استفاده از درمانهای سایکولوژیکال برای اختلال استرس پس از تروما همراه با اختلال سوء مصرف مواد
چکیده
پیشینه
اختلال استرس پس از تروما (post‐traumatic stress disorder; PTSD) یک اختلال ناتوان کننده سلامت روان است که ممکن است پس از قرار گرفتن در معرض حوادث آسیبزننده گسترش یابد. اختلال مصرف مواد (substance use disorder; SUD) یک اختلال رفتاری است که در آن استفاده از یک یا چند ماده با سطح بالایی از اضطراب، اختلال قابل توجه بالینی عملکرد یا هر دو همراه است. PTSD و SUD اغلب با هم رخ میدهند. همراه بودن این دو وضعیت عموما درمان سختی داشته و پیامدهای درمانی آن از پیامدهای درمانی هریک به تنهایی بدتر است. چندین درمان سایکولوژیکال برای درمان این وضعیتهای همراه شکل گرفتهاند، با این حال هیچ توافقی در مورد اینکه کدام درمان موثرترین است، وجود ندارد.
اهداف
تعیین اثربخشی درمانهای سایکولوژیکال در درمان نشانههای استرس پس از تروما، نشانههای سوء مصرف مواد مخدر، یا هر دو در افراد مبتلا به PTSD و SUD در مقایسه با شرایط کنترل (مراقبتهای معمول، شرایط انتظار و عدم درمان) و دیگر درمانهای سایکولوژیکال.
روشهای جستوجو
پایگاه ثبت تخصصی گروه افسردگی، اضطراب و بیماریهای اعصاب در کاکرین (Cochrane Depression, Anxiety and Neurosis Group’s Specialised Register) را در همه سالها تا 11 مارچ 2015 جستوجو کردیم. این پایگاه ثبت تخصصی شامل کارآزماییهای تصادفیسازی و کنترل شده مرتبط از کتابخانه کاکرین (The Cochrane Library) (همه سالها)، MEDLINE (از 1950 تاکنون)، EMBASE (از 1974 تاکنون) و PsycINFO (از 1967 تاکنون) بود. همچنین جستوجو در پلتفرم بینالمللی پایگاه ثبت کارآزماییهای بالینی سازمان جهانی بهداشت (World Health Organization International Clinical Trials Registry Platform) و ClinicalTrials.gov، تماس با کارشناسان، جستوجو در کتابشناختیهای مطالعات وارد شده، و جستوجو در استنادات مقالات را هم انجام دادیم.
معیارهای انتخاب
کارآزماییهای تصادفیسازی و کنترل شده مربوط به رواندرمانی فردی یا گروهی برای افراد مبتلا به PTSD همراه با سوء مصرف مواد، در مقایسه با شرایط لیست انتظار، مراقبتهای معمول، یا مداخلات حداقلی یا سایر شیوههای رواندرمانی.
گردآوری و تجزیهوتحلیل دادهها
از روشهای استاندارد روششناسی مورد نظر کاکرین استفاده کردیم.
نتایج اصلی
14 مطالعه با 1506 شرکتکننده در مرور وارد کردیم، که از میان آنها 13 مطالعه در سنتز کمّی (quantitative synthesis) وارد شدند. اکثر مطالعات بین جمعیت بزرگسالان انجام شده بودند. مطالعات در محیطهای مختلفی انجام شده بودند. چهار مقایسه را شکل دادیم که تاثیرات رواندرمانی را به جز مقایسههای متمرکز بر تروما و غیر‐متمرکز بر تروما در مقابل درمانهایی مانند مداخله معمول/حداقلی و سایر رواندرمانیهای فعال بررسی میکرد. مقایسهها برای درمانهای فردی یا گروهی طبقهبندی شدند. همه مداخلات فعال بر مبنای درمان شناختی رفتاری (cognitive behavioural therapy) بود. یافتههای اصلی ما عبارت بودند از:
رواندرمانی فردی مبتنی بر مولفه متمرکز بر تروما همراه با مداخله SUD موثرتر از درمان به شیوه معمول (TAU)/مداخله حداقلی برای وخامت PTSD پس از درمان (تفاوت میانگین استاندارد شده (SMD): 0.41‐؛ 95% فاصله اطمینان (CI): 0.72‐ تا 0.10‐؛ 4 مطالعه؛ 405 = n؛ شواهد با کیفیت بسیار پائین) و در پیگیریهای 3 تا 4 و 5 تا 7 ماه، بود. هیچ نشانهای از تاثیر بر سطح مصرف مواد مخدر/الکل بعد از درمان (SMD: ‐0.13؛ 95% CI؛ 0.41‐ تا 0.15 ‐؛ 3 مطالعه؛ 388 = n؛ شواهد با کیفیت بسیار پائین) وجود نداشت، اما یک تاثیر کوچک به نفع رواندرمانی فردی در پیگیری 5 تا 7 ماه (SMD: ‐0.28؛ 95% CI؛ 0.48‐ تا 0.07‐؛ 3 مطالعه؛ 388 = n) در مقایسه با TAU دیده شد. شرکتکنندگان کمتری درمان متمرکز بر تروما را نسبت به TAU به پایان رسانده بودند (خطر نسبی (RR)؛ 0.78؛ 95% CI؛ 0.64 تا 0.96؛ 3 مطالعه؛ 316 = n؛ شواهد با کیفیت پائین).
رواندرمانی فردی با تمرکز بر مولفه تروما بهتر از رواندرمانی برای SUD عمل نکرد، مگر در وخامت PTSD؛ (تفاوت میانگین (MD) 3.91‐؛ 95% CI؛ 19.16‐ تا 11.34؛ 1 مطالعه؛ 46 = n؛ شواهد با کیفیت پائین) یا مصرف مواد مخدر/الکل (MD: ‐1.27؛ 95% CI؛ 5.76‐ تا 3.22؛ 1 مطالعه؛ 46 = n؛ شواهد با کیفیت پائین). یافتهها بر اساس یک مطالعه کوچک بودند. تاثیری بر نرخ تکمیل درمان دیده نشد (RR: 1.00؛ 95% CI؛ 0.74 تا 1.36؛ 1 مطالعه؛ 62 = n؛ شواهد با کیفیت پائین).
رواندرمانی غیر‐متمرکز بر تروما بهتر از TAU/مداخله حداقلی برای وخامت PTSD، زمانی که به صورت فردی (SMD: ‐0.22؛ 95% CI؛ 0.83‐ تا 0.39؛ 1 مطالعه؛ 44 = n؛ شواهد با کیفیت پائین) یا گروهی (SMD: ‐0.02؛ 95% CI؛ 0.19‐ تا 0.16؛ 4 مطالعه؛ 513 = n؛ شواهد با کیفیت پائین) تجویز شد، نداشت. هیچ دادهای در مورد تاثیرات استفاده از مواد مخدر/الکل در درمانهای انفرادی وجود ندارد. هیچ شواهدی از تاثیری بر سطح مصرف مواد مخدر/الکل در درمان گروهی وجود نداشت (SMD: ‐0.03؛ 95% CI؛ 0.37‐ تا 0.31؛ 4 مطالعه؛ 414 = n؛ شواهد با کیفیت بسیار پائین). یک آنالیز تعقیبی (post‐hoc) برای دوز کامل گروه درمانی گسترده به نام Seeking Safety نشانگر کاهش مصرف مواد مخدر/الکل پس از درمان بود (SMD: ‐0.67؛ 95% CI؛ 1.14‐ تا 0.19‐؛ 2 مطالعه؛ 111 شرکتکننده) اما نه در پیگیریهای بعدی. دادههای مربوط به مورد تعداد شرکتکنندگانی که درمان را تکمیل کرده بودند، با درمانهای فردی مرتبط نبود. تاثیری در نرخ تکمیل درمان در درمان گروهی دیده نشد (RR: 1.13؛ 95% CI؛ 0.88 تا 1.45؛ 2 مطالعه؛ 217 = n؛ شواهد با کیفیت پائین).
رواندرمانی غیر‐متمرکز بر تروما بهتر از رواندرمانی برای SUD عمل نکرد، به جز در وخامت PTSD؛ (SMD: ‐0.26؛ 95% CI؛ 1.29‐ تا 0.77؛ 2 مطالعه؛ 128 = n؛ شواهد با کیفیت بسیار پائین) یا مصرف الکل یا ماده مخدر (SMD: ‐0.22؛ 95% CI؛ 0.13‐ تا 0.57؛ 2 مطالعه؛ 128 = n؛ شواهد کیفیت پائین). تاثیری بر نرخ تکمیل درمان دیده نشد (RR: 0.91؛ 95% CI؛ 0.68 تا 1.20؛ 2 مطالعه؛ 128 = n؛ شواهد با کیفیت بسیار پائین).
چندین مطالعه عوارض جانبی را گزارش دادند. تفاوتی میان نرخ بروز در هیچ کدام از مقایسهها دیده نشد. چندین مطالعه را دارای خطر سوگیری (bias) بالا یا نامشخص در حوزههای مختلف، شامل سوگیری تشخیص و سوگیری ریزش نمونه (attrition bias) ارزیابی کردیم.
نتیجهگیریهای نویسندگان
اکثر شواهد این مرور را پائین تا بسیار پائین ارزیابی کردیم. شواهد نشان دادند که رواندرمانی فردی متمرکز بر تروما در کنار درمان SUD بهتر از TAU/مداخله حداقلی در کاهش وخامت PTSD پس از درمان و در پیگیری طولانی‐مدت عمل میکند، اما SUD تنها در پیگیری طولانی‐مدت کاهش مییافت. تمام تاثیرات کوچک و مقاطع پیگیری هم عموما بسیار کوتاه بودند. شواهدی وجود داشت که نشان میداد تعداد کمتری از شرکتکنندگانی که درمان متمرکز بر تروما دریافت کردند، درمان را به پایان رساندند. شواهد بسیار کمی برای حمایت از درمانهای یکپارچه فردی یا گروهی غیر‐متمرکز بر تروما وجود دارد. افراد با بروز وخیمتر و پیچیدهتر (به عنوان مثال، بیماری جدی روانی، افراد مبتلا به اختلال شناختی و افراد در معرض خودکشی) از اکثر مطالعات این مرور کنار گذاشته شده بودند، به همین دلیل یافتههای این مرور قابل تعمیم به چنین افرادی نیست. برخی مطالعات از مشکلات ساختاری مشهودی رنج میبردند و برخی دیگر فاقد قدرت بودند، که باعث محدود شدن نتیجهگیریها میشد. انجام پژوهشهای بیشتری در این زمینه مورد نیاز است.
PICOs
خلاصه به زبان ساده
درمانهای روانشناختی برای اختلال استرس پس از تروما و اختلال سوء مصرف مواد
چه کسانی ممکن است به این مرور علاقهمند باشند؟
• افراد مبتلا به اختلال استرس پس از تروما (post‐traumatic stress disorder; PTSD) و اختلال مصرف مواد (substance use disorder; SUD) و خانواده و دوستان آنها.
• ارائه دهندگان خدمات مراقبت سلامت برای افراد مبتلا به PTSD و SUD.
چرا این مرور مهم است؟
بسیاری از افراد دچار PTSD یا SUD هستند. هر دو شرایط میتوانند بر عملکرد روزمره تاثیر داشته باشند. تعدادی از روشهای رواندرمانی متفاوت در درمان PTSD و SUD، وقتی به طور مستقل انجام میشوند، موفق هستند. با این حال، PTSD و SUD اغلب با هم رخ میدهند، و ممکن است درمان افراد مبتلا به هر دوی PTSD و SUD سختتر باشد. تعدادی از روشهای رواندرمانی برای درمان افراد مبتلا به هر دوی PTSD و SUD توسعه یافتهاند، اما مشخص نیست که این درمانها چقدر موثر هستند.
این مرور قصد دارد به چه سوالاتی پاسخ دهد؟
ما به دنبال پیدا کردن این پاسخ بودیم که روشهای رواندرمانی در درمان افراد مبتلا به PTSD و SUD در مقایسه با شرایط کنترلی و دیگر رواندرمانیها موثر هستند یا خیر.
چه مطالعاتی در این مرور وارد شدند؟
بانکهای اطلاعاتی علمی را برای پیدا کردن همه مطالعات منتشر شده و منتشر نشده در مورد روشهای رواندرمانی برای درمان افراد مبتلا به PTSD و SUD را تا 11 مارچ 2015 جستوجو کردیم. 14 مطالعه را با 1506 شرکتکننده در مرور وارد کردیم.
شواهد حاصل از این مرور به ما چه میگوید؟
شواهد نشان داد که رواندرمانی متمرکز بر تروما در کنار درمانهای SUD نسبت به درمان معمول، در کاهش PTSD موثرتر بود. این پیامد در هر دو مقطع پس از درمان و پیگیری طولانی‐مدت صادق بود. با این حال، شدت SUD تنها در پیگیری طولانی‐مدت کاهش یافت. تعداد بیشتری از افراد با درمان متمرکز بر تروما در مقایسه با درمانهای معمول انصراف دادند. به طور کلی، مزایای درمان متمرکز بر تروما کم بود.
شواهد کمی برای نشان دادن مزیت روشهای فردی یا گروهی رواندرمانی غیر‐متمرکز بر تروما یافتیم. برای درمانهای گروهی، متوجه شدیم که استفاده از مواد مخدر در مقطع پس از درمان هنگامی که به شرکتکنندگان دوره کامل 25 جلسه درمان «Seeking Safety» در محیط گروهی پیشنهاد شد، کاهش یافت. با این حال، این تاثیر مثبت در مقاطع زمانی پیگیری بعدی ادامه نیافت. سطح انصراف در تمام مطالعات بالا بود.
کیفیت شواهد را پائین تا بسیار پائین ارزیابی کردیم. این مرور شامل تعداد کمی از مطالعات است. برخی از مطالعات وارد شده طراحی ضعیفی داشتند، و اکثر مطالعات کوچک بودند. همچنین انحراف قابل توجهی در انجام روشهای درمانی و درمانهای کنترلی وجود داشت. این احتمال وجود دارد که شرکتکنندگان مطالعات وارد شده طیف وسیعی از دیگر مداخلات ثبات دهنده را در کنار درمان متمرکز بر تروما دریافت کرده باشند، ما هیچ شواهدی برای پشتیبانی از درمان متمرکز بر تروما بدون درمان متمرکز بر SUD نیافتیم. بنابراین ممکن است که یافتههای ما، با گردآوری شواهد با کیفیت بالاتر در آینده تغییر کند. ارائه دهندگان مراقبت سلامت باید زمانی که ارائه درمانهای توصیف شده در این مرور را در نظر میگیرند، با احتیاط عمل کنند.
Authors' conclusions
Summary of findings
| Trauma‐focused psychological therapy compared to control intervention | ||||||
| Patient or population: Individuals with post‐traumatic stress disorder and comorbid substance use disorder | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| TAU/ minimal intervention | Individual‐based psychological therapyincluding a trauma‐focused component | |||||
| PTSD severity following treatment completion As assessed by the CAPS, PSS‐I, or IES‐R. High scores indicate greater symptom severity | ‐ | The mean PTSD severity following treatment completion in the intervention groups was | ‐ | 405 | ⊕⊝⊝⊝ | SMD ‐0.41 (‐0.72 to ‐0.1) Effect sizes of the range 0.2 to 0.5 indicate a small treatment effect |
| Drug or alcohol use, or both following treatment completion As assessed by the TLFB or CIDI. High scores indicate greater symptom severity | ‐ | The mean drug/alcohol use following treatment completion in the intervention groups was | ‐ | 388 | ⊕⊝⊝⊝ | SMD ‐0.13 (‐0.41 to 0.15) Not significant |
| Treatment completers | Study population | RR 0.80 | 316 | ⊕⊕⊝⊝ | Indicates higher drop‐out in the intervention group | |
| 761 per 1000 | 609 per 1000 | |||||
| Moderate | ||||||
| 718 per 1000 | 574 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Quality of evidence downgraded by one point because the risk of bias in most trials was high or unclear in several domains. SUD based adjunctive therapy was not a formal part of either the experimental or control condition in one study (Coffey 2006). However, participants were recruited through an SUD based service and it is likely that they would have had access to adjunctive SUD‐ based therapy on an informal basis. All other studies in this comparison included formal access SUD‐based adjunctive therapy. | ||||||
| Trauma‐focused psychological therapy compared to active psychological therapy for SUD only | ||||||
| Patient or population: Individuals with post‐traumatic stress disorder and comorbid substance use disorder | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Active psychological therapyfor SUD only | Individual‐based psychological therapyincluding a trauma‐focused component | |||||
| PTSD severity following treatment completion As assessed by the CAPS. High scores indicate greater symptom severity | ‐ | The mean PTSD severity following treatment completion in the intervention groups was | ‐ | 46 | ⊕⊕⊝⊝ | Not significant |
| Drug or alcohol use, or both following treatment completion As assessed by the TLFB. High scores indicate greater symptom severity | ‐ | The mean drug/alcohol use following treatment completion in the intervention groups was | ‐ | 46 | ⊕⊕⊝⊝ | Not significant |
| Treatment completers | Study population | RR 1 | 62 | ⊕⊕⊝⊝ | Not significant | |
| 724 per 1000 | 724 per 1000 | |||||
| Moderate | ||||||
| 724 per 1000 | 724 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Quality of evidence downgraded by two points because findings were based on outcomes from one study with a small sample size. SUD based adjunctive therapy was not a formal part of either the experimental or control condition in the study contributing to this comparison. | ||||||
| Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only compared to control intervention | ||||||
| Patient or population: Individuals with post‐traumatic stress disorder and comorbid substance use disorder | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| TAU/minimal intervention | Group or Indvidual based non‐trauma‐focused psychological therapy | |||||
| PTSD severity following treatment completion ‐ Individual‐based intervention As assessed by the CAPS. High scores indicate greater symptom severity | ‐ | The mean PTSD severity following treatment completion in the intervention groups was | ‐ | 44 | ⊕⊕⊝⊝ | SMD ‐0.22 (‐0.83 to 0.39) |
| PTSD severity following treatment completion ‐ Group‐based intervention As assessed by the CAPS or IES‐R. High scores indicate greater symptom severity | ‐ | The mean PTSD severity following treatment completion in the intervention groups was | ‐ | 513 | ⊕⊕⊝⊝ | SMD ‐0.02 (‐0.19 to 0.16) |
| Drug or alcohol use, or both following treatment completion ‐ Individual‐based intervention | ‐ | No data | ‐ | ‐ | ‐ | Not estimable |
| Drug or alcohol use, or both following treatment completion ‐ Group‐based intervention As assessed by the ASI, TLFB or CIDI. High scores indicate greater symptom severity | ‐ | The mean drug/alcohol use following treatment completion in the intervention groups was | ‐ | 464 | ⊕⊝⊝⊝ | SMD ‐0.41 (‐0.97 to 0.14) Not significant |
| Treatment completers ‐ Individual‐based intervention | ‐ | No data | ‐ | ‐ | ‐ | Not estimable |
| Treatment completers ‐ Group‐based intervention | Study population | RR 1.13 | 381 | ⊕⊕⊝⊝ | ‐ | |
| 538 per 1000 | 608 per 1000 | |||||
| Moderate | ||||||
| 493 per 1000 | 557 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Quality of evidence downgraded by two points because findings were based on outcomes from one study with a small sample size. The individual‐based study (Mueser 2008) in this comparison did not include access to SUD based adjunctive therapy. Participants in all other studies were able to access SUD‐based adjunctive therapy. | ||||||
| Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only compared to active psychological therapy for SUD only | ||||||
| Patient or population: Individuals with post‐traumatic stress disorder and comorbid substance use disorder | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Active psychological therapyfor SUD only | Individual‐based combined non‐trauma‐focused psychological therapy | |||||
| PTSD severity following treatment completion As assessed by the CAPS. High scores indicate greater symptom severity | ‐ | The mean PTSD severity following treatment completion in the intervention groups was | ‐ | 128 | ⊕⊝⊝⊝ | SMD ‐0.26 (‐1.29 to 0.77) Not significant |
| Drug or alcohol use, or both following treatment completion As assessed by the SUI or ASI. High scores indicate greater symptom severity | ‐ | The mean drug/alcohol use following treatment completion in the intervention groups was | ‐ | 128 | ⊕⊕⊝⊝ | SMD 0.22 (‐0.13 to 0.57) Not significant |
| Treatment completers | Study population | RR 0.91 | 128 | ⊕⊝⊝⊝ | Not significant | |
| 618 per 1000 | 563 per 1000 | |||||
| Moderate | ||||||
| 591 per 1000 | 538 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Quality of evidence downgraded by one point because the risk of bias in most trials was high or unclear in several domains. Both studies in this comparison involved access to adjunctive SUD‐based therapy. | ||||||
Background
Description of the condition
Post‐traumatic stress disorder (PTSD) is a relatively common and well‐recognised psychiatric disorder that occurs following a major traumatic event (NCCMH 2005). Characteristic symptoms include re‐experiencing phenomena such as nightmares and recurrent distressing thoughts of the event, avoidance and numbing of general responsiveness such as trying not to talk about or be reminded of the traumatic event, experiencing detachment and estrangement from other people, and hyperarousal symptoms including sleep disturbance, increased irritability, and hypervigilance (APA 2013).
Substance use disorder (SUD) is defined as a complex behavioural disorder characterised by preoccupation with obtaining alcohol or other drugs and a narrowing of behavioural repertoire towards excessive consumption and loss of control over consumption. It is usually also accompanied by the development of tolerance to the substances being consumed and withdrawal and impairment in social and occupational functioning (APA 2013). In diagnostic terms, SUD is characterised by maladaptive misuse of substances (such as alcohol, amphetamines, cannabis, cocaine, hallucinogens, opioids, inhalants, phencyclidine, sedatives, hypnotics, and anxiolytics), which leads to clinically significant impairment or distress (APA 2013). Impairment might include increased tolerance, excessive prolonged usage, recurrent failure to meet important responsibilities, recurrent use in situations when this is likely to be physically dangerous, inability to reduce or limit usage, and considerable time spent obtaining substances or recovering from their effects.
Comorbidity between PTSD and SUD is common (Chilcoat 2003; Ford 2007; Reynolds 2005; Schäfer 2007). Epidemiological studies show significantly increased rates of PTSD amongst individuals with SUD (for example Chilcoat 1998a; Chilcoat 1998b; Cottler 1992; Dragan 2007; Driessen 2008; Helzer 1987; Mills 2006; Najavits 1998; Reynolds 2005; Reynolds 2011; Schäfer 2010), with the prevalence of lifetime PTSD ranging from 26% to 52% and prevalence of current PTSD from 15% to 42% (Driessen 2008; Reynolds 2011; Schäfer 2007; Schäfer 2010). In the Australian National Survey of Health and Wellbeing, Mills 2006 found opiates, sedatives, and amphetamines to be the drug groups to have most frequent comorbid PTSD. SUDs have also been found to be prevalent amongst individuals with PTSD (Chilcoat 2003; Jacobsen 2001; Mills 2006). In PTSD‐diagnosed samples, prevalence rates of comorbid substance abuse range from 19% to 35% and comorbid alcohol abuse from 36% to 52% (Breslau 1992; Kessler 1995; Pietrzak 2011), with estimates being even higher in some clinical populations, such as military veterans (Jacobsen 2001; Keane 1990; Kulka 1990; McDevitt‐Murphy 2010; Ruzek 2003). In a large epidemiological study of over 34,000 individuals in a community sample in the USA, Pietrzak 2011 found that 6.4% of the sample met lifetime diagnosis for full PTSD. Comorbidity was common across the PTSD sample (some 2463 individuals), with 46.4% meeting diagnosis for any alcohol or drug use disorder, 41.8% meeting diagnosis for alcohol abuse or dependence, and 22.3% meeting diagnosis for drug use or dependence. In another large epidemiological study, Kulka 1990 found that 73% of Vietnam veterans who met the diagnosis for PTSD qualified for a lifetime diagnosis of alcohol abuse or dependence. The Australian National Survey of Health and Wellbeing found that 34.4% of those with PTSD also had an SUD, most commonly an alcohol use disorder (24.1%) (Mills 2006). A number of other subgroups have been found to have particularly high rates of comorbidity of PTSD and SUD. Such groups include women, adolescents, the homeless, prisoners, gays and lesbians, rescue workers, sex workers, and victims of domestic violence (Najavits 2006).
Individuals with both disorders have also been found to have a more severe clinical profile than those with either disorder alone, lower general functioning, poorer well‐being, and worse outcomes across a variety of measures (Schäfer 2007). Such individuals are also more likely to meet additional criteria for other psychiatric disorders, such as affective disorders, anxiety disorders, and personality disorders (Mills 2006; Schäfer 2007). For these reasons, randomised controlled trials evaluating PTSD treatment therapies routinely exclude individuals with substance misuse‐related problems (Ouimette 2003b). A number of authors have called for greater understanding of the impact of this comorbidity on treatment outcomes and research to determine which therapies are most effective in treating these comorbid conditions (for example Mills 2006; Ouimette 2003a; Ouimette 2003b; Ouimette 2003c).
Description of the intervention
There are a number of established and evidence‐based forms of psychological therapies for both PTSD and SUD (van Dam 2012). Several forms of trauma‐focused cognitive behavioural therapy (TF‐CBT) have been demonstrated to be effective in treating PTSD (Bisson 2013; Bradley 2005). Evidence‐based therapies include prolonged exposure, cognitive processing therapy, brief eclectic psychotherapy, and cognitive therapy. A common component of these trauma‐focused therapies is that they include some form of guided exposure to the traumatic memory. For example, prolonged exposure involves asking the patient to relive the trauma imaginally. This is often conducted by creating a detailed present‐tense account of exactly what happened during the traumatic event, making an audio recording of it, and asking the individual to listen to this over and over again. Other common components of TF‐CBT include in vivo exposure to feared situations and cognitive therapy focused on distorted thinking and beliefs. Variants of these TF‐CBT models have been developed for specific subgroups. For example, narrative exposure therapy was developed for use with refugees and those who have been exposed to war and violent conflict, and skills training in affective and interpersonal regulation and narrative story telling (STAIR/NST) was developed for individuals with a history of childhood trauma. Eye movement desensitisation and reprocessing (EMDR) has also been well established as an intervention for PTSD (Bisson 2013). EMDR involves the PTSD sufferer focusing on a traumatic image, thought, emotion, and a bodily sensation whilst receiving bilateral stimulation most commonly in the form of eye movements. There is also evidence for the efficacy of stress management training in the treatment of PTSD, although treatment effects have not been demonstrated to be as great as for TF‐CBT‐based interventions or EMDR (Bisson 2013). Concerns remain about the applicability of these types of treatments to complex cases (Ruscio 2006). Studies evaluating interventions for PTSD have typically excluded those individuals with certain complexities such as SUD, suicidality, serious self harm, homelessness, and serious mental illness, and a recent meta‐analysis suggests that the benefits of specific interventions are smaller for individuals with more complex clinical problems (Gerger 2014). This study also highlighted the possible benefits gained from non‐specific interventions. A key principle of treatment that is endorsed by many expert clinicians in the trauma field is that treatment for individuals with complex PTSD presentations should be phased (Herman 1992), with an emphasis on interventions aimed at promoting a sense of safety and stabilisation of symptoms through improving self management and emotional regulation prior to the onset of trauma‐focused intervention (Cloitre 2011).
Cognitive behavioural therapies are also considered to be effective for SUD (Knapp 2007; van Dam 2012). A number of interventions based on the principles of CBT or behaviour therapy have been found to be effective for those with drug and alcohol problems. These include coping‐skills training, relapse prevention, contingency management, and behavioural couples therapy. Coping‐skills training and relapse prevention approaches are aimed at strengthening adaptive coping skills and reducing the risk of relapse in high‐risk or challenging situations. Contingency management is based on principles of operant conditioning. It aims to encourage adaptive abstinence‐focused behaviours through means of positive incentives. Contingency management has been found to be effective in the treatment of cocaine and stimulant misuse (Knapp 2007), and there is some evidence of effectiveness with opioid users (Mayet 2004). Behavioural couples therapy (BCT) recognises that interpersonal and relationship factors are often associated with relapse. In common with other cognitive behavioural therapies, BCT seeks to improve behavioural self control and develop new coping skills to facilitate and maintain abstinence. It also seeks to improve general relationship functioning and partners' coping with drinking or drug use‐related situations. BCT has been found to be effective at reducing frequency of usage, reducing negative consequences of use, and increasing relationship satisfaction in a number of studies with alcohol, opiate, and poly‐substance users (Powers 2008). Other popular psychosocial models for treating addiction include motivational interviewing (MI) and 12‐step approaches. MI is a widely used intervention in many addiction services. MI is a semi‐directive method for enhancing intrinsic motivation to change by exploring and resolving ambivalence through Socratic questioning and cognitive behavioural strategies. There is some evidence for the effectiveness of MI in reducing substance use in a number of studies (Smedslund 2011). One of the most widely used intervention programmes for alcohol misuse and dependence is the 12‐step approach, originally developed by Alcoholics Anonymous. The 12‐step approach consists of a brief, structured, manual‐driven approach to facilitating recovery from alcohol abuse, intended to be implemented over 12 to 15 sessions. Some 12‐step approaches include a spiritual approach, some are led by a professional, and others are led by former alcohol dependents. In a Cochrane review of the 12‐step approach, Ferri 2006 concluded that there was no strong evidence for effectiveness in reducing alcohol dependence, although the programme remains popular.
For various reasons, individuals with PTSD and SUD comorbidity are perceived as being more difficult to treat than individuals with either condition alone (Najavits 2002a; Schäfer 2007). This comorbidity is associated with poorer recruitment and retention in treatment programmes (Foa 2010; Najavits 2002a; Schäfer 2007), poorer treatment outcomes (Berenz 2012; Najavits 2002a; Ouimette 2003a; Ouimette 2003b; Reynolds 2005; Schäfer 2007), poorer treatment adherence, and shorter periods of abstinence post‐treatment (Brown 2003). Despite high prevalence levels, adults in treatment for SUD are frequently not assessed for PTSD (Mills 2006), or offered PTSD‐based interventions (Ford 2007; Ouimette 2003b; Reynolds 2005). There is a paucity of evidence for recommendations about treatment interventions for affective or anxiety disorders that are comorbid with SUD (Watkins 2005; Wilson 2008). In practice, a wide range of pharmacological and psychological therapies are used to treat the comorbidity. A concern for many treating clinicians related to intervention with some pharmacological agents such as benzodiazepines, is that patients might abuse these agents. In recognition of the clinical challenges involved in treating individuals with comorbid PSTD and SUD, a number of specialised psychological therapy approaches have been developed over the past 15 years or so. Three different types of treatment approach are identified in the literature (Gulliver 2010; Weiss 1995a): sequential, concurrent, and integrated. In sequential approaches, one comorbidity ‐ usually substance misuse ‐ is treated first, and the other ‐ usually PTSD ‐ afterwards. One sequential model to have received some attention is 'Transcend', a partially inpatient hospital‐based model (Donovan 2001). With concurrent approaches, each condition is treated separately but simultaneously using established evidence‐based interventions for each condition (Brady 2001; Triffleman 1999). One example of a concurrent approach is concurrent treatment of PTSD and substance use disorders using prolonged exposure (COPE) (Back 2001; Mills 2007). COPE uses cognitive behavioural therapy for substance use throughout the duration of the 13 treatment sessions and prolonged exposure for PTSD from around session five (Foa 1998). Integrative approaches treat both conditions together using interventions to address both disorders at the same time. Amongst integrative models, 'Seeking Safety' has probably received the most attention, with a number of randomised and non‐randomised evaluative studies (Najavits 2002b; Najavits 2007). Seeking Safety is a skills‐based therapy that aims to develop adaptive cognitive, behavioural, and interpersonal coping. Seeking Safety can be delivered on an individual basis or via groups.
Treatment interventions for PTSD and comorbid SUD have recently become a topic for review, in Berenz 2012 and Najavits 2013, and systematic review (Torchalla 2012; van Dam 2012). These reviews suggest some positive preliminary findings in relation to integrated and trauma‐focused psychological therapies for comorbidity. Najavits 2013, Torchalla 2012, and van Dam 2012 based their conclusions on evidence from both controlled and non‐controlled trials. All of these reviews identified significant methodological limitations in the studies reviewed. Several recently published controlled trials were not included in any of these reviews.
How the intervention might work
A number of different explanations for the relationship between SUD and PTSD have been proposed (Meyer 1986; Schäfer 2007). The most widely supported explanation is that PTSD influences the development of SUD, through means such as self medication (Schäfer 2007). Other explanations include the possibility that problematic substance use increases the risk of being exposed to trauma and increases psychological vulnerability to the effects of trauma (Meyer 1986; Schäfer 2007).
psychological therapies may therefore effect change in symptoms and functioning in such individuals through a number of different mechanisms. One potential mechanism by which psychological therapies might work is the development of enhanced coping skills which may increase the ability to regulate negative emotions (Busuttil 2009), leading to increased capacity to tolerate traumatic memories and craving urges. Another potential mechanism is the processing of trauma memories (Ehlers 2000; Foa 1998) leading to a decreased need to 'self medicate'. Psychological therapies such as those based on cognitive behavioural therapy (CBT) are also likely to promote changes in thinking and belief systems underlying trauma memories, and beliefs and ideas about substance use (Ehlers 2000; Najavits 2002b). For example, such interventions may facilitate attitudinal change to substance misuse and aid increased understanding of cognitive and situational risk factors associated with patterns of drug taking or problematic drinking, particularly those associated with past trauma. Other change mechanisms might include the development and reinforcement of adaptive coping skills which support constructive coping with both conditions (Brown 2003). It is likely that different interventions will operate though different means of change.
Why it is important to do this review
A number of systematic reviews of interventions for PTSD have been published in the Cochrane Library. As already noted, Bisson 2013 (along with other reviews, for example Bradley 2005) has described fairly robust evidence for trauma‐focused CBT and EMDR as treatments for chronic PTSD, with emerging evidence for some non‐trauma‐focused CBT‐based interventions and trauma‐focused CBT‐based group interventions. Other Cochrane reviews have considered single‐session psychological ’debriefing’ to prevent PTSD (Rose 2002), multiple‐session early psychological therapies for the prevention of PTSD (Roberts 2009), early psychological therapies to treat acute traumatic stress symptoms (Roberts 2010), pharmacological treatments (Stein 2006), combined pharmacotherapy and psychological therapies for PTSD (Hetrick 2010), and psychological therapies for the treatment of PTSD in children and adolescents (Gillies 2012). Over 70 systematic reviews of interventions for SUD have been published in the Cochrane Library. Reviews of psychological therapies have considered psychosocial interventions for cocaine and psychostimulant amphetamines‐related disorders (Knapp 2007), psychosocial interventions for opiate abuse and dependence (Mayet 2004), motivational interviewing for substance abuse (Smedslund 2011), 12‐step programmes for alcohol dependence (Ferri 2006), and psychosocial interventions to reduce alcohol consumption in concurrent problem alcohol and illicit drug users (Klimas 2014).
The issue of how best to manage or plan intervention for individuals with comorbid PTSD and SUD is a challenging one for clinicians (Najavits 2002a), and there is no real consensus about best practice. Most diagnosis‐specific guidelines for PTSD and other mental health disorders are silent as to whether the specific treatment recommendation applies to co‐occurring disorders (Watkins 2005). As we have discussed, comorbidity is a frequent problem, and those individuals with comorbidity are more challenging for general mental health services, trauma specialists, and addiction services to treat (Schäfer 2007). In clinical practice, many clinicians still argue the addiction should be treated first (for example Busuttil 2009; Foa 2000; Zayfert 2007), or that abstinence is necessary before diagnosis and a management plan can be made (see Watkins 2005). The reality for many people with comorbidity is that they can frequently get passed between services with little co‐ordination of care (Najavits 2006). Watkins 2005 argues that there has been a broad shift in the literature towards more co‐ordinated treatment plans over recent years, although it is far from clear that there is strong evidence to support this shift or that it has translated into change in routine clinical practice. There is also contention about perceived high risk of adverse effects of psychological evidence‐based treatment therapies, such as eye movement desensitisation and reprocessing and prolonged exposure, with comorbid groups (see Watkins 2005). We hope this review will be able to shed some light on what evidence there is to support these different models and treatment approaches, in order to aid clinician decision making.
Objectives
To determine the efficacy of psychological therapies aimed at treating traumatic stress symptoms, substance misuse symptoms, or both in people with comorbid PTSD and SUD in comparison with control conditions (including usual care, waiting‐list conditions, and no treatment) and other psychological therapies.
Methods
Criteria for considering studies for this review
Types of studies
Any randomised or cluster‐randomised controlled trial that considers one or more defined psychological therapy aimed at reducing traumatic stress symptoms, SUD symptoms, or both. We did not use sample size and publication status to determine whether or not a study should be included. Studies published in all languages were eligible for inclusion.
We were willing to include for consideration studies using a cross‐over design (for example specified intervention aimed at reducing traumatic stress symptoms followed by intervention aimed at reducing substance use and vice versa), as we felt that this addresses issues of clinical debate. However, we identified no such studies.
Types of participants
Participant characteristics
We made no restriction on age, although we anticipated that most studies would focus on adult populations. We did not make decisions about inclusion or exclusion on the basis of gender or ethnicity.
Diagnosis
Any individual suffering from comorbid PTSD and SUD. Treatment studies of individuals with PTSD and associated disorders such as acute stress disorder have sometimes included individuals who met most but not all criteria for the condition. In light of this, a previous Cochrane review of psychological therapies for PTSD, Bisson 2013, specified that at least 70% of participants had to be diagnosed as suffering from PTSD according to the International Classification of Diseases (ICD), WHO 1993, or Diagnostic and Statistical Manual of Mental Disorders (DSM), APA 2013. We believe that the issue of inclusion of some individuals with subthreshold diagnosis is likely to occur in comorbid studies as well. For this review, we decided to set a more conservative limit that at least 80% of participants will have been diagnosed as suffering from PTSD according to DSM or ICD criteria. Similarly, at least 80% of participants met formal diagnostic criterion for a substance misuse disorder according to DSM, APA 2013, or equivalent ICD definitions, WHO 1993, based on codes F10 to F19, excluding F15 (caffeine) and F17 (tobacco). Codes F10 to F19 include mental and behavioural disorders due to use of alcohol (F10), opioids (F11), cannabinoids (F12), sedatives or hypnotics (F13), cocaine (F14), other stimulants (amphetamine) (F15), hallucinogens (F16), volatile solvents (F18), and multiple drug use and use of other psychoactive substances (F19). There was no restriction on the basis or severity of PTSD symptoms, type of traumatic event, or nature of substance use (including alcohol).
Comorbidities
We made no restriction on other comorbidity.
Setting
There was no restriction on the setting in which a study took place.
Subset data
Although we applied an 80% threshold for diagnosis of PTSD and SUD, we also decided that when we identified studies where a significant subset of participants met our inclusion criteria (below the 80% threshold), we would approach the study authors to see if we could obtain outcome data for the subset who met inclusion, if such information was not available in the study report. If we were able to obtain these data and other inclusion criteria were met, we would then include the data in the review. We made the decision to potentially include studies on this basis after the review protocol was published.
Types of interventions
Experimental interventions
We considered any experimental psychological therapy designed to reduce symptoms of PTSD, substance usage, or both.
For the purposes of this review, a psychological therapy included any specified non‐pharmaceutical intervention aimed at reducing traumatic stress symptoms, SUD, or both, offered by one or more health professional or layperson. Potential therapy categories included any of the following.
-
Trauma‐focused psychological therapy: any psychological therapy including trauma‐focused cognitive behavioural therapy (TF‐CBT) and eye movement desensitisation and reprocessing (EMDR), delivered to individuals with comorbidity. TF‐CBT includes any intervention that uses predominantly trauma‐focused cognitive, behavioural, or cognitive‐behavioural techniques. This category includes individual exposure therapy and specialised treatment packages such as concurrent treatment of PTSD and substance use disorders using prolonged exposure (COPE), which include interventions for SUD (Back 2001; Mills 2007), and group approaches such as 'Transcend' (Donovan 2001). Individual trauma‐focused interventions for PTSD have been found to be more effective than group‐based intervention (Bisson 2013). We therefore made a post hoc decision to present and analyse individual‐ and group‐based trauma‐focused approaches separately.
-
Non‐trauma‐focused therapy for both PTSD and SUD or PTSD or SUD only: any psychological therapy including CBT aimed at addressing symptoms of PTSD and SUD on a sequential or integrated basis that does not include treatment of PTSD symptoms through a trauma‐focused or exposure‐based therapy. Interventions are likely to be targeted at increasing knowledge through psychoeducation and on improving coping skills. This category includes Seeking Safety (Najavits 2002b), which can be delivered on an individual basis or through groups. Group interventions are generally considered to show weaker effects than individual interventions (Najavits 2014 [personal communication]). We made a post hoc decision to present and analyse individual‐ and group‐based non‐trauma‐focused approaches separately.
-
Active psychological therapy for SUD only. This includes structured therapeutic programmes based on CBT, 12‐step, contingency management, and reinforcement‐based therapies. It also includes interventions based on motivational interviewing and psychological therapies aimed at management of cravings or to achieve abstinence.
The experimental intervention could be delivered as a monotherapy or as an adjunct to an established treatment that was received (in an identical way) by participants in both the experimental and the comparator group, for example TF‐CBT plus CBT for SUD versus CBT for SUD alone.
Comparator interventions
-
A control intervention included no intervention or any minimal intervention such as a waiting‐list control, treatment as usual, minimal or placebo condition.
-
An alternative active psychological therapy as described above.
Types of outcome measures
Primary outcomes
1. Severity of traumatic stress symptoms using a standardised measure such as the Clinician Administered PTSD Symptom Scale (CAPS) (Blake 1995), the Impact of Event Scale (Horowitz 1979), the Davidson Trauma Scale (Davidson 1997), or the Post‐Traumatic Diagnostic Scale (Foa 1997a). In circumstances where an individual study utilised both a clinician‐administered and a self report measure, primacy was given to outcomes using the clinician‐administered measure, as such measures are considered to provide the 'gold standard' in the traumatic stress field (for example Foa 1997b).
2. Reduction in drug use, alcohol use, or both as measured by a standardised measure such as the Addiction Severity Index (ASI) (McLellan 1992), the Substance Use Inventory (Weiss 1995b), the Opiate Treatment Index (Darke 1992), the Severity of Drug Dependence Scale (Gossop 1995), or the Substance Abuse Module (Haro 2006), or biological markers of drug and alcohol use, such as urine, saliva, and hair analysis, or self reported days of substance use/abstinence within a specified period such as the Timeline Followback Interview (Sobell 1995). There is less consensus about gold‐standard outcomes in the addiction field. We prioritised outcomes in the order of standardised instruments, followed by biological markers, followed by self report measures.
3. Treatment completion as measured by number of participants who were identified as treatment completers by study authors. We undertook to interpret drop‐out data with caution, as it is recognised that participants can withdraw from studies for various and complex reasons and reported drop‐out can be influenced by experimental factors related to practice of the research team (Loke 2011).
Secondary outcomes
4. PTSD diagnosis after treatment.
5. SUD diagnosis after treatment.
6. Adverse events reported by number and type.
7. Compliance, as measured by proportion of treatment sessions attended.
8. General functioning, including quality of life measures such as the 36‐Item Short Form Survey (SF‐36) (Ware 2003).
9. Use of health‐related resources (e.g. hospital admission, outpatient contacts, visits to primary care).
Timing of outcome assessment
When information was available primary outcomes were analysed at the following time points.
-
Immediately post‐treatment
-
3 to 4 months post‐treatment
-
5 to 7 months post‐treatment
-
8 to 11 months post‐treatment
-
12 months and beyond post‐treatment
Our primary outcome point was immediately post‐treatment. We analysed secondary outcomes only at this time point.
Search methods for identification of studies
The Cochrane Depression, Anxiety and Neurosis Review Group's Specialised Register (CCDANCTR)
The Cochrane Depression, Anxiety and Neurosis Group (CCDAN) maintains two clinical trials registers at their editorial base in Bristol, UK: a references register and a studies‐based register. The CCDANCTR‐References Register contains over 39,500 reports of randomised controlled trials (RCTs) in depression, anxiety, and neurosis. Approximately 60% of these references have been tagged to individual, coded trials. The coded trials are held in the CCDANCTR‐Studies Register, and records are linked between the two registers through the use of unique Study ID tags. Coding of trials is based on the EU‐Psi coding manual, using a controlled vocabulary; please contact the CCDAN Trials Search Co‐ordinator for further details. Reports of trials for inclusion in the Group's registers are collated from routine (weekly), generic searches of MEDLINE (1950‐), EMBASE (1974‐), and PsycINFO (1967‐); quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL); and review‐specific searches of additional databases. Reports of trials are also sourced from international trials registers c/o the World Health Organization's trials portal (the International Clinical Trials Registry Platform (ICTRP)), pharmaceutical companies, and the handsearching of key journals, conference proceedings, and other (non‐Cochrane) systematic reviews and meta‐analyses.
Details of CCDAN's generic search strategies (used to identify RCTs) can be found on the Group's website.
Electronic searches
We conducted searches for Condition (PTSD) and Population (patients with comorbid substance abuse) to 11 March 2015.
1. CCDANCTR‐Studies Register
We searched the studies register using the following terms:
Condition = ("post‐traumatic stress disorders") AND Comorbidity = ("alcohol dependence" or "substance related disorders" or "substance abuse")
2. CCDANCTR‐References Register
We searched the references register using a more sensitive set of free‐text terms:
[Condition]
1. (PTSD or post‐trauma* or "post trauma*" or posttrauma* or "stress disorder*" or "combat disorder*" or "war neuros*")
2. (trauma* and (psycho* or stress*))
3. (stress* and (extreme or disorder*))
4. DESNOS
5. (1 or 2 or 3 or 4)
[Population: comorbid substance abuse]
6. ("substance use disorder*" or SUD)
7. "drug abuse"
8. (abuser* or abusing or addict* or depend* or habit* or misuse or user*)
9. (abuse and not (child* or sex*))
[Common drugs of abuse]
10. (adinazolam or aerosol* or alcohol* or alprazolam or amphetamin* or anthramycin or anxiolytic* or ativan or barbituat* or bentazepam or benzodiazepin* or bromazepan or brotizolam or buprenorphin* or camazepam or cannabi* or chlordiazepoxid* or cinolazepam or clobazam or clonazepam or clorazepam or clotiazepam or cloxazolam or cocaine* or codeine or crack or crystal or cyprazepam or depressant* or diacetylmorphin* or diazepam* or doxefazepam or ecstasy or estazolam or etizolam or fentanyl or flunitrazepam or flurazepam or flutazoram or flutoprazepam or fosazepam or gases or GHB or girisopam or halazepam or hallucinogen* or haloxazepam or heroin* or hydromorphone or hydroquinone or hypnotic* or inhalant* or ketamin* or ketazolam or librium or loflazepate or loprazolam or lorazepam or lormetazepam or LSD or marihuana* or marijuana* or MDMA or meclonazepam or medazepam or meperidine or mephedrone or mescalin* or metaclazepam or methadone or methamphetamin* or methaqualone or mexazolam or midazepam or midazolam or morphine* or narcotic* or nerisopam or nimetazepam or nitrazepam or nitrites or "nitrous oxide" or "n‐methyl‐3,4‐methylenedioxyamphetamine" or nordazepam or opiate* or opiod* or opium or oxazepam or oxazolam or oxazypam or oxycodone or oxzepam or painkiller* or "pain killer*" or PCP or pethidin* or phencyclidin* or pinasepam or prazepam or propazepam or propoxyphene or psilocybin or psychedelic* or psychoactive* or psychostimulant* or quinazolinone or ripazepam or ritalin or sedative* or serazepin* or solvent* or steroid* or stimulant* or substance* or temazepam or tetrazepam or tofisopam or tramadol or triazolam or triflubazam or valium or vicodin)
11. (drug* and (recreational or street))
12. (6 or 7 or 8 or 9 or 10 or 11)
[Condition + Population]
13. (5 and 12)
We performed a further search on 4 December 2015 (prior to publication). We screened results and placed studies of interest in those awaiting classification; we may include or exclude these in a future update to this review (as appropriate).
3. Cochrane Central Register of Controlled Trials (CENTRAL)
We also searched the Cochrane Central Register of Controlled Trials (CENTRAL) to 3 January 2015 (Appendix 1).
4. International trial registries
We searched the World Health Organization's trials portal (ICTRP) and ClinicalTrials.gov to identify additional unpublished or ongoing studies (11 March 2015 and 4 December 2015).
Searching other resources
We also checked reference lists of studies identified in the search, as well as related review articles and management guidelines. We conducted Internet searches of known websites, conference proceedings, and discussion for the following: American Association for the Treatment of Opioid Dependence (http://www.aatod.org/), DrugScope (http://www.drugscope.org.uk/), European Society for Traumatic Stress Studies (https://www.estss.org), International Harm Reduction Association (http://www.ihra.net/), International Society for Traumatic Stress Studies (http://www.istss.org), Society for the Study of Addiction (http://www.addiction‐ssa.org/), and the United Kingdom Psychological Trauma Society (http://www.ukpts.co.uk). We also searched studies included in the Cochrane review 'Psychological therapies for chronic post‐traumatic stress disorder (PTSD) in adults' (Bisson 2013), and reviews of psychological therapies undertaken for the Cochrane Drug and Alcohol Group. We searched studies within these reviews on the basis that a significant subset of participants might warrant inclusion.
Data collection and analysis
Selection of studies
Two review authors (NPR and PAR) independently read the abstracts of all potential trials. If an abstract appeared to represent an RCT, the two review authors independently read the full report to determine if the trial met the inclusion criteria. In case of disagreement, a third review author was consulted (JIB).
Data extraction and management
We used a data extraction sheet to capture data, which we then entered into Review Manager 5 software (RevMan 2011). Information extracted included demographic details of participants, details of the traumatic event, type of substance use, the randomisation process, the interventions used, drop‐out rates, and outcome data. Three review authors (NPR, PAR, and NJ) independently extracted data. In case of disagreement, the fourth review author was consulted (JIB).
Main planned comparisons
-
Trauma‐focused psychological therapy versus control intervention
-
Trauma‐focused psychological therapy versus non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only
-
Trauma‐focused psychological therapy versus active psychological therapy for SUD only
-
Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only versus control intervention
-
Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only versus active psychological therapy for SUD only
-
Active psychological therapy for SUD only versus control intervention
We undertook to present and analyse data for individual‐ and group‐based interventions separately.
Assessment of risk of bias in included studies
We assessed risk of bias using The Cochrane Collaboration’s 'Risk of bias' tool and reported the results in a standard 'Risk of bias' table. We assessed the following domains:
-
Sequence generation: Was the allocation sequence adequately generated?
-
Allocation concealment: Was allocation adequately concealed?
-
Blinding of participants, personnel, and outcome assessors for each main outcome or class of outcomes: Was knowledge of the allocated intervention adequately prevented during the study?
-
Incomplete outcome data for each main outcome or class of outcomes: Were incomplete outcome data adequately addressed?
-
Selective outcome reporting: Are reports of the study free of suggestion of selective outcome reporting?
-
Other sources of bias: Was the study apparently free of other problems that could put it at a high risk of bias?
We judged the risk of bias for each domain within and across studies, based on the following three categories:
-
low risk of bias;
-
unclear risk of bias;
-
high risk of bias.
Three review authors (NPR, PAR, and NJ) independently assessed risk of bias for each study. Any disagreements were initially to be discussed between the three rating review authors. Where disagreement persisted, advice was sought from the fourth review author (JIB).
Measures of treatment effect
We analysed continuous outcomes using mean difference when all trials had measured outcome on the same scale. When trials measured outcomes on different scales, we used the standardised mean difference. We used risk ratio as the main categorical outcome measure, as this is more widely used than odds ratio in health‐related practice. We presented all outcomes using 95% confidence intervals.
Unit of analysis issues
Cross‐over trials
We did not identify any cross‐over trials. However, we specified at the protocol stage that if we included such trials, we would include final outcomes from these trials where the study addressed order of intervention for trauma‐related intervention and control or management of SUD symptoms. For trials that had a cross‐over design that did not address these clinical pathway issues, we would only consider results from the first randomisation period. We decided that each stage of analysis would be stratified by treatment type and that further analysis would include follow‐up data where these were available. We would only make comparisons involving follow‐up data when outcome data were available for similar time points.
Studies with multiple treatment groups
We specified that if the trial had three (or more) arms, we would consider undertaking pair‐wise meta‐analysis with each arm, depending upon the nature of the intervention in each arm and its relevance to the review objectives. We aimed to avoid multiple comparisons to limit the risk of false‐positive results. When a study had three or more arms that were relevant to the review, we would consider the appropriateness of combining data from two arms if interventions were sufficiently similar or of using data from the arms of the trial that fit closest to the review objective. Decisions would follow the guidance provided in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), and we would report the rationale for any decisions made. In actuality, only one study included in the review had more than two treatment arms, and for reasons described below we only included two arms in comparisons.
Cluster‐randomised trials
We specified that management of cluster‐randomised trials would follow the guidance provided in the Cochrane Handbook. We identified no cluster‐randomised trials.
Dealing with missing data
When intention‐to‐treat (ITT) data were available, we reported this in the results. We attempted to access ITT data wherever possible. For dichotomous outcomes, we conducted ITT analysis by making imputations based on the assumption that all missing participants had a negative outcome. We included completer‐only data when this was the only data source available. In cases where there was inadequate information within a particular paper to undertake analysis, we made attempts to compute missing data from other information available within the paper, using guidance provided by Higgins 2011. For continuous data when only the standard error, t‐statistics, or P values were reported, we calculated standard deviations using the guidance provided by Higgins 2011. When imputation was not possible or when further clarification was required, we attempted to contact the authors to request additional information. In cases where no further useable data was available, we did not include the study in further analysis.
Assessment of heterogeneity
We initially used visual inspection of the forest plots to explore for possible heterogeneity. We also examined heterogeneity between studies by observing the I² statistic and Chi² test (P < 0.10). As suggested in the Cochrane Handbook (Higgins 2011), we took an I² of less than 30% to indicate mild heterogeneity, and we used a fixed‐effect model to synthesise the results. We considered an I² of 30% to 60% to indicate moderate heterogeneity and an I² of 60% to 90% substantial heterogeneity (Higgins 2011). Due to the level of clinical heterogeneity in the included studies, we decided to use a random‐effects model to summarise results including more than one study. We specified that where significant heterogeneity was present, we would attempt to explain the variation.
Assessment of reporting biases
We specified that if sufficient studies (10 or more) were available in a meta‐analysis, we would prepare funnel plots and examine them for signs of asymmetry (Egger 1997). We specified that if asymmetry was identified, we would consider possible reasons for this.
Data synthesis
In recognition of the substantial clinical heterogeneity between included studies, we pooled all data using a random‐effects model.
Subgroup analysis and investigation of heterogeneity
We specified that we would explore the following possible causes of clinical heterogeneity if data were sufficient to allow.
-
Specified treatment intervention model (e.g. Seeking Safety, Transcend, concurrent treatment of PTSD and substance use disorders using prolonged exposure (COPE)).
-
Specified treatment plans (e.g. sequential versus concurrent versus integrated approaches).
-
Participant subgroup (e.g. veterans versus victims of sexual, physical, and domestic violence versus childhood trauma versus rescue workers).
-
Specific substances of misuse (e.g. alcohol versus opioids versus cocaine versus amphetamines).
-
Intervention objectives (treating symptoms of PTSD versus SUD versus general well‐being/coping).
Sensitivity analysis
We specified that we would consider sensitivity analysis to explore possible causes of methodological heterogeneity if data were sufficient to allow. We would base analyses on the following criteria.
We would exclude trials considered most susceptible to bias based on the following quality assessment criteria:
-
those judged to be at high risk of bias or unclear risk of bias for allocation concealment;
-
high levels of postrandomisation losses (more than 40%) or exclusions;
-
unblinded outcome assessment or blinding of outcome assessment uncertain.
Summary of findings
We evaluated the quality of the available evidence of our findings using the GRADE approach (Guyatt 2011; Langendam 2013). We generated 'Summary of findings' tables using GRADEprofiler software (http://tech.cochrane.org/revman/gradepro) using data imported from Review Manager 5.3 (RevMan 2011). These tables provide outcome‐specific information concerning the overall quality of evidence from studies included in the comparison, the magnitude of effect of the interventions examined, and the sum of available data on the outcomes that were considered. We assessed the quality of evidence using five factors:
-
Limitations in study design and implementation of available studies;
-
Indirectness of evidence;
-
Unexplained heterogeneity or inconsistency of results;
-
Imprecision of effect estimates;
-
Potential publication bias.
For each outcome that included pooled data, we classified the quality of evidence for each outcome according to the following categories.
-
High quality: further research is very unlikely to change our confidence in the estimate of effect.
-
Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
-
Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
-
Very low quality: we are very uncertain about the estimate.
We downgraded the evidence from 'high quality' by one level for serious (or by two for very serious) study limitations (risk of bias), indirectness of evidence, serious inconsistency, imprecision of effect estimates, or potential publication bias. We included the primary outcomes of PTSD severity, drug and/or alcohol use, and treatment completion in the 'Summary of findings' tables.
Results
Description of studies
Results of the search
We conducted electronic searches to 11 March 2015 (with results fully incorporated into the review). We also contacted 42 trial investigators; see Appendix 2.
We identified 1099 references, 1057 of which remained after de‐duplication. Two review authors (NPR and PAR) independently screened the titles and abstracts of these records and excluded 885 that did not meet the inclusion criteria. For 3 of the remaining 172 study reports we were only able to obtain conference abstracts. We judged these studies as potentially relevant to the review, but were unable to undertake classification of these abstracts. Twelve references were for ongoing studies. We retrieved and inspected the full‐text papers for the remaining 157 reports, excluding 143 of them as not meeting our inclusion criteria. Thirteen of the remaining studies met the full inclusion criteria and so were included in the review. We also identified a number of studies with a significant subset of individuals who met all inclusion criteria. We were able to obtain data on this subset from the authors of one study (Mueser 2008), resulting in a total of 14 studies being included in the review. Thirteen of these 14 studies contributed to the quantitative synthesis. The study selection process is also detailed in our PRISMA flow diagram (see Figure 1).

Study flow diagram.
Note: We conducted a further search on 4 December 2015, prior to publication, but did not incorporate results at this time. We screened the abstracts (n = 72) and identified 4 new studies, which we've added to those awaiting classification. Two of these studies meet the eligibility criteria for this review (McGovern 2015; Perez‐Dandieu 2015), and a further two will do so if subset data is available (Barrett 2015; Wolf 2015). The December search also identified Stappenbeck 2015 (NCT00760994), which after contacting the trialists was confirmed to be the same trial as Simpson 2011 (already awaiting classification). We also identified an additional five ongoing study protocols (NCT01211106; NCT01457404; NCT01663337; NCT01849029; NCT02335125).
Included studies
We included 14 studies in this review, with characteristics as follows (see also Characteristics of included studies).
Design
All of the included studies were randomised controlled trials or pilot randomised controlled trials. One study was described as a laboratory‐based study investigating the effects of trauma‐focused intervention on alcohol craving elicited by trauma cues (Coffey 2006). One study had two intervention arms in which allocation was randomised (Hien 2004); a third control arm was added part way through the study, and allocation to this arm was made on a non‐randomised basis. We have not included data from this third arm in the review. Studies were randomised at the participant level and used a parallel‐group design.
Sample sizes
A total of 1506 participants were allocated to groups across the 14 included studies. The number of participants ranged from 29, in Norman unpublished, to 353, in Hien 2009. Three other studies had fewer than 50 participants (Coffey 2006; Najavits 2006a; Zlotnick 2009), with the subsample of 44 from a cohort of 108 in Mueser 2008. Three studies had 50 to 100 participants (Hien 2004 ‐ excluding the arm that was non‐randomised; McGovern 2011; Sannibale 2013), and the remaining six studies included more than 100 participants (Boden 2012; Coffey submitted; Foa 2013; Frisman 2008; Hien 2009; Mills 2012).
Setting
Twelve studies were conducted in the USA; the remaining two studies were carried out in Australia (Mills 2012; Sannibale 2013). The majority of studies recruited individuals from community outpatient substance abuse services. One study recruited from veteran outpatient substance abuse services (Boden 2012). Four studies also made use of advertisements or flyers (Foa 2013; Hien 2004; Mills 2012). Najavits 2006a also recruited from hospitals and schools. Sannibale 2013 recruited from a range of services. Coffey submitted recruited from a residential substance misuse service, and Zlotnick 2009 from the minimum‐security wing of a female prison. Mueser 2008 recruited from community mental health services. All participants were seen on an outpatient basis, apart from those in Zlotnick 2009, who received most of their intervention in prison, with some follow‐up on release.
Participants
All studies were of adults, apart from Najavits 2006a, who investigated intervention for adolescent girls with a mean age of 16.06 years. One study recruited from veteran populations with an all‐male cohort (Boden 2012). Zlotnick 2009 recruited female prisoners. Other studies with a female‐only cohort were Hien 2004, Hien 2009, Najavits 2006a, and Norman unpublished. All other studies were of mixed gender and from community groups. All studies met the minimum threshold of 80% of participants meeting full diagnosis for PTSD. Across all studies, 1387 (92.1%) of participants met full diagnosis for PTSD, with the remaining group being described as having subthreshold PTSD. All participants in all studies met minimum criteria for a substance use disorder. Coffey 2006, Coffey submitted, and Foa 2013 included people with alcohol dependence, and Norman unpublished and Sannibale 2013 included people with alcohol use disorder. The majority of participants in Coffey submitted were also drug dependent. The other 10 studies included people with substance abuse. Substance use in these studies was typically polydrug use, with many participants using multiple drugs. None of the included studies targeted one specific substance other than alcohol. The subsample in Mueser 2008 excluded people with substance dependence. Hien 2004 and Mills 2012 only included people with substance dependence, and the majority (93.9%) of participants in Najavits 2006a were also substance dependent.
Exclusion criteria were not identified in Frisman 2008. Most other studies excluded on the basis of current or acute psychosis, current suicidal/homicidal ideation, and significant cognitive impairment (for example resulting from dementia or brain injury). Hien 2009 also excluded on the grounds of past history of psychosis. Mueser 2008 was a study that was primarily interested in intervention for individuals with severe mental illness, and they only excluded individuals who were in psychiatric hospital. In recruiting participants with alcohol dependence, Foa 2013 excluded people with other substance dependence conditions. Sannibale 2013 excluded people with severe substance dependence. Mills 2012 excluded people who had a history of self harm in the past six months. Coffey 2006 excluded people with combat‐related PTSD. Coffey submitted excluded those who were in an abusive relationship at the time of recruitment, and Norman unpublished only included participants who had been out of an abusive relationship for at least a month. Hien 2004 and Hien 2009 excluded people with advanced‐stage medical diseases. Hien 2009 and McGovern 2011 excluded those involved in ongoing legal disputes. Najavits 2006a also excluded if people were mandated to treatment, or had characteristics that would interfere with treatment completion (mental retardation, homelessness, impending incarceration, or a life‐threatening illness). This was the only study to report on exclusion on the basis of homelessness. However, it is argued that people who are homeless are routinely excluded from these kinds of studies (Najavits 2014 [personal communication]).
Interventions
All of the experimental interventions included in the review were based on some form of cognitive behavioural therapy (CBT). Following van Dam 2012, these interventions can perhaps best be summarised and divided into trauma‐focused approaches ‐ some of which included combined interventions for SUD ‐ and non‐trauma‐focused interventions, which mainly involved integrated treatment of PTSD and SUD.
Trauma‐focused/combined interventions
Individual‐based trauma‐focused/combined interventions
Five studies included trauma‐focused/exposure‐based components as a part of the intervention program, delivered individually. Four studies tested combined coping skills‐focused intervention for SUD with exposure‐based interventions for PTSD as the experimental condition (Coffey submitted; Foa 2013; Mills 2012; Sannibale 2013). Coffey submitted compared 9 to 12 sessions imaginal and in vivo exposure plus treatment as usual against an equivalent health‐related psycho‐education intervention. Foa 2013 was a 2x2 study examining the effects of prolonged exposure and naltrexone. For psychological therapies, prolonged exposure plus supportive counselling was compared with supportive counselling alone. The supportive counselling intervention combined medication management with compliance enhancement techniques based on motivational interviewing. We considered this to be equivalent to a treatment‐as‐usual intervention. For medication, naltrexone was compared against a placebo. The numbers of participants receiving the two psychological therapies were equal in the two medication groups. Mills 2012 compared concurrent treatment of PTSD and substance use disorders using prolonged exposure (COPE) against treatment as usual for substance abuse only. COPE includes motivational enhancement and CBT for substance use; psycho‐education relating to both disorders and their interaction; in vivo exposure; imaginal exposure; and cognitive therapy for PTSD. Finally, Sannibale 2013 evaluated integrated CBT for PTSD and alcohol use disorder against CBT for alcohol use disorder and supportive counselling. The experimental condition in this trial included cognitive behavioural exposure‐based therapy for PTSD, based on a prolonged exposure model with cognitive restructuring, in addition to cognitive therapy for problem drinking. The control intervention had no PTSD components in it. Coffey 2006 tested an exposure‐based intervention that has been established for the treatment of PTSD, but recruited from within alcohol abuse services. They compared six sessions of imaginal exposure with six sessions of imagery‐based relaxation training, with the primary aim of evaluating effects on alcohol‐related craving.
Group‐based trauma‐focused/combined interventions
We identified no studies offering trauma‐focused intervention through groups.
Non‐trauma‐focused intervention
Individual‐based non‐trauma‐focused interventions
Four studies evaluated individual integrated PTSD/SUD intervention. One study compared an integrated PTSD/SUD intervention against treatment as usual for SUD (Najavits 2006a). The active condition in this trial was Seeking Safety plus treatment as usual. One study evaluated individual CBT against participants' usual psychiatric care (Mueser 2008). Treatment components included psycho‐education, cognitive restructuring, and generalisation training. As described previously, this study evaluated treatment of PTSD for people with serious mental illness and did not include a component focusing on SUD. Two studies evaluated an integrated PTSD/SUD intervention delivered on an individual basis against an alternative psychological therapy for SUD alone (Hien 2004; McGovern 2011). Hien 2004 compared Seeking Safety plus treatment as usual to a relapse prevention comparison condition and a non‐randomised treatment‐as‐usual arm, which we have not included in this review. McGovern 2011 compared integrated CBT plus treatment as usual (ICBT) with individual addiction counselling plus treatment as usual (IAC) as the control condition. There was no PTSD component to the IAC, which at 10 to 12 sessions was shorter than the 12‐ to 14‐session ICBT intervention, which included psycho‐education, cognitive restructuring, and generalisation training in relation to PTSD and SUD.
Group‐based non‐trauma‐focused interventions
Five studies evaluated group interventions, four of which included Seeking Safety, Najavits 2002b, plus treatment as usual as the active treatment condition (Boden 2012; Hien 2009; Norman unpublished; Zlotnick 2009). Seeking Safety is a structured cognitive behavioural treatment with both safety/trauma and substance use components integrated into each session. Its primary goal is to reduce both PTSD and SUD by focusing on safe coping skills addressed through cognitive, behavioural, interpersonal, and case management domains over 24 to 25 sessions. In two of these trials (Boden 2012; Zlotnick 2009), treatment as usual was the control condition. The intervention in Hien 2009 provided a partial dose of Seeking Safety with 12 sessions to cover the core components of the model. This study used a female health psycho‐education (Women's Health Education) comparison condition, which was delivered over the same number of sessions with the same level of attention given to participants. Norman unpublished included some components from cognitive trauma therapy for battered women with PTSD (CTT‐BW) (Kubany 2004). The control condition in this study was a minimal‐intervention therapist‐led supportive 12‐step group. The fifth study to evaluate a group‐based integrated program was Frisman 2008. This study compared TARGET, an 8‐ to 9‐week intervention that aims to improve adaptive coping skills, with treatment as usual for SUD only.
A fuller description of interventions can be found in the Characteristics of included studies tables.
Comparisons
The included studies compared:
-
psychological therapy versus 'control' (as defined in Types of interventions);
-
psychological therapy versus other psychological therapy (as defined in Types of interventions).
We made the following specific comparisons:
-
Trauma‐focused psychological therapy versus control intervention
-
Individual‐based therapy: Coffey 2006; Coffey submitted; Foa 2013; Mills 2012.
-
Group‐based therapy: No studies.
-
-
Trauma‐focused psychological therapy versus active psychological therapy for SUD only
-
Individual‐based intervention: Sannibale 2013.
-
Group‐based intervention: No studies.
-
-
Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only versus control intervention
-
Individual‐based intervention: Mueser 2008; Najavits 2006a.
-
Group‐based intervention: Boden 2012; Frisman 2008; Hien 2009; Norman unpublished; Zlotnick 2009.
-
-
Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only versus active psychological therapy for SUD only
-
Individual‐based intervention: Hien 2004; McGovern 2011.
-
Group‐based intervention: No studies.
-
Outcomes
PTSD outcomes
Of the 14 studies, 10 used a clinician‐administered measure of PTSD (Coffey submitted; Foa 2013; Hien 2004; Hien 2009; McGovern 2011; Mills 2012; Mueser 2008; Norman unpublished; Sannibale 2013; Zlotnick 2009). In nine cases, this was the Clinician Administered PTSD Symptom Scale (CAPS) (Blake 1995). The Impact of Event Scale ‐ Revised (IES‐R), Weiss 1997, was the primary PTSD outcome measure in two studies (Boden 2012; Coffey 2006). Frisman 2008 used the Post‐Traumatic Cognitions Inventory, which is a measure of trauma‐related beliefs. We considered this to be a reasonable proxy to a PTSD outcome measure.
SUD outcomes
A range of measures were used to assess outcomes for SUD. These included the Timeline Followback Interview (Sobell 1995), which was used in five studies (Coffey submitted; Foa 2013; Norman unpublished; Sannibale 2013; Zlotnick 2009); the Addiction Severity Index (ASI) (McLellan 1992), used in three studies (Boden 2012; McGovern 2011; Zlotnick 2009); the Composite International Diagnostic Interview for DSM–IV (Robins 1989), used in three studies (Hien 2009; Mills 2012; Mueser 2008); and the Substance Use Inventory (Weiss 1995b), used in two studies (Hien 2004; Hien 2009). Toxicology screens were administered in Hien 2009 and McGovern 2011. Some studies used several SUD measures. In meta‐analysis we included outcomes according to the specifications described in Types of outcome measures. Some studies also included outcomes for both alcohol use and drug use. In such cases we included the outcome that was most associated with the treatment condition (that is where alcohol was identified as the key comorbidity, we included the alcohol outcome, and where SUD was identified as the key comorbidity, we included the SUD outcome).
Treatment completion
Many of the included studies recognised high levels of treatment drop‐out as a pervasive problem in the field (for example Hien 2004; Mills 2012). Definitions of the number of sessions attended for a participant to be considered a completer varied across studies. We used the definition of treatment completer provided by each study to undertake analyses of treatment acceptability. Boden 2012, Foa 2013, Mills 2012, Najavits 2006a, and Zlotnick 2009 provided no definition, although Mills 2012 provided data on the number of participants who attended at least one exposure session and the number attending all 13 treatment sessions. Hien 2004 and Norman unpublished identified a "minimum dose" as 25% of sessions attended. Hien 2009, Mueser 2008, and Sannibale 2013 specified a completer as an participants who had attended 50% of sessions. Definitions in the range of 70% to 80% of sessions were described in Coffey submitted, Frisman 2008, and McGovern 2011, and 100% of sessions was described in Coffey 2006.
Secondary outcomes
PTSD diagnostic status was reported in Coffey submitted, McGovern 2011, Mills 2012, Norman unpublished, Sannibale 2013, and Zlotnick 2009. SUD diagnostic status was reported only in Mills 2012. Adverse effects were reported by Boden 2012, Foa 2013, Hien 2009 (see Killeen 2008), Mills 2012, and Norman unpublished. Compliance as measured by the mean number of sessions attended was frequently reported, although some studies only reported attendance for the experimental group (Hien 2004; Najavits 2006a; Zlotnick 2009). General functioning was not evaluated in any study. Use of health‐related resources (other service utilisation) was evaluated in Najavits 2006a, but was not clearly reported.
Timing of outcome assessment
All included trials apart from Frisman 2008 reported PTSD and SUD as a continuous outcome at the end of treatment. Long‐term follow‐up data ranging from 3 to 12 months was reported in all studies except Coffey 2006. Follow‐up data was available at 3 months from the end of treatment in Boden 2012, Coffey submitted, Hien 2004, Hien 2009, McGovern 2011, Mueser 2008, Najavits 2006a, and Zlotnick 2009; at 5 to 6 months post‐treatment in Coffey submitted, Foa 2013, Frisman 2008, Hien 2004, Hien 2009, Mills 2012, Mueser 2008, Sannibale 2013, and Zlotnick 2009; at 9 months in Sannibale 2013; and at 12 months in Frisman 2008 and Hien 2009. We note that Mills 2012 reported their follow‐up points at 6 weeks, 3 months, and 9 months from baseline. As the planned intervention period was 3 months, we took the 3‐month follow‐up point as the end of treatment and the 9‐month follow‐up point as 6‐month follow‐up post‐treatment. However, some participants did continue to receive therapy more than three months after baseline assessment.
Excluded studies
See Characteristics of excluded studies.
We identified 172 studies as being potentially eligible for this review after initial screening, of which 143 were excluded after closer examination. Of these, 21 did not meet study design criteria (that is not RCTs). We excluded 49 on the basis that less that 80% of the sample met diagnosis for PTSD. In some of these studies PTSD was not assessed at all. Five of these 49 studies assessed for traumatic stress symptoms, but a formal and reliable diagnosis of PTSD was not established (for example Ford 2011; Ghee 2009). We excluded 12 studies because less than 80% of the sample met diagnosis for SUD. We excluded seven studies evaluating interventions in trauma‐exposed people with significant SUD history (for example van Dam 2013) on the basis that less than 80% of the sample met diagnosis for PTSD and SUD. Four studies did not provide outcomes that were either PTSD or SUD related, three studies did not evaluate a psychological therapy, and one study evaluated the addition of sertraline to a psychological therapy (Hien 2015). Twenty‐seven studies were companion papers to studies included in this review. The remaining 19 studies were conference abstracts related to other studies that were either included in or excluded from the review.
Ongoing studies
See Characteristics of ongoing studies.
We identified 12 ongoing studies as being of potential relevance to this review (to March 2011) via the World Health Organization's trials portal (ICTRP) and ClinicalTrials.gov and through a published protocol (DRKS00004288; NCT00946322; NCT01029197; NCT01186315; NCT01274741; NCT01338506; NCT01357577; NCT01365247; NCT01597856; NCT01693978; NCT02081417; NTR3084). Interventions currently being evaluated include Seeking Safety plus treatment as usual (TAU) in a Dutch population (planned recruits 130) (NTR3084), a multicentre trial of Seeking Safety versus structured relapse prevention versus TAU (DRKS00004288), a trial of Seeking Safety versus a past‐focused integrated CBT‐based therapy for PTSD and SUD (planned recruits 52) (NCT01274741), a trial of peer‐led versus clinician‐led Seeking Safety (NCT02081417), a trial of CBT in 160 military veterans (NCT01357577), a 3‐arm trial comparing CBT (including prolonged exposure) with relapse prevention and TAU for PTSD and SUD (planned recruits 168) (NCT01365247), a trial of COPE in military veterans (planned recruits 90) (NCT01338506), a trial of prolonged exposure versus prolonged exposure with contingency management for drug users with PTSD (NCT01693978), a trial of prolonged exposure versus prolonged exposure plus virtual reality‐based exposure to addiction cues (NCT01186315), a trial of group and individual CBT and exposure for people with serious mental illness (NCT01029197), a phase 1 trial of couple‐based treatment of PTSD and alcohol use disorder (NCT00946322), and a phase 1 trial evaluating a screening, motivation enhancement, and referral program for US veterans seeking pension and compensation benefits (NCT01597856).
A further search of the trial registries (4 December 2015), prior to publication, identified five additional ongoing studies (NCT01211106; NCT01457404; NCT01663337; NCT01849029; NCT02335125).
Studies awaiting classification
See Characteristics of studies awaiting classification.
We identified these studies through records in clinical trial registries and conference abstracts, but could not identify or access full‐text reports (to 11 March 2015). We have not yet formally evaluated these studies for eligibility, and may include or exclude them in a future update of this review. We initially identified three such studies (Park 2012; Simpson 2011; Skidmore 2013). Park 2012 have evaluated an integrated chronic disease management intervention in a primary care setting for people with SUD and a range of co‐occurring mental disorders. Of the 553 total participants, 204 are reported to have met diagnosis for PTSD at baseline. Simpson 2011 sought to evaluate the feasibility of a methodology focused on deciphering mechanisms of change for decreasing alcohol use and PTSD symptomatology in people with current PTSD and alcohol dependence. Participants were assigned to one of three brief interventions (acceptance, cognitive restructuring, or attention placebo); 84 participants were reported to have been randomised (a report describing the main outcomes of this study has subsequently been published (Stappenbeck 2015)). Skidmore 2013 evaluated integrated cognitive behavioural therapy (ICBT) versus cognitive processing therapy, an established and evidence‐based intervention for PTSD, in a group of 153 participants with co‐occurring alcohol or substance dependence, depression, and trauma exposure. It is unclear whether a subgroup of participants met diagnosis for PTSD.
A further search of the Cochrane Depression, Anxiety and Neurosis Review Group's Specialised Register (4 December 2015), prior to publication, identified four additional studies (added to those awaiting classification). Two met the eligibility criteria for this review (McGovern 2015; Perez‐Dandieu 2015), and a further two will also meet the eligibility criteria if subset data are available (Barrett 2015; Wolf 2015).
Risk of bias in included studies
For details of the 'Risk of bias' judgements for each study, see Characteristics of included studies. Graphical representations of the overall risk of bias in included studies are presented in Figure 2 and Figure 3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Eight studies specified the method of sequence generation and were judged as being at low risk of bias (Boden 2012; Coffey submitted; Frisman 2008; Hien 2009; Mills 2012; Mueser 2008; Norman unpublished; Sannibale 2013). The method of allocation was unclear in the remaining studies. Of the nine studies that adequately reported method of sequence generation, we judged five as also describing their method of allocation adequately (Boden 2012; Hien 2009; Mills 2012; Mueser 2008; Sannibale 2013). We were unclear about the process of sequence generation and allocation for Najavits 2006a, but received additional information from the lead author that allowed us to judge that these were of low risk. The process of sequence generation and allocation were unclear in the remaining studies.
Blinding
In trials of psychological therapy participants cannot normally be blind to the treatment allocation. We therefore classified all trials as being at high risk of performance bias. Eight trials included blinding of the outcome assessor and so were rated as being at low risk of bias (Boden 2012; Coffey 2006; Coffey submitted; Foa 2013; Hien 2009; Mills 2012; Mueser 2008; Sannibale 2013). Research interviewers were not blinded to treatment assignment at the follow‐up assessments in McGovern 2011 and Norman unpublished, which we therefore rated as high risk. We were unclear about the blinding of assessors in the remaining studies.
Incomplete outcome data
Seven studies reported drop‐out and loss to follow‐up clearly and performed intention‐to‐treat (ITT) analyses on all participants who were randomised, so that missing outcome data were replaced using a recognised statistical method, for example last observation carried forward (Foa 2013; Frisman 2008; Hien 2009; Mills 2012; Mueser 2008; Najavits 2006a; Sannibale 2013). We also judged Zlotnick 2009 as low risk because loss to follow‐up was low. Three studies undertook ITT analysis by including participants in analyses if they had attended at least one treatment session, following randomisation (Coffey submitted; Hien 2004; Norman unpublished). For Norman unpublished, people who did not attend any treatment sessions remained blind to their allocation, and based on guidance provided by Fergusson 2002, we judged this study to be of low risk. We were unclear about whether participants in Coffey submitted and Hien 2004 were aware of their allocation and whether this might have influenced drop‐out; we therefore judged these studies to be of unclear risk. We judged that methods of analysis were at high risk of bias in Coffey 2006.
Selective reporting
We were able to identify protocols with prespecified outcome measures for six trials (Boden 2012; Foa 2013; McGovern 2011; Mills 2012; Norman unpublished; Sannibale 2013). We checked that all prespecified outcomes were reported, and rated these studies as being at low risk of bias. We identified two trials as being at high risk (Coffey 2006; Najavits 2006a). We were able to extract only minimal data from Najavits 2006a because all outcomes were not fully reported and tabular data were mainly reported only for positive outcomes. We were unable to make a judgement about reporting bias for the other six trials.
Other potential sources of bias
We could identify no other potential sources of bias in four studies (Foa 2013; Hien 2009; Mueser 2008; Sannibale 2013). We judged that there was a high risk of bias because of additional factors in six studies (Frisman 2008; McGovern 2011; Mills 2012; Najavits 2006a; Norman unpublished; Zlotnick 2009). We were unable to make informed judgements about the remaining trials (Boden 2012; Coffey 2006; Coffey submitted; Hien 2004), and therefore rated them as unclear.
Effects of interventions
See: Summary of findings for the main comparison ; Summary of findings 2 Trauma‐focused psychological intervention compared to active psychological intervention for SUD only; Summary of findings 3 Non‐trauma‐focused psychological intervention for PTSD and SUD or PTSD only compared to control intervention; Summary of findings 4 Non‐trauma‐focused psychological intervention for PTSD and SUD or PTSD only compared to active psychological intervention for SUD only
We have grouped results according to the intervention characteristics identified above in the Interventions section of Included studies.
Comparison 1: Trauma‐focused psychological therapy versus control intervention
Four studies contributed to this comparison. These studies either evaluated trauma‐focused CBT‐based interventions in combination with SUD‐focused interventions, or in the context of a substance abuse setting where SUD interventions were already being received. All studies evaluated interventions delivered individually.
Primary outcomes
1.1 PTSD severity
Four studies including 405 participants reported severity of PTSD symptoms at post‐treatment (Analysis 1.1). We noted a small effect in favour of individual psychological therapy (standardised mean difference (SMD) ‐0.41; 95% confidence interval (CI) ‐0.72 to ‐0.10), although heterogeneity was moderate (I² = 49%). One study with 120 participants reported follow‐up at 3 to 4 months (Analysis 1.2); we again noted a small effect in favour of individual psychological therapy (mean difference (MD) ‐9.83; 95% CI ‐17.11 to ‐2.55). Three studies including 388 participants reported follow‐up at 5 to 7 months (Analysis 1.3). There was a small effect in favour of individual psychological therapy (SMD ‐0.34; 95% CI ‐0.58 to ‐0.10), and we noted no important heterogeneity (I² = 26%).
1.2 Drug or alcohol use, or both
Three studies including 388 participants reported severity of SUD symptoms post‐treatment (Analysis 1.4). We found no significant difference (SMD ‐0.13; 95% CI ‐0.41 to 0.15). We noted a moderate level of heterogeneity (I² = 45%). One study with 120 participants reported SUD symptom severity at 3 to 4 months (Analysis 1.5). No significant difference was found (MD ‐2.33; 95% CI ‐12.87 to 8.21). Three studies including 388 participants reported follow‐up at 5 to 7 months (Analysis 1.6). There was a small effect in favour of individual psychological therapy (SMD ‐0.28; 95% CI ‐0.48 to ‐0.07), and we noted no heterogeneity (I² = 0%).
1.3 Treatment completion
Three studies including 316 participants reported treatment completers (Analysis 1.7). We found a significant difference in favour of the control condition (risk ratio (RR) 0.78; 95% CI 0.64 to 0.96). We noted a moderate level of heterogeneity (I² = 41%).
Secondary outcomes
1.4 PTSD diagnosis after treatment
Only one study with 120 participants reported outcomes for PTSD diagnosis (Analysis 1.8). There was a small treatment effect in favour of individual psychological therapy (RR 0.71; 95% CI 0.51 to 1.00).
1.5 SUD diagnosis after treatment
No data were available for diagnostic status for substance use.
1.6 Adverse events
Two studies provided data on adverse events (Analysis 1.9). These two studies reported a total of 20 events. None of these events were attributed to treatment interventions provided in the studies. We found no significant differences between the two groups (RR 0.81; 95% CI 0.34 to 1.90), noted no heterogeneity (I² = 0%) (Analysis 1.10).
1.7 Compliance, as measured by proportion of treatment sessions attended
Three studies reported data on the mean number of treatment sessions attended by participants in the experimental group (Analysis 1.11), with participants attending a mean of 6.89 (standard deviation (SD) = 4.63) sessions. The proportions of available sessions attended per study varied from 35.2% to 68.0%.
1.8 General functioning
No data were available.
1.9 Use of health‐related resources
No data were available.
Comparison 2: Trauma‐focused psychological therapy versus active psychological therapy for SUD only
One study with 62 participants contributed to the comparison. Intervention in this study was delivered individually.
Primary outcomes
2.1 PTSD severity
One study reported severity of PTSD symptoms. No significant difference was found post‐treatment (MD ‐3.91; 95% CI ‐19.16 to 11.34; n = 46; Analysis 2.1), at 5 to 7 months' follow‐up (MD ‐9.32; 95% CI ‐22.89 to 4.25; n = 45; Analysis 2.2), or at 8 to 10 months' follow‐up (MD 2.11; 95% CI ‐16.10 to 20.32; n = 47; Analysis 2.3). Differences in the numbers of participants contributing to each analysis were a result of the numbers available to follow‐up at each time point.
2.2 Drug or alcohol use, or both
One study reported severity of PTSD symptoms. No significant difference was found post‐treatment (MD ‐1.27; 95% CI ‐5.76 to 3.22; n = 46; Analysis 2.4), at 5 to 7 months' follow‐up (MD 1.90; 95% CI ‐1.65 to 5.45; n = 45; Analysis 2.5), or at 8 to 10 months' follow‐up (MD ‐0.93; 95% CI ‐4.04 to 2.18; n = 47; Analysis 2.6).
2.3 Treatment completion
Data on treatment completers were available from one study (Analysis 2.7). No difference was found between the two groups on rate of treatment completion (RR 1.00; 95% CI 0.74 to 1.36).
Secondary outcomes
2.4 PTSD diagnosis after treatment
One study reported data on PTSD diagnosis post‐treatment (Analysis 2.8). No difference was found between the two groups (RR 1.04; 95% CI 0.67 to 1.62).
2.5 SUD diagnosis after treatment
One study reported data on SUD diagnosis post‐treatment (Analysis 2.9). No difference was found between the two groups (RR 1.16; 95% CI 0.83 to 1.60).
2.6 Adverse events
Adverse events were not reported.
2.7 Compliance, as measured by proportion of treatment sessions attended
No data were available for the mean number of treatment sessions attended.
2.8 General functioning
No data were available.
2.9 Use of health‐related resources
No data were available.
Comparison 3: Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only versus control intervention
One study evaluated non‐trauma‐focused psychological therapy delivered individually (Mueser 2008). Five studies evaluated group‐based interventions. Four studies evaluated Seeking Safety as the experimental condition. Frisman 2008 evaluated an alternative group‐based intervention (Frisman 2008 also had a far lower rate of completion than other studies).
Primary outcomes
3.1 PTSD severity
Individual‐based intervention
One study with 44 participants reported severity of PTSD symptoms. No significant difference was found post‐treatment (SMD ‐0.22; 95% CI ‐0.83 to 0.39; Analysis 3.1), at 3 to 4 months' follow‐up (SMD ‐0.25; 95% CI ‐0.86 to 0.36; Analysis 3.2), or at 5 to 7 months' follow‐up (SMD ‐0.20; 95% CI ‐0.81 to 0.41; Analysis 3.3).
Group‐based intervention
Post‐treatment data were available from 4 studies including 513 participants. All 4 studies evaluated Seeking Safety or partial‐dose Seeking Safety as the experimental condition. We found no significant difference between the two groups (SMD ‐0.02; 95% CI ‐0.19 to 0.16; Analysis 3.1). There was general consistency in study results (I² = 0%). Data were also available from the same four studies at 3 to 4 months' follow‐up (Analysis 3.2); again, we found no significant differences (SMD 0.00; 95% CI ‐0.17 to 0.18; n = 499) and noted no heterogeneity (I² = 0%). Data at 5 to 7 months' follow‐up were available from 4 studies including 566 participants. We identified no effect (SMD ‐0.14; 95% CI ‐0.31 to 0.03) and noted no heterogeneity (I² = 0%) (Analysis 3.3). Two studies with 518 participants provided data at 12 months' follow‐up (Analysis 3.4). No effect was evident (SMD ‐0.07; 95% CI ‐0.25 to 0.10). There was general consistency in study results (I² = 0%).
3.2 Drug or alcohol use, or both
Individual‐based intervention
No data were available.
Group‐based intervention
Post‐treatment data were available from 3 studies including 464 participants (Analysis 3.5). All three studies evaluated Seeking Safety or partial‐dose Seeking Safety as the experimental condition. We found no significant difference between the two conditions (SMD ‐0.41; 95% CI ‐0.97 to 0.14). The degree of heterogeneity was substantial (I² = 79%). It should be noted that there was a significant difference in favour of the Seeking Safety intervention for two studies post‐treatment (Boden 2012; Norman unpublished), but not for the third study (Hien 2009), which was much larger. Hien 2009 differed from Boden 2012 and Norman unpublished in that intervention was based on a partial‐dose programme. This is addressed further under 'Subgroup analyses' below. Data at 3 to 4 months' follow‐up were available from the 4 Seeking Safety or partial‐dose Seeking Safety studies with 499 participants (Analysis 3.6). We found no significant differences (SMD ‐0.08; 95% CI ‐0.40 to 0.23). The degree of heterogeneity post‐treatment was moderate (I² = 48%). Data at 5 to 7 months' follow‐up were available from 4 studies with 572 participants (Analysis 3.7). We found no differences (SMD ‐0.06; 95% CI ‐0.23 to 0.11) and noted no heterogeneity (I² = 0%). Two studies with 528 participants provided data at 12 months (Analysis 3.8). We found no differences (SMD 0.02; 95% CI ‐0.15 to 0.20) and noted no heterogeneity (I² = 0%).
3.3 Treatment completion
Individual‐based intervention
Data on treatment completion were available from one study only for participants receiving the experimental intervention (Analysis 3.9); 70.6% of participants attended a minimum of 6 of the 16 available treatment sessions and were considered treatment completers; 52.9% attended 12 or more sessions.
Group‐based intervention
Two studies including 381 participants reported data on treatment completers for both the experimental and control condition (Analysis 3.10). We found no significant difference between the two conditions (RR 1.13; 95% CI 0.88 to 1.45). There was general consistency in study results (I² = 0%). One study only provided data about the number of participants in the experimental group considered to be completers (Analysis 3.9). At 28%, treatment adherence for the group intervention in this study was very low.
Secondary outcomes
3.4 PTSD diagnosis after treatment
Individual‐based intervention
No data were available.
Group‐based intervention
Two studies with 77 participants provided data on PTSD diagnosis post‐treatment (Analysis 3.11). We found no differences (RR 1.01; 95% CI 0.66 to 1.54) and noted no heterogeneity (I² = 0%). Both studies evaluated full‐dose Seeking Safety interventions as the experimental condition.
3.5 SUD diagnosis after treatment
No data were available.
3.6 Adverse events
Individual‐based intervention
No data were available.
Group‐based intervention
Three studies reported on adverse events (Analysis 3.12). Two of the studies reported no adverse events. The third study reported 83 study‐related adverse events from 353 participants (Analysis 3.13). We found no differences in the number of events experienced between the two conditions (RR 1.03; 95% CI 0.71 to 1.50).
3.7 Compliance, as measured by proportion of treatment sessions attended
Individual‐based intervention
No data were available.
Group‐based intervention
Five studies reported data on the mean number of treatment sessions attended by participants in the experimental group (Analysis 3.14; Analysis 3.15), with participants attending a mean of 6.31 (SD = 5.71) sessions. The proportions of available sessions attended for the experimental group per study ranged from 37.9% to 62.4%.
3.8 General functioning
No data were available.
3.9 Use of health‐related resources
No data were available.
Comparison 4: Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only versus active psychological therapy for SUD only
Two studies including 128 participants contributed to this comparison. Both studies evaluated interventions delivered individually.
Primary outcomes
4.1 PTSD severity
Two studies including 128 participants reported severity of PTSD symptoms. We found no significant difference post‐treatment (SMD ‐0.26; 95% CI ‐1.29 to 0.77; Analysis 4.1). The level of heterogeneity was considerable (I² = 87%). There was a significant difference in favour of the combined intervention post‐treatment (MD ‐16.52; 95% CI ‐27.99 to ‐5.05) for one of these two studies, McGovern 2011, although it was noted that the two groups in this study were not well matched for PTSD severity at baseline. The same studies including 128 participants reported follow‐up at 3 to 4 months, finding no significant difference between the two conditions (SMD 0.12; 95% CI ‐0.31 to 0.55; Analysis 4.2). We noted a moderate level of heterogeneity (I² = 33%). One study with 75 participants reported severity of PTSD symptoms at 5 to 7 months, finding no significant difference (MD 7.52; 95% CI ‐3.78 to 18.82; Analysis 4.3).
4.2 Drug or alcohol use, or both
Two studies including 128 participants reported severity of SUD symptoms. We found no significant differences post‐treatment (SMD 0.22; 95% CI ‐0.13 to 0.57; Analysis 4.4), or at 3 to 4 months' follow‐up (SMD 0.18; 95% CI ‐0.18 to 0.53; Analysis 4.5); we noted no heterogeneity at either follow‐up point (I² = 0%). One study with 75 participants reported severity of SUD symptoms at 5 to 7 months' follow‐up (Analysis 4.6); we found no significant difference (MD 0.10; 95% CI ‐0.20 to 0.40).
4.3 Treatment completion
Data on treatment completers were available from 2 studies with 128 participants. We found no difference between the two groups on rate of treatment completion (RR 0.91; 95% CI 0.68 to 1.20; Analysis 4.7).
Secondary outcomes
4.4 PTSD diagnosis after treatment
One study reported data on PTSD diagnosis post‐treatment (Analysis 4.8). No difference was found between the two groups (RR 0.94; 95% CI 0.68 to 1.30).
4.5 SUD diagnosis after treatment
No data were available.
4.6 Adverse events
Adverse events were not reported.
4.7 Compliance, as measured by proportion of treatment sessions attended
Data were available from 1 study with 75 participants (Analysis 4.9). There was no difference between the two groups for treatment attendance (MD ‐0.10; 95% CI ‐3.75 to 3.55), with attendance of 48.0% at the experimental group sessions and 48.4% at control group sessions.
4.8 General functioning
No data were available.
4.9 Use of health‐related resources
No data were available.
Reporting bias
Twelve of the 14 studies included in this review were published, and one study completed recently, Coffey submitted, was in the process of seeking publication. We followed up all appropriate trials registered with World Health Organization's trials portal (ICTRP) and ClinicalTrials.gov and made attempts to contact authors known to be active in this field. We identified one unpublished study that we were able to include. The numbers of studies in each comparison were insufficient to allow for meaningful consideration of publication bias using funnel plots (Lau 2006).
Subgroup analyses
Comparison 3: Group‐based combined non‐trauma‐focused psychological therapy for PTSD and SUD versus waiting list/treatment as usual/minimal intervention/placebo intervention
We reported analysis for the effects of group‐based interventions on PTSD severity and drug/alcohol use at initial post‐treatment follow‐up above (Analysis 3.1; Analysis 3.5). Seeking Safety is widely used as a group‐based intervention for treatment of comorbid PTSD and SUD. All studies contributing to these analyses evaluated Seeking Safety. Other analyses in Comparison 3 included one study that did not evaluate Seeking Safety (Frisman 2008). We therefore undertook subgroup analyses of PTSD severity and drug/alcohol use at later follow‐up points excluding Frisman 2008. There was no evidence of an effect of Seeking Safety on PTSD severity at 5 to 7 months (SMD ‐0.12; 95% CI ‐0.34 to 0.10; k = 3; n = 425; Analysis 3.16) or at 12 months (SMD ‐0.04; 95% CI ‐0.25 to 0.17; k = 1; n = 353; Analysis 3.17). There was also no evidence of an effect on drug/alcohol use at either 5 to 7 months (SMD ‐0.11; 95% CI ‐0.30 to 0.08; k = 3; n = 425; Analysis 3.18) or at 12 months (SMD 0.00; 95% CI ‐0.21 to 0.21; k = 1; n = 353; Analysis 3.19).
As we noted, the study by Hien 2009 included a 12‐session partial dose of Seeking Safety. We therefore undertook post hoc analyses including only data from the full‐dose Seeking Safety studies. These analyses showed no effect post‐treatment (SMD ‐0.02; 95% CI ‐0.19 to 0.16; k = 3; n = 160), at 3 to 4 months (SMD 0.09; 95% CI ‐0.24 to 0.42; k = 3; n = 146), or at 5 to 7 months (SMD 0.13; 95% CI ‐0.35 to 0.60; k = 2; n = 72) for PTSD severity. We did find a moderate effect in favour of full‐dose Seeking Safety post‐treatment for drug/alcohol use (SMD ‐0.67; 95% CI ‐1.14 to ‐0.19; k = 2; n = 111). We noted no important heterogeneity (I² = 20%). There was no effect at 3 to 4 months (SMD ‐0.03; 95% CI ‐0.62 to 0.56; k = 3; n = 146) or at 5 to 7 months (SMD 0.03; 95% CI ‐0.45 to 0.51; k = 2; n = 72) for drug/alcohol use.
Sensitivity analyses
Comparison 1: Individual‐based psychological therapy including a trauma‐focused component plus SUD intervention versus waiting list/treatment as usual/minimal intervention/placebo intervention
Coffey 2006 provided outcome data only on the basis of participants who were available for follow‐up, and loss to follow‐up was high. We therefore undertook a sensitivity analysis for PTSD severity (Analysis 1.1) excluding this study. We continued to find a small effect post‐treatment in favour of individual‐based psychological therapy, although this effect was reduced (SMD ‐0.33; 95% CI ‐0.56 to ‐0.10; Analysis 1.12). We noted no important heterogeneity (I² = 19%). Coffey 2006 did not contribute to analysis at other follow‐up points.
Discussion
Summary of main results
We included 14 studies including 1506 participants in this review. It was apparent that research attention is mainly focused on two broad types of intervention for PTSD and SUD comorbidity (van Dam 2012). These are CBT‐based interventions delivered on an individual basis consisting of a significant trauma‐focused component; and CBT‐based interventions aimed at developing and enhancing positive coping skills, without a trauma‐focused component. These latter interventions are offered on both an individual and a group basis.
psychological therapy including a trauma‐focused component
We were only able to identify individual‐based studies of psychological therapies including a trauma‐focused component. All trauma‐focused interventions were delivered alongside intervention aimed at treating SUD, or participants were recruited from SUD services. We found evidence of a small benefit for individual‐based psychological therapies that included a trauma‐focused component when compared against usual care or minimal intervention conditions for PTSD at the end of treatment and at 3 to 4 and 5 to 7 months after treatment. We found evidence of a small reduction in drug/alcohol use at 5 to 7 months after treatment, but not at earlier time points. There was evidence of lower rates of treatment completion in those receiving trauma‐focused intervention compared to treatment as usual/minimal intervention, when considered against study‐defined criteria for a treatment completer. There were no differences in PTSD‐ or SUD‐related outcomes when individual‐based trauma‐focused psychological therapy was compared with an active psychological therapy for SUD only. However, data were only available from one trial, which was not well powered.
Non‐trauma‐focused interventions
Individual‐based psychological therapy without a trauma‐focused component
We identified one study that evaluated an individual‐based psychological therapy without a trauma‐focused component against a usual care or minimal intervention condition (Mueser 2008). We obtained outcome data for a small cohort of individuals with SUD; this study did not include any SUD intervention. We identified only one study that evaluated individual‐based psychological therapy and included both PTSD‐ and SUD‐related components (Najavits 2006a). We were not able to use data from this study. We could not identify any benefits for individual‐based psychological therapy that did not offer a trauma‐focused component when compared against a usual care condition or another active psychological therapy. These findings were also based on data from two small trials.
Group‐based psychological therapy without a trauma‐focused component
The majority of the group‐based studies evaluating non‐trauma‐focused interventions were of Seeking Safety (Najavits 2002b). We found no improvement for PTSD severity at any time point when these interventions were compared against usual care/minimal intervention or against another active psychological therapy. We also found no benefits in terms of reduction in drug/alcohol use across studies, but did find a moderate reduction in drug/alcohol use for full‐dose Seeking Safety through post‐hoc analyses, when compared against treatment as usual/minimal intervention. This effect was not sustained at later follow‐up points. Non‐trauma‐focused group‐based interventions maintained a level of retention similar to control conditions for individual‐ and group‐based interventions.
Treatment completion and drop‐out
The level of drop‐out was high across all studies. Study criteria for defining a treatment completer were often modest. Of those studies reporting treatment completers, only one achieved retention of over 70% (Sannibale 2013). Rates of completion in most other studies were between 50% and 70%, with one large study reporting a completion rate of 28% for those in the active intervention group (Frisman 2008). However, studies (including Frisman 2008) were often more successful at retaining participants in follow‐up for research purposes. One study, Hien 2009, did investigate the reasons for drop‐out in a follow‐up study (Pinto 2011). Pinto 2011 found that participants with more education, higher attendance at 12‐step meetings, and strong therapeutic alliance with their therapists had better retention rates. This multisite trial also found some site differences, with retention being highest in a site that offered childcare and had the lowest overall intake.
Adverse events
In contrast to Bisson 2013, 5 of the 14 included studies noted information about adverse events, with 3 studies reporting on adverse events in some detail (Foa 2013; Hien 2009; Mills 2012). There was no evidence of differences in adverse events for these studies (for details see Analysis 1.9 and Analysis 3.12).
Overall completeness and applicability of evidence
The objective of this review was to determine the efficacy of psychological therapies aimed at treating traumatic stress symptoms, substance misuse symptoms, or both in people with comorbid PTSD and SUD. In terms of applicability of findings, the studies included in this review were mainly conducted in veterans groups and amongst groups who had experienced significant abuse and interpersonal violence, and evaluated males only, females only, and both genders together. Studies took place in high‐income, English‐speaking countries, but participants were largely of low income and often living in relatively deprived settings. A strength of this review is that samples were ethnically diverse in the majority of studies. However, the results of this review may not be generalisable to other settings or participant groups. We only identified one study involving adolescents and no studies involving younger children. Most studies did not include people with comorbid psychiatric diagnoses or with cognitive impairment, who are arguably more difficult to treat. Generalising the results to more complex presentations is therefore problematic.
In addition to high drop‐out rates, recruitment appears to have been a significant problem for some studies. Some studies ended before reaching recruitment targets (for example Boden 2012; Mills 2012; Norman unpublished; Sannibale 2013). One study took eight years to reach its recruitment target, with a large number of individuals who met inclusion criteria refusing to participate in the study (Foa 2013).
We outlined earlier that there is little consensus about the process of interventions in terms of treatment pathways. We had hoped this review would help to address this issue. It has to a degree, but in practice, most studies recruited participants from substance misuse services, so many participants had received some level of substance use intervention prior to recruitment, and in most instances it is likely that substance or alcohol use, or both was stabilised to some extent prior to study intervention, often with the aid of pharmacological intervention. It is possible that the efficacy of psychological therapies is stronger than suggested by the data, as in several studies the usual care group were able to access a significant amount of clinician contact and would have been of the understanding that they were being treated, which may have been experienced as therapeutic. The review does include studies that evaluated combined intervention and integrated interventions, but we did not identify any studies where interventions were tested and delivered sequentially. The review also includes studies of some of the most well‐known models for treating comorbidity, such as Seeking Safety, COPE, and programmes based around CBT. Most studies attempted to evaluate follow‐up beyond the immediate completion of treatment, and several of the larger studies reported follow‐up between 6 and 12 months after treatment was completed.
Some studies reported data on medium‐ to long‐term follow‐up. However, follow‐up rates tended to be low, and whilst many studies used intention‐to‐treat (ITT) analyses, true follow‐up effects relied heavily on estimation and may be too conservative or too optimistic of true effects. It should also be noted that whilst the majority of studies undertook ITT analyses, several studies based their ITT sample only on participants who attended at least one treatment session. This can be a legitimate approach when ineligible people are mistakenly randomised into a trial and if a potential participant is prematurely randomised as long as allocation to treatment arm cannot influence the likelihood that people receive the intervention (Fergusson 2002). However, the fact that some studies did this and others did not probably means that some studies included more participants who were likely to be ambivalent about engaging in treatment. We should note further that Coffey 2006, McGovern 2011, and Zlotnick 2009 only reported data for participants who were available to follow‐up, and in some analyses this data was used in conjunction with ITT data from other studies. We undertook several sensitivity analyses excluding these studies. These analyses made no difference to our findings.
Quality of the evidence
We assessed the results for primary outcomes using GRADE protocols; see summary of findings Table for the main comparison; summary of findings Table 2; summary of findings Table 3; summary of findings Table 4. We found the quality of evidence for each comparison to be low or very low.
Risk of bias was a factor in downgrading GRADE judgements in all comparisons. As with the vast majority of trials of psychological therapy, participants and providers in the included studies were unblinded to allocation. We therefore judged all studies as being at high risk in terms of performance bias. More recent studies tended to be rated more favourably. In a number of studies, the information provided by the published report was insufficient to determine the risk of bias associated with key methodological indicators. We judged three studies as being at high risk on at least one other aspect of study design and four studies as at high risk on two other aspects of design. 'Other bias' was the most common aspect of design to be judged as high risk. Negative judgements on this aspect were made for a number of different reasons, and there was no particular common reason for this (see Characteristics of included studies). Lack of blinding of outcome assessors and selective reporting were the other main reasons for judgements of high risk.
We also downgraded GRADE judgements on the basis of unexplained statistical and clinical heterogeneity. Clinical populations were diverse in terms of type of trauma exposure, nature of substance misuse, and severity of substance abuse and dependence, with some studies only including participants with dependence, and one study excluding individuals with substance dependence (Mueser 2008). Mueser 2008 also differed from other studies in that all participants also had comorbidity for a serious mental illness. We attempted to group studies together in a way that was logical and clinically meaningful. It is, however, important for us to acknowledge that there is significant clinical heterogeneity within comparisons. The first of our main comparisons was of individual‐based interventions with a trauma‐focused component versus treatment as usual/minimal intervention (Analysis 1.1 to Analysis 1.12). Whilst all active interventions in this comparison included a trauma‐focused component, the nature of delivery of trauma‐focused intervention and the number of sessions of trauma‐focused intervention differed, as did session length, the number of treatment sessions available, and the nature of additional substance use intervention. There was also significant clinical heterogeneity in the control conditions. The majority of studies included in these comparisons offered what would be considered combined PTSD/ SUD intervention. However, in some studies, SUD intervention was integral to the active intervention (for example through COPE, Mills 2012), whereas in other studies, participants in the active intervention received their SUD intervention from a separate source. Treatment‐as‐usual conditions in the studies in this comparison depended on what was available through local service delivery and therefore varied across studies. Not surprisingly, there was notable statistical heterogeneity in many of the analyses undertaken in this comparison, but the small number of studies limited the additional analyses we were able to undertake. There were also some differences in the interventions in the comparison of non‐trauma‐focused individual‐ and group‐based interventions against treatment as usual/minimal intervention (Analysis 3.1 to Analysis 3.19;Analysis 4.1 to Analysis 4.9). Most group‐based studies evaluated Seeking Safety. One study offered only 12 core sessions, rather than 25 sessions (Hien 2009); another incorporated some other cognitive intervention (Norman unpublished), and in a third participants received intervention whilst in a prison (Zlotnick 2009). Treatment as usual and minimal interventions also varied in this comparison, although statistical heterogeneity tended to be absent or smaller. In attempting to group studies and identify meaningful comparison, we tried to draw a distinction between control interventions evaluating an active psychological therapy from treatment as usual/minimal intervention. However, it is notable that "treatment as usual" interventions were often quite active and in most cases were likely to have contained some form of established or non‐specific psychological therapy. We were only able to undertake limited investigation of factors potentially contributing to statistical heterogeneity because the number of studies included in each comparison was small.
Two of the comparisons used in this review were mostly moderately well powered. We downgraded the GRADE judgements of the other two comparisons (see summary of findings Table 2; summary of findings Table 4) for reasons of imprecision of results, as the numbers of participants contributing to these comparisons were small. Evidence was collected by direct means for most outcomes used in meta analysis in this review.
Potential biases in the review process
The review followed guidelines set out by The Cochrane Collaboration (Higgins 2011). Two review authors independently read all the candidate studies and assessed them for inclusion. Three review authors rated all included studies for risk of bias and independently extracted data from them. In case of disagreements we consulted a fourth review author. This will have minimised potential bias.
Several unavoidable issues remain. For example, we were unable to undertake an assessment of publication bias. We searched numerous online databases systematically, scrutinised reference lists, contacted experts in the field, and handsearched relevant additional sources. We were able to identify a number of unpublished studies from conference abstracts and attempted to contact study authors where possible. We were able to include data from one unpublished study (Norman unpublished). It is, of course, possible that there are other unpublished studies that we have missed. We mainly contacted research groups who were known to us, in English‐speaking countries (particularly the USA) and elsewhere in Europe, and a significant number of authors did not respond. We were not able to identify any relevant research groups outside of these areas of the world. We also included data from one study (Mueser 2008) that did not specifically provide interventions to treat PTSD/SUD comorbidity but included a significant minority of participants who met diagnosis. We included this study on the basis that it may provide evidence on how individuals with PTSD/SUD comorbidity respond to such non‐specific intervention. We attempted to identify other similar studies by reviewing studies included in other relevant Cochrane reviews undertaken by the Cochrane Drugs and Alcohol Group and those reported in Bisson 2013. Some of the reviews that we searched were published several years ago, and it is therefore possible that we missed other relevant studies. We did also approach authors of several other studies, but we were not able to obtain subset data.
Although most studies reported data on an ITT basis, several studies reported incomplete data. We contacted authors to obtain missing results where possible. Some comparisons therefore included data from those participants available to follow‐up, alongside ITT data. As we have outlined above, there was a great deal of clinical heterogeneity between trials included within comparisons within the review. There was also considerable statistical heterogeneity evident in many of the comparisons. In circumstances where we thought statistical heterogeneity to be an issue, we used a random‐effects model, and reported this. The majority of studies that we identified compared an active psychological therapy against treatment‐as‐usual or minimal‐intervention conditions. The studies comparing active psychological therapy against other psychological therapy tended to be small; this may mean that we were unable to identify effects that might be more apparent in studies that are better powered.
We reported some significant findings for treatment completion/drop‐out. These findings were based on study definitions of what constituted a treatment completer. These definitions varied greatly across studies. It was not possible to compile data around more unified definitions, but it is possible that our finding in relation to treatment completion may not have occurred if the studies included were more consistent about their definitions of treatment completers.
Agreements and disagreements with other studies or reviews
This is the first systematic review of psychological therapies for PTSD and SUD that we are aware of to be based only on randomised controlled trials. Other reviews have based their conclusions on findings from both controlled and non‐controlled studies (Berenz 2012; Najavits 2013; Torchalla 2012; van Dam 2012). To our knowledge, this is also the first review to undertake a detailed 'Risk of bias' assessment of included studies using the Cochrane 'Risk of bias' criteria (Higgins 2011), although other reviews have also commented upon methodological concerns (for example Najavits 2013; Torchalla 2012; van Dam 2012). In common with Berenz 2012 and van Dam 2012, we found that the most promising outcome data thus far are for psychological therapies that incorporate trauma‐focused intervention alongside intervention for SUD. However, these treatment effects were small. This finding is consistent with the findings from a recent meta‐analysis that compared treatment effects of studies for people with PTSD who had complex versus non‐complex presentations (Gerger 2014). Gerger 2014 also found that the benefits of specific interventions were small in studies with participants with more complex clinical problems. Our findings are not consistent with the conclusions of Najavits 2013, in that the data we included found little evidence to support the use of non‐trauma‐focused interventions, although our findings were somewhat consistent with this review in that PTSD tended to improve (with some interventions) more than SUD. We also found that fewer participants assigned to trauma‐focused intervention completed treatment than participants assigned to the comparable control condition. This finding is consistent with findings from the recently updated Cochrane review of psychological therapies for PTSD (Bisson 2013), suggesting that such interventions may not always be well tolerated.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
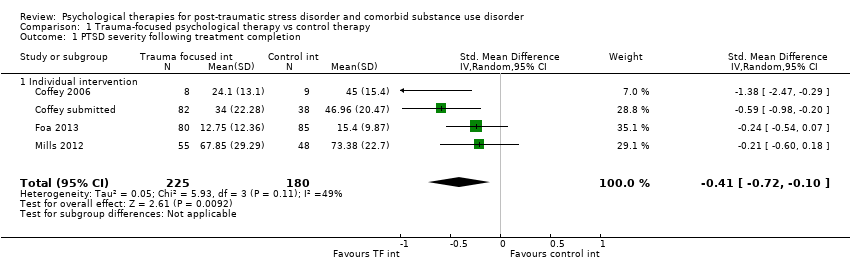
Comparison 1 Trauma‐focused psychological therapy vs control therapy, Outcome 1 PTSD severity following treatment completion.

Comparison 1 Trauma‐focused psychological therapy vs control therapy, Outcome 2 PTSD severity 3‐4 months following treatment completion.

Comparison 1 Trauma‐focused psychological therapy vs control therapy, Outcome 3 PTSD severity 5‐7 months following treatment completion.
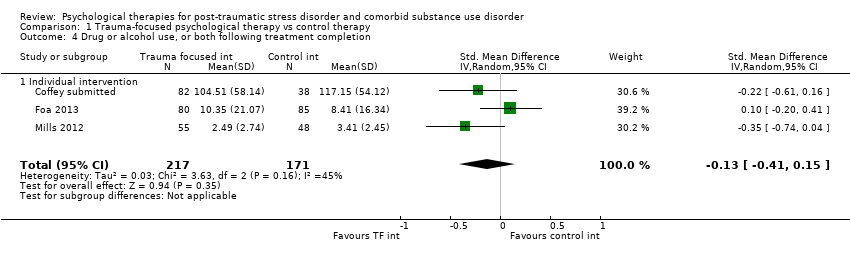
Comparison 1 Trauma‐focused psychological therapy vs control therapy, Outcome 4 Drug or alcohol use, or both following treatment completion.
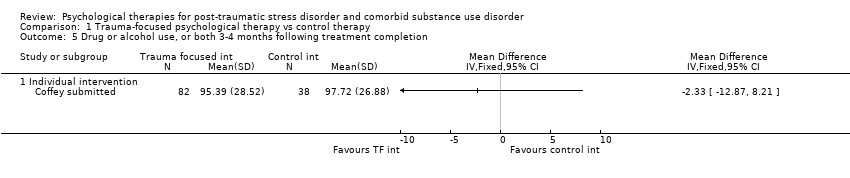
Comparison 1 Trauma‐focused psychological therapy vs control therapy, Outcome 5 Drug or alcohol use, or both 3‐4 months following treatment completion.

Comparison 1 Trauma‐focused psychological therapy vs control therapy, Outcome 6 Drug or alcohol use, or both 5‐7 months following treatment completion.
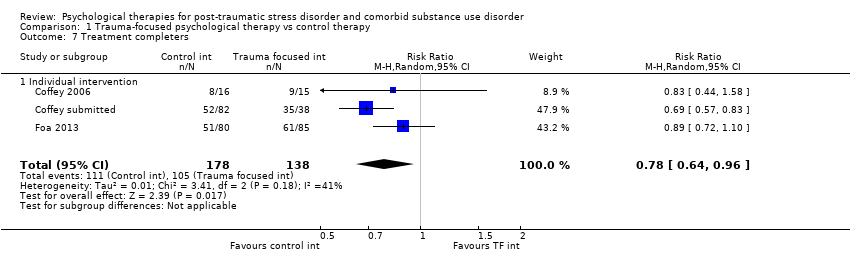
Comparison 1 Trauma‐focused psychological therapy vs control therapy, Outcome 7 Treatment completers.
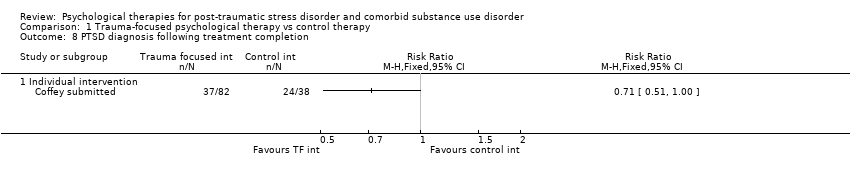
Comparison 1 Trauma‐focused psychological therapy vs control therapy, Outcome 8 PTSD diagnosis following treatment completion.
| Study | |
| Individual intervention | |
| Coffey 2006 | Not reported |
| Coffey submitted | Not reported |
| Foa 2013 | Twelve participants were removed from the study because of serious adverse events (serious suicidal ideation, n = 7; serious medical illness, n = 3; psychotic symptoms, n = 1; death, n = 1; however, none of these events was determined to be related to the study). |
| Mills 2012 | Two participants from the treatment group (3.6%) and 5 participants from the control group (10.4%) attempted suicide during the study (OR, 0.32 [95% CI, 0.06‐1.76]). Although it is possible that these attempts were related to participation in the study, all 7 individuals reported that this was not the case and elected to remain involved with the study. Additionally, 1 participant from the treatment group (1.8%) died as a result of a preexisting medical condition. |
Comparison 1 Trauma‐focused psychological therapy vs control therapy, Outcome 9 Adverse events.

Comparison 1 Trauma‐focused psychological therapy vs control therapy, Outcome 10 Adverse events.
| Study | Mean number sessions attended by intervention group (& SD) | Number sessions available | Percentage attended |
| Studies including intervention for SUD | |||
| Coffey submitted | 8.16 (3.26) approximated | 12 | 68.0% |
| Foa 2013 | 6.33 (5.31) | 18 | 35.2% |
| Mills 2012 | 5.83 (4.94) | 13 | 44.9% |
Comparison 1 Trauma‐focused psychological therapy vs control therapy, Outcome 11 Mean number of sessions attended for intervention group.
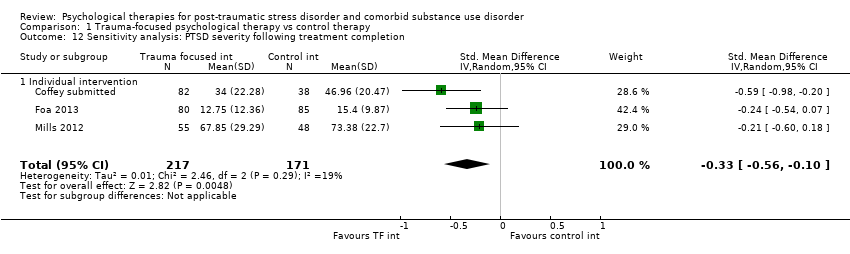
Comparison 1 Trauma‐focused psychological therapy vs control therapy, Outcome 12 Sensitivity analysis: PTSD severity following treatment completion.

Comparison 2 Trauma‐focused psychological therapy vs active psychological therapy for SUD only, Outcome 1 PTSD severity following treatment completion.

Comparison 2 Trauma‐focused psychological therapy vs active psychological therapy for SUD only, Outcome 2 PTSD severity 5‐7 months following treatment completion.

Comparison 2 Trauma‐focused psychological therapy vs active psychological therapy for SUD only, Outcome 3 PTSD severity 8‐10 months following treatment completion.
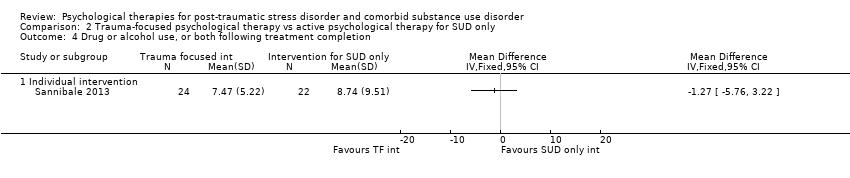
Comparison 2 Trauma‐focused psychological therapy vs active psychological therapy for SUD only, Outcome 4 Drug or alcohol use, or both following treatment completion.

Comparison 2 Trauma‐focused psychological therapy vs active psychological therapy for SUD only, Outcome 5 Drug or alcohol use, or both 5‐7 months following treatment completion.

Comparison 2 Trauma‐focused psychological therapy vs active psychological therapy for SUD only, Outcome 6 Drug or alcohol use, or both 8‐10 months following treatment completion.

Comparison 2 Trauma‐focused psychological therapy vs active psychological therapy for SUD only, Outcome 7 Treatment completers.

Comparison 2 Trauma‐focused psychological therapy vs active psychological therapy for SUD only, Outcome 8 PTSD diagnosis following treatment completion.
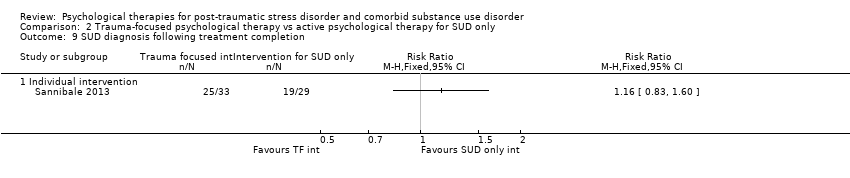
Comparison 2 Trauma‐focused psychological therapy vs active psychological therapy for SUD only, Outcome 9 SUD diagnosis following treatment completion.

Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 1 PTSD severity following treatment completion.

Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 2 PTSD severity 3‐4 months following treatment completion.

Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 3 PTSD severity 5‐7 months following treatment completion.

Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 4 PTSD severity 12 months following treatment completion.

Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 5 Drug or alcohol use, or both following treatment completion.

Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 6 Drug or alcohol use, or both 3‐4 months following treatment completion.

Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 7 Drug or alcohol use, or both 5‐7 months following treatment completion.

Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 8 Drug or alcohol use, or both 12 months following treatment completion.
| Study | |
| Individual intervention | |
| Mueser 2008 | 12/16 (70.6%) |
| Group intervention | |
| Frisman 2008 | 39/141 (28%) |
Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 9 Treatment completers.
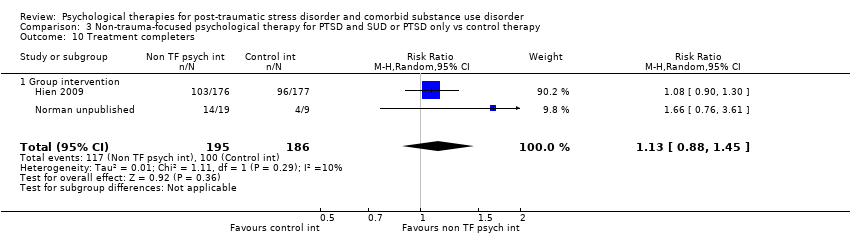
Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 10 Treatment completers.
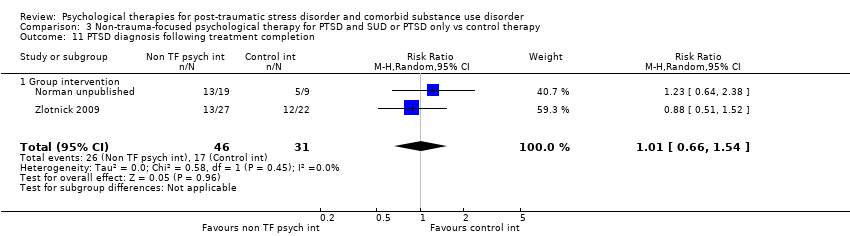
Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 11 PTSD diagnosis following treatment completion.
| Study | |
| Group intervention | |
| Boden 2012 | No harmful or unintended effects were observed during the trial. |
| Frisman 2008 | Not reported |
| Hien 2009 | 83 study related adverse events were identified (Killeen 2008). Of these 61 were rated as moderate to severe: 28 for the experimental condition; 33 for the control condition. |
| Najavits 2006a | Not reported |
| Norman unpublished | No adverse events occurred during the study. |
| Zlotnick 2009 | Not reported |
Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 12 Adverse events.

Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 13 Study‐related adverse events.
| Study | Mean number treatment condition sessions attended by intervention group (& SD) | Number sessions available | Percentage active intervention sessions attended | Mean number sessions attended by control group (& SD) | Percentage attended |
| Group intervention | |||||
| Boden 2012 | Not reported | Not reported | |||
| Frisman 2008 | 3.41 (3.38) active intervention sessions + 30.67 (37.38) TAU sessions | 9 active intervention sessions plus TAU sessions | 37.9% | 39.0 (69.62) TAU sessions | |
| Hien 2009 | 6.2 (4.5) | 12 | 51.7% | 6.9 (4.3) | 57.5% |
| Najavits 2006a | 9.67(5.05) active intervention session (11.78 (6.25) active intervention +TAU sessions) | 25 active intervention sessions plus TAU sessions | 38.7% | Not reported | |
| Norman unpublished | 12.5 (8.77) | 24 | 52.1% | 7.78 (5.78) | 32.4% |
| Zlotnick 2009 | 15.6 (6.2) | 25 | 62.4% | Not reported | |
Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 14 Mean number of sessions attended for intervention group.

Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 15 Mean number of sessions attended.
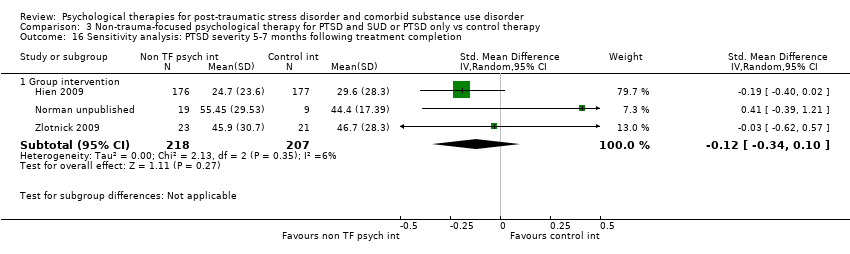
Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 16 Sensitivity analysis: PTSD severity 5‐7 months following treatment completion.
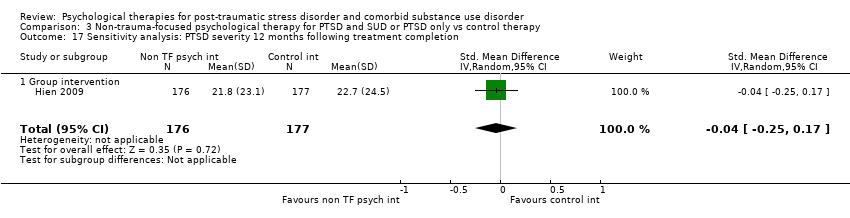
Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 17 Sensitivity analysis: PTSD severity 12 months following treatment completion.

Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 18 Sensitivity analysis: drug or alcohol use, or both 5‐7 months following treatment completion.

Comparison 3 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs control therapy, Outcome 19 Sensitivity analysis: drug or alcohol use, or both 12 months following treatment completion.

Comparison 4 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs active psychological therapy for SUD only, Outcome 1 PTSD severity following treatment completion.

Comparison 4 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs active psychological therapy for SUD only, Outcome 2 PTSD severity 3‐4 months following treatment completion.

Comparison 4 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs active psychological therapy for SUD only, Outcome 3 PTSD severity 5‐7 months following treatment completion.
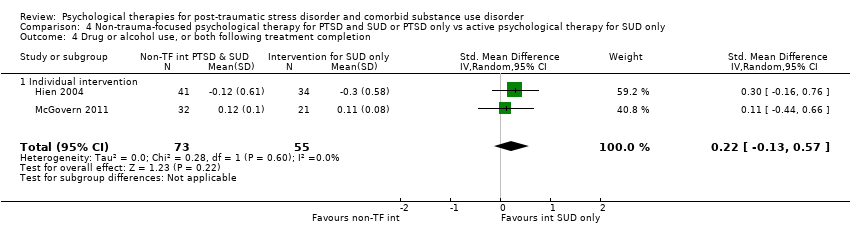
Comparison 4 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs active psychological therapy for SUD only, Outcome 4 Drug or alcohol use, or both following treatment completion.

Comparison 4 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs active psychological therapy for SUD only, Outcome 5 Drug or alcohol use, or both 3‐4 months following treatment completion.

Comparison 4 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs active psychological therapy for SUD only, Outcome 6 Drug or alcohol use, or both 5‐7 months following treatment completion.
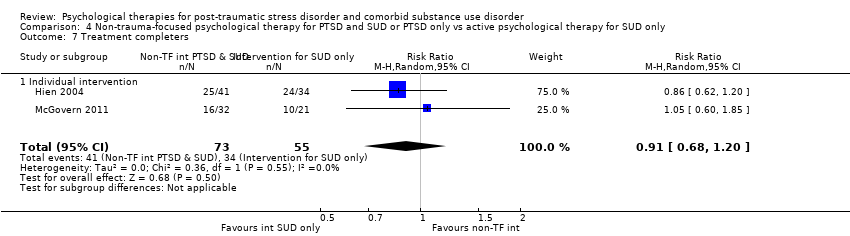
Comparison 4 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs active psychological therapy for SUD only, Outcome 7 Treatment completers.
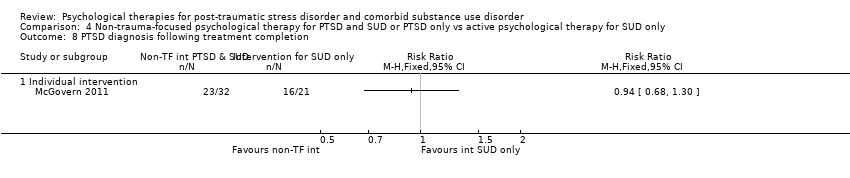
Comparison 4 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs active psychological therapy for SUD only, Outcome 8 PTSD diagnosis following treatment completion.

Comparison 4 Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only vs active psychological therapy for SUD only, Outcome 9 Mean number of sessions attended.
| Trauma‐focused psychological therapy compared to control intervention | ||||||
| Patient or population: Individuals with post‐traumatic stress disorder and comorbid substance use disorder | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| TAU/ minimal intervention | Individual‐based psychological therapyincluding a trauma‐focused component | |||||
| PTSD severity following treatment completion As assessed by the CAPS, PSS‐I, or IES‐R. High scores indicate greater symptom severity | ‐ | The mean PTSD severity following treatment completion in the intervention groups was | ‐ | 405 | ⊕⊝⊝⊝ | SMD ‐0.41 (‐0.72 to ‐0.1) Effect sizes of the range 0.2 to 0.5 indicate a small treatment effect |
| Drug or alcohol use, or both following treatment completion As assessed by the TLFB or CIDI. High scores indicate greater symptom severity | ‐ | The mean drug/alcohol use following treatment completion in the intervention groups was | ‐ | 388 | ⊕⊝⊝⊝ | SMD ‐0.13 (‐0.41 to 0.15) Not significant |
| Treatment completers | Study population | RR 0.80 | 316 | ⊕⊕⊝⊝ | Indicates higher drop‐out in the intervention group | |
| 761 per 1000 | 609 per 1000 | |||||
| Moderate | ||||||
| 718 per 1000 | 574 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Quality of evidence downgraded by one point because the risk of bias in most trials was high or unclear in several domains. SUD based adjunctive therapy was not a formal part of either the experimental or control condition in one study (Coffey 2006). However, participants were recruited through an SUD based service and it is likely that they would have had access to adjunctive SUD‐ based therapy on an informal basis. All other studies in this comparison included formal access SUD‐based adjunctive therapy. | ||||||
| Trauma‐focused psychological therapy compared to active psychological therapy for SUD only | ||||||
| Patient or population: Individuals with post‐traumatic stress disorder and comorbid substance use disorder | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Active psychological therapyfor SUD only | Individual‐based psychological therapyincluding a trauma‐focused component | |||||
| PTSD severity following treatment completion As assessed by the CAPS. High scores indicate greater symptom severity | ‐ | The mean PTSD severity following treatment completion in the intervention groups was | ‐ | 46 | ⊕⊕⊝⊝ | Not significant |
| Drug or alcohol use, or both following treatment completion As assessed by the TLFB. High scores indicate greater symptom severity | ‐ | The mean drug/alcohol use following treatment completion in the intervention groups was | ‐ | 46 | ⊕⊕⊝⊝ | Not significant |
| Treatment completers | Study population | RR 1 | 62 | ⊕⊕⊝⊝ | Not significant | |
| 724 per 1000 | 724 per 1000 | |||||
| Moderate | ||||||
| 724 per 1000 | 724 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Quality of evidence downgraded by two points because findings were based on outcomes from one study with a small sample size. SUD based adjunctive therapy was not a formal part of either the experimental or control condition in the study contributing to this comparison. | ||||||
| Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only compared to control intervention | ||||||
| Patient or population: Individuals with post‐traumatic stress disorder and comorbid substance use disorder | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| TAU/minimal intervention | Group or Indvidual based non‐trauma‐focused psychological therapy | |||||
| PTSD severity following treatment completion ‐ Individual‐based intervention As assessed by the CAPS. High scores indicate greater symptom severity | ‐ | The mean PTSD severity following treatment completion in the intervention groups was | ‐ | 44 | ⊕⊕⊝⊝ | SMD ‐0.22 (‐0.83 to 0.39) |
| PTSD severity following treatment completion ‐ Group‐based intervention As assessed by the CAPS or IES‐R. High scores indicate greater symptom severity | ‐ | The mean PTSD severity following treatment completion in the intervention groups was | ‐ | 513 | ⊕⊕⊝⊝ | SMD ‐0.02 (‐0.19 to 0.16) |
| Drug or alcohol use, or both following treatment completion ‐ Individual‐based intervention | ‐ | No data | ‐ | ‐ | ‐ | Not estimable |
| Drug or alcohol use, or both following treatment completion ‐ Group‐based intervention As assessed by the ASI, TLFB or CIDI. High scores indicate greater symptom severity | ‐ | The mean drug/alcohol use following treatment completion in the intervention groups was | ‐ | 464 | ⊕⊝⊝⊝ | SMD ‐0.41 (‐0.97 to 0.14) Not significant |
| Treatment completers ‐ Individual‐based intervention | ‐ | No data | ‐ | ‐ | ‐ | Not estimable |
| Treatment completers ‐ Group‐based intervention | Study population | RR 1.13 | 381 | ⊕⊕⊝⊝ | ‐ | |
| 538 per 1000 | 608 per 1000 | |||||
| Moderate | ||||||
| 493 per 1000 | 557 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Quality of evidence downgraded by two points because findings were based on outcomes from one study with a small sample size. The individual‐based study (Mueser 2008) in this comparison did not include access to SUD based adjunctive therapy. Participants in all other studies were able to access SUD‐based adjunctive therapy. | ||||||
| Non‐trauma‐focused psychological therapy for PTSD and SUD or PTSD only compared to active psychological therapy for SUD only | ||||||
| Patient or population: Individuals with post‐traumatic stress disorder and comorbid substance use disorder | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Active psychological therapyfor SUD only | Individual‐based combined non‐trauma‐focused psychological therapy | |||||
| PTSD severity following treatment completion As assessed by the CAPS. High scores indicate greater symptom severity | ‐ | The mean PTSD severity following treatment completion in the intervention groups was | ‐ | 128 | ⊕⊝⊝⊝ | SMD ‐0.26 (‐1.29 to 0.77) Not significant |
| Drug or alcohol use, or both following treatment completion As assessed by the SUI or ASI. High scores indicate greater symptom severity | ‐ | The mean drug/alcohol use following treatment completion in the intervention groups was | ‐ | 128 | ⊕⊕⊝⊝ | SMD 0.22 (‐0.13 to 0.57) Not significant |
| Treatment completers | Study population | RR 0.91 | 128 | ⊕⊝⊝⊝ | Not significant | |
| 618 per 1000 | 563 per 1000 | |||||
| Moderate | ||||||
| 591 per 1000 | 538 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Quality of evidence downgraded by one point because the risk of bias in most trials was high or unclear in several domains. Both studies in this comparison involved access to adjunctive SUD‐based therapy. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PTSD severity following treatment completion Show forest plot | 4 | 405 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.72, ‐0.10] |
| 1.1 Individual intervention | 4 | 405 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.72, ‐0.10] |
| 2 PTSD severity 3‐4 months following treatment completion Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Individual intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 PTSD severity 5‐7 months following treatment completion Show forest plot | 3 | 388 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.58, ‐0.10] |
| 3.1 Individual intervention | 3 | 388 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.58, ‐0.10] |
| 4 Drug or alcohol use, or both following treatment completion Show forest plot | 3 | 388 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.41, 0.15] |
| 4.1 Individual intervention | 3 | 388 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.41, 0.15] |
| 5 Drug or alcohol use, or both 3‐4 months following treatment completion Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Individual intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Drug or alcohol use, or both 5‐7 months following treatment completion Show forest plot | 3 | 388 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.48, ‐0.07] |
| 6.1 Individual intervention | 3 | 388 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.48, ‐0.07] |
| 7 Treatment completers Show forest plot | 3 | 316 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.64, 0.96] |
| 7.1 Individual intervention | 3 | 316 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.64, 0.96] |
| 8 PTSD diagnosis following treatment completion Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 Individual intervention | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Adverse events Show forest plot | Other data | No numeric data | ||
| 9.1 Individual intervention | Other data | No numeric data | ||
| 10 Adverse events Show forest plot | 2 | 268 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.34, 1.90] |
| 10.1 Individual intervention | 2 | 268 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.34, 1.90] |
| 11 Mean number of sessions attended for intervention group Show forest plot | Other data | No numeric data | ||
| 11.1 Studies including intervention for SUD | Other data | No numeric data | ||
| 12 Sensitivity analysis: PTSD severity following treatment completion Show forest plot | 3 | 388 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.56, ‐0.10] |
| 12.1 Individual intervention | 3 | 388 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.56, ‐0.10] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PTSD severity following treatment completion Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Individual intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PTSD severity 5‐7 months following treatment completion Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Individual intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 PTSD severity 8‐10 months following treatment completion Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Individual intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Drug or alcohol use, or both following treatment completion Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Individual intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Drug or alcohol use, or both 5‐7 months following treatment completion Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Individual intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Drug or alcohol use, or both 8‐10 months following treatment completion Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 Individual intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Treatment completers Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 Individual intervention | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 PTSD diagnosis following treatment completion Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 Individual intervention | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 SUD diagnosis following treatment completion Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.1 Individual intervention | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PTSD severity following treatment completion Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Individual intervention | 1 | 44 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.83, 0.39] |
| 1.2 Group intervention | 4 | 513 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.19, 0.16] |
| 2 PTSD severity 3‐4 months following treatment completion Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Individual intervention | 1 | 44 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.86, 0.36] |
| 2.2 Group intervention | 4 | 499 | Std. Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.17, 0.18] |
| 3 PTSD severity 5‐7 months following treatment completion Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Individual intervention | 1 | 44 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.81, 0.41] |
| 3.2 Group intervention | 4 | 566 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.31, 0.03] |
| 4 PTSD severity 12 months following treatment completion Show forest plot | 2 | 518 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.25, 0.10] |
| 4.1 Group intervention | 2 | 518 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.25, 0.10] |
| 5 Drug or alcohol use, or both following treatment completion Show forest plot | 3 | 464 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.97, 0.14] |
| 5.1 Group intervention | 3 | 464 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.97, 0.14] |
| 6 Drug or alcohol use, or both 3‐4 months following treatment completion Show forest plot | 4 | 499 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.40, 0.23] |
| 6.1 Group intervention | 4 | 499 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.40, 0.23] |
| 7 Drug or alcohol use, or both 5‐7 months following treatment completion Show forest plot | 4 | 572 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.23, 0.11] |
| 7.1 Group intervention | 4 | 572 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.23, 0.11] |
| 8 Drug or alcohol use, or both 12 months following treatment completion Show forest plot | 2 | 528 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.15, 0.20] |
| 8.1 Group intervention | 2 | 528 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.15, 0.20] |
| 9 Treatment completers Show forest plot | Other data | No numeric data | ||
| 9.1 Individual intervention | Other data | No numeric data | ||
| 9.2 Group intervention | Other data | No numeric data | ||
| 10 Treatment completers Show forest plot | 2 | 381 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.88, 1.45] |
| 10.1 Group intervention | 2 | 381 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.88, 1.45] |
| 11 PTSD diagnosis following treatment completion Show forest plot | 2 | 77 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.66, 1.54] |
| 11.1 Group intervention | 2 | 77 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.66, 1.54] |
| 12 Adverse events Show forest plot | Other data | No numeric data | ||
| 12.1 Group intervention | Other data | No numeric data | ||
| 13 Study‐related adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 13.1 Group intervention | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Mean number of sessions attended for intervention group Show forest plot | Other data | No numeric data | ||
| 14.1 Group intervention | Other data | No numeric data | ||
| 15 Mean number of sessions attended Show forest plot | 2 | 381 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.59, 0.79] |
| 15.1 Group intervention | 2 | 381 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.59, 0.79] |
| 16 Sensitivity analysis: PTSD severity 5‐7 months following treatment completion Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 16.1 Group intervention | 3 | 425 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.34, 0.10] |
| 17 Sensitivity analysis: PTSD severity 12 months following treatment completion Show forest plot | 1 | 353 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.25, 0.17] |
| 17.1 Group intervention | 1 | 353 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.25, 0.17] |
| 18 Sensitivity analysis: drug or alcohol use, or both 5‐7 months following treatment completion Show forest plot | 3 | 425 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.30, 0.08] |
| 18.1 Group intervention | 3 | 425 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.30, 0.08] |
| 19 Sensitivity analysis: drug or alcohol use, or both 12 months following treatment completion Show forest plot | 1 | 353 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.21, 0.21] |
| 19.1 Group intervention | 1 | 353 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.21, 0.21] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PTSD severity following treatment completion Show forest plot | 2 | 128 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐1.29, 0.77] |
| 1.1 Individual intervention | 2 | 128 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐1.29, 0.77] |
| 2 PTSD severity 3‐4 months following treatment completion Show forest plot | 2 | 128 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.31, 0.55] |
| 2.1 Individual intervention | 2 | 128 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.31, 0.55] |
| 3 PTSD severity 5‐7 months following treatment completion Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Individual intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Drug or alcohol use, or both following treatment completion Show forest plot | 2 | 128 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.13, 0.57] |
| 4.1 Individual intervention | 2 | 128 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.13, 0.57] |
| 5 Drug or alcohol use, or both 3‐4 months following treatment completion Show forest plot | 2 | 128 | Std. Mean Difference (IV, Random, 95% CI) | 0.18 [‐0.18, 0.53] |
| 5.1 Individual intervention | 2 | 128 | Std. Mean Difference (IV, Random, 95% CI) | 0.18 [‐0.18, 0.53] |
| 6 Drug or alcohol use, or both 5‐7 months following treatment completion Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Individual intervention | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Treatment completers Show forest plot | 2 | 128 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.68, 1.20] |
| 7.1 Individual intervention | 2 | 128 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.68, 1.20] |
| 8 PTSD diagnosis following treatment completion Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 Individual intervention | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Mean number of sessions attended Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 Individual intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

