Decúbito prono para la insuficiencia respiratoria aguda en adultos
Resumen
Antecedentes
La hipoxemia aguda de novo o con antecedentes de hipoxemia crónica es un motivo frecuente de ingreso a cuidados intensivos y de administración de ventilación mecánica. Se emplean varias mejoras o complementos a la ventilación mecánica para mejorar los resultados del paciente. La mortalidad por síndrome de dificultad respiratoria aguda, uno de los contribuyentes principales a la necesidad de asistencia respiratoria mecánica para la hipoxemia, aún es de aproximadamente el 30‐40%. La asistencia respiratoria en decúbito prono podría mejorar la mecánica pulmonar y el intercambio de gases y podría mejorar los resultados.
Objetivos
Los objetivos de esta revisión son evaluar si la asistencia respiratoria en decúbito prono ofrece ventajas para la mortalidad en comparación con la asistencia respiratoria tradicional en decúbito supino o semisentado en los pacientes adultos con insuficiencia respiratoria aguda grave que requieren asistencia respiratoria artificial invasiva convencional.
Métodos de búsqueda
Se buscaron ensayos controlados aleatorizados en CENTRAL, MEDLINE, EMBASE, LILACS y CINAHL hasta mayo de 2020 mediante una versión actualizada de la estrategia de búsqueda de la anterior versión de la revisión. Se añadió una búsqueda en el Registro de Estudios Cochrane COVID‐19 (Cochrane COVID‐19 Study Register).
También se buscaron estudios mediante la búsqueda manual de listas bibliográficas y citas de artículos relevantes, mediante el contacto con compañeros, mediante la búsqueda manual de actas publicadas de revistas importantes. Se realizaron búsquedas de estudios en curso en los registros de ensayos em noviembre de 2020. No se aplicó ningún límite de idioma o de estado de publicación.
Criterios de selección
Se incluyeron ensayos controlados aleatorizados (ECA) que examinaron los efectos del decúbito prono versus la supino/semisentado durante la asistencia respiratoria mecánica convencional en participantes adultos con hipoxemia aguda.
Obtención y análisis de los datos
Se utilizaron los procedimientos metodológicos estándar previstos por Cochrane. Los datos se analizaron mediante el programa informático Review Manager y los estudios incluidos se agruparon para determinar la razón de riesgos (RR) para la mortalidad y la razón de riesgos o la diferencia de medias (DM) para los desenlaces secundarios; también se realizaron análisis de subgrupos y análisis de sensibilidad.
Resultados principales
Se identificaron nueve ECA abiertos (sin cegamiento) relevantes (12 publicaciones) que incluyeron un total de 2165 participantes. Todos los participantes incluidos padecían trastornos de la función pulmonar que causaban hipoxemia de moderada a grave y requerían ventilación mecánica, por lo que eran bastante comparables dentro de la gran diversidad de diagnósticos específicos en los cuidados intensivos. No fue posible el cegamiento a la asignación a los tratamientos (boca arriba versus boca abajo) de los participantes, los cuidadores, los investigadores del ensayo clínico y otros encargados de tomar decisiones. Esto predispone al sesgo en lo que respecta al uso de cointervenciones y también a la iniciación de mantenimiento o retirada del soporte vital, una práctica habitual en los cuidados intensivos.
Los análisis primarios de la mortalidad a corto y más largo plazo corto agrupados de seis ensayos demostraron una RR de 0,84 a 0,86 a favor del decúbito prono (DP), pero los resultados no fueron estadísticamente significativos: a corto plazo, la mortalidad de los pacientes con asistencia respiratoria en decúbito prono fue del 33,4% (363/1086) y del 38,3% en decúbito supino (395/1031). Lo anterior dio lugar a una RR de 0,84 (intervalo de confianza [IC] del 95%: 0,69 a 1,02). Para la mortalidad a más largo plazo, los resultados mostraron una mortalidad del 41,7% (462/1107) en decúbito prono y del 47,1% (490/1041) en decúbito supino, con una RR de 0,86 (IC del 95%: 0,72 a 1,03). La calidad de la evidencia para ambos resultados se calificó como baja debido al posible sesgo importante y la inconsistencia grave.
Los análisis de subgrupos para la mortalidad identificaron tres grupos que favorecieron sistemáticamente al DP: los pacientes reclutados en el transcurso de las 48 horas de haber cumplido los criterios de ingreso (cinco ensayos; 1024 participantes; RR de 0,75 [IC del 95%: 0,59 a 94]); los pacientes tratados en DP durante 16 o más horas por día (cinco ensayos; 1005 participantes; RR de 0,77 [IC del 95%: 0,61 a 0.99]); y los pacientes con hipoxemia más grave al ingreso al ensayo (seis ensayos; 1108 participantes; RR de 0,77 [IC del 95%: 0,65 a 0,92]). La calidad de la evidencia para estos resultados se calificó como moderada debido al posible riesgo de sesgo importante.
El decúbito prono pareció influir en los efectos adversos: las úlceras por presión (cuatro ensayos; 823 participantes) con una RR de 1,25 (IC del 95%: 1,06 a 1,48) y la obstrucción del tubo traqueal con una RR de 1,78 (IC del 95%: 1,22 a 2,60), aumentaron con la asistencia respiratoria en decúbito prono. Los informes de arritmias se redujeron con el DP, con una RR de 0,64 (IC del 95%: 0,47 a 0,87).
Conclusiones de los autores
No se encontró evidencia convincente del efecto beneficioso o perjudicial de la aplicación universal de DP en adultos con hipoxemia con asistencia respiratoria mecánica en unidades de cuidados intensivos (UCI). Ello a pesar de los beneficios observados en uno de los ensayos abiertos restringidos a los participantes con mayor gravedad de la enfermedad. Tres subgrupos (implementación temprana del DP, adopción prolongada del DP e hipoxemia grave al ingreso al estudio) indicaron que el decúbito prono podría conferir un beneficio en la mortalidad, pero estos resultados deben interpretarse con cautela. Se necesitarían estudios con potencia estadística suficiente para confirmar o refutar definitivamente estas observaciones de beneficios de subgrupos. Esto es problemático, dados los resultados del ensayo más reciente de diseño abierto que muestra un beneficio y las recomendaciones derivadas de varios análisis de subgrupos publicados. Si no es realista realizar una replicación y confirmación de los resultados de esos ensayos, que sería deseable, se podría utilizar un metanálisis formal de los datos de pacientes individuales y estudios observacionales posteriores al ensayo (como ocurre después de los ensayos clínicos de fármacos de fase III) para confirmar el beneficio aparente en las poblaciones en riesgo. Las complicaciones como la obstrucción del tubo traqueal y las úlceras por presión aumentan con el uso de la asistencia respiratoria en decúbito prono. Se necesitan datos de mortalidad a largo plazo (12 meses y más), así como datos funcionales, neuropsicológicos y de la calidad de vida si se desea que los estudios futuros informen mejor la función del DP en el tratamiento de la insuficiencia respiratoria hipoxémica en la UCI.
PICO
Resumen en términos sencillos
Decúbito prono (boca abajo) para la asistencia respiratoria mecánica en adultos con insuficiencia respiratoria aguda
Pregunta de la revisión
Esta revisión intentó investigar si la asistencia respiratoria boca abajo podría mejorar resultados importantes como, por ejemplo, reducir la tasa de muertes (mortalidad) entre los pacientes que requieren asistencia respiratoria mecánica en cuidados intensivos. También se deseaba identificar las desventajas y complicaciones asociadas con el decúbito prono, así como los efectos beneficiosos a largo plazo.
Antecedentes
Los pacientes ingresados en una unidad de cuidados intensivos y que necesitan ayuda para respirar proporcionada por un respirador (ventilación mecánica) debido al daño pulmonar causado por una enfermedad, tienen un alto riesgo de morir. Los pulmones que son afectados por afecciones como la neumonía tendrán áreas normales y anormales o enfermas. La recuperación de las áreas enfermas toma tiempo, y un paciente puede necesitar apoyo con asistencia respiratoria mientras esto ocurre. El apoyo con asistencia respiratoria es una intervención que puede salvar la vida del paciente, ya que mantiene niveles de oxígeno adecuados en la sangre a la vez que elimina los desechos de dióxido de carbono. Sin embargo, el respirador por sí mismo puede causar inflamación y por lo tanto complicaciones pulmonares adicionales. Cuanto más fuerte tenga que trabajar el respirador para lograr una oxigenación normal y extraer el dióxido de carbono, es más probable que las áreas pulmonares sanas normales se dañen y empeore el estado del paciente. La asistencia respiratoria con el paciente acostado boca abajo (prono) en vez de boca arriba (supino) podría mejorar el trabajo del respirador, y reducir por lo tanto estos efectos secundarios indeseables.
Fecha de la búsqueda
La evidencia está actualizada hasta el 1 de mayo de 2020.
Características de los estudios
Se identificaron e incluyeron en esta revisión los ensayos controlados aleatorizados en adultos que compararon la asistencia respiratoria mecánica convencional boca abajo versus boca arriba.
Resultados clave
Los informes de nueve ensayos de 2165 participantes (12 publicaciones) muestran que la asistencia respiratoria en decúbito prono no pareció tener efectos beneficiosos en todos los participantes que requirieron asistencia respiratoria. La evidencia identifica algunas situaciones en las que podría mejorar la supervivencia. Un grupo de participantes con daño pulmonar más grave pareció tener una reducción en la mortalidad, al igual que los participantes que recibieron tratamiento temprano y durante períodos prolongados. Se describieron las complicaciones. Las más frecuentes fueron úlceras por presión y bloqueo u obstrucción del tubo traqueal. También se observó una presión arterial baja y ritmos cardiacos anormales. La evidencia identificada no justificó la aplicación del decúbito prono a todos los pacientes en cuidados intensivos con niveles de oxígeno bajos, pero algunos grupos concretos de pacientes, por ejemplo, los que tienen niveles de oxígeno especialmente bajos, podrían beneficiarse del decúbito prono. La realización de nuevos ensayos clínicos ayudaría a aclarar los posibles beneficios para esos grupos de pacientes, pero es posible que no se realicen más ensayos debido al gran beneficio del tratamiento observado en el ensayo clínico más reciente de los participantes con niveles de oxígeno muy bajos. A falta de nuevos ensayos, el metanálisis de los datos de los pacientes individuales puede facilitar la evaluación adicional así como futuros estudios observacionales en poblaciones en riesgo.
Calidad de la evidencia
La calidad de la evidencia para los desenlaces principales de esta revisión sistemática fue baja debido a inconsistencia grave y a un posible sesgo importante.
Authors' conclusions
Summary of findings
| Mortality: prone position compared with supine for acute respiratory failure in adults requiring mechanical ventilation in intensive care | ||||||
| Patient or population: adults with acute respiratory failure | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Control | Mortality: prone position compared with supine | |||||
| Short‐term mortality (STM) | Study population | RR 0.84 | 2117 | ⊕⊕⊝⊝ | ||
| 383 per 1000 | 322 per 1000 | |||||
| Moderate | ||||||
| 450 per 1000 | 378 per 1000 | |||||
| Longer‐term mortality (LTM) | Study population | RR 0.86 | 2141 | ⊕⊕⊝⊝ | ||
| 470 per 1000 | 404 per 1000 | |||||
| Moderate | ||||||
| 525 per 1000 | 452 per 1000 | |||||
| Subgroup analysis of longer‐term mortality: severe hypoxaemia | Study population | RR 0.77 | 977 | ⊕⊕⊕⊝ | ||
| 547 per 1000 | 421 per 1000 | |||||
| Moderate | ||||||
| 653 per 1000 | 503 per 1000 | |||||
| Subgroup analysis of longer‐term mortality: lower tidal volume ventilation | Study population | RR 0.73 | 911 | ⊕⊕⊕⊝ | ||
| 451 per 1000 | 329 per 1000 | |||||
| Moderate | ||||||
| 523 per 1000 | 382 per 1000 | |||||
| Subgroup analysis of longer‐term mortality: ARDS only | Study population | RR 0.85 | 1758 | ⊕⊕⊕⊝ | ||
| 483 per 1000 | 411 per 1000 | |||||
| Moderate | ||||||
| 522 per 1000 | 444 per 1000 | |||||
| Subgroup analysis of longer‐term mortality: ≥ 16 hours/d prone | Study population | RR 0.77 | 1005 | ⊕⊕⊕⊝ | ||
| 470 per 1000 | 362 per 1000 | |||||
| Moderate | ||||||
| 526 per 1000 | 405 per 1000 | |||||
| Subgroup analysis of longer‐term mortality: enrolment ≤ 48 hours after entry criteria/ventilation | Study population | RR 0.75 | 1024 | ⊕⊕⊕⊝ | ||
| 469 per 1000 | 352 per 1000 | |||||
| Moderate | ||||||
| 523 per 1000 | 392 per 1000 | |||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| aBlinding of participants and carers was not possible. Researchers also may not have been adequately blinded. All analyses were downgraded because of this important potential bias, leading the quality of all subgroup analyses to be rated as moderate | ||||||
Background
Description of the condition
Acute respiratory failure can arise from numerous diseases or disease processes, and is a common reason for admission to hospital. Patients with profound gas exchange abnormalities unresponsive to ward‐based strategies (such as oxygen therapy or continuous positive airways pressure (CPAP) for hypoxaemic respiratory failure, or non‐invasive ventilation (NIV) for hypercapnic ventilatory failure) may be referred to intensive care units (ICUs) for further management. Patients whose problems are predominantly related to oxygenation include those with pneumonia, pulmonary oedema, pulmonary aspiration pneumonitis and pulmonary thromboembolism. Acute lung injury and acute respiratory distress syndrome (Bellani 2016; Bernard 2005; MacCallum 2005; Matthay 2019; Phua 2009; Rubenfeld 2007) are reported in an important subset of patients treated for hypoxaemia within the ICU. Acute respiratory distress syndrome (ARDS) as the phrase suggests is only a syndrome and not a specific or single disease process, It may arise as a result of a wide variety of disparate pulmonary and extrapulmonary disease processes (Rezoagli 2017; Walkey 2012), as can its less physiologically severe counterpart previously called acute lung injury (ALI). Redefinition of ARDS, which has occurred since most studies were designed or published, ALI has been renamed as "mild ARDS" (ARDS definition workforce 2012). For the new criteria of mild, moderate and severe ARDS, mortality is quoted as 27%, 32% and 45% (ARDS definition workforce 2012). The commonly described histological finding of diffuse alveolar damage is found in only 50% of cases (de Hemptinne 2009), and doubt has been cast on the usefulness of the ARDS paradigm (Marini 2008; Soni 2010). Nevertheless, the concept is considered clinically useful by most intensivists (Bernard 2005). Recently different ARDS phenotypes are recognised as important (Reilly 2019; Matthay 2019; Wilson 2020). This has been especially so for ARDS associated with COVID‐19 pneumonia (Marini 2020; Robba 2020). ARDS, originally an abbreviation for Adult Respiratory Distress Syndrome remains a signature medical condition process that intensive care personnel strive to research and improve patient outcomes but is only a subset of conditions that cause acute respiratory failure in adult intensive care.
Mechanical ventilation is also used in younger patients (neonates, infants, children through to adolescents) for paediatric ARDS (PARDS). It is important to stress that the adult‐based definitions of ARDS may not be applicable to paediatrics for a variety of reasons (Cheifetz 2017). These include anatomic and physiologic differences which render infants and children more vulnerable to severe respiratory insult, greater metabolic demand and less cardiorespiratory reserve than adolescents and adults. Special considerations are often necessary to optimise management approaches across the heterogeneous paediatric spectrum ranging from neonates to adolescents. Thomas and colleagues also note children have considerable variability in the predisposing conditions and etiology; their response to therapy was different and often better; and pre‐existing conditions and underlying etiology appeared to influence outcome to a greater extent than the severity of the lung injury itself. They (Thomas 2013) highlight a medical axiom that children should not be considered as "little adults." Kneyber et al also note that with regards to ventilator induced lung injury (VILI) that given the physiological and biological differences in the respiratory systems of infants, children, and adults, it is difficult to directly extrapolate clinical practice from adults to children (Kneyber 2014). For the above discussed reasons children are not considered together with adults in this systematic review. Children and neonates have also been the subject of separate Cochrane Systematic Reviews (Gillies 2012; Rivas‐Fernandez 2016)
Patients with ventilatory failure and hypercapnia include those with chronic obstructive pulmonary disease (COPD) and those receiving central nervous system depressant drugs; patients with neuromuscular problems may also require mechanical ventilation. Thus a wide variety of patients may require mechanical ventilation within the adult ICU. Variability is great with regards to severity of illness and severity of structural lung damage. The reversibility of disease‐driving processes is also inconsistent.
Description of the intervention
Patients with profound hypoxaemia present a significant challenge for carers in dealing with both hypoxaemia and underlying process(es). Although hypoxaemia often is not perceived as the ultimate cause of death in these patients, it does have deleterious effects (Strachan 2001). Avoidance of profound hypoxaemia is one of the goals of supportive therapy in ICU, and a variety of manoeuvres are employed to ameliorate hypoxaemia. Including: positive end‐expiratory pressure (PEEP), inverse ratio ventilation (IRV), alveolar recruitment manoeuvres, restrictive fluid administration strategies, inhaled pulmonary vasodilators such as nitric oxide and prostacyclin, corticosteroids and neuromuscular blockers and mechanical ventilation in the prone position (Adhikari 2004; Adhikari 2007; ARDSnet 2006b; ARDSnet 2006a; Cranshaw 2002;Fielding‐Singh 2018; Klein 2004; Mentzelopoulos 2005; Papazian 2010). All of these therapies have been shown to improve oxygenation, but few have demonstrated a mortality benefit in randomized controlled trials (Diaz 2010; Papazian 2010; Petrucci 2013). Athough a systematic review of high‐frequency oscillation (HFO) suggested their possible utility in the management of ARDS (Fan 2010; Sud 2013), two RCTs reported in 2013 have not confirmed benefit (Ferguson 2013; Young 2013). Notably one of the trials was discontinued early as a result of increased mortality in the treatment group (Ferguson 2013). Extracorporeal membrane oxygenation (ECMO) has been shown to be of benefit (Noah 2011; Noble 2010; Aoyama 2019) but is available only in relatively few specialized centres. Traditional mechanical ventilation, which normally is utilized in supine and semi recumbent patients, while ensuring short‐term survival, may also contribute to lung injury and other deleterious effects (Soni 2008). Ventilator‐induced lung injury has been demonstrated in both experimental animal models and in human participants to perpetuate or even accentuate the original injury to the lung and can cause dysfunction of distant organs (Verbrugge 2007) in the form of barotrauma, volutrauma and biotrauma.
Under normal circumstances, patients ventilated in ICUs are cared for in the semi‐recumbent position, often described as the supine position. This supine or semi‐recumbent position allows better access for carers to provide interventions such as mouth care and airway and vascular access procedures. It is also more appropriate for critical manoeuvres such as cardiopulmonary resuscitation, should this be required. This position is more comfortable for patients and allows them better interaction with their environment when compared with the prone, face‐down position.
This systematic review explores the intervention of placing patients in the prone position (face‐down) while they are mechanically ventilated for severe hypoxaemic respiratory failure via a tracheal tube.
How the intervention might work
Chatte 1997 and others have showed that ventilation provided with the patient in the prone position could have beneficial effects on oxygenation (Gattinoni 2001; Mure 2001). Recent studies in humans and in experimental animal models, have confirmed that ventilation in the prone position is associated with improved oxygenation in most individuals. More than 70% of patients with lung injury show clinical improvement in oxygenation with prone mechanical ventilation. In a retrospective multi‐variate analysis, prone positioning was independently correlated with positive outcomes in patients with ARDS (Venet 2003). The mechanisms by which prone position improves gas exchange include alveolar recruitment, redistribution of ventilation towards dorsal areas that remain well perfused, homogenization of tidal volume distribution and possible improved postural drainage of secretions (Gattinoni 2006; Guerin 2006). Postural drainage has also been suggested to reduce ventilator‐associated pneumonia, although theoretically this could spread organisms and inflammatory mediators within lung tissue, leading to increased damage (Graf 2008; Marini 2010). Homogenization of tidal volume distribution may reduce tissue stress/strain and consequently may diminish the well‐described injurious effects of mechanical ventilation, thus providing additional benefit over and above that associated with improved oxygenation (Gattinoni 2012; Gattinoni 2013; Mentzelopoulos 2005; Slutsky 2013). Other effects include improvements in haemodynamics (Guerin 2014).
Thus, three phenomena might improve survival among patients (Charron 2011).
-
Reduced extent and duration of severe hypoxaemia.
-
Reduced propensity to ventilator‐induced lung injury.
-
Reduced occurrence of nosocomial or ventilator‐associated pneumonia.
Adverse effects associated with the prone position for ventilation most notably include (Faculty of Intensive Care 2019):
-
unplanned extubation and risk of an episode of potentially catastrophic hypoxaemia;
-
inadvertent bronchial intubation, which will also worsen hypoxaemia and increase risk of barotrauma (e.g. pneumothorax);
-
development of pressure sores / ulcers (most cited injury);
-
facial / periorbital edema;
-
ocular complications including severe corneal abrasions and possible ischaemic neuropathy with permanent sight loss;
-
cardiovascular instability;
-
intravenous line displacement;
-
kidney dialysis / filtration line flow problems interfering with renal support;
-
intracranial hypertension, which can compromise cerebral circulation;
-
brachial plexus injuries; and
-
staff injuries, especially if insufficient trained staff are available to perform required turns in sedated intubated patients
Improved oxygenation with the prone position could allow additional time for lung reparative processes, and, by reducing secondary lung infection or injury, has the potential to accelerate recovery and lessen mortality among adults with acute respiratory failure. Adverse effects and complications related to the prone position might reduce the overall impact of these potential benefits.
Why it is important to do this review
Patients admitted to the ICU with severe hypoxaemia are at high risk for mortality (ARDS definition workforce 2012; Walkey 2012). For example, Phua and colleagues reported overall mortality in the important subset of ICU patients with ARDS of 44% in observational studies and 36% in randomized controlled trials. This rate of mortality does not seem to have been significantly reduced since 1994, when the American‐European Consensus Conference redefined ARDS (Phua 2009). Any intervention that reduces mortality, especially one that can be easily implemented at little additional cost, requires adequate exploration. This interim amendment of the original review (Bloomfield 2015) seeks to update evidence from any new randomized clinical trials and evaluate all evidence in the context of current theory and practice. This amendment may be superseded by a complete review update in the future.
Objectives
The objectives of this review are (1) to ascertain whether prone ventilation offers a mortality advantage when compared with traditional supine or semi recumbent ventilation in participants with severe acute respiratory failure requiring conventional invasive artificial ventilation, and (2) to supplement previous systematic reviews on prone ventilation for hypoxaemic respiratory failure in an adult population.
Methods
Criteria for considering studies for this review
Types of studies
We included all randomized controlled trials (RCTs) comparing conventional modes of mechanical ventilation in the supine or semi recumbent position versus mechanical ventilation in the prone position in adults with acute respiratory failure. We did not include observational studies due to the perceived higher risk of bias.
We included unpublished studies and abstracts when identified.
We imposed no language restrictions.
Types of participants
We included studies on adults with critical illness in an ICU setting requiring conventional mechanical ventilation for acute severe respiratory failure.
We excluded studies primarily investigating participants with chronic respiratory impairment such as COPD. This review focused on acute severe respiratory failure.
We excluded studies on neonates or paediatric participants (i.e. younger than 16 years), which are covered separately in updated Cochrane reviews (Gillies 2012; Rivas‐Fernandez 2016) and because of other differences in physiology, aetiology, definitions, comorbidities, cointerventions and rescue treatments for paediatric patients with acute respiratory failure (Cheifetz 2017; Kneyber 2014; Thomas 2013).
Types of interventions
We examined interventions comparing conventional methods of ventilation in the supine or semi recumbent position (which could encompass lateral positioning as part of routine pressure care) versus the prone position.
We excluded studies that used primary positions other than supine or semi recumbent. We excluded rotational therapies provided in the prone position. We excluded studies comparing conventional prone ventilation versus other experimental modes of ventilation such as high‐frequency jet ventilation (HFJV) or high‐frequency oscillation (HFO).
Types of outcome measures
We sought information on the following main outcomes.
Primary outcomes
-
Short‐term mortality (10 to 30 days, or ICU mortality).
-
Longer‐term mortality (> 30 days, or hospital mortality).
Secondary outcomes
We also sought information on the following.
-
Rate of ventilator‐associated pneumonia, as defined in the original studies.
-
Number of days on a ventilator.
-
Length of ICU stay.
-
Length of hospital stay.
-
Improvement in oxygenation.
-
Adverse events.
-
Quality of life.
-
Economic outcomes.
Search methods for identification of studies
Electronic searches
We searched for eligible randomized controlled trials as described in the Cochrane Handbook of Systematic reviews of Interventions Chapter 4 (Lefebvre 2019).
We applied no language or publication status constraints.
We searched the following databases:
-
CENTRAL, Cochrane Central Register of Controlled Trials (2020, Issue 4)
-
MEDLINE ALL (Ovid SP; 2014 to 01 2020 May)
-
EMBASE (Ovid SP; 2014 to 01 May 2020)
-
CINAHL, Cumulative Index to Nursing and Allied Health Literature (Ebsco; 2014 to 01 May 2020)
-
LILACS, Latin American Caribbean Health Sciences Literature (2014 to 01 May 2020)
-
Cochrane COVID 19 Register
We updated the search strategy of Bloomfield 2015 with extra search terms and added filters for randomized controlled trials. The searches were run from 1 January 2014 to 1 May 2020 using the search strategy provided in Appendix 1.
For the earlier version of this review (Bloomfield 2015), we searched: CENTRAL (2014, Issue 1), MEDLINE (Ovid SP; 1950 to 31 January 2014), EMBASE (Ovid SP; 1980 to 31 January 2014), CINAHL (1982 to 31 January 2014) and LILACS (1992 to 31 January 2014).
Searching other resources
We also searched for studies by:
-
hand‐searching reference lists and citations of previous trials and review articles to May 2020;
-
hand‐searching books related to critical care and mechanical ventilation;
-
communicating with colleagues, particularly published trialists; and
-
performing a subject‐specific search of the following journals to look for published proceedings abstracts of clinical trials.
-
American Journal of Respiratory and Critical Care Medicine, volumes 175 to 189, 2007 to January 2014.
-
Critical Care, volumes 11 to 18, 2007 to January 2014.
-
Critical Care Medicine, volumes 35 to 42, 2007 to January 2014.
-
Intensive Care Medicine, volumes 33 to 40, 2007 to January 2014.
-
We searched for relevant ongoing trials at the following websites (searched 20 November 2020):
-
ClinicalTrials.gov (https://www.clinicaltrials.gov/)
-
ISRCTN Registry (http://www.isrctn.com/)
-
World Health Organization ‐ International Clinical Trials Registry Platform (ICTRP) (www.who.int/clinical-trials-registry-platform)
-
Cochrane Covid‐19 study register (https://covid-19.cochrane.org/)
We checked the included studies for retractions in the Retraction Watch Database and in PubMed.
Data collection and analysis
Selection of studies
Two review authors (RB and DWN) independently screened and classified all citations as potential primary studies, review articles or others for inclusion. Two review authors (RB and DWN) examined all potential primary studies and decided whether they should be included in the review. We resolved all disagreements by discussion.
Data extraction and management
Two review authors (RB and DWN) independently extracted in duplicate from each study data on methods and outcomes (Appendix 2). A third review author (AS) checked data subsequently entered onto a Microsoft Excel spreadsheet.
Assessment of risk of bias in included studies
We judged study quality using the Cochrane Risk of bias tool on the basis of criteria and mechanisms described in Table 8.5.d by Higgins et al (Higgins 2011a), which were based on:
-
adequacy of randomization;
-
allocation concealment;
-
blinding of participants and investigators;
-
blinding of outcome assessment;
-
completeness of outcome data;
-
selective reporting; and
-
other relevant potential bias.
We addressed the impact of methodological quality on results and performed a sensitivity analysis that excluded studies at high risk of bias. We rated the quality of evidence by using the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) system (Guyatt 2008; Guyatt 2011a; Guyatt 2011b; Guyatt 2011c), as described below.
Measures of treatment effect
For dichotomous outcomes, we calculated risk ratios (RRs). We used odds ratios (ORs) when outcomes were rare. We used standardized mean differences (SMDs) or mean differences (MDs) as appropriate for continuous outcomes.
Unit of analysis issues
We identified no specific issues.
Dealing with missing data
We did not specify in the original protocol how missing data issues would be managed (Bloomfield 2009).
Assessment of heterogeneity
We measured heterogeneity by using the Higgins test, whereby an I2 statistic greater than 25% is considered to show significant heterogeneity. This test describes the percentage of total variation across studies that is due to heterogeneity rather than to chance (Higgins 2003). We used a fixed‐effect model when the Higgins test showed good homogeneity (low heterogeneity) between studies; otherwise, we used a random‐effects model. Higgins has defined an I2 statistic of 25%, 50% or 75% as low, moderate or high (Higgins 2003). When present, we planned to explore heterogeneity by considering these options listed in the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011).
-
Avoiding formal meta‐analysis when fewer than two studies provided quantitative data for primary outcomes.
-
Ignoring heterogeneity.
-
Using random‐effects meta‐analysis to ascertain mean effect and confidence intervals of the mean effect size. (Deeks 2019)
-
Exploring heterogeneity by using pre‐specified subgroup analyses or meta‐regression when we identified sufficient (> 10) studies.
-
Excluding studies as part of a sensitivity analysis (Deeks 2011).
Assessment of reporting biases
We used a funnel plot to assess the risk of small study effects or reporting bias (Higgins 2011a).
Data synthesis
We reviewed data from included studies qualitatively, and then, when possible, we combined data quantitatively by population, intervention and outcome, using Cochrane's statistical software, RevMan 5.40. We based quantitative analyses of outcomes on "intention‐to‐treat" results (i.e. results based on the intention‐to‐treat principle). We followed the recommendations provided in the Cochrane Handbook for Systematic Reviews of Interventions regarding data synthesis. In cases of very substantial (high) heterogeneity (Higgins 2003), we would not pool the results to perform statistical analysis. We used a fixed‐effect model when homogeneity between studies was good, and a random‐effects model when it was not.
Subgroup analysis and investigation of heterogeneity
We planned to undertake the following subgroup analyses (SGA).
-
Duration of daily ventilation in the prone position (< 16 hours/d vs ≥ 16 hours/d). As any benefit from prone ventilation may be a dose (time)‐related phenomenon, daily duration of time in that position would appear potentially important.
-
Duration of supine ventilation before randomization. As ventilatory‐induced lung injury is relatively rapid in onset, any randomized trials and outcomes reporting very limited exposure to supine ventilation before randomization should be identified.
-
Outcome according to severity (oxygenation index; PaO2/FIO2 ratio or quotient; severity of illness score, e.g. Simplified Acute Physiology Score II (SAPS II)). As patients with more severe lung injury benefit from prone ventilation, this may be an important subgroup to explore. SAPS II and similar scores may indirectly reflect the severity of inciting injury and may be relevant.
-
Tidal volume (size of the mechanical breath given to the participant) in relation to body weight has been shown to affect survival and outcomes between high tidal volume (> 10 mL/kg of ideal body weight), moderate tidal volume (8 to 10 mL/kg of ideal body weight) and low tidal volume (≤ 8 mL/kg of ideal or predicted body weight) and will be explored if the data permit. (Actual body weight exceeds ideal or predicted body weight by a mean factor of as much as 1.25 (Bloomfield 2006) and therefore underestimates the standard metric of tidal volume, which is based on ideal body weight.) We considered "ideal" and "predicted body weight" as interchangeable and based on height and sex of participants.
-
We analysed studies of acute lung injury (ALI) together with acute respiratory distress syndrome (ARDS) separately from those examining other causes of acute severe hypoxaemic respiratory failure.
-
We further sub‐classified acute lung injury and ARDS into pulmonary and extrapulmonary causes and as conditions that may behave differently with different ventilatory strategies (Walkey 2012; Ware 2000). We planned to explore differences in outcomes in these subcategories if collected data allowed.
We explored evidence of substantial heterogeneity in primary outcomes as indicated by the Higgins test by performing subgroup analyses, and, if we identified more than 10 primary studies, by performing meta‐regression (Deeks 2011). We did not employ statistical techniques or adjustments for multiple comparisons when conducting these prespecified analyses.
Sensitivity analysis
We undertook a sensitivity analysis of primary outcomes with regards to the quality of data. We excluded from the sensitivity analysis studies with two or more "red flags" due to the high risk of bias.
Summary of findings and assessment of the certainty of the evidence
We used the principles of the GRADE system (Guyatt 2008; Guyatt 2011a; Guyatt 2011b; Guyatt 2011c) to assess the quality of the body of evidence associated with specific outcomes. In the case of RCTs, the GRADE system allows downgrading of the overall rating of evidence from "high quality" by one or two grades on the basis of study limitations (risk of bias), indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
We applied the GRADE system to these primary outcome measures.
-
Short‐term mortality.
-
Longer‐term mortality.
We also applied this system to four subgroup analyses related to longer‐term mortality.
-
Participants with severe hypoxaemia.
-
Mechanical ventilation with lower tidal volumes.
-
Outcomes for participants with ALI or ARDS.
-
Maintenance of the prone position for 16 or more hours per day.
-
Enrolment within 48 hours of meeting study criteria.
We chose these outcomes for GRADE analysis after the protocol was published, as this tool was not used by The Cochrane Collaboration at that time.
Results
Description of studies
See Characteristics of included studies, Characteristics of excluded studies, and Characteristics of ongoing studies.
Results of the search
Details of the original search are reported in Bloomfield 2015. The results of the updated search from 1st January 2013 to 1st May 2020 are presented in a study flow diagram (Figure 1).
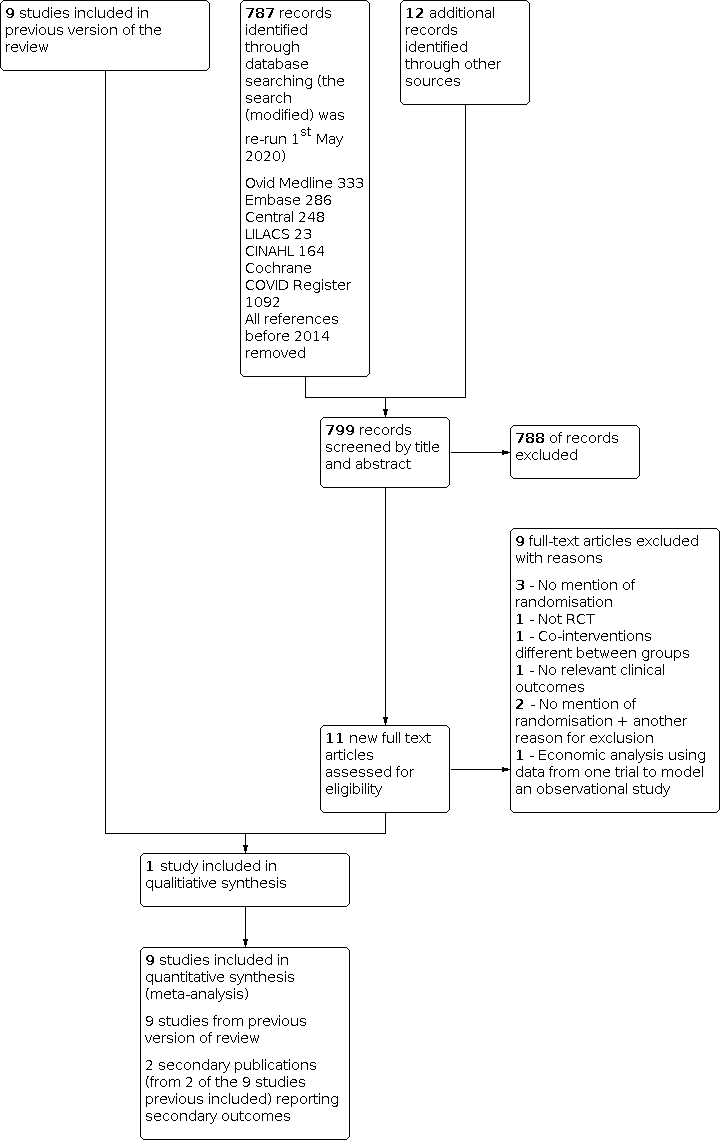
Flow diagram of results from updated search (January 2014 to 1st May 2020)
A search of proceedings supplements of the American Journal of Respiratory and Critical Care Medicine, Critical Care, Critical Care Medicine and Intensive Care Medicine yielded no additional relevant RCTs.
Included studies
We extracted data from nine primary studies reported in 13 publications. Eight were primary studies published in full form in peer‐reviewed journals (Chan 2007; Fernandez 2008; Gattinoni 2001; Guerin 2004; Guerin 2013; Mancebo 2006; Taccone 2009; Voggenreiter 2005). One study was reported as an abstract, with supplementary information given in presentation slides provided by Jan Friederich (Leal 1997). We found additional data regarding some of the primary studies in seven journal publications (Ayzac 2016; Chiumello 2012; Gattinoni 2010; Girard 2014; Sud 2008b; Sud 2010; Sud 2014). These provided additional information on subgroups of participants with very severe hypoxaemia from four studies (Gattinoni 2001; Guerin 2004; Mancebo 2006; Taccone 2009) and on an ARDS subgroup from one study (Sud 2014). Chiumello et al (Chiumello 2012) reported one‐year mortality at five of the centres that contributed to the Taccone 2009 study. Sud et al provided additional data regarding severity of illness through SAPS II scores (Sud 2008b). Chiumello et al reported pulmonary function and quality of life data (Chiumello 2012). Most studies recruited participants with ALI or ARDS, although the largest single study (Guerin 2004) also recruited individuals who would have been excluded from the ALI/ARDS trials. Some information for this subgroup was later made available (Sud 2014).
Two secondary publications were identified in the latest search update and reported new data from the primary trial of Guerin (Guerin 2013) regarding pressure ulcers (Girard 2014) and ventilator associated pneumonia (Ayzac 2016). They are incorporated into this amendment.
Excluded studies
We excluded five studies that were included in other published meta‐analyses. Two studies (Demory 2007; Papazian 2005) investigated the short‐term effects of high‐frequency oscillatory ventilation (HFOV) in prone and supine participants. One was a prevention study (Beuret 2002) in patients with coma, and one (Watanabe 2002) applied an intervention of neuromuscular blockade to the prone group that has been associated with improved outcomes in some but not all trials (Ho 2020; Papazian 2010) and failed to report mortality data. Another study (Curley 2005) included predominantly very young children with a median age of two years and no adults. Two of these studies (Beuret 2002; Watanabe 2002) were conducted in the pre‐low tidal volume ventilation era.
The updated search for this amendment identified eight further studies for possible inclusion (Cao 2014; Cheng 2016; Li G 2015; Li J 2015; Peng 2018; Wang 2015; Yan 2015; Zhou 2014) two directly from the literature search and six from the systematic review of Du (Du 2018). All were ultimately excluded from analysis (Characteristics of excluded studies). Five (Cao 2014; Cheng 2016; Li J 2015; Wang 2015; Yan 2015 ) did not mention randomization. One (Li G 2015) was a retrospective study. The 60 patient 4‐limb randomized clinical study of Peng et al (Peng 2018) was primarily a short‐term physiological investigation with a single episode of prone intervention. It did not report mortality and had major baseline imbalances with regards to age and APACHE scores of participants. Such deficiencies in reporting of trials in the Chinese literature have been previously documented (Zhang 2008). The randomized trial of Zhou et al (Zhou 2014) compared supine position alone versus two interventions, prone position combined with recruitment manoeuvres and was also excluded.
One systematic review (Yue 2017) listed Charron 2011 as a randomized clinical trial in their meta‐analysis. Re‐examination of this study data confirmed results were derived from a clinical database and not a randomized clinical trial.
Studies awaiting classification
There are no additional studies awaiting classification.
Ongoing studies
Three ongoing studies were identified. This included one trial (NCT03891212) comparing prone versus supine positioning in mechanically ventilated patients with severe pneumonia, and two trials (NCT04139733; NCT04607551) comparing prone versus supine positioning in mechanically ventilated patients receiving ECMO (see Characteristics of ongoing studies).
Risk of bias in included studies
We have graphically presented in Figure 2 review authors' assessment of bias within individual studies, and in Figure 3, bias across studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
Allocation sequence generation was of a high standard overall, with most studies employing computer‐generated sequences and blinding sequence allocation by using a computer‐telephone allocation system of sealed opaque envelopes. Allocation bias seems likely for the study of Chan et al (Chan 2007).
Blinding
Complete blinding of participants and clinical staff to allocation would be impossible because participants were placed either with face and feet up or with face and feet down. Some blinding of processes and decision making could be incorporated into trial procedures together with some standardised or protocolised approaches to important co‐interventions to improve methodological rigour. Such measures have not been systematically applied across studies.
Lack of blinding could affect application of important related co‐interventions (Cummings 2013) such as decisions on futility, non‐escalation of treatment, withdrawal of treatment or continuation of active treatment (Forbes 2013; Morgan 2014; Stapleton 2005; Turnbull 2014). We downgraded the quality of evidence assessed by the GRADE system in all analyses in which it was utilized as important clinical decisions would be made with full knowledge of treatment allocation (Jadad 2007). A double downgrade was considered but not applied. It is not clear whether investigators were blind to participant allocation when performing data analyses.
Incomplete outcome data
Most studies reported participants lost to follow‐up and used the intention‐to‐treat principle. Missing data for primary and some major secondary outcomes were small (0 to 5% of participants), and this was unlikely to affect interpretation of findings. However, for some secondary outcomes, the disparity in reporting rates between studies suggests differences in outcome definition, priority for data collection or efforts to minimize these complications.
Selective reporting
Selective reporting within studies was unlikely for the primary outcomes and for subgroup analyses in which death was the outcome of interest. Most studies were conducted at multiple centres, and a pre‐study protocol would define criteria for most reported study endpoints. Post hoc analyses might be at risk of selective reporting e.g. choice of 88 mmHg (11.7 kPa) PaO2/FIO2 quotient as cutoff for post hoc mortality subgroup analysis (Gattinoni 2001).
Other potential sources of bias
For most studies, cross‐over of participants from one limb of the study to another was modest. However, cross‐over or non‐adherence to the protocol was considerable for the study of Guerin 2004. Eighty‐one (21%) participants crossed over from supine to prone, and 170/413 (41%) in the prone group were never actually put in prone position, or the prone position was discontinued before the study met prone weaning criteria (Guerin 2004; Sud 2008). This effect would assume even greater importance in subgroup analyses of sicker participants that included an even higher proportion of cross‐over participants. Although strictly not bias, this will reduce the efficiency (Lipsey 1990) of a trial and will "silently" increase the risk of type II statistical error. Supplementary per‐protocol analysis (Hernan 2017; Sheiner 1995) would be useful for assessing the impact of cross‐overs and of partial and full protocol violations. In addition, one study described differential use of co‐interventions (e.g. blood transfusion, neuromuscular blockers) that would be expected to influence outcomes (Voggenreiter 2005). Participant losses for main analyses were small (0 to 4.2%), and reasons were detailed. Supplementary analyses were not performed as a result of these small participant losses. Several of the trials (Chan 2007; Fernandez 2008; Gattinoni 2001; Mancebo 2006; Voggenreiter 2005 ) were discontinued early which can also be a source of bias (Bassler 2010).
Effects of interventions
Before the last published trial (Guerin 2013) was included, statistical heterogeneity was low overall as assessed by the I2 method. Most analyses had an I2 statistic = 0. With inclusion of this last trial (Guerin 2013), heterogeneity was substantial, and heterogeneity for the primary analyses moved from 0% without the last study to 60% or greater with its inclusion (Analysis 1.1). Among subgroup analyses of mortality that included data from this trial (Guerin 2013), only one had an I2 statistic = 0, and the remaining nine analyses demonstrated I2 values ranging from 39% to 56%. With the last trial of Guerin excluded from the same analyses, all 10 trials had an I2 statistic = 0 (Analysis 1.3; Analysis 1.4; Analysis 1.6; Analysis 1.9; Analysis 1.11).
For reasons of inconsistency and heterogeneity, the quality of the evidence for primary outcomes based on the GRADE system was down‐rated further and was classified as low. The option of not exploring and analysing these results was avoided, and a random‐effects model was employed. The number of studies (<10) available for analysis were insufficient to justify meta‐regression techniques (Deeks 2019).
Fixed‐effect and random‐effects models were determined by I2 statistical value and are presented in the text as appropriate. Presentation of short‐ and longer‐term outcomes in the same forest plot has restricted use of one or the other model for these data pairs, and for some outcomes, minor discrepancies between text and figures may be noted for this reason.
Primary outcomes
Short‐term mortality
Eight clinical trials with 2117 participants reported on short‐term mortality (Chan 2007; Fernandez 2008; Gattinoni 2001; Guerin 2004; Guerin 2013; Leal 1997; Mancebo 2006; Taccone 2009) and were included in this analysis (Analysis 1.1). Overall mortality of participants was 756/2117 (35.7%). Mortality for those ventilated prone was 33.4% (363/1086), and supine 38.3% (395/1031) resulting in a risk ratio of 0.84 (95% CI 0.69 to 1.02) in favour of the prone position.
Prior to the inclusion of the most recent study (Guerin 2013), which exclusively enrolled participants with more severe hypoxaemia than was seen in earlier studies and had a risk ratio for mortality of 0.49, the risk ratio from other seven studies was close to unity at 0.95. In the Higgins test, the I2 statistic moved from 0% to 60% with inclusion of the most recent study (Guerin 2013). Visual inspection of the funnel plot was not supportive of major small study effect or reporting bias (Figure 4). Removal of one study, which applied prone ventilation for only one day (Leal 1997), did not alter the risk ratio, which remained at 0.84.

Funnel plot of comparison: 1 Mortality, outcome: 1.1 Mortality.
Longer‐term mortality
Eight clinical trials with 2140 participants (Chan 2007; Fernandez 2008; Gattinoni 2001; Guerin 2004; Guerin 2013; Mancebo 2006; Taccone 2009; Voggenreiter 2005) reported longer‐term mortality (952/2140), which overall approximated 44.5% (Analysis 1.1). Mortality for prone (462/1099; 42.0%) and supine (490/1041; 47.1%) ventilated participants resulted in a risk ratio of 0.86 (95% CI 0.72 to 1.03) in favour of the prone position. Before inclusion of the last study (Guerin 2013), which had an individual risk ratio of 0.58, the risk ratio from the other studies was again close to unity at 0.97. In the Higggins test (Higgins 2003), the I2 statistic moved from undetected (0%) to "moderate" heterogeneity at 61%, with the addition of Guerin 2013. Visual inspection of the funnel plot was not supportive of major small study effect or reporting bias (Figure 4).
Use of the GRADE system to assess the quality of evidence for major risks of bias from lack of blinding (Guyatt 2011a) and from inconsistency of effect (Guyatt 2011c) reduced the overall rating of evidence quality to "low" for both of these primary outcomes.
One‐year mortality
Only one study (and therefore not part of the quantitative meta‐analysis) reported 12‐month mortality (113/187) in a secondary publication approximating 60% mortality overall (Chiumello 2012). This population of 187 participants accounted for approximately 55% of the original study population. The point estimate for the risk ratio in this secondary study was 1.13 (95% CI 0.89 to 1.42) in favour of supine positioning in this single‐study post hoc analysis. This is a reversal from the findings the parent study (Taccone 2009) which reported a 6 month mortality risk ratio of 0.90 (95% CI 0.73‐1.11) in favour of prone positioning.
Results for primary outcomes and for selected subgroup analyses are included in summary of findings Table 1.
Secondary outcomes
Rate of ventilator‐associated pneumonia
Five studies (Ayzac 2016; Fernandez 2008; Guerin 2004; Mancebo 2006; Voggenreiter 2005) reported rates of ventilator‐associated pneumonia (VAP) with 1473 participants for analysis (Analysis 3.1). The overall rate of VAP for participants (226/1007) was 22.7%. The proportion of participants with VAP for prone positioning was 0.21 compared with 0.22 for the supine position. The risk ratio for VAP of 0.97 (95% CI 0.80 to 1.18) close to unity. The additional data from the PROSEVA trial (Ayzac 2016) for this amendment had the effect of shifting the point estimate closer to unity for this complication.
Number of days on a ventilator
Three studies (Fernandez 2008; Guerin 2004; Voggenreiter 2005) reported duration of mechanical ventilation in 871 participants (Analysis 4.1). Mean duration of ventilation was reduced by 0.47 days (95% CI ‐1.53 to 0.59) for participants in the prone position.
Length of ICU stay
Five studies (Fernandez 2008; Guerin 2004;Guerin 2013Mancebo 2006; Taccone 2009) with 1775 participants reported ICU length of stay (Analysis 5.1), which was increased for participants in the prone position by a mean of 1.06 (95% CI ‐1.13 to 3.26) days.
Analysis of log (base 10) transformed data provided similar results, with an increase (geometric mean) of 1.07 days for participants treated in the prone position (95% CI ‐1.3 to 1.5 days).
Length of hospital stay
Only one study (and therefore not part of the quantitative meta‐analysis) of 40 participants reported hospital length of stay. This very small study favoured the supine position by a mean of 5.8 (range ‐7.9 to 19.5) days.
Improvement in oxygenation
Four studies (Gattinoni 2001; Guerin 2004; Mancebo 2006; Voggenreiter 2005) with 827 participants reported improvement in oxygenation (PaO2/FIO2 ratio or quotient) over seven to 10 days (Analysis 6.1). The mean difference in improvement in the PaO2/FIO2 quotient was 24.6 mmHg (95% CI 13.9 to 35.2 mmHg) compared with baseline measurements at study entry. This equates to 3.3 kPa (95% CI 1.8 to 4.7 kPa) (P value < 0.00001). Variance for two studies (Guerin 2004; Mancebo 2006) was estimated by using the higher of the "paired" variances for the study population. Inflating the entered standard deviations by approximately 50% to 120.0 for these two studies had no impact on inferences. The second study of Guerin (Guerin 2013) was not included in the analysis because of the formal reduction in PEEP mandated by improving oxygenation.
One study (and therefore not part of the quantitative meta‐analysis) provided data for the PaO2/FIO2 quotient for a very small subset of participants (26) (Chiumello 2012) included in one of the primary studies (Taccone 2009; 342 participants) at 12‐month follow‐up. PaO2 data (Chiumello 2012) on air showed a change in the PaO2/FIO2 quotient of 43 mmHg (95% CI 15.8 to 70.2 mmHg) in favour of supine ventilation (P value = 0.002). This equates to a PaO2/FIO2 quotient of 5.7 kPa (95% CI 2.1 to 9.4 kPa).
Adverse events
Several adverse events were documented across studies and were reported in two different ways: Most reported events per participant group, but two studies reported some data as events per participant day. These were analysed separately.
New pressure sores or ulcers
Four studies (Chan 2007; Gattinoni 2001; Girard 2014; Voggenreiter 2005) with 823 participants reported pressure ulcer (or sore) events per participant per group (Analysis 7.1), and one additional study of 791 participants and 10,944 event days presented results on pressure sores as events per day. The four studies reported an event rate of 43% for participants ventilated prone and 34.2% for those ventilated supine, with a risk ratio of 1.25 (95% CI 1.06 to 1.48; P value = 0.01). The addition of data from the PROSEVA trial (Girard 2014) with a doubling of participants for analysis moved the point estimate closer to unity and increased the precision of that analysis. The single study (Guerin 2004) reporting events per day (and therefore not part of the quantitative meta‐analysis) reported pressure sores on 3.6% of event days in prone groups and 3.0% in supine groups, with an odds ratio of 1.20 (95% CI 0.97 to 1.48; P value = 0.09). Both analyses favoured the supine position to avoid this adverse event.
Tracheal tube displacement
Eight studies (Chan 2007; Fernandez 2008; Gattinoni 2001; Guerin 2004; Guerin 2013; Leal 1997; Taccone 2009; Voggenreiter 2005) of 2021 participants provided information on tracheal tube displacement or accidental extubation (Analysis 7.1). Participants ventilated prone experienced a 10.5% event rate compared with 9.2% among those ventilated supine. The risk ratio was 1.09 (95% CI 0.85 to 1.39).
Tracheal tube obstruction
Three studies (Guerin 2004; Guerin 2013; Taccone 2009) of 1599 participants reported the complication of tracheal obstruction. These three studies strongly favoured the supine position, although moderate heterogeneity was noted, with I2 statistic= 31% requiring use of a random‐effects model for analysis (Analysis 7.1). The overall incidence of tracheal obstruction for those ventilated prone was 15.9% compared with supine, which was 9.7%. The risk ratio was 1.78 (95% CI 1.22 to 2.60); P value = 0.003).
Pneumothorax
Four studies (Chan 2007; Fernandez 2008; Guerin 2013; Mancebo 2006) of 664 participants reported an event rate for pneumothoraces (Analysis 7.1), and one study (Guerin 2004) of 791 participants (and therefore not part of the quantitative meta‐analysis) reported pneumothoraces per participant day. The four studies reported an overall event rate of 6.6% for participants ventilated prone and 5.4% for those ventilated supine, with a risk ratio of 1.16 (95% CI 0.65 to 2.08). The largest single study reported risk for pneumothorax per participant day of 0.38% for prone ventilated participants and 0.54% for supine ventilated participants, with an odds ratio of 0.71 (95% CI 0.40 to 1.24).
Arrhythmias
Three studies (Guerin 2013; Mancebo 2006; Voggenreiter 2005) of 642 participants reported on the prevalence of arrhythmias including bradyarrhythmias and cardiac arrest, noting a rate of 15.3% for those ventilated prone and 24.7% for those ventilated supine (Analysis 7.1). This analysis was dominated by one study (Guerin 2013) which had a risk ratio of 0.64 (95% CI 0.47 to 0.87). One other study (Guerin 2004) of 791 participants and 10,942 event days (and therefore not part of the quantitative meta‐analysis) reported bradycardic episodes per participant day as well as cardiac arrests per participant day. For bradycardic episodes per participant day, the rate was 1.41% for prone ventilation and 1.39% for supine ventilation, with an odds ratio of 1.01 (95% CI 0.74 to 1.40). For cardiac arrest, the prevalence for prone ventilation was 1.51% per participant day and for supine 1.70% per participant day, with an odds ratio of 0.89 (95% CI 0.66 to 1.20).
Composite outcome of hypotension, arrhythmias and increased vasopressor use per participant day
This composite outcome was reported by one study (and therefore not part of the quantitative meta‐analysis) of 342 participants and 5524 participant days (Taccone 2009). The reported rate of such cardiovascular compromise was 18% for participants ventilated prone and 12.4% for those ventilated supine, with a risk ratio of 1.45 (1.28 to 1.65; P value < 0.00001) favouring the supine position.
Quality of life
Only one study (Chiumello 2012) (and therefore not part of the quantitative meta‐analysis) reported on quality of life for a small subset of 26 participants from five centres (187 participants) followed up from the Taccone 2009 study of 342 participants. The main quality of life metrics employed were the Short Form‐36 (SF‐36) questionnaire, which reported on eight items, and the Saint George's Respiratory Questionnaire (SGRQ), which reported on four items. For all domains in the SF‐36 questionnaire, results were similar for both groups. For all four SGRQ items, the prone group performed better, but none of these results were statistically significant.
With regards to pulmonary function assessment with standard pulmonary function tests and quantitative evaluation of CT scans, 15 items were evaluated. Two results were statistically significant, and one was of borderline significance. These were PaO2 (P value = 0.03) ‐ reported as the PaO2/FIO2 quotient in the oxygenation section above; and over‐aerated lung tissue on CT scan analysis of 12.5% of total lung weight for participants treated prone versus 5.3% for those treated supine (P value = 0.008). Mean results for well‐aerated lung tissue between groups showed 64.0% for participants treated prone versus 70.2% for those treated supine (P value = 0.052).
Economic outcomes
None of the identified primary papers provided data on economic outcomes. One economic analysis (Baston 2019) is available modelled on results from most recent trial of Guerin (Guerin 2013) and an observational study (Bellani 2016). They conclude based on short‐term mortality outcomes and after extensive modelling, interventions that increase utilization of prone positioning would be cost‐effective from both societal and hospital perspectives under many plausible cost and benefit assumptions. However this modelling is based on the results of a single unblinded trial that has been described as having, "a treatment effect virtually unprecedented in modern medicine." (Soo Hoo 2013). Baston et al did not take into account any requirement for increased staffing required to accomplish patient‐turning in sparsely staffed ICUs.
Planned subgroup analyses (SGA)
Analyses combining short‐ and longer‐term mortality allow for one model (fixed‐effect or random‐effects) only per analysis. In two cases (Analysis 1.6; Analysis 1.10), short‐ and longer‐term analyses required different models. Results presented in the text show actual result based on the correct model. All other analyses presented are correct.
Duration of daily ventilation in the prone position (< 16 hours/d vs ≥ 16 hours/d)
Mean daily application of prone ventilation for the nine included studies (Chan 2007; Fernandez 2008; Gattinoni 2001; Guerin 2004; Guerin 2013; Leal 1997; Mancebo 2006; Taccone 2009; Voggenreiter 2005) was 16.3 hours (range 7 to 24 hours/d) given over a mean of 6.2 days (range 1 to 11.9 days). Mean total hours of prone ventilation for participants in each study ranged from 24 hours (Leal 1997) to 238 hours (Fernandez 2008), with a mean of 100 hours across included studies.
Two studies (Gattinoni 2001; Guerin 2004) of 1095 participants reported short‐term mortality for participants ventilated less than 16 hours/d in the prone position (Analysis 1.2). Mortality was 37.3% for participants ventilated prone and 36.2% for those ventilated supine, yielding a risk ratio for mortality of 1.04 (95% CI 0.89 to 1.21). Three studies (Gattinoni 2001; Guerin 2004; Voggenreiter 2005) of 1135 participants reported on longer‐term mortality for participants ventilated in the prone position for less than 16 hours per day. Mortality was 47.1% for participants ventilated prone and 45.9% for those ventilated supine, yielding a risk ratio for mortality of 1.03 (95% CI 0.92 to 1.17).
Six studies (Chan 2007; Fernandez 2008; Guerin 2013; Leal 1997; Mancebo 2006; Taccone 2009) of 1022 participants reported on short‐term mortality for participants ventilated 16 or more hours per day, with moderate heterogeneity identified (I2 statistic = 41%) (Analysis 1.3). Short‐term mortality was 29.2% for participants ventilated prone and 40.5% for those ventilated supine, yielding a risk ratio of 0.73 (95% CI 0.58 to 0.93; P value = 0.01). Five studies (Chan 2007; Fernandez 2008; Guerin 2013; Mancebo 2006; Taccone 2009) of 1005 participants also reported longer‐term mortality of participants ventilated prone for 16 or more hours per day. Longer‐term mortality was 36.1% for those ventilated prone and 48.6% for those ventilated supine, with a risk ratio of 0.77 (95% CI 0.61 to 0.99; P value = 0.04).
The statistical test for subgroup differences for longer‐term outcomes regarding daily duration of prone ventilation was significant (P value = 0.03; I2 statistic = 78.0%), which provides stronger evidence for the benefit of longer duration prone position ventilation (Analysis 2.1). The quality of the evidence as rated by GRADE was moderate (summary of findings Table 1), with downgrading based on the potential for risk of bias.
Duration of supine ventilation before randomization (< 48 hours vs ≥ 48 hours)
Five studies (Fernandez 2008; Guerin 2013; Leal 1997; Mancebo 2006; Taccone 2009) of 1000 participants enrolled most participants within 48 hours of initiation of mechanical ventilation, allowing exploration of effects on short‐term mortality (Analysis 1.4). Moderate heterogeneity was noted (I2 statistic = 51%). Short‐term mortality among prone participants was 29.0% compared with 40.6% among those in the supine group, with a risk ratio of 0.72 (95% CI 0.56 to 0.93; P value = 0.01). Five studies (Fernandez 2008; Guerin 2013; Mancebo 2006; Taccone 2009; Voggenreiter 2005) of 1024 participants enrolled most of their participants up to 48 hours after initiation of mechanical ventilation with regards to longer‐term mortality (Analysis 1.4). Moderate heterogeneity (I2 statistic = 50%) was noted. Longer‐term mortality among prone participants was 34.3% compared with 46.9% in participants assigned to supine ventilation, with a risk ratio of 0.75 (95% CI 0.59 to 0.94; P value = 0.01).
Three studies (Chan 2007; Gattinoni 2001; Guerin 2004) of 1117 participants enrolled most participants more than 48 hours after initiation of mechanical ventilation (Analysis 1.5). Short‐term mortality for prone participants was 37.7% compared with 36.2% in the supine group, with a risk ratio of 1.04 (95% CI 0.89 to 1.21). For longer‐term mortality three studies (Chan 2007; Gattinoni 2001; Guerin 2004) of 1116 participants enrolled participants after 48 hours or did not state enrolment time. For those ventilated prone, reported mortality was 48.6% compared with 47.2% for those ventilated supine. The overall risk ratio was 1.04 (95% CI 0.92 to 1.17).
The statistical test for subgroup differences for longer‐term outcomes regarding timing of enrolment for prone ventilation was significant (P value = 0.01; I2 statistic = 84.4%), providing stronger evidence for the benefit of longer duration of prone positioning (Analysis 2.2). The quality of evidence as rated by GRADE was moderate (summary of findings Table 1), with downgrading based on the potential for risk of bias.
Outcome according to severity (PaO2/FIO2 ratio; severity of illness score, e.g. Simplified Acute Physiology Score II (SAPS II); oxygenation index)
With regards to short‐term outcomes, six studies (Gattinoni 2001; Guerin 2004; Guerin 2013; Leal 1997; Mancebo 2006; Taccone 2009) of 744 participants explored the effects of prone position in a subset of participants with severe hypoxaemia ‐ PaO2/FIO2 quotient < 150 mmHg (< 20.0 kPa) (Leal 1997); < 105 mmHg Guerin 2013); or < 100 mmHg (< 13.3 kPa) ‐ and in four others based on reanalysis of original data (Gattinoni 2010; Sud 2010). For short‐term mortality among participants with severe hypoxaemia (Analysis 1.6), adoption of prone ventilation was associated with 40.6% mortality in comparison with mortality of 50.1% for those ventilated supine, yielding a risk ratio of 0.80 (95% CI 0.68 to 0.93; P value = 0.003) when a fixed‐effect model was used with I2 statistic = 0. (The figure in the analysis presents results of the random‐effects model, as longer‐term outcomes required application of a random‐effects model.) Twenty‐eight‐day mortality data (as opposed to short‐term mortality) resulting from the combination of original studies and a review (Gattinoni 2010) yielded near identical results, with a risk ratio of 0.80. For longer‐term mortality, seven studies (Chan 2007; Fernandez 2008; Gattinoni 2001; Guerin 2004; Guerin 2013; Mancebo 2006; Taccone 2009) of 977 participants with severe hypoxaemia recorded mortality of 41.5% for participants ventilated prone and 54.7% for those ventilated supine, with a risk ratio of 0.77 (95% CI 0.65 to 0.92; P value = 0.003) when a random‐effects model was used (Analysis 1.6). Moderate heterogeneity was detected (I2 statistic = 39%). These results for short‐term and longer‐term mortality remained significant without inclusion of the most recent trial (Guerin 2013), which itself recorded highly significant results for short‐ and longer‐term mortality (P value < 0.001 for both time periods in favour of prone positioning). The quality of the evidence as rated by GRADE was moderate (summary of findings Table 1), with downgrading based on the potential for risk of bias.
For participants with less severe hypoxaemia, no apparent benefit was observed (Analysis 1.7). Short‐term mortality from four trials (Gattinoni 2001; Guerin 2004; Mancebo 2006; Taccone 2009) of 1095 participants with milder hypoxaemia (PaO2/FIO2 ≥ 100 mmHg to 300 mmHg) failed to establish benefit of prone positioning, with a risk ratio of 1.03 (95% CI 0.87 to 1.21; I2 statistic = 0). Although data from one other study (Guerin 2013) were available, this study included only participants with PaO2/FIO2 ≥ 105 mmHg to 150 mmHg and did not reflect the full spectrum of milder disease, as was evident in the other studies. Therefore, this study was excluded from the analysis. Data were also available from six studies (Chan 2007; Fernandez 2008; Gattinoni 2001; Guerin 2004; Mancebo 2006; Taccone 2009) of 1108 participants undertaken to explore longer‐term effects of the prone position applied in milder hypoxaemia (PaO2/FIO2 > 100 mmHg to 300 mmHg). The risk ratio for this group of participants was 1.06 (95% CI 0.93 to 1.21) and heterogeneity was negligible (I2 statistic = 1%). For long‐term outcomes with regards to severity of hypoxaemia, the statistical test for subgroup differences (Analysis 2.3) was significant (P value = 0.005; I2 statistic = 85.7%).
Two studies (Gattinoni 2001; Mancebo 2006) provided sufficient data to allow exploration of the effects of physiological severity of illness on outcome, with data for one study derived from a journal comment (Sud 2008b). Heterogeneity between studies was considerable. For participants (327) with an SAPS II score of 49 or less, short‐term mortality was 25.8% among those ventilated prone in comparison with 28.5% in those ventilated supine, yielding a risk ratio of 0.85 (95% CI 0.45 to 1.60; I2 statistic = 69%) (Analysis 1.8). For participants (113) with greater severity of illness (SAPS II ≥ 50), short‐term mortality among those ventilated prone was 34.7% and 56.8% for those ventilated supine, with a risk ratio of 0.60 (95% CI 0.25 to 1.40; I2 statistic = 79%). Amalgamated data for two different time intervals (Gattinoni 2001 provided 10‐day mortality data and Mancebo 2006 provided ICU mortality data) were not available for analysis of longer‐term mortality.
Data regarding oxygenation index, most commonly reported in paediatric studies, were not available for analysis. (Oxygenation index was calculated as mean airway pressure × FIO2 × 100/PaO2 in mmHg and was expressed as a unit‐less number.)
Tidal volume (6 to 8 mL/kg vs > 8.0 mL/kg of ideal body weight)
Three studies (Chan 2007; Guerin 2013; Taccone 2009) of 830 participants reported on the effects of ventilation with lower tidal volumes (mean of 6 to 8 mL/kg ideal body weight) on short‐term mortality (Analysis 1.9). Mortality for the prone subgroup was 25.5% compared with 36.7% among those ventilated supine. The risk ratio was 0.72 (95% CI 0.43 to 1.20; P value = 0.2). Substantial heterogeneity was noted (I2 statistic = 76%). Five studies (Chan 2007; Fernandez 2008; Guerin 2013; Taccone 2009; Voggenreiter 2005) of 910 participants reported on longer‐term mortality among participants ventilated with low tidal volumes (mean 6 to 8 mL/kg ideal body weight). Mortality for those ventilated prone was 32.5% and for those ventilated supine 45.1%, with a risk ratio of 0.73 (95% CI 0.53 to 0.96; P value = 0.02). Heterogeneity was moderate (I2 statistic = 43%).
Three studies (Gattinoni 2001; Guerin 2004; Mancebo 2006) of 1231 participants utilized high tidal volumes (mean > 8.0 mL/kg ideal body weight) and reported on short‐term mortality (Analysis 1.10). Mortality for participants ventilated prone was 38.1% and for participants ventilated supine was 38.5%, with a risk ratio of 0.99 (95% CI 0.86 to 1.14; I2 statistic = 38%; random‐effects model). Those studies (Gattinoni 2001; Guerin 2004; Mancebo 2006) with 1231 participants also reported on longer‐term mortality among participants ventilated with high tidal volumes. Mortality for those ventilated prone was 48.8% and for participants ventilated supine 48.5%, with a risk ratio of 1.01 (95% CI 0.9 to 1.13; I2 statistic = 19%; fixed‐effect model).
We categorized studies on the basis of mean tidal volumes (mL/kg) derived from ideal body weight (IBW) as provided by primary studies or imputed from actual body weight data. Two studies provided no measurements (Leal 1997; Voggenreiter 2005). The upper 95% confidence limit for tidal volumes was 7.3, 9.4, 9.8, 11.3, 14.6, 14.7 and 15.8 mL/kg IBW for the seven studies of Chan 2007; Fernandez 2008; Gattinoni 2001; Guerin 2004; Guerin 2013; Mancebo 2006 and Taccone 2009. Notably, only one study (Guerin 2013) actually achieved the 6 to 8 mL/kg ideal body weight envelope in terms of the 95% CI approximating what is currently considered best clinical practice (Needham 2012).
A random‐effects model used to test for subgroup differences between low and high tidal volume ventilation strategies yielded significant findings (P value = 0.04; I2 statistic = 76.5%), strengthening evidence for the prone position in combination with lower tidal volumes (Analysis 2.4). The quality of evidence as rated by GRADE was moderate (summary of findings Table 1), with downgrading based on the potential for risk of bias.
Analysis of studies of ALI and ARDS separate from other causes of acute severe hypoxaemic respiratory failure
Seven studies (Chan 2007; Fernandez 2008; Gattinoni 2001; Guerin 2013; Leal 1997; Mancebo 2006; Taccone 2009) were included in this subgroup analysis of 1326 participants ventilated for ARDS with regards to short‐term mortality (Analysis 1.11). Data from Guerin's first study were not included, as inclusion criteria for participants were broader than the other clinical trials (Guerin 2004). Mortality for those ventilated prone in these subgroups of ARDS participants was 34.0% compared with 42.6% for those ventilated supine. The risk ratio was 0.79 (95% CI 0.63 to 1.00; P value = 0.05). Heterogeneity was moderate (I2 statistic = 57%).
Eight studies (Chan 2007; Fernandez 2008; Gattinoni 2001; Guerin 2004; Guerin 2013; Mancebo 2006; Taccone 2009; Voggenreiter 2005) were included in this subgroup analysis of 1758 participants ventilated for ARDS with regards to longer‐term mortality. Ninety‐day mortality for ARDS participants (PaO2/FIO2 quotient < 300 mmHg) from the first study of Guerin (Guerin 2004) became available through a recent meta‐analysis (Sud 2014). Very minor adjustments were made to original data from another trial (Gattinoni 2001) on the basis of information obtained from this same meta‐analysis. Mortality for those ventilated prone in these subgroups of ARDS participants was 41.3% compared with 48.3% for those ventilated supine. The risk ratio was 0.85 (95% CI 0.71 to 1.01; P value = 0.07), and heterogeneity was moderate (I2 statistic = 56%). The quality of the evidence as rated by GRADE was moderate (summary of findings Table 1), with downgrading based on the potential for risk of bias.
Pulmonary and extrapulmonary causes of ALI or ARDS
Data were insufficient to allow any analysis.
Use of meta‐regression to explore heterogeneity between subgroups
Identified studies were insufficient to meet criteria for use of meta‐regression techniques (Deeks 2011).
Sensitivity analysis based on potential risk of bias or confounding
Removing studies on the basis of potential risk of bias or confounding had little effects on most results. Excluding the studies of Guerin (Guerin 2004) on the basis of the high percentage of cross‐over participants; of Voggenreiter (Voggenreiter 2005) because of the hugely disparate blood transfusion requirements between groups and differential use of muscle relaxants; and of Chan (Chan 2007) because all risk of bias assessments were rated as "unclear" or "high" (Figure 2), produced a small shift in risk ratio for short‐term mortality from 0.84 to 0.79 (95% CI 0.61 to 1.01), and from 0.87 to 0.82 (95% CI 0.65 to 1.04) for longer‐term mortality.
Discussion
Summary of main results
The main findings of this review are presented here.
Primary outcomes
Among all‐comers entered into identified randomized but unblinded clinical trials, a statistically insignificant signal of benefit was seen for prone ventilation, with risk ratios of 0.84 and 0.86 for short‐term and longer‐term mortality. The last published trial (Guerin 2013) approximately halved mortality in its cohort of more severely hypoxaemic participants compared with other included studies, and changed heterogeneity as measured by the I2 statistic from 0% to 60% or more for both primary outcomes. The risk ratio before publication and inclusion of this study was close to unity. This suggests that unselected participants with moderate to severe hypoxaemia requiring mechanical ventilation and ventilated in the prone position may be too diffuse a target population for this intervention. When the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) system was applied, evidence for benefit in unselected populations was rated low (summary of findings Table 1), as the overall rating of quality of evidence was downgraded as a result of risk of bias and inconsistency (Guyatt 2008; Guyatt 2011a; Guyatt 2011c). Longer‐term mortality would seem a more important patient‐centred outcome when compared with short‐term mortality for primary outcomes and for prespecified subgroup analyses of mortality (Hough 2012; Wang 2014; Williams 2008), and formal application of the GRADE approach was limited to primary outcomes and to selected subgroup outcomes for longer‐term mortality only.
One trial later reported a subset of 187 participants, for whom additional 12‐month mortality data were reported (Chiumello 2012). This subset from five centres based in or near Milan, Italy, comprised more than 50% of the population of the original or primary trial (Taccone 2009). For this subset, there was no evidence of benefit for prone ventilation in unselected participants with regards to 12‐month mortality, as the risk ratio was slightly greater than unity (favouring supine positioning), although findings were statistically insignificant. We note this trial (Taccone 2009) was the second most recent published trial and employed low tidal volume ventilation.
With regards to heterogeneity, primary outcomes fell into the moderate heterogeneity category (Higgins 2003), and formal analysis was undertaken with a random‐effects model, wherein the I2 statistic exceeded 25%. In addition, recommended approaches for exploring heterogeneity through pre‐specified subgroup analyses and for excluding studies in sensitivity analyses were undertaken. With only eight studies available for each of the two primary outcomes (short‐term mortality ‐ Chan 2007; Fernandez 2008; Gattinoni 2001; Guerin 2004; Guerin 2013; Leal 1997; Mancebo 2006; Taccone 2009; and longer‐term mortality ‐ Chan 2007; Fernandez 2008; Gattinoni 2001; Guerin 2004; Guerin 2013; Mancebo 2006; Taccone 2009; Voggenreiter 2005), we did not utilize meta‐regression techniques, in accordance with best practice (Deeks 2011).
Secondary outcomes
Pneumonia
Ventilator associated pneumonia (VAP) is an important complication, which definitely increases resource utilization and prolongs intensive care unit (ICU) and hospital length of stay with uncertain attributable mortality. Analysis of data from nearly 1500 participants after the addition of data from the PROSEVA trial (Ayzac 2016) showed little signal of benefit from prone positioning with regards to VAP. The incidence of VAP varied across studies, and to what extent this was driven by different patient populations (patient diversity) and criteria used to diagnose pneumonia (methodological diversity) is uncertain. The diagnosis of ventilator‐associated pneumonia is problematic, given the various criteria in clinical use (Klompas 2008; O'Brien 2011; Stevens 2014; Sud 2008) over the 15‐year time span of these clinical trials.
Duration of mechanical ventilation
Duration of mechanical ventilation was reported in three studies of more than 800 participants (Fernandez 2008; Guerin 2004; Voggenreiter 2005). A small signal suggested benefit from prone positioning. However, the point estimate amounted to less than a half‐day and cannot be considered a major patient‐centred benefit. Such data are complicated to interpret due to differential patient mortality between groups, which will affect time data such as duration of mechanical ventilation and length of stay.
Length of stay (LOS)
Length of stay (LOS) data are difficult to interpret in that they are often skewed (Weissman 1997), and LOS will be influenced in diverse and opposite ways by the effectiveness of treatment. LOS may be reported as median and interquartile range (IQR), and sometimes as mean and standard deviation. The former data pose difficulties for meta‐analysis, although they can be used if it is assumed that the median approximates the mean together with a statistical multiplication factor used to impute the standard deviation (Higgins 2011b). For skewed data, reporting of means and standard deviations may be misleading. It is recommended that both should be reported (Weissman 1997). Furthermore, effective treatment may reduce the LOS of participants already destined to survive but will lengthen the stay of those who would have died but have survived as a result of receiving the intervention. The overall effect will be determined by the balance of these two effects.
In this systematic review, mean and standard deviation were imputed for one study on the basis of non‐parametric data (Taccone 2009). Point estimates for ICU LOS were similar with and without this study and favoured supine, with the mean difference in LOS between 1.34 and 1.37 days and not statistically significant. Only one study (Fernandez 2008) of 40 participants reported on hospital LOS; this again favoured supine ventilation, with the point estimate showing a difference of 5.8 days. Reduction in ICU LOS was not apparent with the use of prone ventilation in the four relevant studies (Fernandez 2008; Guerin 2004; Mancebo 2006; Taccone 2009). Data for hospital LOS were too sparse to allow meaningful comment.
Improved oxygenation
Improved oxygenation in participants ventilated prone was apparent at seven to 10 days in the outcome studies included in this systematic review. The mean difference in the PaO2/FIO2 quotient of 24.6 mmHg or 3.3 kPa is clinically meaningful and was statistically highly significant (P value < 0.00001). In a very small subset of participants (26) from the original Taccone trial (384 participants) examined at 12 months, residual benefit was not apparent, and a small but statistically significant benefit favoured supine‐ventilated participants (Chiumello 2012). Thus oxygenation was substantially improved while participants were critically ill (Analysis 6.1), but robust evidence that this benefit is carried on to or beyond 12 months was not available.
We did not include the second study of Guerin (Guerin 2013) in the analyses, as formally mandated reduction in PEEP would negatively impact oxygenation and would confound such results.
Adverse effects
Studies show that pressure sores and tracheal tube obstruction were increased by mechanical ventilation provided in the prone position. Cardiac arrhythmias were reduced with use of the prone position. This was described in different ways by different studies and required separate analyses for the same complication, sometimes leading to inconsistent results. An important factor for interpretation is how vigorously these events were classified and sought within individual studies (Bent 2006; Ioannidis 2006).
-
With regards to pressure ulcers, four studies (Chan 2007; Gattinoni 2001; Girard 2014; Voggenreiter 2005) demonstrated a statistically significant effect of pressure sores per participant among those ventilated prone (P value = 0.02). Another single study, reporting in such a way that it could not be included in the meta‐analysis, demonstrated the same trend but with borderline statistical significance (P value = 0.09). All five studies favoured the supine position with regards to development of pressure sores. This finding would be consistent with the area of tissue in contact with the bed during supine and prone ventilation and is biologically plausible.
-
Tracheal tube displacement, which might be considered a natural consequence of moving patients from supine to prone position and back, showed differing results across studies, with moderate statistical heterogeneity. For example, the short‐term (24‐hour) study of Leal 1997 reported 50% tracheal tube displacement, whereas Chan 2007, which utilized at least 72 hours of prone positioning per participant, reported a zero rate of displacement. Overall the risk ratio was 1.09 and was statistically insignificant. However, a clear increase in risk of tracheal tube obstruction was evident. Such obstruction might result from increased inspissated secretions or from kinking of the tracheal tube in the face‐down participant. The risk ratio for this complication was 1.78 and was statistically significant (P value = 0.003).
-
Pneumothoraces were counted as events per participant in four studies (Chan 2007; Fernandez 2008; Guerin 2013; Mancebo 2006), and as events per participant day in one study (Guerin 2004). Three studies favoured the supine position (Chan 2007; Guerin 2013; Mancebo 2006), and two favoured the prone position (Fernandez 2008; Guerin 2004): Evidence favouring one position or another is weak.
-
With regards to arrhythmias or bradycardias results from different studies are not concordant. The most recent study (Guerin 2013) heavily influences overall findings for the incidence of arrhthymias The point estimate was 0.64 (P value = 0.005) in favour of the prone position. A statistically insignificant trend from a single study (Guerin 2004) also favoured the prone position with regards to cardiac arrests. However, Taccone 2009, when using the composite endpoint of "hypotension, arrhythmias or increased vasopressor requirements", strongly favoured the supine position (P value = 0.001) (Glantz 2005).
-
Small clinical trials may not reliably quantitate the incidence of uncommon adverse effects: Ocular complications are described among patients undergoing undergoing general anaesthesia, for therapeutic purposes, with prone positioning an associated risk factor, and the incidence of perioperative visual loss ranges between 0.028% and 1.3% (Uribe 2012) in this setting. Permanent blindness can result from ischaemic optic neuropathy or from central artery occlusion, and the zero numerator from this systematic review of 1107 prone participants still indicates a 95% confidence interval of 0 to 0.27% for the incidence of such events (Hanley 1983). Clinicians should remain vigilant for ocular complications, given the potentially important long‐term consequences; a recent abstract has highlighted one such case (Ayoubieh 2014). Brachial Plexus injury is also a potential serious long‐term injury that may result from prone positioning (Goettler 2002)
It is difficult to gauge the relevance of some of the reported findings in terms of the methodological rigour of their detection (Ioannidis 2006) and their clinical importance. Guidelines have been produced to assist prevention of such complications (Faculty of Intensive Care 2019).
Quality of life (QOL)
With regards to quality of life (QOL), only one study of 26 participants has addressed this issue ‐ Chiumello 2012. No clear benefit was seen in this very small study, which encompassed a subgroup of participants originating in the Taccone 2009 trial. Firm conclusions with such a small number of participants would seem inappropriate. More evidence is required.
Intensive care patients comprise a diverse population of individuals admitted from all different hospital specialities, and the aetiology of acute respiratory distress syndrome (ARDS) is also varied (Walkey 2012). The more inclusive umbrella of hypoxaemic respiratory failure is even more disparate. This participant heterogeneity reduces the power of studies and increases the sample size required to avoid type II statistical error (Lipsey 1990). The power of studies to detect differences in outcome is hindered by participants who have crossed over to the opposite treatment, when results are analysed using intention to treat analyses only. Cross‐overs occurred in several studies to a greater or lesser extent (34% of participants in one study, Guerin 2004). This may be important for this systematic review, for which participant numbers available for exploratory analyses are only modest to moderate. Given the importance of optimum treatment of severely hypoxaemic patients in ICUs, it is disappointing that five studies had to be terminated prematurely because of poor participant accrual (Chan 2007; Fernandez 2008; Gattinoni 2001; Mancebo 2006; Voggenreiter 2005).
The almost complete absence of long‐term survival data (12 months and beyond), physiological function data, QOL life data and economic data is notable and is a major limitation with regards to overall evaluation of the benefits (or otherwise) of prone positioning as an adjunct to conventional mechanical ventilation. Such data are likely to be more relevant to patients, their families and society, when compared with short‐term mortality outcomes alone (Herridge 2011; Hough 2012; Wang 2014).
Subgroup analyses
Given clinical diversity in terms of diagnoses and severity of illness (hypoxaemia), as well as methodological diversity, which has contributed to substantial statistical heterogeneity, pre‐specified exploration of subgroups was warranted, and data will be of interest to stakeholders.
Important issues and limitations associated with subgroup analysis include reduced statistical power, increasing type II statistical error; multiple statistical testing, increasing type I error and ecological fallacy in study‐level meta‐analyses. The multiple subgroup analyses reported below should be viewed in this light (Counsell 1994; Lagakos 2006; Oxman 1992; Reade 2008; Sun 2014) as well as noting the relatively few studies (8 or less) which were available for analysis in each subgroup.
Subgroup analyses are presented for short‐term (10 to 30 days) and longer‐term mortality (31 to 180 days, or hospital mortality). As mentioned earlier, longer‐term mortality would seem more important than short‐term mortality from the patient perspective, given reduced longer‐term survival and the ongoing burden of disease following acute lung injury and intensive care stay (Herridge 2011; Hough 2012; Iwashyna 2010; Wang 2014; Williams 2008). Five subgroups are included in the summary of findings Table 1, and all subgroup analyses were downgraded on the basis of potential for important risk of bias. Downgrading of evidence as a result of imprecision was considered on the basis of Figure 5 and Table 1 of Guyatt and colleagues (Guyatt 2011b), both of which base achievement of optimal information size (OIS) on sample size or number of events. Four of the subgroup analyses of longer‐term mortality (Analysis 1.3; Analysis 1.4; Analysis 1.6; Analysis 1.11) clearly met suggested requirements for OIS, with the number of events (deaths) in the subgroup analyses ranging from 411 to 736. For the remaining analysis (Analysis 1.9) exploring the subset of participants ventilated with lower tidal volumes (summary of findings Table 1), events were fewer, at 353. Nevertheless, we also judged the OIS to have been met by taking into consideration the control event rate and the actual relative risk reduction in this subgroup. Although all subgroup analyses demonstrated substantial heterogeneity, as indexed by I2 statistical methods, further downgrading on the basis of inconsistency for these analyses was considered but not implemented, also in keeping with the approach recommended by Guyatt and colleagues (Guyatt 2011c).
A relatively small number of studies are available for these analyses and they must all be interpreted with appropriate caution. For random effects models adjustments or alternatives to the DerSimmonian‐Laird approach used in REVMAN such as the Hartung‐Knapp‐Sidik‐Jonkman adjustment are recommended in the current Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2019). These approaches would likely widen confidence intervals in random‐effects model analyses (Borenstein 2019; Graham 2020).
Duration of prone ventilation
First, the duration or "dose" of prone ventilation might have an impact on outcomes, and we examined the effects of short periods and longer periods of prone ventilation per day. Short periods of ventilation in the prone position appeared to confer no benefit for participants with a risk ratio very close to unity. Periods of prone ventilation for 16 or more hours per day yielded point estimates of 0.73 and 0.75, which were statistically significant for both short‐term (P value = 0.01) and longer‐term mortality (P value = 0.04). We rated the quality of evidence as moderate using the GRADE structure (summary of findings Table 1). We calculated dose of prone ventilation (with a two‐hour change in cutoff) as per our published protocol (Bloomfield 2009). Other methods not employed in this review might also be considered. Total dosage of prone positioning might be equally valid and might produce different results. For example, the most recent trial (Guerin 2013), despite prone positioning participants for 17 hours per day, applied it for only four days (68 hours), and in terms of total hours prone for participants ranks as the fourth shortest across the nine included trials (Characteristics of included studies), after Leal 1997, Gattinoni 2001 and Guerin 2004. Two of the studies excluded from our review but not from others (Characteristics of excluded studies) applied prone ventilation for a single episode of 12 hours (Demory 2007; Papazian 2005), and two other excluded studies applied prone positioning over six days, for a total of 24 hours only (Beuret 2002; Watanabe 2002).
Timing of intervention
We investigated whether early intervention offered an advantage as a strategy with the potential to ameliorate lung injury, as adoption later in the illness might limit benefit. Short‐term mortality and longer‐term mortality analyses of available data showed a risk ratio close to unity for three studies (Chan 2007; Gattinoni 2001; Guerin 2004), which enrolled more than 1000 participants after 48 hours. Participants enrolled earlier in five other studies (short‐term mortality ‐ Fernandez 2008; Guerin 2013; Leal 1997; Mancebo 2006; Taccone 2009; longer‐term mortality ‐ Fernandez 2008; Guerin 2013; Mancebo 2006; Taccone 2009; Voggenreiter 2005) demonstrated a large effect favouring prone ventilation, with risk ratios of 0.72 and 0.75, which were statistically significant (P values = 0.01 and 0.01) for short‐term and longer‐term mortality for a participant sample of 1000 or more. The quality of the evidence was rated as moderate when the GRADE structure was applied (summary of findings Table 1).
Severity of injury
It has been postulated that prone positioning might benefit participants with the most severe lung insult, and data are available from original trials and from further published analyses of the original trials (Gattinoni 2010; Sud 2010). With all trials included that provided data for participants with the most severe hypoxaemia, a large and statistically significant apparent benefit can be seen, with point estimates of 0.80 and 0.74 for short‐ and longer‐term mortality (P values = 0.003 and 0.003). The quality of the evidence was rated as moderate according to the GRADE structure (summary of findings Table 1). Removing data for two additional studies (Gattinoni 2001; Guerin 2004) provided by Sud et al, in which the precise timing of mortality assessment was not specified (Sud 2010), did not change the outcome of this subgroup analysis. Prone ventilation of participants with milder hypoxaemia appeared to confer no benefit, with risk ratios of 1.03 and 1.06 for short‐ and longer‐term mortality. However, the second study of Guerin et al (Guerin 2013) was influential in the overall analysis: Overall short‐term mortality in control groups of the other studies that reported participants with severe hypoxaemia was 58.5%, with mortality of 49.6% among participants treated prone. These rates differ substantially from those of Guerin et al (Guerin 2013), who reported percentage rates of 33.9 and 20.7 with absolute risk reductions of 8.9% for all other studies and 13.2% for Guerin et al. Of particular note is the much lower control mortality observed in the study of Guerin et al compared with other studies which might be explained by the more rigid application of available evidence‐based practices not fully utilized by earlier investigators (ARDS Network 2000). However, this does not fully explain the apparent differences in absolute risk reduction resulting from application of prone positioning.
With regards to overall severity of acute illness (SAPS II scoring system), heterogeneity between studies was considerable. Total numbers of participants studied and actual events (deaths) were low, generating unacceptable imprecision (Guyatt 2011b) which further reduces the relevance and credibility of this analysis. Additionally, two different short‐term outcomes were reported and amalgamated (Gattinoni 2001;.Mancebo 2006; Alsaghir 2008; Sud 2008b): Gattinoni 2001 provided 10‐day mortality data for analysis (70 deaths), whereas Mancebo 2006 provided ICU mortality data. ICU mortality data from Gattinoni 2001 would have provided another 80 deaths for analysis, and the comment in this paper that “These differences in [10 day] mortality rate did not persist after discharge from the intensive care unit (data not shown)” suggests limited relevance of these published data. Use of a random‐effects model to combine data demonstrated lower mortality for participants ventilated in the prone position for both lower and higher severity of illness, but with wide confidence intervals. Both studies were conducted during the high tidal volume ventilation era, making their results even less relevant in the low tidal volume ventilation era. For multiple reasons, as listed above, available data do not support severity of acute illness (SAPS II) as a basis for selection of participants for application of prone ventilation.
Ventilation strategy
As mentioned in the previous section, before publication of the first ARDS Network study (ARDS Network 2000), high tidal volume ventilation was in widespread use, but since low tidal volume ventilation has become the standard of care in clinical trials of adult patients, it is increasingly used in clinical practice (ARDS Network 2000; Needham 2012; Petrucci 2013). Studies conducted before adoption of this standard may be carried out differently and may be less relevant to current practice (Verbrugge 2007). For studies using higher tidal volume ventilation, both short‐term and longer‐term risk ratios for mortality were close to unity. All four studies (Gattinoni 2001; Guerin 2004; Leal 1997; Mancebo 2006) totaling 1200 participants commenced recruitment of participants before the ARDS Network study was published (ARDS Network 2000). Slightly smaller numbers of participants (830 to 911) from identified trials were available for analysis of low tidal volume strategies. All of these trials except the most recent (Guerin 2013) did not achieve tidal volumes of 6 mL/kg of ideal body weight, and low tidal volumes were considered to be 6 to 8 mL/kg of ideal body weight for pragmatic reasons. These showed a risk ratio in favour of prone ventilation for both short‐term (0.72) and longer‐term mortality (0.73), which was statistically significant for longer‐term mortality only (P value = 0.02). For longer‐term mortality, this analysis also utilized the Voggenreiter 2005 study, which, although initiated before publication of the ARDS Network study (ARDS Network 2000), states it employed a low tidal volume lung‐protective strategy. The quality of the evidence was rated as moderate according to the GRADE structure (summary of findings Table 1). Analysis of more than 1200 participants ventilated with higher tidal volumes demonstrated modest or little benefit, with a risk ratio of 0.97 for longer‐term mortality. As use of higher tidal volumes is no longer recommended because of the propensity of this approach to cause ventilator‐induced lung injury (Slutsky 2013), some may consider these older trials that pre‐date lung‐protective ventilation to have very limited relevance to current clinical practice. Notably, only the most recent study (Guerin 2013) truly employed an evidence‐based low tidal volume lung‐protective ventilation strategy (ARDS Network 2000), which is now considered a standard of care by many (Needham 2012). Guerin (Guerin 2013) reported a mean tidal volume of 6.1 mL/kg ideal body weight (95% CI 4.9 to 7.3). For all other studies, the 95% CI breached the 8 mL/kg ideal body weight upper limit for "lung‐protective ventilation" (Characteristics of included studies), and a substantial proportion of participants in studies identified as having received "lung‐protective ventilation" will not have achieved this if reported data were normally distributed.
Aetiology of hypoxaemia
Many aetiologies of hypoxaemia have been identified in ICU populations. Some involve specific treatments and may be effectively and rapidly reversible with non‐ventilatory treatments such as diuretics or haemofiltration for fluid overload and pulmonary oedema. A major group of conditions collectively labelled as acute respiratory distress syndrome (ARDS) (Walkey 2012; Matthay 2019) are of particular interest to intensivists and warrant separate exploration. Acute lung injury, recently re‐termed 'mild ARDS' (ARDS definition workforce 2012), is a less severe form of ARDS, is less threatening to life and is less of an immediate concern for intensive care physicians compared with ARDS (Walkey 2012; ARDS definition workforce 2012).
Only one study of 791 participants included a large proportion of participants with conditions other than ARDS or ALI (Guerin 2004). Outcomes of participants from this clinical trial (Guerin 2004) became available in a recent systematic review (Sud 2014), providing more than 1700 participants for analysis of longer‐term outcomes, but these results changed little overall. The subgroup of participants with predominantly ARDS or ALI (mild ARDS) demonstrated risk ratios of 0.79 and 0.82 (P values = 0.05 and 0.07). This compares with analyses of all‐comers with hypoxaemia who had risk ratios of 0.84 and 0.86 for short‐ and longer‐term mortality. The quality of the evidence was rated as moderate in accordance with the GRADE structure (summary of findings Table 1).
The first study conducted by Guerin et al also reported a high rate (32%) of cross‐over (Guerin 2004; Sud 2008), and removal of this trial on the basis of inclusion of patients without ARDS serves as a sensitivity analysis for excessive cross‐overs ‐ that is, removal from the above analysis also results in exclusion of the only study with a very large cross‐over population.
Overall completeness and applicability of evidence
Primary outcomes analyses of all available studies provides only weak evidence of benefit for application of prone ventilation to all‐comers with hypoxaemic failure who met trial entry criteria in the included studies. Evidence suggests that targeted application to certain subgroups would be appropriate.
The most recently published study (Guerin 2013) has had a large impact on overall results and interpretation of the impact of prone ventilation on primary analyses and subgroup analyses for that intervention. This study investigated the effectiveness of prone ventilation in what would be a population subset of most of the other cited studies (more severe hypoxaemia as a fundamental trial entry criterion). In the study of Guerin et al (Guerin 2013), mortality was approximately halved, which is extraordinary for any medical intervention. The accompanying editorial for this study noted, "The 28‐day mortality with prone ventilation was halved (16.0% vs. 32.8% with supine ventilation, P<0.001), a treatment effect virtually unprecedented in modern medicine" ‐ (Soo Hoo 2013). Consequently, this single study has had a large impact on overall effect size and on assessment of heterogeneity in this systematic review.
Additionally, many studies (Gattinoni 2001; Guerin 2004; Leal 1997; Mancebo 2006) were conducted in an era before lung‐protective ventilation became a standard of practice, thus reducing external validity; results of those studies are likely to be very limited in relation to current practice. Restriction to studies that employed a more lung‐protective strategy with means of 6 to 8 mL/kg tidal volume did result in a risk ratio point estimate of 0.71 for longer‐term mortality, which was statistically significant (P value = 0.05). The study of Voggenreiter et al (Voggenreiter 2005) was also conducted (1999‐2001) before low tidal volume became a standard of care in clinical trials but the text indicates they used a low tidal volume strategy even before the low‐tidal volume era.
The intervention of prone positioning would involve very low cost with adequate staffing (or equipment) to safely turn patients from the supine to the prone position and back again, as required. If the intervention was effective with regards to patient‐centred outcomes, this would almost certainly be translated into an intervention that was also cost‐effective, provided that complications for patients and long‐term injuries to staff from additional lifting of patients did not occur. Cost‐effectiveness data and modelling or other economic data based on more than one study are currently not available.
One subgroup analysis that requires specific mention is the analysis of mortality of patients with severe hypoxaemia. For short‐term mortality in six studies of 744 participants (Gattinoni 2001; Guerin 2004; Guerin 2013; Leal 1997; Mancebo 2006; Taccone 2009), the risk ratio was 0.80 (95% CI 0.68 to 0.93; P value = 0.003) in favour of prone positioning with a fixed‐effect model. For longer‐term mortality, seven studies of 977 participants (Chan 2007; Fernandez 2008; Gattinoni 2001; Guerin 2004; Guerin 2013; Mancebo 2006; Taccone 2009) also demonstrated a risk ratio in favour of prone positioning of 0.77 (95% CI 0.70 to 0.95; P value = 0.003) using a random‐effects model. Although the quality of the evidence was rated as moderate according to the GRADE structure (summary of findings Table 1), findings appear consistent in that the most recent trial (Guerin 2013), which focuses on participants with more severe hypoxaemia, on its own has shown a remarkable survival advantage for participants. This subgroup meta‐analysis with the study included is highly statistically significant, and the subgroup meta‐analysis remains significant when this recent study is removed from the analysis. The subgroup exploration fully supports the conclusions of the most recent randomized controlled trial (Guerin 2013) and adds support to use of prone position ventilation in this specific patient population.
This systematic review found no important signal of benefit among participants recruited after 48 hours upon meeting entry criteria and ventilated prone for less than 16 hours per day, nor among those ventilated with higher tidal volumes or among those with milder hypoxaemia. An earlier systematic review (Sud 2010) also suggested no benefit for patients with moderate hypoxaemia only.
Quality of the evidence
With regards to the primary outcome of mortality, eight studies (Chan 2007; Fernandez 2008; Gattinoni 2001; Guerin 2004; Guerin 2013; Leal 1997; Mancebo 2006; Taccone 2009) were available for short‐term mortality, and eight studies (Chan 2007; Fernandez 2008; Gattinoni 2001; Guerin 2004; Guerin 2013; Mancebo 2006; Taccone 2009; Voggenreiter 2005) were available for longer‐term mortality. Each analysis included data from more than 2100 participants, and internal validity of results must be considered good in that regard. Clinical diversity and methodological diversity (for some outcomes at least) may have contributed to statistical heterogeneity as assessed by the Higgins (I2 statistical) method.
The trials were not fully blinded, and some bias would seem inevitable. With regards to bias, Cummings et al state (Cummings 2013), "In a randomized trial blinding is as important as randomization. Randomization minimises the effects of confounding variables at the time of randomization but has no impact on differences that develop between groups during follow‐up. Blinding minimizes post‐randomization sources of bias such as co‐interventions and biased outcome ascertainment and adjudication". Jadad and Enkin consider, "... that the control of bias is the reason d' êtrefor clinical trials and accept control of bias is the most important factor in diminishing inevitable error." (Jadad 2007).
We rated all studies to be at risk of bias in at least one domain (performance bias): all primary studies had at least one risk, as it would be difficult to blind participants, carers and carer‐researchers from their treatment allocation (face‐up or face‐down). Although actual assessment of alive or dead could not be affected (Guyatt 2011a), end‐of‐life practices are universal but varied and poorly delineated clinically within and between ICUs. End of life practices were not standardized in the included trials in a fashion to minimise such bias by carers as well as trialists. The decision to continue with active management for individual participants or to actively withdraw life‐sustaining treatments, or to move to non‐escalation of treatment (Morgan 2014; Turnbull 2014) is perhaps the most fundamental decision / intervention made in ICU. Differential employment of these or other co‐interventions for trial participants, could be influenced by personal views. It is our assessment that some level of bias with regards to patient management is highly probable at various levels in all included studies. Centres were not chosen at random, but rather by interest in this topic: An early study (Gattinoni 2001) was terminated "largely [because of] an increasing unwillingness among caregivers to forgo the use of prone positioning". Another study (Guerin 2013) stated, "Patients were recruited from 26 ICUs in France and 1 in Spain, all of which have used prone positioning in daily practice for more than 5 years". Unblinded trials are associated with exaggerated estimates of effect (Forbes 2013; Karanicolas 2010; Psaty 2010), and, although outcomes such as death are usually considered as relatively immune to bias, we believe this is not the case in intensive care, where mortality is high over a short time frame and death often is not directly related to hypoxaemia (Stapleton 2005; Turnbull 2014) but to active withholding or withdrawal of care. Of note Ferrand found that "In France, there are no guidelines available on withholding and withdrawal of life‐sustaining treatments, and information on the frequency of such decisions is scarce", (Ferrand 2001). More recent studies also document the similar issues (Ay 2020; Gristina 2018; Mark 2015). It is surprising that important potential bias has been overlooked, disregarded or dismissed by some contributors. For example, in the Scandinavian clinical practice guideline on mechanical ventilation in adults with the acute respiratory distress syndrome with regards to downgrading GRADE ratings they state, "In keeping with the GRADE methodology, the quality of evidence for an intervention (i.e. our confidence in the effect estimates) was rated down for identified risks of bias (e.g. due to lack of blinding...)... Importantly, however, when the outcome in question was death at any stage, we did not downgrade evidence due to lack of blinded outcome assessment."(Claesson 2015). Aoyama and colleagues (Aoyama 2019) adopted a similar approach, "For performance and detection bias domains, we judged that, because mortality is objective it was unlikely to be influenced by lack of blinding....". Others (Griffiths 2019) disagree with that view and identify serious risk of bias also stating, "All trials demonstrated performance bias, because of the impossibility of blinding patients and carers with respect to the intervention. All trials also demonstrated detection bias, where outcome assessors were not blinded to intervention allocation".
Our GRADE assessment of quality of evidence for the primary outcomes of this systematic review was rated weak on the basis of bias (as discussed above) (Guyatt 2011a) and inconsistency (Guyatt 2011c). The Cochrane risk of bias assessment indicated that one trial had three different risks (Chan 2007) and two primary trials had two different risks (Guerin 2004; Voggenreiter 2005). These trials were subjected to a sensitivity analysis.
A small post hoc subgroup of 187 participants from one study (Chiumello 2012) allowed analysis of results at 12 months, which showed no signal of benefit for the prone position and so was inconsistent with the primary outcome measures. The quality of evidence for secondary outcomes and subgroup analyses varied in terms of numbers of participants available for analysis (113 to 1350) and quality of measurement, aspects of which have been mentioned in the secondary outcomes and subgroup analysis sections of the Discussion. Subgroups may not be independent, and this underscores the need to consider most as hypothesis‐generating only in this study‐level meta‐analysis e.g. Subgroups with the worst hypoxaemia will have the highest levels of PEEP, an analysis of one will be inextricably linked to the other and the analyses cannot be considered as independent.
Removal of the Voggenreiter study (Voggenreiter 2005) from our meta‐analysis as part of a sensitivity analysis, which did include a higher proportion of participants with acute lung injury (mild ARDS) and yielded a threefold higher rate of transfusion in the supine group as well as increased usage of neuromuscular blockers among participants treated prone, made little difference to this analysis. Also with regards to change in trial findings over time, the discrepancy between study initiation or completion and study publication was not constant. The time lag between study start (a surrogate of final trial protocol) and publication of results varied between five and eight years for published studies in this review. Time lag from study completion to publication varied from one to four years. Publication date may not be of greatest relevance for tagging studies with regards to the start of the lung‐protective ventilation era and may lead to incorrect data interpretation. The study of Voggenreiter 2005, although commenced in 1999 and completed in 2001, actually started using lung‐protective ventilation before the influential ARDS Network study was published (ARDS Network 2000).
Potential biases in the review process
We believe that the likelihood of bias in the review process of evaluated material is low. Processes used to identify relevant studies included in this review have been supplemented by several high‐quality systematic reviews, which also have involved nearly all of the key trialists. Therefore, it is likely that all relevant studies up to 1st May 2020 were identified. Adherence to most prespecified study inclusion and exclusion criteria in the protocol stage was maintained in the review stage. The cutoff in one subgroup analysis (long‐duration prone positioning) was changed by two hours from 18 hours per day to 16 hours per day post hoc in an effort to allocate and analyse the last published study (Guerin 2013) in the most biologically plausible manner consistent with the original protocol. Ecological fallacy or bias cannot be excluded in a study‐level systematic review of participant subgroups (Porta 2008; Reade 2008).
Agreements and disagreements with other studies or reviews
At least 21 other systematic reviews of prone ventilation have been published and been considered in this review (Abroug 2008; Abroug 2011; Alsaghir 2008; Aoyama 2019; Ball 1999; Beitler 2014; Chang 2014; Curley 1999; Du 2018; Gattinoni 2010; Hu 2014; Kopterides 2009; Lee 2014; Mora‐Arteaga 2015; Munshi 2017; Park 2015; Sud 2008; Sud 2010; Sud 2014Tiruvoipati 2008; Yue 2017). Eleven have been published as full papers since the last major and influential clinical trial of Guerin et al (Guerin 2013). In addition we identified recent abstracts which did not contain additional data (Sim 2014; Sud 2011a; Tabula 2015; Yankech 2017). We also identified one selective overview of systematic reviews which examined seven recent systematic reviews (Dalmedico 2017).
The primary studies the systematic reviews include are tabulated, Figure 5 . None of the 19 other meta‐analyses appear to have published protocols pre‐specifying their approach to data collection, management and analysis, which, since 2009, is a preferred option according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta‐Analyses) statement (Moher 2009), with the possible exception of Sud 2014. Publication of protocols which to some extent protects from the consequences of data dredging, is an important safeguard and is an integral part of Cochrane Systematic Reviews.
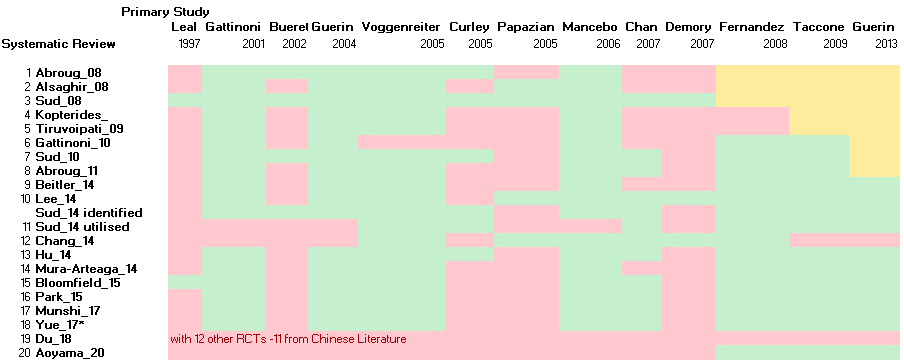
Primary RCTs incorporated in various published Systematic Reviews.
Green denotes primary study was incorporated; Pink denotes primary study was not utilised; Yellow denotes primary study was not available to reviewers. *Yue_17 also included non‐RCT.
Three systematic reviews (Gattinoni 2010; Sud 2010; Sud 2014) are extensively represented by authors of primary studies: In the systematic reviews of Sud et al (Sud 2010; Sud 2014), 13 of 17 listed review authors represent 10 of the 13 primary studies with mortality data. In the systematic review of Gattinoni (Gattinoni 2010), five of six review authors represent the four primary studies included in those analyses. In the recent systematic review of Munshi et al (Munshi 2017) Mancebo and Pesenti are co‐authors so several influential systematic reviews are authored by primary study investigators. Although benefits regarding data clarification and of cooperation are evident, independence and potential conflict of interest issues must also be considered in assessment of these systematic reviews.
The earliest systematic reviews we identified (Ball 1999; Curley 1999) did not contain meta‐analyses and pre‐dated the seminal outcome trial conducted by Gattinoni and colleagues (Gattinoni 2001).
Some subsequent systematic reviews (Abroug 2008; Alsaghir 2008; Curley 1999; Gattinoni 2010; Kopterides 2009; Sud 2008; Tiruvoipati 2008) did not include the two most recent trials (Guerin 2013; Taccone 2009) and despite some valuable insights are now less relevant in terms of both current clinical practice and volume of appropriate data for analysis. Inclusion criteria have differed between reviews, and those with larger numbers of studies have not included exactly the same studies for analyses, even analyses carried out by the same group (Figure 5). For example, Abroug et al included the study of Curley 2005 in one meta‐analysis (Abroug 2008) but not in their updated review (Abroug 2011). In this regard, two of the most recent reviews (Beitler 2014; Lee 2014) identified different numbers of studies for analysis: One (Beitler 2014) identified seven primary studies only and split one study into two to achieve eight data sets for their subgroup meta‐analysis; the other (Lee 2014) identified 11 studies for inclusion in their analyses. Two of the analyses of Sud et al included 10 of 13 primary studies with mortality data (Sud 2010; Sud 2014), but review authors excluded three studies from their original systematic review (Sud 2008). In their most recent review, the review authors state, "Reviewers were in total agreement about the included studies"; however, reviewers were authors of 10 of 11 of the included primary investigations (Sud 2014).
Our systematic review specified at the protocol stage which studies would be included and which excluded; resulting in fewer studies for analysis compared with some of the reviews mentioned above (Bloomfield 2009). In particular, our review consisted of adult participants receiving conventional mechanical ventilation as treatment for hypoxaemia. Thus trials that studied children, prevention and non‐conventional modes of ventilation were not considered for inclusion, and this largely accounts for the differences in numbers of participants studied in primary, secondary and subgroup analyses. Our review did include the small study of Leal (Leal 1997) which had only been included in one other systematic review (Sud 2008) as it met our pre‐specified inclusion criteria. Different studies have also provided different analyses. For example, in this systematic review, mortality was partitioned into short‐term mortality, longer‐term mortality and post hoc to 12‐month mortality. Other reviews have aggregated the latest available data for mortality and have not split data into short‐term and longer‐term categories (Sud 2010). This has resulted in the advantages of increasing numbers of studies and participants available for analysis but obscures where any advantages for participants lie: longer‐term mortality may be of greater relevance to participants (and patient‐centred) than short‐term‐mortality if "short‐term" still equates to being on a ventilator, or still requiring ICU care with the associated discomfort, invasive procedures and clinical burden that it entails. Nevertheless, the primary outcomes of this systematic review are in agreement with most other systematic reviews on this topic ‐ analysis of all studies fails to demonstrate unequivocal benefit for all participants with acute respiratory failure in terms of short‐ or longer‐term mortality. It also is consistent with all reviews in finding that oxygenation is improved and pressure ulcers/sores are increased (Sud 2010). This systematic review (Sud 2010) used data provided by the original investigators in many of the original trials and included many as co‐review authors: their report provided data (from last follow‐up) on participants with severe hypoxaemia and moderate (or less severe) hypoxaemia. These data indicate that participants with moderate hypoxaemia only, did not appear to benefit from prone ventilation, with a risk ratio 1.07 (95% CI 0.93 to 1.22; P value = 0.36) in favour of supine ventilation, which is consistent with the risk ratio of 1.06 obtained in our analysis.
One published systematic review (Abroug 2011) reached some conclusions that differed from the findings of our review. They concluded that no increase occurs in airway complications related to the prone position. However, we found an increase in airway obstruction, as did Sud et al (Sud 2010), and clinicians should be aware of this potentially serious problem. In this regard, we found a risk ratio of 1.78 in favour of the supine position (P value = 0.003) when using a random‐effects model for analysis. Analysing data from four studies only, Sud et al observed a statistically significant mortality benefit in a subgroup of studies enrolling ARDS participants only. They excluded the study of Gattinoni (Gattinoni 2001), although nearly 95% of participants in that study met ARDS criteria. Only with publication of the most recent study (Guerin 2013) could we identify any strong signal of support, and this study included only participants with more severe ARDS. Even with inclusion of this study, statistical significance was not achieved for longer‐term mortality in our analysis.
Early systematic reviews (Abroug 2008; Alsaghir 2008; Kopterides 2009; Sud 2008; Tiruvoipati 2008) generally considered the totality of evidence for prone positioning, but more recent aggregate‐level systematic reviews (Abroug 2011; Beitler 2014; Hu 2014; Munshi 2017; Park 2015; Sud 2010; Sud 2014) have focused on particular subgroups of patients and therefore are potentially subject to the problem of ecological fallacy as well as other biases eg data‐dredging bias (Jadad 2007) and limitations of subgroup analysis which means they should be considered as "entirely observational in their nature" (Borenstein 2019; Deeks 2019) and preclude causal inference.
We have evaluated three recent systematic reviews (Beitler 2014; Lee 2014; Sud 2014), which include the most recent clinical trial of Guerin and colleagues (Guerin 2013).
One review (Lee 2014) focusing on ARDS included studies that we specifically excluded (Beuret 2002; Demory 2007; Papazian 2005) for reasons listed in the Characteristics of excluded studies section. Inclusion of these studies reduced statistical heterogeneity but increased clinical diversity in the meta‐analysis (Bloomfield 2014). The former effect resulted in a statistically significant result for their primary analysis but we remain sceptical that inclusion of these three primary studies is justified on scientific grounds (Bloomfield 2014). Our published protocol specifically excluded such studies a priori. The immense influence of the PROSEVA study (Guerin 2013) was not highlighted. Review authors also rated the risk of bias from lack of blinding of participants and personnel as low, in contrast to our rating of such bias as discussed earlier. Further, they excluded Gattinoni et al (Gattinoni 2001) from their ARDS analysis, although nearly 95% of participants in that study met ARDS criteria (Bloomfield 2014). This meta‐analysis has drawn criticism from other workers similar to the criticisms described above (Iftikhar 2015).
The second systematic review (Beitler 2014), which focused on ARDS in the low tidal volume era, did not include the small study of Chan (Chan 2007), listing it as an observational study without a clearly defined control group, nor that of Leal (Leal 1997). This review explored reasons for heterogeneity but did not address the consistent and most important determinant of heterogeneity in this regard ‐ results from the PROSEVA study of Guerin et al (Guerin 2013). Review authors split the data from one trial (Taccone 2009) into two groups for their analysis, which we consider methodologically problematic. In this last regard, application of mechanical ventilation to more severely ill participants will almost inevitably lead to reduced mechanical ventilation tidal volumes (which was their justification for splitting one trial into two), as clinicians strive to reduce mean and peak ventilatory pressures, even though the two subgroups form one study sharing a single protocol over one study epoch. Their exploration of heterogeneity is puzzling in that almost unprecedented effect size of the PROSEVA trial (Guerin 2013) is not discussed at all (Soo Hoo 2013; Tekwani 2014; Tonelli 2014).
Sud and colleagues (Sud 2014) have updated their original meta‐analysis and have adopted a restrictive approach with regards to study selection for their primary analysis focused on ARDS. This review identified 11 studies, of which only six were used for the primary analysis. Thirteen of the 17 authors of this review contributed to 10 of the original studies, and they selected 11 for inclusion in their study‐level meta‐analysis. The primary analysis was restricted to a subset of studies describing participants with a diagnosis of ARDS and was further restricted to those receiving low tidal volume ventilation. Review authors included studies specifically excluded in this review (Beuret 2002; Curley 2005; Watanabe 2002) for reasons already described (Characteristics of excluded studies). Only one was used in the primary analysis (Curley 2005), which studied a paediatric population with a median age of two years. Review authors rated the quality of findings of their systematic review as high according to the GRADE structure in comparison with our and others (Griffiths 2019) assessment of low quality for our primary analyses and moderate quality for our main subgroup analyses (summary of findings Table 1). A finding of low heterogeneity was emphasized, but no emphasis was placed on the substantial increase since the previous review (Sud 2010), most obviously resulting from inclusion of the most recent trial (Guerin 2013). The classification of heterogeneity is highly subjective, and a variety of ranges are suggested (Deeks 2011; Hatala 2005; Higgins 2003) for low, moderate and high heterogeneity using the I2 approach. We used a more conservative approach and would have rated most of these analyses as demonstrating moderate heterogeneity. Likewise, the GRADE approach to assessment of the quality of evidence is also subjective. We considered the risk of bias to be high, as others have (Griffiths 2019; Park 2015). The inconsistency and increased heterogeneity of results before and after inclusion of the most recent trial (Guerin 2013) could have led to further downgrading of the quality of evidence for this subgroup analysis of participants with an ARDS diagnosis. In this regard, analyses performed before publication of this trial (Guerin 2013) and those that did not include it (nine of 11 analyses) yielded an I2 statistic of 0% for short‐term mortality. For longer‐term mortality, nine of 11 studies also had an I2 statistic = 0, and 10 of 11 had an I2 statistic less than 25%. In contrast, with inclusion of the trial for short‐term mortality, only one of six analyses revealed an I2 statistic = 0 or less than 25%, and for longer‐term mortality, zero analyses of six had an I2 statistic = 0% or less than 25% (i.e. 19 of 22 analyses had zero or low heterogeneity without inclusion of data from Guerin 2013, in contrast to one of 12 analyses with inclusion of these data). With regards to statistical significance, despite increased heterogeneity and increased use of the random‐effects model, the pattern was opposite: A probability value of 0.05 or less was observed in two of the 22 analyses that did not include this influential study but in eight of 12 analyses that included it. The substantial impact of this trial is also apparent upon visual inspection of forest plots for mortality.
Our subgroup analysis results agree in part with the main findings of Sud (Sud 2014), in that longer‐term mortality appears reduced among participants receiving lower tidal volume ventilation (RR 0.73, 95% CI 0.55 to 0.96) and in severely hypoxaemic participants (RR 0.77, 95% CI 0.65 to 0.92), but results for participants with ARDS are only borderline in the analysis (RR 0.85, 95% CI 0.71 to 1.01). All three are only subgroup analyses of the greater body of evidence and in our view show moderate quality when assessed by the GRADE structure.
For this amendment, additional systematic reviews were identified.
Chang (Chang 2014) and colleagues presented a systematic review which incorporated nine randomized or pseudo‐randomized controlled trials and 10 non‐randomized ("comparable cohort / case‐control") studies. It did not identify the recent clinical trials of Taccone et al nor that of Guerin et al nor some older ones and so was not considered further.
Hu and co‐workers also published a systematic review of prone positioning (Hu 2014) and identified eight primary investigation of adult participants and one paediatric study (Figure 5) for their primary outcome of 28‐30 day mortality. An apparent benefit of prone positioning was demonstrated in a subgroup analysis. A proposed benefit of higher positive end‐expiratory pressure (PEEP) in subgroup analyses is doubtful in our view because of primary study misclassification and because of the association of higher PEEP levels with other factors explored in other subgroup analyses. The PROSEVA trial supplement indicates mean PEEP levels below 10cm water (low PEEP category) but appears in the Hu analysis as in the 10‐13cm (high PEEP category). The substantial impact of the PROSEVA trial, exploration of bias and limitations of subgroup analysis are inadequately explored, in our view.
Mora‐Arteaga and colleagues published their systematic review (Mora‐Arteaga 2015) with the primary objective of determining whether ventilation in the prone position reduces mortality in patients with ARDS compared with traditional ventilation in the supine position. With regards to bias assessment they stated, "it was not possible to blind the patients or the treating medical team‐‐‐though we consider that this had no effect upon the results". No basis for this judgement is provided. In the Cochrane Risk of Bias tool all seven primary studies were assessed as having low risk of performance bias (blinding of participants and personnel). They explored multiple sub‐group analyses with stratification and presented results broadly similar to other groups who have also explored the same data. The limitations of subgroup analyses are not highlighted.
Park et al (Park 2015) also published a systematic review with the aim "to evaluate the effects of prone positioning on mortality rates, particularly
with respect to the duration and concurrent use of protective lung strategies". The primary outcome measure was the overall mortality at the longest available follow‐up. Notably, with regards to bias they stated, "Because the prone position with ventilator was always shown and patient progress was explained to the family and patients in the intensive care unit, blinding of participants or outcome measure was not possible. Therefore, there were high selection and detection biases in all included studies ". (Our emphasis). This seems reasonable and we are in agreement but their view contrasts the assessment of nearly all other systematic reviews on this topic. In particular, their Cochrane risk of bias assessment figure is substantially different to that of Mora‐Arteaga et al (Mora‐Arteaga 2015). As with several other systematic reviews on prone positioning they categorised statistical heterogeneity to be low for I2=25‐49%, moderate for I2= 50‐ 74%, and high for I2≥75% and all their analyses are presented as fixed effect models. Notably, the authors requested raw data for all included primary studies, to allow for analysis of subgroups of patients, "however most authors did not respond and one author refused our request". This is unfortunate scientifically, in our opinion, as many primary study authors have previously provided such data for other systematic reviews. Finally although Park et al describe limitations of available evidence they do not specifically discuss the limitations of analysis of multiple subgroup effects.
Munshi et al aimed to determine the effect on mortality (primary outcome) in adults with ARDS in the prone position versus ventilation exclusively in the supine position (Munshi 2017) to inform European and North‐American Societies of Intensive Care formulating mechanical ventilation guidelines (Fan 2017). They considered a study’s overall risk of bias to be high if any domain was judged to be at high risk of bias, with the exception of caregiver blinding, which effectively increased their quality of evidence assessments by GRADE which they rated as moderate to high for their subgroup analyses. In contrast using the same GRADE system we rated the quality of evidence as moderate (due to bias) or low (due to bias and inconsistency) summary of findings Table 1. A recent guideline (Griffiths 2019) generally accords with our GRADE assessments. Many of the primary subgroup analyses of Munshi et al are in broad agreement with our own analyses presented in this Cochrane systematic review. For one subgroup analysis exploring moderate to severe ARDS they excluded the Gattinoni study (Gattinoni 2001) even though nearly 95% of participants in that trial met the the criteria for moderate to severe ARDS. In a secondary publication from that trial (Gattinoni 2010) data for severe ARDS was made available to researchers exploring the impact of disease severity. We do not understand why such data was excluded from analysis. In our own analyses of short and longer term mortality using their selected studies, exclusion and inclusion of Gattinoni's RCT (Gattinoni 2001) would change the conclusions that might be made from this particular subgroup analysis and so their conclusions cannot be considered robust. This systematic review (Munshi 2017) also only managed to identify and reference two other systematic reviews (Beitler 2014; Lee 2014) published after the PROSEVA trial, thus failing to identify contributions made by Hu, Sud, Park and Mora‐Arteaga groups (Hu 2014; Sud 2014; Mora‐Arteaga 2015; Park 2015) as well as the earlier version of this Cochrane Systematic Review. Additional insights generated by this review to the understanding of prone positioning seem limited (Møller 2017; Ioannidis 2016) given the systematic reviews listed above. We also consider their assessment of carer‐researcher bias substantially underestimates its potential impact in an ICU setting.The limitations of subgroup analysis (Guyatt 2008a) and the cautions required making inferences from a multiplicity of subgroup analyses (Borenstein 2019; Deeks 2019) are inadequately highlighted in our view.
Yue and co‐workers (Yue 2017) published a cumulative meta‐analysis in Chinese of nine primary English language studies categorised as randomized controlled trials (RCTs). Results of this cumulative meta‐analysis are invalidated by inclusion of an influential study which clearly is not a RCT (Charron 2011).
Du and colleagues (Du 2018) have provided a systematic review of prone positioning predominantly from the Chinese Language literature encompassing all age groups with pneumonia with the primary outcome of interest, oxygenation. They interrogated PubMed, EMBASE, Cochrane Library, Wanfang, VIP, CNKI databases and identified 12 randomized clinical trials in total. They did not identify or include any of the trials used in this or other systematic reviews but their systematic review provided an additional six studies of adult participants (Cao 2014; Li G 2015; Li J 2015; Wang 2015; Yan 2015; Cheng 2016) for potential inclusion in this amended Cochrane systematic review. Ultimately none were suitable for inclusion (Excluded studies). The other trials identified by Du et al were of paediatric populations and therefore not relevant to this review.
Aoyama et al conducted a network meta‐analysis (Aoyama 2019) with three studies only chosen from randomized trials of prone positioning (Fernandez 2008; Guerin 2013; Taccone 2009). They concluded with regard to prone positioning, that "Specifically our study supports the use of prone positioning (i.e. significant reduction of mortality and high ranking).....". With regards to their approach to potential bias they stated, "that for performance and detection of bias domains, we judged that because mortality is objective, that it was unlikely to be influenced by lack of blinding as long as a strict protocol for both groups was provided". As intensive care support is routinely and subjectively withheld or withdrawn by care providers as part of end of life care we remain surprised by such statements and consider this judgement of lack of bias over‐optimistic. We also note that if we had restricted our Cochrane systematic review to these three studies only, clear and unequivocal evidence of benefit would not be apparent despite inclusion of the PROSEVA study (Guerin 2013) which has been described as having "a treatment effect virtually unprecedented in modern medicine" (Soo Hoo 2013). Our post hoc analysis (generated by the study of Aoyama et al) using these three trials only found the mean effect size confidence interval for longer‐term mortality wide 0.73 (95%CI 0.51‐1.03) breaching unity, not statistically significant and so not in concordance with the results of this network meta‐analysis.
Generally in the more recent systematic reviews discussion of bias is largely limited to "publication bias" and tests thereof in contrast to very little consideration of more serious uncontrolled performance bias with lack of blinding of carers (nurses, attending physicians, other therapists, trialists etc). There were wide differences between studies in Risk of Bias Tool assessments and wide discrepancies regarding judged quality of evidence using the GRADE tool. Subgroup analyses were prominent in recent systematic reviews but their limitations (Oxman 2012; Sun 2014) received relatively little attention. Newer techniques that are now recommended by Cochrane (Deeks 2019) for random effects meta‐analyses to provide better effect size estimates (eg HKSJ adjustment IntHout 2014) have not been applied in this interim amendment nor in the systematic reviews listed in this section.
It is worth noting that despite recent contributions incorporating the GRADE (Grading of Recommendations Assessment, Development and Evaluation) methodology (Mustafa 2013) that findings and recommendations based on largely the same data are substantially discordant (Claesson 2015; Fan 2017; Griffiths 2019; Hashimoto 2017) despite apparently transparent defined processes (Packer 2016).

Flow diagram of results from updated search (January 2014 to 1st May 2020)

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Funnel plot of comparison: 1 Mortality, outcome: 1.1 Mortality.

Primary RCTs incorporated in various published Systematic Reviews.
Green denotes primary study was incorporated; Pink denotes primary study was not utilised; Yellow denotes primary study was not available to reviewers. *Yue_17 also included non‐RCT.

Comparison 1: Mortality, Outcome 1: Mortality

Comparison 1: Mortality, Outcome 2: Sub‐group analysis (SGA) of mortality < 16 hours/d prone

Comparison 1: Mortality, Outcome 3: SGA of mortality prone ≥ 16 hours/d

Comparison 1: Mortality, Outcome 4: SGA of mortality: enrolled ≤ 48 hours after entry criteria met/ventilation

Comparison 1: Mortality, Outcome 5: SGA of mortality: enrolled > 48 hours after entry criteria met/ventilation

Comparison 1: Mortality, Outcome 6: SGA of severe hypoxaemia at entry

Comparison 1: Mortality, Outcome 7: SGA of less severe hypoxaemia at entry

Comparison 1: Mortality, Outcome 8: SGA of SAPS II ≤ 49/≥ 50: short‐term mortality

Comparison 1: Mortality, Outcome 9: SGA of low tidal volume (mean 6 to 8 mL/kg IBW)

Comparison 1: Mortality, Outcome 10: SGA of high tidal volume (> 8 mL/kg IBW)

Comparison 1: Mortality, Outcome 11: SGA of ARDS only

Comparison 2: Intervention comparisons and interactions, Outcome 1: Longer duration vs shorter duration of proning: longer‐term mortality

Comparison 2: Intervention comparisons and interactions, Outcome 2: Early enrolment vs later enrolment to intervention: longer‐term mortality

Comparison 2: Intervention comparisons and interactions, Outcome 3: Severe vs less‐severe hypoxaemia: longer‐term mortality

Comparison 2: Intervention comparisons and interactions, Outcome 4: Lower tidal volume (TV) ventilation vs higher TV ventilation: longer‐term mortality

Comparison 3: Pneumonia, Outcome 1: Pneumonia

Comparison 4: Duration of mechanical ventilation, Outcome 1: Duration of mechanical ventilation

Comparison 5: Length of stay (LOS), Outcome 1: ICU LOS

Comparison 6: Mean change in PaO2/FIO2 quotient (mmHg), Outcome 1: Mean increase in PaO2/FIO2 quotient (mmHg) at 7 or 10 days

Comparison 7: Adverse events, Outcome 1: Adverse events
| Mortality: prone position compared with supine for acute respiratory failure in adults requiring mechanical ventilation in intensive care | ||||||
| Patient or population: adults with acute respiratory failure | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Control | Mortality: prone position compared with supine | |||||
| Short‐term mortality (STM) | Study population | RR 0.84 | 2117 | ⊕⊕⊝⊝ | ||
| 383 per 1000 | 322 per 1000 | |||||
| Moderate | ||||||
| 450 per 1000 | 378 per 1000 | |||||
| Longer‐term mortality (LTM) | Study population | RR 0.86 | 2141 | ⊕⊕⊝⊝ | ||
| 470 per 1000 | 404 per 1000 | |||||
| Moderate | ||||||
| 525 per 1000 | 452 per 1000 | |||||
| Subgroup analysis of longer‐term mortality: severe hypoxaemia | Study population | RR 0.77 | 977 | ⊕⊕⊕⊝ | ||
| 547 per 1000 | 421 per 1000 | |||||
| Moderate | ||||||
| 653 per 1000 | 503 per 1000 | |||||
| Subgroup analysis of longer‐term mortality: lower tidal volume ventilation | Study population | RR 0.73 | 911 | ⊕⊕⊕⊝ | ||
| 451 per 1000 | 329 per 1000 | |||||
| Moderate | ||||||
| 523 per 1000 | 382 per 1000 | |||||
| Subgroup analysis of longer‐term mortality: ARDS only | Study population | RR 0.85 | 1758 | ⊕⊕⊕⊝ | ||
| 483 per 1000 | 411 per 1000 | |||||
| Moderate | ||||||
| 522 per 1000 | 444 per 1000 | |||||
| Subgroup analysis of longer‐term mortality: ≥ 16 hours/d prone | Study population | RR 0.77 | 1005 | ⊕⊕⊕⊝ | ||
| 470 per 1000 | 362 per 1000 | |||||
| Moderate | ||||||
| 526 per 1000 | 405 per 1000 | |||||
| Subgroup analysis of longer‐term mortality: enrolment ≤ 48 hours after entry criteria/ventilation | Study population | RR 0.75 | 1024 | ⊕⊕⊕⊝ | ||
| 469 per 1000 | 352 per 1000 | |||||
| Moderate | ||||||
| 523 per 1000 | 392 per 1000 | |||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| aBlinding of participants and carers was not possible. Researchers also may not have been adequately blinded. All analyses were downgraded because of this important potential bias, leading the quality of all subgroup analyses to be rated as moderate | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Mortality Show forest plot | 9 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1.1 Short‐term mortality | 8 | 2117 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.69, 1.02] |
| 1.1.2 Longer‐term mortality | 8 | 2140 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.72, 1.03] |
| 1.2 Sub‐group analysis (SGA) of mortality < 16 hours/d prone Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.2.1 Short‐term mortality | 2 | 1095 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.89, 1.21] |
| 1.2.2 Longer‐term mortality | 3 | 1135 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.92, 1.17] |
| 1.3 SGA of mortality prone ≥ 16 hours/d Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.3.1 Short‐term mortality | 6 | 1022 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.58, 0.93] |
| 1.3.2 Longer‐term mortality prone | 5 | 1005 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.61, 0.99] |
| 1.4 SGA of mortality: enrolled ≤ 48 hours after entry criteria met/ventilation Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.4.1 Short‐term mortality | 5 | 1000 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.56, 0.93] |
| 1.4.2 Longer‐term mortality | 5 | 1024 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.59, 0.94] |
| 1.5 SGA of mortality: enrolled > 48 hours after entry criteria met/ventilation Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.5.1 Short‐term mortality | 3 | 1117 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.89, 1.21] |
| 1.5.2 Longer‐term mortality | 3 | 1116 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.92, 1.17] |
| 1.6 SGA of severe hypoxaemia at entry Show forest plot | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.6.1 Short‐term mortality | 6 | 744 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.70, 0.95] |
| 1.6.2 Longer‐term mortality | 7 | 977 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.65, 0.92] |
| 1.7 SGA of less severe hypoxaemia at entry Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.7.1 Short‐term mortality | 4 | 1095 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.87, 1.21] |
| 1.7.2 Longer‐term mortality | 6 | 1108 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.93, 1.21] |
| 1.8 SGA of SAPS II ≤ 49/≥ 50: short‐term mortality Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.8.1 SAPS II ≤ 49 | 2 | 327 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.45, 1.60] |
| 1.8.2 SAPS II ≥ 50 | 2 | 113 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.25, 1.40] |
| 1.9 SGA of low tidal volume (mean 6 to 8 mL/kg IBW) Show forest plot | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.9.1 Short‐term mortality | 3 | 830 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.43, 1.20] |
| 1.9.2 Longer‐term mortality | 5 | 911 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.55, 0.96] |
| 1.10 SGA of high tidal volume (> 8 mL/kg IBW) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.10.1 Short‐term mortality | 3 | 1231 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.86, 1.14] |
| 1.10.2 Longer‐term mortality | 3 | 1231 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.90, 1.13] |
| 1.11 SGA of ARDS only Show forest plot | 9 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.11.1 Short‐term mortality | 7 | 1326 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.63, 1.00] |
| 1.11.2 Longer‐term mortality | 8 | 1758 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.71, 1.01] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Longer duration vs shorter duration of proning: longer‐term mortality Show forest plot | 8 | 2140 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.73, 1.04] |
| 2.1.1 > 16 hours | 5 | 1005 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.61, 0.99] |
| 2.1.2 ≤ 16 hours prone | 3 | 1135 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.92, 1.18] |
| 2.2 Early enrolment vs later enrolment to intervention: longer‐term mortality Show forest plot | 8 | 2140 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.72, 1.03] |
| 2.2.2 Late enrolment > 48 hours | 3 | 1116 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.92, 1.17] |
| 2.2.3 Early enrolment ≤ 48 hours | 5 | 1024 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.59, 0.94] |
| 2.3 Severe vs less‐severe hypoxaemia: longer‐term mortality Show forest plot | 7 | 2085 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.76, 1.03] |
| 2.3.1 Severe hypoxaemia | 7 | 977 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.65, 0.92] |
| 2.3.2 Less severe hypoxaemia | 6 | 1108 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.92, 1.26] |
| 2.4 Lower tidal volume (TV) ventilation vs higher TV ventilation: longer‐term mortality Show forest plot | 8 | 2183 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.72, 1.01] |
| 2.4.1 Lower TV ‐ mean 6 to 8 mL/kg IBW | 5 | 911 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.55, 0.96] |
| 2.4.2 High TV ‐ mean > 8 mL/kg IBW | 4 | 1272 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.88, 1.12] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Pneumonia Show forest plot | 5 | 1473 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.80, 1.18] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 4.1 Duration of mechanical ventilation Show forest plot | 3 | 871 | Mean Difference (IV, Fixed, 95% CI) | ‐0.47 [‐1.53, 0.59] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 5.1 ICU LOS Show forest plot | 5 | 1775 | Mean Difference (IV, Fixed, 95% CI) | 1.06 [‐1.13, 3.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 6.1 Mean increase in PaO2/FIO2 quotient (mmHg) at 7 or 10 days Show forest plot | 4 | 827 | Mean Difference (IV, Fixed, 95% CI) | 24.03 [13.35, 34.71] |
| 6.1.1 Change data provided | 2 | 268 | Mean Difference (IV, Fixed, 95% CI) | 16.71 [0.11, 33.32] |
| 6.1.2 Calculated change data | 2 | 559 | Mean Difference (IV, Fixed, 95% CI) | 29.19 [15.24, 43.14] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 7.1 Adverse events Show forest plot | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1.1 Pressure ulcers | 4 | 823 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [1.06, 1.48] |
| 7.1.2 Tracheal tube displacement | 8 | 2021 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.85, 1.39] |
| 7.1.3 Tracheal tube obstruction | 3 | 1597 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.72 [1.35, 2.18] |
| 7.1.4 Pneumothorax | 4 | 664 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.65, 2.08] |
| 7.1.5 Arrhythmias | 3 | 642 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.47, 0.87] |

