Interventions conservatrices pour le traitement des douleurs à l'aine d'origine musculo‐tendineuse, ligamentaire et osseuse liées à l'exercice
Résumé scientifique
Contexte
Les lésions de l'aine d'origine musculosquelettique, ligamentaire et osseuse sont fréquentes chez les athlètes et peuvent les obliger à arrêter le sport pendant plusieurs mois. Même lorsqu'ils sont capables de reprendre leurs activités sportives, il ne leur est pas toujours possible de retrouver leur niveau habituel. Le traitement des douleurs à l'aine liées à l'exercice est principalement conservateur (non chirurgical) et consiste notamment en des exercices, une électrothérapie, une thérapie manuelle ou des injections de stéroïdes.
Objectifs
Évaluer les effets (bénéfiques et délétères) des interventions conservatrices dans le traitement des douleurs à l'aine d'origine musculo‐tendineuse, ligamentaire et osseuse liées à l'exercice.
Stratégie de recherche documentaire
Nous avons consulté le registre spécialisé du groupe Cochrane sur les traumatismes ostéo‐articulaires et musculaires (décembre 2011) ; le registre Cochrane des essais contrôlés (CENTRAL) ( Bibliothèque Cochrane 2011, Numéro 4) ; MEDLINE (1948 à la 3ème semaine de novembre 2011) ; EMBASE (de 1980 à la semaine 49 de 2011) ; CINAHL (1982 à décembre 2011) ; LILACS (1982 à décembre 2011) ; PEDro (1929 à décembre 2011), SPORTDiscus (1985 à décembre 2011), OTseeker (jusqu'en décembre 2011), les références bibliographiques des articles et les actes de congrès (2000 à 2011).
Critères de sélection
Les essais contrôlés randomisés et quasi‐randomisés évaluant des interventions conservatrices dans le traitement des douleurs à l'aine d'origine musculo‐tendineuse, ligamentaire et osseuse liées à l'exercice ont été inclus. Les études comparant des traitements conservateurs à des traitements chirurgicaux ont été exclues.
Recueil et analyse des données
Deux auteurs de revue ont extrait les données et évalué le risque de biais de manière indépendante. Nous n'avons effectué aucun regroupement de données.
Résultats principaux
Deux études portant sur un total de 122 participants présentant des douleurs à l'aine liées aux adducteurs depuis au moins deux mois ont été incluses dans cette revue. Tous les participants sauf un étaient des athlètes de sexe masculin âgés de 18 à 50 ans. Les deux études présentaient un risque de biais élevé pour au moins l'une des catégories de biais. Le critère de jugement de la réussite du traitement rapporté dans les deux études reposait principalement sur les mesures de la douleur.
Une étude basée sur une analyse en intention de traiter rapportait une différence significative en faveur du traitement à base d'exercices (musculation axée sur les adducteurs et les abdominaux et entraînement à la coordination musculaire) par rapport à la physiothérapie standard (exercices d'étirement, électrothérapie et massage par friction transversale) en termes de réussite du traitement lors d'un suivi à 16 semaines (25/34 (74 %) contre 10/34 (29 %) ; risque relatif (RR) de 2,50, IC à 95 %, entre 1,43 et 4,37, P = 0,001). De même, les athlètes suivis ayant fait l'objet d'un traitement à base d'exercices étaient significativement plus nombreux à reprendre le sport à leur niveau habituel (23/29 (79 %) contre 4/30 (13 %) ; RR 5,95, IC à 95% entre 2,34 et 15,09, P = 0,0002). Quoique demeurant favorables au groupe de l'exercice, les différences entre les deux groupes en termes d'évaluation globale subjective des patients à 16 semaines et de réussite du traitement à 8‐12 ans n'étaient pas statistiquement significatives.
La seconde étude (54 participants) ne rapportait aucune différence significative lors d'un suivi à 16 semaines entre un traitement multimodal (chaleur, thérapie manuelle et étirements) et un traitement à base d'exercices (même intervention que dans la première étude) concernant les critères de jugement de la réussite du traitement (14/26 (54 %) contre 12/22 (55 %) ; RR de 0,99, IC à 95 %, entre 0,59 et 1,66, P = 0,96) et de reprise des activités sportives habituelles (13/26 (50 %) contre 12/22 (55 %) ; RR 0,92, IC à 95 % entre 0,53 et 1,58 P = 0,75). Ceux qui reprenaient le sport au niveau habituel le faisaient en moyenne 4,5 semaines plus tôt lorsqu'ils avaient reçu un traitement multimodal (différence moyenne de ‐4,50 semaines, IC à 95 %, entre ‐8,60 et ‐0,40, P = 0,03) par rapport au traitement à base d'exercices. Cette étude ne rapportait aucune complication ou effet secondaire dans aucun des groupes expérimentaux.
Conclusions des auteurs
Les preuves disponibles issues d'essais randomisés sont insuffisantes pour recommander une modalité de traitement conservateur spécifique dans les douleurs à l'aine liées à l'exercice. Bien que de mauvaise qualité, les meilleures preuves sont issues d'un essai rapportant que le traitement à base d'exercices (renforcement des muscles de la hanche et des abdominaux) chez les athlètes améliorait les résultats à court terme (principalement basés sur les mesures de la douleur) et la reprise des activités sportives par rapport à une physiothérapie consistant en des exercices passifs. Compte tenu de la faible qualité des preuves disponibles dans les deux essais inclus, d'autres essais randomisés sont nécessaires afin de confirmer ces résultats.
Résumé simplifié
Traitement conservateur de la douleur à l'aine liée à l'exercice
La douleur à l'aine liée à l'exercice est fréquente chez ceux qui pratiquent une activité sportive, en particulier dans les sports impliquant de courir, de frapper et de changer de direction, comme c'est le cas du football et du hockey. Les athlètes doivent parfois attendre plusieurs mois avant de reprendre le sport et sont parfois incapables de retrouver leur niveau d'activité habituel. Le médecin traitant doit souvent gérer plusieurs troubles coexistants, tels qu'un claquage musculaire, une tendinite, une lésion ligamentaire et une réaction de stress osseux. Les interventions conservatrices constituent généralement le premier choix de traitement et incluent une période de repos initial ; un renforcement des muscles qui stabilisent les articulations du pelvis et de la hanche ; un étirement des muscles de la hanche ; une électrothérapie (ex. : neurostimulation transcutanée (TENS), traitement au laser et ultrasonothérapie) ; une thérapie manuelle ; des anti‐inflammatoires non stéroïdiens ; des injections de stéroïdes ou une prolothérapie (injection de produits qui stimulent la production de facteurs de croissance pour induire la croissance et la réparation des tissus).
Deux essais contrôlés randomisés portant sur un total de 122 athlètes présentant des douleurs à l'aine liées à l'exercice ont été inclus dans cette revue. Les participants étaient âgés de 18 à 50 ans et étaient tous de sexe masculin, à l'exception d'une participante. Ils souffraient de douleurs à l'aine depuis au moins deux mois. Un essai rapportait des résultats positifs chez des athlètes ayant reçu un traitement à base d'exercices (renforcement des muscles des hanches et des abdominaux et entraînement à la coordination musculaire) par rapport à une physiothérapie standard consistant en des exercices passifs (étirements, électrothérapie et massage par friction transversale) 16 semaines après la fin du traitement en termes de réussite du traitement (principalement basée sur les mesures de la douleur) et de taux de reprise du sport au niveau habituel sans douleurs à l'aine. La seconde étude, qui comparait un traitement multimodal (chaleur, thérapie manuelle et étirements) à un traitement à base d'exercices, ne rapportait aucune différence significative entre les groupes en termes de réussite du traitement et de reprise du sport, mais observait une reprise plus rapide des activités sportives chez les athlètes qui avaient reçu un traitement multimodal.
Les preuves disponibles concernent uniquement des athlètes et sont limitées par le nombre réduit d'études et de participants pour chaque critère de jugement. D'autres essais contrôlés randomisés sont nécessaires afin de confirmer ces résultats.
Authors' conclusions
Background
Description of the condition
Musculotendinous, ligamentous and osseous (bony) groin pain is related to and aggravated by exercise and is characterized by overuse (Lynch 1999; Orchard 2000; Pizzari 2008). Given this link, we generally use the term 'exercise‐related groin pain' to describe this injury. Potential contributing factors towards the etiology of this injury are muscle imbalances between the abdominal wall musculature and the hip adductor muscles that, combined with excessive loads, result in an abnormal distribution of forces in this region (Pizzari 2008; Rabe 2010). Hip adduction involves moving the legs together. The converse movement is hip abduction, where the legs are moved apart. The primary adductor muscles of the hip are the pectineus, adductor longus, gracilis, adductor brevis and adductor magnus, while the primary hip abductor muscles include the gluteus medius, gluteus minimus and the tensor fasciae latae (Neumann 2010). It has been demonstrated that restricted hip range of motion (Verrall 2005a; Verrall 2007a), greater hip abductor to adductor muscle strength ratio, or adductor weakness (Engebretsen 2010; Maffey 2007) may be important risk factors for the development of groin pain.
Currently there is no recommendation in the literature regarding the definition of groin pain, which makes the diagnosis of this condition a challenge for clinicians (Hölmich 2007; Jansen 2008a). Usually the clinician deals with the coexistence of two or more disorders, such as adductor strains and pubic bone‐related dysfunction, which are the most frequent musculoskeletal causes of exercise‐related groin pain (Ekberg 1988; Hölmich 2007; Lloyd‐Smith 1985). Any type of hernia, sacroiliac dysfunction, piriformis syndrome, nerve entrapments, lumbar spine, gynaecological or urological diseases, and hip pathologies must first be excluded (Jansen 2008a; Machotka 2009). The most common symptoms are pain and tenderness on palpation of the pubis symphysis and tubercle, which may be referred to the surrounding area including the lower abdominal musculature and adductors, as well as pain provoked by resisted adduction (Hölmich 2004; Verrall 2005b). After clinical evaluation, magnetic resonance imaging (MRI) has been suggested as an important diagnostic tool to visualize any abnormalities of the involved structures (Jansen 2008a).
Musculotendinous, ligamentous and osseous groin pain is related to sports, especially those that involve running, kicking, changing directions, twisting and cutting, such as soccer and hockey (Ekstrand 1999; Emery 1999; Paajanen 2011a). Among male soccer players, the incidence of groin pain is between 8% to 12% per year (Ekstrand 1999; Hawkins 2001; Paajanen 2011a). A study conducted during the Australian Football League season indicated that this condition was responsible for players missing many games, at a cost of AUD 1.7 million in player unavailability during this period (Pizzari 2008).
The prognosis of exercise‐related groin pain is not straightforward and patients may wait more than six months to return to practicing sports without restrictions (Hölmich 1999; Weir 2010). It is not unusual for athletes to play with some symptoms even 24 weeks after the end of treatment, and the rate of failure to return to their prior level of sports function can reach more than 25% (Verrall 2007b; Weir 2011).
The treatment of exercise‐related groin pain is not well‐established in the literature (Jansen 2008b), but conservative modalities, such as physical therapy, are usually tried before surgery is considered. Conservative treatment appears to be a safe, low‐cost and accessible option for patients with exercise‐related groin pain.
Description of the intervention
Conservative treatment is generally based on an initial period of rest or modification of sports activities, pharmacotherapy and physical therapy, which may involve electrotherapy modalities, manual therapy (a clinical approach utilizing a hands‐on technique to treat soft tissues and joint structures (Carnes 2010), including but not limited to manipulation or mobilization), and mainly the strengthening of the abdominal and hip muscles to improve core stability (Verrall 2007b; Vitanzo 2001; Williams 2000). Although exercise therapy appears to be effective, a standardized protocol does not exist and the exercises are usually prescribed based on the therapist’s experience (Machotka 2009). When initial conservative treatment fails, steroid injections and dextrose prolotherapy (a technique which involves the injection of growth factor production stimulants to induce growth and repair of normal tissue (Topol 2005)) may be used (Jansen 2008b).
How the intervention might work
As exercise‐related groin pain is defined as being the result of overuse, a period of rest and reduction of activities that place high loads on the groin region are proposed in order to re‐establish the zone of homeostasis (Pizzari 2008). Improving the hip range of motion, specifically internal and external rotation, has been proposed as a possible method to reduce stress across the pubic symphysis and surrounding structures (Verrall 2005a; Verrall 2007a).
Muscular imbalances between abdominal and hip muscles may contribute towards overloading and loss of optimal functional stability of the groin region (Hölmich 1999). The adductors are essential stabilisers of the pelvis in activities such as running, pivoting and kicking, and these are almost always activated, together with the gluteus, hamstrings and abdominal muscles (Biedert 2003). Thus, it may be possible that improving control of and strengthening the abdominal (Cowan 2004) and hip stabilising muscles may improve the functional stability of the pelvis and therefore restore the functional unit of the groin region.
Why it is important to do this review
Musculoskeletal, ligamentous and osseous groin injuries are common in athletes (Ekstrand 1999; Hawkins 2001; Paajanen 2011a) and have a large economic impact since patients may need more than six months for full return to sports (Hölmich 1999; Weir 2010). There are no recommendations in the literature nor consensus about the effectiveness of the conservative therapeutic approaches (Jansen 2008b; Machotka 2009). This uncertainty motivated us to conduct this systematic review which, through the use of rigorous methods and a comprehensive and up‐to‐date search, may help to provide the information needed to support decision making.
Objectives
To assess the effects (benefits and harms) of conservative interventions for treating exercise‐related musculotendinous, ligamentous and osseous groin pain.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials (RCTs) and quasi‐randomized (method of allocating participants to a treatment which is not strictly random, for example by date of birth, hospital record number or alternation) controlled trials evaluating conservative interventions for treating exercise‐related musculotendinous, ligamentous and osseous groin pain were included.
Types of participants
People with a diagnosis of exercise‐related groin pain caused by pubic bone‐related dysfunction, enthesopathy or muscles strains, established by the primary studies, were included. Excluded were groin pain from any type of hernia, sacroiliac dysfunction, piriformis syndrome, nerve entrapments, lumbar spine, gynaecological or urological diseases, and hip pathologies.
Types of interventions
Included were all forms of conservative treatment for exercise‐related groin pain, such as strengthening of the muscles stabilising the pelvis and hip joints, stretching of the hip muscles, electrotherapy (for example, laser and ultrasound therapy), manual therapy, non‐steroidal anti‐inflammatory drugs (NSAIDs), steroidal injections or prolotherapy. The interventions could be single interventions or complex interventions, such as programmes incorporating different types of exercises or combinations of different interventions. Studies comparing conservative with surgical treatments were excluded.
Our main comparisons were:
-
conservative intervention (single or complex intervention) versus placebo intervention;
-
one conservative intervention (single or complex intervention) versus another conservative intervention (single or complex intervention).
All of the interventions could be set in the context of other interventions being provided to all trial participants.
Types of outcome measures
Primary outcomes
-
Pain relief at rest, on palpation and during physical activity (visual analogue scale, numeric rating scale, and others)
-
Function (Short Form‐36 (SF‐36) physical component, and others)
-
Successful treatment
Secondary outcomes
-
Patient subjective global assessment (for example, classified as much better, better, not better, worse and much worse)
-
Return to sports or normal activities
-
Adverse events (e.g. burns from cryotherapy, reports of severe discomfort from or intolerance of interventions)
If possible, the outcomes were evaluated in the short term (four to six weeks after the end of treatment, for example); mid‐term (12 to 16 weeks after the end of treatment, for example), and long term (one year after the end of treatment, for example).
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (December 2011); the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2011, Issue 4); MEDLINE (1948 to November week 3 2011); EMBASE (1980 to Week 49 2011); CINAHL (1982 to December 2011); Latin American and Caribbean Health Sciences (LILACS) (1982 to December 2011); PEDro, the Physiotherapy Evidence Database (1929 to December 2011); SPORTDiscus (1985 to December 2011); and OTseeker, the Occupational Therapy Systematic Evaluation of Evidence Database (to December 2011). No language restrictions were applied.
The subject‐specific strategy was combined with the sensitivity‐maximizing version of the Cochrane highly sensitive search strategy (Lefebvre 2011) to identify randomized trials in MEDLINE. Complete search strategies are shown for CENTRAL, MEDLINE, EMBASE and LILACS in Appendix 1.
We searched Current Controlled Trials for ongoing studies.
Searching other resources
We contacted professional experts in this field and searched reference lists of papers and conference proceedings (2000 to 2011), such as of the American College of Sports Medicine Annual Meetings; American Physical Therapy Association; American Academy of Physical Medicine and Rehabilitation Annual Assembly; Canadian Physiotherapy Association Annual Congresses; Australian Physiotherapy Association Conferences.
Data collection and analysis
The intended methodology for data collection and analysis was described in our published protocol (Almeida 2012), which was based on the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Selection of studies
Two review authors (MOA and BNGS) independently selected and assessed potentially eligible articles for inclusion in the review. Any disagreements were discussed and resolved by consensus. Where necessary, a third author (MSP) acted as adjudicator. There was no blinding of authors, institution or journal of publication at any stage.
Data extraction and management
Two review authors (MOA and RBA) independently extracted data from selected articles using a standard extraction form. Data extracted included study methods, the characteristics of participants, interventions, outcome measures and results. When necessary, requests were sent to trial authors for additional information or data.
Data entry into RevMan was by three review authors (MOA, BNGS, RBA).
Assessment of risk of bias in included studies
As recommended by The Cochrane Collaboration (Higgins 2011), two review authors (MOA and RBA) independently assessed the risk of bias for each included study. Disagreements were resolved by a third review author (MSP). The following domains were evaluated for risk of bias: random sequence generation; allocation concealment; blinding of participants and personnel; blinding of outcome assessment; incomplete outcome data; selective outcome reporting; and other sources of bias. Risk of bias for the individual domains was assessed as either 'low risk of bias', 'high risk of bias' or 'unclear risk of bias'.
Measures of treatment effect
Dichotomous outcome data were expressed as risk ratios (RR), with 95% confidence intervals. For continuous outcomes, mean differences (MD) were used if the studies use the same instrument of evaluation. However, if the primary trials assessed the same variables using different scales, we planned to use the standardized mean difference (SMD). The estimated effects were reported together with the 95% confidence intervals (95% CI).
Unit of analysis issues
The unit of analysis was based on the individual patient. Due to the biological and epidemiological characteristics of exercise‐related groin pain, cluster randomized controlled trials and cross‐over randomized controlled trials were not expected.
Dealing with missing data
For missing data (for example, publication bias, outcome not measured, incomplete reporting, lack of intention‐to‐treat analysis, attrition from the study) we planned to adopt the following strategies.
-
Whenever possible, we would contact the original investigators to request missing data.
-
Make explicit the assumptions of any methods used to cope with missing data, for example, that the data were assumed to be missing at random, or that missing values were assumed to have a particular value such as a poor outcome.
-
Perform sensitivity analyses to determine how sensitive the results were to reasonable changes in the assumptions that were made.
-
Address the potential impact of missing data on the findings of the review in the Discussion section.
Assessment of heterogeneity
We planned to assess heterogeneity by visual inspection of the forest plot (analysis) along with consideration of the Chi² test for heterogeneity (with a level of significance of P < 0.1) and the I² statistic. We considered that there was probably substantial heterogeneity where I² > 50%.
Assessment of reporting biases
We planned to assess the likelihood of publication bias using funnel plots, if there were at least 10 trials contributing to a primary outcome.
Data synthesis
In the absence of significant clinical and statistical heterogeneity, we planned to use a fixed‐effect model and 95% confidence intervals for pooling the results of trials testing comparable interventions. However, if we had found diversity in clinical or methodological characteristics, or unexplained heterogeneity, we would have considered using a random‐effects model for analysis. Where possible, we planned to perform intention‐to‐treat analysis.
Subgroup analysis and investigation of heterogeneity
If data had been available, we planned to investigate heterogeneous results for specific patient groups, performing subgroup analyses according to gender, duration of symptoms, and activity (recreational versus professional athletes). We planned to investigate whether the results of subgroups were significantly different by inspecting the overlap of confidence intervals and performing the test for subgroup differences that is available in RevMan.
Sensitivity analysis
Where possible, we planned sensitivity analyses examining various aspects of study and review methodology, such as the inclusion or not of studies at high risk of bias (specifically from lack of allocation concealment, assessor blinding, and incomplete outcome data) and inclusion or not of trials only reported in abstracts. We also planned to conduct sensitivity analyses to look at the effects of missing data.
Results
Description of studies
Results of the search
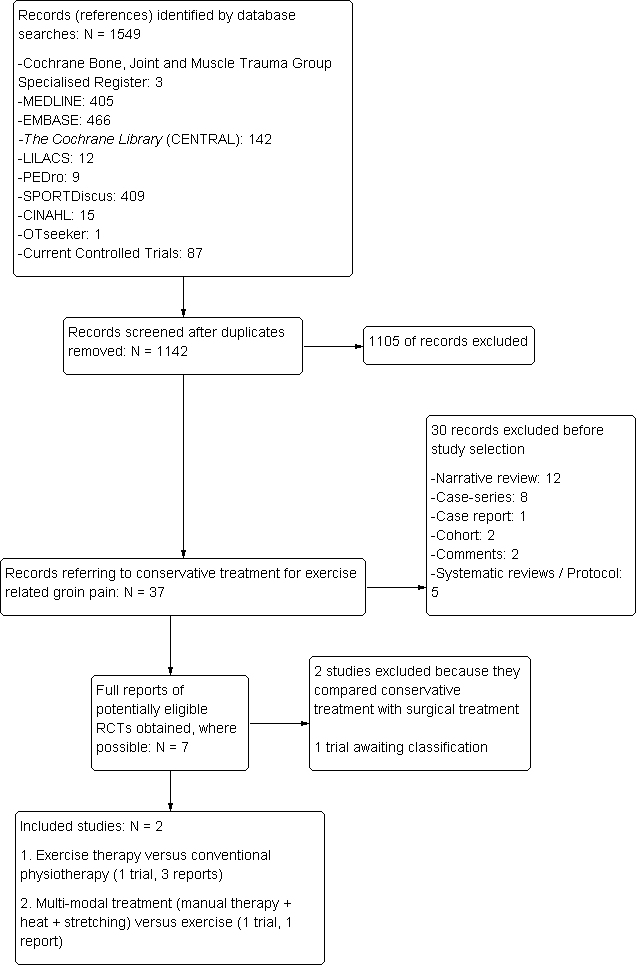
For our search, completed in December 2011, we screened a total of 1549 records from the following databases: Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (3 records); CENTRAL (142), MEDLINE (405), EMBASE (466), CINAHL (15), LILACS (12), PEDro (9), SPORTDiscus (409), OTseeker (1), and Current Controlled Trial (87). After discarding duplicates and obviously ineligible references, 37 references remained. Of these, 30 were excluded because they were clearly not reports of randomized controlled trials. The study flow diagram is presented in Figure 1.
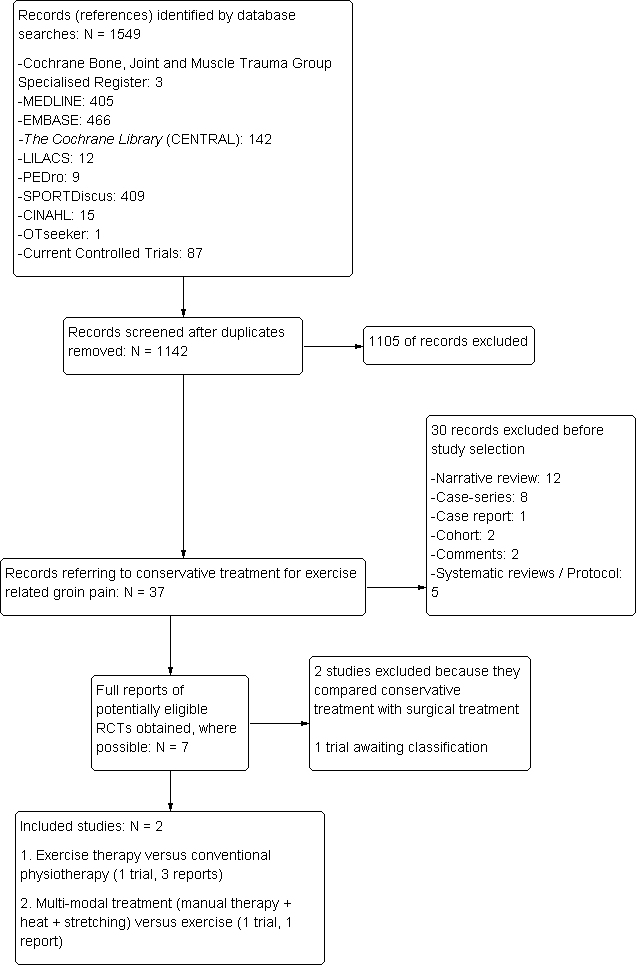
Flow diagram showing the reference screening and study selection.
Where possible, full reports were obtained for the seven potentially eligible studies. Upon study selection, two were included (Hölmich 1999; Weir 2011), two were excluded (Ekstrand 2001; Paajanen 2011), and one is awaiting classification (Backx 2009). The other two articles were additional reports of Hölmich 1999; one was a conference abstract and the other (Hölmich 2011) was a longer‐term follow‐up (eight to 12 years after the original study).
Thus, overall there were two included trials, two excluded studies and one study awaiting classification.
Included studies
Both studies included in the review (Hölmich 1999; Weir 2011) were randomized clinical trials reported in English language journals. They recruited a total of 122 athletes, all with adductor‐related groin pain of at least two months duration.
Hölmich 1999 recruited 68 male athletes aged between 18 and 50 years. The study was carried out in Copenhagen (Denmark). Hölmich 1999 compared exercise therapy (strengthening with emphasis on the adductor and abdominal muscles, and training muscular co‐ordination) with conventional physiotherapy consisting of passive modalities (transverse friction massage, laser therapy, transcutaneous electrical nerve stimulation (TENS), and stretching of adductor, hamstring and hip muscles). The outcomes assessed were 'successful treatment' (based on pain measures), patients' subjective global assessment, and return to sports at the same level without groin pain. Hölmich 1999 reported on the outcomes at four months and, in another report (Hölmich 2011), at eight to 12 years.
Weir 2011 recruited 53 male athletes and one female athlete aged between 18 and 50 years. The study was carried out in Leidschendam (Netherlands). The study compared multi‐modal treatment (consisting of heat followed by manual therapy and stretching of adductor muscles) with exercise therapy (this was the same programme as in Hölmich 1999: strengthening with emphasis on the adductor and abdominal muscles, and training muscular co‐ordination). The outcomes assessed were 'successful treatment', maximum pain during sports, return to sports at the same level without groin pain, time to return to sports, and adverse effects. Weir 2011 reported on the outcomes at 16 weeks.
For further details about the included studies, see the Characteristics of included studies.
Excluded studies
Two studies (Ekstrand 2001; Paajanen 2011) were excluded because they compared conservative treatment with surgical treatment (see the Characteristics of excluded studies).
Studies awaiting classification
Backx 2009 aimed to randomize 80 male athletes with groin pain for at least six weeks to receive either pelvic‐stabilising muscle training or usual care. The outcomes measures listed in the trial registration document are pain, general disability, global change, sport participation, time to return to full athletic activity and recurrences of the same complaints. Participants were evaluated after the period of treatment and 26 and 52 weeks after the start of treatment. Although the trial is indicated as completed in the trial registration document, contact with the trial investigator by email revealed this was not the case and that, in consequence, the trial results have not been published (Backx 2013).
For more details, see the Characteristics of studies awaiting classification.
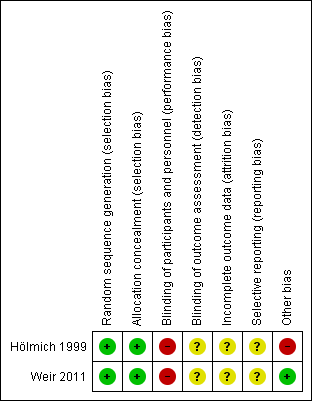
Risk of bias in included studies
Details of the risk of bias assessment for each trial are shown in the Characteristics of included studies, and the judgements are shown visually in Figure 2.
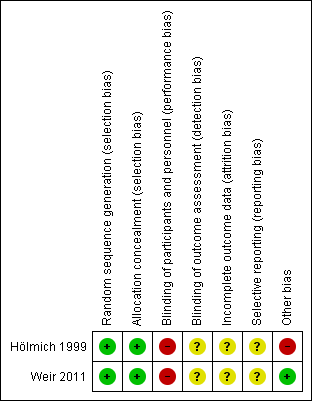
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Randomization
Hölmich 1999 and Weir 2011 clearly reported that the process of randomization involved sequentially numbered opaque envelopes, and were classified as 'low risk of bias'.
Allocation concealment
As both Hölmich 1999 and Weir 2011 used envelopes independently administered by a secretary, they were judged at low risk of selection bias relating to allocation concealment.
Implementation
Hölmich 1999 reported a statistically significant (P = 0.008) and clinically important difference in the baseline proportions of participants with bilateral groin pain in the two groups (5/34 (15%) versus 15/34 (44%)). Hölmich 1999, however, reported that the findings for the 'successful treatment' outcome remained statistically significant for the exercise group when this was adjusted for using either univariate or multiple logistic‐regression analysis. In Weir 2011, the allocation was implemented successfully because no significant difference was found in the baseline characteristics of the treatment groups. Our judgements for selection bias thus remained unaltered.
Blinding
Performance bias
Both studies (Hölmich 1999; Weir 2011) were considered to have high risk of bias because blinding of participants and therapists was not possible due to the nature of the interventions. Therefore, this bias was unavoidable.
Detection bias
In Hölmich 1999 and Weir 2011, the examining physicians were unaware of the treatment allocation, but there were subjective outcomes (that is, successful treatment, patients' subjective global assessment) that meant that the participants, who were not blinded, were the key outcome assessors. Hence both studies were considered as at 'unclear risk of bias'.
Incomplete outcome data
Hölmich 1999 was classified as at 'unclear risk of bias' since the analyses were not entirely intention‐to‐treat analyses; the assumptions for the missing participants in the intention‐to‐treat analysis for the outcome 'successful treatment' were not described. A per protocol analysis was performed for the other outcomes (patients' subjective global assessment and return to sports at the same level without groin pain). The percentage of participants lost at 16 weeks follow‐up was 13% (9/68), and 31% (21/68) at eight to 12 years. Patient flow within the study was clear, missing data were balanced across groups, and reasons for missing data were provided. However, the characteristics of lost participants were not described.
Weir 2011 was also classified as 'unclear risk of bias' because it used a per protocol analysis. Despite the percentage of participants lost to follow‐up being quite small (6/54 (11%)), and missing data being well reported and balanced across groups (three participants in each group), the characteristics of lost participants were not reported.
Selective reporting
Despite the absence of suspected selective outcome reporting, Hölmich 1999 and Weir 2011 were classified as 'unclear risk of bias' because neither study evaluated function, a clinically relevant primary outcome. Furthermore, data from the short‐term follow‐up were not reported in the publications of both included studies. On contact, authors of both studies reported that these data were not available (Hölmich 2012; Weir 2012). These issues can be considered a potential source of reporting bias.
Other potential sources of bias
In Hölmich 1999, there was no explicit information from participants about supplementary treatment and physical activity during the follow‐up period (eight to 12 years) and the study was therefore considered as 'high risk of bias' for this follow‐up outcome. Weir 2011 appeared to be free of other sources of bias and was classified as 'low risk of bias'.
Effects of interventions
Given that the two included studies evaluated different comparisons, these are presented separately below.
Both studies reported on 'successful treatment'. This outcome was assessed based on the following measures: no pain at palpation of the adductors tendon or during resisted adduction; no pain in connection with or after athletic activity in the same sport and at the same level of competition; and return to sports at the same level without groin pain. If all three measures were reached, the result was labelled excellent; if two measures were reached, the result was good; if one measure was reached, the result was fair; and if no measures were reached, the result was poor. Successful treatment was considered for results labelled as excellent and good in the included studies. Given this outcome was based primarily on pain measures, we included this under our intended primary outcome of pain relief at rest, on palpation and during physical activity (visual analogue scale, numeric rating scale, and others).
Exercise therapy versus conventional physiotherapy
Primary outcomes
Pain relief at rest, on palpation and during physical activity
Hölmich 1999 reported 'successful treatment' at follow‐up at 16 weeks using an intention‐to‐treat analysis, which showed significantly better results in the exercise group (25/34 (74%) versus 10/34 (29%); risk ratio (RR) 2.50, 95% CI 1.43 to 4.37, P = 0.001) (seeAnalysis 1.1). This difference was not maintained at eight to 12 years follow‐up (21/24 versus 18/23; RR 1.12, 95% CI 0.86 to 1.45, P = 0.41). As Hölmich 1999 used a per protocol analysis in this follow‐up, we carried out a sensitivity analysis to test the differences using an intention‐to‐treat analysis, where a poor outcome was assumed for the missing participants of both groups. This, likewise, showed no statistically significant difference between the two groups (RR 1.17, 95% CI 0.77 to 1.76, P = 0.46).
Function
Hölmich 1999 did not report this outcome.
Secondary outcomes
Patients' subjective global assessment
In Hölmich 1999, the participants were asked about their groin problems compared with their situation before the treatment. At the 16‐week follow‐up, all participants of the exercise therapy group reported that they were 'much better' or 'better', whereas only 27 out of 30 reported this in the physiotherapy group. The difference between the two groups for this outcome was not statistically significant either using a per protocol analysis (29/29 (100%) versus 27/30 (90%); RR 1.11, 95% CI 0.97 to 1.97, P = 0.13) (seeAnalysis 1.2) or a sensitivity analysis where it was assumed that all missing participants had a poor outcome (RR 1.07, 95% CI 0.86 to 1.34, P = 0.53).
Though the results still tended to favour the exercise group, a similar lack of statistically significant differences between the two groups was found at long‐term follow‐up, either using a per protocol analysis (20/24 versus 16/23; RR 1.20, 95% CI 0.87 to 1.66, P = 0.27) (seeAnalysis 1.2) or a sensitivity analysis (intention‐to‐treat analysis) where missing participants were assumed to have a poor outcome (RR 1.25, 95% CI 0.79 to 1.97, P = 0.34).
Return to sports in the same level without pain
In Hölmich 1999, the proportion of athletes who returned to sports at the same level without pain after 16 weeks was significantly higher in the exercise therapy group (23/29 (79%) versus 4/30 (13%); RR 5.95, 95% CI 2.34 to 15.09, P = 0.0002) (seeAnalysis 1.3). In the sensitivity analysis (intention‐to‐treat analysis where missing participants were assumed not to have returned to sports), the difference between groups remained statistically significantly in favour of the exercise therapy group (RR 5.75, 95% CI 2.23 to 14.86, P = 0.0003).
Adverse events
Hölmich 1999 did not report this outcome.
Uptake of treatment
Hölmich 1999 reported that the median number of treatments in terms of physiotherapy attendance was 15 in the exercise group and 14 in the physiotherapy group.
Multi‐modal therapy versus exercise therapy
Primary outcomes
Pain relief at rest, on palpation and during physical activity
Weir 2011 found no significant difference between the two groups in the achievement of 'successful treatment', see above definition (14/26 (54%) versus 12/22 (55%); RR 0.99, 95% CI 0.59 to 1.66, P = 0.96) (seeAnalysis 2.1). The same finding applied for a sensitivity (intention‐to‐treat) analysis where the three lost to follow‐up in each group were assumed to have had unsuccessful treatment (RR 1.01, 95% CI 0.6 to 1.71, P = 0.96).
Weir 2011 also reported the maximum pain during sports (visual analogue score, 0 to 100: worst pain) in the 25 participants who had returned to full sports participation. While favouring exercise therapy, the difference between the two groups for this subgroup was not statistically significant (MD 15.10, 95% CI ‐7.29 to 37.49, P = 0.19) (seeAnalysis 2.2).
Function
Weir 2011 did not report this outcome.
Secondary outcomes
Patients' subjective global assessment
Weir 2011 did not report this outcome.
Return to sports in the same level without pain
Weir 2011 found no statistically significant difference between the two groups in the numbers who returned to full sports participation (13/26 (50%) versus 12/22 (55%); RR 0.92, 95% CI 0.53 to 1.58, P = 0.75) (Analysis 2.3). The same finding applied for a sensitivity analysis where the three in each group lost to follow‐up were assumed not to have returned to full sports participation (RR 0.93, 95% CI 0.53 to 1.66, P = 0.82). However, the trial participants in the multi‐modal group who returned to full sports participation took significantly less time to do so than those in the exercise group (12.6 weeks versus 17.3 weeks; MD ‐4.5 weeks, 95% CI ‐8.60 to ‐0.40, P = 0.03) (seeAnalysis 2.4).
Adverse events
Weir 2011 reported that there were no complications or side effects found in either intervention group.
Uptake of treatment
Weir 2011 noted that in the multi‐model group, 11 athletes received one treatment and 15 received two treatments. In the exercise group, the mean number of sessions performed was 75% of the programme. They reported that there was no correlation between the dose of treatment and outcome in either group.
Discussion
Summary of main results
The available evidence is limited to two small trials, each of which compared a different comparison. Together the two studies involved 122 participants who had experienced adductor‐related groin pain for at least two months. All participants were young male athletes, except for one female athlete.
Evidence from Hölmich 1999 (68 participants) showed that exercise therapy produced significantly better results at 16 weeks follow‐up than conventional physiotherapy consisting of passive modalities (stretching exercise, electrotherapy and transverse friction massage) for the outcomes of 'successful treatment' (based primarily on pain measures) and return to sports at the same level without groin pain. Although still favouring the exercise group, the differences between the two groups in patient's subjective global assessment and 'successful treatment' at eight to 12 years follow‐up were not statistically significant.
The second study (54 participants) found no significant differences at 16 weeks follow‐up between a multi‐modal treatment and exercise therapy for the outcomes of 'successful treatment' and return to full sports participation. For those returning to full sports participation, Weir 2011 found no significant difference in the maximum pain experienced at 16‐week follow‐up. However, athletes receiving multi‐modal treatment returned on average 4.5 weeks earlier than those treated by exercise therapy. Weir 2011 reported that there were no complications or side effects found in either intervention group.
Overall completeness and applicability of evidence
When interpreting the findings of this review one should be aware of the characteristics of the participants, the types of interventions and the outcomes assessed. The participants were predominantly young male athletes; only one was female. Therefore the evidence found cannot be generalized for both genders because of their anatomical and physiological differences. The high prevalence of male participants was expected because groin pain is more common in sports practiced more by males than females, such as soccer and hockey (Ekstrand 1999; Emery 1999; Paajanen 2011a). The evidence is strengthened by the consistency between the two trials in the population, the exercise intervention and outcome assessment. However, 'successful treatment' as defined in these two trials is a crude and non‐validated measure for assessing outcome.
In clinical practice, physical therapists commonly treat patients with groin pain with the interventions used in the included studies. The studies did not use a single intervention but rather one therapeutic modality in combination with others. This approach is widely used for treating chronic musculoskeletal conditions. It is important to note that, despite the limited evidence, the exercise therapy based on strengthening and co‐ordination exercises appears to be more effective than a more passive treatment (stretching, electrotherapy and transverse friction massage) (Hölmich 1999). Strengthening abdominal and hip muscles seems reasonable because muscular imbalance may contribute to functional instability of the pelvis and the groin region (Cowan 2004).
Quality of the evidence
Neither study was assessed as 'low risk of bias' in all domains. It is encouraging to note that both included studies (Hölmich 1999; Weir 2011) reported quite clearly the process of sequence generation and allocation concealment, and were thus classified as at low risk of selection bias. For the domains of detection bias, attrition bias and reporting bias, there was insufficient information to judge the included studies, and so they were considered at 'unclear risk of bias'. Both studies were assessed as at high risk of performance bias because the nature of the interventions made blinding of participants and personnel impossible. Although this source of bias is unavoidable, it still should be recognized and reported. We judged the long‐term follow‐up outcomes for Hölmich 1999 at high risk of other bias because of the lack of information about the trial participants’ supplementary treatments and physical activity during this follow‐up period.
Both studies were small and the available evidence cannot be considered conclusive. While the results for Hölmich 1999 are strongly in favour of exercise compared with conventional physiotherapy for 'successful treatment', with a 79% return to sports at 16 weeks, Weir 2011 found only 55% in their exercise group had returned to full sports by 16 weeks. The imbalance between groups in the baseline incidence of bilateral groin pain in Hölmich 1999 favoured the exercise group and, as shown in Hölmich 1999, is likely to have exaggerated the effect size. Weir 2011 reported a sample size calculation for the outcome 'time to return to sports without groin pain', requiring 21 athletes in each group. While Weir 2011 found a statistically significant earlier return in the multi‐modal therapy group (MD ‐4.5 weeks, 95% CI ‐8.60 to ‐0.40), this promising result only applies to the subgroup of 25 participants who had returned to sports.
Potential biases in the review process
This systematic review used an adequate search strategy with high sensitivity to avoid missing any randomized controlled trials on conservative treatments for patients with exercise‐related groin pain. There were also no language restrictions in our searches. It is still possible, however, that we have missed unpublished studies or those published in journals that are not listed in the various databases.
The change in the primary outcomes measures between the protocol and the review should be reported as a limitation of the review and a potential selective reporting bias. Unfortunately, there is no consensus on which outcomes should be evaluated for exercise‐related groin pain. When planning the primary outcomes in the protocol, we intended to approach the ideal and more common method of evaluating participants, but both included studies (Hölmich 1999; Weir 2011) used different criteria. In the protocol of this review we defined pain as one of the primary outcomes, but both included studies assessed pain associated with another outcome (return to sports), resulting in the outcome 'successful treatment'. Accordingly, we decided to include 'successful treatment' (despite not being listed in the protocol) as a primary outcome in the review because pain was the main basis for categorising the patient outcome.
Another potential source of bias in the review was our approach to dealing with missing dichotomous data. Both included studies used a per protocol analysis to report some outcome measures, so we decided to do a sensitivity analysis through an intention‐to‐treat analysis by imputing the worst‐case outcomes for the missing participants. Although this approach might not reflect reality, we opted for the worst‐case scenario because the treatment is more likely to be successful if it works even when assuming the worst‐case scenario for those who dropped out of the study regardless of the reason.
Agreements and disagreements with other studies or reviews
We located two other reviews (Jansen 2008b; Machotka 2009) that focused on the treatment of patients with exercise‐related groin pain. Both pre‐date the publication of Weir 2011.
Jansen 2008b investigated the evidence on all interventions (conservative or surgical) in the treatment of patients with longstanding groin pain. As well as covering a more extensive scope of interventions and patients, Jansen 2008b included non‐randomized studies. Its conclusion that exercise therapy should be the first choice of conservative treatment was based primarily on the results of the only identified randomized controlled trial (Hölmich 1999).
Machotka 2009 focused on the evidence for exercise therapy and, similar to Jansen 2008b, included evidence from other study designs, such as case reports and case series. Machotka 2009 concluded that an exercise intervention focused on strengthening of hip and abdominal muscles can lead to favourable results for the return to sports; this again was based on the limited evidence from Hölmich 1999.
Flow diagram showing the reference screening and study selection.
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Exercise therapy versus conventional physiotherapy, Outcome 1 'Successful treatment'.

Comparison 1 Exercise therapy versus conventional physiotherapy, Outcome 2 Patients' subjective global assessment (better or much better).
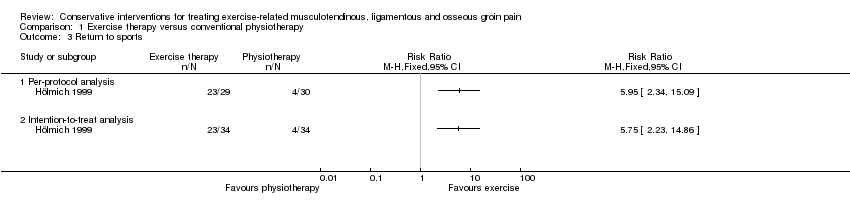
Comparison 1 Exercise therapy versus conventional physiotherapy, Outcome 3 Return to sports.

Comparison 2 Multi‐modal treatment versus exercise therapy, Outcome 1 'Successful treatment'.

Comparison 2 Multi‐modal treatment versus exercise therapy, Outcome 2 Maximum pain during sports.

Comparison 2 Multi‐modal treatment versus exercise therapy, Outcome 3 Return to sports.
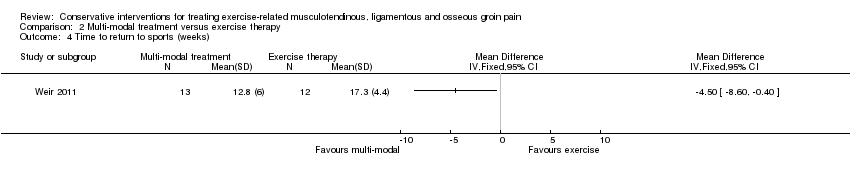
Comparison 2 Multi‐modal treatment versus exercise therapy, Outcome 4 Time to return to sports (weeks).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 'Successful treatment' Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Follow‐up 16 weeks, per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Follow‐up 8 to 12 years, per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Follow‐up 8 to 12 years, intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Patients' subjective global assessment (better or much better) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Follow‐up 16 weeks, per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Follow‐up 16 weeks, intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Follow‐up 8 to 12 years, per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Follow‐up 8 to 12 years, intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Return to sports Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 'Successful treatment' Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Maximum pain during sports Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Return to sports Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Per protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Time to return to sports (weeks) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |

