experienced practitioner trained in the recognition and management of perineal tears (NICE 2007; RCOG 2007). Methods of OASI repair OASI have been examined in a separate Cochrane review (Fernando 2006). To our knowledge, there are no reviews examining suture materials for repair of OASI, the ideal clinician to perform the repair (obstetrician or colorectal surgeon), effectiveness of immediate versus delayed repair, prevention of OASI, or interventions for women in subsequent pregnancies following OASI to reduce the risk of recurrent injury and associated harms.
Description of the condition
NICE and the Royal College of Obstetricians and Gynaecologists guidelines (NICE 2007; RCOG 2007) recommend perineal or genital trauma caused by either tearing or episiotomy at birth should be defined as follows (described by Sultan 1999):
-
first degree – injury to skin only;
-
second degree – injury to the perineal muscles, but not the anal sphincter;
-
third degree – injury to the perineum involving the anal sphincter complex:
-
-
3a – less than 50% of external anal sphincter (EAS) thickness torn;
-
3b – more than 50% of EAS thickness torn;
-
3c – internal anal sphincter (IAS) torn;
-
-
fourth degree – injury to the perineum involving the anal sphincter complex (external and internal anal sphincter) and anal epithelium.
OASI includes third and fourth‐degree perineal tears (RCOG 2007).
Description of the intervention
Antenatal interventions for women who have sustained a previous obstetric anal sphincter injury include: pelvic floor exercises that aim to strengthen the pelvic floor and have recently been found to reduce the risk of urinary incontinence (Stafne 2012); biofeedback training which uses computer‐generated feedback from rectal balloons to (a) improve patient awareness of the presence of faecal material in the rectum and (b) to co‐ordinate contraction of the external anal sphincter with relaxation of the internal sphincter and (c) improve the force of the muscle (Miner 1990; Norton 2012); or stimulation of the sacral nerves that control the lower part of the bowel and sphincters by inserting electrodes in the lower back and connecting them to a pulse generator (Mowatt 2007). Other antenatal interventions include: perineal massage or creams that aim to reduce the risk of perineal tearing.
Intrapartum interventions include: induction of labour to reduce the risk of macrosomia (infant birth weight greater than 4 kg) and subsequent risk of trauma; elective caesarean section to avoid vaginal and perineal trauma; vacuum extraction rather than forceps to reduce the risk of vaginal and perineal trauma; selective episiotomy to reduce the risk of severe perineal trauma; and different flexion techniques of the presenting fetal part to reduce the diameter and in doing so, reduce the risk of subsequent trauma.
How the intervention might work
Interventions may aim to improve the integrity of the anal sphincter (pelvic floor muscle exercises, electrical stimulation), avoid trauma (elective caesarean section) or reduce the risk of trauma (medio‐lateral episiotomy, vacuum and flexion techniques) to the perineum and anal sphincter and in doing so reduce the risk of adverse effects such as incontinence.
Why it is important to do this review
There are currently no systematic reviews, evidence‐based guidance on interventions or strategies for women in subsequent pregnancies following obstetric anal sphincter injury to prevent or reduce the risk of further damage/trauma to the anal sphincter complex. Guidance based on robust evidence would improve the care in subsequent pregnancies for women who have previously sustained a third‐degree tear and in doing so reduce the risk of morbidity and improve health.
Objectives
The objective of this review was to assess the effects of antenatal and intrapartum interventions for women in subsequent pregnancies following a previous obstetric anal sphincter injury to reduce the risk of recurrent injury and associated harms.
Methods
Criteria for considering studies for this review
Types of studies
We planned to include abstracts, published and unpublished randomised controlled trials, cluster‐randomised trials and multi‐arm trials assessing the effects of any intervention in subsequent pregnancies following obstetric anal sphincter injury. Quasi‐randomised controlled trials and trials using a cross‐over design were not eligible for inclusion.
Types of participants
All pregnant women who sustained obstetric anal sphincter injury during a previous birth.
Types of interventions
Any type of intervention (irrespective of when the intervention is delivered i.e. antenatal or intrapartum) aimed at reducing the risk of harm in a subsequent pregnancy following obstetric anal sphincter injury compared with any other intervention or with routine care, i.e. antenatal interventions; such as massage or creams and intrapartum interventions such as vacuum versus selective or routine episiotomy and selective or routine episiotomy with routine care. Different types of the same category of intervention (antenatal or intrapartum) i.e. vacuum versus forceps and flexion of the presenting part versus hands poised or different types of creams.
Types of outcome measures
Primary outcomes
-
Incidence of recurrent third‐/fourth‐degree tear (as defined by authors of individual trials)
-
Anal incontinence (flatus, fluid and solid stool)
Secondary outcomes
Perinatal
-
Induction of labour
-
Instrumental vaginal birth (forceps and vacuum)
-
Caesarean birth
-
Perineal trauma (as defined by authors of individual trials)
-
Gestational age at birth
-
Birthweight
-
Admission to special care baby unit
-
Breastfeeding
-
Maternal well‐being and quality of life
Long term
-
Dyspareunia (as defined by authors of individual trials)
-
Perineal pain (as defined by authors of individual trials)
-
Resumption of sexual intercourse
-
Presence of symptoms of anal sphincter damage (as defined by authors of individual trials and including: flatal (accidental leakage of gas) and faecal incontinence, urgency, urinary incontinence)
-
Maternal well‐being and quality of life (at all time points reported)
Other outcome
1. Cost (as defined by authors of individual trials)
Search methods for identification of studies
The following methods section of this review was based on a standard template used by the Cochrane Pregnancy and Childbirth Group.
Electronic searches
We contacted the Trials Search Co‐ordinator to search the Cochrane Pregnancy and Childbirth Group’s Trials Register (30 September 2014).
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
-
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
-
weekly searches of MEDLINE;
-
weekly searches of Embase;
-
handsearches of 30 journals and the proceedings of major conferences;
-
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL, MEDLINE and Embase, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co‐ordinator searches the register for each review using the topic list rather than keywords.
We did not apply any language or date restrictions.
Data collection and analysis
No completed trials meeting our criteria for inclusion were identified. Methods of data collection and analysis to be used in future updates of this review are provided in Appendix 1.
Results
Description of studies
No completed trials that met the inclusion criteria of the review were identified. One ongoing trial was identified (NCT00632567) Figure 1; for more details, see Characteristics of ongoing studies.
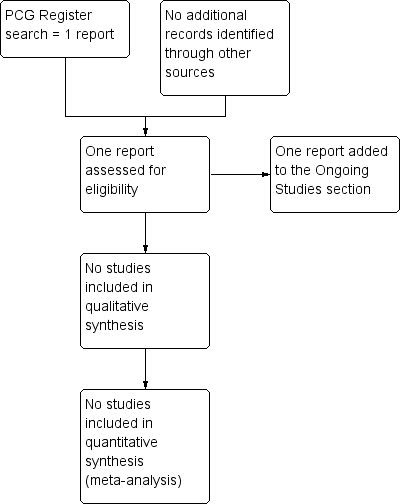
Study flow diagram.
Results of the search
The search retrieved one trial report of an ongoing study (Abramowitz 2008).
Included studies
No randomised trials were found for inclusion in the review.
Excluded studies
There are no excluded studies.
Risk of bias in included studies
Not applicable.
Effects of interventions
No randomised trials were found for inclusion in the review.
Discussion
We identified one ongoing trial (Abramowitz 2008) that will evaluate the relative effects of caesarean birth versus vaginal birth in women who have previously had an anal sphincter rupture diagnosed with anal endosonography.
Evidence on short‐ and long‐term sequelae following primary and secondary obstetric anal sphincter injury (OASI) are limited. However, health and well‐being seem to be severely adversely affected (Brown 2000; Rathfisch 2010; Richter 2006) and these effects may worsen as the woman ages (Fornell 2005). Consequently, interventions for women in subsequent pregnancies following OASI to limit or prevent further sphincter damage may convey substantial health benefits. To date there is no evidence from completed randomised trials, it is therefore important to undertake such trials to identify clinically and cost‐effective interventions for improving the health of these women.
Summary of main results
The effects of interventions for women in subsequent pregnancies following OASI for improving health is unknown.
Overall completeness and applicability of evidence
No randomised trials were found for inclusion in the review.
Quality of the evidence
No randomised trials were found for inclusion in the review.
Potential biases in the review process
No randomised trials were found for inclusion in the review.
Agreements and disagreements with other studies or reviews
No randomised trials were found for inclusion in the review.

Study flow diagram.

