Inhibidores de la aromatasa para pacientes con subfertilidad con síndrome de ovario poliquístico
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomised controlled trial Duration and location of the trial: quote: "The present study was conducted from July 15, 2007, to February 28, 2010, at the Women's Health Center, Assiut University, Assiut, Egypt, after approval was received from the Ethics Committee of Assiut University.“ | |
| Participants | Inclusion criteria: all participants met the Rotterdam consensus criteria for the diagnosis of PCOS. Other inclusion criteria included primary or secondary infertility because of anovulation for at least 1 year and clomiphene resistance. Clomiphene resistance was defined as lack of ovulation after 6 consecutive induction cycles with 50 mg of CC, then with 150 mg of CC each day for 5 days in each cycle. The male partner of each participant was required to have a normal result on semen analysis and each woman was required to have patent tubes on hysterosalpingography or on a diagnostic laparoscopy. Exclusion criteria: exclusion criteria included age below 20 years or above 35 years; hormonal treatment within 3 months prior to the study; hyperprolactinaemia (morning plasma prolactin concentration 30 ng/ml or more); any other endocrine, hepatic, or renal disorder; presence of an organic pelvic mass; and a history of abdominal surgery that might have caused pelvic factor infertility. Number of women randomised: 147, 74 in the letrozole group and 73 in the LOD group Number of women analysed: 70 in the letrozole group and 70 in the LOD group Number of withdrawals/exclusions/loss to follow‐up and reasons: 7 women were lost to follow‐up. Number of centres: 1, Women’s Health Center, Assiut University, Assiut Age (y): group A letrozole: 23.9 ± 3.2, group B LOD: 23.6 ± 3.2 BMI (kg/m²): group A letrozole: 27.3 ± 2.6, group B LOD: 27.1 ± 2.6 Duration of infertility (y): group A letrozole: 4.2 ± 1.7, group B LOD: 4.2 ± 1.7 Country: Egypt | |
| Interventions | Group A: letrozole, 5 mg/day given orally for 5 days during cycle days 3 ‐ 7 for up to 6 cycles Group B: LOD, triple‐puncture laparoscopy, monopolar diathermy, needle electrode set at 40 W pressed against border of ovary for 4 sec to achieve penetration depths of 7 ‐ 8 mm, punctured at 4 ‐ 6 points | |
| Outcomes | Primary outcomes: ovulation rate Secondary outcomes: endometrial thickness on the day of hCG injection, rates of clinical pregnancy, spontaneous abortion, live birth and multiple pregnancies | |
| Notes | Ethical approval: yes, the study was approved by Mansoura University Hospital Research Ethics Committee. Informed consent: yes, all participants gave informed consent before inclusion in the trial. Source of funding: not stated Conflicts of interest: quote:“Conflict of interest statement: We declare that we have no conflict of interest” Authors contacted about information on OHSS Power calculation: quote: "the sample size required to detect a 25% difference between the 2 groups with a power of 80% was estimated to be 68 patients per group." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was performed using a computer‐generated random numbers table. |
| Allocation concealment (selection bias) | Low risk | Allocation concealment was achieved using serially‐numbered opaque envelopes that were only opened once the interventions were assigned. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not mentioned |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) | Low risk | 7 women lost to follow‐up, but similar (3 vs 4) in both groups; losses due to noncompliance |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | None |
| Methods | Randomised controlled clinical trial Duration and location of the trial: quote: "The study comprised of 260 women with CC‐resistant PCOS among those attending the Outpatient Clinic in Mansoura University Hospitals, and a private practice setting in the period from August 2006 to March 2009.“ | |
| Participants | Inclusion criteria: infertile women with CC resistance and PCOS based on the Rotterdam criteria 2003. Patent fallopian tubes proved by hysterosalpingography and normal semen analysis for their partners according to the modified criteria of WHO. Exclusion criteria: other causes of infertility, age over 40 years, BMI > 35, contraindication to general anaesthetic, previous history of LOD and women who had received metformin, gonadotropin, oral contraceptives or other hormonal drugs during the preceding 6 months. Women who intended to start a diet or a specific programme of physical activity were also excluded. Number of centres: 2, outpatient clinic in Mansoura University hospitals and a private practice setting Number of women randomised: 260, 128 in the letrozole group and 132 in the LOD group Number of women analysed: 128 in the letrozole group and 132 in the LOD group Number of withdrawals/exclusions/loss to follow‐up and reasons: none Age (y): group A letrozole: 27.3 ± 2.6, group B LOD: 26.4 ± 2.4 BMI (kg/m²): group A letrozole: 26.4 ± 3.3, group B LOD: 26.6 ± 3.6 Duration of infertility (y): group A letrozole: 4.3 ± 1.11, group B LOD: 4.5 ± 1.24 Country: Egypt | |
| Interventions | Group A: letrozole, 2.5 mg/day orally given for 5 days starting from day 3 of the cycle Group B: LOD, laparoscopy was performed using 3‐puncture technique. Each ovary was cauterised at 4 points, each for 4 s at 40 W for a depth of 4 mm with a mixed current, using a monopolar electrosurgical needle. | |
| Outcomes | Primary outcome: ovulation rate Secondary outcomes: midcycle endometrial thickness (mm), biochemical pregnancy/cycle, clinical pregnancy/participant, biochemical miscarriage/cycle, clinical miscarriage/participant and live birth rates | |
| Notes | Ethical approval: yes, the study was approved by Mansoura University Hospital Research Ethics Committee. Informed consent: yes, all participants gave informed consent before inclusion in the trial. Source of funding: not stated Conflicts of interest: quote:“Conflict of interest statement: We declare that we have no conflict of interest” Power calculation: quote: "Sample size was calculated based on the fact that with an expected rate of ovulation of 70% in the LOD group we needed 244 women to show an absolute increase of 15% in ovulation rate in the letrozole group, with a power of 80% at confidence interval of 95% using a two tailed chi‐square test with a 5% significance level (type alfa error)." We had contact with Prof. Abu Hashim, and all questions were answered in detail. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women were randomised according to a computer‐generated random‐numeric table prepared by an independent statistician. |
| Allocation concealment (selection bias) | Low risk | Concealment of treatment allocation was done by using sealed opaque envelopes that were given to a third party (nurse) who assigned participants to study arms. |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "Once allocated, the treatment was revealed to both the investigator and the patient." |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "Once allocated, the treatment was revealed to both the investigator and the patient." |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts reported |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | None |
| Methods | Randomised controlled clinical trial Duration and location of the trial: quote: "The study comprised of 260 women with CC‐resistant PCOS among those attending the Outpatient Clinic in Mansoura University Hospitals, and a private practice setting in the period from August 2006 to March 2009.“ | |
| Participants | Inclusion criteria: infertile women with PCOS based on the Rotterdam 2003 criteria. Additionally, diagnosed as CC‐resistant, patent fallopian tubes proved by hysterosalpingography and normal semen analysis for their partners according to the modified criteria of WHO 1999 Exclusion criteria: none stated Number of centres: 2, Outpatient clinic in Mansoura University hospitals and a private practice setting Number of women randomised: 250, 123 in the letrozole group and 127 in the CC + metformin (met) group Number of women analysed: 123 in the letrozole group and 127 in the CC + met group Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 Age (y): group A letrozole: 28.3 ± 2.7, group B CC + met: 26.2 ± 2.2 BMI (kg/m²): group A letrozole: 29.1 ± 3.2, group B CC + met: 30.1 ± 2.3 Duration of infertility (y): not stated Country: Egypt | |
| Interventions | Group A: letrozole 2.5 mg/day for 5 days from cycle days 3 to 7 Group B: metformin HCl, 500 mg thrice daily for 6 ‐ 8 weeks, followed by 150 mg of CC orally given for 5 days starting on day 3 of menstruation Participants continued treatment for 3 successive cycles using the same protocol. | |
| Outcomes | Primary outcomes: ovulation rate, number of growing and mature follicles, serum oestrogen, serum progesterone and endometrial thickness Secondary outcomes: pregnancy and miscarriage rates, multiple pregnancies and cases of OHSS | |
| Notes | Ethical approval: yes, the study was approved by the local research ethics committee. Informed consent: yes, all participants gave informed consent before inclusion in the trial. Source of funding: not stated Conflicts of interest: quote: "All authors have nothing to disclose" Power calculation: quote: "the sample size was based on the fact that for an expected rate of ovulation of 70% in the combined metformin‐CC group we needed 244 women to show an absolute increase of 15% in ovulation rate in the letrozole group, with a power of 80% at confidence interval of 95% using a two‐tailed x² test with a 5% significance level." We had contact with Prof. Abu Hashim, and all questions were answered in detail. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random table |
| Allocation concealment (selection bias) | Low risk | Quote: "Dark, sealed envelopes containing the intervention and taken from a computer‐generated random numeric table were prepared by a third party (independent statistician) not involved in the allocation process." |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "patients were not blinded because of the difference in shape, colour and size of letrozole, CC and metformin tablets" (Email with Prof. Abu Hashim) |
| Blinding of outcome assessment (detection bias) | High risk | It is not plausible that outcome assessors were blinded if participants were not. |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts reported |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | None |
| Methods | Randomised double blind clinical trial Duration and location of the trial: not stated | |
| Participants | Inclusion criteria: non‐fertile clomiphene‐resistant women with PCOS Exclusion criteria: tubal, peritoneal and uterine causes of infertility were excluded by laparoscopic hysterosalpingogram or by ultrasonography. Specific endocrine abnormalities and male‐factor causes for infertility were also excluded. Participants had to end clomiphene treatment at least 2 months before enrolment. Number of centres: quote: "The study was done in the Baghdad teaching hospital/ Medical city which is a tertiary ref. hospital affiliated with Baghdad Med college/ University of Baghdad." (Email) Number of women randomised: 22 in the letrozole group and 18 in the anastrozole group Number of women analysed: 22 in the letrozole group and 18 in the anastrozole group Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 Age (y): group A letrozole: 28.4 ± 5.18, group B anastrozole: 25.56 ± 6.26 BMI (kg/m²): group A letrozole: 29.95 ± 3.73, group B anastrozole: 27.90 ± 5.29 Duration of infertility (y): group A letrozole: 3.95 ± 2.70, group B anastrozole: 4.50 ± 3.61 Country: Iraq | |
| Interventions | Group A: letrozole 2.5 mg/day orally given for 5 days during cycle days 3 ‐ 7 Group B: anastrozole 1 mg/day orally given for 5 days during cycle days 3 ‐ 7 Treatment was continued for 3 months. When ovulation or pregnancy did not occur, the same treatment protocol was used with the doubling of the first dose for a maximum of 2 treatment cycles. | |
| Outcomes | Primary outcomes: ovulation rate/cycle, endometrial thickness (mm) measured on day of hCG administration Secondary outcomes: multiple pregnancy rate, pregnancy rate/cycle, E2 (pmol/l), progesterone (nmol/l), LH (U/l), number and size of follicles, pulsatility index, day of hCG administration | |
| Notes | Ethical approval: quote: "Ethical approval was obtained from the Iraqi Board for medical specialization/ Scientific committee" (email contact) Informed consent: quote: "written consent was obtained from all patients" (email contact) Source of funding: quote: "The study was partially funded by the Iraqi Board for medical specialization as well as the Drug Scientific Office of the Iraqi Ministry of Health." Power calculation: not reported We had email contact with Dr. Al‐Omari, but there was no further information available about the outcomes. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Actually, we just put all envelopes in a box, mixing them then the patient herself selected one." (email with Dr. Al‐Omari) |
| Allocation concealment (selection bias) | Unclear risk | Quote: "My associate informed me that for randomisation we distributed blank envelops containing the medications at our Gyn.clinic on twice weekly basis." (email with Dr. Al‐Omari) |
| Blinding of participants and personnel (performance bias) | High risk | Participants were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | It is not plausible that outcome assessors were blinded if participants were not |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts reported |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | None |
| Methods | Randomised double‐blind controlled clinical trial Duration and location of the trial: quote: "This study was conducted at the Fertility Unit, Derby Teaching Hospitals NHS Foundation Trust between April 2007 and June 2014.“ | |
| Participants | Inclusion criteria: quote: "eligible participants were women aged 18 – 39 years with BMI ≤ 35 kg/m2, anovulatory infertility, and a diagnosis of PCOS based on Rotterdam consensus (two of three criteria: oligo‐/anovulation, hyperandrogaenemia and sonographic appearance of polycystic ovaries) (Rotterdam ESHRE/ASRM‐sponsored PCOS consensus workshop group, 2004). Diagnosis of oligo‐/anovulation was based on a menstrual pattern of oligo‐/amenorrhoea (cycle > 35 days) and/or a low mid‐luteal serum progesterone concentration. Hyperandrogenaemia was diagnosed either clinically (acne/hirsutism) or biochemically (testosterone ≥ 2.5 nmol/l or free androgen index [FAI] ≥ 5). Ultrasound criteria included ≥ 12 follicles (2 – 9 mm) and/or an ovarian volume of > 10 ml (Jonard et al., 2003). All participants had proven patency of at least one fallopian tube and normal semen analysis of their male partners (WHO, 1999)." Exclusion criteria: quote: "We excluded patients who have received OI within 6 months and those with uncontrolled thyroid disease or hyperprolactinaemia. Patients with marked hyperandrogaenemia were screened for adult onset congenital adrenal hyperplasia (by measuring serum 17‐ α ‐hydroxyl‐progesterone concentration) and Cushing syndrome (by measuring urinary free cortisol)." Number of women randomised: 159 women were randomised in total; 79 to CC, 80 to letrozole Number of women analysed: all women randomised were also analysed in the ITT analysis. Number of withdrawals/exclusions/loss to follow‐up and reasons: 3 women in the CC group discontinued treatment due to failing to attend; also 3 women discontinued treatment in the letrozole arm (1 due to social reasons, 1 failed to attend, 1 withdrew consent). Number of centres: this was a single centre, 2‐arm double‐blind RCT. Age (y): letrozole: 28.3 (4.4) vs CC: 28.1 (4.2) BMI (kg/m²): letrozole: 27.5 (23.4 ‐ 32.2) vs CC: 27.7 (23.0 ‐ 31.0) Duration of infertility (y): 1.5 (1.0 ‐ 2.0) for both groups Country: United Kingdom | |
| Interventions | Group A: letrozole was prescribed (by the senior investigator, SA) orally daily for 5 days starting on Days 2 – 4 of a menstrual period or a progestogen‐induced bleed (medroxy‐progesterone acetate 10 mg twice daily for 5 days). The starting dose was 1 tablet/day (letrozole 2.5 mg) and if ovulation was not achieved, the dose would be doubled in the second cycle. Group B: CC was prescribed daily for 5 days starting on days 2 – 4 of a menstrual period or a progestogen‐induced bleed (medroxy‐progesterone acetate 10mg twice daily for 5 days). The starting dose was 1 tablet/day (50 mg) and if ovulation was not achieved, the dose would be doubled in the second cycle. Participants who failed to ovulate on the maximum dose (2 tablets) or to conceive after 6 ovulatory cycles were crossed over to the other drug (after a 6‐week wash‐out period) following the same procedures as with the first drug. | |
| Outcomes | Primary outcomes: clinical pregnancy (diagnosed by ultrasonographic visualisation of a gestational sac) rate per participant on primary treatment (before the cross‐over). Secondary outcomes: secondary outcomes included ovulation, live birth, pregnancy by ovulating participant, pregnancy by strata, mono‐ovulation, endometrial development (thickness and grades), pregnancy outcome and pregnancy complications. Other outcomes included pregnancy and live birth rates on secondary and overall (primary and secondary) treatments. | |
| Notes | Ethical approval: the trial was approved by West Midlands Research Ethics Committee (Reference: 07/MRE07/5) and by the Medicines and Healthcare Products Regulatory Agency (MHRA). Informed consent: all participants gave written informed consent and the trial was monitored by the sponsor. Source of funding: it was sponsored by the University of Nottingham. Power calculation: quote: "to detect a clinically significant difference of 20% between the previously reported pregnancy rate of CC (˜35%) and letrozole with a two‐sided 5% significance level and power of 80%, a sample size of 212 participants (106 per arm) was required (Dickey and Holtkamp, 1996;Kousta et al., 1997; Imani et al., 2002)." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "An independent pharmacist randomly allocated participants to letrozole or CC, in 1:1 ratio according to a randomisation list created by the trial statistician using NQuery Advisor v6.0 software. Randomization was stratified by patients’ BMI (non‐obese < 30 kg/m2 and obese 30 – 35 kg/m2) using mixed block sizes." |
| Allocation concealment (selection bias) | Low risk | Quote: "An independent pharmacist randomly allocated participants to letrozole or CC, in 1:1 ratio." |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "Investigators, patients, outcome assessors and the statistician were blinded to the allocation of participants." |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Investigators, patients, outcome assessors and the statistician were blinded to the allocation of participants." |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "Intention‐to‐treat (ITT) analysis included all randomised subjects, regardless of whether or not they received the study drug. Per protocol (PP) analysis included all randomised subjects who received the study drug and were not lost to follow‐up. Participants who were lost to follow‐up were assumed neither to be pregnant nor to have given LB in the ITT analysis." |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | None |
| Methods | Randomised controlled clinical trial Duration and location of the trial: not stated | |
| Participants | Inclusion criteria: women with primary infertility and PCOS with no other known cause of infertility were enrolled into the study. All participants had a history of oligo‐ or amenorrhoea and ovaries with at least 10 subcapsular cysts 2 ‐ 10 mm in diameter and hyperechogenic stroma. Exclusion criteria: none declared Number of centres: setting unknown, tried to contact authors via email Number of women randomised: 51 in the letrozole group and 55 in the CC group Number of women analysed: 51 in the letrozole group and 55 in the CC group Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 Age (y): group A letrozole: 27.1 ± 0.9, group B CC: 26.2 ± 1.1 BMI (kg/m²): group A letrozole: 26.1 ± 1.9, group B CC: 25.8 ± 1.8 Duration of infertility (y): group A letrozole: 2.2 ± 0.7, group B CC: 2.4 ± 0.9 Country: Turkey | |
| Interventions | Group A: letrozole, 2.5 mg/day orally given for 5 days starting on cycle day 3 Group B: clomiphene citrate, 100 mg/day orally given for 5 days starting on cycle day 3 | |
| Outcomes | Outcomes: number of mature follicles, endometrial thickness (mm), day of hCG administration, ovulation rate, pregnancy rate, multiple pregnancies | |
| Notes | Ethical approval: yes, the study protocol was approved by the institutional ethics committee Informed consent: yes, informed consent was obtained from all study participants Source of funding: not stated Conflicts of interest: quote:“Conflicts of interest: No conflicts of interest were declared in relation to this article” Power calculation: not stated We contacted Dr. V Atay via email about the study setting, about how randomisation and allocation were done, blinding and if data are available on OHSS, miscarriage rate and live birth rate, but no response. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear how it was done |
| Allocation concealment (selection bias) | Unclear risk | Unclear how it was done |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts reported |
| Selective reporting (reporting bias) | Unclear risk | Protocol of the study was not available |
| Other bias | Low risk | None |
| Methods | Randomised controlled trial Duration and location of the trial: quote: "The study comprised of 220 women (574 cycles) with CCresistant PCOS among those attending the Fertility Outpatient Clinic in Mansoura University Hospitals, Mansoura University, Egypt, and a private practice setting in the period from May 2005 to January 2007.“ | |
| Participants | Inclusion criteria: diagnosis of PCOS based on the revised 2003 consensus on diagnostic criteria and long‐term health risks related to PCOS. All women were previously treated with 100 mg of CC daily for 5 days each cycle, for 2 ‐ 3 cycles with persistent anovulation or ovulate with very thin endometrium < 5 mm at the time of hCG administration. They had patent fallopian tubes proved by hysterosalpingography and normal semen analysis for their partners according to the modified criteria of WHO. Exclusion criteria: no exclusion criteria stated Number of centres: 2, outpatient clinic in Mansoura University Hospitals and a private practice setting Number of women randomised: 111 in the letrozole group and 109 in the anastrozole group Number of women analysed: 111 in the letrozole group and 109 in the anastrozole group Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 Age (y): group A letrozole: 28.2 ± 2.8, group B anastrozole: 26.3 ± 2.5 BMI (kg/m²): group A letrozole: 29.1 ± 3.1, group B anastrozole: 30.1 ± 2.1 Duration of infertility (y): not stated Country: Egypt | |
| Interventions | Group A: letrozole 2.5 mg/day orally given for 5 days during cycle days 3 ‐ 7 Group B: anastrozole 1 mg/day orally given for 5 days during cycle days 3 ‐ 7 Treatment was continued for 3 months. | |
| Outcomes | Primary Outcomes: number of growing and mature follicles, serum E2 (pg/ml), serum progesterone (ng/mL), and endometrial thickness (mm). Secondary Outcomes: pregnancy rate, miscarriage rate, multiple pregnancy rate, ovarian hyperstimulation syndrome rate | |
| Notes | Ethical approval: yes, the study was approved by the hospital ethics research committee. Informed consent: yes, all participants gave informed consent before inclusion in the trial Source of funding: not stated Power calculation: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly allocated using a computer‐generated random table into 2 treatment groups |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts reported |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | None |
| Methods | Randomised controlled study Duration and location of the trial: quote: "The study comprised 438 women (1063 cycles) with PCOS among those attending the Fertility Outpatient Clinic in Mansoura University Hospitals, Mansoura University, Egypt, and private practices in the period from January 2004 and September 2006.“ | |
| Participants | Inclusion criteria: infertile women with clomiphene‐resistant PCOS, diagnosis of PCOS based on the 2003 Rotterdam criteria. Normal serum PRl, TSH and 17OH‐P. Exclusion criteria: infertility caused by fallopian tube problems, infertility problems caused by male partner Number of centres: 2, outpatient clinic in Mansoura University Hospitals and a private practice setting Number of women randomised: 110 in the short letrozole group and 108 in the long letrozole group Number of women analysed: 110 in the short letrozole group and 108 in the long letrozole group Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 Age (y): group A short letrozole: 25.1 ± 3.2, group B long letrozole: 25.3 ± 3.0 BMI (kg/m²): group A short letrozole: 33.9 ± 3.1, group B long letrozole: 34.2 ± 2.6 Duration of infertility (y): not stated Country: Egypt | |
| Interventions | Group A: letrozole orally given, 5 mg/day for 5 days, from cycle days 3 ‐ 7 Group B: letrozole orally given, 2.5 mg/day for 10 days, from cycle days 3 ‐ 12 | |
| Outcomes | Primary Outcomes: number of growing and mature follicles, serum E2 (pg/mL), serum progesterone (ng/mL), and endometrial thickness (mm) Secondary Outcomes: pregnancy rate, miscarriage rate, multiple pregnancies, OHSS | |
| Notes | Ethical approval: yes, the study was approved by the hospital ethics research committee. Informed consent: yes, all participants gave informed consent before inclusion in the trial Source of funding: not stated Conflicts of interest: quote:"All authors have nothing to disclose" Power calculation: quote: "Sample size calculation, using StatCalc 3.02 computer package 8Acastat software, Leesburg, VA), showed that each arm should contain at least 103 patients to have 80% power of the study at 95% confidence interval (CI)." We contacted the authors, but information on live birth was not collected. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomly allocated into two treatment groups using a computer‐generated random table: short letrozole group and long letrozole group." |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts reported |
| Selective reporting (reporting bias) | Low risk | All stated outcomes were reported |
| Other bias | Low risk | None |
| Methods | Prospective randomised trial Duration and location of the trial: quote: "The study comprised 218 women (444 cycles) with clomiphene‐resistant PCOS among those attending the gynecology outpatient clinic in Mansoura University Hospitals, Egypt, and a private practice setting in the period from December 2005 to December 2007.“ | |
| Participants | Inclusion criteria: diagnosis of PCOS based on the 2003 Rotterdam criteria. All women had patent fallopian tubes proved by hysterosalpingography and their partners had normal semen analysis parameters according to the modified criteria of the WHO. All participants had normal serum prolactin, TSH and 17‐OH progesterone. Exclusion criteria: not stated Number of centres: multiple, University teaching hospital and private practices Number of women randomised: 218 in the letrozole group and 220 in the CC group Number of women analysed: 218 in the letrozole group and 220 in the CC group Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 Age (y): group A letrozole: 27.1 ± 3.2, Group B clomiphene citrate: 29.3 ± 2.9 BMI (kg/m²): group A letrozole: 28.1 ± 3.2, group B CC: 27.1 ± 3.1 Duration of infertility (y): not reported Country: Egypt | |
| Interventions | Group A: letrozole orally given 5 mg/day for 5 days from cycle days 3 ‐ 7 Group B: clomiphene citrate orally given 100 mg/day for 5 days from cycle days 3 ‐ 7 | |
| Outcomes | Primary Outcomes: number of growing and mature follicles, the concentrations of serum E2 (pg/mL) and progesterone (ng/mL), and the endometrial thickness (mm) Secondary Outcomes: ovulation rate, ovarian hyperstimulation rate, pregnancy rate, miscarriage rate, multiple pregnancy rate | |
| Notes | Ethical approval: yes, the study was approved by the hospital research ethics committee. Informed consent: yes, all participants gave informed consent before inclusion in the trial Source of funding: the study was self‐funded Power calculation: not stated Authors were contacted via email and gave all information, but they did not measure the live birth. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly allocated using a computer‐generated random table into 2 groups |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation concealment was done by sequentially numbered opaque sealed envelopes opened by the chief nurse" (by email contact with authors) |
| Blinding of participants and personnel (performance bias) | High risk | Not blinded, email with Prof. Badawy |
| Blinding of outcome assessment (detection bias) | High risk | It is not plausible that outcome assessors were blinded if participants were not |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts reported |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported, Live birth was not measured |
| Other bias | Low risk | None |
| Methods | Randomised controlled study Duration and location of the trial: quote: "During the study period of 2004 through 2005, 80 patients with PCOS who attended the outpatient clinics of the Infertility and Reproductive Medicine Unit of the Zonguldak Karaelmas University Hospital (Zonguldak, Turkey) participated in this study.“ | |
| Participants | Inclusion criteria: women with anovulatory PCOS diagnosed by using 2003 Rotterdam criteria Exclusion criteria: tubal, peritoneal and uterine cause of infertility. Male‐factor infertility. Specific endocrine abnormalities (Cushings disease/syndrome, hypothyroidism, hyperthyroidism, prolactinoma) Number of centres: 1, outpatient clinics of the Infertility and Reproductive Medicine Unit of the Zonguldak Karaelmas University Hospital (Zonguldak, Turkey) Number of women randomised: 80, 40 in group A letrozole and 40 in group B CC Number of women analysed: 38 in group A letrozole and 36 in group B CC Number of withdrawals/exclusions/loss to follow‐up and reasons: 6 lost to follow‐up, no reasons given Age (y): group A letrozole: 32.2 ± 3.9, group B CC: 30.6 ± 4.0 BMI (kg/m²): not stated Duration of infertility (y): group A letrozole: 5 (1 ‐ 10), group B CC: 3 (3 ‐ 11) Country: Turkey | |
| Interventions | Group A: letrozole, 5 mg/day orally given for 5 days during cycle days 3 ‐ 7 Group B: clomiphene citrate, 100 mg/day orally given for 5 days during cycle days 3 ‐ 7 | |
| Outcomes | Outcomes: ovulation rate by cycle, pregnancy rate by cycle, delivery rate by cycle, miscarriage rate, multiple pregnancy rate, endometrial thickness on the day of hCG (mm), N of follicles sized > 15 mm in diameter on the day of hCG, E2 level on the day of hCG (pg/mL), E2 per follicle sized > 15 mm in diameter on the day of hCG (pg/mL) | |
| Notes | Ethical approval: yes, the study was approved by the institutional ethics committee of Karelmal university. Informed consent: not stated Source of funding: no funding source or conflicts of interest stated Power calculation: Sample‐size determination was based on the difference between the median number of follicles sized > 15 mm and E2 concentration on hCG day. A sample size of 60 participants (30 in each group) was targeted to be able to detect a difference of at least one follicle or of 200 pmol/L between the 2 groups, with alfa (type I error) set at 0.05 and 80% power. We contacted Dr. Bayar by email for additional information, but he did not respond. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple randomisation performed by a computer |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was achieved by using central consultation for treatment of eligible participants. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Stated as double‐blind but it is not clear who was actually blinded and how this was achieved |
| Blinding of outcome assessment (detection bias) | Unclear risk | Stated as double‐blind but it is not clear who was actually blinded and how this was achieved |
| Incomplete outcome data (attrition bias) | Low risk | 6 participants lost to follow‐up, 4 and 2 respectively |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | None |
| Methods | Randomised non‐blinded controlled trial Duration and location of the trial: quote: "The study was conducted in a private infertility care setting as a randomized controlled trial between August 2004 and December 2005.“ | |
| Participants | Inclusion criteria: infertile women with PCOS diagnosed by the Rotterdam criteria 2003 who failed to ovulate by taking 100 mg of CC/day for 5 days in 2 consecutive cycles Exclusion criteria: women with hyperprolactinaemia, thyroid disorder, male‐factor infertility, known or suspicious tubal factor infertility (endometriosis and pelvic inflammatory disease), and unexplained infertility were excluded from the study. Number of centres: 1, private infertility care setting Number of women randomised: 32 in each group Number of women analysed: 32 in each group Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 Age (y): group A letrozole: 25.5 ± 4.0, group B clomiphene citrate: 26.1 ± 3.6 BMI (kg/m²): group A letrozole: 22.7 ± 2.8, group B clomiphene citrate: 23.6 ± 3.2 Duration of infertility (y): group A letrozole: 2.7 ± 1.1, group B clomiphene citrate: 2.6 ± 1.1 Country: India | |
| Interventions | Group A: letrozole, 7.5 mg/day orally given for 5 days from cycle days 3 ‐ 7 Group B: clomiphene citrate, 150 mg/day orally given for 5 days from cycle days 3 ‐ 7 | |
| Outcomes | Primary Outcomes: ovulation and pregnancy rate Secondary Outcomes: follicular development by day 16 (mm), serum E2 on day of hCG (pg/mL), endometrial development by day 16 (mm), serum progesterone on day 21 (ng/mL), multiple pregnancies, OHSS cases. Live birth rate was provided by email contact. | |
| Notes | Ethical approval: yes, the study protocol was approved by the institutional review board (IRB) of Dhaka medical college. Informed consent: yes, participants were counselled and informed consent was obtained before recruitment. Source of funding: the study was self‐funded. Power calculation: a study population of 57 women was calculated, considering an average of 60% of PCOS women are associated with insulin resistance, allowing an alfa value of 0.05. Authors were contacted by email, and additional information was provided. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done by lottery method. They put the name of letrozole and CC in a sealed opaque envelope. By calculating sample size they made 64 pieces of paper, 32 for letrozole and 32 for CC. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "All unleveled envelop were put together and the patients drew one piece of envelop from them. Then we opened the envelop to see the name of the drug." (by email contact with Prof. Rashida) |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "There was no blinding" (by email contact with Prof. Rashida) |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "There was no blinding" (email with Prof. Rashida) |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | None |
| Methods | Randomised controlled study Duration and location of the trial: quote: "All patients were admitted in our hospital between January 2013 and January 2015, who were not pregnant without contraception for over one year.“ | |
| Participants | Inclusion criteria: quote: "all the cases were PCOS infertility patients in line with the PCOS diagnostic criteria of the 2003 Rotterdam Conference, i.e. at least two of the following three were met: 1) ovulation abnormality (sporadic ovulation or no ovulation) occurred after continuous monitoring for two or more natural cycles; 2) the results of B ultrasound showed polycystic ovary; 3) patients had hyperandrogenism or showed clinical manifestations of androgen excess. Through salpingography or hydrotubation under transvaginal B ultrasound and other examinations, all cases were confirmed to have tubal patency on at least one side. The semen of male was normal." Exclusion criteria: quote:"Those with androgen excess caused by other diseases such as adrenal hyperplasia Cushing’s syndrome and androgen‐secreting tumours were excluded. Exclusion criteria: 1) Infertility patients caused by non‐PCOS ovulatory disorder or other factors; 2) patients with history of ovarian surgery or complication with endometriosis or pelvic adhesion; 3) patients complicated with liver, kidney or thyroid dysfunction; 4) patients who did not receive treatment after enrolment according to the established regimen or gave up in the midst of treatment." Number of women randomised: 156 patients, 52 in each group Number of women analysed: 156 patients, 52 in each group Number of withdrawals/exclusions/loss to follow‐up and reasons: none reported Number of centres: single‐centre trial Age (y): letrozole group 26.4 ± 4.2; CC group 27.1 ± 4.7; letrozole + HMG group 27.7 ± 5.2 years BMI (kg/m²): letrozole group 22.4 ± 4.5; CC group 23.4 ± 1.5; letrozole + HMG group 22.6 ± 2.6 years Duration of infertility (y): letrozole group 3.4 ± 1.1; CC group 3.2 ± 0.7; letrozole + HMG group 3.3 ± 1.3 years Country: China | |
| Interventions | Group A (letrozole): the participants orally took 2.5 ‐ 5.0 mg/d‐1 LE (trade name: Fu Rui, Jiangsu Hengrui Medicine Co., Ltd.) on the 3rd ‐ 5th days of menstrual cycle for 5 consecutive days. Group B (CC group): the participants were orally administered with 50 ‐ 100 mg/d‐1 CC (trade name: Fertilan, Codal Synto Pharmaceutical Co., Ltd.) on the 3rd ‐ 5th days of menstrual cycle for 5 consecutive days. Group C (letrozole + HMG group): the participants orally took 2.5 ‐ 5.0 mg/d‐1 LE on the 3rd ‐ 5th days of menstrual cycle for 5 consecutive days. Starting from the day of oral administration of CC, 75 IU HMG (trade name: Lebaode, Livzon Group Livzon Pharmaceutical Co. Ltd.) was intramuscularly injected every other day for 5 consecutive days. | |
| Outcomes | Primary outcomes: clinical pregnancy, defined as a fetal heart beat visible via transvaginal ultrasound on 30th day after ovulation Secondary outcomes: OHSS, miscarriage, multiple pregnancy | |
| Notes | Ethical approval: this study has been approved by the ethics committee of our hospital. Informed consent: written consent has been obtained from all patients. Source of funding: quote: “None” Power calculation: no power calculation was reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “ the patients were randomly divided into an LE group, a CC group and an LE + HMG group” |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | All participants randomised were also analysed. |
| Selective reporting (reporting bias) | Low risk | No study protocol was found, but all outcomes reported were also analysed. |
| Other bias | Low risk | None |
| Methods | Single‐blind randomised clinical trial Duration and location of the trial: quote: "In this single blind randomized trial, 148 ovarian cycles were studied in 100 clomiphene‐ resistance patients with PCOS who were chosen among 250 PCOS patients attending the Research and Clinical Center for Infertility, Shahid Sadoughi University of Medical Sciences, Yazd, Iran during the years 2007‐2008.“ | |
| Participants | Inclusion criteria: women who received 150 mg CC daily for 3 cycles and failed to become pregnant, and were diagnosed with anovulatory PCOS based on Rotterdam 2003. Exclusion criteria: quote: “We excluded patients with liver and kidney dysfunction, cardiovascular disease, diabetics, and those who use metformin or drugs affecting insulin secretion and clomiphene citrate in recent 2 cycles.” Number of centres: 1, research and clinical centre for infertility, Shahid Sadoughi University of Medical Sciences, Yazd Number of women randomised: 100 women, 50 in group A met‐letrozole, 50 in group B met‐CC Number of women analysed: 48 in group A met‐letrozole, 50 in group B met‐CC Number of withdrawals/exclusions/loss to follow‐up and reasons: 2, experienced side effects with metformin before letrozole was started Age (y): group A metformin‐letrozole: 28.5 ± 3.1, group B metformin‐clomiphene citrate: 29.6 ± 3.5 BMI (kg/m²): group A met‐letrozole: 29.0 ± 3.8, group B met‐CC: 29.2 ± 2.9 Duration of infertility (y): group A met‐letrozole: 3.8, group B met‐CC: 3.8 Country: Iran | |
| Interventions | Group A: metformin 1500 mg daily for 6 ‐ 8 weeks, followed by 5 mg letrozole daily orally given for 5 days during cycle days 3 ‐ 7 if pregnancy did not occur Group B: metformin 1500 mg daily for 6 ‐ 8 weeks, followed by 100 mg CC daily orally given for 5 days during cycle days 3 ‐ 7 if pregnancy did not occur | |
| Outcomes | E2 (pg/mL) on day of hCG administration, number of follicles > 18 mm in diameter, endometrial thickness on day of hCG administration (mm), clinical pregnancy rate, miscarriage rate | |
| Notes | SEthical approval: yes, the study was approved by ethical board of Shahid Sagoughi University of Medical Sciences, Yazd. Informed consent: no, at least nothing written about it – authors contacted Source of funding: quote: “the study was fully supported and funded by Shahid Sadoughi University of Medical Sciences, Yazd, Iran” Power calculation: quote: "In this study, 50 cases were needed in each group so as to gain a significant difference of 22% in pregnancy rate at a significant level of 5% and a power of 80%" We contacted Dr Davar by email to get additional information, but we did not get a response. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done using a random‐numbers table |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated who was blinded in this single‐blinded trial |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated who was blinded in this single‐blinded trial |
| Incomplete outcome data (attrition bias) | Low risk | 2 participants lost to follow‐up due to side effects experienced with metformin before letrozole was started. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported stated in the protocol |
| Other bias | Low risk | None |
| Methods | Double‐blind randomised study Duration and location of the trial: quote: "During the period of February 2004 through November 2006, 100 patients with PCOS who attended the outpatient infertility clinics at Shiraz University of Medical Sciences participated in the present study.“ | |
| Participants | Inclusion criteria: infertility for at least 1 year, diagnosis of PCOS by the Rotterdam criteria 2003, having patent tubes on hysterosalpingogram, and normal semen analysis of the husband Exclusion criteria: participants must not have received any other medication for ovulation induction before enrolment into the study. Number of centres: 1, outpatient infertility clinics at Shiraz University of Medical Sciences Number of women randomised: 100 women, 50 in each group Number of women analysed: 100 women, 50 in each group Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 Age (y): group A letrozole: 23.6 ± 2.9, group B CC: 24.3 ± 3.4 BMI (kg/m²): group A letrozole: 27.5 ± 4.6, group B CC: 27.1 ± 3.6 Duration of infertility (y): group A letrozole: 2.0 ± 1.3, group B CC: 2.3 ± 1.9 Country: Iran | |
| Interventions | Group A: letrozole, 5 mg/day orally given for 5 days during cycle days 3 ‐ 7 Group B: clomiphene citrate, 100 mg/day orally given for 5 days during cycle days 3 ‐ 7 | |
| Outcomes | Total number of follicles with diameter ≥ 14 mm, endometrial thickness on the day of hCG injection, pregnancy rate, miscarriage rate, multiple pregnancy rate, live birth rate | |
| Notes | Ethical approval: yes, quote: “The study was approved by the Institutional Ethics Committee of the University.” Informed consent: yes, quote: “An informed written consent was obtained from each patient” Source of funding: not stated Conflicts of interest: quote: "Conflicts of interest: None declared" Power calculation: not stated Authors contacted about randomisation, allocation, and information about OHSS | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated how it was done |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Low risk | Only the pharmacist knew the name of the medication that had been taken by the participants. |
| Blinding of outcome assessment (detection bias) | Low risk | Only the pharmacist knew the name of the medication that had been taken by the participants. |
| Incomplete outcome data (attrition bias) | Low risk | No participants excluded or lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | None |
| Methods | Randomised controlled trial Duration and location of the trial: quote: "This prospective intervention study was performed during the period from January 2010 till August 2012 at the outpatient clinic of Tanta University Hospital.“ | |
| Participants | Inclusion criteria: the most important inclusion criteria were fulfilment of at least 2 of Rotterdam criteria of PCOS, negative history of medical problems that can affect fertility such as diabetes mellitus, thyroid dysfunction, hyperprolactinaemia, congenital adrenal hyperplasia, normal hysterosalpingography and BMI between 20 and 30. Exclusion criteria: history of medical problems which affect fertility, history of recent hormonal therapy, having pelvic infections and/or having abnormal laboratory findings other than PCOS findings. Women whose husbands had defective semen were also excluded. Number of women randomised: 60 participants, 30 in each group Number of women analysed: 60 participants analysed Number of withdrawals/exclusions/loss to follow‐up and reasons: no participants were lost to follow‐up. Number of centres: 1, single‐centre trial Age (y): letrozole 26.2 ± 0.9; tamoxifen 26.9 ± 1.1 BMI (kg/m²): letrozole 27.7 ± 4.1; tamoxifen 28.4 ± 3.8 Duration of infertility (y): letrozole 3.2 ± 2.7; tamoxifen 3.0 ± 2.1 Country: Egypt | |
| Interventions | Group A: letrozole (Femara; Novartis) 2.5 mg/day given from day 5 ‐ 9 of the menstrual cycle, for 3 successive cycles Group B: TMX 20 mg/day given from day 5 ‐ 9 of the menstrual cycle, for 3 successive cycles | |
| Outcomes | Pregnancy rate, follicular growth, endometrial thickness, cumulative ovulation | |
| Notes | Ethical approval: the study was approved by the institutional ethics committee of Tanta Faculty of Medicine. Informed consent: all women subjected to history taking, physical examination, counselling and signing a written consent Source of funding: not reported Power calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Methods of randomisation were not sufficiently described: quote: "arranged at random, by sealed envelopes" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | 60 participants were randomised and analysed. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | None |
| Methods | Randomised double‐blind controlled trial Duration and location of the trial: quote: "A prospective double‐blind randomized controlled trial was conducted at the Teaching University Hospital of Cairo University, Cairo, Egypt, between August 1, 2013, and December 31, 2014.“ | |
| Participants | Inclusion criteria: quote: "eligible women were younger than 40 years, had primary or secondary infertility associated with PCOS, and had not ovulated in response to three cycles of 150 mg clomiphene citrate every day for 5 days from day 3 of the menstrual cycle. PCOS diagnoses were based on the revised 2003 Rotterdam consensus criteria. The presence of at least two of the following characteristics was considered diagnostic of PCOS: oligo ovulation or anovulation; hyperandrogenism; and polycystic ovaries detected using vaginal ultrasonography." Exclusion criteria: quote: "exclusion criteria were other factors of infertility, diabetes mellitus, hypertension, liver or kidney malfunction, heart disease, urinary symptoms, persistent hyperprolactinaemia, thyroid dysfunction, gonadotropin induction, and previous ovarian drilling. Male factor infertility was defined as a sperm count of less than 15 × 10^6/mL, a total motility of less than 40%, or normal morphology of less than 4%. Tubal factor infertility was confirmed by hysterosalpingography." Number of women randomised: 100 women were randomised. Number of women analysed: 100 women were analysed, 50 in each group Number of withdrawals/exclusions/loss to follow‐up and reasons: none Number of centres: single centre Age (y): CC 26.6 ± 2.9; letrozole 25.8 ± 3.6 BMI (kg/m²): CC 26.6 ± 2.7; letrozole 26.5 ± 2.8 Duration of infertility (y): CC 3.1 ± 1.4; letrozole 2.7 ± 1.6 Country: Egypt | |
| Interventions | Group A: (control group) received 100 mg clomiphene citrate, given as 2 x 50 mg tablets daily for 5 days from the third day of the menstrual cycle. Group B: 5 mg letrozole, given as 2 x 2.5 mg tablets daily for 5 days from the third day of the menstrual cycle. Participants in both groups also received metformin and pioglitazone, which was taken daily as 1 tablet containing 850 mg metformin and 15 mg pioglitazone, for 10 days starting from the first day of the menstrual cycle. | |
| Outcomes | Primary outcome measure: cumulative ovulation rate (proportion of cycles in which ovulation occurred in the whole follow‐up period). | |
| Notes | Ethical approval: approved by the research ethics committee of the teaching University Hospital of Cairo University Informed consent: all participants signed a written informed consent form. Source of funding: Cairo University Power calculation: Previous data indicated that the ovulation rate in group A would be 62%. If the ovulation rate for the letrozole, metformin, and pioglitazone (experimental) group was 87% (previous unpublished data from the study unit), a total of 47 women would have to be recruited to each group to ensure a sufficiently powered study. Assuming an attrition of 10%, the total number of patients to be recruited was 50 per group. Intention‐to‐treat analyses were planned. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Enrolled women were randomly allocated using computer‐generated random number tables (block size four)" |
| Allocation concealment (selection bias) | Low risk | Quote: "Opaque sealed envelopes containing group allocations were prepared at a separate location every 24 hours. These envelopes were sent to an assigned nurse, who opened them before commencing ovulation induction" |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "Participants, the staff who conducted follow‐up, and data analysts were masked to the allocation to avoid bias" |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Participants, the staff who conducted follow‐up, and data analysts were masked to the allocation to avoid bias" |
| Incomplete outcome data (attrition bias) | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | Low risk | None |
| Methods | Randomised controlled trial Duration and location of the trial: not stated | |
| Participants | Inclusion criteria: clomiphene citrate‐resistant women with infertility due to PCOS, diagnosed according to the Rotterdam 2003 criteria. Clomiphene citrate resistance was defined as failure to achieve adequate follicular maturation after 3 consecutive induction cycles with CC at 150 mg/day for 5 days. Exclusion criteria: exclusion criteria include women with other causes of infertility such as male factor or tubal factor, those with endocrine disorders such as thyroid dysfunction and hyperprolactinaemia, women who received hormonal treatment or ovulation induction drugs 3 months before the study Number of centres: 1, Zagazig University Hospital, Egypt Number of women randomised: 146 women, 73 in each group Number of women analysed: 146 women, 73 in each group Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 Age (y): group A metformin + letrozole: 24.7 ± 1.8, group B LOD: 25.1 ± 2.1 BMI (kg/m²): group A metformin + letrozole: 31.5 ± 3.3, group B LOD: 32.4 ± 4.4 Duration of infertility (y): group A metformin + letrozole: 3.4 ± 0.9, group B LOD: 3.9 ± 1.1 Country: Egypt | |
| Interventions | Group A: metformin 850 to 1700 mg daily for 6 ‐ 8 weeks, followed by 5 mg letrozole daily orally given for 5 days during cycle days 3 ‐ 7 if pregnancy did not occur Group B: LOD, laparoscopy was performed using 3‐puncture technique. | |
| Outcomes | Cycle regularity, ovulation rate, clinical pregnancy rate, miscarriage rate | |
| Notes | Ethical approval: yes, quote: “Ethics Committee of Zagazig University approved the study" Informed consent: yes, quote: “written informed consent was obtained from each patient at the start of the study” Source of funding: not stated Conflicts of interest: quote: "conflicts of interest: none" Power calculation: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The participant women were randomised according to a computer‐generated random numeric table." |
| Allocation concealment (selection bias) | Low risk | The random allocation sequence was concealed in sealed dark envelopes, then participants assigned randomly into group 1 (n = 73) received metformin plus letrozole, and group 2 (n = 73) underwent LOD. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts reported |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | None |
| Methods | Randomised controlled clinical trial Duration and location of the trial: quote: "This clinical trial was performed on 120 infertile women with PCOS who attended in the outpatient infertility clinic in Kashan, Iran during 2008.“ | |
| Participants | Inclusion criteria: quote: "Our inclusion criteria were age 20‐35 years, infertility for at least one year and resistance to Clomiphene (at least 3 cycles Clomiphene usage, 150 mg/day with no ovulatory response)" Exclusion criteria: exclusion criteria were BMI > 27, endocrine disorders such as hypothyroidism, hyperprolactinaemia, infertility due to male factors, uterine factors and adhesive diseases due to pelvic surgery. Number of centres: 1, outpatient infertility clinic in Kashan Number of women randomised: 60 in each group Number of women analysed: 60 in each group Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 Age (y): group A letrozole + hMG: 25.8 ± 3.8, group B CC + hMG: 25.3 ± 4.1 BMI (kg/m²): group A letrozole + hMG: 24.1 ± 2.3, group B CC + hMG: 24.9 ± 2.0 Duration of infertility (y): group A letrozole + hMG: 2.8 ± 2.3, group B CC + hMG: 2.6 ± 2.1 Country: Iran | |
| Interventions | Group A: letrozole, 5 mg/day orally given for 5 days from cycle days 3 ‐ 7 + 150 IU hMG intramuscularly during cycle days 5 ‐ 8 Group B: clomiphene citrate, 100 mg/day orally given for 5 days from cycle days 3 ‐ 7 + 150 IU hMG intramuscularly during cycle days 5 ‐ 8 | |
| Outcomes | Live birth rate, OHSS rate, pregnancy rate, miscarriage rate, multiple birth rate, number of dominant follicles, endometrial thickness (mm), ectopic pregnancies | |
| Notes | Ethical approval: Yes, quote: ”approval was obtained from the Institute Research Board to perform this study.“ Informed consent: Yes, quote: “All patients were informed about possible side effects ad also off label use of letrozole for the purpose of inducing ovulation and written consent were obtained for all participants.” Source of funding: Yes, quote: “Authors acknowledge the research deputy of Kashan University of Medical Sciences for providing the financial support.” Power calculation: Not stated Authors contacted by email, all information provided | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple randomisation was performed by a computer |
| Allocation concealment (selection bias) | Low risk | By sequentially‐numbered opaque sealed envelopes (email with authors) |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "Before commence of the study all patients were informed of the study and were told about this issue that it is possible to be enrolled in letrozole or clomiphene group but none of them knew which group she allocated to and the researcher was blinded also to patients' treatment approach." (email contact with authors) |
| Blinding of outcome assessment (detection bias) | Low risk | See above |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts reported |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | None |
| Methods | Randomised controlled trial Duration and location of the trial: not stated | |
| Participants | Inclusion criteria: 1387 women with PCOS diagnosed by the Rotterdam criteria who had previously failed to conceive or ovulate with CC treatment and undergoing IUI. Specific inclusion criteria for the study were normal TSH and prolactin levels and normozoospermic male partners as per WHO guidelines. Exclusion criteria: women with pre‐existing ovarian cyst on day 3 and previous history of ovarian drilling were excluded. Number of centres: 1, a tertiary infertility care unit, Institute of Reproductive Medicine, Kolkata, India Number of women randomised: 1378 Number of women analysed: 1378 Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 Age (y): group A letrozole: 30.3 ± 4.9, group B CC: 30.4 ± 5.2, group C rFSH: 30.8 ± 4.6 BMI (kg/m²): group A letrozole: 24.5 ± 3.8, group B CC: 24.8 ± 4.1, group C rFSH: 24.1 ± 3.4 Duration of infertility (y): Not reported Country: India | |
| Interventions | Group A: letrozole, 5 mg/day orally given for 5 days from cycle days 3 ‐ 7 Group B: clomiphene citrate, 100 mg/day orally given for 5 days from cycle days 3 ‐ 7 + 75 or 100 IU rFSH during cycle days 3 and 8. Group C: rFSH 75IU/100IU from day 2 until the day of hCG administration | |
| Outcomes | Primary outcome measures: ovulation rate, cancellation rate, miscarriage rate and pregnancy rate | |
| Notes | Ethical approval: yes, approval was obtained from the institutional Research Ethics Board. Informed consent: yes, quote: “Written informed consent was taken from all women included in this study.” Source of funding: quote: "This study was not funded by any funding agency.” Power calculation: not stated Authors contacted by email, all information provided | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The subjects recruited for the study were randomly and blindly assigned to one of the treatment protocols. The procedure was carried out by requesting the patient to pick up randomly an opaque, sealed envelope. Each envelope contained a piece of paper with one of the three protocols written on it. Many such sealed envelopes were prepared and placed randomly. Once the patient picked the envelope, the seal was opened in front of the patient and the coordinator, the content showed and the protocol allocated." (Information by email from the author) |
| Allocation concealment (selection bias) | Low risk | Quote: "the allocation was done using sealed envelopes where the person allocating was blinded to the type of protocol received by the patients." |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "Only researcher was blinded and the patient aware of the protocol followed since the route of administration was different in all the three groups." |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Only researcher was blinded and the patient aware of the protocol followed since the route of administration was different in all the three groups." |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts reported |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | None |
| Methods | Randomised controlled clinical trial Duration of the trial: quote: "This was a randomized prospective clinical trial, including consecutive women with primary or secondary infertility due to PCOS from Jan 2009 to Sept 2011.“ | |
| Participants | Inclusion criteria: the major criteria for diagnosis of PCOS were oligo‐ and/or anovulation, clinical or biochemical signs of hyperandrogenism, and polycystic ovaries, in accord with the revised 2003 Rotterdam criteria of PCOS. Thyroid function, prolactin level, and husband’s sperm analysis were checked for normal values. Exclusion criteria: women with other causes of infertility, infertility < 1 year, and those who got previous treatment(s) for infertility were not included in the study. Number of women randomised: 103; 51 to group A (CC), 52 to group B (letrozole) Number of women analysed: 50 participants in group A, 51 in group B Number of withdrawals/exclusions/loss to follow‐up and reasons: 2 participants, 1 from each group lost to follow‐up due to no show Number of centres: single‐centre study Age (y): no mean age reported for the treatment groups BMI (kg/m²): group A 27.1 ± 4.9; group B 28.2 ± 5.2 Duration of infertility (y): no means reported Country: Iran | |
| Interventions | Group A: clomiphene citrate 100 mg for 5 days starting from day 3 of their menstrual cycle Group B: 5 mg letrozole for 5 days from day 3 of their menstrual cycle Both groups were advised to have intercourse on days 11, 13, and 15 of their menstrual cycles. | |
| Outcomes | Pregnancy rate, miscarriage rate, multiple pregnancies, ectopic pregnancies, OHSS rate | |
| Notes | Ethical approval: the protocol was approved by the ethical investigation committee of the institution Informed consent: informed consent was obtained from all the participants after full informative session. Source of funding: not reported Power calculation: quote: "based on our statistical data, the fair needed number for performing this study was 50 per group (the sample size was calculated by considering z, p, and d as 1.96, 0.15, and 0.1, respectively)." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | All candidates were randomised based on envelope method into either clomiphene citrate group (group A, n = 51) or letrozole group (group B, n = 50) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | 2 of 103 participants were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | Low risk | None |
| Methods | Randomised controlled clinical trial Duration and location of the trial: quote: "The study was performed from March to November 2010 at the Mashhad IVF center, a university based infertility center.“ | |
| Participants | Inclusion criteria: based on Rotterdam criteria, 70 women with PCOS were enrolled in this randomised clinical trial. The diagnosis of PCOS was made when 2 of the following 3 criteria existed: oligomenorrhoea or amenorrhoea, clinical hyperandrogenism, and polycystic ovaries on ultrasonography. The inclusion criteria were as follows: i. Previous diagnosis of PCOS according to Rotterdam criteria, ii. Age between 20 and 30 years, iii. No previous history of ovarian surgery, and iv. lack of ovulation with CC in at least 3 previous cycles (lack of follicle ≥ 18 mm on ultrasound scan). The woman’s age, her partner’s age, duration of infertility, type of infertility (primary and secondary), history of previous intrauterine insemination (IUI) cycles, pattern of ovary (PCO and non‐PCO), pattern of menstruation (regular, oligomenorrhoea and amenorrhoea), BMI and basal LH/FSH ratio were recorded for each participant. Exclusion criteria: the exclusion criteria were as follows: i. No other infertility factors, ii. Exposure to cytotoxic drugs and iii. Pelvic radiation therapy. Number of women randomised: 70 Number of women analysed: 69 Number of withdrawals/exclusions/loss to follow‐up and reasons: 1 patient discontinued treatment in group B Number of centres: single‐centre study Age (y): group A: 25.3 ± 4.4, group B: 25.6 ± 3.5 BMI (kg/m²): group A: 27.0 ± 3.8, group B: 26.4 ± 4.8 Duration of infertility (y): number of previous treatment cycles (CC): group A: 1.1 ± 0.4, group B: 1.3 ± 0.5 Country: Mashhad, Iran | |
| Interventions | Group A: group A (n = 35) receiving 5 mg letrozole (Letrofem; Iran Hormone, Iran) on cycle days 3 ‐ 7 Group B: group B (n = 35) receiving the same amount on cycle days 5 ‐ 9. | |
| Outcomes | The cycle characteristics, the ovulation and pregnancy rate | |
| Notes | Ethical approval: this study was approved by Ethical Committee of Mashhad University of Medical Sciences. Informed consent: a written informed consent was taken from all women participating in this study. Source of funding: not reported Power calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | 1 participant was excluded from analysis due to discontinuation of treatment. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported. |
| Other bias | Low risk | None |
| Methods | Randomised controlled clinical trial Duration and location of the trial: quote: "This was a balanced, randomized (allocation ratio 1:1), parallel group study conducted in Cairo and Beni‐Suef University Hospitals from May 2013 to January 2015.“ | |
| Participants | Inclusion criteria: women included in the study had CC‐resistant PCOS, and were aged 20 – 40 years. PCOS was diagnosed according to the Rotterdam 2003 criteria. CC resistance was defined as failure of ovulation despite receiving 150 mg of CC for 5 days during successive menstrual cycles for 3 months. Exclusion criteria: other causes of infertility, BMI> 35 kg/m², hyperprolactinaemia, allergy to FSH, and previous use of FSH or letrozole therapies. Number of women randomised: 140, 70 to each group Number of women analysed: 140, 70 in each group Number of withdrawals/exclusions/loss to follow‐up and reasons: 3 women in the letrozole group and 2 women in the uFSH group were lost to follow‐up; intention‐to‐treat analysis was adopted in which these participants were considered anovulatory in the 3 cycles. Number of centres: 2‐centre trial Age (y): letrozole group 28.7 ± 6.2, uFSH group 30.0 ± 5.6 BMI (kg/m²): letrozole group 27.6 ± 4.1, uFSH group 27.2 ± 3.8 Duration of infertility (y): letrozole group 87.0 ± 2.1, uFSH group 5.2 ± 2.2 Country: Cairo University and Beni‐Suef University Hospitals, Egypt | |
| Interventions | Group A: quote: "group 1 received letrozole (Femara VR, Novartis, Basel, Switzerland) 2.5 mg twice daily for five days starting from the third day of menstruation or progesterone withdrawal bleeding." Group B: quote: "group 2 received uFSH (Fostimon VR IBSA, Geneva, Switzerland). To minimize the risk of multiple pregnancy and OHSS, we used a low‐dose FSH setup regimen. The starting daily dose of uFSH was 75 IU for seven days starting from the third day of menstruation or progesterone withdrawal bleeding. If the follicular diameter did not exceed 9 mm, the daily dose was increased by 37.5 IU every seven days. The cycle was cancelled if no follicles exceeded 9 mm by four weeks after starting FSH." | |
| Outcomes | Cumulative clinical pregnancy, defined as the presence of an intrauterine gestational sac 5 weeks after timed intercourse Secondary outcomes were ovulation, miscarriage and possible drug side effects, i.e. OHSS, headache, dizziness, hot flushes, nausea, vomiting or constipation | |
| Notes | Ethical approval: the study was approved by the research ethics committees of both institutions. Informed consent: written informed consent was obtained Source of funding: quote: "The study was self‐funded" Power calculation: quote: "The required sample size was estimated using PS Power and Sample Size Calculations software, version 3.0.11 for Microsoft Windows. We needed to study 64 women receiving letrozole and 64 women receiving uFSH for three cycles to be able to reject the null hypothesis that the pregnancy rates for letrozole and uFSH in CC‐resistant women were equal, with a probability (power) of 0.9." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An independent individual generated the allocation sequence using computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | Allocation was concealed using sequentially‐numbered opaque sealed envelopes |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | All participants randomised were also analysed |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | Low risk | None |
| Methods | Randomised controlled clinical trial Duration and location of the trial: not stated | |
| Participants | Inclusion criteria: quote: "infertile patients (defined as one year of unprotected coitus without conception in patients who have never conceived before) with PCOS, aged younger than 35 years, and attending the infertility out‐ patient clinic at Ain Shams University Hospital and/or a local private outpatient setting. Diagnosis of PCOS was based on the Rotterdam criteria (2003 ESHRE/ ASRM consensus), whereby patients diagnosed with PCOS require the presence of two of three criteria, i.e., oligomenorrhoea and/or anovulation, clinical and/ or biochemical signs of hyperandrogenism, and/or polycystic ovaries on ultrasound. All patients had a history of failed induction of ovulation with appropriately timed intercourse at least 4–6 times." Exclusion criteria: women with infertility due to uterine and tubal pathologies or male factor Number of women randomised: 60 women with primary infertility Number of women analysed: 54 women were analysed, 28 in group 1 (letrozole) and 26 in group 2 (clomiphene citrate) Number of withdrawals/exclusions/loss to follow‐up and reasons: during folliculometry, 2 participants in Group 1 and 4 participants in Group 2 showed no follicular response and were excluded from the study. Number of centres: 2‐centre trial Age (y): group 1 included 30 women aged 21 – 34 (mean ± SD, 27.2 ± 5.18) years, group 2 included 30 women aged 20 – 33 BMI (kg/m²): group 1 included 30 women with a BMI of 24 – 31 (26.2 ± 1.8). Group 2 included 30 women with a BMI of 23 – 32 (29.1 ± 2.3) Duration of infertility (y): mean duration of infertility not reported Country: Egypt | |
| Interventions | Group A: group 1 included 30 women who were given letrozole (Femara®, Novartis, Basel, Switzerland) orally at a dose of 2.5 mg once daily on days 3 – 7 of the menstrual cycle. Group B: group 2 included 30 women who were given clomiphene citrate (Clomid®, Sano Aventis, France) 50 mg orally twice daily on days 3 – 7 of the menstrual cycle. | |
| Outcomes | Pregnancy rate, multiple pregnancy rate, number of follicles on hCG administration day, endometrial thickness | |
| Notes | Ethical approval: the study was approved by the medical ethics committee of Ain Shams University Hospital. Informed consent: Informed consent was obtained from all participants Source of funding: not reported Power calculation: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised using a computer‐generated programme |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | double‐blind randomised, but not reported how blinding was achieved |
| Blinding of outcome assessment (detection bias) | Unclear risk | double‐blind randomised, but not reported how blinding was achieved |
| Incomplete outcome data (attrition bias) | Low risk | 6/60 participants were lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was found |
| Other bias | Unclear risk | None |
| Methods | Randomised controlled trial Duration of the trial: quote: "The study was conducted during the period from 1st August 2015 to 30th March 2016.“ | |
| Participants | Inclusion criteria: quote: "age >20 and <35 years old, patients were diagnosed to have PCOS criteria of diagnosis of PCO. Normal HSG and their partners had normal semen analysis according to WHO criteria (WHO, 2010) and CC‐resistant. If patients fail to respond to 150 mg/day for 5 days for 3 consecutive cycles, they are considered as CC‐resistant." Exclusion criteria: quote: "Age less than 20 yr or more than 35 yr, non‐PCOS, and those Patients with poor ovarian reserve i.e. hyperprolactinaemia, hypo and hyperthyroidism, diabetic patients and Cushing’s syndrome were excluded, non‐classical congenital adrenal hyperplasia, current or previous (within the last 6 months) use of oral contraceptives, glucocorticoids, antiandrogens, antidiabetic or antiobesity drugs, or other hormonal drugs, any subject was affected by either neoplastic, metabolic, hepatic, or cardiovascular disorder or other concurrent medical illness (i.e. diabetes, renal disease, or malabsorptive disorders) were excluded, pelvic diseases, previous pelvic surgery, suspected peritoneal factor infertility, tubal infertility and male factor infertility were excluded with a hysterosalpingogram and with semen analysis, respectively." Number of women randomised: 80 women, 40 within each group Number of women analysed: 80 women, 40 within each group Number of withdrawals/exclusions/loss to follow‐up and reasons: none Number of centres: single‐centre trial Age (y): LOD group 28.8 ± 3.1 vs let group 29.7 ± 3.7 BMI (kg/m²): LOD group 29.1 ± 1.6, letrozole group 29.2 ± 1.7 Duration of infertility (y): no mean ± SD reported Country: Egypt | |
| Interventions | Group A: quote: "In group A, laparoscopy was performed under intravenous general anaesthesia with the patient in a supine position. A 5 mm incision was made in the navel, through which a long sheath punctured into the abdominal cavity, and the inflatable pneumoperitoneum was placed. Another two 5‐mm incisions were made on the right and left lower abdomen and the surgical instruments were inserted into the abdominal cavity. The patient was adjusted into a position with the head high up, the pelvic organs were exposed and a comprehensive exploration of the pelvic organs was made, focusing on the structure and position of the adjacent organs of the bilateral ovaries. Once immobilized, each ovary was cauterized at 4–6 points, using a monopolar electrosurgical needle, according to the size of each ovary. Following cauterization, a bilateral tubal hydrotubation with methylene blue was performed. During the procedure. The pelvis was irrigated using physiological saline. Ringer’s solution plus dexamethasone was added into the abdominal cavity to avoid adhesion. The total duration of the procedure, as well as any intra‐operative or post‐operative complications, was noted." Group B: quote: "In group B, 2.5 mg twice daily LE oral tablets were administered on the 3rd day of menses and then every day for 5 days. Treatment was repeated for up to six cycles if the patient failed to ovulate, the patients were followed‐up for 6 months after the treatment in both groups." | |
| Outcomes | Pregnancy rate, abortion rate, ovulation, regular cycles, ovarian volume, antral follicle count (AFC) | |
| Notes | Ethical approval: This study was approved by Minia University Ethical Committee Informed consent: quote: “Informed consent was obtained from all participating women after the nature and purpose of the study had been explained to them and were fully understood” Source of funding: quote: “We have not received any funding from any corporate body or pharmaceutical company. “ Power calculation: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was achieved via the use of a randomisation number allocated prior to dosing, once eligibility had been determined, and a randomisation schedule was produced by an interactive voice response system vendor." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Participants were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Once the patients had been allocated to one of the two groups, the treatment was revealed to the investigator; however, the doctor responsible for performing the transvaginal ultrasound follow up assessment was blinded to the treatment groups." |
| Incomplete outcome data (attrition bias) | Low risk | All women randomised were also analysed. |
| Selective reporting (reporting bias) | Unclear risk | We found no reporting of outcomes in a study protocol or Methods section |
| Other bias | Low risk | None |
| Methods | Randomised double‐blind placebo‐controlled trial Duration and location of the trial: quote: "This trial was conducted in a university teaching hospital between 2007 and 2009.“ | |
| Participants | Inclusion criteria: women with PCOS and clomiphene resistance who were being treated with ovulation induction. Additionally, women had to have a normal hormone profile and a male partner with normal semen parameters by WHO criteria. Normal hormone profile was defined as a FSH level of < 12 IU/L, serum prolactin level of < 25 ng/mL, and a thyroid‐stimulating hormone (TSH) value between 0.3 and 4.5 µIU/mL. Exclusion criteria: women with other endocrine disorders such as Cushing syndrome, and congenital adrenal hyperplasia Number of centres: 1, Reproductive Medicine Unit, Christian Medical College, Vellore, Tamil Nadu, India Number of women randomised: 18 in each group Number of women analysed: 17 in each group Number of withdrawals/exclusions/loss to follow‐up and reasons: 2 lost to follow‐up before treatment started Age (y): group A letrozole: 25.6 ± 3.6, group B placebo: 25.7 ± 3.7 BMI (kg/m²): group A letrozole: 26.1 ± 3.7, group B placebo: 24.7 ± 4.2 Duration of infertility (y): group A letrozole: 5.2 ± 3.2, group B placebo: 3.6 ± 2.2 Country: India | |
| Interventions | Group A: letrozole, orally given 2.5 mg/day for 5 days from cycle days 2 ‐ 6 Group B: placebo, also given for 5 days from cycle days 2 ‐ 6 | |
| Outcomes | Primary Outcome: ovulation rate Secondary Outcomes: live birth rate, OHSS rate, pregnancy rate, miscarriage rate, multiple pregnancy rate, endometrial thickness (mm), day 21 serum progesterone (nmol/L), number of participants with mature follicle (%) | |
| Notes | Ethical approval: yes, the protocol of the study was approved by the institutional review board Informed consent: yes, written informed consent was obtained from each participant Source of funding: not stated Conflicts of interest: quote: "The Authors have nothing to disclose" Power calculation: quote: "Our literature pointed to a 75% ovulation rate when 2.5 mg of letrozole was used in women with PCOS who had clomiphene resistance. We hypothesized an ovulation rate of 60& with letrozole and 10% with placebo. On this basis, a sample size of 17 women in each arm (80% and alpha .05 for a two‐sided test) was calculated." Contacted authors about OHSS rate and how randomisation and allocation concealment were done in detail. All information provided | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly distributed using a computer‐generated randomisation sequence in blocks of 6, into 2 groups. |
| Allocation concealment (selection bias) | Low risk | Allocation concealment was done by using consecutively‐numbered sealed opaque envelopes containing the treatment packets. |
| Blinding of participants and personnel (performance bias) | Low risk | The randomisation code was maintained by the pharmacy department, which revealed the group assignments at the end of the trial. |
| Blinding of outcome assessment (detection bias) | Low risk | The code was revealed after the statistical analysis had been performed. |
| Incomplete outcome data (attrition bias) | Low risk | 1 women in each group was lost to follow‐up, after randomisation and before treatment started. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | None |
| Methods | Randomised controlled trial Duration of the trial: quote "The prospective randomized trial was conducted between July 2010 and July 2011.“ | |
| Participants | Inclusion criteria: quote: "PCOS was diagnosed according to Rotterdam criteria. All women were treatment‐naive i.e. had not undergone any significant treatment for infertility/ovulation induction earlier." Exclusion criteria: quote: "Patients with hyperprolactinaemia, thyroid disorder, male factor, suspected tubal factor, endometriosis, unexplained infertility were not included in the study." Number of centres: quote: "This study was conducted at a private hospital with a large gynaecological practice." Number of women randomised: 103 women, 52 in the letrozole group and 51 in the CC group. Number of women analysed: 103 women, 52 in the letrozole group and 51 in the CC group. Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 Age (y): group A letrozole: 26.3 ± 2.4, group B CC: 26.3 ± 2.5 BMI (kg/m²): group A letrozole: 25.9 ±3.6, group B placebo: 26.0 ± 3.3 Duration of infertility (y): group A letrozole: 3.1 ± 1.9, group B CC: 3.1 ± 2.2 Country: India | |
| Interventions | Group A: letrozole, 5 mg/day orally given for 5 days from cycle days 2 ‐ 6 Group B: clomiphene citrate, 100 mg/day orally given for 5 days from cycle days 2 ‐ 6 | |
| Outcomes | Primary outcomes: ovulation rate, endometrial thickness, mono vs. multi‐follicular rate, and days to ovulation. Secondary outcomes: pregnancy and miscarriage rate | |
| Notes | Ethical approval: yes, quote: "Study protocol was approved by the institutional ethics committee." Informed consent: not stated. Source of funding: quote: "Nil" Power calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomised by lottery" |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts reported |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | Low risk | None |
| Methods | Randomised double‐blind multicentre trial Duration of the trial: quote: "Enrollment began in February 2009 and was completed in January 2012.“ | |
| Participants | Inclusion criteria: women with PCOS defined by the Rotterdam criteria and at least 1 patent fallopian tube and normal uterine cavity, and a male partner with sperm concentration of > 14 million/mL Exclusion criteria: quote: "We will exclude subjects with medical conditions that represent contraindications to CC,letrozole and/or pregnancy or who are unable to comply with the study procedures." Number of centres: multicentre trial Number of women randomised: 750, 374 in the letrozole group and 376 in the CC group Number of women analysed: 750, 374 in the letrozole group and 376 in the CC group Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 Age (y): group A letrozole: 29 ± 5, group B CC: 28 ± 4 BMI (kg/m²): group A letrozole: 35 ± 10, group B CC: 35 ± 9 Duration of infertility (y): not reported Country: USA | |
| Interventions | Group A: letrozole, orally given 2.5 mg/day for 5 days during cycle days 3 ‐ 7 Group B: clomiphene citrate, orally given 100 mg/day for 5 days during cycle days 3 ‐ 7 | |
| Outcomes | Live birth, ovulation rate, clinical pregnancy rate, miscarriage rate, multiple pregnancy rate | |
| Notes | Ethical approval: quote:"The institutional review board at each centre approved the protocol, and all participants (women and their male partners) gave written informed consent." Informed consent: quote: "The institutional review board at each centre approved the protocol, and all participants (women and their male partners) gave written informed consent." Source of funding: quote: "The study is funded through a cooperative agreement by the Eunice Kennedy ShriverNational Institutes of Child Health and Human Development (NICHD)" Power calculation: a sample size of 300 subjects in each arm of the randomisation yields 81% statistical power to prospectively demonstrate a 0.10 absolute difference in live birth proportions between treatment arms (0.20 for CC and 0.30 for letrozole) using the Pearson’s Chi2 test with a 2‐sided significance level of 0.05 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Almac statisticians will generate the randomisation scheme for the study." |
| Allocation concealment (selection bias) | Low risk | Third‐party allocation |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "In order to maintain the double‐blind, CC and letrozole will be over encapsulated and packaged in identically appearing numbered study kits (using AlmacClinical Services, Durham NC) which will then be directly shipped to each clinical site." |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "In order to maintain the double‐blind, CC and letrozole will be over encapsulated and packaged in identically appearing numbered study kits (using AlmacClinical Services, Durham NC) which will then be directly shipped to each clinical site. The randomisation scheme (including block size) will be disclosed to the DCC data manager, but not to any RMN investigators or staff, including the Protocol Lead Investigator." |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts were reported |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | Low risk | None |
| Methods | Randomised controlled clinical trial Duration and location of the trial: not stated | |
| Participants | Inclusion criteria: quote: "the women were diagnosed with PCOS based on the Revised 2003 Consensus Diagnostic Criteria for PCOS. Clomiphene resistance, i.e. failure to ovulate following 100 mg CC for 5 days for at least three cycles; patent fallopian tubes, confirmed by hysterosalpingography or hysteroscopic diagnosis; normal semen analysis parameters of the patients' spouses according to the modified criteria of the World Health Organization (14); normal serum prolactin, thyroid stimulating hormone and 17‑OH progesterone; no systemic disease; no gonadotropin or other hormonal drug treatment during the preceding 3 months; normal blood count and blood chemistry, including glutamic‑pyruvic transaminase, glutamic‑oxaloacetic transaminase, urea nitrogen, creatinine, glucose and urine analysis. The semen of the patients' spouses was tested to strengthen the comparability between the two groups. During the period of treatment, all patients were requested to follow a normal diet and rest regime and to avoid intense physical activities in any form and mental stress and fatigue." Exclusion criteria: infertility induced by reasons other than PCOS; uterine cavity lesions or ovarian cyst; > 40 years old; BMI > 26 kg/m2; contraindications to general anaesthesia; history of pelvic surgery; other endocrine diseases; or a history of liver or kidney disease Number of women randomised: 141 women were randomly assigned, 71 to group A (letrozole) and 70 to group B (LOD) Number of women analysed: all women randomised were also analysed Number of withdrawals/exclusions/loss to follow‐up and reasons: none Number of centres: single‐centre trial Age (y): letrozole group 29.5 ± 3.3, LOD group 28.1 ±3.6 BMI (kg/m²): letrozole group 22.5 ± 1.5, LOD group 22.4 ± 2.1 Duration of infertility (y): letrozole group 3.4 ± 0.4, LOD group 3.2 ± 0.7 Country: China | |
| Interventions | Group A: quote: "In group A, 2.5 mg LE oral tablets (Adooq Bioscience, Nanjing, China) were administered on the fifth day of menses and then every day for 5 days. Treatment was repeated for up to six cycles if the patient failed to conceive." Group B: quote: "In group B, laparoscopy was performed under intravenous general anaesthesia (Diprivan; AstraZeneca S.p.A., Rome, Italy) with the patient in a supine position. A 5‑mm incision was made in the navel, through which a long sheath punctured into the abdominal cavity, and the inflatable pneumoperitoneum (Guangxi University, Yuannan, China) was placed. Another two 5‑mm incisions were made on the right and left lower abdomen and the surgical instruments were inserted into the abdominal cavity. The patient was adjusted into a position with the head high up, the pelvic organs were exposed and a comprehensive exploration of the pelvic organs was made, focusing on the structure and position of the adjacent organs of the bilateral ovaries. Once immobilized, each ovary was cauterized at 4‑6 points, each for 4 sec at 40 W, at a depth of 7‑8 mm and a diameter of 3‑5 mm, using a monopolar electrosurgical needle (Kirgen Co., Shanghai, China), according to the size of each ovary. Following cauterization, a bilateral tubal hydrotubation with methylene blue was performed. During the procedure, small pieces of the ovaries were obtained for pathological analysis. The pelvis was irrigated using physiological saline. Ringer's solution (ZiQi Bioscience, Shanghai, China) plus dexamethasone was added into the abdominal cavity to avoid adhesion. The total duration of the procedure, as well as any intra‑operative or post‑operative complications, was noted. The patients were followed‑up for 6 months after the procedure." | |
| Outcomes | Live birth rate, OHSS, clinical pregnancy was defined by a fetal heart beat monitored by ultrasound at 6 weeks of gestation. Biochemical pregnancy was considered when hCG was > 2.5 mIU/ml in the absence of menstruation. Ovulation rate, endometrial thickness in mm, synchronous cycles, mean follicular diameter, spontaneous abortion rate, multiple pregnancy rate | |
| Notes | Ethical approval: this study was approved by Tongji Hospital Research Ethics Committee (Shanghai, China) Informed consent: all participants provided informed consent prior to inclusion in the trial. Source of funding: the present study was supported by the Shanghai Natural Science Foundation (grant no. 12ZR1434200). Power calculation: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The women were randomly allocated into the either the letrozole or LOD group (groups A and B, respectively)." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "Once the patients had been allocated to one of the two groups, the treatment was revealed to the investigator; however, the doctor responsible for performing the transvaginal ultrasound follow‑up assessment was blinded to the treatment groups." |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Once the patients had been allocated to one of the two groups, the treatment was revealed to the investigator; however, the doctor responsible for performing the transvaginal ultrasound follow‑up assessment was blinded to the treatment groups." |
| Incomplete outcome data (attrition bias) | Low risk | All women randomised were also analysed |
| Selective reporting (reporting bias) | Unclear risk | All expected outcomes were reported |
| Other bias | Unclear risk | None |
| Methods | Randomised controlled clinical trial Duration and location of the trial: quote: "PCOS patients attending the outpatient department of the hospital between April 2012 and March 2014, who had a desire for childbearing and fulfilled the Rotterdam diagnostic criteria as well, were recruited for this study.“ | |
| Participants | Inclusion criteria: quote: "PCOS patients attending the outpatient department of the hospital between April 2012 and March 2014, who had a desire for childbearing and fulfilled the Rotterdam diagnostic criteria as well, were recruited for this study. The inclusion criteria for this study were as follows: (1) patency of at least one side of the fallopian tube and (2) normal spouse’s sperm." Exclusion criteria: quote:"The exclusion criteria were as follows: (1) patients with gynaecologic tumours or genital tract malformations, (2) patients with severe systemic disease or acute and chronic urogenital tract infections, (3) patients with other endocrine diseases such as thyroid disease and adrenal disease, (4) body mass index (BMI)>30, and (5) age over 35 years or below 20 years." Number of women randomised: 268 women Number of women analysed: Unknown if all 268 or only 240 were analysed Number of withdrawals/exclusions/loss to follow‐up and reasons: 28 women left the study; 13 in the CC groups, 15 in the LE groups; 5 in the CC + met and 7 in the LE + met group left the study due to complications; 3 participants were excluded (no reasons reported), the rest were lost to follow‐up Number of centres: single‐centre trial Age (y): group A (CC) 26.8 ± 3.1; group B (CC + met) 27.2 ± 2.8; group C (letrozole) 27.0 ± 3.0; group D (letrozole + met) 27.2 ± 3.3 BMI (kg/m²): group A (CC) 21.1 (19.9, 22.8); Group B (CC + met) 21.4 (19.8, 23.6); group C (letrozole) 20.8 (19.1, 22.3); group D (letrozole + met) 21.6 (19.2, 23.6) Duration of infertility (y): group A (CC) 1 (0, 2); group B (CC + met) 1 (0, 3); group C (let) 1 (0, 2); group D (let + met) 1 (0, 3) Country: China | |
| Interventions | Group A: the oral administration of CC was started in the group CC or CC + met from day 3 to day 5 of the menstrual cycle at a daily dose of 50 mg for 5 days; and the daily dose gradually increased to 100 mg or 150 mg at maximum in the next cycle if the undeveloped follicle (< 16 mm) was present in the previous cycle. Group B: The oral administration of letrozole started in the group letrozole or letrozole + met from day 3 to day 5 of the menstrual cycle at a daily dose of 5 mg for 5 days. Additional met (1000 – 1500 mg/d) was orally administered to participants in the groups CC + met and letrozole + met. | |
| Outcomes | Ovulation rate, pregnancy rate, live birth rate, miscarriage rate, premature delivery, OHSS, multiple pregnancy rate | |
| Notes | Ethical approval: the study was approved by the ethics committee of the West China Second University Hospital, Sichuan University, China (approval No. Medical Research 2012 No. 004), and the study was registered in the Chinese Clinical Trial Registry Center (registration No. ChiCTR‐TRC‐11001821). Informed consent: informed consent was obtained from each participant. Source of funding: self‐supported by West China Women's and Children's Hospital S.C.U Power calculation: ovulation rate as the main indicator, the sample size was calculated by introducing maximal and minimal ovulation rate retrieved in literatures into the formula | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation with computer‐generated blocks |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Not blinded |
| Incomplete outcome data (attrition bias) | High risk | 28 of 268 women left the study (> 10%) Unknown if all 268 or only 240 were analysed |
| Selective reporting (reporting bias) | Low risk | All outcomes expected were reported |
| Other bias | Low risk | None |
| Methods | Randomised controlled clinical trial Duration and location of the trial: quote: "Three hundred and thirty seven infertile women with anovulatory (PCOS) were recruited from the outpatient clinics of both 6th October and Bab Elshaaria University Hospitals from August 2014 and January 2015.“ | |
| Participants | Inclusion criteria: infertile women with anovulatory (PCOS), age between 20 and 35 years, BMI between 18 and 30 kg/m2, normal uterus and patent tubes by hysterosalpingography, normal semen analysis and normal serum prolactin Exclusion criteria: women with endocrinal disturbance, active liver disease, local disease as hydro‐ or pyosalpinx, and history of previous ovarian surgery Number of women randomised: 150 women Number of women analysed: 150 women were analysed, 50 within each group Number of withdrawals/exclusions/loss to follow‐up and reasons: none Number of centres: 2‐centre trial Age (y): group A: 27.5 ± 4.1, group B: 27.2 ± 3.9, group C: 27.5 ± 4.1 BMI (kg/m²): group A: 26.9 ± 1.7, group B: 26.8 ± 1.7, group C: 26.7 ± 1.5 Duration of infertility (y): group A: 1.9 ± 0.7, group B: 1.9 ± 0.7,and group C: 2.2 ± 0.7 Country: Egypt | |
| Interventions | Each of the 3 groups received 2 tablets for 5 days starting from day 3 ‐ day 7 of the cycle Group A: 100 mg (50 mg/tablet) clomiphene citrate Group B: 5 mg (2.5 mg/tablet) letrozole Group C: 40 mg (20 mg/tablet) tamoxifen | |
| Outcomes | Primary outcomes: endometrial thickness and endometrial blood flow (PI and RI) Secondary outcomes: development and number of follicles, and the pregnancy rate | |
| Notes | Ethical approval: the study was approved by the ethical committee of Al Azhar University. Informed consent: not reported Source of funding: authors declare that they have neither conflict of interest nor received financial support. Power calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The patients were prospectively randomised into three groups each containing fifty patients by computer" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | All participants randomised were also analysed |
| Selective reporting (reporting bias) | Unclear risk | We found no study protocol |
| Other bias | Low risk | None |
| Methods | A partly‐randomised controlled clinical trial. Duration and location of the trial: not stated | |
| Participants | Inclusion criteria: infertile women with PCOS, diagnosis based on the 2003 Rotterdam criteria Exclusion criteria: women with ovarian or adnexal surgery, hypothyroidism, hyperprolactinaemia, bilateral tubal occlusion diagnosed with hysterosalpingography and unexplained infertility, and those with follicles greater than 10 mm Number of centres: 1, infertility polyclinic of Atatürk University Medical Faculty Erzurum Number of women randomised: 31 in group A, 33 in group B Number of women analysed: 31 in group A, 33 in group B Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 Age (y): group A letrozole: 25.6 ± 4.5, group B CC: 27.8 ± 6.2 BMI (kg/m²): group A letrozole: 24.7 ± 3.6, group B CC: 24.9 ± 4.8 Duration of infertility (y): group A letrozole: 3.4 ± 3.0, group B CC: 4.4 ± 3.6 Country: Turkey | |
| Interventions | Group A: letrozole, orally given 2.5 mg/day for 5 days during cycle days 3 ‐ 7 Group B: clomiphene citrate, orally given 100 mg/day for 5 days during cycle days 3 ‐ 7 | |
| Outcomes | Primary Outcomes: ovulation rate and pregnancy rate Secondary Outcomes: ovarian hyperstimulation syndrome rate, miscarriage rate, multiple pregnancy rate, number of follicles on day of hCG (≥ 17 mm), E2 (pg/mL) on hCG day, endometrial thickness (mm), other side effects | |
| Notes | Ethical approval: yes, quote: “Ethical approval was obtained from the institutional review board of Atatürk University Medical Faculty in order to conduct this study.” Informed consent: quote: "Instead of written consent verbal approval was obtained from the patients prior to study begin and treatment" ‐ correspondence with Dr. Hakan Nazik Source of funding: quote: "This study was done by researchers without any funding" Power calculation: not stated All questions were answered by Dr. Hakan Nazik | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “The patients were randomly allocated using a computer random list into first and second groups” |
| Allocation concealment (selection bias) | Unclear risk | Quote: “The patients were randomly allocated using a computer random list into first and second groups” |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "There was no blinding in our study" (email with Dr. Hakan Nazik) |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "There was no blinding in our study" (email with Dr. Hakan Nazik) |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts reported |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | High risk | Participants in Group 2 letrozole were significantly younger and had a significantly shorter duration of infertility. |
| Methods | Randomised controlled trial Duration and location of the trial: quote: "The study was conducted in the infertility clinic of a tertiary referral centre (Vali‐E‐asr Hospital–Tehran University of Medical Sciences) as a randomized controlled trial, between March 2009 and February 2010.“ | |
| Participants | Inclusion criteria: women with PCOS with infertility who underwent ovulation induction and timed intercourse for the first time. PCOS was diagnosed by the Rotterdam 2003 criteria. Participants were < 35 years old with at least 1 year of infertility with no other infertility factor. Exclusion criteria: ovarian cysts on cycle day 3 found by transvaginal ultrasound examination. Number of centres: 1, an infertility clinic of a tertiary referral centre Number of women randomised: 80; group A letrozole 5 mg: 40, group B letrozole 7.5 mg: 40 Number of women analysed: group A letrozole 5 mg: 30, group B letrozole 7.5 mg: 37 Number of withdrawals/exclusions/loss to follow‐up and reasons: 4 excluded in group A due to a cyst before treatment, 6 lost to follow‐up in group A and 3 lost to follow‐up in group B Age (y): group A letrozole 5 mg: 28.3 ± 5.0, group B letrozole 7.5 mg: 28.2 ± 4.5 BMI (kg/m²): group A letrozole 5 mg: 25.9 ± 4.2, group B letrozole 7.5 mg: 26.7 ± 3.6 Duration of infertility (y): group A letrozole 5 mg: 3.6 ± 2.3, group B letrozole 7.5 mg: 4.7 ± 3.2 Country: Iran | |
| Interventions | Group A: letrozole orally given, 5 mg/day for 5 days from cycle days 3 ‐ 7 Group B: letrozole orally given, 7.5 mg/day for 5 days from cycle days 3 ‐ 7 | |
| Outcomes | Number and size of follicles and endometrial thickness on days 12 ‐ 14, the number of days to reach mature follicle, day 7 testosterone level, day 21 progesterone level, ovulation rate, pregnancy rate, miscarriage rate, multiple pregnancy rate, ovarian hyperstimulation syndrome rate | |
| Notes | Ethical approval: yes, the hospital research ethics board approved the study. Informed consent: all participants gave informed consent before inclusion in trial. Source of funding: not stated Conflicts of interest: quote: “Conflict of interest: All of the authors do not have any conflict of interest” Power calculation: quote: "Using PASS software and based on two previous studies, a sample size of 30 subjects in each group would provide 80% power to detect a significant difference in the number of mature follicles and duration of stimulation between two groups with a significant level of 0.05." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly allocated using computer‐generated random table into 2 letrozole treatment groups. |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | High risk | 4 participants excluded due to ovarian cyst on day 3 sonography. 9 participants lost to follow‐up, 6 from group A and 3 from group B, without reasons given |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | None |
| Methods | Comparative randomised phase III open‐labelled trial Duration and location of the trial: quote: "A comparative, prospective, phase III, open labelled trial study was conducted in the Eden Hospital, Medical College Kolkata between January 2008 and December 2009.“ | |
| Participants | Inclusion criteria: infertile women aged 20 ‐ 35 with PCOS diagnosis based on the Rotterdam criteria 2003 Exclusion criteria: women with hyperprolactinaemia, thyroid disorder, male‐factor infertility, known or suspicious tubal‐factor infertility (endometriosis and pelvic inflammatory disease). Also women with a history of liver and kidney failure, cardiovascular diseases, diabetes, or women who consumed metformin or drugs affecting insulin secretion or CC in the previous 2 months Number of centres: 1, Eden Hopsital, Mecial College Kolkata Number of women randomised: 147; group A letrozole: 69, group B CC: 78 Number of women analysed: group A letrozole: 69, group B CC: 78 Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 Age (y): group A letrozole: 28 (19 ‐ 35), group B CC: 29 (20 ‐ 35) BMI (kg/m²): group A letrozole: 28.8 (23.2 ‐ 34.6), group B CC: 28.5 (24.2 ‐ 33.6) Duration of infertility (y): group A letrozole: 2.2, group B CC: 2.4 (SD or range not given) Country: India | |
| Interventions | Group A: letrozole, 2.5 mg/day given orally for 5 days from cycle day 3 ‐ 7 Group B: clomiphene citrate, 100 mg/day given orally for 5 days from cycle day 3 ‐ 7 | |
| Outcomes | Primary Outcomes: ovulation rate, average follicular diameter on day 16, number of mature follicles produced by cycle, mean estradiol level on the day of hCG administration, mean endometrial thickness, pregnancy rate Secondary Outcomes: miscarriage rate, live birth rate | |
| Notes | Ethical approval: yes, the study protocol was approved by the ethical committee of Medical College Kolkata Informed consent: yes, participants were counselled and informed consent was obtained before recruitment Source of funding: quote: “Conflict of interest: the authors hereby declare that they have not received any financial support for this study and there is no conflict of interest.” Power calculation: not stated We contacted Dr. Ray by email about randomisation, allocation, blinding, MPR and OHSS, but he did not respond. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear how randomisation was done |
| Allocation concealment (selection bias) | Unclear risk | Unclear how allocation was done |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported if anyone was blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported if anyone was blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | No participants stated as lost, but 147 participants is an odd number to start with, and so are the groups of 69 and 78 respectively; authors contacted for protocol |
| Selective reporting (reporting bias) | Unclear risk | All expected outcomes were reported, but contacted authors for protocol |
| Other bias | Low risk | None |
| Methods | Randomised clinical trial Duration and location of the trial: quote: "This prospective randomized controlled trial was performed at a tertiary care hospital from January 2005 to January 2010.“ | |
| Participants | Inclusion criteria: women aged 20 ‐ 35 years having infertility for > 1 year, BMI < 28, and with anovulatory PCOS based on the Rotterdam 2003 criteria Exclusion criteria: quote: "in all patients, a comprehensive infertility work‐up was done. This included a tubal patency test, pelvic ultrasonography, husband semen analysis, and serum hormone measurements (FSH, LH, prolactin, estradiol, progesterone, and testosterone) on the 2nd to 5th day of the cycle. Patients having abnormality in any of these tests, which may be responsible for reproductive failure, were excluded from the study." Number of centres: 1, a tertiary care hospital in India Number of women randomised: 212 women; group A let: 104, group B CC: 108 Number of women analysed: letrozole group: 98, clomiphene group: 106 Number of withdrawals/exclusions/loss to follow‐up and reasons: 8 lost to follow‐up Age (y): group A letrozole: 26.1 ± 1.8, group B CC: 26.5 ± 1.3 BMI (kg/m²): group A letrozole: 25.8 ± 2.1, group B CC: 25.4 ± 1.6 Duration of infertility (y): group A letrozole: 6.4 ± 3.8, group B CC: 5.8 ± 3.1 Country: India | |
| Interventions | Group A: letrozole, orally given in doses of 2.5 mg/day and 5 mg/day for 5 days during cycle days 3 ‐ 7 Group B: clomiphene citrate, orally given in doses of 50 mg/day and 100 mg/day for 5 days during cycle days 3 ‐ 7 Treatment was continued for 3 months. | |
| Outcomes | The mean number of follicles, endometrial thickness, ovulatory cycle rate, conception rate, pregnancy outcome, miscarriage rate, multiple pregnancies and OHSS rate | |
| Notes | Ethical approval: yes, the necessary ethical approval was taken from Institutional Review Board to conduct this study. Informed consent: yes, the participants were counselled, and informed consent was taken before randomisation. Source of funding: quote: “Source of support: Nil, Conflict of interest: None declared.” Power calculation: quote: "On basis of previous studies, to achieve a statistically valid comparison of pregnancy rates in the two groups, with a type I error of 0.05 and a power of 80%, a sample size of at least 40 women in each arm was required." We contacted Dr. Roy by email to get additional information, but he did not respond. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Online software was used to generate a random number table (www.randomization.com). |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Randomisation codes (A, B) were packed into sealed opaque envelopes by an individual not involved in enrolment, treatment and follow‐up of subjects to ensure concealment of allocation. One resident had the responsibility for dispensing the trial drugs to the patient based on the unique randomisation code. At the end of allocation, the resident provided us with a randomisation list." |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | 8 losses to follow‐up of 112 participants |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | None |
| Methods | Randomised controlled trial Duration and location of the trial: not stated | |
| Participants | Inclusion criteria: diagnosis of PCOS based on Rotterdam criteria provided that anovulation is 1 of the 2 required criteria Exclusion criteria: quote: "exclusion criteria included hyperprolactinaemia, congenital adrenal hyperplasia, thyroid disease, other causes of amenorrhoea such as premature ovarian failure, and clinically suspected Cushing’s syndrome or androgen‐secreting neoplasm. Exclusion criteria also included all women who had received metformin or ovarian drilling in the previous 6 months. Other causes of infertility were excluded by documentation of a normal uterine cavity and at least one patent fallopian tube, and each woman’s current partner had a semen concentration of at least 2 · 107/mL." Number of centres: not reported Number of women randomised: 220; group A letrozole: 110, group B CC: 110 Number of women analysed: group A letrozole: 102, group B CC: 99 Number of withdrawals/exclusions/loss to follow‐up and reasons: quote: "In the letrozole group, eight women were excluded because of missed follow‐up visits (three women), treatment suspension (two women), and homogenous not triple‐line endometrial pattern (three women). In the CC group, 11 women were excluded because of missed follow‐up visits (four women), treatment suspension (two women), and homogenous not triple‐line endometrial pattern (five women)." Age (y): group A letrozole: 26.0 ± 2.7, group B CC: 25.1 ± 3.1 BMI (kg/m²): group A letrozole: 24.4 ± 4.3, group B CC: 23.8 ± 3.7 Duration of infertility (y): group A letrozole: 2.9 ± 0.6, group B CC: 2.6 ± 0.7 Country: Saudi Arabia | |
| Interventions | Group A: 110 participants treated with 5 mg/day of letrozole (Femara; Novartis, Switzerland) in 2 divided doses from cycle day 3 ‐ 7 Group B: 110 participants treated with 100 mg/day of CC (Clomid; Sanofi Aventis, France) in 2 divided doses from cycle day 3 ‐ 7 | |
| Outcomes | quote: "The mean number of follicles, endometrial thickness, the Doppler study of endometrial and sub endometrial vasculatures, ovulation rate, and pregnancy rate were compared in both groups." | |
| Notes | Ethical approval: quote: "approval was obtained from the Institutional Review Board of Jeddah Clinic Hospital, Jeddah, Saudi Arabia." Informed consent: yes, quote: "all participants gave verbal and written informed consent." Source of funding: not stated Conflicts of interest: quote: “No competing financial interests exist.” Power calculation: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly allocated to the letrozole group or CC group by means of a series of blind envelopes numbered from 1 to 220. |
| Allocation concealment (selection bias) | Low risk | Each participant was invited to choose an envelope and was placed by the clinic secretary in either the letrozole group or the CC group. |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "The patients were not blinded about the treating drug in either group." |
| Blinding of outcome assessment (detection bias) | Low risk | To remove any inter‐observational bias, ultrasound on all participants was demonstrated by a single observer (MF Selim) who was blinded to the treating drug. |
| Incomplete outcome data (attrition bias) | Low risk | All dropouts were reported, reasons given. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported. |
| Other bias | Low risk | None |
| Methods | Randomised controlled clinical trial Duration and location of the trial: quote: "This double blind clinical trial study was conducted on 100 PCOS infertile women who have not responded to initial treatment, referring to the Infertility Center of Sanandaj Besat Hospital from June 2014 to December 2015.“ | |
| Participants | Inclusion criteria: PCOS infertile women who have not responded to initial treatment. PCOS was confirmed by Rotterdam criteria (menstrual disturbances: oligomenorrhoea or amenorrhoea, clinical or biochemical hyperandrogenism and sonographic findings of polycystic ovaries). Women with 2 of the 3 PCOS criteria were included in the study. Exclusion criteria: women with hyperprolactinaemia, thyroid problems and anatomical problem in uterus cavity and fallopian tubes confirmed by hysterosalpangiography, sonohysterography or laparoscopy were excluded from the study. Number of women randomised: 100 women, 50 to each group Number of women analysed: 100 women, 50 in each group Number of withdrawals/exclusions/loss to follow‐up and reasons: none Number of centres: single centre Age (y): group A (CC + EV) 30.3 ± 3.1; group B (letrozole) 29.6 ± 5.1 BMI (kg/m²): not reported Duration of infertility (y): group A (CC + EV) 3.4 ± 2.8; group B (letrozole) 3.9 ± 2.4 Country: Iran | |
| Interventions | Group A: 100 mg clomiphene citrate (Iran Hormone Pharmaceutical Company) from day 3 ‐ day 7 of menstruation and 4 mg estradiol valerate (Aburaihan Pharmacy Company) after the 8th day of menstruation until 14th day Group B: 5 mg letrozole (Iran Hormone Pharmaceutical Company) from day 3 ‐ 7 of menstruation with placebo from 8th ‐ 14th day of menstruation | |
| Outcomes | Pregnancy rate, outcome of pregnancy, live birth, miscarriage rate, endometrial thickness | |
| Notes | Ethical approval: quote: "This study was approved by the Ethics Committee of Kurdistan University of Medical Sciences and has been registered in the Iranian Registry of Clinical Trials with registration number IRCT2015052612789N11." Informed consent: quote: "Written consent was taken before the intervention." Source of funding: quote: "Authors would like to thank Vice Chancellor for Research of Kurdistan University of Medical Sciences to support the study financially. " Power calculation: quote: "The sample size was calculated based on previous studies. Considering the mean of endometrial thickness, 5% type I error and 20% type II error, 45 patients were required in each group. To compensate for possible loss and increase the power of the study, 50 patients were studied in each group." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women were block‐randomised and divided in 2 groups |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "To blind the study, transvaginal sonography was performed by a fellow of infertility, the medication was prescribed by a gynaecologist and the patients in group B received placebo." |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: "To blind the study, transvaginal sonography was performed by a fellow of infertility, the medication was prescribed by a gynaecologist and the patients in group B received placebo." |
| Incomplete outcome data (attrition bias) | Low risk | All women randomised were also analysed |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was found |
| Other bias | Low risk | None |
| Methods | Randomised controlled double‐blind trial Duration and location of the trial: not stated | |
| Participants | Inclusion criteria: diagnosis of PCOS based on Rotterdam criteria provided that anovulation is 1 of the 2 required criteria Exclusion criteria: exclusion criteria were BMI > 35, presence of other causes of infertility, > 5 years infertility duration and known poor response to either drugs in previous cycles. Cases found to have baseline ovarian cysts or endometrial pathology were also excluded. Number of centres: 1, an infertility unit of a university hospital Number of women randomised: 124; group A letrozole: 62, group B CC: 62 Number of women analysed: group A letrozole: 59, group B CC: 57 Number of withdrawals/exclusions/loss to follow‐up and reasons: 3 in the letrozole and 5 in the CC group were reported as lost to follow‐up, but no further explanation given Age (y): group A letrozole: 25.0 ± 3.1, group B CC: 25.0 ± 3.6 BMI (kg/m²): group A letrozole: 27.7 ± 3.5, group B CC: 29.2 ± 3.5 Duration of infertility (y): Not reported Country: India | |
| Interventions | Group A: letrozole, 5 mg/day orally given for 5 days, cycle days not given Group B: clomiphene citrate, 100 mg/day orally given for 5 days, cycle days not given | |
| Outcomes | Pregnancy rate, ovulation rate, endometrial thickness (mm), mid‐luteal progesterone level (ng/mL), number of follicles ≥ 12 mm | |
| Notes | Ethical approval: yes, institutional review board (IRB) approval was obtained for the study. Informed consent: yes, informed consent was taken from all included cases Source of funding: not reported, also no conflicts of interest given. Power calculation: not stated We contacted Dr. Sheik‐el‐Arab Elsedeek by email about allocation concealment, blinding of outcome assessors, information on live birth, miscarriage rate, OHSS, multiple pregnancies and funding/COI, but he did not respond. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomised using computer generated tables to undergo one cycle of CC or let induction." |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated if personnel were blinded and how the participants were blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: "Both patients and sonographers were blinded to this allocation." ‐ Unclear if the other outcome assessors were blinded |
| Incomplete outcome data (attrition bias) | Low risk | 8 participants lost to follow‐up, reasons unknown |
| Selective reporting (reporting bias) | Unclear risk | Only pregnancy was reported; we contacted the authors to get study protocol. |
| Other bias | Low risk | None |
| Methods | Randomised controlled clinical trial Duration and location of the trial: quote: "The prospective clinical trial was conducted at Basrah Maternity and Child Hospital, Basrah, Iraq, between January 2012 and April 2013, and comprised women with PCOS and primary infertility.“ | |
| Participants | Inclusion criteria: quote: "Women with PCOS and primary infertility. The subjects were selected from among those who were attending the infertility centre with primary infertility, which was defined as inability of a couple to obtain pregnancy after 1‐2 years of unprotected intercourse. All subjects were diagnosed as having anovulation due to PCOS. PCOS was diagnosed when the ultrasonographic (USG) findings of the ovaries were >10 follicles 2‐8 mm in diameter scattered either around or through an echodense thickened central stroma. In addition, there had to be one or more of the following: oligomenorrhoea, positive progesterone, withdrawal bleeding, hirsutism/acne, obesity, and Luteinizing hormone/Follicle‐stimulating hormone (LH/FSH) ratio >2 or raised circulating androgen, normal thyroid stimulating hormone (TSH). Those included were aged between 18 and 36 years, period of infertility was more than 2 years, serum prolactin level was normal, serum FSH <12u/L, normal thyroid function, and hirsutism, which was diagnosed when the Ferriman and Gallwey score was >8.9 Besides, the male partners had to have a normal seminal analysis by World Health Organisation (WHO) criterion." Exclusion criteria: all women having had patent tubes by either hysterosalpingogram or laparoscopy, history of pelvic surgery with tubal blockage were excluded from the study. Number of women randomised: not stated how many participants were randomised Number of women analysed: 75 women were analysed, 40 in group A, 35 in group B Number of withdrawals/exclusions/loss to follow‐up and reasons: not stated Number of centres: single centre Age (y): group A 25.3 ± 2.1 years, group B 26.1 ± 1.3 years BMI (kg/m²): group A 27.8 ± 1.7, group B 28.1 ± 1.9 Duration of infertility (y): group A 2.3 ± 0.4, group B 2.4 ± 0.6 Country: Iraq | |
| Interventions | Group A: clomiphene citrate for 6 months with a dose between 100 ‐ 200 mg for 5 days beginning on day 3 of the menstrual cycle Group B: letrozole 2.5 ‐ 5 mg daily for 5 days starting from the 3rd day of a spontaneous or progesterone‐induced menstrual bleeding | |
| Outcomes | Pregnancy rate, multiple pregnancies, follicular development,N of follicles, serum E2 on day of HCG, endometrial thickness, ovulation rate | |
| Notes | Ethical approval: approval was obtained from the ethical committee of the College of Medicine, University of Basrah, Iraq. Informed consent: not reported if informed consent was obtained Source of funding: not reported Power calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were randomised into two groups." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported how many women were randomised in first instance |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was found |
| Other bias | Low risk | None |
| Methods | Single‐blinded randomised clinical trial Duration and location of the trial: quote: "In this single‐blind randomized clinical trial, 120 ovarian cycles were studied in 60 clomiphene‐resistant patients with PCOS, who were chosen among 115 PCOS patients attending the infertility clinic of Vali‐e‐Asr Hospital (Tehran, Iran) during the years 2003–2004.“ | |
| Participants | Inclusion criteria: women with PCOS who had failed to become pregnant after 3 courses of 150 mg clomiphene citrate (considered as clomiphene‐resistant), whereas the values of hormonal tests were normal. Tests: thyroid function, prolactin level, hysterosalpingography and husband’s sperm analysis Exclusion criteria: women with a history of liver and kidney failure, cardiovascular disease, diabetes (based on criteria set by the American Diabetic Association) or women who consumed metformin or drugs affecting insulin secretion or clomiphene citrate in the previous 2 months Number of centres: 1, infertility clinic of Vali‐e‐Asr Hospital, Tehran Number of women randomised: 60; group A met‐letrozole: 30, group B met‐CC: 30 Number of women analysed: group A met‐letrozole: 29, group B met‐CC: 30 Number of withdrawals/exclusions/loss to follow‐up and reasons: 1 because she got pregnant after met treatment before letrozole was started Age (y): group A met‐letrozole: 28.2 ± 3.1 , group B met‐CC: 29.6 ± 3.5 BMI (kg/m²): group A met‐letrozole: 30.0 ± 4.8, group B met‐CC: 30.2 ± 3.9 Duration of infertility (y): group A met‐letrozole: 3.8, group B met‐CC: 3.8 Country: Iran | |
| Interventions | Group A: metformin 500 mg x 3/d for 6 ‐ 8 weeks. If pregnancy did not occur, 2.5 mg letrozole from cycle days 3 ‐ 7 was given orally. Group B: metformin 500 mg x 3/d for 6 ‐ 8 weeks. If pregnancy did not occur, 100 mg CC from cycle days 3 ‐ 7 was given orally. Treatment was continued for 2 cycles. | |
| Outcomes | Endometrial thickness on day of hCG administration (cm), N of follicles > 18 mm in diameter, Mean total estradiol level on day of hCG administration (pM/L), mean estradiol level by mature follicle (pM/l), regular menses after metformin, adverse effects of metformin, live birth rate, pregnancy rate, miscarriage rate | |
| Notes | Ethical approval: yes, consent from the deputy of research and the medical ethics committee of Tehran University of Medical Sciences Informed consent: not obtained because quote: “it was the routine treatment protocol and it was just put in the frame of a structured study” (email with Dr Farnaz Sohrabvand) Source of funding: quote: "No funding was necessary" (email with Dr Farnaz Sohrabvand) Power calculation: not stated Authors were contacted about live birth, multiple pregnancies, OHSS per woman randomised, informed consent, funding. No data available on live birth, multiple pregnancies and OHSS. Information retrieved about informed consent and funding (email with Dr Farnaz Sohrabvand) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A series of blind envelopes numbered from 1 to 60 had been prepared. Each patient was invited to pull out an envelope and was placed by the clinic secretary in either the metformin‐letrozole group (number 1‐30) or in the metformin‐CC group (31‐60)." |
| Allocation concealment (selection bias) | Unclear risk | Quote: "A series of blind envelopes numbered from 1 to 60 had been prepared. Each patient was invited to pull out an envelope and was placed by the clinic secretary in either the metformin‐letrozole group (number 1‐30) or in the metformin‐CC group (31‐60)." |
| Blinding of participants and personnel (performance bias) | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) | High risk | It is not plausible that outcome assessors were blinded if participants were not |
| Incomplete outcome data (attrition bias) | Low risk | One participant was excluded due to pregnancy after start of metformin treatment |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Low risk | None |
| Methods | Randomised clinical trial Duration of the trial: quote: "The trial was started on October 2009. Owing to the expiration of the study drug (berberine and matching placebo), the data safety and monitoring board decided to stop enrollment in November 2013“ | |
| Participants | Inclusion criteria: quote: "Chinese women with PCOS attempting to get pregnant were eligible if they fulfilled the following criteria: 1) age 20–40 years; 2) diagnosis of PCOS according to two of the three Rotterdam 2003 criteria, including oligo‐ovulation or anovulation, clinical and/or biochemical signs of hyperandrogenism, and/or polycystic ovaries; 3) at least one open fallopian tube and normal uterine cavity documented by hysterosalpingography, sonohysterography, or diagnostic laparoscopy within the past 3 years; 4) a male partner with sperm concentration of 15 million/mL and motility of 40% in at least one ejaculate; and 5) at least 1 year of infertility." Exclusion criteria: quote: "Subjects were excluded if they used hormonal drugs or other medications, including Chinese herbal prescriptions, in the past 3 months; had known severe organ dysfunction or mental illness; were pregnant, post‐miscarriage, postpartum, or breastfeeding within the past 6 weeks; or had congenital adrenal hyperplasia, clinically suspected Cushing syndrome, or an androgen‐secreting neoplasm." Number of women randomised: 644 women Number of women analysed: 644 women were analysed, 215 in group A, 214 in group B, 215 in group C. Number of withdrawals/exclusions/loss to follow‐up and reasons: 16/215 (7.4%) in the letrozole group, 25/214 (11.7%) in the berberine group, and 15/215 (7.0%) in the combination group (P = 0.16). Reasons for withdrawal were similar among the 3 groups (P = 0.16 for the 3 groups; P = 0.19 for lost to follow‐up; P = 0.88 for dropout; P = 1.0 for protocol violations; and P = 0.33 for adverse events). Number of centres: multicentre trial, 19 hospitals Age (y): group A 27.8 ± 3.6; group B 27.8 ± 3.7; group C 27.8 ± 3.6 BMI (kg/m²): group A 24.8 ± 4.5; group B 24.5 ± 4.1; group C 25.1 ± 5.0 Duration of infertility (months): group A 32.7 ± 24.0; group B 28.5 ± 21.6; group C 29.8 ± 21.3 Country: China | |
| Interventions | Group A: 2.5 mg (1 tablet) of letrozole on days 3 – 7 of the first 3 treatment cycles. This dose was increased to 5 mg letrozole (2 tablets) or 2 tablets of letrozole placebo on days 3 – 7 of the last 3 treatment cycles if not pregnant Group B: berberine was administered orally at a daily dose of 1.5 g for 6 months. Group C: letrozole and berberine were administered in the same doses as reported above. | |
| Outcomes | Cumulative live births, ovulation rate, conception rate, clinical pregnancy rate, multiple pregnancy rate, abortion rate, pregnancy complications, adverse events from study medications | |
| Notes | Ethical approval: the Institutional Review Boards at participating hospitals approved the protocol. Informed consent: every participant gave written informed consent. Source of funding: supported by National Public Welfare Projects for Chinese Medicine (200807021) of China, National Key Discipline of Chinese Medicine in Gynecolog, 2009–14, Heilongjiang Province Foundation for Outstanding Youths (JC200804), Intervention for Polycystic Ovary Syndrome Based on Traditional Chinese Medicine Theory–‘‘TianGui Shi Xu’’ (2011TD006), and National Clinical Research Base in Chinese Medicine, 2009–14, at First Affiliated Hospital, Heilongjiang University of Chinese Medicine. The funding sources had no involvement in the study design, the collection, analysis, and interpretation of data, the writing of the report, or in the decision to submit the article for publication. Power calculation: the sample size calculation was based on anticipated live birth rate. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomisation was performed through a web‐based computer program (http://210.76.97.192:8080/cjbyj) operated by an independent data coordinating centre, the Institute of Basic Clinical Medicine of the China Academy of Chinese Medical Sciences. The randomisation was stratified by the participating sites." |
| Allocation concealment (selection bias) | Low risk | Randomisation was operated by an independent data co‐ordinating centre |
| Blinding of participants and personnel (performance bias) | Low risk | Participants, investigators, physicians taking care of the participants, laboratory technicians, and data analysers were blinded to the assignments. |
| Blinding of outcome assessment (detection bias) | Low risk | Participants, investigators, physicians taking care of the participants, laboratory technicians, and data analysers were blinded to the assignments. |
| Incomplete outcome data (attrition bias) | Low risk | 7% – 12% were lost to follow‐up, had protocol violations or adverse events. ITT analysis was performed. |
| Selective reporting (reporting bias) | Low risk | None, study protocol was published prior to participant enrolment in the study |
| Other bias | Low risk | None |
| Methods | Randomised controlled clinical trial Duration of the trial: quote: "They underwent intra uterine insemination (IUI) between August 2011 and December 2012.“ | |
| Participants | Inclusion criteria: quote: "patients with CC‐resistant PCOS. According to Rotterdam criteria, patients with at least 2 out of 3 of below criteria were included as a PCOS: 1‐ Chronic anovulation, 2‐ Clinical and/or biochemical evidence of hyperandrogenism and 3‐ polycystic appearance of ovaries in Transvaginal Ultrasound (TVS) Moreover, infertility was defined as failure to conceive despite having unprotected and frequent intercourse for at least 1 year. CC‐resistance was considered as absence of ultrasound evidence regarding ovarian response consumption of 150mg of CC between the 5th and the 9th day of menstruation cycle for three consecutive cycles. All participants had a documented normal blood test, renal function test, liver function test, hysterosalpingography (HSG) and negative pregnancy test before the study. The partners should have at least two semen analyses. According to WHO, a normal semen analysis should have these properties: Sperm concentration ≥15 million/ml, total sperm count ≥39 million, mobility rate >40%, progressive motility ≥32% and normal morphology ≥ 4% ." Exclusion criteria: women with breast cancer, renal and liver diseases, autoimmune problems and endocrinological problems such as diabetes, hyperprolactinaemia, thyroid diseases, Cushing’s syndrome and smokers were excluded from the study. Number of women randomised: 140 women Number of women analysed: 131 women were analysed, 67 patients in control group and 64 cases in letrozole group. Number of withdrawals/exclusions/loss to follow‐up and reasons: quote: "during this study, we eliminated 6 patients from the control group, 4 fell out of the study and 2 were finally diagnosed for OHSS. Three patients were also eliminated from the letrozole group; one fell out of the study protocol and 2 due to OHSS." Number of centres: single‐centre trial Age (y): aged 18 ‐ 35: control group: 27.7 ± 1.8, letrozole group: 27.9 ± 1.9 BMI (kg/m²): control group: 25.6 ± 3.2, letrozole group: 25.1 ± 4.4 Duration of infertility (y): control group: 5.4 ± 1.9 , letrozole group: 5.0 ± 3.0 Country: Shiraz, Iran | |
| Interventions | Group A: control group. 75 IU/day highly purified recombinant FSH (Gonal‐f, Serono, Hellas, Puregon, Greece) intramuscularly, from the 3rd day through the day of HCG injection Group B: letrozole group additionally received 5 mg/day letrozole (Razak Drug Laboratory, Tehran, Iran) since the 8th day of cycle up to the day of HCG injection. | |
| Outcomes | Premature LH surge, pregnancy rate, abortion rate, ongoing pregnancy rate, N of follicles > 18 mm, endometrial thickness (mm) | |
| Notes | Ethical approval: not reported Informed consent: not reported Source of funding: not reported. Power calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | quote: "In this study, 140 cases with PCOS resistant to CC were enrolled and divided into two groups of control (n=70) and letrozole (n=70)." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "During this study, we eliminated 6 patients from the control group, 4 fell out of the study and 2 were finally diagnosed for OHSS. Three patients were also eliminated from the letrozole group; one fell out of the study protocol and 2 due to OHSS. Thus, 67 patients (age ranges 18‐39 years) remained in control group and 64 cases (age ranges 21‐37 years) remained in letrozole group." |
| Selective reporting (reporting bias) | Unclear risk | Unclear; Quote: "This trial was registered in Islamic Republic Clinical Trials Database (IRCT2014010615102N2)." We were unable to find the protocol, because the given trial registry number leads to a study protocol for pain medication after rhinoplastic surgery. |
| Other bias | High risk | Methods not very well described, Clinical trial registration number leads to wrong trial. |
| Methods | Randomised controlled trial Duration and location of the trial: quote: "This clinical trial was performed on 107 infertile patients with PCOS who were referred to Fatemeh Zahra Infertility Center, Babol, Iran, in 2006 and 2007.“ | |
| Participants | Inclusion criteria: women with primary infertility, documented PCOS, age < 35 years, < 5 years infertility and BMI between 19 and 26. PCOS was defined on the basis of ultrasonography findings, oligomenorrhoea and an increased luteinising hormone (LH)/follicle‐stimulating hormone (FSH) ratio (> 3). Exclusion criteria: moderate or severe case of OHSS during trial, infertility resulting from male factors, tubular factors and endometriosis. Number of centres: 1, Fatemeh Zahra Infertility Center, Babol Number of women randomised: 107; group A letrozole: 50, group B CC: 57 Number of women analysed: 107; group A letrozole: 50, group B CC: 57 Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 Age (y): group A letrozole: 23.8 ± 3.6, group B CC: 23.1 ± 3.6 BMI (kg/m²): not reported Duration of infertility (y): group A letrozole: 2.4 ± 1, group B CC: 2.6 ± 1.2 Country: Iran | |
| Interventions | Group A: 5 mg letrozole from cycle days 3 ‐ 7 was given orally. Group B: 100 mg CC from cycle days 3 ‐ 7 was given orally. | |
| Outcomes | Ovulation rate, pregnancy rate, number of follicles > 17mm, OHSS rate, multiple pregnancy rate, endometrial thickness. | |
| Notes | Ethical approval: yes, "The study protocol was approved by the ethics committee of Babol Medical University." Informed consent: yes, "All the patients signed a written consent form as to be enrolled in the study" Source of funding: no, but "Financial disclosure: The authors have no connection to any companies or products mentioned in this article” Power calculation: not stated We contacted authors for additional information, but they did not respond. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The participants were assigned to two groups using systematic randomisation method" |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts reported |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | Low risk | None |
BMI: body mass index; CC: clomiphene citrate; FSH: follicle‐stimulating hormone; hCG: human chorionic gonadotropin; hMG: human menopausal gonadotropin; LH: luteinising hormone; LOD: laparoscopic ovarian drilling; OHSS: ovarian hyperstimulation syndrome; PCOS: polycystic ovary syndrome; s: seconds; SD: standard deviation; TSH: thyroid‐stimulating hormone; W: watts; y: year
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| No PCOS | |
| Only short conference abstract; we did not find a published study article. We were unable to retrieve any information from study authors. | |
| Not a RCT | |
| RCT, but not about women with PCOS | |
| Not a RCT | |
| Not a RCT | |
| No PCOS | |
| Not a RCT | |
| Quasi‐randomised trial (quote: "Based on attendance order, patients with odd numbers were given letrozole and those with even numbers were given CC") | |
| Quasi‐randomised trial | |
| Not randomised for clomiphene or letrozole | |
| Not a RCT, no PCOS | |
| Not randomised for letrozole | |
| Not a RCT | |
| Suspected quasi‐randomisation based on attendance order | |
| No published data found, last updated on clinicaltrials.gov in 2008. No response from study authors. | |
| Not a RCT | |
| For the 2018 update, there was no update on clinicaltrials.gov. No study data available, and no response from authors. | |
| No study results found, unable to obtain more information from study authors | |
| Study should be finished. We contacted authors by email found through Google because no contact information was written in the study protocol: [email protected]. For the 2018 update, there was no update on clinicaltrials.gov and still no response from the author. | |
| Unable to obtain information from study authors. No study data found, no update on clinicaltrials.gov. | |
| RCT, but not about women with PCOS | |
| Not randomised for letrozole | |
| Women with PCOS were excluded from the study | |
| Women with PCOS were excluded from the study | |
| Not randomised for letrozole | |
| Only conference abstract available, full article could not be found. Contact address of authors unknown | |
| Not a RCT | |
| Not a RCT (Quote: "the allocation depended on the patients' choice" ‐ translated by Prof Taixiang Wu) | |
| Not a RCT |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Randomised clinical study |
| Participants | 15 infertile women with polycystic ovarian syndrome |
| Interventions | Women were randomised into 3 treatment groups: In group 1, continuous metformin was used at the dose of 850 mg/tid/day for 6 months; afterwards, daily 2.5 mg letrozole between 3 and 7 days of the menstrual cycle was added to the metformin therapy. Group 2 participants received only daily 2.5 mg letrozole between days 3 and 7 of the menstrual cycle. Group 3 participants received daily 100 mg clomiphene citrate only between days 3 and 7 of the menstrual cycle. |
| Outcomes | Unclear |
| Notes | The article was written in Turkish, and we were not able to have it translated properly. |
| Methods | Randomised clinical trial |
| Participants | 100 infertile women with PCOS referred to Asali Hospital and private clinic in 2008 |
| Interventions | The women were randomised into 2 groups of 50 that were treated with 5 mg letrozole or 100 mg clomiphene citrate from day 3 to 7 of the menstrual cycle. |
| Outcomes | Outcomes: Pregnancy rate |
| Notes | The article was written in Persian, but we were not able to have it translated properly. |
| Methods | Randomised controlled trial |
| Participants | 110 infertile women diagnosed as polycystic ovary syndrome (PCOS) aged 20 ‐ 35 distributed randomly |
| Interventions | 55 women will receive letrozole 2.5 mg twice daily orally from the 2nd to the 6th day of the cycle for 3 successive cycles. 55 women will receive clomiphene citrate 50 mg twice daily orally from the 2nd to the 6th day of the cycle for 3 successive cycles. |
| Outcomes |
|
| Notes | We found no study data, although trial completed since 2016 on clinicaltrials.gov |
| Methods | Double‐blind randomised clinical trial |
| Participants | 59 infertile women who had the inclusion criteria for PCOS were evaluated in the Infertility Clinic of Shariati Hospital in Tehran, Iran in 2010 ‐ 2011. |
| Interventions | The participants were assigned to 2 letrozole and 1 letrozole‐plus‐HMG groups. |
| Outcomes | Reported no outcomes of interest to our review |
| Notes | The article was written in Persian, but we were not able to have it translated properly. |
| Methods | Randomised clinical trial, "Quote: The cases were assigned to two groups through simple random sampling" |
| Participants | 100 infertile, 20 ‐ 35‐year‐old women with PCOS attending Vali‐e‐Asr Infertility Clinic from April 2003 to April 2007 |
| Interventions | Group A received clomiphene citrate plus HMG, Group B received letrozole plus HMG |
| Outcomes | Outcomes: pregnancy, miscarriage and multiple pregnancy rates |
| Notes | The article was written in Persian, but we were not able to have it translated properly. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Letrozole versus laparoscopic ovarian drilling in polycystic ovary syndrome |
| Methods | Randomised, open‐label, clinical trial |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | Group A: letrozole 2.5 mg Group B: laparoscopic ovarian drilling |
| Outcomes | Ovulation rate |
| Starting date | January 2017 |
| Contact information | Responsible party: Ahmed Mohamed Abbas, Assiut University |
| Notes | Estimated primary completion date: December 2018 |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Live birth rate Show forest plot | 1 | 36 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.17 [0.12, 83.17] |
| Analysis 1.1  Comparison 1 Letrozole compared to placebo, Outcome 1 Live birth rate. | ||||
| 2 Ovarian hyperstimulation syndrome rate Show forest plot | 2 | 167 | Risk Difference (M‐H, Fixed, 95% CI) | 0.00 [‐0.05, 0.05] |
| Analysis 1.2 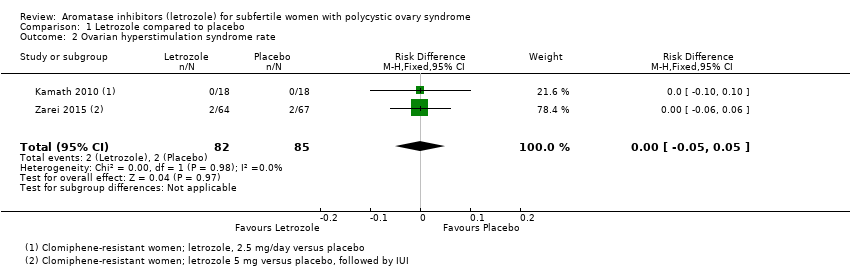 Comparison 1 Letrozole compared to placebo, Outcome 2 Ovarian hyperstimulation syndrome rate. | ||||
| 3 Clinical pregnancy rate Show forest plot | 2 | 167 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.88 [1.08, 7.66] |
| Analysis 1.3 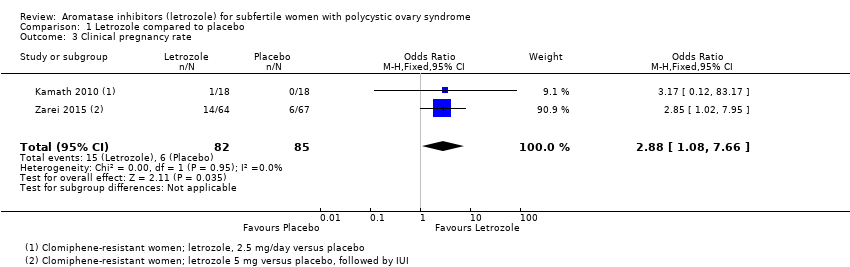 Comparison 1 Letrozole compared to placebo, Outcome 3 Clinical pregnancy rate. | ||||
| 4 Miscarriage rate by woman randomised Show forest plot | 2 | 167 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.60 [0.26, 9.89] |
| Analysis 1.4  Comparison 1 Letrozole compared to placebo, Outcome 4 Miscarriage rate by woman randomised. | ||||
| 5 Miscarriage rate by pregnancies Show forest plot | 1 | 20 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.07, 4.56] |
| Analysis 1.5 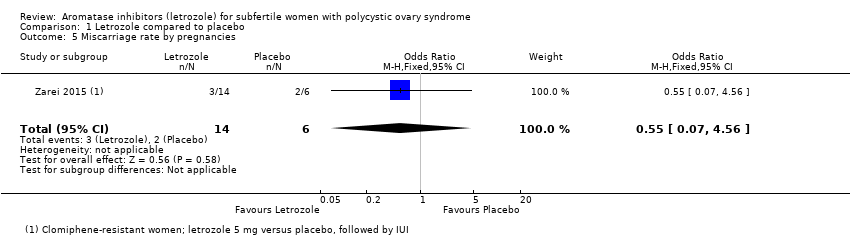 Comparison 1 Letrozole compared to placebo, Outcome 5 Miscarriage rate by pregnancies. | ||||
| 6 Multiple pregnancy rate Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.6  Comparison 1 Letrozole compared to placebo, Outcome 6 Multiple pregnancy rate. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Live birth rate Show forest plot | 13 | 2954 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.68 [1.42, 1.99] |
| Analysis 2.1 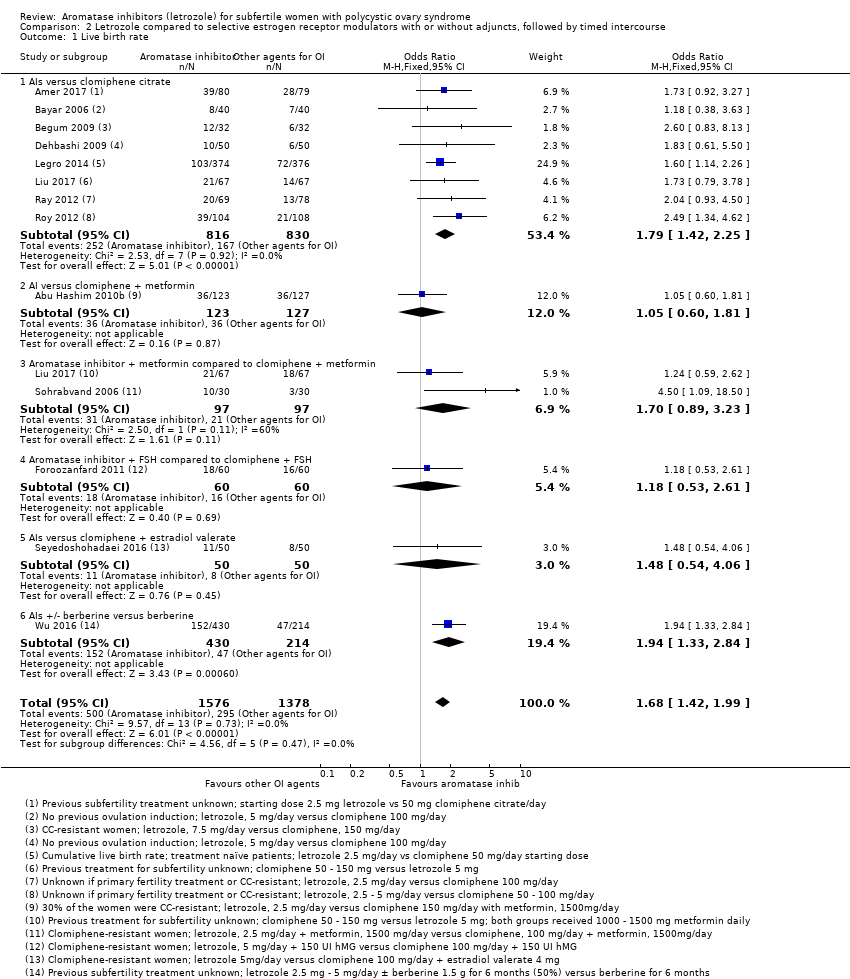 Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 1 Live birth rate. | ||||
| 1.1 AIs versus clomiphene citrate | 8 | 1646 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [1.42, 2.25] |
| 1.2 AI versus clomiphene + metformin | 1 | 250 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.60, 1.81] |
| 1.3 Aromatase inhibitor + metformin compared to clomiphene + metformin | 2 | 194 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.70 [0.89, 3.23] |
| 1.4 Aromatase inhibitor + FSH compared to clomiphene + FSH | 1 | 120 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.53, 2.61] |
| 1.5 AIs versus clomiphene + estradiol valerate | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.54, 4.06] |
| 1.6 AIs +/‐ berberine versus berberine | 1 | 644 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.94 [1.33, 2.84] |
| 2 Live birth rate by BMI Show forest plot | 11 | 2774 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.69 [1.42, 2.02] |
| Analysis 2.2 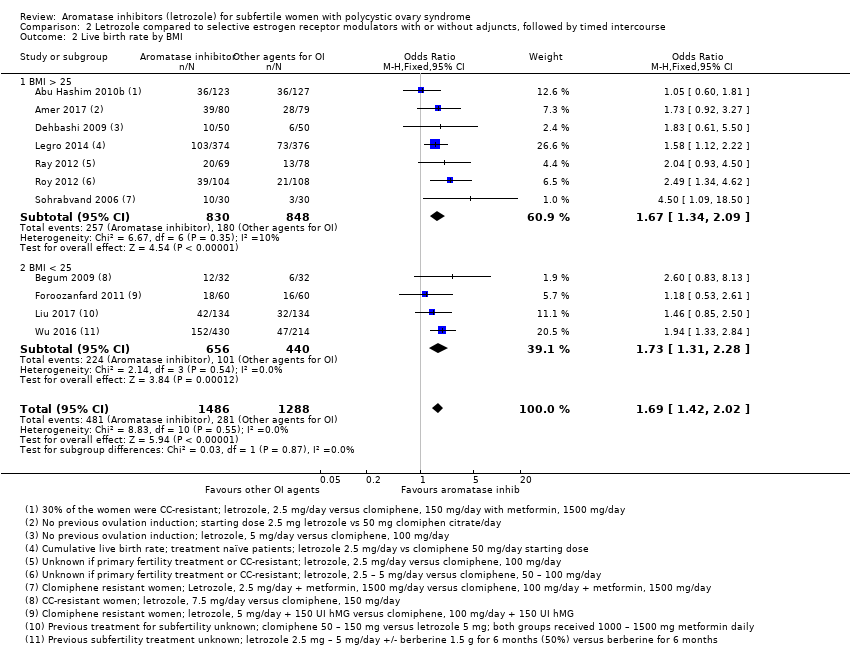 Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 2 Live birth rate by BMI. | ||||
| 2.1 BMI > 25 | 7 | 1678 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.67 [1.34, 2.09] |
| 2.2 BMI < 25 | 4 | 1096 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.73 [1.31, 2.28] |
| 3 Live birth rate by first‐ or second‐line treatment Show forest plot | 13 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.3 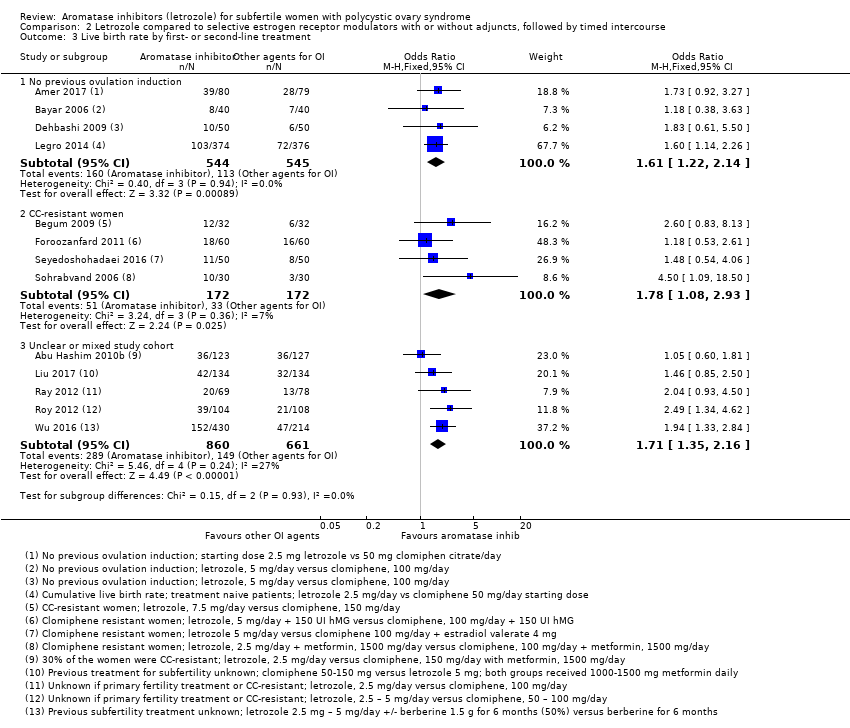 Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 3 Live birth rate by first‐ or second‐line treatment. | ||||
| 3.1 No previous ovulation induction | 4 | 1089 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.61 [1.22, 2.14] |
| 3.2 CC‐resistant women | 4 | 344 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.78 [1.08, 2.93] |
| 3.3 Unclear or mixed study cohort | 5 | 1521 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.71 [1.35, 2.16] |
| 4 Impact of allocation bias for live birth rate Show forest plot | 13 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.4 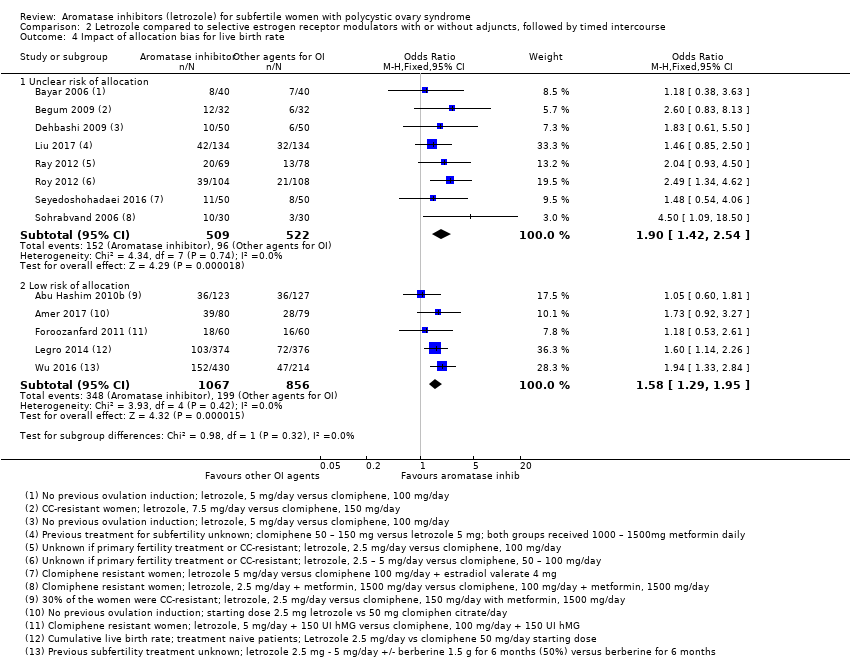 Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 4 Impact of allocation bias for live birth rate. | ||||
| 4.1 Unclear risk of allocation | 8 | 1031 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.90 [1.42, 2.54] |
| 4.2 Low risk of allocation | 5 | 1923 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.58 [1.29, 1.95] |
| 5 Impact of detection bias for live birth rate Show forest plot | 13 | 2954 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.68 [1.42, 1.99] |
| Analysis 2.5 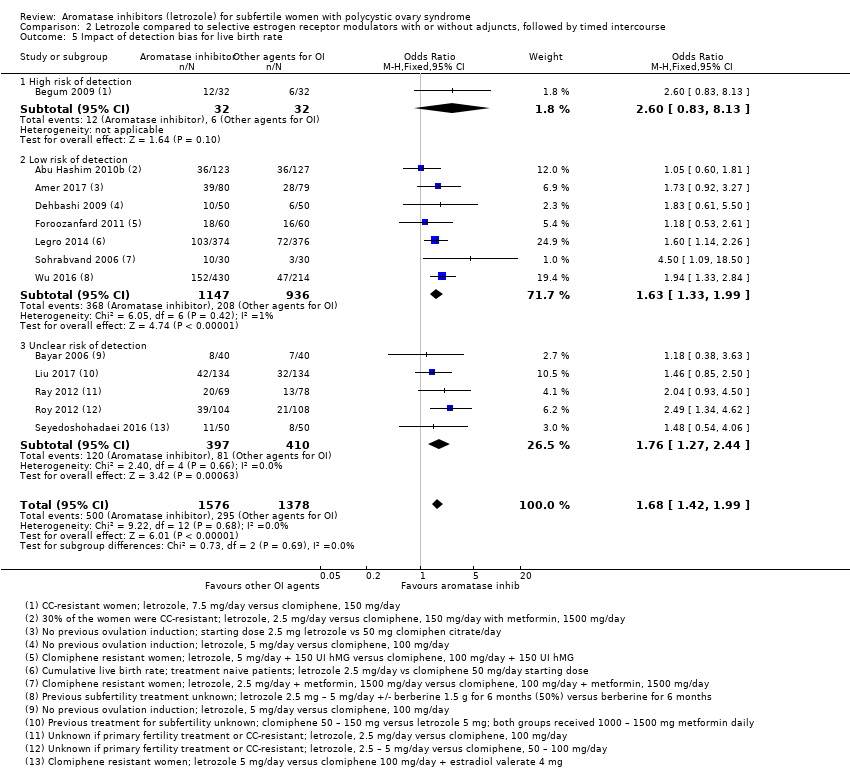 Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 5 Impact of detection bias for live birth rate. | ||||
| 5.1 High risk of detection | 1 | 64 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.6 [0.83, 8.13] |
| 5.2 Low risk of detection | 7 | 2083 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.63 [1.33, 1.99] |
| 5.3 Unclear risk of detection | 5 | 807 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.76 [1.27, 2.44] |
| 6 Impact of attrition bias for live birth rate Show forest plot | 13 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.6  Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 6 Impact of attrition bias for live birth rate. | ||||
| 6.1 Unclear risk of attrition | 1 | 147 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.04 [0.93, 4.50] |
| 6.2 Low risk of attrition | 11 | 2539 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.69 [1.41, 2.03] |
| 6.3 High risk of attrition | 1 | 268 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.46 [0.85, 2.50] |
| 7 Ovarian hyperstimulation syndrome rate Show forest plot | 12 | 2536 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.00 [‐0.01, 0.00] |
| Analysis 2.7  Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 7 Ovarian hyperstimulation syndrome rate. | ||||
| 7.1 AIs versus clomiphene citrate | 9 | 2010 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.00 [‐0.01, 0.00] |
| 7.2 AI versus clomiphene + metformin | 1 | 250 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 7.3 Aromatase inhibitor + hMG versus clomiphene + hMG | 2 | 276 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.04, 0.04] |
| 8 Ovarian hyperstimulation syndrome rate per BMI Show forest plot | 11 | Risk Difference (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.8  Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 8 Ovarian hyperstimulation syndrome rate per BMI. | ||||
| 8.1 BMI > 25 | 6 | 1851 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.00 [‐0.01, 0.00] |
| 8.2 BMI < 25 | 5 | 605 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 9 Clinical pregnancy rate Show forest plot | 25 | 4629 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.56 [1.37, 1.78] |
| Analysis 2.9  Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 9 Clinical pregnancy rate. | ||||
| 9.1 AIs versus clomiphene citrate | 17 | 2930 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.50 [1.28, 1.76] |
| 9.2 AI versus clomiphene + metformin | 1 | 250 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.60, 1.71] |
| 9.3 Aromatase inhibitor + metformin versus clomiphene + metformin | 3 | 294 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.86 [1.05, 3.29] |
| 9.4 Aromatase inhibitor + hMG versus clomiphene + hMG | 2 | 276 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.82, 2.27] |
| 9.5 AIs versus tamoxifen | 2 | 135 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.58 [0.64, 3.90] |
| 9.6 AIs versus clomiphene + estradiol valerate | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.47 [0.94, 6.46] |
| 9.7 AIs ± berberine versus berberine | 1 | 644 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.15 [1.48, 3.13] |
| 10 Impact of allocation bias for clinical pregnancy rate Show forest plot | 23 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.10 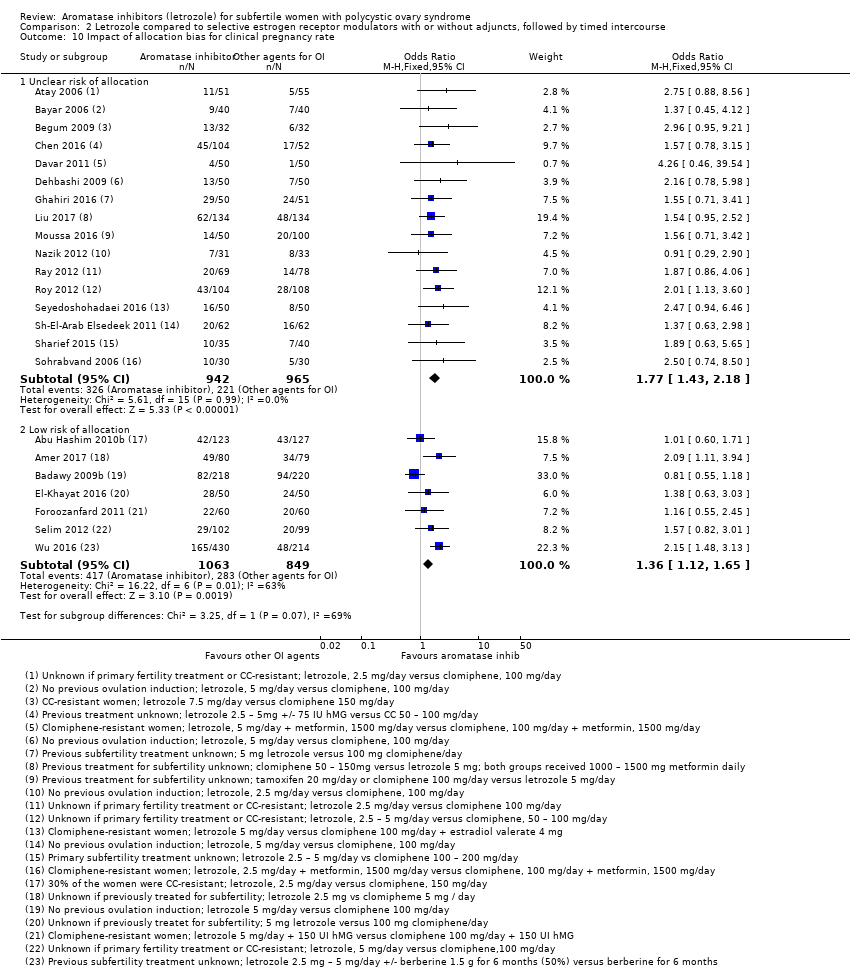 Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 10 Impact of allocation bias for clinical pregnancy rate. | ||||
| 10.1 Unclear risk of allocation | 16 | 1907 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.77 [1.43, 2.18] |
| 10.2 Low risk of allocation | 7 | 1912 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.36 [1.12, 1.65] |
| 11 Miscarriage rate by woman randomised Show forest plot | 18 | 3754 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.39 [1.07, 1.81] |
| Analysis 2.11  Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 11 Miscarriage rate by woman randomised. | ||||
| 11.1 AIs versus clomiphene citrate | 11 | 2190 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.97, 1.93] |
| 11.2 AI versus clomiphene + metformin | 1 | 250 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.25, 4.23] |
| 11.3 Aromatase inhibitor + metformin versus clomiphene + metformin | 3 | 294 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.52, 2.82] |
| 11.4 Aromatase inhibitor + hMG versus clomiphene + hMG | 2 | 276 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.31, 2.27] |
| 11.5 AIs versus clomiphene + estradiol valerate | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 12.21 [0.66, 226.97] |
| 11.6 AIs +/‐ berberine versus berberine | 1 | 644 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.63 [0.87, 3.04] |
| 12 Miscarriage rate by pregnancies Show forest plot | 18 | 1210 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.70, 1.26] |
| Analysis 2.12  Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 12 Miscarriage rate by pregnancies. | ||||
| 12.1 AIs versus clomiphene citrate | 11 | 705 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.65, 1.42] |
| 12.2 AI versus clomiphene + metformin | 1 | 85 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.24, 4.40] |
| 12.3 Aromatase inhibitor + metformin versus clomiphene + metformin | 3 | 79 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.32, 2.02] |
| 12.4 Aromatase inhibitor + hMG versus clomiphene + hMG | 2 | 104 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.23, 1.96] |
| 12.5 AIs versus clomiphene + estradiol valerate | 1 | 24 | Odds Ratio (M‐H, Fixed, 95% CI) | 8.13 [0.39, 167.90] |
| 12.6 AIs +/‐ berberine versus berberine | 1 | 213 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.43, 1.80] |
| 13 Multiple pregnancy rate Show forest plot | 17 | 3579 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.41, 1.16] |
| Analysis 2.13  Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 13 Multiple pregnancy rate. | ||||
| 13.1 AIs versus clomiphene citrate | 13 | 2409 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.32, 1.16] |
| 13.2 AI versus clomiphene + metformin | 1 | 250 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.82] |
| 13.3 Aromatase inhibitor + hMG versus clomiphene + hMG | 2 | 276 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.29, 3.05] |
| 13.4 AIs +/‐ berberine versus berberine | 1 | 644 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.53 [0.24, 84.46] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Ovarian hyperstimulation syndrome rate Show forest plot | 2 | 1494 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.00 [‐0.01, 0.00] |
| Analysis 3.1  Comparison 3 Letrozole compared to clomiphene citrate, followed by IUI, Outcome 1 Ovarian hyperstimulation syndrome rate. | ||||
| 1.1 AI versus Clomiphene | 1 | 107 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.02 [‐0.07, 0.03] |
| 1.2 AI versus Clomiphene +rFSH and rFSH only | 1 | 1387 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.00 [‐0.01, 0.00] |
| 2 Clinical pregnancy rate Show forest plot | 3 | 1597 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.71 [1.30, 2.25] |
| Analysis 3.2  Comparison 3 Letrozole compared to clomiphene citrate, followed by IUI, Outcome 2 Clinical pregnancy rate. | ||||
| 2.1 AI versus Clomiphene | 2 | 210 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.09 [0.97, 4.53] |
| 2.2 AI versus Clomiphene +rFSH and rFSH only | 1 | 1387 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.66 [1.23, 2.22] |
| 3 Miscarriage rate by woman randomised Show forest plot | 2 | 1490 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.62, 2.40] |
| Analysis 3.3 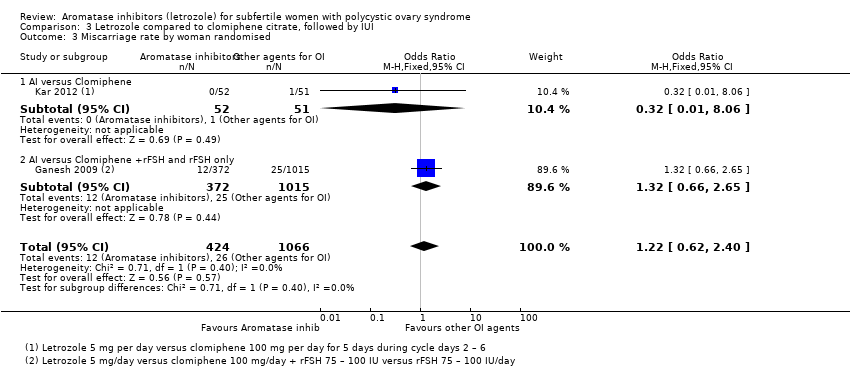 Comparison 3 Letrozole compared to clomiphene citrate, followed by IUI, Outcome 3 Miscarriage rate by woman randomised. | ||||
| 3.1 AI versus Clomiphene | 1 | 103 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.06] |
| 3.2 AI versus Clomiphene +rFSH and rFSH only | 1 | 1387 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.66, 2.65] |
| 4 Miscarriage rate by pregnancies Show forest plot | 2 | 260 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.37, 1.57] |
| Analysis 3.4  Comparison 3 Letrozole compared to clomiphene citrate, followed by IUI, Outcome 4 Miscarriage rate by pregnancies. | ||||
| 4.1 AI versus Clomiphene | 1 | 15 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.00, 3.09] |
| 4.2 AI versus Clomiphene +rFSH and rFSH only | 1 | 245 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.40, 1.79] |
| 5 Multiple pregnancy rate Show forest plot | 3 | 1597 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.49, 2.13] |
| Analysis 3.5 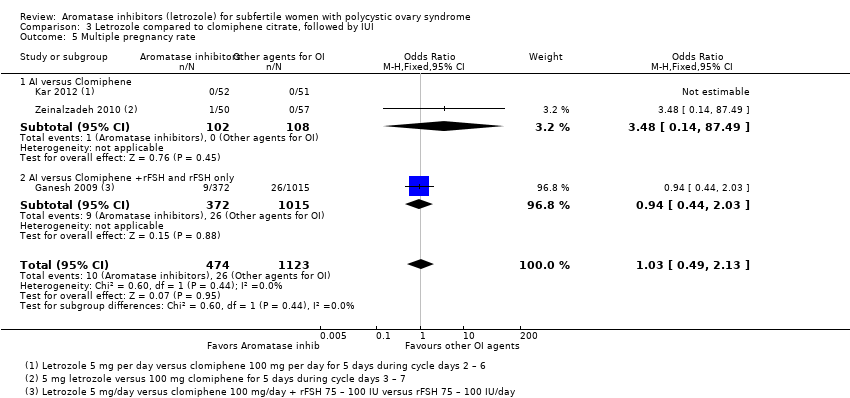 Comparison 3 Letrozole compared to clomiphene citrate, followed by IUI, Outcome 5 Multiple pregnancy rate. | ||||
| 5.1 AI versus Clomiphene | 2 | 210 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.48 [0.14, 87.49] |
| 5.2 AI versus Clomiphene +rFSH and rFSH only | 1 | 1387 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.44, 2.03] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Live birth rate Show forest plot | 3 | 548 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.38 [0.95, 2.02] |
| Analysis 4.1 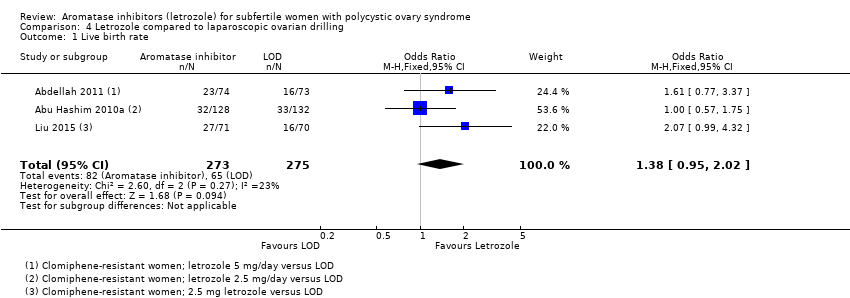 Comparison 4 Letrozole compared to laparoscopic ovarian drilling, Outcome 1 Live birth rate. | ||||
| 2 Ovarian hyperstimulation syndrome rate Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.2  Comparison 4 Letrozole compared to laparoscopic ovarian drilling, Outcome 2 Ovarian hyperstimulation syndrome rate. | ||||
| 3 Clinical pregnancy rate Show forest plot | 5 | 774 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.94, 1.74] |
| Analysis 4.3 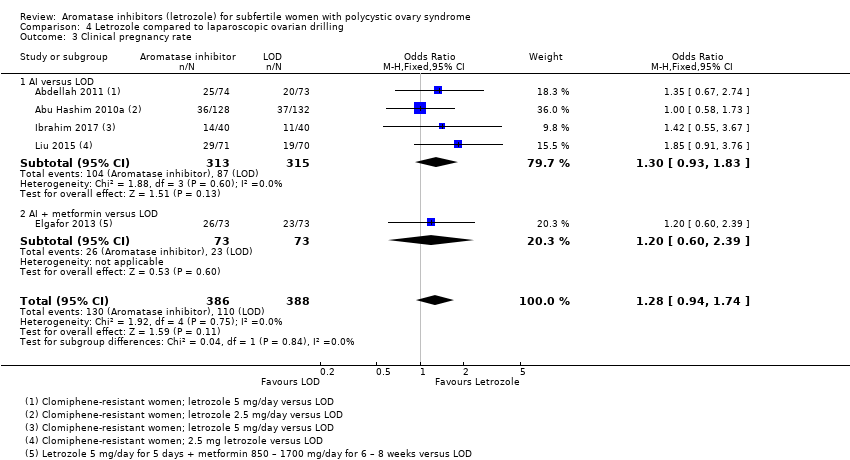 Comparison 4 Letrozole compared to laparoscopic ovarian drilling, Outcome 3 Clinical pregnancy rate. | ||||
| 3.1 AI versus LOD | 4 | 628 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.93, 1.83] |
| 3.2 AI + metformin versus LOD | 1 | 146 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.60, 2.39] |
| 4 Miscarriage rate by woman randomised Show forest plot | 5 | 774 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.38, 1.70] |
| Analysis 4.4 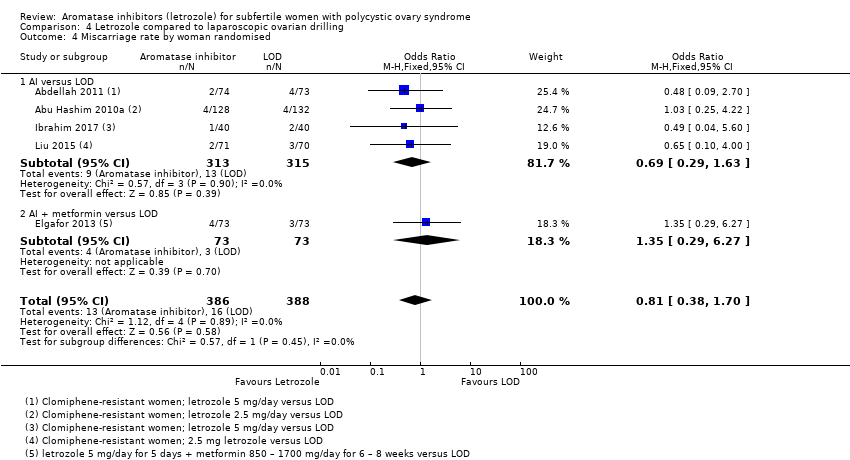 Comparison 4 Letrozole compared to laparoscopic ovarian drilling, Outcome 4 Miscarriage rate by woman randomised. | ||||
| 4.1 AI versus LOD | 4 | 628 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.29, 1.63] |
| 4.2 AI + metformin versus LOD | 1 | 146 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.35 [0.29, 6.27] |
| 5 Miscarriage rate by pregnancies Show forest plot | 5 | 240 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.30, 1.43] |
| Analysis 4.5  Comparison 4 Letrozole compared to laparoscopic ovarian drilling, Outcome 5 Miscarriage rate by pregnancies. | ||||
| 5.1 AI versus LOD | 4 | 191 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.22, 1.33] |
| 5.2 AI + metformin versus LOD | 1 | 49 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.24, 6.09] |
| 6 Multiple pregnancy rate Show forest plot | 3 | 548 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.00 [0.12, 74.90] |
| Analysis 4.6 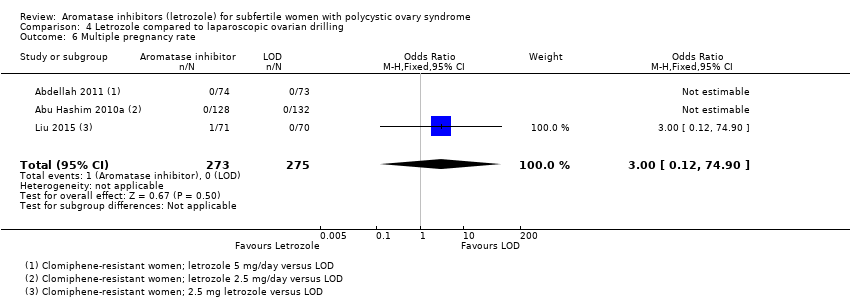 Comparison 4 Letrozole compared to laparoscopic ovarian drilling, Outcome 6 Multiple pregnancy rate. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Ovarian hyperstimulation syndrome rate Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.1  Comparison 5 Letrozole compared to FSH, Outcome 1 Ovarian hyperstimulation syndrome rate. | ||||
| 2 Clinical pregnancy rate Show forest plot | 1 | 140 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.40, 1.67] |
| Analysis 5.2  Comparison 5 Letrozole compared to FSH, Outcome 2 Clinical pregnancy rate. | ||||
| 3 Miscarriage rate by woman randomised Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.3  Comparison 5 Letrozole compared to FSH, Outcome 3 Miscarriage rate by woman randomised. | ||||
| 4 Miscarriage rate by pregnancies Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.4 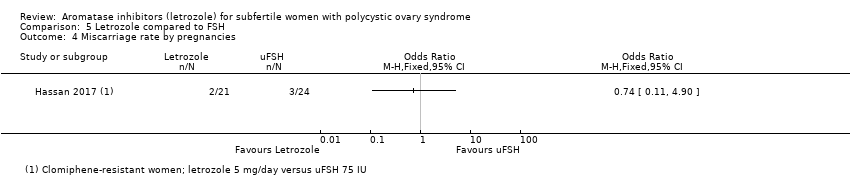 Comparison 5 Letrozole compared to FSH, Outcome 4 Miscarriage rate by pregnancies. | ||||
| 5 Multiple pregnancy rate Show forest plot | 1 | 140 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.01, 4.12] |
| Analysis 5.5  Comparison 5 Letrozole compared to FSH, Outcome 5 Multiple pregnancy rate. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Ovarian hyperstimulation syndrome rate Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.1 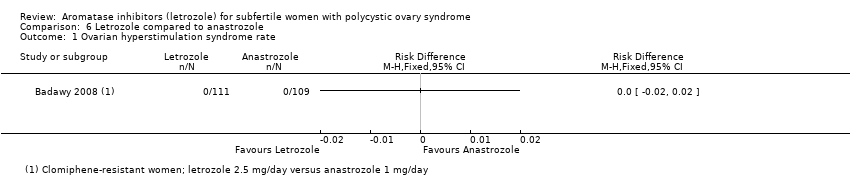 Comparison 6 Letrozole compared to anastrozole, Outcome 1 Ovarian hyperstimulation syndrome rate. | ||||
| 2 Clinical pregnancy rate Show forest plot | 2 | 260 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.51, 1.43] |
| Analysis 6.2  Comparison 6 Letrozole compared to anastrozole, Outcome 2 Clinical pregnancy rate. | ||||
| 3 Miscarriage rate by woman randomised Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.3 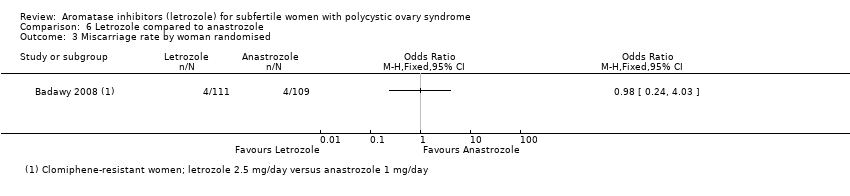 Comparison 6 Letrozole compared to anastrozole, Outcome 3 Miscarriage rate by woman randomised. | ||||
| 4 Miscarriage rate by pregnancies Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.4  Comparison 6 Letrozole compared to anastrozole, Outcome 4 Miscarriage rate by pregnancies. | ||||
| 5 Multiple pregnancy rate Show forest plot | 2 | 260 | Odds Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.24, 105.35] |
| Analysis 6.5  Comparison 6 Letrozole compared to anastrozole, Outcome 5 Multiple pregnancy rate. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Ovarian hyperstimulation syndrome rate Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.1  Comparison 7 Different administration protocols of letrozole, Outcome 1 Ovarian hyperstimulation syndrome rate. | ||||
| 1.1 Five days compared to 10 days administration protocol of letrozole | 1 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Clinical pregnancy rate Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.2  Comparison 7 Different administration protocols of letrozole, Outcome 2 Clinical pregnancy rate. | ||||
| 2.1 Five days compared to 10 days administration protocol of letrozole | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Letrozole day 3‐7 administratio versus day 5‐9 administration | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Miscarriage rate by woman randomised Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.3 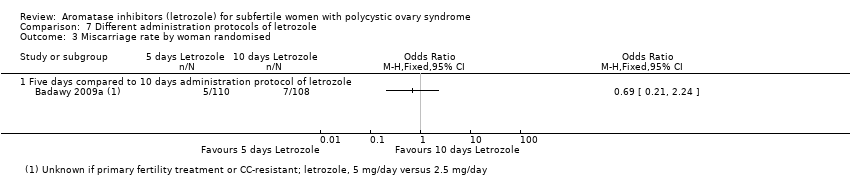 Comparison 7 Different administration protocols of letrozole, Outcome 3 Miscarriage rate by woman randomised. | ||||
| 3.1 Five days compared to 10 days administration protocol of letrozole | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Miscarriage rate by pregnancies Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.4  Comparison 7 Different administration protocols of letrozole, Outcome 4 Miscarriage rate by pregnancies. | ||||
| 4.1 Five days compared to 10 days administration protocol of letrozole | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Multiple pregnancy rate Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.5  Comparison 7 Different administration protocols of letrozole, Outcome 5 Multiple pregnancy rate. | ||||
| 5.1 Five days compared to 10 days administration protocol of letrozole | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Ovarian hyperstimulation syndrome rate Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.1  Comparison 8 Dosage studies of letrozole, Outcome 1 Ovarian hyperstimulation syndrome rate. | ||||
| 1.1 5mg vs 7.5mg letrozole | 1 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Clinical pregnancy rate Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.2 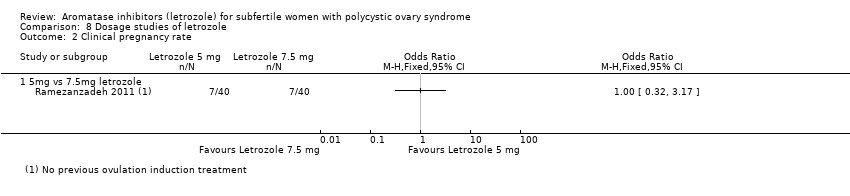 Comparison 8 Dosage studies of letrozole, Outcome 2 Clinical pregnancy rate. | ||||
| 2.1 5mg vs 7.5mg letrozole | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Miscarriage rate by woman randomised Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.3  Comparison 8 Dosage studies of letrozole, Outcome 3 Miscarriage rate by woman randomised. | ||||
| 3.1 5mg vs 7.5mg letrozole | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Miscarriage rate by pregnancies Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.4  Comparison 8 Dosage studies of letrozole, Outcome 4 Miscarriage rate by pregnancies. | ||||
| 4.1 5mg vs 7.5mg letrozole | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Multiple pregnancy rate Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.5  Comparison 8 Dosage studies of letrozole, Outcome 5 Multiple pregnancy rate. | ||||
| 5.1 5mg vs 7.5mg letrozole | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
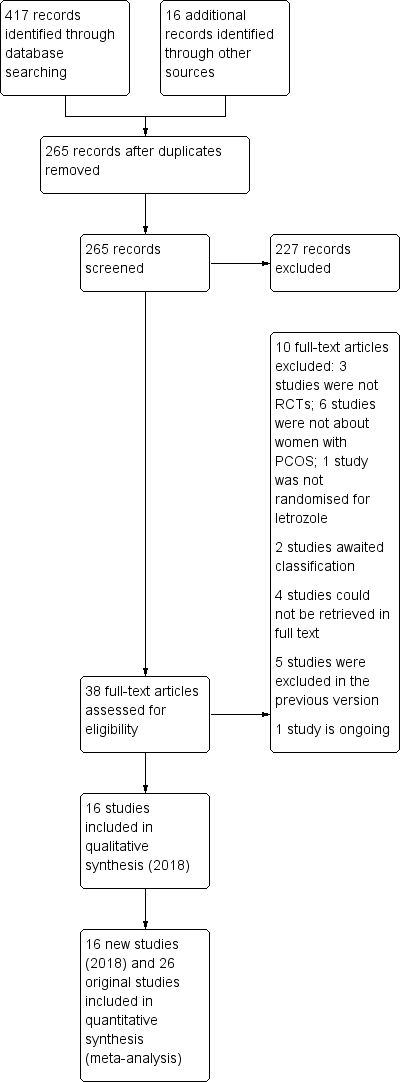
Study flow diagram for update 2018
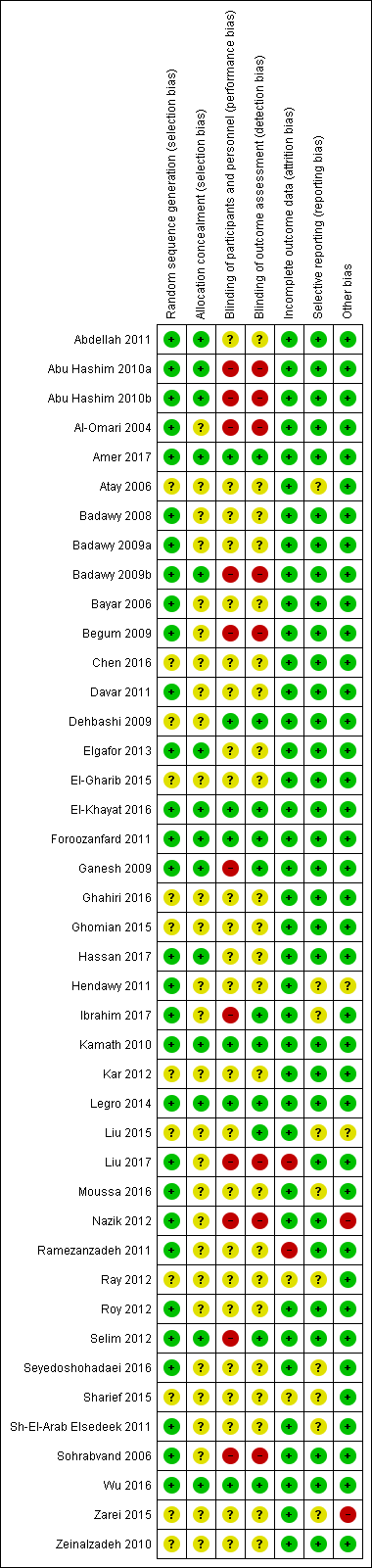
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
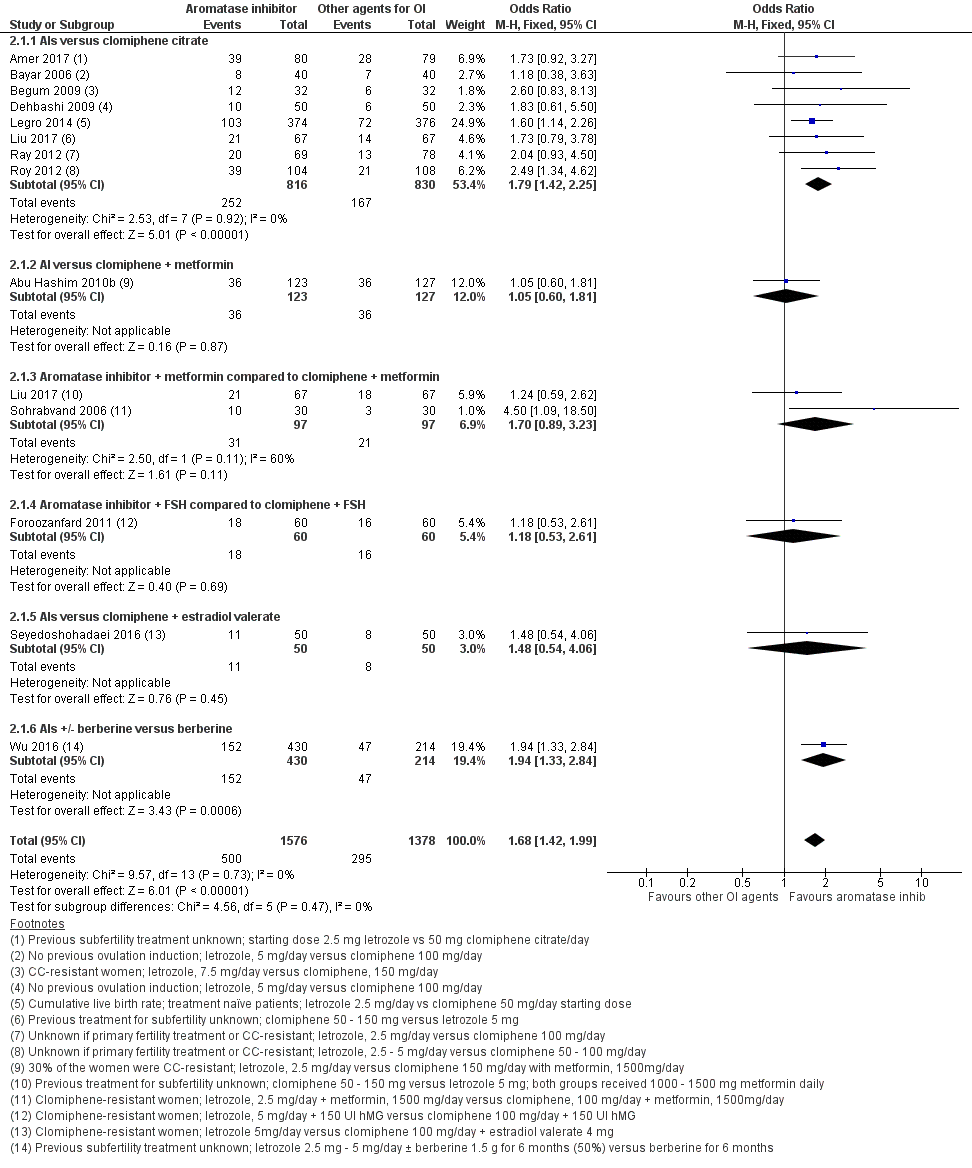
Forest plot of comparison: 2 Aromatase inhibitors compared to other ovulation induction agents, outcome: 2.1 Live birth rate.

Funnel plot of comparison: 2 Aromatase inhibitors compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, outcome: 2.1 Live birth rate.
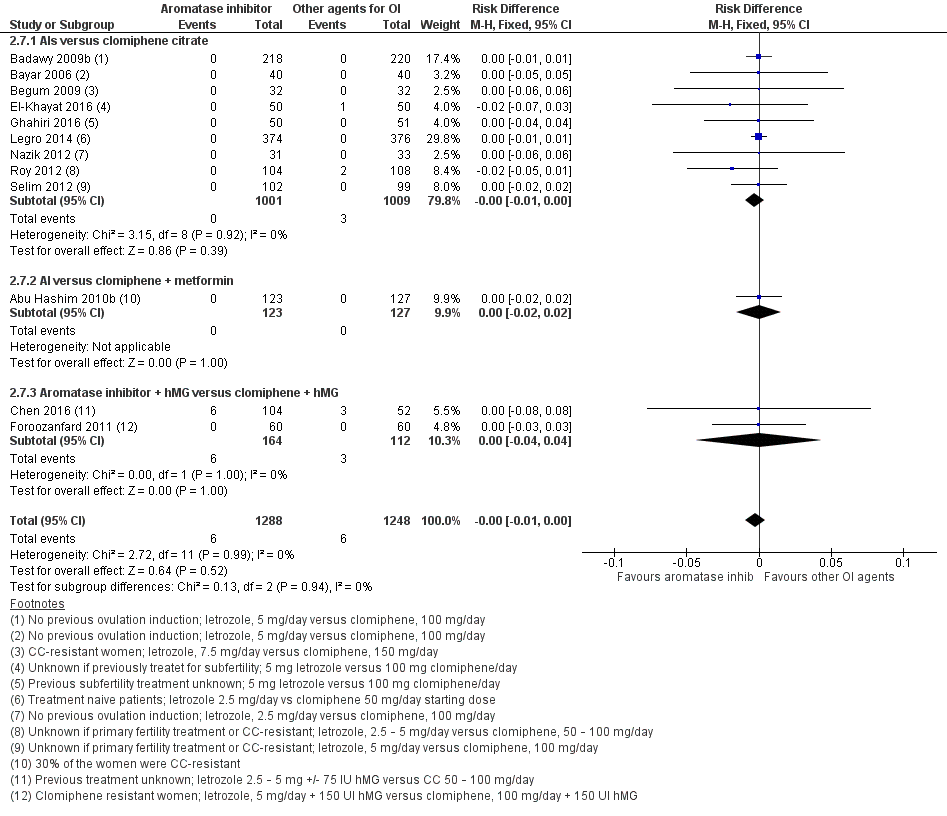
Forest plot of comparison: 2 Aromatase inhibitors compared to other ovulation induction agents, outcome: 2.6 Ovarian hyperstimulation syndrome rate.
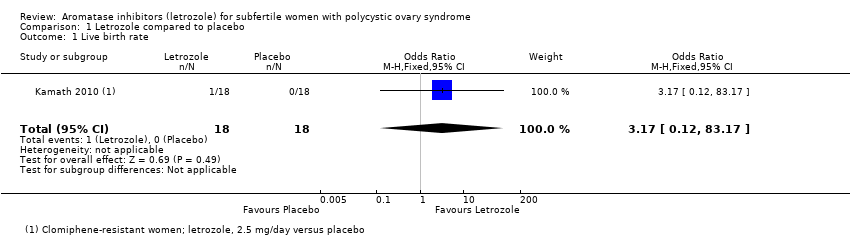
Comparison 1 Letrozole compared to placebo, Outcome 1 Live birth rate.

Comparison 1 Letrozole compared to placebo, Outcome 2 Ovarian hyperstimulation syndrome rate.

Comparison 1 Letrozole compared to placebo, Outcome 3 Clinical pregnancy rate.

Comparison 1 Letrozole compared to placebo, Outcome 4 Miscarriage rate by woman randomised.

Comparison 1 Letrozole compared to placebo, Outcome 5 Miscarriage rate by pregnancies.
Comparison 1 Letrozole compared to placebo, Outcome 6 Multiple pregnancy rate.

Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 1 Live birth rate.

Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 2 Live birth rate by BMI.
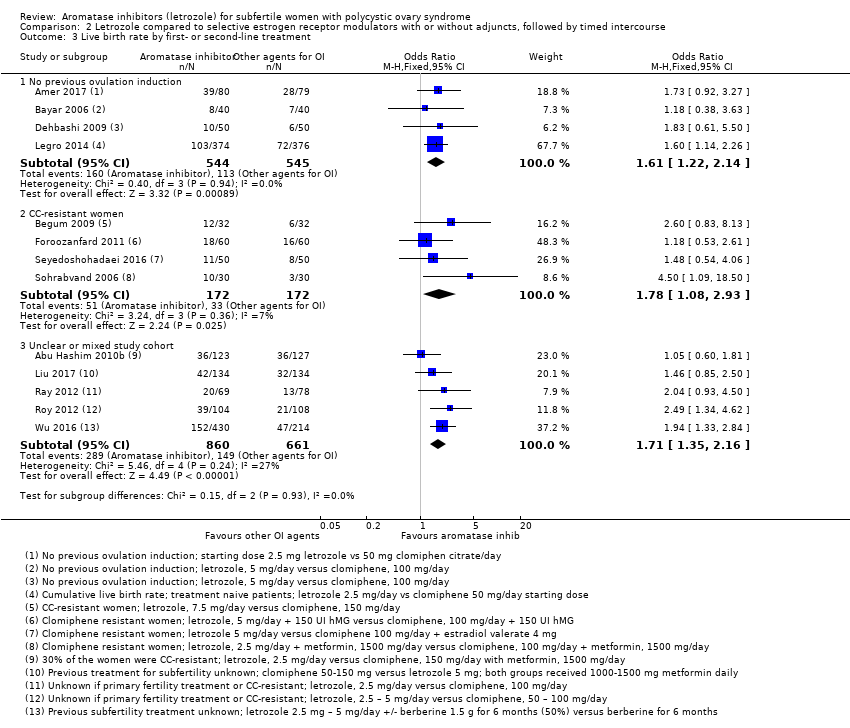
Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 3 Live birth rate by first‐ or second‐line treatment.

Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 4 Impact of allocation bias for live birth rate.

Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 5 Impact of detection bias for live birth rate.

Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 6 Impact of attrition bias for live birth rate.
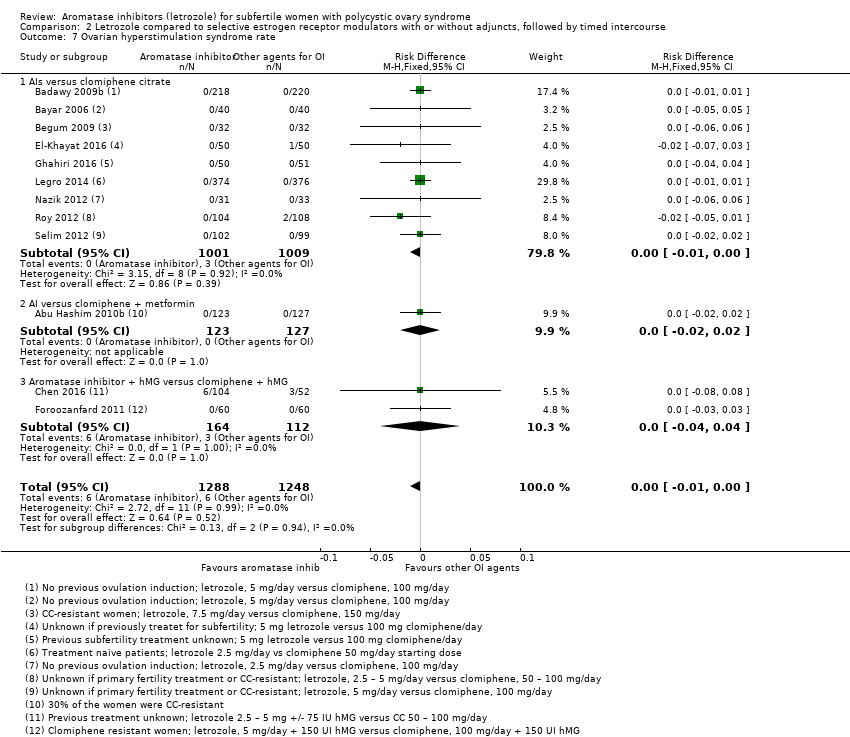
Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 7 Ovarian hyperstimulation syndrome rate.

Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 8 Ovarian hyperstimulation syndrome rate per BMI.

Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 9 Clinical pregnancy rate.

Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 10 Impact of allocation bias for clinical pregnancy rate.

Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 11 Miscarriage rate by woman randomised.

Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 12 Miscarriage rate by pregnancies.
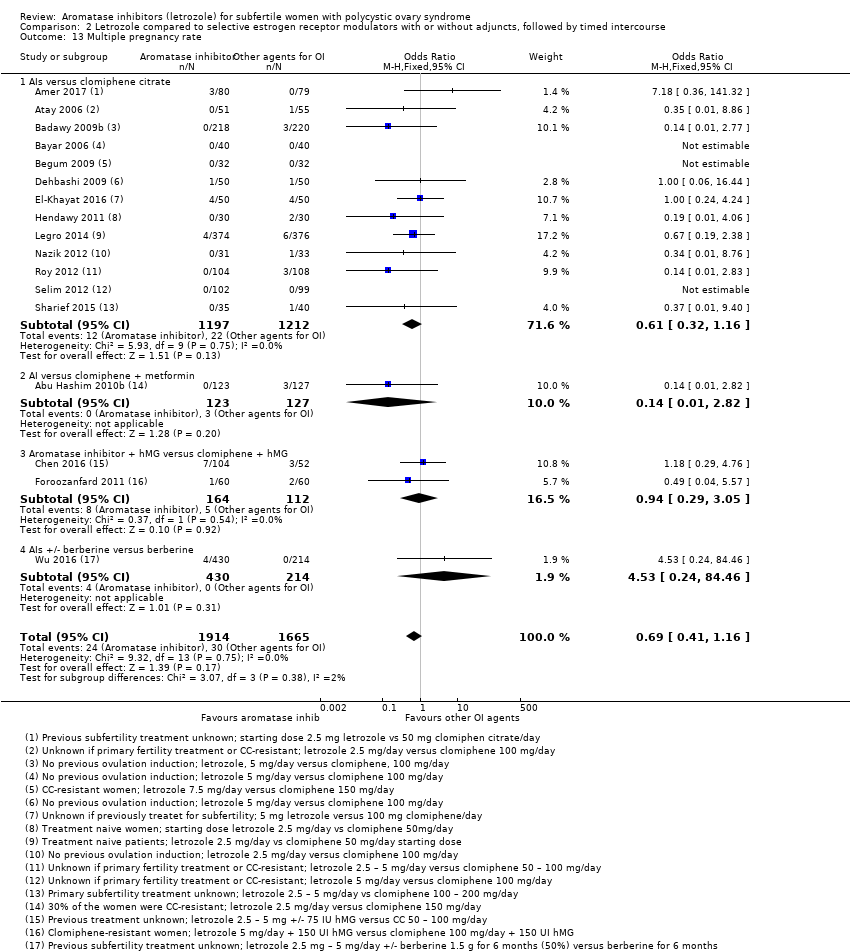
Comparison 2 Letrozole compared to selective estrogen receptor modulators with or without adjuncts, followed by timed intercourse, Outcome 13 Multiple pregnancy rate.

Comparison 3 Letrozole compared to clomiphene citrate, followed by IUI, Outcome 1 Ovarian hyperstimulation syndrome rate.

Comparison 3 Letrozole compared to clomiphene citrate, followed by IUI, Outcome 2 Clinical pregnancy rate.
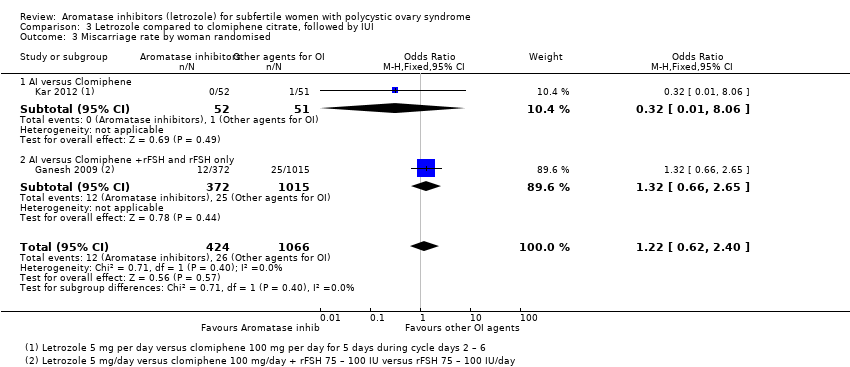
Comparison 3 Letrozole compared to clomiphene citrate, followed by IUI, Outcome 3 Miscarriage rate by woman randomised.
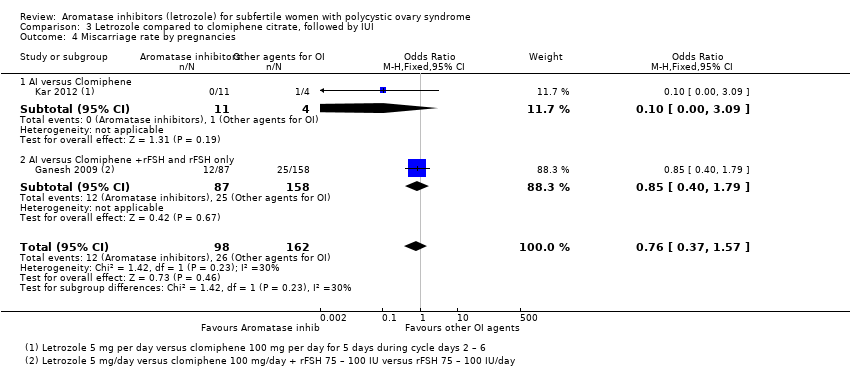
Comparison 3 Letrozole compared to clomiphene citrate, followed by IUI, Outcome 4 Miscarriage rate by pregnancies.

Comparison 3 Letrozole compared to clomiphene citrate, followed by IUI, Outcome 5 Multiple pregnancy rate.

Comparison 4 Letrozole compared to laparoscopic ovarian drilling, Outcome 1 Live birth rate.
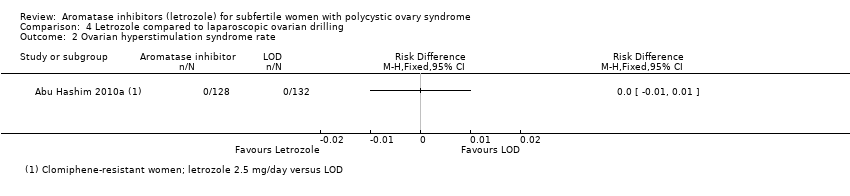
Comparison 4 Letrozole compared to laparoscopic ovarian drilling, Outcome 2 Ovarian hyperstimulation syndrome rate.

Comparison 4 Letrozole compared to laparoscopic ovarian drilling, Outcome 3 Clinical pregnancy rate.

Comparison 4 Letrozole compared to laparoscopic ovarian drilling, Outcome 4 Miscarriage rate by woman randomised.
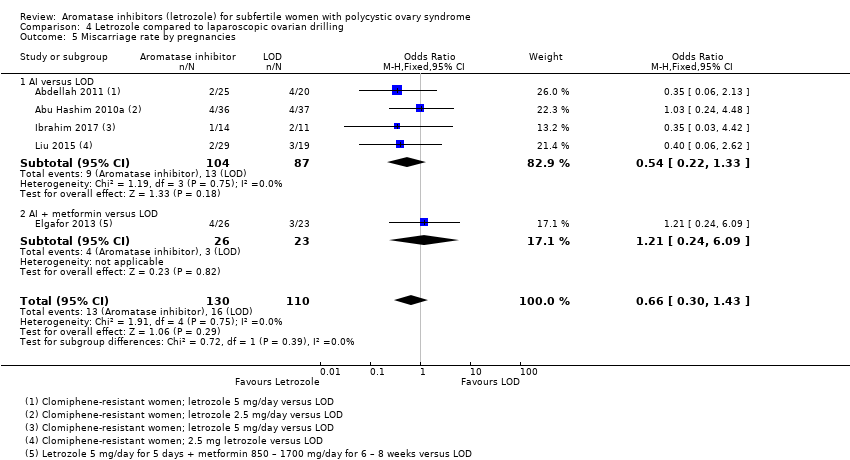
Comparison 4 Letrozole compared to laparoscopic ovarian drilling, Outcome 5 Miscarriage rate by pregnancies.

Comparison 4 Letrozole compared to laparoscopic ovarian drilling, Outcome 6 Multiple pregnancy rate.
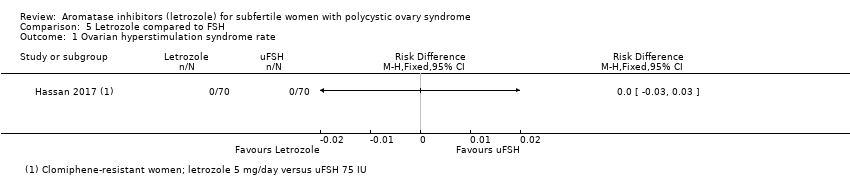
Comparison 5 Letrozole compared to FSH, Outcome 1 Ovarian hyperstimulation syndrome rate.

Comparison 5 Letrozole compared to FSH, Outcome 2 Clinical pregnancy rate.
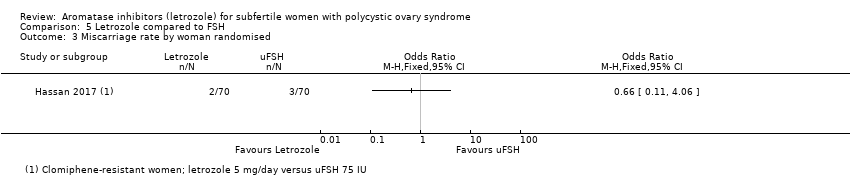
Comparison 5 Letrozole compared to FSH, Outcome 3 Miscarriage rate by woman randomised.
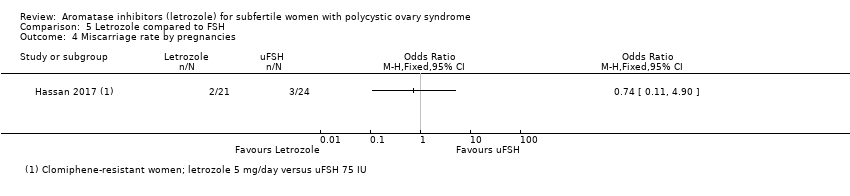
Comparison 5 Letrozole compared to FSH, Outcome 4 Miscarriage rate by pregnancies.

Comparison 5 Letrozole compared to FSH, Outcome 5 Multiple pregnancy rate.

Comparison 6 Letrozole compared to anastrozole, Outcome 1 Ovarian hyperstimulation syndrome rate.

Comparison 6 Letrozole compared to anastrozole, Outcome 2 Clinical pregnancy rate.

Comparison 6 Letrozole compared to anastrozole, Outcome 3 Miscarriage rate by woman randomised.

Comparison 6 Letrozole compared to anastrozole, Outcome 4 Miscarriage rate by pregnancies.
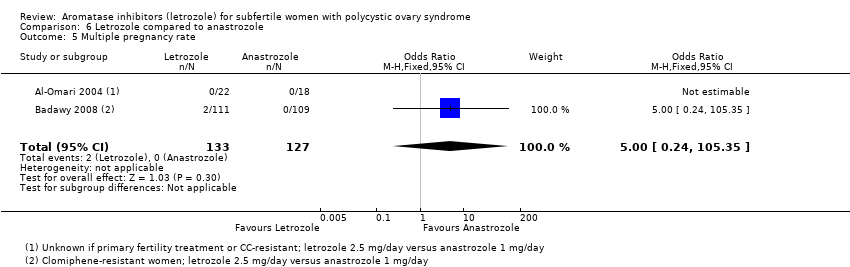
Comparison 6 Letrozole compared to anastrozole, Outcome 5 Multiple pregnancy rate.
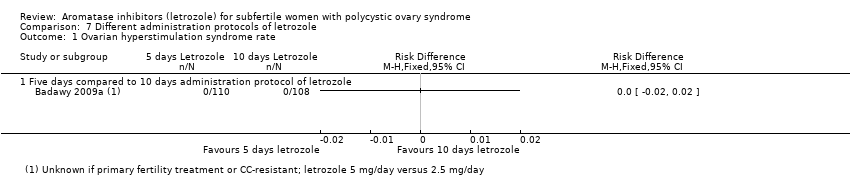
Comparison 7 Different administration protocols of letrozole, Outcome 1 Ovarian hyperstimulation syndrome rate.

Comparison 7 Different administration protocols of letrozole, Outcome 2 Clinical pregnancy rate.

Comparison 7 Different administration protocols of letrozole, Outcome 3 Miscarriage rate by woman randomised.

Comparison 7 Different administration protocols of letrozole, Outcome 4 Miscarriage rate by pregnancies.

Comparison 7 Different administration protocols of letrozole, Outcome 5 Multiple pregnancy rate.

Comparison 8 Dosage studies of letrozole, Outcome 1 Ovarian hyperstimulation syndrome rate.

Comparison 8 Dosage studies of letrozole, Outcome 2 Clinical pregnancy rate.

Comparison 8 Dosage studies of letrozole, Outcome 3 Miscarriage rate by woman randomised.

Comparison 8 Dosage studies of letrozole, Outcome 4 Miscarriage rate by pregnancies.
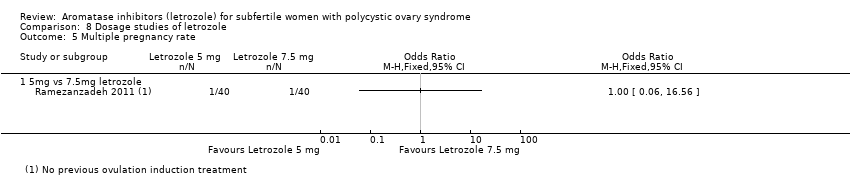
Comparison 8 Dosage studies of letrozole, Outcome 5 Multiple pregnancy rate.
| Letrozole with or without adjuncts compared to clomiphene citrate (CC) with or without adjuncts for subfertile women with polycystic ovary syndrome | ||||||
| Patient or population: subfertile women with polycystic ovary syndrome | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
| Risk with CC with or without adjuncts | Risk with letrozole with or without adjuncts | |||||
| Live birth rate | 214 per 1000 | 314 per 1000 | OR 1.68 | 2954 | ⊕⊕⊕⊝ | |
| Ovarian hyperstimulation syndrome rate | 5 per 1000 | 5 per 1000 | RD 0.00 | 2536 | ⊕⊕⊕⊕ | |
| Clinical pregnancy rate | 264 per 1000 | 359 per 1000 | OR 1.56 | 4629 | ⊕⊕⊕⊝ | |
| Miscarriage rate by pregnancies | 201 per 1000 | 191 per 1000 | OR 0.94 | 1210 | ⊕⊕⊕⊕ | |
| Multiple pregnancy rate | 17 per 1000 | 13 per 1000 | OR 0.69 | 3579 | ⊕⊕⊕⊕ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded one level for serious risk of bias associated with potential selective reporting: Studies that reported live birth tended to report higher clinical pregnancy rates in the letrozole group than studies that failed to report live birth, suggesting that results might be less favourable to letrozole if all studies reported live birth. | ||||||
| Letrozole compared to laparoscopic ovarian drilling compared to placebo for subfertile women with polycystic ovary syndrome | ||||||
| Patient or population: Subfertile women with polycystic ovary syndrome | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
| Risk with LOD | Risk with letrozole | |||||
| Live birth rate | 236 per 1000 | 299 per 1000 | OR 1.38 | 548 | ⊕⊕⊕⊝ | |
| Ovarian hyperstimulation syndrome rate | 0 per 1000 | 0 per 1000 | RD 0.00 | 260 | ⊕⊕⊝⊝ | |
| Clinical pregnancy rate | 284 per 1000 | 336 per 1000 | OR 1.28 | 774 | ⊕⊕⊕⊝ | |
| Miscarriage rate by pregnancies | 145 per 1000 | 101 per 1000 | OR 0.66 | 240 | ⊕⊕⊕⊝ | |
| Multiple pregnancy rate | 0 per 1000 | 0 per 1000 | OR 3.00 | 548 | ⊕⊕⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aInsufficient data to allow judgement of risk of bias in some studies ‐ downgraded one level for serious risk of bias. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Live birth rate Show forest plot | 1 | 36 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.17 [0.12, 83.17] |
| 2 Ovarian hyperstimulation syndrome rate Show forest plot | 2 | 167 | Risk Difference (M‐H, Fixed, 95% CI) | 0.00 [‐0.05, 0.05] |
| 3 Clinical pregnancy rate Show forest plot | 2 | 167 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.88 [1.08, 7.66] |
| 4 Miscarriage rate by woman randomised Show forest plot | 2 | 167 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.60 [0.26, 9.89] |
| 5 Miscarriage rate by pregnancies Show forest plot | 1 | 20 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.07, 4.56] |
| 6 Multiple pregnancy rate Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Live birth rate Show forest plot | 13 | 2954 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.68 [1.42, 1.99] |
| 1.1 AIs versus clomiphene citrate | 8 | 1646 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [1.42, 2.25] |
| 1.2 AI versus clomiphene + metformin | 1 | 250 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.60, 1.81] |
| 1.3 Aromatase inhibitor + metformin compared to clomiphene + metformin | 2 | 194 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.70 [0.89, 3.23] |
| 1.4 Aromatase inhibitor + FSH compared to clomiphene + FSH | 1 | 120 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.53, 2.61] |
| 1.5 AIs versus clomiphene + estradiol valerate | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.54, 4.06] |
| 1.6 AIs +/‐ berberine versus berberine | 1 | 644 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.94 [1.33, 2.84] |
| 2 Live birth rate by BMI Show forest plot | 11 | 2774 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.69 [1.42, 2.02] |
| 2.1 BMI > 25 | 7 | 1678 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.67 [1.34, 2.09] |
| 2.2 BMI < 25 | 4 | 1096 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.73 [1.31, 2.28] |
| 3 Live birth rate by first‐ or second‐line treatment Show forest plot | 13 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 No previous ovulation induction | 4 | 1089 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.61 [1.22, 2.14] |
| 3.2 CC‐resistant women | 4 | 344 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.78 [1.08, 2.93] |
| 3.3 Unclear or mixed study cohort | 5 | 1521 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.71 [1.35, 2.16] |
| 4 Impact of allocation bias for live birth rate Show forest plot | 13 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Unclear risk of allocation | 8 | 1031 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.90 [1.42, 2.54] |
| 4.2 Low risk of allocation | 5 | 1923 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.58 [1.29, 1.95] |
| 5 Impact of detection bias for live birth rate Show forest plot | 13 | 2954 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.68 [1.42, 1.99] |
| 5.1 High risk of detection | 1 | 64 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.6 [0.83, 8.13] |
| 5.2 Low risk of detection | 7 | 2083 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.63 [1.33, 1.99] |
| 5.3 Unclear risk of detection | 5 | 807 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.76 [1.27, 2.44] |
| 6 Impact of attrition bias for live birth rate Show forest plot | 13 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Unclear risk of attrition | 1 | 147 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.04 [0.93, 4.50] |
| 6.2 Low risk of attrition | 11 | 2539 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.69 [1.41, 2.03] |
| 6.3 High risk of attrition | 1 | 268 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.46 [0.85, 2.50] |
| 7 Ovarian hyperstimulation syndrome rate Show forest plot | 12 | 2536 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.00 [‐0.01, 0.00] |
| 7.1 AIs versus clomiphene citrate | 9 | 2010 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.00 [‐0.01, 0.00] |
| 7.2 AI versus clomiphene + metformin | 1 | 250 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 7.3 Aromatase inhibitor + hMG versus clomiphene + hMG | 2 | 276 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.04, 0.04] |
| 8 Ovarian hyperstimulation syndrome rate per BMI Show forest plot | 11 | Risk Difference (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 BMI > 25 | 6 | 1851 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.00 [‐0.01, 0.00] |
| 8.2 BMI < 25 | 5 | 605 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 9 Clinical pregnancy rate Show forest plot | 25 | 4629 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.56 [1.37, 1.78] |
| 9.1 AIs versus clomiphene citrate | 17 | 2930 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.50 [1.28, 1.76] |
| 9.2 AI versus clomiphene + metformin | 1 | 250 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.60, 1.71] |
| 9.3 Aromatase inhibitor + metformin versus clomiphene + metformin | 3 | 294 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.86 [1.05, 3.29] |
| 9.4 Aromatase inhibitor + hMG versus clomiphene + hMG | 2 | 276 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.82, 2.27] |
| 9.5 AIs versus tamoxifen | 2 | 135 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.58 [0.64, 3.90] |
| 9.6 AIs versus clomiphene + estradiol valerate | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.47 [0.94, 6.46] |
| 9.7 AIs ± berberine versus berberine | 1 | 644 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.15 [1.48, 3.13] |
| 10 Impact of allocation bias for clinical pregnancy rate Show forest plot | 23 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 Unclear risk of allocation | 16 | 1907 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.77 [1.43, 2.18] |
| 10.2 Low risk of allocation | 7 | 1912 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.36 [1.12, 1.65] |
| 11 Miscarriage rate by woman randomised Show forest plot | 18 | 3754 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.39 [1.07, 1.81] |
| 11.1 AIs versus clomiphene citrate | 11 | 2190 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.97, 1.93] |
| 11.2 AI versus clomiphene + metformin | 1 | 250 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.25, 4.23] |
| 11.3 Aromatase inhibitor + metformin versus clomiphene + metformin | 3 | 294 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.52, 2.82] |
| 11.4 Aromatase inhibitor + hMG versus clomiphene + hMG | 2 | 276 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.31, 2.27] |
| 11.5 AIs versus clomiphene + estradiol valerate | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 12.21 [0.66, 226.97] |
| 11.6 AIs +/‐ berberine versus berberine | 1 | 644 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.63 [0.87, 3.04] |
| 12 Miscarriage rate by pregnancies Show forest plot | 18 | 1210 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.70, 1.26] |
| 12.1 AIs versus clomiphene citrate | 11 | 705 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.65, 1.42] |
| 12.2 AI versus clomiphene + metformin | 1 | 85 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.24, 4.40] |
| 12.3 Aromatase inhibitor + metformin versus clomiphene + metformin | 3 | 79 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.32, 2.02] |
| 12.4 Aromatase inhibitor + hMG versus clomiphene + hMG | 2 | 104 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.23, 1.96] |
| 12.5 AIs versus clomiphene + estradiol valerate | 1 | 24 | Odds Ratio (M‐H, Fixed, 95% CI) | 8.13 [0.39, 167.90] |
| 12.6 AIs +/‐ berberine versus berberine | 1 | 213 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.43, 1.80] |
| 13 Multiple pregnancy rate Show forest plot | 17 | 3579 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.41, 1.16] |
| 13.1 AIs versus clomiphene citrate | 13 | 2409 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.32, 1.16] |
| 13.2 AI versus clomiphene + metformin | 1 | 250 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.82] |
| 13.3 Aromatase inhibitor + hMG versus clomiphene + hMG | 2 | 276 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.29, 3.05] |
| 13.4 AIs +/‐ berberine versus berberine | 1 | 644 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.53 [0.24, 84.46] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Ovarian hyperstimulation syndrome rate Show forest plot | 2 | 1494 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.00 [‐0.01, 0.00] |
| 1.1 AI versus Clomiphene | 1 | 107 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.02 [‐0.07, 0.03] |
| 1.2 AI versus Clomiphene +rFSH and rFSH only | 1 | 1387 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.00 [‐0.01, 0.00] |
| 2 Clinical pregnancy rate Show forest plot | 3 | 1597 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.71 [1.30, 2.25] |
| 2.1 AI versus Clomiphene | 2 | 210 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.09 [0.97, 4.53] |
| 2.2 AI versus Clomiphene +rFSH and rFSH only | 1 | 1387 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.66 [1.23, 2.22] |
| 3 Miscarriage rate by woman randomised Show forest plot | 2 | 1490 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.62, 2.40] |
| 3.1 AI versus Clomiphene | 1 | 103 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.06] |
| 3.2 AI versus Clomiphene +rFSH and rFSH only | 1 | 1387 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.66, 2.65] |
| 4 Miscarriage rate by pregnancies Show forest plot | 2 | 260 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.37, 1.57] |
| 4.1 AI versus Clomiphene | 1 | 15 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.00, 3.09] |
| 4.2 AI versus Clomiphene +rFSH and rFSH only | 1 | 245 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.40, 1.79] |
| 5 Multiple pregnancy rate Show forest plot | 3 | 1597 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.49, 2.13] |
| 5.1 AI versus Clomiphene | 2 | 210 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.48 [0.14, 87.49] |
| 5.2 AI versus Clomiphene +rFSH and rFSH only | 1 | 1387 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.44, 2.03] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Live birth rate Show forest plot | 3 | 548 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.38 [0.95, 2.02] |
| 2 Ovarian hyperstimulation syndrome rate Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Clinical pregnancy rate Show forest plot | 5 | 774 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.94, 1.74] |
| 3.1 AI versus LOD | 4 | 628 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.93, 1.83] |
| 3.2 AI + metformin versus LOD | 1 | 146 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.60, 2.39] |
| 4 Miscarriage rate by woman randomised Show forest plot | 5 | 774 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.38, 1.70] |
| 4.1 AI versus LOD | 4 | 628 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.29, 1.63] |
| 4.2 AI + metformin versus LOD | 1 | 146 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.35 [0.29, 6.27] |
| 5 Miscarriage rate by pregnancies Show forest plot | 5 | 240 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.30, 1.43] |
| 5.1 AI versus LOD | 4 | 191 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.22, 1.33] |
| 5.2 AI + metformin versus LOD | 1 | 49 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.24, 6.09] |
| 6 Multiple pregnancy rate Show forest plot | 3 | 548 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.00 [0.12, 74.90] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Ovarian hyperstimulation syndrome rate Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Clinical pregnancy rate Show forest plot | 1 | 140 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.40, 1.67] |
| 3 Miscarriage rate by woman randomised Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Miscarriage rate by pregnancies Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Multiple pregnancy rate Show forest plot | 1 | 140 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.01, 4.12] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Ovarian hyperstimulation syndrome rate Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Clinical pregnancy rate Show forest plot | 2 | 260 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.51, 1.43] |
| 3 Miscarriage rate by woman randomised Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Miscarriage rate by pregnancies Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Multiple pregnancy rate Show forest plot | 2 | 260 | Odds Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.24, 105.35] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Ovarian hyperstimulation syndrome rate Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Five days compared to 10 days administration protocol of letrozole | 1 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Clinical pregnancy rate Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Five days compared to 10 days administration protocol of letrozole | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Letrozole day 3‐7 administratio versus day 5‐9 administration | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Miscarriage rate by woman randomised Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Five days compared to 10 days administration protocol of letrozole | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Miscarriage rate by pregnancies Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 Five days compared to 10 days administration protocol of letrozole | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Multiple pregnancy rate Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 Five days compared to 10 days administration protocol of letrozole | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Ovarian hyperstimulation syndrome rate Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 5mg vs 7.5mg letrozole | 1 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Clinical pregnancy rate Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 5mg vs 7.5mg letrozole | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Miscarriage rate by woman randomised Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 5mg vs 7.5mg letrozole | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Miscarriage rate by pregnancies Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 5mg vs 7.5mg letrozole | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Multiple pregnancy rate Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 5mg vs 7.5mg letrozole | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

