Effectiveness of the Valsalva Manoeuvre for reversion of supraventricular tachycardia
Abstract
Background
People with the cardiac arrhythmia supraventricular tachycardia (SVT) frequently present to clinicians in the prehospital and emergency medicine settings. Restoring sinus rhythm by terminating the SVT involves increasing the refractoriness of atrioventricular nodal tissue within the myocardium by means of vagal manoeuvres, pharmacological agents, or electrical cardioversion. A commonly used first‐line technique to restore the normal sinus rhythm (reversion) is the Valsalva Manoeuvre (VM). This is a non‐invasive means of increasing myocardial refractoriness by increasing intrathoracic pressure for a brief period, thus stimulating baroreceptor activity in the aortic arch and carotid bodies, resulting in increased parasympathetic (vagus nerve) tone.
Objectives
To assess the evidence of effectiveness of the VM in terminating SVT.
Search methods
We updated the electronic searches of the Cochrane Central Register of Controlled Trials (CENTRAL; 2014, Issue 7); MEDLINE Ovid (1946 to August week 3, 2014); EMBASE Classic and EMBASE Ovid (1947 to 27 August 2014); Web of Science (1970 to 27 August 2014); and BIOSIS Previews (1969 to 22 August 2014). We also checked trials registries, the Index to Theses, and the bibliographies of all relevant publications identified by these strategies.
Selection criteria
We included all randomised controlled trials (RCTs) that examined the effectiveness of VM in terminating SVT.
Data collection and analysis
Two review authors independently extracted the data using a standardised form. We assessed each trial for internal validity, resolving any differences by discussion. We then extracted and entered data into Review Manager 5.
Main results
In this update, we did not identify any new RCT studies for inclusion. We identified two RCT studies as ongoing that we are likely to include in future updates. Accordingly, our results are unchanged and include three RCTs with a total of 316 participants. All three studies compared the effectiveness of VM in reverting SVT with that of other vagal manoeuvres in a cross‐over design. Two studies induced SVT within a controlled laboratory environment. Participants had ceased all medications prior to engaging in these studies. The third study reported on people presenting to a hospital emergency department with an episode of SVT. These participants were not controlled for medications or other factors prior to intervention.
The two laboratory studies demonstrated reversion rates of 45.9% and 54.3%, whilst the clinical study demonstrated reversion success of 19.4%. This discrepancy may be due to methodological differences between studies, the effect of induced SVT versus spontaneous episodic SVT, and participant factors such as medications and comorbidities. We were unable to assess any of these factors, or adverse effects, further, since they were either not described in enough detail or not reported at all.
Statistical pooling was not possible due to heterogeneity between the included studies.
Authors' conclusions
We did not find sufficient evidence to support or refute the effectiveness of VM for termination of SVT. Further research is needed, and this research should include a standardised approach to performance technique and methodology.
PICO
Plain language summary
The effectiveness of the Valsalva Manoeuvre for stopping an abnormal heart rhythm
Supraventricular tachycardia (SVT) is a common heart abnormality that presents as a fast heart rate. This heart rhythm disturbance can occur in healthy individuals and may include such symptoms as chest pain, palpitations, shortness of breath, sweating, and feeling faint. In rarer instances, unconsciousness may occur. The treatment of SVT is usually a combination of physical straining manoeuvres (also known as vagal manoeuvres), medications, or electrical therapy (used in severe cases where blood pressure drops to a low level). A vagal manoeuvre is a term used to describe any physical intervention that results in stimulation of the 10th cranial nerve (vagus nerve), which in turn can lead to slowing of the heart rate in the setting of SVT. One such manoeuvre, the Valsalva Manoeuvre (VM), is performed by having a patient blow into a syringe whilst lying down (face up) for 15 seconds. This generates increased pressure within the chest cavity and triggers a slowing of heart rate that may stop the abnormal rhythm. This review examined the available evidence to see how effective the VM is in restoring normal heart rate (known as reversion success). This is an updated version of the original review published in 2013.
Three studies involving a total of 316 participants were included in this review. Analysis of the results showed that reversion success lies somewhere between 19.4% and 54.3%. We could not calculate the likelihood and severity of side effects (adverse events) as the studies provided insufficient information to perform this analysis. Potential side effects have been reported in other articles on the subject; these have included hypotension (sudden lowering of blood pressure) or syncope (brief loss of consciousness). No side effects were reported in the three studies reviewed here. In the three studies, reversion was achieved on completion of each VM.
Overall, the VM appears to be a simple, non‐invasive method of stopping abnormal heart rhythm, but its safety and overall effectiveness are difficult to quantify. Further research is required to improve the evidence surrounding this practice.
Authors' conclusions
Summary of findings
| Valsalva Manoeuvre for induced supraventricular tachycardia | ||||
| Patient or population: People with induced SVT Settings: Clinical laboratory Intervention: VM Comparison: Nil | ||||
| Outcomes | Study | VM Performance (posture, strain duration, pressure) | Reversion n (%) | Quality of the evidence |
| Reversion | Mehta 1988 | Supine, 15 and 30 seconds*, 35 mmHg | 19/35 (54.3) | ⊕⊕⊝⊝ |
| Wen 1998 | Supine, 30 seconds, 35 mmHg | 61/133 (45.9) | ⊕⊕⊝⊝ | |
| GRADE Working Group grades of evidence *Although applying both 15‐ and 30‐second strain durations, the Mehta study found no statistical significance of bradycardia effect (increased vagal tone) on participants when assessed in sinus rhythm. | ||||
| Abbreviations: SVT: supraventricular tachycardia VM: Valsalva Manoeuvre | ||||
| Valsalva Manoeuvre for clinical supraventricular tachycardia (patients presenting with arrhythmia) | ||||
| Patient or population: Patients presenting to emergency department with SVT Settings: Emergency department (hospital) Intervention: VM Comparison: Nil | ||||
| Outcomes | Study | VM Performance | Reversion n (%) | Quality of the evidence |
| Reversion | Lim 1998 | Sitting*, 30 seconds, 40 mmHg | 12/62 (19.4) | ⊕⊕⊝⊝ |
| GRADE Working Group grades of evidence *Although a deviation from accepted standard of performance technique, this posture is acceptable as a known method of performance in the clinical setting. Also, this posture has been demonstrated to precipitate adverse effects. The absence of reported adverse effects (such as hypotension or syncope) is not clear within the study. | ||||
| Abbreviations: SVT: supraventricular tachycardia VM: Valsalva Manoeuvre | ||||
Background
Description of the condition
Supraventricular tachycardia (SVT) is a generic term applied in reference to any tachycardia originating above the ventricles and which involves atrial tissue or atrioventricular (AV) nodal tissue (Medi 2009). It encompasses such arrhythmias as atrioventricular nodal reentrant tachycardia (AVNRT), atrioventricular reentrant tachycardia (Wolff‐Parkinson‐White syndrome) (AVRT), atrial flutter, atrial fibrillation, and the sinus tachycardias. More specificity can be applied when SVT is used to describe those tachycardias that involve a nodal dependent re‐entrant circuit, such as that found in AVNRT or AVRT (Medi 2009). The incidence of SVT in the United States is approximately 35 cases per 100,000 population annually, with a prevalence of approximately 2.25 cases per 1000 population (Medi 2009). We identified no data to indicate incidence and prevalence in other regions.
These arrhythmias result from the establishment of a re‐entry circuit within (or inclusive of) the atrioventricular node. They are usually episodic in nature and may result in the patient exhibiting signs and symptoms ranging from tachycardia or palpitations, shortness of breath, chest pain, anxiety, nausea, and dizziness to presyncope/syncope as a consequence of reduced cardiac output (McGuire 2007; Scheinman 2005; Wellens 2003). It is these symptoms that usually precipitate an ambulance request or attendance at hospital. The establishment of AVNRT is believed to occur as a result of a premature atrial complex delivered across the AV node during the relative refractory period. As a consequence of the identification of dual nodal tract pathways for conduction of atrial impulses (fast depolarisation with slow repolarisation and slow depolarisation with fast repolarisation) (Akhtar 1993; Delacretaz 2006; McGuire 2007; Scheinman 2005; Wellens 2003), it is believed that this atrial ectopic complex stimulates a re‐entry circuit.
The mechanism of AVRT differs in the existence of accessory pathways (bundles of Kent). These conductive accessory pathways pass through the atrioventricular septum and thus provide for a larger re‐entry circuit, albeit one that passes through the AV node and is similarly affected by increased vagal tone (McGuire 2007; Scheinman 2005; Wellens 2003).
A range of therapies (vagal manoeuvres, pharmacological therapy, or synchronised direct current countershock therapy) are employed within emergency medicine and prehospital emergency care practice, in order to extend the refractoriness of AV nodal tissue, which will result in reversion of the arrhythmia. The use of pharmacologic agents such as adenosine and calcium channel blockers (verapamil and diltiazem) is well known and has been the subject of systematic review and meta‐analysis to determine their levels of effectiveness in this setting (Delaney 2011; Holdgate 2009). Synchronised direct current countershock therapy is generally reserved for those patients who are rapidly decompensating as a consequence of the arrhythmia, and although the evidence is somewhat limited within the literature, there is support for this practice within medical circles globally. Vagal manoeuvres have also been employed for some time, with demonstrated effectiveness in reverting AVNRT and AVRT of between 12% and 54% (with a median of 25%) across the range of studies conducted (Lim 1998; Mehta 1988; Taylor 1999; Wen 1998).
The arrhythmia is usually transient and may be precipitated by such factors as cardiac disease, stimulant use, electrolyte imbalance, and stress. In certain circumstances the frequency of episodes or consequences of episodic poor perfusion associated with SVT may require more significant therapies such as beta blockers or radio frequency ablation in order to improve patient quality of life. Recent studies have also identified increased troponin I enzyme levels (0.02 ng/dL to 1.05 ng/dL, mean 0.20 ng/dL) in people suffering episodic SVT in the absence of infarction, and although no studies have quantified the potential for patient harm at this time, it is suggested that these elevated troponin I levels may be linked with myocardial damage (Carlberg 2011; Redfearn 2005; Zellweger 2003). These studies also suggest that enzyme levels rise with increasing age of the patient, although the consequences are again at this time unquantified (Carlberg 2011; Redfearn 2005; Zellweger 2003).
Description of the intervention
The Valsalva Manoeuvre was first published by Antonio Maria Valsalva in 1704 in his seminal work De Aura Humana Tractatus, as a means of expelling pus from the middle ear of a patient (Jellinek 2006; Junqueira 2007; Waxman 1980; Yale 2005). It continues to retain relevance in modern medicine across a range of medical and scientific disciplines. Although it is unclear exactly when the manoeuvre was first applied to terminating haemodynamically stable SVT (in the form of AVNRT or AVRT), it is likely to have coincided with the advent of the electrocardiogram (Einthoven 1906). The VM constitutes three specific elements in order to provide a maximum effect, as follows (Taylor 2004).
-
posture of the patient (supine)
-
pressure generation within the intrathoracic cavity (40 mmHg)
-
duration of strain (15 seconds)
These elements provide a set of values which, when adhered to, should maximise parasympathetic (vagal) response and cause reversion of the arrhythmia (in the absence of any compliance or other patient issues that may affect performance or the nature of effect).
The VM is defined by four phases of activity, first described by Hamilton et al in 1936, as follows (Junqueira 2007).
-
Phase 1 can be defined by a transient increase in pressure within the thoracic aorta, coupled with a compensatory decrease in heart rate triggered by the baroreceptors within the aortic arch. This pressure increase results from the compressive effect of the generated intrathoracic pressure on the thoracic aorta.
-
Phase 2 is defined by the end of this transient period, resulting in decreasing aortic pressure and increasing heart rate.
-
Phase 3 occurs at the end of the strain phase of the VM (and includes a resulting decrease in intrathoracic pressure exerted on the aorta), leading to a brief pressure drop within the aorta and a compensatory rise in heart rate.
-
Phase 4 occurs as a result of increased venous return and a subsequent increase in preload, resulting in increased aortic pressure as cardiac output is elevated, and a compensatory decrease in heart rate.
We have selected the VM for review as it provides a simple, quantifiable (method), and non‐invasive means of inducing increased vagal tone. Other manoeuvres such as carotid sinus massage and dive reflex therapy have limitations within the prehospital setting regarding patient safety, standardisation and reproducibility, and the logistics of application (for example the acquisition and use of ice).
How the intervention might work
The VM is a simple, quantifiable, and non‐invasive method of increasing vagal tone, thereby increasing the refractory period of myocardial cells in order to terminate the established nodal re‐entry circuit. The manoeuvre was traditionally performed by expiring against a closed glottis to increase intrathoracic pressure, thereby triggering baroreceptor activity and increased vagal tone. However, this also has potentially deleterious side effects such as increased intraocular pressure and profound hypotension as a consequence of unfettered vagal stimulation (Junqueira 2007; Looga 2004; Taylor 2004; Vaisrub 1974). Since Rushmer introduced the measurement of intraoral pressure in 1947 (Junqueira 2007), the manoeuvre is now more commonly described and instructed as an exhalation against a defined pressure (measurable) in order to avoid significant side effects and to improve performance and patient safety. Maximum vagal response occurs on release of the sustained intrathoracic pressure, which occurs in phase 4 of the VM, and it is at this point that reversion of the arrhythmia is most likely to occur (Looga 2004; Waxman 1980). Recently, efforts have been made to provide a standard of instruction of the VM for use in the haemodynamically stable patient suffering AVNRT, including the use of a 10 ml syringe to generate the 40 mmHg pressure required (Smith 2009a; Taylor 2004).
Why it is important to do this review
There is currently a plethora of definitions of Valsalva performance, and it is used across a variety of medical and scientific disciplines to promote different effects (cardiac or non‐cardiac) (Smith 2009b). The effectiveness of the VM is challenged by the lack of available interventional and observational non‐randomised clinical studies (7.3% to 54% of study sample) (Taylor 1999; Taylor 2004; Waxman 1980) and the many definitions of method (specifically variations in the three elements of posture, pressure, and duration) (Smith 2009b). We hoped with this review to ascertain the nature of evidence available to demonstrate VM effectiveness, and the need for further study to define the effectiveness of the VM for the development of future therapy regimens in the treatment of SVT.
Objectives
To assess the evidence of effectiveness of the VM in terminating SVT.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) of VM effectiveness in terminating SVT.
Types of participants
Participants whose normal cardiac rhythm is sinus rhythm and who have no known cardiac disease, with acute onset or induced episodes of haemodynamically stable AVNRT or AVRT.
Types of interventions
The definition of a VM for the purpose of this review is a physical manoeuvre that has three elements (posture, strain duration, and pressure) and when performed results in an increase in intrathoracic pressure and increased refractoriness of AV nodal tissue. Although we preferred the model of practice described in the Description of the intervention section, currently a range of values are used in the literature to describe the VM. As such, we accepted the following values for this review:
-
posture (supine, or supine with legs elevated);
-
strain duration (15 to 30 seconds);
-
pressure (30 mmHg to 50 mmHg).
Comparison: We included only those study results identifying the effectiveness of the VM for SVT reversion in this review. We excluded reported comparisons of effectiveness of VM with other vagal manoeuvres (such as carotid sinus massage or dive reflex) within included studies in accordance with the aims of the review.
Types of outcome measures
Studies were eligible for inclusion if they reported any of the following outcome measures:
Primary outcomes
Reversion of SVT to a sinus rhythm.
Secondary outcomes
-
Failure to revert SVT to a sinus rhythm, followed by:
-
repeated attempts at VM or other vagal manoeuvres;
-
pharmacological intervention; or
-
direct current countershock therapies.
-
-
Cardiovascular effects of VM performance (e.g. hypotension, bradycardia).
-
Frequency and severity of adverse events resulting from application of the VM.
-
Mortality resulting from the VM.
Search methods for identification of studies
Electronic searches
We ran the initial searches in February 2012. We re‐ran them on 28 August 2014 to identify new evidence. We searched the following sources:
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2014, Issue 7)
-
MEDLINE OVID (1946 to August week 3, 2014)
-
EMBASE & EMBASE Classic OVID (1947 to 27 August 2014)
-
Conference Proceedings Citations Index (Web of Science) (1970 to 27 August 2014)
-
Conference abstracts (BIOSIS Previews) (1969 to 22 August 2014)
We also searched for adverse events using:
-
MEDLINE OVID (1946 to August week 3, 2014)
We presented the search strategies in Appendix 1 and Appendix 2. We applied no language restrictions to the searches. We combined the MEDLINE and EMBASE strategies with the Cochrane sensitivity‐maximising RCT filter (Lefebvre 2011).
Searching other resources
-
World Health Organization International Clinical Trials Registry Platform (ICTRP): apps.who.int/trialsearch/default.aspx (Search terms used: Valsalva, Manoeuvre. Accessed 28 August 2014.)
-
Clinical Trials Registry: www.anzctr.org.au/TrialSearch.aspx (Search terms used: Valsalva, Manoeuvre. Accessed 28 August 2014.)
We also handsearched the following literature:
-
Index to Theses
-
International Standard Randomised Controlled Trial Number (ISRCTN) registry
-
The bibliographies of all relevant publications identified by the electronic and handsearches
Data collection and analysis
Selection of studies
Two review authors (GS and MF) independently screened the search results (titles and abstracts). In Figure 1 we presented the results from the search strategy as a flow chart based on the PRISMA statement (Lefebvre 2011). We retained all potentially relevant studies and examined the full texts of these studies to determine which of them satisfied the inclusion criteria. We used a two‐stage process to select studies for inclusion: (i) independent selection (without blinding) by two review authors (GS and MF) to short list potential studies, and (ii) a final group selection involving discussion between two review authors (GS and MF) to define which studies met the inclusion criteria. Arbitration by a third review author to resolve any disagreements was not required.
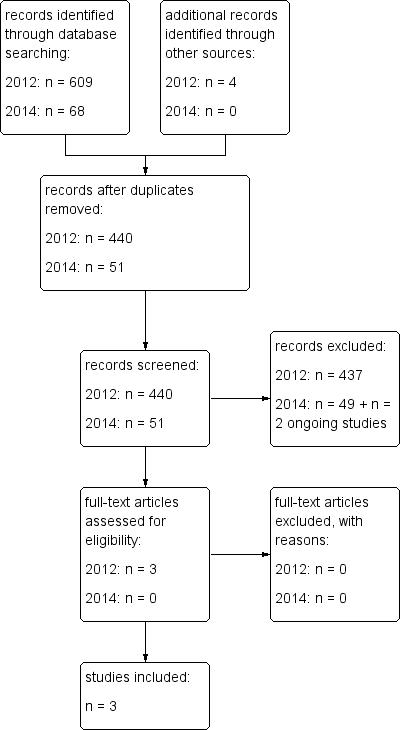
Study flow diagram.
Data extraction and management
The same review authors carried out data extraction independently using predefined data extraction forms. We identified no RCT studies requiring translation to English. We found no important data missing that would have required contacting the original study authors for clarification. Two review authors (GS and MF) performed data extraction independently without blinding and using a paper data collection form to record and tabulate search results. The results were compared, discussed and collated prior to being transcribed to an electronic spreadsheet for tabulation. There were no disagreements regarding applicability for inclusion or exclusion.
Assessment of risk of bias in included studies
We used the 'Risk of bias' assessment guidelines in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) to address the following sources of potential bias:
-
selection bias;
-
performance bias;
-
attrition bias; and
-
detection bias.
We addressed each of these using a three‐point grading (high, unclear, or low) to measure the following:
-
allocation concealment (did the method enable concealment to the point of assignment);
-
blinding of outcome assessment (were the investigators were aware of the treatment allocation);
-
adequacy of controls (did the study provide for equal numbers of treatment and control participants);
-
adequacy of follow‐up (did the method account for all participants including withdrawal, dropout, or protocol deviation);
-
intention‐to‐treat analysis (did the study provide for post‐treatment bias control through an intention‐to‐treat analysis, follow‐up of withdrawals and completeness, and analysis of results by original treatment and treatment given).
A third review author (AM) arbitrated any disagreements regarding 'Risk of bias' assessment.
Measures of treatment effect
We assigned unit measures using common terms to all papers as follows:
-
reversion rate;
-
time to reversion (number of VM attempts);
-
relapse rate;
-
minor adverse events;
-
major adverse events.
Unit of analysis issues
The unit of analysis was the individual participant. Consultation with an appropriately qualified statistician was not required as no unit of analysis issues arose.
Dealing with missing data
Contact with the study authors was not required as no data were missing.
Assessment of heterogeneity
The presence of high levels of clinical and methodological heterogeneity resulted in studies being presented using descriptive statistics only.
Assessment of reporting biases
We assessed measurement of reporting bias by the following:
-
clear definition of inclusion/exclusion criteria;
-
clear definition of outcome measure(s);
-
reported accuracy, precision, and observer variation of outcome measures;
-
appropriately timed outcome measures.
Data synthesis
We were unable to synthesise data statistically, and results were demonstrated using descriptive statistics only.
Subgroup analysis and investigation of heterogeneity
Subgroup analysis was not undertaken due to insufficient specific data within the available studies.
Sensitivity analysis
As we undertook no meta‐analysis due to high levels of clinical and methodological heterogeneity, no sensitivity analysis was possible. We used descriptive statistics to present results.
Results
Description of studies
See: Characteristics of included studies.
Results of the search
The literature search identified 663 potentially relevant studies. After filtering for duplication, we excluded 221 studies. We examined each of the remaining 442 studies (title and abstract) and excluded those that were either not an RCT or that did not demonstrate effectiveness of VM in reverting SVT. We retrieved three studies for more detailed evaluation; we subsequently included these in the review. We identified two RCT studies as ongoing; we will likely include these in future revisions (Para‐SVT 2014 1; REVERT 2014 1).
In Figure 1 we described the literature search results graphically. Two studies included a cross‐over design where an alternative intervention was used irrespective of primary intervention success (Mehta 1988; Wen 1998). The Lim 1998 study was also a cross‐over design, where subsequent intervention was dependent upon failed primary intervention in reversion of SVT. This offered challenges in providing analysis appropriate for the question of VM effectiveness in terminating SVT, as each RCT used varied methodology (multiple attempts of a variety of vagal manoeuvre interventions and performance techniques). As a result, heterogeneity of methods precluded meta‐analysis. It was not possible to provide descriptions of reported adverse effects of VM used in the management of SVT as the search did not identify any. In Figure 2 we described the results of the adverse effects search graphically.
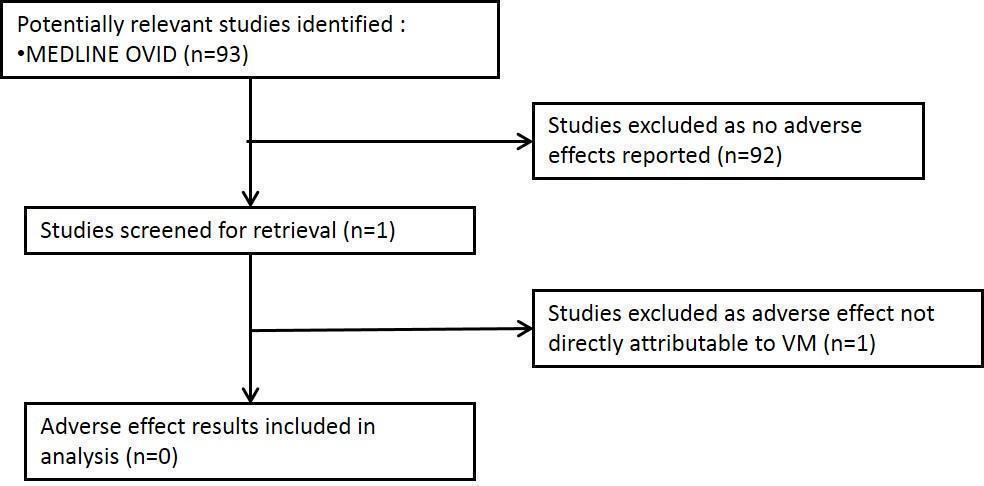
Adverse events search results.
Included studies
The three selected RCTs were conducted in three different countries (Singapore, England, and Taiwan) and comprised 316 participants. All three studies reported a primary outcome measure of reversion (or effectiveness) of VM used in terminating SVT. Each study included application of the VM between one and three times to achieve effect. All studies included a cross‐over design, and the nature of this design enabled descriptive analysis of two of these (Mehta 1988; Wen 1998). The Lim 1998 study reported patients in the clinical setting presenting with SVT to an emergency department, whereas the Mehta 1988 and Wen 1998 studies described induced SVT in participants with significant control of other variables (such as cessation of medication for adequate half‐life time prior to participation in the study). It is possible that an induced SVT (by programmed electrical stimulation) in a healthy adult may be more susceptible to reversion by vagal manoeuvres than a patient presenting to hospital who is experiencing an episode of SVT (of varied duration). The use of induced SVT may not represent clinical presentations of SVT, as an arrhythmia generated by a period of external electrical stimulation is likely to self resolve more rapidly than one that is triggered or maintained by a stimulus from within the myocardium, although this is not clearly evidenced within the available literature. As a consequence, the reversion rate demonstrated by the Lim 1998 study is more likely to represent clinical effectiveness. It is also likely that individuals who have a history of SVT are more likely to be familiar with the VM and its correct application, suggesting they would be more likely to be adept at applying the VM than healthy participants within the two laboratory studies, which may affect the results of these studies. It was not possible to gauge the potential effect of this factor within this review. Also, given the cross‐over design of each study, this review data represented primary intervention (VM) reversion within the available RCT data, and is not affected by other vagal manoeuvres. We decided that both the Mehta 1988 and Wen 1998 studies provided an appropriate inclusion defined by the review question, whilst the Lim 1998 study added value as a clinical application of VM in people presenting with SVT to an emergency department, and so is presented separately.
Excluded studies
We excluded no identified RCTs.
Risk of bias in included studies
We presented the details of quality assessment based upon the Cochrane Handbook for Systematic Reviews of Interventions method (Higgins 2011) in the Characteristics of included studies table. In addition, we have provided a brief analysis of the risk of bias of included studies below. No studies demonstrated adequate allocation concealment. Blinding was not possible due to the nature of the intervention.
Allocation
There is a high risk of selection bias within the Mehta 1988 and Wen 1998 studies, which did not report allocation concealment. The Lim 1998 study contained an unclear risk of selection bias, as the use of cards in an envelope (to be selected by a staff nurse) with the intervention written on each appears inadequate to demonstrate appropriate random allocation of participants to intervention.
Blinding
There was no evidence of blinding in any of the three studies included in this review. It is worth noting that the nature of the intervention (performance of a vagal manoeuvre) prevents blinding of investigators or participants to either intervention or effect. Thus, performance bias was not practical within the three studies, and detection bias was not reported in any of the three studies.
Incomplete outcome data
There was a low risk of attrition bias within the three included studies, as results in each study included outcome reporting for all participants.
Selective reporting
There was a low risk of reporting bias within the three included studies, as all outcomes for each intervention were reported in all cases.
Other potential sources of bias
None noted.
Effects of interventions
See: Summary of findings for the main comparison Summary of findings ‐ induced SVT; Summary of findings 2 Summary of findings ‐ clinical SVT
Each of the three identified RCT studies used a cross‐over design to compare effectiveness of the VM against other vagal manoeuvres (the dive reflex and carotid sinus massage). As this review was to specifically address the effectiveness of VM for SVT reversion, we have not assessed or analysed its comparative effect against other vagal manoeuvres here. Also, heterogeneity of method between studies would make such a comparison difficult. All three RCTs provided adequate data on the primary outcome of the review (termination of SVT), and, as a consequence, we did not contact the study investigators for further information. The data in the included RCT studies did not provide us the opportunity to report on reversion success, adverse effects, and mortality outcomes. The absence of reported data prevented us from assessing other listed outcomes. Those outcomes we were able to assess are reported as follows.
Reversion rate
The Mehta 1988 and Wen 1998 studies provided reversion success rates of 54.3% (19 out of 35) and 45.9% (61 out of 133), respectively, whilst the Lim 1998 study reported reversion success of 19.4% (12 out of 62). As a result of heterogeneity between included studies, statistical pooling was not possible.
Adverse effects
We were unable to calculate the nature of significant cardiovascular effects such as hypotension and bradycardia resulting from VM application to SVT, as these were not reported. Within the Lim 1998 study, a single participant was reported to be diagnosed with myocardial infarction, but it is unclear if this was a result of the SVT or if it precipitated the arrhythmia.
Mortality
None of the studies reported deaths. As a consequence, the mortality rate for VM use in SVT within this review was zero.
Discussion
Summary of main results
This updated systematic review identified no new RCT studies for inclusion. However, we did identify two ongoing studies that we will likely include in future reviews. Consequently, the updated results offered no new findings at this time.
The Mehta 1988 and Wen 1998 studies provided reversion success rates of 54.3% (19 out of 35) and 45.9% (61 out of 133), respectively, whilst the Lim 1998 study reported reversion success of 19.4% (12 out of 62). There were important methodological differences and significant heterogeneity between the studies that prevented meta‐analysis. Also, as sufficient validity could not be ascribed to the primary studies, only descriptive statistics for VM reversion of SVT were reported.
The three included studies did not report side effects, cardiovascular effects, and mortality associated with VM use for SVT, precluding reporting or analysis.
Overall completeness and applicability of evidence
The data on the primary outcome were available for analysis. The identified studies specifically assessed the effectiveness of the VM in reverting SVT and so were applicable. It was noted that two of the studies (Mehta 1988; Wen 1998) provided assessment in the setting of induced SVT, whereas the third study assessed the effectiveness of VM in patients presenting to an emergency department with an episode of SVT. This third study offered more relevant data for the clinical setting. Although the identified studies are somewhat dated, it is unlikely that we have failed to detect a relevant study given the comprehensive search strategy.
Quality of the evidence
The quality of evidence was generally poor, as a consequence of sample size and number of available RCTs. Also, the nature of variability in performance of (and indeed what quantified) a VM for this application ensured that it was not possible to make a definitive analysis of effectiveness of the VM for termination of SVT. Whilst all three studies provided a primary outcome (reversion), there was little or no information regarding other outcomes (mortality, adverse effects, and cardiovascular effects). Precision of the results was low, with confidence intervals specific to reversion not reported in two studies. Generalisability was challenged by the setting of the Mehta 1988 and Wen 1998 studies, and the Lim 1998 study provided the only example of clinical applicability.
At this time there is no universally accepted, standardised VM, although the method described in the Description of the intervention section is often used in the clinical setting. Future studies should consider using this method to improve homogeneity between studies and the generalisation of results.
Potential biases in the review process
None identified.
Agreements and disagreements with other studies or reviews
There was insufficient evidence available to determine if these review findings represent concurrence, as there are no other systematic reviews of this intervention.
Study flow diagram.

Adverse events search results.
| Valsalva Manoeuvre for induced supraventricular tachycardia | ||||
| Patient or population: People with induced SVT Settings: Clinical laboratory Intervention: VM Comparison: Nil | ||||
| Outcomes | Study | VM Performance (posture, strain duration, pressure) | Reversion n (%) | Quality of the evidence |
| Reversion | Mehta 1988 | Supine, 15 and 30 seconds*, 35 mmHg | 19/35 (54.3) | ⊕⊕⊝⊝ |
| Wen 1998 | Supine, 30 seconds, 35 mmHg | 61/133 (45.9) | ⊕⊕⊝⊝ | |
| GRADE Working Group grades of evidence *Although applying both 15‐ and 30‐second strain durations, the Mehta study found no statistical significance of bradycardia effect (increased vagal tone) on participants when assessed in sinus rhythm. | ||||
| Abbreviations: SVT: supraventricular tachycardia VM: Valsalva Manoeuvre | ||||
| Valsalva Manoeuvre for clinical supraventricular tachycardia (patients presenting with arrhythmia) | ||||
| Patient or population: Patients presenting to emergency department with SVT Settings: Emergency department (hospital) Intervention: VM Comparison: Nil | ||||
| Outcomes | Study | VM Performance | Reversion n (%) | Quality of the evidence |
| Reversion | Lim 1998 | Sitting*, 30 seconds, 40 mmHg | 12/62 (19.4) | ⊕⊕⊝⊝ |
| GRADE Working Group grades of evidence *Although a deviation from accepted standard of performance technique, this posture is acceptable as a known method of performance in the clinical setting. Also, this posture has been demonstrated to precipitate adverse effects. The absence of reported adverse effects (such as hypotension or syncope) is not clear within the study. | ||||
| Abbreviations: SVT: supraventricular tachycardia VM: Valsalva Manoeuvre | ||||

