Interwencje optymalizujące przepisywanie leków u osób w podeszłym wieku w domach opieki
Abstract
Background
There is a substantial body of evidence that prescribing for care home residents is suboptimal and requires improvement. Consequently, there is a need to identify effective interventions to optimise prescribing and resident outcomes in this context. This is an update of a previously published review (Alldred 2013).
Objectives
The objective of the review was to determine the effect of interventions to optimise overall prescribing for older people living in care homes.
Search methods
For this update, we searched the Cochrane Central Register of Controlled Trials (CENTRAL) (including the Cochrane Effective Practice and Organisation of Care (EPOC) Specialised Register), MEDLINE, EMBASE and CINAHL to May 2015. We also searched clinical trial registries for relevant studies.
Selection criteria
We included randomised controlled trials evaluating interventions aimed at optimising prescribing for older people (aged 65 years or older) living in institutionalised care facilities. Studies were included if they measured one or more of the following primary outcomes: adverse drug events; hospital admissions; mortality; or secondary outcomes, quality of life (using validated instrument); medication‐related problems; medication appropriateness (using validated instrument); medicine costs.
Data collection and analysis
Two authors independently screened titles and abstracts, assessed studies for eligibility, assessed risk of bias and extracted data. We presented a narrative summary of results.
Main results
The 12 included studies involved 10,953 residents in 355 (range 1 to 85) care homes in ten countries. Nine studies were cluster‐randomised controlled trials and three studies were patient‐randomised controlled trials. The interventions evaluated were diverse and often multifaceted. Medication review was a component of ten studies. Four studies involved multidisciplinary case‐conferencing, five studies involved an educational element for health and care professionals and one study evaluated the use of clinical decision support technology. We did not combine the results in a meta‐analysis due to heterogeneity across studies. Interventions to optimise prescribing may lead to fewer days in hospital (one study out of eight; low certainty evidence), a slower decline in health‐related quality of life (one study out of two; low certainty evidence), the identification and resolution of medication‐related problems (seven studies; low certainty evidence), and may lead to improved medication appropriateness (five studies out of five studies; low certainty evidence). We are uncertain whether the intervention improves/reduces medicine costs (five studies; very low certainty evidence) and it may make little or no difference on adverse drug events (two studies; low certainty evidence) or mortality (six studies; low certainty evidence). The risk of bias across studies was heterogeneous.
Authors' conclusions
We could not draw robust conclusions from the evidence due to variability in design, interventions, outcomes and results. The interventions implemented in the studies in this review led to the identification and resolution of medication‐related problems and improvements in medication appropriateness, however evidence of a consistent effect on resident‐related outcomes was not found. There is a need for high‐quality cluster‐randomised controlled trials testing clinical decision support systems and multidisciplinary interventions that measure well‐defined, important resident‐related outcomes.
PICOs
Streszczenie prostym językiem
Interwencje optymalizujące przepisywanie leków u osób w podeszłym wieku w domach opieki
Wstęp
Osoby w podeszłym wieku mieszkające w domach opieki (zwanych również domami spokojnej starości, placówkami opieki pielęgniarskiej, placówkami dla osób w podeszłym wieku) mają dużo złożonych problemów zdrowotnych, zarówno fizycznych, jak i psychicznych. Mieszkańcom domów opieki przepisuje się więcej leków w porównaniu z osobami mieszkającymi we własnych domach, często jest to średnio 8 leków. W międzynarodowych badaniach wykazano, że leki te są często źle nadzorowane, a niektórym z mieszkańców ‐ leki przepisywano w niewłaściwy sposób. Prowadzi to potencjalnie do szkodliwych efektów ubocznych i utraty korzyści z ich stosowania. Z tych powodów ważne jest, aby mieszkańcom domów opieki przepisywano odpowiednie leki w odpowiednich dawkach. To jest aktualizacja poprzedniego przeglądu (Alldred 2013).
Charakterystyka badań
Odnaleźliśmy 12 badań obejmujących 10953 mieszkańców przebywających w 355 domach opieki w dziesięciu krajach. W badaniach oceniano interwencje mające na celu optymalizację przepisywania leków w domach opieki. Większość interwencji miała kilka składowych, często obejmujących analizę stosowanych leków przez farmaceutę i lekarza. Niektóre interwencje obejmowały również czynnik edukacyjny, a w jednym badaniu wykorzystywano technologię informacyjną (IT).
Kluczowe wyniki
Nie znaleźliśmy danych naukowych wskazujących na skuteczność interwencji w odniesieniu do zmniejszenia liczby działań niepożądanych (szkodliwych skutków wywoływanych przez leki) lub zgonu. W jednym badaniu wykazano skrócenie czasu pobytu osoby w szpitalu, jednak w większości badań nie potwierdzono korzyści w odniesieniu do zmniejszenia liczby hospitalizacji. W jednym z badań stwierdzono spowolnienie pogarszania się jakości życia związanej ze zdrowiem. Za pomocą interwencji użytych w badaniach znaleziono problemy związane z lekami i je rozwiązano. W pięciu badaniach stwierdzono poprawę w zakresie przepisywania leków na podstawie kryteriów oceny stosowności przepisywania leków.
Wiarygodność danych naukowych
Oceniliśmy ogólną jakość danych naukowych dla opisanych wskaźników jako niską dla zdarzeń niepożądanych (szkodliwe efekty wywołane przez leki), przyjęcia do szpitala, zgonu, jakości życia, problemów związanych z lekami, prawidłowości w przepisywaniu leków oraz bardzo niską dla kosztów leków. Istnieje potrzeba przeprowadzenia badań wysokiej jakości w celu uzyskania większej ilości danych dla tych i innych rodzajów interwencji. Dalsze badania są konieczne, aby ocenić nowe technologie, m.in. systemy komputerowe wspierające decyzje dotyczące przepisywania leków. Potrzeba więcej pracy, aby upewnić się, że badacze konsekwentnie mierzą wskaźniki, które są ważne dla mieszkańców domu opieki.
Authors' conclusions
Summary of findings
| Interventions to optimise prescribing compared with usual GP care for care home residents | |||
| Patient or population: older people (aged 65 years or older) living in care homes Settings: Institutionalised care facilities in Australia, Finland, Israel, Netherlands, New Zealand, Spain, Sweden, United Kingdom, and USA and Canada Intervention: Intervention to optimise prescribing (single or multicomponent intervention) Comparison: Usual care by general practitioner | |||
| Outcomes | Impact | No of Participants | Quality of the evidence |
| Adverse drug events | There was no evidence of an effect on adverse drug events | 1228 in 87 care homes (2 studies) | ⊕⊕⊝⊝ |
| Hospital admissions | It is uncertain whether medication review reduces hospital admissions | 7606 in 309 care homes (8 studies) | ⊕⊕⊝⊝ |
| Mortality | There was no evidence of an effect on mortality | 6805 in 188 care homes (6 studies) | ⊕⊕⊝⊝ |
| Quality of life | It is uncertain whether medication review improves quality of life | 586 in 21 care homes (2 studies) | ⊕⊕⊝⊝ |
| Medication‐related problems | Medication review may lead to the identification and resolution of medication‐related problems | 6640 in 251 care homes (7 studies) | ⊕⊕⊝⊝ |
| Medication appropriateness | Medication review may lead to an improvement in medication appropriateness | 1566 in 152 care homes (5 studies) | ⊕⊕⊝⊝ |
| Medicine costs | It is uncertain whether medication review decreases medication costs | 4734 in 142 care homes (5 studies) | ⊕⊝⊝⊝ |
| GRADE Working Group grades of evidence | |||
| Quality assessment of evidence for each outcome was based on study design, risk of bias, inconsistency, indirectness and imprecision. The evidence was downgraded from high to low for adverse drug events (Crotty 2004b; Gurwitz 2008) due to a serious risk of bias and imprecision. The evidence was downgraded from high to low for hospital admissions (Furniss 2000; Roberts 2001; Crotty 2004b; Zermansky 2006; Frankenthal 2014; Garcia‐Gollarte 2014; Pitkala 2014; Connolly 2015), mortality (Furniss 2000; Roberts 2001; Zermansky 2006; Frankenthal 2014; Pitkala 2014; Connolly 2015), quality of life (Frankenthal 2014; Pitkala 2014) and medication appropriateness (Crotty 2004a; Crotty 2004b; Frankenthal 2014; Garcia‐Gollarte 2014; Pitkala 2014) due to a serious risk of bias and inconsistency. The evidence for medicines costs (Furniss 2000; Roberts 2001; Crotty 2004a; Zermansky 2006; Frankenthal 2014 was downgraded from high to very low due to a serious risk of bias, inconsistency and imprecision. The evidence for medicine‐related problems (Strikwerda 1994; Claesson 1998; Furniss 2000; Roberts 2001; Crotty 2004b; Zermansky 2006; Frankenthal 2014 was reduced from high to low due to design, risk of bias and imprecision. | |||
Background
Globally, the proportion of older people in the population is increasing. The proportion of people aged 60 years and over was 11% in 2009 and this is projected to double by the middle of this century (United Nations 2009), with developed countries experiencing the fastest rise in number of older people. In the United Kingdom (UK), it is estimated that by 2034 nearly a quarter of the population will be aged 65 years and over. The most rapid rise has been in the 'oldest old' that is those aged 85 years and over; it is projected that by 2034 there will be a 2.5 fold increase in the number of the oldest old, representing 5% of the population (Office for National Statistics 2010). As a consequence, there will continue to be an increasing demand for long‐term care across the world.
Long‐term care may be provided in people's homes or in institutional facilities such as nursing homes or hospitals. The terminology used to describe homes that provide care for older people (defined as 65 years or older (Department of Health 2001)) differs across the world. In the UK the homes are known as 'care homes', in the United States (US) 'long‐term care facilities' and in Australia 'aged‐care facilities'. Care homes are usually classified into two main categories, those that provide 24‐hour nursing care (nursing homes in the UK, skilled‐nursing facilities in the US and aged‐care facilities providing high‐level care in Australia); and those that provide personal care (residential homes in the UK, assisted‐living in the US and aged‐care facilities providing low‐level care in Australia). Some care homes provide both types of care.
Older people living in care homes are often frail, and they are one of the most vulnerable groups in society. They have complex health needs due to multiple co‐morbidities and age‐related changes in pharmacokinetics and pharmacodynamics (Armour 2002). Polypharmacy, usually defined as greater than four or more medicines (Department of Health 2001; Rollason 2003; Patterson 2014), is common in this setting across the world with residents prescribed an increasing number of medicines over the last decade or so. In the UK, the mean number of medicines prescribed per resident was 4.9 in 1998 (Furniss 2000), 6.9 in 2003 (Zermansky 2006), and by 2007 this had risen to 8.0 (Barber 2009). Many care home residents also have cognitive impairment and this can impede their ability to communicate medicine‐related problems (Matthews 2002; Alldred 2007a).
The complexity of prescribing for this population is compounded by multiple clinicians prescribing. This may involve family physicians and community‐based consultants (for example old age psychiatrists and geriatricians) in primary care; and secondary care doctors from multiple specialities. In addition, the lack of representation of older people in clinical trials limits the evidence base and further increases the complexity (Beglinger 2008). It is, therefore, perhaps unsurprising that there is extensive evidence that prescribing is suboptimal for care home residents. Inappropriate prescribing, measured using validated, explicit and implicit definitions, has been found to be common in nursing and residential homes in several countries including the US (Beers 1992; Hanlon 1996; Sloane 2002; Gray 2003; Lau 2005; Perri 2005), Canada (Brymer 2003), the UK (Oborne 2003) and Australia (Crotty 2004a).
Perri 2005 found that over a one month duration, 47% of 1117 residents of 15 US nursing homes received at least one inappropriate medicine, with 13% of residents having at least one adverse health outcome. Inappropriate prescribing more than doubled the risk of a resident experiencing at least one adverse health outcome (odds ratio (OR) 2.34, 95% confidence interval (CI) 1.61 to 3.40). Lau 2005 reported that 50% of 3372 US nursing home residents were prescribed at least one inappropriate medicine over one year. The risks of hospitalisation and death were greater in those residents exposed to an inappropriate medicine (OR 1.27, 95% CI 1.09 to 1.47; OR 1.28, 95% CI 1.05 to 1.55, respectively). Gray 2003 found that 22% of 282 US residents of residential care facilities were prescribed at least one inappropriate medicine. There is also evidence that care home residents are under‐prescribed beneficial drugs and are poorly monitored with respect to their long‐term conditions and their medicines (Fahey 2003; Alldred 2007b; Barber 2009).
For the reasons discussed above, care home residents are particularly susceptible to adverse drug events. In two US long‐term care facilities, Gurwitz 2005 found 9.8 adverse drug events per 100 resident‐months, with 42% being judged as preventable. Drug‐related problems have been found to be responsible for 3% to 31% of hospital admissions of older people, and up to half of these are potentially avoidable (Howard 2007).
This is an update of a previously published review (Alldred 2013).
Description of the condition
As described above, suboptimal prescribing for older people living in care homes is common and may occur due to the prescribing of inappropriate medicines, the omission of beneficial medicines or the failure to appropriately monitor residents and the effects of their medicines. There are a variety of instruments that can be employed to measure the appropriateness of prescribing in older people (Spinewine 2007). However, the predictive validity of these instruments on health outcomes such as adverse drug events and hospital admissions has not been unequivocally established (Spinewine 2007).
Description of the intervention
For this review, we were interested in interventions concerned with optimising the whole medication regime for care home residents, not those concentrating solely on isolated drugs or classes such as benzodiazepines or antipsychotics nor those concentrating on one disease state. Financial and regulatory interventions tend to fall into this latter category.
There are several types of interventions that can potentially optimise prescribing in this setting, including:
-
professional interventions, for example educational programmes aimed at prescribers
-
organisational interventions, for example medication review services or specialist clinics, case conferencing, information and communication technology (ICT) interventions such as clinical decision support systems.
Medication review interventions may be aimed at specific drugs or the whole regime and can be uni‐ or multiprofessional, involving physicians, nurses and pharmacists.
How the intervention might work
Interventions designed to improve prescribing for care home residents may have an impact by discontinuing inappropriate medication; commencing beneficial medicines; and ensuring appropriate monitoring of long‐term conditions and medicines. Consequently, this may lead to a reduction in adverse drug events, improved quality of life and a reduction in medicine costs.
Why it is important to do this review
There is a substantial body of evidence that prescribing for care home residents is suboptimal and requires improvement. Furthermore, there are other Cochrane reviews being undertaken which address similar issues in different populations (Soe 2009; Christensen 2011). We evaluated the evidence for interventions to address suboptimal prescribing in this setting to identify how care can be improved for this frail and vulnerable population. We intended to achieve this by determining which interventions were effective and by identifying gaps in the evidence to inform future research.
Objectives
The objective of the review was to determine the effect of interventions to optimise overall prescribing for older people living in care homes.
Methods
Criteria for considering studies for this review
Types of studies
We included patient‐randomised controlled trials (patient‐RCT) and cluster‐randomised controlled trials (cluster‐RCT).
Types of participants
We included studies of older people (aged 65 years or older) living in institutionalised care facilities. Institutionalised care facilities include: nursing homes and residential homes (UK); skilled‐nursing facilities and assisted‐living facilities (US); and aged‐care facilities providing low‐level and high‐level care (Australia). If there was any ambiguity in the description of the institution, we clarified this with the authors of relevant papers. We considered trials for inclusion if they had a majority (80% or more) of participants aged 65 years or more, or if the mean age was greater than 65 years.
We excluded studies where the intervention focused on a single medical condition or a specific drug or class of drugs. We also excluded studies where the main focus was to reduce medication errors because such studies have a narrow focus and do not consider the whole medication regime. In addition, they do not seek to optimise prescribing, for example by adhering to evidence‐based guidelines or by reducing inappropriate prescribing, but are designed solely to reduce errors.
Types of interventions
We assessed interventions aimed at optimising prescribing for care home residents compared with usual care as defined by the study. These interventions potentially included: educational interventions aimed at prescribers; medication review services (uni‐ or multiprofessional, conducted by nurses, pharmacists or physicians); case conferencing; and ICT interventions such as clinical decision support systems. We excluded financial and regulatory interventions.
Types of outcome measures
We included a range of outcome measures including patient‐related outcomes, health service utilisation, and economic outcomes. Studies were included if they reported at least one primary outcome measure or at least one secondary outcome measure.
Primary outcomes
The primary outcome measures for the review were:
-
adverse drug events;
-
hospital admissions;
-
mortality.
Secondary outcomes
Secondary outcome measures were:
-
quality of life (using validated instrument);
-
medication‐related problems;
-
medication appropriateness (using validated instrument);
-
medicine costs.
Search methods for identification of studies
Paul Miller, Trials Search Co‐ordinator (TSC) for Cochrane Effective Practice and Organisation of Care (EPOC) updated the search terms used previously and conducted searches of the following electronic databases on 14 May 2015. Searches were limited by date to material published between 2012 and the search date.
Electronic searches
-
Cochrane Central Register of Controlled Trials (CENTRAL) 2015, Issue 4, part of The Cochrane Library. www.cochranelibrary.com, (including Cochrane Effective Practice and Organisation of Care (EPOC) Specialised Register)
-
MEDLINE In‐Process and Other Non‐Indexed Citations and Ovid MEDLINE 1946 to present, OvidSP
-
EMBASE 1996 to 2015 Week 19, OvidSP
-
CINAHL (Cumulative Index to Nursing and Allied Health Literature), 1981 to present, EbscoHost
Search strategies were comprised of keywords and, when available, controlled vocabulary such as MeSH (Medical Subject Headings). We applied no language restrictions. See Appendix 1 for strategies used in this update.
Searching other resources
We searched the following trial registries for relevant studies on 18 May 2015:
-
International Clinical Trials Registry Platform (ICTRP), World Health Organization (WHO) http://www.who.int/ictrp/en/
-
ClinicalTrials.gov, US National Institutes of Health (NIH) http://clinicaltrials.gov/
For search terms used in this update and number of results, see Appendix 2
We also contacted authors of relevant studies to clarify reported published information.
Data collection and analysis
Selection of studies
Two review authors (DPA and MCK) independently screened titles and abstracts to decide which studies met the inclusion criteria. Any papers not meeting the inclusion criteria were excluded at this stage. If there was uncertainty or disagreement, consensus was reached by discussion with co‐review authors. Two review authors (DPA and MCK) independently assessed the full text articles to ensure they still met the inclusion criteria. Full text articles not published in English were translated prior to being assessed for inclusion.
Data extraction and management
Two review authors (DPA and MCK) independently extracted details of articles included in the review, including the study design, the study population, the intervention, usual care, outcome measures used and length of follow‐up data, using a specially designed data extraction form based on the EPOC template (EPOC 2013). Where necessary, we contacted authors for missing information or clarification. We intended to use information from the data extraction forms to guide extraction of numerical data for meta‐analysis in Review Manager (RevMan) 5.3 (RevMan 2014).
Assessment of risk of bias in included studies
Two review authors (DPA and MCK) assessed the internal validity of each included study. We used the Cochrane Collaboration’s tool for assessing risk of bias (Higgins 2011) based on six standard criteria: adequate sequence generation; concealment of allocation; blinded or objective assessment of primary outcome(s); adequately addressed incomplete outcome data; freedom from selective reporting; freedom from other risk of bias. We used four additional criteria specified by EPOC (EPOC 2015): similar baseline outcome measurements; similar baseline characteristics; reliable primary outcome measures; and adequate protection against contamination. We made judgements as to whether studies were at low risk, high risk or unclear risk of bias and reported all included studies in the Cochrane ‘Risk of bias’ tables.
Measures of treatment effect
We initially planned to conduct a meta‐analysis, however, this was not possible due to heterogeneity (see Results). Therefore, we presented a narrative summary of the results. Wherever possible, we presented results with 95% confidence intervals.
Unit of analysis issues
We critically examined the methods of analysis of all study types. We identified cluster‐RCTs with unit of analysis errors (for example, randomisation by care home with analysis by residents without adjustments for clustering) and where appropriate, commented on unit of analysis errors in the results and discussion.
Dealing with missing data
We intended to exclude studies from a meta‐analysis if there was differential loss to follow‐up between groups, greater than 20%. However, as meta‐analysis was not appropriate, this did not apply.
Assessment of heterogeneity
See Data synthesis section.
Assessment of reporting biases
We intended to examine funnel plots corresponding to meta‐analysis of the primary outcome in order to assess the potential for small study effects such as publication bias. However, this was not possible as meta‐analysis was not undertaken.
Data synthesis
We intended to synthesise the results of the studies depending on their quality, design and heterogeneity, and we intended to pool the results of studies if at least two studies were homogeneous regarding the participants, interventions and outcomes. As stated above, this was not possible and, therefore, we presented a narrative summary. We described studies according to setting, type of intervention and study design together with an assessment of the evidence on the theoretical basis for each of the approaches described.
Certainty of the evidence
We assessed the certainty of the evidence for the main comparison using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) criteria (GRADE 2012) and presented our judgements in a 'Summary of findings' table. We downgraded the quality of the evidence when there were concerns about the design, risk of bias, inconsistency, indirectness and/or imprecision. One author (DPA) made the judgements informed by the previous version of the review (Alldred 2013) and this was agreed by a second author (MCK).
Subgroup analysis and investigation of heterogeneity
We intended to conduct subgroup analyses for professional and organisational interventions where possible. If we had found that one type of intervention was common, for example medication review, we intended to analyse this separately. If possible, we also planned to undertake subgroup meta‐analyses based on the specific nature of the intervention, for example pharmacist‐led medication review. However, subgroup analyses were not possible due to heterogeneity.
See Data synthesis section for the investigation of heterogeneity.
Sensitivity analysis
We intended to perform sensitivity analysis for pooled results based on the risk of bias. However, as we could not pool results this did not apply.
Results
Description of studies
We included 12 studies evaluating the effectiveness of interventions to optimise overall prescribing for older people living in care homes. See: Characteristics of included studies.
Results of the search
The searches identified 1469 articles for potential inclusion. Following independent screening of titles and abstracts by DPA and MCK, nine full‐text articles were assessed for eligibility and four new studies (Frankenthal 2014; Garcia‐Gollarte 2014; Pitkala 2014; Connolly 2015) met the inclusion criteria . Three studies are ongoing (Desborough ongoing; NCT02238652; Wouters ongoing) and two were excluded (Lapane 2011; Milos 2013). See PRISMA flowchart Figure 1 for details (Liberati 2009). The search yielded five related systematic reviews (Kaur 2009; Ostini 2009; Verrue 2009; LaMantia 2010; Loganathan 2011) and one narrative review (Markum 2010) and their references were reviewed along with the references from the included studies; we did not identify any further studies from these.
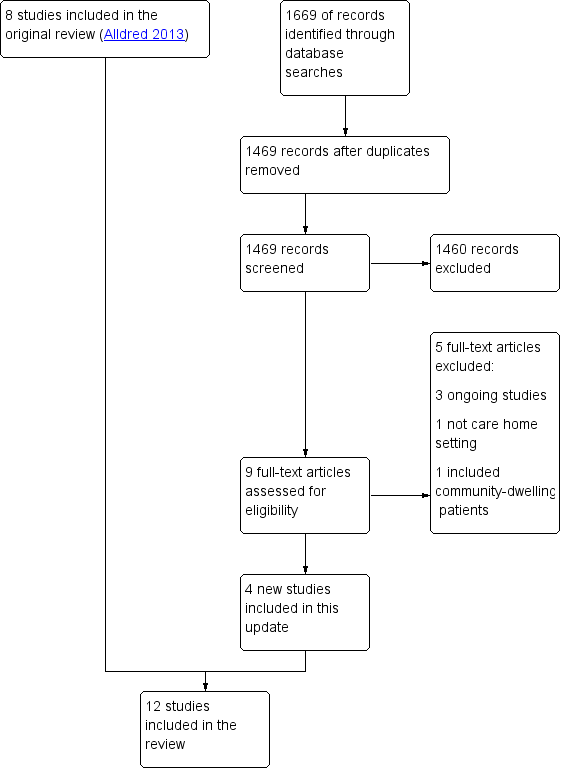
Study flow diagram.
Included studies
The 12 included studies involved 10,953 residents in 355 (range 1 to 85) care homes. Three studies were conducted in Australia (Roberts 2001; Crotty 2004a; Crotty 2004b), two in the UK (Furniss 2000; Zermansky 2006), one in Sweden (Claesson 1998), one in the Netherlands (Strikwerda 1994), one in the USA and Canada (Gurwitz 2008), one in New Zealand (Connolly 2015), one in Israel (Frankenthal 2014), one in Spain (Garcia‐Gollarte 2014) and one in Finland (Pitkala 2014).
Design
Nine studies were cluster‐RCTs (Strikwerda 1994; Claesson 1998; Furniss 2000; Roberts 2001; Crotty 2004a; Gurwitz 2008; Garcia‐Gollarte 2014; Pitkala 2014; Connolly 2015) and three studies were patient‐RCTs (Crotty 2004b; Zermansky 2006; Frankenthal 2014). Two cluster‐RCTs appeared to have made unit of analysis errors in that they did not account for the effect of clustering (Garcia‐Gollarte 2014; Pitkala 2014) and therefore, P values and 95% CIs from these two studies may be over precise.There was a wide range of study duration and follow‐up between the studies, ranging from six weeks to two years (see Table 1).
| Study,Country, Design | Participants | Intervention | Outcome measures | Duration |
| Sweden Cluster‐RCT | 1854 residents in 33 nursing homes | Multidisciplinary meetings with physician, pharmacist and nurse(s) | Medication‐related problems | 14 months |
| Australia Cluster‐RCT | 1998 residents in 36 nursing homes | Multidisciplinary meetings with study geriatrician, a GP, a pharmacist and a nurse manager. Education of nurses and care‐givers | Hospital admissions Mortality | 14 months |
| Australia Cluster‐RCT | 154 residents in 10 nursing homes | Multidisciplinary case conferencing with GP, a geriatrician, a pharmacist, residential care staff and an Alzheimer's Association representative | Medication Appropriateness Index | 3 months |
| Australia Patient‐RCT | 110 patients discharged to 85 long‐term care facilities | Pharmacist transition co‐ordinator. Transfer of medicines information to nursing staff, family physician and community pharmacist plus medication review and case conferencing | Adverse drug events Hospital admissions Medication‐related problems Medication Appropriateness Index | 8 weeks |
| Israel Patient‐RCT | 359 residents in 1 chronic care geriatric facility | Medication review by the study pharmacist | Hospital admissions Mortality Quality of life Medication appropriateness (STOPP‐START) Medication‐related problems Medicine costs | 12 months |
| UK Cluster‐RCT | 330 residents in 14 nursing homes | Medication review by a single pharmacist | Hospital admissions Mortality Medication‐related problems Medicine costs | 8 months |
| Spain Cluster‐RCT | 716 residents in 36 nursing homes | Physician educational programme followed by on‐demand support (prescription advice) by phone | Hospital admissions (total number of days spent in hospital) Medication appropriateness (STOPP‐START) | 6 months |
| USA/Canada Cluster‐RCT | 1118 residents in 29 units in 2 long‐term care facilities | Computerised provider order entry with clinical decision support | Adverse drug events | 12 months |
| Finland Cluster‐RCT | 227 residents in 20 assisted living facilities | Nurse training and education | Hospital admissions Mortality Health‐related Quality of Life Medication appropriateness (Beer's criteria plus others) | 12 months |
| Australia Cluster‐RCT | 3230 residents in 52 nursing homes | Introduction of new professional role, nurse education and medication review by pharmacists | Hospital admissions Mortality Medication‐related problems Medicine costs | 24 months |
| Netherlands Cluster‐RCT | 196 residents in 1 nursing home | Feedback on GP prescribing from community pharmacist | Medication‐related problems | 6 weeks |
| UK Patient‐RCT | 661 residents in 65 care homes | Medication review by a single pharmacist | Hospital admissions Mortality Medication‐related problems Medicine costs | 6 months |
Participants
All studies involved older people living in care homes (long‐term care facilities). Mean age ranged from 81.2 years (Furniss 2000) to 87.2 years (Gurwitz 2008) and the majority of residents were female (range 59.7% (Crotty 2004a) to 77% (Zermansky 2006)). The study by Roberts 2001 did not report mean age or gender.
Strikwerda 1994 studied 196 residents in one nursing home, Claesson 1998 studied 1854 residents in 33 nursing homes, Crotty 2004a studied 154 residents in 10 high‐level residential facilities, Crotty 2004b studied 110 residents in 85 long‐term care facilities, Furniss 2000 studied 330 residents in 14 nursing homes, Gurwitz 2008 studied 1118 residents in 29 units in two long‐term care facilities, Roberts 2001 studied 3230 residents in 52 nursing homes, Zermansky 2006 studied 661 residents in 65 nursing and residential homes for older people, Frankenthal 2014 studied 359 residents in one chronic care geriatric facility, Garcia‐Gollarte 2014 studied 716 residents in 36 nursing homes, Pitkala 2014 studied 227 residents in 20 assisted living facilities and Connolly 2015 studied 1998 residents in 36 residential aged care facilities.
Interventions
The interventions evaluated were diverse and often multifaceted. Medication review (conducted by various methods) was a component of ten studies (Strikwerda 1994; Claesson 1998; Furniss 2000; Roberts 2001; Crotty 2004a; Crotty 2004b; Zermansky 2006; Frankenthal 2014; Garcia‐Gollarte 2014; Connolly 2015). Four studies involved multidisciplinary case‐conferencing (Claesson 1998; Crotty 2004a; Crotty 2004b; Connolly 2015) and five studies involved an educational element for care home staff (Roberts 2001; Crotty 2004a; Garcia‐Gollarte 2014; Pitkala 2014; Connolly 2015). One study evaluated the use of clinical decision support technology (Gurwitz 2008). Other components of interventions included introducing a new professional role to stakeholders (Roberts 2001) and the transfer of medicines information (Crotty 2004b). Further descriptions of interventions are presented below.
Strikwerda 1994 evaluated the effect of community pharmacist feedback to GPs on their patients' prescriptions over a four‐week period.
Claesson 1998 evaluated the effectiveness of monthly multidisciplinary team meetings between the physician, pharmacist and nurse(s) over 12 months. The aim of the meetings was to discuss and improve the use of drugs. Pharmacists received a total of 65.5 hours of education and training prior to and during the intervention period.
Furniss 2000 investigated the effectiveness of pharmacist‐conducted medication review (in addition to usual care by the GP) versus usual care by the GP. The intervention was a single medication review conducted by one pharmacist with access to medical and nursing home records. No details were provided on the education and training of the pharmacist.
The intervention evaluated by Roberts 2001 had three components: (i) introducing a new professional role and relationship‐building; (ii) nurse education; (iii) medication review by pharmacists holding a postgraduate diploma in clinical pharmacy. Medication reviews were undertaken for a non‐random subsample of 500 residents (total intervention residents 905) selected by nursing staff. Most of the contact between pharmacists and GPs was indirect.
Crotty 2004a evaluated the effectiveness of an 'outreach medication advisory service'. This involved a medication review prepared by the pharmacist, followed by two multidisciplinary case conferences held six to 12 weeks apart (with the GP, geriatrician, pharmacist, care staff and an Alzheimer’s Association of South Australia representative). No details were provided on the education and training of the pharmacist.
Crotty 2004b investigated the effectiveness of a pharmacist transition co‐ordinator for residents who were being discharged from hospital to a long‐term care facility. The intervention focused on the transfer of medicines information to the nursing home staff, GP and the community pharmacist. Following this, a medication review was conducted by the community pharmacist contracted to the care home. In addition, the transition pharmacist co‐ordinated a multidisciplinary case conference 14 to 28 days after transfer involving him or herself, the GP, community pharmacist and a nurse.
Zermansky 2006 evaluated the effectiveness of a clinical medication review (in addition to usual care by the GP) undertaken by a pharmacist who held a post‐graduate clinical pharmacy qualification versus usual care by the GP. The pharmacist reviewed the medicines with the medical and care home records in conjunction with a consultation with the resident (if possible) and a nurse or carer.
The intervention investigated by Gurwitz 2008 was a clinical decision support system in facilities that had computerised provider order entry systems. The clinical decision support system was designed based on previous research on preventable adverse drug events, criteria for suboptimal prescribing in older people and drug‐drug interactions. Warning messages were displayed to prescribers in a pop‐up box in real time when medicines were entered into the computer provider order entry system. Prescribers were free to either act on alerts or ignore them.
Frankenthal 2014 investigated pharmacist‐led medication review using the Screening Tool of Older Persons’ potentially inappropriate Prescriptions (STOPP) and Screening Tool to Alert doctors to Right Treatment (START) criteria (Gallagher 2008) to identify potentially inappropriate prescriptions and potential prescription omissions. The chief physician decided whether to accept these recommendations and implemented changes.
Garcia‐Gollarte 2014 evaluated a structured educational intervention for nursing home physicians. This involved education delivered by an expert nursing home physician on drug use in older patients, medication review and adverse drug reactions. In addition, on‐demand prescribing advice was provided to physicians and educational material provided to participants.
Pitkala 2014 investigated educational information for nurses to recognise harmful medicines and adverse drug events. The nurses were then asked to identify medication‐related problems and highlight these to the physician. In addition, two‐thirds of the physicians received the training.
Connolly 2015 evaluated a multifaceted complex intervention involving: baseline facility assessment and care planning; monitoring and benchmarking of quality‐of‐care indicators; multidisciplinary team meetings including medication review (only 23% of the intervention group received medication review) by geriatrician, nurse specialist, GP, pharmacist and nurse manager; education and clinical coaching for nursing staff and caregivers.
Outcomes
Outcomes were diverse with differing definitions, methods of data collection, varying time points and different reporting methods. Studies reported measures other than those specified for this review and these are listed in the Characteristics of included studies tables.
Primary outcome measures
Adverse drug events
Only two studies specified adverse drug events as an outcome measure (Crotty 2004b; Gurwitz 2008). However, Crotty 2004b did not define adverse drug events. Adverse drug events were the primary outcome measure in the Gurwitz 2008 study and were defined as 'an injury resulting from the use of a drug'; such adverse drug events may have resulted from medication errors or from adverse drug reactions in which there was no error.
Hospital admissions
Eight studies included hospital admissions as an outcome measure (Furniss 2000; Roberts 2001; Crotty 2004b; Zermansky 2006; Frankenthal 2014; Garcia‐Gollarte 2014; Pitkala 2014; Connolly 2015). Furniss 2000 reported hospital admissions as the number of inpatient days. Roberts 2001 reported the proportion of residents hospitalised and Zermansky 2006 reported the mean number of non‐elective hospitalisations per resident. Crotty 2004b grouped together emergency department visits and hospital readmissions. Frankenthal 2014 reported hospital admissions (not defined). Garcia‐Gollarte 2014 reported the total number of days spent in hospital. Pitkala 2014 reported hospital days/per person/per year. Connolly 2015 reported ambulatory sensitive hospitalisations and all acute admissions.
Mortality
Six studies included mortality as an outcome measure (Furniss 2000; Roberts 2001; Zermansky 2006; Frankenthal 2014; Pitkala 2014; Connolly 2015). Furniss 2000 and Zermansky 2006 reported mortality as the number of deaths over eight and six months, respectively. Roberts 2001 reported the proportion of residents who had died over 12 months together with cumulative survival. Frankenthal 2014 reported the number of deaths over 12 months. Pitkala 2014 calculated hazard ratios (HR) using the Cox proportional hazard model. Connolly 2015 calculated the relative risk (RR) of death over the 14 month follow up period.
Secondary outcome measures
Quality of life
Two studies measured quality of life (Frankenthal 2014; Pitkala 2014). Pitkala 2014 used the 15 dimensional instrument of health‐related quality of life (15D) and Frankenthal 2014 used the Medical Outcomes Study 12‐item Short‐form Health survey (SF‐12).
Medication‐related problems
Medication‐related problems from the intervention arms were measured and classified in diverse ways in seven studies. Strikwerda 1994 reported the number of pharmacists' recommendations and described their type. Claesson 1998 described the type and frequency of drug‐related problems along with pharmacists' recommendations. Furniss 2000 measured the number of pharmacist's recommendations, accepted recommendations by the GP, and the number of treatment changes. Reasons were provided for the pharmacist's recommendations. Roberts 2001 measured the number of medicine changes likely to be due to medication review. Crotty 2004b identified medication‐related problems and classified them into categories. Zermansky 2006 measured the number of changes in medication per participant as the primary outcome; pharmacist's recommendations were identified, collated and classified along with GPs' acceptance of the recommendations. Frankenthal 2014 reported the number of recommendations based on the STOPP‐START criteria along with the proportion of recommendations accepted by the physician.
Medication appropriateness
Five studies assessed medication appropriateness using a validated tool (Crotty 2004a; Crotty 2004b; Frankenthal 2014; Garcia‐Gollarte 2014; Pitkala 2014). Crotty 2004a and Crotty 2004b used the Medication Appropriateness Index (MAI) (Hanlon 1992). Frankenthal 2014 and Garcia‐Gollarte 2014 used STOPP‐START (Gallagher 2008). Pitkala 2014 used a composite of Beers criteria, Anticholinergic Risk Scale, > 2 psychotropic medications, nonsteroidal anti‐inflammatory drugs (NSAIDs) and proton pump inhibitors.
Medicine costs
Five studies calculated medicine costs (Furniss 2000; Roberts 2001; Crotty 2004a; Zermansky 2006; Frankenthal 2014). Furniss 2000 calculated drug costs per resident throughout the observation and intervention phases of the study. Roberts 2001 collected yearly drug costs from prescription claims data based on the Australian Pharmaceutical Benefits Scheme. Crotty 2004a calculated monthly drug costs for all regular medicines based on the Australian Pharmaceutical Benefits Scheme. Zermansky 2006 calculated the 28‐day net ingredient cost of repeat medicines per resident. Frankenthal 2014 calculated medication costs per month.
Excluded studies
We excluded four studies (Avorn 1992; Crotty 2004c; Lapane 2011; Milos 2013) and we report reasons for their exclusion in the Characteristics of excluded studies section.
Risk of bias in included studies
Studies were heterogeneous with regard to risk of bias (see Figure 2; Figure 3). Risk of bias is summarised below for each domain.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
We judged nine studies to have a low risk of bias based on random sequence generation (Furniss 2000; Roberts 2001; Crotty 2004a; Crotty 2004b; Zermansky 2006; Gurwitz 2008; Garcia‐Gollarte 2014; Pitkala 2014; Connolly 2015;). The studies by Strikwerda 1994, Claesson 1998 and Frankenthal 2014 did not report how the sequence was generated. Seven studies utilised computer‐generated random or pseudo‐random numbers (Furniss 2000; Crotty 2004a; Crotty 2004b; Zermansky 2006; Gurwitz 2008; Pitkala 2014; Connolly 2015;), Roberts 2001 drew from a hat and Garcia‐Gollarte 2014 used random number tables. Allocation was adequately concealed via centralisation in two of the patient‐RCTs (Crotty 2004b; Zermansky 2006),the study by Frankenthal 2014 did not report sufficient information on allocation concealment to permit judgement. Due to the remaining nine studies having a cluster design, we deemed them to be at low risk of bias with regard to allocation concealment (Strikwerda 1994; Claesson 1998; Furniss 2000; Roberts 2001; Crotty 2004a; Gurwitz 2008; Garcia‐Gollarte 2014; Pitkala 2014; Connolly 2015).
Blinding
Due to the nature of the interventions it was not possible to blind participants and personnel in any of the studies and, therefore, we judged performance bias to be high for each study. Three studies blinded outcome assessment for subjective outcomes (Crotty 2004a; Crotty 2004b; Gurwitz 2008) and, therefore, we judged detection bias to be low for these studies. The studies by Strikwerda 1994, Pitkala 2014 and Garcia‐Gollarte 2014 did not report if subjective outcomes were blinded and therefore, the risk was unclear, while the studies by Claesson 1998; Furniss 2000; Roberts 2001; Zermansky 2006; and Frankenthal 2014 we deemed to be high risk. We deemed detection bias to be low for objective outcomes for studies that reported them.
Incomplete outcome data
We judged five studies to be at low risk of attrition bias as they reported similar baseline characteristics with a similar number of dropouts for similar reasons (Crotty 2004a; Crotty 2004b; Zermansky 2006; Frankenthal 2014; Connolly 2015). The only outcome in the Claesson 1998 study was a description of medicine‐related problems in the intervention group and attrition bias was not relevant. We judged the risk of attrition bias to be unclear for six studies due to a lack of information (Strikwerda 1994; Furniss 2000; Roberts 2001; Gurwitz 2008; Garcia‐Gollarte 2014; Pitkala 2014).
Selective reporting
Although there was no evidence of selective reporting in the studies, that is, all outcome measures stated in the methods were reported, research protocols were not available for all but one study (Connolly 2015) and, therefore, we deemed that there was insufficient information to permit judgement for 11 out of the 12 studies. The protocol for Connolly 2015 indicated that the pre‐specified outcomes were reported in the pre‐specified way and, therefore, we judged this to be low risk of bias.
Other potential sources of bias
Similar baseline outcome measurements
We deemed six studies (Roberts 2001; Crotty 2004b; Zermansky 2006; Frankenthal 2014; Garcia‐Gollarte 2014; Connolly 2015) to be at low risk of bias as baseline outcome measurements were similar. We judged Furniss 2000 to be at high risk of bias because there were fewer deaths in the control group compared with the intervention group. We also judged Crotty 2004a to be at a high risk of bias because of baseline differences in the Medication Appropriateness Index. We deemed the study by Pitkala 2014 to be at unclear risk of bias because of baseline outcome measurement differences in health‐related quality of life and the number of harmful medicines; however, these differences were adjusted for in the analysis. We deemed the three remaining studies to be at an unclear risk of bias as outcomes were not measured at baseline (Strikwerda 1994; Claesson 1998; Gurwitz 2008).
Similar baseline characteristics
Eight studies reported similar baseline characteristics and we therefore judged them to be at low risk of bias (Claesson 1998; Roberts 2001; Crotty 2004a; Crotty 2004b; Zermansky 2006; Frankenthal 2014; Garcia‐Gollarte 2014; Connolly 2015). The study by Strikwerda 1994 reported fewer males in group A and fewer medicines in group B compared to group C and we judged this to be at high risk. We deemed the study by Furniss 2000 to be at high risk because in the control group the residents were younger and there were fewer females. We deemed Gurwitz 2008 to be at unclear risk because baseline characteristics of residents were not reported (although units were matched for general characteristics, bed size and general characteristics of residents). We also deemed the study by Pitkala 2014 to be at unclear risk because there was a higher proportion of males, a higher prevalence of 'as‐needed' medications and a higher number of co‐morbidities in the intervention group; however, these differences were adjusted for in the analysis.
Reliable primary outcome measure
We deemed all twelve studies to have reliable primary outcome measures (although not all the outcome measures were included in this review).
Adequate protection against contamination
We assessed five studies that were of a cluster design to be at an unclear risk of adequate protection against contamination because although they were randomised by care home it was unclear whether the healthcare professionals may have moved between intervention and control homes (Claesson 1998; Roberts 2001; Garcia‐Gollarte 2014; Pitkala 2014; Connolly 2015). We deemed the study by Crotty 2004a to be at low risk of contamination because in addition to the cluster design the GPs were checked to avoid contamination between intervention and control residents. We judged the study by Strikwerda 1994 to be at high risk because although residents were randomised by GP they all resided in the same nursing home. Furniss 2000 randomised care homes in different geographical areas and we therefore deemed at low risk of contamination. Gurwitz 2008 attempted to limit the crossover of prescribers between intervention and control units, however some prescribers worked simultaneously on both units and consequently we judged the trial to be at high risk of contamination. We deemed the three studies that were patient‐RCTs to be at high risk as contamination was possible (Crotty 2004b; Zermansky 2006; Frankenthal 2014).
Other bias
The medications reviews undertaken by Roberts 2001 and Connolly 2015 were completed for a non‐random subset of intervention residents; we determined this to have a high risk of bias. Garcia‐Gollarte 2014 measured medication appropriateness for a random subsample of residents, therefore the risk of bias in this study was judged to be unclear.
Effects of interventions
See: Summary of findings for the main comparison
See summary of findings Table for the main comparison for the main comparison.
Due to the heterogeneity in interventions, outcomes and risk of bias, it was deemed inappropriate to conduct a meta‐analysis. The effectiveness of the interventions are described below.
Primary outcome measures
Adverse drug events
Crotty 2004b found no evidence of an effect of a pharmacist transition co‐ordinator on adverse drug events (relative risk 1.05, 95% CI 0.66 to 1.68). Gurwitz 2008 tested a clinical decision support system and found no evidence of an effect on all adverse drug events (adjusted rate ratio 1.06, 95% CI 0.92 to 1.23) or preventable adverse drug events (adjusted rate ratio 1.02, 95% CI 0.81 to 1.30).
Hospital admissions
Furniss 2000 found fewer inpatient days per resident in the intervention group compared with the control group during the four‐month intervention phase of the study (0.55 versus 1.26); however, small numbers precluded statistical analysis. In the Roberts 2001 study, no difference was found in the mean proportion of residents hospitalised between the intervention and control groups. Crotty 2004b demonstrated a reduction in the combination of emergency room visits and hospital readmissions with a relative risk ratio of 0.38 (95% CI 0.15 to 0.99) when analysing residents who were alive at follow‐up. When residents who had died were included, there was no evidence of an effect on hospital admissions (relative risk 0.58, 95% CI 0.28 to 1.21). Zermansky 2006 showed no evidence of an effect on the mean number of hospitalisations per resident (relative risk 0.75, 95% CI 0.52 to 1.07). Frankenthal 2014 showed no evidence of an effect on the average number of hospitalisations (intervention 0.5 ± 1.0 vs 0.5 ± 0.9 control, P = 0.10). The study by Garcia‐Gollarte 2014 found a small increase in days in hospital in the control group (+ 0.38 days, P = 0.011) but no difference in the intervention group (+ 0.01 days, P = 0.822). Pitkala 2014 found that residents in the intervention group used fewer hospital days (1.4/person/year, 95% CI 1.2 to 1.6) than control residents (2.3/person/year, 95% CI 2.1 to 2.7) (adjusted RR 0.60, 95% CI 0.49 to 0.75). It is important to note that Garcia‐Gollarte 2014 and Pitkala 2014 committed unit of analysis errors and therefore, P‐values and 95% CIs may be over precise. Connolly 2015 showed no difference in ambulatory sensitive hospitalisations (RR 1.07, 95% CI 0.85 to 1.36) or total acute admissions (RR 1.02, 95% CI 0.83 to 1.26).
Mortality
Furniss 2000 found fewer deaths in the intervention group compared with the control group during the intervention phase of the study (4 versus 14, P = 0.028); however when the observation phase of the study was taken into account, the number of deaths in the control and intervention groups were 28 and 26 (P value not reported), respectively. In the Roberts 2001 study, no difference was found in the mean proportion of residents who had died between the intervention and control groups. A survival analysis found a hazard ratio of 0.85 (95% CI 0.68 to 1.06). Zermansky 2006 showed no evidence of an effect on the number of deaths (relative risk 1.06, 95% CI 0.70 to 1.64). Frankenthal 2014 reported that 15/183 (8.2%) and 17/176 (9.7%) residents died in the intervention and control groups respectively. However, this was not formally analysed as an outcome measure. Pitkala 2014 found no difference in mortality between the intervention and control groups (adjusted HR 1.04, 95% CI 0.79 to 1.36; it should be noted that the 95% CI may be over precise due to unit of analysis error). Connolly 2015 showed no evidence of an effect on mortality (RR 1.11, 95% CI 0.76 to 1.61).
Secondary outcome measures
Quality of life
Frankenthal 2014 found no difference between groups in the physical (P = 0.09) and mental (P = 0.70) components of SF‐12. Pitkala 2014 found that health‐related quality of life declined more slowly in intervention residents (‐0.038, 95% CI –0.054 to ‐0.022) than control residents (‐0.072, 95% CI ‐0.089 to ‐0.055). However, unit of analysis error was identified for this study and therefore, the confidence intervals may be over precise. Breathing, sleeping and speech were the dimensions of 15D that showed differences in favour of the intervention.
Medication‐related problems
Strikwerda 1994 reported that 122 potential medication‐related problems were identified in 61 residents. As a result, nine medicines were discontinued and four medicines had a dose reduction. The most common medication‐related problem was a potential interaction (51, 42%), followed by dose (31, 25%), indication (23, 19%) and duration of the prescription (17, 14%).
Claesson 1998 identified 819 drug‐related problems in 395 residents (2.1 per resident). The most common problem was 'choice of drug' (348, 43%), with the majority of these being inappropriate according to Swedish Medical Product Agency guidelines. Two hundred and seventy‐six (34%) problems were due to 'unclear indication' whereby the team did not know why a drug had been prescribed or the drug had not been adequately re‐evaluated. Ninety per cent (737) of the problems discussed were acted upon, with 368 (45%) resulting in stopping the medicine and 162 (20%) led to a change of medicine. This study evaluated 532 medicine changes with 404 (76%) still in place after a month, 59 (11%) discontinued and previous therapy was restored, and 69 (13%) were difficult to evaluate as partial changes had occurred.
Furniss 2000 made 261 recommendations of which 239 (92%) were accepted by the GP. This resulted in 144 actual treatment changes. Thirty residents did not require a change in therapy, and the mean number of recommendations per resident (for those who needed at least one recommendation) was 2.46 (range 0 to 7). The most common reasons for recommendations were 'indication for the medication no longer present' (85, 33%) and 'safer or more efficacious use of drug' (77, 30%).
Roberts 2001 followed up 137 of the 500 medication reviews conducted and found that 54 (39%) of the residents had changes likely to be due to the review. No further information was provided.
Crotty 2004b identified medicine‐related problems at admission to the long‐term care facility for intervention and control residents. The most common issue classified as a medicine‐related problem by the authors was that a resident had been appointed a new physician. The next most common problems identified were: discrepancy between medication discharge summary and medication (32, 57% intervention; 26, 48% control); precaution with use (18, 32% intervention; 14, 26% control); no indication for medication (18, 32% intervention; 8, 15% control).
In the study by Zermansky 2006, at least one recommendation was made in 256 (77%, 95% CI 73.1 to 81.7) residents, with a mean of 2.3 recommendations per resident. The study made 672 medication‐related recommendations, along with an additional 75 recommendations related to the residents' conditions. The most common recommendation was technical (for example generic switching, amending quantities, removing discontinued items from the repeat prescription) with 225 (30%) recommendations. Following technical reasons, the most common recommendations were to conduct a test to monitor therapy (161, 22%) and to stop a medicine (100, 13%). The GP accepted 565 (76%) of the pharmacist's recommendations and rejected 52 (7%); there was no response to the review or the resident died before the review could be actioned in the remaining cases. The GP actioned 433 (77%) of the accepted recommendations.
Frankenthal 2014 made 327 recommendations in total including 245 in 129 residents based on STOPP and 82 in 65 residents based on START. 82.4% of STOPP recommendations and 92.6% of START recommendations were accepted by the physician.
Medication appropriateness
Crotty 2004a found that, based on the Medication Appropriateness Index (MAI), medication appropriateness improved in the intervention group (MAI mean change 4.1, 95% CI 2.1 to 6.1) compared with the control group (MAI mean change 0.4, 95% CI ‐0.4 to 1.2). MAI scores were higher at baseline for intervention group residents compared with control residents (mean MAI 7.4, 95% CI 4.5 to 10.3 versus 4.1, 95% CI 2.4 to 5.7). There were no baseline differences in mean MAI scores between the control (3.7, 95% CI 2.2 to 5.2) and intervention groups (3.2, 95% CI 1.8 to 4.6) in the Crotty 2004b study. Following the intervention, there was no change in MAI in the intervention group (2.5, 95% CI 1.4 to 3.7) whereas the MAI in the control group had worsened (6.5, 95% CI 3.9 to 9.1). The effect of the intervention on MAI scores remained when controlled for baseline MAI, Charlson Comorbidity Index and the number of drugs discontinued during hospital admission.
Based on STOPP‐START criteria at six months' follow‐up, Frankenthal 2014 found a reduction in potentially inappropriate prescriptions (37.4% intervention vs 56% control, P < 0.01) and potential prescribing omissions (9.2% intervention vs 25.2% control, P < 0.01) in intervention residents at six months' follow‐up and this was sustained at 12 months.
Garcia‐Gollarte 2014 evaluated medication appropriateness using STOPP‐START criteria in a random subsample of 411 residents (200 control, 211 intervention). At follow‐up, the mean number of inappropriate drugs was lower in the intervention group than the control group (0.81 ± 1.13 vs 1.29 ± 1.56) with a decrease from baseline in the intervention group (P < 0.01) and an increase from the baseline in the control group (P < 0.01). The proportion of participants without potentially inappropriate prescriptions increased in the intervention group (33.2% at baseline vs 56.4% at follow‐up), as opposed to the control group where there was no change (37.6% at baseline vs 38.7% at follow up). Potential prescribing omissions decreased in the intervention group (0.91 ± 1.19 at baseline vs 0.13 ± 0.44 at follow up) whereas there was no change in the control group. As noted for this study previously, Garcia‐Gollarte 2014 appeared to commit a unit of analysis error and therefore, P values and confidence intervals may be over precise.
Pitkala 2014 found no change in the prevalence of harmful medication use in control residents (3.4%, 95% CI ‐3.7 to 10.6) at follow‐up, however there was a decrease in the intervention group (‐11.7, 95% CI ‐20.5 to ‐2.9). Similarly, there was a decrease in the mean number of harmful medicines in intervention residents (‐0.43, 95% CI ‐0.15 to ‐0.71) but no corresponding change in control residents (0.11, 95% CI ‐0.09 to 0.31). It should again be noted that unit of analysis error was identified in this study and therefore, confidence intervals may be over precise.
Medicine costs
The cost of medicines per resident in the observation phase of Furniss 2000 was GB Pounds (GBP) 142.53 in the control group and GBP 159.01 in the intervention group. Following the intervention phase, costs were GBP 141.24 in the control group versus GBP 131.54 in the intervention group, representing a reduction in medicine costs of GBP 27.47 per resident over a four‐month period. Accounting for the pharmacist’s time, the cost saving on medicines in the intervention group was calculated to be GBP 22 per resident. Roberts 2001 calculated a drug cost saving of Australian Dollars (AUD) 64 per resident per year in the intervention group compared to the control group. When the cost of the intervention was accounted for, the net cost saving was AUD 16 per resident per year. Crotty 2004a found no difference in mean medicine costs per month per resident between the intervention and control groups (mean change AUD 5.72 intervention vs AUD 3.37 control, P = 0.837). Zermansky 2006 reported little difference on the cost of 28 days' repeat medicines per resident (mean difference GBP ‐0.70, 95% CI GBP ‐7.28 to GBP 5.71). Frankenthal 2014 demonstrated a reduction in the average monthly medication costs in the intervention group at follow‐up compared to baseline (382.7 ± 279.3 at baseline vs 279 ± 171.9 at follow‐up, Israeli New Shekel (ILS), P < 0.01), with a difference between the intervention group and control group at follow up (279 ± 171.9 vs 402.3 ± 291.2, ILS, P < 0.01).
Certainty of the evidence
The overall quality/certainty of the evidence for the outcomes reported was judged to be low or very low, see: summary of findings Table for the main comparison. The evidence was downgraded from high to low for adverse drug events (Crotty 2004b; Gurwitz 2008) due to a serious risk of bias and imprecision. The evidence was downgraded from high to low for hospital admissions (Furniss 2000; Roberts 2001; Crotty 2004b; Zermansky 2006; Frankenthal 2014; Garcia‐Gollarte 2014; Pitkala 2014; Connolly 2015), mortality (Furniss 2000; Roberts 2001; Zermansky 2006; Frankenthal 2014; Pitkala 2014; Connolly 2015), quality of life (Frankenthal 2014; Pitkala 2014) and medication appropriateness (Crotty 2004a; Crotty 2004b; Frankenthal 2014; Garcia‐Gollarte 2014; Pitkala 2014) due to a serious risk of bias and inconsistency. The evidence for medicines costs (Furniss 2000; Roberts 2001; Crotty 2004a; Zermansky 2006; Frankenthal 2014 was downgraded from high to very low due to a serious risk of bias, inconsistency and imprecision. The evidence for medicine‐related problems (Strikwerda 1994; Claesson 1998; Furniss 2000; Roberts 2001; Crotty 2004b; Zermansky 2006; Frankenthal 2014 was reduced from high to low due to design, risk of bias and imprecision.
Discussion
Summary of main results
12 studies were included in the review and three ongoing studies. The primary outcomes of the review were adverse drug events, mortality and hospital admissions.There was no evidence of an effect of the interventions on adverse drug events (Crotty 2004b; Gurwitz 2008) and mortality (Furniss 2000; Roberts 2001; Zermansky 2006; Frankenthal 2014; Pitkala 2014; Connolly 2015). There was evidence from one study that the intervention led to fewer days in hospital (Pitkala 2014); however, there was no evidence of an effect in the remaining studies (Furniss 2000; Roberts 2001; Crotty 2004b; Zermansky 2006; Frankenthal 2014; Garcia‐Gollarte 2014; Connolly 2015). One study found evidence that the intervention led to a slower decline in health‐related quality of life (Pitkala 2014) with one study showing no effect on quality of life (Frankenthal 2014). There was evidence that the interventions led to the identification and resolution of medication‐related problems (Strikwerda 1994; Claesson 1998; Furniss 2000; Roberts 2001; Crotty 2004b; Zermansky 2006; Frankenthal 2014). There was evidence from five studies that medication appropriateness was improved (Crotty 2004a; Crotty 2004b; Frankenthal 2014; Garcia‐Gollarte 2014; Pitkala 2014). However, the link between improved medication appropriateness and patient‐related outcomes is not clear. The evidence for an effect on medicine costs was mixed with three studies finding a reduction in costs (Furniss 2000; Roberts 2001; Frankenthal 2014) and two studies finding no difference (Crotty 2004a; Zermansky 2006).
Overall completeness and applicability of evidence
The review was designed to identify interventions that considered residents’ whole medication regimens to optimise prescribing. Consequently, a broad range of interventions (professional and organisational) were eligible for the review and diverse, multifaceted interventions were ultimately implemented to address the objectives of the review.
The interventions were tested in the population of interest; however, there was considerable variability in the outcomes measured with quality of life only represented in two of the included studies (Frankenthal 2014; Pitkala 2014).
Current practice varies considerably internationally. Multidisciplinary teams (involving physicians, nurses and pharmacists) play a significant role in optimising prescribing for care home residents and this was reflected in the studies; the majority of interventions involved multidisciplinary teamwork, usually with pharmacists conducting medication reviews. However, the effectiveness of this has not been demonstrated. Information and communication technology is increasingly being employed to optimise prescribing in many settings, and one study tested the impact of a clinical decision support system (Gurwitz 2008).
Quality of the evidence
We could not draw robust conclusions from the evidence due to variability in design, interventions, outcomes and results. The review included 12 studies of varying quality that included 10,953 residents living in 355 care homes in ten countries and are summarised in the 'Summary of findings' table (summary of findings Table for the main comparison). The overall quality of the evidence for the outcomes reported was judged to be low or very low and therefore, there is uncertainty of the effect of interventions to optimise prescribing in this context. The interventions that were tested may reduce medication‐related problems and improve medication appropriateness; however, there may be little or no difference in adverse drug events, mortality, quality‐of‐life or hospital admissions. It is also uncertain whether the interventions decrease medication costs. The majority of the included studies were cluster‐RCTs and this was appropriate given the complex nature of interventions, the difficulty of blinding and the consequential threat of contamination. However, two of the nine cluster‐RCTs appeared to commit unit of analysis errors. The patient‐RCTs did not adequately protect against contamination and, therefore, the effects of the intervention may have potentially been diluted. Some of the studies had short follow‐up periods, which may have potentially limited the detection of effects on outcomes. None of the studies blinded participants and personnel; although this was unlikely to have been achievable due to the nature of the interventions, it may still introduce bias. The interventions tested were complex and multifaceted and none of the studies attempted to disentangle the 'black box' effect, that is to understand the effects of the contributing components. Not all the studies attempted blinding of assessment for subjective outcomes, and this could have been implemented. A major limitation of the evidence was the diversity of outcome measures and the fact that they differed in the way they were defined (if at all), collected and analysed.
Potential biases in the review process
We minimised bias when conducting this review by several methods. We conducted an extensive literature search which was guided by EPOC and we screened the included studies from published systematic reviews. We did not limit studies to those in the English language. Two review authors independently screened titles and abstracts, assessed studies for eligibility, evaluated risk of bias and extracted data.
Agreements and disagreements with other studies or reviews
We identified five previously published systematic reviews (Kaur 2009; Ostini 2009; Verrue 2009; LaMantia 2010; Loganathan 2011) and one narrative review (Markum 2010) related to the objectives of this review. We did not identify further studies from these reviews and the conclusions were similar, that is mixed results were obtained from the several intervention types tested in heterogeneous studies.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
| Interventions to optimise prescribing compared with usual GP care for care home residents | |||
| Patient or population: older people (aged 65 years or older) living in care homes Settings: Institutionalised care facilities in Australia, Finland, Israel, Netherlands, New Zealand, Spain, Sweden, United Kingdom, and USA and Canada Intervention: Intervention to optimise prescribing (single or multicomponent intervention) Comparison: Usual care by general practitioner | |||
| Outcomes | Impact | No of Participants | Quality of the evidence |
| Adverse drug events | There was no evidence of an effect on adverse drug events | 1228 in 87 care homes (2 studies) | ⊕⊕⊝⊝ |
| Hospital admissions | It is uncertain whether medication review reduces hospital admissions | 7606 in 309 care homes (8 studies) | ⊕⊕⊝⊝ |
| Mortality | There was no evidence of an effect on mortality | 6805 in 188 care homes (6 studies) | ⊕⊕⊝⊝ |
| Quality of life | It is uncertain whether medication review improves quality of life | 586 in 21 care homes (2 studies) | ⊕⊕⊝⊝ |
| Medication‐related problems | Medication review may lead to the identification and resolution of medication‐related problems | 6640 in 251 care homes (7 studies) | ⊕⊕⊝⊝ |
| Medication appropriateness | Medication review may lead to an improvement in medication appropriateness | 1566 in 152 care homes (5 studies) | ⊕⊕⊝⊝ |
| Medicine costs | It is uncertain whether medication review decreases medication costs | 4734 in 142 care homes (5 studies) | ⊕⊝⊝⊝ |
| GRADE Working Group grades of evidence | |||
| Quality assessment of evidence for each outcome was based on study design, risk of bias, inconsistency, indirectness and imprecision. The evidence was downgraded from high to low for adverse drug events (Crotty 2004b; Gurwitz 2008) due to a serious risk of bias and imprecision. The evidence was downgraded from high to low for hospital admissions (Furniss 2000; Roberts 2001; Crotty 2004b; Zermansky 2006; Frankenthal 2014; Garcia‐Gollarte 2014; Pitkala 2014; Connolly 2015), mortality (Furniss 2000; Roberts 2001; Zermansky 2006; Frankenthal 2014; Pitkala 2014; Connolly 2015), quality of life (Frankenthal 2014; Pitkala 2014) and medication appropriateness (Crotty 2004a; Crotty 2004b; Frankenthal 2014; Garcia‐Gollarte 2014; Pitkala 2014) due to a serious risk of bias and inconsistency. The evidence for medicines costs (Furniss 2000; Roberts 2001; Crotty 2004a; Zermansky 2006; Frankenthal 2014 was downgraded from high to very low due to a serious risk of bias, inconsistency and imprecision. The evidence for medicine‐related problems (Strikwerda 1994; Claesson 1998; Furniss 2000; Roberts 2001; Crotty 2004b; Zermansky 2006; Frankenthal 2014 was reduced from high to low due to design, risk of bias and imprecision. | |||
| Study,Country, Design | Participants | Intervention | Outcome measures | Duration |
| Sweden Cluster‐RCT | 1854 residents in 33 nursing homes | Multidisciplinary meetings with physician, pharmacist and nurse(s) | Medication‐related problems | 14 months |
| Australia Cluster‐RCT | 1998 residents in 36 nursing homes | Multidisciplinary meetings with study geriatrician, a GP, a pharmacist and a nurse manager. Education of nurses and care‐givers | Hospital admissions Mortality | 14 months |
| Australia Cluster‐RCT | 154 residents in 10 nursing homes | Multidisciplinary case conferencing with GP, a geriatrician, a pharmacist, residential care staff and an Alzheimer's Association representative | Medication Appropriateness Index | 3 months |
| Australia Patient‐RCT | 110 patients discharged to 85 long‐term care facilities | Pharmacist transition co‐ordinator. Transfer of medicines information to nursing staff, family physician and community pharmacist plus medication review and case conferencing | Adverse drug events Hospital admissions Medication‐related problems Medication Appropriateness Index | 8 weeks |
| Israel Patient‐RCT | 359 residents in 1 chronic care geriatric facility | Medication review by the study pharmacist | Hospital admissions Mortality Quality of life Medication appropriateness (STOPP‐START) Medication‐related problems Medicine costs | 12 months |
| UK Cluster‐RCT | 330 residents in 14 nursing homes | Medication review by a single pharmacist | Hospital admissions Mortality Medication‐related problems Medicine costs | 8 months |
| Spain Cluster‐RCT | 716 residents in 36 nursing homes | Physician educational programme followed by on‐demand support (prescription advice) by phone | Hospital admissions (total number of days spent in hospital) Medication appropriateness (STOPP‐START) | 6 months |
| USA/Canada Cluster‐RCT | 1118 residents in 29 units in 2 long‐term care facilities | Computerised provider order entry with clinical decision support | Adverse drug events | 12 months |
| Finland Cluster‐RCT | 227 residents in 20 assisted living facilities | Nurse training and education | Hospital admissions Mortality Health‐related Quality of Life Medication appropriateness (Beer's criteria plus others) | 12 months |
| Australia Cluster‐RCT | 3230 residents in 52 nursing homes | Introduction of new professional role, nurse education and medication review by pharmacists | Hospital admissions Mortality Medication‐related problems Medicine costs | 24 months |
| Netherlands Cluster‐RCT | 196 residents in 1 nursing home | Feedback on GP prescribing from community pharmacist | Medication‐related problems | 6 weeks |
| UK Patient‐RCT | 661 residents in 65 care homes | Medication review by a single pharmacist | Hospital admissions Mortality Medication‐related problems Medicine costs | 6 months |

