Histeroscopia para el tratamiento de la subfertilidad asociada con presuntas anomalías graves de la cavidad uterina
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Parallel‐group, randomised, controlled, single‐centre trial Power calculation not reported Approved by the hospital's ethics committee No source of funding or conflict of interest reported | |
| Participants | Country: Italy Setting: AGUNCO Obstetrics and Gynecology Centre, Rome Population: women referred to the centre from January 1998 to April 2005 for fertility problems were examined for inclusion. All women underwent routine examinations including the study of ovarian function (FSH, luteinising hormone, oestradiol and progesterone concentrations); prolactin, free triiodothyronine, free thyroxine and thyroid‐stimulating hormone concentrations; postcoital test; TVUS; HSG and analysis of the partner's semen. The TVUS was performed to diagnose the presence of uterine fibroids. After these examinations, all women found to be affected by uterine fibroids excluding all other causes of infertility were asked to participate in the study. Type of subfertility: infertility for ≥ 1 year (range: 1 to 5 years); no further clarification on primary versus secondary subfertility Mean age: women with submucous fibroids alone: 31.4 ± 2.5 years; women with mixed submucous‐intramural fibroids: 32.2 ± 2.5 years Number recruited: 193 women Number participants: 181 women Number participants with submucous fibroids only: 52 women Number participants with mixed submucous‐intramural fibroids: 42 women Inclusion criteria: aged ≤ 35 years; infertility for ≥ 1 year; presence of 1 knot or fibroid of diameter ≤ 40 mm (or both) and absence of other causes of infertility at the performed examinations Exclusion criteria: presence of ≥ 2 knots or fibroids of diameter > 40 mm (or both); body weight > 20% of normal weight; and use of medication containing oestrogens, progestins or androgens within 8 weeks prior to study Duration of study: 86 months; conducted January 1998 to April 2005 | |
| Interventions |
Participants were examined by TVUS 3 months after surgery. Participants who underwent surgery were suggested to abstain from having sexual intercourse for 3 months and then to start having regular fertility‐oriented intercourse. Participants who did not undergo surgery were asked to immediately start having regular fertility‐oriented intercourse (intercourse during the 6‐day fertile interval ending on the day of ovulation). Participants were monitored for up to 12 months after study commencement. | |
| Outcomes | Clinical pregnancy defined by the visualisation of an embryo with cardiac activity at 6–7 weeks of pregnancy Miscarriage classified as clinical loss of an intrauterine pregnancy between the 7th and 12th weeks of gestation | |
| Notes | Authors stated that the differences in pregnancy rates between the comparison groups were statistically significant for the women with submucous fibroids (P < 0.05), which is in contrast with the calculation of the results in Review Manager 5. The definition of knot was unclear: it could not be clarified since we were unable to contact the study authors. Unclear whether a hysteroscopy was done in all women to confirm the exact position of the ultrasonically detected fibroids. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Subsequently, women of each group were randomized into two subgroups, according to a randomisation table." Comment: low risk of selection bias related to random sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Method not stated: no further clarification obtained from the study authors. Comment: unclear risk of selection bias related to allocation concealment. |
| Blinding of participants and personnel (performance bias) | Low risk | Method not stated: no further clarification obtained from the study authors. Comment: not applicable as this is a surgical study with unequivocal outcomes. |
| Blinding of outcome assessment (detection bias) | Low risk | Method not stated: no further clarification obtained from the study authors. Comment: not applicable as this is a surgical study with unequivocal outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "One hundred and ninety‐three patients were diagnosed as affected by uterine fibroid excluding all other causes of infertility and met the requirements of the inclusion and exclusion criteria. Of these, 181 decided to participate in the study. Among the 181 patients, 52 had submucosal fibroids (SM group) while 45 had intramural fibroids (IM group), 11 had subserosal fibroids (SS group), 42 had a mix of submucosal–intramural (SM‐IM group) and 31 patients had a mix of intramural–subserosal fibroids (IM‐SS group)." Quote: "Out of 181 women, 68 become pregnant." Comment: low risk for attrition bias. |
| Selective reporting (reporting bias) | High risk | All specified outcomes reported in the results section. Nevertheless, the published report failed to include results for the live birth rate, which was the primary outcome of interest that would be expected to have been reported for a trial on fertility treatment conducted over a 7‐year period. |
| Other bias | Unclear risk | The mean ages and duration of infertility in the intervention and control group of women with submucous fibroids were not reported. No further clarification by the authors was obtained. It was unclear whether there might have been imbalance in the baseline characteristics between the comparison groups. Failure to do a hysteroscopy in all women to confirm the position of the ultrasonically detected fibroids could have caused information bias. |
| Methods | Parallel‐group, randomised, controlled, single‐centre trial Power analysis performed. To detect an expected difference in pregnancy rate between the intervention and control group of 15% at a level of 0.05 with a power of 80%, a sample size of 200 women (i.e. 100 women per group) was required. From 2800 women attending the centre, 452 women fulfilling the inclusion criteria were selected; 215 women were randomised (107 women in the intervention group and 108 women in the control group). Data on outcomes of 204 women were available for analysis (101 in the intervention group and 103 in the control group). This study had therefore adequate statistical power to detect a difference between the comparison groups if really present. Approved by the hospital's ethics committee. No source of funding or conflict of interest reported. | |
| Participants | Country: Spain Setting: infertility unit of an university tertiary hospital in the Spanish capital Madrid Population: women with unexplained, male or female factor infertility for ≥ 24 months bound to undergo IUI with a sonographic diagnosis of endometrial polyps Unexplained infertility was diagnosed in women with normal ovulatory cycles, semen analysis, HSG and postcoital testing. Male factor infertility was diagnosed if 2 semen analyses obtained ≥ 1 month apart were subnormal according to the WHO criteria. Female factor infertility was diagnosed in women with ovulatory dysfunction, cervical factor or endometriosis. Type of subfertility: primary subfertility (correspondence with study authors) Mean age: treatment group: 30.8 years (range 26.7 to 34.9); control group: 30.9 years (range 26.5 to 35.3) Number recruited: 452 women Number randomised: 215 women Inclusion criteria: women with ≥ 24 months of subfertility with a sonographic diagnosis of endometrial polyps bound to undergo IUI for unexplained, male or female factor infertility Exclusion criteria: women aged > 39 years, anovulation, azoospermia, uncorrected tubal disease or previous unsuccessful use of recombinant FSH Duration of the study: 50 months; conducted January 2000 to February 2004 | |
| Interventions | 1 surgeon (the first author of the study) performed all hysteroscopic procedures by intention in an outpatient clinic setting under local anaesthesia
Duration: women were scheduled to receive 4 cycles of IUI with subcutaneous injection of recombinant FSH 50 IU daily from the 3rd day, and the first IUI was planned for 3 cycles after hysteroscopy in both groups. 4 IUI cycles were attempted before finishing the trial. | |
| Outcomes | Primary: quote: "We studied the crude pregnancy rate in both groups" Comment: clinical pregnancy; crude pregnancy was defined by the study authors as follows: "the presence of a gestational sac on ultrasound" (correspondence with the study authors) | |
| Notes | All study data were obtained in personal communication from the study authors. 1. Quote: "Patients underwent a complete infertility evaluation that included TVUS in the early proliferative phase, basal body temperature recording to assess ovulation, postcoital test (PCT), HSG, semen analysis and, in some patients, diagnostic laparoscopy." Comment: according to correspondence with the first author, the aim of the laparoscopy was exclusively diagnostic in the evaluation of cases of unexplained infertility of unknown origin. If tubal pathology was detected by laparoscopy, the participant was excluded from randomisation. The numbers of women undergoing a laparoscopy were balanced between the 2 comparison groups. 2. This study performed IUI for various indications: male factor (21%), cervical factor (11%), endometriosis (11%), or unexplained subfertility (49%) and ovulation disorder (33%). Anovulation was reported in the methods section as an exclusion criterion. The study authors defined ovulation disorder as follows: quote: "A combination of irregular menstrual cycles with multicystic ovaries on TVUS and basal gonadotrophin measurements within the normal range" (correspondence with the first study author). Comment: in everyday clinical practice ovulation disorder is not an indication for IUI by itself. 3. Data on the number or the localisation of the polyps could not be retrieved since the first author no longer works in the university hospital. 4. Data on the size of the polyps in the control group could not be obtained for similar reasons as note 3. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomised to one of the two groups with use of an opaque envelope technique, with assignment determined by a computerized random number table." Quote: "Subjects were randomised into one of two groups in a 1:1 ratio using a restricted randomisation." Comment: probably done, but using simple randomisation, with an equal allocation ratio, by referring to a table of random numbers generated by a computer. |
| Allocation concealment (selection bias) | Low risk | Quote: "Patients were randomised to one of the two groups with use of an opaque envelope technique, with assignment determined by a computerized random number table." Comment: sequentially numbered, opaque, sealed envelopes were used according to correspondence with the first author; probably done. |
| Blinding of participants and personnel (performance bias) | Low risk | Method not stated: no further clarification obtained from the study authors. Comment: not applicable as this is a surgical study with unequivocal outcomes. |
| Blinding of outcome assessment (detection bias) | Low risk | Method not stated: no further clarification obtained from the study authors. Comment: not applicable as this is a surgical study with unequivocal outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "11 patients were lost from the study, 6 in the study group (3 lost to follow‐up, 2 pathologic reports of submucosal myoma and 1 in whom the polyp was not confirmed) and 5 in the control group (1 lost to follow‐up, 2 in whom the polyp was not confirmed and 2 pathologic reports of myoma)." Comment: missing outcome data were balanced in numbers across the comparison groups, with similar reasons for missing data across groups. |
| Selective reporting (reporting bias) | High risk | All specified outcomes reported in the results section. The final study report nevertheless failed to include results for the live birth rate, which is the primary outcome of interest expected for a trial on fertility treatment conducted over a 4‐year period. Data on the outcomes live birth and miscarriage were not available since most the majority of randomised women were referred by gynaecologists from outside the tertiary university hospital and were referred back when pregnant for further follow‐up by the referring gynaecologist. No clarification could be obtained for the lack of data on hysteroscopic complications. |
| Other bias | Low risk | No evidence for imbalance in the baseline characteristics. |
CI: confidence interval; FSH: follicle‐stimulating hormone; HSG: hysterosalpingography; IU: international units; IUI: intrauterine insemination; TVUS: transvaginal ultrasound; WHO: World Health Organization.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not addressing the research questions described in the protocol. RCT in women with no suspected major uterine cavity abnormalities undergoing a first IVF treatment cycle. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing intrauterine balloon stenting vs no stenting following hysteroscopic treatment for septate uterus. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial studying the efficacy of hyaluronic acid gel in preventing the development of intrauterine adhesions following hysteroscopic adhesiolysis. Mixed population of women with intrauterine adhesions, presenting with subfertility or other gynaecological complaints. Primary outcome: adhesion scores. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing hysteroscopy prior to a subsequent IVF attempt vs immediate IVF without prior hysteroscopy conducted in women with ≥ 2 failed IVF cycles with unsuspected or no uterine cavity abnormalities. Main outcomes: biochemical pregnancy, clinical pregnancy and delivery rates. | |
| Not addressing the research questions described in the protocol. Randomised controlled open pilot clinical trial studying the efficacy of the intrauterine infusion of autologous platelet rich plasma vs saline infusion after operative hysteroscopy for the management of moderate‐to‐severe Asherman's syndrome. | |
| Not addressing the research questions described in the protocol. RCT studying the effectiveness of routine hysteroscopy compared to no prior hysteroscopy in women with normal transvaginal ultrasound and HSG before the first ICSI treatment cycle. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial in subfertile women comparing the application of amnion graft, either fresh or dried to an intrauterine balloon vs the application of an intrauterine balloon without amnion graft as an adjunctive procedure after the hysteroscopic lysis of severe intrauterine adhesions, diagnosed at clinic hysteroscopy in women with infertility with or without menstrual disorders as the primary symptom. Outcomes: improvement in adhesion grade, improvement in menstruation, increased uterine length at sounding, complications and reproductive outcome. | |
| Not addressing the research questions described in the protocol. Women with detectable uterine pathology by ultrasound were excluded from participating in the trial aiming to study the effectiveness of hysteroscopy before a first trial ICSI. | |
| Not addressing the research questions described in the protocol. Systematic review including clinical trials of hysteroscopy with or without endometrial biopsy in women with recurrent implantation failure and no suspected intrauterine lesions. | |
| Not addressing the research questions described in the protocol. RCT investigating the effects of mindfulness‐based stress reduction on anxiety, depression and quality of life in women with intrauterine adhesions. | |
| Not addressing the research questions described in the protocol. The target population included women with abnormal uterine bleeding and hysteroscopically diagnosed uterine polyps. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing 2 different surgical techniques for metroplasty: operative hysteroscopy using the resectoscope with a unipolar knife vs the Versapoint device. Mixed population of women with septate uterus and a history of recurrent miscarriage or primary subfertility. Outcomes: operative parameters, complications, need for a second intervention and reproductive outcome parameters. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing extended sectioning by resectoscopy vs sequential cold knife excision for treating a complete utero‐cervicovaginal septum in a mixed population of women with infertility or pregnancy loss. Main outcomes: operating time, perioperative bleeding, complications, reproductive outcome, and participant and husband satisfaction. | |
| Study on the effectiveness of hysteroscopic metroplasty for small septate uterus in women with repeated IVF implantation failure. Although denoted by the authors as the first prospective randomised controlled study on this subject, the trial did not use a valid random sequence generation. Quote: "These patients, once informed about the situation, were randomly allocated, depending on their personal decision ..." | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing the application of hyaluronan derivative gel (Hyalobarrier gel) after hysteroscopic surgery vs surgical treatment alone in women aged 18–65 years, with gynaecological conditions other than subfertility. Primary outcome: adhesion score at second‐look hysteroscopy. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised comparison between clinic hysteroscopy prior to a subsequent IVF attempt or immediate IVF without prior clinic hysteroscopy conducted in women with ≥ 2 failed IVF cycles with unsuspected or no uterine cavity abnormalities. Outcomes: number of oocytes retrieved, fertilisation rate, number of embryos transferred, first trimester miscarriage and clinical pregnancy rates. | |
| Not addressing the research questions described in the protocol. RCT comparing the new 16 Fr mini‐resectoscope with the traditional 22 Fr resectoscope and Bettocchi 15 Fr hysteroscope for the treatment of uterine cavitary lesions. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing the use of Intercoat absorbable adhesion barrier gel vs no adhesion barrier after hysteroscopic synechiolysis in a mixed population of women with infertility or other gynaecological conditions. Primary outcomes: incidence of de novo intrauterine adhesions, adhesion scores and patency of the internal uterine ostium. | |
| Not addressing the research questions described in the protocol. RCT evaluating the role of endometrial injury in the cycle preceding ovarian stimulation for IUI cycle on the clinical pregnancy rate. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing diagnostic hysteroscopy with directed biopsy or hysteroscopic treatment of unsuspected uterine cavity abnormalities (or both) vs no hysteroscopy in women with primary infertility treated with ICSI. Primary outcome: clinical pregnancy. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing hysteroscopy vs no hysteroscopy in women with recurrent implantation failure with IVF. Status: completed. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial aimed at assessing the role of using clinic hysteroscopy as a routine investigation in improving ICSI pregnancy rates in 2 groups of infertile women with no abnormality detected on transvaginal ultrasonographic examination. | |
| Not addressing the PICO research question of this Cochrane Review. | |
| Not addressing the PICO research question of this Cochrane review. RCT evaluating the safety and effectiveness of Oxiplex/AP gel (Intercoat) in reducing intrauterine adhesion formation after hysteroscopic treatment because of retained products of conception. | |
| Not addressing the PICO research question of this Cochrane Review. RCT studying the efficacy of freeze‐dried amnion graft for prevention of intrauterine adhesion reformation after hysteroscopic adhesiolysis. | |
| Observational non‐randomised study on the effectiveness of hysteroscopy in women with repeated implantation failure. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing hysteroscopic surgery for the removal of polyps, fibroids or septa followed by the application of auto‐cross linked hyaluronic acid gel vs hysteroscopic surgery without the adhesion barrier in a mixed population of women with subfertility and other gynaecological symptoms associated with endometrial polyps, submucous fibroids or septa. Main outcomes: rates of adhesion formation and adhesion scores. | |
| Not addressing the research questions described in the protocol. Prospective, randomised, controlled trial to evaluate the efficacy of different doses of oestrogen treatment (2 mg and 6 mg daily) after hysteroscopic adhesiolysis in women with moderate‐to‐severe adhesion according to the American Fertility Society classification of intrauterine adhesions. | |
| Not addressing the research questions described in the protocol. Multicentre, open‐label, randomised, controlled trial comparing hysteroscopic morcellation with bipolar resectoscopy for removal of endometrial polyps, in terms of procedure time, peri‐ and postoperative adverse events, tissue availability and short‐term effectiveness. | |
| Not addressing the research questions described in the protocol. Single‐blind RCT assessing whether exogenous hormone administration starting immediately after a successful hysteroscopic adhesiolysis, in women with Asherman's syndrome may reduce the incidence of spontaneous recurrence of adhesions more than the endogenic production of hormones. | |
| Not addressing the research questions described in the protocol. Randomised controlled study examining the effect of scratching in a normal visually and histologically endometrium. Women with uterine pathology were excluded before or during clinic hysteroscopy. | |
| Not addressing the research questions described in the protocol. Single‐blind RCT to assess the outcomes of surgery in a group of women who were randomly submitted to preoperative gonadotropin‐releasing hormone agonists in comparison with women who received no medication. | |
| Not addressing the research questions described in the protocol. Randomised controlled study to compare mechanical (cold scissor) vs electrosurgical metroplasty (bipolar twizzle) in terms of feasibility and pain scoring during ambulatory‐based hysteroscopic metroplasty for short, narrow‐based uterine septa. | |
| Not addressing the research questions described in the protocol. RCT comparing the resection of endometrial polyps with 2 different devices: the Versapoint bipolar electrode and the diode laser. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing transcervical resection by hysteroscopy of endometrial polyps suspected on TVUS and SIS vs observation for 6 months. The study population included premenopausal women with bleeding problems associated with endometrial polyps. The aim of the trial was to study the clinical effectiveness of transcervical resection of endometrial polyps for the outcome periodic blood loss. Women wishing to become pregnant were excluded from the trial. Primary outcome: periodic blood loss measured by the Pictorial Blood Assessment Chart. | |
| Not addressing the research questions described in the protocol. Randomised trial comparing the efficacy of intrauterine balloon and intrauterine contraceptive device in the prevention of adhesion reformation following hysteroscopic adhesiolysis. | |
| Not addressing the research questions described in the protocol. RCT randomly comparing oestradiol valerate (Progynova) 3 mg or 9 mg per diet before surgery or no hormonal treatment before transcervical resection of adhesions. | |
| Comparative non‐randomised study on the value of hysteroscopy prior to IVF/ICSI. | |
| Not addressing the research questions described in the protocol. RCT studying the effectiveness of hysteroscopy before IUI on reproductive outcome in infertile women with no suspected intrauterine lesions during baseline fertility assessment. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial in women aged 18–75 years comparing operative hysteroscopy using the monopolar resectoscope vs hysteroscopic bipolar electrode excision for the treatment of endometrial polyps. Outcomes: operating times, difficulty of the operation, surgeon satisfaction with the procedure, complications, postoperative pain and participant satisfaction. | |
| Not addressing the research questions described in the protocol. Multicentric randomised trial in 180 women affected by endometrial hyperplasia, myomas or endometrial polyps undergoing operative hysteroscopy comparing cefazolin 2 g intravenously 30 minutes prior to the procedure vs no antibiotic treatment. | |
| Not addressing the research questions described in the protocol. Double‐blind, randomised, placebo‐controlled study to assess the incidence of infectious complications and the protective effect of antibiotic administration during operative hysteroscopic procedures in a clinic setting. 1046 consecutively enrolled women with intrauterine lesions were randomly allocated to the intervention group (523 participants administered cefazolin 1 g intramuscularly) and the control group (523 participants administered with 10 mL of isotonic sodium chloride solution), and treated in clinic setting by operative hysteroscopy for endometrial polypectomy, uterine septa, submucosal myomas and intrauterine adhesions. | |
| Quasi‐randomised trial comparing early second‐look clinic hysteroscopic adhesiolysis after hysteroscopic adhesiolysis and IUD insertion vs no early second‐look operative hysteroscopy in subfertile women with intrauterine adhesions. The method of sequence generation was based on alternation: women were allocated to the intervention or control groups based on their study entry. Main outcomes: pregnancy and live birth rate. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial in a mixed study population of women with a history of pregnancy wastage or infertility and an associated complete uterine septum comparing metroplasty with complete section of the cervical septum vs metroplasty with preservation of the cervical septum. Outcomes: operating time, distending media deficit, total distending media used, intraoperative bleeding, complications and reproductive outcome. | |
| Not addressing the research questions described in the protocol. Randomised, double‐blind, controlled trial to evaluate the efficacy and safety of Intercoat (Oxiplex/AP Gel) in preventing intrauterine adhesions after operative hysteroscopy. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial conducted in women with ≥ 2 failed IVF cycles with unsuspected or no uterine cavity abnormalities comparing clinic hysteroscopy prior to a subsequent IVF attempt or immediate IVF without prior hysteroscopy. Outcomes: number of oocytes retrieved, fertilisation rate, number of embryos transferred and clinical pregnancy rates. | |
| Not addressing the research questions described in the protocol. Parallel‐group RCT assessing the safety of hyaluronic acid gel to prevent intrauterine adhesions in hysteroscopic surgery | |
| Not addressing the research questions described in the protocol. RCT to evaluate the efficacy of oestrogen in preventing intrauterine adhesions following hysteroscopic septal resection and to investigate its effect on reproductive outcome. | |
| Not addressing the research questions described in the protocol. RCT to compare the operation and reproductive outcome of hysteroscopic septal resection using unipolar resectoscope vs bipolar resectoscope. | |
| Not addressing the research questions described in the protocol. Randomised, prospective, parallel, comparative, single‐blinded study comparing the operative and reproductive outcome of hysteroscopic myomectomy using unipolar resectoscope vs bipolar resectoscope in women with infertility and menorrhagia. | |
| Not addressing the research questions described in the protocol. Randomised, prospective, comparative setting clinical trial to examine efficacy of hysteroscopic removal of polyps and myomas on health‐related quality of life and symptom severity at 1‐year postprocedure in a clinic vs ambulatory surgical centre. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial conducted to determine the incidence of unsuspected uterine cavity abnormalities detected by clinic hysteroscopy in women before ICSI treatment compared to ICSI without prior hysteroscopy. Main outcomes: incidence of unsuspected uterine abnormalities, and implantation and clinical pregnancy rates. | |
| Published report describing a parallel‐group randomised trial comparing hysteroscopic myomectomy vs diagnostic hysteroscopy and biopsy in women with otherwise unexplained primary infertility and submucous fibroids. Primary outcome: clinical pregnancy rates. Quote from Fertility and Sterility searched on 16 January 2012: "This article has been retracted at the request of the editor as it duplicates parts of a paper that had already appeared in Hum. Reprod., 20 (2005) 1632–1635, DOI:10.1093/humrep/deh822." | |
| Not addressing the research questions described in the protocol. RCT assessing the interobserver agreement among gynaecologists who were randomised into 2 groups: 1 group received diagnostic criteria for a septate uterus before assessment of videos, whereas the other group assessed the recordings without instruction. | |
| Not addressing the research questions described in the protocol. Pragmatic, multicentre, RCT in women with a normal TVUS of the uterine cavity and no previous hysteroscopy who were scheduled for their first IVF treatment randomly comparing treatment with hysteroscopy of detected intracavitary abnormalities before starting IVF vs immediate start of the IVF treatment. | |
| Not addressing the research questions described in the protocol. Multicentre, single‐blind, randomised, controlled trial to evaluate whether hysteroscopic morcellation or bipolar electrosurgical resection was more favourable for removing endometrial polyps in a clinic setting in terms of feasibility, speed, pain and acceptability. | |
| Not addressing the research questions described in the protocol. Parallel‐group RCT to assess the effectiveness of diagnostic hysteroscopy in women prior to IVF/IICSI. The study population included women with a normal hysterosonography and normal vaginal ultrasound during the past 12 months. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised study comparing hysteroscopic lysis of intrauterine adhesions with or without adjunctive therapy (cyclical hormone replacement therapy alone or intrauterine device alone or both cotreatments combined) after hysteroscopic metroplasty in a mixed population of women with subfertility or recurrent miscarriage (or both). Main outcomes: incidence of de novo adhesion formation and ongoing pregnancy rate. | |
| Clinical controlled trial on the effectiveness of hysteroscopy prior to IVF; no random sequence generation. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing the hysteroscopic removal of polyps or fibroids by conventional hysteroscopy using a resectoscope vs hysteroscopic morcellation in a mixed population of women with infertility or other gynaecological conditions. Outcomes: mean number of insertions into the uterine cavity and mean operating time. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised comparing metroplasty using the resectoscope vs microscissors for treating uterine septum in women with repeated miscarriage. Outcomes: mean operating time, mean amount of distension medium used and complications. | |
| Not addressing the research questions described in the protocol. Parallel‐group RCT to determine whether performing curettage the month prior to embryo transfer increases the chance of embryo implantation. | |
| Not addressing the research questions described in the protocol. Prospective, randomised, double‐blind, controlled clinical trial assessing the efficacy and safety of auto‐crosslinked hyaluronic acid gel for preventing intrauterine adhesions after hysteroscopic adhesiolysis. | |
| Not addressing the research questions described in the protocol. Parallel‐group randomised trial comparing 2 different surgical techniques for metroplasty: resectoscopy with monopolar knife vs small‐diameter hysteroscopy fitted with a 5 Fr reusable bipolar electrode. Outcomes: pregnancy, miscarriage and live birth rates. |
HSG: hysterosalpingography; ICSI: intracytoplasmic sperm injection; IUD: intrauterine device; IUI: intrauterine insemination; IVF: in vitro fertilisation; PICO: Participants, Interventions, Comparisons and Outcomes; RCT: randomised controlled trial; SIS: saline infusion sonography; TVUS: transvaginal ultrasound.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Assessment of hysteroscopic metroplasty in women with a uterine septum and a history of miscarriage: a randomised controlled trial – SEPTUM. |
| Methods | Pilot multicentre randomised controlled trial to assess feasibility for a larger adequately powered trial. |
| Participants | Women with septate uteri, history of miscarriage or preterm birth, or infertility |
| Interventions | Intervention: hysteroscopic septal resection Comparator: no intervention |
| Outcomes | Primary outcome
Secondary outcomes
|
| Starting date | 9 December 2014 |
| Contact information | Dr Matthew Prior Subspecialty Registrar in Reproductive Medicine and Surgery Newcastle Fertility Centre email: [email protected] mobile: +44 7817 627 712 |
| Notes | Quote: "The trial is ongoing but closed to recruitment due to feasibility issues with recruitment. Six participants were recruited and will be followed up for 24 months post intervention." |
| Trial name or title | TRUST – The Randomised Uterine Septum Transsection trial |
| Methods | Multicentre, parallel‐group, randomised controlled trial. No masking/blinding |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Intervention: hysteroscopic metroplasty Comparator: no surgical resection |
| Outcomes | Primary outcome
Secondary outcomes
|
| Starting date | 1 October 2008 |
| Contact information | Dr JFW Rikken |
| Notes | 4 May 2018: inclusion of 63rd participant; targeted sample size = 68. Trial website: www.studies‐obsgyn.nl/trust/ |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical pregnancy Show forest plot | 1 | 94 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.44 [0.97, 6.17] |
| Analysis 1.1  Comparison 1 Operative hysteroscopy versus control in women with otherwise unexplained subfertility and suspected major uterine cavity abnormalities, Outcome 1 Clinical pregnancy. | ||||
| 1.1 Removal of submucous fibroids only vs no surgery | 1 | 52 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.04 [0.62, 6.66] |
| 1.2 Removal of mixed submucous‐intramural fibroids vs no surgery | 1 | 42 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.24 [0.72, 14.57] |
| 2 Adverse events: miscarriage Show forest plot | 1 | 94 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.54 [0.47, 5.00] |
| Analysis 1.2  Comparison 1 Operative hysteroscopy versus control in women with otherwise unexplained subfertility and suspected major uterine cavity abnormalities, Outcome 2 Adverse events: miscarriage. | ||||
| 2.1 Removal of submucous fibroids only vs no surgery | 1 | 52 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.27, 5.97] |
| 2.2 Removal of mixed submucous‐intramural fibroids vs no surgery | 1 | 42 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.32, 12.33] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical pregnancy Show forest plot | 1 | 204 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.41 [2.45, 7.96] |
| Analysis 2.1  Comparison 2 Operative hysteroscopy versus control in women undergoing medically assisted reproduction with suspected major uterine cavity abnormalities, Outcome 1 Clinical pregnancy. | ||||
| 1.1 Hysteroscopic polypectomy vs diagnostic hysteroscopy and biopsy only prior to intrauterine insemination | 1 | 204 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.41 [2.45, 7.96] |

Study flow diagram: summary of searches since 2014. CR: Cochrane Review; PICO: Population, Intervention, Comparator, Outcome; RCT: randomised controlled trial; SR: systematic review.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
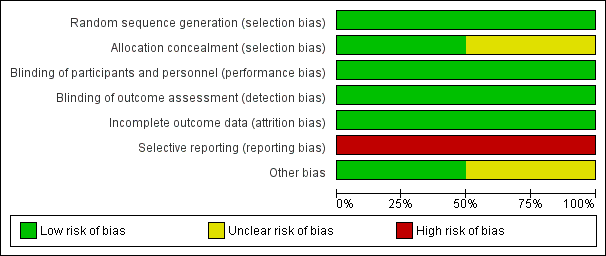
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
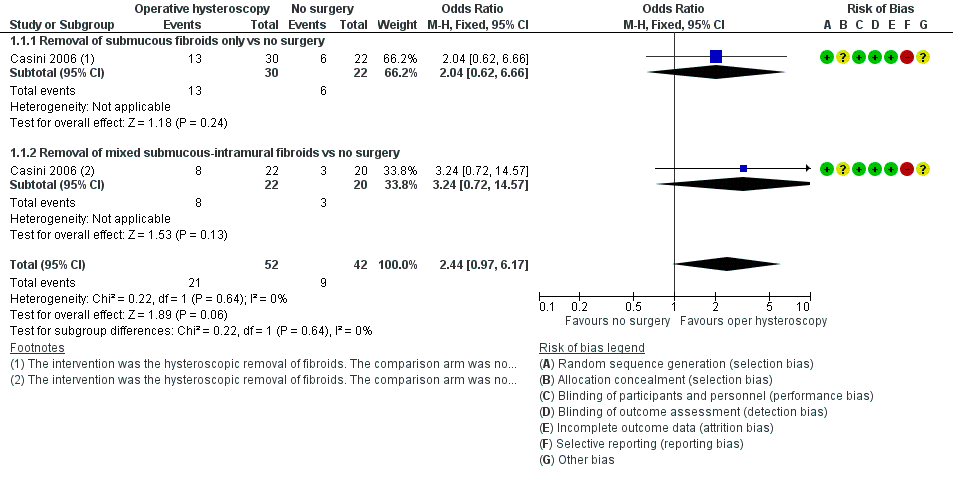
Forest plot of comparison: 1 Hysteroscopic myomectomy vs no surgery in women with unexplained subfertility and submucous fibroids. Outcome: 1.1 Clinical pregnancy per woman randomised.

Forest plot of comparison: 1 Hysteroscopic myomectomy vs no surgery in women with unexplained subfertility and submucous fibroids. Outcome: 1.2 Miscarriage per clinical pregnancy.
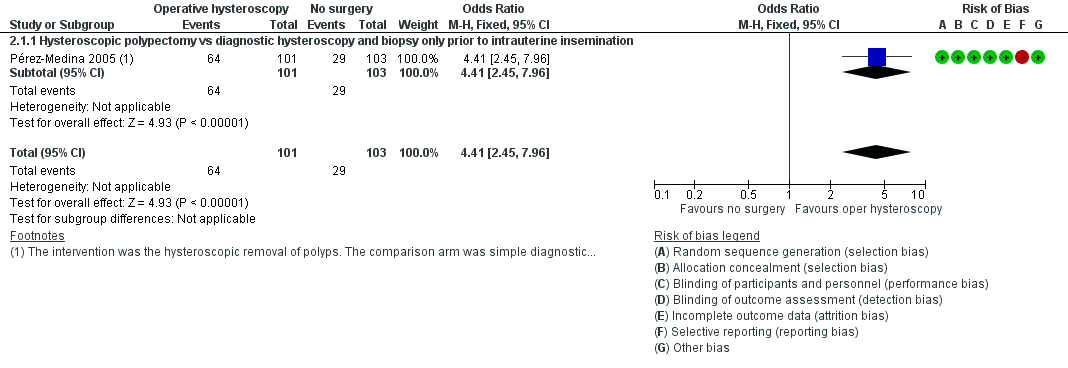
Forest plot of comparison: 2 Hysteroscopic removal of polyps vs diagnostic hysteroscopy and biopsy only prior to intrauterine insemination. Outcome: 2.1 Clinical pregnancy per woman randomised.

Comparison 1 Operative hysteroscopy versus control in women with otherwise unexplained subfertility and suspected major uterine cavity abnormalities, Outcome 1 Clinical pregnancy.
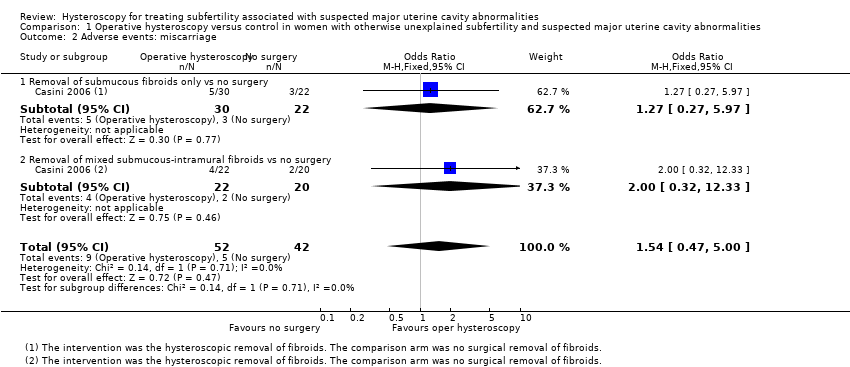
Comparison 1 Operative hysteroscopy versus control in women with otherwise unexplained subfertility and suspected major uterine cavity abnormalities, Outcome 2 Adverse events: miscarriage.
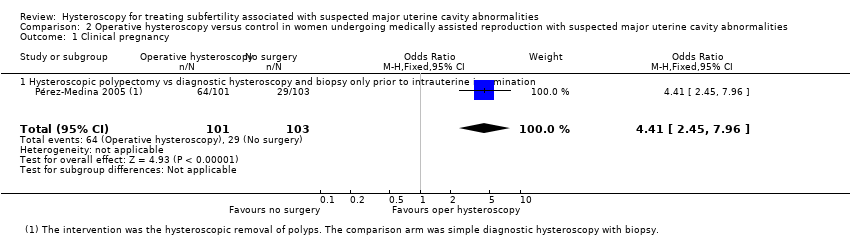
Comparison 2 Operative hysteroscopy versus control in women undergoing medically assisted reproduction with suspected major uterine cavity abnormalities, Outcome 1 Clinical pregnancy.
| Operative hysteroscopy versus control in women with otherwise unexplained subfertility and suspected major uterine cavity abnormalities | ||||||
| Patient or population: women with submucous fibroids and otherwise unexplained subfertility Settings: infertility centre in Rome, Italy Intervention: hysteroscopic removal of 1 submucous fibroid ≤ 40 mm Comparison: no surgery | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No surgery | Myomectomy | |||||
| Live birth | No data reported. | |||||
| Adverse events: hysteroscopy complications | No data reported. | |||||
| Clinical pregnancya Ultrasound 12 months | 214 per 1000 | 400 per 1000 | OR 2.44 (0.97 to 6.17) | 94 | ⊕⊝⊝⊝ | — |
| Adverse events: miscarriaged Ultrasound 12 months | 119 per 1000 | 172 per 1000 | OR 1.54 (0.47 to 5.00) | 94 women | ⊕⊝⊝⊝ | — |
| *The basis for the assumed risk is the control group risk of the single included study (Casini 2006). The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aClinical pregnancy defined by the visualisation of an embryo with cardiac activity at six to seven weeks' gestational age. bDowngraded by two levels for very serious risk of bias (unclear allocation concealment, high risk of selective outcome reporting and unclear whether there is other bias caused by imbalance in the baseline characteristics). cDowngraded by one level for serious imprecision (wide confidence interval of the effect size estimate). dMiscarriage was defined by the clinical loss of an intrauterine pregnancy between the 7th and 12th weeks of gestation. | ||||||
| Operative hysteroscopy versus control in women undergoing medically assisted reproduction with suspected major uterine cavity abnormalities | ||||||
| Patient or population: subfertile women with endometrial polyps diagnosed by ultrasonography prior to treatment with gonadotropin and intrauterine insemination Settings: infertility unit of a university tertiary hospital in Madrid, Spain Intervention: hysteroscopic polypectomy using a 5.5 mm continuous flow office hysteroscope with a 1.5 mm scissors and forceps Comparison: diagnostic hysteroscopy using a 5.5 mm continuous flow office hysteroscope and polyp biopsy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Polypectomy | |||||
| Live birth | No data reported. | |||||
| Adverse events: hysteroscopy complications | No data reported. | |||||
| Clinical pregnancya Ultrasound 4 intrauterine insemination cycles | 282 per 1000 | 634 per 1000 | OR 4.41 (2.45 to 7.96) | 204 | ⊕⊕⊝⊝ | — |
| Adverse events: miscarriage | No data were reported for this secondary outcome. | |||||
| *The basis for the assumed risk is the control group risk of the single included study (Pérez‐Medina 2005). The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aClinical pregnancy was defined by the presence of at least one gestational sac on ultrasound. bDowngraded by one level for serious risk of bias (high risk for selective outcome reporting). cDowngraded by one level for serious imprecision (wide confidence interval of the effect size estimate). | ||||||
| Polyp size | Clinical pregnancya | Clinical pregnancy rate (95% CI)b |
| < 5 mm | 19/25 | 76% (72% to 80%) |
| 5–10 mm | 18/32 | 56% (53% to 59%) |
| 11–20 mm | 16/26 | 61% (58% to 65%) |
| > 20 mm | 11/18 | 61% (58% to 64%) |
| CI: confidence interval. aClinical pregnancy is defined by a pregnancy diagnosed by ultrasound visualisation of at least one gestational sac per woman randomised. bNo significant difference was found for the clinical pregnancy rates between the 4 subgroups (P = 0.32). | ||
| Quality assessment Submucous fibroids and unexplained subfertility | ||||||
| No of studies | Design | Limitations | Inconsistency | Indirectness | Imprecision | Other considerations |
| Clinical pregnancy (follow‐up 1 year; ultrasounda) | ||||||
| 1 | RCT | Very seriousb | Not serious | Not indirectness | Seriousc | None |
| Miscarriage (follow‐up 1 year; ultrasoundd) | ||||||
| 1 | RCT | Very seriousb | Not serious | Not serious | Seriousc | None |
| aA clinical pregnancy was defined by the visualisation of an embryo with cardiac activity at six to seven weeks' gestational age. bUnclear allocation concealment and high risk of selective outcome reporting. cWide confidence intervals. dMiscarriage was defined by the clinical loss of an intrauterine pregnancy between the 7th and 12th weeks of gestation. | ||||||
| Quality assessment Endometrial polyps prior to gonadotropin and IUI treatment | ||||||
| No of studies | Design | Limitations | Inconsistency | Indirectness | Imprecision | Other considerations |
| Clinical pregnancy (follow‐up 4 IUI cycles; ultrasounda) | ||||||
| 1 | RCT | Seriousb | Not serious | Not serious | Not serious | None |
| IUI: intrauterine insemination; RCT: randomised controlled trial. aClinical pregnancy was defined by the presence of at least one gestational sac on ultrasound. bThere was high risk for selective outcome reporting bias. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical pregnancy Show forest plot | 1 | 94 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.44 [0.97, 6.17] |
| 1.1 Removal of submucous fibroids only vs no surgery | 1 | 52 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.04 [0.62, 6.66] |
| 1.2 Removal of mixed submucous‐intramural fibroids vs no surgery | 1 | 42 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.24 [0.72, 14.57] |
| 2 Adverse events: miscarriage Show forest plot | 1 | 94 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.54 [0.47, 5.00] |
| 2.1 Removal of submucous fibroids only vs no surgery | 1 | 52 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.27, 5.97] |
| 2.2 Removal of mixed submucous‐intramural fibroids vs no surgery | 1 | 42 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.32, 12.33] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical pregnancy Show forest plot | 1 | 204 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.41 [2.45, 7.96] |
| 1.1 Hysteroscopic polypectomy vs diagnostic hysteroscopy and biopsy only prior to intrauterine insemination | 1 | 204 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.41 [2.45, 7.96] |

