Hábito dietético "mediterráneo" para la prevención primaria de las enfermedades cardiovasculares
Resumen
Antecedentes
El estudio Seven Countries de los años sesenta indicó que las poblaciones de la región mediterránea presentaban menor mortalidad por enfermedades cardiovasculares (ECV), probablemente como resultado de diferentes hábitos dietéticos. Estudios observacionales posteriores han confirmado los efectos beneficiosos de seguir un hábito dietético mediterráneo sobre los factores de riesgo de ECV. Las pruebas de ensayos clínicos son limitadas, y provienen principalmente de la prevención secundaria.
Objetivos
Determinar la efectividad de un hábito dietético mediterráneo para la prevención primaria de ECV.
Métodos de búsqueda
Se hicieron búsquedas en las siguientes bases de datos electrónicas: el Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials, CENTRAL, número 9 de 12, septiembre de 2012); MEDLINE (Ovid, desde 1946 hasta octubre de 2012, semana 1); EMBASE (Ovid, desde 1980 hasta 2012, semana 41); ISI Web of Science (desde 1970 hasta 16 de octubre de 2012); Database of Abstracts of Reviews of Effects (DARE), Health Technology Assessment Database and Health Economics Evaluations Database (número 3 de 12, septiembre de 2012). Se realizaron búsquedas en los registros de ensayos y en listas de referencias de revisiones, y no se aplicaron restricciones de idioma.
Criterios de selección
Se seleccionaron los ensayos controlados aleatorios realizados en adultos saludables y en adultos con alto riesgo de ECV. Un hábito dietético mediterráneo se definió como aquel que incluía al menos dos de los siguientes componentes: (1) cociente alto de grasas monoinsaturadas / saturadas, (2) consumo bajo a moderado de vino tinto, (3) consumo alto de leguminosas, (4) consumo alto de granos y cereales, (5) consumo alto de frutas y vegetales, (6) consumo bajo de carnes y productos derivados de la carne y aumento del consumo de pescado y (7) consumo moderado de leche y productos lácteos. El grupo de comparación no recibió intervención o recibió una intervención mínima. Los resultados incluyeron eventos clínicos y factores de riesgo de ECV.
Obtención y análisis de los datos
Dos revisores extrajeron los datos de forma independiente y establecieron contacto con los investigadores principales para obtener información relevante adicional.
Resultados principales
Se incluyeron 11 ensayos (15 artículos) (52 044 participantes asignados al azar). Los ensayos fueron heterogéneos en cuanto a los participantes reclutados, el número de componentes dietéticos y los períodos de seguimiento. Siete ensayos describieron la intervención como una dieta mediterránea. Los eventos clínicos se informaron solamente en un ensayo (Women's Health Initiative, 48 835 mujeres posmenopáusicas, intervención no descrita como una dieta mediterránea pero con un aumento de la ingesta de frutas, vegetales y cereales), donde no se observaron efectos estadísticamente significativos de la intervención en las variables principales de evaluación mortales y no mortales a los ocho años. Se observaron reducciones pequeñas en el colesterol total (‐0,16 mmol/l; intervalo de confianza [IC] del 95%: ‐0,26 a ‐0,06; modelo de efectos aleatorios) y en el colesterol lipoproteína de baja densidad (LDL) (‐0,07 mmol/l; IC del 95%: ‐0,13 a ‐0,01) con la intervención. Los análisis de subgrupos mostraron reducciones mayores estadísticamente significativas en el colesterol total en los ensayos que describieron la intervención como una dieta mediterránea (‐0,23 mmol/l; IC del 95%: ‐0,27 a ‐0,2) en comparación con control (‐0,06 mmol/l; IC del 95%: ‐0,13 a 0,01). La heterogeneidad impidió los metanálisis de otros resultados. Las reducciones en la presión arterial se observaron en tres de cinco ensayos que informaron este resultado. Ninguno de los ensayos informó sobre eventos adversos.
Conclusiones de los autores
Las pruebas limitadas hasta la fecha indican algunos efectos favorables sobre los factores de riesgo cardiovasculares. Intervenciones más exhaustivas que se describen como una dieta mediterránea pueden producir más efectos beneficiosos sobre los niveles de lípidos que las intervenciones con menos componentes dietéticos. Se necesitan más ensayos para examinar la repercusión de la heterogeneidad de los participantes y de la intervención sobre los resultados.
PICOs
Resumen en términos sencillos
Dieta mediterránea para la prevención de enfermedades cardiovasculares
Está bien establecido que la dieta desempeña una función principal en el riesgo de enfermedades cardiovasculares. El hábito dietético mediterráneo tradicional es de interés particular debido a las observaciones desde los años sesenta de que las poblaciones de los países de la región mediterránea como Grecia e Italia, tenían una baja mortalidad por enfermedades cardiovasculares comparadas con las poblaciones del norte de Europa o de los EE.UU., probablemente como resultado de diferentes hábitos alimentarios.
Esta revisión evaluó los efectos de proporcionar asesoramiento dietético para seguir un hábito dietético de estilo mediterráneo a adultos sanos o pacientes con un aumento del riesgo de enfermedades cardiovasculares para prevenir la aparición de enfermedades cardiovasculares y reducir los factores de riesgo asociados a ellos. Las definiciones de un hábito dietético mediterráneo varían y solamente se incluyeron ensayos controlados aleatorios (ECA) de intervenciones que informaron al menos dos de los siguientes componentes: (1) cociente alto de grasas monoinsaturadas / saturadas, (2) consumo bajo a moderado de vino tinto, (3) consumo alto de leguminosas, (4) consumo alto de granos y cereales, (5) consumo alto de frutas y vegetales, (6) consumo bajo de carnes y productos derivados de la carne y aumento del consumo de pescado y (7) consumo moderado de leche y productos lácteos. El grupo control no recibió intervención o recibió una intervención mínima. Se encontraron 11 ECA (15 artículos) que cumplieron estos criterios. Los ensayos variaron grandemente en cuanto a los participantes reclutados y las diferentes intervenciones dietéticas. Cuatro ensayos se realizaron solamente en mujeres, dos ensayos solamente en hombres y los cinco restantes se realizaron en hombres y mujeres. Cinco ensayos se realizaron en individuos saludables y seis ensayos fueron en pacientes con aumento del riesgo de enfermedades cardiovasculares o cáncer. El número de componentes relevantes para un hábito dietético mediterráneo varió de dos a cinco y sólo siete ensayos describieron la intervención como una dieta mediterránea.
El ensayo más grande, que solamente reclutó mujeres posmenopáusicas y no se describió como una dieta mediterránea solo cumplió dos de los criterios descritos anteriormente, y no informó diferencias en la aparición de enfermedades cardiovasculares entre el grupo de asesoramiento dietético y el grupo control. Los otros ensayos midieron los factores de riesgo de las enfermedades cardiovasculares. Como los estudios fueron tan diferentes, no fue posible combinar los estudios para la mayoría de los resultados. Cuando fue posible combinar los estudios, se encontraron reducciones pequeñas en los niveles de colesterol total, así como en las concentraciones del colesterol lipoproteína de baja densidad (LDL) perjudicial. Las reducciones en el colesterol total fueron mayores en los estudios que describieron que proporcionaron una dieta mediterránea. Ninguno de los ensayos informó sobre efectos secundarios.
La revisión concluye que, de las pruebas limitadas hasta la fecha, un hábito dietético mediterráneo reduce algunos factores de riesgo cardiovasculares. Sin embargo, se necesitan más ensayos para examinar los efectos de las diferencias en los participantes reclutados y las diferentes intervenciones dietéticas y analizar qué intervenciones podrían funcionar mejor en diferentes poblaciones.
Authors' conclusions
Background
Description of the condition
Cardiovascular disease (CVD) is one of the leading causes of death worldwide (WHO 2011a). In 2008, it accounted for 30% of total global deaths, including 6.2 million deaths due to stroke and 7.2 million due to coronary heart disease (CHD) (WHO 2011a). The burden of CVD also varies considerably between regions (Müller‐Nordhorn 2008; Reddy 1998). Within Europe, there is a northeast to southwest gradient in mortality from ischaemic heart disease where mortality rates are higher in counties within Eastern Europe. The highest age‐adjusted standardised mortality rates (SMR) are found in Latvia (SMR 461), Estonia (SMR 446), Slovakia (SMR 369) and Lithuania (SMR 357), while the lowest rates are found in France (SMR 65), Portugal (SMR 87), Italy (SMR 92) and Spain (SMR 92) (Müller‐Nordhorn 2008). More globally, while reductions in CVD mortality have been observed in developed countries, there are increases in CVD mortality in developing countries (Reddy 1998). The World Health Organization state that over 80% of CVD deaths occur in low‐ and middle‐income countries and the number of CVD deaths will increase to 23.3 million by 2030, with CVD remaining the single leading cause of death (Mathers 2006; WHO 2011b).
There is a longstanding recognition that diet plays a major role in the aetiology of many chronic diseases, thereby contributing to a significant geographical variability in morbidity and mortality rates from chronic disease across different countries and populations worldwide (WHO 2003). In particular, early data from the Seven Countries study in the 1960s showed that populations in countries of the Mediterranean region, such as Greece and Italy, experienced lower mortality from CVD compared with northern European populations such as Finland or the US, probably as a result of different dietary patterns (Keys 1986). Thereafter, the potential beneficial effects of the Mediterranean dietary pattern on longevity and health outcomes have become a source of much interest and investigation. Several observational studies have shown greater longevity and quality of life, as well as reduced mortality and morbidity from CVD, cancer and other nutrition‐related diseases with greater adherence to a Mediterranean dietary pattern (Benetou 2008; Buckland 2009; Feart 2009; Fung 2009; Knoops 2004; Lagiou 2006; Mitrou 2007; Trichopoulou 1995; Trichopoulou 2003; Trichopoulou 2007). For example, findings from the Spanish European Prospective Investigation into Cancer and Nutrition (EPIC) cohort study showed that a 1‐unit increase in Mediterranean diet score (scale from 0 to 18 units) was associated with a 6% reduced risk of CHD, with similar risk estimates by sex (Buckland 2009). Systematic reviews of observational prospective studies have confirmed that greater adherence to a Mediterranean diet is associated with a significant improvement in health status and a significant reduction in overall mortality, as well as in morbidity and mortality from CVD and other major chronic diseases (Sofi 2008; Sofi 2010). Specifically, in the latest published meta‐analysis of prospective cohort studies, a 2‐point increase (scale from 0 to 7‐9 points) in adherence to a Mediterranean dietary pattern was associated with an 8% reduction in all‐cause mortality and a 10% reduction in CVD incidence or mortality (Sofi 2010).
Furthermore, the Mediterranean diet has been associated with favourable effects on major CVD risk factors. For example, studies have documented a decreased incidence of hypertension, diabetes mellitus and metabolic syndrome as a whole with a greater adherence to a Mediterranean dietary pattern (Martnez‐Gonzalez 2008; Nunez‐Cordoba 2009; Psaltopoulou 2004; Rumawas 2009; Sánchez‐Taínta 2008). These findings have been corroborated by systematic reviews supporting beneficial effects of the Mediterranean diet on metabolic syndrome and its individual components (Buckland 2008; Kastorini 2011).
Against this large body of epidemiological observational studies, there is less evidence from well‐conducted and adequately powered randomised controlled trials (RCTs), especially with regard to the potential efficacy of the Mediterranean diet in the primary prevention of CVD (Serra‐Majem 2006). Most of the RCTs have addressed the effect of a Mediterranean type of diet on the occurrence of complications and recurrent events in people with existing CVD, showing favourable effects in CVD secondary prevention (Barzi 2003; de Lorgeril 1994; de Lorgeril 1996; de Lorgeril 1999). There is also considerable variability in the definition of, and duration of, the interventions evaluated.
Description of the intervention
The Mediterranean diet has been defined (Helsing 1989; Nestle 1995; Serra‐Majem 1993; Willett 1995), and includes the following dietary factors: a high intake of plant foods comprising mainly fruits and vegetables, cereals and whole‐grain breads, beans, nuts and seeds; locally grown, fresh and seasonal, unprocessed foods; large quantities of fresh fruit consumed daily whereas concentrated sugars or honey are consumed a few times per week in smaller quantities; olive oil as a main cooking ingredient and source of fat; low to moderate amounts of cheese and yogurt; low quantities of red meat and higher quantities of fish; and low to moderate amounts of red wine often accompanying main meals. The original Mediterranean type of diet reflects the common dietary pattern of communities in countries of the Mediterranean region in the early 1960s (Keys 1986), which was an expression of common cultural and historical roots, and a shared set of lifestyle and eating habits rather than a mere assortment of specific micro‐ and macro‐nutrients (Trichopoulou 1997).
The intervention under investigation for the current review was dietary advice to follow a Mediterranean‐style diet or a provision of foods relevant to the Mediterranean diet. At least two components from the following list were required to reach our definition of a Mediterranean‐style dietary pattern (Helsing 1989; Nestle 1995; Serra‐Majem 1993; Willett 1995):
-
high monounsaturated/saturated fat ratio (use of olive oil as main cooking ingredient);
-
low to moderate red wine consumption;
-
high consumption of legumes;
-
high consumption of grains and cereals;
-
high consumption of fruits and vegetables;
-
low consumption of meat and meat products and increased consumption of fish;
-
moderate consumption of milk and dairy products.
We chose at least two of the above components as our definition of a Mediterranean‐style dietary pattern as one component does not constitute a dietary pattern.
How the intervention might work
There is a large quantity of observational and experimental evidence supporting potential mechanisms to explain the beneficial effect of the Mediterranean diet on cardiovascular health (Serra‐Majem 2006). For example, there is evidence of favourable effects of the Mediterranean diet on insulin resistance and endothelium‐dependent vasoreactivity, as well as of the antioxidant and anti‐inflammatory effects of the Mediterranean diet and its individual components such as fruits and vegetables, olive oil, whole grains, fish and red wine (Chrysohoou 2004; Dai 2008; Pitsavos 2005; Ryan 2000). In addition, the Mediterranean dietary pattern has been associated with beneficial effects on many cardiovascular risk factors, including lipoproteins, obesity, diabetes mellitus and hypertension (Buckland 2008; Kastorini 2011; Martnez‐Gonzalez 2008; Nunez‐Cordoba 2009; Psaltopoulou 2004; Rumawas 2009; Sánchez‐Taínta 2008). There is additionally a large body of consistent epidemiological evidence supporting the notion that light to moderate red wine intake (one or two drinks/day), and moderate alcohol consumption in general, is associated with reduced all‐cause and cardiovascular mortality and morbidity, and has beneficial effects on cardiovascular risk factors, when compared with both abstention and heavy drinking (Brien 2011; Corrao 2000; Di Castelnuovo 2002; Di Castelnuovo 2006; Ronksley 2011). In contrast, excess alcohol consumption is associated with an increased risk of cardiovascular mortality and morbidity, primarily through an increased risk of hypertension and stroke (Stranges 2004; Taylor 2009).
Why it is important to do this review
Modification of dietary factors forms an integral part of the primary prevention of CVD disease. A Mediterranean‐style dietary pattern is likely to produce a beneficial effect on the occurrence of several chronic diseases, primarily CVD, which are closely linked to lifestyle and eating habits. This notion is corroborated by dietary recommendations of several scientific associations for the prevention of major chronic disease (AHA 2006; WHO 2003). To our knowledge, there have been no systematic reviews conducted to examine the effectiveness of the Mediterranean dietary pattern in the primary prevention of CVD. Most of the randomised evidence has addressed the effect of a Mediterranean type of diet on the occurrence of complications and recurrent events in people with existing CVD, rather than in the primary prevention setting (Barzi 2003; de Lorgeril 1994; de Lorgeril 1999; Serra‐Majem 2006). There is also a wide degree of heterogeneity in the definition and duration of the intervention.
Objectives
To determine the effectiveness of dietary advice to follow a Mediterranean‐style dietary pattern or the provision of foods relevant to the Mediterranean diet for the primary prevention of CVD.
Methods
Criteria for considering studies for this review
Types of studies
RCTs
Types of participants
Adults of all ages (18 years or more) from the general population and those at high risk of CVD. The review focused on the effects of a Mediterranean dietary pattern for the primary prevention of CVD. Therefore, we excluded studies where more than 25% of participants had CVD at baseline including people who had experienced a previous myocardial infarction (MI), stroke, revascularisation procedure (coronary artery bypass grafting (CABG) or percutaneous transluminal coronary angioplasty (PTCA)), people with angina, or angiographically defined CHD, cerebrovascular disease (stroke) and peripheral arterial disease. We also excluded studies where more than 25% of the participants had type 2 diabetes as while patients with type 2 diabetes are at increased risk of CVD, interventions for diabetes are covered specifically by the Cochrane Metabolic and Endocrine Disorders review group.
Types of interventions
The intervention was specific dietary advice to follow a Mediterranean‐style dietary pattern or provision of dietary factors relevant to the Mediterranean diet. At least two components from the following list were required to meet our definition of a Mediterranean‐style diet (Helsing 1989; Nestle 1995; Serra‐Majem 1993; Willett 1995).
-
High monounsaturated/saturated fat ratio (use of olive oil as main cooking ingredient).
-
Low to moderate red wine consumption.
-
High consumption of legumes.
-
High consumption of grains and cereals.
-
High consumption of fruits and vegetables.
-
Low consumption of meat and meat products and increased consumption of fish.
-
Moderate consumption of milk and dairy products.
We intended to consider studies examining dietary advice to follow a Mediterranean‐style diet separately from studies examining the provision of foods, but, for all studies that met our inclusion criteria, the intervention was dietary advice. It was also our intention to stratify results according to the number of components constituting the Mediterranean dietary pattern, the intensity and duration of the intervention and follow‐up period, and the effects of age and gender. However, there were insufficient trials that met the inclusion criteria to perform these analyses. We did consider interventions describing themselves as a Mediterranean diet or style of diet including the core components of increased fruit and vegetable consumption and exchange of saturated fat for monounsaturated fat, compared with other interventions that met our criteria, in subgroup analyses.
We focused on follow‐up periods of three months or more. We only considered trials where the comparison group was no intervention or minimal intervention (e.g. leaflet to follow a dietary pattern with no person‐to‐person intervention or reinforcement). The rationale for this was to determine the effects of a Mediterranean dietary pattern more clearly rather than to include other dietary interventions as comparison groups. We did not exclude studies where loss to follow‐up was greater than 20%, but we carried out sensitivity analyses to examine the effect of excluding these studies on the overall effect estimate.
Types of outcome measures
Endpoints were measured using validated measures.
Primary outcomes
-
Cardiovascular mortality.
-
All‐cause mortality.
-
Non‐fatal endpoints such as MI, CABG, PTCA, angina, or angiographically defined CHD, stroke, carotid endarterectomy or peripheral arterial disease (PAD).
Secondary outcomes
-
Changes in blood lipids (total cholesterol, high‐density lipoprotein (HDL) cholesterol, low‐density lipoprotein (LDL) cholesterol, triglycerides), and blood pressure (systolic and diastolic blood pressure).
-
Occurrence of type 2 diabetes as a major CVD risk factor.
-
Health‐related quality of life.
-
Adverse effects (as defined by the authors of the included trials).
-
Costs.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases:
-
Cochrane Central Register of Controlled Trials (CENTRAL, Issue 9 of 12, September 2012);
-
MEDLINE (Ovid, 1946 to October week 1 2012);
-
EMBASE (Ovid, 1980 to 2012 week 41);
-
ISI Web of Science (1970 to 16 October 2012);
-
Database of Abstracts of Reviews of Effects (DARE), Health Technology Assessment Database and Health Economic Evaluations Database (Issue 3 of 12, September 2012).
We used medical subject headings (MeSH) or equivalent and text word terms and the Cochrane sensitive‐maximising RCT filter for MEDLINE (Lefebvre 2011), and adaptations of it for EMBASE and Web of Science. We applied no language restrictions. We tailored searches to individual databases (Appendix 1).
Searching other resources
In addition, we checked reference lists of reviews for additional studies.
We searched the metaRegister of controlled trials (mRCT) (www.controlled‐trials.com/mrct), Clinicaltrials.gov (www.clinicaltrials.gov) and the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (apps.who.int/trialsearch/) for ongoing trials.
We contacted authors where necessary for additional information.
Data collection and analysis
Selection of studies
From the searches, two review authors (KR, LH or NF) reviewed the title and abstract of each paper and retrieved potentially relevant references. Following this initial screening, we obtained the full‐text reports of potentially relevant studies, and two review authors (KR, LH or NF) independently selected studies to be included in the review using predetermined inclusion criteria. In all cases, we resolved disagreements about any study inclusions by consensus and consulted a third review author (MT) if disagreement persisted.
Data extraction and management
Two review authors (KR, LH or NF) independently extracted data using a proforma, and contacted chief investigators to request additional relevant information if necessary. We extracted details of the study design, participant characteristics, study setting, intervention (including number of components and duration), and outcome data including details of outcome assessment, adverse effects, and methodological quality (randomisation, blinding, attrition) from each of the included studies. We resolved disagreements about extracted data by consensus.
Assessment of risk of bias in included studies
We assessed risk of bias by examining the quality of the random sequence generation and allocation concealment, description of dropouts and withdrawals (including analysis by intention to treat (ITT)), blinding (participants, personnel and outcome assessment) and selective outcome reporting (Higgins 2011). Two review authors (KR, LH or NF) independently assessed the risk of bias of included studies and rated each domain as having a 'low risk of bias', a 'high risk of bias' or an 'unclear risk of bias'.
Measures of treatment effect
We processed data in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We expressed dichotomous outcomes (available for only one trial) as hazard ratios (HR) with 95% confidence intervals (CI). For continuous variables, we compared net changes (i.e. intervention group minus control group differences) and calculated mean differences (MD) and 95% CIs for each study.
Assessment of heterogeneity
For each outcome, we carried out tests of heterogeneity (using the Chi2 test of heterogeneity and the I2 statistic). In the situation of no heterogeneity, we performed a fixed‐effect meta‐analysis. If we detected substantial heterogeneity, we looked for possible explanations for this (e.g. participants and intervention). If we could not explain the heterogeneity, the review authors considered the following options: provide a narrative overview and not aggregate the studies at all, or use a random‐effects model with appropriate cautious interpretation.
Subgroup analysis and investigation of heterogeneity
It was our intention to report the results separately for dietary advice to follow a Mediterranean dietary pattern and provision of foods relevant to a Mediterranean‐style diet. However, to date we have found only trials of dietary advice to follow a Mediterranean dietary pattern. If there were sufficient trials that met the inclusion criteria it was also our intention to examine the impact of the number of components of the Mediterranean dietary pattern, the intensity and duration of the intervention, the follow‐up period, and the effects of gender and age. We have performed subgroup analyses to examine the effect of interventions described as the Mediterranean diet or style of diet or those including both of the core components of increased fruit and vegetable consumption and exchange of saturated fat for monounsaturated fat, compared with other interventions meeting our criteria.
Sensitivity analysis
If there had been sufficient trials that met the inclusion criteria, it was our intention to perform sensitivity analyses excluding studies of low methodological quality and undertake funnel plots and tests of asymmetry to assess possible publication bias (Egger 1997). We did perform sensitivity analyses excluding studies where loss to follow‐up exceeded 20%.
Results
Description of studies
Results of the search
The database searches generated 13,406 hits and 10,680 after de‐duplication. We identified two additional records by searching other resources. Screening the titles and abstracts of the 10,682 records identified 249 papers for formal inclusion or exclusion. Of these, 11 RCTs (15 papers) met the inclusion criteria. We identified one ongoing trial and one trial is awaiting classification. The flow of studies throughout the review is presented in the PRISMA diagram in Figure 1.
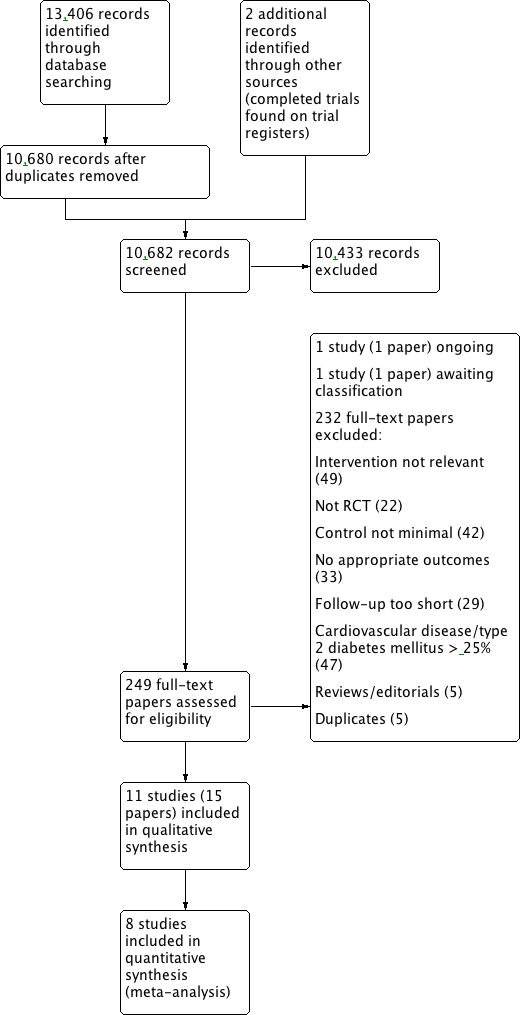
Study flow diagram.
Included studies
Details of the methods, participants, intervention, comparison group and outcome measures for each of the studies included in the review are shown in the Characteristics of included studies table. Eleven trials (15 papers) were included with 52,044 participants randomised. The majority of participants were enrolled in one large multicentre trial (48,835 women; WHI)
The health status of participants varied between studies. The majority of participants (49,185 randomised) were classified as healthy and were recruited by five of the trials (Abedi 2010; Castagnetta 2002; Djuric 2009; Konstantinidou 2010; WHI). The remaining six trials recruited previously untreated hypercholesteraemic participants (Jula 2002; Wardle 2000), elderly participants with long‐standing hypercholesterolaemia (Lindman 2004), overweight or obese participants with untreated hypertension (ENCORE), sedentary people with metabolic syndrome (Esposito 2004), and one trial recruited participants at high risk of colorectal cancer (Lanza 2001). Three trials including the largest trial recruited only women who were postmenopausal (Abedi 2010; Castagnetta 2002; WHI), and one trial recruited only women aged 25 to 65 years (Djuric 2009). In contrast, two trials recruited only men (Jula 2002; Lindman 2004), and the remaining five recruited both men and women (ENCORE; Esposito 2004; Konstantinidou 2010; Lanza 2001; Wardle 2000). The trials were conducted in the US (Djuric 2009; ENCORE; Lanza 2001; WHI), Italy (Castagnetta 2002; Esposito 2004), Finland (Jula 2002), Spain (Konstantinidou 2010), Norway (Lindman 2004), Iran ( Abedi 2010), and the UK (Wardle 2000), and the duration of the intervention and follow‐up periods varied from three months (Jula 2002; Konstantinidou 2010; Wardle 2000 ), four months (ENCORE), six months (Abedi 2010; Castagnetta 2002; Djuric 2009; Lindman 2004), two years (Esposito 2004), four years (Lanza 2001), and up to eight years (WHI).
One trial had a dietary intervention that comprised five components that met our definition of a Mediterranean‐style diet (see Types of interventions for list of components) (Castagnetta 2002), one trial had a dietary intervention that comprised four components (ENCORE), five trials had dietary interventions that comprised three components (Esposito 2004; Jula 2002; Konstantinidou 2010; Lindman 2004; Wardle 2000). The remaining four trials had a dietary intervention comprising two components (Abedi 2010; Djuric 2009; Lanza 2001; WHI). Seven trials described the intervention as a Mediterranean diet or Mediterranean‐style diet (Castagnetta 2002; Djuric 2009; Esposito 2004; Jula 2002; Konstantinidou 2010; Lindman 2004; Wardle 2000). The remaining trials fulfilled our definition of two or more components of the Mediterranean diet but did not include both of the key components associated with the Mediterranean diet (increasing fruit and vegetable intake and exchanging saturated fat for monounsaturated fat) (Abedi 2010; ENCORE; Lanza 2001; WHI).
We identified one ongoing trial (Sanders 2012) (see Characteristics of ongoing studies table). Briefly, this trial examines the effects of a cardioprotective diet (decreased salt and saturated fatty acids intake, and increased whole grain cereals, fruit and vegetables and oily fish intake) with a control diet (average UK diet), in healthy men and women, for a period of three months. The outcomes measured include systolic blood pressure and lipid levels. The anticipated end date for this trial was December 2012.
One study is awaiting classification (Inguaggiato 2011) (see Characteristics of studies awaiting classification table).
Excluded studies
Details and reasons for exclusion for the studies that most closely missed the inclusion criteria are presented in the Characteristics of excluded studies table. Reasons for exclusion for the majority of studies was due to the control group not being minimal (e.g. receiving face‐to‐face dietary advice) and studies not being RCTs.
Risk of bias in included studies
Details are provided for each of the included studies in the 'Risk of bias' section of the Characteristics of included studies table. We assessed risk of bias as 'low', 'high' or 'unclear'.
Allocation
The methods of random sequence generation were unclear in seven of the 11 included studies (Abedi 2010; Castagnetta 2002; Djuric 2009; Jula 2002; Lanza 2001; Lindman 2004; Wardle 2000). In the four studies where this was clear, we judged the methods used to be of low risk of bias (ENCORE; Esposito 2004; Konstantinidou 2010; WHI). The methods of allocation concealment were unclear in eight of the 11 included studies. Where this was clear, we judged the methods used to be at low risk of bias (ENCORE; Esposito 2004; Wardle 2000).
Blinding
The blinding of participants and personnel was unclear in all 11 trials. However, the blinding of participants and personnel for behavioural interventions is difficult, if not impossible, in most cases. Blinding of outcome assessment was unclear in seven of the 11 trials (Abedi 2010; Castagnetta 2002; Djuric 2009; Konstantinidou 2010; Lanza 2001; Lindman 2004; Wardle 2000). In the remaining four trials, outcome assessments were made blind to the group assignment and were judged to be at low risk of bias (ENCORE; Esposito 2004; Jula 2002; WHI).
Incomplete outcome data
We judged four of the 11 trials to be of low risk of bias as reasons for exclusions and loss‐to‐follow‐up were provided or ITT analyses were performed, or both (ENCORE; Esposito 2004; Konstantinidou 2010; WHI). We judged three studies to be at high risk of bias as no reasons were provided for excluded participants (Jula 2002), and there was differential loss to follow‐up that exceeded 20% in the control group in one trial (Abedi 2010), and in the intervention group in another trial (Djuric 2009). We examined the exclusion of these two trials in sensitivity analyses. For the remaining trials, we judged the risk of bias as unclear.
Selective reporting
For four of the studies, the risk of bias associated with selective reporting was unclear (Castagnetta 2002; Jula 2002; Konstantinidou 2010; Lindman 2004), the remaining seven studies clearly stated the primary and secondary outcomes and reported the results for these.
Other potential sources of bias
There was insufficient information to judge the risk of bias in other sources of bias not covered above and we categorised all studies as unclear.
Effects of interventions
Clinical events
The largest trial had long‐term follow‐up of eight years and was the only trial reporting clinical events (WHI). In participants without a history of CVD (3.4% had CVD at baseline), there were no statistically significant effects of the dietary intervention on non‐fatal MI (HR 0.91, 95% CI 0.8 to 1.04), CHD death (HR 1.01, 95% CI 0.81 to 1.27), revascularisation (HR 0.91, 95% CI 0.82 to 1.01), fatal stroke (HR 0.94, 95% CI 0.65 to 1.35), non‐fatal stroke (HR 1.04, 95% CI 0.90 to 1.19) and total CVD events (clinical MI, silent MI, death due to CHD, CABG/percutaneous coronary intervention and stroke) (HR 0.96, 95% CI 0.89 to 1.03). The WHI trial was not described as a Mediterranean‐style diet neither did it comprise of both an increase in fruit and vegetable consumption and exchanging saturated fat for monounsaturated fat. It met our inclusion criteria of two components that included increasing fruit and vegetable and cereal and grain intake. None of the studies describing their interventions as a Mediterranean diet reported clinical events.
Cardiovascular risk factors
Lipid levels
Total cholesterol
Eight trials (4151 participants randomised) measured total cholesterol levels and reported data that could be used in meta‐analyses (Abedi 2010; Djuric 2009; ENCORE; Esposito 2004; Konstantinidou 2010; Lanza 2001; Wardle 2000; WHI). Lipid levels were measured in only a subgroup (n = 2816) of the large WHI trial (WHI). There was significant heterogeneity between trials (I2 = 74%). Pooling the studies resulted in similar estimates for both fixed‐effect and random‐effects models indicating that there was no strong evidence of small study effects, so we reported the random‐effects model, with appropriate cautious interpretation. The dietary intervention reduced total cholesterol levels by 0.16 mmol/L (95% CI 0.06 to 0.26; random‐effects model, P value = 0.003; Analysis 1.1). Two of the trials were at high risk of bias as there was differential loss to follow‐up that just exceeded 20% in the control group (Abedi 2010), and intervention group (Djuric 2009), of each trial. Sensitivity analyses excluding these two trials produced a similar effect estimate (MD ‐0.18, 95% CI ‐0.28 to ‐0.07).
Two further trials measured total cholesterol but did not provide data in a useable format for meta‐analyses despite our efforts to obtain these (Castagnetta 2002; Jula 2002). Both trials reported significant reductions in total cholesterol levels with the dietary intervention.
We performed subgroup analyses to examine the effect of interventions described as a Mediterranean or Mediterranean‐style diet and those that comprised at least two components but did not comprise both of the core components of increasing fruit and vegetable intake and exchanging saturated fat for monounsaturated fat. The reduction in total cholesterol was statistically significantly greater for interventions describing themselves as a Mediterranean diet (MD 0.23, 95% CI ‐0.27 to ‐0.2) compared with those that did not (MD ‐0.06, 95% CI ‐0.13 to 0.01; Analysis 1.2).
Low‐density lipoprotein cholesterol
Six trials (3227 participants randomised) measured LDL‐cholesterol and provided data that could be pooled in a meta‐analysis (Abedi 2010; Djuric 2009; ENCORE; Konstantinidou 2010; Wardle 2000; WHI). Heterogeneity was low to moderate (I2 = 22%) and we performed a fixed‐effect meta‐analysis. There was a small but statistically significant reduction in LDL‐cholesterol (MD ‐0.07 mmol/L, 95% CI ‐0.13 to ‐0.01) with the dietary intervention, and results were dominated by the largest trial (WHI) (Analysis 1.3). Two of the trials were at high risk of bias as there was differential loss to follow‐up that just exceeded 20% in the control group (Abedi 2010) and intervention group (Djuric 2009) of each trial. Sensitivity analyses excluding these two trials produced a similar effect estimate (MD ‐0.08, 95% CI ‐0.14 to ‐0.02).
A further trial reported LDL‐cholesterol but did not report follow‐up data and attempts to retrieve this were unsuccessful (Jula 2002). This trial reported a statistically significant reduction in LDL‐cholesterol of 10.8% with the intervention.
We performed subgroup analyses to examine the effect of interventions describing themselves as a Mediterranean or Mediterranean‐style diet and those that comprised at least two components but did not comprise both of the core components of increasing fruit and vegetable intake and exchanging saturated fat for monounsaturated fat. The reduction in LDL‐cholesterol was greater for interventions describing themselves as a Mediterranean diet (MD ‐0.16, 95% CI ‐0.39 to 0.07; random‐effects model) compared with those that did not (MD ‐0.06, 95% CI ‐0.12 to 0.00; random‐effects model), but this did not reach statistical significance (Analysis 1.4).
High‐density lipoprotein cholesterol
Eight trials measured the effect of the diet on HDL‐cholesterol (Abedi 2010; Djuric 2009; ENCORE; Esposito 2004; Jula 2002; Konstantinidou 2010; Wardle 2000; WHI, 3527 participants randomised) but we could not obtain follow‐up data from one of the authors (Jula 2002). There was significant heterogeneity between the remaining seven trials (I2 = 83%) and so we did not perform a meta‐analysis. One trial reported a statistically significant increase in HDL‐cholesterol levels with the intervention (MD 0.08 mmol/L, 95% CI 0.06 to 0.09) (Esposito 2004). The remaining six trials found no effect of the intervention on HDL‐cholesterol levels (MD 0.01 mmol/L, 95% CI ‐0.08 to 0.1 (Abedi 2010); MD 0.03 mmol/L, 95% CI ‐0.15 to 0.2 (Djuric 2009); MD ‐0.04 mmol/L, 95% CI ‐0.17 to 0.09 (ENCORE); MD 0.00 mmol/L, 95% CI ‐0.08 to 0.08 (Konstantinidou 2010); MD ‐0.06 mmol/L, 95% CI ‐0.18 to 0.06 (Wardle 2000); MD ‐0.01 mmol/L, 95% CI ‐0.03 to 0.02 (WHI)). The study that did not provide follow‐up data reported a statistically significant reduction in HDL‐cholesterol of 4.9% (Jula 2002).
Triglycerides
Nine trials measured triglyceride levels (Abedi 2010; Djuric 2009; ENCORE; Esposito 2004; Jula 2002; Konstantinidou 2010; Lindman 2004; Wardle 2000; WHI, 3626 participants randomised). Two of the trials provided postintervention values as medians (with 25th and 75th percentiles) and were not included in the analysis (Konstantinidou 2010; Lindman 2004) and one trial did not report follow‐up data (Jula 2002). There was significant heterogeneity between the remaining six trials (I2 = 94%) and so we did not perform a meta‐analysis. There was a statistically significant reduction in triglyceride levels with the intervention in one trial (MD ‐0.21, 95% CI ‐0.23 to ‐0.19; Esposito 2004). In four trials, the dietary intervention showed no effect on triglyceride levels (MD ‐0.05 mmol/L, 95% CI ‐0.49 to 0.39 (Abedi 2010); MD 0.00 mmol/L, 95% CI ‐0.23 to 0.23 (Djuric 2009); MD ‐0.01 mmol/L, 95% CI ‐0.24 to 0.22 (ENCORE); MD 0.00, 95% CI ‐0.05 to 0.05 (WHI)). In the remaining trial, the dietary intervention produced a statistically significant increase in triglyceride levels (MD 0.36 mmol/L, 95% CI 0.15 to 0.57; Wardle 2000). In the two trials reporting medians, no effect of the diet on triglyceride levels was observed (Konstantinidou 2010; Lindman 2004). Similarly, in the study where no follow‐up data were reported, no effect of the diet on triglyceride levels was seen (Jula 2002).
Blood pressure
Five trials measured systolic and diastolic blood pressure (Abedi 2010; ENCORE; Esposito 2004; Konstantinidou 2010; WHI, 42,724 participants randomised). Substantial heterogeneity existed between the trials for both outcomes (I2 = 94% and 93%, respectively), and differences were observed between fixed‐ and random‐effects models suggesting small trial effects, so we did not perform meta‐analyses. A statistically significant reduction in systolic blood pressure was observed in three of the trials (MD ‐7.8 mmHg, 95% CI ‐12.11 to ‐3.49 (ENCORE); MD ‐3.00 mmHg, 95% CI ‐3.46 to ‐2.54 (Esposito 2004); MD ‐0.70 mmHg, 95% CI ‐1.03 to ‐0.37 (WHI)). The remaining two trials did not show a statistically significant reduction in systolic blood pressure (Abedi 2010; Konstantinidou 2010). For diastolic blood pressure, a statistically significant reduction was observed in three of the trials (MD ‐3.7 mmHg, 95% CI ‐6.1 to ‐1.3 (ENCORE); MD ‐2.00 mmHg, 95% CI ‐2.29 to ‐1.71 (Esposito 2004); MD ‐0.70 mmHg, 95% CI ‐0.88 to ‐0.52 (WHI)). The remaining two trials did not show a statistically significant reduction in diastolic blood pressure (Abedi 2010; Konstantinidou 2010).
Type 2 diabetes
Incident‐treated diabetes was reported during the eight years of follow‐up of the WHI trial (WHI). They found no statistically significant difference in the diabetes risk between the intervention and control group (HR 0.96, 95% CI 0.90 to 1.03).
Health‐related quality of life, adverse effects or costs
None of the trials reported health‐related quality of life, adverse effects or costs.
There was significant heterogeneity in many of the outcomes and, in most cases, a narrative synthesis was performed. The heterogeneity is probably due to the varying interventions with different numbers of components relevant to the Mediterranean diet and also the participants, both healthy populations and those at high risk of CVD. It was our intention to explore this heterogeneity further in stratified analyses but, to date, there are insufficient studies included in this review to do this. However, we will conduct this in an update of this review when more evidence accrues.
Discussion
The aim of this review was to evaluate the effectiveness of dietary advice to follow a Mediterranean‐style diet or the provision of foods relevant to the Mediterranean diet for the primary prevention of CVD. We also examined the effects of a Mediterranean‐style diet on major cardiovascular risk factors including blood lipids, blood pressure and occurrence of type 2 diabetes.
Summary of main results
Relatively few trials were included in this review, 11 completed RCTs (15 papers) and one ongoing RCT met the inclusion criteria of our definition of a Mediterranean dietary pattern. All trials examined the effects of dietary advice to follow a Mediterranean‐style dietary pattern; none of the trials examined the effects of provision of foods relevant to a Mediterranean diet. The number of components of the Mediterranean diet varied from two to five, and seven trials described the intervention as a Mediterranean diet. Only one trial, the largest with 48,835 postmenopausal women randomised, reported clinical events and showed no statistically significant effects of the intervention on both fatal and non‐fatal endpoints at eight years' follow‐up (WHI), and incident diabetes rates were also similar between the intervention and control group for this trial. The WHI trial was not described as Mediterranean diet and comprised only two of the components in our definition (WHI). None of the studies describing the intervention as a Mediterranean diet reported clinical events. Cardiovascular risk factors were measured in all trials but heterogeneity between trials precluded meta‐analysis for some outcomes. Small reductions in total cholesterol and LDL‐cholesterol occurred with the dietary interventions where pooling was appropriate (total cholesterol: MD ‐0.16 mmol/L, 95% CI ‐0.26 to ‐0.06, random‐effects model; LDL‐cholesterol: ‐0.07 mmol/L, 95% CI ‐0.13 to ‐0.01, respectively). Subgroup analyses revealed larger reductions in total cholesterol in those studies describing the intervention as a Mediterranean diet (MD ‐0.23 mmol/L, 95% CI ‐0.27 to ‐0.2 versus ‐0.06 mmol/L, 95% CI ‐0.13 to 0.01; P value < 0.001). Blood pressure was reduced in three of the five trials reporting this outcome. None of the trials reported health‐related quality of life, adverse events or costs. There was significant heterogeneity in the different dietary interventions both in terms of the number of components relevant to a Mediterranean dietary pattern, intensity and duration, the participants recruited and the follow‐up periods. To date there are an insufficient number of trials to perform stratified analyses to examine the effects of these further on outcomes.
Overall completeness and applicability of evidence
We included 11 trials (15 papers) with 52,044 participants randomised. We also identified one ongoing trial (Sanders 2012). However, only the largest trial (WHI), which recruited postmenopausal women only (48,835 randomised), contributed data to our primary outcomes of major CVD clinical endpoints. Therefore, the applicability of these findings to the male population is uncertain, given the well‐established differences in cardio‐metabolic risk factor profiles between women and men (Mosca 2011). In addition, the intervention was not described as a Mediterranean diet and satisfied only two components of a Mediterranean dietary pattern.
There was also a large variation in the health status of participants between studies. The majority of participants (49,185 randomised) were classified as healthy and were recruited by five of the trials (Abedi 2010; Castagnetta 2002; Djuric 2009; Konstantinidou 2010; WHI); most of these were in women. The remaining six trials recruited high‐risk individuals, that is hypercholesteraemic participants (Jula 2002, Lindman 2004; Wardle 2000), overweight or obese participants with untreated hypertension (ENCORE), and sedentary people with metabolic syndrome (Esposito 2004), and one trial recruited participants at high risk of colorectal cancer (Lanza 2001). Hence, the applicability of these findings to different population groups is uncertain. All trials were conducted in developed countries and most in Western populations; therefore, the generalisability of these findings to lower‐income settings has to be confirmed.
The effectiveness of the provision of foods relevant to the Mediterranean diet could not be assessed, because all studies that met the inclusion criteria were based on dietary advice to follow a Mediterranean‐style diet. It was also our intention to stratify results according to the number of components constituting the Mediterranean dietary pattern and the intensity and duration of the intervention. However, there was an insufficient number of trials that met the inclusion criteria to perform these analyses. However, we did perform subgroup analyses to examine the effect of interventions described as the Mediterranean diet with those that did not but met our criteria of two or more components. We found greater reductions in total cholesterol for interventions describing themselves as a Mediterranean diet that was statistically significant. A similar trend was seen for LDL‐cholesterol but few studies were included in this analysis. Therefore, it seems that a more comprehensive intervention such as those described as a Mediterranean diet targeting several food groups simultaneously may be more effective at least in reducing lipid levels.
The duration of the intervention and follow‐up periods varied widely across studies, ranging from short‐term trials (three to six months, Abedi 2010; Castagnetta 2002; Djuric 2009; ENCORE; Jula 2002; Konstantinidou 2010; Lindman 2004; Wardle 2000) to long‐term interventions (two to eight years, Esposito 2004; WHI). Both short‐ and long‐term health effects of dietary interventions are plausible in terms of cardiovascular health, given the relatively quick response of cardiovascular risk factors such as blood lipids and blood pressure to lifestyle and dietary modifications (AHA 2006; Appel 1997; Appel 2001; Appel 2006). However, it is likely that potential beneficial effects of dietary interventions for the prevention of major chronic disease endpoints, such as mortality, CVD and type 2 diabetes, should represent the outcome of a long‐term process linked to the interplay of dietary patterns with genetic and environmental factors. In addition, the sustainability of long‐term lifestyle and dietary modifications is challenging. Therefore, the public health relevance of trials with extremely short‐term dietary interventions or follow‐up periods in this context is questionable.
Quality of the evidence
Overall, the studies included in this review, especially the smaller short‐term trials, were at some risk of bias or there was insufficient information to judge the risk of bias; hence, results should be treated with some caution. The methods of random sequence generation were unclear in seven of the 11 included studies, in the four studies where this was clear, we judged the methods used to be of low risk of bias (ENCORE; Esposito 2004; Konstantinidou 2010; WHI). Similarly, the methods of allocation concealment were unclear in most of the included studies, and where this was clear, we judged the methods used to be at low risk of bias (ENCORE; Esposito 2004; Wardle 2000).
The blinding of participants and personnel was unclear in all 11 trials but the blinding of participants and personnel for behavioural interventions is difficult, if not impossible, in most cases. Blinding of outcome assessment was also unclear in most trials, outcome assessments were made blind to the group assignment in four trials and we judged them to be at low risk of bias (ENCORE; Esposito 2004; Jula 2002; WHI).
We judged four of the 11 trials to be of low risk of attrition bias as reasons for exclusions and loss‐to‐follow‐up were provided or ITT analyses were performed, or both (ENCORE; Esposito 2004; Konstantinidou 2010; WHI). We judged three studies to be at high risk of bias as no reasons were provided for excluded participants (Jula 2002), and there was differential loss to follow‐up that exceeded 20% in two trials (Abedi 2010; Djuric 2009). We examined the exclusion of these two trials in sensitivity analyses but they did not impact significantly on the effect estimates for either total cholesterol or LDL‐cholesterol levels. For the remaining trials, we judged the risk of bias as unclear.
We judged selective reporting to be at low risk of bias for the majority of studies as the primary and secondary outcomes were stated and results were reported for these. For four of the studies, the risk of bias associated with selective reporting was unclear (Castagnetta 2002; Jula 2002; Konstantinidou 2010; Lindman 2004). For all trials, there was insufficient information provided to assess the risk of bias in other sources of bias not covered above.
Potential biases in the review process
There was a high degree of heterogeneity between trials, from different sources (participants, nature and duration of intervention and follow‐up, outcome data), which precluded statistical pooling for most outcomes.
The WHI was the largest trial included, the only study contributing data to our primary outcomes, and dominated findings of this review (WHI). However, this study was based on a highly selected group of participants (i.e. postmenopausal women aged 50 to 79 years), which makes the generalisability of these findings uncertain. In fact, the possibility of different or greater effects by dietary interventions of this nature among men or younger age groups cannot be ruled out. Furthermore, a good proportion of WHI participants were on cardiovascular medication at baseline (approximately 12% on lipid‐lowering medication, 18% on aspirin and 43% had treated hypertension or blood pressure ≥140/90 mmHg), and some had prevalent CVD (3.4%). The distribution of cardiovascular medication was not different between intervention and comparison groups at baseline and did not change during the trial; however, this may have biased the results toward null findings if CVD risk factors such as blood pressure and lipid levels were optimally controlled prior to the intervention (bias against seeing no effect of the intervention). Indeed, after excluding participants with baseline CVD, there was an apparent trend toward small protective effects for CHD events in women without baseline disease (WHI), although this did not reach statistical significance. Finally, the WHI Dietary Modification Trial intervention comprised only two components that met our definition of a Mediterranean‐style diet, and was not specifically tailored for CVD prevention. However, it is plausible that more aggressive and targeted dietary interventions are necessary to influence CVD risk factors and, therefore, achieve a significant public health impact on CVD events (AHA 2006; Appel 1997; Appel 2001; Appel 2006).
Our decision to restrict this review to interventions that only focused on the effectiveness of a Mediterranean dietary pattern per se avoided the potential confounding effects of other behavioural interventions on our outcomes, for example, those involving increased exercise or weight loss in the context of multifactorial trials. Also, our strict inclusion criteria, particularly with regard to the comparison group, excluded a number of well‐known trials, such as the PREDIMED (Prevention with Mediterranean Diet) trial in Spain (Estruch 2006; Estruch 2013) or the DASH (Dietary Approaches to Stop Hypertension) trials (Appel 1997; Appel 2001; Appel 2006), where the control groups were not minimal. Our decision to exclude trials in people with diabetes who are at increased risk for CVD may also have missed relevant studies, but interventions for the management of diabetes are covered by the Cochrane Metabolic and Endocrine Disorders Group, and are not within the remit of the Cochrane Heart Group. Finally, the definition of the Mediterranean dietary pattern is not homogeneous, and may vary across different geographical and cultural contexts (Helsing 1989; Nestle 1995; Serra‐Majem 1993; Serra‐Majem 2006; Willett 1995). The result of this potential misclassification would probably be to underestimate the true effect of the dietary intervention on the selected outcomes (Copeland 1977). Our choice to use a classification system rather than include only those studies describing the intervention as a Mediterranean diet attempted to address this heterogeneity, and given sufficient studies would allow further exploration of active components. The components required to meet our definition of a Mediterranean dietary pattern were based on previous definitions (Helsing 1989; Nestle 1995; Serra‐Majem 1993; Serra‐Majem 2006; Willett 1995), and two or more components were required to meet our inclusion criteria. However, this definition resulted in the inclusion of several trials whose interventions included advice to follow a low‐fat diet (ENCORE; Lanza 2001; WHI), which does not constitute a Mediterranean dietary pattern, in addition to at least two other relevant components. Given the view that the original Mediterranean type of diet was an expression of common cultural and historical roots, and a shared set of lifestyle and eating habits rather than a mere assortment of specific micro‐ and macro‐nutrients (Trichopoulou 1997), we have performed some further analyses to examine the effects of interventions describing themselves as the Mediterranean diet and those that do not. Where this was possible, more comprehensive interventions targeting a number of components simultaneously showed greater reductions in total cholesterol than less comprehensive interventions. Future updates of this review will explore this further when more evidence accrues.
Agreements and disagreements with other studies or reviews
We are not aware of any previous systematic review involving only RCTs that has specifically examined the effectiveness of dietary advice to follow a Mediterranean‐style diet or the provision of foods relevant to the Mediterranean diet, as the only dietary intervention compared with no or minimal intervention, for the primary prevention of CVD in the general population of healthy adults across all ages and among individuals at high risk of CVD.
For example, one systematic review and meta‐analysis examined the effectiveness of a Mediterranean‐style diet compared with a low‐fat diet in RCTs among overweight/obese individuals with at least one additional cardiovascular risk factor or with established coronary artery disease (Nordmann 2011). Trials had to have a minimum follow‐up of six months, and to report ITT data on cardiovascular risk factors (i.e. changes in body weight, blood pressure and lipid levels). In this review, Mediterranean diets were defined as diets with moderate‐fat intake (where the main sources of added fat were olive oil and nuts), rich in vegetables and low in red meat (with poultry and fish replacing beef and lamb). Low‐fat diets were defined as diets aiming at an energy intake with 30% or less of calories from fat, based on the American Heart Association (AHA) dietary guidelines (Krauss 2000). Six trials were identified, including one secondary prevention trial, with 2650 participants randomised (50% women). Results of this meta‐analysis suggested favourable, though modest, effects of the Mediterranean diet, as compared with a low‐fat diet, on a wide range of cardiovascular risk factors and inflammatory markers, such as body weight, systolic and diastolic blood pressure, fasting plasma glucose, total cholesterol and high‐sensitivity C‐reactive protein. These results are generally consistent with the favourable but relatively modest effects on total cholesterol and blood pressure levels reported by individual trials in our review. The main methodological differences between the two reviews were the inclusion or exclusion of secondary prevention trials and the different definitions of the dietary intervention (whole dietary pattern vs. individual components).
Other systematic reviews have pooled together the evidence from both observational studies and RCTs on the effects of the Mediterranean dietary pattern on metabolic syndrome and individual cardiovascular risk factors, supporting favourable effects of the Mediterranean diet on cardio‐metabolic risk factors (Buckland 2008; Kastorini 2011).
The large primary prevention trial PREDIMED, which did not meet our strict inclusion criteria as the comparison group was not minimal, has reported beneficial effects of the Mediterranean diet on clinical endpoints (Estruch 2013). In this trial, 7447 participants were randomised to a dietary intervention that comprised five components of our definition of a Mediterranean‐style dietary pattern in contrast to two components for the WHI trial included in our review that also reports clinical endpoints (WHI). After 4.8 years of follow‐up, these authors showed a reduction of major CVD events of 30% (HR 0.7, 95% CI 0.54 to 0.92) with the Mediterranean dietary intervention and supplemented olive oil compared with a low‐fat control group (Estruch 2013). The individuals recruited to this trial were all at high risk of CVD (type 2 diabetes or at least three CVD risk factors from smoking, hypertension, hypercholesterolaemia, overweight or obesity, or family history of CVD).
Likewise, systematic reviews and meta‐analyses of observational prospective studies have confirmed that a greater adherence to a Mediterranean‐style diet is associated with a significant improvement in health status and a significant reduction in overall mortality, as well as in morbidity and mortality from CVD and other major chronic diseases (Sofi 2008; Sofi 2010). Specifically, in the latest published meta‐analysis of prospective cohort studies, a 2‐point increase (scale from 0 to 7‐9 points) in adherence to a Mediterranean dietary pattern was associated with an 8% reduction in all‐cause mortality and a 10% reduction in CVD incidence or mortality (Sofi 2010).
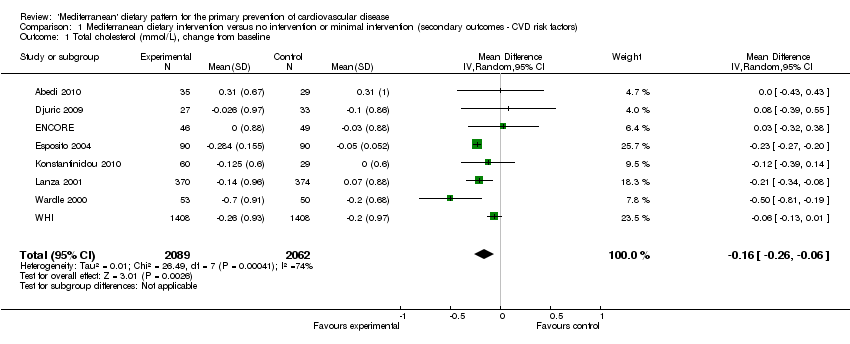
Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 1 Total cholesterol (mmol/L), change from baseline.

Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 2 Total cholesterol (mmol/L), change from baseline, subgroup analysis.

Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 3 LDL‐cholesterol (mmol/L), change from baseline.
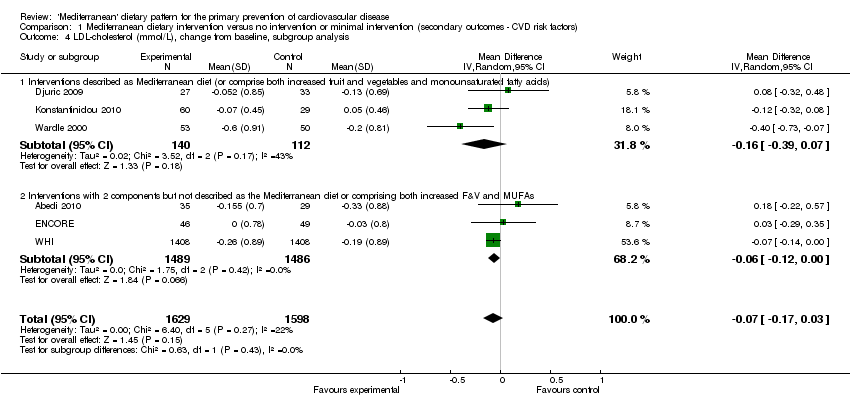
Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 4 LDL‐cholesterol (mmol/L), change from baseline, subgroup analysis.
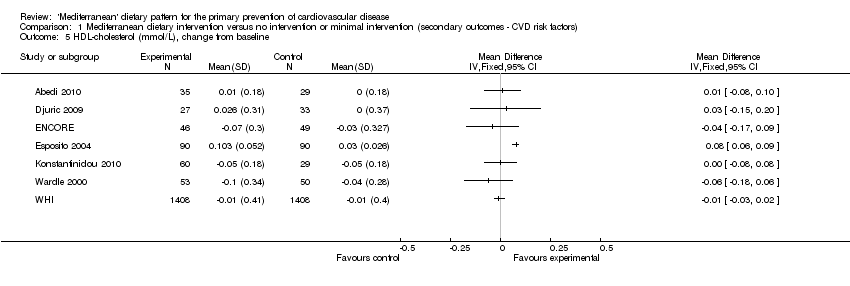
Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 5 HDL‐cholesterol (mmol/L), change from baseline.

Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 6 Triglycerides (mmol/L), change from baseline.
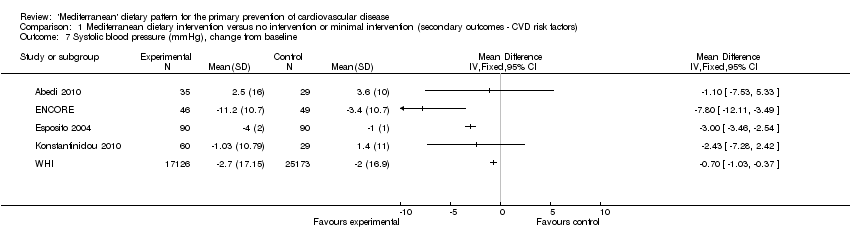
Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 7 Systolic blood pressure (mmHg), change from baseline.

Comparison 1 Mediterranean dietary intervention versus no intervention or minimal intervention (secondary outcomes ‐ CVD risk factors), Outcome 8 Diastolic blood pressure (mmHg), change from baseline.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total cholesterol (mmol/L), change from baseline Show forest plot | 8 | 4151 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.26, ‐0.06] |
| 2 Total cholesterol (mmol/L), change from baseline, subgroup analysis Show forest plot | 8 | 3815 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.23, ‐0.17] |
| 2.1 Interventions described as Mediterranean diet (or comprise both increased fruit and vegetables and monounsaturated fatty acids) | 4 | 436 | Mean Difference (IV, Fixed, 95% CI) | ‐0.23 [‐0.27, ‐0.20] |
| 2.2 Interventions with 2 components but not described as Mediterranean diet or comprising both increased fruit and vegetables and monounsaturated fatty acids | 4 | 3379 | Mean Difference (IV, Fixed, 95% CI) | ‐0.06 [‐0.13, 0.01] |
| 3 LDL‐cholesterol (mmol/L), change from baseline Show forest plot | 6 | 3227 | Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.13, ‐0.01] |
| 4 LDL‐cholesterol (mmol/L), change from baseline, subgroup analysis Show forest plot | 6 | 3227 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.17, 0.03] |
| 4.1 Interventions described as Mediterranean diet (or comprise both increased fruit and vegetables and monounsaturated fatty acids) | 3 | 252 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.39, 0.07] |
| 4.2 Interventions with 2 components but not described as the Mediterranean diet or comprising both increased F&V and MUFAs | 3 | 2975 | Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.12, 0.00] |
| 5 HDL‐cholesterol (mmol/L), change from baseline Show forest plot | 7 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Triglycerides (mmol/L), change from baseline Show forest plot | 6 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Systolic blood pressure (mmHg), change from baseline Show forest plot | 5 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8 Diastolic blood pressure (mmHg), change from baseline Show forest plot | 5 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |

