Preparación vaginal con solución antiséptica antes de la cesárea para la prevención de las infecciones posoperatorias
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Study characteristics | ||
| Methods | RCT | |
| Participants | 218 women randomized (109 in each group) Inclusion: pregnant women scheduled for term elective cesarean section ‐ indications were prior cesarean, abnormal presentation, maternal request, prior cystocele repair or prior perineal tear Exclusion: emergency cesarean, premature ruptured membranes, placenta previa, immunocompromized status Setting: Saudi Arabia | |
| Interventions | Intervention: chlorhexidine 0.25% antiseptic wipes in vagina (3 lots of 10 cm x 10 cm pieces used from apex to introitus including fornices for approximately 1 minute total time) Control: no vaginal cleansing Intention‐to‐treat analysis | |
| Outcomes | Outcomes
| |
| Notes | All outcomes are summed for overall results. Apparently no one with endometritis also had a wound infection. These are not necessarily mutually exclusive. October 2014 to end of December 2015. October 2014 to December 2015 Funding source: not stated Authors' declarations of interest: no conflicts of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple randomization method used |
| Allocation concealment (selection bias) | Unclear risk | No other information was provided beside the use of sealed envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | Vaginal scrub was performed while the surgeon was in the room. |
| Blinding of outcome assessment (detection bias) | Low risk | Clinical care team was blinded to either arm. |
| Incomplete outcome data (attrition bias) | Low risk | 7 in intervention and 11 in control arm lost to follow‐up. Otherwise, complete outcome data |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting. |
| Other bias | Low risk | None |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 226 women randomized (113 in each group) Inclusion: singleton term pregnancy, scheduled elective cesarean section Exclusion: emergency cesarean section, PROM, positive bacterial vaginosis and/or GBS within 2 weeks prior to cesarean section, women with autoimmune disease or immunosuppression (chronic steroid use, diabetes) Setting: single institution, Saudi Arabia | |
| Interventions | Intervention: povidone‐iodine 10% solution on gauze vaginal wash for 1 minute Control: no vaginal wash Intention‐to‐treat: not stated | |
| Outcomes |
| |
| Notes | September 2016 to December 2017 Funding source: stated the authors received no financial support Authors' declaration of interest: no conflict of interest or financial support | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "simple randomization method" Comment: but not stated how sequence was generated |
| Allocation concealment (selection bias) | Low risk | 2 sealed envelopes, women chose the envelope themselves, thus likely low risk of bias |
| Blinding of participants and personnel (performance bias) | High risk | Scrub nurse did vaginal cleansing while surgeons did the abdominal scrub. No mention of participant blinding |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | Number of withdrawals: 7 study, 12 control (8.4%) |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported on |
| Other bias | Low risk | No other sources of bias identified |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 434 women randomized (217 in each group) Inclusion: women undergoing emergency cesarean with labor duration > 6 hours regardless of membrane rupture Exclusion: diabetes, anemia, obstructed labor, any febrile condition Setting: Islamabad, Pakistan | |
| Interventions | Intervention: vaginal cleansing with povidone‐iodine Control: no vaginal cleansing | |
| Outcomes |
| |
| Notes | 1 February 2016 to 31 July 31 2016 Funding source: not stated Author declarations of interest: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Population randomized, but not clearly stated how it was accomplished |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | None |
| Study characteristics | ||
| Methods | Double‐blind quasi‐RCT | |
| Participants | 585 women randomized (294 vaginal preparation, 291 control) Inclusion: women undergoing non‐emergent or laboring cesarean delivery Exclusion: iodine sensitivity, chorioamnionitis, gestational herpes, abnormal vaginal discharge, emergency cesarean (due to fetal distress, placenta previa) Setting: Iran | |
| Interventions | Intervention: 2 lots of 4 x 4 gauze sponges soaked in 10% povidone‐iodine solutions rotated 360 degrees for 30 seconds from vault to introitus Control: no vaginal cleansing Intention‐to‐treat analysis | |
| Outcomes |
| |
| Notes | May 2007 to April 2008 Funding source: not stated Author declarations of interest: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomized, alternating sequence |
| Allocation concealment (selection bias) | High risk | Quasi‐randomized, alternating sequence |
| Blinding of participants and personnel (performance bias) | Low risk | Participants: unclear but stated "double‐blind" |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors blinded ‐ all data reviewed by 1 physician without knowledge of patient assignment |
| Incomplete outcome data (attrition bias) | Low risk | Complete outcome data. 10 withdrawals from intervention group, 7 from control group |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | High risk | Large differences in baseline characteristics ‐ more examinations, longer labor, more preterm, longer surgery, longer duration of PROM in vaginal cleansing group |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 400 women randomized (200 in each group) Inclusion: term singleton pregnancy undergoing elective cesarean delivery Exclusion: allergy to povidon‐iodine, antepartum hemorrhage, and premature rupture of membrane. Also those suffering from diabetes and those on antibiotics or under cortisone treatment were excluded from the study. Setting: single university setting in Babol, Iran | |
| Interventions | Intervention: povidone‐iodine 10% vaginal preparation Control: no vaginal preparation Intention‐to‐treat: not stated | |
| Outcomes |
| |
| Notes | 2013 to 2014 (months not specified) Funding source: not stated Authors' conflict of interest: no conflict of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number table |
| Allocation concealment (selection bias) | Unclear risk | Not specified |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Low risk | Data collected by one of the "researchers, blinded to the allocation" |
| Incomplete outcome data (attrition bias) | Low risk | No attrition noted |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | No other sources of bias identified |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 600 women randomized (299 analyzed in vaginal cleansing, 300 in control group) Inclusion: women undergoing cesarean, > 17 years old without previous history of allergy to iodine, fever before delivery, and vaginal bleeding Exclusion: unknown Setting: Nakhon Pathom Hospital, Thailand Calculated sample size to account for 20% incomplete data was 600 women | |
| Interventions | Intervention: 1% povidone‐iodine vaginal painting before cesarean Control: no vaginal painting Intention‐to‐treat: unknown | |
| Outcomes |
| |
| Notes | Only abstract and data tables in English. Unable to get translated from original. September 2010 to January 2011 Funding source: unknown Authors' declaration of interest: unknown (no translation of those areas of manuscript) From translated methods section | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "random allocation software was used." Comment: This is likely the equivalent to a computer generated list |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | Only 1 woman lost to follow up |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | No other sources of bias identified |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 120 women randomized (41 in povidone‐iodine group, 39 in benzalkonium group, 40 in control group) Inclusion: pregnant women undergoing elective cesarean delivery, no active infection, completion of week 37 of gestation Exclusion: preterm labor, PROM, emergency cesarean, body temperature above 38 °C, severe anemia, allergic reaction to agents Setting: Sanko University, Turkey | |
| Interventions | Intervention group 1: povidone‐iodine vaginal cleansing for 30 seconds Intervention group 2: benzalkonium chloride vaginal cleansing for 30 seconds Control: no vaginal cleansing Intention‐to‐treat analysis | |
| Outcomes |
| |
| Notes | July 2014 to August 2014 Funding source: not stated Author declarations of interest: no conflicts of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple randomization method |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Operating physician applied cleansing agents |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | Complete outcome data, all women were in hospital, so none lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of selective outcome reporting |
| Other bias | Low risk | None |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 160 randomized (80 in each group) Inclusion: 160 women undergoing cesarean delivery Exclusion: medical contraindications to vaginal preparation ‐ emergency cesarean, allergy, placenta previa Setting: University Medical Center in TX, USA | |
| Interventions | Intervention: povidone‐iodine vaginal wash (concentration not specified) Control: saline vaginal wash | |
| Outcomes |
| |
| Notes | March 2000 to July 2001 Funding source: not stated Authors' declarations of interest: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not specified, simply states "randomized into one of two arms" |
| Allocation concealment (selection bias) | Unclear risk | Not specified |
| Blinding of participants and personnel (performance bias) | Low risk | Cleansing done by nurse while providers outside and thus providers were blinded to the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | Outcomes assessors blinded |
| Incomplete outcome data (attrition bias) | Low risk | No incomplete outcome data |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 300 women randomized (155 in vaginal preparation group, 145 in control group) Inclusion: all women undergoing cesarean delivery, age ≥ 18 years Exclusion: emergency cesarean delivery, allergy to iodine Setting: academic medical center in Indiana, USA | |
| Interventions | Intervention: preoperative vaginal cleansing with 1% povidone‐iodine scrubs. 3 sponge sticks soaked in 1% povidone‐iodine in a prepackaged sterile pouch. The vaginal scrub encompassed the vaginal apex to the introitus with attention to the anterior, posterior, and lateral walls including all fornices Control: no preoperative vaginal cleansing Intention‐to‐treat analysis | |
| Outcomes |
| |
| Notes | The trial was stopped early due to difficulty recruiting. September 2006 to January 2009 Funding source: internally funded Author declarations of interest: no conflicts of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number table, replacement randomization |
| Allocation concealment (selection bias) | Low risk | Sequentially‐numbered opaque security envelopes |
| Blinding of participants and personnel (performance bias) | Low risk | Not specifically blinded, but after anesthesia care providers did not necessarily know group |
| Blinding of outcome assessment (detection bias) | Low risk | Outcomes assessor blinded |
| Incomplete outcome data (attrition bias) | Low risk | Appeared to be complete data on all participants |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Unclear risk | Trial stopped early at safety analysis due to difficulty recruiting and effect seen. |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 150 women randomized (50 in each of the three groups) Inclusion: women aged 20 to 40 years, primipara, singleton undergoing an elective cesarean, healthy and free of any medical, infectious, obstetrical and gynecological diseases Exclusion: povidone‐iodine sensitivity, emergency cesarean Setting: single center at Mansoura University Hospital, Egypt | |
| Interventions | 3 groups total: Intervention: vaginal washing with 10% povidone‐iodine solution (n = 50) Control: 1 group had no washing (n = 50), 1 group had vaginal washing with 0.9% saline for 30 seconds (n = 50) Intention‐to‐treat: yes | |
| Outcomes |
| |
| Notes | September 2015 to March 2016 Funding source: not stated Authors' declaration of interest: no conflict of interests | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Used numbered patient' name list. Even ‐ assigned to control (group 1); Odd ‐ assigned to intervention group starting with group 2 then when complete went to the povidone‐iodine group 3 |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated, unlikely blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No apparent participant losses |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | No evidence of other bias |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 328 women randomized (159 in vaginal cleansing group, 161 in control group) Inclusion: all women undergoing elective or emergency cesarean delivery, age ≥ 16 years Exclusion: known allergy to chlorhexidine, receiving intravenous antibiotics for GBS or other suspected infection, enrolled in another RCT aimed to decrease postop surgical site infections Setting: 4 UK maternity units | |
| Interventions | Intervention: chlorhexidine 0.05% vaginal cleansing with a single swab/sponge mounted on a sponge holder soaked in 50 mL of the antiseptic Control: no vaginal wash Intention‐to‐treat analysis stated | |
| Outcomes |
| |
| Notes | 13 November 2017 to 3 March 2018 Funding source: Birmingham Women's and Children's NHS Foundation Trust Authors' declaration of interest: no competing interests | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Secure automated telephone randomization system 24/7 |
| Allocation concealment (selection bias) | Low risk | Central allocation not disclosed or recorded in the notes |
| Blinding of participants and personnel (performance bias) | Low risk | Attempts made to blind the women to the intervention, unable to blind the care providers |
| Blinding of outcome assessment (detection bias) | Low risk | All data collection from maternal notes were blinded, telephone follow‐up by midwife blinded to the group |
| Incomplete outcome data (attrition bias) | Low risk | Planned to recruit 250 women, but abstract says they 320 consented but that only 68% were followed up at the 14 and 30 day telephone interviews. However, medical note data were collected on > 96% of women so likely low risk for the main outcomes. |
| Selective reporting (reporting bias) | Low risk | No evidence of other bias |
| Other bias | Low risk | No evidence of other bias |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 434 women randomized (217 in each group) Inclusion: women undergoing emergency cesarean in labor for more than 6 hours after admission with or without intact membranes Exclusion: gestational diabetes, severe anemia (Hgb < 7), placenta previa on ultrasound, obstructed labor or any preoperative febrile condition | |
| Interventions | Intervention: vaginal cleansing with povidone‐iodine Control: no vaginal cleansing Intention‐to‐treat: not specifically stated | |
| Outcomes |
| |
| Notes | September 2014 to January 2015 Funding source: not stated Authors' conflict of interest: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Low risk | Allocation was not placed in medical record so unlikely outcomes assessor knew allocation |
| Incomplete outcome data (attrition bias) | Low risk | No attrition bias |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported |
| Other bias | Low risk | No evidence of other bias. |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 200 women randomized (100 in each group) Inclusion: women > 18 years of age undergoing cesarean section Exclusion: allergy to iodine solution, bleeding placenta previa Setting: Hyderabad, Pakistan | |
| Interventions | Intervention: 10% pyodine soaked pieces of gauze (3) used for vaginal scrub immediately before cesarean from vaginal apex to introitus with attention to vaginal walls Control: no vaginal cleansing Intention‐to‐treat: unclear | |
| Outcomes |
| |
| Notes | February 2010 to July 2010 Funding source: not stated Author declarations of interest: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stated "randomly assigned" with no other details |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Low risk | Stated that physician evaluating the data was unaware of any woman's participation |
| Incomplete outcome data (attrition bias) | Low risk | Appeared to be complete data on all participants |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias. Poorly defined composite infectious morbidity overall outcome appears to be the sum of endometritis, fever, and wound infection |
| Study characteristics | ||
| Methods | Quasi‐RCT | |
| Participants | 200 women randomized (100 in each group) Inclusion: full term pregnant women, elective cesarean delivery, age 20 to 35 yo Exclusion: women at risk for developing postpartum infection as premature rupture of membranes, diabetes mellitus, anemia, history of post‐cesarean section infection, obstructed labor, or pre‐eclampsia, given history of being allergic to antiseptic cetrimide solutions Setting: single site in Mansoura University, Egypt | |
| Interventions | Intervention: vaginal cleansing with cetrimide solution (diluted 0.5 cc cetrimide and 49.5cc of tap water) before cesarean. Authors note in their publication that cetrimide contains 0.3% chlorhexidine gluconate and 0.3% "Stremed" Control: no vaginal cleansing Intention‐to‐treat: not stated but no mention of women not getting the assigned intervention | |
| Outcomes |
| |
| Notes | May 2014 ‐ August 2014 Quasi‐RCT due to odd and even number assignment Funding source: not stated Author declaration of interest: no conflicts of interest Included in chlorhexidine subgroup due to author note that the solution they used contained chlorhexidine | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | By random assignment …odd numbers were recruited as the intervention group and the even numbers are recruited as control group |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No withdrawals |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | No evidence of other bias. Pilot study of 20 women for feasibility were later excluded from the study sample and not analyzed. |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 397 women randomized (201 in vaginal cleansing group, 196 in control group) Inclusion: women undergoing elective and emergency cesarean delivery at gestational age of ≥ 28 weeks Exclusion: cord prolapse, placenta previa, antepartum hemorrhage of unknown cause, uterine rupture, chorioamnionitis, vulval/vaginal warts, low presenting part making it difficult to perform the intervention, fetal head descent 1/5, known hypersensitivity to povidone‐iodine or related chemicals Setting: referral hospital in Nairobi, Kenya | |
| Interventions | Intervention: preoperative vaginal cleansing with povidone‐iodine (2 lots of 4 x 4 cm gauze sponges soaked in solution) Control: no vaginal cleansing Intention‐to‐treat: yes | |
| Outcomes |
| |
| Notes | Abstract of results, dissertation thesis publication Study timeline for enrollment in appendix: July 2016 to October 2016 Funding source: Kenyatta National Hospital Author declaration of interest: no conflicts of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomization done by investigator with no clinical involvement using computer‐generated random number sequences |
| Allocation concealment (selection bias) | Low risk | Cards in sealed opaque envelopes sequentially numbered |
| Blinding of participants and personnel (performance bias) | Low risk | "single blind" that blinded study participants, did not mention blinding care providers |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded research assistants that collected outcome data |
| Incomplete outcome data (attrition bias) | Low risk | 4 of 397 lost to follow‐up (1%) |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | No evidence of other bias |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 294 women randomized (147 in each group) Inclusion: all women undergoing cesarean section over 18 years of age Exclusion: cesarean section with deeply engaged head, bleeding placenta previa, active genital herpes, or allergy to iodine Setting: single institution, India | |
| Interventions | Intervention: 5% povidone‐iodine vaginal scrub Control: no vaginal scrub Intention‐to‐treat: not stated | |
| Outcomes |
| |
| Notes | January 2013 to July 2014 Funding source: not stated Authors' declaration of interest: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Surgeon and patient not blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | 9 women in intervention group and 11 in the control group lost to follow‐up (6.8%) |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | No other sources of bias identified |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 667 women randomized (332 in vaginal wash group, 335 in control group) Inclusion: > 37 weeks' gestation, emergency or elective cesarean Exclusion: placental abruption, previa, and fever Setting: single state hospital in Turkey | |
| Interventions | Invervention: povidone‐iodine solution 30 seconds vaginal wash Control: no vaginal wash Intention‐to‐treat: not stated | |
| Outcomes |
| |
| Notes | Translated using online document translator from Turkish September 2009 to July 2010 Funding source: not stated Author declarations of interest: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Only states "randomly divided" |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes used |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No withdrawals noted |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | No evidence of other bias |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 498 women randomized (247 in vaginal preparation group, 251 in control group) Inclusion: women admitted and mentally competent to consent for a cesarean delivery Exclusion: medical contraindications to the cleansing ‐ highly emergent cesarean, bleeding placenta previa, allergy to iodine or shellfish, active genital herpes Setting: University of North Carolina Women's Hospital, North Carolina, USA | |
| Interventions | Intervention: 10% povidone‐iodine surgical scrub solution vaginally immediately before cesarean Control: no vaginal cleansing Intention‐to‐treat analysis | |
| Outcomes |
| |
| Notes | Chorioamnionitis participants excluded from analysis May 1996 to September 1998 Funding source: not stated Author declarations of interest: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated, permuted block randomization schedule |
| Allocation concealment (selection bias) | Low risk | Opaque sealed and numbered envelopes taped to abdominal prep packs |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not specifically stated. Cleansing done by residents during routine prep. These may have been the same surgeons who did the surgery and postoperative care. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcomes assessor masked |
| Incomplete outcome data (attrition bias) | Low risk | 3 withdrawals lacked necessary charting information |
| Selective reporting (reporting bias) | High risk | Large number of participants excluded after randomization who had chorioamnionitis (a known risk factor for postoperative infectious morbidity) because their inclusion "distorted the absolute rates of fever and infectious morbidity." That trial states that when the 68 participants with antepartum infection were included, the estimates of effect of vaginal preparation were not meaningfully different. Thus they planned to exclude those participants from reports of outcomes. As this represented 13.5% of the originally randomized sample, however, there is a risk that this introduced selective reporting bias into the trial. |
| Other bias | Low risk | No evidence of other bias |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 1024 women enrolled in the overall trial (508 to vaginal chlorhexidine wash, 516 to placebo/control wash) Inclusion: women admitted for delivery > 24 weeks' gestation Exclusion: contraindications to digital examinations, placenta previa, active herpes, chorioamnionitis before randomization or allergy to chlorhexidine Setting: University of Alabama ‐ Birmingham, USA | |
| Interventions | Intervention: 200 mL irrigation of 0.2% chlorhexidine solution in labor or if a planned cesarean then immediately before surgery Control: 200 mL sterile water placebo solution Intention‐to‐treat analysis | |
| Outcomes |
| |
| Notes | February 1994 to January 1996. 1024 women enrolled and trial designed for vaginal irrigation during labor. Trial did report on 14 women who had elective cesarean before labor and thus just got the irrigation before the procedure, thus qualifying the study for inclusion in the analysis for those 14 women only. Funding source: Agency for Health Care Policy Research Contract DHHS No. 290‐92‐0055 Authors' declarations of interest: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list |
| Allocation concealment (selection bias) | Low risk | Sequentially‐numbered study labels on identical bottles prepared by Investigational Drug Service at the site. |
| Blinding of participants and personnel (performance bias) | Low risk | Active and placebo solutions were clinically indistinguishable. |
| Blinding of outcome assessment (detection bias) | Low risk | Data collection was done before the assignment was known |
| Incomplete outcome data (attrition bias) | Low risk | 10 total withdrawals, allocation not determined |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | No evidence of other bias |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 308 women randomized (142 in vaginal preparation group, 166 in control group) Inclusion: women to undergo non‐emergency cesarean delivery Exclusion: placenta previa, chorioamnionitis Setting: Chicago Lying‐In Hospital, Illinois, USA | |
| Interventions | Intervention: pre‐packaged povidone‐iodine solution (EZ Prep 200, 5%) vaginal preparation for 30 seconds Control: no preoperative vaginal cleansing | |
| Outcomes |
| |
| Notes | November 1997 to March 2000 Funding source: University of Chicago Hospitals Resident Research Fund Authors' declarations of interest: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random digit table |
| Allocation concealment (selection bias) | Low risk | Sequentially‐numbered, opaque, sealed envelopes |
| Blinding of participants and personnel (performance bias) | Low risk | Not stated for participants, but treating providers at the time of fever were unaware of participation status |
| Blinding of outcome assessment (detection bias) | Low risk | Chart reviewer unaware of group |
| Incomplete outcome data (attrition bias) | Unclear risk | Ultimately 92 participants excluded from analysis post‐randomization (400 originally randomized), reasons explained: 33 due to lost envelopes, 6 for violations of inclusion criteria, and 53 because their hospital charts could not be located. Of all the women excluded, 54 were in the vaginal cleansing group and 38 were in the control group. Only outcomes for women for whom all data were available were reported. The large number of women excluded also makes this trial subject to an unclear risk of bias, however as there are no outcome data for the excluded participants, the potential impact is unclear. Unclear if exclusions impacted data |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
| Study characteristics | ||
| Methods | RCT | |
| Participants | 670 women randomized (335 in each group) Inclusion: women undergoing either a scheduled or emergency cesarean delivery Exclusion: umbilical cord prolapse, placenta previa, or known allergy to povidone‐iodine Setting: Istanbul, Turkey | |
| Interventions | Intervention: 30 second vaginal cleansing with 2 prepackaged povidone‐iodine solution‐soaked foam sponges preoperatively performed in conjunction with the abdominal preparation with 2 prepackaged foam sponges that contained the solution, rotated 360 degrees Control: no preoperative vaginal preparation | |
| Outcomes |
| |
| Notes | January 2011 to August 2011 Funding source: not stated Authors' declarations of interest: no conflicts of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Computer generated randomization process." |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes containing random numbers. Assignment based on those numbers |
| Blinding of participants and personnel (performance bias) | High risk | The researchers in the study were not blinded and the assignment was written in the medical record. |
| Blinding of outcome assessment (detection bias) | High risk | The researchers in the study were not blinded and the assignment was written in the medical record. |
| Incomplete outcome data (attrition bias) | Low risk | Only one participant withdrew. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
CDC: Centers for Disease Control and Prevention
CRP: C‐reactive protein
GBS: Group B streptococcal infection
Hb: hemoglobin
NICE: National Institute for Health and Care Excellence
Plt: platelets
PROM: premature rupture of membranes
RCT: randomized controlled trial
WBC: white blood cell
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Study retracted | |
| Wrong comparison ‐ compared vaginal cleansing with iodine versus chlorhexidine | |
| Wrong comparison ‐ compared vaginal cleansing with iodine versus chlorhexidine | |
| Wrong comparison ‐ compared vaginal cleansing with iodine versus chlorhexidine | |
| Wrong comparison ‐ compared vaginal cleansing with iodine versus chlorhexidine | |
| Not all women received surgical prophylactic antibiotics. 79% of 1 group and 85% of the other group received antibiotics and results were not stratified. | |
| Use of vaginal wash during labor | |
| Wrong comparison ‐ compared vaginal cleansing with iodine versus chlorhexidine |
Characteristics of studies awaiting classification [ordered by study ID]
| Methods | RCT |
| Participants | 526 women getting cesarean at term, excluding chorioamnionitis |
| Interventions | Intervention: vaginal irrigation with povidone‐iodine Control: no vaginal preparation |
| Outcomes | Primary: fever (body temperature) |
| Notes | Iranian Clinical Trials Registry record says complete. Emailed study contact 7 December 2017: no response as of September 2019 |
| Methods | RCT |
| Participants | 400 women getting elective cesarean delivery at term, Iran |
| Interventions | Intervention: vaginal washing with 2 gauze with 10% povidone‐iodine for 30 seconds Control: no vaginal preparation |
| Outcomes | Primary: fever, uterine tenderness, tachycardia, foul‐smelling lochia |
| Notes | Iranian Clinical Trials Registry record says complete. Emailed study contact 7 December 2017: no response |
| Methods | RCT |
| Participants | 203 |
| Interventions | Intervention: vaginal wash with chlorhexadine solution prior to cesarean Control: vaginal wash with saline solution |
| Outcomes | Primary: endometritis |
| Notes | ClinicalTrials.gov record says completed. Last update December 9, 2019. Email sent to author in September 2019, no reply |
| Methods | RCT |
| Participants | 30 |
| Interventions | Intervention: vaginal preparation with chlorhexadine‐alcohol Intervention 2: vaginal preparation with povidine‐iodine Control: vaginal preparation with sterile saline |
| Outcomes | Change in bacterial colony counts |
| Notes | ClinicalTrials.gov record states completed (record last updated July 24, 2019) and notes actual study completion date as June 14, 2019. emailed author in September 2019, no reply. |
RCT: randomized controlled trial
Characteristics of ongoing studies [ordered by study ID]
| Study name | Vaginal cleansing before cesarean delivery to reduce infection: a randomized trial |
| Methods | RCT |
| Participants | 608 women undergoing cesarean |
| Interventions | Intervention: vaginal cleansing with 2 sponge sticks soaked in 1% povidone‐iodine Control: no cleansing All will receive standard abdominal cleansing using chlorhexidine or Betadine per provider preference |
| Outcomes | Primary: composite postoperative infectious morbidity up to 30 days ‐ fever, endometritis, infection or abscess, wound complications or infection |
| Starting date | August 2015 |
| Contact information | Lorene Temming, Washington University, St. Louis |
| Notes | Recruitment status is recruiting. Anticipated completion is December 2020. Last update posted July 16, 2019. NCT02495753 |
| Study name | Preoperative vaginal cleansing with povidone‐iodine and the risk of post‐cesarean endometritis |
| Methods | RCT |
| Participants | 306 women undergoing cesarean |
| Interventions | Intervention: vaginal cleansing with 3 gauze pieces soaked in 10% povidone‐iodine from vaginal apex to introitus Control: no vaginal cleansing |
| Outcomes | Primary outcome: post‐cesarean endometritis diagnosed by fever 38.4 °C or greater in first 48 hours with either uterine tenderness, foul smelling lochia or positive C‐reactive protein |
| Starting date | April 2015 |
| Contact information | Amer Ahmed Mahmoud Riad, Ain Shams Maternity Hospital |
| Notes | Listed as recruiting as of February 2016 |
| Study name | Vaginal antimicrobacterial preparation before cesarean section for endometritis prevention |
| Methods | RCT |
| Participants | 1040 women getting a cesarean delivery |
| Interventions | Intervention: vaginal preparation with septal soap before cesarean Control: no vaginal preparation |
| Outcomes | Primary: endometritis |
| Starting date | April 2017, anticipated completion April 2020 |
| Contact information | Hila Ben‐Asher, Rambam Health Care |
| Notes | Not yet recruiting, verified in ClinicalTrials.gov by PI April 2017. Estimated completion date listed as April 30, 2020 |
| Study name | Effect of Vaginal Douching With Betadine Before CS for Prevention of Post Operative Infections |
| Methods | RCT |
| Participants | 1200 |
| Interventions | Intervention: vaginal preparation with betadine douches before cesarean Control: no vaginal preparation |
| Outcomes | Primary: postpartum endometritis |
| Starting date | January 3, 2019, anticipated completion December 2019 |
| Contact information | Ahmed Maged, MD, Cairo University |
| Notes | ClinicalTrials.gov record says recruiting (record last updated July 26, 2019) but estimated completion date is December 2019. Email sent to author (September 13, 2019), no reply. |
| Study name | Preoperative application of chlorhexidine to reduce infection with cesarean section after labor (PRACTICAL) |
| Methods | RCT |
| Participants | 800 women getting a cesarean delivery in labor |
| Interventions | Intervention: 4% chlorhexidine gluconate vaginal scrub prior to cesarean Control: no vaginal cleansing |
| Outcomes | Primary: rate of surgical site infection up to 6 weeks postpartum: composite of wound infection and postpartum endometritis, defined as fever of 100.4 °F or more 24 hours after delivery associated with uterine tenderness and persistent foul‐smelling lochia requiring broad spectrum intravenous antibiotic administration |
| Starting date | March 2018, anticipated completion March 2020 |
| Contact information | Angela Bianco at Icahn School of Medicine at Mount Sinai, New York |
| Notes | Status is 'recruiting' (last update posted March 2, 2020). Estimated completion date is October 2021 |
| Study name | Effectiveness of preoperative vaginal cleansing with povidone‐iodine in post‐caesarean infectious morbidity; a randomized controlled trial |
| Methods | RCT |
| Participants | 180 |
| Interventions | Intervention: vaginal cleansing with 50 ml povidone‐ iodine for 30 seconds Control: no vaginal preparation |
| Outcomes | Post‐cesarean endometritis |
| Starting date | December 1, 2017 anticipated |
| Contact information | Benjamin Ozumba, University of Nigeria |
| Notes | Pan African Clinical Trials Registry record states not yet recruiting Last updated July 5, 2018 Email sent to author (September 2019), no reply |
RCT: randomized controlled trial
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Post‐cesarean endometritis Show forest plot | 20 | 6918 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.29, 0.58] |
| Analysis 1.1  Comparison 1: Vaginal preparation with antiseptic solution before cesarean section versus control (no preparation or saline preparation), Outcome 1: Post‐cesarean endometritis | ||||
| 1.1.1 Iodine‐based solution | 16 | 6197 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.28, 0.60] |
| 1.1.2 Chlorhexidine‐based solution | 4 | 721 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.16, 0.89] |
| 1.2 Postoperative fever Show forest plot | 16 | 6163 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.50, 0.82] |
| Analysis 1.2  Comparison 1: Vaginal preparation with antiseptic solution before cesarean section versus control (no preparation or saline preparation), Outcome 2: Postoperative fever | ||||
| 1.2.1 Iodine‐based solution | 14 | 5763 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.50, 0.87] |
| 1.2.2 Chlorhexidine‐based solution | 2 | 400 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.23, 0.83] |
| 1.3 Postoperative wound infection Show forest plot | 18 | 6385 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.50, 0.77] |
| Analysis 1.3  Comparison 1: Vaginal preparation with antiseptic solution before cesarean section versus control (no preparation or saline preparation), Outcome 3: Postoperative wound infection | ||||
| 1.3.1 Iodine‐based solution | 15 | 5767 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.50, 0.81] |
| 1.3.2 Chlorhexidine‐based solution | 3 | 618 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.31, 0.90] |
| 1.4 Composite wound complication Show forest plot | 2 | 729 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.37, 1.07] |
| Analysis 1.4  Comparison 1: Vaginal preparation with antiseptic solution before cesarean section versus control (no preparation or saline preparation), Outcome 4: Composite wound complication | ||||
| 1.5 Composite wound complication or endometritis Show forest plot | 2 | 499 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.26, 0.82] |
| Analysis 1.5  Comparison 1: Vaginal preparation with antiseptic solution before cesarean section versus control (no preparation or saline preparation), Outcome 5: Composite wound complication or endometritis | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Post‐cesarean endometritis Show forest plot | 7 | 2677 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.27, 0.81] |
| Analysis 2.1  Comparison 2: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of labor, Outcome 1: Post‐cesarean endometritis | ||||
| 2.1.1 Women in labor | 6 | 1634 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.19, 0.67] |
| 2.1.2 Women not in labor | 5 | 1043 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.33, 2.21] |
| 2.2 Postoperative fever Show forest plot | 5 | 2233 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.55, 0.95] |
| Analysis 2.2  Comparison 2: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of labor, Outcome 2: Postoperative fever | ||||
| 2.2.1 Women in labor | 5 | 1415 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.42, 0.87] |
| 2.2.2 Women not in labor | 3 | 818 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.60, 1.43] |
| 2.3 Postoperative wound infection Show forest plot | 5 | 2233 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.37, 0.88] |
| Analysis 2.3  Comparison 2: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of labor, Outcome 3: Postoperative wound infection | ||||
| 2.3.1 Women in labor | 5 | 1415 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.30, 0.90] |
| 2.3.2 Women not in labor | 3 | 818 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.35, 1.31] |
| 2.4 Composite wound complication Show forest plot | 2 | 729 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.38, 1.09] |
| Analysis 2.4  Comparison 2: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of labor, Outcome 4: Composite wound complication | ||||
| 2.4.1 Women in labor | 2 | 314 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.36, 1.61] |
| 2.4.2 Women not in labor | 2 | 415 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.25, 1.16] |
| 2.5 Composite wound complication or endometritis Show forest plot | 2 | 499 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.27, 0.85] |
| Analysis 2.5  Comparison 2: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of labor, Outcome 5: Composite wound complication or endometritis | ||||
| 2.5.1 Women in labor | 2 | 164 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.13, 0.87] |
| 2.5.2 Women not in labor | 2 | 335 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.29, 1.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Post‐cesarean endometritis Show forest plot | 9 | 2634 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.30, 0.55] |
| Analysis 3.1  Comparison 3: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of ruptured membranes, Outcome 1: Post‐cesarean endometritis | ||||
| 3.1.1 Women with ruptured membranes | 5 | 552 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.12, 0.45] |
| 3.1.2 Women with intact membranes | 8 | 2082 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.34, 0.68] |
| 3.2 Postoperative fever Show forest plot | 8 | 2474 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.38, 0.78] |
| Analysis 3.2  Comparison 3: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of ruptured membranes, Outcome 2: Postoperative fever | ||||
| 3.2.1 Women with ruptured membranes | 4 | 480 | Risk Ratio (M‐H, Random, 95% CI) | 0.42 [0.22, 0.80] |
| 3.2.2 Women with intact membranes | 7 | 1994 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.49, 0.99] |
| 3.3 Postoperative wound infection Show forest plot | 9 | 2634 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.47, 0.91] |
| Analysis 3.3  Comparison 3: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of ruptured membranes, Outcome 3: Postoperative wound infection | ||||
| 3.3.1 Women with ruptured membranes | 5 | 552 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.19, 1.50] |
| 3.3.2 Women with intact membranes | 8 | 2082 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.50, 1.07] |
| 3.4 Composite wound complication Show forest plot | 1 | 300 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.28, 1.44] |
| Analysis 3.4  Comparison 3: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of ruptured membranes, Outcome 4: Composite wound complication | ||||
| 3.4.1 Women with ruptured membranes | 1 | 76 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.15, 1.89] |
| 3.4.2 Women with intact membranes | 1 | 224 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.25, 2.10] |
| 3.5 Composite wound complication or endometritis Show forest plot | 2 | 500 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.27, 0.85] |
| Analysis 3.5  Comparison 3: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of ruptured membranes, Outcome 5: Composite wound complication or endometritis | ||||
| 3.5.1 Women with ruptured membranes | 2 | 134 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.39 [0.13, 1.13] |
| 3.5.2 Women with intact membranes | 2 | 366 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.26, 1.04] |
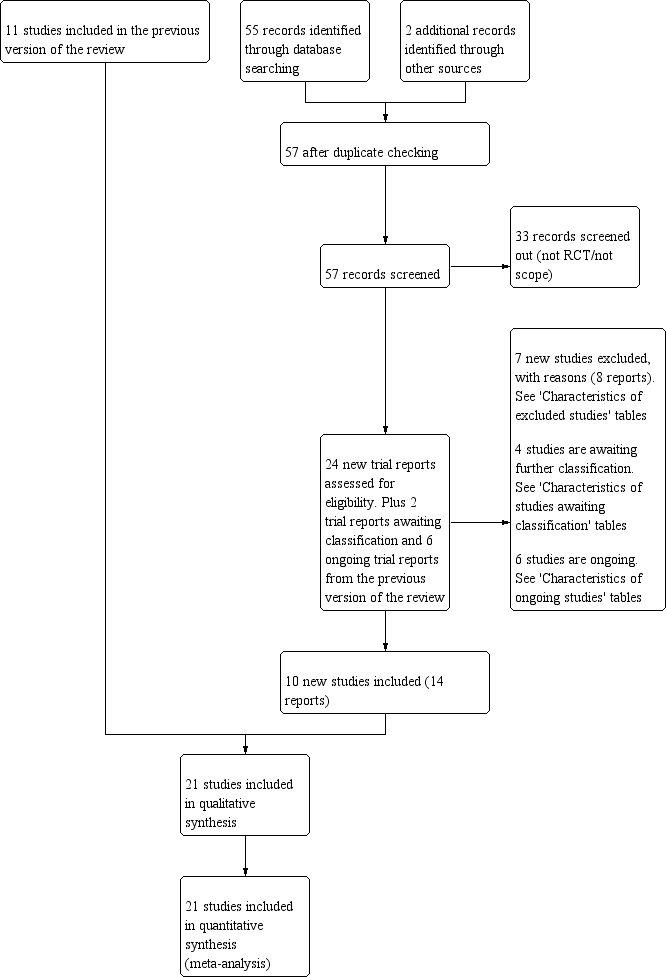
Study flow diagram.

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.

Funnel plot of comparison: 1 Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation), outcome: 1.1 Post‐cesarean endometritis.

Comparison 1: Vaginal preparation with antiseptic solution before cesarean section versus control (no preparation or saline preparation), Outcome 1: Post‐cesarean endometritis

Comparison 1: Vaginal preparation with antiseptic solution before cesarean section versus control (no preparation or saline preparation), Outcome 2: Postoperative fever

Comparison 1: Vaginal preparation with antiseptic solution before cesarean section versus control (no preparation or saline preparation), Outcome 3: Postoperative wound infection

Comparison 1: Vaginal preparation with antiseptic solution before cesarean section versus control (no preparation or saline preparation), Outcome 4: Composite wound complication

Comparison 1: Vaginal preparation with antiseptic solution before cesarean section versus control (no preparation or saline preparation), Outcome 5: Composite wound complication or endometritis

Comparison 2: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of labor, Outcome 1: Post‐cesarean endometritis

Comparison 2: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of labor, Outcome 2: Postoperative fever

Comparison 2: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of labor, Outcome 3: Postoperative wound infection

Comparison 2: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of labor, Outcome 4: Composite wound complication

Comparison 2: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of labor, Outcome 5: Composite wound complication or endometritis

Comparison 3: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of ruptured membranes, Outcome 1: Post‐cesarean endometritis

Comparison 3: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of ruptured membranes, Outcome 2: Postoperative fever

Comparison 3: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of ruptured membranes, Outcome 3: Postoperative wound infection

Comparison 3: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of ruptured membranes, Outcome 4: Composite wound complication

Comparison 3: Vaginal preparation with antiseptic solution versus control (no preparation or saline preparation) ‐ stratified by presence of ruptured membranes, Outcome 5: Composite wound complication or endometritis
| Vaginal preparation with antiseptic solution compared to control (no preparation or saline preparation) for preventing postoperative infections | ||||||
| Patient or population: pregnant women undergoing cesarean section | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with control (no preparation or saline preparation) | Risk with vaginal preparation with antiseptic solution | |||||
| Post‐cesarean endometritis | Study population | RR 0.41 | 6918 | ⊕⊕⊕⊝ | ||
| 72 per 1000 | 30 per 1000 | |||||
| Postoperative fever | Study population | RR 0.64 | 6163 | ⊕⊕⊕⊝ | ||
| 120 per 1000 | 77 per 1000 | |||||
| Postoperative wound infection | Study population | RR 0.62 | 6385 | ⊕⊕⊕⊝ | ||
| 61 per 1000 | 38 per 1000 | |||||
| Composite wound complication or endometritis | Study population | RR 0.46 | 499 | ⊕⊕⊕⊝ | ||
| 135 per 1000 | 62 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aThere is some funnel plot asymmetry. Having conducted sensitivity analyses to investigate the contribution of small studies and studies at high risk of bias, we do not believe that the effect estimate has been biased by possible missing results due to non‐publication. We did not downgrade. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Post‐cesarean endometritis Show forest plot | 20 | 6918 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.29, 0.58] |
| 1.1.1 Iodine‐based solution | 16 | 6197 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.28, 0.60] |
| 1.1.2 Chlorhexidine‐based solution | 4 | 721 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.16, 0.89] |
| 1.2 Postoperative fever Show forest plot | 16 | 6163 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.50, 0.82] |
| 1.2.1 Iodine‐based solution | 14 | 5763 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.50, 0.87] |
| 1.2.2 Chlorhexidine‐based solution | 2 | 400 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.23, 0.83] |
| 1.3 Postoperative wound infection Show forest plot | 18 | 6385 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.50, 0.77] |
| 1.3.1 Iodine‐based solution | 15 | 5767 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.50, 0.81] |
| 1.3.2 Chlorhexidine‐based solution | 3 | 618 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.31, 0.90] |
| 1.4 Composite wound complication Show forest plot | 2 | 729 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.37, 1.07] |
| 1.5 Composite wound complication or endometritis Show forest plot | 2 | 499 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.26, 0.82] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Post‐cesarean endometritis Show forest plot | 7 | 2677 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.27, 0.81] |
| 2.1.1 Women in labor | 6 | 1634 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.19, 0.67] |
| 2.1.2 Women not in labor | 5 | 1043 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.33, 2.21] |
| 2.2 Postoperative fever Show forest plot | 5 | 2233 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.55, 0.95] |
| 2.2.1 Women in labor | 5 | 1415 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.42, 0.87] |
| 2.2.2 Women not in labor | 3 | 818 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.60, 1.43] |
| 2.3 Postoperative wound infection Show forest plot | 5 | 2233 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.37, 0.88] |
| 2.3.1 Women in labor | 5 | 1415 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.30, 0.90] |
| 2.3.2 Women not in labor | 3 | 818 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.35, 1.31] |
| 2.4 Composite wound complication Show forest plot | 2 | 729 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.38, 1.09] |
| 2.4.1 Women in labor | 2 | 314 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.36, 1.61] |
| 2.4.2 Women not in labor | 2 | 415 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.25, 1.16] |
| 2.5 Composite wound complication or endometritis Show forest plot | 2 | 499 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.27, 0.85] |
| 2.5.1 Women in labor | 2 | 164 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.13, 0.87] |
| 2.5.2 Women not in labor | 2 | 335 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.29, 1.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Post‐cesarean endometritis Show forest plot | 9 | 2634 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.30, 0.55] |
| 3.1.1 Women with ruptured membranes | 5 | 552 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.12, 0.45] |
| 3.1.2 Women with intact membranes | 8 | 2082 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.34, 0.68] |
| 3.2 Postoperative fever Show forest plot | 8 | 2474 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.38, 0.78] |
| 3.2.1 Women with ruptured membranes | 4 | 480 | Risk Ratio (M‐H, Random, 95% CI) | 0.42 [0.22, 0.80] |
| 3.2.2 Women with intact membranes | 7 | 1994 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.49, 0.99] |
| 3.3 Postoperative wound infection Show forest plot | 9 | 2634 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.47, 0.91] |
| 3.3.1 Women with ruptured membranes | 5 | 552 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.19, 1.50] |
| 3.3.2 Women with intact membranes | 8 | 2082 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.50, 1.07] |
| 3.4 Composite wound complication Show forest plot | 1 | 300 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.28, 1.44] |
| 3.4.1 Women with ruptured membranes | 1 | 76 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.15, 1.89] |
| 3.4.2 Women with intact membranes | 1 | 224 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.25, 2.10] |
| 3.5 Composite wound complication or endometritis Show forest plot | 2 | 500 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.27, 0.85] |
| 3.5.1 Women with ruptured membranes | 2 | 134 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.39 [0.13, 1.13] |
| 3.5.2 Women with intact membranes | 2 | 366 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.26, 1.04] |

